Abstract
AIM: To identify an appropriate therapeutic regimen for using aconite cake-separated moxibustion to treat diarrhea-predominant irritable bowel syndrome (D-IBS).
METHODS: A factorial design was employed to examine the two factors of moxibustion frequency and number of cones. The two tested frequencies were three or six moxibustion sessions per week, and the two tested doses were one or two cones per treatment. A total of 166 D-IBS patients were randomly divided into four treatment groups, which included each combination of the examined frequencies and doses. The bilateral Tianshu acupoints (ST25) and the Qihai acupoint (RN6) were selected for aconite cake-separated moxibustion. Each patient received two courses of treatment, and each course had a duration of 2 wk. For each group, the scores on the Birmingham irritable bowel syndrome (IBS) symptom questionnaire, the IBS Quality of Life scale, the Self-Rating Depression Scale (SDS), the Self-Rating Anxiety Scale (SAS), the Hamilton Depression (HAMD) scale, and the Hamilton Anxiety (HAMA) scale were determined before treatment, after the first course of treatment, and after the second course of treatment.
RESULTS: The symptom, quality of life, SDS, SAS, HAMD, and HAMA scores of the patients in all 4 aconite cake-separated moxibustion groups were significantly lower after the first and second courses of treatment than before treatment (P < 0.001 for all). The symptom, quality of life, SDS, SAS, HAMD, and HAMA scores of the patients in all four aconite cake-separated moxibustion groups were significantly lower after the second course of treatment than after the first course of treatment (P < 0.001 for all). Between-group comparisons after the second course of treatment revealed that the symptom scores for group 1 (1 cone, 3 treatments/wk) and group 3 (2 cones, 3 treatments/wk) were significantly lower than that for group 2 (1 cone, 6 treatments/wk) (5.55 ± 5.05 vs 10.45 ± 6.61, P < 0.001; 5.65 ± 4.00 vs 10.45 ± 6.61, P < 0.001). Regarding the two levels of the two examined factors for aconite cake-separated moxibustion, after the first course of treatment, the changes in HAMA scores were significantly different for the two tested moxibustion frequencies (P = 0.011), with greater changes for the “6 treatments/wk” groups than for the “3 treatments/wk” groups; in addition, there were interaction effects between the number of cones and moxibustion frequency (P = 0.028). After the second course of treatment, changes in symptom scores for the 2 tested moxibustion frequencies were significantly different (P = 0.002), with greater changes for the “3 treatments/wk” groups than for the “6 treatments/wk” groups.
CONCLUSION: An aconite cake-separated moxibustion treatment regimen of 3 treatments/wk and 1 cone/treatment appears to produce better therapeutic effects for D-IBS compared with the other tested regimens.
Keywords: Diarrhea-predominant irritable bowel syndrome, Aconite cake-separated moxibustion, Factorial design, Moxibustion quantity, Clinical research
Core tip: This is a clinical factorial study focusing on aconite cake-separated moxibustion in the treatment of diarrhea-predominant irritable bowel syndrome. What is the effect of this ancient therapy on diarrhea-predominant irritable bowel syndrome patients? Which is the key factor in the treatment, the number of cones or the moxibustion frequency? This paper details answers to these questions.
INTRODUCTION
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. Epidemiological surveys have indicated that the worldwide incidence of IBS is approximately 10%-15%[1], the incidence of IBS among East Asians is approximately 5%-10%[2], and the incidence of IBS is higher among females than among males[3]. With respect to age distribution, IBS is mainly found among young adults[4]. In addition, this disease is more common among brain workers than among manual workers[5]. IBS causes tremendous mental stresses and heavy financial burdens for patients. Therefore, it is necessary to search for effective and rational therapeutic regimens for IBS.
In recent years, complementary and alternative medicine (CAM) has become widely accepted. CAM-based approaches have exhibited extremely good efficacy for treating chronic diseases. In particular, a study has revealed that 51% of IBS patients have received CAM-based treatment[6]. Moxibustion is an important treatment approach in CAM that has been widely applied in clinical contexts to treat various health issues, including gastrointestinal problems, cancer pain, insomnia and other diseases[7-9]. We have been committed to the study on technology and clinical application of treating bowel diseases with moxibustion for a long time, and have achieved innovative achievements[10]. Previous studies have indicated that moxibustion can significantly improve abdominal pain, diarrhea, and other symptoms in IBS patients[11,12] and in a rat model of IBS[13-17].
Herb cake-separated moxibustion is an indirect moxibustion therapy with a variety of materials[18]. Previous studies have demonstrated that herb cake-separated moxibustion can improve the pain thresholds of rats with chronic visceral hypersensitivity and reduce 5-hydroxytryptamine (5-HT) expression in the colonic mucosa of rats, thereby relieving the symptoms of abdominal pain and diarrhea[19]. Clinical studies have confirmed the efficacy of herbal cake-separated moxibustion in IBS patients[20,21]; however, the relationship between the quantity of stimulation with herb cake-separated moxibustion and the resulting therapeutic efficacy has not yet been established.
The number of cones and the moxibustion frequency are important factors that affect the quantity of moxibustion stimulation a patient receives. In this study, a factorial design was used to examine these two factors. In particular, the Birmingham IBS symptom questionnaire, the IBS-Quality of Life Scale (IBS-QOL Scale), the Self-Rating Depression Scale (SDS), the Self-Rating Anxiety Scale (SAS), the Hamilton Depression Scale (HAMD Scale), and the Hamilton Anxiety Scale (HAMA Scale) were used to evaluate the clinical efficacy of aconite cake-separated moxibustion treatments involving different moxibustion doses and frequencies in IBS patients. This approach allowed the selection of the optimal examined aconite cake-separated moxibustion regimen for IBS treatment, thereby providing a reliable basis for treating IBS with aconite cake-separated moxibustion in clinical practice.
MATERIALS AND METHODS
Subjects
All patients were treated at the medical outpatient department of the Shanghai Research Institute of Acupuncture and Meridian or at community health service stations in Fenglin, which is located in the Xuhui District of Shanghai, between July 2010 and April 2012. This clinical trial was registered in the Chinese Clinical Trial Register (registration number: ChiCTR-TRC-10000887) and was reviewed and approved by the ethics committee of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, which is affiliated to Shanghai University of Traditional Chinese Medicine (approval number: 2010-01).
