Introduction
There is no national law in the United States concerning the number of embryos that can be transferred into the uterus following fertilization in vitro.
However, the American Fertility Society (AFS) (later the American Society for Reproductive Medicine) (ASRM) first referred to a limitation of numbers to transfer in 1994 (Ethics Committee, American Fertility Society). The recommendation did not specify specific numbers but charged programs to transfer a number which would eliminate quadruplets and limit triplets to no more than 1-2%. These recommendations were later converted into specific numbers and the guidelines have been revised from time to time since then. The 2009 revision is the first to mention, much less recommend, SET in “favorable patients” under the age of 35 years (Table 1).
Table I. Recommended limits on the numbers of embryos to transfer.
| Age | ||||
|---|---|---|---|---|
| Prognosis | < 35 yrs | 35-37 yrs | 38-40 yrs | 41-42 yrs |
| Cleavage-stage embryosa | ||||
| Favorableb | 1-2 | 2 | 3 | 5 |
| All others | 2 | 3 | 4 | 5 |
| Blastocystsa | ||||
| Favorableb | 1 | 2 | 2 | 3 |
| All others | 2 | 2 | 3 | 3 |
a See text for more complete explanations. Justification for transferring one additional embryo more than the recommended limit should be clearly documented in the patient’s medical record.
b Favorable = first cycle of IVF, good embryo quality, excess embryos available for cryopreservation, or previous successful IVF cycle.
Practice Committee Number of Embryos Transferred. Fertil Steril 2009.
It is not easy to correlate the effect of the ever restricting guidelines with the incidence of multiple pregnancies from IVF.
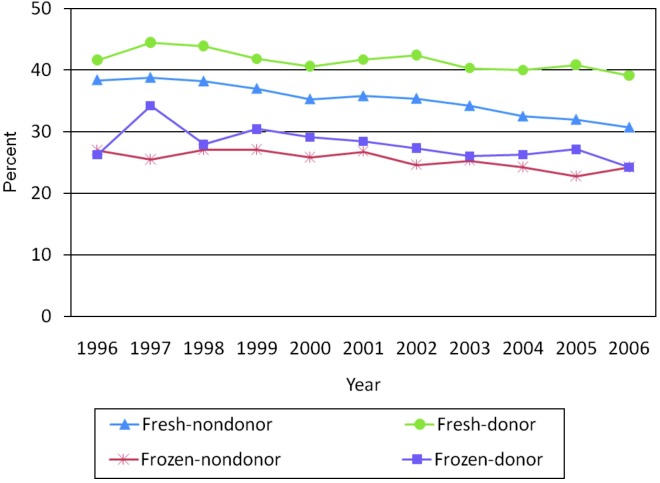
From 1996 through 2006, there was a very modest decrease in the percentage of multiple births from IVF as compared to total births from IVF (Fig. 1). Nevertheless, in 2006, multiples still accounted for 25.1% of live births from IVF (2006 CDC Assisted Reproductive Technology Report).
Fig. 1. Percentage of IVF cycles that resulted in multiple infant live births by type of ART cycle 1996-2006 (2006 Assisted Reproductive Technology [ART] report.
The situation is further complicated by the fact that in the United States there is no tabulation of the use of selective reduction. It is necessary to consider the possibility that the modest decrease in multiple births shown in figure 1 is almost entirely the consequence of selective reduction.
A complete understanding of the multiple pregnancy problem in the United States is incomplete without considering the role of ovulation induction and ovulation enhancement (OI/OE). There is no reporting requirement but an estimate of the role of OI/OE can be made on the basis of the National Vital Statistics which tabulate multiple births as well as the total number of births as reported on birth certificates which by law are required to be filed.
Using these data, it can be derived that multiple births from OI/OE can be ascertained by subtracting from the total number of multiple births those multiple births estimated to occur naturally and those births reported to the Center for Disease Control for IVF. When this is done for the years 2000-2003, IVF accounts for about 8% of twin births, OI/OE about 30%, and natural twinning the remainder. For triplets, IVF accounts for 15%, OI/OE 65%, and natural twinning for the residual 20% (Jones, 2007).
