Summary
This review highlights recent research on Achilles tendon healing, and comments on the current clinical controversy surrounding the diagnosis and treatment of injury. The processes of Achilles tendon healing, as demonstrated through changes in its structure, composition, and biomechanics, are reviewed. Finally, a review of tendon developmental biology and mechano transductive pathways is completed to recognize recent efforts to augment injured Achilles tendons, and to suggest potential future strategies for therapeutic intervention and functional tissue engineering. Despite an abundance of clinical evidence suggesting that current treatments and rehabilitation strategies for Achilles tendon ruptures are equivocal, significant questions remain to fully elucidate the basic science mechanisms governing Achilles tendon injury, healing, treatment, and rehabilitation.
Keywords: biomechanics, foot and ankle, tendinopathy, Achilles tendon rupture, injury, developmental biology, tissue engineering
Introduction
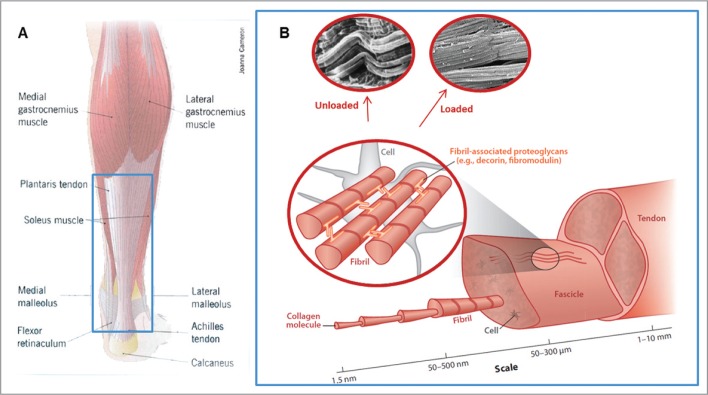
The Achilles is the strongest and largest tendinous structure in the body. It is defined anatomically as the distal confluence of the gastrocnemius and soleus muscles and may also include the plantaris longus1 (Fig. 1). During activity, the Achilles tendon can bear loads in excess of 3500 N2,3, yet despite its tremendous strength, is frequently injured. Acute and chronic Achilles tendon pathology is estimated to be responsible for as much as 50% of all sports-related injuries4. 75% of Achilles tendon ruptures occur in middle-aged men between the ages of 30 and 49 while participating in sport4–7 and the incidence is rising4, 6–8. The association of Achilles rupture with obesity, amongst a number of similarly trending parameters, may also play a role7. Chronic Achilles tendon injuries are generally defined by activity associated Achilles pain (e.g. swelling and tenderness) in conjunction with impaired performance during sporting activity4, and asymptomatic degeneration may occur in 4% of active adults9,10. Rare causes of Achilles tendon rupture include fluoroquinalone-induced ruptures (0.02–2.0%) and those associated with systemic disease (2.0%)4,7,11.
Figure 1.
Gross anatomy and structure of the Achilles tendon. (A) The Achilles tendon emerges at the distal confluence of the gastrocnemius and soleus muscles and inserts into the calcaneus. (B) Similar to other tendons, the Achilles exhibits a hierarchical structure composed of fascicles, fibers, and fibrils. When loaded, fibrils straighten, decrease in crimp amplitude and frequency, and become more aligned.
Panel A: Image reproduced with permission from Joanna Cameron (2013). Panel B: Image reproduced with permission from Franchi et al. (2007)38 and Voleti et al. (2012)33.
The primary means of diagnosing Achilles tendon rupture is through patient history and physical examination12. In acute Achilles ruptures, patients often present with a history of eccentric loading associated with a popping sensation, immediately followed by pain and difficulty during ambulation. In some cases of partial rupture where the diagnosis can be more difficult, MRI or advanced Doppler ultrasound may be beneficial13. Ultrasound may provide further benefit as a tool to monitor the healing process14.
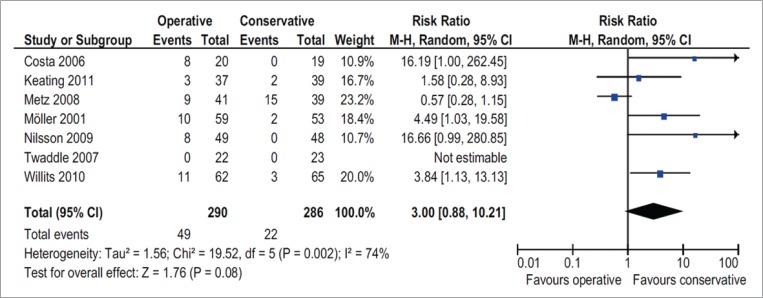
Meta-analyses evaluating treatment of the acute Achilles tendon rupture15–18 have established the need for improved intervention given moderate outcomes12. Although early trials pointed to a decreased risk of re-rupture with surgical intervention at the cost of an associated increased risk of other major and minor complications18, best practices regarding the treatment of Achilles tendon rupture remains an ongoing topic of debate12,16 (Fig. 2). The known response of the Achilles tendon to mechanical stimulation19–22 underlies the importance of rehabilitation in healing. In therapy initiated after rupture there is good evidence supporting early return to activity, however optimized protocols have not been defined and long term benefits have not been demonstrated23–26. Treatment of chronic Achilles tendinopathy remains challenging and usually consists of early rehabilitation with eccentric strengthening protocols but in intractable cases can result in continued symptoms eventually requiring surgical intervention27, 28. Therefore, well controlled basic science studies are important in resolving outstanding fundamental questions regarding means of treatment in a consistent and well established model. In this review we highlight recent research on Achilles tendon healing, and suggest potential strategies for therapeutic intervention and functional tissue engineering.
Figure 2.
Summary of several randomized control trials (RCTs) highlighting the current clinical controversy surrounding surgical versus non-surgical treatment of Achilles tendon ruptures. This Table and Forest plot indicates that no significant difference in either major or minor complications exist between patients receiving operative and non-operative treatment. Image reproduced with permission from van der Eng et al. (2011)15.
Compositional, structural, and biomechanical properties of normal Achilles tendon
Defining baseline compositional properties for normal tendon is necessary to set appropriate benchmarks for healing and to determine appropriate strategies for successful functional tissue engineering. Unfortunately, basic Achilles tendon compositional data is currently lacking, with the most thorough compositional studies performed using flexor tendons. As an extrapolation from data in other systems, Achilles tendons are thought to be composed of approximately 90% type I collagen that forms a hierarchical structure of fibrils, fibers, and fascicles bound together by small matrix molecules, such as proteoglycans29. The Achilles tendon insertion is composed of types II, IX, and X collagen, with type X collagen localized in the mineralized zone and type IX distributed throughout30. Although elastin only accounts for up to 2% of the tendon’s dry mass, recent studies have shown it makes important contributions to the mechanical properties of tendons31. Digestion of glycosaminoglycans has been shown to decrease tendon modulus and ultimate load specifically at the tendon insertion site, suggesting a regional variance in composition that may mirror regional differences in structure and mechanical performance32. Alterations in tendon structure and loading elicit biochemical changes that are exacerbated in cases of injury and healing.
The structure of tendon directly relates to its mechanical function33. Baseline characterization of normal Achilles tendon structure is necessary to identify the mechanisms governing tendon injury and failure. Generally, tendon is an inhomogeneous, anisotropic, nonlinear34, fiber-reinforced, biocomposite material35 primarily composed of a collagen extracellular matrix36 and non-collagenous molecules. The dry weight of tendon is primarily composed of longitudinal collagen fibers that are believed to be the primary load bearing components in mature tissue37. At the most basic level, the collagen fibers in tendon are highly organized structures that demonstrate high strength in the direction of fiber alignment36. Under polarized light, tendons exhibit periodic banding due to its waveform configuration known as “crimp”. This property extends down in a hierarchical fashion from macro- to nano-structural scales38. When initially loaded, the force-displacement curve demonstrates a distinct nonlinearity or “toe region” that arises from uncrimping and an associated increase in collagen alignment39. This concept is supported by the observed decrease in crimp frequency and amplitude in loaded Achilles tendons38. Glycosaminoglycans (GAGs) and structural proteins, such as elastin31, connect adjacent fibrils. Such molecules may play a role in tendon structure-function relationships, though their specific role requires further elucidation31,37. Disruption to any of these load bearing elements may be detrimental to physiologic function, potentially leading to injury and failure.
