Abstract
There have been no comprehensive reviews of the relation of breakfast cereal consumption to nutrition and health. This systematic review of all articles on breakfast cereals to October 2013 in the Scopus and Medline databases identified 232 articles with outcomes related to nutrient intake, weight, diabetes, cardiovascular disease, hypertension, digestive health, dental and mental health, and cognition. Sufficient evidence was available to develop 21 summary evidence statements, ranked from A (can be trusted to guide practice) to D (weak and must be applied with caution). Breakfast cereal consumption is associated with diets higher in vitamins and minerals and lower in fat (grade B) but is not associated with increased intakes of total energy or sodium (grade C) or risk of dental caries (grade B). Most studies on the nutritional impact are cross-sectional, with very few intervention studies, so breakfast cereal consumption may be a marker of an overall healthy lifestyle. Oat-, barley-, or psyllium-based cereals can help lower cholesterol concentrations (grade A), and high-fiber, wheat-based cereals can improve bowel function (grade A). Regular breakfast cereal consumption is associated with a lower body mass index and less risk of being overweight or obese (grade B). Presweetened breakfast cereals do not increase the risk of overweight and obesity in children (grade C). Whole-grain or high-fiber breakfast cereals are associated with a lower risk of diabetes (grade B) and cardiovascular disease (grade C). There is emerging evidence of associations with feelings of greater well-being and a lower risk of hypertension (grade D), but more research is required.
Introduction
The role of breakfast cereals in a balanced diet has been recognized for many years (1–3). Dietary guidelines note that the high nutrient density of breakfast cereals (especially those that are whole grain or high in cereal fiber) makes them an important source of key nutrients (4). In addition to providing an important source of vitamins and minerals, breakfast cereals are also potentially important sources of antioxidants (5–7) and phytoestrogens (8) and are 1 of the most important sources of whole grains (9). However, there have been no comprehensive reviews of their health benefits and there is some uncertainty about their nutritional merits because of concerns about the amounts of salt, sugar, or saturated fat in some products (10).
The Australian Breakfast Cereal Manufacturers Forum commissioned this systematic review to summarize the evidence relating the consumption of breakfast cereals and a range of health outcomes. The review covers the breakfast cereal category generally and not individual products or cereal components or properties such as whole grains, dietary fiber, or glycemic index (GI)5.
Methods
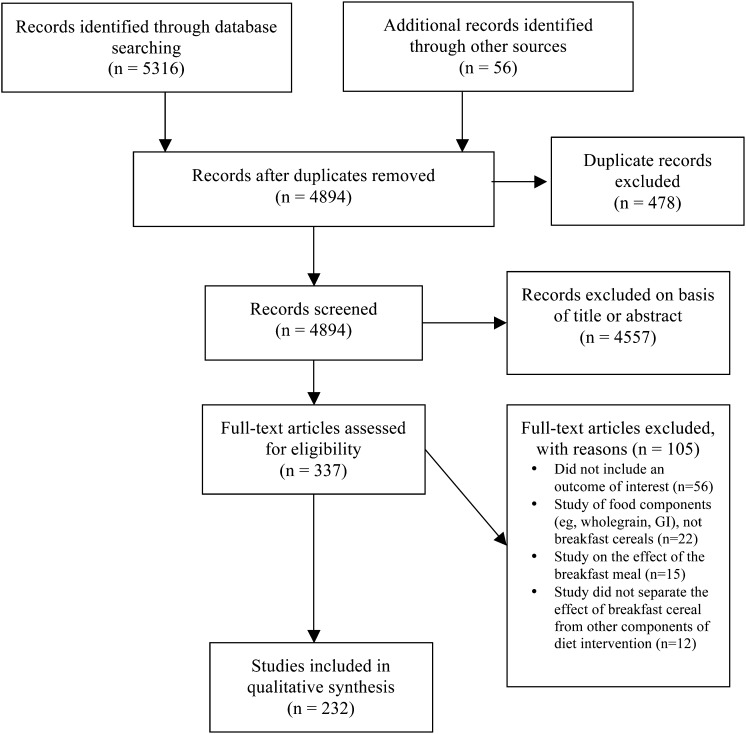
For this review, “breakfast cereal” was defined to include ready-to-eat breakfast cereal (RTEC), oats/porridge, and muesli. Exclusions were breakfast bars, muesli bars, liquid breakfast products, milk drinks, and yogurt products. The author conducted a systematic review of the published scientific literature from all dates until October 2013 in the Scopus and Medline databases by using the search terms listed in Supplemental Table 1. Inclusion criteria were as follows: English-language publications only, studies in adult and children and males and females of all ages and health conditions, and all study types including reviews. Exclusion criteria were as follows: animal studies or articles primarily focused on the breakfast meal, dietary fiber, whole grains, cereal fiber, or other components of cereal foods in general. Relevant studies cited in review articles or those identified in the search were also considered. Figure 1 shows the study selection flowchart. From the 5316 articles originally identified in the database search, a total of 232 were used in the qualitative synthesis presented in the Results section.
FIGURE 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. GI, glycemic index.
Quantitative data were extracted from the relevant articles, including the study methods, populations, and outcomes of significance to the review. Study quality was examined by using the methods of the American Dietetic Association Evidence Analysis Manual, and scored as positive, neutral, or negative (11).
Body of evidence tables were developed to present the main findings with the use of the methodology and format recommended by the Australian National Health and Medical Research Council (12, 13). These statements summarize the scientific findings in a standardized manner, with a grading from A (body of evidence can be trusted to guide practice), B (can be trusted to guide practice in most situations), C (provides some support but care should be taken in its application), to D (body of evidence is weak and must be applied with caution) (14).
Results
Contribution of breakfast cereals to healthy diets
Contribution to energy and nutrient intakes.
Reviews.
There have been 3 major reviews of the contributions of breakfast cereals to nutrient intake and overall good health: 2 general narrative reviews (15, 16) and 1 systematic review of studies in children and adolescents (17). One other review of the breakfast meal also summarized some of the studies that reported the effects of RTEC consumption (18).
These reviews are largely in agreement that, compared with those who consume lower amounts of breakfast cereal or nonconsumers, regular breakfast cereal consumers have
• higher intakes of carbohydrate;
• higher intakes of total sugars;
• lower intakes of fat;
• lower cholesterol intakes;
• enhanced micronutrient intakes;
• higher milk intakes;
• greater likelihood of meeting micronutrient recommended intakes;
• improved nutritional status; and
• lower serum cholesterol concentrations.
Intervention studies.
Table 1 summarizes findings from 11 intervention studies that incorporated additional breakfast cereal into subjects’ diets and shows the nutrients that were increased, decreased, or remained unchanged in the subjects’ total daily intakes. Those studies generally show an increase in vitamin and mineral intakes, and decreases in fat, but no consistent effect on daily energy, protein, or carbohydrate intakes.
TABLE 1.
Intervention trials with added breakfast cereal consumption: impact on daily nutrient intake1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Nutrients increased | Nutrients decreased | Nutrients unchanged |
| Hambidge et al. (263) | Positive | 96 children aged 33–90 mo; US | Randomized double-blind controlled 9-mo trial. Participants were provided with Kellogg’s cereal—fortified or nonfortified. | Zinc-fortified breakfast cereal to provide 25% of RDA. Calculated intake average, 2.57 mg Zn/d from cereal. | Zinc | — | — |
| Kirk et al. (77)2 | Positive | 59 students, mean age 23 y; Scotland | Randomized controlled trial for 12 wk. Intervention group instructed to consume 2 servings (60 g) RTEC/d with semi-skimmed milk. Controls given no dietary advice. | 3 Kellogg’s cereals provided: Corn Flakes, Rice Krispies, Special K. All fortified with B1, B2, B3, B6, B12, folate, vitamin D, and iron. | Thiamin | — | Energy |
| Riboflavin | |||||||
| Niacin | |||||||
| Pyridoxine | |||||||
| Folate | |||||||
| Vitamin D | |||||||
| Calcium | |||||||
| Iron | |||||||
| Kleemola et al. (91)2 | Positive | 209 adults aged 29–71 y; Finland | Randomized crossover trial for 6 wk. Intervention group instructed to consume 60 g (women) or 80 g (men) RTEC with skim milk, fat-free yogurt, and juice at breakfast. Controls followed normal eating patterns. | 2 Kellogg’s cereals provided: Corn Flakes and Rice Krispies | %E from CHO | Energy | %E from protein |
| %E from fat | Fiber | ||||||
| Kirk et al. (107) | Positive | 22 overweight adults (mean BMI, in kg/m2: 31); UK | Within-person pre-post study design; 2 wk replacing 1 meal with breakfast cereal, followed by 4 wk ad libitum high-CHO diet. | Stage 1: 45 g RTEC with skim milk | %E from protein | Energy | Sugars |
| Stage 2: encouraged to use RTEC as a snack | %E from CHO | %E from fat | Fiber | ||||
| Abrams et al. (264) | Positive | 27 children aged 6–9 y; US | Randomized double-blind controlled 14-d trial. Participants provided with General Mills cereal—fortified or nonfortified. | 2 servings per day of calcium-fortified breakfast cereal (156 mg/serving) | Calcium | Iron | |
| Mattes (87) | Positive | 82 overweight men and women (mean BMI: 29; mean age 42 y); US | Randomized, parallel, controlled trial with subjects eating RTEC with skim milk and fruit for breakfast and either lunch or dinner meal | Intervention groups: either Special K or a variety of RTECs to select from | Energy | ||
| Control: normal diet | Protein | ||||||
| Fat | |||||||
| CHO | |||||||
| Ortega et al. (105) | Positive | 67 overweight women (mean BMI: 28.4); Spain | Randomized controlled trial on 20% hypocaloric diet with 2 diets with increased consumption of C or V | Diet C: breakfast cereals and cereal bars at least 3×/d, in addition to normal cereal foods | Vitamin B-6 | Energy | CHO |
| Diet V: vegetables at least 3×/d in addition to normal cereal foods | Folate | Protein | |||||
| Fat | |||||||
| Ortega et al. (74) | Positive | 57 women aged 20–35 y; Spain | Randomized controlled trial on 20% hypocaloric diet with 2 diets with increased consumption of C or V | Diet C: breakfast cereals and cereal bars at least 3×/d, in addition to normal cereal foods | Thiamin | — | — |
| Diet V: vegetables at least 3×/d in addition to normal cereal foods | |||||||
| Lightowler and Henry (104) | Positive | 41 overweight and obese men and women; UK | 6-wk randomized trial with subjects required to consume one of two 45-g equicaloric RTEC choices (SC or VC) with semi-skimmed milk at breakfast and lunch, without control of other meals. | 2 choices of RTECs compared: | — | Energy (SC group) | Energy (VC group) |
| SC: Fitnesse (1.7 g fiber/ serving) | Fat | Protein | |||||
| VC: Shredded Wheat (5.4 g fiber), or Berry Shredded Wheat (5.0 g fiber) (Cereal Partners UK) | Fiber (VC only) | CHO | |||||
| 3-d food diaries used to record diet intake | Fiber (SC) | ||||||
| Matthews et al. (106) | Positive | 70 overweight men and women who were self-reported evening snackers; UK | Randomized, controlled 6-wk intervention study. The intervention group was given a selection of breakfast cereals to consume instead of their normal evening snack. Control group maintained normal habits. | 9 different varieties of Kellogg’s RTECs were provided with external packaging removed. Participants were advised to try each at least once. | g CHO | Energy | |
| %E from CHO | |||||||
| g fat | |||||||
| %E from fat | |||||||
| g protein | |||||||
| %E from protein |
B1, vitamin B-1 (thiamin); B2, vitamin B-2 (riboflavin); B3, vitamin B-3 (niacin); B6, vitamin B-6, pyridoxine; B12, vitamin B-12 (cyanocobalamin); C, cereals; CHO, carbohydrate; RDA, recommended dietary allowance; RTEC, ready-to-eat breakfast cereal; SC, single choice; V, vegetables; VC, variable choice; %E, percentage of energy.
Study included in 1 of the review articles.
Cross-sectional studies.
There are 51 studies that reported on the nutritional impact of regular breakfast cereal consumption in those who eat breakfast: that is, comparing consumption of a breakfast cereal–based breakfast vs. other breakfast types (see Supplemental Tables 2 and 3). Of these studies, 30 were in children (19–48) and 21 were in adults (31, 49–68). The results from the cross-sectional studies and the randomized controlled trials (RCTs) showed very consistent results.
Children and adolescents who consume breakfast cereals regularly have daily diets that are
• higher in percentage of energy (%E) from carbohydrate, total sugars, dietary fiber, vitamins A and D, thiamin, riboflavin, niacin, pyridoxine, folate, calcium, iron, magnesium, and zinc;
• no different in total energy intake, %E from protein, or sodium; and
• lower in %E from fat.
Almost all of the studies are for RTEC only. Many of the micronutrient differences are related to the fortification profile of the breakfast cereals, but the increased milk intake would contribute significantly to the higher daily calcium and riboflavin intakes. In both Australia and the United States, approximately one-quarter of all milk consumed by children and adolescents is added to breakfast cereal (69, 70).
Other findings from the studies show that children and adolescents who eat breakfast cereal regularly
• are less likely to have vitamin and mineral intakes below the recommended daily requirements, especially for calcium (21, 22, 24, 25, 27, 33, 37, 38, 41, 44, 46, 48);
• have better diets overall, measured by the Healthy Eating Index score (48);
• have lower daily cholesterol intakes (20); and
• have better nutritional status (assessed by blood measures), especially for the vitamins thiamin, riboflavin, and pyridoxine (32) and iron (34).
In food-insecure children in the United States, the percentage whose daily nutrient intake was below the Estimated Average Requirement was higher in those who did not consume breakfast cereal for several key nutrient, including 62.7% vs. 39.9% for calcium, 26.3% vs. 19.4% for magnesium, 33.4% vs 8.1% for vitamin A, 15.4% vs. 3.2% for zinc, and 9.4% vs. 0.1% for folate, respectively (48). The difference in total milk consumption (345 vs. 142 g for cereal consumers vs. nonconsumers) was significantly greater than the difference in food-secure children (324 vs. 161g; P < 0.05)—that is, RTEC was even more important in food-insecure children in improving milk intakes. Comparing Healthy Eating Index scores, both food-secure and food-insecure children achieved better scores when they consumed breakfast cereals, but the improvement in total grain intake was significantly greater for food-insecure children (46).
In the 1995 Australian National Nutrition Survey, breakfast cereals as consumed with milk and sugar contributed only 6–9% of total energy intakes of children and adolescents but provided >25% of the Recommended Dietary Intake (RDI) for thiamin, riboflavin, and iron (for boys) and >10% of the RDI for niacin, folate (for boys), calcium, iron (for girls), and magnesium (37). In the 2007 Australian National Children’s Nutrition and Activity Survey, RTEC consumption provided 10% of total daily fiber intake (47).
Adults who consume breakfast cereals regularly have daily diets that are
• higher in %E from carbohydrate, total sugars, dietary fiber, vitamins A and D, thiamin, riboflavin, niacin, pyridoxine, folate, calcium, iron, magnesium, and zinc;
• no different in total energy intake, sodium, or %E from protein; and
• lower in %E from fat.
The latest national survey from the United Kingdom found that whereas breakfast cereals contribute 3–5% of the daily energy intake and 2–5% of dietary fiber intake, they provide only 1% of fat and 1–2% of sodium in the total diet (3). Similarly, breakfast cereals contribute only 2.1–2.6% of total sodium intake in adults in the United States (71) and <2.5% in Australia (72).
Other findings show that adults who eat breakfast cereal regularly
• are less likely to have vitamin and mineral intakes below the recommended daily requirements, especially for thiamin, riboflavin, niacin, folate, vitamin C, calcium, magnesium, iron, zinc, and fiber (54, 56, 57, 60–63, 66–68);
• have better diets overall, measured by the Healthy Eating Index (63); and
• have better nutritional status (assessed by blood measures), especially for the vitamins thiamin, riboflavin, and folate (31, 60, 73, 74).
Those consuming whole-grain and high-fiber breakfast cereals, compared with those consuming other breakfast cereals, had significantly higher daily intakes of %E from protein, fiber, niacin, folate, calcium, and zinc (65); however, whole-grain cereal intake in particular is likely to be a marker of a healthy lifestyle and therefore potentially subject to residual confounding.
Benefits of a breakfast cereal meal pattern.
There are clearly nutritional benefits from including breakfast cereals in a breakfast meal. A recently proposed Breakfast Quality Index has the inclusion of breakfast cereals as a key factor to improve the overall breakfast meal score (75). Findings from the cross-sectional studies show that
• eating breakfast cereal facilitates greater milk consumption in children (39, 48, 76) and in adults (51, 54, 56, 62, 63, 65, 77);
• those who eat breakfast cereal regularly have higher whole-grain consumption per day, both in children (42, 46, 48, 78) and in adults (63, 79); and
• children and adults eating RTEC also eat a greater range of different foods at the breakfast meal (28, 63).
Comparison of breakfast cereal eaters with breakfast skippers.
Eleven cross-sectional studies (summarized in Supplemental Table 4) compared the daily nutrient intakes of people eating a cereal-based breakfast with breakfast skippers (20, 41, 44, 46, 50, 53, 54, 60, 63, 64, 67). Those results mostly supported the comparisons of consumers of breakfasts with or without the inclusion of breakfast cereals. Consistently, the daily diets of breakfast cereal eaters (compared with breakfast skippers) are
• higher in energy and %E from carbohydrate, dietary fiber, and all vitamins and minerals, and
• lower in %E from fat.
The results from comparisons of %E from protein, total sugars, and sodium are more varied and there are no clear trends. The consistent finding of higher milk intakes in those who consume breakfast cereals is part of the reason that studies have shown higher riboflavin status in those who consume breakfast cereals (80).
Presweetened vs. minimally presweetened cereals.
Analysis of data from the 2007 Australian National Children’s Survey of children and adolescents aged 2–16 y compared the intakes of those consuming presweetened breakfast cereals with ≥15% total sugars or minimally presweetened (PS) breakfast cereals (non-PS) (81) and found that total daily energy and nutrient intakes were not significantly different, including intake of total sugars (PS vs. non-PS consumers: 121 vs. 118 g/d). Another analysis of the same survey data noted that RTECs provided 34% of the total sugars consumed at breakfast but only 7% of the total sugars consumed over the whole day (44).
A recent study of 312 Australian breakfast cereals showed that there was no relation between the total sugar content and the energy density of breakfast cereals, both ready-to-eat and other breakfast types (82), which supports the finding of no difference in total daily energy intake regardless of the amount of sugar in breakfast cereals themselves.
These results are consistent with several studies in American children. A study in 5- to 12-y-old children found that that compared with children consuming RTEC with >25% total sugars, those consuming nonsweetened cereals (<25% total sugars) had higher daily intakes of protein, carbohydrate, fiber, folate, vitamin A, calcium, and magnesium, but there were no significant differences in intakes of total energy, fat, total sugars, thiamin, riboflavin, niacin, ascorbic acid, iron, zinc, or sodium (19). Another cross-sectional study in U.S. children and adolescents reported that children aged 6–11 y who consumed PS breakfast cereals had higher total added sugars in their diet (93 vs. 83 g/d), but that in adolescents aged 12–17 y there was no difference in daily total sugar consumption between consumers and nonconsumers of PS breakfast cereals (76).
In a more recent study in PS vs. non-PS breakfast cereal consumers aged 4–13 y, daily energy and total sugar intakes were higher in those consuming PS cereals (defined as those with >6 g total sugars per serving), but there were no differences found for adolescents aged 14–18 y. Daily sodium intakes were lower in those consuming PS cereals at all ages. There were no differences in BMI or waist circumference between any age group (43).
In 1 experimental study (83), children aged 5–12 y were offered a choice of 1 of 3 high-sugar breakfast cereals (with 11–12 g of total sugars per serving) or low-sugar cereals (1–4 g total sugars per serving) plus free access to added sugar, milk, fruit, and juice. The study found that
• children reported greater liking of the high-sugar cereals and consumed almost twice the amount per eating occasion compared with those served the low-sugar cereals (61.3 vs. 34.6 g);
• children offered low-sugar cereals added more table sugar than those eating high-sugar cereals, and the total sugar content (from cereal and added sugar) was almost twice as high as with the high-sugar cereals (24.4 vs. 12.5 g; P < 0.001);
• there was no difference in the amount of milk consumed with the 2 types of cereals, nor the total energy consumed at the breakfast meal; and
• children in the low-sugar group were more likely to put fresh fruit on their breakfast cereal compared with the high-sugar cereal condition (54% vs. 8%; P = 0.05).
Table 2 provides body of evidence summaries of the main findings from the studies on the contribution of breakfast cereals to dietary intake.
TABLE 2.
Body of evidence summaries related to breakfast cereals and dietary intake
| Evidence statement and components | Grade | Rating | Notes |
| Regular consumption of breakfast cereals is associated with diets that are lower in fat | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Good | 6 Level II studies: RCTs1 (all positive quality) | |
| 45 Level IV studies: 4 reviews and 41 cross-sectional studies (all positive quality) | |||
| Consistency | Good | All reviews and 37/41 studies reported lower fat content | |
| Clinical impact | Good | %E from fat reduced by 3–4% | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of breakfast cereals is associated with diets that are higher in vitamins and minerals for adults, adolescents, and children | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Good | 5 Level II studies: RCTs (all positive quality) | |
| 49 Level IV studies: 4 reviews and 45 cross-sectional studies (all positive quality) | |||
| Consistency | Good | Of a total of 452 measurements, 85% were increased, none decreased, and 15% were unchanged. | |
| Clinical impact | Satisfactory | All significant, P < 0.05 | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of breakfast cereals is associated with a greater likelihood of meeting recommended nutrient intakes | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Poor | 20 Level IV studies (cross-sectional studies) (all positive quality) | |
| Consistency | Excellent | All cross-sectional studies report consistent effect | |
| Clinical impact | Satisfactory | All significant, P < 0.05 | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations where breakfast cereals are consumed regularly | |
| Consumption of breakfast cereals is associated with higher daily milk intake | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Poor | 10 Level IV studies (cross-sectional studies) (all positive quality) | |
| Consistency | Excellent | All cross-sectional studies report consistent effect | |
| Clinical impact | Good | 25–140% increase in milk intake | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of presweetened breakfast cereals does not increase the total daily energy intake in children’s diets | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Satisfactory | 1 Level II studies (RCTs) (positive quality) | |
| 4 Level IV studies (cross-sectional studies) (all positive quality) | |||
| Consistency | Good | 3 of 4 cross-sectional studies and the 1 RCT reported no difference in energy consumed; 1 cross-sectional study reported a higher energy intake in consumers of presweetened cereals aged 4–13 y but not in adolescents aged 14–18 y | |
| Clinical impact | Poor | Mostly nil effect | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of breakfast cereals does not increase the total daily sodium intake | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Poor | 27 Level IV studies (cross-sectional studies) (all positive quality) | |
| Consistency | Good | 22 studies reported no significant effect; 3 reported an increase in total sodium; and 2 reported a reduction | |
| Clinical impact | Poor | Mostly nil effect | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of presweetened breakfast cereals does not increase total daily sugar intake of children and adolescents | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Poor | 1 Level II study (positive quality) | |
| 4 Level IV studies (cross-sectional studies) (all positive quality) | |||
| Consistency | Poor | 1 Australian and 2 U.S. studies reported no significant effect; 2 U.S. studies (including RCT) reported an increase in total sugar intake for children to 13 y only but not for adolescents | |
| Clinical impact | Poor | Mostly small differences (0–20 g/d higher total sugar intake) | |
| Generalizability | Good | Studies conducted in Australia and the United States | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Weight gain, overweight, and obesity
Meta-analysis.
