Summary
Background:
quadriceps tendon subcutaneous rupture is an uncommon injury affecting predominantly middle-aged men as a result of direct or indirect trauma; aim of this work is to evaluate clinical outcome and tendon morphology in patients treated surgically with transpatellar drilling suture.
Methods:
20 patients (20 male) with an average age of 54 (42–59) were evaluated with a mean follow-up of 36 months.
Measurements of range of motion (ROM) and of tight circumference were collected. Lysholm and Rougraff Score were also performed.
All the patients underwent a US evaluation the morphologic changes of the repaired tendon.
Results:
mean active ROM was 1°–117°; average difference in the circumference of the quadriceps was 2.6% 10 C and 3.3% 15 C. The mean Lysholm Score calculated was 88/100; the mean Rougraff Score 17/25.
At ultrasonographic evaluation all tendons were continuous; heterotopic ossification was present in 18 quadriceps tendons. Thickness was augmented in 18 quadriceps tendons and in 5 patellar tendons. Vascularization was always conserved. Lateral subluxation of patella was reported in 1 case.
Conclusions:
patellar drilling holes repair is a non-demanding procedure, inexpensive and technically uncomplicated.
US evaluation confirms tendon healing; tendon remodeling does not affect patient’s clinical outcome and quality of life.
Level of incidence: IV
Keywords: Patellar drilling holes, quadriceps, tendon rupture, ultrasound
Introduction
Quadriceps tendon rupture is an uncommon injury with an incidence of 1.37/100,000 patients per year1. Men are more frequently affected than women (M: F = 4.2:1), and the mean age is around 50 years old1. Fatty and cystic degeneration of tendons, mixed degeneration, microangioblastic dysplasia, decrease in collagen and calcification occurs naturally with aging2 but while these structural changes weaken the structural stability of the tendon, rarely spontaneous rupture is observed even in the elderly3.
Most commonly this injury is the result of direct or indirect trauma. A violent eccentric contraction is the most frequent cause of quadriceps tear rupture4. Spontaneous ruptures, even sometimes bilaterally, have been reported in people with predisposing conditions such as chronic renal failure, rheumatoid arthritis, diabetes, gout and steroids abuse5 or quinolone antibiotics use6.
The patient often describes the traumatic mechanism as a traumatic event while the limb is in hyperextension, followed by a sharp pain in the anterior side of the tight and absolute inability to actively extend the affected knee. Pain is sudden and severe. Testing the knee extended relieves the pain.
At the physical examination a gap in the suprapatellar zone is palpable and effusion might be present. Despite all these obvious signs and symptoms, the rupture of quadriceps tear may be missed. The radiological procedures for the diagnosis are direct radiography, ultrasound (US) and magnetic resonance imaging (MRI)7. The sensitivity of US in determining the localization of the rupture is high. It is also quite sensitive in differentiating complete by partial ruptures. MRI is the most effective imaging method8.
In our series of cases we repaired the lesion with transpatellar drilling suture; we re-evaluated active patients (less than 60 years old and without important comorbidities) with physical examination, functional scores, and US in order to study the effectiveness of this surgical technique and the post-operative recover in this population.
Aim of this work is to study the clinical outcome of a series of quadriceps tendon repaired with patellar drilling holes, and to compare it with Literature. This is the first clinical study evaluating the ultrasonographic changes in the morphology of quadriceps tendon surgically repaired.
Materials and methods
In our study we evaluated 20 patients (20 male) treated in our Institute after the subcutaneous traumatic rupture of the quadriceps tendon from January 2009 to January 2011 with a mean follow-up of 36 months. Data were prospectively collected and retrospectively analyzed.
In this study were included all the patients treated with transpatellar drilling repair after acute quadriceps tear rupture, younger than 60 years. Patients with important comorbidities predisposing to rupture, bilateral simultaneous ruptures, ruptures repaired more than 7 days after the injury and patients that didn’t give the written consent to the evaluation were excluded from this study.
All the patients referred a sudden and fierce pain in the supra patellar region and the inability to actively extend the knee.
All the lesions have been confirmed by using the US, and only in 3 cases the MRI was necessary to confirm the diagnosis (Fig. 1).
Figure 1.
MR image of subcutaneous quadriceps tendon rupture.
All the patients underwent surgery tendon repair with patellar drill holes technique.
