Abstract
Background
Sleep deprivation and fatigue are common subjective complaints among astronauts. We conducted the first large-scale evaluation of objectively-estimated sleep of astronauts on both short- and long-duration spaceflight missions.
Methods
Allnon-Russian crewmembers assigned to space shuttle flights with inflight experiments from July 2001 until July 2011 or ISS Expeditions from 2006 –2011 were eligible to participate. We objectively assessed, via wrist actigraphy and daily logs, sleep-wake timing of 64 astronauts on 80 Space Shuttle missions, encompassing 26 Space Transportation System flights (1,063 inflight days), and 21 astronauts on the International Space Station (ISS) (3,248 inflight days) and, for each astronaut, during two Earth-based data-collection intervals prior to and one following spaceflight (4,013 ground-based days).
Findings
Astronauts attempted and obtained significantly less actigraphically-estimated sleep per night on space shuttle missions (7·35 ± 0·47 and 5·96 ± 0·56 hours, respectively), in the 11-days before spaceflight (7·35 ± 0·51 and 6·04 ± 0·72 hours, respectively) and even three months before spaceflight (7·40 ± 0·59 and 6·29 ± 0·67 hours, respectively) than they did upon their return to Earth (8·01 ± 0·78 and 6·74 ± 0·91 hours, respectively) (p < 0·0001 for each) Astronauts on ISS missions also obtained significantly less sleep three months prior (6.41 ± 0.65), in the 11 days prior (5.86 ± 0.94) and during spaceflight (6.09 ± 0.67 hours), as compared to the first week post-mission (6.95 ± 1.04 hours; p < 0·0001). Seventy-eight percent (61/78) of shuttle mission-crewmembers reported taking a dose of sleep-promoting medications on 52% of nights (500/963) and 2 doses on 17% of nights during flight (87/500); 75% of ISS crewmembers (12/16) reported using sleep-promoting medications.
Interpretation
Sleep deficiency in astronauts was prevalent not only during space shuttle and ISS missions, but also throughout a 3-month pre-flight training interval. Despite chronic sleep curtailment, sleeping pill use was pervasive during spaceflight. As chronic sleep loss produces performance decrements, these findings highlight the need for development of effective counter measures to promote sleep.
Funding
The study was supported by NASA cooperative agreement NCC 9–119. Drs. Czeisler and Barger received support from the NSBRI (HFP01601).
Keywords: fatigue, spaceflight
INTRODUCTION
After landing on the moon in 1969, Astronaut Neil Armstrong was reportedly unable to sleep all night and Astronaut Buzz Aldrin managed only “a couple of hours of fitful drowsing” during their 21.6 hours on the moon, reportedly because they could not escape from light and noise in the small cabin of their spacecraft and the spacesuit’s cooling system made it too cold for sleeping.1 Because sleep deficiency, an inadequate quantity or quality of sleep2, increases the risk of errors and accidents3 and human error contributes to 60% and 80% of aviation accidents,4 NASA has improved sleeping conditions for astronauts during spaceflight, and even provides light- and sound-attenuated (less than 50 decibels)5 sleep stations for astronauts aboard the International Space Station (ISS). Yet sleep deprivation and fatigue remain common complaints among astronauts,6 leading some to the hypothesis that microgravity interferes with the ability to sleep.
Previous studies of sleep and hypnotic use in space have been limited to post-flight subjective survey data7 or in-flight objective data collection from a small number of crewmembers as part of specific science payloads.8;9 In order to characterize more representative sleep patterns of astronauts during spaceflight, we conducted a large-scale study before, during and after multiple Space Transportation System (STS) Space Shuttle and ISS missions measuring both objective and subjective measures of sleep that have been validated against polysomnographically-recorded sleep in space.8;9
METHODS
Participants
All non-Russian crewmembers assigned to shuttle flights with inflight experiments from July 2001 until July 2011 or ISS Expeditions from 2006 –2011 were eligible to participate. NASA excluded the Russian cosmonauts due to conflicting policies regarding participation in research and individual commanders sometimes limited the number of crewmembers on a mission who could participate in any given experiment due to operational time constraints. Although the shuttle docked with the ISS on most missions, those astronauts assigned to the short duration shuttle flights were considered shuttle astronauts. Similarly, even though astronauts assigned to ISS missions may have been transported to or from the ISS via the shuttle, they were considered ISS astronauts. The Partners HealthCare System Human Research Committee and the NASA Committee for the Protection of Human Subjects approved the protocol. Participants provided written informed consent prior to the start of the study. Out of the 193 eligible mission-crewmembers, 114 consented to participate (59%). Of those who consented, 94% (n=101) of those who returned to Earth safely completed the study (54% of eligible crewmembers who returned to Earth safely).
Procedures
To assess sleep-wake timing during spaceflight, we recorded actigraphy of the non-dominant wrist continuously throughout three terrestrial data collection intervals (two weeks scheduled 90 days before launch [SL-90], from 11 days prior to the day of launch [L-11] and for the first 7 days post-landing [R+7]) and inflight. All crewmembers slept at home during the SL-90 data collection interval. Prior to launch (during the L-11 data collection interval), crewmembers moved to astronaut crew quarters, with individual sleep rooms, at Johnson Space Center, Kennedy Space Center or in Moscow. After landing, all shuttle and ISS crewmembers who returned to Earth aboard the shuttle slept at home during the R+7 data collection interval; those ISS crewmembers who returned in the Soyuz slept in crew quarters during that interval. During spaceflight aboard the shuttle, crewmembers slept in sleeping bags (Figure S1a). ISS crewmembers usually slept in individual sleeping quarters (Figure S1b).
Unlike prior studies of sleep in space, neither participant behavior (e.g., sleep schedule) nor countermeasure (e.g., sleeping pill) use was restricted during any of these data collection intervals. Crew members continuously wore a small, light-weight activity- and light-recording device [Actiwatch-L (AWL); MiniMitter/Phillips Respironics, Bend, OR] and kept a daily sleep and medication log during the data collection intervals. Due to operational and technical constraints, actigraphy data were collected and scored in two-minute epochs inflight. On the ground, such data were collected in one-minute epochs and scored in two-minute epochs. ISS crewmembers used a computerized version of the sleep log inflight and were scheduled to complete it on a daily basis during specified intervals (e.g., one week out of every three weeks), whereas on shuttle missions and during all terrestrial data collection intervals the log was completed daily via paper/pencil. Actigraphy was analyzed during reported sleep episodes using a standard algorithm (see supplemental methods).