Ultimately, Achilles tendon mechanical properties govern the tendon’s ability to respond and adapt to its loading environment. Achilles tendon mechanical nonlinearity is shown through its stress strain curve at low strains40. At higher strains, Achilles tendons deform linearly prior to yield and rupture. Although the Achilles tendon is commonly referred to as a viscoelastic material containing both elastic (stress and strain occur in phase) and viscous (90 degree phase difference between stress and strain) components that store and release energy during loading to protect soft tissues from being damaged41, recent evidence in humans has suggested that its elastic properties dominate42. These elastic spring-like properties allow the Achilles tendon to deliver explosive propulsion during ambulation as they may bear up to 3500 N before rupture2. Aside from cases of injury, Achilles tendon mechanical properties may be influenced by genetics43, development44, and aging45.
Several studies have used conventional quasi-static methods to evaluate tendon mechanical properties46,47. However, given that the Achilles tendon typically performs at high and repetitive loads at or near failure, the clinical relevance of utilizing fatigue testing becomes increasingly important. Cadaveric and animal studies have shown that the response of tendon to fatigue loading is marked by three phases of damage48. In particular, stiffness initially increases, reaches a maximum, and then gradually decreases. This gradual decrease in stiffness is attributed to accumulated sub-rupture damage, which ultimately leads to the dramatic increase in peak deformation and decrease in stiffness prior to failure48–50. Interestingly, measured tendon fatigue in vivo in humans51,52 has been less than that observed in vivo or ex vivo in animals53. Future work is necessary to fully evaluate this mechanism since these studies were not designed to control for the loads evaluated, which affects ex vivo fatigue damage54.
Compositional, structural, and biomechanical properties of pathologic Achilles tendon
Following injury, Achilles tendons are biologically altered at both the cell and ECM levels47, including a high density of inflammatory cells within the repair site47,55. Collagen content is decreased compared to control tendons56, and is correlated with failure stress in ruptured tendons56. Within a few days of injury, tenocyte numbers are greatly reduced, expression of scleraxis (Scx, often used as a tenocyte marker) is substantially diminished, and apoptosis is evident19. Throughout early to intermediate healing, collagen-3 and biglycan have been shown to be upregulated57. In addition, in the middle-stages of healing, collagen-157, versican57, decorin57, matrix metalloproteinases (MMPs)58,59, tissue inhibitory metalloproteinases (TIMPs)58, and ADAMs58 become upregulated, indicating further tissue remodeling. With healing, cell number and density return to baseline values47. Together, these findings suggest that healing results in altered Achilles tendon compositional properties that may reflect the structural and mechanical quality of the newly deposited tissue.
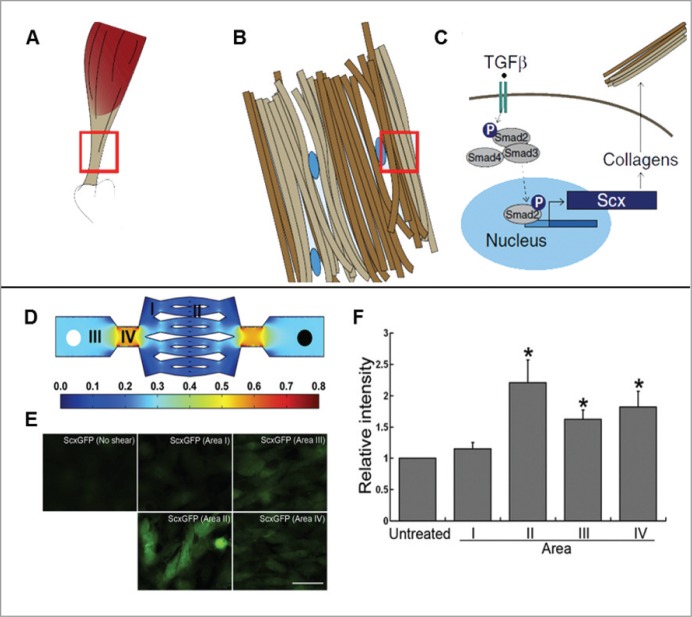
The Achilles tendon undergoes high repetitive loading demonstrated to influence tendon composition, suggesting the importance of the underlying mechanotransductive signaling response19–22,57,60,61. Harnessing the therapeutic effects of mechanical loading, as evidenced in normal tendon, may provide potentially transformative methods to enhance healing in injured tissues. Moderate running in mice was found to increase growth factor production, proliferation of tendon stem cells, expression of collagen-1 and tenomodulin, but had not effect on the expression of genes associated with cartilage and bone pheno-types20. However increasing the length of running episodes resulted in increased expression of both tendon, cartilage, and bone genes, indicating that excessive mechanical loading may cause metabolic changes and differentiation of TSCs into non-tenocyte lineages20. In a separate study, uphill running had a positive effects on tendon composition and mechanics, showing increased expression of collagen-3 and IGF-1, and decreased expression of fibromodulin, biglycan, degradative enzymes, TGF-β1, and CTGF21. Identifying changes in collagen synthesis in in vivo human studies has been more challenging. Following a 2-week single-limb immobilization period, humans were subjected to one hour of treadmill running60. After one hour of treadmill running, increased collagen synthesis was detected in both Achilles tendons. No changes were observed by Power Doppler ultrasound or in tendon cross-sectional area60. To further characterize the downstream signaling effects of mechanical loading, studies have investigated the role of TGF-β (Fig. 3A–C). Specifically, the effect of cyclic strain has been shown to mirror that of TGF-β stimulation22. In a related study, it was found that a single session of activity and treatment of TGF-β modulated the expression of collagen-1, Scx, and three mechanosensitive miRNAs, suggesting a mechanism for tendon adaptation and healing61. Additionally, fluid shear stress used as a surrogate for cyclic strain, was found to induce Scx expression19 (Fig.3D–F). Taken together, these studies demonstrate that mechanical loading and its downstream mediators directly affect tendon composition.
Figure 3 A–F.
Effects of mechanical loading on Achilles tendon composition. (A–C): The Achilles tendon (A) is composed of an extracellular matrix (B) containing cells known as tenocytes. (C) TGF-β signaling leads to downstream activation of the smad proteins, leading to expression of scleraxis (Scx) and collagens. (D–F): To elucidate the effects of fluid shear stresses on the downstream expression of Scx, a microfluidics device was used to provide a dose dependent response of fluid shear stresses (D, regions I–IV). (E,F) Moderate shear stresses promote increased expression of Scx, whereas removal of shear stress resulted in no expression of Scx. Collectively, these studies suggest that mechanical loading and its downstream mediators directly affect tendon and may be partially mediated by TGF-β signaling.
Panels A–C: Image reproduced with permission from Sharir et al. (2011)62. Panels D–F: Image reproduced with permission from Maeda et al. (2011)19.
Compositional property changes stimulated through variations in loading protocols may allow for potentially therapeutic treatment strategies. In a study examining the effects of post rupture mobilization, late changes in ECM in addition to a 14-fold increase in mRNA expression of collagen-I, collagen-II, versican, decorin and biglycan were observed when compared to an immobilized group57. Such compositional findings were confirmed with histological evidence that showed increased blood vessel, fibroblast, and new collagen formation57. Conversely, stress deprivation via Achilles tendon detachment resulted in increased MMP-13, MMP-3, TIMP-2 in culture, and the addition of cyclic hydrostatic compression had no effects on subsequent gene expression63. Surrogate measures for in vivo composition such as tendon strength, stiffness, and ultrasound echo intensity have been correlated with collagen type and content47. Although several studies have aimed to demonstrate the potential clinical benefit of load dependent therapies, additional characterization is warranted prior to translation into humans.
