Abstract
The aim of this review is to provide a comprehensive update on the biology, epidemiology, clinical features, diagnosis, treatment, and prevention of canine cardio-pulmonary angiostrongylosis. This cardiopulmonary disease is caused by infection by the metastrongyloid nematode Angiostrongylus vasorum. The parasite has an indirect life cycle that involves at least two different hosts, gastropod molluscs (intermediate host) and canids (definitive host). A. vasorum represents a common and serious problem for dogs in areas of endemicity, and because of the expansion of its geographical boundaries to many areas where it was absent or uncommon; its global burden is escalating. A. vasorum infection in dogs can result in serious disorders with potentially fatal consequences. Diagnosis in the live patient depends on faecal analysis, PCR or blood testing for parasite antigens or anti-parasite antibodies. Identification of parasites in fluids and tissues is rarely possible except post mortem, while diagnostic imaging and clinical examinations do not lead to a definitive diagnosis. Treatment normally requires the administration of anthelmintic drugs, and sometimes supportive therapy for complications resulting from infection.
Table of contents
Introduction
Historical perspective
- Biology
-
3.1.Life-cycle of A. vasorum
-
3.2.Morphological characteristics
-
3.3.Host-specificity
-
3.1.
- Epidemiology
-
4.1.Pattern of spread
-
4.2.Risk factors and at risk-populations
-
4.3.Role of wildlife reservoirs
-
4.1.
- Disease clinical features
-
5.1.Pulmonary
-
5.2.Coagulopathy
-
5.3.Cardiovascular
-
5.4.Nervous
-
5.1.
- Diagnosis of angiostrongylosis
-
6.1.Laboratory diagnosis
-
6.1.1.Pathological findings
-
6.1.2.General laboratory findings
-
6.1.3.Parasitological findings
-
6.1.1.
-
6.2.Immuno-diagnosis
-
6.2.1.Antigen-based assays
-
6.2.2.Antibody-based assays
-
6.2.1.
-
6.3.Molecular techniques
-
6.4.Problems in diagnosing angiostrongylosis
-
6.1.
Treatment
Control and prevention
Conclusions
Competing interests
Authors’ contributions
Acknowledgements
References
1. Introduction
As a disease with a substantial animal health impact, canine angiostrongylosis remains a high priority for clinicians and researchers. Infected dogs usually exhibit signs of respiratory and/or cardiovascular disease, and occasionally coagulopathies and neurological signs, with fatal consequences in severe cases [1,2]. This disease is caused by the metastrongyloid nematode Angiostrongylus vasorum (Baillet, 1866) Kamensky, 1905 (Nematoda: Metastrongylidae). Even though A. vasorum was discovered over a century ago in France [3] knowledge of its epidemiology and clinical importance has grown in the last 20 years. In this time, infection has dramatically increased in significance and apparent incidence, and the parasite has expanded from established “hotspots” into previously uninfected areas. Popular theories include climatic change, increased urbanisation of the red fox (Vulpes vulpes) which acts as a reservoir host [4,5] and increased movement of domestic dogs both within and between countries [6]. However, the spread of the parasite is likely due to a combination of these and possibly other factors, and this makes infection with A. vasorum unpredictable.
Extremely valuable clinical observations have been obtained in previous studies [7-11], including studies examining moderate numbers of animals, e.g. 160 cases [1] and 54 cases [12], which document trends in the signalment of presenting animals. However, more studies with larger sample sizes in a range of settings are needed in order to draw robust conclusions. The use of signalment trends is valuable to veterinary practitioners, as it allows improved education of dog owners and perhaps facilitates faster diagnosis. Useful information includes identification of at-risk breeds, or breed groups, as well as some knowledge regarding the degree of influence that the sex or age of an animal has upon likelihood of infection. Likewise, knowledge of the way in which A. vasorum affects physical parameters, haematological and biochemical parameters assists practitioners in compiling a list of differential diagnoses. When a diagnosis of A. vasorum has been established it is useful for practitioners to have additional information regarding the most effective treatment strategies.
Over the last few decades A. vasorum has not escaped the interest of veterinary clinicians and parasitologists. This is reflected in the variety and growing number of scientific publications, which continue to advance the knowledge on this parasite and the disease it causes. Hence, we here review the seminal literature and summarise the latest advances in the epidemiology, clinical, and laboratory diagnostics of A. vasorum infection, and discuss current treatment and prevention strategies. Additionally, the historical perspective, biology, morphological characteristics and host specificity are discussed.
2. Historical perspective
The name A. vasorum was derived from the Greek words “angion” meaning bottle, “strongylos” meaning round, and “vasorum” meaning blood vessels. The pseudonym “French Heartworm”, by which A. vasorum is commonly known, was given based on the first locality from which the parasite was recognized. When studying historical accounts relating to the distribution of A. vasorum in Toulouse, France in the 1800s to various countries throughout Europe, Africa and the Americas to date, the nematode appears to have spread at an alarming rate and to a wide geographical expanse. Thus, from its initial recognition in France, A. vasorum has been described in bordering countries within Northern Europe, whereby infection appeared to establish within well-defined endemic foci. There were also reports of A. vasorum infection within canid populations outside of Europe, more specifically in South America, Newfoundland in North America, and Uganda [1,13]. For many years, very few cases of infection were documented outside of these “hotspots”. More recent studies have begun to highlight an apparent change in the range of A. vasorum, reporting instances of infection from new localities a considerable distance from the previously recognised foci [1,14,15].
3. Biology
3.1. Life-cycle of A. vasorum
The dioecious adult A. vasorum lives in the pulmonary arteries and heart of the definitive hosts, i.e. dogs and other canids, and produces eggs that hatch to first-stage larvae (L1). These penetrate the alveoli, migrate up to the oropharynx, after which they are swallowed and then eliminated in the faeces. A definitive host can shed as many as 280 000 larvae per gram of faeces [16]. These L1 must infect a gastropod mollusc intermediate host (slug or snail), for the development of the infective third-stage larvae (L3), which occurs within 10-16 days under optimum conditions [1,14,17]. Until now virtually all investigated snails and slugs have proven to be able to function as intermediate host to this parasite. Frogs act as paratenic hosts, following the ingestion of infected snails or slugs, and can also act as intermediate hosts [18]. L3 of A. vasorum are able to infect the dog (Canis familiaris) either directly, through ingestion of L3 present in the environment, or indirectly, through ingestion of an intermediate gastropod or paratenic (transport) host. Then, L3 penetrate the gut wall and migrate to the abdominal lymph nodes, where they moult to fourth-stage larvae (L4); then enter the portal circulation, migrate through the liver parenchyma and eventually reach the right ventricle and pulmonary arteries, where they mature to adults. The time from which a definitive host is infected to when larvae can be recovered from faeces, otherwise known as the pre-patent period, is reported to be 38–57 days; however, it can range widely from 28 to 108 days [19].
To date, no work has been done to determine whether infection status affects longevity of molluscs experimentally infected with A. vasorum. The survival of A. vasorum larvae was found to be greater at lower temperatures, with larvae remaining active until day 15 and alive until day 24 at 5°C, while high temperatures can induce higher mortality [20]. A seasonal pattern to infection by A. vasorum has been detected in dogs in Denmark [10]. A study carried out by Morgan et al., [4] approximated an eco-climatic index to predict the success of A. vasorum establishment and growth in different climatic locations. The index correlated a high eco-climatic index with areas known to have high A. vasorum infection, thus highlighting a potential use to anticipate infection in currently non-endemic areas.