Statistical analysis
Univariate summary statistics were calculated for all participants to evaluate population characteristics. Objective and subjective measures of sleep and medication used to promote sleep were quantified and compared among SL-90, L-11, inflight and R+7 data collection intervals using mixed-effects model with data collection interval and sleep episode as fixed effects and participant as random effect, and controlled for age (continuous variable) and gender. Nested random effects were added to the model in order to account for correlation from the same crewmembers completing repeat missions. Self-reported sleep latency >240 minutes (n=11) was excluded as error. Statistical analysis was completed using SAS 9.2 (SAS Institute, Inc., Cary, NC). Mean, standard deviation in Tables 1 and 2 and mean difference and 95% CI in table 3 are based on raw data and p-values in these tables are from statistical models.
Table 1.
Space Shuttle Missions/ISS Mission Sleep Outcomes
| SL-90 STS(Mean/SD) ISS(Mean/SD) |
L-11 STS(Mean/SD) ISS(Mean/SD) |
Inflight STS(Mean/SD) ISS(Mean/SD) |
R+7 STS(Mean/SD) ISS(Mean/SD) |
P STS ISS |
Night before EVAs - STS (Mean/SD) |
|
|---|---|---|---|---|---|---|
| Time in Bed (Diary) (hours) | 7·40/0·59 7·37/0·83 |
7·35/0·51 7·14/1·16 |
7·35/0·47 7·46/1·22 |
8·01/0·78 8·34/1·14 |
<0·0001 <0·0001 |
7·47/0·60 |
| Sleep Episode Time (Actigraphy) (hours) | 7·27/0·61 7·27/0·60 |
7·00/0·62 6·77/0·99 |
6·73/0·46 6·84/0·75 |
7·90/0·81 8·17/0·88 |
<0·0001 <0·0001 |
6·61/0·90 |
| Total Sleep Time (Diary) (hours) | 6·86/0·57 6·77/0·71 |
6·73/0·47 6·33/0·76 |
6·32/0·53 6·54/0·67 |
7·23/0·71 7·17/0·85 |
<0·0001 <0·0001 |
6·33/0·84 |
| Total Sleep Time (Actigraphy) (hours) | 6·29/0·67 6·41/0·65 |
6·04/0·72 5·86/0·94 |
5·96/0·56 6·09/0·67 |
6·74/0·91 6·95/1·04 |
<0·0001 <0·0001 |
5·94/0·96 |
| Sleep Latency (Diary) (mins) * | 15·54/8·82 12·99/5·87 |
16·44/9·29 14·41/9·46 |
23·63/14·75 13·74/10·64 |
13·67/8·98 15·29/15·15 |
<0·0001 0·8903 |
28·47/27·62 |
| Sleep Quality (Diary) | 67·91/13·37 67·51/14·02 |
65·88/13·35 62·32/15·64 |
63·70/13·35 66·51/13·43 |
69·23/13·13 66·87/11·13 |
<0·0001 0·0084 |
61·77/18·01 |
| Alertness (Diary) | 65·17/15·51 61·68/17.76 |
64·30/14·56 55·98/19·46 |
64·92/13·51 57·69/18·73 |
67·46/12·83 61·40/17·55 |
<0·0001 0·0026 |
64·81/16·29 |
| Use of sleep-promoting medication (Shuttle only) (% mission-crewmembers/% nights) | 27/5 | 72/33 | 78/52 | 25/8 | <0·0001 | 70/60 |
Mean and standard deviation are based on raw data and p-values are from statistical models.
SL>240 minutes were excluded.
Table 2.
Nightly Sleep Percentages on Space Shuttle and ISS Missions
| SL-90 (Space Shuttle/ISS) | ||||
|---|---|---|---|---|
| Number of Hours |
Time in Bed N=1059/260 n(%)/n(%) |
Sleep Episode Time (Actigraphy) N=1047/257 n(%)/n(%) |
Total Sleep Time (Subjective Diary) N=1024/242 n(%)/n(%) |
Total Sleep Time (Actigraphy) N=1047/257 n(%)/n(%) |
| < 4 | 1(0·1)/1(0·4) | 2(0·2)/2(0·8) | 1(0·1)/2(0·8) | 23(2·2)/10(3·9) |
| ≥ 4 and < 5 | 10(0·9)/7(2·7) | 36(3·4)/13(5·1) | 22(2·2)/11(4·6) | 90(8·6)/28(10·9) |
| ≥ 5 and < 6 | 79(7·5)/35(13·5) | 114(10·9)/30(11·7) | 135(13·2)/39(16·1) | 294(28·1)/40(15·6) |
| ≥ 6 and < 7 | 243(23·0)/51(19·6) | 278(26·6)/60(23·4) | 335(32·7)/78(32·2) | 392(37·4)/94(36·6) |
| ≥ 7 and < 8 | 415(39·2)/89(34·2) | 371(35·4)/76(29·6) | 333(32·5)/53(21·9) | 177(16·9)/58(22·6) |
| ≥ 8 | 311(29·4)/77(29·6) | 246(23·5)/76(29·6) | 198(19·3)/59(24·4) | 71(6·8)/27(10·5) |
| L-11 (Space Shuttle/ISS) | ||||
|---|---|---|---|---|
| Number of Hours |
Time in Bed N=873/196 n(%)/n(%) |
Sleep Episode Time (Actigraphy) N=862/214 n(%)/n(%) |
Total Sleep Time (Subjective Diary) N=830/190 n(%)/n(%) |
Total Sleep Time (Actigraphy) N=863/214 n(%)/n(%) |
| < 4 | 0(0)/4(2·0) | 3(0·4)/7(3·3) | 4(0·5)/6(3.2) | 16(1·9)/18(8·4) |
| ≥ 4 and < 5 | 7(0·8)/5(2·6) | 24(2·8)/19(8·9) | 14(1·7)/9(4·7) | 5(12·9)/37(17·3) |
| ≥ 5 and < 6 | 45(5·2)/22(11·2) | 118(13·7)/28(13·1) | 93(11·2)/37(19·5) | 291(33·7)/48(22·4) |
| ≥ 6 and < 7 | 211(24·2)/43(21·9) | 280(32·5)/56(26·2) | 310(37·4)/64(33·7) | 306(35·5)/68(31·8) |
| ≥ 7 and < 8 | 388(44·4)/73(37·2) | 298(34·6)/66(30·8) | 329(39·6)/51(26·8) | 110(12·8)/34(15·9) |
| ≥ 8 | 222(25·4)/49(25·0) | 139(16·1)/38(17·8) | 80(9·6)/23(12·1) | 29(3·4)/9(4·2) |
| Inflight (Space Shuttle/ISS) | ||||
|---|---|---|---|---|
| Number of Hours |
Time in Bed N=922/996 n(%)/n(%) |
Sleep Episode Time (Actigraphy) N=1020/2948 n(%)/n(%) |