All the surgeons performed the repair with the same surgical technique.
In this surgical approach the patient is positioned to permit at least 90° of knee flexion during the procedure. When the tourniquet was used (by choice of the operating surgeon) it has always been deflated before the final suture of the tendon to allow complete tendons lengthen. The surgical technique entails a longitudinal midline incision from the inferior pole of the patella going proximally for 6–7 centimeters.
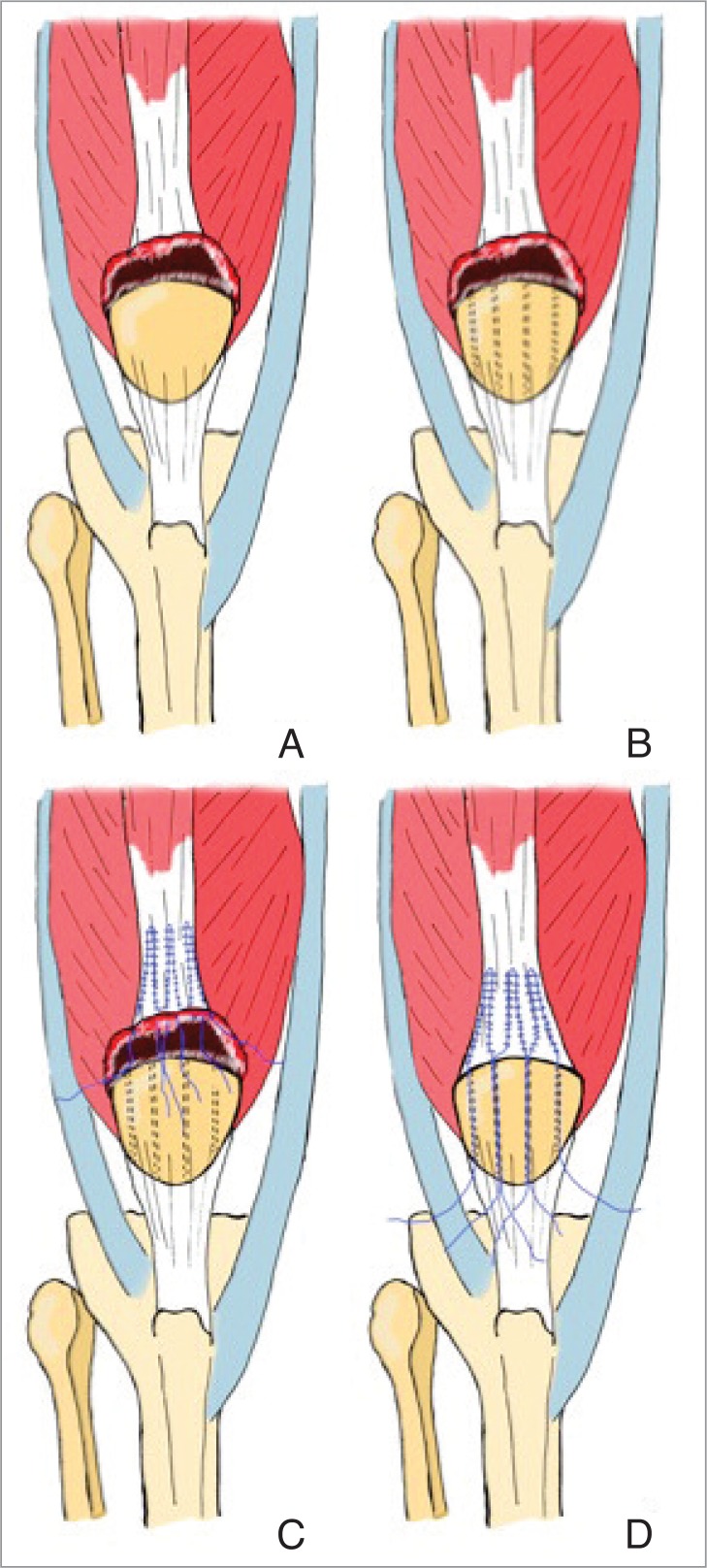
In the proximity of the patellar surface the injured quadriceps tendon was isolated in its proximal and distal insertion (Fig. 2A).
Figure 2.
A–D. A. Quadriceps tendon rupture. B. Patellar drill. C. Krackow chains with absorbable wire in the proximal side of injured tendon. D. The suture chains are passed in the holes.