3.2. Morphological characteristics
The basic morphological appearance of A. vasorum is like that of most nematodes, taking a cylindrical form that tapers at each end. Members of the superfamily Metastrongyloidea, to which A. vasorum belongs, are all known to feature a small buccal capsule, rather than just a simple oral aperture. Distinguishing features that allow specific identification of A. vasorum can be split into gross and microscopic categories and characterized by sex and larval stage. Males are 14-18 mm in length, with visible bursa, spicules and bursal rays, their ventral rays are fused for the majority of their body and the dorsal ray is short with short terminal branches. Females are slightly larger, 18-25 mm in length, and have a gross appearance similar to the “barber’s pole” appearance of Haemonchus sp. The white ovaries of female A. vasorum are wrapped in a coil around the intestine with the vulva located in the posterior region of the body (Figures 1 and 2). The undifferentiated eggs that hatch from the oviparous female develop into L1 larvae (Figure 3) that are 280 to 330 μm in length, have an anterior cephalic button, a dorsal spine and a sinus wave curve in their tail [17,21]. Knowledge of L1 morphology is essential for diagnosis using Baermann’s technique.
Figure 1.
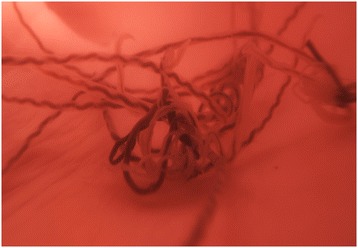
Mimicking of adult Angiostrongylus vasorum in situ using reconstructive filming. Note the characteristic barber’s pole appearance of female worms in a still image taken from a filmed sequence of adult live worms, which were collected from naturally infected dogs and placed in a pig’s heart through which fluid was pumped.
Figure 2.

SEM photograph of adult Angiostrongylus vasorum . (A) Caudal region, (B) anterior region, (C) a higher magnification of the anterior end showing the oral orifice. Scale bars; A & B = 1 mm; C = 10 μm.
Figure 3.

Angiostrongylus vasorum first-stage larva recovered from faeces using the Baermann technique. Note the characteristic kinked tail of the larva with a sinusoidal curve and a spine and distinct notch on the dorsal surface.
3.3. Host-specificity
It is now recognised that A. vasorum infection is commonly seen in wild canids, such as red foxes [22], which act as reservoir hosts, and can also infect the wolf (Canis lupus), coyote (Canis latrans), and jackal (Canis aureus), as well as other wild canid species [23-25]. A correlation between the prevalence of A. vasorum infection in foxes and in dogs has been suggested. This connection has led to studies exploring other potential reservoirs of infection that may threaten the dog population. New potential definitive hosts, such as the Eurasian badger (Meles meles) were identified [26,27]. Also, natural A. vasorum infection has been reported in captive red panda (Ailurus fulgens) in the United Kingdom and Denmark [28,29] and in free living otters in Denmark [30].
4. Epidemiology
A. vasorum is recognised as having a worldwide distribution. But, when focussing on the enzootic prevalence of A. vasorum globally there are limited data from which to draw conclusions. No national or international surveillance mechanisms are in place to determine the prevalence and global distribution of A. vasorum infection. The geographic distribution of A. vasorum in the Americas and Africa is less defined than in Europe, thus preventing the assumption of global “trends” in infection. Nonetheless, canine angiostrongylosis is considered endemic in certain areas of Europe, including regions of Denmark, Germany, Hungary, Finland, France, Ireland, Italy, the Netherlands, Poland, Slovakia, Spain, Sweden, Switzerland, Turkey and the United Kingdom, in Canada (Newfoundland), in South America (Brazil and Colombia), and in Uganda in Africa. The country list is growing as the A. vasorum geographic distribution continues to evolve in several countries of Europe [31], and there is a growing risk of establishment in the Americas [32]. Studies carried out within dog populations in the United Kingdom, Denmark, Germany and Greece estimate the prevalence of A. vasorum to range from 0.3-9.8%. Estimated prevalence varies widely between different canine populations (e.g. pet, hunting or stray dogs), health status (e.g. clinically affected or healthy), and methods used (e.g. variations on coprological methods). This is in contrast to studies within fox populations in Canada, Denmark, Hungary, Italy, and Spain, which estimate prevalence of A. vasorum to be often higher at 5-56% [1]. These data suggest that foxes are the most important reservoir of infection, but must be interpreted with care, as figures exclude the recently recognised shifts in prevalence both within and outside of regions of endemic foci [6].
4.1. Pattern of spread
Information on the exact geographic range of A. vasorum in dogs is lacking due to apparent expansion both around known endemic foci and into previously free regions. Attention should be drawn to the fact that the lack of evidence of A. vasorum in a given region does not ensure its non-existence, and therefore, geographic location should not be used as the sole criterion to suspect or rule out diagnosis. Likewise, increasing awareness of the parasite among clinicians and parasitologists has driven surveillance and recognition of infection in an expanding area, some of which might have been pre-existing. However, this is unlikely to fully explain apparent range expansion, given that such a highly pathogenic disease would not lie unrecognised for so long in countries with a well-developed veterinary clinical sector. A caveat worth mentioning here is that this disease may go unnoticed unless clinicians are looking for it or test for it since making a clinical diagnosis can be difficult because of varying magnitudes of severity and a variable and sometimes vague presentation.
In Europe, A. vasorum is known to be spreading into previously un-infected areas in Denmark, Germany, Greece, the Netherlands, Ireland, Italy, Sweden and the United Kingdom [6,10,11,33–36]. In the British Isles, A. vasorum infection was first reported in a Greyhound in Ireland in 1968 [37] and 7 years later a single infection was reported in England in a Greyhound that had been imported from Ireland [38]. Following this, the infection has rapidly spread to establish regions of endemic foci in the South-West, as well as the South-East of England and Wales. Furthermore, subsequent studies have identified new pockets of A. vasorum infection in both dog and fox populations reaching the North of England [39], Scotland [40] and Ireland [41]. This pattern of expansion appears to be repeated at a range of scales, and in some cases the disease is appearing in different countries, for example, A. vasorum infection has been reported for the first time in a native dog in Slovakia in 2013, [42], the latest in a long series of new national records in Europe.
In North America, the situation is different to that seen in South America and Europe. Until recently, Newfoundland in Canada was regarded as the only A. vasorum endemic location in North America [9]. However, an autochthonous infection has been recently identified in the lungs of a red fox from West Virginia, USA [15]. Two cases of natural A. vasorum infection had been previously reported in domestic dogs in the USA; one at Michigan State University in 1985, in a Greyhound imported from Ireland [43] and the other in an abandoned dog in Long Island, based on the tentative identification of A. vasorum in the faeces [44].
It is difficult to say why A. vasorum has spread in the manner that it has, and why it is moving to different locations. Three of the more commonly proposed hypotheses are climate change, urbanisation of red fox populations and increased pet movements. Other equally plausible explanations include the increasing awareness of A. vasorum within the veterinary profession and continually improving, more readily available diagnostics. A recent report, analysing the genetic sequence in nematodes recovered from Europe and South America, questioned previous assumptions about the worldwide spread of A. vasorum from France. It is likely that A. vasorum in Europe and South America occurred as a result of evolutionary divergence along with canid radiation (Figure 4), rather than recent historical spread [13,45].
Figure 4.

Phylogenetic relationships among three species of Angiostrongylus . Neighbor joining analysis was conducted on the concatenated sequences of COI and ITS-2 using the Kimura two-parameter model of nucleotide substitution. Bootstrap values based on 500 replications are given at the internal nodes. Taxa are labeled with the species, strain designation, and country of origin for each isolate.