The study subjects were patients between 18 and 65 years of age who were diagnosed with diarrhea-predominant IBS (D-IBS) based on the Rome III diagnostic criteria[22], who volunteered to participate in this trial and signed informed consent forms. Patients with organic diseases of the intestinal tract and patients whose conditions were complicated with heart, liver, or kidney disease and/or mental illness were excluded from the study. Patients with constipation-predominant IBS or mixed IBS were excluded from this investigation. Patients who were currently being treated with Dioctahedral Smectite, Pinaverium Bromide Tablets, Cisapride or traditional Chinese medicine were also excluded.
Methods
A factorial design approach was used to examine the two factors of moxibustion frequency and number of cones. There were 41 patients in aconite cake-separated moxibustion group 1 (1 cone of moxibustion per treatment, 3 treatments/wk), 42 patients in group 2 (1 cone of moxibustion per treatment, 6 treatments/wk), 42 patients in group 3 (2 cones of moxibustion per treatment, 3 treatments/wk), and 41 patients in group 4 (2 cones of moxibustion per treatment, 6 treatments/wk).
Treatment method
The bilateral Tianshu acupoints (ST25) and the Qihai acupoint (RN6) were selected for the moxibustion treatments in this study. The positioning of the acupoints was based on the national standards of the People’s Republic of China, which are set forth in “Nomenclature and location of acupuncture points” (GB/T12346-2006). According to traditional Chinese medicine theory, the Tianshu and Qihai acupoints can regulate gastrointestinal functions; moreover, our previous studies have confirmed that these acupoints can be used to effectively treat IBS[19].
The aconite cakes used in the aconite cake-separated moxibustion groups were produced as follows. Aconite (Radix Aconitilateralis Preparata, Sichuan) was ground into powder, sieved with a 100-mesh sieve, and yellow rice wine was added to make a thick paste (with a 5:6 ratio of aconite powder to yellow wine). The paste was pressed into a mold to form aconite cakes with a diameter of 28 mm and a thickness of 5 mm. Refined pure moxa sticks were selected (Hanyi, Nanyang, China; size: 17 mm × 200 mm) and cut into moxa cones with a height of 16 mm and a weight of 1.8 g; these cones were then used to perform aconite cake-separated moxibustion.
The moxa cones were placed on top of the aconite cakes and ignited. Moxibustion was then performed by placing the aconite cakes atop the Tianshu (ST25) and Qihai (RN6) acupoints on the patient’s abdomen (Figure 1). One cone referred to the dosage received when a moxa cone had completed burning naturally. Moxibustion was performed on the patients in each group in accordance with the aforementioned frequencies and numbers of cone. Each course of treatment lasted 2 wk, and the patients received two courses of treatment.
Figure 1.
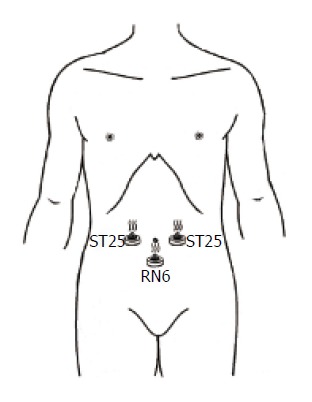
Diagram of aconite cake-separated moxibustion. ST25: Tianshu acupoint; RN6: Qihai acupoint.
Questionnaires
Patients were asked to complete the following questionnaires:
IBS symptom severity scale: This scale was initially developed and validated by Francis et al[23]. The scoring system is primarily used to assess patients’ abdominal pain severity and frequency, abdominal distention severity, defecation feelings, and quality of life. We used a Visual Analogue Scale (VAS) to score the aforementioned five questions, with higher scores indicating more severe symptoms. A previous study classified severity scores for IBS as follows: scores lower than 175 indicate mild IBS symptoms, scores between 175 and 300 indicate moderate, and scores higher than 300 indicate severe[23].
Birmingham IBS symptom questionnaire: This scale[24], which is based on symptoms that frequently occur in IBS cases, examines abdominal discomfort status, stool properties, and defecation feelings. The scale includes a total of 14 items, with 6 possible grades for each item that range from 0 points (never having this symptom) to 5 points (the symptom is always present). The total score is the sum of the scores for each item.
IBS-QOL scale: The IBS-QOL scale was formulated and developed by Drossman et al[25] to assess the extent to which IBS symptoms have affected the following nine aspects of a subject’s quality of life within the prior month: emotional state, psychological state, sleep, energy, daily activities, eating habits, social activities, major activities or work, and sex life. The scale contains 34 items, with each item measured independently based on the patient’s subjective feelings. A 5-point scale ranging from 1 point (the symptom has never occurred) to 5 points (the symptom’s description is completely accurate) was used for each item. Each item was scored separately, and then, the points for all items were summed to obtain a total score. Lower scores indicate better quality of life for patients, whereas higher scores indicate worse quality of life[26].
SDS: The Zung SDS is the prototype of the SDS[27]. The advantages of the SDS include its ease of use and ability to directly reflect patients’ subjective feelings. In particular, the SDS can assess specific feelings associated with the depressive states of patients in the four experimental groups; the phenomena detected by this scale include spiritual emotions, somatic disorders, psychomotor disorders, and psychological disorders. The SDS contains a total of 20 items that measure a subject’s depression level during the prior wk. Each item was scored on a scale ranging from 0 = never to 4 = very often, and the total raw score was the sum of the scores for each item. The standard score was the integer portion of the product of 1.25 and the total raw score. In China, an SDS standard score ≥ 50 indicates conscious depression.
SAS: The SAS[28] is similar to the SDS with respect to its structure and evaluation method. In particular, the SAS contains 20 items that measure the subject’s anxiety levels during the prior wk. Each item receives 1 of 4 responses ranging from A = never to D = very often. Responses to positively phrased questions are scored as follows: A = 1, B = 2, C = 3, and D = 4. Responses to negatively phrased questions are scored as A = 4, B = 3, C = 2, and D = 1. The standard score for these 20 items is the integer portion of the product of 1.25 and the total raw score. An SAS standard score ≥ 50 indicates conscious anxiety. Lower SAS scores indicate milder anxiety.
The SAS and the SDS are standard assessment tools that have been proven to accurately reflect patients’ subjective feelings of anxiety and depression, respectively. These two questionnaires have been translated into Chinese and have been extensively utilized in China[29].
