Abstract
Aims/Introduction
To assess the feasibility, convergent validity and sensitivity of four cardiovascular risk prediction functions in Chinese diabetic patients in the primary care setting.
Materials and Methods
A cross‐sectional study of 1,140 diabetic patients was carried out to compare four cardiovascular risk functions, which were respectively developed from the Framingham heart study, the USA–People's Republic of China Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort (PRC), the United Kingdom Prospective Diabetes Study (UKPDS) and the Joint Asia Diabetes Evaluation program (JADE). Feasibility was assessed by the percentage of patients with complete data for risk prediction. Convergent validity was measured by Spearman's rank correlation, paired Wilcoxon signed‐rank sum test and Bland–Altman plots. Effect size differences between clinical risk groups were used to assess the sensitivity.
Results
Risk prediction was feasible by the Framingham, UKPDS and PRC risk functions in more than 98% patients, whereas just 74% of patients had complete data for the JADE function. The annual total coronary heart disease (CHD) risk predicted by the JADE and the UKPDS functions showed excellent agreement with no significant difference, and a correlation of 0.8048. The Framingham and the PRC functions predicted significantly lower CHD risk than those by the UKPDS and the JADE functions. The UKPDS and the Framingham functions were more sensitive in differentiating clinical risk groups.
Conclusions
The UKPDS risk engine showed good feasibility, convergent validity and sensitivity in predicting CHD risk in Chinese diabetic patients. The JADE function showed excellent agreement with the UKPDS risk engine, but it was less feasible in the primary care setting.
Keywords: Cardiovascular diseases, Diabetes complications, Risk
Introduction
The prevalence of diabetes mellitus (DM) has increased markedly in the past few decades, and the trend will continue. According to the latest estimate by the International Diabetes Federation (IDF), at least 371 million people worldwide had diabetes mellitus by 20121, and the number is expected to reach 439 million by 20302. China has the largest number of diabetic patients, with approximately a quarter of the world's diabetic population being Chinese1. The prevalence of DM in Hong Kong Special Administrative Region, one of the most developed districts in China, is significantly higher than the average in China3.
Cardiovascular diseases (CVD) are the leading causes of death in diabetic patients, and account for the largest proportion of diabetes care expenditure4. The National Cholesterol Education Program in the USA recommends that all diabetic patients should be managed as if they had coronary heart disease (CHD), and hence without the need for risk stratification5. However, observed CVD rates vary greatly among different diabetic patients6. Many international guidelines on diabetes management continue to take CVD risk stratification into account. For example, the guideline from the Canadian Diabetes Association sets the low‐density lipoprotein cholesterol treatment goal as 70 mg/dL (1.8 mmol/L) for diabetic patients with a 10‐year hard CHD risk higher than 20%, and 100 mg/dL (2.6 mmol/L) for patients with a 10‐year hard CHD risk <10%7. The American Diabetes Association recommends aspirin treatment for diabetic patients with a 10‐year CVD risk >10%8. Statin treatment is recommended by the National Institute for Health and Clinical Excellence for patients stratified to have a 10‐year CVD risk >20%9. Based on the concepts of risk stratification, risk‐specified comprehensive diabetes management programs have been developed10, showing significantly better clinical outcomes than usual care12.
Patients with diabetes mellitus require not only medication, but also behavior modification, self‐management support, and long‐term medical follow up in order to have optimal control of their diabetes while being able to continue to live in their society and maintain their quality of life. Primary care is well suited for providing this kind of diabetic care, because it is easily accessible and whole‐person oriented. Most diabetic patients are managed exclusively in primary care in developed countries12. To enable cost‐effective use of medical resources in the care of a large number of diabetic patients, the identification of high‐risk patients for additional specialist and allied health professional care is required. Furthermore, a precise calculation of the absolute cardiovascular risk is also important in informing patients about their prognosis, and to evaluate the effectiveness of therapeutic interventions. Therefore, a validated and efficient cardiovascular risk prediction function should form the base of management of diabetes mellitus in primary care.
We reviewed the literature and identified four risk functions that can potentially be applicable to Chinese diabetic patients in the primary care setting. Two of them (the Framingham15 and the United Kingdom Prospective Diabetes Study [UKPDS]16 risk functions) were developed from large high‐quality cohort studies, and were widely tested in different populations. The other two (the USA–People's Republic of China Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort [PRC]17 and the Joint Asia Diabetes Evaluation program [JADE]18 risk functions) were developed specifically in Chinese populations that included diabetic patients. Table 1 summarizes their characteristics.
