Abstract
The effects of a polymerized bovine hemoglobin-based oxygen carrier (HBOC) and two derivatives on arteriolar vasoactivity and tissue oxygen tension were explored by administering HBOC in a dose-response fashion to normovolemic rats. The effect of oxygen affinity (P50) and viscosity were also explored, where the P50 and viscosity of the parent compound (HBOC-201) and its modifications (MP50 and LP50A) were as follows: 40 mmHg and 3.0 cP (HBOC-20l); 18 mmHg and 4.4 cP (MP50); and 17 mmHg and 12.1 cP (LP50A). Anesthetized male Sprague-Dawley rats (N = 32) were randomized to receive one of the HBOC solutions, and were administered four infusions that increased in concentration for each dose (2, 22, 230 and 780 mg/kg, IV). Data were compared to rats receiving an equivalent volume for each of the four infusions (0.4, 0.4, 3.8, 13.1 ml/kg, IV) of iso-oncotic 5.9% human serum albumin (HSA). Increasing doses of either HBOC solutions or HSA were associated with increasing MAP. Doses 3 and 4 of HBOC-201, MP50 and HSA produced significant increases in MAP, whereas similar increases began at a lower dose (Dose 2) with LP50A. There were no significant changes in arteriolar diameters at any dose for any group. Interstitial partial pressure of oxygen (ISF PO2) remained unchanged for HBOC-201, MP50 and HSA, but LP50A caused a significant decrease in ISF PO2 compared to baseline after Doses 3 and 4. In conclusion, there was no evidence that HBOC-201 would perform better with increased oxygen affinity (40 to 18 mmHg) or viscosity (3.0 to 4.4 cP).
Keywords: HBOC, HBOC vasoactivity, interstitial PO2, microcirculation, oxygen therapeutic, oxygen transport
INTRODUCTION
Although hemoglobin-based oxygen carriers (HBOCs) have distinct advantages over stored blood in certain circumstances (Riess, 2001; Moore, 2003; Dube et al., 2008), there is a concern that the observed vasopressor effect may be one of the underlying causes of the serious complications observed during clinical trials (Natanson et al., 2008). Since arterioles are major contributors to peripheral resistance in the systemic circulation, the occasional substantial increase in mean arterial pressure (MAP) is thought to be the result of arteriolar constriction. Two mechanisms have been implicated that associates arteriolar constriction with either the reaction of extracellular hemoglobin with vascular nitric oxide (NO), the “NO Scavenging” theory (Schultz et al., 1993; Thompson et al., 1994; Gould & Moss, 1996; Doherty et al., 1998), or the “Autoregulation” hypothesis where the vasculature is capable of sensing and responding to hyperoxygenation (Rohlfs et al., 1998; Winslow, 2003).
The widely accepted “NO Scavenging” theory suggests that the reaction of cell-free hemoglobin with NO produced by the endothelial cells results in vasoconstriction (Schultz et al., 1993; Thompson et al., 1994; Gould & Moss, 1996; Doherty et al., 1998). Because NO is a vasodilator, a decrease in its concentration near the vascular wall would result in vasoconstriction. The vasoconstrictor response may be intensified when smaller extracellular hemoglobin molecules extravasate into or across the vessel wall and react with NO found in the endothelium and/or smooth muscle layer (Kavdia et al., 2002; Matheson et al., 2002; Olson et al., 2004). Data indicate that decreasing the fraction of monomers and dimers (Thompson et al., 1994; Rice et al., 2008), and increasing the molecular size (Gould & Moss, 1996; Olson et al., 2004; Hare et al., 2006; Yu et al., 2006) of the HBOC molecule mitigates extravasation. Thus, to attenuate the vasoactivity of HBOCs, hemoglobin tetramers have been enlarged by covalently attaching polyethylene glycols (Aftershock™, Prolong Pharmaceuticals Inc.; MP4, Sangart), or polymerization (Hemopure, Biopure Corp.; PolyHeme, Northfield Laboratories, Inc.; and OxyVita®, OXYVITA, Inc.).
The “Autoregulation” hypothesis states that vasoconstriction occurs in response to a hyperoxic state caused by the increase in oxygen-carrying capacity of the blood brought on by the addition of the HBOC. To compensate, the arterioles constrict and the reduction of blood flow restores a state of normoxia (Rohlfs et al., 1998; Winslow, 2003). In hamsters, arterioles ranging between 20 to 40 μm in diameter are typically exposed to a partial pressure of oxygen (PO2) that is near the P50 of hemoglobin in red blood cells. The P50 is defined as the PO2 where half of the binding sites of the hemoglobin are occupied with oxygen, corresponding to the steepest part of the oxygen-hemoglobin dissociation curve (Villela et al., 2009). Saltzman and co-workers have demonstrated that these arterioles have the densest adrenergic innervation (Saltzman et al., 1992), which may be indicative of not only oxygen sensing in these regions but the ability to provide rapid (seconds to minutes) vasoconstrictive responses to regulate blood flow and oxygen delivery (Winslow, 2003). Advocates of the “Autoregulation” hypothesis favorHBOCs that have a higher oxygen affinity (lower P50) to prevent “premature” oxygen off-loading to upstream regions; hence, this would avert vasoconstriction and promote oxygen delivery to tissue regions where PO2 is low (Sakai et al., 1999; Tsai et al., 2003; Winslow, 2003; Villela et al., 2009).
A third type of HBOC modification involves the molecule’s impact on vascular wall shear stress, which is a known stimulator of endothelial NO production (Rohlfs et al., 1998; Winslow et al., 1998; Tsai & Intaglietta, 2001; Winslow, 2003; Tsai et al., 2005). In this context, it is thought that HBOCs with a viscosity similar to blood (4 cP) will perform better than many current HBOCs, which have a viscosity of approximately 2 cP (Winslow et al., 1998; Tsai & Intaglietta, 2002).
The purpose of the present study was to investigate the differential effects of HBOC-201 and its two derivatives on vascular tone, blood pressure, and tissue oxygenation. The two HBOC-201 derivatives, MP50 and LP50A were similar to the parent molecule except that the oxygen affinity of MP50 was higher than that of HBOC-201, and the LP50A had nearly the same oxygen affinity as MP50 but increased viscosity. Thus comparing MP50 to HBOC-201 evaluated oxygen affinity, comparing MP50 to LP50A evaluated viscosity and comparing LP50A to HBOC-201 evaluated both parameters simultaneously. A stepwise dose-response protocol using normovolemic rats was used, as previously reported by our laboratory (Song et al., 2013) to establish a dose-response relationship, as well as evaluate the cumulative dose effect on systemic (i.e., blood pressure) and microcirculatory (i.e., arteriolar diameter and interstitial PO2) vasoactivity parameters. Although hemorrhage models or exchange transfusions to produce extreme hemodilution have a higher clinical and military relevance than infusion to healthy normovolemic rats, we chose a healthy rat model to prevent any possibility that a physiological response to hypovolemia or anemia would confound the HBOCs’ effects on blood pressure and vasomotor responses.
