Abstract
Background
Hand hygiene compliance has improved significantly through hand hygiene promotion programs that have included poster campaign, monitoring and performance feedback, and education with special attentions to perceived subjective norms. We investigated factors associated with improved hand hygiene compliance, focusing on whether the improvement of hand hygiene compliance is associated with changed perception toward hand hygiene among medical personnel.
Materials and Methods
Hand hygiene compliance and perceptions toward hand hygiene among medical personnel were compared between the second quarter of 2009 (before the start of a hand hygiene promotion program) and the second quarter of 2012. We assessed adherence to hand hygiene among medical personnel quarterly according to the WHO recommended method for direct observation. Also, we used a modified self-report questionnaire to collect perception data.
Results
Hand hygiene compliance among physicians and nurses improved significantly from 19.0% in 2009 to 74.5% in 2012 (P < 0001), and from 52.3% to 91.2% (P < 0.001), respectively. These improvements were observed in all professional status or all medical specialties that were compared between two periods, regardless of the level of the risk for cross-transmission. Hand hygiene compliance among the medical personnel continued to improve, with a slight decline in 2013. Perceptions toward hand hygiene improved significantly between 2009 and 2012. Specifically, improvements were evident in intention to adhere to hand hygiene, knowledge about hand hygiene methods, knowledge about hand hygiene indications including care of a dirty and a clean body site on the same patient, perceived behavioral and subjective norms, positive attitude toward hand hygiene promotion campaign, perception of difficulty in adhering to hand hygiene, and motivation to improve adherence to hand hygiene.
Conclusions
The examined hand hygiene promotion program resulted in improved hand hygiene compliance and perception toward hand hygiene among medical personnel. The improved perception increased hand hygiene compliance. Especially, the perception of being a role model for other colleagues is very important to improve hand hygiene compliance among clinicians.
Keywords: Hand Hygiene, Health personnel, Quality Improvement
Introduction
Hand hygiene is a widely-recognized effective measure to prevent healthcare-associated infections [1, 2]. Hand hygiene promotion programs including the introduction of alcohol-based hand disinfectant produce sustained improvement in compliance with hand hygiene coinciding with a reduction of nosocomial infection and transmission of methicillin-resistant Staphylococcus aureus [3]. Yet, in most hospitals, hand hygiene compliance has remained low among physicians, despite the improvement of a hospital-wide hand hygiene adherence. Interventions are needed that target multiple factors including perceptions toward hand hygiene among doctors [3, 4].
In Hallym University Sacred Heart Hospital, hand hygiene improvement events and education programs have been conducted yearly since the hospital opened in 1999, and alcohol-based hand disinfectants have been available throughout the hospital since 2004. Despite these actions, in the second quarter of 2009, adherence to hand hygiene remained poor among physicians < 40 years of age, and recognition of the importance of hand hygiene among physicians remained poor [5]. Especially, perceptions associated with poor hand hygiene compliance were perceived behavioral norm (i.e., the individual's perception of colleagues' hand hygiene performance) and perceived subjective norm (i.e., the individual's perception of social pressure to perform a hand hygiene) in multivariate logistic regression analysis [5].
Based on these results, a hand hygiene promotion program that included a poster campaign, monitoring and performance feedback and education with special attention to the perception of physicians as a role model of hand hygiene performance for other colleagues was instituted in the third quarter of 2009. Although there were several outside challenges to hand hygiene including the 2009 H1N1 influenza pandemic, the national healthcare accreditation of the hospital in 2011, and the emphasis on hand hygiene in a clinical skill test portion of the national health personnel licensing examination, hand hygiene compliance continued to improve every year.
To minimize the direct influence of outside factors, we investigated hand hygiene adherence and perceptions toward hand hygiene during the second quarter of 2012. These results were compared with those of a survey performed during the second quarter of 2009, immediately prior to the commencement of the hand hygiene campaign. Our study aimed to investigate factors associated with improved hand hygiene compliance, especially whether hand hygiene compliance is associated with change in beliefs and perceptions in medical personnel.