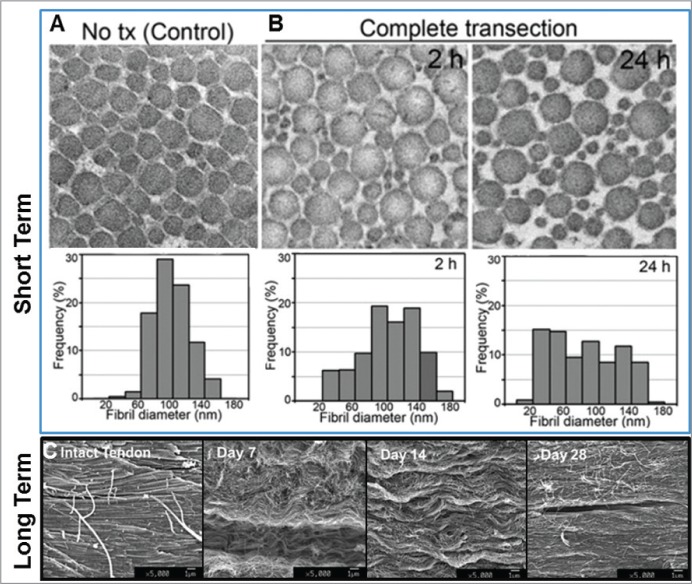
Compositional changes with healing are mirrored by structural and biomechanical alterations. Following complete Achilles transection in animal models, tendon stumps remain well defined. During healing the gross appearance of the tendon changes, becoming wider, denser, and less translucent with time64. The reduction in tendon transparency occurs in conjunction with deposition of new fibrils with altered diameter distributions19 and decreased longitudinal organization55,65 (Fig.4). With healing, new fibers gradually become more aligned65,66 and with this altered structure, tendons may elongate67. Notably, Achilles tendon elongation has been correlated with poor clinical outcomes68. Despite the increased alignment of newly deposited elements, scarred portions may remain non-recoverably disorganized with associated inferior mechanical properties69.
Figure 4.
Effects of injury on Achilles tendon structural properties.(A–B) Within 24 hours of complete Achilles tendon transection, fibril diameter distributions show a greater number of large and small diameter fibrils, indicating a structural change in response to injury. (C) In the longer term, transverse SEM data indicates that the initial disorganization observed gradually leads to more longitudinally aligned collagen fibrils with healing.
Panels A–B: Image reproduced with permission from Maeda et al. (2011)19. Panel C: Image reproduced with permission from Sasaki et al. (2012)65.
Promising new imaging methods have proven effective in assessing structural components and predicting mechanical properties. Tissue birefringence, a measure of structural organization, was able to predict tendon modulus throughout healing69. Similarly, echo intensity using low frequency B-mode ultrasound is correlated with tendon stress and normalized stiffness during healing70. This method may also measure strain directly and be useful to identify partially torn Achilles or those susceptible to rupture71. Taken further, high frequency ultrasound has been able to directly measure fiber alignment72 a critical property in determining mechanical performance of tissue36. Such imaging techniques capable of structural and mechanical analysis offer an exciting means of monitoring tissue healing as well as risk of injury or re-injury.
The specific effects of mechanical loading on structural remodeling in healing Achilles tendon remain controversial. Structural adaptation to mechanical load is evident through increased tendon thickness following exercise in rats73. Consistently, after prolonged ankle immobilization in multiple species, structural organization is known to decrease57,74. Attempts at creating a model to explore how excessive loading may participate in Achilles tendinopathy has generated mixed histological results21,73,75–77. These varied results21,73,75–77 suggest that the response of tendon to mechanical load is protocol dependent and that histological evidence alone is insufficient to fully characterize tendinopathy. Determining the optimum loading conditions and the mechanisms by which this impacts tendon remodeling requires careful evaluation, with particular focus on load magnitude, frequency, and duration.
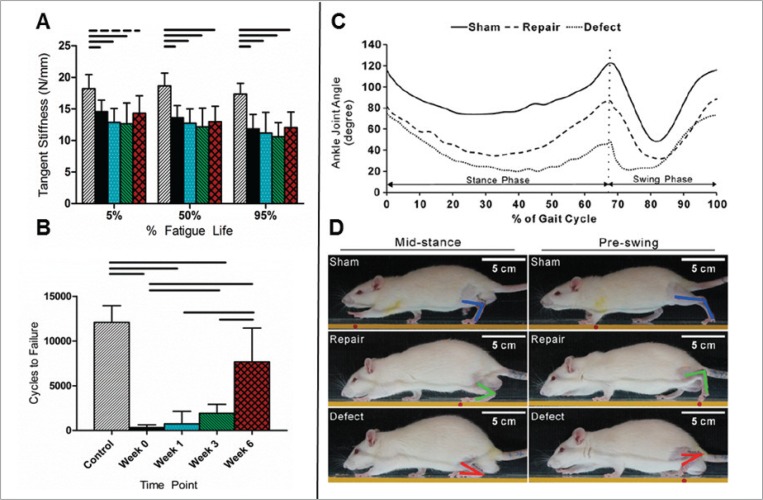
Injured Achilles tendons display inferior mechanical properties and increase in cross sectional area during healing46,47,56. Examples of inferior quasi-static mechanical properties following injury include decreased ultimate stress, maximum load, stiffness (Fig. 5A), elongation to failure, modulus, and percent relaxation (a measure of tendon viscoelasticity)46,47,69. Although conventional quasi-static mechanical tests have shown inferior material properties following injury, they lack the clinical parallel to in vivo tendon performance observed in fatigue testing. In particular, the number of cycles to failure, as a result of fatigue testing, has been shown to decrease dramatically following injury69 (Fig. 5B) and may better mirror the collagen breakdown process observed with repeated loading in vivo78. The mechanisms driving mechanical changes in tendons likely stem from changes in structure and composition with injury. For example, it is believed that viscoelastic properties that decrease in injured tendon79 may be a result of alterations in collagen structure80 that, in turn, affect friction between collagen fibers and ECM41, fluid flow through the ECM81, and cross links between molecules82. With healing, tendon mechanical properties may demonstrate partial recovery47, but complete recovery is not achieved.
Figure 5.
A–D. Biomechanical response of the Achilles tendon to injury and healing. (A–B) Following an acute injury, the tangent stiffness (A) and the number of cycles to failure (B) decreased. (C–D) Video-based measures to evaluate rat gait following injury demonstrated that injured and repaired animals ambulated with lower ankle joint angles compared to normal controls. When quantified over the course of healing, the ankle joint angle was shown to be a more sensitive metric compared to the Achilles Functional Index.
Panels A–B: Image reproduced with permission from Freedman et al. (2013)69. Panels C–D: Image reproduced with permission from Liang et al. (2013)90.
To evaluate the effects of dose-dependent loading on healing, tail suspension83,84, Botox85, immobilization74, whole body vibration86, and exercise21,83 have been used as model systems. Collectively, these studies have demonstrated that Achilles tendon mechanics are highly influenced by the magnitude83–85, timing83, and duration21 of loading. Specifically, tendon mechanics were shown to improve with just four loading periods for both early and late healing83 and inhibition of loading via treatment with Botox and tail suspension could reduce quasi-static mechanical properties by up to 80%85. Dynamic mechanical properties, such as the loss and storage modulus, were inferior in Achilles tendons that were immobilized74. Interestingly, one study attempting to create degenerate conditions in the Achilles tendon via uphill running found that the loading protocol actually led to improved tendon modulus and failure stress21. To determine if animal-based findings supporting the positive impact of loading during tendon healing translate to humans, a randomized control trial was conducted where subjects were randomized into an early tensional loading or cast immobilization87. The groups showed no differences in functional outcomes measured by the Achilles Tendon Total Rupture Score (ATRS) or heel-raise index after 52 weeks, but the elastic modulus was improved. This further supports the concept that simple in vivo assays do not directly assess tendon function suggesting the need for in vivo image-based assays that assess tendon structure-function relationships.
Several studies have utilized sophisticated biomechanical tests to characterize injured and healing tendons, but, due to their high cost and complexity these have remained research tools. Three dimensional gait analysis found that individuals with Achilles tendinopathy had less tibial external rotation moment and peak internal rotation compared to healthy runners88. Although this study gives insight into the prospect of future exercise programs that may avoid such potentially harmful movements, it is unknown whether the change in gait was due to aberrant running biomechanics or was followed by the Achilles tendinopathy. In a separate study, runners with a non-rearfoot strike exhibit a higher Achilles tendon impulse during running, which may contribute to injury89. In rats, a video-based gait system detected differences in healing Achilles tendons that showed improvement with healing90 (Fig.5C,D). Still, the severity of injury remains unknown since no uninjured controls were included in the study90. In another in vivo functional assay, the passive elastic properties as assessed by ankle equilibrium position and dynamic torque of the rat ankle were affected by torn dorsiflexor and extensor ankle muscles91. This technique may have significant application in the clinic, where a constant effort exists to link in vivo ankle properties to tissue level mechanics. Finally, ultrasound-based measures of tendon mechanics have been investigated. For example, conventional and shear wave elastography have shown that tissue elasticity decreases in ruptured Achilles tendons, thus highlighting potential clinical utility92,93. However, such methods assume that material properties and wave velocity remain constant with loading, which therefore may restrict application of these techniques to small strains. Other ultrasound-based methods may overcome such limitations, such as the acoustoelastic strain gauge that relates changes in echo intensity during movement to tissue mechanical properties and has shown excellent reliability and agreement between limbs94.