Table 1. Characteristics of the four cardiovascular risk prediction functions.
| Population and risk factors | Risk functions | |||
|---|---|---|---|---|
| Framingham | PRC | UKPDS | JADE | |
| Population setting | North American | Mainland Chinese | White, Afro‐Caribbean and Asian‐Indian | Hong Kong residents |
| Cohort size | 8491 | 9903 | 4,540 | 7,067 |
| Inclusion criteria | General population, Free from CVD | General population, Free from MI and stroke | Diabetic patients free from CHD and heart failure | Diabetic patients free from CHD and heart failure |
| Baseline age | 30 –74 | 35 –59 | 25 – 65 | 46 – 67 |
| Outcomes | General CVD(CHD, cerebrovascular events, peripheral artery disease, heart failure) | Ischemic CVD (ischemic stroke and MI, coronary death) | Hard CHD (MI, coronary death, or sudden death) | Total CHD: (MI or ischemic heart disease, coronary death) |
| Observed event rates (% per year) | 1.15 | 0.37 | NR | 0.99 |
| Predicted years | 10 | 10 | 1–10 | 5 |
| Predictors (√ if include) | ||||
| Age | √ | √ | √ | |
| Age at diagnosis of DM | √ | |||
| Sex | √ | √ | √ | √ |
| Ethnicity | √ | |||
| Blood pressure | √ | √ | √ | |
| Smoking | √ | √ | √ | √ |
| DM | √ | √ | — | — |
| Duration of DM | √ | √ | ||
| TC | √ | √ | ||
| LDL‐C | ||||
| HDL‐C | √ | |||
| Non‐HDL‐C | √ | |||
| TC/HDL‐C ratio | √ | |||
| HbA1c | √ | |||
| eGFR | √ | |||
| Spot urine ACR | √ | |||
ACR, albumin: creatinine ratio; CVD, cardiovascular disease; CHD, coronary heart disease; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; Framingham, the risk function developed from the Framingham heart study; HbA1c, glycated hemoglobin; HDL‐C, high density lipid cholesterol; JADE, the risk function developed from the Joint Asia Diabetes Evaluation program; LDL‐C, low density lipid cholesterol; MI, myocardial infarction; PRC, the risk function developed from USA–People's Republic of China Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort; TC, total cholesterol; UKPDS, the risk engine developed from the United Kingdom Prospective Diabetes Study.
In 2008, an updated Framingham cardiovascular risk prediction function specified for primary care was published15. This latest Framingham function uses risk factors that are widely available in the primary care setting, and provides adjustment factors for individual CVD components, such as CHD and stroke. However, its validity and applicability has never been assessed in a Chinese diabetic population. Earlier Framingham cardiovascular risk functions tended to overestimate cardiovascular risk in Chinese populations19. Chinese researchers estimated from the data of the Chinese Multi‐provincial Cohort Study new β coefficients of the risk factors included in the Framingham Cox regression model to recalibrate the Framingham function for the Chinese population19. However, external validation in another Chinese cohort found the recalibrated Framingham function significantly overestimated the risk of CHD in both men and women17.
The UKPDS risk engines for CHD and stroke were developed in a cohort of newly diagnosed diabetic patients16. Caucasians are dominant in this cohort, and studies have shown that the UKPDS risk engines tend to overestimate the CHD risks in Chinese diabetic patients18.
To estimate cardiovascular risk for the Chinese population, researchers developed a prediction function for the 10‐year ischemic cardiovascular (ICVD) risk in a cohort of 9,903 Chinese people (the USA‐PRC Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort), and this PRC function showed good external validity in another large Chinese cohort17. The PRC risk prediction function was developed in a general population sample in mainland China, but its validity for diabetic patients is unknown.
The Asia Diabetes Foundation launched the JADE program in 2006 to provide risk stratified and evidence‐based care to diabetic patients in Asia. JADE provides a risk classification to guide clinical management of diabetic patients. This program also includes a series of 5‐year cardiovascular risk functions developed from the database of the Hong Kong Diabetes Registry. The JADE CHD risk function shows more accurate prediction than the UKPDS in a Hong Kong diabetic population in the secondary care setting18. Theoretically, the JADE CHD risk prediction function should be the most valid and accurate for Chinese diabetic patients in Hong Kong. Its feasibility and validity in the primary care setting need to be confirmed.
In the present study, we aimed at evaluating the clinimetric performance of four cardiovascular risk functions, namely the Framingham15, the PRC17, the UKPDS16 and the JADE23 risk prediction functions (Table 1) in Chinese diabetic patients in the primary care setting. The objectives were to evaluate these four risk prediction functions in terms of their: (i) feasibility in estimating the cardiovascular risk of diabetic patients; (ii) convergent validity in terms of correlation, comparison of the predicted risks and Bland–Altman plots; and (iii) sensitivity to discriminate different risk groups defined by external clinical criteria.
Materials and Methods
Participants and Design
We used data obtained from the evaluation of the Multi‐disciplinary Risk Assessment and Management Programme for patients with diabetes mellitus (RAMP‐DM) of the Hospital Authority (HA) primary care clinics in Hong Kong. The details of RAMP‐DM and the evaluation study were described in another paper24. In brief, from August 2009 to March 2011, a total of 48,823 patients from 84,996 eligible diabetic patients were enrolled in the RAMP‐DM program, in which they underwent a set of diabetic complication screenings. Based on their medical history and screening results, patients were stratified into very high‐risk, high‐risk, medium‐risk and low‐risk groups according to the JADE classification25. A total of 1,248 patients were randomly selected from the RAMP‐DM participants for the evaluation of the effectiveness of the RAMP‐DM and were the patients included in the present study. Demographic, clinical and biochemical data required by the four risk prediction functions were extracted from the computerized medical records of HA Clinical Management System. We used the cross‐sectional data collected at enrolment into the RAMP‐DM program as baseline data. Participants with known CVD were stratified into the very high‐risk group, and these 108 very high‐risk patients were excluded, as the four cardiovascular risk functions are intended for primary event prediction. A total of 1,140 participants were included in the final analysis.
