Abstract
Atelectasis is a pulmonary disorder that lengthens the hospitalization time of newborns in intensive care units, resulting in increased morbidity among these infants. High-flow nasal cannulae have been used in newborns to prevent atelectasis and/or expand pulmonary regions affected by atelectasis; however, to date, no evidence-based data regarding this approach have been reported. In this paper, we report on the cases of two male newborn patients. The first and second patients described in this report were hospitalized for a neurosurgical procedure and the treatment of abdominal disease, respectively, and were subjected to invasive mechanical ventilation for 4 and 36 days, respectively. After extubation, these patients continued receiving oxygen therapy but experienced clinical and radiological worsening typical of atelectasis. In both cases, by 24 hours after the implantation of an high-flow nasal cannulae to provide noninvasive support, radiological examinations revealed the complete resolution of atelectasis. In these cases, the use of an high-flow nasal cannulae was effective in reversing atelectasis. Thus, this approach may be utilized as a supplemental noninvasive ventilatory therapy to avoid unnecessary intubation.
Keywords: Infant, newborn; Pulmonary atelectasis/rehabilitation; Noninvasive ventilation; Positive-pressure breathing; Case reports
Abstract
A formação de atelectasias é um dos distúrbios pulmonares responsável pelo maior tempo de internação dos recém-nascidos nas unidades de terapias intensivas e pelo consequente aumento da morbidade. O cateter nasal de alto fluxo tem sido utilizado na faixa etária neonatal, para evitar e/ou expandir áreas pulmonares atelectasiadas, mesmo que até o momento não existam estudos baseados em evidência. Relatamos os casos de dois pacientes do sexo masculino internados por doença neurocirúrgica e abdominal submetidos à ventilação pulmonar mecânica invasiva por 4 e 36 dias, respectivamente. Após a extubação, foram mantidos em oxigenioterapia, quando, então, ambos apresentaram piora clínica e radiológica compatível com atelectasia. Após 24 horas de instalado o cateter nasal de alto fluxo como suporte não invasivo, novos exames radiológicos mostraram a reversão completa da atelectasia. O uso do cateter de alto fluxo mostrou-se eficaz na reversão de atelectasias, podendo ser utilizada como mais uma das terapias ventilatórias não invasivas, evitando, assim, nova intubação.
INTRODUCTION
Atelectasis is a pulmonary disorder that often occurs after extubation, particularly during patients' postoperative periods. In these patients, underlying diseases can be associated with other conditions, resulting in respiratory complications that include bloating, antalgic positioning, shallow breathing, and a need for optimized analgesia. Atelectasis is associated with increased hospitalization time for newborns (NBs) admitted to neonatal intensive care units (NICUs); the resulting prolonged hospitalization duration can lead to increased morbidity among these NBs.(1,2)
Respiratory therapy is one resource used to resolve atelectasis. This treatment involves not only the use of specific techniques for the removal of bronchial secretions but also the application of positive end-expiratory pressure (PEEP) in the airways to prevent collapses or expand collapsed regions, thereby improving gas exchange and reducing respiratory effort.(2)
In addition to the aforementioned techniques, the use of a high-flow nasal cannula (HFNC) can prevent the complete occlusion of the nostrils and maintain the perfusion of the nasal mucosa. These effects may be achieved because an HFNC has a smaller internal diameter than a standard nasal catheter. Gases provided using HFNCs (at a flow rate of 2 to 8 L/min for neonates) are heated and humidified to reduce bleeding and pulmonary hemorrhage by preventing the heat loss and drying of the mucosa.(3,4)
Therefore, HFNCs can be used to treat the same diseases for which continuous positive airway pressure (CPAP) is indicated, such as apnea of prematurity, and to transition from invasive mechanical ventilation (IMV) to noninvasive mechanical ventilation.(5)
The objective of this study was to report on the use of an HFNC as an alternative approach for the resolution of post-extubation atelectasis.