METHODS
Rats
Thirty-two male Sprague-Dawley rats (Harlan, Indianapolis, IN) were housed two per cage in plastic cages. Temperature and humidity were set in accordance with the current Guide for the Care and Use of Laboratory Animals of the National Academy of Sciences. Rats were maintained in a 12 h light/12 h dark cycle and fed rat chow and water ad libitum. The protocol for this study was approved by the Institutional Animal Care and Use Committee of Virginia Commonwealth University.
Intravital Microscopy
Rats were divided into four study groups: HBOC-201 (289 ± 9 g; N = 8); MP50 (276 ± 17 g; N = 7); LP50A (313 ± 6 g; N = 8); and 5.9% human serum albumin (HSA) volume control (274 ± 11 g; N = 9). Animals were anesthetized with a mixture of ketamine (72 mg/kg, IP) and acepromazine (3 mg/kg, IP). Once femoral vein access was obtained, animals received supplemental anesthesia of Alfaxalone acetate (Alfaxan, Schering-Plough Animal Health, Welwyn Garden City, UK) at 0.1 mg/kg/min for the duration of the experiment. The animals were tracheostomized and the right jugular vein was cannulated for infusion of either control or experimental solutions. Blood pressures were measured continuously via a pressure transducer connected to a PE-50 catheter in the femoral artery (MP-150, BIOPAC Systems, Goleta, CA). Arterial blood sampling was obtained using the same catheter.
In vivo microcirculatory studies were made on an exteriorized spinotrapezius muscle, which was surgically prepared as previously reported (Gray, 1973). Briefly, the muscle was moistened with a phosphate-buffered salt solution throughout the surgical procedure, and bleeding was controlled with the use of a cautery unit. The spinotrapezius muscle was placed on a thermo-stabilized transillumination pedestal of the microscope platform (Golub & Pittman, 2003). Temperatures of the animal heating pad and the spinotrapezius pedestal were separately controlled by electronic heating units to maintain body and muscle temperatures at 37 °C. The spinotrapezius muscle was covered with a gas barrier film (polyvinylidene chloride, Krehalon CB-100, Kureha, Japan) minimizing desiccation of the tissue and its exposure to atmospheric oxygen.
Observations and measurements of the exteriorized spinotrapezius muscle were carried out with an intravital microscope (Axioimager2m, Carl Zeiss, Germany) configured for both epi- and trans-illumination through a 20X/0.8 objective (Plan-APOCHROMATE, Zeiss, Germany). The microvasculature of the spinotrapezius muscle was visualized under transillumination with white light from a light emitting diode (Luxeon V Star white, Quadica Developments Inc., Brantford, Ontario). Images were captured in real-time using a color CCD camera (KP-D20BU, Hitachi, Tokyo, Japan) and displayed on a flat-screen color video monitor (Model LN19A450C1D, Samsung, Japan). Transillumination was used to select measurement sites, establish appropriate focal planes and verify flow conditions. Measurements of arteriolar diameter were made using the 20X objective focused in the diametral plane and the image was displayed on the video monitor. Internal vessel widths were measured in mm from the image on the screen and then converted to μm using a previous calibration.
Interstitial PO2
The phosphorescent probe (palladium meso-tetra-(4-carboxyphenyl)-porphyrin dendrimer, Oxyphor R2, Oxygen Enterprises, Philadelphia, PA) used for the phosphorescence quenching measurement of interstitial PO2 was applied topically to the spinotrapezius muscle and measurements were made 30 min later to allow for distribution of the probe in the interstitium of the muscle. Excitation of the probe was achieved via epi-illumination with a xenon flash lamp (Model FX249, EG&G Electro-optics Co., Salem, MA), which delivered 0.5 J/Flash for a duration of 4 μs to a region of tissue 300 μm in diameter at a frequency of 1 Hz. The subsequent phosphorescence emission was collected through the 20X objective and detected by a photomultiplier tube. PO2 was related to the rate of phosphorescence decay, K, according to the Stern-Volmer equation, K = Ko + Kq PO2, where the values of the calibration constants for Oxyphor R2 were Ko = 1.53×10−4 μs−1 and Kq = 4.3×10−4 μs−1mmHg−1. Details of the phosphorescence quenching microscopy technique have been previously published (Golub et al., 2007; Golub et al., 2011, Golub & Pittman, 2012).
Solutions
HBOC-201 (Biopure Corporation (currently OPK Biotech), Cambridge, MA) is a glutaraldehyde-polymerized bovine hemoglobin (13 ± 1 g/dL) with an average molecular weight of 250 kDa, containing ~98% polymerized hemoglobin, and less than 2.5% free tetramers (≤ 64 kDa). HBOC-201 has properties similar to human blood; osmolality is between 290 to 310 mOsm/kg, and oncotic pressure ranges from 25 to 27 mmHg (Dube et al., 2008). Two additional products, MP50 and LP50A, were developed through modification of the HBOC-201 (supplied by Biopure Corporation (currently OPK Biotech)). The P50 and viscosity of HBOC-201 were 40 ± 6 mmHg and 3.0 cP, respectively, while MP50 had an increased oxygen affinity (P50 = 18 mmHg) and a somewhat similar viscosity (4.4 cP, similar to human blood), and LP50A has a P50 of 17 mmHg and a greatly increased viscosity (12.1 cP). Information regarding viscosity (measured at room temperature) and oxygen affinity was provided by OPK Biotech. Human Serum Albumin (25% HSA, ZLB Behring AG, Berne, Switzerland) was diluted with normal saline to 5.9% to provide an iso-oncotic volume control solution to HBOC-201 (Mongan et al., 2009; Muir et al., 2011).