4.2. Risk factors and at risk-populations
Published data in the United Kingdom suggest that some purebred dogs are at higher risk than crossbreeds, and in particular Cavalier King Charles Spaniels and Staffordshire Bull Terriers [8] and beagles [9]. Reports of breed predisposition might reflect popular breeds in the locations assessed. However, data from Canada suggest a higher prevalence in hunting dog breeds [9,32], and data from The Netherlands, Germany, Denmark and Italy do not report breed preferences [10,11,34]. The most likely age for infection has been reported as around 10 months [7,8]. There are no data to suggest that age, sex or body condition influence A. vasorum infection in foxes [5].
4.3. Role of wildlife reservoirs
Besides the natural definitive host (domestic dog), A. vasorum has been reported from a wide range of wild canids in several geographic areas (reviewed in [1,14]). The lack of genetic separation between A. vasorum obtained from dogs, foxes and coyotes supports the hypothesis that transmission can occur between wild and domestic canids [13]. Indeed, infection in dogs seems to occur due to geographic over-lap with wild canid hosts [14].
The most important and best-studied wildlife reservoir for A. vasorum infection is the red fox (Vulpes vulpes). A possible explanation for increased transmission of infection between red fox and dog populations is an increasing density of foxes. It can be assumed that an increased density of foxes in an area populated with dogs is likely to increase the number of fox-dog interactions, and hence increase the opportunity for transmission of infection. Direct wild canid-dog interaction is not necessary for (and does not lead to) transmission of this parasite from one to the other because transmission occurs via ingestion of L3 (in gastropods or frogs, or possibly free in the environment). An unrelated disease outbreak could decrease the overall health of foxes, and hence increase susceptibility to A. vasorum infection. This could have been the case in the United Kingdom, where A. vasorum infection appeared simultaneously with an outbreak of sarcoptic mange [14], although this outbreak was also associated with a marked decrease in fox population density, which should have reduced A. vasorum infection pressure.
Studies in the United Kingdom have demonstrated a prevalence of 23.2% A. vasorum infection in fox populations residing in a known endemic hotspot for dog infection, compared to a countrywide prevalence of 7.3% [5]. Interestingly, we identified one case of A. vasorum in red fox in the Midlands of England (Figure 5), which may explain the recently identified cases of canine infection in that locality [4,46]. This finding would correspond with the situation in Canada, whereby A. vasorum infection was first identified in red foxes in Newfoundland in 1973, where the parasite is still endemic [47], before it emerged in domestic dogs in 1996 and then in coyotes in 2003 [25,48–50]. A. vasorum was recently identified in foxes in Scotland [51] where a single case of A. vasorum had been identified in a dog that had never travelled [40].
Figure 5.
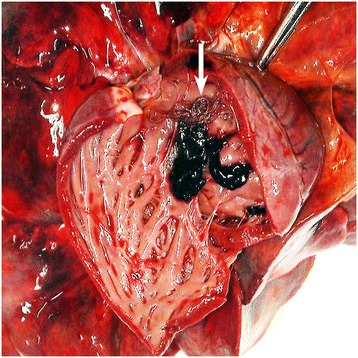
Photograph showing Angiostrongylus vasorum in situ. Adult male and female A. vasorum (arrow) in the heart of a red fox from the East Midlands region, England.
While A. vasorum is commonly found in and known to cause pathology in red foxes [5,52], only two cases have been described in wolves, first in northwestern Spain [23] and recently in Rome, Italy [24], again coinciding with increasing records of A. vasorum in dogs and foxes in the same geographic region, where infection with the parasite is also expanding in dogs [31,36]. Eurasian badgers, Meles meles (Linnaeus, 1758) have been identified as potential reservoirs for infection, however their role in transmission to dogs remains uncertain [26]. Much remains to be understood about the dynamics of infection in wild populations and factors underlying spill-over to dogs.
5. Disease clinical features
Infection with A. vasorum may be asymptomatic in some cases or may result in a wide spectrum of clinical signs, ranging from mild respiratory manifestations to severe forms [1], which are characterized by coagulative, respiratory or neurological disorders [53]. Respiratory signs are the most common clinical manifestations, with coagulation disorders being less common but more likely to be fatal. Ocular signs, including intraocular larval migration, while rare, have been reported [54].
5.1. Pulmonary
By far the most common clinical presentations in dogs diagnosed with A. vasorum are pulmonary related. The most significant of these are coughs (either productive or unproductive), and dyspnoea, with or without tachypnoea. Related clinical signs that are less commonly reported are intolerance to exercise and lethargy. It is expected that a dog positive for infection with A. vasorum would show some pulmonary changes upon lateral or ventrodorsal radiography (Figure 6). General findings include increased interstitial, peribronchial and alveolar patterns, pneumothorax [16,55,56], subcutaneous emphysema and an abnormally wide cranial mediastinum. The most common signs noted upon radiographic analysis are an alveolar infiltrate and bronchial thickening. Characteristic serpiginous/circular areas of radiopacities have been detected in asymptomatic dogs, which were attributed to fistulas developed during migration of larvae from the pulmonary capillaries into the alveoli [57]. There is some evidence as to the time following infection that clinicians should expect to see radiographic changes. It has been suggested that five to seven weeks after infection a bronchial-interstitial pattern can be observed, which will be most obvious at nine weeks post infection, and decrease up until approximately twenty one weeks when evidence of fibrosis will be seen [7]. Correlation between time and radiographic pattern can be followed in experimentally infected dogs [58] using computer tomography. It is evident that there are always fibrotic tissues left, showing that after A.vasorum infection the lesions cannot fully regress.
Figure 6.

Radiographic feature of Angiostrongylus vasorum . Latero-lateral thoracic radiograph of an 18 month old English Setter, before treatment for Angiostrongylus vasorum. Diagnosis was confirmed by faecal analysis. Note the marked bronchial-alveolar pattern (arrows).
5.2. Coagulopathy
A less common but often more severe consequence of infection is a varying degree of coagulopathy [14]. Despite recent interest in this aspect of infection there is actually very little evidence based knowledge of how or why coagulopathy occurs. Coagulopathy when present can be wide ranging with some animals presenting with clinical or clinico-pathological signs more suggestive of primary (e.g. Disseminated Intravascular Coagulation (DIC) [59], immune-mediated thrombocytopenia [60,61]), secondary and tertiary coagulopathy (dysregulation of the anticoagulation pathway [59,62]) or combinations of the three. Abnormalities attributed directly to coagulopathies include haematoma, anaemia, intracranial haemorrhage, sub-conjunctival haemorrhage, melaena and increased post traumatic bleeding tendencies.
5.3. Cardiovascular
Cardiovascular abnormalities associated with infection include; attenuated cardiac sounds, myocarditis, heart murmurs of grade II to VI, heart failure, periarteritis, pale mucous membranes and haematoma (causing pulmonary hypertension or right heart failure secondary to obstruction) [8,60]. Pulmonary hypertension occurs in less than 5% dogs infected with A. vasorum in primary practice but affects up to one third of infected dogs presenting at referral practice, documented by echocardiography [1]. Echocardiology of dogs positive for A. vasorum has indicated dilation of the right ventricle and atrium, a bulging interatrial septum, dilated vena cava and hepatic veins, and a severe tricuspid incompetence [63,64]. Some abnormalities identified upon cardiac radiography include right ventricular enlargement, truncated pulmonary arteries and an increase in vertebral heart scale. Cardiac abnormalities are relatively rare and therefore not that commonly diagnosed, in some cases Doppler ultrasound is used as a supplementary method [7,63].