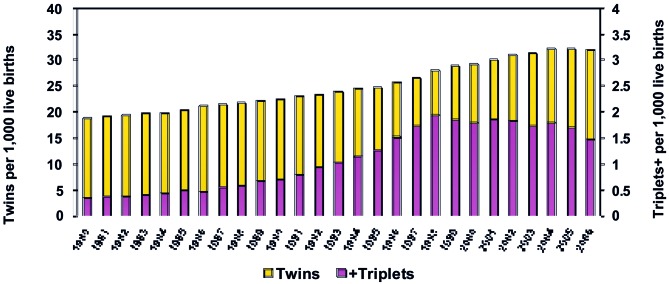
A final background point is that nationally triplets as a percentage of total births peaked in 1998 and have declined definitely but slightly since that time. However, triplets still accounted for 1.5/1,000 live births compared to a natural incidence of less than 0.5/1,000 live births (Fig. 2). Furthermore, twins as a percentage of all births peaked in 2004 and have plateaued in the remaining years of data available. As of 2006, twins for the entire U.S. population were 1.8 times as frequent as could be expected from spontaneous twinning (Fig. 2).
Fig. 2. Twin and triplet birth rates for the entire United States as a percentage of total births (U.S. Vital Statistics).
While there has been only limited support for SET by any national organization in the United States, there have been individual voices promoting the concept.
Thus, Gardner and Lane (2003) advocated the use of blastocysts rather than earlier stages if SET were to be applied. In addition, the Shady Grove Center reported results from 784 eSET using blastocysts in a selected group of patients. The twinning for this class of patients dropped from 44% to 1% (Stillman et al., 2009).
SET and Health Insurance
IVF health insurance coverage in the United States is complicated since independent health insurance companies determine reimbursable benefits and not the government. Coverage for the treatment of infertility, including IVF, is limited. IVF benefits vary from small, lifetime dollar amounts to a few insurance plans having unlimited IVF coverage with most patients having benefits for one to two IVF attempts. There is no uniformity in the design of IVF benefits and patients with limited coverage may exhaust them prior to becoming pregnant. Most insurance companies or employers do not provide treatment coverage leaving the majority of IVF patients to pay for all their services out of pocket. These healthcare payers perceive infertility benefits to be expensive so they are excluded from coverage (Employer Guide on Fertility Benefits).
The insurance plans that cover IVF services are aware that multiple pregnancies are a consequence of treatment but have not developed policies with providers to attempt to reduce multiples. They typically focus on the reimbursement of IVF services only. This is expensive for the plans as a patient may not be covered for IVF but if she becomes pregnant all maternity services are covered including multiples. Some insurance companies are now acknowledging the large costs associated with neonatal intensive care and are actively looking for solutions to this issue.
SET is a key starting point in redefining infertility coverage in the United States. Hundreds of millions of dollars would be saved when medical providers implement a SET policy for IVF services. (Jones and Allen, 2009). Providers have been reluctant to change their current medical practices as they fear their overall success rate will decrease with SET and so will patient volumes. Insurance plans would be wise to collaborate with providers and share a portion of the savings with them. Using SET to reduce multiple pregnancies costs associated with IVF is the first step. The second step would involve reducing multiple pregnancy costs associated with ovulation induction which greatly outnumber the costs from IVF. These savings are estimated to be billions of dollars and could be redirected to allow infertility coverage for all in the United States. These savings can be translated into dollars for 2006 and amount over 4.5 billion dollars (Table 2). The total dollar figure is underestimated as not all IVF clinics report to their outcomes to SART and the total number of SART twins and triplets or higher was calculated from the Fresh Embryos from Non-Donor Oocytes category only.