Materials and Methods
1. Setting
Hallym University Sacred Heart Hospital is an 829-bed tertiary care teaching hospital in South Korea. Since 2004, gel or liquid type, alcohol-based hand disinfectant stations have been located throughout the hospital including entrance to patient's rooms, at the end of each sickbed, on nursing and dressing carts, and in the nursing station and the outpatient clinic. Hand-washing facilities equipped with one or two sinks, unmedicated soap, and paper towels are conveniently located in each patient room, nursing station, and the outpatient clinic. Pocket carriage of an alcohol-based hand disinfectant by each healthcare worker was not available.
2. Study design
1) Assessment of hand hygiene compliance
Hand hygiene compliance was investigated every quarter, except between the third quarter of 2009 and the first quarter of 2010, due to the demands of the H1N1 pandemic. As the national healthcare accreditation of hospital was performed in early 2011, data of hand hygiene compliance in the first quarter of 2011 could be exaggerated, and so were excluded. Hand hygiene adherence between April and May 2012 was compared with that between April and May 2009. In 2009, 364 doctors and 530 nurses worked at our hospital, and comprised 166 staff, 154 residents, and 44 interns. In 2012, 390 doctors and 547 nurses worked at the hospital; 180 staff, 169 residents, and 41 interns. Individual medical personnel that routinely cared for patients at each ward were directly observed by two infection control nurses twice a day during a 1-2 week period every quarter. The nurses noted all potential opportunities for hand hygiene and assess adherence to hand hygiene among medical personnel according to the World Health Organization recommended method for direct observation [2]. Interobserver variability was not recorded during monitoring sessions. Each of the medical personnel was observed once during each study period and anonymity was guaranteed. Hand hygiene compliance was evaluated according to professional status, medical specialty, and level of the risk for cross-transmission (Table 1). The risk for cross-transmission was stratified into three categories: high risk (before direct patient contact; between care of a dirty and a clean body site; before intravenous or arterial care; before urinary, respiratory, or wound care); medium risk (after direct patient contact; after intravenous or arterial care; after urinary, respiratory, or wound care; after contact with biological body fluid); and low risk (other conditions, such as after contact with patient surroundings) [4, 6].
