Abstract
We have investigated the in vitro antimicrobial effects of antibiotic combinations against Orientia tsutsugamushi, the causative agent of scrub typhus. ECV304 cells were infected with the Boryong strain of O. tsutsugamushi and incubated in a medium containing doxycycline (4 µg/mL), azithromycin (0.5 µg/mL), rifampin (4 µg/mL), ciprofloxacin (25 µg/mL), gentamicin (5 µg/mL), cefotaxime (2 µg/mL), or combinations of these agents for 7 days, after which immunofluorescent staining for O. tsutsugamushi was performed. The percentages of infective foci in cultures containing antibiotics compared to those in cultures without antibiotics were 6.2% for doxycycline, 9.6% for azithromycin, 8.8% for rifampin, 96.6% for cefotaxime, 29.7% for doxycycline plus cefotaxime, 23.6% for azithromycin plus cefotaxime, and 41.4% for rifampin plus cefotaxime. These findings show an in vitro antagonism between anti-rickettsial agents and cefotaxime against O. tsutsugamushi. These results suggest that the efficacy of antibiotic combinations involving cefotaxime for the treatment of patients with scrub typhus, particularly those with severe pneumonia, needs to be investigated.
Keywords: Azithromycin, Cefotaxime, Drug combination, Doxycycline, Drug antagonism, Orientia tsutsugamushi, Scrub typhus
Introduction
Scrub typhus, which is caused by Orientia species, can be successfully treated with certain antibiotics such as doxycycline, rifampin, and azithromycin. These antibiotics, however, have only bacteriostatic effects against O. tsutsugamushi [1]. Therefore, they cannot prevent the persistence of O. tsutsugamushi in humans [2]. Persistence of the organism is associated with early recurrence, prolonged convalescence, and recrudescent pneumonia [2, 3].
Combination antibiotic therapy has been used to lower the treatment failure rate for various difficult-to-treat bacterial infections such as tuberculosis or brucellosis. Because there are several situations in which combination antibiotic therapy is needed for scrub typhus, e.g., when the patient presents with secondary bacterial pneumonia, it is important to investigate how combinations of antibiotics influence the clinical outcome of scrub typhus. A clinical trial of rifampin combined with doxycycline for treating scrub typhus was terminated prematurely because of a poor clinical response [4]. However, there have been no investigations into the mechanism(s) underlying the poor response to this combination. Results of a previous in vitro experiment with flow cytometry revealed that antagonism occurred when azithromycin was combined with cefotaxime against O. tsutsugamushi [5]. In the present study, we have investigated the antimicrobial effects of various combinations of doxycycline, azithromycin, rifampin, ciprofloxacin, gentamicin, and cefotaxime against O. tsutsugamushi.
The procedure has been described in detail previously [2, 6]. A stock solution of the O. tsutsugamushi Boryong strain was inoculated onto a monolayer of ECV304 cells seeded in a 75-cm2 culture flask. When the infected ECV304 cells showed maximal cytopathic effects, the degree of infection of ECV304 cells was assessed by immunofluorescence (IF) staining. The cells were then disrupted with glass beads and centrifuged at 350 g for 5 minutes. The resultant supernatant was divided equally into 9 aliquots, which were inoculated onto ECV304 monolayers grown on cover slips in 6-well culture plates and incubated for 4 hours. At the end of the initial incubation period, the inoculum was replaced with fresh medium containing doxycycline (4 µg/mL), azithromycin (0.5 µg/mL), rifampin (4 µg/mL), cefotaxime (2 µg/mL), ciprofloxacin (25 µg/mL), gentamicin (5 µg/mL), one of the combinations shown in Table 1, or doxycycline plus azithromycin plus gentamicin. All antibiotics were obtained from Sigma (St. Louis, MO, USA). The cultures with antibiotics were incubated for 3 days, after which the medium was replaced with fresh medium containing the same antibiotic or combination of antibiotics. On day 8 after inoculation with O. tsutsugamushi, the ECV304 cells were washed twice with phosphate-buffered saline (PBS) and IF staining for O. tsutsugamushi was performed. Uninfected cells served as controls.
Table 1.
