Abstract
Epidemiology is now well recognized as the foundation of public health. The Da Qing study in 1986 was the first milestone study to show that lifestyle intervention can prevent or delay the onset of diabetes. The lead investigator of that study, Professor Xiaoren Pan, is regarded as the forerunner epidemiologist for diabetes in China and even in Asia. In 2006, study participants were followed up to assess the long‐term effects of the interventions after 20 years. As compared with the control group, those in the combined lifestyle intervention group had a 51% lower incidence of diabetes during the active intervention period and a 43% lower incidence over the 20‐year period, adjusted by age. Recently, the National Diabetes Prevalence Survey in China was carried out from 2007 to 2008. The data from that study showed that the prevalence of diabetes in Chinese adults was 9.7%, and the increased rate of diabetes prevalence in China exceeded the International Diabetes Federation estimation. Very recently, we have reported that acarbose is a viable choice for initial therapy in Chinese patients newly diagnosed with type 2 diabetes who have a lower body mass index and exaggerated postprandial glucose excursion compared with Caucasian patients. We are expecting more contributions from epidemiology to the study of diabetes.
Keywords: Diabetes, Epidemiology, Prevention
Epidemiology is the science and methodology of medical research using defined populations as basic study units. The word ‘epidemiology’ is derived from Greek epi, demos and logos; literally meaning the study (logos) of what is upon (epi) the people (demos). Epidemiology is now well recognized as the foundation of public health. Epidemiological studies can be divided into the two major areas: observation and experimentation. In the former, researchers simply observe the outcome and factors associated with the disease. Whereas, an experimental study is usually carried out in a clinical, community intervention and field trial setting. Clinical trials, as one of the classic experimental methods, have been widely used in the field of clinical medicines, including diabetes. Although epidemiology has been widely assessed in the study of infectious disease since past two centuries, its role in the study of non‐communicable chronic diseases, such as diabetes, has not been fully explored until recently.
Because of the distinguished work of diabetic epidemiologists; for example, Professor Kelly West, Professor Paul Zimmet, Professor Xiaoren Pan and so on, epidemiology has been well incorporated in the studies of diabetes, and has made a huge contribution to the development of diagnosis criteria, treatment target and clinical guidelines. Professor Kelly West (1925–1980) is widely regarded as the ‘father of diabetes epidemiology’. His landmark book, Epidemiology of Diabetes and its Vascular Lesions1, brought everything in the field into one place, and saw the ‘epidemiology of diabetes coming of age’2. Before this, there had been little systematic study of this topic3. Now the Kelly West Award from the American Diabetes Association for Outstanding Achievement in Epidemiology is given in memory of his great contribution.
The Da Qing study in China was the first milestone study in the world showing that lifestyle intervention can prevent or delay the onset of diabetes. The lead investigator of that study, Professor Xiaoren Pan, is regarded as the forerunner epidemiologist for diabetes in China and even in Asia. The Da Qing Study examined the effect of a 6‐year diet and exercise intervention in Chinese subjects with impaired glucose tolerance (IGT). A large population‐based program that consisted of 110,660 individuals screened with an oral glucose tolerance test (OGTT) to identify people with IGT was carried out in Da Qing, China, in 19864. A total of 33 participating clinics (cluster randomization) were randomized to carry out the intervention according to one of the four specified intervention protocols (diet alone, exercise alone, diet‐exercise combined or none). Altogether, 577 men and women with IGT participated in the trial, and of them, 533 participated in the measurements at the end of the 6‐year lifestyle intervention in 1992. Diet intervention alone was associated with a 35% reduction, while the exercise intervention alone showed a 39% reduction in the risk of developing type 2 diabetes. However, the combined diet and exercise group had a similar 32% reduction in the risk of developing type 2 diabetes during a 6‐year follow‐up period4. We also reported the results from a 20‐year follow up of the China Da Qing Diabetes Prevention Study in which 98% (568/577) of the participants were reassessed to establish the effect of lifestyle interventions on diabetes and other related health outcomes in people at high risk for diabetes5. In 2006, study participants were followed up to assess the long‐term effects of the interventions after 20 years. As compared with the control group, those in the combined lifestyle intervention groups had a 51% lower incidence of diabetes (hazard rate ratio 0.49, 95% confidence interval 0.33–0.73) during the active intervention period and a 43% lower incidence (hazard rate ratio 0.57; 95% confidence interval 0.41–0.81) over the 20‐year period, adjusted by age. Likewise, the average annual incidence of diabetes was 7% for intervention participants vs 11% in control participants, with 20‐year cumulative incidence of 80% in the intervention groups and 93% in the control group (Table 1)5. However, whether lifestyle intervention also leads to reduced cardiovascular disease and mortality remains unclear in this population.