HAMD scale: The HAMD scale[30-32] was used to evaluate the depressive states of patients during the prior week. This scale is commonly utilized by clinicians to assess depressive states. The 24-item version of the HAMD scale was used in this study. This version of the scale has clear criteria and is suitable for adults with depressive symptoms. Most of the HAMD items are scored on a 5-point scale ranging from 0 to 4, with scores of 0, 1, 2, 3, and 4 indicating no, mild, moderate, severe, and extremely severe depressive symptoms, respectively. A few HAMD items are scored on a 3-point scale ranging from 0 to 2, with scores of 0, 1, and 2 indicating no, mild-moderate, and severe depressive symptoms, respectively. The final HAMD score was the sum of the scores for each item. The following criteria were used for the total HAMD score: a score < 8 points indicates that a patient is normal; a score ≥ 8 points and < 20 points indicates that a patient might suffer from depression; a score ≥ 20 points and < 35 points indicates that a patient certainly suffers from depression; and a score ≥ 35 points indicates that a patient is severely depressed.
HAMA scale: The HAMA scale[30-32] mainly examines two categories of factors, physical and mental. A 5-point scoring system ranging from 0 points (no symptoms) to 4 points (extremely severe symptoms) is used for each item on this scale. The sum of the scores for the 14 items on the HAMA scale is the total score. Scores < 7 points indicate no anxiety; scores ≥ 7 points and < 14 points indicate possible anxiety; scores ≥ 14 points and < 21 points indicate definite anxiety; scores ≥ 21 points and < 29 points indicate definite and significant anxiety; and scores ≥ 29 points indicate possible severe anxiety.
The HAMD and HAMA scale items were scored by two doctors who assessed these items by conversing with and observing patients. After examining each patient, the two raters independently scored the items on these scales, and the average HAMD and HAMA scores produced by the two raters were then determined.
All the questionnaires were completed before and after treatment, and the pretreatment and post-treatment results were compared.
Safety assessment
The safety evaluation encompassed the following two types of safety considerations: vital signs, which included body temperature, respiration, heart rate, blood pressure, and liver and kidney function after treatment; and moxibustion abnormalities, which included skin burns, blisters, or other moxibustion-induced discomfort. All adverse events and adverse reactions were accurately recorded.
If an adverse event occurred after treatment, a necessary treatment was provided as appropriate for the circumstances of the event in question. If extremely small blisters occurred after moxibustion, no special treatment was required; in contrast, blisters with areas larger than 1 cm2 were broken and treated with topical ointment.
Statistical analysis
Sample size: After calculation, a required sample size of 35 cases in each group was obtained; to account for possible dropout rates of up to 10%, each group should include no fewer than 39 cases.
Data analysis: The SPSS16.0 (SPSS, Chicago, IL) statistical software package was used for statistical analysis. Normally distributed measurement data are expressed as mean ± SD; non-normally distributed measurement data are expressed in terms of median and inter quartile range. The change trends of indicators were analyzed using repeated-measures analysis of variance. Between-group comparisons of changes in indicators were analyzed using factorial analysis of variance. Count data were analyzed using χ2 tests. Non-normally distributed measurement data and ordinal data were analyzed using nonparametric rank-sum tests. P < 0.05 was considered statistically significant.
RESULTS
The flow chart of this investigation is presented in Figure 2.
Figure 2.
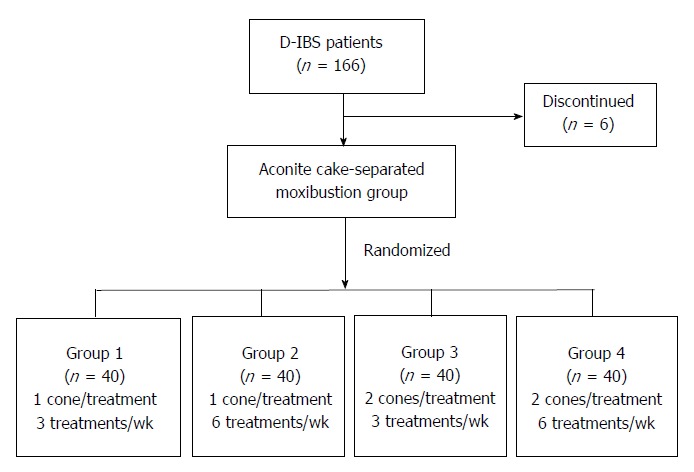
Flow chart overviewing the progress of patients during the course of the study. D-IBS: Diarrhea-predominant irritable bowel syndrome.
A total of 166 patients were included in this study. However, 6 patients dropped out during the study; in particular, 1 case, 2 cases, 2 cases, and 1 case were lost from aconite cake-separated moxibustion groups 1, 2, 3, and 4, respectively. Thus, ultimately, each group had 40 cases that were included in the results and the statistical analysis of this investigation.
General condition of the patients
Table 1 presents comparisons of the baseline characteristics of the patients in the four randomized aconite cake-separated moxibustion groups. Comparisons of the age (P = 0.196), gender (P = 0.330), disease duration (P = 0.300), and disease severity score (P = 0.582) of the patients in these four groups revealed no significant differences, indicating that the four groups were comparable.
Table 1.
An analysis of the general baseline conditions of the patients in each group
| Group 1 | Group 2 | Group 3 | Group 4 | P value | |
| n | 40 | 40 | 40 | 40 | |
| Age (yr) | 55 | 46.5 | 51.5 | 52 | 0.196 |
| Gender | 0.330 | ||||
| Male | 42.5% | 45% | 42.5% | 45% | |
| Female | 57.5% | 55% | 57.5% | 55% | |
| Disease duration (yr) | 3 | 5 | 4 | 5 | 0.300 |
| Disease severity scores | 231.7 ± 68.0 | 221.5 ± 79.2 | 233.3 ± 73.9 | 241.5 ± 79.3 | 0.698 |
Group 1: 1 cone of moxibustion per treatment, 3 treatments/wk; Group 2: 1 cone of moxibustion per treatment, 6 treatments/wk; Group 3: 2 cones of moxibustion per treatment, 3 treatments/wk; Group 4: 2 cones of moxibustion per treatment, 6 treatments/wk.
