Abstract
SUMMARY
Bloodstream infection (BSI) is a major cause of infectious disease morbidity and mortality worldwide. While a positive blood culture is mandatory for establishment of the presence of a BSI, there are a number of determinants that must be considered for establishment of this entity. Community-onset BSIs are those that occur in outpatients or are first identified <48 h after admission to hospital, and they may be subclassified further as health care associated, when they occur in patients with significant prior health care exposure, or community associated, in other cases. The most common causes of community-onset BSI include Escherichia coli, Staphylococcus aureus, and Streptococcus pneumoniae. Antimicrobial-resistant organisms, including methicillin-resistant Staphylococcus aureus and extended-spectrum β-lactamase/metallo-β-lactamase/carbapenemase-producing Enterobacteriaceae, have emerged as important etiologies of community-onset BSI.
INTRODUCTION
Bloodstream infection (BSI) is a major cause of infectious disease morbidity and mortality worldwide (1–15). Due to a number of determinants, not limited to changing population demographics, shifts in health care delivery models, and increasing globalization, the epidemiology of community-onset BSI has been changing in recent decades. In addition, antimicrobial-resistant organisms, most notably methicillin-resistant Staphylococcus aureus (MRSA) and extended-spectrum β-lactamase (ESBL)/metallo-β-lactamase-producing Enterobacteriaceae, have emerged as important etiologies of community-onset BSI. However, despite its importance and extensive investigation, as a result of inconsistent application of definitions and a reliance on hospital-based studies that are highly subject to a range of potential biases, the burden of community-onset BSI has not been well summarized.
Knowledge of the epidemiology and microbiology of community-onset BSI is needed to assess its impact on the health of the world community and to provide a basis from which development of interventional strategies may be created. Obtaining that epidemiological and microbiological knowledge first requires a detailed understanding of the technical and clinical factors that constitute a community-onset BSI. These factors include how a community-onset BSI is detected and the determinants influencing its ascertainment, including understanding the roles of different organisms as etiologic agents of community-onset BSI, the importance of utilizing study designs that minimize bias, and the use of definitions that are concise, unambiguous, and clinically relevant.
The primary objective of this report was therefore to provide a state-of-the-art review of the population-based incidence and microbiology of community-onset BSI. However, unlike the case with hospital-onset/nosocomial infections, for which widely accepted definitions exist and hospitalized patients represent a captive population for surveillance, establishment of the burden of community-onset BSI is more methodologically challenging and complex. Within this report, we therefore first review methodological issues surrounding establishment of the diagnosis of community-onset BSI. Key themes in this area include the provision of rational and precise definitions, determinants of positivity, and the importance of classification of community-onset BSIs into community-associated and health care-associated community-onset BSIs. In the second part of the report, we conduct a detailed review of the published population-based literature in order to first define the overall and then the species- or organism group-specific burden of community-onset BSI. Following this, we briefly highlight the importance of the emergence of resistant organisms as agents of community-onset BSI.
ESTABLISHING THE PRESENCE OF AND DEFINING COMMUNITY-ONSET BLOODSTREAM INFECTION
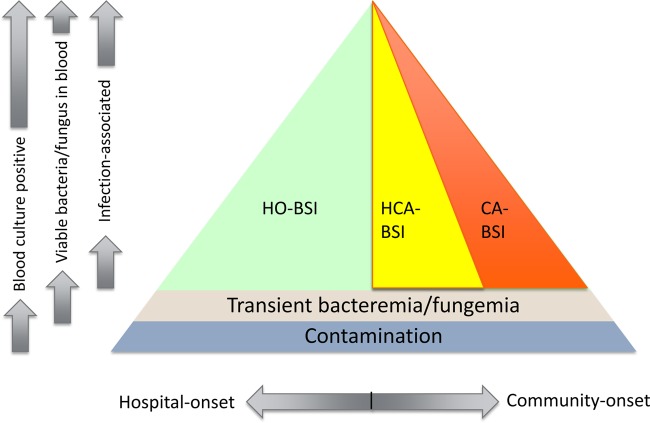
There are a number of diagnostic and classification considerations related to ascertainment of the presence of a BSI episode. However, definitions of BSI, especially with regard to community-onset disease, are not consistently used and applied in studies. For this review, precise and unambiguous definitions were identified, and these are listed in Table 1. Although no single definition has been accepted as a reference standard, BSI is generally deemed to be present when an organism associated with disease is cultured from the blood of an infected patient. It is therefore requisite in any definition of BSI that a positive blood culture for one or more organisms be demonstrated. However, a positive blood culture does not necessarily imply BSI. Positive blood cultures may arise in three main different settings, namely, contamination and true positivity in the absence or presence of associated clinical disease. Figure 1 shows the diagnostic hierarchy involved in establishing the presence of a community-onset BSI. It should be noted that organisms that may not be cultured from blood may be detected by using other methods, such as antigen detection or nucleic acid-based techniques. While future definitions may include these cases, present definitions are limited to those that demonstrate growth in blood cultures.
TABLE 1.
Definitions of bloodstream infection and associated entities
| Entity | Definition |
|---|---|
| Contamination of blood cultures | Blood cultures are positive for growth due to organisms that were not present in the bloodstream |
| Bacteremia | Presence of viable bacteria in the blood; blood cultures positive for bacterial growth where contamination has been ruled out |
| Fungemia | Presence of viable fungi in the blood; blood cultures positive for fungal growth where contamination has been ruled out |
| Transient bacteremia/fungemia | Brief episode of bacteremia/fungemia that is not associated with infection |
| Bloodstream infection | Bacteremia/fungemia that is associated with infection |
| Hospital-onset bloodstream infection | Bloodstream infection that is first identified (culture drawn) ≥48 h after hospital admission and within 48 h following hospital discharge |
| Community-onset bloodstream infection | Bloodstream infection occurring in an outpatient or first identified (culture drawn) <48 h following admission to hospital |
| Health care-associated community-onset bloodstream infection | Community-onset bloodstream infection associated with significant prior health care exposure (as evidenced by recent hospitalization, specialized in-home medical services, care in a hospital-based clinic or hemodialysis unit, or residence in a nursing home) |
| Community-associated community-onset bloodstream infection | Community-onset bloodstream infection not fulfilling criteria for health care-associated infection |
| Polymicrobial bloodstream infection | Episode of bloodstream infection associated with two or more different organisms isolated within 48 h of each other |
FIG 1.
Diagnostic hierarchy from positive blood cultures to community-onset bloodstream infection. BSI, bloodstream infection; HO, hospital onset; HCA, health care associated; CA, community associated. The overall triangular area indicates all positive blood cultures, which may represent contamination (first level), transient bacteremia/fungemia (second level), or “true” BSI (third level). Bloodstream infections are further classified into the three mutually exclusive categories of hospital-associated, health care-associated community-onset, and community-associated community-onset BSIs.
Contamination (pseudobacteremia) occurs when cultures are positive due to organisms not present in the bloodstream and arises as a result of inadequate sterile technique in obtaining and/or processing blood culture specimens. The terms “bacteremia” and “fungemia” are defined by the presence of viable bacteria and fungi in the blood, respectively. These may be operationalized as positive blood cultures in cases where contamination has been excluded. The term “bacteremia” is frequently used interchangeably with “BSI.” However, these terms are not synonymous, and there are two important distinctions. First, the term “BSI” is more comprehensive, in that it encompasses both bacterial and fungal etiologies. Second, implicit within the term “bloodstream infection” is that the positive blood culture is associated with clinical infection. While most bacteremias are associated with infections, transient bacteremias may occasionally be observed following minor manipulations of nonsterile body surfaces that are not infection associated (16–26).
Determinants of Blood Culture Positivity
Documentation of a positive blood culture is a mandatory step in BSI diagnosis. A blood culture or culture set (one or more bottles) containing broth media is immediately inoculated with a volume of blood collected under aseptic conditions, preferably by venipuncture. While blood may be drawn through indwelling intravascular catheters, at least one set of blood cultures should be collected by venipuncture (27–29). Use of a single needle for blood draw and inoculation is recommended (30, 31). Although there are a number of clinical and laboratory-based determinants that lead to a positive blood culture, this review focuses on the most clinically relevant determinants in community-based patients. An extensive review of this topic was previously published within this journal (32).
Blood culture sampling and bloodstream infection diagnosis.
Practices related to sampling of patients with suspected BSI will influence its presence. In the extreme case, if a specimen is not submitted for culture, diagnosis of BSI is precluded. In contrast, liberal sampling for blood cultures may result in higher rates of detection (33). Studies conducted at the population level have correlated the rate of submission of cultures with the rate of detection of BSI (8). However, whether there is a threshold at which this effect is not further observed remains to be determined.
The volume of blood drawn is associated with the probability of detecting a patient with bacteremia. Some conditions, such as endocarditis and septic thrombophlebitis, are associated with a continuous bacteremia where a sustained high organism load is present in the bloodstream, and cultures will be positive even if small volumes of blood are drawn for culture. However, with most other infections, lower organism loads are present and larger volumes of blood are required to increase the probability of detection. Contemporary studies reviewing multiple 20-ml blood cultures drawn in a 24-h period have indicated that among patients with bacteremia, approximately 70% will have positive cultures after the first draw, 85% after the second, 97% after the third, and >99% after the fourth (34, 35). While the ability to detect positive blood cultures with repeated draws over time may reflect detection of intermittent bacteremia, it most likely reflects a greater total volume of blood drawn (36). Inclusion of an anaerobic bottle as part of a blood culture set enables the detection of anaerobes, increases the probability of detecting facultative anaerobes, and shortens the time to detection for some fastidious organisms (37, 38).
Bloodstream infection may arise as a primary infection or may be secondary to a focal infection at a defined body site, most commonly arising from the respiratory, gastrointestinal, and urogenital tracts (32, 39). Endocarditis, meningitis, and septic shock typically have high rates of blood culture positivity, while other conditions, such as soft tissue infection, have very low rates (40).
Influence of blood culture systems and other laboratory-based determinants.
There are many different laboratory protocols and procedures possible for blood culture. However, most modern laboratories utilize automated incubation and detection systems, due to their higher efficiency, lower risk for contamination, and requirement for shorter duration of incubation than those of manual blood culture approaches (35, 41–45). Although various media and detection systems are used with different commercially available automated systems, generally speaking, performances are comparable provided that similar volumes of blood are cultured. However, the use of media containing charcoal or resins improves the recovery of organisms in the presence of antimicrobials, and the use of specialized media enhances the recovery of anaerobes, mycobacteria, and fungi (46, 47). A detailed review of these aspects has been published previously (32).
Determining the Significance of Positive Blood Cultures
Following exclusion of contamination, it is important to ascertain whether bacteremia/fungemia is infection associated (i.e., BSI) or not. However, there is no widely accepted “gold standard” for defining these different entities. In most cases, integration of clinical, laboratory, and microbiological factors is required (48).
Factors to consider in classifying positive blood cultures.
(i) Identified organism(s).
Isolation of organisms from an aseptically obtained and processed blood sample indicates BSI in most cases. However, there are a number of skin commensal organisms that, when growing in blood cultures, represent contaminants (i.e., false-positive blood cultures) in the majority of cases. These organisms include coagulase-negative staphylococci (CoNS), Bacillus spp. (not Bacillus anthracis), Micrococcus spp., Corynebacterium spp. (not Corynebacterium jeikieum), and Propionibacterium acnes (48). Among immunocompetent patients who do not have an indwelling prosthetic device, such as an intravascular catheter, these organisms are rare but possible causes of community-onset BSI (49). Viridans group streptococci are occasional blood culture contaminants, although when not infection associated they may represent transient bacteremia from a dental or upper gastrointestinal source rather than contamination per se. In the absence of advanced immune suppression, identification of molds in blood cultures usually indicates environmental contamination. In contrast, isolation of yeasts and dimorphic fungi in blood cultures invariably indicates fungemia and BSI.
(ii) Number and timing of positive cultures.
Adequate sampling volume is the single most important factor for detecting BSI. The Clinical and Laboratory Standards Institute (CLSI) guidelines recommend four 10-ml bottles of blood (e.g., two sets of blood cultures, each consisting of an aerobic and an anaerobic bottle, equivalent to 40 ml of blood) to be taken for the initial evaluation in order to detect about 90 to 95% of bacteremias. A third blood culture set (i.e., an additional 20 ml of blood) increases the detection rate to 95 to 99% (39, 50). Recent studies also suggest that even larger blood volumes may need to be cultured in order to achieve the optimal recovery of specific organisms and that larger blood volumes also decrease the detection time for common pathogens (34, 51). Lee and colleagues showed that Staphylococcus aureus bacteremia was detected in the first blood culture ∼90% of the time, whereas only 60% of Pseudomonas aeruginosa bacteremia cases and candidemia cases due to Candida albicans were detected with only a single blood culture (34). Similar data were found for polymicrobial episodes, where only 67% of all the organisms present were detected with the first blood culture, but most of them (99.1%) were detected by the third blood culture (34).
For common skin contaminants, the number of positive cultures may be used as a means of differentiating contamination from bacteremia. However, most of the published literature in this regard has focused on hospital-onset coagulase-negative staphylococcal infections (48, 49, 52–55). Based on this literature, a single positive culture represents contamination in 75 to 95% of cases. In a patient with bacteremia, there is a high likelihood (>75%) of a second blood culture growing the same organism as that from the initial draw (39). However, a second blood culture is not usually positive when the initial isolate is a contaminant. Although less well defined, the time to culture positivity has also been used to establish the presence of contamination, with earlier positivity being suggestive of bacteremia (48, 56).
(iii) Transient bacteremia.
On occasion, low-grade bacteremia may occur that is transient (i.e., lasting less than 30 min) and not associated with infection. Transient bacteremia is a “true” bacteremia in that viable organisms are present in the bloodstream (i.e., not contaminants), but it is not a BSI because it is not infection associated. There are a number of well-recognized causes of transient bacteremia, and these generally involve manipulation of colonized or contaminated mucosal surfaces, including dental manipulations (16–19), endoscopic gastrointestinal procedures (20–23), and invasive respiratory procedures (24, 25). Transrectal needle prostate biopsy is associated with transient bacteremia in approximately 20% of cases, and this may subsequently evolve into BSI (26).
(iv) Clinical variables.
A BSI may be confirmed if an evident infective focus is temporally associated with a positive blood culture. A focus may be documented clinically and/or microbiologically by isolation of the same species from a normally sterile body site, such as cerebrospinal, synovial, or pleural fluid or samples obtained from deep-tissue aspirates. However, determination of a focus of infection is often less overt, and by definition, no focus of infection is present in primary BSI. In these cases, other parameters are often employed to classify positive blood cultures as contaminants or as infection associated or not. The presence of fever and an elevated white blood cell count are often cited as important determinants, but these alone are only weakly associated with BSI. Along with the number of positive blood cultures, the presence of an indwelling catheter, hypotension, and an increasing number of criteria for systemic inflammatory response syndrome (SIRS) will increase the probability of a BSI with potential blood culture contaminants (52, 55). Some criteria utilize whether patients are treated with antimicrobials to define a BSI. However, this factor may simply be a marker of excessive therapy rather than proof of BSI per se (57).
Approaches to classification of positive blood cultures.
With individual patient care, a clinician determines the presence of a BSI based on an integration of available microbiological, clinical, and radiologic information. However, such an individualized approach has significant limitations for surveillance and research purposes. Use of standardized definitions and algorithms has been developed in an attempt to improve consistency (52), although where a subjective component is included, substantial interobserver variability has been a major problem (58). In part as an attempt to promote consistency, but also efficiency, electronic surveillance systems have been developed and increasingly reported in recent years (59–61).
Classification of Community-Onset Bloodstream Infections
Traditionally, BSIs were classified as community-acquired or nosocomial infections (62). Community-acquired BSIs were those deemed to be present prior to or incubating at hospital admission, and nosocomial BSIs were those acquired after admission to hospital. Two important challenges have arisen with the use of such a binary definition. First, it is very difficult to objectively determine the true acquisition of infecting isolates, and interobserver variation in application of these definitions is a major problem (58). Second, shifts in health care delivery models have changed dramatically in recent years, with much higher levels of complex medical care (such as home hemodialysis and outpatient parenteral antimicrobial therapy) being delivered in the community setting. As a result, it is increasingly recognized that community-based patients may have infections that are hospital associated/acquired.