Total Sleep Time (Subjective Diary) N=925/987 n(%)/n(%) |
Total Sleep Time (Actigraphy) N=1020/2951 n(%)/n(%) |
| < 4 | 2(0·2)/16(1·6) | 12(1·2)/89(3·0) | 11(1·2)/31(3·12) | 38(3·7)/142(4·8) |
| ≥ 4 and < 5 | 6(0·7)/30(3·0) | 47(4·6)/161(5·5) | 54(5·8)/44(4·5) | 110(10·8)/376(12·7) |
| ≥ 5 and < 6 | 28(3·0)/110(11·0) | 120(11·8)/508(17·2) | 145(15·7)/166(16·8) | 332(32·6)/776(26·3) |
| ≥ 6 and < 7 | 156(16·9)/282(28·3) | 366(35·9)/818(27·8) | 414(44·8)/317(32·1) | 422(41·4)/942(31·9) |
| ≥ 7 and < 8 | 464(50·3)/282(28·3) | 443(43·4)/755(25·6) | 277(30·0)/266(27·0) | 115(11·3)/487(16·5) |
| ≥ 8 | 266(28·9)/276(27·7) | 32(3·1)/617(20·9) | 24(2·6)/163(16·5) | 3(0·3)/228(7·7) |
| R+7 (Space Shuttle/ISS) | ||||
|---|---|---|---|---|
| Number of Hours |
Time in Bed N=503/135 n(%)/n(%) |
Sleep Episode Time (Actigraphy) N=511/132 n(%)/n(%) |
Total Sleep Time (Subjective Diary) N=488/132 n(%)/n(%) |
Total Sleep Time (Actigraphy) N=511/121 n(%)/n(%) |
| < 4 | 3(0·6)/1(0·7) | 4(0·8)/2(1·5) | 3(0·6)/2(1·7) | 11(2·2)/3(2·3) |
| ≥ 4 and < 5 | 4(0·8)/1(0·7) | 7(1·4)/1(0·8) | 7(1·4)/3(2·5) | 34(6·7)/13(9·9) |
| ≥ 5 and < 6 | 19(3·8)/7(5·2) | 31(6·1)/9(6·8) | 39(8·0)/14(11·6) | 108(21·1)/17(12·9) |
| ≥ 6 and < 7 | 66(13·1)/17(12·6) | 92(18·0)/21(15·9) | 121(24·8)/23(19·0) | 145(28·4)/33(25·0) |
| ≥ 7 and < 8 | 137(27·2)/27(20·0) | 141(27·6)/26(19·7) | 164(33·6)/32(26·5) | 137(26·8)/26(19·7) |
| ≥ 8 | 274(54·5)/82(60·7) | 236(46·2)/73(55·3) | 154(31·6)/47(38·8) | 76(14·9)/40(30·3) |
| Night before EVA (Shuttle only) | ||||
|---|---|---|---|---|
| Number of Hours |
Time in Bed N=72 n(%) |
Sleep Episode Time (Actigraphy) N=80 n(%) |
Total Sleep Time (Subjective Diary) N=69 n(%) |
Total Sleep Time (Actigraphy) N=80 n(%) |
| < 4 | 0(0) | 0(0) | 0(0) | 1(1·3) |
| ≥ 4 and < 5 | 0(0) | 3(3·8) | 6(8·7) | 11(13·8) |
| ≥ 5 and < 6 | 1(1·4) | 11(13·8) | 13(18·8) | 29(36·3) |
| ≥ 6 and < 7 | 17(23·6) | 43(53·8) | 28(40·6) | 28(35·0) |
| ≥ 7 and < 8 | 34(47·2) | 20(25·0) | 19(27·5) | 10(12·5) |
| ≥ 8 | 20(27·8) | 3(3·8) | 3(4·3) | 1(1·3) |
Table 3.
Crewmembers’ sleep outcomes on nights aboard Shuttle and ISS missions with and without sleep-promoting medication
| (n=607) (n=324) |
Nights without Medication Mean (SD) Shuttle ISS |
Nights with Medication Mean (SD) Shuttle ISS |
Difference between nights with and without medication (95% CI) Shuttle (N=49) ISS (N=9) |
p value |
|---|---|---|---|---|
| Total Sleep Time (Actigraphy)(hours) | 5·82 (0·88) 6.17 (1.10) |
6·00 (0·57) 6.75(1.86) |
0.19 (−0.01, 0.38) 0.58 (−0.52, 1.68) |
0·0808 0.3884 |
| Sleep Efficiency (Actigraphy)(%) | 86·6 (7·3) 87.0 (9.8) |
87·9 (5·6) 90.6 (5.5) |
1.3 (−0.2, 2.8) 3.6 (−2.2, 9.4) |
0·0438 0.4227 |
| Sleep Latency (Diary)(min) | 35.16 (25.90) 20.95 (18.52) |
24.12 (16.20) 12.48 (7.72) |
−11.01 (−19.43, −2.60) −8.47 (−21.42, 4.47) |
0·0013 0.0254 |
| Sleep Quality (Diary) | 57·98 (20·39) 59.45 (16.35) |
65·97 (13·91) 66.62 (17.92) |
8.59 (3.32, 13.87) 7.17 (−3.14, 17.48) |
0·0419 0.5168 |
| Alertness (Diary) | 61·50 (17·74) 47.39 (24.40) |
66·00 (15·98) 50.36 (23.95) |
5.22 (1.57, 8.87) 2.97 (−3.93, 9.87) |
0·1909 0.1837 |
| Disturbed Sleep (Diary)(%) | 61·4 (36·5) 41.0 (25.2) |
50·6 (34·4) 49.1 (43.0) |
−14.1 (−23.6, −4.5) 8.1 (−32.4, 48.7) |
0·0525 0.1119 |
Mean, standard deviation, mean difference and 95% CI are based on raw data and p-values are from statistical models.
SL>240 minutes were excluded.
During spaceflight, crewmembers removed the Actiwatch-L for all EVAs and sometimes for other operational duties or for exercise. Occasionally, they forgot to put back on the Actiwatch-L before they went to sleep resulting in the loss of 3.8% (40/1063) of actigraphy data on shuttle missions and 9.1% (297/3248) of actigraphy data on ISS missions. Because only a small percentage of data were missing sporadically, we did not impute missing data.
Role of the funding source
The study sponsors had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study and the corresponding author had final responsibility for the decision to submit for publication.
RESULTS
Sixty-four crewmembers (female=10) participated in 80 missions on 26 shuttle flights. Fifteen participants completed the study twice and one crewmember completed the study three times. Mean age of shuttle crewmembers was 46·4 ± 4·5 (mean ± SD; range 37·7–57·9) years. Investigation of sleep among shuttle crewmembers includes 4,173 nights of data collection, including 1,063 nights during spaceflight.