Top-Load
Solutions were administered through the jugular vein to normovolemic animals. For the three HBOC solutions, the sequence of doses targeted specific cell-free hemoglobin concentrations (monomer basis) in the blood: Dose 1, 2 mg/kg or ~1 μM;Dose 2, 22 mg/kg or ~10 μM; Dose 3, 230 mg/kg or ~100 μM; and Dose 4, 780 mg/kg or ~300 μM. HSA was administered in volumes that corresponded to volumes of HBOC infusions 1 through 4, respectively: Dose 1, 0.4 ml/kg; Dose 2, 0.4 ml/kg; Dose 3, 3.8 ml/kg; and Dose 4, 13.1 ml/kg. All infusions were administered at 1 ml/min.
Experimental Protocol
For each experiment, three to six sites in the spinotrapezius muscle were randomly selected for interstitial fluid (ISF) PO2 measurements. Arterioles near the PO2 measurement sites were chosen for diameter measurements and categorized into feed arterioles (inside diameter ~100 μm) and arcade arterioles (inside diameter ~60 μm). Baseline measurements of systemic (arterial blood pressure) and microvascular (ISF PO2 and arteriolar diameter) variables were made (measurement time was ~2 minutes at each site). At baseline and the end of each experiment, arterial blood samples were collected for measurement of hemoglobin and methemoglobin concentrations (Radiometer OSM-3 Hemoximeter, Copenhagen, Denmark). Systemic variables were continuously recorded throughout each experiment, and microcirculatory measurements were made at baseline and about 30 seconds after each infusion. Following completion of the microcirculatory measurements, the next higher dose was infused after approximately 10 minutes, and the set of measurements was repeated through to the last infusion. Animals were euthanized while anesthetized with a bolus infusion of Euthasol (150 mg/kg, IV; Delmarva, Midlothian, VA).
Statistics
Data are expressed as mean ± standard error of the mean (SEM). Statistical comparisons were made within groups and across doses using Analysis of Variance and an F test (JMP v. 8.0, SAS Institute Inc., Cary NC). In cases where a significant difference (p < 0.05) was detected, an appropriate multiple comparison test (Tukey’s HSD) was carried out. Paired comparisons were made between baseline and final blood hemoglobin values.
RESULTS
Mean Arterial Pressure (MAP)
The baseline (PRE Dose 1) MAP among the four treatment groups were not statistically different and did not change after Dose 1 (2 mg/kg) (Fig. 1). However, compared to baseline MAP (95 ± 4 mmHg), LP50A significantly increased MAP (134 ± 7 mmHg) after Dose 2 (22 mg/kg), which was also higher compared to HSA (99 ± 2 mmHg). After Dose 3 (230 mg/kg, corresponding to an 8% estimated cumulative blood volume increase), MAP was significantly elevated compared to baseline for all groups, with only MAP for LP50A (148 ± 5 mmHg) being statistically higher than that for HSA (109 ± 2 mmHg). In all four treatment groups, MAP did not completely return to baseline after Dose 3 resulting in the MAP of PRE Dose 4 being significantly increased compared to baseline. Following Dose 4 (780 mg/kg, corresponding to an additional 30% estimated cumulative blood volume increase), all groups displayed a significant increase in MAP compared to baseline; however, only LP50A MAP (161 ± 6 mmHg) was statistically elevated compared to HSA MAP (124 ± 2 mmHg).
Figure 1.
Dose-response relationship of MAP. For the HBOC solutions, HBOC-201 (N = 6), MP50 (N = 6) and LP50A (N = 8), the sequence of doses was intended to reach the following target cell-free hemoglobin concentrations (monomer basis) in the blood: Dose 1, 2 mg/kg or ~1 μM; Dose 2, 22 mg/kg or ~10 μM; Dose 3, 230 mg/kg or ~100 μM; and Dose 4, 780 mg/kg or ~300 μM. For the volume control, HSA (N = 8) corresponded to the four doses of HBOC solutions: Dose 1, 0.4 ml/kg; Dose 2, 0.4 ml/kg; Dose 3, 3.8 ml/kg; and Dose 4, 13.1 ml/kg. PRE represents the value of MAP immediately prior to the infusion and POST represents the peak in MAP that generally occurred within 30 s of the end of the infusion. * signifies a statistically significant difference (p < 0.05) compared to baseline (PRE 2 mg/kg dose). † signifies a statistical significance (p < 0.01) compared to LP50A at the applied dose.
Arteriolar Diameter
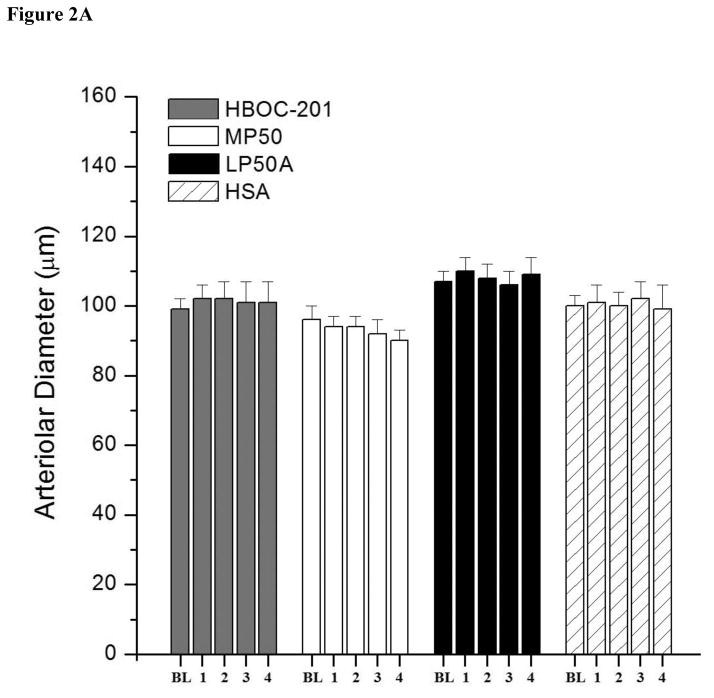
If elevated MAP following infusions of HBOC solutions was due to peripheral vasoconstriction, then one would expect arteriolar vasoconstriction in skeletal muscle beds in response to the infusions. However, as Fig. 2 shows, there were no significant changes in feed (Panel A) and arcade (Panel B) arteriolar diameters to increasing doses of HBOC-201, MP50, LP50A or HSA.
Figure 2.
Dose-response relationship of arteriolar diameter. There were no significant differences (p > 0.05) in both feed (Panel A and NA) and arcade (Panel B and NB) arteriolar diameters in response to increasing doses of HBOC-201 (NA = 12 sites; NB = 10 sites), MP50 (NA = 16 sites; NB = 9 sites), LP50A (NA = 13 sites; NB = 10 sites) or 5.9% HSA (NA = 16 sites; NB = 7 sites).