The present study received ethics approval from the institutional review board of the University of Hong Kong/Hospital Authority Hong Kong East Cluster (HKEC‐2010‐093), Kowloon East and Kowloon Central Cluster (KC/KE‐10‐0210/ER‐3), Kowloon West Cluster (KW/EX/10‐317 (34–04)) and New Territories East Cluster (CRE‐2010.543).
Feasibility
Feasibility is an indicator of whether the risk prediction function is applicable to routine practice in primary care. We measured feasibility by the proportion of the study sample with complete data required for the calculation of the risks by each function. A value of 80% was set as the standard of good feasibility.
Convergent Validity
Convergent validity refers to the agreement between the results of two similar measures to support their validity in measuring what they intend to measure. We used correlation, paired Wilcoxon signed‐rank sum test of the predicted cardiovascular risk and Bland–Altman spots as measures of convergent validity.
To assess the convergent validity among the four functions, we calculated the cardiovascular risks of the participants with complete data for all four risk prediction functions (n = 837) by each prediction function published in the literature15. The PRC ICVD risk prediction tool is available in a simplified form in the published paper17, and we obtained the Cox proportional hazard ratio model from the authors for the risk calculation in our analysis.
The definitions of outcomes are not exactly the same among the four cardiovascular risk functions. The JADE function predicts the 5‐year total CHD risk (myocardial infarction or ischemic heart disease and coronary death); the original Framingham function predicts the 10‐year total CVD risk (coronary heart disease, cerebrovascular events, peripheral artery disease and heart failure), the UKPDS engine predicts the risk of ‘hard’ CHD events (fatal and non‐fatal myocardial infarction, coronary death, and sudden death), whereas the PRC risk function estimates the risk of ICVD events (coronary heart disease and ischemic stroke). To make the outcomes comparable, we converted the original cardiovascular risk of each function to the total CHD risk. The CVD risk of the Framingham function was adjusted to the total CHD risk by multiplying a factor of 0.6086, which was found to match the observed CHD risk in the original study15. The UKPDS ‘hard’ CHD risk was converted to total CHD risk by age‐category adjustment based on results from the Framingham study. Generally, the 10‐year hard CHD risk is approximately one‐third to five‐sixths of that of the 10‐year total CHD risk according to different age groups26. We carried out the conversion by applying age‐category ratios between hard CHD and total CHD to each participant. The ICVD risk of the PRC function was transformed to an equivalent total CHD risk using sex‐specific incidence ratios observed in the cohort study (incidence ratios of ICVD to total CHD were 219:66 for men and 141:39 for women, respectively)17. The total CHD risk calculated by each prediction function was further converted to an average annual risk for direct comparison.
Sensitivity
Effect size differences were used to assess the cardiovascular risk prediction functions' sensitivity to detect differences between groups of diabetic patients classified into the high‐risk, medium‐risk or low‐risk group by the JADE classification25. Patients with existing CVD complications were classified by JADE as the very high‐risk group, and they were excluded from the present study. We calculated both the original cardiovascular risks (risks directly predicted by risk functions) and the converted average annual CHD risks of patients in each group by each risk prediction function. We compared the risks between groups by Wilcoxon–Mann–Whitney tests. Effect size differences were calculated as the mean difference in cardiovascular risk between risk groups divided by the standard deviation of the risk of all the patients. Effect size differences of 0.2, 0.5 and 0.8 are regarded as the thresholds of ‘small’, ‘medium’ and ‘large’ differences, respectively28.
All data analyses were carried out using Stata 12 for Windows (StataCorp LP, College Station, TX, USA).
Results
Patient Characteristics
The characteristics of the included patients, overall and by JADE risk groups, are shown in Table 2. The mean age of the participants was 64 ± 11 years, with about equal sex distribution. A total of 84.47% patients were receiving antihypertensive treatment, and 38.18% and 10.71% patients were receiving antilipid drug treatment in the high and low risk groups, respectively. The prevalence of smoking was relatively low (10.53%), but 72.18% patients were overweight or obese (body mass index [BMI] ≥23 kg/m2) according to the World Health Organization categories for Asian populations29.
Table 2. Basic characteristics of study participants.