Twenty-one crewmembers (female=6) participated during 13 ISS expeditions (Expedition 14 until Expedition 26). Mean age of ISS crewmembers was 46·7 ± 3·9 (mean ± SD; range 40·1 – 55·8) years. Investigation of sleep among ISS crewmembers includes 4,152 nights of data collection, including 3,248 nights during spaceflight.
Crew members who completed the study were similar in age and gender to those who did not enroll or complete the study (46.4 ± 4.4 years versus 45.9 ± 4.6 years, 18.8% versus 16.3% female, respectively).
Sleep on Shuttle Missions
Duration of Attempted Sleep
The duration of time astronauts attempted to sleep per night was significantly less on shuttle missions, during the 11-days before spaceflight and three months before spaceflight than it was upon their return to Earth (p < 0·0001 for each; Table 1).
Objective Sleep Quantity (Actigraphy)
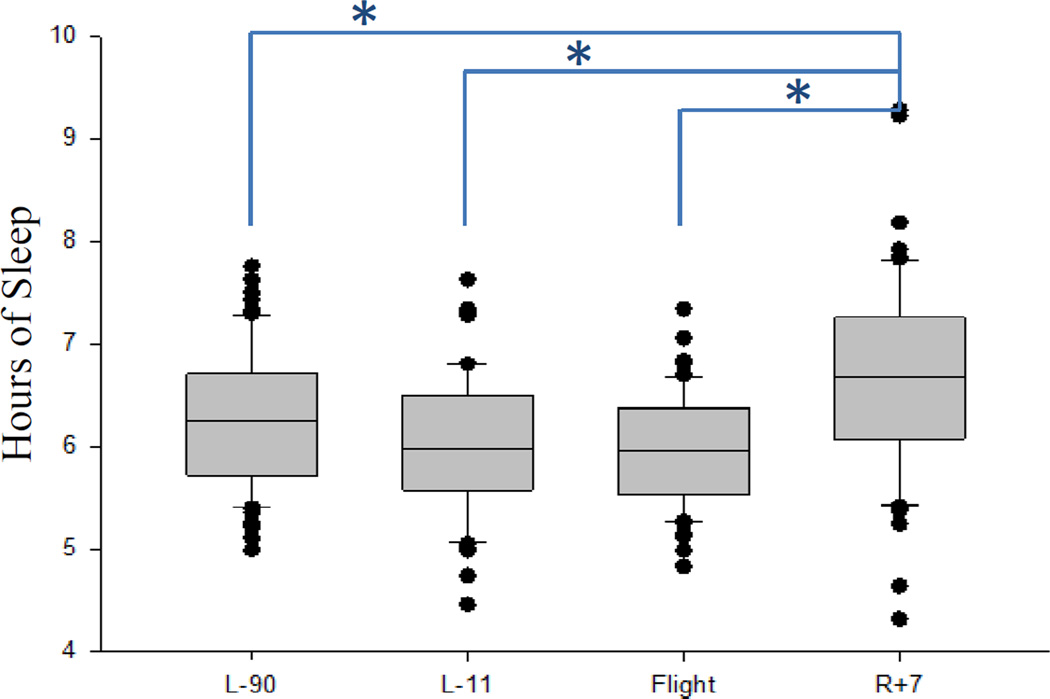
It took longer for crewmembers to fall asleep and they slept significantly less on shuttle missions and during SL-90 and L-11 compared to R+7 (p<0·0001, Figure 1, Table 1). Age and gender were not significant in the model. The mean duration of sleep during spaceflight was 5·96 ± 0·56 hours. Crewmembers slept on average 20 minutes longer each night during SL-90 and 47 minutes longer each night during R+7 (Table 1).
Figure 1.
Mean sleep duration was significantly less on shuttle missions and during the SL-90 and L-11 pre-flight data collection intervals than during the post-flight data collection interval (marked with asterisks; p < 0·0001). The box plot indicates the median with a line, the 25th and 75th percentiles with the bottom and top of the box, respectively, and the10th and 90th percentiles as error bars. The dots are individual subjects with means outside lower than the 10th or higher than the 90th percentile.
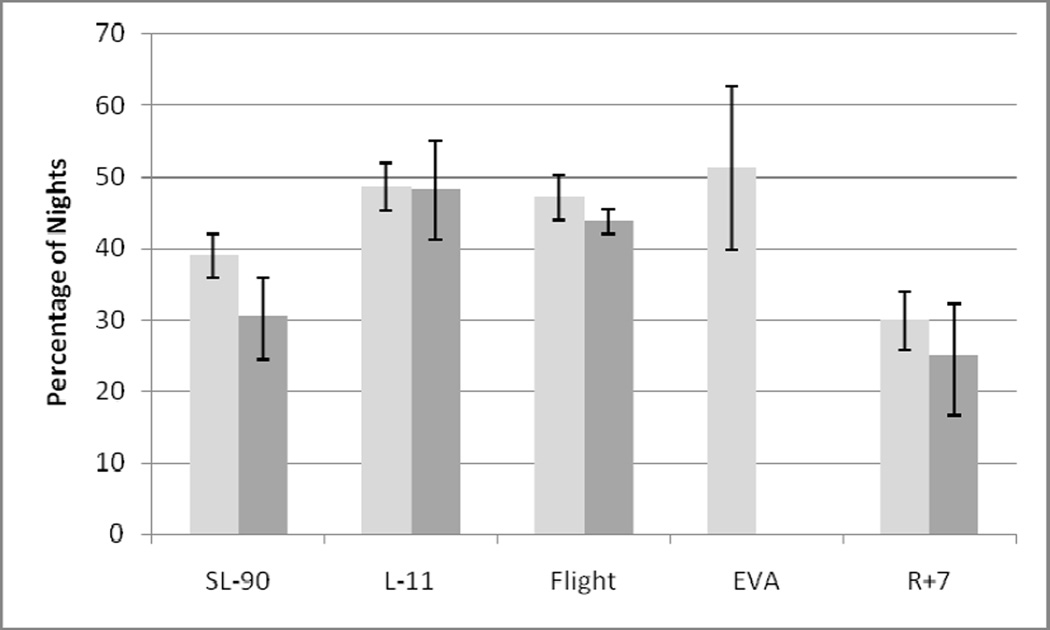
On 47·1% of nights aboard shuttle missions (480/1020), astronauts obtained less than 6 hours of sleep (Figure 2). This may in part be because a reduction in the duration of the time attempting to sleep before and during the flight. Objective actigraphy recordings revealed that only 32 (3·1%) of sleep episodes (i.e., the duration of time in bed attempting to sleep) on shuttle flights, 131(16·1 %) sleep episodes during L-11 and 236 (23·5%) sleep episodes during SL-90 were 8 or more hours long, as compared to 236 (46·2%) post-flight sleep episodes (Table 2). Crewmember-reported causes of sleep disturbances are reported in supplementary material.