Using absorbable suture wire (polysorb 0 Covidien©), as described by Krackow, 2 or 3 chains (depending on patella size) were made in the proximal side of the injured tendon (Figs. 2B, 3).
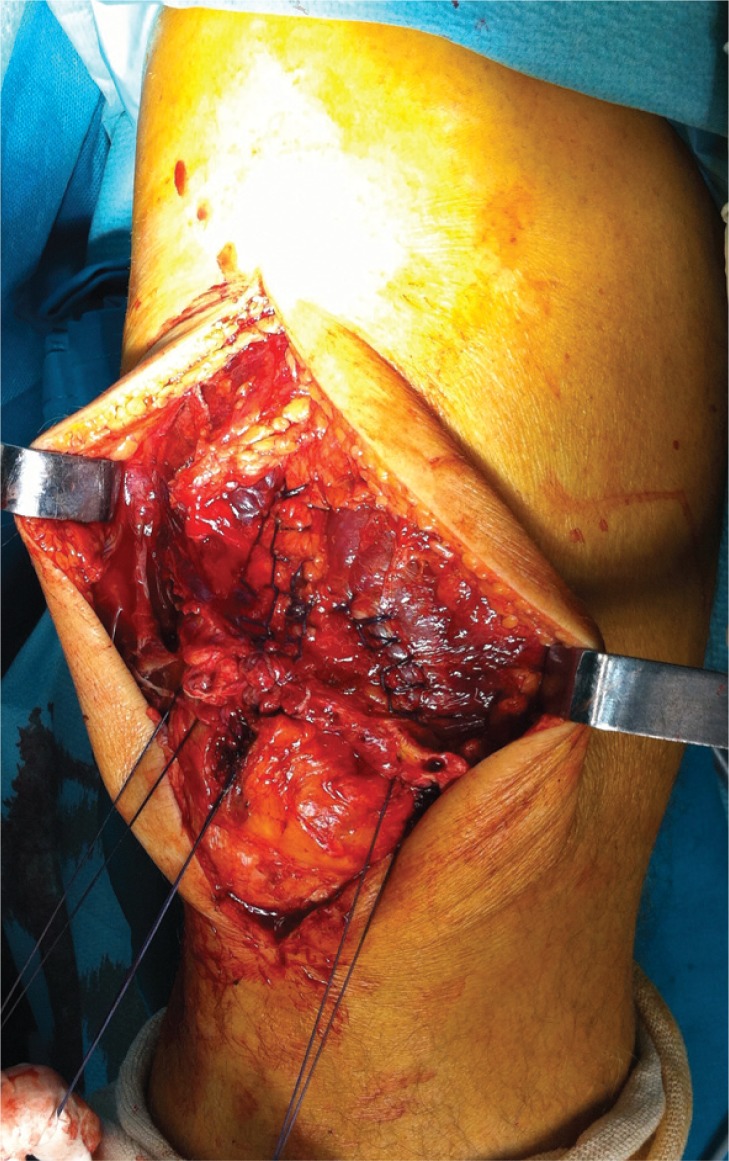
Figure 3.
Intraoperative picture of suture chains.
The second step was drilling 3 or 4 longitudinal holes, with a diameter 2 K-wire, in the patella (Fig. 2C) and to pass the suture chains in the holes (Fig. 2D).
At this point of the procedure the tourniquet, if in use, must be deflated in order to test the tendon with functional tests. Tractioning distally the suture chains, the margins of the lesion must match perfectly with no anatomical gap.
The suture chains are then tied by positioning the knee in maximal extension staying as close as possible to the inferior pole of the patella.
The post-operative treatment consisted of a plaster cast in total extension and then a splint for a total of 30 days; after this period of immobilization, each patient underwent kinesis to regain complete ROM of the knee and quadriceps strength.
Each patient was evaluated studying the ROM with articular goniometer, the muscular tropism with measurements of the thigh circumferences 10 cm (10C) and 15 cm (15C) from the top of the patella (Fig. 4). Lysholm Score9 and Rougraff Score10 were also performed. All the patients underwent a US check, all performed by the same operator, to evaluate:
Tendon quality;
Quadriceps and patellar tendons thickness (comparing with contralateral);
Tendon vascularization;
Presence of heterotopic calcifications;
Patellar tracking.
Figure 4.
10C thigh circumference measurement.