Interstitial (ISF) PO2
Because there were differences among the treatment group baseline values for ISF PO2, the data were normalized to baseline (Fig 3). There were no statistical differences compared to baseline with any dose of HBOC-201, MP50 or HSA. However, the ISF PO2 of LP50A decreased significantly from baseline (65 ± 2 mmHg) after Doses 3 (55 ± 4 mmHg) and 4 (51 ± 4 mmHg). Although HSA was not statistically different compared to HBOC-201 or MP50, it was significantly higher than LP50A after Doses 3 and 4. Additionally, ISF PO2 of LP50A was significantly lower than HBOC-201 and MP50 after Doses 2, 3 and 4. There were no significant changes in heart rate to increasing doses of HBOC-201, MP50, LP50A or HSA (data not shown).
Figure 3.
Dose-response relationship of ISF PO2 normalized to baseline values. The baseline ISF PO2 values for HBOC-201 (N = 16 sites), MP50 (N = 21 sites), LP50 (N = 25 sites), and HSA group (N = 17 sites) were 56 ± 3, 53 ± 2, 65 ± 2 and 54 ± 2 mmHg, respectively. * signifies a statistically significant difference (p < 0.05) between that value and the baseline (BL) for that group. † signifies a statistical significance (p < 0.05) compared to LP50A at the applied dose.
Arterial Blood Hemoglobin
The total hemoglobin (tHb) increased significantly compared to baseline with all HBOC solutions, while it decreased for HSA (Table 1). There was also a positive correlation between HBOC and methemoglobin (metHb), but there was no observed change in metHb with HSA.
Table 1.
Comparison of total hemoglobin (tHb) and methemoglobin (metHb).
| HBOC-201 | MP50 | LP50A | HSA | ||
|---|---|---|---|---|---|
| tHb (g/dl) | Baseline | 12.8 ± 0.1 | 13.7 ± 0.5 | 14.3 ± 0.4 | 13.1 ± 0.2 |
| Final | 14.0 ± 0.2* | 14.7 ± 0.4* | 15.4 ± 0.3* | 12.4 ± 0.3* | |
|
| |||||
| metHb (%) | Baseline | 0.35 ± 0.06 | 0.22 ± 0.06 | 0.80 ± 0.12 | 0.28 ± 0.04 |
| Final | 0.70 ± 0.05* | 0.98 ± 0.13* | 1.36 ± 0.25* | 0.42 ± 0.08 | |
signifies a statistically significant difference (p < 0.05) compared to baseline.
DISCUSSION
This study utilized a hypervolemia protocol, where a normovolemic system received additional fluid volume, to test the effect of HBOC-201 and its two derivatives with different oxygen affinity (P50) and viscosity on systemic blood pressure, microcirculatory vessel diameter and tissue oxygenation. To our knowledge, the effects of HBOC-201 have not previously been examined in this manner. This study design aids in establishing a dose-response relationship, as well as evaluating a cumulative dose effect. Furthermore, a top-load model, while resulting in a hypervolemic animal, is a more sensitive model in detecting systemic and microcirculatory vasoactivity than having the complexity of additional compensatory changes associated with hypovolemia (hemorrhagic shock) or anemia (exchange-transfusion) models.
HBOC-201 and HSA both exhibited a significant increase in MAP after Doses 3 (230 mg/kg; 3.8 ml/kg) and 4 (780 mg/kg; 13.1 ml/kg) compared to BL, while not being significantly different from each other (Fig. 1). As there was no difference between the two fluid types, these results simply suggest that an acute cumulative 8% (Dose 3) to 30% (Dose 4) increase in blood volume in a healthy animal will produce a corresponding increase in MAP when either colloidal fluid, with their long intravascular retention times, is infused. This result is contradictory to some earlier studies, which showed that the MAP after HBOC-201 was higher than the MAP of the volume control (Philbin et al., 2007; Katz et al., 2010; Arnaud et al., 2012). An explanation could be that these earlier studies did not use an iso-oncotic colloid or because these studies also included the influences of hypovolemia, anemia or tissue trauma. A literature search for research pertaining to HBOC-201 and iso-oncotic HSA revealed only two other studies (Mongan et al., 2009; Muir et al., 2011). Both investigators utilized the same hemodilution model where swine underwent three transfusions to attain volume exchanges of 10%, 30% and 50%. Muir et al found that HBOC-201 caused an increase in MAP compared to iso-oncotic HSA; however, Mongan et al observed an increase in HBOC-201 MAP compared to the baseline, but did not report statistical significance between HBOC-201 and iso-oncotic HSA. Thus, using the same model, there are contradictory findings on whether there is a pressor response when comparing HBOC-201 to iso-oncotic HSA. None of these earlier studies, including Mongan et al, were top-load models and, to our knowledge, there is no HBOC-201 study evaluating models (hypervolemia, hypovolemia, or hemodilution) as the single study variable to show how compensatory physiological mechanisms might affect our parameters of interest. Nonetheless, all studies reported an immediate increase in MAP following HBOC-201 infusion when compared to baseline and the more critical question is whether or not this is entirely due to volume (inferred by comparing to an oncotically-matched colloid) or if some or all of the pressor effect is also due to vasoconstriction. This latter possibility requires direct measurement of arteriolar vessel diameter, as discussed below.
Arteriolar diameter measurements were collected to determine if changes in blood pressure might be related to vasoactivity of the HBOC-201 test infusion. There was no change in arteriolar diameter from two different branching orders in the skeletal spinotrapezius muscle over the dose ranges tested for any of the HBOC solutions (Fig. 2). These findings suggest that the observed increases in MAP after HBOC-201 were not due to vasoconstriction, and were more likely due to the cumulative 30% increase in blood volume as the comparison to the volume control indicates. Because our experimental model used normovolemic rats undergoing serial infusions, it is plausible that the increased blood volume could activate the baroreceptor reflex. This response would cause arteriolar dilation and alter the microcirculatory diameter measurements. However, the data presented herein were collected immediately (30 seconds) after dose infusion; therefore, the acute response was unaffected by baroreceptors as demonstrated by the unaltered heart rate in response to increasing infusion doses. Furthermore, the data were compared to an iso-oncotic volume control, which did not differ significantly.