| Items | Total participants with data | Subjects with complete data for the four functions | ||||
|---|---|---|---|---|---|---|
| n | mean ± SD or % | Total (n = 837) | High‐risk group (n = 639) | Medium‐risk group (n = 170) | Low‐risk group (n = 28) | |
| Age (years) | 1140 | 64 ± 11 | 65 ± 11 | 65 ± 11 | 63 ± 10 | 59 ± 9 |
| Male (%) | 1140 | 48.68% | 50.3% | 48.8% | 56.5% | 46.4% |
| Current smoker (%) | 1140 | 10.53% | 11.6% | 13.8% | 4.7% | 3.6% |
| Age at diagnosis of DM (years) | 1132 | 56.59 ± 11.12 | 56.91 ± 11.09 | 57.46 ± 11.18 | 55.76 ± 10.80 | 51.44 ± 8.88 |
| Duration of DM (years) | 1132 | 7.69 ± 6.10 | 7.60 ± 5.77 | 7.75 ± 5.75 | 7.02 ± 5.84 | 7.63 ± 5.65 |
| SBP (mmHg) | 1140 | 137.88 ± 17.92 | 137.58 ± 18.10 | 138.89 ± 17.68 | 135.58 ± 18.47 | 119.75 ± 15.11 |
| TC (mmol/L) | 1129 | 5.05 ± 0.95 | 5.07 ± 0.98 | 5.12 ± 1.00 | 4.94 ± 0.91 | 4.65 ± 0.80 |
| HDL‐C (mmol/L) | 1125 | 1.23 ± 0.34 | 1.21 ± 0.33 | 1.17 ± 0.31 | 1.29 ± 0.34 | 1.56 ± 0.43 |
| HBA1c (%) | 1140 | 7.30 ± 1.21 | 7.30 ± 1.20 | 7.45 ± 1.23 | 6.80 ± 0.97 | 6.73 ± 0.64 |
| BMI (kg/m2) | 1136 | 25.20 ± 3.77 | 25.42 ± 3.82 | 26.05 ± 3.84 | 23.67 ± 2.96 | 21.75 ± 2.66 |
| BMI > 23 kg/m2 (%) | 1136 | 72.18% | 73.60% | 79.81% | 57.06% | 32.14% |
| eGFR(mL/min/1.73 m2) | 1132 | 83.22 ± 22.52 | 82.94 ± 22.84 | 80.39 ± 22.91 | 88.83 ± 20.55 | 105.46 ± 14.43 |
| Urine ACR (mg/g) | 856 | 8.86 ± 36.76 | 8.87 ± 36.98 | 11.18 ± 42.03 | 1.53 ± 3.17 | 0.76 ± 0.82 |
| Treatment of hypertension (%) | 1140 | 84.47% | 90.44% | 91.39% | 70.59% | 35.71% |
| On anti‐lipid drug treatment (%) | 1140 | 35.96% | 36.80% | 38.18% | 35.88% | 10.71% |
ACR, albumin to creatinine ratio; BMI, body mass index; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; HbA1c, glycated hemoglobin; HDL‐C, high density lipid cholesterol; SBP, systolic blood pressure; SD, standard deviation; TC, total cholesterol.
Anti‐lipid drugs included statins, bile acid sequestrants, fibrates, nicotinic acid group and omega‐3 fatty acid compounds.
A total of 837 participants had complete data for risk prediction by all four functions. Compared with the total participants, these 837 patients had a higher percentage on antihypertensive treatment (90.44% vs 84.47%, P < 0.05).
Feasibility
Risk estimation by the Framingham, PRC and UKPDS risk functions was feasible in over 98% of participants in the present study (Table 3). The JADE risk function was feasible in just 73.7% participants.
Table 3. Feasibility, comparison of predicted cardiovascular risks and effect size differences of four cardiovascular risk functions.
| Prediction function | ||||||||
|---|---|---|---|---|---|---|---|---|
| Framingham | PRC | UKPDS | JADE | |||||
| Feasibility n (%) with complete data | 1125 (98.7%) | 1126 (98.8%) | 1117 (98.0%) | 840 (73.7%) | ||||
| Original cardiovascular risk (%) (n = 837) | 37.07 ± 21.13 (10‐year CVD) | 8.85 ± 10.67 (10‐year ICVD) | 24.69 ± 17.55 (10‐year hard CHD) | 14.82 ± 8.06 (5‐year total CHD) | ||||
| Annual total CHD risk (%) (n = 837) | 2.52 ± 1.54†,‡ | 0.26 ± 0.32§,¶ | 3.09 ± 2.03** | 2.96 ± 1.61†† | ||||
| Effect size differences | vs PRC | 7.06 | vs UKPDS | 8.84 | vs JADE | 0.08 | vs Framingham | 0.29 |
| vs UKPDS | 0.37 | vs JADE | 8.43 | vs Framingham | 0.37 | vs PRC | 8.43 | |
| vs JADE | 0.29 | vs Framingham | 7.06 | vs PRC | 8.84 | vs UKPDS | 0.08 | |
†Compare Framingham with USA‐PRC Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology (PRC), P < 0.001; ‡Framingham compared with United Kingdom Prospective Diabetes Study (UKPDS), P < 0.001; §Compare PRC with UKPDS, P < 0.001; ¶Compare PRC with Joint Asia Diabetes Evaluation program (JADE), P < 0.001; **Compare UKPDS with JADE, P = 0.1345; ††JADE compared with Framingham, P < 0.001. CVD, cardiovascular disease; CHD, coronary heart disease; ICVD, ischemic cardiovascular disease; Framingham, the risk function developed from the Framingham heart study; JADE, the risk function developed from the Joint Asia Diabetes Evaluation program; PRC, the risk function developed from USA–People's Republic of China Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort; UKPDS, the risk engine developed from the United Kingdom Prospective Diabetes Study; USA‐PRC, United States of America‐Peoples' Republic of China.