New classification schemes have been developed in order to address the challenges associated with the traditional binary definitions (63, 64). Classification of infections as either community-onset or hospital-onset infections provides a discrete and objective means of classification. In this regard, community-onset infections can be defined as occurring among outpatients or those first identified (cultures drawn) within 2 days (<48 h) of admission to hospital, and hospital-onset infections can be defined as those where culture is first identified 2 or more days (≥48 h) following hospital admission or within 2 days (<48 h) of hospital discharge (63). In addition, community-onset infections may be subclassified further as health care associated or community associated, based on prior exposure of patients to significant health care or not, respectively (65). It is important that while these new categories are likely reflective of the location of acquisition of infection, this is not necessarily the case.
Community-associated versus health care-associated community-onset disease.
Morin and Hadler first proposed categorization of community-onset BSI into further subcategories that included previously hospitalized patients (health care-associated community-onset BSI) and those patients not recently admitted, either with or without comorbid medical illnesses (63). Friedman and colleagues later proposed categorizing patients with community-onset BSI into those having either health care-associated or community-acquired disease, and these categories were subsequently widely recognized (65). Their definition of health care-associated community-onset BSI included at least one of the following: patients who had recently been hospitalized and patients who received recent specialized medical services in the home, who attended a hospital-based clinic or hemodialysis unit, or who were nursing home residents. Patients who did not have at least one of these criteria had community-acquired BSI. In order to avoid confusion with the previous binary definitions, we use the term “community-associated disease” in preference to “community-acquired BSI” in referring to community-onset disease not associated with prior health care exposure.
There have been a number of investigations that have sought to validate the entity of health care-associated community-onset BSI as distinct from community-associated and hospital-onset BSIs. Studies not limited to specific etiologies are summarized in Table 2 (50, 65–70). While definitions and study populations have varied to some degree, compared to community-associated BSIs, health care-associated BSIs are more likely in older patients with comorbid illness, have a different distribution of pathogens (higher rates of Staphylococcus aureus and Pseudomonas aeruginosa and lower rates of Streptococcus pneumoniae and Escherichia coli), have higher rates of antimicrobial resistance, and are more lethal (65). Health care-associated infections are readily definable using objective criteria and, as a result, are readily applicable for use in electronic surveillance systems (71). However, because not all patients with community-onset BSI are admitted to hospital, surveillance systems that do not ascertain all cases of community-onset BSI, with admittance to hospital or not, will be subject to a selection bias that may challenge the ability to adequately define the problem and provide a rational basis for devising potential preventative strategies.
TABLE 2.
Studies comparing health care-associated (HCA) and community-associated (CA) community-onset BSIs
| First author (reference) | Setting/population | HCA BSI definition | Patient differences (vs CA BSI) | Microbiology (vs CA BSI) | Outcome difference (vs CA BSI) |
|---|---|---|---|---|---|
| Friedman (65) | Adults admitted to three hospitals in North Carolina (143 with CA BSI and 186 with HCA BSI) | Community-onset BSI with any specialized therapy in the home, recent attendance at a hospital, hemodialysis, or chemotherapy clinic, recent hospitalization, or residence in a nursing home | More likely to have cancer and renal failure with HCA BSI, and less likely to have HIV infection | Urinary tract infection more common in CA BSI; Staphylococcus aureus most common in HCA BSI and Escherichia coli and Streptococcus pneumoniae most common in CA BSI; MRSA much more common in HCA BSI | 3- to 6-month mortality higher (29% versus 16%; P = 0.019) for HCA BSI than for CA BSI |
| Lenz (66) | Adult residents of Calgary, Canada (3,088 with CA BSI and 2,492 with HCA BSI) | Minor modification of criteria of Friedman et al. (60, 65) | Older, more comorbid illness with HCA BSI | Different distribution of pathogens and higher rates of resistant organisms, including MRSA; more polymicrobial infections with HCA BSI | Longer length of stay and higher 28-day case fatality rate (18% versus 10%; P < 0.001) with HCA BSI |
| Al-Hasan (67) | Gram-negative BSI in residents of Olmsted County, MN (306 with HCA BSI and 427 with CA BSI) | Per criteria of Friedman et al. (65) | Patients with HCA BSI were older | Different distribution of infection foci and pathogens; higher rates of resistance with HCA BSI | Higher 28-day case fatality rate (15% versus 4%; P < 0.001) with HCA BSI |
| Son (50) | Patients admitted to nine university hospitals in Korea (380 with CA BSI and 206 with HCA BSI) | Per criteria of Friedman et al. (65) | Patients with HCA BSI more likely to be male and to have comorbidities and immune-suppressant therapy | Different distribution of infection foci and pathogens; higher rates of resistance with HCA BSI | Higher 30-day case fatality rate (18% versus 10%; P = 0.007) with HCA BSI |
| Kollef (68) | Adults admitted to seven hospitals in the United States (728 [64%] with HCA BSI and 415 with CA BSI) | Recent hospitalization, immune suppression, hemodialysis, or nursing home residence | Patients with HCA BSI were older and more likely to be male and to have comorbidities and a higher severity of illness | Different distribution of infection pathogens; higher rates of primary BSI and resistance with HCA BSI | Higher hospital case fatality (14% versus 4%; P < 0.001) with HCA BSI |
| Evans (69) | Adults with spinal cord injury admitted to two hospitals in the United States (110 with HCA BSI and 36 with CA BSI) | Per criteria of Friedman et al. (65) | Patients with HCA BSI were older and more likely to have comorbidities | Trend for higher rates of resistance with HCA BSI | No difference in hospital or 30-day mortality rates |
| Valles (70) | Adults admitted to three teaching hospitals in Spain (581 with CA BSI and 281 with HCA BSI) | Per criteria of Friedman et al. (65) | Patients with HCA BSI were older and more likely to have comorbidities | Different distribution of pathogens and higher rates of resistance, including MRSA; more polymicrobial infections with HCA BSI | Higher case fatality rate (28% versus 10%; P < 0.001) with HCA BSI |
BURDEN OF COMMUNITY-ONSET BLOODSTREAM INFECTION
Although not likely recognized by both the lay and medical communities, the burden of community-onset BSI is comparable in magnitude to those of acute myocardial infarction, stroke, and major trauma (4). Most investigations studying the adverse impact of BSI have been performed with selected patient cohorts, such as those admitted to hospital. However, such studies suffer from a number of important limitations, including selection bias and a lack of adequate denominator data (72). As a result, population-based studies have been recognized as an optimal design for establishment of the burden of illness related to an infectious disease (73). In population-based studies, all episodes of infection occurring among residents of a defined geographical region are ascertained, and nonresidents are excluded (74). By including all cases, selection bias is minimized (75). Furthermore, as a result of the ability to define the population at risk, both incidence and mortality rates can be calculated.
Overall Populations
Rare studies have been published that report (or at least contain adequate data to estimate) the overall burden of community-onset BSI at the population level, and these are displayed in Table 3 (1–5). Filice et al. were the first to publish a study investigating BSIs in a nonselected population (1). These investigators did not focus on community-onset BSI, and the value in Table 3 represents an estimate based on the information provided in their report. Importantly, they had a number of cases that remained unclassified, such that the rate of community-onset BSI may have been as high as 6 per 100,000 higher than that reported. Uslan et al. reported an overall case fatality rate of 13.5% in their study, but this rate also included nosocomial cases, so the rate for community-onset cases could not be determined (2). Sogaard et al. found significant increases in incidence over the time of their study, and as a result, the most recent data are displayed in Table 3 (3). In the first study reported from Calgary, it is important that all common skin contaminants were excluded, such that the rate may be a falsely low estimate of the incidence of community-onset BSI in that population (4). In addition, that study did not differentiate between community-associated and health care-associated community-onset BSIs. Subsequent studies conducted in the pediatric (<18 years) population during 2000 to 2006 demonstrated an incidence of community-onset disease of 40 per 100,000 population (26 per 100,000 were community-associated BSIs, and 14 per 100,000 were health care-associated BSIs), an approximate case fatality rate of 5%, and mortality of 2 per 100,000 (76). In an adult cohort studied from 2000 to 2007, 28-day case fatality rates for health care-associated and community-associated BSIs were 19% and 10%, respectively (66). In another analysis of adult patients, during 2003 to 2007, all-cause case fatality rates were 12% (28 days), 17% (90 days), and 25% (365 days) (77). Notably, the study from Victoria evaluated only in-hospital deaths, which likely underestimated the true burden of disease (5).
TABLE 3.
Population-based studies investigating the overall burden of disease associated with community-onset bloodstream infection
| First author (reference) | Setting, yr | Annual incidence | Case fatality rate (%) | Mortality per 100,000 population |
|---|---|---|---|---|
| Filice (1) | Charleston County, SC (population 250,000), 1974–1976 | 43 per 100,000 | Not reported | Not reported |
| Uslan (2) | Olmsted County, MN (population 124,277), 2003–2005 | 154 per 100,000 (70 per 100,000 were health care associated, and 84 were community acquired) | Not reported | Not reported |
| Sogaard (3) | Northern Denmark (population 500,000), 1992–2006 | 112 per 100,000 (79 per 100,00 were CA, and 34 were HCA) during 2002 to 2006 | 17 (15 for CA BSI and 22 for HCA BSI) during 2002 and 2006 | 19 (12 for CA BSI and 7 for HCA BSI) during 2002 to 2006 |
| Laupland (4) | Calgary area, Alberta, Canada (population 1 million), 2000–2004 | 81.6 per 100,000 | 13 (in hospital) | 11 (in hospital) |
| Laupland (5) | Victoria area, British Columbia, Canada (population 358,000), 1998–2005 | 101.2 per 100,000 | 12.6 (in hospital) | 12.8 (in hospital) |
Several other studies have evaluated BSIs at the population level but have had incomplete case ascertainment, have limited analysis to subpopulations, have not specifically defined rates, or have not clearly differentiated between community- and hospital-onset disease (6–15).
It is difficult to precisely define the contemporary (within the last 20 years) overall burden of community-onset BSI, for a number of potential reasons. First, there are few studies that have been conducted (Table 3). Second, studies were conducted over different periods during the past 4 decades, and it is well documented that the rate of BSI has increased in many jurisdictions, at least up to the early 2000s (3, 6, 8). Third, the demographic profiles of the populations are different. Age and gender standardization alone has been shown to potentially result in differences of 20 to 30% in reported incidences among populations (73), and this may even be observed within different regions of the same country (5). Fourth, and perhaps most importantly, these studies were all reported from high-income Western countries. The burden of community-onset disease may be substantially different elsewhere worldwide (12–15).
Specific Etiologies
Although population-based data are limited in defining the overall community-onset BSI burden, there is a significant and growing number of studies investigating the epidemiology of community-onset BSI with selected pathogens. Escherichia coli, Staphylococcus aureus, and Streptococcus pneumoniae are the most frequent causes of community-onset BSI and are responsible for more than one-half of all cases overall (1, 2, 4, 5). The following sections review the incidence of community-onset BSI among selected etiologies, with an emphasis on contemporary studies conducted in populations without age restriction.
Escherichia coli.
Escherichia coli is the most common cause of BSI reported in overall population-based studies (1–9). However, few population-based studies have specifically focused on E. coli BSI (78–81). Kennedy and colleagues investigated E. coli bacteremia in Canberra, Australia (population 366,000), between 2000 and 2004 (78). The annual incidence was 28 per 100,000, and among infections, 68% were community associated and 13% were health care associated. The incidence of community-onset disease was 23 per 100,000 annually. Laupland et al. investigated E. coli BSI in the Calgary area of Canada (population 1.2 million) during 2000 to 2006 and found an incidence of 30.3 per 100,000 annually (79). Overall, 32% of BSIs were health care associated, and 53% were community associated, for a community-onset incidence of 25.6 per 100,000. During 1998 to 2007, Al-Hasan et al. investigated E. coli BSI in Olmsted County, MN (population 124,277) (80). The incidence rates for females and males were 48 and 34 per 100,000, respectively. Fifty-nine percent of cases were community associated, and 32% were health care associated, for incidence rates of approximately 44 and 31 per 100,000 for community-onset disease among females and males, respectively. Williamson and colleagues investigated E. coli BSI in Auckland, New Zealand (population 0.5 million), during 2005 to 2011 (81). They reported an incidence of 52 per 100,000, and among infections, 34% were community associated and 40% were health care associated, for an incidence of community-onset disease of 39 per 100,000 annually. They also observed marked differences in incidence based on ethnicity, with the highest rates observed in Pacific peoples and Maoris.
Staphylococcus aureus.
Staphylococcus aureus is the second most common species causing BSI in population-based studies, and there is an evolving body of literature focusing specifically on this pathogen (2, 6, 8, 9). Table 4 displays studies investigating the burden of community-onset Staphylococcus aureus BSI in nonselected populations (63, 82–86). Several other population-based studies, in addition to those presented in Table 3, have been reported but either had older or duplicative data with tabulated studies (87–90), were limited to subgroups such as MRSA only (91–94), included selected age groups (95–101), or did not report or clearly differentiate between community- and hospital-onset disease (102–106). Overall, these data support the estimate that the contemporary incidence of community-onset Staphylococcus aureus BSI is approximately 15 per 100,000 in Western countries and is associated with a 30-day all-cause case fatality rate of 20% and a mortality rate of 3 per 100,000 (107). Notably, MRSA strains vary widely internationally, and in some cases MRSA appears to add to and in others replaces the burden due to methicillin-sensitive S. aureus (MSSA) (85).
TABLE 4.
Contemporary population-based studies investigating the overall burden of Staphylococcus aureus community-onset bloodstream infection
| First author (reference) | Population, yr | MSSA incidence per 100,000/yr | MRSA incidence per 100,000/yr | Total incidence per 100,000/yr | Mortality (%) |
|---|---|---|---|---|---|
| Morin (63) | Four areas in Connecticut, 1998 | 14.5 | 2.5 | 17 | 10 for MSSA, 14 for MRSA, 11 overall (case fatality rates) |
| Lyytikainen (82) | Finland, 1995–2001 | 7 | <0.1 | 7 | 13 (28-day case fatality rate) |
| Collignon (83) | Australia, 1999–2002 | 15 | 2 | 17 | 18 (28-day case fatality rate) |
| Huggan (84) | Canterbury, New Zealand, 1998–2006 | 14 | <0.3 | 14 | Not reported |
| Laupland (85) and Tom (86) | Multinational, 2000–2008 | 30-day case fatality rates of 20.2 for MSSA and 22.3 for MRSA, mortality rates of 3.4 for MSSA and 0.3 for MRSA per 100,000 per year | |||
| Canberra, Australia | 14.5 | 2.0 | 16.5 | ||
| Calgary, Canada | 15.3 | 2.4 | 16.5 | ||
| Victoria, Canada | 15.1 | 2.4 | 17.4 | ||
| Sherbrooke, Canada | 13.0 | 1.8 | 14.8 | ||
| Northern Denmark | 16.2 | 0 | 16.2 | ||
| Copenhagen County, Denmark | 14.7 | 0.2 | 14.9 | ||
| Copenhagen City, Denmark | 16.5 | 0.2 | 16.7 | ||
| Finland | 11.9 | 0.2 | 12.1 | ||
| Western Sweden | 18.1 | 0 | 18.2 | ||
| Overall | 15.0 | 1.0 | 16.0 |
Streptococcus pneumoniae.
Streptococcus pneumoniae is the third most common overall BSI etiology reported in population-based studies, and there is a significant body of literature focusing specifically on this pathogen (1–9). Several contemporary studies have been reported from overall populations and are summarized in Table 5 (108–125). Other studies have been conducted in pediatric (126–137) and adult (137–143) subpopulations worldwide.
TABLE 5.
