Abstract
This article presents an oral health (OH) strategy and pilot study focusing on individuals with intellectual and/or developmental disabilities (IDD) living in group homes. The strategy consists of four components: (1) planned action in the form of the behavioral contract and caregiver OH action planning; (2) capacity building through didactic and observation learning training; (3) environmental adaptations consisting of additional oral heath devices and strategies to create a calm atmosphere; and (4) reinforcement by post-training coaching. A pilot study was conducted consisting of pre- and post-assessment data collected one week before and one week after implementing a one-month OH strategy. The study sample comprised 11 group homes with 21 caregivers and 25 residents with IDD from one service organization in a Midwestern city. A process evaluation found high-quality implementation of the OH strategy as measured by dosage, fidelity, and caregiver reactions to implementing the strategy. Using repeated cross-sectional and repeated measures analyses, we found statistically significant positive changes in OH status and oral hygiene practices of residents. Caregiver self-efficacy as a mechanism of change was not adequately evaluated; however, positive change was found in some but not all types of caregiver OH support that were assessed. Lessons learned from implementing the pilot study intervention and evaluation are discussed, as are the next steps in conducting an efficacy study of the OH strategy.
Keywords: Oral health, Health disparities, Intellectual and developmental disability, Intervention design, Process and outcome evaluation
1. Background1
It is well known that oral health (OH) problems continue to exist among children and adults across the world (Petersen, 2004; Petersen, Bourgeois, Ogawa, Estupinan-Day, & Ndiaye, 2005). Further, poor OH has been linked to a variety of physical health problems, including respiratory, cardiovascular, and endocrine disease (Rautemaa, Lauhio, Cullinan, & Seymour, 2007). Notably, OH is impacted by good oral hygiene practices that reduce the development of caries (cavities) (Ashkenazi, Bidoosi, & Levin, 2014) and periodontal (gum) disease (Araujo, Gusmao, Batista, & Cimoes, 2010). Poor OH and dental hygiene are particularly prevalent among vulnerable populations such as individuals with intellectual and developmental disabilities (IDD). These individuals are more likely to have poorer oral hygiene, increased decay, and increased periodontal disease than the general population—a significant health disparity (Anders & Davis, 2010; Girgis, 1985; Glassman & Miller, 2003; Hood, Dean, Cornett, & Boggs, 2001; Lindemann, Zaschel-Grob, Opp, Lewis, & Lewis, 2001; Pezzementi & Fisher, 2005; Reid, Chenette, & Macek, 2003).
This study focuses on the OH of individuals with IDD and efforts to improve oral hygiene practices among this population who live in community-based group homes (hereinafter referred to as residents with IDD or residents). Historically, individuals with IDD either lived at home or were placed in large state institutions with fully staffed medical and dental facilities and stable, well-trained workers. However, over the past several decades, efforts to deinstitutionalize these individuals and place them in smaller community residences, commonly referred to as group homes, have been successful. Although the overall quality of life may have been improved for this vulnerable population, their access to dental care and trained caregivers may have become more limited and their OH may have suffered (Stanfield, Scully, Davison, & Porter, 2003). Most individuals with IDD are insured by Medicaid, which many dentists do not accept. In addition, many dentists do not believe they are adequately trained to treat special-needs patients (Dao, Zwetchkenbaum, & Inglehart, 2005; Waldman & Perlman, 2002). Among dentists who do treat individuals with IDD, 99% have identified poor oral hygiene as the single greatest threat to their patient’s OH (Hood, Dean, Cornett, & Boggs, 2001).
Unfortunately, the OH of this population is compromised by their lack of preventive dental treatment and by their inability to adequately brush and/or floss their own teeth. Thus, the oral hygiene provided or supervised by caregivers is critical to maintaining OH and reducing the need for extensive restoration or extraction of teeth. Providing oral care for individuals with IDD is challenging because they may have physical impairments and may exhibit uncooperative behaviors (Perlman, 1991). Caregivers often only clean the anterior teeth, ignoring the posterior teeth and causing the posterior oropharyngeal area to be at risk for colonization with bacteria and infection (Glassman & Miller, 2003; Tesini & Fenton, 1994; Vigild, Brinck, & Christensen, 1993).
There has been limited effort to develop and evaluate promotional strategies to improve the oral hygiene and OH of this vulnerable population living in group homes (Avenali, Guerra, Cipriano, Corridore, & Ottolenghi, 2011; Faulks & Hennequin, 2000; Fickert & Ross, 2012; Glassman & Miller, 2006). Systematic reviews of OH promotion educational interventions conducted with other populations have produced diverse findings, but generally, they have produced short-term reductions in plaque and gingival bleeding (Watt & Marinho, 2005). What is not known is the relevance of a short-term reduction to the sustained impact on oral health. This void in the literature and practice led to the pilot study of the OH strategy being presented in preparation for a larger randomized controlled trial (RCT). We used the National Institute of Dental and Craniofacial Research (NIDCR) clinical trial planning grant mechanism and the National Institutes of Health (NIH) multiple-principal-investigator (PI) approach to take advantage of the expertise of two PIs – one clinical researcher in dentistry and one social and behavioral scientist. This approach allowed us to develop and pilot test a social science, theoretically based intervention strategy focusing on OH.
2.0 The Oral Health Strategy
2.1 Conceptual view
Figure 1 shows our conceptual framework, which assumes interrelationships between the OH strategy and its proximal, intermediate, and distal outcomes. Moving left to right in the figure, we posit that the OH strategy described in the next subsection will affect caregiver self-efficacy and OH support, which are proximal outcomes. Self-efficacy is an important mechanism of behavioral change in social cognitive theory (Bandura, 2004). We also identified in a qualitative assessment that caregiver OH support (oral hygiene, environmental adaptations, rewards, dietary supervision, and monitoring) may serve as an additional important mechanism of change (Authors, 2013). Further, the PIs posited that impacting these two mechanisms of change would improve oral hygiene practices (intermediate outcomes) of group home residents with IDD and subsequently improve their overall OH (distal outcome).
Figure 1.
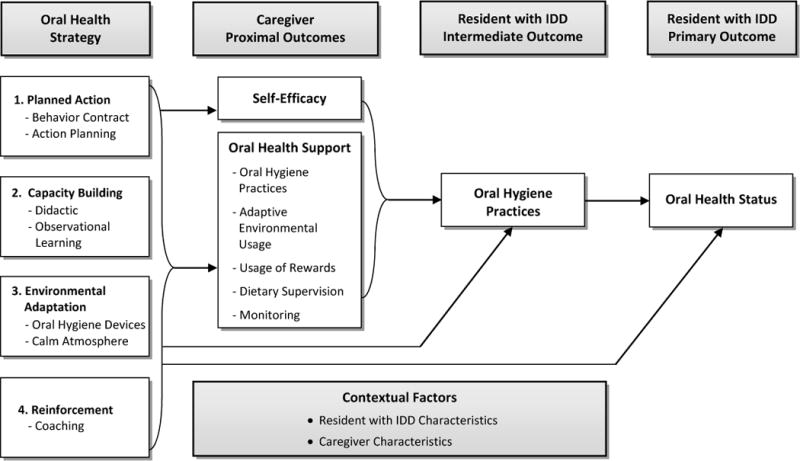
Conceptual View of an Oral Health Strategy for Residents with IDD Living in Group Homes
Possibly, not all OH strategy effects are mediated by caregivers’ self-efficacy and OH support. Therefore, we posited direct effects of the intervention on residents’ oral hygiene practices and residents’ OH status. Finally, we believe that contextual factors consisting of characteristics of residents with IDD and their caregivers may be associated with the outcomes; therefore, they should be statistically controlled in a larger controlled trial with a larger sample.