Post-treatment evaluations
Table 2 presents comparisons of the symptom scores at different treatment stages with the pretreatment symptom scores for the patients in each group. For the patients in all four groups, the Birmingham IBS symptom questionnaire, IBS-QOL, SDS, SAS, HAMD, and HAMA scores were significantly lower after the first and second courses of treatment than before treatment (P < 0.001 for all). In addition, for the patients in all four groups, the Birmingham IBS symptom questionnaire, IBS-QOL, SDS, SAS, HAMD, and HAMA scores were significantly lower after the second course of treatment than after the first course of treatment (P < 0.001 for all). Between-group comparisons indicated that after the second course of treatment, the Birmingham IBS symptom questionnaire score was significantly lower for group 1 (1 cone, 3 treatments/wk) and group 3 (2 cones, 3 treatments/wk) than for group 2 (1 cone, 6 treatments/wk) (5.55 ± 5.05 vs 10.45 ± 6.61, P < 0.001; 5.65 ± 4.00 vs 10.45 ± 6.61, P < 0.001). However, comparisons of quality of life scores for the patients in the 4 groups before treatment, after the first course of treatment, and after the second course of treatment revealed that at any given time point, these scores were similar across the treatment groups, with no significant between-group differences (P > 0.05 for all).
Table 2.
Comparisons of the symptom scores for patients in each group at different stages of treatment
| Group | n | Birmingham | IBS-QOL | SDS | SAS | HAMD | HAMA | |
| Group 1 | 40 | Before | 21.10 ± 8.62 | 75.75 ± 21.72 | 45.33 ± 11.04 | 42.83 ± 9.62 | 6.13 ± 5.43 | 5.90 ± 5.22 |
| 1st course | 11.60 ± 7.53a | 60.20 ± 14.82a | 36.20 ± 8.37a | 36.65 ± 9.37a | 3.75 ± 3.40a | 4.05 ± 3.57a | ||
| 2nd course | 5.55 ± 5.05abc | 50.65 ± 10.86ab | 32.43 ± 6.94ab | 32.08 ± 6.95ab | 1.75 ± 2.31ab | 2.23 ± 2.90ab | ||
| Group 2 | 40 | Before | 23.45 ± 8.25 | 75.38 ± 21.02 | 43.45 ± 13.93 | 43.10 ± 12.86 | 7.25 ± 7.06 | 6.68 ± 4.74 |
| 1st course | 15.58 ± 9.15a | 59.40 ± 18.02a | 38.13 ± 10.54a | 37.35 ± 10.03a | 4.03 ± 3.28a | 3.28 ± 3.03a | ||
| 2nd course | 10.45 ± 6.61ab | 47.90 ± 10.49ab | 32.53 ± 7.26ab | 32.25 ± 7.14ab | 1.98 ± 2.38ab | 1.93 ± 2.14ab | ||
| Group 3 | 40 | Before | 21.50 ± 8.82 | 78.53 ± 24.22 | 46.80 ± 13.53 | 46.15 ± 12.74 | 9.05 ± 6.54 | 7.53 ± 5.37 |
| 1st course | 13.03 ± 8.23a | 58.28 ± 13.39a | 38.40 ± 10.41a | 37.95 ± 8.65a | 4.60 ± 2.77a | 3.98 ± 2.30a | ||
| 2nd course | 5.65 ± 4.00abc | 48.83 ± 9.38ab | 32.50 ± 7.95ab | 33.70 ± 7.00ab | 2.10 ± 1.95ab | 2.20 ± 1.60ab | ||
| Group 4 | 40 | Before | 23.65 ± 7.62 | 76.88 ± 19.90 | 46.00 ± 12.59 | 44.38 ± 12.02 | 7.50 ± 7.66 | 6.63 ± 4.78 |
| 1st course | 13.95 ± 7.69a | 60.00 ± 16.09a | 38.15 ± 9.76a | 37.23 ± 10.50a | 4.10 ± 4.89a | 3.68 ± 2.67a | ||
| 2nd course | 8.38 ± 6.17ab | 48.48 ± 13.87ab | 32.38 ± 9.15ab | 33.45 ± 8.73ab | 1.90 ± 3.04ab | 2.20 ± 2.39ab |
Group 1: One cone of moxibustion per treatment, three treatments/wk; Group 2: One cone of moxibustion per treatment, six treatments/wk; Group 3: Two cones of moxibustion per treatment, three treatments/wk; Group 4: Two cones of moxibustion per treatment, six treatments/wk; Before: Before treatment; 1st course: After the first course of treatment; 2nd course: After the second course of treatment; Birmingham: Birmingham irritable bowel syndrome symptom questionnaire; IBS-QOL: Irritable bowel syndrome Quality of Life Scale; SDS: Self-Rating Depression Scale; SAS: Self-Rating Anxiety Scale; HAMD: Hamilton Depression Scale; HAMA: Hamilton Anxiety Scale. Compared with the first course after treatment;
P < 0.001 vs before treatment;
P < 0.001 vs the first course after treatment;
P < 0.001 vs group 2.
Table 3 presents comparisons of the degree of symptom improvement for the patients in each group at different treatment stages. After the first course of treatment, an examination of the two levels of the two tested factors of aconite cake-separated moxibustion revealed that there were significant differences between the two moxibustion frequency levels with respect to the extent of the changes in HAMA scores, with greater changes noted for the “6 treatments/wk” groups than for the “3 treatments/wk” groups (P = 0.011); in addition, there were interaction effects between the number of cones and moxibustion frequency (P = 0.028). However, after the first course of treatment, there were no significant differences between the two tested dosage levels or the two tested frequency levels with respect to the degree of improvement in the Birmingham IBS symptom questionnaire, IBS-QOL, SDS, SAS, and HAMD scores (P > 0.05 for all). After the second course of treatment, an examination of the two levels of the two tested factors of aconite cake-separated moxibustion revealed that there were significant differences between the two moxibustion frequency levels with respect to the extent of changes in the Birmingham IBS symptom questionnaire scores, with greater changes in the “3 treatments/wk” groups than in the “6 treatments/wk groups (P = 0.002); in addition, there were no interactive effects between number of cones and the moxibustion frequency (P = 0.078). However, after the second course of treatment, there were no significant differences between the two tested dosage levels or the two tested frequency levels with respect to the degree of improvement in IBS-QOL, SDS, SAS, HAMD, and HAMA scores (P > 0.05 for all).
Table 3.