Contemporary studies of invasive disease and/or bloodstream infection due to Streptococcus pneumoniae in nonselected populations
| First author (reference) | Population, yr | Annual invasive disease incidence per 100,000 | BSI rate or proportion (%) of isolates in blood |
|---|---|---|---|
| Rudnick (108) | Toronto, Canada, 1995–2011 | 9 | Not reported |
| Feemster (109) | Philadelphia, PA, 2005–2008 | Not reported | 12.3 per 100,000 |
| Helferty (110) | Northern Canada, 1999–2010 | 25.8 | Not reported |
| Ingels (111) | Denmark, 2000–2010 | 17.7 (2008–2010) | Not reported |
| Rosen (112) | Eight U.S. regions, 1998–2009 | 13.5 (overall; range of 11.2 to 18 between regions during 2009) | Not reported |
| Harboe (113) | Denmark, 1938–2007 | Approximately 20 (1998–2007) | 81 |
| Weatherholtz (114) | Navajo Nation, USA, 1995–2006 | 51 (2004–2006) | Not reported |
| Motlova (115) | Czech Republic, 2000–2006 | 2.3–4.3 | Not reported |
| Hsieh (116) | Taiwan, 2007 | 2.6 | ≥94 |
| Kellner (117) | Calgary, Canada, 1998–2007 | 11.2 (2003–2007) | 89 |
| Baggett (118) | Two areas in rural Thailand, 2005–2007 | Not reported | 3.7 per 100,000 (Sa Kaeo Province) and 7.6 per 100,000 (Nakhon Phanom Province) |
| Bruce (119) | Seven circumpolar regions, 1999–2005 | 21.6 for Canada (2003–2005), 19.8 for Greenland (2000–2005), 16.2 for Norway (2000–2005), 15.8 for Alaska (2001–2005), 14.6 for Iceland (2000–2005), 11.6 for Finland (2000–2005), 9.1 for Sweden (2003–2005) | Not reported |
| Heffernan (120) | New Zealand, 1998–2005 | 12.4 | 93 |
| Lacapa (121) | Fort Apache Indian Reserve, USA, 1991–2006 | 87 (2001–2006) | Not reported |
| Klemets (122) | Finland, 1995–2002 | 10.6 | 9.9 per 100,000 |
| Einarsdottir (123) | Iceland, 1975–2004 | 16.7 (1990–2004) | Not reported |
| Stephens (124) | Atlanta, GA, 1994–2002 | 18 (2000–2002) | 95 |
| Andresen (125) | Canberra, Australia, 1998–2000 | 15.2 | Not reported |
Although the current annual incidence of community-onset Streptococcus pneumoniae BSI likely ranges between 10 and 20 per 100,000 in most Western countries, it is difficult to precisely define an overall rate, for several reasons (4, 5). First, this organism usually causes community-onset disease, with only approximately 10% of cases overall showing hospital-onset disease (144). Studies to date have not typically differentiated between community- and hospital-onset disease. Second, most studies, to date, have focused on invasive disease, and while approximately 90% of all invasive Streptococcus pneumoniae infections are associated with BSI, these data are not usually reported independently. Third, certain chronic comorbid illnesses, acute coinfections, and a range of ethnic and socioeconomic factors can greatly influence the risk of developing invasive Streptococcus pneumoniae infections (109, 110, 137, 145). As a result, populations differing in these characteristics will have different observed rates. Fourth, and most importantly, the epidemiology of invasive Streptococcus pneumoniae infection has undergone major changes in recent years, related to implementation of the universal use of protein-conjugate pneumococcal vaccines in infants in many populations. This has led to serotype shifts and major decreases in childhood invasive pneumococcal disease, with a commensurate reduction in disease among nonvaccinated adults due to herd immunity (146).
Klebsiella species.
Klebsiella species are the fourth most frequent agents of community-onset BSI (2, 4, 5). Meatherall et al. investigated Klebsiella pneumoniae BSI in Canada (2000 to 2007) and found a community-onset incidence of 5.2 per 100,000 (3.1 per 100,000 were health care associated, and 2.1 per 100,000 were community associated), with an associated case fatality rate of 14% (147). This is similar to the incidence of 5.7 per 100,000 observed in Victoria, Canada, during 1998 to 2005 (5). In a study investigating Klebsiella species BSI from the United States (1998 to 2007), Al-Hasan and colleagues found overall incidence (including hospital-onset disease) rates of 15.4 per 100,000 for males and 9.4 per 100,000 for females (148). Among a cohort of 127 patients, 60 (47%) patients had community-acquired BSI (50 with Klebsiella pneumoniae, 9 with Klebsiella oxytoca, and 1 with Klebsiella ornithinolytica), and 53 (42%) had health care-associated BSI (46 with Klebsiella pneumoniae and 7 with Klebsiella oxytoca).
Salmonella enterica.
Although Salmonella enterica is a relatively infrequent cause of BSI in high-income Western countries, it is a frequent cause of BSI in many other areas of the world. In one study conducted during 2000 to 2007 in six regions in Australia, Canada, Denmark, and Finland, an overall rate of 1.02 per 100,000 population was observed; the rate of typhoidal disease (with S. enterica serotypes Typhi and Paratyphi) was 0.21 per 100,000, with a disease rate of 0.81 per 100,000 for other serotypes (149). Where data were available, more than 90% of cases were classified as community-onset BSI. A study from northern Denmark during 1994 to 2003 reported an overall incidence of nontyphoidal Salmonella enterica BSI of 2.3 per 100,000 population per year (150). A later study demonstrated international travel as a risk factor (151). Tabu et al. reported on non-S. Typhi Salmonella BSI in Kenya during 2006 to 2009 and reported rates of 78 and 13 per 100,000 population in rural and urban sites, respectively (152). In another study from these investigators, in Kenya during 2007 to 2009, Salmonella enterica serovar Typhi incidences were 29 and 247 per 100,000 population in rural and urban sites, respectively (153).
Other Enterobacteriaceae.
As a group, the Enterobacteriaceae are frequent causes of community-onset BSI, largely due to Escherichia coli and Klebsiella pneumoniae, as previously detailed. Proteus mirabilis was among the 10 most frequent species of bacteria causing community-onset BSI in some studies (1, 4). A rate of 1.3 per 100,000 was observed in Calgary, Canada (2000 to 2004) (4), and a rate of approximately 2 per 100,000 was seen in Olmsted County, MN (1998 to 2007) (67). Other Proteus species are rare and occur at rates of <0.1 per 100,000 (154). Enterobacter species BSIs were investigated in Olmsted County during 1998 to 2007 and were found to occur at a rate of 3.3 per 100,000 population; 58% and 21% of cases were health care-associated and community-associated BSIs, respectively, for an incidence of community-onset BSI of 2.6 per 100,000 (155). There is increasing recognition of the importance of Serratia species as causes of community-onset BSI, with rates of 0.6 and 0.5 per 100,000 observed in Calgary, Canada (2000 to 2005), and Canberra, Australia (1998 to 2007), respectively (156, 157). Few population-based data on Citrobacter species have been published, and a rate of ≤1 per 100,000 was estimated for Olmsted County, MN (67). Rare Enterobacteriaceae etiologies of community-onset BSI include Hafnia alvei (0.1 per 100,000) (158), Morganella morganii (0.3 per 100,000) (154), and Providencia species (0.15 per 100,000) (154).
Haemophilus influenzae.
Prior to widespread use of protein-conjugate serotype b vaccines, Haemophilus influenzae was among the predominant causes of community-onset BSI (1). Although now less common, it remains an important cause of invasive disease, and there has been a shift toward non-serotype b etiologies. A multinational study conducted during 2000 to 2008 within Australia, Canada, and Denmark found an incidence of Haemophilus influenzae BSI of 1.31 per 100,000, with 89% of infections being community-onset BSIs (159). Incidences were 0.08, 0.22, and 0.98 per 100,000 for serotype b, serotypes a and c to f, and nontypeable H. influenzae, respectively. A large study including invasive infections from 14 European countries during 1996 to 2006 identified rates of 0.15, 0.04, and 0.28 for serotype b, serotypes a and c to f, and nontypeable H. influenzae, respectively (160). Studies of invasive disease from Canadian regions, including Manitoba (2000 to 2006), northern Canada (2000 to 2005), and Ontario (1989 to 2007), reported rates of 1 to 2, 8, and 1.4 per 100,000, respectively (161–163). The overall incidence of invasive disease in Illinois was reported to be 1.0 per 100,000 in 2004 (164), and an incidence of 1.5 per 100,000 was reported for Iceland during 1990 to 2008 (165). The rate of community-onset BSI due to Haemophilus influenzae was approximately 1.5 per 100,000 in a large multiregional study in the United States during 1989 to 2008 (166).
Pseudomonas aeruginosa.
Pseudomonas aeruginosa is variably listed among the 10 most frequent etiologies of community-onset BSI (2–4). Al-Hasan and colleagues reported overall rates (including hospital-onset disease) of Pseudomonas aeruginosa BSI for males and females of 10.8 and 3.7 per 100,000, respectively (167). Eighty-three percent of the cases had a community onset, suggesting an incidence of community-onset BSI of 6 per 100,000 annually. Parkins et al. identified an overall rate (including hospital-onset cases) of Pseudomonas aeruginosa BSI of 3.6 per 100,000 in Calgary during 2000 to 2006 (168). Fifty-five percent of cases had a community onset, for an incidence of community-onset BSI of 2 per 100,000 annually (4, 168).
Beta-hemolytic streptococci.
Beta-hemolytic streptococci represent a large group of organisms causing community-onset BSI (2, 4, 5). Invasive Streptococcus pyogenes (group A) and Streptococcus agalactiae (group B) have been studied extensively worldwide, although fewer studies have specifically examined community-onset BSI in nonselected populations (169, 170). A rate of 2.5 per 100,000 was reported for community-onset BSI due to S. pyogenes in Connecticut in 1998 (63). A high rate of 11.6 per 100,000 population for S. pyogenes BSI was observed during 2000 to 2005 in Fiji, although it is not clear what proportion of cases may have had a hospital onset (171). Respective rates of community-onset BSI due to S. pyogenes and S. agalactiae were reported as 2.3 and 2.5 per 100,000 in Victoria, Canada, during 1998 to 2005 (5), and as 3.3 and 2.3 per 100,000 in Calgary, Canada, during 2000 to 2004 (4). Large-colony group C and G streptococci (Streptococcus dysgalactiae subsp. equisimilis) are also important causes of community-onset BSI, with incidence rates of approximately 2 to 3 per 100,000 observed in Canada, Denmark, and Finland (5, 172–174).
Enterococci.
Enterococci, particularly Enterococcus faecalis, are consistently reported among the top 10 most frequent isolates in community-onset BSI (2, 4, 5). Incidence rates for Enterococcus faecalis community-onset BSI were reported as 3.6 per 100,000 in Victoria, Canada, during 1998 to 2005 (5), and 2.9 per 100,000 in Calgary, during 2000 to 2004 (4). Pinholt et al. examined enterococcal BSI in two Danish regions during 2006 to 2009 and found rates of 7 and 1 per 100,000 for Enterococcus faecalis and Enterococcus faecium, respectively (175).
Anaerobes.
Anaerobes as a group are frequently observed causes of community-onset BSI (2–5). Ngo and colleagues reported on all anaerobic BSIs in Calgary during 2000 to 2008 and found incidence rates of 3.6 and 2.9 per 100,000 for community-associated and health care-associated community-onset BSIs, respectively (176). Bacteroides fragilis is the most commonly observed anaerobic species causing community-onset BSI, with reported rates (per 100,000 per year) of 2.4 in Calgary, Canada, from 2000 to 2004 (4), and 2.1 in Victoria, Canada, from 1998 to 2005 (5). Clostridium species represent the second most common anaerobes causing community-onset BSI, with a rate of 1.2 per 100,000 (177). Fusobacterium species are uncommon but potentially severe causes of community-onset BSI, with rates of approximately 0.3 to 0.5 per 100,000 annually observed in New Zealand (2002 to 2007), Denmark (1998 to 2001), and Canada (2000 to 2008) (178–180).
Candida species.
Candida species are occasional causes of community-onset BSI and are typically health care associated. While there are many population-based studies reporting incidences of Candida species BSI (181–185), few independently report rates of community-onset disease. Incidence rates for community-onset Candida species BSI include 0.5 per 100,000 in Calgary, Canada, during 2000 to 2005 (186), approximately 0.4 per 100,000 in Barcelona, Spain, during 2002 to 2003 (187), 4 per 100,000 in Connecticut and Maryland, during 1998 to 2000 (188), and 0.8 in Iceland, during 2000 to 2012 (189).
Coagulase-negative staphylococci and other Gram-positive organisms.
Coagulase-negative staphylococci (CoNS) are frequently listed as agents of community-onset BSI and are predominantly related to health care-associated disease (2, 3, 5). However, determination of rates of community-onset BSI is complicated by the fact that CoNS are common blood culture contaminants and ascertainment of a BSI due to CoNS involves a degree of subjective clinical assessment (54). In addition, the vast majority of studies involving CoNS BSI are hospital based. Similar issues challenge the establishment of the incidence of community-onset BSI with viridans group streptococci (190). Listeria monocytogenes is a rare but potentially serious cause of community-onset BSI that may be associated with community-based outbreaks related to contaminated food sources. Rates of 0.2 to 0.3 per 100,000 were observed in the United States in the early 2000s (191).
Other Gram-negative bacteria.
A number of Gram-negative bacteria not previously listed have been identified as causes of community-onset BSI, but these are either rare or restricted to certain geographical regions worldwide. The incidence of meningococcemia demonstrates considerable geographical and temporal variability and is influenced by the immunization status of populations as well as by outbreaks, such that it is difficult to define an “average” or typical incidence rate for community-onset BSI (192–194). Melioidosis, caused by Burkholderia pseudomallei, is a severe illness that is most widely diagnosed in northern Australia and Southeast Asia. Bacteremic melioidosis rates were reported as 4.9 and 14.9 per 100,000 population in two regions of Thailand during 2006 to 2008 (195), 3 per 100,000 in Australia during 1989 to 2003 (196), 0.3 per 100,000 in Singapore during 1989 to 1996 (197), and 4 and 8 per 100,000 in Malaysia during 2000 to 2003 and 2005 to 2008, respectively (198, 199). A number of other Gram-negative bacteria causing community-onset BSI, including Brucella species and Bartonella species, demonstrate marked geographical variation (200–202).
EMERGENCE OF RESISTANT COMMUNITY-ONSET BLOODSTREAM INFECTIONS
Traditionally, BSIs due to antimicrobial-resistant organisms have been recognized to occur principally among patients admitted to high-acuity hospital environments, especially intensive care units (203, 204). However, the past decade has witnessed the emergence of a number of multiply antimicrobial-resistant pathogens arising in the community setting worldwide. Notable examples include community-onset MRSA (205, 206) and ESBL (207)-, metallo-β-lactamase-, and other carbapenemase-producing Enterobacteriaceae (208).
Community-Onset MRSA Bloodstream Infection
Although community-associated MRSA infections were first recognized among injection drug users in Detroit, MI, in the early 1980s (209), MRSA largely remained a hospital-onset pathogen in most jurisdictions worldwide, until recently. Since the turn of the millennium, community-associated MRSA infections have emerged worldwide and have either replaced or added to the MSSA disease burden (205, 206, 210). Five clones have been associated with the majority of disease worldwide, with multilocus sequence type 1 (ST-1)/USA400 and ST-8/USA300 predominantly observed in North America, ST-59 observed in the Asia-Pacific region, ST-80 observed in Europe, and ST-30 distributed broadly worldwide (205). Initially, community-associated MRSA strains were noted to occur in previously healthy individuals, and higher rates were observed among injection drug users, homeless or incarcerated individuals, men who have sex with men, and military recruits. However, in many jurisdictions, strains that initially caused community-onset disease subsequently moved into the hospital environment and now represent the predominant strains causing hospital-onset disease (211).
Several population-based studies have evaluated the epidemiology of community-onset BSI due to MRSA worldwide (88, 93, 94, 210). Klevens et al. investigated invasive MRSA in 9 U.S. communities during 2005 and reported an overall incidence of 31.8 per 100,000 population; 80% or more of cases were bacteremic, 58% were health care associated, and 14% were community associated, suggesting an incidence of approximately 18 per 100,000 for community-onset MRSA BSI (93). In another study comparing rates of MRSA BSI between the United States and the United Kingdom during 2006 to 2007, rates were 21.9 and 3.5 per 100,000 population, respectively (94). In a multinational study investigating all Staphylococcus aureus BSIs during 2000 to 2008, major shifts were observed, with an increasing incidence of community-onset MRSA BSI (210).