Other studies have demonstrated that HBOCs are vasoconstrictive using direct vessel measurements by intravital microscopy. However, all of these studies used cross-linked, polyethylene glycol (PEG) conjugated and polymerized hemoglobin; HBOC-201 was never used (Sakai et al, 2000; Cabrales et al., 2008; Cabrales, 2010). Studies that have evaluated HBOC-201 did not directly measure vessel diameter, and vasoactivity was indirectly assessed through systemic and/or pulmonary vascular resistance parameters (Rivera-Chavez et al., 2007; Rice et al, 2008; Katz et al., 2010; Arnaud et al., 2011) or localized blood flow (Mongan et al., 2009). Although some critics of HBOCs have suggested that the cause of adverse events in clinical trials is an association between HBOC-201-induced increased blood pressure and vasoconstriction (Natanson et al., 2008), it is somewhat surprising that there were no studies showing a correlation between elevated MAP and direct measures of vasoconstriction. This relationship has been frequently suggested by other investigators (Schultz et al, 1993; Gould and Moss, 1996; Doherty et al, 1998; Olson et al, 2004) who used first generation HBOCs, and specifically with HBOC-201 (Rice et al, 2008; Freilich et al., 2009; Katz et al., 2010; Arnaud et al., 2011). Without direct vascular measurements of changes in vessel diameters, the assumption that increased systemic vascular resistance or MAP after HBOC infusion is associated with vasoconstriction is plausible, but speculative. Our study did not show evidence of direct arteriolar vasoconstriction in skeletal muscle when HBOC-201 was administered to normovolemic rats.
An additional purpose of this study was to investigate the effects of modifying the oxygen affinity (P50) and viscosity of HBOC-201 on the microvasculature and tissue oxygenation. In our study, HBOC-201 and MP50 displayed a similar blood pressure and tissue oxygenation profile to the HSA control solution, while LP50A produced a higher MAP with infusions 2 (22 mg/kg), 3 (230 mg/kg) and 4 (780 mg/kg), and lower tissue PO2 for infusions 3 and 4. There was no difference in MAP or tissue oxygenation between HBOC-201 and MP50, suggesting that this range of different P50 values (40 and 18 mmHg) did not affect the microvasculature or the ability to oxygenate skeletal muscle in healthy rats. Our data concur with another study that compared two otherwise identical HBOCs with P50’s of 11 and 70 mmHg on cerebral tissue oxygen in a hemorrhage and resuscitation rat model (Hare et al., 2006). That study, like ours, showed that there was no benefit (increased tissue oxygenation) of increasing the P50 of otherwise identical HBOCs. Other investigators, who also compared HBOCs with different P50 (P50 from 3 to 30 mmHg (Doherty et al., 1998) and P50 from 3 to 46 mmHg (Olson et al., 2004)) but unfortunately did not collect tissue oxygenation measurements, similarly showed no differences in MAP. These results are in contrast to previous reports (Sakai et al., 1999; Tsai & Intaglietta, 2002; Winslow, 2003; Cabrales et al., 2005), in which a lower P50 conferred improved tissue oxygenation. Many of these latter studies evaluated HBOCs with different chemical formulations, i.e., hemoglobin with covalently attached polyethylene glycols (PEG) compared against cross-linked (αα) or polymerized hemoglobin (Winslow et al., 1998; Tsai et al., 2003). It is likely that there are other drug characteristics, independent of P50, which may be the cause of these differences (Doherty et al., 1998; Matheson et al., 2002; Olson et al., 2004; Hare et al., 2006; Yu et al., 2006).
Viscosity of the HBOC fluid may also be an important characteristic because a higher viscosity will increase microvascular wall shear stress and result in the production of NO to stimulate vasodilation (Rohlfs et al., 1998; Winslow et al., 1998; Tsai & Intaglietta, 2001; Winslow, 2003; Tsai et al., 2005). We did not observe a difference in systemic and microcirculatory vasoactivity between HBOC-201 (3.0 cP) and MP50 (4.4 cP), but our data clearly showed the detrimental effects of extreme viscosity after infusion of LP50A (12.1 cP). It caused an increase in MAP and a decrease in tissue oxygenation. Since resistance to blood flow is proportional to viscosity, a reduction in blood flow would decrease oxygen delivery. This is the most likely explanation for the decrease in tissue PO2 observed after higher cumulative doses of LP50A. However, this study is speculative since circulating blood flow and viscosity were not directly measured. Contrary to LP50A, the tissue PO2 of HBOC-201, MP50 and HSA were not statistically different from baseline or each other, likely because this was a healthy animal model. The measurement of ISF PO2 was undertaken because, had vasoconstriction been measured after HBOC-201 or its modifications, then it would have determined whether or not the test fluid was providing adequate oxygen to the tissue despite the vasoconstriction (Golub & Pittman, 2012). The observed interstitial PO2 values for skeletal muscle were consistent with other studies indicating adequate accuracy in our tissue oxygenation technique (Shibata et al., 2001; Golub et al., 2007; Golub et al., 2011; Song et al., 2013).
There is much scientific interest in understanding the association between vasoconstriction and the presence of extracellular hemoglobin. A recent article states that the “introduction of cell-free hemoglobin, even at low concentrations, greatly augments oxygen supply, engaging protective mechanisms that include vasoconstriction and ischemia” (Winslow, 2013). This concept has been reported by others (Rohlfs et al., 1998; Tsai et al., 2003; Winslow, 2003) and states that it is the increase in oxygen supply due to an increase in hemoglobin (not PaO2) that causes vasoconstriction and this then leads to detrimental effects on tissue oxygenation. However, the results from our study suggest that if increasing oxygen supply causes vasoconstriction (which we did not observe), then it may be through some other mechanism than simply increasing the cell-free hemoglobin concentration (which we did observe). That is, infusion of HBOC-201 increased both total hemoglobin and functional extracellular hemoglobin content (the extracellular hemoglobin is considered functional as it was elevated greater than the observed increase in non-oxygen carrying methemoglobin), with no significant change in ISF PO2 or arteriolar diameter. However, the association of hyperoxia from elevated partial pressure of oxygen and vasoconstriction has been documented in animals (via 100% O2 as the inspired gas mixture) and tissues (superfusion with 660 mmHg of O2) (Duling, 1972; Sullivan & Johnson, 1981; Lindbom & Arfors, 1985; Bertuglia et al., 1991; Messina et al., 1994; Tsai et al., 2003). Thus, the concern of vasoconstriction and ischemia from hyper-oxygenation following a HBOC infusion was not supported by our data, which showed functional cell-free hemoglobin increased total hemoglobin with no vasoconstriction or reduction in tissue oxygenation in normovolemic animals breathing room air.