Figure 2.
Percentage of nights with total sleep time (actigraphy) less than 6 hours in space shuttle (light gray; n=77 shuttle mission-crewmembers) and ISS (dark gray; n=21 ISS crewmembers) crewmembers during three terrestrial data collection intervals, inflight and on the nights before EVAs (Space Shuttle only). 95% confidence intervals are indicated.
Critical tasks
33 crewmembers were required to perform 83 extra vehicular activities (EVA). Actigraphy data were available on 80 of those nights before EVAs. On more than one-half of the nights (41/80, 51.3%) before accomplishing EVAs, crewmembers slept less than 6 hours. On 1·3% of nights before these critical tasks did crewmembers obtain 8 hours of sleep (1/80) Figure 2/Table 2).
Subjective Sleep and Alertness Outcomes
Astronauts reported sleeping significantly less on shuttle missions and during SL-90 and L-11 compared to R+7 (p<0·0001, Figure 1/Table 1). Subjective ratings of sleep quality and alertness were significantly higher post flight compared to during the shuttle missions (p<0·0001, p<0·0001, respectively), during SL-90 (p=0·0002, p<0·0001, respectively), and L-11 (p<0·0001, p<0·0001, respectively) compared to R+7 (Table 1).
Sleep and Alertness on International Space Station Missions
Sleep deficiency on ISS missions was similar to shuttle missions. Astronauts slept significantly less on ISS missions compared to SL-90 (p=0·0019) and R+7 (p<0·0001) (Table 1). On 43·8% of nights aboard ISS missions (1294/2951), astronauts obtained less than 6 hours of sleep (Table 2/Figure 2). There were no significant trends in sleep variables over the duration of the mission. At R+7, crewmembers reported sleeping on average >40 min more per night than they did at L-11 and inflight (Table 1). Subjective ratings of alertness were significantly lower during L-11 as compared to R+7 (p=0·007).
Sleep and Wakefulness Countermeasure Use During Spaceflight
Medication use on shuttle missions
Seventy-eight percent of shuttle mission-crewmembers (61/78) reported taking sleep medications inflight. Sleep medications use was reported on 52% of the inflight nights (500/963) with 2 doses of sleep medication on 17% of nights that sleep medications were taken (87/500; Figure s3). Sleep medication use was reported on 60% of nights before EVAs. Sleep medications were taken less frequently during SL-90, L-11 and R+7 than inflight (p<0.0001, Table 1).
Zolpidem and zolpidem CR were the most frequently used mediations on shuttle missions, accounting respectively for 73 % (301/413) and 12% (49/413) of nights when a single dose of medication was reported. Zaleplon was reported on 11% (45/413) of nights when a single dose of medication was used. Other sleep-promoting medications reported by shuttle crewmembers include temazepam (8/13, 2%), eszopiclone (2/413, 0.5%), melatonin (7/413, 2%) and quetiapine fumarate (1/413, 0.2%). When two doses of medications were reported, it was most commonly two doses of zolpidem (22/87, 25%) or zolpidem CR (15/87, 17%). A variety of combinations were used when two different medications were reported in the same night--the most common being zolpidem and zaleplon (14/87, 16%), zolpidem and melatonin (10/87, 11%), zolpidem CR and melatonin (8/87, 9%), and zolpidem CR and zaleplon (7/87, 8%).
Within-subject analysis (n=607) showed that total sleep time estimated by actigraphy and self-reported sleep disturbance and alertness were similar in the inflight nights regardless when sleep medications were reported used or not used (Table 3). However, sleep efficiency was lower, self-reported sleep latency was greater and subjective sleep quality was rated lower on nights without medication use.
Medication use on ISS missions
Of the twenty-one ISS crewmembers, more than one-third (n=8) declined to answer the medication use question on the sleep log at some point during the mission preventing the question on medication use from being asked in future logs. Three of those eight indicated sleep-promoting medication use in the mission prior to declining to answer the question. Thus, 75% (12/16) of crewmembers reported using sleep promoting medications. Sleep medications were reported used on 11% of sleep logs (96/852). On 19% of days when sleep-promoting medications were used (18/96), two doses were reported.
Wake-promoting countermeasures are described in supplementary materials.
DISCUSSION
In the most comprehensive study of objectively assessed sleep-wake timing in the history of both short-duration and long-duration spaceflight, we found that sleep deficiency is pervasive among crewmembers despite NASA regulations that mandate 8·5 hours of protected time for sleep each night10 and widespread use of sleep medications during spaceflight, consistent with subjective post-flight reports of sleep duration aboard nine early short-duration shuttle missions (n=58).7 Prior polysomnographic recordings of sleep in space, which were much more invasive, were unable to assess the spontaneous timing of sleep in space because the limited number of crewmembers were tethered to the equipment during the scheduled sleep episode and use of hypnotic medications was prohibited.8,9,11,12(See Panel: Research in Context). In fact, significantly longer sleep durations were documented by actigraphy on nights when sleep was polsomnographically recorded (6·96 ± 0·11 h) as part of an experimental protocol for the science payload than on nights when sleep was not polysomnographically recorded (6·36 ± 0·22 h; p=0·0215).9 The present results indicate that on shuttle flights in which there is not a sleep science payload, average nightly sleep durations are even shorter (5·96 ± 0·56 h).
We found crewmembers aboard long-duration ISS missions also averaged 6·09 ± 0·67 h per night, comparable with short-duration shuttle missions, contrary to anecdotal reports that ISS crewmembers obtain substantially more sleep than shuttle crewmembers13 That such sleep curtailment was problematic for ISS crewmembers is revealed by an analysis of ISS astronaut journal entries, which showed entries about sleep to be among the top ten topic categories, with the majority of those entries being negative (e.g., “I found myself getting pretty inefficient; by the time I go to bed tonight my work day will have been about 27 hours, and that’s on top of 2 nights with pretty minimal sleep….”; “The fatigue was evident when a couple of minor mistakes were made today on some payload activities. The ground caught the mistake…but it is an obvious indicator of fatigue.”; “Very tired. Woke up at 2 am and couldn’t get back to sleep. Finally fell asleep and overslept.”; “I fell asleep while typing.”; and “I just need sleep.”).6 However, we did find that on the 7·7% of nights, ISS crewmembers slept 8 hours or more, whereas shuttle crewmembers obtained that much sleep on only 0·30% of inflight nights (p<0·0001).