Enterobacteriaceae
A number of multidrug-resistant members of the Enterobacteriaceae, in particular Klebsiella pneumoniae and Escherichia coli, have emerged as important causes of community-onset BSI in recent years. During the 1990s, ESBL-producing Enterobacteriaceae were associated with hospital environments and were infrequently recognized causes of community-onset disease. However, since the turn of the millennium, these have emerged as major community-onset pathogens worldwide (207, 212). Series of community-onset BSIs due to a range of ESBL-producing Enterobacteriaceae have been reported from around the globe (13, 81, 213–216). Molecular epidemiology studies have identified a globally distributed clone, ST131, and defined the importance of international travel in the acquisition and spread of these infections (217–222). Within the ST131 clone, most of the fluoroquinolone-resistant and ESBL-producing strains have been identified within a highly pathogenic H30 subclone (223–227). Health care-associated BSI due to ESBL-producing Escherichia coli has been recognized as a significant complication following transrectal prostate biopsy (228, 229). A number of other resistant Enterobacteriaceae, such as those harboring Klebsiella pneumoniae carbapenemases and New Delhi metallo-β-lactamases, may result in community-onset BSI, but to date, these have largely caused either hospital-onset or health care-associated infections not associated with BSI (230, 231).
CONCLUSIONS
Community-onset BSI is a major health problem that is associated with a burden of illness similar to those of major trauma, acute stroke, and myocardial infarction (4). While heart disease and stroke, in particular, have garnered great attention and financial support by both public and private organizations, this is much less the case for severe bacterial infections, including community-onset BSI. It is therefore important to document the major burden of disease associated with community-onset BSI in order to bring the greater public attention and awareness that is needed to gain support for enhanced efforts aimed at reducing its major adverse impact. Population-based studies have demonstrated that Escherichia coli, Staphylococcus aureus, and Streptococcus pneumoniae are responsible for the majority of community-onset BSIs in many jurisdictions, while other key pathogens have important roles in other regions. Demonstration of the importance of these pathogens regionally provides a rational basis for prioritizing future potential preventative strategies, such as immunization, environmental hygiene, and optimized management of chronic comorbid medical diseases. Community-onset BSI will likely increase in importance in the coming years, due to rising rates of health care-associated community-onset BSI related to management of older and increasingly complex patients in the community setting. The emergence of resistant organisms will have a major impact on the epidemiology of community-onset BSI in our increasingly global community in the coming years.
Biographies

Kevin B. Laupland, M.D., M.Sc., F.R.C.P.C., earned his medical degree at the University of Toronto and then completed residency training in Internal Medicine and subspecialty training in both Critical Care Medicine and Infectious Diseases at the University of Calgary. He also was awarded an M.Sc. in Epidemiology at the University of Calgary. For the first 10 years of his career, he practiced at the Peter Lougheed Centre in Calgary and was appointed a member of the Faculty of Medicine at the University of Calgary, where he focused his research on the epidemiology of severe infections and those due to antimicrobial-resistant pathogens. He recently relocated to Kamloops, British Columbia, where he is presently an intensivist, infectious disease consultant, and Head, Department of Medicine, at the Royal Inland Hospital. He is cofounder and leader of the International Bloodstream Infection Surveillance Collaborative and is an Adjunct Professor at the University of Calgary.

Deirdre L. Church, M.D., Ph.D., F.R.C.P.C., earned her medical degree from the University of Calgary. She completed residency training in Internal Medicine and subspecialty training in both Clinical Microbiology and Infectious Diseases and was also awarded a Ph.D. in Medical Sciences (Medical Microbiology) from the University of Calgary. She has practiced for more than 25 years as an Infectious Diseases Consultant at the Foothills Medical Centre and as a Medical Microbiologist, Division of Microbiology, Calgary Laboratory Services. She is currently the Vice Chair, Microbiology Resource Committee, for the College of American Pathologists. She is also the Consultant, Microbiology, for the Alberta Quality Enhancement Program (ALQEP), College of Physicians & Surgeons of Alberta. She has held an academic appointment with the University of Calgary throughout her career and is a Professor in the Departments of Pathology & Laboratory Medicine and Medicine. Her research interests include the pathogenesis of gut HIV infection, including viral evolution in the gut compartments, epidemiology of antibiotic-resistant organisms, mechanisms of antibiotic resistance, and molecular microbiology.
REFERENCES
- 1.Filice GA, Van Etta LL, Darby CP, Fraser DW. 1986. Bacteremia in Charleston County, South Carolina. Am. J. Epidemiol. 123:128–136 [DOI] [PubMed] [Google Scholar]
- 2.Uslan DZ, Crane SJ, Steckelberg JM, Cockerill FR, 3rd, St Sauver JL, Wilson WR, Baddour LM. 2007. Age- and sex-associated trends in bloodstream infection: a population-based study in Olmsted County, Minnesota. Arch. Intern. Med. 167:834–839. 10.1001/archinte.167.8.834 [DOI] [PubMed] [Google Scholar]
- 3.Sogaard M, Norgaard M, Dethlefsen C, Schonheyder HC. 2011. Temporal changes in the incidence and 30-day mortality associated with bacteremia in hospitalized patients from 1992 through 2006: a population-based cohort study. Clin. Infect. Dis. 52:61–69. 10.1093/cid/ciq069 [DOI] [PubMed] [Google Scholar]
- 4.Laupland KB, Gregson DB, Flemons WW, Hawkins D, Ross T, Church DL. 2007. Burden of community-onset bloodstream infection: a population-based assessment. Epidemiol. Infect. 135:1037–1042. 10.1017/S0950268806007631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laupland KB, Kibsey PC, Gregson DB, Galbraith JC. 2013. Population-based laboratory assessment of the burden of community-onset bloodstream infection in Victoria, Canada. Epidemiol. Infect. 141:174–180. 10.1017/S0950268812000428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skogberg K, Lyytikainen O, Ollgren J, Nuorti JP, Ruutu P. 2012. Population-based burden of bloodstream infections in Finland. Clin. Microbiol. Infect. 18:E170–E176. 10.1111/j.1469-0691.2012.03845.x [DOI] [PubMed] [Google Scholar]
- 7.Madsen KM, Schonheyder HC, Kristensen B, Sorensen HT. 1999. Secular trends in incidence and mortality of bacteraemia in a Danish county 1981–1994. APMIS 107:346–352. 10.1111/j.1699-0463.1999.tb01563.x [DOI] [PubMed] [Google Scholar]
- 8.Skogberg K, Lyytikainen O, Ruutu P, Ollgren J, Nuorti JP. 2008. Increase in bloodstream infections in Finland, 1995–2002. Epidemiol. Infect. 136:108–114. 10.1017/S0950268807008138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson J, Elgohari S, Livermore DM, Cookson B, Johnson A, Lamagni T, Chronias A, Sheridan E. 2011. Trends among pathogens reported as causing bacteraemia in England, 2004–2008. Clin. Microbiol. Infect. 17:451–458. 10.1111/j.1469-0691.2010.03262.x [DOI] [PubMed] [Google Scholar]
- 10.Reacher MH, Shah A, Livermore DM, Wale MC, Graham C, Johnson AP, Heine H, Monnickendam MA, Barker KF, James D, George RC. 2000. Bacteraemia and antibiotic resistance of its pathogens reported in England and Wales between 1990 and 1998: trend analysis. BMJ 320:213–216. 10.1136/bmj.320.7229.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Einsiedel LJ, Woodman RJ. 2010. Two nations: racial disparities in bloodstream infections recorded at Alice Springs Hospital, central Australia, 2001–2005. Med. J. Aust. 192:567–571 [DOI] [PubMed] [Google Scholar]
- 12.Deen J, von Seidlein L, Andersen F, Elle N, White NJ, Lubell Y. 2012. Community-acquired bacterial bloodstream infections in developing countries in south and southeast Asia: a systematic review. Lancet Infect. Dis. 12:480–487. 10.1016/S1473-3099(12)70028-2 [DOI] [PubMed] [Google Scholar]
- 13.Kanoksil M, Jatapai A, Peacock SJ, Limmathurotsakul D. 2013. Epidemiology, microbiology and mortality associated with community-acquired bacteremia in northeast Thailand: a multicenter surveillance study. PLoS One 8:e54714. 10.1371/journal.pone.0054714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thriemer K, Ley B, Ame S, von Seidlein L, Pak GD, Chang NY, Hashim R, Schmied WH, Busch CJ, Nixon S, Morrissey A, Puri MK, Ali M, Ochiai RL, Wierzba T, Jiddawi MS, Clemens JD, Ali SM, Deen JL. 2012. The burden of invasive bacterial infections in Pemba, Zanzibar. PLoS One 7:e30350. 10.1371/journal.pone.0030350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nielsen MV, Sarpong N, Krumkamp R, Dekker D, Loag W, Amemasor S, Agyekum A, Marks F, Huenger F, Krefis AC, Hagen RM, Adu-Sarkodie Y, May J, Schwarz NG. 2012. Incidence and characteristics of bacteremia among children in rural Ghana. PLoS One 7:e44063. 10.1371/journal.pone.0044063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang W, Daly CG, Mitchell D, Curtis B. 2013. Incidence and magnitude of bacteraemia caused by flossing and by scaling and root planing. J. Clin. Periodontol. 40:41–52. 10.1111/jcpe.12029 [DOI] [PubMed] [Google Scholar]
- 17.Duvall NB, Fisher TD, Hensley D, Hancock RH, Vandewalle KS. 2013. The comparative efficacy of 0.12% chlorhexidine and amoxicillin to reduce the incidence and magnitude of bacteremia during third molar extractions: a prospective, blind, randomized clinical trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 115:752–763. 10.1016/j.oooo.2012.11.019 [DOI] [PubMed] [Google Scholar]
- 18.Maharaj B, Coovadia Y, Vayej AC. 2012. An investigation of the frequency of bacteraemia following dental extraction, tooth brushing and chewing. Cardiovasc. J. Afr. 23:340–344. 10.5830/CVJA-2012-016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK. 2008. Bacteremia associated with toothbrushing and dental extraction. Circulation 117:3118–3125. 10.1161/CIRCULATIONAHA.107.758524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonilha DQ, Correia LM, Monaghan M, Lenz L, Santos M, Libera ED. 2011. Prospective study of bacteremia rate after elective band ligation and sclerotherapy with cyanoacrylate for esophageal varices in patients with advanced liver disease. Arq. Gastroenterol. 48:248–251 [DOI] [PubMed] [Google Scholar]
- 21.Chun YJ, Yoon NR, Park JM, Lim CH, Cho YK, Lee IS, Kim SW, Choi MG, Choi KY, Chung IS. 2012. Prospective assessment of risk of bacteremia following colorectal stent placement. Dig. Dis. Sci. 57:1045–1049. 10.1007/s10620-011-1962-x [DOI] [PubMed] [Google Scholar]
- 22.Levy MJ, Norton ID, Clain JE, Enders FB, Gleeson F, Limburg PJ, Nelson H, Rajan E, Topazian MD, Wang KK, Wiersema MJ, Wilson WR. 2007. Prospective study of bacteremia and complications with EUS FNA of rectal and perirectal lesions. Clin. Gastroenterol. Hepatol. 5:684–689. 10.1016/j.cgh.2007.02.029 [DOI] [PubMed] [Google Scholar]
- 23.Janssen J, Konig K, Knop-Hammad V, Johanns W, Greiner L. 2004. Frequency of bacteremia after linear EUS of the upper GI tract with and without FNA. Gastrointest. Endosc. 59:339–344. 10.1016/S0016-5107(03)02707-X [DOI] [PubMed] [Google Scholar]
- 24.Steinfort DP, Johnson DF, Irving LB. 2010. Incidence of bacteraemia following endobronchial ultrasound-guided transbronchial needle aspiration. Eur. Respir. J. 36:28–32. 10.1183/09031936.00151809 [DOI] [PubMed] [Google Scholar]
- 25.Konstantinou E, Argyra E, Avraamidou A, Fotis T, Tsakiri M, Voros D, Baltopoulos G. 2008. Difficult intubation provokes bacteremia. Surg. Infect. 9:521–524. 10.1089/sur.2007.057 [DOI] [PubMed] [Google Scholar]
- 26.Zani EL, Clark OA, Rodrigues Netto N., Jr 2011. Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane Database Syst. Rev. 2011:CD006576. 10.1002/14651858.CD006576.pub2 [DOI] [PubMed] [Google Scholar]
- 27.Bryant JK, Strand CL. 1987. Reliability of blood cultures collected from intravascular catheter versus venipuncture. Am. J. Clin. Pathol. 88:113–116 [DOI] [PubMed] [Google Scholar]
- 28.DesJardin JA, Falagas ME, Ruthazer R, Griffith J, Wawrose D, Schenkein D, Miller K, Snydman DR. 1999. Clinical utility of blood cultures drawn from indwelling central venous catheters in hospitalized patients with cancer. Ann. Intern. Med. 131:641–647 [DOI] [PubMed] [Google Scholar]
- 29.Everts RJ, Vinson EN, Adholla PO, Reller LB. 2001. Contamination of catheter-drawn blood cultures. J. Clin. Microbiol. 39:3393–3394. 10.1128/JCM.39.9.3393-3394.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Isaacman DJ, Karasic RB. 1990. Lack of effect of changing needles on contamination of blood cultures. Pediatr. Infect. Dis. J. 9:274–278. 10.1097/00006454-199004000-00010 [DOI] [PubMed] [Google Scholar]
- 31.Leisure MK, Moore DM, Schwartzman JD, Hayden GF, Donowitz LG. 1990. Changing the needle when inoculating blood cultures. A no-benefit and high-risk procedure. JAMA 264:2111–2112 [PubMed] [Google Scholar]
- 32.Reimer LG, Wilson ML, Weinstein MP. 1997. Update on detection of bacteremia and fungemia. Clin. Microbiol. Rev. 10:444–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breiman RF, Spika JS, Navarro VJ, Darden PM, Darby CP. 1990. Pneumococcal bacteremia in Charleston County, South Carolina. A decade later. Arch. Intern. Med. 150:1401–1405 [PubMed] [Google Scholar]
- 34.Lee A, Mirrett S, Reller LB, Weinstein MP. 2007. Detection of bloodstream infections in adults: how many blood cultures are needed? J. Clin. Microbiol. 45:3546–3548. 10.1128/JCM.01555-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cockerill FR, 3rd, Wilson JW, Vetter EA, Goodman KM, Torgerson CA, Harmsen WS, Schleck CD, Ilstrup DM, Washington JA, 2nd, Wilson WR. 2004. Optimal testing parameters for blood cultures. Clin. Infect. Dis. 38:1724–1730. 10.1086/421087 [DOI] [PubMed] [Google Scholar]