Percentage of positive immunofluorescent foci in cultures containing each antibiotic combination on day 8 after inoculation of Orientia tsutsugamushi
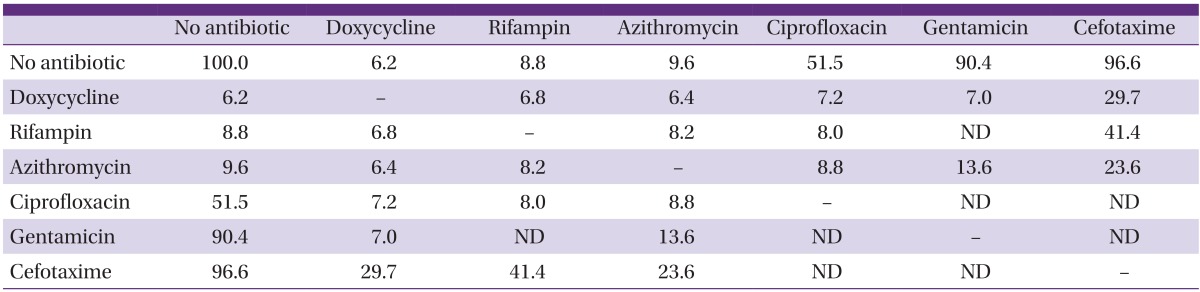
ND, not done.
IF staining was performed as previously described [6], and the number of IF-positive foci per field was counted using the ImageJ program [7]. To account for differences in the inoculation numbers, values are expressed as percentages of inhibition (calculated as the observed values in cultures containing each of the antibiotics divided by the corresponding bacterial numbers in cultures without antibiotic on day 8 after inoculation with O. tsutsugamushi) for each experiment.
The percentages of IF-positive foci in cultures containing each of the antibiotics are shown in Table 1. The combination of 3 antibiotics (doxycycline plus azithromycin plus gentamicin) resulted in a decrease in the percentage of IF-positive foci to 11% of that observed in control. Uninfected ECV304 cells did not show any IF-positive foci.
Although certain combinations of the antibiotics (azithromycin plus rifampin, azithromycin plus ciprofloxacin, and rifampin plus ciprofloxacin) exhibited a slightly smaller number of IF-positive foci than the corresponding single antibiotic, the overall results suggest there is no need to use antibiotic combination therapy for scrub typhus. Furthermore, antibiotic combination therapy for 7 days may not prevent the persistence of O. tsutsugamushi. The results also confirm that ciprofloxacin, even at a 10-fold higher concentration than the expected peak serum concentration, showed only moderate in vitro antimicrobial activity against O. tsutsugamushi. Reports that all tested strains of O. tsutsugamushi have a Ser83Leu mutation in the quinolone resistance-determining region of the gyrA gene support the results of the present in vitro study [8]. Because of their moderate in vitro effect, fluoroquinolones would be expected to have marginal clinical efficacy against scrub typhus. In clinical studies, pefloxacin and ciprofloxacin each showed a 20% failure rate [9], and levofloxacin showed a 9% failure rate [10]. Treatment at the late phase of illness may be a determining factor for this poor outcome [10]. Inconsistent clinical responses noted in case reports or case series employing fluoroquinolones for the treatment of scrub typhus are comparable with those observed in the above-mentioned studies. As suggested in the present study, however, the efficacy of fluoroquinolones may not have been evaluated properly, as many of these cases concomitantly received beta-lactam antibiotics that may be antagonistic to fluoroquinolones. For example, a study reporting that ciprofloxacin had low efficacy included 2 pregnant women who received ceftriaxone or ampicillin among 4 patients receiving ciprofloxacin [11].
There are several situations indicating combination antibiotic therapy for scrub typhus. Co-infection of O. tsutsugamushi with other bacteria is an absolute indication. Co-infection with leptospirosis and scrub typhus is an example of when ceftriaxone and an anti-rickettsial agent should be used in combination. Furthermore, the requirement for combination therapy may be higher with scrub typhus than with non-persistent bacterial infections, because O. tsutsugamushi can be reactivated from a dormant state because of a new infection. In addition, scrub typhus occurrences in tropical or subtropical regions are frequently not accompanied with its characteristic findings such as eschar or rash and cannot be discriminated from enteric fever. Therefore, when patients present with severe manifestations of enteric fever, a combination antibiotic treatment covering both enteric fever and scrub typhus may be employed empirically before identification of the causative agent. Furthermore, spreading of multi-drug resistant typhoid or paratyphoid fever necessitates the use of cefotaxime or ceftriaxone.