SUMMARY
No arteriolar constriction was observed in the spinotrapezius skeletal muscle following serial infusions of HBOC-201, MP50 or LP50A or control fluid HSA when administered to normovolemic healthy rats spontaneously breathing room air. The elevated MAP measured following infusions of these HBOCs was not different from the MAP increase observed following oncotically-matched HSA. Thus, this study does not indicate that HBOC-201 is a vasopressor, but rather that the MAP increase may have been a volume artifact. It has been hypothesized that an increased presence of cell-free hemoglobin will cause vasoconstriction, and that increased oxygen affinity and/or a viscosity similar to whole blood are characteristics of the ideal HBOC. However, vasoconstriction was not observed in the presence of cell-free hemoglobin, and MP50 produced similar ISF PO2, MAP and arteriolar diameters as HBOC-201. These results suggest that increased oxygen affinity (40 to 18 mmHg) and viscosity (3.0 to 4.4 cP) do not play a significant role in the performance of HBOCs in healthy rats. On the other hand, a high viscosity HBOC (12.1 cP for LP50A) was directly correlated with increased MAP and decreased tissue oxygenation that is likely due to reduced blood flow. The adverse effects associated with administering fluids with increased viscosity above normal blood raises concerns about other resuscitation fluids such as packed red blood cells that may perform optimally if administered at viscosities similar to that of whole blood. Though HBOC-201 produced similar outcomes as the iso-oncotic volume control in this hypervolemia study, we acknowledge that future studies using a more clinically relevant model such as hemorrhagic shock are required to increase the understanding of cell-free hemoglobin-based oxygen carriers on both systemic and microcirculatory parameters.
Highlights.
Top-load infusion of three polymerized hemoglobin-based oxygen carriers in rats
Measured arterial pressure (MAP), arteriolar diameter and tissue oxygen tension (PO2)
Explored effects of altered oxygen affinity (P50) and viscosity with HBOC derivatives
Increasing doses of HBOC associated with increasing MAP and no change in diameter
Interstitial PO2 unchanged except for decrease with high viscosity HBOC
Acknowledgments
The Naval Medical Research Center supplied samples of HBOC-201, MP50 and LP50A manufactured for NMRC by Biopure Corporation (currently OPK Biotech; Cambridge, MA) to Virginia Commonwealth University for this study. The funding for the HBOC-201, MP50 and LP50A and the preclinical work performed at Virginia Commonwealth University was supported by BUMED congressional funding work unit number 604771N.9737.001.A0315. This work was also supported in part by grant R01 HL18292 from the National Heart, Lung and Blood Institute.
Footnotes
Declaration of Interest
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government. The experiments reported herein were conducted in compliance with the Animal Welfare Act and in accordance with the principles set forth in the “Guide for the Care and Use of Laboratory Animals,” Institute of Laboratory Animals Resources, National Research Council, National Academy Press, 1996. Paula F. Moon-Massat (Naval Medical Research Unit) is an employee of the US Government. Title 17 USC §105 provides that ‘copyright protection under this title is not available for any work of the US Government.’ Title 17 USC §101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could a3ect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arnaud F, Scultetus AH, Haque A, Saha B, Kim B, Auker C, Moon-Massat P, McCarron R, Freilich D. Sodium nitroprusside ameliorates systemic but not pulmonary HBOC-201-induced vasoconstriction: an exploratory study in a swine controlled haemorrhage model. Resuscitation. 2012;83(8):1038–45. doi: 10.1016/j.resuscitation.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Arnaud F, Scultetus AH, Kim B, Haque A, Saha B, Nigam S, Moon-Massat P, Auker C, McCarron R, Freilich D. Dose response of sodium nitrite on vasoactivity associated with HBOC-201 in a swine model of controlled hemorrhage. Artif Cells Blood Substit Immobil Biotechnol. 2011;39(4):195–205. doi: 10.3109/10731199.2010.533126. [DOI] [PubMed] [Google Scholar]
- 3.Bertuglia S, Colantuoni A, Coppini G, Intaglietta M. Hypoxia- or hyperoxia-induced changes in arteriolar vasomotion in skeletal muscle microcirculation. Am J Physiol. 1991;260(2 Pt 2):H362–72. doi: 10.1152/ajpheart.1991.260.2.H362. [DOI] [PubMed] [Google Scholar]
- 4.Cabrales P. Low oxygen-affinity hemoglobin solution increases oxygenation of partially ischemic tissue during acute anemia. J Am Coll Surg. 2010;210(3):271–9. doi: 10.1016/j.jamcollsurg.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cabrales P, Tsai AG, Intaglietta M. Isovolemic exchange transfusion with increasing concentrations of low oxygen affinity hemoglobin solution limits oxygen delivery due to vasoconstriction. Am J Physiol Heart Circ Physiol. 2008;295(5):H2212–8. doi: 10.1152/ajpheart.00751.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabrales P, Sakai H, Tsai AG, Takeoka S, Tsuchida E, Intaglietta M. Oxygen transport by low and normal oxygen affinity hemoglobin vesicles in extreme hemodilution. Am J Physiol Heart Circ Physiol. 2005;288(4):H1885–92. doi: 10.1152/ajpheart.01004.2004. [DOI] [PubMed] [Google Scholar]