- 36.Li J, Plorde JJ, Carlson LG. 1994. Effects of volume and periodicity on blood cultures. J. Clin. Microbiol. 32:2829–2831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel R, Vetter EA, Harmsen WS, Schleck CD, Fadel HJ, Cockerill FR., 3rd 2011. Optimized pathogen detection with 30- compared to 20-milliliter blood culture draws. J. Clin. Microbiol. 49:4047–4051. 10.1128/JCM.01314-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cobos-Trigueros N, Rinaudo M, Sole M, Castro P, Pumarol J, Hernandez C, Fernandez S, Nicolas JM, Mallolas J, Vila J, Morata L, Gatell JM, Soriano A, Mensa J, Martinez JA. 2014. Acquisition of resistant microorganisms and infections in HIV-infected patients admitted to the ICU. Eur. J. Clin. Microbiol. Infect. Dis. 33:611–620. 10.1007/s10096-013-1995-5 [DOI] [PubMed] [Google Scholar]
- 39.Weinstein MP, Reller LB, Murphy JR, Lichtenstein KA. 1983. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev. Infect. Dis. 5:35–53 [DOI] [PubMed] [Google Scholar]
- 40.Perl B, Gottehrer NP, Raveh D, Schlesinger Y, Rudensky B, Yinnon AM. 1999. Cost-effectiveness of blood cultures for adult patients with cellulitis. Clin. Infect. Dis. 29:1483–1488. 10.1086/313525 [DOI] [PubMed] [Google Scholar]
- 41.Zadroga R, Williams DN, Gottschall R, Hanson K, Nordberg V, Deike M, Kuskowski M, Carlson L, Nicolau DP, Sutherland C, Hansen GT. 2013. Comparison of 2 blood culture media shows significant differences in bacterial recovery for patients on antimicrobial therapy. Clin. Infect. Dis. 56:790–797. 10.1093/cid/cis1021 [DOI] [PubMed] [Google Scholar]
- 42.Wilson ML, Mirrett S, Reller LB, Weinstein MP, Reimer LG. 1993. Recovery of clinically important microorganisms from the BacT/Alert blood culture system does not require testing for seven days. Diagn. Microbiol. Infect. Dis. 16:31–34. 10.1016/0732-8893(93)90127-S [DOI] [PubMed] [Google Scholar]
- 43.Cockerill FR, 3rd, Torgerson CA, Reed GS, Vetter EA, Weaver AL, Dale JC, Roberts GD, Henry NK, Ilstrup DM, Rosenblatt JE. 1996. Clinical comparison of Difco ESP, Wampole isolator, and Becton Dickinson Septi-Chek aerobic blood culturing systems. J. Clin. Microbiol. 34:20–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henry NK, McLimans CA, Wright AJ, Thompson RL, Wilson WR, Washington JA., 2nd 1983. Microbiological and clinical evaluation of the isolator lysis-centrifugation blood culture tube. J. Clin. Microbiol. 17:864–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walker RC, Henry NK, Washington JA, 2nd, Thompson RL. 1986. Lysis-centrifugation blood culture technique. Clinical impact in Staphylococcus aureus bacteremia. Arch. Intern. Med. 146:2341–2343 [PubMed] [Google Scholar]
- 46.Jorgensen JH, Mirrett S, McDonald LC, Murray PR, Weinstein MP, Fune J, Trippy CW, Masterson M, Reller LB. 1997. Controlled clinical laboratory comparison of BACTEC Plus Aerobic/F resin medium with BacT/Alert Aerobic FAN medium for detection of bacteremia and fungemia. J. Clin. Microbiol. 35:53–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pohlman JK, Kirkley BA, Easley KA, Basille BA, Washington JA. 1995. Controlled clinical evaluation of BACTEC Plus Aerobic/F and BacT/Alert Aerobic FAN bottles for detection of bloodstream infections. J. Clin. Microbiol. 33:2856–2858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hall KK, Lyman JA. 2006. Updated review of blood culture contamination. Clin. Microbiol. Rev. 19:788–802. 10.1128/CMR.00062-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chu VH, Woods CW, Miro JM, Hoen B, Cabell CH, Pappas PA, Federspiel J, Athan E, Stryjewski ME, Nacinovich F, Marco F, Levine DP, Elliott TS, Fortes CQ, Tornos P, Gordon DL, Utili R, Delahaye F, Corey GR, Fowler VG., Jr 2008. Emergence of coagulase-negative staphylococci as a cause of native valve endocarditis. Clin. Infect. Dis. 46:232–242. 10.1086/524666 [DOI] [PubMed] [Google Scholar]
- 50.Son JS, Song JH, Ko KS, Yeom JS, Ki HK, Kim SW, Chang HH, Ryu SY, Kim YS, Jung SI, Shin SY, Oh HB, Lee YS, Chung DR, Lee NY, Peck KR. 2010. Bloodstream infections and clinical significance of healthcare-associated bacteremia: a multicenter surveillance study in Korean hospitals. J. Korean Med. Sci. 25:992–998. 10.3346/jkms.2010.25.7.992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin HH, Liu YF, Tien N, Ho CM, Hsu LN, Lu JJ. 2013. Evaluation of the blood volume effect on the diagnosis of bacteremia in automated blood culture systems. J. Microbiol. Immunol. Infect. 46:48–52. 10.1016/j.jmii.2012.03.012 [DOI] [PubMed] [Google Scholar]
- 52.Beekmann SE, Diekema DJ, Doern GV. 2005. Determining the clinical significance of coagulase-negative staphylococci isolated from blood cultures. Infect. Control Hosp. Epidemiol. 26:559–566. 10.1086/502584 [DOI] [PubMed] [Google Scholar]
- 53.Favre B, Hugonnet S, Correa L, Sax H, Rohner P, Pittet D. 2005. Nosocomial bacteremia: clinical significance of a single blood culture positive for coagulase-negative staphylococci. Infect. Control Hosp. Epidemiol. 26:697–702. 10.1086/502605 [DOI] [PubMed] [Google Scholar]
- 54.Rahkonen M, Luttinen S, Koskela M, Hautala T. 2012. True bacteremias caused by coagulase negative Staphylococcus are difficult to distinguish from blood culture contaminants. Eur. J. Clin. Microbiol. Infect. Dis. 31:2639–2644. 10.1007/s10096-012-1607-9 [DOI] [PubMed] [Google Scholar]
- 55.Elzi L, Babouee B, Vogeli N, Laffer R, Dangel M, Frei R, Battegay M, Widmer AF. 2012. How to discriminate contamination from bloodstream infection due to coagulase-negative staphylococci: a prospective study with 654 patients. Clin. Microbiol. Infect. 18:E355–E361. 10.1111/j.1469-0691.2012.03964.x [DOI] [PubMed] [Google Scholar]
- 56.Kassis C, Rangaraj G, Jiang Y, Hachem RY, Raad I. 2009. Differentiating culture samples representing coagulase-negative staphylococcal bacteremia from those representing contamination by use of time-to-positivity and quantitative blood culture methods. J. Clin. Microbiol. 47:3255–3260. 10.1128/JCM.01045-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bates DW, Goldman L, Lee TH. 1991. Contaminant blood cultures and resource utilization. The true consequences of false-positive results. JAMA 265:365–369 [PubMed] [Google Scholar]
- 58.Mayer J, Greene T, Howell J, Ying J, Rubin MA, Trick WE, Samore MH. 2012. Agreement in classifying bloodstream infections among multiple reviewers conducting surveillance. Clin. Infect. Dis. 55:364–370. 10.1093/cid/cis410 [DOI] [PubMed] [Google Scholar]
- 59.Leal J, Laupland KB. 2008. Validity of electronic surveillance systems: a systematic review. J. Hosp. Infect. 69:220–229. 10.1016/j.jhin.2008.04.030 [DOI] [PubMed] [Google Scholar]
- 60.Leal J, Gregson DB, Ross T, Flemons WW, Church DL, Laupland KB. 2010. Development of a novel electronic surveillance system for monitoring of bloodstream infections. Infect. Control Hosp. Epidemiol. 31:740–747. 10.1086/653207 [DOI] [PubMed] [Google Scholar]
- 61.Trick WE, Zagorski BM, Tokars JI, Vernon MO, Welbel SF, Wisniewski MF, Richards C, Weinstein RA. 2004. Computer algorithms to detect bloodstream infections. Emerg. Infect. Dis. 10:1612–1620. 10.3201/eid1009.030978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. 1988. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control 16:128–140. 10.1016/0196-6553(88)90053-3 [DOI] [PubMed] [Google Scholar]
- 63.Morin CA, Hadler JL. 2001. Population-based incidence and characteristics of community-onset Staphylococcus aureus infections with bacteremia in 4 metropolitan Connecticut areas, 1998. J. Infect. Dis. 184:1029–1034. 10.1086/323459 [DOI] [PubMed] [Google Scholar]
- 64.Siegman-Igra Y, Fourer B, Orni-Wasserlauf R, Golan Y, Noy A, Schwartz D, Giladi M. 2002. Reappraisal of community-acquired bacteremia: a proposal of a new classification for the spectrum of acquisition of bacteremia. Clin. Infect. Dis. 34:1431–1439. 10.1086/339809 [DOI] [PubMed] [Google Scholar]
- 65.Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ. 2002. Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann. Intern. Med. 137:791–797. 10.7326/0003-4819-137-10-200211190-00007 [DOI] [PubMed] [Google Scholar]
- 66.Lenz R, Leal JR, Church DL, Gregson DB, Ross T, Laupland KB. 2012. The distinct category of healthcare associated bloodstream infections. BMC Infect. Dis. 12:85. 10.1186/1471-2334-12-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Al-Hasan MN, Eckel-Passow JE, Baddour LM. 2012. Impact of healthcare-associated acquisition on community-onset Gram-negative bloodstream infection: a population-based study: healthcare-associated Gram-negative BSI. Eur. J. Clin. Microbiol. Infect. Dis. 31:1163–1171. 10.1007/s10096-011-1424-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kollef MH, Zilberberg MD, Shorr AF, Vo L, Schein J, Micek ST, Kim M. 2011. Epidemiology, microbiology and outcomes of healthcare-associated and community-acquired bacteremia: a multicenter cohort study. J. Infect. 62:130–135. 10.1016/j.jinf.2010.12.009 [DOI] [PubMed] [Google Scholar]
- 69.Evans CT, Hershow RC, Chin A, Foulis PR, Burns SP, Weaver FM. 2009. Bloodstream infections and setting of onset in persons with spinal cord injury and disorder. Spinal Cord 47:610–615. 10.1038/sc.2009.2 [DOI] [PubMed] [Google Scholar]
- 70.Valles J, Calbo E, Anoro E, Fontanals D, Xercavins M, Espejo E, Serrate G, Freixas N, Morera MA, Font B, Bella F, Segura F, Garau J. 2008. Bloodstream infections in adults: importance of healthcare-associated infections. J. Infect. 56:27–34. 10.1016/j.jinf.2007.10.001 [DOI] [PubMed] [Google Scholar]
- 71.Gradel KO, Knudsen JD, Arpi M, Ostergaard C, Schonheyder HC, Sogaard M. 2012. Classification of positive blood cultures: computer algorithms versus physicians' assessment—development of tools for surveillance of bloodstream infection prognosis using population-based laboratory databases. BMC Med. Res. Methodol. 12:139. 10.1186/1471-2288-12-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Laupland KB. 2004. Population-based epidemiology of intensive care: critical importance of ascertainment of residency status. Crit. Care 8:R431–R436. 10.1186/cc2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Laupland KB. 2013. Defining the epidemiology of bloodstream infections: the ‘gold standard' of population-based assessment. Epidemiol. Infect. 141:2149–2157. 10.1017/S0950268812002725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schuchat A, Hilger T, Zell E, Farley MM, Reingold A, Harrison L, Lefkowitz L, Danila R, Stefonek K, Barrett N, Morse D, Pinner R. 2001. Active bacterial core surveillance of the emerging infections program network. Emerg. Infect. Dis. 7:92–99. 10.3201/eid0701.010114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rempel OR, Laupland KB. 2009. Surveillance for antimicrobial resistant organisms: potential sources and magnitude of bias. Epidemiol. Infect. 137:1665–1673. 10.1017/S0950268809990100 [DOI] [PubMed] [Google Scholar]
- 76.Laupland KB, Gregson DB, Vanderkooi OG, Ross T, Kellner JD. 2009. The changing burden of pediatric bloodstream infections in Calgary, Canada, 2000–2006. Pediatr. Infect. Dis. J. 28:114–117. 10.1097/INF.0b013e318187ad5a [DOI] [PubMed] [Google Scholar]
- 77.Laupland KB, Svenson LW, Gregson DB, Church DL. 2011. Long-term mortality associated with community-onset bloodstream infection. Infection 39:405–410. 10.1007/s15010-011-0149-x [DOI] [PubMed] [Google Scholar]
- 78.Kennedy KJ, Roberts JL, Collignon PJ. 2008. Escherichia coli bacteraemia in Canberra: incidence and clinical features. Med. J. Aust. 188:209–213 [DOI] [PubMed] [Google Scholar]
- 79.Laupland KB, Gregson DB, Church DL, Ross T, Pitout JD. 2008. Incidence, risk factors and outcomes of Escherichia coli bloodstream infections in a large Canadian region. Clin. Microbiol. Infect. 14:1041–1047. 10.1111/j.1469-0691.2008.02089.x [DOI] [PubMed] [Google Scholar]
- 80.Al-Hasan MN, Lahr BD, Eckel-Passow JE, Baddour LM. 2009. Antimicrobial resistance trends of Escherichia coli bloodstream isolates: a population-based study, 1998–2007. J. Antimicrob. Chemother. 64:169–174. 10.1093/jac/dkp162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Williamson DA, Lim A, Wiles S, Roberts SA, Freeman JT. 2013. Population-based incidence and comparative demographics of community-associated and healthcare-associated Escherichia coli bloodstream infection in Auckland, New Zealand, 2005–2011. BMC Infect. Dis. 13:385. 10.1186/1471-2334-13-385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lyytikainen O, Ruotsalainen E, Jarvinen A, Valtonen V, Ruutu P. 2005. Trends and outcome of nosocomial and community-acquired bloodstream infections due to Staphylococcus aureus in Finland, 1995–2001. Eur. J. Clin. Microbiol. Infect. Dis. 24:399–404. 10.1007/s10096-005-1345-3 [DOI] [PubMed] [Google Scholar]
- 83.Collignon P, Nimmo GR, Gottlieb T, Gosbell IB. 2005. Staphylococcus aureus bacteremia, Australia. Emerg. Infect. Dis. 11:554–561. 10.3201/eid1104.040772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huggan PJ, Wells JE, Browne M, Richardson A, Murdoch DR, Chambers ST. 2010. Population-based epidemiology of Staphylococcus aureus bloodstream infection in Canterbury, New Zealand. Intern. Med. J. 40:117–125. 10.1111/j.1445-5994.2009.01910.x [DOI] [PubMed] [Google Scholar]
- 85.Laupland KB, Lyytikainen O, Sogaard M, Kennedy KJ, Knudsen JD, Ostergaard C, Galbraith JC, Valiquette L, Jacobsson G, Collignon P, Schonheyder HC. 2013. The changing epidemiology of Staphylococcus aureus bloodstream infection: a multinational population-based surveillance study. Clin. Microbiol. Infect. 19:465–471. 10.1111/j.1469-0691.2012.03903.x [DOI] [PubMed] [Google Scholar]
- 86.Tom S, Galbraith JC, Valiquette L, Jacobsson G, Collignon P, Schonheyder HC, Sogaard M, Kennedy KJ, Knudsen JD, Ostergaard C, Lyytikainen O, Laupland KB, The International Bacteraemia Surveillance Collaborative 24 January 2014. Case fatality ratio and mortality rate trends of community-onset Staphylococcus aureus bacteraemia. Clin. Microbiol. Infect. 10.1111/1469-0691.12564 [DOI] [PubMed] [Google Scholar]
- 87.Jacobsson G, Dashti S, Wahlberg T, Andersson R. 2007. The epidemiology of and risk factors for invasive Staphylococcus aureus infections in western Sweden. Scand. J. Infect. Dis. 39:6–13. 10.1080/00365540600810026 [DOI] [PubMed] [Google Scholar]