Table 1.
Compliance with hand hygiene among medical personnel between 2009 and 2012
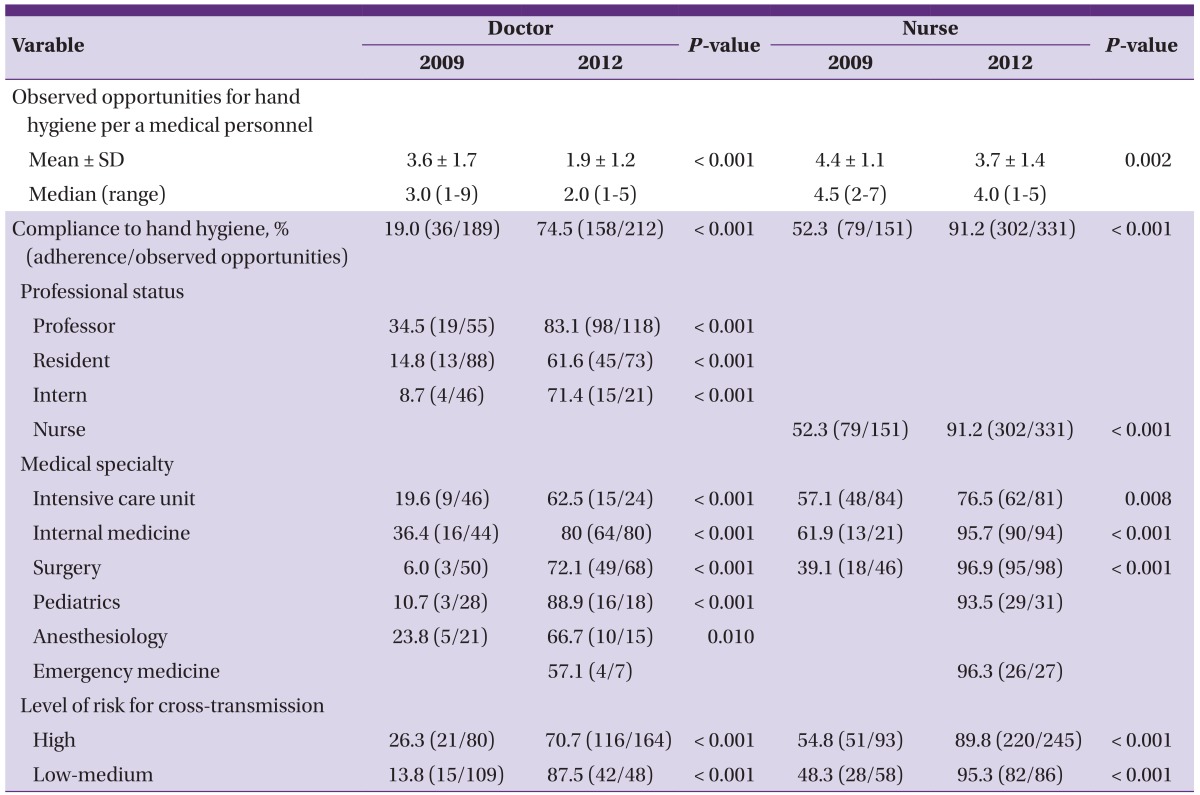
SD, standard deviation.
2) Self-report questionnaire
A self-report questionnaire was used to collect data of perceptions toward hand hygiene. Data between April and May 2012 were compared with data acquired between April and May 2009. After medical personnel were observed, they received the self-report questionnaire directly in hard copy or via electronic-mail. Anonymity was guaranteed. The self-report questionnaire was modified from that used at the University of Geneva Hospital [4]. By using single items for measures and a 7-point scale for answers, the following cognitive factors were assessed: intention to adhere to hand hygiene, perception of knowledge of hand hygiene methods and indications, perception of the risk for cross-transmission linked to non-compliance, perception of social norms concerning hand hygiene (both behavioral and subjective norms), attitude toward hand hygiene promotion campaign, and perception of difficulty in adhering to hand hygiene. The last two points of the scale closest to the positive perceptive evaluation were considered positive answers, with all other points considered negative answers. Motivation to improve hand hygiene was assessed using a three-point scale, with only a "yes" response considered a positive answer (Table 2). In the self-report questionnaire, medical personnel were also asked to respond to whether they were aware of being observed, and whether they perceived their own hand hygiene workload exceeded five opportunities per hour (for details of a modified self-report questionnaire, see the Supplementary Appendix, available with the full text of this article at www.icjournal.org ).
Table 2.
Perceptions associated with hand hygiene adherence among medical personnel between 2009 and 2012
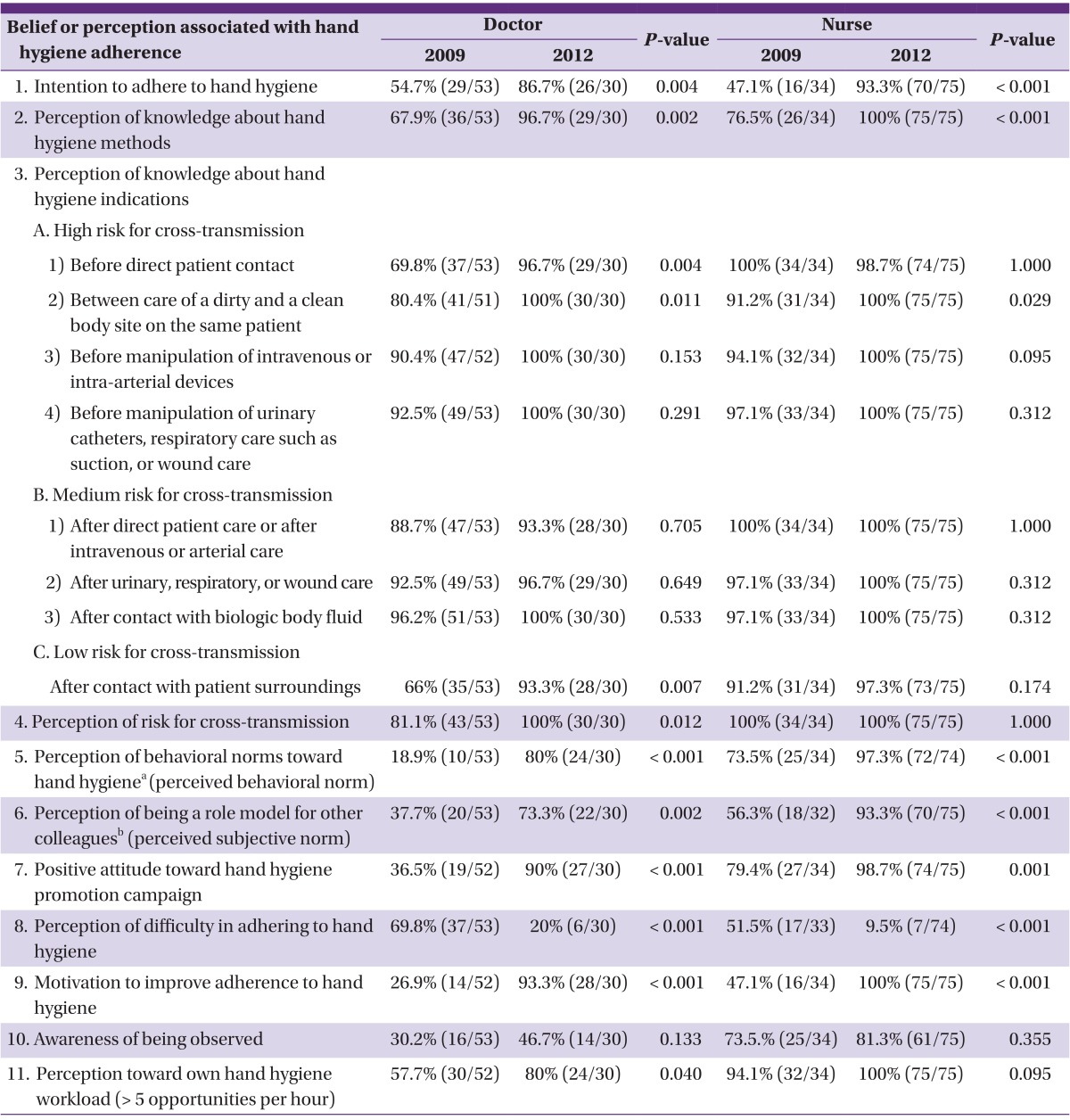