- 7.Doherty DH, Doyle MP, Curry SR, Vali RJ, Fattor TJ, Olson JS, Lemon DD. Rate of reaction with nitric oxide determines the hypertensive effect of cell-free hemoglobin. Nat Biotechnol. 1998;16(7):672–6. doi: 10.1038/nbt0798-672. [DOI] [PubMed] [Google Scholar]
- 8.Dube GP, Vranckx P, Greenburg AG. HBOC-201: The multi-purpose oxygen therapeutic. EuroIntervention. 2008;4(1):161–5. doi: 10.4244/eijv4i1a26. [DOI] [PubMed] [Google Scholar]
- 9.Duling BR. Microvascular responses to alterations in oxygen tension. Circ Res. 1972;31(4):481–9. doi: 10.1161/01.res.31.4.481. [DOI] [PubMed] [Google Scholar]
- 10.Freilich D, Pearce LB, Pitman A, Greenburg G, Berzins M, Bebris L, Ahlers S, McCarron R. HBOC-201 vasoactivity in a phase III clinical trial in orthopedic surgery subjects--extrapolation of potential risk for acute trauma trials. J Trauma. 2009;66(2):365–76. doi: 10.1097/TA.0b013e3181820d5c. [DOI] [PubMed] [Google Scholar]
- 11.Golub AS, Pittman RN. Oxygen dependence of respiration in rat spinotrapezius muscle in situ. Am J Physiol Heart Circ Physiol. 2012;303(1):H47–56. doi: 10.1152/ajpheart.00131.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Golub AS, Song BK, Pittman RN. The rate of O2 loss from mesenteric arterioles is not unusually high. Am J Physiol Heart Circ Physiol. 2011;301(3):H737–45. doi: 10.1152/ajpheart.00353.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golub AS, Barker MC, Pittman RN. PO2 profiles near arterioles and tissue oxygen consumption in rat mesentery. Am J Physiol Heart Circ Physiol. 2007;293(2):H1097–106. doi: 10.1152/ajpheart.00077.2007. [DOI] [PubMed] [Google Scholar]
- 14.Golub AS, Pittman RN. Thermostatic animal platform for intravital microscopy of thin tissues. Microvasc Res. 2003;66(3):213–7. doi: 10.1016/s0026-2862(03)00061-x. [DOI] [PubMed] [Google Scholar]
- 15.Gould SA, Moss GS. Clinical development of human polymerized hemoglobin as a blood substitute. World J Surg. 1996;20(9):1200–7. doi: 10.1007/s002689900183. [DOI] [PubMed] [Google Scholar]
- 16.Gray SD. Rat spinotrapezius muscle preparation for microscopic observation of the terminal vascular bed. Microvasc Res. 1973;5(3):395–400. doi: 10.1016/0026-2862(73)90055-1. [DOI] [PubMed] [Google Scholar]
- 17.Hare GM, Harrington A, Liu E, Wang JL, Baker AJ, Mazer CD. Effect of oxygen affinity and molecular weight of hbocs on cerebral oxygenation and blood pressure in rats. Can J Anaesth. 2006;53(10):1030–8. doi: 10.1007/BF03022533. [DOI] [PubMed] [Google Scholar]
- 18.Katz LM, Manning JE, McCurdy S, Sproule C, McGwin G, Jr, Moon-Massat P, Cairns CB, Freilich D. Nitroglycerin attenuates vasoconstriction of HBOC-201 during hemorrhagic shock resuscitation. Resuscitation. 2010;81(4):481–7. doi: 10.1016/j.resuscitation.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 19.Kavdia M, Tsoukias NM, Popel AS. Model of nitric oxide diffusion in an arteriole: Impact of hemoglobin-based blood substitutes. Am J Physiol Heart Circ Physiol. 2002;282(6):H2245–53. doi: 10.1152/ajpheart.00972.2001. [DOI] [PubMed] [Google Scholar]
- 20.Lindbom L, Arfors KE. Mechanisms and site of control for variation in the number of perfused capillaries in skeletal muscle. Int J Microcirc Clin Exp. 1985;4(1):19–30. [PubMed] [Google Scholar]
- 21.Matheson B, Kwansa HE, Bucci E, Rebel A, Koehler RC. Vascular response to infusions of a nonextravasating hemoglobin polymer. J Appl Physiol. 2002;93(4):1479–86. doi: 10.1152/japplphysiol.00191.2002. [DOI] [PubMed] [Google Scholar]
- 22.Messina EJ, Sun D, Koller A, Wolin MS, Kaley G. Increases in oxygen tension evoke arteriolar constriction by inhibiting endothelial prostaglandin synthesis. Microvasc Res. 1994;48(2):151–60. doi: 10.1006/mvre.1994.1046. [DOI] [PubMed] [Google Scholar]
- 23.Mongan PD, Moon-Massat PF, Rentko V, Mihok S, Dragovich A, Sharma P. Regional blood flow after serial normovolemic exchange transfusion with hboc-201 (hemopure) in anesthetized swine. J Trauma. 2009;67(1):51–60. doi: 10.1097/TA.0b013e3181838030. [DOI] [PubMed] [Google Scholar]
- 24.Moore EE. Blood substitutes: The future is now. J Am Coll Surg. 2003;196(1):1–17. doi: 10.1016/s1072-7515(02)01704-0. [DOI] [PubMed] [Google Scholar]
- 25.Muir WW, Ilangovan G, Zweier JL, Moon-Massat PF, Rentko VT. Vital organ tissue oxygenation after serial normovolemic exchange transfusion with HBOC-201 in anesthetized swine. Shock. 2011;35(6):597–603. doi: 10.1097/SHK.0b013e31821366f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Natanson C, Kern SJ, Lurie P, Banks SM, Wolfe SM. Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death: A meta-analysis. Jama. 2008;299(19):2304–12. doi: 10.1001/jama.299.19.jrv80007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olson JS, Foley EW, Rogge C, Tsai AL, Doyle MP, Lemon DD. No scavenging and the hypertensive effect of hemoglobin-based blood substitutes. Free Radic Biol Med. 2004;36(6):685–97. doi: 10.1016/j.freeradbiomed.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 28.Philbin N, Handrigan M, Rice J, McNickle K, McGwin G, Williams R, Warndorf M, Arnaud F, Malkevich N, McCarron R, Freilich D. Resuscitation following severe, controlled hemorrhage associated with a 24 h delay to surgical intervention in swine using a hemoglobin based oxygen carrier as an oxygen bridge to definitive care. Resuscitation. 2007;74(2):332–43. doi: 10.1016/j.resuscitation.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 29.Rice J, Philbin N, Light R, Arnaud F, Steinbach T, McGwin G, Collier S, Malkevich N, Moon-Massatt P, Rentko V, Pearce LB, Ahlers S, McCarron R, Handrigan M, Freilich D. The effects of decreasing low-molecular weight hemoglobin components of hemoglobin-based oxygen carriers in swine with hemorrhagic shock. J Trauma. 2008;64(5):1240–57. doi: 10.1097/TA.0b013e318058245e. [DOI] [PubMed] [Google Scholar]