Predictive power of thigh circumferences at 10C and 15C far from the top of patella in terms of clinical outcome and quality of life was investigated, comparing measurements with Lysholm and Rougraff Score with Mann-Whitney test11.
This research has been conducted according to the international standard and as required by the journal12.
Results
Mean age of patients was 54 (42–59); the affected limb was the right one in 12 cases and the left one in 8 cases. The lesion was located at the patellar insertion in 14 cases, at the middle third of the tendon in 6 cases. No ruptures in the myotendinous junction were found. The mean time from injury to surgery was 2.6 days (+−1).
In all patients after the post surgical evaluation the mean active flexion was 117 (+−10)°; the mean active extension is 1° (+−2), all patients re-gained full extension except for 3 who re-gained 5° and 1 that regained 10°. No re-ruptures were registered.
The mean difference of circumference of the quadriceps is 2.6% (+−1.9) 10C far from patella and 3.3% (+−2.1) 15C. No patients had problems of squatting after the reconstruction of the tendon (Tab. 1).
Table 1.
Patients data.
| PATIENT | AGE | SIDE | GENDER | FOLLO-UP | TRAUMA | MAX FLESSION | MAX ESTENSION | 10C | 15C | LYSHOM-KNEE SCORE | ROU–GRAF SCORE |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 59 | R | M | 47 | MOUNTAIN HIKING | 110 | 0 | 2 | 3 | 89 | 6 |
| 2 | 52 | L | M | 45 | MOUNTAIN HIKING | 100 | 0 | 0 | 3 | 86 | 11 |
| 3 | 58 | R | M | 44 | WALKING DOWNHILL | 110 | 5 | 3 | 4 | 89 | 8 |
| 4 | 56 | R | M | 47 | ACCIDENAL FALL | 130 | 0 | 4 | 5 | 100 | 5 |
| 5 | 42 | R | M | 30 | WALKING DOWSTAIRS | 105 | 5 | 2 | 2 | 85 | 6 |
| 6 | 57 | R | M | 36 | MOUNTAIN HIKING | 120 | 0 | 1 | 2 | 89 | 8 |
| 7 | 46 | L | M | 29 | WALKING DOWNHILL | 130 | 0 | 1 | 1 | 98 | 7 |
| 8 | 57 | R | M | 25 | WALKING DOWSTAIRS | 100 | 0 | 5 | 4 | 72 | 12 |
| 9 | 53 | L | M | 29 | MOUNTAIN HIKING | 125 | 0 | 2 | 3 | 88 | 8 |
| 10 | 55 | R | M | 32 | KICKING AN OBJECT | 115 | 0 | 2 | 2 | 83 | 9 |
| 11 | 51 | R | M | 29 | MOUNTAIN HIKING | 115 | 0 | 6 | 9 | 77 | 12 |
| 12 | 55 | L | M | 34 | WALKING DOWSTAIRS | 120 | 0 | 7 | 8 | 100 | 7 |
| 13 | 54 | L | M | 29 | WALKING DOWSTAIRS | 125 | 10 | 2 | 1 | 95 | 5 |
| 14 | 52 | R | M | 32 | SKIING | 125 | 0 | 3 | 2 | 81 | 11 |
| 15 | 49 | R | M | 41 | SKIING | 130 | 0 | 1 | 2 | 100 | 7 |
| 16 | 52 | L | M | 29 | ACCIDENL FALL | 105 | 5 | 4 | 3 | 79 | 10 |
| 17 | 55 | R | M | 32 | MOUNTAIN HIKING | 115 | 0 | 3 | 4 | 85 | 7 |
| 18 | 58 | L | M | 36 | WALKING DOWNHILL | 110 | 0 | 2 | 2 | 88 | 8 |
| 19 | 58 | L | M | 48 | MOUNTAIN HIKING | 125 | 0 | 0 | 3 | 96 | 7 |
| 20 | 53 | R | M | 42 | KICKING AN OBJECT | 130 | 0 | 1 | 3 | 74 | 9 |
Only 1 patient complained pain and 1 complained lack of strength.
2 patients had skin healing delay. No other post-operative complications were reported.