Convergent Validity
Correlation
The four risk functions showed a medium to strong correlation in predicting annual total CHD risks (Table 4). The Framingham function and PRC function had the strongest correlation in predicting annual total CHD risks (r = 0.8794, P < 0.001). Both the UKPDS engine and the Framingham function showed a strong correlation with other risk functions. The correlation between the JADE function and the PRC function was medium (r = 0.6840, P < 0.001).
Table 4. Spearman's rank correlation between the annual total coronary heart disease risk predicted by the four risk functions.
| Framingham | PRC | UKPDS | JADE | |
|---|---|---|---|---|
| Framingham | – | 0.8794** | 0.8261** | 0.7628** |
| PRC | 0.8794** | – | 0.7439** | 0.6840** |
| UKPDS | 0.8261** | 0.7439** | – | 0.8048** |
| JADE | 0.7628** | 0.6840** | 0.8048** | – |
Framingham, the risk function developed from the Framingham heart study; JADE, the risk function developed from the Joint Asia Diabetes Evaluation program; PRC, the risk function developed from USA‐PRC Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort; UKPDS, the risk engine developed from the United Kingdom Prospective Diabetes Study. **P < 0.001.
Comparison of Predicted Annual Total CHD Risks
The annual total CHD risk predicted by the UKPDS risk engine and the JADE function showed no significant difference with effect size differences of 0.08 (3.09% vs 2.96%, P = 0.13). The Framingham function predicted lower annual total CHD risks than those predicted by both the JADE function and UKPDS engine (2.52% vs 2.96%, 3.09%, respectively, P < 0.001). The PRC function predicted much lower annual total CHD risk, which was only about one‐tenth of those predicted by the other functions. (Table 3).
Bland–Altman Plots
We constructed Bland–Altman plots between the Framingham function, the JADE function and the UKPDS engine to explore the distribution of the differences in predicted annual total CHD risks. The Bland–Altman plots showed that the majority of differences in annual total CHD risks predicted by these three functions fell within narrow ranges (Framingham vs JADE, −1.95% to 2.84%; UKPDS vs JADE, −2.65% to 2.39%; Framingham vs UKPDS, −2.82% to 1.67%). The distributions of differences were all heteroscedatic, with a cone‐shaped distribution indicating bigger variability among patients with higher total CHD risks (Figure 1). We did not carry out the Bland–Altman plots for PRC function compared with the other three functions, as the CHD risk predicted by the PRC function was so small, and the differences in estimated total CHD risks would be dominated by the total CHD risks predicted by the other risk functions.
Figure 1.
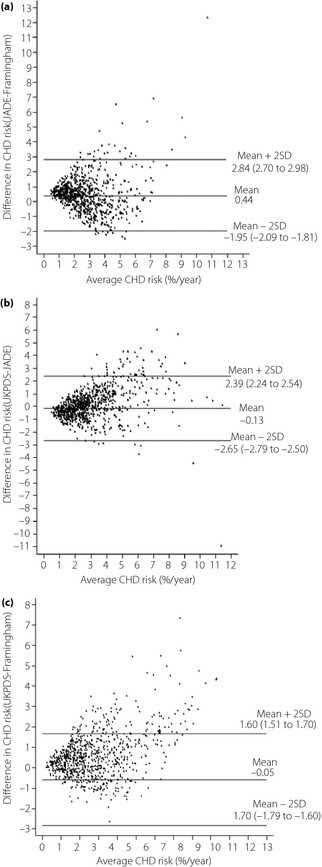
Bland–Altman plots to show the differences in predicted annual total coronary heart disease (CHD) risks between the risk functions. (a) Individual annual total CHD risks predicted by the Framingham vs the Joint Asia Diabetes Evaluation program (JADE) function. (b) Individual annual total CHD risks predicted by the United Kingdom Prospective Diabetes Study (UKPDS) vs the JADE function. (c) Individual annual total CHD risks predicted by the Framingham vs the UKPDS function.
Sensitivity
Table 5 shows the original cardiovascular risks (part a) and converted annual total CHD risks (part b) of 837 patients stratified by high‐, medium‐ and low‐risk groups by the JADE classification. The cardiovascular risks predicted by the four functions showed a consistent trend with the JADE risk group classification. All four cardiovascular risk prediction functions showed significant differences in predicted cardiovascular risks between groups. Table 5 also shows the effect size differences between risk groups for the different functions in terms of the original cardiovascular risks and the converted annual total CHD. The UKPDS engine was the most sensitive in differentiating the high‐ from the medium‐risk group. To differentiate the low‐risk patients from the medium‐ or high‐risk patients, the Framingham function was more sensitive than the other three functions with effect size differences of 0.72 and 1.10, respectively.