aDefined as the individual's perception of others' behavior ("Do your collegues perform hand hygiene according to the recommended guidelines?").
bDefined as the individual's perception of social pressure to perform a behavior ("Do you think that your behavior toward hand hygiene is taken as an example by your collegues?").
3) Hand hygiene promotion program
Based on the result of the previous survey performed during the second quarter of 2009 [5], the hand hygiene promotion campaign was commenced beginning in the third quarter of 2009. The campaign included a poster campaign, monitoring and performance feedback, and educations with special attentions to importance of perception of being a role model for other colleagues (perceived subjective norm). In 2009, Because only 50% of medical personnel intended to adhere to hand hygiene, and because of large knowledge gap concerning hand hygiene methods and indications and hand hygiene compliance (Tables 1 and 2), the poster campaign was initiated as a visual reminder in the workplace. The color posters were positioned on walls throughout the hospital walls, with emphasis on high traffic areas. The poster emphasized the importance of hand hygiene and provided illustrations of proper hand hygiene. Hospital-wide monitoring and feedback of hand hygiene compliance were performed quarterly. Compliance rates were reported by professional status, medical specialty or hospital wards, and level of the risk for cross-transmission. These results were utilized to educate medical personnel in hand hygiene practice. Education sessions were conducted at least twice a year, according to professional status, medical specialty, or hospital ward. Special attention was given to the perception of being a role model of hand hygiene for other colleagues (perceived subjective norm). Education emphasized the importance of the perceived subjective norm, in which infectious diseases specialists visited directly the conferences of individual clinical department where present during the session. Many of the attributes associated with being an excellent attending-physician role model are related to skills that can be acquired and to modifiable behavior [7]. Therefore, we emphasized that hand hygiene is an easy skill to learn and correct, and urged senior doctors to become a role model of hand hygiene for junior doctors.