Comparisons of the degrees of improvement in symptoms and relevant scales for patients in each group at different stages of treatment
|
Frequency |
P value |
|||||||
| Scale | n | Cone | Three treatments/wk | Six treatments/wk | Cone | Frequency | Conefrequency | |
| Birmingham | 40 | 1 | 42.24 ± 36.12 | 35.20 ± 23.84 | 0.643 | 0.845 | 0.254 | |
| 40 | 2 | 30.30 ± 77.95 | 40.25 ± 29.15 | |||||
| IBS-QOL | 40 | 1 | 17.40 ± 19.04 | 20.25 ± 14.37 | 0.255 | 0.847 | 0.348 | |
| 40 | 2 | 22.63 ± 15.67 | 20.76 ± 13.83 | |||||
| SDS | 40 | 1 | 17.99 ± 17.02 | 10.49 ± 9.66 | 0.734 | 0.133 | 0.140 | |
| 1st course | 40 | 2 | 15.13 ± 19.32 | 15.06 ± 15.81 | ||||
| SAS | 40 | 1 | 13.72 ± 13.53 | 11.96 ± 9.97 | 0.279 | 0.535 | 0.849 | |
| 40 | 2 | 15.65 ± 13.50 | 14.72 ± 16.67 | |||||
| HAMD | 40 | 1 | 27.69 ± 48.61 | 39.54 ± 32.69 | 0.347 | 0.071 | 0.987 | |
| 40 | 2 | 33.78 ± 40.44 | 45.84 ± 42.93 | |||||
| HAMA | 40 | 1 | 12.04 ± 65.36 | 46.90 ± 28.61 | 0.458 | 0.011 | 0.028 | |
| 40 | 2 | 33.62 ± 44.65 | 36.19 ± 37.95 | |||||
| Birmingham | 40 | 1 | 73.74 ± 19.43 | 56.19 ± 21.62 | 0.393 | 0.002 | 0.078 | |
| 40 | 2 | 70.46 ± 27.24 | 65.56 ± 20.91 | |||||
| IBS-QOL | 40 | 1 | 29.98 ± 16.59 | 34.26 ± 13.63 | 0.247 | 0.208 | 0.562 | |
| 40 | 2 | 34.02 ± 15.29 | 35.60 ± 12.88 | |||||
| SDS | 40 | 1 | 26.12 ± 16.15 | 21.65 ± 14.35 | 0.149 | 0.373 | 0.373 | |
| 2nd course | 40 | 2 | 27.51 ± 17.52 | 27.51 ± 15.12 | ||||
| SAS | 40 | 1 | 23.68 ± 12.83 | 22.54 ± 12.14 | 0.871 | 0.604 | 0.996 | |
| 40 | 2 | 24.02 ± 15.77 | 22.90 ± 13.81 | |||||
| HAMD | 40 | 1 | 63.06 ± 36.74 | 68.88 ± 32.05 | 0.139 | 0.182 | 0.845 | |
| 40 | 2 | 69.63 ± 30.35 | 77.45 ± 29.05 | |||||
| HAMA | 40 | 1 | 49.62 ± 46.44 | 62.61 ± 38.66 | 0.502 | 0.238 | 0.450 | |
| 40 | 2 | 59.19 ± 49.29 | 62.04 ± 32.62 | |||||
1st course: After the first course of treatment; 2nd course: After the second course of treatment; Birmingham: Birmingham irritable bowel syndrome symptom questionnaire; IBS-QOL: Irritable bowel syndrome Quality of Life Scale; SDS: Self-Rating Depression Scale; SAS: Self-Rating Anxiety Scale; HAMD: Hamilton Depression Scale; HAMA: Hamilton Anxiety Scale.
Table 4 presents a correlation analysis indicating how the degrees of improvement in the scores of the utilized scales relate to the degree of improvement in symptoms. Because there were significant improvements in the scores for each scale after the second course of treatment, we performed a correlation analysis for the extent of changes in each scale and the degree of improvement in symptoms after the second course of treatment. The results of this analysis indicated that in the aconite cake-separated moxibustion groups, there were statistically significant correlations between the degree of symptom improvement and the degrees of SDS and SAS score improvement (SDS: r = 0.165, P = 0.037; SAS: r = 0.161, P = 0.042). Thus, for aconite cake-separated moxibustion treatment, the degrees of improvement in SDS and SAS scores appeared to be linearly correlated with the degrees of improvement in symptoms.
Table 4.
Correlation analysis of the degrees of improvements in relevant scales and the degrees of symptom improvement
| Group | n | Degrees of symptom improvement (Birmingham) | Degrees of improvements in relevant scales | r | P value | |
| Aconite cake-separated moxibustion groups | 160 | 66.49 ± 23.25 | IBS-QOL | 33.46 ± 14.68 | 0.080 | 0.317 |
| SDS | 25.70 ± 15.87 | 0.165 | 0.037 | |||
| SAS | 23.28 ± 13.59 | 0.161 | 0.042 | |||
| HAMD | 69.75 ± 32.28 | 0.088 | 0.276 | |||
| HAMA | 58.36 ± 42.19 | 0.331 | 0.077 | |||
Birmingham: Birmingham irritable bowel syndrome symptom questionnaire; IBS-QOL: Irritable bowel syndrome Quality of Life Scale; SDS: Self-Rating Depression Scale; SAS: Self-Rating Anxiety Scale; HAMD: Hamilton Depression Scale; HAMA: Hamilton Anxiety Scale.
Safety assessment
Two adverse events occurred during treatment (2/160). Both of these events were mild burns during moxibustion (with one event in group 2 and the other event in group 4). No serious adverse events occurred.
DISCUSSION
In modern medicine, medication time and frequency are regulated in accordance with drug half-lives; these restrictions lead to the strict control of drug cycles. The most significant difference between moxibustion and medication is that moxibustion requires cooperation between doctors and patients. The required time and the frequency of moxibustion treatments are mainly determined by doctors’ experiences. This approach will clearly result in certain errors that diminish moxibustion efficacy. Therefore, the standardization of moxibustion frequency, number of cones, and the size and weight of moxa cones, among other factors, has important significance for improving the clinical efficacy of moxibustion.
We know that effects associated with moxibustion depend largely on the thermal effects of this treatment approach[33]; in turn, the generation of these thermal effects depends on the quality of the moxibustion material, the moxa cone volume, and the number of cones applied. Aconite cake-separated moxibustion, which is an important component of moxibustion therapy, has certain distinctive characteristics. Each aspect of aconite cake-separated moxibustion may influence treatment outcomes; in particular, factors that may affect outcomes include the quality of the moxibustion material, the size of the moxa cones, the weight of the moxa cones, the aconite cake production process, the number of cones used for moxibustion, and the moxibustion frequency and duration, among other considerations. In this study, the quality of the moxibustion material, the size of the moxa cones, and the aconite cake production process were standardized. A factorial design approach was used to examine various combinations of number of cones and moxibustion frequency and thereby investigate the effects of number of cones and moxibustion frequency on the efficacy of aconite cake-separated moxibustion.