CASE REPORT
The two evaluated NBs were extubated according to a ventilator weaning protocol and placed on oxygen therapy (via nebulization) with sustained physical therapy. After the failure of conventional ventilatory support, a noninvasive ventilatory support (Fisher and Paykel Healthcare, Irvine, California, USA) was chosen. This nasal cannula is specifically designed for neonates and features less unheated space than other cannulae, breathing circuits with spiral wire technology, and an MR850 humidifier that ensures an ideal gas temperature.
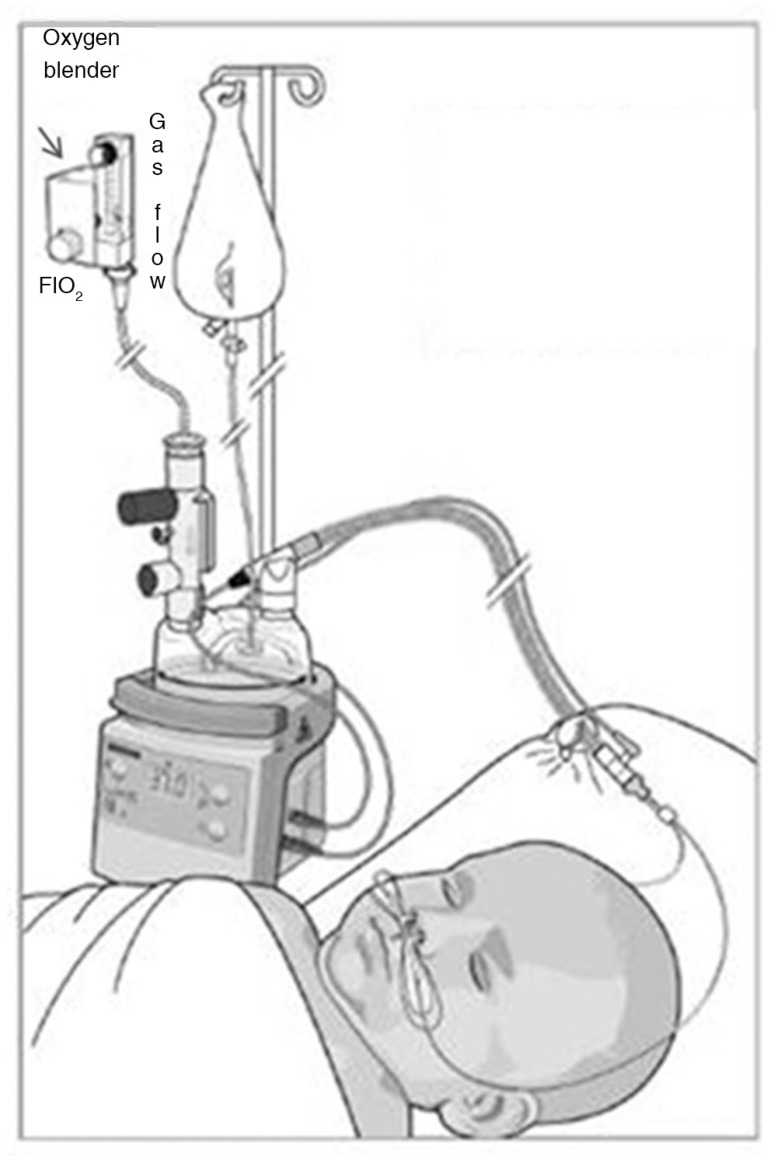
In the present study, the oxygen blender from a Newport Medical E100 ventilator (Plainfield, Indiana, USA) was coupled to oxygen and a compressed air system. As illustrated in figure 1, this configuration allowed for the intake of the desired fraction of inhaled oxygen (FiO2). After mixing, the gas circulated through the flow meter of the ventilator. Based on the gestational age and weight of each NB, gas flow was adjusted to 7L/min in accordance with the manufacturer's instructions.
Figure 1.
A schematic of a high-flow nasal cannula circuit.
FiO2 - fraction of inhaled oxygen.
The NB patients were monitored with a Dixthal Healthcare Dx 2020 multiparameter monitor (Amsterdam, the Netherlands).