3. Statistical analyses
Hand hygiene adherence and hand hygiene associated factors including perceptions were compared between 2009 and 2012. Differences in proportions were compared only by Chi-square test or Fisher's exact test, because the observed medical personnel differed between the two periods. Continuous variables were compared by t-test or Wilcoxon-Mann-Whitney test. All tests were two-tailed, and a P-value < 0.05 was defined as statistically significant. Analysis was performed in IBM SPSS Statistics 21 Standard for Medical Service Network.
Results
1. Hand hygiene compliance
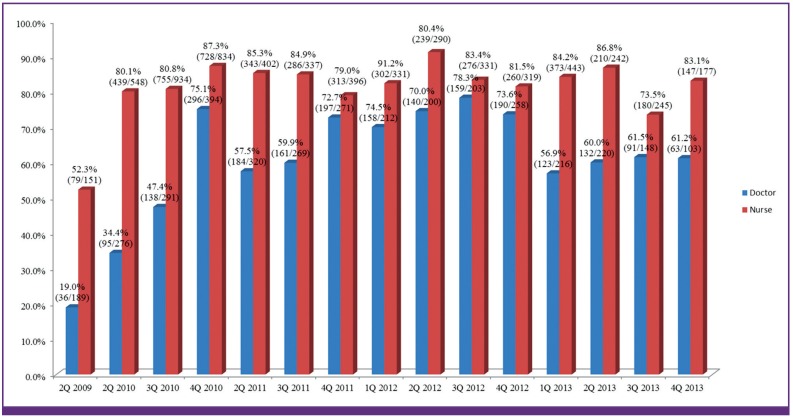
Fifty-three doctors and 34 nurses were observed in 2009, and 110 doctors and 90 nurses were observed in 2012. The number of opportunities for evaluation of hand hygiene compliance among doctors increased from 189 to 212, and those among nurses also increased from 151 to 331 between the two years. However, the mean number of opportunities for each medical personnel decreased from 3.6 in 2009 to 1.9 in 2012 among doctors, and from 4.4 in 2009 to 3.7 in 2012 among nurses (Table 1). According to professional status, medical specialty, and level of the risk for cross-transmission, hand hygiene compliance rates were compared between the two periods (Table 1). Hand hygiene compliance among doctors improved significantly from 19.0% in 2009 to 74.5% in 2012 (P < 0.001). Compliance among nurses improved from 52.3% in 2009 to 91.2% in 2012 (P <0.001). Markedly improved adherence was noted in all professional physician categories including professors, residents, and interns. In all medical specialties of doctors and nurses compare between 2009 and 2012 hand hygiene compliance increased significantly. Also, regardless of the level of risk for cross-transmission, compliance improved significantly among doctors and nurses. Hand hygiene compliance rates among doctors increased gradually from the second quarter of 2009, although a slight decline was evident in 2013 (Fig. 1).
Figure 1.
Five-year trend of hand hygiene compliance among medical personnel before and after the start of hand hygiene promotion campaign, 2009-2013. Hand hygiene compliance, % (adherence to hand hygiene/opportunities observed for hand hygiene).