This randomized controlled trial used IBS-related scales to observe the effects of aconite cake-separated moxibustion treatment approaches involving different numbers of cone per treatment and different moxibustion frequencies on the improvement of symptoms in IBS patients. The results demonstrated that in all four treatment groups, aconite cake-separated moxibustion could significantly decrease the Birmingham IBS symptom questionnaire scores and the IBS-QOL, SDS, SAS, HAMD, and HAMA scores of IBS patients. These results indicated that for IBS patients, aconite cake-separated moxibustion treatment approaches involving different numbers of cone per treatment and different moxibustion frequencies could produce significant therapeutic effects that include improving clinical symptoms, increasing quality of life, and relieving anxiety and depression.
In addition to gastrointestinal symptoms, IBS is also closely associated with anxiety and depression[34,35]. IBS-related gastrointestinal symptoms and psychological conditions can severely affect patients’ quality of life[36-38]. The survey results from a prior study[39] have indicated that populations with high anxiety and depression scores had a higher incidence of IBS compared with other populations. Investigations[40,41] have also revealed correlations among the severity of gastrointestinal symptoms, the severity of psychological conditions, and the abnormal activation of certain brain regions in IBS patients; once patients’ emotional states improved, this abnormal activation of brain regions diminished. These results provided objective evidence that psychological factors influence the pathogenesis of IBS. A previous study by our research group[42] also found that in clinical practice, mild emotional stimuli can aggravate or induce gastrointestinal symptoms in IBS patients. This phenomenon occurred repeatedly; as a result, a considerable percentage of IBS patients treated in a clinical context had conditions accompanied by various degrees of anxiety, depression, and other psychological symptoms. Through brain-gut interactions, these psychological conditions can further aggravate gastrointestinal symptoms, thus creating a reciprocal causation of the physical and psychological symptoms of IBS. In this study, to examine the improvement of IBS patients’ mood-related symptoms with aconite cake-separated moxibustion, we selected two types of mood-related scales to determine patients’ anxiety and depression scores and their self-perceived anxiety and depression scores. The results demonstrated that IBS patients suffered from emotional disorders to various extents. In the four aconite cake-separated moxibustion groups, the average symptom, quality of life, SDS, SAS, HAMD, and HAMA scores were all significantly lower after the first and second courses of treatment than before treatment. A further correlation analysis examining how the degrees of symptom improvement related to the degrees of improvement in relevant scales revealed that improvements in SAS and SDS scores were linearly correlated with improvements in symptoms. These findings indicated that aconite cake-separated moxibustion could significantly improve emotional disorders in IBS patients and that these emotional improvements could also significantly relieve patients’ IBS symptoms.
We performed statistical analyses on the symptom and quality of life scale scores and four emotion-related scales for the four groups of aconite cake-separated moxibustion patients at different time points. The results of these analyses demonstrated that the post-treatment scores significantly differed from the pretreatment scores. The scores on all scales were significantly lower after the first course of treatment than before treatment, and after the second course of treatment than after the first course of treatment, indicating that treatment duration may influence efficacy. After the end of the second course of treatment, the Birmingham IBS symptom questionnaire score was significantly lower for group 1 (1 cone, 3 treatments/wk) and group 3 (2 cones, 3 treatments/wk) compared with group 2 (1 cone, 6 treatments/wk). In particular, the “1 cone, 3 treatments/wk” group produced the lowest symptom score, suggesting that this regimen may produce the best therapeutic efficacy for the second course of aconite cake-separated moxibustion treatment.
We can draw the following conclusions from the factorial analysis results for the number of cones and moxibustion frequency. After the first course of treatment, an examination of the two levels of the two tested factors of aconite cake-separated moxibustion revealed that there were significant differences between the two moxibustion frequency levels in terms of the extent of the HAMA score changes, with greater changes observed in the “6 treatments/wk” groups than in the “3 treatments/wk” groups; in addition, there were interactive effects between the number of cones and moxibustion frequency (P = 0.028). After the second course of treatment, an examination of the two levels of the two tested factors of aconite cake-separated moxibustion revealed that there were significant differences between the two moxibustion frequency levels with respect to the extent of symptom score changes, with greater changes observed in the “3 treatments/wk” groups than in the “6 treatments/wk groups. These results indicated that moxibustion frequency had a significant impact on the degree of improvement in HAMA scores after the first course of treatment and the degree of symptom improvement after the second course of treatment. Interactive effects between the number of cones and the moxibustion frequency had a significant influence on the degree of HAMA score improvement. Therefore, we infer that moxibustion frequency is a key factor in symptom improvement and anxiety relief resulting from aconite cake-separated moxibustion and that the factor of number of cones has synergistic effects with moxibustion frequency for relieving anxiety. The study results demonstrated that during the first course of treatment, patient anxiety was improved more with 6 treatments/wk than with 3 treatments/wk; during the second course of treatment, patient symptoms were improved more with three treatments/wk than with six treatments/wk. We speculated that during the early stages of treatment, a higher number of moxibustion treatments could better relieve IBS patients’ anxiety; as the treatment duration extended, 3 treatments/wk produced more improvement in patient conditions than 6 treatments/wk did. IBS is a chronic and recurrent functional intestinal disorder; most IBS patients require long-term treatment. Therefore, based on the comprehensive results of our study, we propose that of the examined treatment regimens, the optimal regimen for treating D-IBS with aconite cake-separated moxibustion involves one cone per treatment and three treatments per wk.
However, this study had certain limitations. Notably, better experimental results could be obtained if the study subjects could be stratified in various ways, such as by creating specific patient subgroups based on gender, disease duration, and age, or if an increased number of moxibustion frequency and dosage groups could be tested. In addition, patient follow-up after treatment is an important aspect of evaluating D-IBS treatment using aconite cake-separated moxibustion. Therefore, the aforementioned improvements to the current investigation will serve as important bases for our future research.