Although there were significant differences in the subjective ratings of sleep quality and alertness, the effect size is small. Operational importance of these small differences could not be determined. There was no trend in sleep over the duration of ISS missions (See supplement Figure S4). This could be due to the operationally required changes in sleep-wake schedules that occurred throughout the missions, which included repeated “slam shifts” required when the shuttle docked with the ISS. Further research on sleep is planned for the future one-year ISS missions and may be able to inform on trends in sleep over longer durations, which is especially relevant for future exploration missions to Mars and beyond.
Although astronauts obtained, on average, significantly less sleep inflight than during Earth-based data collection, our data suggest that their build-up of sleep deficiency began long before launch, as they averaged less than 6·5 hours during the training-intensive SL-90 interval, about one-half hour less actigraphically estimated sleep per night than the average American adult.14;15 and approximately 40 minutes less per night than at R+7. Such pre-flight sleep deficiency makes individuals more vulnerable to the effects of subsequent sleep loss.16
The sleep deficiency we observed prior to spaceflight launch is not dissimilar to sleep loss that commonly occurs with stress prior to important events such as exams, athletic events or difficult work.17 Sleep deficiency is also common in modern society before both business and leisure travel and whenever individuals must manage high workloads, family and other obligations. Such sleep deficiency typically leads to shorter sleep latencies and greater sleep duration in subsequent sleep episodes.18
Despite a history of chronic sleep curtailment, which is used clinically to improve sleep consolidation in insomnia, three-quarters of shuttle and ISS crewmembers chose to use hypnotics to obtain this limited amount of sleep, an approach that has been used to address this problem since the start of the space program. Seconal, a short-acting barbiturate, was added to the inflight medication kit after the Apollo 7 crew reported sleep difficulties.19 Records from 79 early U.S. shuttle missions revealed that sleeping pills accounted for 45% of all medication use by astronauts in space. More doses of medication were taken for sleep than any other indication, with more than 500 unit doses administered.20 Nineteen percent of the shuttle crewmembers on single shift missions and 50% of crewmembers in dual shift operations reported using sleep-promoting medications inflight.20 The percentage of crewmembers using sleep-promoting medications was even higher in the later years of the shuttle program and in the ISS increments measured in this study, even though all missions were single shift, and most ISS crewmembers had individual sleep stations. The reported incidence of sleep-promoting medication use during spaceflight is 20 times greater than the percentage of Americans estimated to use hypnotics at any time in a given year.21
Moreover, astronauts reported taking two doses of sleep medications on approximately 1 in 6 nights when sleep medication was used. Although subjective data from shuttle crewmembers indicate that self-reported sleep latency and quality were improved on nights when sleeping pills were taken, objective data of actigraphically-recorded sleep aboard the shuttle indicate that, on average, sleep efficiency was increased by only 1·3%; (p=0·04) although the 11-minute difference in sleep duration was not statistically significant (p=0·08).
Such a marginal benefit must be balanced against the risks associated with hypnotic use. The ability for a crewmember to optimally perform if awakened from sleep by an emergency alarm may be jeopardized by the use of sleep-promoting pharmaceuticals. Routine use of such medications by crewmembers operating spacecraft are of particular concern, given the FDA warning that patients using sleeping pills “should be cautioned against engaging in hazardous occupations requiring complete mental alertness or motor coordination…including potential impairment of the performance of such activities that may occur the day following ingestion of sedative/hypnotics.”22 This consideration is especially important because all crewmembers on a given mission may be under the influence of a sleep-promoting medication at the same time. Moreover, despite the FDA’s additional warning that patients should, “Use this medicine only when you are able to get a full night's sleep (7 to 8 hours),” crewmembers reported taking a second dose of hypnotic medications—most commonly Ambien® (zolpidem)—often only a few hours before awakening.22 Although crewmembers are encouraged to try such medications on the ground at home at least once prior to their use in flight, such try-outs likely do not involve multiple dosing or dosing with two different medications on the same night. Furthermore, such try-outs do not include any measure of objective efficacy or safety such as what would occur in the case of abrupt awakening during an inflight night time emergency. Zolpidem, for example, produces safety significant performance decrements and impaired balance following awakening from sleep.23 Further, sleep-related eating, sleep walking and sleep driving events have been reported with the use of zolpidem, leading the FDA to require a “black box” warning on all hypnotic medications that driving and performance of other tasks may be impaired in the morning following the use of the such medications: “A variety of abnormal thinking and behavior changes have been reported to occur in association with the use of sedative/hypnotics…. Complex behaviors such as ‘sleep-driving’… have been reported. Amnesia, anxiety and other neuro-psychiatric symptoms may occur unpredictably.”24;25 Yet, sleep medication use was reported on more than half of the nights before EVA were performed. Further, prolonged use of benzodiazepines or benzodiazepine receptor agonists carry the risk of dependency.26
This study is limited by the constraints of operational research. First, as actigraphy does not directly measure sleep stages, we therefore are not able to detect differences in sleep structure associated with sleep-promoting medications. However, actigraphy has shown to be highly correlated with polysomnographically defined sleep timing, even under spaceflight conditions.9;27 Second, we have utilized post flight sleep duration as a comparator, which could be influenced by sleep deficiency during flight. However, preflight intervals would have been an in appropriate baseline reference due to the intensive astronaut training and transmeridian travel schedules that interfered with sleep and began more than one year before flight.
Because this was an observational study taking place during operational spaceflight, we were unable to capture objective measures of cognitive or operational performance or errors. Therefore, we can only infer from research in other operational situations as to how chronic sleep restriction and sleep-promoting medication use might interfere with mission safety and success. The use of sleep medications during spaceflight requires further investigation in order to develop and recommend best practices for crewmembers aboard the ISS and in missions beyond low earth orbit. The minimal improvement we observed in objective measures of sleep duration and efficiency afforded by sleep-promoting medications reveals the need for better counter measures and for further investigation into the stability, absorption and efficacy of such medications inflight.28–30 and the impact of chronic sleep deficiency and hangover effects from sleep-promoting medication use on operationally relevant outcomes, such as robotic operations.
The monitoring and evaluation of sleep duration and timing should continue in future spaceflight missions as a medical requirement including baseline data collection prior to astronaut selection for flight to estimate more accurately individual baseline sleep duration. The development of other effective counter measures to promote sleep inflight is essential, and may include scheduling modifications and behavioral strategies to ensure adequate sleep, which is essential for maintaining health, performance and safety.31–38
Panel: Research in Context
Systematic Review
We conducted a systematic literature review to identify prior studies that reported sleep outcomes during spaceflight. On June 22, 2014 we searched PubMed using the search terms “human,” “astronaut,” and “sleep.” This literature search yielded 88 candidate manuscripts. We narrowed our search to original reports, written in English, that included sleep duration measured objectively (using inflight actigraphy and/or polysomnography) during spaceflight, and that were published during the interval from October 4, 1957 (day Sputnik 1 launched) to June 22, 2014. In cases where multiple manuscripts included data on the same cohort of astronauts, only one manuscript was included.