2.2 Designing and implementing the oral health strategy
We assessed social, epidemiological, behavioral, environmental, educational, and ecological factors that inform the development of an intervention with underlying behavioral change theory assumptions presented in the conceptual framework (Authors, 2013). This assessment identified a set of enabling factors that are said to facilitate or impede individual behavior change (Greene & Kreuter, 2005). It is helpful to view enabling factors as a combination of forces that, taken together, influence the degree of initiation and continuation of some action. First, our assessment identified an enabling factor concerning an intervention component that motivates participants to take a given action. A second enabling factor is caregivers’ skills to provide OH services to residents with IDD in group homes. A third enabling factor stemming from our assessment uncovered the need for environmental adaptations in the form of oral hygiene devices and mechanisms to create a calming atmosphere that caregivers do not have available. Fourth, we identified reinforcement and potential reward of the action taken as an important enabling factor. Based on these enabling factors, we designed an OH strategy with four integrated intervention components: (1) planned action, (2) capacity building, (3) environmental adaptation, and (4) reinforcement/coaching.
Planned action involved obtaining agreement to a behavioral contract and engaging in action planning for OH. For the pilot study, a dental hygienist or the dental PI presented a behavioral contract to the study caregivers who were asked to participate in a program to improve the OH of the residents with IDD in their respective group homes. At the end of OH implementation, the dental hygienist met with each caregiver who agreed to the behavioral contract to review and evaluate the extent to which he or she met the expectations of the contract. Along with presenting the behavioral contract, the dental hygienist worked with each caregiver in developing an OH action plan for each of his/her residents. An action plan template was used in the initial training session that included actions targeting oral hygiene, the use of dental devices, strategies to create a calm atmosphere and improve cooperation, dietary concerns, and monitoring of the residents’ practices. Importantly, the plan included ways to motivate the residents by using one or more of the following: rewards, encouragement, praise, or a disclosing solution to show residents the amount of plaque on their teeth. Mechanisms to cope with resistant behavior included taking small steps toward OH, using reinforcements, limiting the setting, finding another time or location, or seeing if another caregiver had better cooperation with the resident. The physical and behavioral challenges to OH for each resident are also described in the plan. Finally, the OH plan specified what steps the caregiver and resident should work on before the first coaching visit.
Capacity building
The capacity-building component involved two types of training. First, caregivers were provided cognitive and skills training via a DVD video that provided (1) desired oral hygiene practices for residents with IDD, (2) interpersonal strategies such as desensitization, (3) the use of rewards, (4) dietary supervision, and (5) monitoring goals for OH care. This didactic training was adapted from the Overcoming Obstacles program (Glassman & Miller, 2006) and included a PowerPoint presentation developed by the Dental PI and a 20-minute DVD demonstrating oral hygiene and behavioral management techniques. This portion of the training provided caregivers with basic knowledge on the issue of OH among this population and how they could help. Second, immediately following the didactic portion, the dental hygienist provided a demonstration, working with at least one caregiver and one consented resident in the home. This portion of the training provided opportunities for observational learning. The caregivers were encouraged to model the same dental hygiene practices with the residents while the hygienist watched and offered praise, reassurance, and suggestions for improvement. The majority of caregivers in the pilot test participated in the capacity building activities as described in section 3.4 below and Table 2.
Table 2.
Implementation Quality (Dosage & Fidelity) by Key Elements of the Oral Health Strategy (N = 21 Caregivers (CG))
| Intervention Component | Dosage | Fidelity (Adherence) |
|---|---|---|
|
| ||
| Planned Action | ||
|
| ||
| Behavioral Contract |
|
|
|
| ||
| Action Planning (Oral Health action plan) |
|
|
|
| ||
| Capacity Building | ||
|
| ||
| Didactic Training (100% of key points completely covered in PowerPoint and video) |
|
|
|
| ||
| Observational Learning (Dentoform) (100% of oral hygiene practices key points completely covered) |
|
|
|
| ||
| Observational Learning (Oral Hygiene Demo with Resident) |
|
|
|
| ||
| Environmental Adaptation | ||
|
| ||
| Dental Devices (100% of key points completely covered) |
|
|
|
| ||
| Strategies for a calm atmosphere (90% of strategy adaptation key points completely covered) |
|
|
|
| ||
| Reinforcement | ||
|
| ||
| Coaching |
|
|
Note: CG = Caregivers
Environmental adaptation
A variety of adaptations to the group home environment were offered to caregivers. These adaptations included (1) providing additional dental devices such as special toothbrushes and pastes, floss aids, mouth props, rinses and plaque-disclosing solution and (2) creating a calming atmosphere by changing the location of oral hygiene practices (e.g., from the bathroom to the kitchen) or position (e.g., from standing to sitting) and using behavioral strategies to reduce resident stress. The dental hygienist worked with each caregiver throughout the intervention to find and evaluate environmental adaptations to provide the greatest benefit for the resident, thereby increasing participation and cooperation.
Reinforcement
Action planning and oral hygiene skill building continued in the first in-home coaching session that lasted 1½ to 2 hours. The dental hygienist inquired about any problems the caregivers had encountered; modified any needed dental hygiene goals for each resident; suggested different behavioral techniques, products, or locations where oral hygiene might be performed; and reviewed and updated the OH care plan for each resident with IDD.
In a second in-home coaching session, the dental hygienist reviewed issues and challenges regarding the OH care plan and discussed with caregivers some ways to improve supervising and/or providing oral hygiene practices, supervising the diets of residents with IDD, and planning and monitoring the OH of residents with IDD. This second coaching session lasted approximately 30 minutes. For the pilot study, the two coaching visits occurred 2 weeks apart over the 1-month intervention.
3.0 Pilot Study Methods
3.1 Research questions
In our pilot study, we examined changes in the proximal, intermediate, and distal outcomes and the quality of implementation of the OH strategy. Our research questions follow.
What are the changes in the distal outcomes (OH status of residents with IDD)?
What are the changes in intermediate outcomes (oral hygiene practices of residents with IDD)?
What are the changes in proximal outcome (caregiver self-efficacy and caregiver OH support)?
What is the level of implementation quality as measured by dosage, fidelity, and caregiver reactions to implementing the OH strategy?
3.2 Study design and sample
The design for our pilot study was a pre- and a post-intervention without a control group. Outcome data were collected via oral examinations, a caregiver self-administered questionnaire, a daily checklist, and video camera observation. Process data measuring dosage, fidelity, and caregiver reactions were collected by a self-administered questionnaire and a video camera at the post-assessment. The Institutional Review Board (IRB) of the University of Louisville reviewed the research and approved the study, including the recruitment methodology, the consent process, and all consent forms for the pilot test of the OH strategy.