- 30.Riess JG. Oxygen carriers (“blood substitutes”)--raison d’etre, chemistry, and some physiology. Chem Rev. 2001;101(9):2797–920. doi: 10.1021/cr970143c. [DOI] [PubMed] [Google Scholar]
- 31.Rivera-Chavez FA, Huerta S, Brown R, York GB, Minei JP. Resuscitation from hemorrhagic shock comparing standard hemoglobin-based oxygen carrier (HBOC)-201 versus 7.5% hypertonic HBOC-201. J Trauma. 2007;63(5):1113–9. doi: 10.1097/TA.0b013e3181561157. [DOI] [PubMed] [Google Scholar]
- 32.Rohlfs RJ, Bruner E, Chiu A, Gonzales A, Gonzales ML, Magde D, Magde MD, Jr, Vandegriff KD, Winslow RM. Arterial blood pressure responses to cell-free hemoglobin solutions and the reaction with nitric oxide. J Biol Chem. 1998;273(20):12128–34. doi: 10.1074/jbc.273.20.12128. [DOI] [PubMed] [Google Scholar]
- 33.Sakai H, Hara H, Yuasa M, Tsai AG, Takeoka S, Tsuchida E, Intaglietta M. Molecular dimensions of hb-based O2 carriers determine constriction of resistance arteries and hypertension. Am J Physiol Heart Circ Physiol. 2000;279(3):H908–15. doi: 10.1152/ajpheart.2000.279.3.H908. [DOI] [PubMed] [Google Scholar]
- 34.Sakai H, Tsai AG, Rohlfs RJ, Hara H, Takeoka S, Tsuchida E, Intaglietta M. Microvascular responses to hemodilution with hb vesicles as red blood cell substitutes: Influence of o2 affinity. Am J Physiol. 1999;276(2 Pt 2):H553–62. doi: 10.1152/ajpheart.1999.276.2.H553. [DOI] [PubMed] [Google Scholar]
- 35.Saltzman D, DeLano FA, Schmid-Schonbein GW. The microvasculature in skeletal muscle. Vi. Adrenergic innervation of arterioles in normotensive and spontaneously hypertensive rats. Microvasc Res. 1992;44(3):263–73. doi: 10.1016/0026-2862(92)90086-5. [DOI] [PubMed] [Google Scholar]
- 36.Schultz SC, Grady B, Cole F, Hamilton I, Burhop K, Malcolm DS. A role for endothelin and nitric oxide in the pressor response to diaspirin cross-linked hemoglobin. J Lab Clin Med. 1993;122(3):301–8. [PubMed] [Google Scholar]
- 37.Shibata M, Ichioka S, Ando J, Kamiya A. Microvascular and interstitial PO(2) measurements in rat skeletal muscle by phosphorescence quenching. J Appl Physiol. 2001;91(1):321–7. doi: 10.1152/jappl.2001.91.1.321. [DOI] [PubMed] [Google Scholar]
- 38.Song BK, Nugent WH, Moon-Massat PF, Auker CR, McCarron R, Pittman RN. Effects of top-loading a zero-Link bovine hemoglobin, OxyVita, on systemic and microcirculatory variables. Military Medicine. 2013;178(5):570–7. doi: 10.7205/MILMED-D-12-00408. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan SM, Johnson PC. Effect of oxygen on arteriolar dimensions and blood flow in cat sartorius muscle. Am J Physiol. 1981;241(4):H547–56. doi: 10.1152/ajpheart.1981.241.4.H547. [DOI] [PubMed] [Google Scholar]
- 40.Thompson A, McGarry AE, Valeri CR, Lieberthal W. Stroma-free hemoglobin increases blood pressure and gfr in the hypotensive rat: Role of nitric oxide. J Appl Physiol. 1994;77(5):2348–54. doi: 10.1152/jappl.1994.77.5.2348. [DOI] [PubMed] [Google Scholar]
- 41.Tsai AG, Acero C, Nance PR, Cabrales P, Frangos JA, Buerk DG, Intaglietta M. Elevated plasma viscosity in extreme hemodilution increases perivascular nitric oxide concentration and microvascular perfusion. Am J Physiol Heart Circ Physiol. 2005;288(4):H1730–9. doi: 10.1152/ajpheart.00998.2004. [DOI] [PubMed] [Google Scholar]
- 42.Tsai AG, Vandegriff KD, Intaglietta M, Winslow RM. Targeted o2 delivery by low-p50 hemoglobin: A new basis for o2 therapeutics. Am J Physiol Heart Circ Physiol. 2003;285(4):H1411–9. doi: 10.1152/ajpheart.00307.2003. [DOI] [PubMed] [Google Scholar]
- 43.Tsai AG, Cabrales P, Winslow RM, Intaglietta M. Microvascular oxygen distribution in awake hamster window chamber model during hyperoxia. Am J Physiol Heart Circ Physiol. 2003;285(4):H1537–45. doi: 10.1152/ajpheart.00176.2003. [DOI] [PubMed] [Google Scholar]
- 44.Tsai AG, Intaglietta M. The unusual properties of effective blood substitutes. Keio J Med. 2002;51(1):17–20. doi: 10.2302/kjm.51.17. [DOI] [PubMed] [Google Scholar]
- 45.Tsai AG, Intaglietta M. High viscosity plasma expanders: Volume restitution fluids for lowering the transfusion trigger. Biorheology. 2001;38(2–3):229–37. [PubMed] [Google Scholar]
- 46.Villela NR, Cabrales P, Tsai AG, Intaglietta M. Microcirculatory effects of changing blood hemoglobin oxygen affinity during hemorrhagic shock resuscitation in an experimental model. Shock. 2009;31(6):645–52. doi: 10.1097/SHK.0b013e31818bb98a. [DOI] [PubMed] [Google Scholar]
- 47.Winslow RM. Oxygen: The poison is in the dose. Transfusion. 2013;53(2):424–37. doi: 10.1111/j.1537-2995.2012.03774.x. [DOI] [PubMed] [Google Scholar]
- 48.Winslow RM. Current status of blood substitute research: Towards a new paradigm. J Intern Med. 2003;253(5):508–17. doi: 10.1046/j.1365-2796.2003.01150.x. [DOI] [PubMed] [Google Scholar]
- 49.Winslow RM, Gonzales A, Gonzales ML, Magde M, McCarthy M, Rohlfs RJ, Vandegriff KD. Vascular resistance and the efficacy of red cell substitutes in a rat hemorrhage model. J Appl Physiol. 1998;85(3):993–1003. doi: 10.1152/jappl.1998.85.3.993. [DOI] [PubMed] [Google Scholar]
- 50.Yu B, Liu Z, Chang TM. Polyhemoglobin with different percentage of tetrameric hemoglobin and effects on vasoactivity and electrocardiogram. Artif Cells Blood Substit Immobil Biotechnol. 2006;34(2):159–73. doi: 10.1080/10731190600580223. [DOI] [PubMed] [Google Scholar]