Table 1. Incidence of diabetes in the active intervention (1986–1992) and entire follow‐up period (1986–2006)5.
| Diabetes | Incidence per 100 person years per year (95% CI) | Cumulative incidence, % (95% CI) | Multivariate adjusted HRR (95% CI) | ||
|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | ||
| 1986–1992 | 14.1 (11.2–17.0) | 7.9 (6.8–9.1) | 65.8 (57.7–73.9) | 42.8 (38.0–47.5) | 0.49 (0.33–0.73) |
| 1986–2006 | 11.3 (9.3–13.3) | 6.9 (5.8–7.2) | 92.8 (88.3–97.3) | 79.7 (75.6–83.8) | 0.57 (0.41–0.81) |
CI, confidence interval; HRR, hazard rate ratio.
According to the data from the International Diabetes Federation (IDF) in 2012, the prevalence of diabetes worldwide is approximately 8.3%. There are approximately 371 million diabetic patients in the world and half of them are undiagnosed. In addition, all but two of the top 10 countries with the biggest diabetic population are low‐ or middle‐income rapidly developing countries. Combined, these countries make up 75% of the total prevalence of diabetes in the world6. However, the health systems in most of these countries are not equipped to deal with the rapidly rising burden of diabetes.
Twenty years ago, we observed that the prevalence of diabetes and IGT in China was 2.5 and 3.2%, respectively, and two‐thirds (70.3%) of the cases had newly recognized diabetes7; therefore, we concluded that the prevalence of diabetes in China was increasing as a result of socioeconomic development and changed lifestyle from traditional to modernized, especially in people with lower levels of education and socioeconomic development. Today, China has been opened up to the world for more than 30 years, and had become the second largest economy in the world. The living standard and lifestyle in the Chinese population have been greatly changed in the past decades. In this situation, chronic disease, such as diabetes, hypertension and dyslipidemia, are even more common than they were 20 years ago.
Recently, the National Diabetes Prevalence Survey in China was carried out from 2007 to 2008. The data from that study showed that the prevalence of diabetes in Chinese adults was 9.7%, and the rate of increase diabetes prevalence in China especially exceeded the IDF estimation8. In our study, a multistage, stratified sampling method was used to select a nationally representative sample of persons aged 20 years or older in the general population in China and used OGTT as diabetes diagnosis8. The methodology is reliable as it uses a large, well‐constructed sample and the gold standard method for detecting diabetes, the OGTT, as recommended by the World Health Organization, which is more reasonable than just testing fasting blood glucose as other similar studies did in Western countries. Also, based on this study, both the prevalence of diabetes and prediabetes increased with age, compared with the data from 13 years ago7; the most increased prevalence was found in the middle‐aged group, 35–55 years‐of‐age (Figure 1). That means the aging population will consequently create a heavy burden of diabetes and its complications in the near future. Males, in comparison with females, contribute more to the overall prevalence, especially in the middle‐age group. The prevalence of diabetes is different in urban and rural area; diabetes still is more prevalent in urban areas than in rural areas (Figure 2)8. Compared with 10 years ago, urbanization in China has been greatly accelerated. People living in cities increased by 13%, which might drive the spread diabetes in China; the prevalence of prediabetes in China should be noted, especially in rural areas. That will be the reserve of diabetes in the near future. It is noteworthy that obesity is more common in the Chinese population than in the past9. This could be caused by economic development and lifestyle change10. The prevalence of diabetes has increased with the body mass index (BMI); and even in lean subjects, the prevalence is 7.6%8. However, the body size of Chinese patients is relatively smaller compared with that of Western people. That is probably related to the fragile β‐cell function in eastern Asians11. Briefly, by using multi‐logistic model analysis, we found that risk factors, such as sex, age, obesity and urbanization, are closely related to the onset of diabetes in China8.