Table 5. Predicted risks categorized by clinical risk groups and the effect size differences between clinical risk groups.
| Predicted cardiovascular risks | Effect size differences between risk groups | |||||
|---|---|---|---|---|---|---|
| High‐risk n = 639 | Medium‐risk n = 170 | Low‐risk n = 28 | High medium‐risk | High low‐risk | Medium low‐risk | |
| (a) Predicted original cardiovascular risks | ||||||
| Framingham | 39.46 ± 21.15 | 31.52 ± 19.29† | 16.27 ± 12.10‡ | 0.38 | 1.10 | 0.72 |
| PRC | 9.73 ± 11.22 | 6.65 ± 8.49† | 1.97 ± 1.73‡ | 0.29 | 0.73 | 0.44 |
| UKPDS | 26.79 ± 17.96 | 19.17 ± 14.47† | 10.25 ± 9.37‡ | 0.43 | 0.94 | 0.51 |
| JADE | 15.64 ± 8.30 | 12.59 ± 6.62† | 9.64 ± 5.77‡ | 0.38 | 0.74 | 0.37 |
| (b) Converted annual total CHD risks | ||||||
| Framingham | 2.67 ± 1.55 | 2.16 ± 1.40† | 1.11 ± 0.89‡ | 0.33 | 1.01 | 0.68 |
| PRC | 0.28 ± 0.33 | 0.20 ± 0.25† | 0.06 ± 0.05‡ | 0.25 | 0.69 | 0.44 |
| UKPDS | 3.35 ± 2.07 | 2.39 ± 1.65† | 1.35 ± 1.04‡ | 0.47 | 0.99 | 0.51 |
| JADE | 3.13 ± 1.66 | 2.52 ± 1.32† | 1.93 ± 1.15‡ | 0.38 | 0.75 | 0.37 |
Framingham, the risk function developed from the Framingham heart study; JADE, the risk function developed from the Joint Asia Diabetes Evaluation program; PRC, the risk function developed from USA–People's Republic of China Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology cohort; UKPDS, the risk engine developed from the United Kingdom Prospective Diabetes Study. †High‐risk group compared with medium risk group, P < 0.001; ‡Medium‐risk group compared with low‐risk group, P < 0.001.
Discussion
To the best of our knowledge, this is the first study comparing the performance of four cardiovascular risk functions for Chinese diabetic patients in primary care. The significance of the present study is that it confirmed the applicability of all four cardiovascular risk functions for diabetic patients in primary care. Except for the JADE function, all could estimate the cardiovascular risk for more than 98% of the diabetic patients in primary care. Second, the differences in the annual total CHD risk predicted by JADE and UKPDS were not statistically significant, and the predicted risks showed a strong correlation with the differences falling into a small range. Although the Framingham function predicted lower CHD risk than JADE and UKPDS in Chinese diabetic patients, the UKPDS risk engine was more sensitive in discriminating high‐risk patients.
Compared with cardiovascular risk functions developed for general populations (the Framingham function and the PRC function), the diabetes‐specific risk functions (the JADE function and UKPDS function) tend to include more diabetes‐related risk factors, such as the duration of diabetes, and the level of glycated hemoglobin to enhance the validity and sensitivity of prediction. The inclusion of extra risk factors did not affect the feasibility of the UKPDS risk engine, and the present study confirmed that it had better sensititivity than the other three functions to discriminate between high‐ and medium‐risk patients. In contrast, the inclusion of urine albumin creatinine ratio and estimated glomerular filtration rate made the JADE function less feasible without any demonstrable increase in sensitivity.
Both the UKPDS engine and the JADE function are specific to diabetic patients. The present study showed excellent convergent validity between them, with no significant difference in the estimated annual total CHD risks. Although the mean CHD risk predicted by the UKPDS engine was slightly higher than that of the JADE function, the Bland–Altman plots showed the differences were within a narrow range, especially for patients with lower than 3% annual CHD risk. Nevertheless, a study by Yang et al.18 in a cohort of Hong Kong Chinese diabetic patients found that the UKPDS engine overestimated the risk of hard CHD, whereas the JADE function showed a good fit with the observed total CHD events. The research participants of Yang's study were diabetic patients from the public specialist outpatient clinic in one hospital, whereas our participants were a random sample from public primary care clinics in different regions of Hong Kong. The discrepancy in participant characteristics and different cardiovascular outcomes might be explanations for the inconsistent findings with the UKPDS engine between the present study and Yang's study.
The present study found that the annual total CHD risk predicted by the 2008 Framingham function was significantly lower than that predicted by the JADE function and UKPDS engine in Chinese diabetic patients. A cohort study in Taiwan also showed that the 2008 Framingham function overestimated the cardiovascular risk compared with the risk prediction model developed from Taiwanese data21. The 2008 Framingham function might underestimate the cardiovascular risk of diabetic patients, as it was developed from a general population with just 7% diabetic patients. Other studies have also found that the Framingham functions tended to underestimate the CHD risk for diabetic patients compared with observed events30 or the risk predicted by the UKPDS engines33. Current evidence shows that the CHD risk of patients with diabetes is two‐ to fourfold higher than that of non‐diabetic patients35. Although the 2008 Framingham function includes diabetes as a risk factor, the adjustment is much less than two‐ to fourfold. A small number of participants in the present study were classified as the low‐risk group (n = 28), as most patients were elderly with reduced estimated glomerular filtration rate and coexisting cardiovascular risk factors. The small number of low‐risk participants was unlikely to be the reason for the underestimation of cardiovascular risk by the Framingham function, because there was no obvious trend in the descrepancies between the risks predicted by the Framingham function and other functions among the different risk groups (Table 5).
