Abstract
INTRODUCTION
De Garengeot hernia is a rare occurrence whereby an appendix is found in a femoral hernia sac. It is rarer still to find an acutely inflamed appendix manifesting itself as a strangulated femoral hernia. This case is important to report as it highlights the diagnostic difficulty this particular condition presents to an emergency surgeon.
PRESENTATION OF CASE
We report the case of an 86 year old female who was found to have a De Garengeot hernia containing a necrotic appendix. A retrograde appendicectomy was performed to prevent peritoneal contamination. The hernia defect was repaired using a standard repair with non-absorbable suture.
DISCUSSION
De Garengeot's hernia is a rare occurrence, is often unexpected and tends to be diagnosed intra-operatively. Pre-operative diagnosis remains difficult and it will often masquerade as a strangulated femoral hernia. In stable patients, where there is a diagnostic uncertainty CT scanning is a useful adjunct and may allow a laparoscopic approach to be undertaken in the absence of appendicitis.
CONCLUSION
A De Garengeot's hernia should be considered as a differential diagnosis in patients presenting with clinical signs of a strangulated femoral hernia. It is often an incidental finding during an emergency operation. Although mesh repairs in the presence of appendicitis have been reported, the safest approach remains a primary suture repair.
1. Introduction
The presence of an appendix in a femoral hernial sac is a rare occurrence and was first described in 1731 by the French surgeon De Garengeot. Although the number of reported cases has been steadily increasing over the last few decades, the diagnosis is almost always made intra-operatively due to the atypical clinical presentation and the non-specific radiological findings. We present a case report of De Garengeot's hernia, with an associated appendicitis and briefly discuss the presentation, pathogenesis, diagnosis and surgical considerations when faced with this rare clinical entity.
2. Case report
An 86-year-old woman was admitted to a district general hospital with a three-day history of right inguinal swelling and tenderness. On physical examination she was haemo-dynamically stable and afebrile. On closer examination of the right groin there was a 4 cm × 5 cm tender, irreducible mass located inferior and lateral to the pubic tubercle, associated with erythematous skin changes. There was no clinical evidence of bowel obstruction. Laboratory tests revealed: Hb 13.3 g/dl, WCC 12,200/mm3, CRP 55. A strangulated femoral hernia was suspected and the patient was subsequently evaluated with an ultrasound scan. This was reported as an irreducible femoral hernia, with a hernial sac containing undilated small bowel.
She received a course of antibiotics and was then taken to theatre for an open exploration. A standard oblique incision at the level of the inguinal ligament was used to access the femoral hernial sac. A necrotic appendix was found upon opening the sac (Fig. 1), associated with purulent fluid. A McEvedy approach was then used to enter the peritoneal cavity. It was found that the peritoneal aspect of the appendix was normal. A retrograde appendicectomy was thus performed to prevent peritoneal contamination. The hernia defect was repaired using a standard repair with non-absorbable sutures. The patient made an uneventful post-operative recovery. She was able to eat and drink the same evening and was discharged on the fourth postoperative day. Histological examination of the appendix revealed acute appendicitis.
Fig. 1.
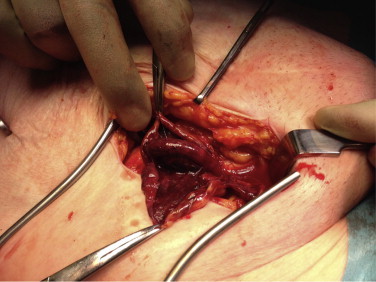
A De Garengeot hernia demonstrating a necrotic appendix.
3. Discussion
Although an incarcerated femoral hernia, containing the vermiform appendix was first described in 1731, by the French surgeon Rene Jacques Croissant de Garengeot, it wasn’t given its eponymous name until very recently.1 In their 2005 article, Akopian et al. proposed the eponymous nomenclature, but had only identified 70 cases in the literature at the time. Indeed, the incidence of an appendix within a femoral hernia sac is very rare, accounting for only 1% of the cases 2 and the finding of an acutely inflamed appendix is rarer still occurring in 0.08–0.013% of all patients.3 De Garengeot's hernia is more common in women, particularly in post-menopausal females, as one would expect given the higher incidence of femoral hernias in general.3 As was found in our case, a De Garengeot hernia is often an incidental finding at the time of surgery, usually following a provisional diagnosis of strangulated bowel in a femoral hernia.