Three of the OH strategy components (planned action, capacity building, and environmental adaptation) were pre-tested in one home, but the fourth component (reinforcement) was not pretested due to time constraints. For the pilot test, one part-time dental hygienist under the direction of the dental PI implemented the entire OH strategy in 2 cohorts, first in 7 group homes and then in the remaining 5 group homes. An implementation protocol required documentation of the caregiver’s participation in each intervention component. A form was developed for the hygienist to use in documenting the level of adherence to each planned intervention component. The hygienist also documented whether caregivers made changes in implementing the planned intervention components and the reasons why a change was made.
3.2.1. Recruitment
Recruitment of the participants in the study, persons with IDD and caregivers, was conducted in conjunction with our partner organization. The consent forms approved by the IRB explained the study, including a section on acceptance or rejection of the participant being video recorded. The participants were advised that they could reject being recorded and still be in the study, or if they initially agreed, they could refuse to be video recorded at any time during the study.
Recruitment of the persons with IDD who were their own guardians (approximately 25% of the sample) was done by the research team after staff at the partner organization identified them and provided contact information. The research team met with these individuals in person and explained the study to them in the presence of a staff member of the partner organization. The majority of potential persons with IDD had legally authorized representatives (LARs) who were on record with the partner organization. Staff at the partner organization mailed a letter (approved by the IRB) and a consent form to each LARs. We needed to use this method of recruitment and consent because most of the LARs resided all over the state of Kentucky and face-to-face methods of obtaining consent were not feasible.
Recruitment of caregivers was also done with the assistance of staff from the partner organization who provided contact information for the caregivers. A research team member met with each caregiver in person to fully explain the study, the protections against risk, and his/her rights and responsibilities as a study participant. Caregivers who agreed to participate were asked to sign the consent and HIPAA forms and were given a copy of the consent.
Originally, we attempted to recruit 15 group homes to participate in the study with four group homes dropping out early due to disinterested caregivers or residents moving out (retention rate = 73%). Over a period of 3 months in the 11 recruited homes, we recruited 33 caregivers (direct care staff, not managers) from a sample of 37 to participate in the study, resulting in an 89% consent rate. Of the 33 caregivers who consented, 12 dropped out of the study before the intervention began in their assigned group home, mainly because they were dismissed from employment with the partner organization that was undergoing reorganization throughout the study.
We recruited 36 residents with IDD (5% = younger than age 21 years). Six LARs for the residents declined to provide consent, resulting in 30 consented residents (83% consent rate). Of the 30 consented residents with IDD, 5 moved out of a participating group home before the intervention began.
3.2.2 Intervention retention
Twenty one caregivers provided baseline data but 6 did not provide post intervention data resulting in a retention rate of 76%. Twenty five residents provided baseline data and 25 provided post intervernion data resulting in a 100% retention rate.
3.3 Measures
The study measures included outcomes (distal, intermediate, and proximal outcomes), OH strategy processes for each of the four intervention components, caregivers, and residents with IDD characteristics. We provide operational definitions for these measures and a description of the instruments.
3.3.1 Distal outcomes
Calibration and preparation for use of indices
The dental examiner was trained and calibrated in the oral examination procedures before enrollment began. She was calibrated with a periodontist for both for intra- and inter-examiner error using the periodontist as the “Gold Standard” examiner. The calibration protocol involved three representative subjects being measured twice by each examiner. The dental examiner qualified for the study after she achieved the following criteria established by the Oral Assessment Guide (OAG) and the O’Leary Plaque Index: At least 80% intra- and inter-examiner exact reproducibility plus 95% intra- and inter-examiner reproducibility within ± 1 index unit.
OH status was measured by an oral examination (percentage of plaque and an OH assessment guide score). We operationally defined OH status as evidenced by the percentage of the residents with teeth that had visible plaque after using a disclosing solution. The O’Leary Plaque Control Index (O’Leary, Drake, & Naylor, 1972) provided a score ranging from 0% to 100% of teeth present with visible plaque. Secondarily, we also defined OH using the revised OAG, a visual assessment of eight oropharyngeal areas – gingiva, teeth, voice, saliva, mucous membranes, lips, tongue, and swallow (Andersson, Hallberg, & Renvert, 2002; Eilers, Berger, & Petersen, 1988). Using the OAG, we operationally defined the OH status of the resident with IDD as a score on the OAG, which has a floor of 8 and a ceiling of 24. Whereas the OAG items are usually scored by summing across eight items rated on a scale of 1 = excellent to 3 = poor, we reflected the items such that 0 = poor and 2 = excellent; then, we took the average across these eight items. Inter-rater reliability for the modified OAG used in this study has been reported to produce a Kappa coefficient equal to 0.81–0.94 (Andersson et al., 2002; Gibson et al., 2010).
3.3.2 Intermediate outcome
Six measures of oral hygiene practices of residents with IDD were constructed as a new index because no index or scale specifically for this population could be found in the literature. First, we used five single indicators as measures of resident oral hygiene practices (percentage of residents using a disclosing solution, toothbrush, dental floss, and/or mouth rinse across observations), and whether the average number of minutes spent on daily oral hygiene activities was above or below the mean. These indicators were then summed to create an emergent, variable measuring oral hygiene practices. Bollen and Lennox (1991) discussed emergent versus latent variables and why an emergent variable does not require a psychometric analysis.
3.3.3 Proximal outcomes
Caregiver self-efficacy was measured by a seven-item scale on how confident caregivers felt in their ability to perform the following: (1) assisting residents with their oral hygiene practices, (2) influencing residents’ oral hygiene practices, (3) supervising residents’ oral hygiene practices, (4) supervising residents’ diet to reduce his/her sugar intake, (5) using new alternative devices that make oral hygiene easier for residents, (6) using new alternative strategies or techniques to improve residents’ cooperation with oral hygiene, and (7) keeping records of residents’ oral hygiene practices. The response categories for these items were: 0 = not at all likely, 1 = not very likely, 2 = somewhat likely or 3 = likely. The alpha reliability is 0.70. Self-efficacy data were captured in the caregiver self-administered questionnaire.
Caregiver OH support was operationalized as a new emergent index by averaging the percentages of caregivers who provided support to residents with IDD during five OH activities: (1) assistance to residents during oral hygiene activities; (2) use of adaptive dental devices and strategies to create a calm atmosphere to increase resident participation in OH activities; (3) use of rewards in the form of incentives (praise, TV time, etc.) to residents; (4) monitoring by supervising oral hygiene activities of residents; and (5) supervising diet by limiting sugary foods, the number of juice or juice-type beverages drank, and the number of regular sodas drank regularly.
3.3.4 Intervention processes
These measures pertain to the implementation quality of the intervention and include intervention dosage, implementation fidelity (adherence), and caregiver reactions to the OH strategy.
Dosage and implementation fidelity measures were developed for the initial session (didactic and observational learning components) and the subsequent reinforcement (coaching component). Dosage measured whether caregivers were present for the entire session, part of the session, or not present. Fidelity (adherence) measured whether key points were completely covered or partially covered/not covered.
Caregiver reaction was measured by questionnaire items that queried caregivers on the quality and usefulness of a behavioral contract, the in-home training including training materials, and the in-home training demonstrations. Responses for “quality” included excellent, good, fair, or poor, and responses for “usefulness” included not at all useful, somewhat useful, and useful. Caregivers were also asked about their reactions to the coaching sessions and were given response options of very helpful, somewhat helpful, not very helpful, and not at all helpful. The caregivers were also asked about the overall training usefulness and were given response options of not at all useful, somewhat useful, or useful. The alpha reliability of scales ranged from 0.67 to 0.94.