- 88.Laupland KB, Ross T, Gregson DB. 2008. Staphylococcus aureus bloodstream infections: risk factors, outcomes, and the influence of methicillin resistance in Calgary, Canada, 2000–2006. J. Infect. Dis. 198:336–343. 10.1086/589717 [DOI] [PubMed] [Google Scholar]
- 89.Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD. 2003. Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections. J. Infect. Dis. 187:1452–1459. 10.1086/374621 [DOI] [PubMed] [Google Scholar]
- 90.Frimodt-Moller N, Espersen F, Skinhoj P, Rosdahl VT. 1997. Epidemiology of Staphylococcus aureus bacteremia in Denmark from 1957 to 1990. Clin. Microbiol. Infect. 3:297–305. 10.1111/j.1469-0691.1997.tb00617.x [DOI] [PubMed] [Google Scholar]
- 91.Rodriguez-Bano J, Angeles Dominguez M, Blas Millan A, Borraz C, Pau Gonzalez M, Almirante B, Cercenado E, Padilla B, Pujol M. 2009. Clinical and molecular epidemiology of community-acquired, healthcare-associated and nosocomial methicillin-resistant Staphylococcus aureus in Spain. Clin. Microbiol. Infect. 15:1111–1118. 10.1111/j.1469-0691.2009.02717.x [DOI] [PubMed] [Google Scholar]
- 92.Wilson J, Guy R, Elgohari S, Sheridan E, Davies J, Lamagni T, Pearson A. 2011. Trends in sources of meticillin-resistant Staphylococcus aureus (MRSA) bacteraemia: data from the national mandatory surveillance of MRSA bacteraemia in England, 2006–2009. J. Hosp. Infect. 79:211–217. 10.1016/j.jhin.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 93.Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE, McDougal LK, Carey RB, Fridkin SK. 2007. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763–1771. 10.1001/jama.298.15.1763 [DOI] [PubMed] [Google Scholar]
- 94.Lessa FC, Mu Y, Davies J, Murray M, Lillie M, Pearson A, Fridkin SK. 2010. Comparison of incidence of bloodstream infection with methicillin-resistant Staphylococcus aureus between England and United States, 2006–2007. Clin. Infect. Dis. 51:925–928. 10.1086/656414 [DOI] [PubMed] [Google Scholar]
- 95.Vanderkooi OG, Gregson DB, Kellner JD, Laupland KB. 2011. Staphylococcus aureus bloodstream infections in children: a population-based assessment. Paediatr. Child Health 16:276–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Asgeirsson H, Gudlaugsson O, Kristinsson KG, Heiddal S, Kristjansson M. 2011. Staphylococcus aureus bacteraemia in Iceland, 1995–2008: changing incidence and mortality. Clin. Microbiol. Infect. 17:513–518. 10.1111/j.1469-0691.2010.03265.x [DOI] [PubMed] [Google Scholar]
- 97.El Atrouni WI, Knoll BM, Lahr BD, Eckel-Passow JE, Sia IG, Baddour LM. 2009. Temporal trends in the incidence of Staphylococcus aureus bacteremia in Olmsted County, Minnesota, 1998 to 2005: a population-based study. Clin. Infect. Dis. 49:e130–e138. 10.1086/648442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Frederiksen MS, Espersen F, Frimodt-Moller N, Jensen AG, Larsen AR, Pallesen LV, Skov R, Westh H, Skinhoj P, Benfield T. 2007. Changing epidemiology of pediatric Staphylococcus aureus bacteremia in Denmark from 1971 through 2000. Pediatr. Infect. Dis. J. 26:398–405. 10.1097/01.inf.0000261112.53035.4c [DOI] [PubMed] [Google Scholar]
- 99.Benfield T, Espersen F, Frimodt-Moller N, Jensen AG, Larsen AR, Pallesen LV, Skov R, Westh H, Skinhoj P. 2007. Increasing incidence but decreasing in-hospital mortality of adult Staphylococcus aureus bacteraemia between 1981 and 2000. Clin. Microbiol. Infect. 13:257–263. 10.1111/j.1469-0691.2006.01589.x [DOI] [PubMed] [Google Scholar]
- 100.Allard C, Carignan A, Bergevin M, Boulais I, Tremblay V, Robichaud P, Duperval R, Pepin J. 2008. Secular changes in incidence and mortality associated with Staphylococcus aureus bacteraemia in Quebec, Canada, 1991–2005. Clin. Microbiol. Infect. 14:421–428. 10.1111/j.1469-0691.2008.01965.x [DOI] [PubMed] [Google Scholar]
- 101.Hill PC, Birch M, Chambers S, Drinkovic D, Ellis-Pegler RB, Everts R, Murdoch D, Pottumarthy S, Roberts SA, Swager C, Taylor SL, Thomas MG, Wong CG, Morris AJ. 2001. Prospective study of 424 cases of Staphylococcus aureus bacteraemia: determination of factors affecting incidence and mortality. Intern. Med. J. 31:97–103. 10.1111/j.1444-0903.2001.00029.x [DOI] [PubMed] [Google Scholar]
- 102.Tong SY, Bishop EJ, Lilliebridge RA, Cheng AC, Spasova-Penkova Z, Holt DC, Giffard PM, McDonald MI, Currie BJ, Boutlis CS. 2009. Community-associated strains of methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus in indigenous Northern Australia: epidemiology and outcomes. J. Infect. Dis. 199:1461–1470. 10.1086/598218 [DOI] [PubMed] [Google Scholar]
- 103.Mejer N, Westh H, Schonheyder HC, Jensen AG, Larsen AR, Skov R, Benfield T. 2012. Stable incidence and continued improvement in short term mortality of Staphylococcus aureus bacteraemia between 1995 and 2008. BMC Infect. Dis. 12:260. 10.1186/1471-2334-12-260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McDonald P, Mitchell E, Johnson H, Rossney A, Humphreys H, Glynn G, Burd M, Doyle D, McDonnell R. 2002. MRSA bacteraemia: North/South study of MRSA in Ireland 1999. J. Hosp. Infect. 52:288–291. 10.1053/jhin.2002.1274 [DOI] [PubMed] [Google Scholar]
- 105.Morgan M, Salmon R, Keppie N, Evans-Williams D, Hosein I, Looker DN. 1999. All Wales surveillance of methicillin-resistant Staphylococcus aureus (MRSA): the first year's results. J. Hosp. Infect. 41:173–179. 10.1016/S0195-6701(99)90014-2 [DOI] [PubMed] [Google Scholar]
- 106.Griffiths C, Lamagni TL, Crowcroft NS, Duckworth G, Rooney C. 2004. Trends in MRSA in England and Wales: analysis of morbidity and mortality data for 1993–2002. Health Stat. Q. 2004:15–22 [PubMed] [Google Scholar]
- 107.van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. 2012. Predictors of mortality in Staphylococcus aureus bacteremia. Clin. Microbiol. Rev. 25:362–386. 10.1128/CMR.05022-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rudnick W, Liu Z, Shigayeva A, Low DE, Green K, Plevneshi A, Devlin R, Downey J, Katz K, Kitai I, Krajden S, Ostrowska K, Richardson D, Richardson S, Sarabia A, Silverman M, Simor AE, Tyrrell G, McGeer A. 2013. Pneumococcal vaccination programs and the burden of invasive pneumococcal disease in Ontario, Canada, 1995–2011. Vaccine 31:5863–5871. 10.1016/j.vaccine.2013.09.049 [DOI] [PubMed] [Google Scholar]
- 109.Feemster KA, Li Y, Localio AR, Shults J, Edelstein P, Lautenbach E, Smith T, Metlay JP. 2013. Risk of invasive pneumococcal disease varies by neighbourhood characteristics: implications for prevention policies. Epidemiol. Infect. 141:1679–1689. 10.1017/S095026881200235X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Helferty M, Rotondo JL, Martin I, Desai S. 2013. The epidemiology of invasive pneumococcal disease in the Canadian North from 1999 to 2010. Int. J. Circumpolar Health 2013:72. 10.3402/ijch.v72i0.21606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ingels H, Rasmussen J, Andersen PH, Harboe ZB, Glismann S, Konradsen H, Hoffmann S, Valentiner-Branth P, Lambertsen L. 2012. Impact of pneumococcal vaccination in Denmark during the first 3 years after PCV introduction in the childhood immunization programme. Vaccine 30:3944–3950. 10.1016/j.vaccine.2012.03.060 [DOI] [PubMed] [Google Scholar]
- 112.Rosen JB, Thomas AR, Lexau CA, Reingold A, Hadler JL, Harrison LH, Bennett NM, Schaffner W, Farley MM, Beall BW, Moore MR. 2011. Geographic variation in invasive pneumococcal disease following pneumococcal conjugate vaccine introduction in the United States. Clin. Infect. Dis. 53:137–143. 10.1093/cid/cir326 [DOI] [PubMed] [Google Scholar]
- 113.Harboe ZB, Benfield TL, Valentiner-Branth P, Hjuler T, Lambertsen L, Kaltoft M, Krogfelt K, Slotved HC, Christensen JJ, Konradsen HB. 2010. Temporal trends in invasive pneumococcal disease and pneumococcal serotypes over 7 decades. Clin. Infect. Dis. 50:329–337. 10.1086/649872 [DOI] [PubMed] [Google Scholar]
- 114.Weatherholtz R, Millar EV, Moulton LH, Reid R, Rudolph K, Santosham M, O'Brien KL. 2010. Invasive pneumococcal disease a decade after pneumococcal conjugate vaccine use in an American Indian population at high risk for disease. Clin. Infect. Dis. 50:1238–1246. 10.1086/651680 [DOI] [PubMed] [Google Scholar]
- 115.Motlova J, Benes C, Kriz P. 2009. Incidence of invasive pneumococcal disease in the Czech Republic and serotype coverage by vaccines, 1997–2006. Epidemiol. Infect. 137:562–569. 10.1017/S0950268808001301 [DOI] [PubMed] [Google Scholar]
- 116.Hsieh YC, Lin PY, Chiu CH, Huang YC, Chang KY, Liao CH, Chiu NC, Chuang YC, Chen PY, Chang SC, Liu JW, Yen MY, Wang JH, Liu CY, Lin TY. 2009. National survey of invasive pneumococcal diseases in Taiwan under partial PCV7 vaccination in 2007: emergence of serotype 19A with high invasive potential. Vaccine 27:5513–5518. 10.1016/j.vaccine.2009.06.091 [DOI] [PubMed] [Google Scholar]
- 117.Kellner JD, Vanderkooi OG, MacDonald J, Church DL, Tyrrell GJ, Scheifele DW. 2009. Changing epidemiology of invasive pneumococcal disease in Canada, 1998–2007: update from the Calgary-area Streptococcus pneumoniae research (CASPER) study. Clin. Infect. Dis. 49:205–212. 10.1086/599827 [DOI] [PubMed] [Google Scholar]
- 118.Baggett HC, Peruski LF, Olsen SJ, Thamthitiwat S, Rhodes J, Dejsirilert S, Wongjindanon W, Dowell SF, Fischer JE, Areerat P, Sornkij D, Jorakate P, Kaewpan A, Prapasiri P, Naorat S, Sangsuk L, Eampokalap B, Moore MR, Carvalho G, Beall B, Ungchusak K, Maloney SA. 2009. Incidence of pneumococcal bacteremia requiring hospitalization in rural Thailand. Clin. Infect. Dis. 48(Suppl 2):S65–S74. 10.1086/596484 [DOI] [PubMed] [Google Scholar]
- 119.Bruce MG, Deeks SL, Zulz T, Bruden D, Navarro C, Lovgren M, Jette L, Kristinsson K, Sigmundsdottir G, Jensen KB, Lovoll O, Nuorti JP, Herva E, Nystedt A, Sjostedt A, Koch A, Hennessy TW, Parkinson AJ. 2008. International Circumpolar Surveillance system for invasive pneumococcal disease, 1999–2005. Emerg. Infect. Dis. 14:25–33. 10.3201/eid1401.071315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Heffernan HM, Martin DR, Woodhouse RE, Morgan J, Blackmore TK. 2008. Invasive pneumococcal disease in New Zealand 1998–2005: capsular serotypes and antimicrobial resistance. Epidemiol. Infect. 136:352–359. 10.1017/S0950268807008588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lacapa R, Bliss SJ, Larzelere-Hinton F, Eagle KJ, McGinty DJ, Parkinson AJ, Santosham M, Craig MJ, O'Brien KL. 2008. Changing epidemiology of invasive pneumococcal disease among White Mountain Apache persons in the era of the pneumococcal conjugate vaccine. Clin. Infect. Dis. 47:476–484. 10.1086/590001 [DOI] [PubMed] [Google Scholar]
- 122.Klemets P, Lyytikainen O, Ruutu P, Kaijalainen T, Leinonen M, Ollgren J, Nuorti JP. 2008. Trends and geographical variation in invasive pneumococcal infections in Finland. Scand. J. Infect. Dis. 40:621–628. 10.1080/00365540801938931 [DOI] [PubMed] [Google Scholar]
- 123.Einarsdottir HM, Erlendsdottir H, Kristinsson KG, Gottfredsson M. 2005. Nationwide study of recurrent invasive pneumococcal infections in a population with a low prevalence of human immunodeficiency virus infection. Clin. Microbiol. Infect. 11:744–749. 10.1111/j.1469-0691.2005.01221.x [DOI] [PubMed] [Google Scholar]
- 124.Stephens DS, Zughaier SM, Whitney CG, Baughman WS, Barker L, Gay K, Jackson D, Orenstein WA, Arnold K, Schuchat A, Farley MM. 2005. Incidence of macrolide resistance in Streptococcus pneumoniae after introduction of the pneumococcal conjugate vaccine: population-based assessment. Lancet 365:855–863. 10.1016/S0140-6736(05)71043-6 [DOI] [PubMed] [Google Scholar]
- 125.Andresen DN, Collignon PJ. 2004. Invasive pneumococcal disease in the Australian Capital Territory and Queanbeyan region: do high infant rates reflect more disease or better detection? J. Paediatr. Child Health 40:184–188. 10.1111/j.1440-1754.2004.00334.x [DOI] [PubMed] [Google Scholar]
- 126.Yildirim I, Stevenson A, Hsu KK, Pelton SI. 2012. Evolving picture of invasive pneumococcal disease in Massachusetts children: a comparison of disease in 2007–2009 with earlier periods. Pediatr. Infect. Dis. J. 31:1016–1021. 10.1097/INF.0b013e3182615615 [DOI] [PubMed] [Google Scholar]
- 127.Riva E, Salvini F, Garlaschi ML, Radaelli G, Giovannini M. 2012. The status of invasive pneumococcal disease among children younger than 5 years of age in north-west Lombardy, Italy. BMC Infect. Dis. 12:106. 10.1186/1471-2334-12-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Benavides JA, Ovalle OO, Salvador GR, Gray S, Isaacman D, Rodgers GL. 2012. Population-based surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Bogota, Colombia. Vaccine 30:5886–5892. 10.1016/j.vaccine.2012.03.054 [DOI] [PubMed] [Google Scholar]
- 129.Arguedas A, Abdelnour A, Soley C, Jimenez E, Jimenez AL, Ramcharran D, Porat N, Dagan R, Gray S, Rodgers GL. 2012. Prospective epidemiologic surveillance of invasive pneumococcal disease and pneumonia in children in San Jose, Costa Rica. Vaccine 30:2342–2348. 10.1016/j.vaccine.2012.01.047 [DOI] [PubMed] [Google Scholar]
- 130.Andrade AL, Oliveira R, Vieira MA, Minamisava R, Pessoa V, Jr, Brandileone MC, Alves SL, Alfieri F, Pagliarini R, Moraes JC, Gray S, Rodgers GL. 2012. Population-based surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Goiania, Brazil. Vaccine 30:1901–1909. 10.1016/j.vaccine.2011.12.012 [DOI] [PubMed] [Google Scholar]
- 131.Wenger JD, Zulz T, Bruden D, Singleton R, Bruce MG, Bulkow L, Parks D, Rudolph K, Hurlburt D, Ritter T, Klejka J, Hennessy T. 2010. Invasive pneumococcal disease in Alaskan children: impact of the seven-valent pneumococcal conjugate vaccine and the role of water supply. Pediatr. Infect. Dis. J. 29:251–256. 10.1097/INF.0b013e3181bdbed5 [DOI] [PubMed] [Google Scholar]
- 132.Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, Reingold A, Thomas A, Schaffner W, Craig AS, Smith PJ, Beall BW, Whitney CG, Moore MR. 2010. Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J. Infect. Dis. 201:32–41. 10.1086/648593 [DOI] [PubMed] [Google Scholar]