5.4. Nervous
Neurological clinical presentation of A. vasorum infection is less frequent than cardio-vascular and pulmonary, but is still of clinical importance. Most neurological signs arise from bleeding in or around the central nervous system, secondary to coagulopathies. Neurological deficits or abnormalities will reflect the area of CNS haemorrhage and prompt clinicians to consider testing for A. vasorum in young animals with acute onset central neurological signs before embarking on expensive and potentially risky CNS imaging whether they present with or without respiratory signs. Neurological defects associated with A. vasorum infection are difficult to diagnose using conventional radiographs; instead MRI and CT imaging can be used. Studies using these techniques have noted accumulation of fluid on the spinal cord, intramedullary haemorrhage and intraparenchymal haemorrhage in infected dogs [60,61,65,66]. Although nervous signs may be due to the disseminated spread of L1 no reported cases to date reflect neurological signs secondary to ectopic parasite or hypoxia as has been previously speculated [1,8,57,65,67].
6. Diagnosis of angiostrongylosis
6.1. Laboratory diagnosis
6.1.1. Pathological findings
Post mortem reports in dogs and foxes infected with A. vasorum show evidence of a thickened right ventricle, with pneumonia and breakdown in alveolar structure [5,68]. Histopathological analysis typically reveals the presence of inflammatory cells, in particular neutrophils, and granulomatous foci with multinucleated giant cells, a pattern also seen in less usual definitive hosts such as the wolf [24] and coyote [25]. These observations are attributed to the inflammatory response to eggs and migrating larvae [1]. A number of studies have shown the presence of immature and adult nematodes in ectopic locations, for example in the eye [54,66,69], where they can provide a highly suggestive ante mortem diagnosis.
6.1.2. General laboratory findings
Various haematological and biochemical abnormalities have been noted in infected dogs, including increased ß-globulin fraction, anaemia, eosinophilia, thrombocytopenia, hypercalcaemia and low serum fructosamine. However, these vary between cases, with no typical or pathognomonic profile evident [2,70,71]. While peripheral eosinophilia is not a consistent finding in dogs with angiostrongylosis, if present in an animal with appropriate clinical findings it should prompt investigation for the parasite. Coagulation parameters are also inconsistent, even in cases with clinical coagulopathies [8,59]. Thromboelastography is a useful technique, both in terms of giving additional information about the kind of coagulopathy, and also in follow-up assessment.
6.1.3. Parasitological findings
The most common method for diagnosing A. vasorum infection is the Baermann migration-sedimentation technique, in which larvae are recovered from faeces and identified based on morphological features. Larvae have a characteristic sinusoidal terminal appendage that is quite unlike other parasitic and non-parasitic nematodes commonly found in dog faeces [72]. However, the fact that larvae cannot be found in the faeces during the pre-patent period, and the limited sensitivity of the test on a single faecal examination, are important limitations of the test [73]. This has led to modifications attempting to improve the diagnostic value of faecal larval analysis [74]. Sensitivity can be improved by pooling faeces over a three day period [1], but this and the fact that the Baermann test can take up to 24 hours to yield results, makes it onerous in clinical practice. Early examination of the Baermann’s test leads to more rapid results but at the cost of sensitivity, while direct smear examination of faeces is a simple test to perform at the pet-side but with a low sensitivity of up to 54-61% [6,75]. L1 may be detected in faecal flotation preparations, but do not float reliably in standard flotation solutions, and so are unlikely to be found in routine screening tests for parasite ova. FLOTAC, an improved flotation-based coprological method for visualising parasite eggs, oocysts and larvae in faecal samples, has been found to be more sensitive than the Baermann method for detecting A. vasorum L1 when used with higher specific gravity solutions [76]. Bronchoalveolar lavage (BAL), in which fluid is injected into and then recovered from the lungs and analysed for the presence of larvae, can be useful to demonstrate infection [77], but is difficult and not without risk, especially in dyspnoeic patients. It is worth mentioning, however, that evidence for the utility of BAL in the diagnosis of angiostrongylosis [77] was based on experimental findings and, hence might not accurately reflect performance in clinical cases.
6.2. Immuno-diagnosis
6.2.1. Antigen-based assays
Detection of circulating parasite antigen was identified as a promising diagnostic approach [73], and an antigen blood test is now commercially available in the form of an in-hospital lateral flow device (AngioDetect®, Idexx Laboratories, USA). The test can be performed on plasma or serum with results obtained in 15 minutes. Antigen detection by Enzyme-linked immunosorbent assay (ELISA) has a high specificity (94%) and sensitivity (95%), much higher than faecal examination [78]. As such, this is likely to be increasingly relevant to clinical diagnosis in practice, as well as monitoring of parasite distribution and spread [79]. Baermann can still be a reliable method for diagnosis of A. vasorum, if performed appropriately.
Antigen is reported to be detectable around five weeks after experimental infection, hence during the pre-patent period, and to persist until after elimination of the parasite, while cross-reactions with other common canine parasites were not found [78]. Commercial antigen-detection kits for Dirofilaria immitis, on the other hand, were tested with sera from dogs infected with A. vasorum, and some cross-reactions were detected [80]. Given the emergence of A. vasorum in areas endemic for D. immitis [15], this is of some concern. It is also worth mentioning that initiation of adequate treatment has been shown to decrease the level of detected circulatory antigens. No circulating antigen was observed in dogs treated with imidacloprid/moxidectin at 4 or 32 day post infection (dpi), while in dogs treated at 88-92 dpi, circulatory antigens decreased within 13-34 days [78]. Antigen detection could therefore be useful as an indicator of response to treatment.
6.2.2. Antibody-based assays
Detection of specific antibodies against A. vasorum also hold potential for clinical diagnosis [81]. However, a study using Western Blot and ELISA serology of 14 dogs experimentally infected with A. vasorum, successfully identified only five animals over a period of 0-56 dpi [82]. Other attempts to identify antibodies, based on crudely extracted parasite antigens, suffered from lack of specificity [83]. Further work has been carried out to identify specific proteins produced by both L1 and adult nematodes, that are recognised by antibodies, in order to improve the sensitivity of such tests [84,85]. A novel antibody-detection ELISA, based on monoclonal antibodies to A. vasorum, succeeded in achieving high sensitivity and specificity [80], and has been applied alongside antigen-detection in serological surveys [46,79]. In theory, persistence of antibodies in dogs historically infected could lead to false positives when using antibody detection as a clinical diagnostic tool, especially in areas with high background levels of exposure. Hence, antibody testing alone is of limited value except as a means of screening for exposure in presumably non-endemic regions. The options for combining antigen and antibody detection ELISA in clinical and epidemiological settings are discussed in Schnyder et al. [46]. There may also be some potential for combining an antibody detection ELISA with the Baermann technique to increase the latter’s sensitivity but retaining the early detection benefits of the former.
6.3. Molecular techniques
Polymerase chain reaction (PCR) has been used to successfully recognise unique nucleic acid sequences of A. vasorum [40]. Real-time PCR was developed for A. vasorum in definitive and intermediate hosts, and shown to be capable of detecting DNA circulating in canine blood [81,85]. Although highly specific and requiring a blood sample rather than faeces, real-time blood PCR offered no great advantage over the Baermann test in terms of sensitivity in naturally infected dogs [85]. PCR has also been used to detect A. vasorum in the faeces of dogs [83] and foxes [86]. However, PCR inhibitors in faeces can limit sensitivity and there is no obvious advantage over the Baermann test unless faeces are to be stored for long periods prior to examination, such that L1 die and are unable to migrate in the Baermann apparatus. PCR can also be useful in cases where faecal Baermann is not suggestive of a diagnosis of L1 of A. vasorum because they are morphologically altered or less motile than usual. However, the effect of treatment (e.g. fenbendazole) on the size or motility of the larvae prior to faecal screening remains unknown or poorly understood. PCR may be also useful in instances where a clinician is faced with a case that clinically resembles A. vasorum (i.e. respiratory signs with either clinical or clinico-pathological evidence of bleeding diathesis) but faecal analysis is not supportive.