There has been only 1 meta-analysis of the evidence of the effect of breakfast cereal consumption on obesity (84). It examined 14 studies in 33,205 children and adolescents and calculated that, compared with low or nonconsumers of cereal, high consumers had a lower mean BMI by 1.13 kg/m2 (95% CI: 0.81, 1.46; P < 0.0001). Most of the studies were cross-sectional in design; only 1 intervention trial and 2 prospective studies were included. Breakfast cereal manufacturers funded all but 1 of the studies.
The studies in this meta-analysis did not always control for physical activity or dieting behavior, and these could be important confounding factors in the results. The article concludes: “Overall the evidence reviewed is suggestive that regular consumption of breakfast cereals results in a lower BMI and a reduced likelihood of being overweight in children and adolescents. However, more evidence from long-term trials and investigations into mechanisms is needed to eliminate possible confounding factors and determine causality.”
Systematic reviews.
Three other systematic reviews of the topic have been published (Table 3). There is a significant overlap between the studies included in these reviews and the meta-analysis; the total numbers of publications included in all 4 articles are as follows: 8 intervention studies (40, 85–91), 6 prospective studies (36, 40, 92–95), and 15 cross-sectional studies (24, 27, 32, 33, 35, 38, 41, 42, 55, 59, 96–100).
TABLE 3.
Systematic reviews of breakfast cereals and obesity1
| Authors, year (reference) |
|||
| Timlin and Pereira, 2007 (265) | de le Hunty and Ashwell, 2007 (84) | Kosti et al., 2010 (248) | |
| Study type | 2 prospective | 6 XS | 10 XS |
| 2 RCTs | 2 prospective | 5 prospective | |
| 1 RCT | 6 RCTs | ||
| Intervention/outcome | RTEC consumption at breakfast/BMI, weight loss | RTEC consumption frequency/BMI, weight loss, risk of becoming overweight | RTEC consumption at breakfast or other meals/BMI, WHR, body weight |
| Subjects, n | 19,225 adults (prospective) | 205 children (XS) | 8272 children (XS) |
| 261 adults (RCTs) | 2379 children (prospective) | 4754 children (prospective) | |
| 11,336 adults (XS) | 20,670 adults (XS) | ||
| 17,881 adults (prospective) | 119,054 adults (prospective) | ||
| 52 adults (RCT) | 535 adults (RCTs) | ||
| Study population | Men and women; normal, overweight and obese adults; US, Finland | Males and females, children 4–15 y, normal and overweight; US, UK, Spain, France | Males and females; normal, overweight, and obese; US, Sweden, Greece, UK, Finland |
| Quality2 | Neutral | Positive | Neutral |
| Results | Inverse association between RTEC consumption and BMI in XS studies | Inverse association between RTEC consumption and BMI in all XS studies, although not all statistically significant. In prospective study in adults, 13-y risk of becoming overweight was lower for those eating RTEC daily (OR: 0.88; 95% CI: 0.76, 1.0). | Inverse association between RTEC consumption and BMI and % body fat in all XS studies and prospective studies and RCTs (in children: only when accompanied by nutrition education) |
| No significant effects in intervention trials | |||
RCT, randomized controlled trial; RTEC, ready-to-eat breakfast cereal; WHR, waist-to-hip ratio; XS, cross-sectional.
Determined by using the American Dietetic Association quality rating tool (11): positive, neutral, poor.
The only study that examined breakfast cereal consumption and prospective weight change was that of Bazzano et al. (93). They reported that mean body weight gain over 13 y follow-up of 17,881 U.S. male physicians was significantly less in those who consumed at least 1 serving of breakfast cereal per day compared with those rarely consuming cereals: 1.18 vs. 2.27 kg (P = 0.007). The RR of becoming overweight (BMI ≥25 kg/m2) over the same period was 0.88 (95% CI: 0.67, 0.91; P = 0.01) in regular consumers compared with those rarely consuming cereals.
The 3 reviews suggest that people who eat breakfast cereals regularly have a lower BMI and are less likely to be overweight. However, results from intervention trials are inconsistent and there is limited evidence for any proposed causal mechanism. Furthermore, although the reported benefits from RTEC might be more pronounced among the higher-fiber cereals, there is a need for more large-scale randomized clinical trials.
Additional intervention studies.
Sixteen intervention studies exist in addition to those in the meta-analysis or the 3 reviews and are summarized in Table 4. Most of these studies are short-term and focus only on immediate effects on satiety and next-meal food consumption, and so do not provide strong evidence for claims about longer-term health effects. Of the 3 longer studies (>6 wk), 2 included cereals in hypocaloric diets and found no significant effect (101, 102). One study with 2 servings of oats in an otherwise free diet does provide evidence to support the benefit of oat-based cereals (103). However, that study did not provide information on the control cereal used for comparison and required 2 servings/d to be consumed (103). The other three 6-wk studies had differing results: 1 reported a beneficial effect with an oat-based breakfast cereal taken at 2 meals in a day (104); another also found that increased breakfast cereal consumption assisted weight loss in a hypocaloric diet (105); and another found no effect when evening snacks were replaced by RTEC (106).
TABLE 4.
Additional intervention studies with breakfast cereals and weight management1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Burley et al. (266) | Positive | 20 normal-weight women divided into restrained and unrestrained eaters; UK | Randomized crossover design; comparing high- (12.5 g) and low- (3.0 g) fiber breakfasts on subsequent hunger ratings and food consumption 2.5 h after breakfast | Meals of cereal, full-fat milk, white bread (plain or guar enriched), butter, marmalade, and juice; 2 cereals tested: 40 g Kellogg’s Bran Flakes or 40 g Kellogg’s Corn Flakes | Visual analog ratings of hunger and fullness at 30, 60, 90, 150, and 210 min | There were no significant effects of breakfast type on ratings of hunger or fullness, although restrained eaters consistently expressed less hunger. |
| Food consumed from at 150 min from buffet selection (sandwiches, crisps, yogurt, or biscuits) | There were no significant differences between the breakfasts in ratings of food pleasantness, or on subsequent food intake, comparing the breakfasts with high- or low-fiber cereals. | |||||
| “Greater quantities of fiber may be required to achieve a substantial hunger-reducing effect” (p93) | ||||||
| Levine et al. (267) | Positive | 36 normal-weight men and women; US | Randomized controlled trial; breakfast with different cereals followed by ad libitum buffet lunch 3.5 h later | 5 different RTECs of varying fiber content (range 0–39 g/100 g) served with milk and juice | Energy intake at breakfast and lunch | Subjects were less hungry after eating higher-fiber cereals (P = 0.052) and there was a significant inverse correlation between fiber content of RTEC and energy intake at lunch. Total breakfast + lunch energy intake was lower with the highest vs. the lowest fiber RTEC (1176 vs. 2324 kcal; P < 0.05). |
| Hunger rating after breakfast | “Cereals containing relatively large quantities of dietary fiber may decrease short-term food intake.” (p1303) | |||||
| Geliebter (268) | Unknown | 32 normal- and overweight men and women; US | Randomized controlled trial; isoenergetic high- or low-fiber RTEC breakfast followed by ad libitum lunch 3 h later of preferred flavor of Sustacal taken through a straw | Oatmeal with 8 g fiber or sugared corn flakes (0 g fiber), with water as a control | Food intake measured at lunch | Lunch intakes were significantly smaller after oatmeal (550 g) than cornflakes (790 g) or water (794 g); P < 0005. Appetite ratings from after breakfast to lunch were lowest after the oatmeal breakfast. |
| Hunger rating after breakfast and at interval until lunch | ||||||
| Holt et al. (242) | Positive | 141 normal-weight men and women; UK | Repeated-measures crossover trial comparing 4 isoenergetic breakfasts, consumed over different days; weighed food record of ad libitum intake over the day | Corn Flakes or All-Bran (plus milk, sugar, bread, and jam); RTEC = 42% energy | Energy consumed over the day, measured with weighed food diaries; hunger ratings using visual analog scale | No differences in energy consumed at lunch but total day’s intake was lowest after All-Bran breakfast vs. eggs and bacon (10.1 ± 0.8 vs. 12.0 ± 1.0 MJ; P < 0.05) and hunger returned more slowly after the high-fiber CHO-rich breakfast. No difference with Corn Flakes |
| Other meals: croissant + margarine and jam or fried eggs and bacon and bread and margarine | ||||||
| Kirk et al. (107) | Positive | 22 overweight adults [mean BMI (in kg/m2): 31]; UK | Within person pre-post study design; 2 wk of replacing 1 meal with breakfast cereal, followed by 4 wk ad libitum high-CHO diet | Stage 1: 45 g RTEC with skim milk | Energy intake | After 2 wk: |
| Stage 2: encouraged to use RTEC as a snack | Weight and BMI | Mean energy intake declined from 9.06 to 6.77 MJ/d (P < 0.001) | ||||
| Waist circumference % body fat | Mean BMI declined from 31.0 to 30.3 (P < 0.001). No significant change in body fat or waist circumference. Changes maintained at 6 wk. | |||||
| “Replacing one main meal with breakfast cereal led to moderate weight loss” (p277) | ||||||
| Saltzman et al. (101) | Positive | 41 healthy men and women, both normal- and overweight (mean BMI: 26); US | 8-mo randomized controlled trial, with all food provided in the first 10 wk; hypocaloric diet for 6 wk followed by 6 mo ad libitum | Hypocaloric diet for 6 wk with either a low-soluble-fiber control diet or 45 g rolled oats/1000 kcal | Weight | Both groups lost weight and fat mass at 10 and 36 wk, but there were no significant differences between groups. Weight change at 36 wk: |
| Fat-free mass | Control group: −3.06 ± 0.78 kg | |||||
| Oat group: −2.77 ± 0.69 kg | ||||||
| “Use of an oat cereal rich in soluble fiber in a closely monitored hypocaloric feeding regime does not improve weight loss or dietary compliance” (p50) | ||||||
| Melanson et al. (102) | Positive | 180 overweight and obese adults; US | 24-wk randomized controlled trial with 3 arms | 1: 500 kcal hypocaloric diet plus exercise (avoiding cereals) | Weight | In both diet interventions weight loss was more than with the exercise intervention, but there was no significant difference in weight lost between the 2 diet groups: |
| 2: Hypocaloric fiber-rich diet with 2 servings/d whole-grain cereals plus exercise | Diet + exercise: −6.2 ± 0.7 kg | |||||
| 3: Exercise only | Diet + cereal: −5.7 ± 0.7 kg | |||||
| Ortega et al. (105) | Positive | 67 overweight women (mean BMI: 28.4); Spain | Randomized controlled trial with 20% hypocaloric diet with 2 diets with increased consumption of cereals (C) or vegetables (V) | Diet C: breakfast cereals and cereal bars at least 3×/d, in addition to normal cereal foods | Weight loss | At 6 wk, a weight loss of 2.0 kg (SD: 1.3) was achieved with the V diet and 2.8 kg (SD: 1.4) with the C diet (P < 0.001) |
| Diet V: vegetables at least 3×/d in addition to normal cereal foods | ||||||
| Hlebowicz et al. (135) | Positive | 12 normal-weight men and women; Sweden | Repeated-measures crossover blinded trial; after 8-h fast subjects consumed breakfast, each 1 wk apart | 50 g cereal (All-Bran, or Corn Flakes) (Kellogg) or wholemeal oat flakes (Frebaco) plus 300 g sour milk | GER measured by ultrasound and satiety scores with validated numerical scale over 2 h | Bran cereal had a significantly lower GER than oat cereal (P = 0.023) but was not different from Corn Flakes. |
| There were no significant differences in satiety scores between the 3 cereals. | ||||||
| Rodríguez-Rodríguez et al. (233) | Positive | 57 overweight women (BMI: 24–35); Spain | 6-wk randomized controlled trial with hypocaloric diet (20% less than requirements) with increased consumption of cereals (C) or vegetables (V) | Diet C: 2 servings of RTEC/d (30 g breakfast, 40–60 g dinner) plus a cereal bar midmorning | Satiety quotient (SQ) (= fasting – post meal sensation of hunger/energy consumed at meal) | The mean SQ was greater in women on diet C than diet V at the end of the study (0.3 ± 0.1 vs. 0.2 ± 0.1; P < 0.001). |
| The improved satiety among women consuming the diet with higher cereal content may have contributed to their lower withdrawal rate. | ||||||
| Lightowler and Henry (104) | Positive | 41 overweight and obese men and women; UK | 6-wk randomized trial with subjects required to consume 1 of 2 45-g equicaloric RTEC choices [single choice (SC) or variable choice (VC)] with semi-skimmed milk at breakfast and lunch, without control of other meals | Two choices of RTEC compared: | Weight loss over 6 wk | Mean weight loss from baseline was significantly greater in the VC vs. the SC group (−2.0 vs. −0.6 kg; P = 0.023); % body fat mass also declined significantly in the VC group (−0.9 ± 2.0; P = 0.04) but not in the SC group. |
| SC: Fitnesse (Cereal Partners UK) (1.7 g fiber/serving) | “RTEC cereals are an effective short-term weight-loss strategy when used as a meal replacement” (p53) | |||||
| VC: Shredded Wheat (5.4 g fiber), or Berry Shredded Wheat (5.0 g fiber) | ||||||
| 3-d food diaries used to record diet intake | ||||||
| Hamedani et al. (269) | Positive | 32 normal-weight men and women; Canada | Repeated-measures crossover design of test breakfast, after overnight fast, followed by ad libitum lunch of pizza and water 3 h later | 2 test breakfasts of 60 g RTEC in 1% fat milk): | Visual analog scores of subjective appetite | The high-fiber cereal breakfast suppressed appetite more than the low-fiber cereal (subjective appetite = 17.6. ± 0.1 vs. −10.0. ± 1.1 mm · min· kcal#x22121; P < 0.01). |
| High fiber: Fiber One (28 g fiber/serving) | Energy intake at breakfast and lunch | Cumulative energy intake (breakfast + lunch) was lower after the high-fiber cereal than after the low-fiber cereal: 1130 ± 57 vs. 1422 ± 66 kcal; P = 0.01. | ||||
| Low fiber: Corn Flakes (1.5 g fiber/serving) | “A high-fiber breakfast cereal contributes to energy reduction at breakfast and lunch, possibly due to its high satiety value” (p1343) | |||||
| Matthews et al. (106) | Positive | 70 overweight men and women who were self-reported evening snackers; UK | Randomized controlled 6-wk study; subjects given a selection of breakfast cereals to consume instead of their normal evening snack; control maintained normal habits | 9 different varieties of Kellogg’s RTECs were provided with external packaging removed; participants were advised to try each at least once | Dietary intake measured by 3-d food diaries at weeks 0, 2, 4, and 6; anthropometry measures taken at 2-weekly intervals | There was a trend to lower total daily energy intake in the intervention group but this was not significant. |
| “There were no significant differences between groups in any anthropometric measurements.” (p107) | ||||||
| Chang et al. (103) | Neutral | 34 overweight subjects aged 18–65 y; Taiwan | 12-wk randomized double-blind intervention, with a β-glucan–containing oat cereal or placebo | 37.5 g of cereal mixed with 250 mL hot water, replacing usual food twice daily; both cereals provided 145 kcal and 3.7 g fiber, but oat cereal included 1.5 g β-glucan | Body weight | All 4 anthropometric measures were significantly improved in the intervention compared with control, over 12 wk: |
| BMI | Weight: −2.08 ± 2.05 vs. 0.52 ± 1.74 kg; P = 0.000 | |||||
| % body fat | BMI: −0.81 ± 0.80 vs. 0.15 ± 0.62; P = 0.000 | |||||
| Waist-to-hip ratio | % body fat: −0.93 ± 1.73 vs. 0.39 ± 1.94; P = 0.045 | |||||
| Waist-to-hip ratio: −0.01 ± 0.02 vs. 0.01 ± 0.03; P = 0.003 | ||||||
| Falaize et al. (261) | Neutral | 30 normal-weight men; UK | 3-way crossover design with 3 isocaloric (1370 kJ) breakfasts with differing protein content after a 12-h overnight fast | 1: Two poached eggs and white toast (18.4 g protein) | Energy consumed via weighed food records | The egg-based breakfast was associated with a lower energy intakes compared with the cereal-based breakfast at the following times: |
| Ad libitum lunch of cheese sandwiches and crisps, and dinner of pasta with tomato and cheese sauce provided | 2: Cornflakes, milk and white toast (9.3 g protein) | Subjective ratings of satiety every 30 min using an electronic watch diary (AUC) | Lunch: 1284 ± 464 vs. 1407 ± 379 kcal (NS) | |||
| 3: Croissant, jam, and orange juice (5.0 g protein) | Dinner: 1899 ± 729 vs. 2214 ± 620 kcal (P = 0.023) | |||||
| And over the whole day (P = 0.007) | ||||||
| Satiety scores over the whole day were also all higher with the egg vs. cereal breakfast | ||||||
| How hungry do you feel: 227 vs. 262, P < 0.01 | ||||||
| How much could you eat: 237 vs. 269, P < 0.05 | ||||||
| How full do you feel: 234 vs. 206, P < 0.05 | ||||||
| Rebello et al. (270) | Positive | 46 adults aged 18–75 y (mean BMI: 26.1); US | Randomized 2-way crossover trial with 2 isoenergetic breakfasts (363 kcal) of oat-based cereal (250 kcal) served with fat-free milk and Splenda, consumed after overnight fast | Quaker old-fashioned oatmeal, cooked with water (8.35 g protein, 1.67 g sugar, 6.69 g fiber; 2.63 g β-glucan/serving) vs. | Visual analog scale measures of hunger, fullness, stomach fullness, desire to eat, prospective intake, and satisfaction | There was no significant difference in satisfaction with the 2 cereals; however, oatmeal, which was higher in protein and fiber but lower in sugar than the RTEC, resulted over 4 h in: |
| Electronic visual analog scale measures administered at 30, 60, 120, 180, and 240 min after start of breakfast | Honey Nut Cheerios (General Mills) (4.54 g protein, 20.44 g sugar, 4.54 g fiber; 1.73 g β-glucan/serving) | |||||
| Reduced hunger (P = 0.0036) | ||||||
| Increased fullness (P = 0.005) | ||||||
| Reduced desire to eat (P = 0.002) | ||||||
| Reduced prospective food intake (P = 0.0012) | ||||||
| “Oatmeal improves appetite control and increases satiety. The effects may be attributed to the viscosity and hydration properties of the β-glucan content” (p272) |
CHO, carbohydrate; GER, gastric emptying rate; RTEC, ready-to-eat breakfast cereal.
Several of the intervention studies showed breakfast cereal consumption to be helpful in assisting weight loss when used as snack or meal replacements (87–89, 102–104, 107), although 1 study did not find any significant effect (106).
In contrast, most of the intervention studies that added cereal at breakfast did not show any significant impact on measures of weight (85, 86, 90, 91, 101, 102, 106). It is often difficult to distinguish the effect of a breakfast meal from the effect of breakfast cereals specifically; there is thus a need for larger long-term intervention trials comparing the impact of different types of breakfast cereals when consumed at breakfast.
Additional cross-sectional studies.
Sixteen additional cross-sectional studies were identified that were not included in the 4 systematic reviews (see Supplemental Table 5) (41–43, 45, 46, 66, 68, 81, 108–115). Three of these studies compared the weight status of consumers of PS or non-PS RTECs and found no differences in BMI or waist circumference in children and adolescents (43, 81, 112). This is valuable suggestive information, but results from cohort studies would be ideal to support a firm statement on this issue.
Perhaps the best evidence for a preventive effect of breakfast cereal on weight gain comes from the single-cohort study that has examined this (116), and the computed ORs from cross-sectional studies in the meta-analysis support those results (117). However, in the absence of further cohort and intervention trials, the current evidence is not yet strong enough to claim a direct protective effect.
The summaries in Table 5 reflect the current evidence in the literature. There is insufficient evidence to describe the best types of breakfast cereals, although there are suggestions of a greater protective effect of higher fiber and oat cereals in some (but not all) of the studies.
TABLE 5.
Body of evidence summaries on breakfast cereals and obesity1
| Evidence statement and components | Grade | Rating | Notes |
| Regular consumption of breakfast cereals is associated with a lower BMI and a reduced risk of being overweight or obese in adults and children | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Excellent | 4 Level I studies: 1 meta-analysis (positive quality) plus 3 systematic reviews covering 8 RCTs, 6 cohort studies, and 15 cross-sectional studies) (2 neutral and 1 positive quality) | |
| 14 Level II studies (RCTs) (2 neutral, 12 positive quality) | |||
| 15 Level IV studies (cross-sectional studies) (all positive quality) | |||
| Consistency | Good | All cohort and cross-sectional studies report consistent effect; RCTs results are less consistent | |
| Clinical impact | Satisfactory | ORs for overweight/obesity = 0.19–0.87 in meta-analysis | |
| = 0.88 in cohort study | |||
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of breakfast cereal as a meal or snack replacement can assist in weight loss in adults | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Excellent | 7 Level II studies (RCTs) (all positive quality) | |
| Consistency | Good | Six of the 7 studies reported a beneficial effect on weight loss | |
| Clinical impact | Good | Range of reported weight loss: 1.9–3.4 kg over 6 wk | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of presweetened breakfast cereal does not increase the risk of being overweight or obese in children | C | — | Body of evidence provides some support but care should be taken in its interpretation |
| Evidence base | Poor | 3 Level IV studies (cross-sectional) (all positive quality) | |
| Consistency | Good | All 3 studies show no difference in weight measures | |
| Clinical impact | Poor | Nil effect | |
| Generalizability | Good | Populations studied in the body of evidence cover includes studies in children in the US and Australia | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of high-fiber breakfast cereals improves satiety and reduces hunger after a meal | C | — | Body of evidence provides some support but care should be taken in its interpretation |
| Evidence base | Good | 8 Level II studies (RCTs) (6 positive quality, 1 neutral, 1 poor quality) | |
| Consistency | Poor | 5 of the 8 studies reported a beneficial effect on satiety and hunger; 3 found no effect | |
| Clinical impact | Good | Range of improvement ranges from 13% to 76% in supportive studies | |
| Generalizability | Good | Populations studied in the body of evidence cover a range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Diabetes, glucose intolerance, and metabolic syndrome
Meta-analysis.