- 133.Castaneda E, Agudelo CI, Regueira M, Corso A, Brandileone MC, Brandao AP, Maldonado A, Hormazabal JC, Martinez IT, Llanes R, Sanchez J, Feris JM, Echaniz-Aviles G, Carnalla-Barajas MN, Terrazas MG, Monroy IH, Chamorro G, Weiler N, Camou T, Gabarrot GG, Spadola E, Payares D, Gabastou JM, Di Fabio JL, de la Hoz F. 2009. Laboratory-based surveillance of Streptococcus pneumoniae invasive disease in children in 10 Latin American countries: a SIREVA II project, 2000–2005. Pediatr. Infect. Dis. J. 28:e265–e270. 10.1097/INF.0b013e3181a74b22 [DOI] [PubMed] [Google Scholar]
- 134.Arifeen SE, Saha SK, Rahman S, Rahman KM, Rahman SM, Bari S, Naheed A, Mannan I, Seraji MH, Ahmed NU, Hassan MS, Huda N, Siddik AU, Quasem I, Islam M, Fatima K, Al-Emran H, Brooks WA, Baqui AH, Breiman RF, Sack D, Luby SP. 2009. Invasive pneumococcal disease among children in rural Bangladesh: results from a population-based surveillance. Clin. Infect. Dis. 48(Suppl 2):S103–S113. 10.1086/596543 [DOI] [PubMed] [Google Scholar]
- 135.Bodle EE, Cunningham JA, Della-Latta P, Schluger NW, Saiman L. 2008. Epidemiology of nontuberculous mycobacteria in patients without HIV infection, New York City. Emerg. Infect. Dis. 14:390–396. 10.3201/eid1403.061143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ho PL, Chiu SS, Cheung CH, Lee R, Tsai TF, Lau YL. 2006. Invasive pneumococcal disease burden in Hong Kong children. Pediatr. Infect. Dis. J. 25:454–455. 10.1097/01.inf.0000215004.85582.30 [DOI] [PubMed] [Google Scholar]
- 137.Feikin DR, Jagero G, Aura B, Bigogo GM, Oundo J, Beall BW, Karani A, Morpeth S, Njenga MK, Breiman RF. 2010. High rate of pneumococcal bacteremia in a prospective cohort of older children and adults in an area of high HIV prevalence in rural western Kenya. BMC Infect. Dis. 10:186. 10.1186/1471-2334-10-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Liu Z, Nachamkin I, Edelstein PH, Lautenbach E, Metlay JP. 2012. Serotype emergence and genotype distribution among macrolide-resistant invasive Streptococcus pneumoniae isolates in the postconjugate vaccine (PCV-7) era. Antimicrob. Agents Chemother. 56:743–750. 10.1128/AAC.05122-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Vila-Corcoles A, Ochoa-Gondar O, Gomez-Bertomeu F, Raga-Luria X. 2011. Invasive pneumococcal disease in Catalonian elderly people, 2002–2009: serotype coverage for different anti-pneumococcal vaccine formulations at the beginning of the new conjugate vaccines era. Vaccine 29:7430–7434. 10.1016/j.vaccine.2011.07.066 [DOI] [PubMed] [Google Scholar]
- 140.Deutscher M, Lewis M, Zell ER, Taylor TH, Jr, Van Beneden C, Schrag S. 2011. Incidence and severity of invasive Streptococcus pneumoniae, group A Streptococcus, and group B Streptococcus infections among pregnant and postpartum women. Clin. Infect. Dis. 53:114–123. 10.1093/cid/cir325 [DOI] [PubMed] [Google Scholar]
- 141.Burckhardt I, Burckhardt F, Van Der Linden M, Heeg C, Reinert RR. 2010. Risk factor analysis for pneumococcal meningitis in adults with invasive pneumococcal infection. Epidemiol. Infect. 138:1353–1358. 10.1017/S0950268809991683 [DOI] [PubMed] [Google Scholar]
- 142.Plevneshi A, Svoboda T, Armstrong I, Tyrrell GJ, Miranda A, Green K, Low D, McGeer A. 2009. Population-based surveillance for invasive pneumococcal disease in homeless adults in Toronto. PLoS One 4:e7255. 10.1371/journal.pone.0007255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Reinert RR, Haupts S, van der Linden M, Heeg C, Cil MY, Al-Lahham A, Fedson DS. 2005. Invasive pneumococcal disease in adults in North-Rhine Westphalia, Germany, 2001–2003. Clin. Microbiol. Infect. 11:985–991. 10.1111/j.1469-0691.2005.01282.x [DOI] [PubMed] [Google Scholar]
- 144.Lyytikainen O, Klemets P, Ruutu P, Kaijalainen T, Rantala M, Ollgren J, Nuorti JP. 2007. Defining the population-based burden of nosocomial pneumococcal bacteremia. Arch. Intern. Med. 167:1635–1640. 10.1001/archinte.167.15.1635 [DOI] [PubMed] [Google Scholar]
- 145.Vanderkooi OG, Church DL, MacDonald J, Zucol F, Kellner JD. 2011. Community-based outbreaks in vulnerable populations of invasive infections caused by Streptococcus pneumoniae serotypes 5 and 8 in Calgary, Canada. PLoS One 6:e28547. 10.1371/journal.pone.0028547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whitney CG, Farley MM, Hadler J, Harrison LH, Bennett NM, Lynfield R, Reingold A, Cieslak PR, Pilishvili T, Jackson D, Facklam RR, Jorgensen JH, Schuchat A. 2003. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N. Engl. J. Med. 348:1737–1746. 10.1056/NEJMoa022823 [DOI] [PubMed] [Google Scholar]
- 147.Meatherall BL, Gregson D, Ross T, Pitout JD, Laupland KB. 2009. Incidence, risk factors, and outcomes of Klebsiella pneumoniae bacteremia. Am. J. Med. 122:866–873. 10.1016/j.amjmed.2009.03.034 [DOI] [PubMed] [Google Scholar]
- 148.Al-Hasan MN, Lahr BD, Eckel-Passow JE, Baddour LM. 2010. Epidemiology and outcome of Klebsiella species bloodstream infection: a population-based study. Mayo Clin. Proc. 85:139–144. 10.4065/mcp.2009.0410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Laupland KB, Schonheyder HC, Kennedy KJ, Lyytikainen O, Valiquette L, Galbraith J, Collignon P. 2010. Salmonella enterica bacteraemia: a multi-national population-based cohort study. BMC Infect. Dis. 10:95. 10.1186/1471-2334-10-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Gradel KO, Schonheyder HC, Pedersen L, Thomsen RW, Norgaard M, Nielsen H. 2006. Incidence and prognosis of non-typhoid Salmonella bacteraemia in Denmark: a 10-year county-based follow-up study. Eur. J. Clin. Microbiol. Infect. Dis. 25:151–158. 10.1007/s10096-006-0110-6 [DOI] [PubMed] [Google Scholar]
- 151.Koch K, Kristensen B, Holt HM, Ethelberg S, Molbak K, Schonheyder HC. 2011. International travel and the risk of hospitalization with non-typhoidal Salmonella bacteremia. A Danish population-based cohort study, 1999–2008. BMC Infect. Dis. 11:277. 10.1186/1471-2334-11-277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tabu C, Breiman RF, Ochieng B, Aura B, Cosmas L, Audi A, Olack B, Bigogo G, Ongus JR, Fields P, Mintz E, Burton D, Oundo J, Feikin DR. 2012. Differing burden and epidemiology of non-Typhi Salmonella bacteremia in rural and urban Kenya, 2006–2009. PLoS One 7:e31237. 10.1371/journal.pone.0031237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Breiman RF, Cosmas L, Njuguna H, Audi A, Olack B, Ochieng JB, Wamola N, Bigogo GM, Awiti G, Tabu CW, Burke H, Williamson J, Oundo JO, Mintz ED, Feikin DR. 2012. Population-based incidence of typhoid fever in an urban informal settlement and a rural area in Kenya: implications for typhoid vaccine use in Africa. PLoS One 7:e29119. 10.1371/journal.pone.0029119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Laupland KB, Parkins MD, Ross T, Pitout JD. 2007. Population-based laboratory surveillance for tribe Proteeae isolates in a large Canadian health region. Clin. Microbiol. Infect. 13:683–688. 10.1111/j.1469-0691.2007.01715.x [DOI] [PubMed] [Google Scholar]
- 155.Al-Hasan MN, Lahr BD, Eckel-Passow JE, Baddour LM. 2011. Temporal trends in Enterobacter species bloodstream infection: a population-based study from 1998–2007. Clin. Microbiol. Infect. 17:539–545. 10.1111/j.1469-0691.2010.03277.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Laupland KB, Parkins MD, Gregson DB, Church DL, Ross T, Pitout JD. 2008. Population-based laboratory surveillance for Serratia species isolates in a large Canadian health region. Eur. J. Clin. Microbiol. Infect. Dis. 27:89–95. 10.1007/s10096-007-0400-7 [DOI] [PubMed] [Google Scholar]
- 157.Engel HJ, Collignon PJ, Whiting PT, Kennedy KJ. 2009. Serratia sp. bacteremia in Canberra, Australia: a population-based study over 10 years. Eur. J. Clin. Microbiol. Infect. Dis. 28:821–824. 10.1007/s10096-009-0707-7 [DOI] [PubMed] [Google Scholar]
- 158.Laupland KB, Church DL, Ross T, Pitout JD. 2006. Population-based laboratory surveillance of Hafnia alvei isolates in a large Canadian health region. Ann. Clin. Microbiol. Antimicrob. 5:12. 10.1186/1476-0711-5-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Laupland KB, Schonheyder HC, Ostergaard C, Knudsen JD, Valiquette L, Galbraith J, Kennedy KJ, Gradel KO. 2011. Epidemiology of Haemophilus influenzae bacteremia: a multi-national population-based assessment. J. Infect. 62:142–148. 10.1016/j.jinf.2010.11.009 [DOI] [PubMed] [Google Scholar]
- 160.Ladhani S, Slack MP, Heath PT, von Gottberg A, Chandra M, Ramsay ME. 2010. Invasive Haemophilus influenzae disease, Europe, 1996–2006. Emerg. Infect. Dis. 16:455–463. 10.3201/eid1603.090290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Tsang RS, Sill ML, Skinner SJ, Law DK, Zhou J, Wylie J. 2007. Characterization of invasive Haemophilus influenzae disease in Manitoba, Canada, 2000–2006: invasive disease due to non-type b strains. Clin. Infect. Dis. 44:1611–1614. 10.1086/518283 [DOI] [PubMed] [Google Scholar]
- 162.Degani N, Navarro C, Deeks SL, Lovgren M. 2008. Invasive bacterial diseases in northern Canada. Emerg. Infect. Dis. 14:34–40. 10.3201/eid1401.061522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Adam HJ, Richardson SE, Jamieson FB, Rawte P, Low DE, Fisman DN. 2010. Changing epidemiology of invasive Haemophilus influenzae in Ontario, Canada: evidence for herd effects and strain replacement due to Hib vaccination. Vaccine 28:4073–4078. 10.1016/j.vaccine.2010.03.075 [DOI] [PubMed] [Google Scholar]
- 164.Dworkin MS, Park L, Borchardt SM. 2007. The changing epidemiology of invasive Haemophilus influenzae disease, especially in persons > or = 65 years old. Clin. Infect. Dis. 44:810–816. 10.1086/511861 [DOI] [PubMed] [Google Scholar]
- 165.Berndsen MR, Erlendsdottir H, Gottfredsson M. 2012. Evolving epidemiology of invasive Haemophilus infections in the post-vaccination era: results from a long-term population-based study. Clin. Microbiol. Infect. 18:918–923. 10.1111/j.1469-0691.2011.03700.x [DOI] [PubMed] [Google Scholar]
- 166.Livorsi DJ, Macneil JR, Cohn AC, Bareta J, Zansky S, Petit S, Gershman K, Harrison LH, Lynfield R, Reingold A, Schaffner W, Thomas A, Farley MM. 2012. Invasive Haemophilus influenzae in the United States, 1999–2008: epidemiology and outcomes. J. Infect. 65:496–504. 10.1016/j.jinf.2012.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Al-Hasan MN, Wilson JW, Lahr BD, Eckel-Passow JE, Baddour LM. 2008. Incidence of Pseudomonas aeruginosa bacteremia: a population-based study. Am. J. Med. 121:702–708. 10.1016/j.amjmed.2008.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Parkins MD, Gregson DB, Pitout JD, Ross T, Laupland KB. 2010. Population-based study of the epidemiology and the risk factors for Pseudomonas aeruginosa bloodstream infection. Infection 38:25–32. 10.1007/s15010-009-9145-9 [DOI] [PubMed] [Google Scholar]
- 169.Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, Hadler JL, Danila R, Cieslak PR, Schuchat A. 2000. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N. Engl. J. Med. 342:15–20. 10.1056/NEJM200001063420103 [DOI] [PubMed] [Google Scholar]
- 170.Davies HD, McGeer A, Schwartz B, Green K, Cann D, Simor AE, Low DE. 1996. Invasive group A streptococcal infections in Ontario, Canada. Ontario Group A Streptococcal Study Group. N. Engl. J. Med. 335:547–554 [DOI] [PubMed] [Google Scholar]
- 171.Steer AC, Jenney AJ, Oppedisano F, Batzloff MR, Hartas J, Passmore J, Russell FM, Kado JH, Carapetis JR. 2008. High burden of invasive beta-haemolytic streptococcal infections in Fiji. Epidemiol. Infect. 136:621–627. 10.1017/S095026880700917X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Laupland KB, Ross T, Church DL, Gregson DB. 2006. Population-based surveillance of invasive pyogenic streptococcal infection in a large Canadian region. Clin. Microbiol. Infect. 12:224–230. 10.1111/j.1469-0691.2005.01345.x [DOI] [PubMed] [Google Scholar]
- 173.Rantala S, Vuopio-Varkila J, Vuento R, Huhtala H, Syrjanen J. 2009. Clinical presentations and epidemiology of beta-haemolytic streptococcal bacteraemia: a population-based study. Clin. Microbiol. Infect. 15:286–288. 10.1111/j.1469-0691.2008.02672.x [DOI] [PubMed] [Google Scholar]
- 174.Ekelund K, Skinhoj P, Madsen J, Konradsen HB. 2005. Invasive group A, B, C and G streptococcal infections in Denmark 1999–2002: epidemiological and clinical aspects. Clin. Microbiol. Infect. 11:569–576. 10.1111/j.1469-0691.2005.01169.x [DOI] [PubMed] [Google Scholar]
- 175.Pinholt M, Ostergaard C, Arpi M, Bruun NE, Schonheyder HC, Gradel KO, Sogaard M, Knudsen JD. 2014. Incidence, clinical characteristics and 30-day mortality of enterococcal bacteraemia in Denmark 2006–2009: a population-based cohort study. Clin. Microbiol. Infect. 20:145–151. 10.1111/1469-0691.12236 [DOI] [PubMed] [Google Scholar]
- 176.Ngo JT, Parkins MD, Gregson DB, Pitout JD, Ross T, Church DL, Laupland KB. 2013. Population-based assessment of the incidence, risk factors, and outcomes of anaerobic bloodstream infections. Infection 41:41–48. 10.1007/s15010-012-0389-4 [DOI] [PubMed] [Google Scholar]
- 177.Leal J, Gregson DB, Ross T, Church DL, Laupland KB. 2008. Epidemiology of Clostridium species bacteremia in Calgary, Canada, 2000–2006. J. Infect. 57:198–203. 10.1016/j.jinf.2008.06.018 [DOI] [PubMed] [Google Scholar]
- 178.Huggan PJ, Murdoch DR. 2008. Fusobacterial infections: clinical spectrum and incidence of invasive disease. J. Infect. 57:283–289. 10.1016/j.jinf.2008.07.016 [DOI] [PubMed] [Google Scholar]
- 179.Hagelskjaer Kristensen L, Prag J. 2008. Lemierre's syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur. J. Clin. Microbiol. Infect. Dis. 27:779–789. 10.1007/s10096-008-0496-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Afra K, Laupland K, Leal J, Lloyd T, Gregson D. 2013. Incidence, risk factors, and outcomes of Fusobacterium species bacteremia. BMC Infect. Dis. 13:264. 10.1186/1471-2334-13-264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.St-Germain G, Laverdiere M, Pelletier R, Rene P, Bourgault AM, Lemieux C, Libman M. 2008. Epidemiology and antifungal susceptibility of bloodstream Candida isolates in Quebec: report on 453 cases between 2003 and 2005. Can. J. Infect. Dis. Med. Microbiol. 19:55–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Odds FC, Hanson MF, Davidson AD, Jacobsen MD, Wright P, Whyte JA, Gow NA, Jones BL. 2007. One year prospective survey of Candida bloodstream infections in Scotland. J. Med. Microbiol. 56:1066–1075. 10.1099/jmm.0.47239-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Arendrup MC, Fuursted K, Gahrn-Hansen B, Jensen IM, Knudsen JD, Lundgren B, Schonheyder HC, Tvede M. 2005. Seminational surveillance of fungemia in Denmark: notably high rates of fungemia and numbers of isolates with reduced azole susceptibility. J. Clin. Microbiol. 43:4434–4440. 10.1128/JCM.43.9.4434-4440.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Poikonen E, Lyytikainen O, Anttila VJ, Koivula I, Lumio J, Kotilainen P, Syrjala H, Ruutu P. 2010. Secular trend in candidemia and the use of fluconazole in Finland, 2004–2007. BMC Infect. Dis. 10:312. 10.1186/1471-2334-10-312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sandven P, Bevanger L, Digranes A, Haukland HH, Mannsaker T, Gaustad P. 2006. Candidemia in Norway (1991 to 2003): results from a nationwide study. J. Clin. Microbiol. 44:1977–1981. 10.1128/JCM.00029-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Laupland KB, Gregson DB, Church DL, Ross T, Elsayed S. 2005. Invasive Candida species infections: a 5 year population-based assessment. J. Antimicrob. Chemother. 56:532–537. 10.1093/jac/dki258 [DOI] [PubMed] [Google Scholar]