Figure 1.
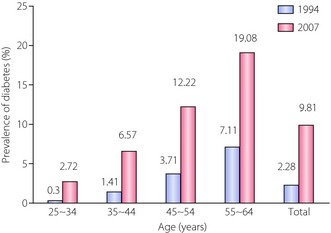
Trends in the prevalence of diabetes with different age in China. The prevalence of diabetes with different age in 1994 (blue bar) and in 2007 (pink bar) in China. Total means the total population surveyed in 1994 (blue bar) or in 2007 (pink bar).
Figure 2.

Prevalence of diabetes and absolute numbers of cases among Chinese adults aged 20 years or older, according to urban or rural residence.8 The prevalence of (a) total diabetes and (b) the estimated numbers of cases of total diabetes (among men (blue bar) and women (yellow bar) are shown, according to rural or urban residence in China. Total diabetes includes both previously diagnosed and previously undiagnosed diabetes.
Our epidemic study gained attention from the government, and both officials and physicians are now fully aware of the situation regarding diabetes in China. More and more measures are being taken to fight against the diabetes tsunami. However, risk determinants for non‐communicable diseases, such as type 2 diabetes, go to the very core of the social, cultural, economic and behavioral factors in a society. There is an urgent need to address the socioeconomic, behavioral, nutritional and public health issues that have led to type 2 diabetes, obesity and cardiovascular disease. Epidemic methodology, such as clinical and community studies of diabetes (including descriptive and/or intervention), definitely provide a unique way to help to explore and confirm these risk factors, and develop population‐based diabetes prevention strategy in the Asian population, which is believed to be racially heterogeneous. Very recently, we reported that acarbose is a viable choice for initial therapy in Chinese patients newly diagnosed with type 2 diabetes who have lower BMI and exaggerated postprandial glucose excursion compared with Caucasian patients12.
Epidemiology has come a long way since those early years. The application of epidemiology to the study of diabetes mellitus has already provided new insights into many aspects of this major public health problem including its natural history, prevalence, incidence, morbidity and mortality in diverse populations around the globe. We are expecting more contributions from epidemiology to the study of diabetes. One of the most famous poems from the ancient Chinese poet, Qu Yuan, could be used to describe the future of epidemic studies in diabetes: The way ahead is long; I see no ending, yet high and low I will search with my will unbending.
Acknowledgments
This study was supported by the China‐Japan Friendship Hospital. The authors declare no conflict of interest.
J Diabetes Invest. 2014
References
- 1.West K. Epidemiology of Diabetes and its Vascular Lesions. Elsevier, New York, 1978 [Google Scholar]
- 2.Zimmet P. Epidemiology of diabetes‐its history in the last 50 years. Br J Diabetes Vasc Dis 2002; 2: 435–439 [Google Scholar]
- 3. http://www.diapedia.org/introduction/kelly-west-1925-1980
- 4.Pan X, Li G, Yang W, et al Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care 1997; 20: 537–544 [DOI] [PubMed] [Google Scholar]
- 5.Li G, Zhang P, Wang J, et al The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20‐year follow‐up study. Lancet 2008; 371: 1783–1789 [DOI] [PubMed] [Google Scholar]
- 6. http://www.idf.org/sites/defaul/files/5E_IDFAtlasPoster_2012_EN.pdf
- 7.Pan X, Yang W, Li G, et al Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care 1997; 20: 1664–1669 [DOI] [PubMed] [Google Scholar]
- 8.Yang W, Lu J, Weng J, et al China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–1101 [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Mi J, Shan XY, et al Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007; 31: 177–188 [DOI] [PubMed] [Google Scholar]
- 10.Reynolds K, Gu D, Whelton PK, et al Prevalence and risk factors of overweight and obesity in China. Obesity (Silver Spring) 2007; 15: 10–18 [DOI] [PubMed] [Google Scholar]
- 11.Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci 2013; 1281: 64–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang W, Liu J, Shan Z, et al Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 diabetes: an open‐label, non‐inferiority randomised trial. Lancet Diabetes Endocrinol 2014; 2: 46–55 [DOI] [PubMed] [Google Scholar]