There has been 1 meta-analysis of the evidence of the effect of whole-grain breakfast cereal consumption on diabetes (118). That study examined 16 cohort studies looking at whole and refined grains in general, but only 3 studies (with follow-ups ranging from 6 to 19 y) had subanalyses on breakfast cereals specifically, all conducted in the United States (119–121). The RR of incident type 2 diabetes (T2D) comparing the highest vs. the lowest consumption of whole-grain breakfast cereal was 0.72 (95% CI: 0.55, 0.93; P = 0.01). For each additional serving of whole-grain breakfast cereal, the RR was 0.73 (95% CI: 0.59, 0.91; P = 0.006). The authors noted the relatively small number of studies and did not report any results on refined-grain breakfast cereals separately, although their overall conclusion was that refined grains in general are not associated with a reduced risk of T2D.
The largest prospective study in this meta-analysis examined the association of breakfast cereal consumption and the risk of development of T2D among 21,152 male participants in the U.S. Physicians’ Health Study I (120). Weekly cereal consumption in 4 categories (none, ≤1/wk, 2–6 times/wk, and ≥7/wk) was estimated by using an FFQ and breakfast cereals were categorized as whole grain or refined grain by using the method of Jacobs et al. (122). Incident T2D over 19 y of follow-up was ascertained by annual follow-up questionnaires.
When adjusted for age, cigarette smoking, BMI, physical activity, and vegetable and alcohol intake, the HR for T2D in the highest category of consumption compared with the lowest was 0.69 (95% CI: 0.60, 0.79; P-trend < 0.0001). There was evidence for a stronger protective effect of whole-grain breakfast cereals compared with refined-grain cereals at ≥7 servings/wk: an HR of 0.60 (95% CI: 0.50, 0.71) for whole-grain cereals vs. an HR of 0.95 (95% CI: 0.73, 1.3) for refined-grain cereals. However, both were associated with significant risk reductions at 2–6 servings/wk (whole-grain HR: 0.76; 95% CI: 0.66, 0.87; refined-grain HR: 0.69; 95% CI: 0.53, 0.90). The authors speculated that the effect might be due to the fiber content attenuating glycemic responses or that diverse micronutrients such as magnesium, vitamin E, antioxidants, or phytoestrogens may be responsible for the beneficial effects. They conclude: “These results suggest that intake of breakfast cereals might confer a lower risk of DM [type 2 diabetes].”
It should be noted that the population in this study consisted of highly educated male physicians who are likely to have more generally healthy behaviors than the general population, so further studies in other populations are required to confirm the findings.
Cohort studies.
There are 2 other cohort studies (not included in the meta-analysis) that reported on breakfast cereals. The Melbourne Collaborative Cohort Study (123) recruited 41,258 people aged 27–75 y at baseline and examined self-reported diabetes incidence after 4 y of follow-up. There was no significant relation between total breakfast cereal consumption, with an adjusted OR for incident diabetes of 1.01 (95% CI: 0.75, 1.35; P = 0.6). This study did not analyze separately for whole-grain and refined-grain cereals but did report no significant trend with cereal fiber consumption (OR: 1.08; 95% CI: 0.88, 1.32; P = 0.46 for each additional 10 g/d).
The second study aimed to identify a dietary pattern associated with development of T2D (124). It examined data from 7339 British civil servants in the Whitehall II Study who were followed for an average of 12 y. The study used reduced rank regression to identify a dietary pattern that was associated with increased risk of incident T2D (adjusted HR: 1.51; 95% CI: 1.10, 2.09; P < 0.0001). This pattern was characterized by high consumption of soft drinks, onions, burgers, crisps, and white bread and low consumption of medium- and high-fiber breakfast cereals. However, none of the individual foods (including breakfast cereals) showed significant associations with risk of T2D.
One other relevant cohort study is from the Nurses’ Health Study (125). Although it did not analyze for breakfast cereals specifically, it reported on whole-grain, bran, and germ intake and risk of T2D and found a reduced risk with total whole-grain intake when the highest and lowest quintiles of intakes were compared (RR: 0.75; 95% CI: 0.68, 0.83; P < 0.001). The results for bran were similar (RR: 0.72; 95% CI: 0.65, 0.80; P < 0.001), but there was no significant relation with germ intake. However, the whole grain and bran in these studies were from all foods, so would include bread and other grain food sources as well as breakfast cereals.
Overall, there were conflicting results from these cohort studies. Although the Physicians’ Health Study showed a protective effect of all breakfast cereals, the Melbourne and Whitehall studies did not find this. It may be that the protective effects of whole-grain cereals or cereals with bran were diluted in these studies, which did not separate out breakfast cereals by subtypes.
Cross-sectional studies.
There were 3 relevant cross-sectional studies. A small Malaysian study in diabetic subjects found an association between oat consumption and better blood glucose control but no relation with cornflakes (113). A U.S. study in young adults reported that RTEC consumers were less likely to be overweight or have elevated serum insulin, but the only association related to diabetes was a slightly higher glycosylated hemoglobin concentration in those who included RTEC in their breakfasts. There was no difference in the prevalence of metabolic syndrome (114). Results from the 2001–2008 NHANES showed that, compared with breakfast skippers, RTEC breakfast consumers aged 19–51 y were less likely to have elevated blood glucose and metabolic syndrome, but there were no differences in those aged 51–70 y (115).
Intervention trials.
Most of the other evidence comes from 11 short-term studies examining the effect of different food products on carbohydrate metabolism (126–136). Table 6 summarizes the results from these RCTs: 6 in diabetic and 5 in nondiabetic adults. All but 1 were short-term studies comparing the effect of different breakfast cereals on glucose and insulin responses. One 6-mo study compared the effect of high- or low-GI cereals added to the diet of subjects with non–insulin-dependent diabetes (131).
TABLE 6.
Intervention trials of breakfast cereals and diabetes1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Diabetic subjects | ||||||
| Colagiuri et al. (127) | Positive | 8 subjects (males and females, aged 42–69 y) with NIDDM but treated with insulin; Australia | Randomized crossover design study. Subjects given 3 test breakfast meals in random order of 3 d, 48 h apart. Meals prepared by a dietitian; blood collected at 30 min intervals for 3 h. | 3 meals matched in energy (470–480 kJ) and CHO (54–60 g) | Postprandial glucose (PG), serum insulin (SI), and C-peptide (CP) responses | Postprandial responses to meals A and B were similar. Meal C (muesli and skim milk) produced lower PG and SI responses to both other meals (P < 0.02) and less endogenous insulin secretion CP: C = 62.8 vs. B = 99.8 vs. A = 89.8 pmol ⋅ min#x22121 ⋅ mL#x22121 (P < 0.05). |
| A: 2 eggs, 2 slices whole-meal toast, orange juice | ||||||
| B: 2 Weet-Bix, whole-meal toast, | ||||||
| C: 75 g muesli | ||||||
| All with milk, tea, or coffee | ||||||
| Golay et al. (126) | Positive | 14 adults with type 2 NIDDM, treated with insulin; mean age = 69 y; mean BMI (in kg/m2) = 29; Switzerland | Randomized crossover design study: two 1-wk periods separated by 1-wk washout. Patients followed normal diet but provided with SRS or FRS breakfast (46 g CHO) and morning snack food | 2 breakfast meals: | Plasma glucose and insulin throughout the day, and over 3 h after oral GTT at end of diet period | Mean daily blood glucose concentration 21% lower with muesli breakfast compared with cornflakes (7.7 ± 0.7 vs. 9.7 ± 0.9; P = 0.023) |
| SRS: 65 g muesli + 120 mL whole milk | Fasting insulin was 17% lower after the muesli compared with cornflakes (126 vs. 150; P < 0.05). No change in Hb A1c. | |||||
| FRS: 35 g cornflakes + 12 g sugar + 120 mL whole milk | Patients reduced daily insulin doses from mean of 28 ± 4 to 24 ± 4 U (P < 0.05) during the muesli period. | |||||
| “Switching at breakfast only from standard cereals to slow-release starch cereals improves the CHO metabolism of diabetic patients” (p135) | ||||||
| Tappy et al. (129) | Positive | 8 subjects (males and females, aged 49–65 y) with NIDDM; Switzerland | Randomized crossover design study. Subjects given 4 breakfast meals, in random order on different days, each providing 35 g CHO. | 3 meals with milk and an extruded breakfast cereal with 4, 6, or 8.4 g β-glucan from oats, and 1 with whole-meal bread, ham, and jam | AUC of postprandial plasma glucose and insulin measured over 4 h | Compared with the noncereal breakfast, all 3 cereal breakfasts significantly decreased the peak and average glucose and insulin increments. Maximum increases in plasma glucose after cereal breakfast were 67% (P < 0.05), 42%, and 38% (P < 0.001) with 4, 6, or 8.4 g β-glucan cereal compared with the noncereal breakfast. |
| Wheeler et al. (128) | Positive | 24 subjects (males and females) aged 14–25 y with IDDM; US | Randomized crossover design study. Subjects given 4 test breakfast meals in random order of 4 d, 72 h apart. Meals were prepared by a dietitian; blood collected at 30 min intervals for 3 h. | 4 meals matched for CHO (50 g/1.73 m2 body surface) | AUC over 3 h for: | There was no difference in the AUC for the 2 cereals for plasma glucose. |
| 1) unsweetened cornflake cereal | Plasma glucose | There were no differences in insulin response to any of the meals. | ||||
| 2) sweetened cornflake cereal (40% sucrose) (both Kellogg Co) | Free insulin | “Equivalent gram amounts of CHO as presweetened cereals are not detrimental to people with IDDM compared to unsweetened cereals.” (p458) | ||||
| 3) sucrose alone | ||||||
| 4) glucose alone | ||||||
| All consumed with water | ||||||
| Tsihlias et al. (131) | Positive | 72 subjects with type 2 NIDDM; mean age = 62 y, mean BMI = 27; Canada | Randomized parallel design with 3 treatment arms each lasting 6 mo: 10% energy from high-GI breakfast cereal, low-GI breakfast cereal, or high-MUFA intake with no breakfast cereal | High-GI cereals: cornflakes (Nature's Path), puffed rice (Arrowhead Mills), crispy rice (Our Compliments) | Hb A1c | Compared with MUFA treatment, with cereal breakfasts subjects consumed 10% more energy from CHO. |
| Low-GI cereals: Bran Buds with psyllium (Kellogg) or prototype extruded oat cereal with psyllium | Fasting glucose | There were no significant differences in Hb A1c or fasting glucose between treatments, although cereal treatment groups had higher 8-h plasma insulin concentrations after cereal breakfast compared with the MUFA group (P < 0.05). | ||||
| MUFA-diet subjects given margarine and olive oil | Plasma insulin | “A 10% increase in CHO intake from breakfast cereal had no deleterious effects on glycemic control over 6 mo in subjects with type 2 DM [diabetes mellitus].” (p439) | ||||
| Rendell et al. (136) | Positive | 16 nondiabetic men and women (mean age = 56 y, mean BMI = 30)and18 type 2 NIDDM men and women (mean age = 62 y, mean BMI = 33); US | Randomized crossover design comparing 2 cereal breakfast test meals, and a liquid meal replacement control, each test day separated by 3–7 d washout. Subjects tested after standardized evening meal and overnight. | 65 g oatmeal (7 g fiber) or Prowash barley flakes (23 g fiber) cooked with 360 mL water | AUC postprandial plasma glucose and insulin over 2 h | The AUC glucose and insulin concentrations were significantly lower with the Prowash barley compared with oatmeal in both normal and diabetic subjects. |
| Prowash barely contained 15% β-glucan vs. 5% in oats | In diabetics: | |||||
| Glucose: 83 ± 13 vs. 200 ± 34 mg/dL (P < 0.001) | ||||||
| Insulin: 30 ± 6 vs. 93 ± 32 mIU/dL (P < 0.001) | ||||||
| “Inclusion of foods with CHO that are absorbed slowly is beneficial in both the diabetic and prediabetic states” (p66) | ||||||
| Nondiabetic subjects | ||||||
| Wolever et al. (132) | Positive | 77 healthy nondiabetic men aged 18–75 y; BMI = 18.5–34; divided into normal and high fasting insulin (≥41 pmol/L); Canada | Randomized crossover design study with 2 breakfasts consumed after overnight fast. | 1) High-fiber cereal (Fiber One): 36.8 g available CHO + 36.7 g fiber | Plasma glucose and insulin measured over 2 h after breakfast | In all subjects, 2-h AUC plasma glucose increase was less after high-fiber cereal (107 ± 7 vs .130 ± 8 mmol × min/L; P < 0.001). |
| 2) Low-fiber cereal (Cornflakes): 36.8 g available CHO + 0.8 g dietary fiber) | Insulin peak response was only reduced by high-fiber cereal in hyperinsulinemic men (351 ± 29 vs. 485 ± 55 pmol/L; P = 0.044) but not normal controls. | |||||
| Both consumed with 250 mL low-fat milk. | “RTEC rich in nonviscous cereal fiber reduces glucose responses in normal and hyperinsulinemic men” (p1285) | |||||
| Maki et al. (133) | Positive | 27 healthy nondiabetic nonsmoking men aged 25–54 y with BMI <32; US | Randomized crossover study with two 2-wk treatment periods with a 1-wk washout, incorporating oat- or wheat-based breakfast cereals into usual diet. | Two energy- and fiber-matched cereals provided: | Postprandial glucose and insulin responses over 10 h after a fat-loading breakfast including hot cereal | “Postprandial insulin and glucose responses over 10 h did not differ between [oat and wheat] treatments” (p347) |
| Oat: 76 g/d oat bran RTEC plus 60 g/d hot oatmeal | ||||||
| Wheat: 84 g/d Frosted Mini-Wheats (Kellogg) plus 60 g/d hot rolled-wheat cereal | ||||||
| Hlebowicz et al. (135) | Positive | 12 healthy nondiabetic men and women; mean age = 28 y, mean BMI = 22; Sweden | Randomized crossover design study with 3 breakfast meals taken after an overnight fast, more than 1 wk apart. | Each 50 g cereal served with 300 g sour milk: | 1) GER measured by real-time ultrasonography | The wheat-bran-based cereal resulted in a lower GER (33%) compared with the oat-based cereal (51%) (P < 0.05) but was not significantly different from cornflakes. |
| 1) All-Bran (7.5 g fiber) | 2) Blood glucose from finger-prick samples | There were no significant differences in the 2-h AUC for glucose or satiety. | ||||
| 2) Whole-meal oat flakes (4 g fiber) | 3) Validated satiety score | “Cereal bran flakes slows the GER when compared to oat flakes and corn flakes, probably due to a higher fiber content.” (p1) | ||||
| 3) Cornflakes (1.5 g fiber) | ||||||
| Granfeldt et al. (130) | Positive | 19 healthy nondiabetic mean and women; mean age = 38 y, mean BMI = 22.4; Sweden | Crossover design study with 2 breakfast test meals taken after an overnight fast, 1 wk apart. | 2 oat bran mueslis, made with 3 or 4 g of β-glucan, served with vanilla yogurt, plus a sandwich of white bread, cheese, and butter | AUC of blood glucose and insulin measured over 2 h after breakfast meal | Muesli with 3 g β-glucans gave no significant difference in glycemic response compared with the reference. |
| Meals standardized to a total of 50 g available CHO | Muesli with 4 g β-glucans compared with a reference meal (no muesli) produced a lower glycemic response: | |||||
| Reference meal used muesli with corn rather than oat flakes | AUC: glucose, −29.3%; insulin, −42% (P < 0.05) | |||||
| “4 g β-glucan from oats seems to be a critical level for a significant decreases in glucose and insulin responses in healthy people” (p600) | ||||||
| Kim et al. (134) | Positive | 17 normoglycemic obese women, age 51 y, mean BMI = 33.2; US | Randomized crossover design comparing 5 cereal breakfast test meals, each test day separated by 7-d washout. Subjects tested after standardized evening meal and overnight fast. | 5 energy- and CHO-matched hot cereals (mixed wheat and barley) with 0, 2.5, 5, 7.5, or 10 g β-glucan per serving | Postprandial plasma glucose and insulin measured over 3 h | The 10-g β-glucan cereal significantly reduced peak glucose at 30 min (P < 0.05), but 2-h AUC did not differ between cereals. |
| 10 g β-glucan cereal significantly reduced AUC for insulin (P < 0.05) vs. 0 or 5 g. | ||||||
| “High β-glucan whole-grain products may prove useful in the inclusion of dietary management of hyperglycemia in obese women” (p174) |
CHO, carbohydrate; FRS, fast release starch; GER, gastric emptying rate; GI, glycemic index; GTT, glucose tolerance test; Hb A1c, glycated hemoglobin; IDDM, insulin dependent diabetes mellitus; NIDDM, non–insulin-dependent diabetes mellitus; RTEC, ready-to-eat breakfast cereal; SRS, slow release starch.
Several studies reported improved glucose or insulin responses with oat-, barley-, or psyllium-based cereal or muesli breakfasts compared with other breakfast cereals in diabetic subjects (126, 127, 129, 131, 136), and the effect was also seen in some studies in normal subjects when cereals with β-glucan were studied (130, 134). In normoglycemic subjects, higher-fiber breakfast cereals seemed to reduce postprandial plasma glucose responses (132), but 2 studies found no difference between oat- and wheat-based breakfast cereals in this regard (133, 135). One study reported no difference in insulin or glucose responses in subjects with non–insulin-dependent diabetes whether breakfast cereals were sweetened with 40% sucrose or were unsweetened (128).
Several of the studies compared the effects of high- and low-GI breakfast cereals. However, many factors can affect GI values, and its practical application may be limited as a method of assessing the healthiness of individual foods. This is supported by a study in women who consumed high- or moderate-GI breakfast cereal breakfasts (GI: 77 vs. 51) (137). There were no differences related to the breakfast type in plasma glucose or insulin responses, nor estimated fat and carbohydrate oxidation rates during the subsequent exercise periods. Furthermore, a recent study of 43 Australian breakfast cereals showed that there was no relation between the sugar content and the GI value of breakfast cereals (82).
In summary, there are few long-term studies examining the relation between breakfast cereal consumption and diabetes risk. There is some evidence supporting the role of breakfast cereals, especially those higher in fiber, in the management of diabetes, but the evidence is not strong. Table 7 summarizes the evidence, but more studies in different populations are needed to confirm these relations.
TABLE 7.
Body of evidence summaries on breakfast cereals and diabetes
| Evidence statement and components | Grade | Rating | Notes |
| Regular consumption of whole-grain and high-fiber breakfast cereals is associated with a reduced risk of diabetes | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Good | 1 Level I study (meta-analysis of 3 cohort studies) (positive quality) | |
| Consistency | Good | All studies reported a protective effect from whole-grain breakfast cereal consumption | |
| Clinical impact | Good | RR = 0.76 (95% CI: 0.69, 0.84) for daily consumption of whole-grain breakfast | |
| RR = 0.73 (95% CI: 0.59, 0.91) for each additional daily serving | |||
| Generalizability | Satisfactory | 2 of the 3 studies were in U.S. health professionals, and it is hard to judge if it is reasonable to generalize to the total population | |
| Applicability | Good | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of breakfast cereals is associated with a reduced risk of diabetes | D | — | Body of evidence is weak and recommendation must be applied with caution |
| Evidence base | Good | 3 Level III–2 studies (cohort studies) (all positive quality) | |
| 2 Level IV (cross-sectional) (positive quality) | |||
| Consistency | Poor | One large cohort study reported a protective effect from breakfast cereal consumption but 2 others found no effect, nor did the 1 cross-sectional study | |
| Clinical impact | Satisfactory | RR = 0.69 (95% CI: 0.60, 0.79) for daily consumption of breakfast cereals in the Physicians’ Health Study | |
| Generalizability | Satisfactory | Studies were conducted in the US, UK, and Australia | |
| Applicability | Good | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Consumption of high-fiber breakfast cereals, especially those high in soluble fiber, may assist in the management of hyperglycemia in people with diabetes | C | — | Body of evidence provides some support for recommendation but care should be taken in its application |
| Evidence base | Satisfactory | 5 Level II studies (RCTs1) (all positive quality) | |
| 1 Level IV study (cross-sectional studies) (positive quality) | |||
| Consistency | Good | All studies consistent | |
| Clinical impact | Good | Plasma glucose 21–67% lower after high-fiber cereal vs. controls | |
| Generalizability | Good | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Cardiovascular disease
Meta-analyses and reviews.
There are no meta-analyses of the relation of breakfast cereals with the incidence of cardiovascular disease (CVD). However, there are 5 meta-analyses of whole-grain cereals generally (138–142), which all reported a finding of reduced risk of coronary heart disease with whole-grain consumption, ranging from 19% to 30% reductions with intakes of ≥3 servings/d. Similarly, a meta-analysis of the effect of dietary fibers on blood cholesterol reported significant decreases in total and LDL cholesterol with the consumption of oats and psyllium (143), and a recent meta-analysis concluded that insoluble fiber from cereal sources is inversely associated with risk of coronary heart disease and CVD (144).
Bioactive components of the aleurone in bran may be particularly important in reducing the risks of CVD (145), and the position of the ASN is that “consumption of foods rich in cereal fiber or mixtures of whole grains and bran is modestly associated with reduced risk of obesity, T2D, and CVD” (146).
A Cochrane review of whole grains and heart disease noted specifically that 8 of the 10 studies were with oats, and that their meta-analysis found effects of lower total cholesterol (−0.20 mmol/L; 95% CI: −0.31, −0.01 mmol/L; P = 0.0001) and LDL cholesterol (−0.18 mmol/L; 95% CI: −0.28, −0.09 mmol/L; P < 0.0001) from oats (141). There are also meta-analyses reporting significant cholesterol-lowering effects of barley (−0.30 mmol/L; 95% CI: −0.39, −0.21 mmol/L; P < 0.001) (147) and psyllium-enriched cereals (−0.30 mmol/L; 95% CI: −0.40, −0.20 mmol/L; P = 0.001) (148).
At least 8 other systematic literature reviews (149–156) all reported a finding of reduced risk of coronary heart disease with oat, barley, or psyllium consumption, ranging from 19% to 30% reductions in cholesterol concentrations with the highest intakes of ≥3 servings/d.
Cohort and case-control studies.