3.3.5 Contextual factors
The administrative and medical records of the residents with IDD were reviewed at the organization’s offices to collect demographic data including level of disability, age, gender, race, age, dental visits in the past year, and number of months since the last dental visit. The caregivers provided demographic data in the baseline caregiver self-administered questionnaire including age, gender, race, education level, years worked in the organization, and years worked with residents with disability.
3.4 Data collection and level of participation
The dental PI collected distal outcome data from all 25 eligible residents with IDD (i.e., those who provided written consent and remained in the study) by way of pre- and post-oral examination assessments. Intermediate outcome data on resident oral hygiene practices were collected by the Resident Assessment Questionnaire that was completed by caregivers at pre-and post-assessments for each resident in their care. All 21 eligible caregivers completed the Resident Questionnaire at the pre-assessment, and 16 caregivers completed the survey at the post-assessment, yielding a retention rate of 76%.
The proximal outcome data were collected in two ways. First, a Caregiver Self-Administered Questionnaire was completed by caregivers at pre- and post-assessments that included self-efficacy items. All 21 eligible caregivers completed this questionnaire at the pre-assessment, and 16 caregivers completed it at the post-assessment, yielding a retention rate of 76%. Second, a Caregiver Daily Checklist was completed by the caregiver for each resident every time he/she provided OH support relating to oral hygiene, dental devices used, reward(s), and monitoring involving a consented resident performing an oral hygiene activity. These data were collected 7 days before intervention implementation and 7 days immediately after completing the implementation. The caregivers were trained at baseline and asked to complete the checklist via a tablet as the preferred method of data collection; they were also given paper forms in case the Internet was down, the tablet was not charged, or the caregiver had trouble using the tablet due to unfamiliarity with the device. Thirty-three percent (7 of 21) of the caregiver sample opted for the paper forms. Nineteen of 21 eligible caregivers completed the daily checklist at the pre-assessment and 16 at the post-assessment, yielding a respectable retention rate of 76%.
We tested data collection for the caregiver OH support measures by asking caregivers to use the tablet to record video during oral hygiene activities. We developed a caregiver video outcome observation coding form to be used by the research team. The evaluators completed this form while watching videos of the residents performing OH behaviors. Caregivers were instructed that the camera was to be placed in acceptable locations in bathrooms, kitchens, or bedrooms. Videos were to be collected for one week at baseline and one week for post-assessment. The coding form collected information on the time of day, length of OH session, and location of the oral hygiene behavior, what teeth were brushed and flossed, whether the caregiver intervened or showed encouragement/reinforcement, and whether environmental adaptations were used.
Regarding the intervention process data, we collected video-camera observation and dental hygienist log dosage and fidelity data. Due to problems with the cameras only covering part of the session in each group home, we used the dental hygienist’s implementation log data for examining quality assurance in implementing the intervention. Most of the caregivers (20 of 21) participated in the didactic training and assessment, and 18 of 21 caregivers participated in the demonstration training and assessment. The majority of the caregivers (16) also participated in the two coaching sessions and the assessments (retention = 76%). The Caregiver Reactions Questionnaire was completed by caregivers immediately following the initial capacity-building training and then again after completion of their coaching sessions. All 21 of the caregivers completed the questionnaires after the initial training, and 76% completed questionnaires for the coaching sessions as part of the post-assessment (i.e., 16 of 21 caregivers).
Contextual data for the residents were collected from the records at the IDD service organization, and the contextual data for the caregivers were collected from the baseline caregiver self-administered questionnaire.
3.6 Final analysis strategy
The final analysis focused on answering Research Questions 1 – 4 presented earlier. First, we examined distal, intermediate, and proximal change over time using hierarchical linear modeling (HLM) to regress each outcome on a dummy variable representing time for Research Questions 1.1 – 1.4. All models were run in SPSS 20 (Statistical Product and Service Solutions, Armonk, New York). We assumed there was random variability in the outcome as a result of multiple observations being nested within each participant, so all models posed the intercept as a random effect. The effect size r was first calculated for the time effect for each model from the t-value and accompanying Satterthwaite approximated degrees of freedom. r was then transformed to d (Cohen, 1988), as d has a more intuitive interpretation for changes over time. We refer to this analysis as our repeated cross-sectional analysis. This analysis confers the benefits of allowing the use of all the data, regardless of whether a case is missing a post-test observation (Raudenbush & Bryk, 2002). Also, it is consistent with an intent-to-treat approach. Further, we present the results of the more conventional repeated measures t-test with only those cases with data at both waves. These results were nearly identical. Due to the limited degrees of freedom because of our small sample size, we did not enter any covariates into the repeated measures or the cross-sectional analysis using HLM (Shadish, Cook, & Campbell, 2002). We did find marginal correlation with the level of disability (a potential proxy for level of cooperation) to change in the OAG outcome, but not the O’Leary Plaque Index outcome.
Our assessment of implementation quality (Research Question 1.5) simply examined descriptive statistics (e.g., percentages and means) for implementation dosage, fidelity, and participant reactions to the implemented OH strategy.
4.0 Results
4.1 Sample descriptions
The sample consisted of 11 group homes with 25 group home residents with IDD aged 19 years or older of whom 29% had a mild disability, 39% had a moderate disability, 21% had a severe disability, and none had a profound disability. The average age of the residents was 45 with one resident younger than 21 years, and the majority were male (62%) and White (68%). Considering the characteristics of the sample relevant to OH, they had an average of 22 teeth, less than one carious/fractured tooth on average (0.32), and an average of 5 filled teeth (5.1). On average, they had seen the dentist 2.4 times in the past year, and it had been 4.5 months since their last dental visit. The average age of the 21 caregivers was 37, the majority were female (71%), the minority were White (24%), and 48% had an associate’s or a bachelor’s degree. The average years worked with disabled residents was 4.6 years.
4.2 Outcome change
We focused on an examination of change in a set of primary, intermediate, and distal outcomes using a pre- and post-intervention design. Notably, without a control group, cause-effect relationships could not be established. In addition, the samples were too small to assess mediation or moderation of the proximal and intermediate outcomes.
Table 1 presents change over time on the outcomes associated with Research Questions 1 – 3 presented earlier. There were statistically significant improvements over time on both of the direct distal outcome measures of resident OH: the O’Leary plaque score (100% to 49%) and the OAG (1.60 to 1.78).
Table 1.