In summary, aconite cake-separated moxibustion is an effective and safe therapeutic approach for D-IBS. One cone per treatment and three treatments per wk is a reasonable therapeutic regimen for D-IBS. This recommended regimen can ensure therapeutic efficacy for patients without excessively increasing the economic pressure on patients. The findings of this study provide a reliable basis for the clinical treatment of D-IBS using aconite cake-separated moxibustion.
COMMENTS
Background
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. Clinical studies have confirmed the efficacy of herbal cake-separated moxibustion in IBS patients; however, the relationship between the quantity of stimulation with herbal cake-separated moxibustion and the resulting therapeutic efficacy has not yet been established.
Research frontiers
Herb cake-separated moxibustion is an indirect moxibustion therapy with a variety of materials. It can relieve the symptoms of abdominal pain and diarrhea, and effectively treat diarrhea-IBS (D-IBS). Therefore, factorial design was used to study the effect relationship of aconite cake-separated moxibustion in the treatment of D-IBS and to pick out a better treatment. The findings of this study provide a reliable basis for the clinical treatment of D-IBS with aconite cake-separated moxibustion.
Innovations and breakthroughs
Many previous studies on treatment of IBS with moxibustion are merely observation of efficacy. Based on moxibustion being effective for IBS, this research adopts factorial design to explore the efficacy of aconite cake-separated moxibustion in the treatment of D-IBS, as well as effects of different frequency and different cone number of aconite cake-separated moxibustion in the treatment of D-IBS, and to pick out an optimal regimen as a better treatment for D-IBS. The study provides a reliable clinical basis for future clinical treatment of D-IBS with aconite cake-separated moxibustion.
Applications
The findings of this study provide a reliable basis for the clinical treatment of D-IBS with aconite cake-separated moxibustion.
Peer review
This is a well-designed study in which authors adopt factorial design to study the effect of aconite cake-separated moxibustion in the treatment of D-IBS, and pick out an optimal regimen as a better treatment of D-IBS, and provide a reliable clinical basis for the clinical treatment of D-IBS with aconite cake-separated moxibustion.
Footnotes
Supported by National Basic Research Program of China (973 Program), No. 2009CB522900, 2009CB522901; Shanghai Top Clinical Medical Center of Acupuncture, Moxibustion and Tuina; and National Natural Sciences Foundation of China, Nos. 81303031 and 81202752
P- Reviewer: Rahimi R, Rhoads JM S- Editor: Nan J L- Editor: Wang TQ E- Editor: Du P
References
- 1.Spiller R. Recent advances in understanding the role of serotonin in gastrointestinal motility in functional bowel disorders: alterations in 5-HT signalling and metabolism in human disease. Neurogastroenterol Motil. 2007;19 Suppl 2:25–31. doi: 10.1111/j.1365-2982.2007.00965.x. [DOI] [PubMed] [Google Scholar]
- 2.Brooks JC, Zambreanu L, Godinez A, Craig AD, Tracey I. Somatotopic organisation of the human insula to painful heat studied with high resolution functional imaging. Neuroimage. 2005;27:201–209. doi: 10.1016/j.neuroimage.2005.03.041. [DOI] [PubMed] [Google Scholar]
- 3.Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9:463–484. doi: 10.1016/j.ejpain.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Ochsner KN, Ludlow DH, Knierim K, Hanelin J, Ramachandran T, Glover GC, Mackey SC. Neural correlates of individual differences in pain-related fear and anxiety. Pain. 2006;120:69–77. doi: 10.1016/j.pain.2005.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan G, Lu S, Ke M, Han S, Guo H, Fang XC. An epidemiologic study of irritable bowel syndrome in Beijing-a stratified randomized study by clustering sampling. Zhonghua Liuxingbingxue Zazhi. 2000;21:26–29. [PubMed] [Google Scholar]
- 6.Carmona-Sánchez R, Tostado-Fernández FA. Prevalence of use of alternative and complementary medicine in patients with irritable bowel syndrome, functional dyspepsia and gastroesophageal reflux disease. Rev Gastroenterol Mex. 2005;70:393–398. [PubMed] [Google Scholar]
- 7.Park JW, Lee BH, Lee H. Moxibustion in the management of irritable bowel syndrome: systematic review and meta-analysis. BMC Complement Altern Med. 2013;13:247. doi: 10.1186/1472-6882-13-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee J, Yoon SW. Efficacy and Safety of Moxibustion for Relieving Pain in Patients With Metastatic Cancer: A Pilot, Randomized, Single-Blind, Sham-Controlled Trial. Integr Cancer Ther. 2013;13:211–216. doi: 10.1177/1534735413510025. [DOI] [PubMed] [Google Scholar]
- 9.Gao X, Xu C, Wang P, Ren S, Zhou Y, Yang X, Gao L. Curative effect of acupuncture and moxibustion on insomnia: a randomized clinical trial. J Tradit Chin Med. 2013;33:428–432. doi: 10.1016/s0254-6272(13)60143-0. [DOI] [PubMed] [Google Scholar]
- 10.Yan J. New breakthrough of treating bowel diseases with moxibustion, Project of technology and clinical application of treating bowel diseases with moxibustion. Zhongguo Keji Jiangli. 2014;3:58–59. [Google Scholar]
- 11.Wu HG, Zhao C, Shi Z, Chen HP, Liu Y, Liu SM. Clinical study on spleen-stomach-reinforcing moxibustion treatment of diarrhea-type irritable bowel syndrome. World J Acupunct-Moxibust. 2002;1:10–15. [Google Scholar]
- 12.Liu HR, Hua XG, YangY , Wu HG. Clinical study on 5-HT expression in colonic mucosa and the treatment of herb-partition moxibustion in diarrhea-predominant IBS. Liaoning Zhongyi Zazhi. 2006;33:984–985. [Google Scholar]
- 13.Wu LY, Bao CH, Ge LB, Zhou CL, Liu HR, Qi L, Wu HG, Wang XM. Mild moxibustion at Tianshu (ST 25) decreases expression of prokineticin-1 and prokineticin receptor-1 in colon tissue of rats with chronic visceral hyperalgesia. Neural Regen Res. 2011;6:2600–2604. [Google Scholar]