Four cohort studies and 1 case-control study reported on CVD outcomes with breakfast cereal consumption (Table 8). The study in UK vegetarians only looked at bran-based breakfast cereals and found no relation with ischemic heart disease incidence, but the other 4 studies all reported protective effects from whole-grain breakfast cereal consumption.
TABLE 8.
Cohort and case-control studies of breakfast cereals and risk of CVD1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Key et al. (210) | Positive | 4336 men and 6453 women recruited from 1973–1979; 42% vegetarians; mean age = 46 y; UK | Prospective cohort study with 17 y follow-up; causes of death ascertained from death certificates | 5 foods reported; frequency of bran cereal consumption assessed with questionnaire: at least daily, at least once a week, less than once a week | SMRs | 27% ate bran cereals daily. |
| 350 deaths from IHD | Vegetarian diet associated with 15% reduction in mortality from heart disease, but no significant association of daily bran cereal consumption with IHD. SMR = 0.99 (95% CI: −0.79, 1.25) | |||||
| Liu et al. (195) | Positive | 86,190 male physicians aged 40–84 y in 1992, free of CVD at baseline, in the Physicians’ Health Study; US | Prospective cohort study with 5.5 y follow-up | Semiquantitative FFQ; for breakfast cereals, specific brands, portion sizes, and frequencies recorded; 7 frequency categories from never to ≥2 servings/d; whole-grain classified according to Jacobs (≥25% whole-grain or bran content) (122) | 1381 deaths from CVD | Compared with those who never or rarely consumed cereals, the relative risk of CVD mortality for men in the highest consumption category (≥1 serving/d) was: |
| Multiadjusted hazard RR for CVD mortality; deaths classified based on death certificates | All breakfast cereals: | |||||
| RR = 0.87 (0.74, 01.03); P = 0.08 | ||||||
| Refined-grain breakfast cereals: | ||||||
| RR = 1.04 (0.84, 1.27); P = 0.37 | ||||||
| Whole-grain breakfast cereals: | ||||||
| RR = 0.80 (0.66, 0.97); P = 0.008 | ||||||
| “CVD-specific mortality [was] inversely associated with whole-grain but not refined-grain breakfast cereal intake.” (p594) | ||||||
| Djoussé and Gaziano (271) | Positive | 21,376 male physicians aged 40–84 y in 1992, free of CVD at baseline, in the Physicians’ Health Study; US | Prospective cohort study with 19.6 y follow-up | Semiquantitative FFQ; for breakfast cereals, specific brands, portion sizes, and frequencies were recorded; 7 frequency categories from never to ≥2 servings/d; whole-grain classified according to Jacobs (≥25% whole-grain or bran content) (122) | 1018 cases of HF | Compared with those who never or rarely consumed cereals, men in the highest consumption category (≥1 serving/d) |
| Multiadjusted hazard RR for HF incidence from self-report questionnaire | All breakfast cereals: | |||||
| RR = 0.0.71 (95% CI: 0.60, 0.85); P < 0.001 | ||||||
| Refined-grain breakfast cereals: | ||||||
| RR = 0.83 (95% CI: 0.58, 1.18); P = 0.70 | ||||||
| Whole-grain breakfast cereals: | ||||||
| RR = 0.72 (95% CI: 0.59, 0.88); P < 0.001 | ||||||
| “A higher intake of whole-grain breakfast cereals is associated with lower risk of HF” (p2080) | ||||||
| Lockheart et al. (272) | Positive quality | 106 first MI cases and 105 controls matched for age, sex, and location; men and women aged 45–75 y; Norway | Case-control | Previous year’s diet assessed with validated 190-item FFQ, grouped into 35 food groups: “whole-grain breakfast cereals” = rolled oats, 4-grain cereal, corn and oat flakes, or muesli (refined grain cereals not reported) | ORs calculated by parallel logistic regression across tertiles of intake | Lowest median intake (0 g/d) vs. highest tertile (36 g/d): OR = 0.38 (95% CI: 0.16, 0.92); P < 0.05 |
| “Whole-grain breakfast cereals [were] significantly associated with reduced risk of MI” (p384) | ||||||
| Djoussé et al. (273) | Neutral | 20,900 male physicians aged 40–84 y in 1992, free of CVD at baseline, in the Physicians’ Health Study; US | Prospective cohort study with 22.4 y follow-up | Semiquantitative FFQ; for breakfast cereals, specific brands, portion sizes, and frequencies were recorded; 7 frequency categories from never to ≥2 servings/d; whole-grain classified according to Jacobs (≥25% whole-grain or bran content) (122) | 1200 cases of HF | Compared with those who never or rarely consumed cereals, men who consumed ≥1 serving/wk had a lower lifetime risk of HF: |
| Lifetime risk of HF at age 40 y according to 6 lifestyle factors, including breakfast cereal consumption | % Lifetime risk: 12.9 (95% CI:11.7, 14.1) vs. 15.0 (95% CI: 13.5, 16.50) (P value not stated) | |||||
| “Consumption of breakfast cereal and fruits and vegetables were individually associated with a lower lifetime risk of heart failure.” (p397) |
CVD, cardiovascular disease; HF, heart failure; IHD, ischemic heart disease, MI, myocardial infarction; SMR, standardized mortality rate.
Intervention trials.
Most intervention trials measured short-term effects on blood lipids or blood pressure. Four looked at the influence of folate-fortified breakfast cereals on plasma homocysteine. In addition to those studies in the reviews and meta-analyses, 3 recent RCTs with oat-based breakfast cereals confirmed their cholesterol-lowering effects. A 12-wk study in overweight Taiwanese subjects reported a 10% reduction in total and LDL cholesterol when 2 servings of oat cereals were consumed per day (103). A 12-wk U.S. study in 204 overweight and obese adults found that 2 portions/d of ready-to-eat oat cereal lowered total cholesterol by 5.4% and non–HDL cholesterol by 6.3% (86). In Australia, a 6-wk trial providing mildly hypercholesterolemic men and women with 3.2 g of β-glucan/d in 2 servings of oat-based porridge or cereal bars resulted in reductions of 7.8% in total cholesterol and 8.4% in LDL cholesterol (157).
Wheat-based cereals do not have any effect on serum cholesterol. The 2002 review by Truswell (156) noted that of 34 published trials with wheat fiber, 27 showed no effect and 2 showed increases in total cholesterol. This negative finding has been repeated in several recent trials with wheat-based breakfast cereals (158–160).
A Canadian study in 72 subjects with T2D randomly assigned them to 10% more energy from carbohydrate in the form of low-GI breakfast cereals (Bran-Buds or oat cereals with psyllium) (Kellogg) or high-GI options [cornflakes (Nature's Path), puffed rice (Arrowhead Mills), or crispy rice (Our Compliments)], with a higher MUFA control (131). There were no significant differences in serum total, LDL, or HDL cholesterol between the 2 types of breakfast cereals, nor any significant effect on blood lipids over the 6-mo study (161).
One study that added 60–80 g/d of 2 refined-grain breakfast cereals (Kellogg Corn Flakes and Rice Krispies) to the diets of 209 free-living subjects in Finland found that this led to a 2.5% reduction in saturated fat intake and a subsequent small (1%) reduction in total cholesterol over one 6-wk period, which was significantly different from controls only because their concentrations increased over the same time (P = 0.007). However, in a second arm of the study, there was no effect on blood lipids (91).
High plasma total homocysteine (tHcy) may be an independent risk factor for CVD (162) and supplemental folate can decrease homocysteine concentrations. Several studies showed that folate-fortified RTEC can reduce elevated homocysteine (163–165), and 1 New Zealand trial reported that fortified breakfast cereal was more effective in reducing tHcy concentrations than supplements or dietary education (166). Another study in 70 subjects at the upper end of the normal range of tHcy found that 4 wk of daily consumption of breakfast cereal fortified with 100 μg of folate resulted in a 16% reduction in tHcy (167).
However, these results should be interpreted cautiously. Subjects with moderate homocysteine concentrations who are already eating other folate food sources regularly may not benefit (168), and a meta-analysis of 19 studies concluded that B-vitamin supplementation to reduce homocysteine does not have any significant effect on risk of CVD (169).
Cross-sectional studies.
Ten cross-sectional studies were identified, which were not included in the systematic reviews (32, 40, 110, 113–115, 170–173). Given the low value of cross-sectional designs, only brief descriptions of these studies are summarized in Supplemental Table 6.
In summary, there is strong evidence from the RCTs that consumption of breakfast cereals that are sources of soluble fiber (from oats, barley, and psyllium) is associated with better cardiovascular lipid profiles —specifically lower total and LDL cholesterol—although there seems to be no effect on HDL cholesterol. There are few intervention studies examining the long-term risk of CVD outcomes, but the few cohort and case-control studies mostly support a protective effect for whole-grain breakfast cereals. Table 9 summarizes the body of evidence statements.
TABLE 9.
Body of evidence summaries on breakfast cereals and CVD1
| Evidence statement and components | Grade | Rating | Notes |
| Regular consumption of oat-, barley- or psyllium-based breakfast cereals can help lower total and LDL cholesterol concentrations | A | — | Body of evidence can be trusted to guide practice |
| Evidence base | Excellent | 6 Level I studies: 3 meta-analysis plus 3 systematic reviews covering over 70 different RCTs (all positive quality) | |
| 3 Level II studies: RCTs (2 servings of oat-based cereals/d) (all positive quality) | |||
| Consistency | Excellent | RCTs results show consistent protective effect | |
| Clinical impact | Good | In meta-analyses, reductions ranged from 0.2 to 0.3 mmol/L (total cholesterol) and from 0.1 to 0.35 mmol/L (LDL cholesterol). | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of whole-grain breakfast cereals is associated with lower risk of CVD | C | — | Body of evidence provides some support but care should be taken in its application |
| Evidence base | Satisfactory | 4 Level III studies (3 cohort and 1 case-control) all positive quality) | |
| 1 Level IV study (cross-sectional) (all positive quality) | |||
| Consistency | Good | Most studies consistent. Lack of effect in 1 cohort study may be due to low background risk in the vegetarian cohort and limited diet intake data. | |
| Clinical impact | Good | RR for CVD: 0.72–0.80 | |
| OR for IHD incidence: 0.38 | |||
| Generalizability | Good | Populations studied in the US, UK, and Norway | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of breakfast cereals is associated lower total and LDL-cholesterol concentrations | D | — | Body of evidence is weak and must be applied with caution |
| Evidence base | Poor | 10 Level IV studies (cross-sectional in children and adults) (all positive quality) | |
| Consistency | Good | Mostly consistent effect, but some report effect only with whole-grain cereals | |
| Clinical impact | Satisfactory | Moderate effect: generally 1–7% reduction | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
CVD, cardiovascular disease; IHD, ischemic heart disease; RCT, randomized controlled trial.
Hypertension
Evidence examining the relation between breakfast cereals and hypertension is limited to just 3 RCTs, 1 cohort and 2 cross-sectional studies (Table 10). The most convincing evidence comes from the Physicians’ Health Study (174). It found a 19% reduction in hypertension risk with daily breakfast cereal consumption and a stronger relation with whole-grain than with refined-grain cereals. The authors suggested that a number of components in cereals—including folate, magnesium, potassium, and fiber—may be responsible for this effect. However, these results were obtained in physicians who are likely to have generally healthy lifestyles, and the results do not provide any data on hypertension risk in women.
TABLE 10.
Studies of breakfast cereal and risk of hypertension1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Davy et al. (175) | Positive | 36 overweight mildly hypertensive men [mean age = 59 y; mean BMI (in kg/m2) = 29.4]; US | 12-wk randomized controlled trial, with participants consuming whole-grain oat or wheat cereals, providing 14 g dietary fiber/d | Normal diet plus 2 cereal meals per day: | Resting supine and seated BP | No effect on casual or 24-h BP in mildly hypertensive men with either the oat or wheat cereal diets |
| Wheat cereals used: Kellogg’s Mini-Wheats; Mother’s Whole Wheat hot natural cereal; oat cereals used: Quaker oat-bran cold cereal or oatmeal | 1) A hot cereal (oat or wheat) at breakfast | BP variability | “Any cardioprotective benefit of regular oat consumption may not be conferred via an arterial BP-lowering effect” (p394) | |||
| 2) A cold cereal (oat or wheat) as a snack | ||||||
| Cereals increased the mean CHO in both groups by 5%E. | ||||||
| Pins et al. (176) | Positive | 45 men and 43 women being treated for hypertension (mean age = 47.6 y; mean BMI = 30.9); US | 12 wk pseudo-randomized controlled parallel-group trial, with either oat cereal or isocaloric low-fiber wheat/corn cereal interventions | Diets incorporating 2 servings of cereal per day: | Antihypertensive medication | Reduced need for antihypertensive medication: 73% in oats group vs. 42% in control (P < 0.05) |
| Oats (1 serving oatmeal + 1 serving Quaker oat squares = 5.42 g β-glucan/d) | “A diet containing soluble fiber-rich whole oats can reduce the need for antihypertensive medication and improve BP control” (p353) | |||||
| Control: wheat/corn-based cereals | ||||||
| Maki et al. (177) | Positive | 97 men and women with elevated BP (systolic = 130–179 mm Hg; and/or diastolic = 85–109 mm Hg); US | 12-wk randomized double-blind controlled trial, with participants consuming 7.7 g/d β-glucan from oats or control foods | Intervention subjects consumed an oat bran RTEC, a hot oatmeal cereal, and a β-glucan powder as a drink, throughout the day | Resting BP | No change in BP between arms overall |
| Obese subjects (BMI >31.5) only with β-glucan diet had lower BP vs. with control foods: | ||||||
| Systolic: −5.6 vs. + 2.7 mm Hg | ||||||
| Diastolic: −2.3 vs. +1.9 mm Hg (both P < 0.02) | ||||||
| “Beneficial effects of foods containing β-glucan from oats on blood pressure in obese subjects.” (p786) | ||||||
| Kochar et al. (174) | Positive | 13,638 men in the Physicians Health Study I aged 40–86 y; US | Prospective cohort study commenced in 1981–1983 with mean follow-up of 16.3 y | Diet assessed by validated FFQ with 7 frequency categories of breakfast cereals (from rarely/never to ≥2/d); whole-grain cereals categorized by using the Jacobs definition (122) | Hypertension HR (adjusted for age, smoking, BMI, alcohol, fruit and vegetables, physical activity, and history of type 2 diabetes) | HRs for daily breakfast cereal consumption: |
| 7367 cases of self-reported incident hypertension (systolic = ≥140 mm Hg, diastolic = ≥90 mm Hg) | All cereals = 0.81 (95% CI: 0.75, 0.86); P < 0.0001 | |||||
| Refined = 0.86 (95% CI: 0.74, 1.00); P = 0.003 | ||||||
| Whole-grain = 0.80 (95% CI: 0.74, 0.86); P < 0.0001 | ||||||
| “Whole-grain breakfast cereal consumption confers a lower risk of hypertension in middle-aged males.” (p89) | ||||||
| McGill et al. (115) Sanders et al. (173) | Positive | 9292 adults aged 19–50 y and 5024 adults aged 51–70 y from the 2001–2008 NHANES; US | Cross-sectional study using the NHANES 2001–2008 database | Self-defined RTEC consumers (any amount) in 24-h diet recall survey (n = 1148) | Hypertension incidence and OR (adjusted for age, ethnicity, income, energy intake, physical activity, smoking, alcohol, BMI) | In 19–50-y-olds, % incidence of hypertension: RTEC breakfast consumers vs. other breakfast consumers: |
| BP recorded as mean of 3 or 4 readings | ||||||
| Hypertension = ≥130 mm Hg systolic, ≥85 mm Hg diastolic | 21 ± 0.2 vs. 25 ± 0.1; P < 0.05 | |||||
| Risk of hypertension: RTEC breakfast consumers vs. other breakfast consumers: | ||||||
| OR = 0.64 (95% CI: 0.50, 0.82). P = 0.007 | ||||||
| There were no significant differences in adults aged 51–70 y. | ||||||
| Deshmukh-Taskar et al. (114) | Positive | 5316 adults aged 20–39 y; US | Cross-sectional study using the NHANES 1999–2006 database | Diet assessed from 24 diet recalls; breakfast characterized as skippers (BS), RTEC, or other breakfast (OB) (i.e., no RTEC consumed) | Hypertension. ORs adjusted for energy intake, age, sex, ethnicity, income, smoking, alcohol, physical activity, marital status | Compared with other breakfast consumers, RTEC consumers were 24% less likely to have hypertension. ORs: |
| BP recorded as mean of 3 or 4 readings | RTEC vs. OB = 0.76 (95% CI: 0.58, 0.99); P < 0.0167 | |||||
| Hypertension = ≥130 mm Hg systolic, ≥85 mm Hg diastolic | RTEC vs. BS = 0.63 (95% CI: 0.46, 0.87); P < 0.0167 |
BP, blood pressure; CHO, carbohydrate; RTEC, ready-to-eat breakfast cereal.
In the 2 cross-sectional studies analyzing data from NHANES, the consumption of RTEC at breakfast was associated with a 36% reduction in hypertension risk (114, 115, 173). The results from the 3 RCTs are less consistent and were all primarily focused on oats. One study with both oat- and wheat-based cereals reported no effect on blood pressure (175). Of the 2 others with oats, 1 found a reduction in the need for hypertensive medication (176), whereas the other found a hypotensive effect of foods with β-glucan (of which only 2 of the 3 daily servings were from breakfast cereals), but only in obese, hypertensive subjects (177). None of these studies examined the effect of breakfast cereals in normotensive subjects. The evidence base is therefore very limited, if suggestive, and this is reflected in the evidence summary in Table 11.
TABLE 11.
Body of evidence summary on breakfast cereals and hypertension1
| Evidence statement and components | Grade | Rating | Notes |
| Regular consumption of breakfast cereals may reduce the risk of hypertension | D | — | Body of evidence is weak and must be applied with caution |
| Evidence base | Satisfactory | 3 Level II studies (RCTs) (all positive quality) | |
| 1 Level III study (cohort) (positive quality) | |||
| 2 Level IV studies (cross-sectional studies) (all positive quality) | |||
| Consistency | Poor | 1 cohort and 2 cross-sectional studies suggest protective effect but 2 of 3 RCTs with oats show no effect | |
| Clinical impact | Good | ORs: 0.64–0.81 in cohort and cross-sectional studies | |
| Generalizability | Satisfactory | The largest cohort study and 1 of the RCTs are both in men only | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly | |
| Regular consumption of breakfast cereals is not associated with an increased risk of hypertension | C | — | Body of evidence provides some support for recommendation but care should be taken in its application |
| Evidence base | Satisfactory | 3 Level II studies (RCTs) (all positive quality) | |
| 1 Level III study (cohort) (positive quality) | |||
| 3 Level IV studies (cross-sectional studies) (all positive quality) | |||
| Consistency | Excellent | None show increased blood pressure or risk of hypertension | |
| Clinical impact | Poor | Nil effect | |
| Generalizability | Satisfactory | The largest cohort study and 1 of the RCTs are both in men only | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Digestive and gut health
Celiac disease.
There has been debate about the extent to which oats may be tolerated in a gluten-free diet because of their lower prolamine gliadin content compared with wheat, rye, and barley. Uncontaminated oats are consumed by >70% of patients with celiac disease in countries such as Sweden, Finland, and The Netherlands (178), and at least 1 randomized trial found that oats do not induce antibody responses in children with celiac disease (179). The Canadian Celiac Association notes that it is possible to produce oats without contamination from other grains and that in well-controlled individuals the incorporation of up to 50–70 g/d of pure oats may be possible (180).
One systematic review of 15 clinical studies in adults and children concluded that the majority of people with celiac disease can tolerate moderate amounts of pure oats, but that individuals should have both initial and long-term assessments by a health professional when introducing oats (181). A more recent systematic review identified 17 primary studies, of which 6 met inclusion criteria. None of the 6 studies found any significant differences in the serology between oat consumers and control groups, although 2 found significant differences in intraepithelial lymphocyte counts (182). The authors concluded that oats can be symptomatically tolerated by most patients but that long-term effects of a diet with oats remain unknown.
These conclusions were supported by a recent double-blind multicenter study in 8 pediatric clinics in Sweden with 93 patients on strict gluten-free diets, which showed that the addition of moderate amounts of oats (25–50 g/d) did not prevent clinical or small bowel mucosal healing or humoral immunologic downregulation in children (183).
Laxation and constipation.
The effect of dietary fiber on stool weight was estimated in a meta-analysis of >100 studies (184). Breakfast cereals provide 8–12% of the dietary fiber in adult diets in the United States, the United Kingdom, and Australia (64, 185, 186) and therefore have an important role in supporting healthy laxation, but clearly this varies depending on the type of breakfast cereal and its fiber content.
Several studies have shown that adding dietary fiber (via bran or other means) to breakfast cereals in institutional settings such as nursing homes can alleviate problems of constipation (187–190), but there have been few studies directly examining the association of breakfast cereal consumption with digestive problems generally. Five such studies were identified—4 randomized trials (1 reported in 2 separate articles) and 1 cross-sectional study—and are summarized in Table 12. The number of studies is small, but the consistent findings, supported by many other studies on dietary fiber in other forms, allows an evidence statement to be developed with confidence (Table 13).
TABLE 12.