Change in Primary, Intermediate, and Proximal Outcomes
| Pre-Test M(SD) | Post-Test M(SD) | d Change | Repeated Cross-Sections | Repeated Measures | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| t | df | t | df | ||||
| O’Leary Plaque Index | 100(2) | 49(29) | −3.66 | −8.19** | 20.00 | −8.19** | 20 |
| Oral Assessment Guide Index | 1.60(.26) | 1.78(.22) | 1.57 | 3.81** | 23.63 | 3.85** | 23 |
| Oral Hygiene Practice Index | 1.71(.77) | 2.64(.82) | 2.30 | 4.59** | 15.95 | 4.21** | 13 |
| % Disclosing solution | 11(24) | 58(34) | 3.04 | 5.71** | 14.11 | 5.47** | 13 |
| % Brushed | 78(30) | 87(28) | .45 | 1.02 | 20.28 | 1.32 | 13 |
| % Flossed | 14(29) | 44(34) | 1.92 | 3.72** | 15.06 | 3.43** | 13 |
| % Rinse | 26(34) | 18(35) | −.66 | −1.11 | 11.33 | −1.03 | 10 |
| Average time brushing | 1.55(1.06) | 1.76(1.02) | .18 | .34 | 14.34 | −.52 | 10 |
| Oral Health Support Index | 3.47(1.01) | 3.87(1.23) | .36 | 1.29 | 51.00 | 1.33 | 24 |
| % Oral Hygiene Supervision | 77(28) | 94(11) | 1.06 | 2.15* | 16.50 | 2.23* | 10 |
| % Environmental Adaptations | 32(34) | 46(45) | 1.07 | 1.73 | 10.51 | 2.60* | 10 |
| % Reward | 40(32) | 42(41) | −.02 | −.04 | 12.89 | −.34 | 10 |
| Dietary Supervision Index | 2.86(.48) | 2.69(.79) | −.27 | −.81 | 35.00 | −1.17 | 15 |
| % Monitoring | 56(36) | 76(26) | .65 | 1.88+ | 34.00 | 1.29 | 13 |
| Caregiver Self-Efficacy | 2.75(.30) | 2.84(.23) | .51 | 1.03 | 16.17 | .60 | 15 |
Note:
p <.01,
p <.05, + p <.10; the effect size d is calculated from the repeated cross-sectional analysis where the effect size r was first calculated from the t-value and accompanying Satterthwaite degrees of freedom and then r was transformed to d (see Cohen, 1988); the repeated cross-sectional analysis uses all cases (i.e., including those with missing post-test data) in the examination of change over time using HLM to adjust estimates for nonindependence; the repeated measures analysis uses a standard repeated measures t-test with only those cases with data at both pre- and post-test; these data represent N = 24 residents at pre-test and n = 11 to 24 participants at post-test and N = 16 caregivers at pre-test and post-test.
For the intermediate outcomes, there were statistically significant improvements on two of the five resident single oral hygiene practices (% use of disclosing solution: 11% to 58% and % flossed: 14% to 44%), as well as the oral hygiene practices index that included all five of the oral hygiene practices defined earlier (d = 2.30).
For the proximal outcomes, there was no significant change in caregiver self-efficacy. This may have occurred because of a ceiling effect from this proximal outcome being high at the pre-assessment. For the caregiver OH support outcome, the only significant improvement was in the caregivers’ oral hygiene support, where there was an increase in the number of residents supported by their caregivers from 77% to 94% and caregivers’ monitoring of residents’ OH approached significance with a change from 56% to 76%.
4.3 Implementation quality
Question 4 focused on assessing implementation quality as measured by dosage, fidelity, and caregiver reactions to key elements of the OH strategy. Table 2 presents the level of dosage and fidelity by key OH strategy elements by intervention components. The level was measured by both a percentage and the counts of participation. Level of dosage was high across three of the four components of our strategy’s implementation ranging from 86% to 95%. Lower dosage in the coaching component (71%) suggests a need for special attention in future studies.
Implementation fidelity was high, ranging from 81% to 90% for three or the four components. Implementation of the planning action component consisting of the behavioral contract and implementing the observational learning elements as designed was fair with 71% and 76%, respectively. Caregivers’ reactions to the component of the OH strategy were rated high for all key elements of the OH strategy with means of 2.53 or larger on a 0-to-3 response scale representing perceived usefulness to the caregivers (see Table 3). However, these data were collected as part of the post-assessment; consequently, only 76% (i.e., 16 of 21 caregivers) responded to a self-administered questionnaire. Nevertheless, appraisals of the strategy were high for the caregivers who continued to participate in the study.
Table 3.
Average Caregiver Reaction to Key Elements of the Oral Health Strategy (N=16)
| Key Elements by Intervention Component | Average |
|---|---|
| Planned Action | |
| Behavioral Contract Quality | 2.56 |
| Capacity Building | |
| Quality Didactic Training | 2.78 |
| Quality In-Home Training Demonstrations | 2.83 |
| Quality Training Materials | 2.80 |
| Overall Usefulness of Training | 2.84 |
| Environmental Adaptation | |
| Dental Device Use | 2.54 |
| Calming Atmosphere/Cooperation Strategy Use | 2.61 |
| Reinforcement | |
| Coaching | 2.89 |
Note: Scores range from 0–3 where 3 is a more desirable rating.
5.0 Discussion
The purpose of this study was to pilot test an OH strategy to determine the feasibility of conducting a larger RCT. In this section, we discuss the change in outcomes from pre- to post-assessments, as well as the quality of implementation of the OH strategy. We also describe the challenges and lessons learned from our study.
5.1. Change in outcomes
The distal outcome of the OH status of residents with IDD was a composite of oral hygiene status, as measured by the O’Leary Plaque Index, and overall OH, as measured by the OAG score. The Plaque Index ranging from 0% to 100% assessed the amount of plaque on all teeth, and the significant change was approximately a 50% reduction in plaque from baseline to post-assessment. Other plaque indices that have been used with this population include the Ramfjord’s Index (Lange, Cook, Dunning, Froeschle, & Kent, 2000) and the Simplified Oral Hygiene Index (Glassman & Miller, 2006), both of which only used 6 indicator teeth for oral hygiene assessment. The O’Leary Plaque Index gave an accurate and reliable assessment of overall plaque, did not take long to complete, and was easy to perform with this population. The overall OH status measured by the OAG also significantly improved from a baseline score of 1.60 to a post-assessment score of 1.78 (0 = poor and 2 = excellent). To the best of our knowledge, the OAG has not been used to assess the impact of an OH strategy in this population.
The intermediate outcome of residents’ oral hygiene practices was also positively impacted with a significant increase in the percentage of residents using disclosing solution and dental floss from baseline to post-assessment but without a significant increase in average time brushing. This is in contrast with Glassman and Miller (2006) who reported the results of a pilot test of a preventive dentistry training program conducted in three group homes with 11 adult clients with IDD in California. They reported that oral hygiene practices, measured by the duration of tooth brushing of the clients, improved after caregiver staff training and increased even more after coaching of the caregivers.
The proximal outcome of caregiver self-efficacy was not impacted by the pilot test of the intervention from baseline to the post-assessment. Our lack of positive results may be due to the fact that we adapted a general composite scale rather than a specific OH-related scale. Mac Giolla Phadraig, Guerin, and Nunn (2013) conducted an RCT of an OH education program with caregivers of individuals with IDD in Ireland and also found no impact on a global self-efficacy scale. Thus, one explanation for the failure to find an impact on self-efficacy may be that the instruments used to measure this outcome have not been developed and tested specifically for this population and for assessing self-efficacy in providing OH support. Also, there may be other mechanisms of change from social cognitive theory in addition to self-efficacy that should be included as proximal outcomes. We discuss these potential mechanisms of change in our lessons learned section of this article.
We found some evidence of change in our caregiver OH support outcome, especially in caregiver supervision and the use of environmental adaptation. The rationale for including this outcome came from our qualitative assessment rather than a theoretical rationale (Authors, 2013). Glassman and Miller (2006) also reported that caregiver OH support, measured by the percentage of oral hygiene sessions where a caregiver was present with the client with IDD during oral hygiene activities, significantly increased from baseline to post-assessment. We found positive change in the level of caregivers’ (1) oral hygiene supervision; (2) use of environmental adaptations (i.e., use of recommended dental devices and creation of a calm atmosphere); and (3) to some extent, monitoring of residents’ oral hygiene practices.