Biological augmentation for tendon healing
Overview
Tendon development and healing is a well-orchestrated process requiring highly ordered molecular signaling events influenced by mechanical stimulation and surrounding environmental factors95. To best augment Achilles tendon healing through targeted therapeutics and tissue engineering strategies requires sufficient understanding of the in vivo milieu that dictates tendon development. Importantly, tendons injured during early phases of development heal without scar at an accelerated rate96,97.
Tendon Development
In early studies regarding tendon formation, there was substantial emphasis on the extracellular matrix98. Recent work has focused on tenocyte differentiation, and requisite molecular and mechanical signaling. Axial tendon formation has been shown to require early FGF signaling for induction of Scx expression, an early marker of commitment to the tenocyte lineage that persists through maturation99–101. In chick wing buds, BMP over expression decreased Scx expression, while Noggin over expression, a BMP antagonist, had the converse effect. Despite over expression of Scx in the presence of Noggin no ectopic tendon formation occurred100. These studies suggest that although Scx may be necessary for tendon formation, it is not sufficient. TGF-β signaling is also required for tendon formation. In mouse limb buds, removal of TGF-β signaling resulted in absent expression of Scx and tenomodulin, a downstream differentiation marker102. Interestingly, mechanical stimulation in mouse tendons resulted in TGF-β signaling and downstream Scx expression. Many other factors influence this process, and the detailed biological program responsible for healthy tendon formation remains a highly active field of research.
Molecular biology of tendon healing
Numerous signaling pathways have been demonstrated to participate in the orchestration of tendon healing. It is no surprise that several such pathways shown to have a significant impact on healing are also key regulators of development (e.g., BMP, TGF-β, and early growth response (EGR)103. In the rat, over expression of BMP-14 at the Achilles tendon during healing resulted in increased tendon tensile strength as compared to control tendons104. As BMP signaling has been demonstrated to interfere with Scx expression, this highlights the intricate and not always straight forward nature of healing. In contrast, EGR1, a transcription factor that unlike BMP has been demonstrated to participate in tendon differentiation, also promoted healing of the Achilles tendon in a rat model. Further, and similar to development, there are numerous other molecular signaling pathways involved in healing (e.g., CTGF, VEGF, TGF-β, IGF-1, and FGF)105. As each of these pathways appears to play a specific role in development, exploration of their function in healing as well as tissue engineering remains critical.
Therapeutics and tissue engineering
Several studies have used therapeutics and tissue engineering approaches in attempts to reduce signs of tendinopathy and to enhance Achilles tendon healing following rupture. Several studies have suggested the prospect of stem cell therapies in the treatment of tendinopathy106. When seeded on decellularized tendon matrices107,108 these cells produced a surrounding environment very similar to native tissue. In addition, compared to traditional culture, MSCs maintained under hypoxic conditions109 were found to demonstrate a more physiologic phenotype. Other therapeutics such as amnion derived multipotent progenitor cells demonstrated improved mechanical properties after application in injured rat Achilles tendons110. Finally, although whole blood injection111, Platelet Rich Plasma (PRP)27,112, and other adjuvant therapies have demonstrated potential clinical use113, some even supported by small trials, none has a sufficiently consistent track record to merit a consensus recommendation.
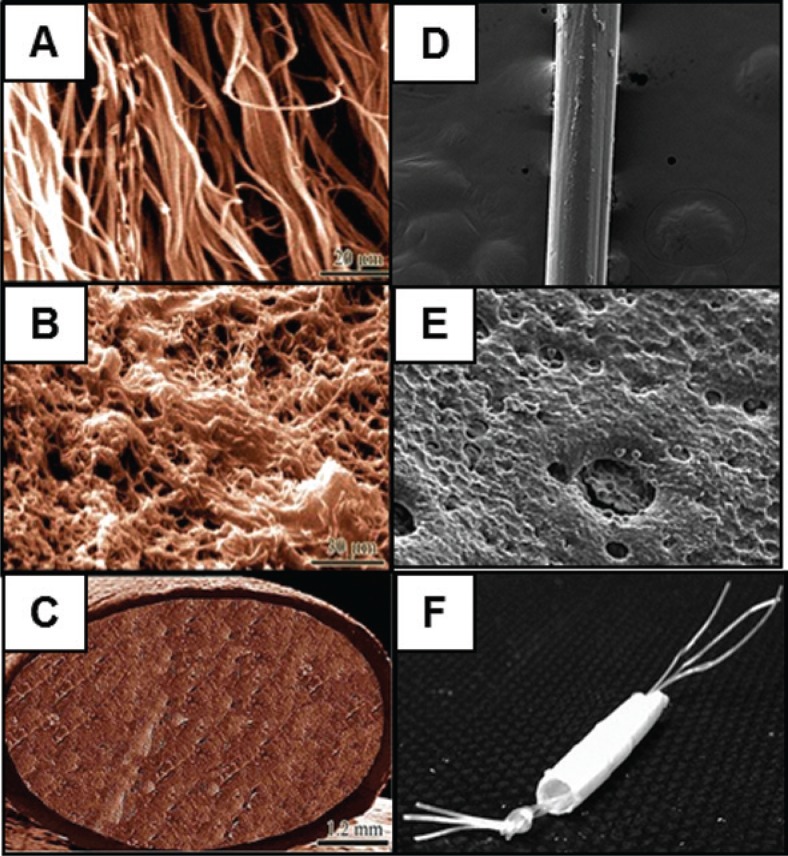
Tissue engineering strategies utilizing 3D scaffolds have been engineered to integrate between ruptured ends of Achilles tendons in rats114 and rabbits115 (Fig. 6). For example, in vivo and ex vivo experiments demonstrating that collagen-PDF implants recapitulate the structural, compositional, and mechanical properties of control tendons, and show capacity for good integration in vivo116. Incorporation of biodegradable synthetic scaffolds may present an additional strategy for future research117,118.
Figure 6 A–F.
Tissue Engineering Strategies to Repair Ruptured Achilles Tendons. Tissue engineering strategies utilizing 3D scaffolds have been engineered to integrate between ruptured ends of Achilles tendons. (A–C) The collagen-PDS implant engineered demonstrated fibril-like characteristics when viewed in the transverse direction (A, scale: 20μm) and porous morphology with fibers connected by cross links in the transverse direction (B, scale: 20μm). In vivo and ex vivo experiments demonstrated that collagen-PDS implants recapitulate the structural, compositional, and mechanical properties of control tendons, and show capacity for good integration116. (C) SEM showing the entire collagen-PDS implant (scale: 1.2 mm). (C–F) In a separate approach, poly(3-hydroxybutryrate-co-3-hydroxyhexanoate) (PHBHHx) was evaluated as a potential scaffold for rat Achilles tendon healing. SEM images demonstrated that the fibers (D; scale: 200× magnification)used to construct the PHBHHx tubular scaffold also contained surface pores (E; scale: 500×). (F) SEM showing entire PHBHHx implant. Once implanted, these scaffolds showed comparable mechanical properties to rat tendon, no secondary immune response, evidence of tissue remodeling and cell alignment, and a return to normal animal load bearing.
Panels A–C: Image reproduced with permission from Meimandi-Parizi et al. (2013)115. Panels D–F: Image reproduced with permission from Webb et al. (2013)114.