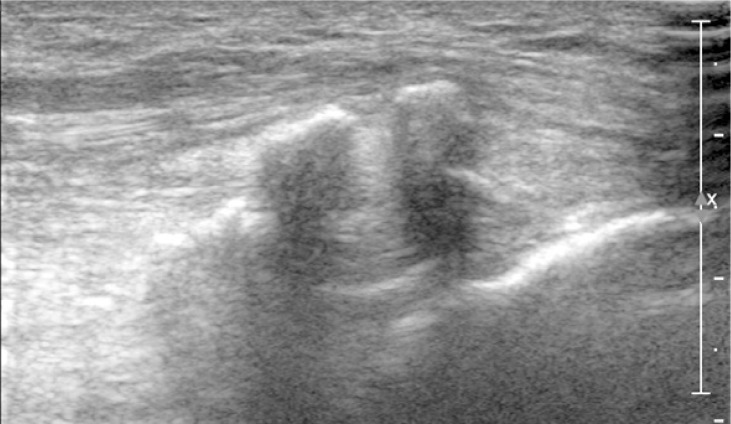
The mean Lysholm Score calculated is 88/100 (+−9). The mean Rougraff Score is 17/25 (+−2) (Tab. 1). The US indicated good healing of the repaired tendon since all of them were continuous; heterotopic ossifications were present in 18 quadriceps tendons (90%) (Fig. 5). Structural inhomogeneity was recorded in 17 patients (85%); vascularization was conserved in 100% of patients. Quadriceps tendon thickness was augmented in 18 cases (90%), and the patellar tendon thickness in 5 cases (20%).
Figure 5.
US view of heterotopic calcifications in repaired tendon.
Lateral subluxation of the patella was observed in 1 case (0,5 cm of tilting in maximal flexion, absent in contralateral knee). Early patella-femoral arthritis was also observed in this case. Patellar tracking was regular in all other patients.
Statistical analysis
Univariate analysis with Mann-Whitney test was performed to investigate the predictive power of the difference in the circumference of quadriceps 10C and 15C for the clinical score and patient quality of life, measured with Lysholm and Rougraff Score.
No statistical significance has been documented with Mann-Whitney test: comparing circumference10C with Lysholm Score p: 0.312 (>0.05); 10C with Rougraff Score p: 0.904 (>0.05); 15C with Lysholm Score p: 0.521 (>0.05); 15C with Rougraff Score p: 0.473 (>0.05).
Discussion
The most represented surgical techniques for quadriceps tendon repair in acute lesions are, as reported by Ciriello et al. in his review13, simple end-to-end sutures and patellar drilling holes10,14–23. Wenzl et al. asserted that the type of repair (direct or trans-osseous suture) had no influence on the final outcome17; Puranik et al. found the best results in patients treated with patellar drill holes, comparing with direct repair (with or without augmentation) 15.
Anchors repair has recently been described by different authors24–26. Biomechanical studies were performed and showed no significant difference between anchor repair and patellar drilling holes technique27. Hart investigated biomechanical differences between trans-osseous equivalent double-row suture anchor and trans-osseous tunnel repair: he reported that both were effective in terms of strength, repair stiffness and gap formation with similar results, but the transosseous repairs were stronger28. Lighthart et al. found no significant differences in terms of displacement after 1000 cycles, adding that suture anchors are more expensive but, as confirmed also by Richards et al.24, Maniscalco et al.25 and Bushnell et al.26, allow a smaller skin incision and reduce operative times29.
For delayed repair and re-ruptures are suggested Scuderi technique4 to reinforce and Codivilla technique to lengthen the tendon. Authors agree that tendon repair in chronic ruptures gives poorer results than in acute tears4,10,17,23.
Our cases treated with patellar drill holes were satisfactory since the average active ROM re-gained by the patients was 1°–117°. Nobody presented impairment in squatting and only one patient complained weakness. This patient had the earliest follow-up (25 months) and also presented the second highest quadriceps hypotrophy 10 cm proximal to the top of patella (6%) and the highest 15 cm proximal (9%). This patient had a delayed rehabilitation and was addressed to physiotherapy.
One patient only reported post-operative pain, but this patient presented also an untreated anterior cruciate ligament lesion (diagnosed 25 years prior), and we can assume he had developed both instability and ostheo-arthritis (as demonstrated by x-rays assessment). Anyway there was no muscle hypotrophy and the patient didn’t refer lack of strength; the US check indicated good healing of the treated tendon rupture.