Table II. 2006 National Multiple Births and 2005 Institute of Medicine (IOM) ART Preterm Delivery Percentages.
| 2006 National Multiple Births | Twins | Triplets or More | Total | |||
|---|---|---|---|---|---|---|
| 2006 SART (Fresh Embryos from Non-Donor Oocytes only) | 7.433 | 5% | 472 | 7% | ||
| Ovulation Induction (OI) & Ovulation Enhancement (OE) | 52.872 | 39% | 4.490 | 69% | ||
| Natural Mutiples | 76.780 | 56% | 1.578 | 24% | ||
| Total Multiple Births | 137.085 | 6.540 | ||||
| SART | 7.433 | 472 | ||||
| IOM Preterm % | 61,7% | 97,2% | ||||
| Est SART Preterm Deliveries | 4.586 | 459 | ||||
| Number of Infants per Pregnancy | 2 | 3 | ||||
| Total Number of Infants | 9.172 | 1.376 | 10.549 | |||
| IOM Cost per Infant Born Preterm | $ 51.500 | $ 51.500 | ||||
| Estimated SART Costs | $ 472.374.583 | $ 70.882.128 | $ 543.256.711 | 12% | ||
| OI & OE | 52.872 | 4.490 | ||||
| IOM Preterm % | 61,7% | 97,2% | ||||
| Est OI & OE Preterm Deliveries | 32.622 | 4.364 | ||||
| Number of Infants per Pregnancy | 2 | 3 | ||||
| Total Number of Infants | 65.244 | 13.092 | 78.336 | |||
| IOM Cost per Infant Born Preterm | $ 51.500 | $ 51.500 | ||||
| Estimated OI & OE Costs | $ 3.360.069.108 | $ 674.242.913 | $ 4.034.312.021 | 88% | ||
| SART & OI & OE | 60.305 | 4.962 | ||||
| IOM Preterm % | 61,7% | 97,2% | ||||
| Est SART & OI & OE Preterm Deliveries | 37.208 | 4.823 | ||||
| Number of Infants per Pregnancy | 2 | 3 | ||||
| Total Number of Infants | 74.416 | 4.468 | 88.885 | |||
| IOM Cost per Infant Born Preterm | $ 51.500 | $ 51.500 | ||||
| Estimated SART & OI & OE Costs | $ 3.832.443.691 | $ 745.125.041 | $ 4.577.568.732 | |||
Education will be a key component to redesigning infertility benefits. Patients need education regarding the risks of multiple pregnancies including long-term care for disabling infant conditions, providers need education that reducing multiple pregnancy rates does not affect the clinic’s ability to compete, and insurance plans need education on the appropriate management of cost-effective infertility services. These updates could provide infertility coverage to the majority of infertility patients who are not currently covered in the United States.
Conclusion
SET has not been widely used in the United States. The substantial reduction or elimination of costs associated with multiple pregnancies caused by IVF and ovulation induction or enhancement would provide ample funds to pay for IVF insurance for all women in the reproductive age. However, such insurance would necessarily provide for SET to achieve that goal. An approach to the acceptance of SET is therefore the cost savings associated with it. However, in the United States, IVF accounts for a relatively small portion of the multiple pregnancy problem. In the United States the principle multiple pregnancy problem is associated with ovulation induction or ovulation enhancement. The implication is that on a cost basis to really eliminate the multiple pregnancies, most cases now treated by ovulation induction or ovulation enhancement would have to be converted to IVF.
References
- Ethics Committee American Fertility Society. Ethical Considerations of Assisted Reproductive Technologies. Fertil Steril. 1994;62(Suppl 1):37. [PubMed] [Google Scholar]
- Gardner DK, Lane M. Towards a single embryo transfer. Reprod Biomed Online. 2003;4:470–481. doi: 10.1016/s1472-6483(10)62170-0. [DOI] [PubMed] [Google Scholar]
- Jones HW. Iatrogenic multiple births: a 2003 checkup. Fertil Steril. 2007;87:453–455. doi: 10.1016/j.fertnstert.2006.11.079. [DOI] [PubMed] [Google Scholar]
- Stillman RJ, Richter KS, Banks NK, et al. Elective single embryo transfer: a 6-year progressive implementation of 784 single blastocyst transfers and the influence of payment method on patient choice. Fertil Steril . 2009;92:1895–1906. doi: 10.1016/j.fertnstert.2008.09.023. [DOI] [PubMed] [Google Scholar]
- Employer Guide on Fertility Benefits. Organon USA Inc; 2007. [Google Scholar]
- Jones HW, Allen BA. Strategies for designing an efficient insurance fertility benefit: a 21st century approach. Fertil Steril. 2009;91:2295–2297. doi: 10.1016/j.fertnstert.2008.03.006. [DOI] [PubMed] [Google Scholar]