Pneumonia is the most common complication of scrub typhus, occasionally accompanied by other bacterial infections. Therefore, severe pneumonia or adult respiratory distress syndrome (ARDS) as a complication of scrub typhus is sometimes managed empirically with combined antibiotics such as beta-lactam antibiotics and either a macrolide or doxycycline, as recommended by the Infectious Diseases Society of America and American Thoracic Society [12]. Cefotaxime, as a beta-lactam antibiotic, is commonly employed because of its safety, broad antimicrobial spectrum, and lack of antagonistic effects with most other antibiotics.
However, in the present study, cefotaxime showed antagonistic effects with respect to all 3 anti-rickettsial agents against O. tsutsugamushi. These effects are not likely to be a result of chemical interactions among these antibiotics because all 3 tested anti-rickettsial antibiotics differ in physical characteristics. Previous in vitro antimicrobial susceptibility tests have revealed that beta-lactam antibiotics have little antimicrobial effect against O. tsutsugamushi. Consequently, these antibiotics have not been used for the treatment of scrub typhus. However, to date, it has not been considered whether cefotaxime adversely influences the antimicrobial effects of anti-rickettsial agents. The concentration of cefotaxime employed in the present study represents a clinically achievable trough concentration. This suggests that its interfering effects may be greater at peak therapeutic levels (80-100 µg/mL).
The number of IF-positive foci in cultures treated with the antibiotic combinations with cefotaxime was fewer than that in the culture treated with ciprofloxacin. Therefore, it is expected that the clinical efficacy of combination therapy with cefotaxime may be superior to that of ciprofloxacin, but inferior to that of doxycycline. In clinical cases, there are reports of good responses when cefotaxime/ceftriaxone is combined with either minocycline or doxycycline [13, 14]; however, there are also cases showing poor responses [14, 15]. For example, one patient with extensive pneumonia (case 5) died 24 hours after hospital admission, following treatment with ceftriaxone and doxycycline, while another patient (case 3) with severe scrub typhus survived after treatment with doxycycline alone [14]. A pregnant woman (case 2) died after receiving cefotaxime and azithromycin [15]. There are also cases reporting a delayed response. A patient with ARDS who received ceftazidime, amoxicillin-clavulanate, and doxycycline displayed a delayed response (48 hours or until administration of a steroid) [16]. These case reports suggest that the efficacy of combinations with cephalosporin antibiotics may be effective in the usual situations, but poor in severe scrub typhus, particularly when complicated by ARDS.
Prior to the present report, with the exception of our previous experiment [5], there have been no reports suggesting that cefotaxime has an antagonist effect. While beta-lactam antibiotics, including cefotaxime, kill bacteria by inhibiting cross-linking of peptidoglycan polymers, it is generally accepted that peptidoglycan is absent in O. tsutsugamushi. Therefore, it might be concluded that cefotaxime has no antagonistic effects on anti-rickettsial agents against O. tsutsugamushi, nor does it have an effect on the organism. However, other modes of action, including induction of holin-like proteins in bacterial membranes [17], may be involved in the antagonistic effects of beta-lactam antibiotics.
Most clinical studies evaluating risk factors for poor outcomes in scrub typhus also do not investigate this factor. One clinical study, which evaluated delayed defervescence in patients with rickettsial infections and treated with doxycycline, revealed that antibiotic combination therapy was more frequently used in the delayed group than in the non-delayed group, though the difference was not statistically significant [18]. In clinical studies evaluating antibiotic efficacies on scrub typhus, all clinical trials have only excluded patients receiving anti-rickettsial antibiotics before enrollment in the trial. Therefore, it is unknown how many of the enrolled patients received cephalosporins concomitantly with anti-rickettsial antibiotics, and the degree to which cephalosporins may have interfered with the efficacy of the antibiotics is unknown.