The average Lysholm-Knee Score was 88.5/100 that is an excellent result. The average Rougraff Score of 17.1/25, was excellent as well. All patients resumed their previous life style and activities.
The patient that presented lateral subluxation of the patella had the second poorest Lysholm Score (74/100); ROM was not reduced (0–130°). Kaya studied the relationship between patellar tracking and quadriceps activity, involving also the importance of balancing with hamstring30.
Statistical analysis shows no correlation between thigh circumferences of 10C and 15C, that we considered as indexes of quadriceps tropism. Although without direct measurement of quadriceps strength (that was performed by other Authors14,10,16–19,31 with isokinetic and isometric tests), our findings show that thigh circumference has poor predictive power in terms of patient satisfaction and clinical outcome at mid-term follow-up.
No other works evaluated tendon’s morphology after repair. The US check indicated that all the tendons examined were continuous; in 18 cases heterotypic ossifications were found. In all the tendons inhomogeneity was present; this may be because of healing and of previous degeneration. That is consistent with tendon degeneration as direct cause of rupture. Higher thickness was found in 90% of the quadriceps tendons and 25% of the patellar tendons. It’s interesting to notice that the mean follow-ups of patients with this founding were respectively 46 for heterotypic ossifications and 36 for quadriceps tendon and 45 for patellar tendon thickness increase. Except for the thickening of the quadriceps tendons, affecting a high percentage of patients, the other structural changes have a higher mean follow-up compared with the total mean. Further studies may be needed to demonstrate the influence of time on quadriceps tendon and patellar restoring after surgical repair.
The population we assessed is the youngest affected by quadriceps tear rupture, since we excluded patients older than 60 that could have comorbidities or problems in practicing post-operative rehabilitation. It’s interesting to observe that 7 on 20 (35%) were mountain hiking when they got injured and 2 of them were skiing. They referred that these were their leisure activities since they were active people; 8 of our patients said that when they were younger they used to be frequent sport-player (football and tennis). This founding agrees with Shah who asserted that quadriceps tear rupture32 may affect healthy people while they’re playing sport. Huberti et al. studied the connection between the degrees of flexion and the interaction of the forces between the quadriceps and the tendon of patella, observing that most of QTR occur when the knee is at semi-flexion because the tension are higher33; an elevated cycle of flexion-extension of the knee (observable in a middle-aged sport-player) develops before and easier the limit of rupture of the tendon and histological degeneration anticipates the rupture34,35. Further epidemiological and ethiological studies should be performed to study possible relationship between sport practice, tendon degeneration and quadriceps tear rupture.
As supported by statistical analysis, patellar drilling holes technique gives satisfying results in acute lesions in terms of complete knee function and the patients’ ability to resume the same regular activities pre-injury, as confirmed also by various Authors13,13,15–18,20–22 (Tab. 2). US show good healing, restoration of tendon continuity while structural changes (increase of thickness, heterotypic calcifications) (Fig. 6) are asymptomatic and do not impair function.
Table 2.
Outcomes in recent Literature.
| NUMBER OF PATIENTS | ROM | LYSHOLM SCORE | ROUGRAFF SCORE | |
|---|---|---|---|---|
| RASUL JR ET AL. (1993) | 19 | 0–116° | - | - |
| ROUGRAFF ET AL. (1996) | 53 | 123° | - | 8.5/10 |
| KONRATH ET AL. (1998) | 40 | 2–125° | 87/100 | - |
| O’SHEA ET AL. (2002) | 27 | 116.3° | - | 22.9/25 |
| DE BAERE ET AL. (2002) | 24 | 2–120° | - | - |
| WENZL ET AL. (2005) | 35 | 131.8° | 92.5/100 | - |
| RAMSEIER ET AL. (2006) | 21 | No significant difference with not affected limb | - | - |
| PURANIK ET AL. (2006) | 21 | 0.5–102.5° | - | 21.3/25 |
| THE CURRENT STUDY (2014) | 20 | 1–117° | 88/100 | 17/25 |
Figure 6.
RX showing heterotopic calcifications in repaired tendon.
Limitations of this study are the lack of an objective measurement of strength with isokinetic tests and the wide range of follow-up (25–48 months).
The fact that the load tension is applied far from the site of rupture may have a role in preventing possible re-ruptures.
This is an inexpensive and non-demanding technique that if performed in acute ruptures and followed by the correct post-operative protocol, restores an acceptable knee function in subjective and objective terms.