Future perspective and conclusion
There is much information regarding the anatomy, diagnosis, treatment, and biomechanics of normal and healing Achilles tendons, however there remains many research areas requiring further investigation. Although well controlled basic science studies are not a direct substitute for large scale clinical trials, they are important in resolving outstanding fundamental questions regarding means of treatment in a consistent and well established model. This includes studies designed to determine whether non-operative treatment of Achilles tendon ruptures is equivalent to operative treatment, and identification of the optimal rehabilitation protocol. For example, the benefits of eccentric exercise on Achilles tendon healing have only been performed in the context of tendinopathy12,118–124, and its potentially therapeutic effects following injury or repair require further evaluation. Future studies should provide a comprehensive approach to study tendon healing, through careful evaluation of mechanical, structural, compositional, and functional tissue properties. In particular, it will be informative to relate image-based modalities evaluating tendon structure to dynamic mechanical properties. These studies should be prioritized due to their potentially translatable nature. Additionally, there is a need for greater characterization of the dose-dependent response of mechanical load on tendon. Results from such studies would further allow for much needed research into development of effective adjuvant therapies that could be translated into improved outcomes.
Continued investigation into promising direct biologic interventions, such as BMP, EGR1 or other combinations of cells and cytokines would seem capable of generating useful therapies in a reasonable time course. Lessons from development may continue to expand this list of putative treatments, as well as our fundamental understanding of the healing process. Cell based therapies and tissue engineering also represent a related avenue well suited to facilitate Achilles tendon healing. While none of these promising therapies has had a marked impact on patient outcomes thus far, recent and ongoing work offers reasons to be optimistic regarding facilitation of Achilles tendon healing and coming improvements in patient centered outcomes.
References
- 1.Kotian SR, Sachin KS, Bhat KM. Bifurcated plantaris with rare relations to the neurovascular bundle in the popliteal fossa. Anat Sci Int. 2013;88:239–241. doi: 10.1007/s12565-013-0184-z. [DOI] [PubMed] [Google Scholar]
- 2.Fukashiro S, Komi PV, Jarvinen M, Miyashita M. In vivo Achilles tendon loading during jumping in humans. Eur J Appl Physiol Occup Physiol. 1995;71:453–458. doi: 10.1007/BF00635880. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81:1019–1036. doi: 10.2106/00004623-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Jarvinen TA, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot Ankle Clin. 2005;10:255–266. doi: 10.1016/j.fcl.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Nyyssonen T, Luthje P, Kroger H. The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987–1999. Scand J Surg. 2008;97:272–275. doi: 10.1177/145749690809700312. [DOI] [PubMed] [Google Scholar]
- 6.Houshian S, Tscherning T, Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish county. Injury. 1998;29:651–654. doi: 10.1016/s0020-1383(98)00147-8. [DOI] [PubMed] [Google Scholar]
- 7.Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34:475–480. doi: 10.1177/1071100713477621. [DOI] [PubMed] [Google Scholar]
- 8.Vosseller JT, Ellis SJ, Levine DS, et al. Achilles tendon rupture in women. Foot Ankle Int. 2013;34:49–53. doi: 10.1177/1071100712460223. [DOI] [PubMed] [Google Scholar]
- 9.Nicol AM, McCurdie I, Etherington J. Use of ultrasound to identify chronic Achilles tendinosis in an active asymptomatic population. J R Army Med Corps. 2006;152:212–216. doi: 10.1136/jramc-152-04-03. [DOI] [PubMed] [Google Scholar]
- 10.Joseph MF, Crowley J, Dilieto L, O’Neil B, Denegar CR. Incidence of morphologic changes in asymptomatic Achilles tendons in an active young adult population. J Sport Rehabil. 2012;21:249–252. doi: 10.1123/jsr.21.3.249. [DOI] [PubMed] [Google Scholar]
- 11.Stephenson AL, WuW Cortes D, Rochon PA. Tendon Injury and Fluoroquinolone Use: A Systematic Review. Drug Saf. 2013 doi: 10.1007/s40264-013-0089-8. [DOI] [PubMed] [Google Scholar]
- 12.Chiodo CP, Glazebrook M, Bluman EM, et al. Diagnosis and treatment of acute Achilles tendon rupture. The Journal of the American Academy of Orthopaedic Surgeons. 2010;18:503–510. doi: 10.5435/00124635-201008000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Alfredson H, Masci L, Ohberg L. Partial mid-portion Achilles tendon ruptures: new sonographic findings helpful for diagnosis. Br J Sports Med. 2010;45:429–432. doi: 10.1136/bjsm.2009.067298. [DOI] [PubMed] [Google Scholar]
- 14.Margetić P, Miklić D, Rakić-Ersek V, Doko Z, Lubina ZI, Brkljacić B. Comparison of ultrasonographic and intraoperative findings in Achilles tendon rupture. Coll Antropol. 2007;31:279–284. [PubMed] [Google Scholar]
- 15.van der Eng DM, Schepers T, Goslings JC, Schep NW. Re-rupture Rate after Early Weightbearing in Operative Versus Conservative Treatment of Achilles Tendon Ruptures: A Meta-analysis. J Foot Ankle Surg. 2013;52:622–628. doi: 10.1053/j.jfas.2013.03.027. [DOI] [PubMed] [Google Scholar]
- 16.Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database. Syst Rev. :CD003674. doi: 10.1002/14651858.CD003674.pub4. [DOI] [PubMed] [Google Scholar]
- 17.Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94:2136–2143. doi: 10.2106/JBJS.K.00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhandari M, Guyatt GH, Siddiqui F, et al. Treatment of acute Achilles tendon ruptures: a systematic overview and meta-analysis. Clin Orthop Relat Res. 2002:190–200. doi: 10.1097/00003086-200207000-00024. [DOI] [PubMed] [Google Scholar]
- 19.Maeda T, Sakabe T, Sunaga A, et al. Conversion of mechanical force into TGF-beta-mediated biochemical signals. Curr Biol. 2011;21:933–941. doi: 10.1016/j.cub.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang J, Wang JH. The effects of mechanical loading on tendons - an in vivo and in vitro model study. PLoS One. 2013;8:e71740. doi: 10.1371/journal.pone.0071740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heinemeier KM, Skovgaard D, Bayer ML, et al. Uphill running improves rat Achilles tendon tissue mechanical properties and alters gene expression without inducing pathological changes. J Appl Physiol. 1985;113:827–836. doi: 10.1152/japplphysiol.00401.2012. [DOI] [PubMed] [Google Scholar]
- 22.Jones ER, Jones GC, Legerlotz Km, Riley GP. Cyclical strain modulates metalloprotease and matrix gene expression in human tenocytes via activation of TGFbeta. Biochim Biophys Acta. 1833:2596–2607. doi: 10.1016/j.bbamcr.2013.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garrick JG. Does accelerated functional rehabilitation after surgery improve outcomes in patients with acute achilles tendon ruptures? Clin J Sport Med. 2012;22:379–380. doi: 10.1097/JSM.0b013e3182603905. [DOI] [PubMed] [Google Scholar]
- 24.Mortensen HM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. A prospective, randomized clinical and radiographic study. J Bone Joint Surg Am. 1999;81:983–990. doi: 10.2106/00004623-199907000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Costa ML, Shepstone L, Darrah C, Marshall T, Donell ST. Immediate full-weight-bearing mobilisation for repaired Achilles tendon ruptures: a pilot study. Injury. 2003;34:874–876. doi: 10.1016/s0020-1383(02)00205-x. [DOI] [PubMed] [Google Scholar]
- 26.Maffulli N, Tallon C, Wong J, Peng Lim K, Bleakney R. No adverse effect of early weight bearing following open repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness. 2003;43:367–379. [PubMed] [Google Scholar]