Case 1
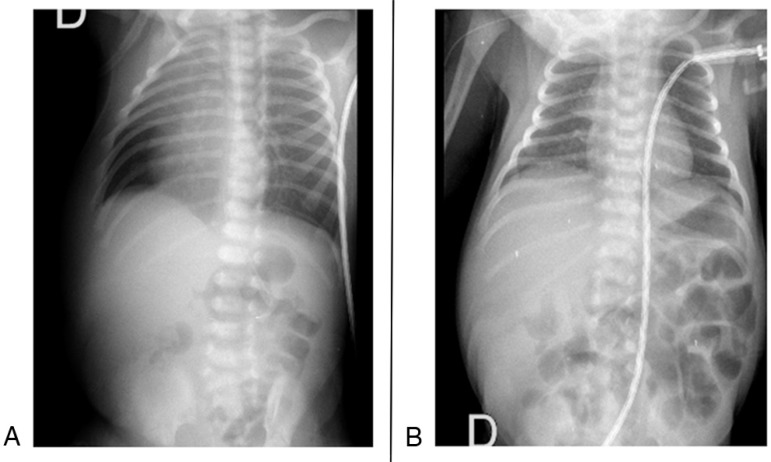
We examined a late-preterm male NB with a gestational age of 35 weeks. At birth, this NB weighed 2,810g, which was adequate given his gestational age. He was admitted to the NICU at the age of 3 days. The patient presented with septic shock and required invasive ventilatory and hemodynamic support as well as the administration of broad-spectrum antibiotics. The patient, who presented with myelomeningocele as the underlying disease, remained intubated for 4 days to treat infection and preserve airways. Ventilator weaning was performed quickly because no pulmonary changes were observed. Pre-extubation blood gas analysis results indicated a pH of 7.39, a partial pressure of carbon dioxide (pCO2) of 25.8, a partial pressure of oxygen (pO2) of 190, a bicarbonate (HCO3-) concentration of 18mEq/L, a base excess (BE) of -1.5, and an oxygen saturation (SatO2) of 99%. The patient was extubated, and treatment with nebulized oxygen was immediately provided. After 6 hours, the patient developed tachydyspnea and exhibited decreased pulse oxygen saturation, with a vesicular murmur in the right hemithorax. A plain chest radiograph revealed that the upper two-thirds of the right lung was opaque (Figure 2A).
Figure 2.
(A) A bedside anteroposterior simple chest radiograph indicating opacity of the top half of the lung and rightward deviation of the mediastinum and trachea. (B) A bedside anteroposterior chest radiograph revealing the improved resolution of the anterior opacity in the upper half of the right chest and the centralization of the trachea and mediastinum.
An HFNC system with a gas flow of 7L/min and an FiO2 of 30% was implanted in the patient. After 24 hours, a new plain chest radiograph indicated that atelectasis had been completely resolved (Figure 2B); therefore, the use of the HFNC system was suspended.