- 187.Rodriguez D, Almirante B, Cuenca-Estrella M, Rodriguez-Tudela JL, Mensa J, Ayats J, Sanchez F, Pahissa A. 2010. Predictors of candidaemia caused by non-albicans Candida species: results of a population-based surveillance in Barcelona, Spain. Clin. Microbiol. Infect. 16:1676–1682. 10.1111/j.1469-0691.2010.03208.x [DOI] [PubMed] [Google Scholar]
- 188.Sofair AN, Lyon GM, Huie-White S, Reiss E, Harrison LH, Sanza LT, Arthington-Skaggs BA, Fridkin SK. 2006. Epidemiology of community-onset candidemia in Connecticut and Maryland. Clin. Infect. Dis. 43:32–39. 10.1086/504807 [DOI] [PubMed] [Google Scholar]
- 189.Asmundsdottir LR, Erlendsdottir H, Gottfredsson M. 2013. Nationwide study of candidemia, antifungal use, and antifungal drug resistance in Iceland, 2000 to 2011. J. Clin. Microbiol. 51:841–848. 10.1128/JCM.02566-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tan LK, Lacey S, Mandalia S, Melzer M. 2008. Hospital-based study of viridans streptococcal bacteraemia in children and adults. J. Infect. 56:103–107. 10.1016/j.jinf.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 191.Voetsch AC, Angulo FJ, Jones TF, Moore MR, Nadon C, McCarthy P, Shiferaw B, Megginson MB, Hurd S, Anderson BJ, Cronquist A, Vugia DJ, Medus C, Segler S, Graves LM, Hoekstra RM, Griffin PM. 2007. Reduction in the incidence of invasive listeriosis in foodborne diseases active surveillance network sites, 1996–2003. Clin. Infect. Dis. 44:513–520. 10.1086/511006 [DOI] [PubMed] [Google Scholar]
- 192.Gil-Prieto R, Garcia-Garcia L, Alvaro-Meca A, Gonzalez-Escalada A, Viguera Ester P, Gil De Miguel A. 2011. The burden of hospitalizations for meningococcal infection in Spain (1997–2008). Vaccine 29:5765–5770. 10.1016/j.vaccine.2011.05.089 [DOI] [PubMed] [Google Scholar]
- 193.Harrison LH, Trotter CL, Ramsay ME. 2009. Global epidemiology of meningococcal disease. Vaccine 27(Suppl 2):B51–B63. 10.1016/j.vaccine.2009.04.063 [DOI] [PubMed] [Google Scholar]
- 194.Cohen C, Singh E, Wu HM, Martin S, de Gouveia L, Klugman KP, Meiring S, Govender N, von Gottberg A. 2010. Increased incidence of meningococcal disease in HIV-infected individuals associated with higher case-fatality ratios in South Africa. AIDS 24:1351–1360. 10.1097/QAD.0b013e32833a2520 [DOI] [PubMed] [Google Scholar]
- 195.Bhengsri S, Baggett HC, Jorakate P, Kaewpan A, Prapasiri P, Naorat S, Thamthitiwat S, Tanwisaid K, Chantra S, Salika P, Dejsirilert S, Peruski LF, Maloney SA. 2011. Incidence of bacteremic melioidosis in eastern and northeastern Thailand. Am. J. Trop. Med. Hyg. 85:117–120. 10.4269/ajtmh.2011.11-0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Currie BJ, Jacups SP, Cheng AC, Fisher DA, Anstey NM, Huffam SE, Krause VL. 2004. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop. Med. Int. Health 9:1167–1174. 10.1111/j.1365-3156.2004.01328.x [DOI] [PubMed] [Google Scholar]
- 197.Heng BH, Goh KT, Yap EH, Loh H, Yeo M. 1998. Epidemiological surveillance of melioidosis in Singapore. Ann. Acad. Med. Singapore 27:478–484 [PubMed] [Google Scholar]
- 198.How SH, Ng KH, Jamalludin AR, Shah A, Rathor Y. 2005. Melioidosis in Pahang, Malaysia. Med. J. Malaysia 60:606–613 [PubMed] [Google Scholar]
- 199.Hassan MR, Pani SP, Peng NP, Voralu K, Vijayalakshmi N, Mehanderkar R, Aziz NA, Michael E. 2010. Incidence, risk factors and clinical epidemiology of melioidosis: a complex socio-ecological emerging infectious disease in the Alor Setar region of Kedah, Malaysia. BMC Infect. Dis. 10:302. 10.1186/1471-2334-10-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Nimri LF, Batchoun R. 2004. Community-acquired bacteraemia in a rural area: predominant bacterial species and antibiotic resistance. J. Med. Microbiol. 53:1045–1049. 10.1099/jmm.0.05503-0 [DOI] [PubMed] [Google Scholar]
- 201.Porter S, Ketheesan N, Norton R. 2013. Bacteraemias in tropical Australia: changing trends over a 10-year period. Diagn. Microbiol. Infect. Dis. 75:266–270. 10.1016/j.diagmicrobio.2012.11.017 [DOI] [PubMed] [Google Scholar]
- 202.Chamberlin J, Laughlin LW, Romero S, Solorzano N, Gordon S, Andre RG, Pachas P, Friedman H, Ponce C, Watts D. 2002. Epidemiology of endemic Bartonella bacilliformis: a prospective cohort study in a Peruvian mountain valley community. J. Infect. Dis. 186:983–990. 10.1086/344054 [DOI] [PubMed] [Google Scholar]
- 203.Tabah A, Koulenti D, Laupland K, Misset B, Valles J, Bruzzi de Carvalho F, Paiva JA, Cakar N, Ma X, Eggimann P, Antonelli M, Bonten MJ, Csomos A, Krueger WA, Mikstacki A, Lipman J, Depuydt P, Vesin A, Garrouste-Orgeas M, Zahar JR, Blot S, Carlet J, Brun-Buisson C, Martin C, Rello J, Dimopoulos G, Timsit JF. 2012. Characteristics and determinants of outcome of hospital-acquired bloodstream infections in intensive care units: the EUROBACT International Cohort Study. Intensive Care Med. 38:1930–1945. 10.1007/s00134-012-2695-9 [DOI] [PubMed] [Google Scholar]
- 204.Timsit JF, Laupland KB. 2012. Update on bloodstream infections in ICUs. Curr. Opin. Crit. Care 18:479–486. 10.1097/MCC.0b013e328356cefe [DOI] [PubMed] [Google Scholar]
- 205.Chuang YY, Huang YC. 2013. Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Asia. Lancet Infect. Dis. 13:698–708. 10.1016/S1473-3099(13)70136-1 [DOI] [PubMed] [Google Scholar]
- 206.David MZ, Daum RS. 2010. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 23:616–687. 10.1128/CMR.00081-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Pitout JD, Laupland KB. 2008. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect. Dis. 8:159–166. 10.1016/S1473-3099(08)70041-0 [DOI] [PubMed] [Google Scholar]
- 208.Nordmann P. 2014. Carbapenemase-producing Enterobacteriaceae: overview of a major public health challenge. Med. Mal. Infect. 44:51–56. 10.1016/j.medmal.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 209.Saravolatz LD, Pohlod DJ, Arking LM. 1982. Community-acquired methicillin-resistant Staphylococcus aureus infections: a new source for nosocomial outbreaks. Ann. Intern. Med. 97:325–329. 10.7326/0003-4819-97-3-325 [DOI] [PubMed] [Google Scholar]
- 210.Laupland KB, Lyytikainen O, Sogaard M, Kennedy KJ, Knudsen JD, Ostergaard C, Galbraith JC, Valiquette L, Jacobsson G, Collignon P, Schonheyder HC. 2013. The changing epidemiology of Staphylococcus aureus bloodstream infection: a multinational population-based surveillance study. Clin. Microbiol. Infect. 19:465–471. 10.1111/j.1469-0691.2012.03903.x [DOI] [PubMed] [Google Scholar]
- 211.Skov RL, Jensen KS. 2009. Community-associated meticillin-resistant Staphylococcus aureus as a cause of hospital-acquired infections. J. Hosp. Infect. 73:364–370. 10.1016/j.jhin.2009.07.004 [DOI] [PubMed] [Google Scholar]
- 212.Pitout JD, Hanson ND, Church DL, Laupland KB. 2004. Population-based laboratory surveillance for Escherichia coli-producing extended-spectrum beta-lactamases: importance of community isolates with blaCTX-M genes. Clin. Infect. Dis. 38:1736–1741. 10.1086/421094 [DOI] [PubMed] [Google Scholar]
- 213.Kang CI, Wi YM, Lee MY, Ko KS, Chung DR, Peck KR, Lee NY, Song JH. 2012. Epidemiology and risk factors of community onset infections caused by extended-spectrum beta-lactamase-producing Escherichia coli strains. J. Clin. Microbiol. 50:312–317. 10.1128/JCM.06002-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Lowe CF, Katz K, McGeer AJ, Muller MP. 2013. Efficacy of admission screening for extended-spectrum beta-lactamase producing Enterobacteriaceae. PLoS One 8:e62678. 10.1371/journal.pone.0062678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ho PL, Chow KH, Lai EL, Lau EH, Cheng VC. 2012. Extended-spectrum-beta-lactamase-positive Escherichia coli mainly adds to, rather than replaces, extended-spectrum-beta-lactamase-negative E. coli in causing bacteraemia in Hong Kong, 2000–10. J. Antimicrob. Chemother. 67:778–780. 10.1093/jac/dkr502 [DOI] [PubMed] [Google Scholar]
- 216.de Kraker ME, Jarlier V, Monen JC, Heuer OE, van de Sande N, Grundmann H. 2013. The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin. Microbiol. Infect. 19:860–868. 10.1111/1469-0691.12028 [DOI] [PubMed] [Google Scholar]
- 217.Laupland KB, Church DL, Vidakovich J, Mucenski M, Pitout JD. 2008. Community-onset extended-spectrum beta-lactamase (ESBL) producing Escherichia coli: importance of international travel. J. Infect. 57:441–448. 10.1016/j.jinf.2008.09.034 [DOI] [PubMed] [Google Scholar]
- 218.Freeman JT, McBride SJ, Nisbet MS, Gamble GD, Williamson DA, Taylor SL, Holland DJ. 2012. Bloodstream infection with extended-spectrum beta-lactamase-producing Enterobacteriaceae at a tertiary care hospital in New Zealand: risk factors and outcomes. Int. J. Infect. Dis. 16:e371–e374. 10.1016/j.ijid.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 219.Walsh TR, Weeks J, Livermore DM, Toleman MA. 2011. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. Lancet Infect. Dis. 11:355–362. 10.1016/S1473-3099(11)70059-7 [DOI] [PubMed] [Google Scholar]
- 220.Karfunkel D, Carmeli Y, Chmelnitsky I, Kotlovsky T, Navon-Venezia S. 2013. The emergence and dissemination of CTX-M-producing Escherichia coli sequence type 131 causing community-onset bacteremia in Israel. Eur. J. Clin. Microbiol. Infect. Dis. 32:513–521. 10.1007/s10096-012-1765-9 [DOI] [PubMed] [Google Scholar]
- 221.Peirano G, van der Bij AK, Gregson DB, Pitout JD. 2012. Molecular epidemiology over an 11-year period (2000 to 2010) of extended-spectrum beta-lactamase-producing Escherichia coli causing bacteremia in a centralized Canadian region. J. Clin. Microbiol. 50:294–299. 10.1128/JCM.06025-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.van der Bij AK, Pitout JD. 2012. The role of international travel in the worldwide spread of multiresistant Enterobacteriaceae. J. Antimicrob. Chemother. 67:2090–2100. 10.1093/jac/dks214 [DOI] [PubMed] [Google Scholar]
- 223.Adams-Sapper S, Diep BA, Perdreau-Remington F, Riley LW. 2013. Clonal composition and community clustering of drug-susceptible and -resistant Escherichia coli isolates from bloodstream infections. Antimicrob. Agents Chemother. 57:490–497. 10.1128/AAC.01025-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Banerjee R, Johnston B, Lohse C, Chattopadhyay S, Tchesnokova V, Sokurenko EV, Johnson JR. 2013. The clonal distribution and diversity of extraintestinal Escherichia coli isolates vary according to patient characteristics. Antimicrob. Agents Chemother. 57:5912–5917. 10.1128/AAC.01065-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Colpan A, Johnston B, Porter S, Clabots C, Anway R, Thao L, Kuskowski MA, Tchesnokova V, Sokurenko EV, Johnson JR. 2013. Escherichia coli sequence type 131 (ST131) subclone H30 as an emergent multidrug-resistant pathogen among US veterans. Clin. Infect. Dis. 57:1256–1265. 10.1093/cid/cit503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Johnson JR, Tchesnokova V, Johnston B, Clabots C, Roberts PL, Billig M, Riddell K, Rogers P, Qin X, Butler-Wu S, Price LB, Aziz M, Nicolas-Chanoine MH, Debroy C, Robicsek A, Hansen G, Urban C, Platell J, Trott DJ, Zhanel G, Weissman SJ, Cookson BT, Fang FC, Limaye AP, Scholes D, Chattopadhyay S, Hooper DC, Sokurenko EV. 2013. Abrupt emergence of a single dominant multidrug-resistant strain of Escherichia coli. J. Infect. Dis. 207:919–928. 10.1093/infdis/jis933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Price LB, Johnson JR, Aziz M, Clabots C, Johnston B, Tchesnokova V, Nordstrom L, Billig M, Chattopadhyay S, Stegger M, Andersen PS, Pearson T, Riddell K, Rogers P, Scholes D, Kahl B, Keim P, Sokurenko EV. 2013. The epidemic of extended-spectrum-β-lactamase-producing Escherichia coli ST131 is driven by a single highly pathogenic subclone, H30-Rx. mBio 4:e00377-13. 10.1128/mBio.00377-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Carignan A, Roussy JF, Lapointe V, Valiquette L, Sabbagh R, Pepin J. 2012. Increasing risk of infectious complications after transrectal ultrasound-guided prostate biopsies: time to reassess antimicrobial prophylaxis? Eur. Urol. 62:453–459. 10.1016/j.eururo.2012.04.044 [DOI] [PubMed] [Google Scholar]
- 229.Williamson DA, Roberts SA, Paterson DL, Sidjabat H, Silvey A, Masters J, Rice M, Freeman JT. 2012. Escherichia coli bloodstream infection after transrectal ultrasound-guided prostate biopsy: implications of fluoroquinolone-resistant sequence type 131 as a major causative pathogen. Clin. Infect. Dis. 54:1406–1412. 10.1093/cid/cis194 [DOI] [PubMed] [Google Scholar]
- 230.Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Cornaglia G, Garau J, Gniadkowski M, Hayden MK, Kumarasamy K, Livermore DM, Maya JJ, Nordmann P, Patel JB, Paterson DL, Pitout J, Villegas MV, Wang H, Woodford N, Quinn JP. 2013. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect. Dis. 13:785–796. 10.1016/S1473-3099(13)70190-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, Chaudhary U, Doumith M, Giske CG, Irfan S, Krishnan P, Kumar AV, Maharjan S, Mushtaq S, Noorie T, Paterson DL, Pearson A, Perry C, Pike R, Rao B, Ray U, Sarma JB, Sharma M, Sheridan E, Thirunarayan MA, Turton J, Upadhyay S, Warner M, Welfare W, Livermore DM, Woodford N. 2010. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect. Dis. 10:597–602. 10.1016/S1473-3099(10)70143-2 [DOI] [PMC free article] [PubMed] [Google Scholar]