6.4. Problems in diagnosing angiostrongylosis
Clinicians are faced with many diagnostic challenges when it comes to definitively identifying A. vasorum infection in a patient. In this regard several points are worth mentioning. Firstly, due to the recent erratic and somewhat unexplained spread of infection, from the classified ‘hotspots’ to previously uninfected areas, it is no longer possible to reliably determine whether an animal is at a high or low risk of infection according to its location. Secondly, it is possible that a clinician may overlook clinical signs suggestive of A. vasorum infection, and treat for a condition with a similar presentation such as kennel cough, because of a belief that A. vasorum is not present in the area. Thirdly, it is widely accepted that tests such as Baermann faecal examination do not always recognise the presence of A. vasorum in an animal, especially in pre-patent infection or as a result of low larval loads, intermittent larval shedding, poor sample quality or operator error. Finally, the low performance of faecal tests in terms of sensitivity and immediacy has led many clinicians to treat presumptively for angiostrongylosis in suspicious cases, rather than pursue a definitive parasitological diagnosis. This has the disadvantage of removing an important source of evidence to the clinician on local level of risk, as well as monitoring of treatment success. Blind treatment, without attempts to make a diagnosis, in cases of high suspicion should be discouraged for this reason and because the required duration of treatment is dependent on the animal not continuing to shed L1. Wider availability of pet-side antigen-detection tests is likely to provide important clinical and epidemiological information in the future, on which decisions on treatment and prevention regimes can be based.
7. Treatment
A. vasorum is susceptible to a variety of anthelmintics. Historically levamisole and ivermectin were routinely used but this has not been the case in the past decade. This is in part due the risk of anaphylaxis with levamisole use [87], the risk of toxicosis with ivermectin use in any breed with an MDR 1 mutation (e.g., collie breeds), and, most importantly, safer and licensed products becoming available. Fenbendazole remains a popular treatment of choice and is efficacious at 25-50 mg/kg for 5-21 days [1,12,88], but in many territories is not licensed as a treatment for A. vasorum. The reasoning behind fenbendazole use is that it produces a “slow kill” and therefore reduces the risk of anaphylaxis but there remains no peer reviewed data to support this theory. There are currently only two widely licensed parasite treatments that include A. vasorum among their label claims. One is a moxidectin/imidacloprid spot-on solution (Advocate®, Bayer Animal Health) and the other a milbemycin oxime tablet, in combination with praziquantel (Milbemax®, Novartis Animal Health). Moxidectin has been shown to be effective in removing adult A. vasorum and immature stages (L4 and L5) and milbemycin in reducing levels of adult and immature adult (L5) infection [12,89]. Moxidectin requires a single monthly spot-on application to eliminate infection. Milbemycin requires weekly oral administration for 4 weeks to treat clinical A. vasorum infection. Both are highly efficacious treatments. The study comparing the efficacy of moxidectin/imidacloprid to fenbendazole [12] as a treatment option actively excluded severe cases of angiostrongylosis and therefore little is known about this drug’s performance in severe cases. Milbemycin was also recently shown to have 98.8% preventative efficacy against development of adult A. vasorum infection in a combination product with spinosad (Trifexis®, Elanco Animal Health) but at the time of writing this combination is not yet licensed for A. vasorum treatment and prophylaxis [90]. Licensed claims often differ between territories and change with time, and readers are advised to check on the current situation in their locality before making recommendations on treatment. Supportive treatment is often indicated, depending on the clinical presentation. Anti-inflammatory doses of steroids have been used to moderate potential anaphylaxis and/or treat significant respiratory signs [54]. Oxygen administration is also indicated in the respiratory compromised patient. Patients with coagulopathies have received lifesaving treatment with coagulation factors delivered in fresh frozen plasma or whole blood, although cases with coagulopathies may recover also with treatment of the parasite alone [63]. Where congestive heart failure is present as a result of infection then treatment with diuretics, ACE inhibitors and phosphodiesterase inhibitors (e.g., pimobendan or sildenafil) for pulmonary hypertension, are indicated.
8. Control and prevention
Eradication of A. vasorum is impractical in any given area since significant reservoirs of infection will almost certainly be present in the wild fox and intermediate host populations. Measures should be considered to avoid dogs consuming L3 (third stage larvae) either directly or in gastropod molluscs. These include feeding dogs indoors, cleaning outdoor bowls and toys frequently (or making them less accessible to slugs/snails) to reduce the risk of contamination with L3.
While molluscicides can be employed to reduce slug and snail abundance, many of these are not pet safe and to prevent access of pet dogs to molluscs completely is unrealistic. Infected molluscs killed by pesticides in gardens might be more available to dogs and actually increase risk of infection. Correct disposal of dog faeces, while being desirable for control of parasites such as Toxocara canis, is unlikely to make a significant impact on environmental contamination with L1 as current data suggest that domestic dogs are a much smaller reservoir of infection when compared to foxes; nevertheless, treatment of dogs and faecal removal might enhance local protection, for example if environmental contamination is predominantly from dogs in one locale, or in public areas highly frequented by dogs. An interesting recent study has experimentally explored the use of nematophagous fungi in the environmental control of A. vasorum, by demonstrating an efficacious destruction of L1 [91], but currently anthelmintic prophylactic treatment remains the mainstay of disease prevention. Education is essential to raise public awareness as canine angiostrongylosis continues to be seen with increasing frequency in regions where it was not traditionally thought to be endemic and it should be considered an emerging disease of which veterinarians should be aware. Moxidectin and milbemycin oxime can be used effectively for A. vasorum prophylaxis if used monthly [89,90]. So far, no report has been published on resistance of A. vasorum to chemotherapeutic compounds and large intermediate host and wildlife reservoirs are expected to buffer against resistance. However, long term excessive treatment may potentially favour the development of anthelmintic resistance and as a result the need for monthly prophylaxis should be based on risk factors such as whether the patient is known to come into frequent contact with slugs or snails or has had previous exposure to the parasite. Prophylactic treatment should be initiated in all dogs having suffered from A. vasorum infection as it would imply that the area is endemic and the dog is coming into contact with the intermediate host. Alternatively, dogs may be regularly checked for the presence of A. vasorum, something that is easier with the availability of the new diagnostic tests described above.
9. Conclusions
On any ranked list of cardiopulmonary nematode parasites of veterinary importance, A. vasorum would have to lie towards the top. In recent years the threat of A. vasorum to companion animal populations has become increasingly apparent. This parasite has considerable impact on dogs’ health and has shown both regional endemicity and geographic expansion. Going from its original discovery in France in the 1800s [3], to the recent cutting-edge elucidation of the A. vasorum proteome [92], mitochondrial genome [93] and transcriptome [94] considerable insights into understanding of the contribution of virulence determinants to the pathophysiological aspects of canine angiostrongylosis have been gained. However, important gaps remain in the available literature surrounding the epidemiology of infection. It would be useful to establish why infection is so prevalent in hotspots around the world and the factors that cause infection to spread. The role of red foxes and other wild canids in the transmission cycles of A. vasorum is not adequately understood. Also, the prevalence and geographic distribution of A. vasorum among wild canids, as well as how A. vasorum was introduced to new localities (e.g. the USA) warrant further epidemiological investigation. Attention should be drawn to the fact that the lack of evidence of A. vasorum in a given region does not guarantee its nonexistence. Thus, location should not be used as the sole criterion to suspect or rule out diagnosis. While intense investigations in multiple directions have been conducted to elucidate the mechanisms conducive to the development of coagulopathies, no consensus has yet emerged. Knowledge of this may help to reduce the number of fatal cases observed. Better control of A. vasorum will have implications for the health of domestic dogs. Development of a safe and efficacious canine vaccine for the prophylaxis of angiostrongylosis disease could, if feasible, be a significant tool in future prevention programmes.