Studies of breakfast cereals and laxation
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Odes et al. (274) | Neutral | 8 men and 12 women (mean age = 55 y) suffering chronic constipation; Israel | Double-blind crossover trial of 2 breakfast cereals for 2 wk | 50 g of high-fiber cereal made from oats, corn, wheat, and soy (12.5 g fiber/serving) | Bowel habits and laxative consumption recorded by subjects | The high-fiber cereal relieved constipation in all subjects and decreased stool hardness. All subjects in intervention group stopped taking laxatives. |
| Equicaloric placebo made from corn starch (2 g fiber/serving). | Compared with low-fiber placebo: | |||||
| Stool frequency/wk: 11.9 ± 4.1 vs. 9.5 ± 3.8; P < 0.05 | ||||||
| Stool hardness score: 1.4 ± 0.9 vs. 2.4 ± 0.7; P < 0.05. | ||||||
| “The high-fiber cereal tested here was able to produce relief from constipation within a relatively short period of time” (p984) | ||||||
| Turconi et al. (275), | Negative | 12 men (M) and 12 women (F), all healthy, aged 21–36 y; Italy | Crossover trial; subjects consumed 1 of 2 high-fiber breakfast cereals for 2 wk, increasing gradually from 15 (F) or 20 (M) g/d to 35 (F) and 40 (M) g/d in second week | 2 Kellogg’s cereals: | Bowel function questionnaire | Although total daily fiber intake increased compared with the normal diet, the increases were not significant because of reductions in fiber at other times of the day. For All-Bran (test vs. washout): |
| Turconi et al. (276) | Bran Flakes (13% fiber) | Men: 24.8 ± 3.9 vs. 15.7 ± 3.7 g fiber/d | ||||
| All-Bran (24% fiber) | Women: 21.1 ± 4.6 vs. 14.0 ± 3.4 g fiber/d | |||||
| 3-d diet diaries used to assess intakes | With Bran flakes/All-Bran, 83%/100% of women and 75%/83% of men reported improved bowel function (no statistical results); 6 subjects developed some flatulence and cramps | |||||
| 2-wk washout period between test cereals allowed normal diet | “Considerable improvements in bowel function were reported in virtually all of the subjects during the trial” (p229) | |||||
| Ouellet et al. (190) | Neutral | 81 male and female subjects (mean age = 67 y) undergoing orthopedic surgery; US | Randomized controlled trial; postoperatively the trial group received dietary wheat fiber supplementation as high-fiber cereals at breakfast | Wheat fiber trial: 20 g combination of All-Bran and natural wheat bran | Bowel status (stool number, size, consistency) rated from 1 (good) to 5 (poor) | Good bowel status trial vs. control OR = 4.95 (P < 0.001) |
| Control: 20 g crushed Special K | Use of laxatives and enemas; measured 8 d postoperatively | The intervention group also required fewer laxatives, suppositories, and enemas (P = 0.00) | ||||
| “Bowel function in participants who had wheat bran added to their diets was five times better than in the control group…. and decreases the likelihood of developing constipation” (p435) | ||||||
| Vuksan et al. (277) | Positive | 23 free-living healthy subjects (12 M, 11 F) aged 19–59 y; Canada | 5-phase randomized crossover trial with each subject acting his own control; each treatment for 21 d with 7-d washout in between | 4 cereals providing 25–20 g fiber: | Fecal weights | All study cereals significantly increased fecal bulk from 128 g/d with the control to the following: |
| Last week subjects provided all food and fecal samples were collected | AB (All-Bran) | Transit times (based on radio-opaque pellets) | AB 199 g, BBC 199 g, BBP 247 g, VFB 197 g (all P < 0.05) | |||
| BBC (Bran Buds with corn) | Bowel habits and symptom diaries | All cereals reduced median transit time from 32 h in control to the following: | ||||
| BBP (Bran Buds with psyllium) | AB, 28 h; BBC, 27 h; BBP, 25 h; VFB, 25 h (all P < 0.05) | |||||
| VFB (BBC with viscous fiber blend) | Stool frequency all increased (0.97 to 1.2/d) (P < 0.05) | |||||
| Control (low fiber; 1.3 g) | No significant changes in ease of movement, stool consistency, flatulence, abdominal pain, although bloating slightly greater with high-fiber cereals | |||||
| Lawton et al. (237) | Positive | 153 low-fiber consumers (<15 g/d) aged 18–50 y with BMI (in kg/m2) 18.5–30; UK | Within-subject pre-post design; 14 d usual diet followed by 14 d intervention | 4 different high-fiber cereals (mean 14% fiber). All consumed Bran Shreds (27%) and 1 of 6 others [Wheat Bran Flakes (BF), BF + Sultanas, Frosted Mini Wheats, Raisin Mini Wheats, Chocolate BF, Apple&Fig BF] | Digestive Wellbeing Questionnaire | In intervention periods there were significant (<0.0001) improvements in self-reported constipation, bloating, sluggishness, digestive discomfort, ease of defecation, and stool quantity. There were no changes in reported indigestion or pain in the digestive system. |
| Smith (230) | Neutral | 14,952 adults aged 16–98 y in the Bristol Stress and Health at Work Study; UK | Cross-sectional study | Breakfast cereal consumption self-rated on a 5-point scale from never to every day | Presence of symptoms: constipation, diarrhea, heartburn, gas, indigestion | 51% of sample reported no digestive problems. |
| Secondary analysis of survey data | In all the analyses there were significant main effects of breakfast cereal consumption and digestive problems; however, none of the interactions were significant. | |||||
| Symptom checklist for the last 14 d |
TABLE 13.
Body of evidence summary on breakfast cereals and digestive health1
| Evidence statement and components | Grade | Rating | Notes |
| Consumption of high-fiber wheat-based breakfast cereals helps prevent constipation and improves bowel function | A | — | Body of evidence can be trusted to guide practice |
| Evidence base | Good | 5 Level II studies (RCTs) (2 positive quality; 2 neutral, 1 negative) | |
| 1 Level IV study (cross-sectional) (all positive quality) | |||
| Consistency | Good | All clinical trials reported improvements in stool frequency, bulk, and transit time. One cross-sectional study found no relation with consumption, but this was with all types of breakfast cereals, not just high-fiber. | |
| Clinical impact | Good | Stool frequency increased on average by at least 25% | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Dental health
Three published studies examined the relation between breakfast cereal consumption and dental health in children and adolescents (Table 14). No studies in adults were found. In all but 1 of these studies (191) the authors reported the total sugar content of cereal products, which includes not only added sucrose but also sugars from fruit or milk ingredients.
TABLE 14.
Studies on breakfast cereal consumption and dental caries1
| Authors (reference) | Quality rating | Subjects and study location | Study design | Diet | Outcomes | Key results |
| Rowe et al. (278) | Neutral | 375 adolescent schoolchildren (mean age = 13 y); US | Prospective intervention study | 7 varieties of General Mills RTECs [4 presweetened: Trix, Cocoa Puffs, Frosty Os, and Corn Bursts (sugar content not defined)]. Children were free to eat whatever foods they liked. Consumption estimated by records of food supplied; 60% of cereals chosen were presweetened. | Incidence of DMFT measured at dental examinations at 0, 12, 24, and 36 mo | There was no association between DMFT scores in those who ate RTEC and those who did not. |
| For 3 y, students given free monthly samples of breakfast cereals along with toothbrushes and toothpaste | Incremental DMF surfaces of eaters vs. non-eaters: | |||||
| 5.20 ± 4.67 vs. 6.41 ± 5.62 (NS) | ||||||
| Glass and Fleisch (279) | Positive | 949 children aged 7–11 y; US | Prospective intervention study | 14 varieties of Kellogg’s RTECs (6 presweetened) | Incidence of DMFT measured at dental examinations at 0, 12, 24, and 36 mo | There were no significant associations between incidence of DMFT or restorative treatments with RTEC consumption overall or for presweetened RTEC specifically. |
| For 2 y, RTEC available freely and mothers asked to encourage children to eat at least 1 serving daily | Consumption estimated from records of food supplied and participants classified as high, medium, or low users; 46% of cereals consumed were presweetened (but no definition of this category) | Incremental DMFT of high vs. low RTEC consumers: | ||||
| Presweetened RTEC: 4.01 ± 4.04 vs. 4.04 ± 5.02 (NS) | ||||||
| Regular RTEC: 3.53 ± 3.93 vs. 4.24 ± 4.87 (NS) | ||||||
| Gibson (191) | Positive | 1450 children aged 1.5–4.5 y in the 1995 UK National Diet and Health Survey; UK | Cross-sectional study | 4-d weighed diet record completed by main caregiver. Children classified into tertiles of breakfast cereal (BC) consumption and NMES | % of children with caries based on dental examination | Caries prevalence was unrelated to consumption of BC or NMES in cereals, although there was a trend to lower incidence in the higher consumers. |
| High vs. low BC consumption: 16 ± 2 vs. 18 ± 2 (NS) | ||||||
| High vs. low NMES in BC: 14 ± 2 vs. 18 ± 2 (NS) |
DMF, decayed missing or filled; DMFT, decayed, missing, or filled teeth; NMES, nonmilk extrinsic sugars; RTEC, ready-to-eat cereal.
One study examined the cariogenic potential of PS breakfast cereals by using 3 methods to measure the in vitro ability of a cariogenic strain of Streptococcus mutans to produce acid from fermentable carbohydrate after the consumption of breakfast cereal by volunteers either with or without milk (192). The 12 cereals tested ranged in total sugar content from 3% to 45.9%, with 9 cereals containing >25% sugar. A positive correlation was found between total sugar content and the production of acid, and the 6 cereals with the greatest pH change had a total sugar content of ≥42%. The cereals judged the least cariogenic (with the smallest change in pH, concentration of calcium release from hydroxyapatite, and decreased salivary retention time) all had total sugar contents of <10%.
However, because of the complex interactions between dietary constituents and teeth in the development of dental caries, it is not possible to give absolute determinations of cariogenicity (193). Most breakfast cereals are consumed with milk, which acts as a buffer in pH lowering, and the calcium encourages enamel remineralization (191). All 3 studies in Table 14 showed no relation between breakfast cereal consumption, although, interestingly, all showed lower (but nonsignificant) caries incidence among cereal consumers. This might be related to the known role of breakfast cereal consumption in promoting high milk intakes. Table 15 sets out an evidence summary based on the 3 studies.
TABLE 15.
Body of evidence summary on breakfast cereals and dental caries
| Evidence statement and components | Grade | Rating | Notes |
| Consumption of breakfast cereals by children is not associated with increased risk of dental caries | B | — | Body of evidence can be trusted to guide practice in most situations |
| Evidence base | Satisfactory | 2 Level II studies (RCTs1) (1 positive quality, 1 neutral) | |
| 1 Level IV study (cross-sectional) (positive quality) | |||
| Consistency | Excellent | All studies showed no significant association (if anything, a trend to lower caries incidence with cereal consumption) | |
| Clinical impact | Poor | No effect | |
| Generalizability | Excellent | Populations studied in the body of evidence cover a wide range of ages and countries of residence | |
| Applicability | Excellent | Directly applicable in populations in whom breakfast cereals are consumed regularly |
RCT, randomized controlled trial.
Other relations
All-cause mortality.
Two cohort studies examined the relation of breakfast cereal consumption to overall mortality. In 1984, the 21-y follow-up of 27,530 adults in the Seventh-day Adventist study calculated the adjusted OR of all-cause mortality when the most-frequent and the least-frequent breakfast cereal consumers were compared as 0.84 (95% CI: 0.73, 0.97; P < 0.01) (194).
In the U.S. Physicians’ Health Study, over a mean follow-up of 5.5 y, total mortality was inversely associated with whole-grain breakfast cereal intake (OR: 0.83; 95% CI: 0.73, 0.94; P < 0.001) but not with refined-grain breakfast cereal intake (OR: 1.09; 95% CI: 0.95, 1.25; P = 0.07) (195). The OR for total breakfast cereals was also not significantly different from unity (OR: 0.92; 95% CI: 0.82, 1.02; P = 0.07). It is striking that the results from the Adventist study were very similar to those for whole-grain cereals in the Physicians’ Health Study, which may reflect a likely preference for whole-grain cereals in the former group.
Cancer.
There have been no reviews specifically about the impact of breakfast cereal consumption on cancer risk, although there are a number of reviews and meta-analyses on the relation between dietary fiber, cereal fiber, and cereal foods generally with risk of cancer (196–199).
There has been concern about the potential carcinogenic risks of acrylamide in cereals since the International Agency for Research on Cancer designated it a “probable human carcinogen” in 1994. In most Western countries, breakfast cereals contribute only 2–10% of total acrylamide intake (200–202). A recent study in participants of the Health Professionals Follow-Up Study estimated that cold breakfast cereals contributed 13% of total acrylamide intakes in the United States but there was no association between acrylamide intake and risk of prostate cancer (203). Other prospective studies of breast and colon cancer also found no significant associations with acrylamide intake (204–206).
It has been suggested that whole grains are a major source of vitamins, minerals, and phytochemicals, which have anticancer properties (207). Dietary fiber could also decrease colorectal cancer risk by increasing stool bulk, diluting fecal carcinogens, and decreasing transit time (208). In addition, bacterial fermentation of fiber results in the production of short-chain FAs, which may have protective effects (209).
A total of 13 studies examined the effect of breakfast cereals with a range of cancer types (colorectal, lung, endometrial, breast, prostate, and pancreas) in 5 cohort and 5 case-control studies and 3 RCTs (210–222). It should be noted that some of these studies were with wheat bran– or bran-based cereals only. In none of the studies reporting all cancer or lung, colorectal, breast, or endometrial cancer outcomes were breakfast cereal intakes related to cancer risk. One study identified an increased risk of pancreatic cancer (for cooked but not cold cereal) (218) and another for prostate cancer from whole-grain but not refined-grain breakfast cereals (216), but there are no plausible mechanisms that could account for these findings and they would need to be confirmed before any firm conclusions can be made.
Mental health.
Feelings of well-being and positive mood state are increasingly recognized as important components of good health, and there has been a growth in studies looking at the relation of nutrition with these outcomes (223). Many studies in the literature have focused on the role of the breakfast meal, rather than breakfast cereals in particular. This search identified 7 cross-sectional studies (224–230) and 9 intervention trials (229, 231–238) that examined the effects of a breakfast cereal on mood, stress, anxiety, and depression. All of the cross-sectional studies suggested that regular breakfast cereal consumers have lower levels of mental health problems, including less stress, anxiety, and depression. However, with studies of this type there is always the possibility of reverse causality: that stress and mental health problems lead to changes in diet. Therefore, intervention studies are particularly important to understand the potential relation.
In 3 of the intervention studies (229, 231, 235), breakfast cereal consumption was compared with no food for breakfast, so it is not possible to draw any conclusions about the effect of the type of breakfast food—the effects are likely to be a general breakfast (or carbohydrate) consumption effect. Two of the other studies used high-fiber, wheat-based cereals in the intervention, so the applicability to breakfast cereals in general is also uncertain. Authors of 1 study comparing a breakfast cereal with a muffin breakfast suggested that some of the differences were due to perceptions of different energy content of the breakfasts. That study also included toasted bread along with cereal in the “breakfast cereal” intervention. There have been no studies in subjects selected because of high levels of anxiety or depression.
Given the diverse interventions and outcome measures used in these studies, much more research is needed to understand the relations between well-being and breakfast cereals.
Cognitive performance.
One review of 22 studies examining the association of breakfast consumption and academic performance in children and adolescents concluded that breakfast consumption may improve cognitive function related to memory, test grades, and school attendance (17). The effects could come from alleviating hunger, or they might be attributable to enhanced blood glucose (239).
A more recent review of 45 articles concluded that breakfast consumption is more beneficial than skipping breakfast, but that this effect is mainly apparent in children whose nutritional status is compromised (240). The authors noted, “there is a lack of research comparing breakfast type, precluding recommendations for the size and composition of an optimal breakfast for children’s cognitive function.”
Most studies have focused on the cognitive functioning of children. There is 1 prospective study of RTEC consumption among 3831 men and women aged >65 y in Utah who were followed for 11 y and had their cognitive function assessed by the Modified Mini-Mental State Examination (241). In multivariate models, more frequent RTEC consumption was not associated with cognitive benefit, and daily RTEC consumers had patterns of cognitive decline over 11 y similar to infrequent consumers.
Seven RCTs looked at the effect of breakfast cereals on different measures of mental performance: 1 in adults (242) and the others in children and adolescents (229, 243–247). The adult study found the best alertness after an All-Bran meal, which is known to have a low GI. Four of the studies in children compared high- and low-GI breakfast meals (243–246). One study (245) reported superior performance in the high-GI breakfast cereal group, but the other 3 reported cognitive enhancements with the low-GI breakfast cereal option. None of these studies independently measured the GI values of their test meals; all used calculated values. In 1 case other foods (bread and apple juice) were added to the breakfast cereal meal. None of the studies seem to have considered other possible explanations for the performance differences aside from the glycemic effect of the foods.
It is difficult to summarize results from these studies because a variety of different outcome measures were used and in many cases only a small number of the measured outcomes were significant. It appears that the consumption of low-GI breakfast cereals may be beneficial for some aspects of the cognitive functioning of children and adolescents, but more research in this area is needed.
Physical activity and performance.
One of the explanations for the observed association of RTEC consumption with lower BMI is the association with lifestyle habits such as greater physical activity and reduced television watching (248). One prospective cohort study in the United States in 2379 girls compared the cumulative percentage of days that each girl consumed breakfast cereal in childhood with results from 30-d physical activity diaries. Girls who ate cereal more often were more likely to exhibit high levels of physical activity and less television viewing (P < 0.05) with no difference according to the amount of fiber or total sugars in the breakfast cereals consumed (92, 110). There was no association between physical activity and number of days eating noncereal breakfasts (39).
Another cross-sectional study in Greece in schoolchildren aged 12–17 y reported a similar relation. Multiple regression analysis revealed that the consumption of breakfast cereals was associated with a higher likelihood of participation in more physical activity (97). However, it is uncertain whether there is anything causal in this relationship: it is very possible that families who promote cereal-eating also encourage healthier lifestyles in general (249).
A few clinical studies used breakfast cereals to examine the effect of foods provided before exercise performance (250–253). All of these studies were in young active people and the performance testing regimes were prolonged and strenuous, so their relevance for the normal population in everyday activities is uncertain. Only 2 of these studies compared >1 breakfast cereal, and the only significant difference was in the trial that compared rolled oats with puffed rice (253). The authors assumed that this difference was due to the GI of the products, but there have been no studies comparing foods of similar nutritional content with different GI values.
Given the paucity of relevant trials, it is not possible to develop evidence summaries in relation to breakfast cereal consumption and physical activity or exercise performance without further research.
Other effects.
There is some limited research on breakfast cereals and probiotic effects (160, 254, 255), immune function (256, 257), exercise recovery (258), and anemia (259), but the information is too preliminary to draw any firm conclusions.
Discussion
This review developed 21 statements on the evidence for the health benefits of breakfast cereal consumption, including 2 Grade A, 5 Grade B, 11 Grade C, and 3 Grade D statements. Evidence levels A–C have been used to support the development of dietary guidelines previously (260). Some of the statements related to obesity, CVD, diabetes, and laxation are only for whole-grain or high-fiber breakfast cereals, but many are for the whole category of breakfast cereals. It should be noted that when the evidence is only derived from cohort or cross-sectional observational studies the statements refer to an association with breakfast cereal consumption, and do not necessarily imply a causal relation. Only when there is good evidence from intervention trials do the statements use more direct language (e.g., “help lower” or “improve”).
Regular breakfast cereal consumers usually have higher daily milk intakes and are more likely to meet their recommended nutrient needs: in particular, they have better intakes of dietary fiber, B-vitamins, folate, calcium, iron, magnesium, and zinc. Much of this effect is likely to be due to the fortification of many breakfast cereals. Breakfast cereal consumption is also associated with diets that are lower in fat but not with increased daily intakes of sodium or energy.
A large number of cross-sectional studies all reported that breakfast cereal consumption is associated with lower measures of overweight or obesity. Indeed, the consistency of this finding in studies from many different countries in different age groups suggests that there is no need for additional studies of this type to be undertaken.
It is possible that a breakfast including breakfast cereal, especially one that is higher in fiber, may provide better satiety and prevent overconsumption later in the day. However, although there is evidence to support this hypothetical mode of action, not all studies showed that total daily energy intakes are lower when breakfast cereal is consumed; indeed, several studies showed just the opposite (24, 27, 38, 41, 59, 66, 261). This higher total energy intake by breakfast cereal consumers may be because those who are overweight were trying to lose weight by skipping breakfast, but the possible causal relations are unclear and may not simply be due to reduced total energy intake.
Another possible mechanism could be that breakfast cereal consumption increases energy expenditure via better insulin sensitivity in the morning, but this is unlikely to be a food-specific effect. On the other hand, breakfast cereal consumption may simply be a marker for an overall healthy lifestyle and merely indicate eating and physical activity patterns that are more favorable overall for weight maintenance. Thus, there is a need for better-controlled cohort and intervention trials to understand this relation. There is insufficient evidence to describe the best types of breakfast cereals to prevent weight gain, although there are suggestions of a greater protective effect of higher-fiber and oat cereals in some (but not all) studies.
Studies that compared the effects of consumption of PS or non-PS breakfast cereals mostly found no significant differences in daily nutrient or energy intake, although the consumption of total sugars may be increased, and that consumption of PS breakfast cereals does not increase the risk of overweight or obesity in children.
There is an emerging evidence base suggesting that breakfast cereal consumption may be associated with feelings of better mental well-being, improved cognitive functioning, and reduced risk of hypertension, but better trials are required before any firm conclusions can be drawn.
There are several limitations of this review. First, it was undertaken by a single author, whereas ideally at least 2 people would independently assess the studies. However, the reviewer was experienced in this task, having led the evidence reviews that supported the last review of the Australian dietary guidelines (262). Second, almost all of the studies in the literature on the nutritional impacts of breakfast cereal consumption are cross-sectional in design (mostly of RTEC only) with very few RCTs, which is a weakness in the evidence base overall. Furthermore, the mechanisms for many of the health effects summarized in this review are not always clear. In some cases, the fortification profile from added vitamins and minerals may be a factor, but the natural nutrient content of cereals, including inherent bioactive substances such as antioxidants and phytoestrogens, as well as the significant contribution of breakfast cereals to whole-grain and dietary fiber intakes, are also likely to contribute.
In summary, breakfast cereals are relatively inexpensive, nutrient-dense, and convenient foods, which can be recommended to form part of a healthy balanced diet. Their regular consumption can help ensure an adequate nutrient intake and may assist in reducing the risks of being overweight or of developing CVD or diabetes.
Acknowledgments
The sole author had responsibility for all parts of the manuscript.
Footnotes
Abbreviations used: CVD, cardiovascular disease; GI, glycemic index; PS, presweetened; RCT, randomized controlled trial; RTEC, ready-to-eat cereal; T2D, type 2 diabetes; tHcy, total homocysteine; %E, percentage of energy.