Our failure to find positive change in caregivers’ providing rewards and dietary supervision may have resulted from these support behaviors not being strongly emphasized during implementation of the capacity-building component and the reinforcement component of the OH strategy.
5.2. Quality of implementation of the strategy
There is increasing emphasis on the assessment, monitoring, and enhancement of intervention implementation quality in OH research (Borrelli, 2011). When implementation quality is not taken into consideration, protocol deviations may not be detected, which could affect the study’s outcomes and reduce confidence in the study’s results. To the best of our knowledge, there is only one report in the OH literature assessing implementation quality. Van den Branden, Van den Broucke, Leroy, Declerck, and Hoppenbrouwers (2013) recently reported the results of a systematic evaluation of implementation fidelity of an intervention for OH (“Smile for Life”) in preschool children in Belgium. Similar to the dosage (coverage) results of our pilot study, they reported that 88% of parents attended all the basic home visits, but only 57% received 9 of the 11 planned follow-up visits. Their implementation fidelity (adherence) was lower than in our study, with 64% of the intervention delivered to the parents compared to our 81% to 90% fidelity. This may have been due to multiple nurse interventionists and integration of the intervention with usual well baby care. Van den Branden and colleagues did not report participant reactions to the implementation of the intervention, so our positive participant reactions cannot be compared.
5.3. Challenges and lessons learned
The pilot study of the OH strategy yielded insights that can be of value to other OH researchers who are designing, implementing, and evaluating OH strategies with residents with IDD who live in a group-home setting. Pilot-testing the theoretical rationale, intervention design, recruitment, measurement and outcome data collection, intervention implementation fidelity, and partnerships may provide invaluable information to the design and implementation of a larger study with a similar focus. Following is a description of the challenges and lessons learned from the conduct of the pilot study.
5.3.1 Theoretical challenges
We learned that our proximal psychosocial outcomes, which serve as mechanisms of change, need to be expanded to include not only self-efficacy (personal factor) from social cognitive theory, but also outcome expectancies (personal factor), behavioral capability (behavioral factor), and environmental influences (environmental factor). Outcome expectancy of caregivers’ OH support should be impacted by the planned action and capacity-building components of the OH strategy. Caregiver’s behavioral capability for providing OH support should be impacted by the capacity building, environmental adaptation, and reinforcement/coaching components of the strategy. For the OH strategy to impact environmental influences, we believe that the environmental adaptation intervention component needs to be expanded to include group-home corporate-level administrative support in the form of incentive policy and continual verbal support for OH to caregivers to assist residents in OH activities.
5.3.2. Intervention design challenges
Individually, the majority of the intervention components proved to be well designed, but we did learn the following lessons from the implementation of each intervention component: (1) the behavioral contracts were taken more seriously when they were negotiated by the dental clinical PI rather than by the dental hygienist, (2) the dental plaque disclosing solution (environmental adaptation) used in the capacity-building and reinforcement/coaching sessions was a valuable tool to motivate the caregivers and residents with IDD, (3) the first coaching session needs to be more intensive than the next two sessions to keep caregivers motivated, and (4) the entire period of the intervention should be 4 months to assess sustained outcome change.
We also learned there was a need to revisit the intervention design to strengthen the capacity-building and reinforcement/coaching components. Special attention needs to be given to caregivers’ dietary supervision and to the extent that rewards are being provided to residents for improved oral hygiene practices. We determined that more attention should be given to caregivers’ monitoring residents’ oral hygiene practices, as well.
5.3.3 Recruitment challenges
The pilot study provided valuable lessons regarding recruitment of study participants. First, unbeknown to us early in the process, our partner organization was undergoing an administrative reorganization. The entire management team was replaced, as was many of the direct care staff and their immediate supervisors during the study period. Consequently, we experienced difficulty in recruitment because administrators who were assisting us in recruitment were replaced, and many direct-care staff (caregivers) whom had already been consented were dismissed from employment. We learned the importance of discerning if reorganization is planned for a partner organization and how to deal with it. Second, we first recruited the residents with IDD over a 2–3-month period and then recruited the entire sample of caregivers over a subsequent 2–3-month period. We then implemented the OH strategy first in a cohort of 7 homes and subsequently in the remaining 5 homes. We learned that in a larger study the recruitment should be simultaneous for residents and caregivers in a cohort of group homes.
5.3.4 Measurement and outcome data-collection challenges
We learned important measurement lessons from challenges encountered during the pilot study. We used a Plaque Index score and a composite OAG score as two measures of oral health status, which is our distal outcome. We learned that in a larger study we should use an index that would evaluate the status of the oral soft tissues, such as the Modified Gingival Index (Lobene, Weatherford, Ross, Lamm, & Menaker, 1986), as well as an index that would evaluate the status of the oral hard tissues, such as the Decayed, Missing and Filled Teeth (DMFT) score.
Further, we determined that we need to use a self-efficacy scale with specific items concerning caregivers’ OH support that is more sensitive to intervention change than the global self-efficacy scale that we used in the pilot study. We also determined that measures to assess outcome expectancy, behavioral capability, and environmental influences need to be adapted from validated measures used in other public health disciplines and pre-tested for validity and reliability. Appropriate measurement of these additional constructs of the social cognitive theory could not be found in the literature for the pilot study.
Given the acceptable standard that observation data are more reliable than self-reported data, we experimented with the collection of observation data via video camera for caregiver outcome data. We found that the caregiver outcome assessment (caregiver OH support and resident with IDD oral hygiene practices) via video cameras at the pre- and post-assessments was problematic. We learned that video observational data collected by caregivers was neither reliable nor of high quality. Only 16 of the 21 eligible caregivers participated in the video recording in the pre-assessment period, and only 7 participated in the post-assessment, yielding an attrition of 76% for the video pre- and post-assessments.
To determine the best method of outcome data collection for a larger efficacy study, we compared the reliability of this data source for caregiver outcomes with caregivers’ daily checklist for several important oral hygiene support indicators. We compared checklist data with coded, video-recorded data for 41 pre-assessment sessions on six oral hygiene indicators. Videos were coded by two coders and disagreements were resolved through discussion and consensus. Coders agreed 98% of the time prior to consensus. Data from the coded videos and checklists were similar, where agreement was greater than 82% for most measures. There was slightly lower agreement for some behaviors, such as whether teeth were flossed (66%), praise was used (63%), and OH was supervised (59%).
5.3.5. Methodology for monitoring intervention implementation fidelity
We also experimented with using a video camera to record dosage and fidelity process data on the didactic and in-home demonstration training. However, due to technical difficulties (i.e., the camera memory was insufficient to record the entire session), only 30 minutes of data were recorded. Our pilot study suggests that that the video-recording methodology is a viable option, but for a larger study, we would need more sophisticated equipment capable of reliably recording the entire 1–2 hour initial training sessions. We also determined that a research evaluation team member would need to be present to operate the equipment instead of assigning this task to the dental hygienist. In addition, we believe that with adequate camera equipment and an on-site research assistant, we can also collect video observations on the coaching sessions, which we did not do in the pilot study.