12. Acknowledgements
Figure 6 is reprinted with kind permission of Kingfisher Veterinary Practice, England. Figures 1 and 3 and graphic abstract image are courtesy of Bayer Animal Health. We apologize to the authors of articles we could not include in this review due to space limitations.
Footnotes
10. Competing interests
The authors declare that they have no competing interests.
11. Authors’ contributions
HME designed the review. SH reviewed the literature and prepared the initial draft of the manuscript. DWL performed phylogenetic analyses. HME, IW, ERM revised and substantially updated the manuscript. All authors read and approved the final version of the manuscript.
Contributor Information
Hany M Elsheikha, Email: hany.elsheikha@nottingham.ac.uk.
Sarah A Holmes, Email: holmsie80@hotmail.com.
Ian Wright, Email: hammondia@hotmail.com.
Eric R Morgan, Email: eric.morgan@bristol.ac.uk.
David W Lacher, Email: David.Lacher@fda.hhs.gov.
13. References
- 1.Koch J, Willesen JL. Canine pulmonary angiostrongylosis: an update. Vet J. 2009;179:348–359. doi: 10.1016/j.tvjl.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 2.Schnyder M, Fahrion A, Riond B, Ossent P, Webster P, Kranjc A, Glaus T, Deplazes P. Clinical, laboratory and pathological findings in dogs experimentally infected with Angiostrongylus vasorum. Parasitol Res. 2010;107:1471–1480. doi: 10.1007/s00436-010-2021-9. [DOI] [PubMed] [Google Scholar]
- 3.Serres E. Entozoaires trouvés dans l’oreille droite, le ventricule correspondant et l’artère pulmonaire d’un chien. J Vet Midi. 1854;7:70. [Google Scholar]
- 4.Morgan ER, Jefferies R, Krajewski M, Ward P, Shaw SE. Canine pulmonary angiostrongylosis: the influence of climate on parasite distribution. Parasitol Int. 2009;58:406–410. doi: 10.1016/j.parint.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Morgan ER, Tomlinson A, Hunter S, Nichols T, Roberts E, Fox MT, Taylor MA. Angiostrongylus vasorum and Eucoleus aerophilus in foxes (Vulpes vulpes) in Great Britain. Vet Parasitol. 2008;154:48–57. doi: 10.1016/j.vetpar.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 6.Morgan ER, Shaw S. Angiostrongylus vasorum infection in dogs: continuing spread and developments in diagnosis and treatment. J Small Anim Pract. 2010;51:616–621. doi: 10.1111/j.1748-5827.2010.01000.x. [DOI] [PubMed] [Google Scholar]
- 7.Boag AK, Lamb CR, Chapman PS, Boswood A. Radiographic findings in 16 dogs infected with Angiostrongylus vasorum. Vet Rec. 2004;154:426–430. doi: 10.1136/vr.154.14.426. [DOI] [PubMed] [Google Scholar]
- 8.Chapman PS, Boag AK, Guitian J, Boswood A. Angiostrongylus vasorum infection in 23 dogs (1999–2002) J Small Anim Pract. 2004;45:435–440. doi: 10.1111/j.1748-5827.2004.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 9.Conboy G. Natural infections of Crenosoma vulpis and Angiostrongylus vasorum in dogs in Atlantic Canada and their treatment with milbemycin oxime. Vet Rec. 2004;155:16–18. doi: 10.1136/vr.155.1.16. [DOI] [PubMed] [Google Scholar]
- 10.Taubert A, Pantchev N, Vrhovec MG, Bauer C, Hermosilla C. Lungworm infections (Angiostrongylus vasorum, Crenosoma vulpis, Aelurostrongylus abstrusus) in dogs and cats in Germany and Denmark in 2003-2007. Vet Parasitol. 2009;159:175–180. doi: 10.1016/j.vetpar.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Van Doorn DCK, Van de Sande AH, Nijsse ER, Eysker M, Ploeger HW. Autochthonous Angiostrongylus vasorum infection in dogs in The Netherlands. Vet Parasitol. 2009;162:163–166. doi: 10.1016/j.vetpar.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 12.Willesen JL, Kristensen AT, Jensen AL, Heine J, Koch J. Efficacy and safety of imidacloprid/moxidectin spot-on solution and fenbendazole in the treatment of dogs naturally infected with Angiostrongylus vasorum (Baillet, 1866) Vet Parasitol. 2007;147:258–264. doi: 10.1016/j.vetpar.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Jefferies R, Shaw SE, Viney ME, Morgan ER. Angiostrongylus vasorum from South America and Europe represent distinct lineages. Parasitology. 2009;136:107–115. doi: 10.1017/S0031182008005258. [DOI] [PubMed] [Google Scholar]
- 14.Morgan ER, Shaw SE, Brennan SF, De Waal TD, Jones BR, Mulcahy G. Angiostrongylus vasorum: a real heartbreaker. Trends Parasitol. 2005;21:49–51. doi: 10.1016/j.pt.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Kistler WM, Brown JD, Allison AB, Nemeth NM, Yabsley MJ. First report of Angiostrongylus vasorum and Hepatozoon from a red fox (Vulpes vulpes) from West Virginia, U. S. A. Vet Parasitol. 2014;200:216–220. doi: 10.1016/j.vetpar.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Martin MWS, Ashton G, Simpson VR, Neal C. Angiostrongylosis in Cornwall: clinical presentations of eight cases. J Small Anim Pract. 1993;34:20–25. doi: 10.1111/j.1748-5827.1993.tb02570.x. [DOI] [Google Scholar]
- 17.Guilhon J. Recherches sur le cycle évolutif du strongle des vaisseaux du chien. Bull Acad Vet. 1963;36:431–442. [Google Scholar]
- 18.Bolt G, Monrad J, Frandsen F, Henriksen P, Dietz HH. The common frog (Rana temporaria) as a potential paratenic and intermediate host for Angiostrongylus vasorum. Parasitol Res. 1993;79:428–430. doi: 10.1007/BF00931834. [DOI] [PubMed] [Google Scholar]
- 19.Bolt G, Monrad J, Koch J, Jensen AL. Canine angiostrongylosis: a review. Vet Rec. 1994;135:447–452. doi: 10.1136/vr.135.19.447. [DOI] [PubMed] [Google Scholar]
- 20.Dias SR, Dos Santos Lima W. Effect of temperature on activity of third-stage larvae of Angiostrongylus vasorum. Parasitol Res. 2012;110:1327–1330. doi: 10.1007/s00436-011-2624-9. [DOI] [PubMed] [Google Scholar]
- 21.Taylor MA, Coop RL, Wall RL. Veterinary Parasitology. West Sussex: Wiley-Blackwell; 2007. [Google Scholar]
- 22.Sreter T, Szell Z, Marucci G, Pozio E, Varga I. Extraintestinal nematode infections of red foxes (Vulpes vulpes) in Hungary. Vet Parasitol. 2003;115:329–334. doi: 10.1016/S0304-4017(03)00217-6. [DOI] [PubMed] [Google Scholar]
- 23.Segovia JM, Torres J, Miquel J, Llaneza L, Feliu C. Helminths in the wolf, Canis lupus, from north-western Spain. J Helminthol. 2001;75:183–192. [PubMed] [Google Scholar]