Conclusions
Fixation by patellar drilling holes is a reliable procedure, technically uncomplicated, straightforward to perform and inexpensive for the low hardware’s costs.
According to our data the thigh circumference at a mean follow-up of 36 months is not predictive in terms of clinical outcome and quality of life.
This study is the first work that evaluates tendon morphology after surgical repair, showing a remodeling (in terms of thickness increase and presence of heterotopic calcifications) that does not influence patients’ clinical outcome and quality of life.
Acknowledgments
Paolo Schiavi (MD) for statistical analysis; Carlo Bocchi (MD) for US performing.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338–1344. doi: 10.1016/j.injury.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Vidil A, Ouaknine M, Anract P, Tomeno B. Trauma-induced tears of the quadriceps tendon: 47 cases. Rev Chir Orthop. 2004;90:40–48. doi: 10.1016/s0035-1040(04)70005-7. [DOI] [PubMed] [Google Scholar]
- 3.Stern RE, Harwin SF. Spontaneous and simultaneous rupture of both quadriceps tendons. Clin Orthop Relat Res. 1980;147:188–189. [PubMed] [Google Scholar]
- 4.Scuderi C. Rupture of the quadriceps tendon: study of twenty tendon ruptures. American Journal of Surgery. 1958;95:626–635. doi: 10.1016/0002-9610(58)90444-6. [DOI] [PubMed] [Google Scholar]
- 5.Shah MK. Simultaneous bilateral rupture of quadriceps tendons: analysis of risk factors and associations. Southern Medical Journal. 2002;95:860–866. [PubMed] [Google Scholar]
- 6.Khalid Y, Zhanel GG. Musculoskeletal injury associated with fluoroquinolones antibiotics. Clin Plast Surg. 2005;32:495–502. doi: 10.1016/j.cps.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Spector ED, Di Marcangelo MT, Jacoby JH. The radiologic diagnosis of quadriceps tendon rupture. N Eng J Med. 1995;92:590–592. [PubMed] [Google Scholar]
- 8.Ehman RL, Berquist TH. Magnetic resonance imaging of musculoskeletal trauma. Radiol Clin North Am. 1986;24(2):291–319. [PubMed] [Google Scholar]
- 9.Tegner Y, Lysholm J. Rating system in the evaluation of knee ligament injuries. Clinical Orthopaedics and Related Research. 1995;198:43–48. [PubMed] [Google Scholar]
- 10.Rougraff BT, Reeck CC, Essenmacher J. Complete quadriceps tendon rupture. Orthopaedics. 1996;166 [PubMed] [Google Scholar]
- 11.Mann HB, Whitney DR. On a test of whether one of two random variables is stochastically larger than the other. Annals of Mathematical Statistics. 1947;18(1):50–60. [Google Scholar]
- 12.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal. Basic principles and recommendations in clinical and field science research. MLTJ. 2013;4:250–252. [PMC free article] [PubMed] [Google Scholar]
- 13.Ciriello V, Gudipati S, Tosounidis T, Soucacos PN, Giannoudis PV. Clinical outcomes after repair of quadriceps tendon rupture: a systematic review. Injury. 2012;43(11):1931–1938. doi: 10.1016/j.injury.2012.08.044. [DOI] [PubMed] [Google Scholar]
- 14.O’Shea K, Kenny P, Donovan J, Condon F, McElwain JP. Outcomes following quadriceps tendon ruptures. Injury. 2002;33:257–260. doi: 10.1016/s0020-1383(01)00110-3. [DOI] [PubMed] [Google Scholar]
- 15.Puranik GS, Faraj A. Outcome of quadriceps tendon repair. Acta Orthopaedica Belgica. 2006;72:176–178. [PubMed] [Google Scholar]
- 16.Ramseier LE, Werner CM, Heinzelmann M. Quadriceps and patellar tendon rupture. Injury. 2006;37:516–519. doi: 10.1016/j.injury.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Wenzl ME, Kirchner R, Seide K, Strametz S, Jurgens C. Quadriceps tendon ruptures - is there a complete functional restitution? Injury. 2004;35:922–926. doi: 10.1016/S0020-1383(03)00261-4. [DOI] [PubMed] [Google Scholar]