Case 2
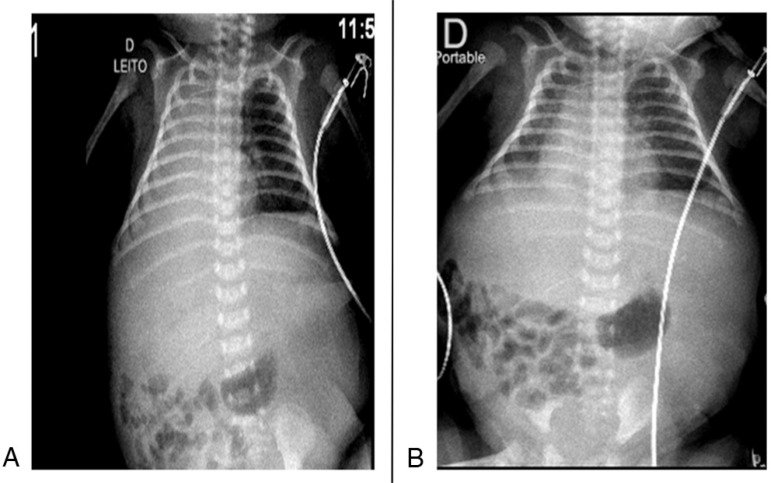
We evaluated a full-term male NB with a gestational age of 37 weeks. At birth, this patient weighed 3,380g, which was appropriate for his gestational age. The patient's mother was hypertensive, and the patient not only had been diagnosed with meconium peritonitis and intrauterine intestinal perforation but also exhibited ascites and anasarca. The patient underwent various surgical procedures that compromised his respiratory mechanics and hampered early weaning from IMV. After the patient was clinically stabilized, his arterial blood analysis results (pH=7.41, pCO2=45.8, pO2=67.9, HCO3=27mEq/L, BE=-2, and SatO2=92%) indicated that he was eligible for extubation. After 36 days of orotracheal intubation, extubation was performed, and treatment with nebulized oxygen was provided. At 6 hours after extubation, a plain chest radiograph produced images consistent with atelectasis throughout the right hemithorax (Figure 3A). An HFNC system with a gas flow of 7L/min and an FiO2 of 30% was implanted in the patient. A chest radiograph obtained after 24 hours of HFNC treatment revealed no atelectasis; therefore, the use of the HFNC system was suspended (Figure 3B).
Figure 3.
(A) A bedside anteroposterior simple chest radiograph indicating opacity of the entire right hemithorax. (B) A bedside anteroposterior simple chest radiograph revealing a lack of right lung opacity.
DISCUSSION
In this paper, we report on the successful use of high-flow nasal cannulae for the treatment of extensive post-extubation atelectasis in two infants who underwent surgical treatment.
Post-extubation atelectasis typically occurs within the first 24 hours after extubation in 10-30% of patients who have been subjected to IMV. In these cases, atelectasis is generally treated by reintubation or by providing noninvasive ventilatory support.
When providing non-invasive ventilation to neonates, we rely on the use of CPAP, which can be implemented via nasal prongs. However, this intervention can cause nasal septal injury and discomfort to the patient.(1,3,4,6)
The use of an HFNC is another approach that can be adopted for applying positive pressure. However, this approach is not yet routinely used in NICUs despite prior reports indicating positive HFNC-related results.(3-5,7) Among neonates, HFNCs were first used in preterm infants (PTIs) in 2001 for the treatment of apnea of prematurity; since that time, HFNC systems have become an alternative to traditional non-invasive respiratory support.(8)
According to Dysart et al.,(3) the generation of PEEP through HFNC-based support rather than traditional approaches produces improved pulmonary mechanics, reduced dead space, decreased inspiratory resistance, and consequent improvement in patient oxygenation.
It is challenging to compare HFNC systems with nasal CPAP because of difficulties in measuring the pressures generated by various approaches and the existence of divergent data in studies that have measured gas pressure at different locations. However, the conclusions of these studies are similar. In particular, these investigations have indicated that both approaches are effective and that the pressure generated by different treatments can be influenced by several factors, including the ratio of catheter size to nostril size and the need to ensure that the patient's mouth remains closed. However, certain studies have reported better tolerance for an HFNC than for CPAP.(6,8,9)
In a prospective randomized study, Miller and Dowd(9) compared two types of HFNC systems with respect to the success of tracheal extubation. In this comparison, 39 PTIs were classified into 2 groups; the Fisher and Paykel (FP) system was used for one group, and the Vapotherm 2000i (VP) system was used for the other group. Prong size was chosen in accordance with inner nostril diameter. A gas flow of 6L/min and an FiO2 of ≤ 30% were utilized, with weaning of the HFNC by 1L/min every 24 hours based either on peripheral oxygen saturation and a PaCO2 of ≤45mmHg or on transcutaneous carbon dioxide monitoring. However, when any level of respiratory distress was detected, weaning was suspended, and gas flow was returned to initial values. Extubation failure was regarded as the occurrence of respiratory distress in the first 72 hours after extubation. All of the evaluated parameters were statistically similar for the two HFNC systems, with the exception of the cost of support, which was lower for the FP system than for the VP system.