References
- 1.Toma R, Curtis D. Ready-to-eat cereals: role in a balanced diet. Cereal Foods World. 1989;34:387–90 [Google Scholar]
- 2.McKevith B. Nutritional aspects of cereals. Nutr Bull 2004;29:111–42 [Google Scholar]
- 3.McKevith B, Jarzebowska A. The role of breakfast cereals in the UK diet: headline results from the National Diet and Nutrition Survey (NDNS) year 1. Nutr Bull 2010;35:314–9 [Google Scholar]
- 4.National Health and Medical Research Council. Australian dietary guidelines. Canberra (Australia): National Health and Medical Research Council; 2013[cited 2013 Feb 18]. Available from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/n55_australian_dietary_guidelines.pdf
- 5.Miller HE, Rigelhof F, Marquart L, Prakash A, Kanter M. Antioxidant content of whole grain breakfast cereals, fruits and vegetables. J Am Coll Nutr 2000;19:312S–9S [DOI] [PubMed] [Google Scholar]
- 6.Baublis AJ, Lu C, Clydesdale F, Decker E. Potential of wheat-based breakfast cereals as a source of dietary antioxidants. J Am Coll Nutr 2000;19:308S–11S [DOI] [PubMed] [Google Scholar]
- 7.Ryan L, Thondre P, Henry C. Oat-based breakfast cereals are a rich source of polyphenols and high in antioxidant potential. J Food Compos Anal 2011;24:929–34 [Google Scholar]
- 8.Kuhnle GG, Dell'Aquila C, Aspinall S, Mulligan A, Bingham S. Phytoestrogen content of cereals and cereal-based foods consumed in the UK. Nutr Cancer 2009;61:302–9 [DOI] [PubMed] [Google Scholar]
- 9.Devlin NF, McNulty B, Gibney M, Thielecke F, Smith H, Nugent A. Whole grain intakes in the diets of Irish children and teenagers. Br J Nutr 2013;110:354–62 [DOI] [PubMed] [Google Scholar]
- 10.Williamson C. Breakfast cereals—why all the bad press? Nutr Bull 2010;35:30–3 [Google Scholar]
- 11.American Dietetic Association. Evidence analysis manual. Chicago: ADA Scientific Affairs and Research; 2008. Available from: https://www.adaevidencelibrary.com/vault/editor/File/Evidence_Analysis_Manual_January_2008.pdf (cited 2014 August 8)
- 12.National Health and Medical Research Council. How to use the evidence: assessment and application of scientific evidence. Canberra (Australia): AusInfo; 2000. Available from: http://www.nhmrc.gov.au/publications/synopses/cp69syn.htm. (Cited 2014 August 8)
- 13. National Health and Medical Research Council. Additional levels of evidence and grades for recommendations for developers of guidelines. Stage 2 consultation (early 2008 - end June 2009). Canberra (Australia): National Health and Medical Research Council; 2009 [cited 2013 Nov 21]. Available from: http://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/stage_2_consultation_levels_and_grades.pdf.
- 14.Allman-Farinelli M, Byron A, Collins C, Gifford J, Williams P. Challenges and lessons from systematic reviews for the Ausralian dietary guidelines. Aust J Prim Health 2014;20:236–40 [DOI] [PubMed] [Google Scholar]
- 15.Hill G. The impact of breakfast especially ready-to-eat breakfast cereals on nutrient intake and health of children. Nutr Res 1995;15:595–613 [Google Scholar]
- 16.Ruxton CH, Kirk T. Breakfast: a review of associations with measures of dietary intake, physiology and biochemistry. Br J Nutr 1997;78:199–213 [DOI] [PubMed] [Google Scholar]
- 17.Rampersaud GC, Pereira M, Girard B, Adams J, Metzl J. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005;105:743–60 [DOI] [PubMed] [Google Scholar]
- 18.Mullan B, Singh M. A systematic review of the quality, content, and context of breakfast consumption. Nutr Food Sci 2010;40:81–114 [Google Scholar]
- 19.Morgan KJ, Zabik M, Leveille G. The role of breakfast in nutrient intake of 5- to 12-year old children. Am J Clin Nutr 1981;34:1418–27 [DOI] [PubMed] [Google Scholar]
- 20.Morgan K, Zabik M, Stampley G. Breakfast consumption patterns of US children and adolescents. Nutr Res 1986;6:635–46 [Google Scholar]
- 21.Albertson A, Tobelman R. Impact of ready-to-eat cereal consumption on the diets of children 7–12 years old. Cereal Foods World. 1993;38:428–31 [Google Scholar]
- 22.Crawley H. The role of breakfast cereals in the diets of 16–17-year-old teenagers in Britain. J Hum Nutr Diet 1993;6:205–16 [Google Scholar]
- 23.Nicklas T, Myers L, Berenson G. Impact of ready-to-eat cereal consumption on total dietary intake of children: the Bogalusa Heart Study. J Am Diet Assoc 1994;94:316–8 [DOI] [PubMed] [Google Scholar]
- 24.Gibson SA, O'Sullivan K. Breakfast cereal consumption patterns and nutrient intakes of British schoolchildren. J R Soc Health 1995;115:366–70 [DOI] [PubMed] [Google Scholar]
- 25.Sampson AE, Dixit S, Meyers A, Houser R. The nutritional impact of breakfast consumption on the diets of African-American elementary school children. J Natl Med Assoc 1995;87:195–202 [PMC free article] [PubMed] [Google Scholar]
- 26.Ruxton CH, O'Sullivan K, Kirk T, Belton N. The contribution of breakfasts to the diets of a sample of 136 primary-school children in Edinburgh. Br J Nutr 1996;75:419–31 [DOI] [PubMed] [Google Scholar]
- 27.McNulty H, Eaton-Evans J, Cran G, Woulahan G, Boreham C, Savage J, Fletcher R, Strain J. Nutrient intakes and impact of fortified breakfast cereals in schoolchildren. Arch Dis Child 1996;75:474–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ortega RM, Requejo A, Redondo R, Lopez-Sobaler A, Andres P, Ortega A, Gaspar M, Quintas E, Navia B. Influence of the intake of fortified breakfast cereals on the dietary habits and nutritional status of Spanish schoolchildren. Ann Nutr Metab 1996;40:146–56 [DOI] [PubMed] [Google Scholar]
- 29.Nicklas TA, O'Neil C, Berenson G. Nutrient contribution of breakfast, secular trends, and the role of ready-to-eat cereals: a review of data from the Bogalusa Heart Study. Am J Clin Nutr 1998;67 Suppl:757S–63S [DOI] [PubMed] [Google Scholar]
- 30.Gibson SA. Iron intake and iron status of preschool children: associations with breakfast cereals, vitamin C and meat. Public Health Nutr 1999;2:521–8 [PubMed] [Google Scholar]
- 31.Preziosi P, Galan P, Deheeger M, Yacoub N, Drenowski A, Hercberg S. Breakfast type, daily nutrient intakes and vitamin and mineral status of French children, adolescents and adults. J Am Coll Nutr 1999;18:171–8 [DOI] [PubMed] [Google Scholar]
- 32.Gibson S. Micronutrient intakes, micronutrient status and lipid profiles among young people consuming different amounts of breakfast cereals: further analysis of data from the National Diet and Nutrition Survey of Young People aged 4 to 18 years. Public Health Nutr 2003;6:815–20 [DOI] [PubMed] [Google Scholar]
- 33.Albertson AM, Anderson GH, Crockett SJ, Goebel MT, Albertson AM, Anderson GH, Crockett SJ, Goebel MT. Ready-to-eat cereal consumption: its relationship with BMI and nutrient intake of children aged 4 to 12 years. J Am Diet Assoc 2003;103:1613–9 [DOI] [PubMed] [Google Scholar]
- 34.Thorsdottir I, Gunnarsson BS, Atladottir H, Michaelsen KF, Palsson G. Iron status at 12 months of age—effects of body size, growth and diet in a population with high birth weight. Eur J Clin Nutr 2003;57:505–13 [DOI] [PubMed] [Google Scholar]
- 35.Kafatos A, Linardakis M, Bertsias GIM, Fletcher R, Bervanaki F. Consumption of ready-to-eat cereals in relation to health and diet indicators among school adolescents in Crete, Greece. Ann Nutr Metab 2005;49:165–72 [DOI] [PubMed] [Google Scholar]
- 36.Barton BA, Eldridge A, Thompson D, Affenito S, Striegel-Moore R, Franko D, Albertson A, Crockett S. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc 2005;105:1383–9 [DOI] [PubMed] [Google Scholar]
- 37.Williams P. Breakfast and the diets of Australian children and adolescents: an analysis of data from the 1995 National Nutrition Survey. Int J Food Sci Nutr 2007;58:201–16 [DOI] [PubMed] [Google Scholar]
- 38.Williams BM, O'Neil C, Keast D, Cho S, Nicklas T. Are breakfast consumption patterns associated with weight status and nutrient adequacy in African-American children? Public Health Nutr 2009;12:489–96 [DOI] [PubMed] [Google Scholar]
- 39.Albertson AM, Thompson D, Franko D, Kleinman R, Barton B, Crockett S. Consumption of breakfast cereal is associated with positive health outcomes: evidence from the National Heart, Lung, and Blood Institute Growth and Health Study. Nutr Res 2008;28:744–52 [DOI] [PubMed] [Google Scholar]
- 40.Albertson AM, Affenito S, Bauserman R, Holschuh N, Eldridge A, Barton B. The relationship of ready-to-eat cereal consumption to nutrient intake, blood lipids, and body mass index of children as they age through adolescence. J Am Diet Assoc 2009;109:1557–65 [DOI] [PubMed] [Google Scholar]
- 41.Deshmukh-Taskar PR, Nicklas T, O'Neil C, Keast D, Radliffe J, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999–2006. J Am Diet Assoc 2010;110:869–78 [DOI] [PubMed] [Google Scholar]
- 42.Albertson AM, Thompson D, Franko D, Holschuh N. Weight indicators and nutrient intake in children and adolescents do not vary by sugar content in ready-to-eat cereal: results from the National Health and Nutrition Examination Survey 2001–2006. Nutr Res 2011;31:229–36 [DOI] [PubMed] [Google Scholar]
- 43.O'Neil C, Zanovec M, Nicklas T, Cho S. Presweetened and nonpresweetened ready-to-eat cereals at breakfast are associated with improved nutrient intake but not with increased body weight in children and adolescents: NHANES 1999–2001. Am J Lifestyle Med. 2012;6:63–74 [Google Scholar]
- 44.Grieger JA, Cobiac L. Comparison of dietary intakes according to breakfast choice in Australian boys. Eur J Clin Nutr 2012;66:667–72 [DOI] [PubMed] [Google Scholar]
- 45.Balvin Frantzen L, Trevino R, Echon R, Garcia-Dominic O, DeMarco N. Association between frequency of ready-to-eat cereal consumption, nutrient intakes, and body mass index in fourth- to sixth-grade low-income minority children. J Acad Nutr Diet. 2013;113:511–9 [DOI] [PubMed] [Google Scholar]
- 46.Affenito SG, Thompson D, Dorazio A, Albertson A, Loew A, Holschuh N. Ready-to-eat cereal consumption and the school breakfast program: the relationship to nutrient intake and weight. J Sch Health 2013;83:28–35 [DOI] [PubMed] [Google Scholar]
- 47.Grieger J, Kim S, Cobiac L. Where do Australian children get their dietary fibre? A focus on breakfast food choices. Nutr Diet. 2013;70:132–8 [Google Scholar]
- 48.Albertson A, Franko D, Thompson D, Tuttle C, Holschuh N. Ready-to-eat cereal intake is associated with an improved nutrient intake profile among food insecure children in the United States. J Hunger Environ Nutr 2013;8:200–20 [Google Scholar]
- 49.Morgan KJ, Zabik M. The influence of ready-to-eat cereal consumption at breakfast on nutrient intakes of individuals 62 years and older. J Am Coll Nutr 1984;3:27–44 [DOI] [PubMed] [Google Scholar]
- 50.Zabik M. Impact of ready-to-eat cereal consumption on nutrient intake. Cereal Foods World. 1987;32:234–9 [Google Scholar]
- 51.Syrette J, Baghurst K, Record S. Breakfast cereals—patterns of consumption and nutritional value of regular usage. Food Aust 1990;42:568–73 [Google Scholar]
- 52.Emmett P, Symes C, Heaton K. The contribution of breakfast cereals to non-starch polysaccharide intakes in English men and women. J Hum Nutr Diet 1993;6:217–22 [PubMed] [Google Scholar]
- 53.McNulty H, Eaton-Evans J, Woulahan G, Strain J. The contribution of breakfast to daily micronutrient intakes of adults in Great Britain. Proc Nutr Soc 1994;53:251A7972139 [Google Scholar]
- 54.Schmidt T, Carden-Robinson J, North B, Nicklas T. Impact of breakfast consumption and RTE cereals on nutritional adequacy of the diets of young adults in Bogalusa, LA: ethnic and gender contrast. J Am Diet Assoc 1998;98 Suppl:A68. [DOI] [PubMed] [Google Scholar]
- 55.Bertrais S, Luque M, Presiosi P, Fieux B, de Flot M, Hercberg S. Contributions of ready-to-eat cereals to nutrition intakes in French adults and relations to corpulence. Ann Nutr Metab 2000;44:249–55 [DOI] [PubMed] [Google Scholar]
- 56.van den Boom A, Serra-Majem L, Ribas L, Ngo J, Perez-Rodrigo C, Aranceta J, Fletcher R. The contribution of ready-to-eat cereals to daily nutrient intake and breakfast quality in a Mediterranean setting. J Am Coll Nutr 2006;25:135–43 [DOI] [PubMed] [Google Scholar]
- 57.Galvin MA, Kiely M, Flynn A. Impact of ready-to-eat breakfast cereal (RTEBC) consumption on adequacy of micronutrient intakes and compliance with dietary recommendations in Irish adults. Public Health Nutr 2003;6:351–63 [DOI] [PubMed] [Google Scholar]
- 58.Mattisson I, Wirfalt E, Andren C, Gullberg B, Berglund G. Dietary fat intake—food sources and dietary correlates in the Malmo Diet and Cancer cohort. Public Health Nutr 2003;6:559–69 [DOI] [PubMed] [Google Scholar]
- 59.Cho S, Dietrich M, Brown C, Clark C, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003;22:296–302 [DOI] [PubMed] [Google Scholar]
- 60.Cho S, Morris D, Clark C, Steinberg S, Block G. Effect of ready-to-eat cereal consumption on serum total homocysteine concentrations and folate status. Cereal Foods World. 2004;49:23–7 [Google Scholar]
- 61.Williams P. Breakfast and the diets of adult Australian adults: an analysis of data from the 1995 National Nutrition Survey. Int J Food Sci Nutr 2005;56:65–79 [DOI] [PubMed] [Google Scholar]
- 62.Song WO, Chun O, Kerver J, Cho S, Chung C, Chung S-J. Ready-to-eat breakfast cereal consumption enhances milk and calcium intake in the US population. J Am Diet Assoc 2006;106:1783–9 [DOI] [PubMed] [Google Scholar]
- 63.Deshmukh-Taskar PR, Radliffe J, Liu Y, Nicklas T. Do breakfast skipping and breakfast type affect energy intake, nutrient intake, nutrient adequacy, and diet quality in young adults? NHANES 1999–2002. J Am Coll Nutr 2010a;29:407–18 [DOI] [PubMed] [Google Scholar]
- 64.Gibson S, Gunn P. What's for breakfast? Nutritional implications of breakfast habits: insights from the NDNS dietary records. Nutr Bull 2011;36:78–86 [Google Scholar]
- 65.Holmes BA, Kaffa N, Campbell K, Sanders T. The contribution of breakfast cereals to the nutritional intake of the materially deprived UK population. Eur J Clin Nutr 2012;66:10–7 [DOI] [PubMed] [Google Scholar]
- 66.Albertson AM, Wold A, Joshi N. Ready-to-eat cereal consumption patterns: the relationship to nutrient intake, whole grain intake, and body mass index in an older American population. J Aging Res 2012;631310. doi: 10.1155/2012/631310. Epub 2012 Oct 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barr SI, DiFrancesco L, Fulgoni V., III Consumption of breakfast and the type of breakfast consumed are positively associated with nutrient intakes and adequacy of Canadian adults. J Nutr 2013;143:86–92 [DOI] [PubMed] [Google Scholar]
- 68.Albertson A, Affenito S, Cupl J, Buklis P, Johshi N. The association between ready-to-eat cereal consumption, nutrient intakes of the Canadian population 12 years and older and body weight measures: results from a nationally representative Canadian population. J Food Res 2013;2:11–21 [Google Scholar]
- 69.Sebastian R, Goldman J, Wilkinson Enns C, LaComb R. Fluid milk consumption in the United States: What We Eat in America, NHANES 2005–2006. Food Surveys Research Group Dietary Data Brief No. 3. USDA; 2010 [cited 2014 Feb 6]. Available from: http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/DBrief/3_milk_consumption_0506.pdf.
- 70.Fayet F, Ridges L, Wright J, Petocz P. Australian children who drink milk (plain or flavored) have higher milk and micronutrient intakes but similar body mass index to whose who do not drink milk. Nutr Res 2013;33:95–102 [DOI] [PubMed] [Google Scholar]
- 71.Drewnowski A, Rehm C. Sodium intakes of US children and adults from foods and beverages by location of origin and by specific food source. Nutrients 2013;5:1840–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Australian Bureau of Statistics. Australian Health Survey: nutrition first results—foods and nutrients, 2011–2012. Canberra (Australia): Australian Bureau of Statistics; 2014 [cited 2014 Jun 16]. Available from: http://www.abs.gov.au/australianhealthsurvey
- 73.McNeill G, Vyvyan J, Peace H, McKie L, Seymour G, Hendry J, MacPherson I. Predictors of micronutrient status in men and women over 75 years old living in the community. Br J Nutr 2002;88:555–61 [DOI] [PubMed] [Google Scholar]
- 74.Ortega RM, Lopez-Plaza B, Andres P, Rodriguez-Rodriguez E, Aparicio A, Bermejo L. Increasing consumption of breakfast cereal improves thiamine status in overweight/obese women following a hypocaloric diet. Int J Food Sci Nutr 2009;60:69–79 [DOI] [PubMed] [Google Scholar]
- 75.Monteagudo C, Palacin-Arce A, del Mar Bibiloni M, Pons A, Tur J, Olea-Serrano F, Mariscal-Arcas M. Proposal for a breakfast quality index (BQI) for children and adolescents. Public Health Nutr 2013;16:639–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Frary CD, Johnson R, Wang M. Children and adolescents’ choices of foods and beverages high in added sugars are associated with intakes of key nutrients and food groups. J Adolesc Health 2004;34:56–63 [DOI] [PubMed] [Google Scholar]
- 77.Kirk TR, Burskill S, Cursiter M. Dietary fat reduction achieved by increasing consumption of a starch food—an intervention study. Eur J Clin Nutr 1997;51:455–61 [DOI] [PubMed] [Google Scholar]
- 78.Thane CW, Jones AR, Stephen AM, Seal CJ, Jebb SA. Whole-grain intake of British young people aged 4–18 years. Br J Nutr 2005;94:825–31 [DOI] [PubMed] [Google Scholar]
- 79.Thane CW, Jones AR, Stephen AM, Seal CJ, Jebb SA. Comparative whole-grain intake of British adults in 1986–7 and 2000–1. Br J Nutr 2007;97:987–92 [DOI] [PubMed] [Google Scholar]
- 80.Powers HJ. Riboflavin (vitamin B-2) and health. Am J Clin Nutr 2003;77:1352–60 [DOI] [PubMed] [Google Scholar]
- 81.Fayet Moore F, Ridges L, Sritharan N, Petocz P. Sugar content of breakfast cereals: does it matter? Proc Nutr Soc Aust. 2012;36:67 [Google Scholar]
- 82.Shrapnel B. Amount of sugar in Australian breakfast cereals is not associated with energy density or glycaemic index: results of a systematic survey. Nutr Diet. 2013;70:236–40 [Google Scholar]
- 83.Harris JL, Schwartz M, Ustjanauskas A, Ohri-Vachaspati P, Brownell K. Effects of serving high-sugar cereals on children's breakfast-eating behavior. Pediatrics 2011;127:71–6 [DOI] [PubMed] [Google Scholar]
- 84.de la Hunty A, Ashwell M. Are people who regularly eat breakfast cereals slimmer than those who don't? A systematic review of the evidence. Nutr Bull 2007;32:118–28 [Google Scholar]
- 85.Rosado JL, Arellano M, Montemayor K, Garcia O, MDC Caamano An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: a randomized controlled trial. Nutr J 2008;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Maki KC, Beiseigel J, Jonnalagadda S, Gugger C, Reeves M, Farmer M, Kaden V, Rains T. Whole-grain ready-to-eat oat cereal, as part of a dietary program for weight loss, reduces low-density lipoprotein cholesterol in adults with overweight and obesity more than a dietary program including low-fiber foods. J Am Diet Assoc 2010;110:205–14 [DOI] [PubMed] [Google Scholar]
- 87.Mattes RD. Ready-to-eat cereal used as a meal replacement promotes weight loss in humans. J Am Coll Nutr 2002;21:570–7 [DOI] [PubMed] [Google Scholar]
- 88.Vander Wal JS, McBurney M, Cho S, Dhurandhar N. Ready-to-eat cereal products as meal replacements for weight loss. Int J Food Sci Nutr 2007;58:331–40 [DOI] [PubMed] [Google Scholar]
- 89.Waller SM, Vander Wal JS, Klurfeld DM, McBurney MI, Cho S, Bijlani S, Dhurandhar NV, Waller SM, Vander Wal JS, Klurfeld DM, et al. Evening ready-to-eat cereal consumption contributes to weight management. J Am Coll Nutr 2004;23:316–21 [DOI] [PubMed] [Google Scholar]
- 90.Schlundt DG, Hill J, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 1992;55:645–51 [DOI] [PubMed] [Google Scholar]
- 91.Kleemola P, Puska P, Variainen E, Roos E, Luoto R, Ehnholm C. The effect of breakfast cereal on diet and serum cholesterol: a randomized trial in North Karelia, Finland. Eur J Clin Nutr 1999;53:716–21 [DOI] [PubMed] [Google Scholar]
- 92.Albertson AM, Thompson D, Franko D, Holschuh N, Bauserman R, Barton B. Prospective associations among cereal intake in children and adiposity, lipid levels, and physical activity during late adolescence. J Am Diet Assoc 2009;109:1775–80 [DOI] [PubMed] [Google Scholar]
- 93.Bazzano LA, Song Y, Bubes V, Good C, Manson J, Liu S. Dietary intake of whole and refined grain breakfast cereals and weight gain in men. Obes Res 2005;13:1952–60 [DOI] [PubMed] [Google Scholar]
- 94.Koh-Banerjee P, Franz M, Sampson L, Liu S, Jacobs D, Spiegelman D, Willett W, Rimm E. Changes in whole-grain, bran, and cereal fiber consumption in relation to 8-y weight gain among men. Am J Clin Nutr 2004;80:1237–45 [DOI] [PubMed] [Google Scholar]