- 27.de Vos RJ, Weir A, van Schie HT, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA. 2010;303:144–149. doi: 10.1001/jama.2009.1986. [DOI] [PubMed] [Google Scholar]
- 28.Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med. 2003;22:727–741. doi: 10.1016/s0278-5919(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 29.Longo UG, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc. 2009;17:112–126. doi: 10.1097/JSA.0b013e3181a3d625. [DOI] [PubMed] [Google Scholar]
- 30.Fukuta S, Oyama M, Kavalkovich K, Fu FH, Niyibizi C. Identification of types II, IX and X collagens at the insertion site of the bovine achilles tendon. Matrix Biol. 1998;17:65–73. doi: 10.1016/s0945-053x(98)90125-1. [DOI] [PubMed] [Google Scholar]
- 31.Henninger HB, Underwood CJ, Romney SJ, Davis GL, Weiss JA. Effect of elastin digestion on the quasi-static tensile response of medial collateral ligament. J Orthop Res. 2013;31:1226–1233. doi: 10.1002/jor.22352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rigozzi S, Muller R, Snedeker JG. Local strain measurement reveals a varied regional dependence of tensile tendon mechanics on glycosaminoglycan content. J Biomech. 2009;42:1547–1552. doi: 10.1016/j.jbiomech.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 33.Voleti PB, Buckley MR, Soslowsky LJ. Tendon healing: repair and regeneration. Annu Rev Biomed Eng. 2012;14:47–71. doi: 10.1146/annurev-bioeng-071811-150122. [DOI] [PubMed] [Google Scholar]
- 34.Miller KS, Connizzo BK, Feeney E, Tucker JJ, Soslowsky LJ. Examining differences in local collagen fiber crimp frequency throughout mechanical testing in a developmental mouse supraspinatus tendon model. J Biomech Eng. 2012;134:041004. doi: 10.1115/1.4006538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ciarletta P, Ben Amar M. A finite dissipative theory of temporary interfibrillar bridges in the extracellular matrix of ligaments and tendons. J R Soc Interface. 2009;6:909–924. doi: 10.1098/rsif.2008.0487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lake SP, Miller KS, Elliott DM, Soslowsky LJ. Effect of fiber distribution and realignment on the nonlinear and inhomogeneous mechanical properties of human supraspinatus tendon under longitudinal tensile loading. J Orthop Res. 2009;27:1596–1602. doi: 10.1002/jor.20938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmadzadeh H, Connizzo BK, Freedman BR, Soslowsky LJ, Shenoy VB. Determining the contribution of glycosaminoglycans to tendon mechanical properties with a modified shearlag model. J Biomech. 2013;46:2497–2503. doi: 10.1016/j.jbiomech.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Franchi M, Fini M, Quaranta M, et al. Crimp morphology in relaxed and stretched rat Achilles tendon. J Anat. 2007;210:1–7. doi: 10.1111/j.1469-7580.2006.00666.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miller KS, Connizzo BK, Feeney E, Soslowsky LJ. Characterizing local collagen fiber re-alignment and crimp behavior throughout mechanical testing in a mature mouse supraspinatus tendon model. J Biomech. 2012;45:2061–2065. doi: 10.1016/j.jbiomech.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]
- 41.Woo SL, Johnson GA, Smith BA. Mathematical modeling of ligaments and tendons. J Biomech Eng. 1993;115:468–473. doi: 10.1115/1.2895526. [DOI] [PubMed] [Google Scholar]
- 42.Peltonen J, Cronin NJ, Stenroth L, Finni T, Avela J. Viscoelastic properties of the Achilles tendon in vivo. Springerplus. 2013;2:212. doi: 10.1186/2193-1801-2-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang VM, Banack TM, Tsai CW, Flatow EL, Jepsen KJ. Variability in tendon and knee joint biomechanics among inbred mouse strains. J Orthop Res. 2006;24:1200–1207. doi: 10.1002/jor.20167. [DOI] [PubMed] [Google Scholar]
- 44.Neugebauer JM, Hawkins DA. Identifying factors related to Achilles tendon stress, strain, and stiffness before and after 6 months of growth in youth 10–14 years of age. J Biomech. 2012;45:2457–2461. doi: 10.1016/j.jbiomech.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Plate JF, Wiggins WF, Haubruck P, et al. Normal aging alters in vivo passive biomechanical response of the rat gastrocnemius-Achilles muscle-tendon unit. J Biomech. 2013;46:450–455. doi: 10.1016/j.jbiomech.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Beason DP, Kuntz AF, Hsu JE, Miller KS, Soslowsky LJ. Development and evaluation of multiple tendon injury models in the mouse. J Biomech. 2012;45:1550–3. doi: 10.1016/j.jbiomech.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chamberlain CS, Duenwald-Kuehl SE, Okotie G, Brounts SH, Baer GS, Vanderby R. Temporal Healing in Rat Achilles Tendon: Ultrasound Correlations. Ann Biomed Eng. 2013;41:477–487. doi: 10.1007/s10439-012-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wren TA, Lindsey DP, Beaupre GS, Carter DR. Effects of creep and cyclic loading on the mechanical properties and failure of human Achilles tendons. Ann Biomed Eng. 2003;31:710–717. doi: 10.1114/1.1569267. [DOI] [PubMed] [Google Scholar]
- 49.Fung DT, Wang VM, Andarawis-Puri N, et al. Early response to tendon fatigue damage accumulation in a novel in vivo model. J Biomech. 2010;43:274–279. doi: 10.1016/j.jbiomech.2009.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fung DT, Wang VM, Laudier DM, et al. Subrupture tendon fatigue damage. J Orthop Res. 2009;27:264–273. doi: 10.1002/jor.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peltonen J, Cronin NJ, Stenroth L, Finni T, Avela J. Achilles tendon stiffness is unchanged one hour after a marathon. J Exp Biol. 2012;215:3665–3671. doi: 10.1242/jeb.068874. [DOI] [PubMed] [Google Scholar]
- 52.Farris DJ, Trewartha G, McGuigan MP. The effects of a 30-min run on the mechanics of the human Achilles tendon. Eur J Appl Physiol. 2012;112:653–660. doi: 10.1007/s00421-011-2019-8. [DOI] [PubMed] [Google Scholar]
- 53.Lichtwark GA, Cresswell AG, Newsham-West RJ. Effects of running on human Achilles tendon length-tension properties in the free and gastrocnemius components. J Exp Biol. 2013;216:4388–94. doi: 10.1242/jeb.094219. [DOI] [PubMed] [Google Scholar]
- 54.Schechtman H, Bader DL. In vitro fatigue of human tendons. J Biomech. 1997;30:829–835. doi: 10.1016/s0021-9290(97)00033-x. [DOI] [PubMed] [Google Scholar]
- 55.Ehrlich HP, Lambert PA, Saggers GC, Myers RL, Hauck RM. Dynamic changes appearing in collagen fibers during intrinsic tendon repair. Ann Plast Surg. 2005;54:201–206. doi: 10.1097/01.sap.0000141380.52782.db. [DOI] [PubMed] [Google Scholar]
- 56.Hansen P, Kovanen V, Hölmich P, et al. Micromechanical properties and collagen composition of ruptured human achilles tendon. Am J Sports Med. 2013;41:437–443. doi: 10.1177/0363546512470617. [DOI] [PubMed] [Google Scholar]
- 57.Bring DK, Reno C, Renstrom P, Salo P, Hart DA, Ackermann PW. Joint immobilization reduces the expression of sensory neuropeptide receptors and impairs healing after tendon rupture in a rat model. J Orthop Res. 2009;27:274–280. doi: 10.1002/jor.20657. [DOI] [PubMed] [Google Scholar]
- 58.Jones GC, Corps AN, Pennington CJ, et al. Expression profiling of metalloproteinases and tissue inhibitors of metalloproteinases in normal and degenerate human achilles tendon. Arthritis Rheum. 2006;54:832–842. doi: 10.1002/art.21672. [DOI] [PubMed] [Google Scholar]
- 59.Karousou E, Ronga M, Vigetti D, Passi A, Maffulli N. Collagens, proteoglycans, MMP-2, MMP-9 and TIMPs in human achilles tendon rupture. Clin Orthop Relat Res. 2008;466:1577–1582. doi: 10.1007/s11999-008-0255-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moerch L, Pingel J, Boesen M, Kjaer M, Langberg H. The effect of acute exercise on collagen turnover in human tendons: influence of prior immobilization period. Eur J Appl Physiol. 2013;113:449–455. doi: 10.1007/s00421-012-2450-5. [DOI] [PubMed] [Google Scholar]