5.3.6. Acceptability of the intervention by our target population
Although caregiver participant reactions to the intervention strategy were very positive, we found that the data-collection burden was high. We learned that we needed to reduce the number of items on the caregiver questionnaires, reduce the caregiver assessments of oral hygiene practices from 7 to 4 days at each data-collection point, and eliminate the caregiver data collection of oral hygiene practices via video.
5.3.7. Partnership challenges
We learned that it is essential to have excellent working relationships with partner organizations, including a commitment to full participation in the study. For our larger study, we have added several policies and procedures for our partner organizations related to OH to strengthen the intervention. These include immediate notification of staff turnover so we can recruit, consent, and train replacement staff and having established administrative policies in the partner organizations related to improving the OH of the residents with IDD.
6.0 Conclusions
The clinical trial planning grant requirement by NIDCR proved to be valuable in preparation for a larger RCT of our OH intervention strategy application. The NIH multiple-PI approach also proved valuable in conducting this multidisciplinary pilot study because of the OH expertise of one PI and behavioral science expertise of the other PI. Although the pilot test was only a pre-and a post-evaluation, the OH and oral hygiene practices of the residents with IDD showed significant improvement with a significant increase in caregivers’ supervision of oral hygiene. Further, the quality of implementation as measured by intervention component dosage, fidelity, and caregiver reactions was moderate to high. In addition, the lessons learned can strengthen both the intervention and research components for future study.
Highlights.
An oral health strategy is designed for persons with intellectual and developmental disabilities (IDD) living in community group homes.
A pilot study examines outcome change and implementation quality.
The oral health of residents with IDD significantly improved as measured by cleanliness of their teeth and the overall assessment of the oral cavity.
The oral health strategy was implemented with high quality as measured by dosage, fidelity, and caregiver reactions.
Observation data to assess caregiver outcome change in a group home setting was difficult to collect.
Acknowledgments
This research was funded by the National Institute of Dental and Craniofacial Research (NIDCR) by Grant R34DE022274. The content of this publication does not necessarily reflect the view or the policies of the NIDCR. The authors wish to acknowledge the members of the IDD service organization’s administration and staff members for their crucial assistance in the recruitment and consenting of the study participants and implementation of the OH strategy.
Biographies
Catherine J. Binkley, DDS, MSPH, PhD, is an Associate Professor in the Department of Surgical & Hospital Dentistry at the University of Louisville. Her research interests include oral health disparities and the relationship between oral health and systemic health. She has served as the principal investigator for several NIH funded studies and previously was the director the General Practice Residency program at the University of Louisville.
Knowlton W. Johnson, PhD, is currently a Senior Scientist for the Pacific Institute for Research and Evaluation (PIRE) – Louisville Center. He has engaged in evaluation program planning in prevention and treatment research for 45 years while at the University of Maryland, College Park, University of Alaska, Anchorage, University of Louisville, and PIRE. He has conducted formative and outcome evaluations in a variety of problem areas. For the past 10 years, he has served as an investigator and a multiple principal investigator on several oral health prevention studies.
Melissa Abadi, PhD, is an Associate Research Scientist at the Pacific Institute for Research and Evaluation. Dr. Abadi has a diverse background in health behavior promotion, applied behavior change theory, and quantitative and qualitative research methods. She has managed and directed field research in various areas of health with multidisciplinary teams. Her work focuses on mixed-methods evaluation of applied health behavior change models, health messages, community-level efforts for policy change and environmental strategies, and program and training evaluation.
Kirsten Thompson has her BS and MA in Anthropology. In her current position as a Research Associate at PIRE, she has focused on the coordination, implementation, and project management of evaluation and intervention activities on the topics of youth access to harmful legal products, prescription drug abuse, substance abuse, alcohol abuse, youth mentoring, rural access to healthcare education and continued education credits, rural access to shelter for homeless teen mothers, and oral health interventions with intellectually and developmentally disabled individuals
Stephen R. Shamblen, PhD, completed his doctorate in social psychology, where there was a heavy focus in this training on methodology and statistics. His statistical expertise includes random effects/hierarchical linear modeling, structural equation modeling, meta-analysis, psychometrics, and complex survey analysis. His interests and first-author published work has focused largely on the efficacy of various secondary data indicators as measures of need for prevention (e.g., Shamblen & Springer, 2007), as well as the most efficient substance abuse prevention methods (e.g., Shamblen & Derzon, 2009). He currently serves as the subcontract project director for SAMHSA’s data collection, analysis, and reporting subcontract (DCAR).
Linda Young, M.A, is a Senior Research Scientist at the Pacific Institute for Research and Evaluation. Her primary areas of expertise are international research, survey methods, technical plan development, and project implementation, including quality control methods and procedures for large and complex research projects. She has collaborated with research scientists to develop and direct research projects covering a wide range of substantive areas including the evaluation of healthcare policies and programs, alcohol and drug prevention and treatment, economic impact studies, and criminal victimization. She has managed multi-million dollar research projects funded by the Agency for Health Care Policy and Research, the Agency for Toxic Substance and Disease Registry, the National Science Foundation, the National Institute for Alcohol Abuse and Alcoholism and the Robert Wood Johnson Foundation.
Brigit Zaksek is a registered dental hygienist who has worked in private practice for 17 years. She earned a BS in Dental Hygiene from The Ohio State University in 1997. She completed her MS in Oral Biology at the University of Louisville in 2014. Her interests are in the area of improving the oral health of all people but especially those who are intellectually and/or developmentally disabled. She plans to further her education and pursue a dental degree.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations: Caregivers (CG), Decayed, Missing and Filled Teeth (DMFT), hierarchical linear modeling (HLM), Institutional Review Board (IRB), intellectual and developmental disabilities (IDD), legally authorized representatives (LARs), multiple principal investigator (PI), National Institute of Dental and Craniofacial Research (NIDCR), National Institutes of Health (NIH), Oral Assessment Guide (OAG), oral health (OH), randomized controlled trial (RCT)
Contributor Information
Catherine J. Binkley, Email: cjbink01@louisville.edu.
Knowlton W. Johnson, Email: kwjohnson@PIRE.org.
Melissa Abadi, Email: mabadi@PIRE.org.
Kirsten Thompson, Email: kthompson@PIRE.org.
Stephen R. Shamblen, Email: sshamblen@PIRE.org.
Linda Young, Email: young@PIRE.org.
Brigit Zaksek, Email: brzaks01@gmail.com.