Six studies met those criteria, with an average of 4 participants in each study (range: 1–7) and a cumulative total of 25 crewmembers studied during that 57-year interval.
Interpretation
This manuscript reports the results of the most extensive study of sleep during spaceflight ever conducted with more than half of all eligible crewmembers completing the study. Unlike prior studies of sleep in space that were conducted on a few crewmembers during single missions, this study includes data from more than 4,000 nights of sleep recording on the ground before and after spaceflight and more than 4,200 nights of sleep recording in space from 64 astronauts aboard the space shuttle and 21 astronauts aboard the International Space Station. The high participation rate and scope of the study enhances the representativeness of the astronaut population and generalizability of the findings.
Supplementary Material
Acknowledgements
The authors thank the shuttle and ISS crewmembers who participated in this study; Eymard Reil; Mia Jacobsen; Lauren Brogna, Liza Burke and Sean Benedix; for data archiving and analysis; Jason Sullivan for technical support; NASA, Lockheed Martin and Wyle, Inc. for logistical support, especially, Marty Bost, Curtis Kershner, Scott Humbert, Karen Lawrence, Pam Baskin, Kristine Ohnesorge and Lauran Johnson; and Drs. Smith L. Johnston, Lauren B. Leveton, and Alexandra Whitmire and Suzanne McCollum and Laura Bollweg at NASA Johnson Space Center for research support. The study was supported by NASA cooperative agreement NCC 9–119. Drs. Barger, Flynn-Evans, Wright and Czeisler and Mr. Ronda were supported in part by the National Space Biomedical Research Institute through NASA NCC 9–58. Drs. Barger and Evans were the recipients of National Heart, Lung and Blood Institute fellowships in the program of training in Sleep, Circadian and Respiratory Neurobiology at Brigham and Women’s Hospital (NHLBI; T32 HL079010). Dr. Walsh was supported through the FÃS Science Challenge Programme, Ireland. We dedicate this paper to the memory of crewmembers lost aboard STS-107.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Study concept and design: Barger, Flynn-Evans, Ronda, Wright, Czeisler
Data collection: Barger, Flynn-Evans, Ronda, Wright
Data analysis and interpretation: Barger, Flynn-Evans, Kubey, Walsh, Ronda, Wang, Wright, Czeisler
Drafting of the manuscript: Barger, Flynn-Evans, Wright, Czeisler
Critical revision of the manuscript for important intellectual content: Barger, Flynn-Evans, Kubey, Walsh, Ronda, Wang, Wright, Czeisler
Statistical analysis: Barger, Flynn-Evans, Wang
Obtained funding: Barger, Wright, Czeisler
Administrative, technical, or material support: Barger, Flynn-Evans, Kubey, Walsh, Ronda, Wang, Wright, Czeisler
Study supervision: Barger, Flynn-Evans, Wright, Czeisler
Conflicts of Interest
Dr. Barger has previously received research support from Cephalon, Inc., non-public sponsors of research. She consults for Alertness Solutions and San Jose State University Foundation.
Dr. Flynn-Evans is now an employee of NASA Ames Research Center. This research was completed before she moved from Brigham and Women’s Hospital to NASA Ames..
Dr. Kubey has a patent, REM-Sleep Directed Visual Alarm System and Method, issued.
Dr. Walsh reports grants from Fujitsu Ireland and personal fees from Irish Centre for Manufacturing Research, outside the submitted work.
Mr. Ronda has nothing to disclose.
Dr. Wang has no conflicts to report.
Dr. Wright reports grants from NASA, during the conduct of the study; grants from Philips, Inc, personal fees from Takeda Pharmaceuticals, personal fees from Zeo, Inc, personal fees from Northwestern University American Waterways Operators Towboat Project, outside the submitted work.
Dr. Czeisler has received consulting fees from or served as a paid member of scientific advisory boards for: Teva Pharmaceutical Industries Ltd.; Koninklijke Philips Electronics, N.V.; Purdue Pharma LP; and Vanda Pharmaceuticals, Inc. Dr. Czeisler owns an equity interest in Vanda Pharmaceuticals, Inc. and receives royalties and research support from Philips Respironics, Inc. The Harvard Medical School Sleep and Health Education Program has received Educational Grant funding from Cephalon, Inc., Takeda Pharmaceuticals, Sanofi-Aventis, Inc. and Sepracor, Inc. Dr. Czeisler is the incumbent of an endowed professorship provided to Harvard University by Cephalon, Inc. and holds a number of process patents in the field of sleep/circadian rhythms (e.g., photic resetting of the human circadian pacemaker). Since 1985, Dr. Czeisler has also served as an expert witness on various legal cases related to sleep and/or circadian rhythms.
References
- 1.National Aeronautics and Space Administration. Wide Awake on the Sea of Tranquility. [Accessed April 12, 2013];NASA's Apollo Chronicles. 2006 Jul 20; http://www.nasa.gov/exploration/home/19jul_seaoftranquillity.html.