- 61.Mendias CL, Gumucio JP, Lynch EB. Mechanical loading and TGF-beta change the expression of multiple miRNAs in tendon fibroblasts. J Appl Physiol. 1985;113:56–62. doi: 10.1152/japplphysiol.00301.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharir A, Zelzer E. Tendon homeostasis: the right pull. Curr Biol. 2011;21:R472–474. doi: 10.1016/j.cub.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 63.Thornton GM, Shao X, Chung M, et al. Changes in mechanical loading lead to tendonspecific alterations in MMP and TIMP expression: influence of stress deprivation and intermittent cyclic hydrostatic compression on rat supraspinatus and Achilles tendons. Br J Sports Med. 2010;44:698–703. doi: 10.1136/bjsm.2008.050575. [DOI] [PubMed] [Google Scholar]
- 64.Eliasson P, Andersson T, Aspenberg P. Rat Achilles tendon healing: mechanical loading and gene expression. J Appl Physiol. 1985;107:399–407. doi: 10.1152/japplphysiol.91563.2008. [DOI] [PubMed] [Google Scholar]
- 65.Sasaki K, Yamamoto N, Kiyosawa T, Sekido M. The role of collagen arrangement change during tendon healing demonstrated by scanning electron microscopy. J Electron Microsc (Tokyo) 2012;61:327–334. doi: 10.1093/jmicro/dfs057. [DOI] [PubMed] [Google Scholar]
- 66.Enwemeka CS. Inflammation, cellularity, and fibrillogenesis in regenerating tendon: implications for tendon rehabilitation. Phys Ther. 1989;69:816–825. doi: 10.1093/ptj/69.10.816. [DOI] [PubMed] [Google Scholar]
- 67.Schepull T, Kvist J, Aspenberg P. Early E-modulus of healing Achilles tendons correlates with late function: similar results with or without surgery. Scand J Med Sci Sports. 2010;22:18–23. doi: 10.1111/j.1600-0838.2010.01154.x. [DOI] [PubMed] [Google Scholar]
- 68.Maquirriain J. Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med. 2011;84:289–300. [PMC free article] [PubMed] [Google Scholar]
- 69.Freedman BR SJ, Buckley MR, Voleti PB, Soslowsky LJ. Biomechanical and structural response of healing Achilles tendon to fatigue loading following acute injury. doi: 10.1016/j.jbiomech.2013.10.054. (in review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chamberlain CS, Duenworld-Kuehl SE, Okotie G, Brounts SH, Baer GS, Vanderby R. Temporal healing in rat achilles tendon: ultrasound correlations. Ann Biomed Eng. 2013;41:477–487. doi: 10.1007/s10439-012-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Okotie G, Duenwald-Kuehl S, Kobayashi H, Wu MJ, Vanderby R. Tendon strain measurements with dynamic ultrasound images: evaluation of digital image correlation. J Biomech Eng. 2012;134:024504. doi: 10.1115/1.4006116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Riggin CN, Sarver JJ, Freedman BR, Thomas SJ, Soslowsky LJ. Analysis of Collagen Organization in Mouse Achilles Tendon Using High-Frequency Ultrasound Imaging. J Biomech Eng. 2013 doi: 10.1115/1.4026285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cho NS, Hwang JH, Lee YT, Chae SW. Tendinosis-like histologic and molecular changes of the Achilles tendon to repetitive stress: a pilot study in rats. Clin Orthop Relat Res. 2011;469:3172–3180. doi: 10.1007/s11999-011-2000-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ikoma K, et al. Effects of stress-shielding on the dynamic viscoelasticity and ordering of the collagen fibers in rabbit Achilles tendon. J Orthop Res. 2013;31:1708–12. doi: 10.1002/jor.22424. [DOI] [PubMed] [Google Scholar]
- 75.Ng GY, Chung PY, Wang JS, Cheung RT. Enforced bipedal downhill running induces Achilles tendinosis in rats. Connect Tissue Res. 2011;52:466–471. doi: 10.3109/03008207.2011.562334. [DOI] [PubMed] [Google Scholar]
- 76.Glazebrook MA, Wright JR, Jr, Langman M, Stanish WD, Lee JM. Histological analysis of achilles tendons in an overuse rat model. J Orthop Res. 2008;26:840–846. doi: 10.1002/jor.20546. [DOI] [PubMed] [Google Scholar]
- 77.Dirks RC, Galley MR, Childress PJ, et al. Uphill treadmill running does not induce histopathological changes in the rat Achilles tendon. BMC Musculoskelet Disord. 2013;14:90. doi: 10.1186/1471-2474-14-90. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Veres SP, Harrison JM, Lee JM. Repeated subrupture overload causes progression of nanoscaled discrete plasticity damage in tendon collagen fibrils. J Orthop Res. 2013;31:731–737. doi: 10.1002/jor.22292. [DOI] [PubMed] [Google Scholar]
- 79.Dunkman AA, Buckley MR, Mienaltowski MJ, et al. Decorin Expression Is Required for Age-Related Changes in Tendon Structure and Mechanical Properties. Matrix Biol. 2013;32:3–13. doi: 10.1016/j.matbio.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Provenzano PP, Vanderby R., Jr Collagen fibril morphology and organization: implications for force transmission in ligament and tendon. Matrix Biol. 2006;25:71–84. doi: 10.1016/j.matbio.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 81.Elliott DM, Robinson PS, Gimbel JA, et al. Effect of altered matrix proteins on quasilinear viscoelastic properties in transgenic mouse tail tendons. Ann Biomed Eng. 2003;31:599–605. doi: 10.1114/1.1567282. [DOI] [PubMed] [Google Scholar]
- 82.Lakes R. Viscoelastic Materials. Cambridge University Press; 2009. [Google Scholar]
- 83.Eliasson P, Andersson T, Aspenberg P. Achilles tendon healing in rats is improved by intermittent mechanical loading during the inflammatory phase. J Orthop Res. 2012;30:274–279. doi: 10.1002/jor.21511. [DOI] [PubMed] [Google Scholar]
- 84.Eliasson P, Andersson T, Hammerman M, Aspenberg P. Primary gene response to mechanical loading in healing rat Achilles tendons. J Appl Physiol. 1985;114:1519–1526. doi: 10.1152/japplphysiol.01500.2012. [DOI] [PubMed] [Google Scholar]
- 85.Andersson T, Eliasson P, Hammerman M, Sandberg O, Aspenberg P. Low-level mechanical stimulation is sufficient to improve tendon healing in rats. J Appl Physiol. 1985;113:1398–1402. doi: 10.1152/japplphysiol.00491.2012. [DOI] [PubMed] [Google Scholar]
- 86.Keller BV, Davis ML, Thompson WR, Dahners LE, Weinhold PS. Varying whole body vibration amplitude differentially affects tendon and ligament structural and material properties. J Biomech. 2013;46:1496–1500. doi: 10.1016/j.jbiomech.2013.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schepull T, Aspenberg P. Early Controlled Tension Improves the Material Properties of Healing Human Achilles Tendons After Ruptures: A Randomized Trial. Am J Sports Med. 2013 doi: 10.1177/0363546513501785. [DOI] [PubMed] [Google Scholar]
- 88.Williams DS, Zambardino JA, Banning VA. Transverse-plane mechanics at the knee and tibia in runners with and without a history of achilles tendonopathy. J Orthop Sports Phys Ther. 2008;38:761–767. doi: 10.2519/jospt.2008.2911. [DOI] [PubMed] [Google Scholar]
- 89.Almonroeder T, Willson JD, Kernozek TW. The effect of foot strike pattern on achilles tendon load during running. Ann Biomed Eng. 2013;41:1758–1766. doi: 10.1007/s10439-013-0819-1. [DOI] [PubMed] [Google Scholar]
- 90.Liang JI, et al. Video-based gait analysis for functional evaluation of healing achilles tendon in rats. Ann Biomed Eng. 2012;40:2532–2540. doi: 10.1007/s10439-012-0619-z. [DOI] [PubMed] [Google Scholar]
- 91.Wu MM, Pai DK, Tresch MC, Sandercock TG. Passive elastic properties of the rat ankle. J Biomech. 2012;45:1728–1732. doi: 10.1016/j.jbiomech.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen XM, Cui Lg, He P, Shen WW, Qian YJ, Wang JR. Shear wave elastographic characterization of normal and torn achilles tendons: a pilot study. J Ultrasound Med. 2013;32:449–455. doi: 10.7863/jum.2013.32.3.449. [DOI] [PubMed] [Google Scholar]
- 93.Brown PG, Alsousou J, Cooper A, Thompson MS, Noble JA. The AutoQual ultrasound elastography method for quantitative assessment of lateral strain in post-rupture Achilles tendons. J Biomech. 2013 doi: 10.1016/j.jbiomech.2013.07.044. [DOI] [PubMed] [Google Scholar]