References
- Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Special Care Dentistry. 2010;30(3):110–117. doi: 10.1111/j.1754-4505.2010.00136.x. [DOI] [PubMed] [Google Scholar]
- Andersson P, Hallberg IR, Renvert S. Inter-rater reliability of an oral assessment guide for elderly patients residing in a rehabilitation ward. Special Care Dentistry. 2002;22(5):181–186. doi: 10.1111/j.1754-4505.2002.tb00268.x. [DOI] [PubMed] [Google Scholar]
- Araujo AC, Gusmao ES, Batista JE, Cimoes R. Impact of periodontal disease on quality of life. Quintessence International. 2010;41(6):e111–118. [PubMed] [Google Scholar]
- Ashkenazi M, Bidoosi M, Levin L. Effect of Preventive Oral Hygiene Measures on the Development of New Carious lesions. Oral Health & Preventive Dentistry. 2014;12(1):61–69. doi: 10.3290/j.ohpd.a31219. [DOI] [PubMed] [Google Scholar]
- Avenali L, Guerra F, Cipriano L, Corridore D, Ottolenghi L. Disabled patients and oral health in Rome, Italy: long-term evaluation of educational initiatives. Annali di Stomatologia. 2011;2(3–4):25–30. [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior : The Official Publication of the Society for Public Health Education. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bollen K, Lennox R. Conventional Wisdom on Measurement: A Structural Equation Perspective. Psychological Bulletin. 1991;110:305–314. [Google Scholar]
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. [Research Support, N.I.H., Extramural] Journal of Public Health Dentistry. 2011;71(Suppl 1):S52–63. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Eribaum; 1988. [Google Scholar]
- Dao LP, Zwetchkenbaum S, Inglehart MR. General dentists and special needs patients: does dental education matter? Journal of Dental Education. 2005;69(10):1107–1115. [PubMed] [Google Scholar]
- Eilers J, Berger AM, Petersen MC. Development, testing, and application of the oral assessment guide. Oncology Nursing Forum. 1988;15(3):325–330. [PubMed] [Google Scholar]
- Faulks D, Hennequin M. Evaluation of a long-term oral health program by carers of children and adults with intellectual disabilities. Special Care Dentististry. 2000;20(5):199–208. doi: 10.1111/j.1754-4505.2000.tb00020.x. [DOI] [PubMed] [Google Scholar]
- Fickert NA, Ross D. Effectiveness of a caregiver education program on providing oral care to individuals with intellectual and developmental disabilities. Intellectual and Developmental Disabilities. 2012;50(3):219–232. doi: 10.1352/1934-9556-50.3.219. [DOI] [PubMed] [Google Scholar]
- Gibson F, Auld EM, Bryan G, Coulson S, Craig JV, Glenny AM. A systematic review of oral assessment instruments: what can we recommend to practitioners in children’s and young people’s cancer care? Cancer Nursing. 2010;33(4):E1–E19. doi: 10.1097/NCC.0b013e3181cb40c0. [DOI] [PubMed] [Google Scholar]
- Girgis SS. Dental health of persons with severe mentally handicapping conditions. Special Care Dentistry. 1985;5(6):246–248. doi: 10.1111/j.1754-4505.1985.tb00586.x. [DOI] [PubMed] [Google Scholar]
- Glassman P, Miller C. Dental disease prevention and people with special needs. Journal of the California Dental Association. 2003;31(2):149–160. [PubMed] [Google Scholar]
- Glassman P, Miller CE. Effect of preventive dentistry training program for caregivers in community facilities on caregiver and client behavior and client oral hygiene. New York State Dental Journal. 2006;72(2):38–46. [PubMed] [Google Scholar]
- Greene L, Kreuter M. Health Program Planning: An Educational and Ecological Approach. 4. New York, NY: McGraw-Hill Higher Education; 2005. [Google Scholar]
- Hood H, Dean J, Cornett T, Boggs K. The Hazelwood study: dental care of the profoundly cognitively impaired in the southeastern region of the United States. Journal of the Southeastern Society of Pediatric Dentistry. 2001;7(3):40–41. [Google Scholar]
- Lange B, Cook C, Dunning D, Froeschle ML, Kent D. Improving the oral hygiene of institutionalized mentally retarded clients. Journal of Dental Hygiene: JDH/American Dental Hygienists’ Association. 2000;74(3):205–209. [PubMed] [Google Scholar]
- Lindemann R, Zaschel-Grob D, Opp S, Lewis MA, Lewis C. Oral health status of adults from a California regional center for developmental disabilities. Special Care Dentistry. 2001;21(1):9–14. doi: 10.1111/j.1754-4505.2001.tb00217.x. [DOI] [PubMed] [Google Scholar]
- Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clinical preventive dentistry. 1986;8(1):3–6. [PubMed] [Google Scholar]
- Mac Giolla Phadraig C, Guerin S, Nunn J. Train the trainer? A randomized controlled trial of a multi-tiered oral health education programme in community-based residential services for adults with intellectual disability. Community Dentistry and Oral Epidemiology. 2013;41(2):182–192. doi: 10.1111/cdoe.12006. [DOI] [PubMed] [Google Scholar]
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. Journal of Periodontology. 1972;43(1):38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- Perlman S, Friedman C, Tesini D. Prevention and Treatment Considerations for People with Special Needs. Skillman, NJ: Johnson & Johnson, Inc; 1991. [Google Scholar]
- Petersen PE. Challenges to improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. International Dental Journal. 2004;54(6 Suppl 1):329–343. doi: 10.1111/j.1875-595x.2004.tb00009.x. [DOI] [PubMed] [Google Scholar]
- Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bulletin of the World Health Organization. 2005;83(9):661–669. [PMC free article] [PubMed] [Google Scholar]
- Pezzementi ML, Fisher MA. Oral health status of people with intellectual disabilities in the southeastern United States. The Journal of the American Dental Association. 2005;136(7):903–912. doi: 10.14219/jada.archive.2005.0291. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical Linear Models. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Rautemaa R, Lauhio A, Cullinan MP, Seymour GJ. Oral infections and systemic disease—an emerging problem in medicine. Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases. 2007;13(11):1041–1047. doi: 10.1111/j.1469-0691.2007.01802.x. [DOI] [PubMed] [Google Scholar]
- Reid BC, Chenette R, Macek MD. Prevalence and predictors of untreated caries and oral pain among Special Olympic athletes. Special Care Dentistry. 2003;23(4):139–142. doi: 10.1111/j.1754-4505.2003.tb00300.x. [DOI] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- Stanfield M, Scully C, Davison MF, Porter S. Oral healthcare of clients with learning disability: changes following relocation from hospital to community. British Dental Journal. 2003;194(5):271–277. doi: 10.1038/sj.bdj.4809931. discussion 262. [DOI] [PubMed] [Google Scholar]
- Tesini DA, Fenton SJ. Oral health needs of persons with physical or mental disabilities. Dental Clinic of North America. 1994;38(3):483–498. [PubMed] [Google Scholar]
- Van den Branden S, Van den Broucke S, Leroy R, Declerck D, Hoppenbrouwers K. Evaluating the Implementation Fidelity of a Multicomponent Intervention for Oral Health Promotion in Preschool Children. Prevention Science: The Official Journal of the Society for Prevention Research. 2013 doi: 10.1007/s11121-013-0425-3. [DOI] [PubMed] [Google Scholar]
- Vigild M, Brinck JJ, Christensen J. Oral health and treatment needs among patients in psychiatric institutions for the elderly. Community Dentistry and Oral Epidemiolology. 1993;21(3):169–171. doi: 10.1111/j.1600-0528.1993.tb00745.x. [DOI] [PubMed] [Google Scholar]
- Waldman HB, Perlman SP. Preparing to meet the dental needs of individuals with disabilities. Journal of Dental Education. 2002;66(1):82–85. [PubMed] [Google Scholar]
- Watt RG, Marinho VC. Does oral health promotion improve oral hygiene and gingival health? Periodontology 2000. 2005;37:35–47. doi: 10.1111/j.1600-0757.2004.03796.x. [DOI] [PubMed] [Google Scholar]