- 95.Liu S, Willett W, Manson J, Hu F, Rosner B, Colditz G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr 2003;78:920–7 [DOI] [PubMed] [Google Scholar]
- 96.Ortega RM, Ortega A, Lopez-Sobaler A, Quintas M, Andres P, Redondo M, Navia B, Lopez-Bonilla M, Rivas T. Differences in the breakfast habits of overweight/obese and normal weight schoolchildren. Int J Vitam Nutr Res 1998;68:125–32 [PubMed] [Google Scholar]
- 97.Kosti RI, Panagiotakos D, Zampelas A, Mihas C, Alevizos A, Leonard C, Tountas Y, Mariolis A. The association between consumption of breakfast cereals and BMI in schoolchildren aged 12–17 years: the VYRONAS study. Public Health Nutr 2008;11:1015–21 [DOI] [PubMed] [Google Scholar]
- 98.Panagiotakos DB, Antonogeorgos G, Papadimitriou A, Anthracopoulos M, Papadopoulos M, Konstantinidou M, Fretzayas A, Priftis K. Breakfast cereal is associated with a lower prevalence of obesity among 10–12-year-old children: the PANACEA study. Nutr Metab Cardiovasc Dis 2008;18:606–12 [DOI] [PubMed] [Google Scholar]
- 99.Vågstrand K, Barkeling B, Forslund H, Eflhag K, Linne Y, Rossner Y, Lindroos A-K. Eating habits in relation to body fatness and gender in adolescents—results from the 'SWEDES’ study. Eur J Clin Nutr 2007;61:517–25 [DOI] [PubMed] [Google Scholar]
- 100.Song WO, Chun O, Obayashi S, Cho S, Chung C. Is consumption of breakfast associated with body mass index in US adults? J Am Diet Assoc 2005;105:1373–82 [DOI] [PubMed] [Google Scholar]
- 101.Saltzman E, Moriguti J, Das S, Corrales A, Fuss P, Greenberb A, Roberts S. Effects of a cereal rich in soluble fiber on body composition and dietary compliance during a hypocaloric diet. J Am Coll Nutr 2001;20:50–7 [DOI] [PubMed] [Google Scholar]
- 102.Melanson KJ, Angelopoulos T, Nguyen V, Martini M, Zukley L, Lowndes J, Dube T, Fiutem J, Yount B, Rippe J. Consumption of whole-grain cereals during weight loss: effects on dietary quality, dietary fiber, magnesium, vitamin B-6, and obesity. J Am Diet Assoc 2006;106:1380–8 [DOI] [PubMed] [Google Scholar]
- 103.Chang H-C, Huang C-N, Yeh D-M, Wang S-J, Peng C-H, Wang C-J. Oats prevents obesity and abdominal fat distribution, and improves liver function in humans. Plant Foods Hum Nutr 2013;68:18–23 [DOI] [PubMed] [Google Scholar]
- 104.Lightowler HJ, Henry CJK. An investigation of the effectiveness of ready-to-eat breakfast cereals in weight loss: comparison between single and mixed varieties. Nutr Bull 2009;34:48–53 [Google Scholar]
- 105.Ortega RM, Lopez-Sobaler A, Andres P, Rodriguez-Rodriguez E, Aparicio A, Bermejo L, Lopez-Plaza B. Changes in folate status in overweight/obese women following two different weight control programmes based on an increased consumption of vegetables or fortified breakfast cereals. Br J Nutr 2006;96:712–8 [PubMed] [Google Scholar]
- 106.Matthews A, Hull S, Angus F, Johnston K. The effect of ready-to-eat cereal consumption on energy intake, body weight and anthropometric measurements: results from a randomized, controlled trial. Int J Food Sci Nutr 2012;63:107–13 [DOI] [PubMed] [Google Scholar]
- 107.Kirk T, Crombie N, Cursiter M. Promotion of dietary carbohydrate as an approach to weight maintenance after initial weight loss: a pilot study. J Hum Nutr Diet 2000;13:277–85 [Google Scholar]
- 108.de Castro JM. When, how much and what foods are eaten are related to total daily food intake. Br J Nutr 2009;102:1228–37 [DOI] [PubMed] [Google Scholar]
- 109.Huus K, Brekke H, Ludvigsson J, Ludvigsson J. Relationship of food frequencies as reported by parents to overweight and obesity at 5 years. Acta Paediatr 2009;98:139–43 [DOI] [PubMed] [Google Scholar]
- 110.Franko DL, Alberson A, Thompson D, Barton B. Cereal consumption and indicators of cardiovascular risk in adolescent girls. Public Health Nutr 2011;14:584–90 [DOI] [PubMed] [Google Scholar]
- 111.Deshmukh-Taskar P, Nicklas T, Radliffe J, O'Neil C, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. the National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr 2013;16:2073–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Miller K, Liska D, Fulgoni V., III The association between body metrics and breakfast food choice in children. Infant Child Adolesc Nutr 2013;5:43–50 [Google Scholar]
- 113.Munirah M, Shafurah A, Norazmir A, Adilin M, Ajau D. Roles of whole grains-based products in maintaining treatment targets among type 2 diabetes mellitus patients. Asian J Clin Nutr 2012;4:67–76 [Google Scholar]
- 114.Deshmukh-Taskar P, Nicklas T, Radliffe J, O'Neil C, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr 2013;16:2073–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.McGill C, Sanders L, Miller K, Fulgoni V., III Breakfast and ready-to-eat cereal consumption are associated with improved markers of cardiometabolic health in adults: results from the National Health and Nutrition Examination Survey 2001–2008. J Aging Res Clin Pract 2013;3:168–73 [Google Scholar]
- 116.Bazzano LA. Effects of soluble fiber on low-density lipoprotein cholesterol and coronary heart disease. Curr Atheroscler Rep 2008;10:473–7 [DOI] [PubMed] [Google Scholar]
- 117.de la Hunty A, Gibson S, Ashwell M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obes Facts 2013;6:70–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Aune D, Norat T, Romundstad P, Vatten L. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol 2013. (Epub ahead of print; DOI: 10.1007/s10654-013-9852–5) [DOI] [PubMed] [Google Scholar]
- 119.Liu S, Manson J, Stampfer M, Hu F, Giovanucci E, Colditz G, Hennekens C, Willett W. A prospective study of whole-grain intake and risk of type 2 diabetes mellitus in US women. Am J Public Health 2000;90:1409–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kochar J, Djousse L, Gaziano J. Breakfast cereals and risk of type 2 diabetes in the Physicians’ Health Study 1. Obesity (Silver Spring) 2007;15:3039–44 [DOI] [PubMed] [Google Scholar]
- 121.Meyer KA, Kushi L, Jacobs D, Slavin J, Sellers T, Folsom A. Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr 2000;71:921–30 [DOI] [PubMed] [Google Scholar]
- 122.Jacobs DR, Meyer K, Kushi L, Folsom A. Whole-grain intake may reduce the risk of ischemic heart disease in postmenopausal women: the Iowa Women's Health Study. Am J Clin Nutr 1998;68:248–57 [DOI] [PubMed] [Google Scholar]
- 123.Hodge AM, English D, O'Dea K, Giles G. Glycemic index and dietary fiber and the risk of type 2 diabetes. Diabetes Care 2004;27:2701–6 [DOI] [PubMed] [Google Scholar]
- 124.McNaughton SA, Mishra G, Brunner E. Dietary patterns, insulin resistance, and incidence of type 2 diabetes in the Whitehall Study. Diabetes Care 2008;31:1343–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.de Munter JS, Hu FB, Spiegelman D, Franz M, van Dam RM, de Munter JSL, Hu FB, Spiegelman D, Franz M, van Dam RM. Whole grain, bran, and germ intake and risk of type 2 diabetes: a prospective cohort study and systematic review. PLoS Med 2007;4(8):e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Golay A, Koellreutter B, Bloise D, Assal J-P, Wursch P. The effect of muesli or cornflakes at breakfast on carbohydrate metabolism in type 2 diabetic patients. Diabetes Res Clin Pract 1992;15:135–41 [DOI] [PubMed] [Google Scholar]
- 127.Colagiuri S, Miller J, Holliday J, Phelan E. Comparison of plasma glucose, serum insulin, and C-peptide responses to three isocaloric breakfasts in non-insulin-dependent diabetic subjects. Diabetes Care 1986;9:250–4 [DOI] [PubMed] [Google Scholar]
- 128.Wheeler ML, Fineberg E, Gibson R, Fineberg N. Controlled portions of presweetened cereals present no glycemic penalty in persons with insulin-dependent diabetes mellitus. J Am Diet Assoc 1996;96:458–63 [DOI] [PubMed] [Google Scholar]
- 129.Tappy L, Gugolz E, Wursch P. Effects of breakfast cereals containing various amounts of beta-glucan fibers on plasma glucose and insulin responses in NIDDM subjects. Diabetes Care 1996;19:831–4 [DOI] [PubMed] [Google Scholar]
- 130.Granfeldt Y, Nyberg L, Bjorck J. Muesli with 4g oat beta-glucans lowers glucose and insulin responses after a bread meal in healthy subjects. Eur J Clin Nutr 2008;62:600–7 [DOI] [PubMed] [Google Scholar]
- 131.Tsihlias EB, Gibbs A, McBurney M, Wolever T. Comparison of high- and low-glycemic-index breakfast cereals with monounsaturated fat in the long-term management of type 2 diabetes. Am J Clin Nutr 2000;72:439–49 [DOI] [PubMed] [Google Scholar]
- 132.Wolever TM, Campell J, Geleva D, Anderson G. High-fiber cereal reduces postprandial insulin responses in hypercholesterolemic but not normolipemic subjects. Diabetes Care 2004;27:1281–5 [DOI] [PubMed] [Google Scholar]
- 133.Maki KC, Davidson M, Witchger M, Dicklin M, Subbaiah P. Effects of high-fiber oat and wheat cereals on postprandial glucose and lipid responses in healthy men. Int J Vitam Nutr Res 2007;77:347–56 [DOI] [PubMed] [Google Scholar]
- 134.Kim H, Stote K, Behall K, Spears K, Vinyard B, Conway J. Glucose and insulin responses to whole grain breakfasts varying in soluble fiber, beta-glucan: a dose response study in obese women with increased risk for insulin resistance. Eur J Nutr 2009;48:170–5 [DOI] [PubMed] [Google Scholar]
- 135.Hlebowicz J, Wickenberg J, Fahlstrom R, Bjorgell O, Almer L-O, Darwiche G. Efffect of commercial breakfast fibre cereals compared with corn flakes on postprandial blood glucose, gastric emptying and satiety in healthy subjects: a randomized blinded crossover trial. Nutr J 2007;6:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rendell M, Vanderhoof J, Venn M, Shehan M, Arndt E, Rao C, Gill G, Newman R, Newman C. Effect of a barley breakfast cereal on blood glucose and insulin response in normal and diabetic patients. Plant Foods Hum Nutr 2005;60:63–7 [DOI] [PubMed] [Google Scholar]
- 137.Backhouse SH, Williams C, Stevenson E, Nute M. Effects of the glycemic index of breakfast on metabolic responses to brisk walking in females. Eur J Clin Nutr 2007;61:590–6 [DOI] [PubMed] [Google Scholar]
- 138.Anderson JW, Hanna T, Peng X, Kryscio R. Whole grain foods and heart disease risk. J Am Coll Nutr 2000;19:291S–9S [DOI] [PubMed] [Google Scholar]
- 139.Anderson JW. Whole grains protect against atherosclerotic cardiovascular disease. Proc Nutr Soc 2003;62:135–42 [DOI] [PubMed] [Google Scholar]
- 140.Pereira MA, O'Reilly E, Augustsson K, Fraser G, Goldbourt U, Heitman B, Hallmans G, Knekt P, Liu S, Pietinen P, et al. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med 2004;164:370–6 [DOI] [PubMed] [Google Scholar]
- 141.Kelly SA, Summerbell C, Brynes A, Whittaker V, Frost G. Wholegrain cereals for coronary heart disease. Cochrane Database Syst Rev 2007; (2):CD005051. [DOI] [PubMed] [Google Scholar]
- 142.Mellen PB, Walsh T, Herrington D. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis 2008;18:283–90 [DOI] [PubMed] [Google Scholar]
- 143.Brown L, Rosner B, Willett W, Sacks F. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr 1999;69:30–42 [DOI] [PubMed] [Google Scholar]
- 144.Threapleton DE, Greenwood D, Evans C, Cleghorn C, Nykjaer C, Woodhead C, Cade J, Gale C, Burley V. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 2013;347:f6879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lillioja S, Neal A, Tapsell L, Jacobs D., Jr Whole grains, type 2 diabetes, coronary heart disease, and hypertension: links to the aleurone preferred over indigestible fiber. Biofactors 2013;39:242–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cho SS, Qi L, Fahey G, Jr, Klurfield D. Consumption of cereal fiber, mixtures of whole grains and bran, and whole grains and risk reduction in type 2 diabetes, obesity, and cardiovascular disease. Am J Clin Nutr 2013;98:594–619 [DOI] [PubMed] [Google Scholar]
- 147.AbuMweis SS, Jew S, Ames N. Beta-glucan from barley and its lipid-lowering capacity: a meta-analysis of randomized, controlled trials. Eur J Clin Nutr 2010;64:1472–80 [DOI] [PubMed] [Google Scholar]
- 148.Olson BH, Anderson S, Becker M, Anderson JW, Hunninghake D, Jenkins D, LaRosa J, Rippe J, Roberts D, Stoy D, et al. Psyllium-enriched cereals lower blood total cholesterol and LDL cholesterol, but not HDL cholesterol, in hypercholesterolemic adults: results of a meta-analysis. J Nutr 1997;127:1973–80 [DOI] [PubMed] [Google Scholar]
- 149.Jacobs DR, Gallaher D. Whole grain intake and cardiovascular disease: a review. Curr Atheroscler Rep 2004;6:415–23 [DOI] [PubMed] [Google Scholar]
- 150.Flight I, Clifton P. Cereal grains and legumes in the prevention of coronary heart disease and stroke: a review of the literature. Eur J Clin Nutr 2006;60:1145–59 [DOI] [PubMed] [Google Scholar]
- 151.Mente A, de Koning L, Shannon H, Anand S. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009;169:659–69 [DOI] [PubMed] [Google Scholar]
- 152.Harris KA, Kris-Etherton P. Effects of whole grains on coronary heart disease risk. Curr Atheroscler Rep 2010;12:368–76 [DOI] [PubMed] [Google Scholar]
- 153.Ryan D, Kendall M, Robards K, Ryan D, Kendall M, Robards K. Bioactivity of oats as it relates to cardiovascular disease. Nutr Res Rev 2007;20:147–62 [DOI] [PubMed] [Google Scholar]
- 154.Ruxton C, Derbyshire E. A systematic review of the association between cardiovascular risk factors and regular consumption of oats. Br Food J 2008;110:1119–32 [Google Scholar]
- 155.Bernstein AM, Titgemeier B, Kirkpatrick L, Golubic M, Roizen M. Major cereal greain fibres and psyllium in relation to cardiovascular disease. Nutrients. 2013;5:1471–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Truswell AS. Cereal grains and coronary heart disease. Eur J Clin Nutr 2002;56:1–14 [DOI] [PubMed] [Google Scholar]
- 157.Charlton KE, Tapsell L, Batterham M, O'Shea J, Thorne R, Beck E, Tosh S. Effect of 6 weeks’ consumption of beta-glucan rich oat products on cholesterol levels in mildly hypercholesterolaemic overweight adults. Br J Nutr 2012;107:1037–47 [DOI] [PubMed] [Google Scholar]
- 158.Jenkins DJ, Kendall C, Vuksan V, Augustin L, Mehling C, Parker T, Vidgen E, Lee B, Faulkner D, Seyler H, et al. Effect of wheat bran on serum lipids: influence of particle size and wheat protein. J Am Coll Nutr 1999;18:159–65 [DOI] [PubMed] [Google Scholar]
- 159.Davy BM, Davy K, Ho R, Beske S, Davrath L, Melby C. High-fiber oat cereal compared with wheat cereal consumption favorably alters LDL-cholesterol subclass and particle numbers in middle-aged and older men. Am J Clin Nutr 2002;76:351–8 [DOI] [PubMed] [Google Scholar]
- 160.Costabile A, Klinder A, Fava F, Napolitano A, Fogliano V, Leonard C, Gibson GR, Tuohy KM. Whole-grain wheat breakfast cereal has a prebiotic effect on the human gut microbiota: a double-blind, placebo-controlled, crossover study. Br J Nutr 2008;99:110–20 [DOI] [PubMed] [Google Scholar]
- 161.Wolever TMS, Tsihlias EB, McBurney MI, Le N-A. Long-term effect of reduced carbohydrate or increased fiber intake on LDL particle size and HDL composition in subjects with type 2 diabetes. Nutr Res 2003;23:15–26 [Google Scholar]
- 162.Boushey CJ, Bereford S, Omenn G, Motulsky A. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. JAMA 1995;274:1049–57 [DOI] [PubMed] [Google Scholar]
- 163.Tucker KL, Olson B, Bakun P, Dallal G, Selhub J, Rosenberg I. Breakfast cereal fortified with folic acid, vitamin B-6, and vitamin B-12 increases vitamin concentrations and reduces homocysteine concentrations: a randomized trial. Am J Clin Nutr 2004;79:805–11 [DOI] [PubMed] [Google Scholar]
- 164.Schorah CJ, Devitt H, Lucock M, Dowell A. The responsiveness of plasma homocysteine to small increases in dietary folic acid: a primary care study. Eur J Clin Nutr 1998;52:407–11 [DOI] [PubMed] [Google Scholar]
- 165.Malinow MR, Duell P, Irvin-Jones A, Upson B, Graf E. Increased plasma homocyst(e)ine after withdrawal of ready-to-eat breakfast cereal from the diet: prevention by breakfast cereal providing 200 micrograms folic acid. J Am Coll Nutr 2000;19:452–7 [DOI] [PubMed] [Google Scholar]
- 166.Riddell LJ, Chisolm A, Williams S, Mann JI. Dietary strategies for lowering homocysteine concentrations. Am J Clin Nutr 2000;71:1448–54 [DOI] [PubMed] [Google Scholar]
- 167.Venn BJ, Mann JI, Williams SM, Riddell LJ, Chisholm A, Harper MJ, Aitken W, Rossaak JI. Assessment of three levels of folic acid on serum folate and plasma homocysteine: a randomised placebo-controlled double-blind dietary intervention trial. Eur J Clin Nutr 2002;56:748–54 [DOI] [PubMed] [Google Scholar]
- 168.Holmes T, Gates GE. The effect of fortified breakfast cereal on plasma homocyst(e)ine concentrations in healthy older men already consuming a folate fortified diet. Nutr Res 2003;23:435–49 [Google Scholar]
- 169.Huang T, Chen Y, Yang B, Wahlqvist M, Li D. Meta-analysis of B vitamin supplementation on plasma homocysteine, cardiovascular and all-cause mortality. Clin Nutr 2012;31:448–54 [DOI] [PubMed] [Google Scholar]
- 170.Resnicow K. The relationship between breakfast habits and plasma cholesterol levels. J Sch Health 1991;61:81–5 [DOI] [PubMed] [Google Scholar]
- 171.Ganji V, Kafai M. Frequent consumption of milk, yoghurt, cold breakfast cereals, peppers, and cruciferous vegetables and intakes of dietary folate and riboflavin but not vitamins B-12 and B-6 are inversely associated with serum total homocysteine concentrations in the US population. Am J Clin Nutr 2004;80:1500–7 [DOI] [PubMed] [Google Scholar]
- 172.Bel-Serrat S, Mouratidou T, Bornhorst C, Pepies J, De Henauw S, Marild S, Molnar D, Siani A, Tornaritis M, Veidebaum T, et al. Food consumption and cardiovascular risk factors in European children: the IDEFICS study. Pediatr Obes 2013;8:225–36 [DOI] [PubMed] [Google Scholar]
- 173.Sanders L, Miller K, Fulgoni V., III Breakfast and ready-to-eat cereal consumption is associated with improved makers of cardio-metabolic health in adults: results from National Health and Nutrition Examination Survey 2001–2008. FASEB J 2012;26:626.21 [Google Scholar]
- 174.Kochar J, Gaziano J, Djousse L. Breakfast cereals and risk of hypertension in the Physicians’ Health Study 1. Clin Nutr 2012;31:89–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Davy BM, Melby C, Beske S, Ho R, Davrath L, Davy K. Oat consumption does not affect resting casual and ambulatory 24-h arterial blood pressure in men with high-normal blood pressure to stage I hypertension. J Nutr 2002;132:394–8 [DOI] [PubMed] [Google Scholar]
- 176.Pins JJ, Geleva D, Keenan J, Frazel C, O'Connor P, Cherney L. Do whole-grain oat cereals reduce the need for antihypertensive medications and improve blood pressure control? J Fam Pract 2002;51:353–9 [PubMed] [Google Scholar]
- 177.Maki KC, Galant R, Samuel P, Tesser J, Witchger M, Ribaya-Mercado J, Blumberg J, Geohas J. Effects of consuming foods containing oat beta-glucan on blood pressure, carbohydrate metabolism and biomarkers of oxidative stress in men and women with elevated blood pressure. Eur J Clin Nutr 2007;61:786–95 [DOI] [PubMed] [Google Scholar]
- 178.Londono D, Van't Westernde W, Goryunova S, Salentijn E, van den Broeck H, van der Meer I, Visser R, Gilissen L, Smulders M. Avenin diversity analysis of the genus Avena (oat): relevance for people with celiac disease. J Cereal Sci 2013;58:170–7 [Google Scholar]
- 179.Koskinen O, Villanen M, Korponay-Szabo I, Lindfors K, Maki M, Kaukinen K. Oats do not induce systemic or mucosal autoantibody response in children with coeliac disease. J Pediatr Gastroenterol Nutr 2009;48:559–65 [DOI] [PubMed] [Google Scholar]
- 180.Rashid M, Butzner D, Burrows V, Zarkadas M, Case S, Molloy M, Warren R, Pulido O, Switzer C. Consumption of pure oats by individuals with celiac disease: a position statement by the Canadian Celiac Association. Can J Gastroenterol 2007;21:649–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Pulido OM, Gillespie Z, Zarkadas M, Dubois S, Vavasour E, Rashid M, Switzer C, Godefroy S. Introduction of oats in the diets of individuals with celiac disease: a systematic review. Adv Food Nutr Res 2009;57:235–85 [DOI] [PubMed] [Google Scholar]
- 182.Haboubi NY, Taylor S, Jones S. Coeliac disease and oats: a systematic review. Postgrad Med J 2006;82:672–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Högberg L, Laurin P, Falth-Magnusson K, Grant C, Grodzinsky E, Jansson G, Ascher H, Browaldh L, Hammersjo J-A, Lindberg E, et al. Oats to children with newly diagnosed coeliac disease: a randomised double blind study. Gut 2004;53:649–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cummings J. The effect of dietary fibre on stool weight and composition. In: Spiller G, editor. Handbook of dietary fibre in human nutrition. Boca Raton (FL): CRC Press; 1993. p. 547–73.