- 24.Eleni C, De Liberato C, Azam D, Morgan ER, Traversa D. Angiostrongylus vasorum in wolves in Italy. Int J Parasitol Parasites Wildl. 2014;3:12–14. doi: 10.1016/j.ijppaw.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bourque A, Whitney H, Conboy G. Angiostrongylus vasorum Infection in a Coyote (Canis latrans) from Newfoundland and Labrador, Canada. J Wildl Dis. 2005;41:816–819. doi: 10.7589/0090-3558-41.4.816. [DOI] [PubMed] [Google Scholar]
- 26.Millán J, Sevilla I, Gerrikagoitia X, García-Pérez AL, Barral M. Helminth parasites of the Eurasian badger (Meles meles L.) in the Basque Country (Spain) Eur J Wildl Res. 2004;50:37–40. doi: 10.1007/s10344-003-0032-x. [DOI] [Google Scholar]
- 27.Torres J, Miquel J, Motjé M. Helminth parasites of the eurasian badger (Meles meles L.) in Spain: a biogeographic approach. Parasitol Res. 2001;87:259–263. doi: 10.1007/s004360000316. [DOI] [PubMed] [Google Scholar]
- 28.Bertelsen MF, Meyland-Smith F, Willesen JL, Jefferies R, Morgan ER, Monrad J. Diversity and prevalence of metastrongyloid nematodes infecting the red panda (Ailurus fulgens) in European zoos. Vet Parasitol. 2010;172:299–304. doi: 10.1016/j.vetpar.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 29.Patterson-Kane JC, Gibbons LM, Jefferies R, Morgan ER, Wenzlow N, Redrobe SP. Pneumonia from Angiostrongylus vasorum infection in a red panda (Ailurus fulgens fulgens) J Vet Diagn Invest. 2009;21:270–273. doi: 10.1177/104063870902100219. [DOI] [PubMed] [Google Scholar]
- 30.Madsen AB, Dietz HH, Henriksen P, Clausen B. Survey of Danish free living Otters Lutra lutra - a consecutive collection and necroscopy of dead bodies. IUCN Otter Spec Group Bull. 1999;16:65–76. [Google Scholar]
- 31.Traversa D, Di Cesare A, Conboy G. Canine and feline cardiopulmonary parasitic nematodes in Europe: emerging and underestimated. Parasit Vectors. 2010;6:62. doi: 10.1186/1756-3305-3-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conboy GA. Canine angiostrongylosis: the French heartworm: an emerging threat in North America. Vet Parasitol. 2011;6:382–389. doi: 10.1016/j.vetpar.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 33.Papazahariadou M, Founta A, Papadopoulos E, Chliounakis S, Antoniadou-Sotiriadou K, Theodorides Y. Gastrointestinal parasites of shepherd and hunting dogs in the Serres Prefecture, Northern Greece. Vet Parasitol. 2007;148:170–173. doi: 10.1016/j.vetpar.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 34.Traversa D, Torbidone A, Malatesta D, Guglielmini C. Occurrence of fatal canine Angiostrongylus vasorum infection in Italy. Vet Parasitol. 2008;152:162–166. doi: 10.1016/j.vetpar.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Barutzki D, Schaper R. Results of parasitological examinations of faecal samples from cats and dogs in Germany between 2003 and 2010. Parasitol Res. 2011;109(Suppl 1):S45–S60. doi: 10.1007/s00436-011-2402-8. [DOI] [PubMed] [Google Scholar]
- 36.Traversa D, Di Cesare A, Meloni S, Frangipane di Regalbono A, Milillo P, Pampurini F, Venco L. Canine angiostrongylosis in Italy: occurrence of Angiostrongylus vasorum in dogs with compatible clinical pictures. Parasitol Res. 2013;112:2473–2480. doi: 10.1007/s00436-013-3412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roche MM, Kelliher DJ. Angiostrongylus vasorum infestation in the dog: a case report. Irish Vet J. 1968;22:108–113. [Google Scholar]
- 38.Jacobs DE, Prole JH. Angiostrongylus vasorum and other nematodes in British greyhounds. Vet Rec. 1975;96:180. doi: 10.1136/vr.96.8.180. [DOI] [PubMed] [Google Scholar]
- 39.Yamakawa Y, McGarry JW, Denk D, Dukes-McEwan J, Macdonald N, Mas A, McConnell F, Tatton B, Valentine EG, Wayne J, Williams JM, Hetzel U. Emerging canine angiostrongylosis in northern England: five fatal cases. Vet Rec. 2009;164:149–152. doi: 10.1136/vr.164.5.149. [DOI] [PubMed] [Google Scholar]
- 40.Helm J, Gilleard JS, Jackson M, Redman E, Bell R. A case of canine Angiostrongylus vasorum in Scotland confirmed by PCR and sequence analysis. J Small Anim Pract. 2009;50:255–259. doi: 10.1111/j.1748-5827.2009.00741.x. [DOI] [PubMed] [Google Scholar]
- 41.Brennan SF, McCarthy G, McAllister H, Bassett H, Jones BR. Clinical signs, diagnosis and treatment of three dogs with angiostrongylosis in Ireland. Irish Vet J. 2004;57:103–109. doi: 10.1186/2046-0481-57-2-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hurníková Z, Miterpáková M, Mandelík R. First autochthonous case of canine Angiostrongylus vasorum in Slovakia. Parasitol Res. 2013;112:3505–3508. doi: 10.1007/s00436-013-3532-y. [DOI] [PubMed] [Google Scholar]
- 43.Williams JF, Lindemann B, Padgett GA, Smith OL. Angiostrongylosis in a greyhound. J Am Vet Med Assoc. 1985;186:1101–1103. [PubMed] [Google Scholar]
- 44.Georgi JR, Georgi ME. Canine Clinical Parasitology. Philadelphia, USA: Lea & Febiger; 1992. pp. 186–188. [Google Scholar]
- 45.Morgan ER, Claire EL, Jefferies R, Stevens JR. Parasite epidemiology in a changing world: can molecular phylogeography help us tell the wood from the trees? Parasitology. 2012;14:1924–1938. doi: 10.1017/S0031182012001060. [DOI] [PubMed] [Google Scholar]
- 46.Schnyder M, Schaper R, Bilbrough G, Morgan ER, Deplazes P. Seroepidemiological survey for canine angiostrongylosis in dogs from Germany and the UK using combined detection of Angiostrongylus vasorum antigen and specific antibodies. Parasitology. 2013;140:1442–1450. doi: 10.1017/S0031182013001091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith FR, Threlfall W. Helminths from some mammals from Newfoundland. Am Midld Nat. 1973;90:215–218. doi: 10.2307/2424284. [DOI] [Google Scholar]
- 48.Bourque A, Conboy G, Miller L, Whitney H, Ralhan S. Angiostrongylus vasorum infection in 2 dogs from Newfoundland. Can Vet J. 2002;43:876–879. [PMC free article] [PubMed] [Google Scholar]
- 49.Jeffery RA, Lankester MW, Mcgrath MJ, Whitney HG. Angiostrongylus vasorum and Crenosoma vulpis in red foxes (Vulpes vulpes) in Newfoundland, Canada. Can J Zool. 2004;82:66–74. doi: 10.1139/z03-211. [DOI] [Google Scholar]
- 50.Bridger KE, Baggs EM, Finney-Crawley J. Endoparasites of the coyote (Canis latrans), a recent migrant to insular Newfoundland. J Wildl Dis. 2009;45:1221–1226. doi: 10.7589/0090-3558-45.4.1221. [DOI] [PubMed] [Google Scholar]
- 51.Philbey AW. Detection of Angiostrongylus vasorum in red foxes in Scotland. Vet Rec. 2013;173:148. doi: 10.1136/vr.f4948. [DOI] [PubMed] [Google Scholar]