The PCR function predicted a much lower CHD risk than the other three risk functions, including the JADE function. The discrepancy could not be explained by differences in ethnicity or case disparities. Another study also raised doubts about the accuracy of the low cardiovascular risk predicted by the PRC function. It was found that more than 80% of 461,157 study participants in mainland China had a low (<0.5% per year) risk for ICVD and, in a group of 19,830 middle‐aged diabetic patients, just 5.5% were stratified into the high‐risk group (≥1.2% per year)37. We were aware that a point‐based, simplified evaluation chart could reduce the discriminative ability, so we sought the Cox proportional hazard ratio function of the PRC function from the authors, but the PRC function still showed poorer sensitivity to discriminate between risk groups.
There were several limitations in the present study. First, we included patients whose age fell beyond the age ranges of the original studies of the four risk functions, which might affect the validity of the prediction. Second, we converted the hard CHD risk predicted by the UKPDS risk engine and ICVD risk predicted by the PRC function to an annual total CHD risk for direct comparison, which could affect the results on risk comparison. Third, the participants in the present study were selected from a multidisciplinary management program (RAMP‐DM), which included comprehensive risk factors and complication assessment of all enrolled patients, which might have overestimated the feasibility of the risk prediction fucntions. For diabetic patients under usual primary care, there could be more missing data for some of the variables, such as urine albumin creatinine ratio, which might not be routinely measured. The generalizability could improve with an international trend to implement comprehensive diabtetes management strategies, including cardiovascular and renal risk assessment and stratification8.
In conclusion, All four cardiovascular risk functions (the Framingham, PRC, UKPDS and JADE) are valid and sensitive for Chinese diabetic patients in primary care. There were significant differences in the absolute risk prediction between some functions. The present study suggested that the UKPDS risk engine might be the most useful cardiovascular risk prediction tool for Chinese diabetic patients in primary care, taking into account feasibility, convergent validity and sensitivity. The Framingham and PRC function might underestimate the cardiovascular risks in Chinese diabetic patients. The present study cannot conclude which risk function is the most accurate for Chinese diabetic patients, which will need to be evaluated by a longitudinal study on the development of cardiovascular events in a cohort of Chinese diabetic patients over at least 5 years.
Acknowledgements
The present study was funded by the Health and Health Services Research Fund, Food and Health Bureau, HKSAR commissioned Research on Enhancing Primary Care Study (Ref.no EPC‐HKU‐1A). The authors acknowledge the contributions of the Multi‐disciplinary Risk Assessment and Management Programme teams at the Hospital Authority head office, all involved representatives and clinical staff. We thank Mr Yuk Fai Wan in the Department of Family Medicine and Primary Care for his help in database building. We also express our gratitude to the researchers developing the PRC function, Professor Yangfeng Wu and Professor Xian Li, for providing us unpublished information. There is no conflict of interest to declare.
J Diabetes Invest 2014; 5: 606–614
References
- 1.International Diabetes Federation . Diabetes Atlas, 5rd ednhttp://www.idf.org/diabetesatlas/2012 Available from: http://www.idf.org/diabetesatlas/
- 2.Shaw J, Sicree R, Zimmet P. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4–14 [DOI] [PubMed] [Google Scholar]
- 3.Wong KC, Wang Z. Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract 2006; 73: 126–134 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association . Standards of medical care in diabetes 2012. Diabetes Care 2012; 35(Suppl 1): S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults . Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001; 285: 2486–2497 [DOI] [PubMed] [Google Scholar]
- 6.Chamnan P, Simmons RK, Sharp SJ, et al Cardiovascular risk assessment scores for people with diabetes: a systematic review. Diabetologia 2009; 52: 2001–2014 (English). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canadian Diabetes Association . 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2008; 32(Suppl 1): S1–S201 [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association . Standards of medical care in diabetes 2013. Diabetes Care 2013; 36(Suppl 1): S11–S66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence . Type 2 Diabetes National Clinical Guideline for Management in Primary and Secondary Care (Update). Royal College of Physicians, London, UK, 2008 [PubMed] [Google Scholar]
- 10.Clark CM, Snyder JW, Meek RL, et al A systematic approach to risk stratification and intervention within a managed care environment improves diabetes outcomes and patient satisfaction. Diabetes Care 2001; 24: 1079–1086 [DOI] [PubMed] [Google Scholar]