- 94.Ellison M, Kobayashi H, Delaney F, et al. Feasibility and repeatability for in vivo measurements of stiffness gradients in the canine gastrocnemius tendon using an acoustoelastic strain gauge. Vet Radiol Ultrasound. 2013;54:548–554. doi: 10.1111/vru.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Killian ML, Cavinatto L, Galatz LM, Thomopoulos S. The role of mechanobiology in tendon healing. J Shoulder Elbow Surg. 2012;21:228–237. doi: 10.1016/j.jse.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ansorge HL, Hau JE, Edelstein L, Adams Birk DE, Soslowsky LJ. Recapitulation of the Achilles tendon mechanical properties during neonatal development: a study of differential healing during two stages of development in a mouse model. J Orthop Res. 2012;30:448–456. doi: 10.1002/jor.21542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Beredjiklian PK, Favata M, Cartmell JS, Flanagan ZL, Crombleholme TM, Soslowsky LJ. Regenerative versus reparative healing in tendon: a study of biomechanical and histological properties in fetal sheep. Ann Biomed Eng. 2003;31:1143–1152. doi: 10.1114/1.1616931. [DOI] [PubMed] [Google Scholar]
- 98.Hurle JM, Hinchliffe JR, Ros MA, Critchlow MA, Genis-Galvez JM. The extracellular matrix architecture relating to myotendinous pattern formation in the distal part of the developing chick limb: an ultrastructural, histochemical and immunocytochemical analysis. Cell Differ Dev. 1989;27:103–120. doi: 10.1016/0922-3371(89)90740-5. [DOI] [PubMed] [Google Scholar]
- 99.Brent AE, Tabin CJ. FGF acts directly on the somitic tendon progenitors through the Ets transcription factors Pea3 and Erm to regulate scleraxis expression. Development. 2004;131:3885–3896. doi: 10.1242/dev.01275. [DOI] [PubMed] [Google Scholar]
- 100.Schweitzer R, Chyung JH, Murtaugh LC, et al. Analysis of the tendon cell fate using Scleraxis, a specific marker for tendons and ligaments. Development. 2001;128:3855–3866. doi: 10.1242/dev.128.19.3855. [DOI] [PubMed] [Google Scholar]
- 101.Schweitzer R, Zelzer E, Volk T. Connecting muscles to tendons: tendons and musculoskeletal development in flies and vertebrates. Development. 2010;137:2807–2817. doi: 10.1242/dev.047498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pryce BA, Watson SS, Murchison ND, Staverosky JA, Dünker N, Schweitzer R. Recruitment and maintenance of tendon progenitors by TGFbeta signaling are essential for tendon formation. Development. 2009;136:1351–1361. doi: 10.1242/dev.027342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guerquin MJ, Betz O, Ochsner PE, Liu F, Porter RM, Evans CH. Transcription factor EGR1 directs tendon differentiation and promotes tendon repair. J Clin Invest. 2013;123:3564–3576. doi: 10.1172/JCI67521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Majewski M, Betz O, Ochsner PE, Liu F, Porter RM, Evans CH. Ex vivo adenoviral transfer of bone morphogenetic protein 12 (BMP-12) cDNA improves Achilles tendon healing in a rat model. Gene Ther. 2008;15:1139–1146. doi: 10.1038/gt.2008.48. [DOI] [PubMed] [Google Scholar]
- 105.Chen CH, Cao Y, Wu YF, Bais AJ, Gao JS, Tang JB. Tendon healing in vivo: gene expression and production of multiple growth factors in early tendon healing period. J Hand Surg Am. 2008;33:1834–1842. doi: 10.1016/j.jhsa.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 106.Muttini A, Salini V, Valbonetti L, Abate M. Stem cell therapy of tendinopathies: suggestions from veterinary medicine. Muscles Ligaments Tendons J. 2012;2:187–192. [PMC free article] [PubMed] [Google Scholar]
- 107.Yin Z, Chen X, Zhu T, et al. The effect of decellularized matrices on human tendon stem/progenitor cell differentiation and tendon repair. Acta Biomater. 2013 doi: 10.1016/j.actbio.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 108.Ning LJ, Zhang Y, Chen XH, et al. Preparation and characterization of decellularized tendon slices for tendon tissue engineering. J Biomed Mater Res A. 2012;100:1448–1456. doi: 10.1002/jbm.a.34083. [DOI] [PubMed] [Google Scholar]
- 109.Huang TF, Yew TL, Chiang ER, et al. Mesenchymal stem cells from a hypoxic culture improve and engraft Achilles tendon repair. Am J Sports Med. 2013;41:1117–1125. doi: 10.1177/0363546513480786. [DOI] [PubMed] [Google Scholar]
- 110.Philip J, Hackl F, Canseco JA, et al. Amnion-derived multipotent progenitor cells improve achilles tendon repair in rats. Eplasty. 2013;13:e31. [PMC free article] [PubMed] [Google Scholar]
- 111.Bell KJ, Fulcher ML, Rowlands DS, Kerse N. Impact of autologous blood injections in treatment of mid-portion Achilles tendinopathy: double blind randomised controlled trial. BMJ. 2013;346:f2310. doi: 10.1136/bmj.f2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Parafioriti A, Armiraglio E, Del Bianco S, Tibalt E, Oliva F, Berardi AC. Single injection of platelet-rich plasma in a rat Achilles tendon tear model. Muscles Ligaments Tendons J. 2011;1:41–47. [PMC free article] [PubMed] [Google Scholar]
- 113.Al-Abbad H, Simon JV. The effectiveness of extracorporeal shock wave therapy on chronic achilles tendinopathy: a systematic review. Foot Ankle Int. 2013;34:33–41. doi: 10.1177/1071100712464354. [DOI] [PubMed] [Google Scholar]
- 114.Webb WR, Dale TP, Lomas AJ, et al. The application of poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) scaffolds for tendon repair in the rat model. Biomaterials. 2013;34:6683–6694. doi: 10.1016/j.biomaterials.2013.05.041. [DOI] [PubMed] [Google Scholar]
- 115.Kaux JF, Drion P, Libertiaux V, et al. Tendon tissue engineering and its role on healing of the experimentally induced large tendon defect model in rabbits: a comprehensive in vivo study. PLoS One. 2013;8:e73016. doi: 10.1371/journal.pone.0073016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Oryan A, Moshiri A, Parizi Meimandi A, Silver IA. A long-term in vivo investigation on the effects of xenogenous based, electrospun, collagen implants on the healing of experimentally-induced large tendon defects. J Musculoskelet Neuronal Interact. 2013;13:315–329. [PubMed] [Google Scholar]
- 117.Reverchon E, Baldino L, Cardea S, De Marco I. Biodegradable synthetic scaffolds for tendon regeneration. Muscles Ligaments Tendons J. 2012;2:181–186. [PMC free article] [PubMed] [Google Scholar]
- 118.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal. Basic principles and recommendations in clinical and field science research. MLTJ. 2013;4:250–252. [PMC free article] [PubMed] [Google Scholar]
- 119.Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360–366. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 120.Horstmann T, Jud HM, Frohlich V, Mundermann A, Grau S. Whole-body vibration versus eccentric training or a wait-and-see approach for chronic Achilles tendinopathy: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43:794–803. doi: 10.2519/jospt.2013.4762. [DOI] [PubMed] [Google Scholar]
- 121.Knobloch K. Eccentric training in Achilles tendinopathy: is it harmful to tendon microcirculation? Br J Sports Med. 2007;41:e2. doi: 10.1136/bjsm.2006.030437. ; discussion e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Maffulli N, Walley G, Sayana MK, Longo UG, Denaro V. Eccentric calf muscle training in athletic patients with Achilles tendinopathy. Disabil Rehabil. 2008;30:1677–1684. doi: 10.1080/09638280701786427. [DOI] [PubMed] [Google Scholar]
- 123.Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med. 2007;35:374–383. doi: 10.1177/0363546506295940. [DOI] [PubMed] [Google Scholar]
- 124.Kaux JF, Drion P, Libertiaux V, et al. Eccentric training improves tendon biomechanical properties: a rat model. J Orthop Res. 2013;31:119–124. doi: 10.1002/jor.22202. [DOI] [PubMed] [Google Scholar]