- 18.De Baere T, Geulette B, Manche E, Barras L. Functional results after surgical repair of quadriceps tendon rupture. Acta Orthopaedica Belgica. 2002;68:146–149. [PubMed] [Google Scholar]
- 19.Konrath GA, Chen D, Lock T, et al. Outcomes following repair of quadriceps tendon ruptures. J of Orthop Trauma. 1998;12:273–279. doi: 10.1097/00005131-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Rasul AT, Jr, Fischer DA. Primary repair of quadriceps tendon ruptures. Results of treatment. Clin Orthop and Relat Res. 1993;289:205–207. [PubMed] [Google Scholar]
- 21.Larsen E, Lund PM. Ruptures of the extensor mechanism of the knee joint. Clinical results and patellofemoral articulation. Clin Orthop and Relat Res. 1986;213:150–153. [PubMed] [Google Scholar]
- 22.Vainionpaa S, Bostman O, Patiala H, Rokkanen P. Rupture of the quadriceps tendon. Acta Orthopaedica Scandinavica. 1985;56:433–435. doi: 10.3109/17453678508994366. [DOI] [PubMed] [Google Scholar]
- 23.Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg. 1981;63:932–937. [PubMed] [Google Scholar]
- 24.Richards DP, Barber FA. Repair of quadriceps tendon ruptures using suture anchors. Arthroscopy. 2002;18:556–559. doi: 10.1053/jars.2002.30729. [DOI] [PubMed] [Google Scholar]
- 25.Maniscalco P, Bertone C, Rivera F, Bocchi L. A new method of repair for quadriceps tendon ruptures. A case report. Panminerva Med. 2000;42:223–225. [PubMed] [Google Scholar]
- 26.Bushnell BD, Whitener GB, Rubright JH, Creighton RA, Logel KJ, Wood ML. The use of suture anchors to repair the ruptured quadriceps tendon. J of Orthop Trauma. 2007;21:407–413. doi: 10.1097/BOT.0b013e31806dd93b. [DOI] [PubMed] [Google Scholar]
- 27.Cohen DA, Levine RG, Parks BG, Boucher HR. Suture anchor versus suture through tunnel fixation for quadriceps tendon rupture: a biomechanical study. Orthopedics. 2008;31:441. doi: 10.3928/01477447-20080501-18. [DOI] [PubMed] [Google Scholar]
- 28.Hart ND, Wallace MK, Scovell JF, Krupp RJ, Cook C, Wyland DJ. Quadriceps tendon rupture: a biomechanical comparison of transosseous equivalent double-row suture anchor versus transosseous tunnel repair. J Knee Surg. 2012;25(4):335–339. doi: 10.1055/s-0031-1299656. [DOI] [PubMed] [Google Scholar]
- 29.Lighthart WA, Cohen DA, Levine RG, Parks BG, Boucher HR. Suture Anchor Versus Suture Through Tunnel Fixation for Quadriceps Tendon Rupture: A Biomechanical Study. Orthopaedics. 2008;31(5):441. doi: 10.3928/01477447-20080501-18. [DOI] [PubMed] [Google Scholar]
- 30.Kaya D, Doral MN, Callaghan M. How can we strengthen the quadriceps femoris in patients with patellofemoral pain syndrome? Muscles, Ligaments and Tendons Journal. 2012;2(1):25–32. [PMC free article] [PubMed] [Google Scholar]
- 31.West JL, Keene JS, Kaplan LD. Early motion after quadriceps and patellar tendon repairs: outcomes with single-suture augmentation. Am J of SportsMed. 2008;36:316–323. doi: 10.1177/0363546507308192. [DOI] [PubMed] [Google Scholar]
- 32.Shah M, Jooma N. Simultaneous bilateral quadriceps tendon rupture while playing basketball. British Journal of Sports Medicine. 2002;36:152–153. doi: 10.1136/bjsm.36.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huberti HH, Hayes WC, Stone JL, Shybut GT. Force ratios in the quadriceps and ligamentum patellae. J Orthop Res. 1984;2(1):49–54. doi: 10.1002/jor.1100020108. [DOI] [PubMed] [Google Scholar]
- 34.Maffulli N, Del Buono A, Spiezia F, Longo UG, Denaro V. Light microscopic histology of quadriceps tendon ruptures. Int Orthop. 2012;36:2367–2371. doi: 10.1007/s00264-012-1637-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. 1991;73:1507–1525. [PubMed] [Google Scholar]