- 11.Ko GT, So WY, Tong PC, et al From design to implementation–the Joint Asia Diabetes Evaluation (JADE) program: a descriptive report of an electronic web‐based diabetes management program. BMC Med Inform Decis Mak 2010; 10: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Task Force on Conceptual Model and Preventive Protocols Working Group on Primary Care . Food and Health Bureau. Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings, Hong Kong, 2010 [Google Scholar]
- 13.Khunti K, Ganguli S. Who looks after people with diabetes: primary or secondary care? J R Soc Med 2000; 93: 183–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Care WP. Chronic illness management: what is the role of primary care? Ann Intern Med 2003; 138: 256–261 [DOI] [PubMed] [Google Scholar]
- 15.D'Agostino RB Sr, Vasan RS, Pencina MJ, et al General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008; 117: 743–753 [DOI] [PubMed] [Google Scholar]
- 16.Stevens RJ, Kothari V, Adler AI, et al The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clin Sci (Lond) 2001; 101: 671–679 [PubMed] [Google Scholar]
- 17.Wu YF, Liu XQ, Li X, et al Estimation of 10‐year risk of fatal and nonfatal ischemic cardiovascular diseases in Chinese adults. Circulation 2006; 114: 2217–2225 [DOI] [PubMed] [Google Scholar]
- 18.Yang X, So WY, Kong AP, et al klDevelopment and validation of a total coronary heart disease risk score in type 2 diabetes mellitus. Am J Cardiol 2008; 101: 596–601 [DOI] [PubMed] [Google Scholar]
- 19.Liu J, Hong Y, D'Agostino RB Sr, et al Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi‐Provincial Cohort Study. JAMA 2004; 291: 2591–2599 [DOI] [PubMed] [Google Scholar]
- 20.Barzi F, Patel A, Gu D, et al Cardiovascular risk prediction tools for populations in Asia. J Epidemiol Community Health 2007; 61: 115–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chien KL, Hsu HC, Su TC, et al Constructing a point‐based prediction model for the risk of coronary artery disease in a Chinese community: a report from a cohort study in Taiwan. Int J Cardiol 2012; 157: 263–268 [DOI] [PubMed] [Google Scholar]
- 22.Kothari V, Stevens RJ, Adler AI, et al UKPDS 60 risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke 2002; 33: 1776–1781 [DOI] [PubMed] [Google Scholar]
- 23.Yang X, So WY, Kong AP, et al Development and validation of stroke risk equation for Hong Kong Chinese patients with type 2 diabetes: the Hong Kong Diabetes Registry. Diabetes Care 2007; 30: 65–70 [DOI] [PubMed] [Google Scholar]
- 24.Fung CS, Chin WY, Dai DS, et al Evaluation of the quality of care of a multi‐disciplinary risk factor assessment and management programme (RAMP) for diabetic patients. BMC Fam Pract 2012; 13: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan J, So W, Ko G, et al The Joint Asia Diabetes Evaluation (JADE) Program: a web‐based program to translate evidence to clinical practice in Type 2 diabetes. Diabet Med 2009; 26: 693–699 [DOI] [PubMed] [Google Scholar]
- 26.Wilson PWF, D'Agostino RB, Levy D, et al Prediction of coronary heart disease using risk factor categories. Circulation 1998; 97: 1837–1847 (English). [DOI] [PubMed] [Google Scholar]
- 27.de Visser CL, Bilo HJG, Thomsen TF, et al Prediction of coronary heart disease: a comparison between the Copenhagen risk score and the Framingham risk score applied to a Dutch population. J Intern Med 2003; 253: 553–562 (English). [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum Associaties, Inc, New Jersey, 1988 [Google Scholar]
- 29.WHO Expert Consultation . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157. [DOI] [PubMed] [Google Scholar]
- 30.Guzder RN, Gatling W, Mullee MA, et al Prognostic value of the Framingham cardiovascular risk equation and the UKPDS risk engine for coronary heart disease in newly diagnosed Type 2 diabetes: results from a United Kingdom study. Diabet Med 2005; 22: 554–562 [DOI] [PubMed] [Google Scholar]
- 31.McEwan P, Williams JE, Griffiths JD, et al Evaluating the performance of the Framingham risk equations in a population with diabetes. Diabet Med 2004; 21: 318–323 [DOI] [PubMed] [Google Scholar]
- 32.Yeo W, Yeo KR. Predicting CHD risk in patients with diabetes mellitus. Diabet Med 2001; 18: 341–344 [DOI] [PubMed] [Google Scholar]
- 33.Song SH, Brown PM. Coronary heart disease risk assessment in diabetes mellitus: comparison of UKPDS risk engine with Framingham risk assessment function and its clinical implications. Diabet Med 2004; 21: 238–245 [DOI] [PubMed] [Google Scholar]
- 34.Davis WA, Colagiuri S, Davis TM. Comparison of the Framingham and United Kingdom Prospective Diabetes Study cardiovascular risk equations in Australian patients with type 2 diabetes from the Fremantle Diabetes Study. Med J Aust 2009; 190: 180. [DOI] [PubMed] [Google Scholar]
- 35.Koskinen P, Manttari M, Manninen V, et al Coronary heart disease incidence in NIDDM patients in the Helsinki Heart Study. Diabetes Care 1992; 15: 820–825 [DOI] [PubMed] [Google Scholar]
- 36.UK Prospective Diabetes Study Group . Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317: 703–713 [PMC free article] [PubMed] [Google Scholar]
- 37.Wu HY, Wu LX, Zen QA, et al Do currently recommended risk prediction tools help primary prevention of cardiovascular disease in Chinese population? Int J Cardiol 2011; 146: 299–301 (English). [DOI] [PubMed] [Google Scholar]
- 38.International Diabetes Federation . Global Guideline for Type 2 Diabetes: recommendations for standard, comprehensive, and minimal care. Diabet Med 2006; 23: 579–593 [DOI] [PubMed] [Google Scholar]