2. Perceptions of hand hygiene
All 53 doctors responded to the self-report questionnaire in the second quarter of 2009, but only 30 of 110 doctors (27.3%) responded in the second quarter of 2012. All 34 nurses responded in 2009, and 75 of 90 nurses (83.3%) responded in 2012. Perceptions that improved greatly in doctors and nurses included the following: intention to adhere to hand hygiene, perception of knowledge about hand hygiene methods, perception of knowledge about hand hygiene indications (e.g., between care of a dirty and a clean body site on the same patient), positive perception of behavioral norms toward hand hygiene, perception of being a role model for other colleagues, positive attitude toward hand hygiene promotion campaign, motivation to improve adherence to hand hygiene, and perception of difficulty in adhering to hand hygiene (Table 2). In addition, knowledge about hand hygiene indications, such as before direct patient contact or after contact with patient surroundings, and perception of risk for cross-transmission of microorganisms resulting from non-adherence, also improved significantly among doctors (Table 2). Although awareness of being observed increased both in doctors and nurses, it was not significant statistically. Even if both doctors and nurses responded that their own hand hygiene workload was higher in 2012, hand hygiene compliance did not decrease accordingly (Table 2).
Discussion
In our institution, implementation of a hand hygiene promotion program including a poster campaign, monitoring and performance feedback, and education with special attention to the perception of being a role model for other colleagues resulted in improvement of hand hygiene compliance and perceptions toward hand hygiene among medical personnel.
In Korea, no study has addressed the perceptions toward hand hygiene among doctors as a risk factor of poor hand hygiene compliance [8, 9]. In a prior study, we documented perceptions associated with poor hand hygiene compliance as perceived behavioral norm (the individual's perception of colleagues' hand hygiene performance) and perceived subjective norm (the individual's perception of social pressure to perform a hand hygiene) in multivariate logistic regression analysis [5]. We have emphasized a senior doctors' role model for junior doctors in hand hygiene practice [7, 10]. Presently, on the back of the emphasis on the belief of being a role model for other colleagues concerning hand hygiene, the perceived subjective and behavioral norms improved significantly following the hand hygiene promotion program. These changes could result in an increased intention to adhere to hand hygiene, perception of ease in the adherence, and motivation to improve adherence to hand hygiene. Therefore, we judged that the perceptional change drove the improvement of hand hygiene adherence, although this was not evaluated directly.
Our study has several limitations. First, the number of opportunities to observe hand hygiene in each subject in the second quarter of 2012 was less than in the second quarter of 2009 (3.6 to 1.9 per doctor, P < 0.001; 4.4 to 3.7 per nurse, P = 0.002), although the total of number of observed opportunities to hand hygiene in medical personnel was larger in 2012 (189 to 212 in doctors; 151 to 331 in nurses). The decrease of the number of opportunities to observe hand hygiene could have artifactually increased the rates of hand hygiene compliance in doctors and nurses. Especially among doctors, the perception that their own hand hygiene workload exceeded five per hour increased from 57.7% to 80% between 2009 and 2012 (P = 0.040). The number of opportunities to observed hand hygiene of doctors could have been small for the doctors' hand hygiene workload. Second, the number of opportunities to observe hand hygiene for interns and personnel in intensive care units among doctors, which are known risk factors of poor hand hygiene compliance [2], was smaller in the second quarter of 2012, while observation of hand hygiene indications of high risk for cross-transmission was significantly increased in the second quarter of 2012. If the number of opportunities to observe hand hygiene for interns and in intensive care units among doctors was much more than in the second quarter of 2012, the actual hand hygiene compliance could be lower than that observed among doctors. Third, interobserver variability can affect reported hand hygiene compliance rates [3, 4, 11]. We did not evaluate interobserver agreement for the reported hand hygiene compliance, although two infection control nurses investigated hand hygiene compliance in every quarter since 2007, and the infection control nurses did not change between two periods. Fourth, awareness of being observed increased from 30.2% to 46.7% among doctors, and from 73.5% to 81.3% among nurses between the two periods. Although hand hygiene compliance could be improved due to the Hawthorne effect, the change in awareness of being observed was not statistically significant, and was much smaller than that of hand hygiene compliance. Fifth, only 27.3% of doctors who were observed for hand hygiene adherence in the second quarter of 2012 responded to a self-report questionnaire. Because doctors with high compliance rates responded to a questionnaire, a selection bias that perceptions associated with hand hygiene were mistaken to be improved could occur. Sixth, the improvement of hand hygiene compliance could not be directly correlated with that of perceptions associated with hand hygiene. The same medical personnel could not be selected to investigate adherence and perception of hand hygiene between two periods. Therefore, we could only compare proportion of adherence and perception of hand hygiene between two periods. Seventh, hand hygiene compliance continued to improve from 2009 to 2012, but decreased somewhat in 2013. If tools for hand hygiene improvement, such as the World Health Organization (WHO) hand hygiene self-assessment framework can be utilized for future systematic assessment of hand hygiene, the goal of hand hygiene compliance more than 80% to 90% could be sustained in our hospital [12].