A report by Watt et al. [19] also only excluded patients receiving anti-rickettsial agents within 2 weeks before enrollment. The authors compared the clinical response to doxycycline in hospitalized patients with scrub typhus in 2 areas of northern Thailand: Chiang Rai, where scrub typhus that was poorly responsive to doxycycline was prevalent and Mae Sod district, where scrub typhus was responding well to doxycycline. Antibiotic susceptibility testing in vitro and in mice strengthened this clinical study; however, antibiotic susceptibility was measured only in strains isolated from patients with a delayed resolution of scrub typhus and not in strains isolated from patients with a rapid response. Instead, the authors used the reference Karp strain as an antibiotic-susceptible strain. If the strains isolated from the rapid responders reveal similar in vitro results, the antibiotic-susceptibility tests may only represent growth characteristics of strains prevailing in Thailand. We previously reported that high in vitro infectivity is responsible for in vitro resistance of the AFSC-4 strain, a doxycycline-insensitive strain isolated in Thailand [6]. As for the delayed clinical response to doxycycline, if clinical practice of antibiotic use differed significantly between the 2 hospitals, the difference in the defervescence times might be attributed to the frequency of cefotaxime use. Another study conducted in Chiang Rai has not reported a delayed clinical improvement [20], which further supports this suggestion.
Taken together, the poor responsiveness of scrub typhus to antibiotics in northern Thailand may not be a matter of antibiotic resistance, but a result of multiple coincidental phenomena. These phenomena include high in vitro infectivity and delayed clinical responses because of the antagonistic effects of cephalosporin antibiotics on doxycycline. Although clinical studies are needed to determine whether the in vitro antagonistic effects observed in the present study correlate with a delayed clinical response, these antibiotic combinations should be used with caution for critically ill patients with scrub typhus. If the superimposed bacteria are susceptible to ciprofloxacin or gentamicin, fluoroquinolone or aminoglycoside antibiotics may be used as an alternative to cefotaxime. In particular, respiratory fluoroquinolones such as levofloxacin or moxifloxacin have an antimicrobial spectrum similar to that of cefotaxime; therefore, these antibiotics can be used in combination with anti-rickettsial antibiotics for empirical treatment of severe pneumonia complicating scrub typhus.
The present experiment was performed only once. When combined with any of the 3 anti-rickettsial antibiotics, cefotaxime showed antagonistic effects; therefore, the in vitro antagonistic effect of combinations with cefotaxime is unequivocal.
Footnotes
No conflicts of interest.
References
- 1.Im JH, Baek JH, Lee JS, Chung MH, Lee SM, Kang JS. In vitro bacteriostatic effects of rifampin on Orientia tsutsugamushi. J Korean Med Sci. 2014;29:183–189. doi: 10.3346/jkms.2014.29.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung MH, Lee JS, Baek JH, Kim M, Kang JS. Persistence of Orientia tsutsugamushi in humans. J Korean Med Sci. 2012;27:231–235. doi: 10.3346/jkms.2012.27.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Im JH, Baek JH, Lee JS, Chung MH, Lee SM, Kang JS. A case series of possibly recrudescent Orientia tsutsugamushi infection presenting as pneumonia. Jpn J Infect Dis. 2014;67:122–126. doi: 10.7883/yoken.67.122. [DOI] [PubMed] [Google Scholar]
- 4.Watt G, Kantipong P, Jongsakul K, Watcharapichat P, Phulsuksombati D, Strickman D. Doxycycline and rifampicin for mild scrub-typhus infections in northern Thailand: a randomised trial. Lancet. 2000;356:1057–1061. doi: 10.1016/S0140-6736(00)02728-8. [DOI] [PubMed] [Google Scholar]