- 14.Yi T, Qi L, Wu HG, Ma XP, Liu HR, Wang XM. Analgesic action of suspended moxibustion in rats with chronic visceral hyperalgesia correlates with enkephalins in the spinal cord. Neural Regen Res. 2012;7:219–222. doi: 10.3969/j.issn.1673-5374.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou EH, Liu HR, Wu HG, Shi Y, Wang XM, Tan LY, Yao LQ, Zhong YS, Jiang Y, Zhang LL. Suspended moxibustion relieves chronic visceral hyperalgesia via serotonin pathway in the colon. Neurosci Lett. 2009;451:144–147. doi: 10.1016/j.neulet.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 16.Liu HR, Qi L, Wu LY, Ma XP, Qin XD, Huang WY, Dong M, Wu HG. Effects of moxibustion on dynorphin and endomorphin in rats with chronic visceral hyperalgesia. World J Gastroenterol. 2010;16:4079–4083. doi: 10.3748/wjg.v16.i32.4079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou EH, Wang XM, Ding GH, Wu HG, Qi L, Liu HR, Zhang SJ. Suspended moxibustion relieves chronic visceral hyperalgesia and decreases hypothalamic corticotropin-releasing hormone levels. World J Gastroenterol. 2011;17:662–665. doi: 10.3748/wjg.v17.i5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qi L, Liu HR, Yi T, Wu LY, Liu XR, Zhao C, Shi Y, Ma XP, Wu HG. Warming Moxibustion Relieves Chronic Visceral Hyperalgesia in Rats: Relations to Spinal Dynorphin and Orphanin-FQ System. Evid Based Complement Alternat Med. 2013;2013:920675. doi: 10.1155/2013/920675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou EH, Liu HR, Wu HG, Shi Y, Wang XM, Yao LQ, Zhong YS, Yang Y. Herb-partition moxibustion relieves chronic visceral hyperalgesia and 5-HT concentration in colon mucosa of rats. Neurol Res. 2009;31:734–737. doi: 10.1179/174313209X382313. [DOI] [PubMed] [Google Scholar]
- 20.Ma YX, Liu X, Liu CZ, Wang LP, Guo G, Du DQ, Wang ZL, Ma H, Qi P, Li ZF, et al. Randomized clinical trial: the clinical effects of herb-partitioned moxibustion in patients with diarrhoea-predominant irritable bowel syndrome. Evid Based Complement Alternat Med. 2013;2013:605460. doi: 10.1155/2013/605460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qi L, Li N, Liu HR, Ma XP, Wu LY, Wang XM, Zhou CL, Wu HG. Clinical and experimental studies on muxibustion for treatment of irritable bowel syndrome. Zhonghua Zhongyiyao Zazhi. 2010;25:2224–2227. [Google Scholar]
- 22.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 23.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 24.Roalfe AK, Roberts LM, Wilson S. Evaluation of the Birmingham IBS symptom questionnaire. BMC Gastroenterol. 2008;8:30. doi: 10.1186/1471-230X-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, Jia H, Bangdiwala SI. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95:999–1007. doi: 10.1111/j.1572-0241.2000.01941.x. [DOI] [PubMed] [Google Scholar]
- 26.Li HY, Gao L, Li NX. Evaluation of IBS-QOL scale in irritable bowel syndrome. Zhongguo Xunzheng Yixue Zazhi. 2004;12:875–877. [Google Scholar]
- 27.Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. 1965;13:508–515. doi: 10.1001/archpsyc.1965.01730060026004. [DOI] [PubMed] [Google Scholar]
- 28.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 29.Xu J, Wei Y. Social support as a moderator of the relationship between anxiety and depression: an empirical study with adult survivors of Wenchuan earthquake. PLoS One. 2013;8:e79045. doi: 10.1371/journal.pone.0079045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 31.Miller IW, Bishop S, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- 32.Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14:61–68. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- 33.Lee MS, Kang JW, Ernst E. Does moxibustion work? An overview of systematic reviews. BMC Res Notes. 2010;3:284. doi: 10.1186/1756-0500-3-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li SJ, Su BZ. Irritable bowel syndrome investigation of psychological factors. Inner Mongolia Yixue Zazhi. 2011;43:833–834. [Google Scholar]
- 35.Tosic-Golubovic S, Miljkovic S, Nagorni A, Lazarevic D, Nikolic G. Irritable bowel syndrome, anxiety, depression and personality characteristics. Psychiatr Danub. 2010;22:418–424. [PubMed] [Google Scholar]
- 36.Tarrerias AL, Costil V, Vicari F, Létard JC, Adenis-Lamarre P, Aisène A, Batistelli D, Bonnaud G, Carpentier S, Dalbiès P, et al. The effect of inactivated Lactobacillus LB fermented culture medium on symptom severity: observational investigation in 297 patients with diarrhea-predominant irritable bowel syndrome. Dig Dis. 2011;29:588–591. doi: 10.1159/000332987. [DOI] [PubMed] [Google Scholar]
- 37.Coffin B, Dapoigny M, Cloarec D, Comet D, Dyard F. Relationship between severity of symptoms and quality of life in 858 patients with irritable bowel syndrome. Gastroenterol Clin Biol. 2004;28:11–15. doi: 10.1016/s0399-8320(04)94834-8. [DOI] [PubMed] [Google Scholar]
- 38.Sabate JM, Veyrac M, Mion F, Siproudhis L, Ducrotte P, Zerbib F, Grimaud JC, Dapoigny M, Dyard F, Coffin B. Relationship between rectal sensitivity, symptoms intensity and quality of life in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2008;28:484–490. doi: 10.1111/j.1365-2036.2008.03759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spence MJ, Moss-Morris R. The cognitive behavioural model of irritable bowel syndrome: a prospective investigation of patients with gastroenteritis. Gut. 2007;56:1066–1071. doi: 10.1136/gut.2006.108811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drossman DA, Ringel Y, Vogt BA, Leserman J, Lin W, Smith JK, Whitehead W. Alterations of brain activity associated with resolution of emotional distress and pain in a case of severe irritable bowel syndrome. Gastroenterology. 2003;124:754–761. doi: 10.1053/gast.2003.50103. [DOI] [PubMed] [Google Scholar]
- 41.Morgan V, Pickens D, Gautam S, Kessler R, Mertz H. Amitriptyline reduces rectal pain related activation of the anterior cingulate cortex in patients with irritable bowel syndrome. Gut. 2005;54:601–607. doi: 10.1136/gut.2004.047423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen YH, Chen XK, Yin XJ. [Comparison of the therapeutic effects of electroacupuncture and probiotics combined with deanxit in treating diarrhea-predominant irritable bowel syndrome] Zhongguo Zhongxiyi Jiehe Zazhi. 2012;32:594–598. [PubMed] [Google Scholar]