The pathogenesis of De Garengeot's hernia remains controversial. Nguyen et al. suggested an abnormal intestinal rotation during embryological development, with an atypical appendocaecal attachment. This in theory would give rise to a caecal appendix with a high risk of herniation through the femoral canal.4 Zissin et al. however, suggest that an anatomically large caecum could contribute and push the appendix into the femoral hernia.5 There are also several theories as to the cause of the appendicitis. Some have suggested that there is an initial inflammation of the appendix within the peritoneum and then a subsequent gradual migration into the hernia sac. However, others suggest that the migration is the initial event and that the narrow and rigid femoral neck leads to the incarceration and strangulation of the appendix.6 This seems consistent with our findings whereby the peritoneal component of the appendix was normal.
The majority of cases, like ours, present with symptoms and signs of an incarcerated or strangulated femoral hernia. The tight neck of the femoral canal can mask the signs of appendicitis by preventing the spread of inflammation back into the peritoneal cavity. Even patients with a perforated appendix can present without signs of peritonitis.9 In a recent review of 36 cases, Kalles et al. demonstrated that all patients presented with a tender groin mass, with 35 of them being on the right side.10 Furthermore, only 14% of the patients reported any bowel symptoms such as nausea and vomiting. These results correlate with our case but also highlight the difficulty in making a clinical diagnosis. In particular, the numerous differential diagnoses of a groin lump such as inguinal hernias, lymphoma, lipoma, a varix node makes the clinical diagnosis challenging.
Where there is diagnostic uncertainty, ultrasound scanning (USS) is usually the imaging modality of first choice. However, it is well known that USS is operator dependent and there is only one reported case in which a De Garengeot hernia was diagnosed using USS.11 The most useful from of imaging in cases of diagnostic uncertainty appears to be computed tomography (CT). The majority of cases that have been diagnosed pre-operatively have been by CT scanning.6–8 Typical findings demonstrated on CT are a femoral hernia associated with a tubular structure and a low positioned caecum.5,7,8,10
With regards to surgical management, no standard treatment of choice exists. There are several potential options, which include laparoscopic or open approaches either with a mesh or simple suture herniorrhaphy, with or without appendicectomy. The treatment modality depends on a number of factors, including the patient's condition, any co-morbidities, surgeon preference and clinical findings during surgery. In general, most cases are treated with an emergency appendectomy and hernioplasty. Some authors have suggested that a finding of a normal appendix doesn’t necessitate appendectomy and report several successful cases of simple reduction of the appendix followed by a laparoscopic hernia mesh repair.12,13 Most cases, however, report an open hernia repair due to the fact that most patients are diagnosed intra-operatively in an emergency setting. It is clear that a laparoscopic approach has advantages and is a particularly useful approach in the absence of appendicitis allowing a better characterization of the hernia.3 However, an open approach should be used in cases such as ours where there is the possibility of strangulated bowel. Where possible, peritoneal contamination should be avoided and we suggest that a retrograde appendicectomy is an option in the surgeon's armamentarium particularly when there is no evidence of peritoneal appendicitis. Whether one uses a mesh repair or a suture repair remains open to debate. Although some authors have reported successful mesh repairs in the presence of appendicitis, we would advocate a suture repair in the presence of a perforation, abscess formation or the presence of purulent fluid as was found in our case.4,14
4. Conclusion
De Garengeot's hernia is a rare occurrence, is often unexpected and tends to be diagnosed intra-operatively. Pre-operative diagnosis remains difficult and it will often masquerade as a strangulated femoral hernia. In stable patients, where there is a diagnostic uncertainty CT scanning is a useful adjunct and may allow a laparoscopic approach to be undertaken in the absence of appendicitis. Although mesh repairs in the presence of appendicitis have been reported, the safest approach remains a primary suture repair.