- 185.Reicks M, Jonnalagadda S, Alberson A, Joshi N. Total dietary fiber intakes in the US population are related to whole grain consumption: results from the National Health and Nutrition Examination Survey 2009 to 2010. Nutr Res 2014;34:226–34 [DOI] [PubMed] [Google Scholar]
- 186.McLennan W, Podger A. National Nutrition Survey. Nutrient intakes and physical measurements. Canberra (Australia): Australian Bureau of Statistics; 1998. ABS Catalog No. 4805.0. [Google Scholar]
- 187.Kaçmaz Z, Kasikci M. Effectiveness of bran supplement in older orthopaedic patients with constipation. J Clin Nurs 2007;16:928–36 [DOI] [PubMed] [Google Scholar]
- 188.Sturtzel B, Elmadfa I. Intervention with dietary fiber to treat constipation and reduce laxative use in residents of nursing homes. Ann Nutr Metab 2008;52:54–6 [DOI] [PubMed] [Google Scholar]
- 189.Hull C, Greco R, Brooks D. Alleviation of constipation in the elderly by dietary fiber supplementation. J Am Geriatr Soc 1980;28:410–4 [DOI] [PubMed] [Google Scholar]
- 190.Ouellet LL, Turner T, Pond S, McLaughlin H, Knorr S. Dietary fibre and laxation in postop orthopedic patients. Clin Nurs Res 1996;5:428–40 [DOI] [PubMed] [Google Scholar]
- 191.Gibson SA. Breakfast cereal consumption of young children: associations with non-milk extrinsic sugars and caries experience: further analysis of data from the UK National Diet and Nutrition Survey of children aged 1.5–4.5 years. Public Health Nutr 2000;3:227–32 [DOI] [PubMed] [Google Scholar]
- 192.Minton KL, Berry C. Cariogenic potential of presweetened breakfast cereals. Pediatr Dent 1985;7:282–6 [PubMed] [Google Scholar]
- 193.Edgar WM. Prediction of the cariogenicity of various foods. Int Dent J 1985;35:190–4 [PubMed] [Google Scholar]
- 194.Kahn HA, Phillips R, Snowdon D, Choi W. Association between reported diet and all-cause mortality: twenty-one-year follow-up on 27,530 adult Seventh-Day Adventists. Am J Epidemiol 1984;119:775–87 [DOI] [PubMed] [Google Scholar]
- 195.Liu S, Sesso H, Manson J, Willett W, Buring J. Is intake of breakfast cereals related to total and cause-specific mortality in men? Am J Clin Nutr 2003;77:594–9 [DOI] [PubMed] [Google Scholar]
- 196.World Cancer Research Fund/American Institute for Cancer Research. Continuous update report interim report summary. Food, nutrition, physical activity and the prevention of colorectal cancer. Washington: American Institute for Cancer Research; 2011 [Google Scholar]
- 197.Aune D, Chan D, Lau R, Vieira R, Greenwood D, Kampman E, Norat T. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ 2011;343:d6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Jacobs ET, Lanza E, Alberts DS, Hsu CH, Jiang R, Schatzkin A, Thompson PA, Martinez ME, Jacobs ET, Lanza E, et al. Fiber, sex, and colorectal adenoma: results of a pooled analysis. Am J Clin Nutr 2006;83:343–9 [DOI] [PubMed] [Google Scholar]
- 199.Aune D, Chan D, Greenwood D, Vieira A, Navarro Rosenblatt D, Vieira R, Norat T. Dietary fiber and breast cancer risk: a systematic review and meta-analysis of prospective studies. Ann Oncol 2012;23:1394–402 [DOI] [PubMed] [Google Scholar]
- 200.Cressy P, Thomson B, Ashworth M, Grounds P, McGill E. Acrylamide in New Zealand food and updated exposure assessment. Wellington (New Zealand): Ministry of Agriculture and Forestry; 2012. MAF Technical Paper No. 2011/19. Available from: http://www.foodsafety.govt.nz/elibrary/industry/acrylamide-in-nz-food-updated-exposure-assessment.pdf. (Cited 2014 August)
- 201.Svensson K, Abramsson L, Becker W, Glynn A, Hellenas K, Rosen L. Dietary intake of acrylamide in Sweden. Food Chem Toxicol 2003;41:1581–6 [DOI] [PubMed] [Google Scholar]
- 202.Normandin L, Bouchard M, Ayotte P, Blanchet C, Becalski A, Bonvalot Y, Phaneuf D, Lapointe C, Gagne M, Courteau M. Dietary exposure to acrylamide in adolescents from a Canadian urban center. Food Chem Toxicol 2013;57:75–83 [DOI] [PubMed] [Google Scholar]
- 203.Wilson KM, Giovanucci E, Stampfer M, Mucci L. Dietary acrylamide and risk of prostate cancer. Int J Cancer 2012;131:479–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Wilson KM, Mucci L, Rosner B, Willett W. A prospective study of dietary acrylamide intake and the risk of breast, endometrial, and ovarian cancers. Cancer Epidemiol Biomarkers Prev 2010; 19:2503–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Hogervorst JG, Schouten L, Konings E, Goldbohm R, van den Brandt P. Dietary acrylamide intake is not associated with gastrointestinal risk. J Nutr 2008;138:2229–36 [DOI] [PubMed] [Google Scholar]
- 206.Larsson SC, Akesson A, Bergkvist L, Wolk A. Dietary acrylamide intake and risk of colorectal cancer in a prospective cohort of men. Eur J Cancer 2009;45:513–6 [DOI] [PubMed] [Google Scholar]
- 207.Slavin JL, Martini M, Jacobs D, Marquart L. Plausible mechanisms for the protectiveness of whole grains. Am J Clin Nutr 1999;70 suppl:459S–63S [DOI] [PubMed] [Google Scholar]
- 208.Lipkin M, Reddy B, Newmark H, Lamprecht S. Dietary factors in human colorectal cancer. Annu Rev Nutr 1999;19:545–86 [DOI] [PubMed] [Google Scholar]
- 209.Slavin J, Marquart L, Jacobs D. Consumption of whole-grain foods and decreased risk of cancer: proposed mechanism. Cereal Foods World. 2000;45:54–8 [Google Scholar]
- 210.Key TJ, Thorogood M, Appleby P, Burr M. Dietary habits and mortality in 11000 vegetarians and health conscious people: results of a 17 year follow up. BMJ 1996;313:775–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Breslow RA, Graubard B, Sinha R, Subar A. Diet and lung cancer mortality: a 1987 National Health Interview Survey. Cancer Causes Control 2000;11:419–31 [DOI] [PubMed] [Google Scholar]
- 212.Aarestrup J, Kyro C, Christensen J, Kristensen M, Wurtz A, Johnsen N, Overvad K, Tjonneland A, Olsen A. Whole grain, dietary fiber, and incidence of endometrial cancer in a Danish cohort study. Nutr Cancer 2012;64:1160–8 [DOI] [PubMed] [Google Scholar]
- 213.Kyrø C, Skeie G, Loft S, Landberg R, Christensen J, Lund E, Nilsson L, Palmqvist R, Tjonneland A, Olsen A. Intake of whole grains from different cereal and food sources and incidence of colorectal cancer in the Scandinavian HELGA cohort. Cancer Causes Control 2013;24:1363–74 [DOI] [PubMed] [Google Scholar]
- 214.Abe SK, Inoue M, Sawada N, Iwasaki M, Ishihara J, Sasazuki S, Shimazu T, Tamaji T, Shibuya K, Tsugane S, et al. Rice, bread, noodle and cereal intake and colorectal cancer in Japanese men and women: the Japan Public Health Centre-based Prospective Study (JPHC study). Br J Cancer 2014;110:1316–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Heilbrun LK, Nomura A, Hankin J, Stemmermann G. Diet and colorectal cancer with special reference to fiber intake. Int J Cancer 1989;44:1–6 [DOI] [PubMed] [Google Scholar]
- 216.Jain MG, Hislop G, Howe G, Ghadirian P. Plant foods, antioxidants, and prostate cancer risk: findings from case-control studies in Canada. Nutr Cancer 1999;34:173–84 [DOI] [PubMed] [Google Scholar]
- 217.Nkondjock A, Ghadirian P. Associated nutritional risk of breast and colon cancers: a population-based case-control study in Montreal, Canada. Cancer Lett 2005;223:85–91 [DOI] [PubMed] [Google Scholar]
- 218.Chan JM, Wang F, Holly E. Whole grains and risk of pancreatic cancer in a large population-based case-control study in the San Francisco Bay Area, California. Am J Epidemiol 2007;166:1174–85 [DOI] [PubMed] [Google Scholar]
- 219.Hardin J, Cheng I, Witte J. Impact of consumption of vegetable, fruit, grain, and high glycemic index foods on aggressive prostate cancer risk. Nutr Cancer 2011;63:860–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.MacLennan R, Macrae F, Bain C, Battistutta D, Chapuis P, Gratten H, Lambert J, Newland R, Ngu M, Russell A, et al. Randomized trial of intake of fat, fibre and beta carotene to prevent colorectal adenomas. J Natl Cancer Inst 1995;87:1760–6 [DOI] [PubMed] [Google Scholar]
- 221.Macrae FA, Selbie D, Abbott M, Sharpe K, Young G. Efffect of cereal fibre source and processing on rectal epithelial cell proliferation. Gut 1997;41:239–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Alberts DS, Martinez M, Roe D, Guillen-Rodriguez J, Marshall J, van Leeuwem B, Reid M, Ritenbaugh C, Vargas P, Bhattacharyya A, et al. Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. N Engl J Med 2000;342:1156–62 [DOI] [PubMed] [Google Scholar]
- 223.Smith AP. The concept of well-being: relevance to nutrition research. Br J Nutr 2005;93 Suppl 1:S1–5 [DOI] [PubMed] [Google Scholar]
- 224.Smith AP. Breakfast and mental health. Int J Food Sci Nutr 1998;49:397–402 [DOI] [PubMed] [Google Scholar]
- 225.Smith AP. Breakfast cereal consumption and subjective reports of health. Int J Food Sci Nutr 1999;50:445–9 [DOI] [PubMed] [Google Scholar]
- 226.Smith AP. Stress, breakfast cereal consumption and cortisol. Nutr Neurosci 2002;5:141–4 [DOI] [PubMed] [Google Scholar]
- 227.Sarlio-Lähteenkorva S, Lahelma E, Roos E. Mental health and food habits among employed women and men. Appetite 2004;42:151–6 [DOI] [PubMed] [Google Scholar]
- 228.O'Sullivan TA, Robinson M, Kendall G, Miller M, Jacoby P, Silburn S, Oddy W. A good-quality breakfast is associated with better mental health in adolescence. Public Health Nutr 2009;12:249–58 [DOI] [PubMed] [Google Scholar]
- 229.Smith A. An investigation of the effects of breakfast cereals on alertness, cognitive function and other apects of the reported well-being of children. Nutr Neurosci 2010;13:230–6 [Google Scholar]
- 230.Smith A. Breakfast cereal, digestive problems and well-being. Stress Health 2011;27:388–94 [Google Scholar]
- 231.Smith AP, Clark R, Gallagher J. Breakfast cereal and caffeinated coffee: effects on working memory, attention, mood, and cardiovascular function. Physiol Behav 1999;67:9–17 [DOI] [PubMed] [Google Scholar]
- 232.Foster J, Smith M, Woodman M, Zombor R, Ashton J. Impact of wholegrain breakfast cereal meal on blood glucose level, mood and affect. Food Aust 2007;59:593–6 [Google Scholar]
- 233.Rodríguez-Rodríguez E, Aparicio A, Bermejo L, Lopez-Sobaler A, Ortega R. Changes in the sensation of hunger and well-being before and after meals in overweight/obese women following two types of hypoenergetic diet. Public Health Nutr 2009;12:44–50 [DOI] [PubMed] [Google Scholar]
- 234.Smith A, Bazzoni C, Beale J, Elliott-Smith J, Tiley M. High fibre breakfast cereals reduce fatigue. Appetite 2001;37:249–50 [DOI] [PubMed] [Google Scholar]
- 235.Smith AP, Wilds A. Effects of cereal bars for breakfast and mid-morning snacks on mood and memory. Int J Food Sci Nutr 2009;60 Suppl 4:63–9 [DOI] [PubMed] [Google Scholar]
- 236.Lattimore P, Walton J, Bartlett S, Hackett A, Stevenson L. Regular consumption of a cereal breakfast. Effects on mood and body image satisfaction in adult non-obese women. Appetite 2010;55:512–21 [DOI] [PubMed] [Google Scholar]
- 237.Lawton CL, Walton J, Hoyland A, Howarth E, Allan P, Chesters D, Dye L. Short term (14 days) consumption of insoluble wheat bran fibre-containing breakfast cereals improves subjective digestive feelings, general wellbeing and bowel function in a dose dependent manner. Nutrients 2013;5:1436–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Probst A, Humpeler S, Heinzl H, Blasche G, Ekmekcioglu C. Short-term effect of macronutrient composition and glycemic index of a yoghurt breakfast on satiety and mood in healthy young men. Forsch Komplementmed 2012;19:247–51 [DOI] [PubMed] [Google Scholar]
- 239.Pollitt E. Does breakfast make a difference at school? J Am Diet Assoc 1995;95:1134–9 [DOI] [PubMed] [Google Scholar]
- 240.Hoyland A, Dye L, Lawton C. A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr Res Rev 2009;22:220–43 [DOI] [PubMed] [Google Scholar]
- 241.Wengreen H, Nelson C, Munger R, Corcoran C. Prospective study of ready-to-eat breakfast cereal consumption and cognitive decline among elderly men and women. J Nutr Health Aging 2011;15:202–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Holt SH, Delargy H, Lawton C, Blundell J. The effects of high-carbohydrate vs high-fat breakfasts on feeling of fullness, alertness, and subsequent food intake. Int J Food Sci Nutr 1999;50:13–28 [DOI] [PubMed] [Google Scholar]
- 243.Mahoney CR, Taylor HA, Kanarek RB, Samuel P. Effect of breakfast composition on cognitive processes in elementary school children. Physiol Behav 2005;85:635–45 [DOI] [PubMed] [Google Scholar]
- 244.Ingwersen J, Defeyter M, Kennedy D, Wesnes K, Scholey A. A low glycaemic index breakfast cereal preferentially prevents children's cognitive performance from declining throughout the morning. Appetite 2007;49:240–4 [DOI] [PubMed] [Google Scholar]
- 245.Smith MA, Foster J. The impact of a high versus a low glycaemic index breakfast cereal meal on verbal episodic memory in healthy adolescents. Nutr Neurosci 2008;11:219–27 [DOI] [PubMed] [Google Scholar]
- 246.Cooper SB, Bandelow S, Nute M, Morris J, Nevill M. Breakfast glycaemic index and cognitive function in adolescent school children. Br J Nutr 2012;107:1823–32 [DOI] [PubMed] [Google Scholar]
- 247.Defeyter M, Russo R. The effect of breakfast cereal consumption on adolescents’ cognitive performance and mood. Front Hum Neurosci 2013;7:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Kosti RI, Panagiotakos D, Zampelas A. Ready-to-eat cerals and the burden of obesity in the context of their nutritional contribution: are all ready-to eat cereals equally healthy? A systematic review. Nutr Res Rev 2010;23:314–22 [DOI] [PubMed] [Google Scholar]
- 249.Boutelle KN, Birkeland R, Hannan P, Story M, Neumark-Sztainer D. Associations between maternal concern for healthful eating and maternal eating behaviors, home food availability, and adolescent eating behaviors. J Nutr Educ Behav 2007;39:248–56 [DOI] [PubMed] [Google Scholar]
- 250.Paul GL, Rokusek J, Dykstra G, Boileau R, Layman D. Preexercise meal composition alters plasma neutral amino acid responses during exercise and recovery. Am J Clin Nutr 1996;64:778–86 [DOI] [PubMed] [Google Scholar]
- 251.Kirwan JP, O'Gorman D, Evans W. A moderate glycemic meal before endurance exercise can enhance performance. J Appl Physiol 1998;84:53–9 [DOI] [PubMed] [Google Scholar]
- 252.Kirwan JP, O'Gorman D, Cyr-Campbell D, Campbell W, Yarasheski K, Evans W. Effects of moderate glycemic meal on exercise duration and substrate utilization. Med Sci Sports Exerc 2001;33:1517–23 [DOI] [PubMed] [Google Scholar]
- 253.Kirwan JP, Cyr-Campbell D, Campbell W, Scheiber J, Evans W. Effects of moderate and high glycemic index meals on metabolism and exercise performance. Metabolism 2001;50:849–55 [DOI] [PubMed] [Google Scholar]
- 254.Connolly ML, Tuohy K, Lovegrove J. Wholegrain oat-based cereals have prebiotic potential and low glycemic index. Br J Nutr 2012;108:2198–206 [DOI] [PubMed] [Google Scholar]
- 255.Carvalho-Wells AL, Helmolz K, Nodet C, Molzer C, Leonard C, McKevith B, Thielecke F, Jackson K, Tuohy K. Determination of the in vitro prebiotic potential of a maize-based whole grain breakfast cereal: a human feeding study. Br J Nutr 2010;104:1353–6 [DOI] [PubMed] [Google Scholar]
- 256.Smith AP. Stress, breakfast cereal consumption and objective signs of upper respiratory tract illnesses. Nutr Neurosci 2002;5:145–8 [DOI] [PubMed] [Google Scholar]
- 257.Nieman DC, Henson D, Sha W. Ingestion of micronutrient fortified breakfast cereal has no influence on immune function in healthy children: a randomized controlled trial. Nutr J 2011;10:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Kammer L, Ding Z, Wang B, Hara D, Liao Y-H, Ivy J. Cereal and nonfat milk support muscle recovery following exercise. J Int Soc Sports Nutr 2009;6:11–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Thomson CA, Stanaway J, Neuhouser M, Snetselaar L, Stefanick M, Arendell L, Chen Z. Nutrient intake and anemia risk in the Women's Health Initiative Observational Study. J Am Diet Assoc 2011;111:532–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.National Health and Medical Research Council. A review of the evidence to address targeted questions to inform the revision of the Australian dietary guidelines. Canberra (Australia): National Health and Medical Research Council; 2011 [cited 2013 Feb 18]. Available from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/n55d_australian_dietary_guidelines_evidence_report.pdf
- 261.Fallaize R, Wilson L, Gray J, Morgan L, Griffiin B. Variation in the effects of three different breakfast meals on subjective satiety and subsequent intake of energy at lunch and evening meal. Eur J Nutr 2013;52:1353–9 [DOI] [PubMed] [Google Scholar]
- 262.Williams P, Allman-Farinelli M, Collins C, Gifford J, Byron A. A review of the evidence to address targeted questions to inform the revision of the Australian dietary guidelines 2009. Process manual. Canberra (Australia): Dieticians Association of Australia; 2011. Available from: http://daa.asn.au/wp-content/uploads/2011/03/Process-manual-Sept-2011.pdf. (Cited 2014 August 8) [Google Scholar]
- 263.Hambidge KM, Chavez M, Brown R, Walravens P. Zinc nutritional status of young middle-income children and effects of consuming zinc-fortified breakfast cereals. Am J Clin Nutr 1979;32:2532–9 [DOI] [PubMed] [Google Scholar]
- 264.Abrams SA, Griffin I, Davila P, Liang L. Calcium fortification of breakfast cereal enhances calcium absorption in children without affecting iron absorption. J Pediatr 2001;139:522–6 [DOI] [PubMed] [Google Scholar]
- 265.Timlin MT, Pereira MA. Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev 2007;65:268–81 [DOI] [PubMed] [Google Scholar]
- 266.Burley VJ, Leeds A, Blundell J. The effect of high and low-fibre breakfasts on hunger, satiety and food intake in a subsequent meal. Int J Obes 1987;11 Suppl 1:87–93 [PubMed] [Google Scholar]
- 267.Levine AS, Tallman J, Grace M, Parker S, Billington C, Levitt M. Effect of breakfast cereals on short-term food intake. Am J Clin Nutr 1989;50:1303–7 [DOI] [PubMed] [Google Scholar]
- 268.Geliebter A. Lunch meal intake following high and low fiber breakfast cereals. Obes Res 1999;7 Suppl 1:44S [Google Scholar]
- 269.Hamedani A, Akhavan T, Samra RA, Anderson GH, Hamedani A, Akhavan T, Samra RA, Anderson GH. Reduced energy intake at breakfast is not compensated for at lunch if a high-insoluble-fiber cereal replaces a low-fiber cereal. Am J Clin Nutr 2009;89:1343–9 [DOI] [PubMed] [Google Scholar]
- 270.Rebello CJ, Johnson W, Martin C, Xie W, O'Shea M, Kurilich A, Bordenave N, Andler S, van Klinken J, Chu Y-I, et al. Acute effect of oatmeal on subjective measures of appetite and satiety compared to a ready-to-eat breakfast cereal: a randomised crossover trial. J Am Coll Nutr 2013;32:272–9 [DOI] [PubMed] [Google Scholar]
- 271.Djoussé L, Gaziano JM. Breakfast cereals and risk of heart failure in the Physicians’ Health Study I. Arch Intern Med 2007;167:2080–5 [DOI] [PubMed] [Google Scholar]
- 272.Lockheart MS, Steffen L, Rebnord H, Fimreite R, Ringstad J, Thelle D, Pedersen J, Jacobs D., Jr Dietary patterns, food groups and myocardial infarction: a case-control study. Br J Nutr 2007;98:380–7 [DOI] [PubMed] [Google Scholar]
- 273.Djoussé L, Driver J, Gaziano J. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA 2009;302:394–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Odes H, Lazovski H, Stern I, Madar Z. Double-blind trial of a high dietary fiber, mixed grain cereal in patients with chronic constipation and hyperlipidemia. Nutr Res 1993;13:979–85 [Google Scholar]
- 275.Turconi G, Bazzano R, Caramella T, Tagliabue A, Lanzola E. The effect of a high-fibre cereal-based breakfast on daily dietary intakes and bowel function. J Hum Nutr Diet 1993;6:229–43 [PubMed] [Google Scholar]
- 276.Turconi G, Bazzano R, Caramella R, Lanzola E. The effects of high-fibre cereal-based breakfast meals on daily dietary intakes and bowel function. Eur J Clin Nutr 1995;49 Suppl 3:S312–6 [PubMed] [Google Scholar]
- 277.Vuksan V, Jenkins A, Jenkins D, Rogovik A, Sievenpiper J, Jovanovski E. Using cereal to increase dietary fiber intake to the recommended level and the effect of fiber on bowel function in healthy persons consuming North American diets. Am J Clin Nutr 2008;88:1256–62 [DOI] [PubMed] [Google Scholar]
- 278.Rowe NH, Anderson R, Wanninger L. Effects of ready-to-eat cereals on dental caries experience in adolescent children: a three-year study. J Dent Res 1974;53:33–6 [DOI] [PubMed] [Google Scholar]
- 279.Glass RL, Fleisch S. Diet and dental caries: dental caries incidence and the consumption of ready-to-eat cereals. J Am Dent Assoc 1974;88:807–13 [DOI] [PubMed] [Google Scholar]