- 2.National Institutes of Health Sleep Disorders Research Plan. National Center on Sleep Disorders Research, National Institutes of Health. 2011 Nov [Google Scholar]
- 3.Czeisler CA. Impact of sleepiness and sleep deficiency on public health--utility of biomarkers. J Clin Sleep Med. 2013;7:S6–S8. doi: 10.5664/JCSM.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aldershot, Great Britian: Ashgate Publishing Company; 2003. A human error approach to aviation accident analysis: the human factors analysis and classification system. [Google Scholar]
- 5.Allen CS, Denham SA. International Space Station Acoustics – A Status Report. 41st International Conference on Environmental Systems; 17 – 21 July 2011; Portland, Oregon. [Google Scholar]
- 6.Stuster J. Behavioral issues associated with long-duration space expeditions: review and analysis of astronaut journals. Houston, TX: Johnson Space Center; 2010. NASA/TM-2010-216130. [Google Scholar]
- 7.Santy PA, Kapanka H, Davis JR, Stewart DF. Analysis of sleep on shuttle missions. Aviat Space Environ Med. 1988;59:1094–1097. [PubMed] [Google Scholar]
- 8.Monk TH, Buysse DJ, Billy BD, Kennedy KS, Willrich LM. Sleep and circadian rhythms in four orbiting astronauts. J Biol Rhythms. 1998;13:188–201. doi: 10.1177/074873098129000039. [DOI] [PubMed] [Google Scholar]
- 9.Dijk DJ, Neri DF, Wyatt JK, et al. Sleep, performance, circadian rhythms, and light-dark cycles during two space shuttle flights. Am J Physiol. 2001;281:R1647–R1664. doi: 10.1152/ajpregu.2001.281.5.R1647. [DOI] [PubMed] [Google Scholar]
- 10.NASA International Space Station Program. Generic Groundrules, Requirements, and Constraints Part 1: Strategic and Tactical Planning. Revision G Incorporates DCN 063. Johnson Space Center, NASA. NNJ10GA20B. 2012. [Google Scholar]
- 11.Kelly T, Hienz R, Zacone T, Wurster R, Brady J. Crewmember performance before, during and after spaceflight. J Exp Anal Behav. 2005;84:227–241. doi: 10.1901/jeab.2005.77-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gundel A, Polyakov VV, Zulley J. The alteration of human sleep and circadian rhythms during spaceflight. J Sleep Res. 1997;6:1–8. doi: 10.1046/j.1365-2869.1997.00028.x. [DOI] [PubMed] [Google Scholar]
- 13.Achenbach J. The skies. The limits. [Accessed on 14 Oct 2013];The Washington Post. 2013 http://www.washingtonpost.com/sf/national/2013/09/14/the-skies-the-limits/?hpid=z5. [Google Scholar]
- 14.Ertel K, Berkman L, Buxton O. Socioeconomic status, occupational characteristics and sleep duration in African/Caribbean immigrants and US white health care workers. Sleep. 2011;34:509–518. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berkman L, Buxton O, Erkel KOC. Managers' practices related to work-family balance precict employee cardiovascular risk and sleep duration in extended care settings. J of Occup Health Psychol. 2010;15:316–329. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rupp T, Wesensten NJ, Balkin T. Sleep history affects task acquisition during subsequent sleep restriction and recovery. J Sleep Res. 2010;19:289–297. doi: 10.1111/j.1365-2869.2009.00800.x. [DOI] [PubMed] [Google Scholar]
- 17.Kecklund G, Akerstedt T. Apprehension of the subsequent working day is associated with a low amount of slow wave sleep. Biol Psychol. 2004 Apr;66(2):169–176. doi: 10.1016/j.biopsycho.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Akerstedt T, Kecklund G, Ingre M, Lekander M, Axelsson J. Sleep homeostasis during repeated sleep restriction and recovery: support from EEG dynamics. Sleep. 2009 Feb;32(2):217–222. doi: 10.1093/sleep/32.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkins W, Zieglschmid J. Johnston R, Dietlein L, Berry C, editors. Chapter 1. Clinical aspects of crew health. SP-368 Biomedical Results of Apollo. Lyndon B. Johnson Space Center. 1975 http://history/nasa.gove/SP-368/s2ch1.htm.
- 20.Putcha L, Berens KL, Marshburn TH, Ortega HJ, Billica RD. Pharmaceutical use by U.S. astronauts on space shuttle missions. Aviat Space Environ Med. 1999;70:705–708. [PubMed] [Google Scholar]
- 21.Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medicatins for insomnia: NHANES 1999–2010. Sleep. 2014;37:343–349. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zolpidem [package insert] Sanofi-Aventis, Bridgewater, NJ: 2012. May, [Google Scholar]
- 23.Frey DJ, Ortega JD, Wiseman C, Farley CT, Wright KP., Jr Influence of zolpidem on balance and cognition during night time awakening: a randomized placebo controlled trial. J Am Geriatr Soc. 2011;59:73–81. doi: 10.1111/j.1532-5415.2010.03229.x. [DOI] [PubMed] [Google Scholar]
- 24.US Food and Drug Administration. US Food and Drug Administration. FDA Consumer Health Information; 2013. Jan, Some sleep drugs can impair driving. ( http://www.fda.gov/forconsumers/consumerupdates/ucm322743.htm) [Google Scholar]
- 25.Hoque R, Chesson AL., Jr Zolpidem-induced sleepwalking, sleep related eating disorder, and sleep-driving; fluorine-18-flourodeoxyglucose positron emission tomography analysis, and a literature review of other unexpected clinical effects of zolpiem. J Clin Sleep Med. 2009;5:471–476. [PMC free article] [PubMed] [Google Scholar]
- 26.Clay E, Falissard B, Moore N, Toumi M. Contribution of prolonged-release melatonin and anti-benzodiazepine campaigns to the reduction of benzodiazepine and Z-drugs consumption in nine European countries. Eur J Clin Pharmacol. 2013 Apr;69(4):1–10. doi: 10.1007/s00228-012-1424-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Monk TH, Buysse DJ, Rose LR. Wrist actigraphic measures of sleep in space. Sleep. 1999;22:948–954. [PubMed] [Google Scholar]
- 28.Tietze K, Putcha L. Factors affecting drug bioavailability in space. J Clin Psychopharmacol. 1994;34:671–676. doi: 10.1002/j.1552-4604.1994.tb02022.x. [DOI] [PubMed] [Google Scholar]
- 29.Du B, Daniels V, Vaksman Z, Boyd J, Crady C, Putcha L. Evaluation of physical and chemical changes in pharmaceuticals flown on space missions. AAPS J. 2011;13:299–308. doi: 10.1208/s12248-011-9270-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Putcha L, Cintron NM. Pharmacokinetic consequences of spaceflight. Ann NY Acad Sci. 1991;618:615–618. doi: 10.1111/j.1749-6632.1991.tb27292.x. [DOI] [PubMed] [Google Scholar]
- 31.Colten HR, Alteveogt BM, editors. Institute of Medicine. Sleep disorders and sleep deprivation: An unmet public health problem. Washington, D.C.: National Academies Press; 2006. ISBN:0-309-66012-2-1-500. [PubMed] [Google Scholar]
- 32.Institute of Medicine. Board on Health Care Services. Washington, D.C.: National Academies Press; 2008. Resident duty hours: enhancing sleep, supervision, and safety. [PubMed] [Google Scholar]
- 33.Hursh SR, Raslear TG, Kaye AS, Farzone JF. Validation and Calibration of a Fatigue Assessment Tool for Railroad Work Schedules, Summary Report. Washington, DC: U.S. Department of Transportation Federal Railroad Administration; 2006. [Google Scholar]
- 34.Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296:1055–1062. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 35.Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 36.Barger LK, Ayas NT, Cade BE, et al. Impact of Extended-Duration Shifts on Medical Errors, Adverse Events, and Attentional Failures. PLoS Med. 2006;3:0001–0009. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 38.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.