A review by Wilkinson et al.(10) described 4 randomized studies involving PTIs (with gestational ages <37 weeks). Subsets of these infants received respiratory support after birth. In addition, these patients were treated with a high gas flow (>1L/min) of pure or mixed oxygen and were subjected to various alternative interventions, including headbox oxygen, low-flow nasal cannulae, nasal CPAP, and HFNCs. The authors of the review concluded that there was a lack of scientific evidence regarding the effectiveness of HFNC for respiratory support in PTIs and that the number of reintubations was higher among PTIs treated with HFNCs than among PTIs treated with CPAP.
Although the extant literature includes controversial findings regarding HFNCs, the two cases described in this study benefited from the use of HFNCs, which allowed for the resolution of post-extubation atelectasis within the first 24 hours after the initiation of treatment. Moreover, HFNCs are well tolerated by patients, particularly among patients who are recovering from neurosurgery and/or abdominal surgery.
CONCLUSION
The use of an high-flow nasal cannulae was effective and tolerated well by newborn patients, suggesting that this intervention can serve as a complement to physical therapy management in the treatment of post-extubation atelectasis.
Footnotes
Conflicts of Interest: None.
Responsible editor: Ruth Guinsburg
REFERENCES
- 1.Johnson C, Carvalho WB. Atelectasias em pediatria: mecanismos, diagnósticos e tratamento. Rev Assoc Med Bras. 2008;54(5):455–460. doi: 10.1590/s0104-42302008000500021. [DOI] [PubMed] [Google Scholar]
- 2.Bagley CE, Gray PH, Tudehope DI, Flenady V, Sherman AD, Lamont A. Routine neonatal postextubation chest physiotherapy: a randomized controlled trial. J Paediatr Child Health. 2005;41(11):592–597. doi: 10.1111/j.1440-1754.2005.00728.x. [DOI] [PubMed] [Google Scholar]
- 3.Dysart K, Miller TL, Wolfson MR, Shaffer TH. Research in high flow therapy: mechanisms of action. Respir Med. 2009;103(10):1400–1405. doi: 10.1016/j.rmed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Ojha S, Gridley E, Dorling J. Use of heated humidified high-flow nasal cannula oxygen in neonates: a UK wide survey. Acta Paediatr. 2013;102(3):249–253. doi: 10.1111/apa.12090. [DOI] [PubMed] [Google Scholar]
- 5.Ward JJ. High-flow oxygen administration by nasal cannula for adult and perinatal patients. Respir Care. 2013;58(1):98–122. doi: 10.4187/respcare.01941. [DOI] [PubMed] [Google Scholar]
- 6.Lee JH, Rehder KJ, Williford L, Cheifetz IM, Turner DA. Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med. 2013;39(2):247–257. doi: 10.1007/s00134-012-2743-5. [DOI] [PubMed] [Google Scholar]
- 7.Sreenan C, Lemke RP, Hudson-Mason A, Osiovich H. High-flow nasal cannulae in the management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics. 2001;107(5):1081–1083. doi: 10.1542/peds.107.5.1081. [DOI] [PubMed] [Google Scholar]
- 8.Hasan RA, Habib RH. Effects of flow rate and airleak at the nares and mouth opening on positive distending pressure delivery using commercially available high-flow nasal cannula systems: a lung model study. Pediatr Crit Care Med. 2011;12(1):e29–e33. doi: 10.1097/PCC.0b013e3181d9076d. [DOI] [PubMed] [Google Scholar]
- 9.Miller SM, Dowd SA. High-flow nasal cannula and extubation success in the premature infant: a comparison of two modalities. J Perinatol. 2010;30(12):805–808. doi: 10.1038/jp.2010.38. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson D, Andersen C, O'Donnell CP, De Paoli AG. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst Rev. 2011;(5): doi: 10.1002/14651858.CD006405.pub2. [DOI] [PubMed] [Google Scholar]