In conclusion, a hand hygiene promotion program that included a poster campaign, monitoring and performance feedback, and education resulted in improvement of hand hygiene compliance and perceptions toward hand hygiene among medical personnel in a hospital in Korea. The improvement of perceptions associated with hand hygiene affected hand hygiene compliance. Especially, the perception of being a role model for other colleagues was important to improve hand hygiene compliance among doctors.
References
- 1.Boyce JM, Pittet D Healthcare Infection Control Practices Advisory Committee; Society for Healthcare Epidemiology of America; Association for Professionals in Infection Control; Infectious Diseases Society of America; Hand Hygiene Task Force. Guideline for Hand Hygiene in Health-Care Settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Infect Control Hosp Epidemiol. 2002;23(12 Suppl):S3–S40. doi: 10.1086/503164. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) WHO Guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care. [Accessed 18 December 2013]. Available at: http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf. [PubMed]
- 3.Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, Perneger TV. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 4.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. doi: 10.7326/0003-4819-141-1-200407060-00008. [DOI] [PubMed] [Google Scholar]
- 5.Lee SS, Park SJ, Lee JH. Analysis of factors associated with poor hand hygiene adherence among doctors and nurses in a Korean hospital. Infect Chemother. 2009;41(Suppl 2):S176. [Google Scholar]
- 6.Hugonnet S, Perneger TV, Pittet D. Alcohol-based handrub improves compliance with hand hygiene in intensive care units. Arch Intern Med. 2002;162:1037–1043. doi: 10.1001/archinte.162.9.1037. [DOI] [PubMed] [Google Scholar]
- 7.Wright SM, Kern DE, Kolodner K, Howard DM, Brancati FL. Attributes of excellent attending-physician role models. N Engl J Med. 1998;339:1986–1993. doi: 10.1056/NEJM199812313392706. [DOI] [PubMed] [Google Scholar]
- 8.Kweon OM, Park E, Lee D, Lee JH, Ha EJ, Yong D, Choi JY, Kim KH, Lee C, Lee K. A three-year study of the effectiveness of hand-hygiene protocol implementation at a university hospital. Korean J Nosocomial Infect Control. 2012;17:53–60. [Google Scholar]
- 9.Kim YC, Kim MH, Song JE, Ahn JY, Oh DH, Kweon OM, Lee D, Kim SB, Kim HW, Jeong SJ, Ku NS, Han SH, Park ES, Yong D, Song YG, Lee K, Kim JM, Choi JY. Trend of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia in an institution with a high rate of MRSA after the reinforcement of antibiotic stewardship and hand hygiene. Am J Infect Control. 2013;41:e39–e43. doi: 10.1016/j.ajic.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 10.Lankford MG, Zembower TR, Trick WE, Hacek DM, Noskin GA, Peterson LR. Influence of role models and hospital design on hand hygiene of healthcare workers. Emerg Infect Dis. 2003;9:217–223. doi: 10.3201/eid0902.020249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pittet D, Mourouga P, Perneger TV. Compliance with handwashing in a teaching hospital. Infection Control Program. Ann Intern Med. 1999;130:126–130. doi: 10.7326/0003-4819-130-2-199901190-00006. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) Hand hygiene self-assessment framework 2010. [Accessed 18 December 2013]. Available at: http://www.who.int/gpsc/country_work/hhsa_framework_October_2010.pdf.