Conflicts of interest
The authors declare that there is no conflict of interest.
Funding
None.
Ethical approval
N/A.
Author contributions
All authors were involved in the researching and editing of the manuscript. A Hussain and A Slesser wrote the case report. The surgery was done by A Slesser and J Maalo. M soskin was the anesthetist and took the photograph. J Arbuckle was the consultant in charge of the patients care.
Consent
Written informed consent was obtained from the patient for publication of this case report and case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Key learning points.
-
•
De Garengeot hernia is a rare occurrence whereby an appendix is found in a femoral hernia sac.
-
•
Pre-operative diagnosis remains difficult and it will often masquerade as a strangulated femoral hernia.
-
•
It is often an incidental finding during an emergency operation.
-
•
Although mesh repairs in the presence of appendicitis have been reported, the safest approach remains a primary suture repair.
References
- 1.Akopian G., Alexander M. De. Garengeot hernia: appendicitis within a femoral hernia. Am Surg. 2005;71(6):526–527. [PubMed] [Google Scholar]
- 2.Voitk A.J., McFarlane J.K., Estrada R.L. Ruptured appendicitis in femoral hernias: report of two cases and review of the literature. Ann Surg. 1974;179:24–26. doi: 10.1097/00000658-197401000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rajan S.S., Girn H.R., Ainslie W.G. Inflamed appendix in a femoral hernial sac: de Garengeot's hernia. Hernia. 2009;13(5):551–553. doi: 10.1007/s10029-009-0472-7. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen E.T., Komenaka I.K. Strangulated femoral hernia containing a perforated appendix. Can J Surg. 2004;47:68–69. [PMC free article] [PubMed] [Google Scholar]
- 5.Zissin R., Brautbar O., Shapiro-Feinberg M. CT diagnosis of acute appendicitis in a femoral hernia sac. Br J Radiol. 2000;73:1013–1014. doi: 10.1259/bjr.73.873.11064659. [DOI] [PubMed] [Google Scholar]
- 6.Barbaros U., Asoglu O., Seven R., Kalayci M. Appendicitis in incarcerated femoral hernia. Hernia. 2004;8:281–282. doi: 10.1007/s10029-004-0209-6. [DOI] [PubMed] [Google Scholar]
- 7.D’Ambrosio N., Katz D., Hines J. Perforated appendix within a femoral hernia. AJR. 2006;186:906–907. doi: 10.2214/AJR.05.0080. [DOI] [PubMed] [Google Scholar]
- 8.Fukukura Y., Chang S. Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom Imaging. 2005;30(5) doi: 10.1007/s00261-004-0283-3. [DOI] [PubMed] [Google Scholar]
- 9.Cordera F., Sarr M.G. Incarcerated appendix in a femoral hernia sac. Comtemp Surg. 2009;59:35–37. [Google Scholar]
- 10.Kalles V., Mekras A., Mekras D., Papapanagiotou I., Al-Harethee W., Sotiropoulos G. De Garengeot's hernia: a comprehensive review. Hernia. 2013;17:177–182. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]
- 11.Filatov J., Ilibitzki A., Davidovitch S., Soudack M. Appendicitis within a femoral hernia: sonographic appearance. J Ultrasound Med. 2006;25:1233–1235. doi: 10.7863/jum.2006.25.9.1233. [DOI] [PubMed] [Google Scholar]
- 12.Doddi S., Sagar V., Singhal T. vol. 2010. 2010. Femoral hernia with a twist. (Case Reports in Medicine). Article ID 650829, 3 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma H., Jha P.K., Shekhawat N.S. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11:235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 14.Ebisawa K., Yamazaki S., Kimura Y., Kashio M., Kurito K., Yasumuro S. Acute appendicitis in an incarcerated femoral hernia: a case of De Garengeot hernia. Case Rep Gastroenterol. 2009;3:313–317. doi: 10.1159/000250821. [DOI] [PMC free article] [PubMed] [Google Scholar]