- 5.Kim ES, Kim MK, Lee HM, Chung MH, Lee JS, Kang JS. In vitro efficacy of antibiotic combinations against Orientia tsutsugamushi. Infect Chemother. 2008;40:311–315. [Google Scholar]
- 6.Kim MS, Baek JH, Lee JS, Chung MH, Lee SM, Kang J. High in vitro infectivity of a doxycycline-insensitive strain of Orientia tsutsugamushi. Infect Chemother. 2013;45:431–434. doi: 10.3947/ic.2013.45.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siritantikorn S, Jintaworn S, Noisakran S, Suputtamongkol Y, Paris DH, Blacksell SD. Application of ImageJ program to the enumeration of Orientia tsutsugamushi organisms cultured in vitro. Trans R Soc Trop Med Hyg. 2012;106:632–635. doi: 10.1016/j.trstmh.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang HC, Choi SM, Jang MO, Ahn JH, Kim UJ, Kang SJ, Shin JH, Choy HE, Jung SI, Park KH. Inappropriateness of quinolone in scrub typhus treatment due to gyrA mutation in Orientia tsutsugamushi Boryong strain. J Korean Med Sci. 2013;28:667–671. doi: 10.3346/jkms.2013.28.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oh SY, Chung MH, Oh SJ, Son MS, Ahn SW. An open clinical trial to compare the efficacy of ciprofloxacin, pefloxacin, and doxycycline in the treatment of scrub typhus. Korean J Infect Dis. 1995;27:193–198. [Google Scholar]
- 10.Tsai CC, Lay CJ, Wang CL, Ho YH, Wang LS, Chen LK. Levofloxacin versus tetracycline antibiotics for the treatment of scrub typhus. Int J Infect Dis. 2010;14:e62–e67. doi: 10.1016/j.ijid.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Mathai E, Rolain JM, Verghese L, Mathai M, Jasper P, Verghese G, Raoult D. Case reports: scrub typhus during pregnancy in India. Trans R Soc Trop Med Hyg. 2003;97:570–572. doi: 10.1016/s0035-9203(03)80032-9. [DOI] [PubMed] [Google Scholar]
- 12.Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Jr, Musher DM, Niederman MS, Torres A, Whitney CG Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsumura Y, Shimizu T. Case of imported scrub typhus contracted in Myanmar. Kansenshogaku Zasshi. 2009;83:256–260. doi: 10.11150/kansenshogakuzasshi.83.256. [DOI] [PubMed] [Google Scholar]
- 14.Gupta N, Mittal V, Gurung B, Sherpa U. Pediatric scrub typhus in South Sikkim. Indian Pediatr. 2012;49:322–324. [PubMed] [Google Scholar]
- 15.Mahajan SK, Rolain JM, Kashyap R, Gupta D, Thakur S, Sharma A, Kaushal SS, Raoult D. Scrub typhus complicating pregnancy. J Assoc Physicians India. 2009;57:720–721. [PubMed] [Google Scholar]
- 16.Kurup A, Issac A, Loh JP, Lee TB, Chua R, Bist P, Chao CC, Lewis M, Gubler DJ, Ching WM, Ooi EE, Sukumaran B. Scrub typhus with sepsis and acute respiratory distress syndrome. J Clin Microbiol. 2013;51:2787–2790. doi: 10.1128/JCM.00463-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bayles KW. The bactericidal action of penicillin: new clues to an unsolved mystery. Trends Microbiol. 2000;8:274–278. doi: 10.1016/s0966-842x(00)01762-5. [DOI] [PubMed] [Google Scholar]
- 18.Lai CH, Huang CK, Weng HC, Chung HC, Liang SH, Lin JN, Lin CW, Hsu CY, Lin HH. Clinical characteristics of acute Q fever, scrub typhus, and murine typhus with delayed defervescence despite doxycycline treatment. Am J Trop Med Hyg. 2008;79:441–446. [PubMed] [Google Scholar]
- 19.Watt G, Chouriyagune C, Ruangweerayud R, Watcharapichat P, Phulsuksombati D, Jongsakul K, Teja-Isavadharm P, Bhodhidatta D, Corcoran KD, Dasch GA, Strickman D. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet. 1996;348:86–89. doi: 10.1016/s0140-6736(96)02501-9. [DOI] [PubMed] [Google Scholar]
- 20.Chanta C, Chanta S. Clinical study of 20 children with scrub typhus at Chiang Rai Regional Hospital. J Med Assoc Thai. 2005;88:1867–1872. [PubMed] [Google Scholar]