- 52.Gerrikagoitia X, Barral M, Juste RA. Angiostrongylus species in wild carnivores in the Iberian peninsula. Vet Parasitol. 2010;174:175–180. doi: 10.1016/j.vetpar.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 53.Helm JR, Morgan ER, Jackson MW, Wotton P, Bell R. Canine angiostrongylosis: an emerging disease in Europe. J Vet Emerg Crit Care (San Antonio) 2010;20:98–109. doi: 10.1111/j.1476-4431.2009.00494.x. [DOI] [PubMed] [Google Scholar]
- 54.Manning SP. Ocular examination in the diagnosis of angiostrongylosis in dogs. Vet Rec. 2007;160:625–627. doi: 10.1136/vr.160.18.625. [DOI] [PubMed] [Google Scholar]
- 55.Gallagher B, Brennan SF, Zarelli M, Mooney CT. Geographical, clinical, clinicopathological and radiographic features of canine angiostrongylosis in Irish dogs: a retrospective study. Ir Vet J. 2012;65:5. doi: 10.1186/2046-0481-65-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spodsberg EH, Miles JE, McEvoy FJ, Willesen JL. Spontaneous pneumothorax secondary to granulomatous pneumonia caused by Angiostrongylus vasorum in a dog in Denmark. J Small Anim Pract. 2013;54:114. doi: 10.1111/jsap.12023. [DOI] [PubMed] [Google Scholar]
- 57.Capogna A, Sasanelli M, Lia RP, Spagnolo PP, Paradies P. Further insights into the clinical aspects of Angiostrongylus vasorum natural infection in symptomatic and asymptomatic dogs. J Vet Sci Med Diagn. 2012;1:2. doi: 10.4172/2325-9590.1000106. [DOI] [Google Scholar]
- 58.Kranjc A, Schnyder M, Dennler M, Fahrion A, Maa M, Ossent P, Morgan J, Deplazes P, Glaus TM. Pulmonary artery thrombosis in experimental Angiostrongylus vasorum infection does not result in pulmonary hypertension and echocardiographic right ventricular changes. J Vet Intern Med. 2010;24:855–862. doi: 10.1111/j.1939-1676.2010.0529.x. [DOI] [PubMed] [Google Scholar]
- 59.Cury MC, Lima WS, Guimaraes MP, Carvalho MG. Haematological and coagulation profiles in dogs experimentally infected with Angiostrongylus vasorum (Baillet, 1866) Vet Parasitol. 2002;104:139–149. doi: 10.1016/S0304-4017(01)00616-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gould SM, McInnes EL. Immune-mediated thrombocytopenia associated with Angiostrongylus vasorum infection in a dog. J Small Anim Pract. 1999;40:227–232. doi: 10.1111/j.1748-5827.1999.tb03068.x. [DOI] [PubMed] [Google Scholar]
- 61.O’Neill E, Acke E, Tobin E, McCarthy G. Immune-mediated thrombocytopenia associated with Angiostrongylus vasorum infection in a Jack Russell terrier. Ir Vet J. 2010;63:434–440. doi: 10.1186/2046-0481-63-7-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Whitley NT, Corzo-Menendez N, Carmichael NG, McGarry JW. Cerebral and conjunctival haemorrhages associated with von Willebrand factor deficiency and canine angiostrongylosis. J Small Anim Pract. 2005;46:75–78. doi: 10.1111/j.1748-5827.2005.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 63.Estèves I, Tessier D, Dandrieux J, Polack B, Carlos C, Boulanger V, Muller C, Pouchelon JL, Chetboul V. Reversible pulmonary hypertension presenting simultaneously with an atrial septal defect and angiostrongylosis in a dog. J Small Anim Pract. 2004;45:206–209. doi: 10.1111/j.1748-5827.2004.tb00226.x. [DOI] [PubMed] [Google Scholar]
- 64.Sasanelli M, Paradies P, Otranto D, Lia RP, De Caprariis D. Haemothorax associated with Angiostrongylus vasorum infection in a dog. J Small Anim Pract. 2008;49:417–420. doi: 10.1111/j.1748-5827.2008.00551.x. [DOI] [PubMed] [Google Scholar]
- 65.Denk D, Matiasek K, Just FT, Hermanns W, Baiker K, Herbach N, Steinberg T, Fischer A. Disseminated angiostrongylosis with fatal cerebral haemorrhages in two dogs in Germany: a clinical case study. Vet Parasitol. 2009;160:100–108. doi: 10.1016/j.vetpar.2008.10.077. [DOI] [PubMed] [Google Scholar]
- 66.King MCA, Grose RMR, Startup G. Angiostrongylus vasorum in the anterior chamber of a dog’s eye. J Small Anim Pract. 1994;35:326–328. doi: 10.1111/j.1748-5827.1994.tb03297.x. [DOI] [Google Scholar]
- 67.Gredal H, Willesen JL, Jensen HE, Nielsen OL, Kristensen AT, Koch J, Kirk RK, Pors SE, Skerritt GC, Berendt M. Acute neurological signs as the predominant clinical manifestation in four dogs with Angiostrongylus vasorum infections in Denmark. Acta Vet Scand. 2011;53:43. doi: 10.1186/1751-0147-53-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bourque AC, Conboy G, Miller LM, Whitney H. Pathological findings in dogs naturally infected with Angiostrongylus vasorum in Newfoundland and Labrador, Canada. J Vet Diag Investig. 2008;20:11–20. doi: 10.1177/104063870802000103. [DOI] [PubMed] [Google Scholar]
- 69.Oliveira-Júnior SD, Barçante JMP, Barçante TA, Ribeiro VM, Lima WS. Ectopic location of adult worms and first-stage larvae of Angiostrongylus vasorum in an infected dog. Vet Parasitol. 2004;121:293–296. doi: 10.1016/j.vetpar.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 70.Willesen JL, Jensen AL, Kristensen AT, Kock J. Haematological and biochemical changes in dogs naturally infected with Angiostrongylus vasorum before and after treatment. Vet J. 2009;180:106–111. doi: 10.1016/j.tvjl.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 71.Willesen JL, Jensen AL, Kristensen AT, Kjelgaard-Hansen M, Jessen R, Koch J. Serum fructosamine concentrations in 59 dogs naturally infected with Angiostrongylus vasorum. J Vet Med A Physiol Pathol Clin Med. 2006;53:266–269. doi: 10.1111/j.1439-0442.2006.00828.x. [DOI] [PubMed] [Google Scholar]
- 72.McGarry JW, Morgan ER. Identification of first-stage larvae of metastrongyles from dogs. Vet Rec. 2009;165:258–261. doi: 10.1136/vr.165.9.258. [DOI] [PubMed] [Google Scholar]
- 73.Verzberger-Epshtein I, Markham RJF, Sheppard JA, Stryhn H, Whitney H, Conboy GA. Serologic detection of Angiostrongylus vasorum infection in dogs. Vet Parasitol. 2008;151:53–60. doi: 10.1016/j.vetpar.2007.09.028. [DOI] [PubMed] [Google Scholar]
- 74.Barçante JM, Barçante TA, Dias SR, Vieira LQ, Lima WS, Negrão-Corrêa D. A method to obtain axenic Angiostrongylus vasorum first-stage larvae from dog feces. Parasitol Res. 2003;89:89–93. doi: 10.1007/s00436-002-0719-z. [DOI] [PubMed] [Google Scholar]
- 75.Humm K, Adamantos S. Is evaluation of a faecal smear a useful technique in the diagnosis of canine pulmonary angiostrongylosis? J Small Anim Pract. 2010;51:200–2003. doi: 10.1111/j.1748-5827.2009.00905.x. [DOI] [PubMed] [Google Scholar]
- 76.Schnyder M, Maurelli MP, Morgoglione ME, Kohler L, Deplazes P, Torgerson P, Cringoli G, Rinaldi L. Comparison of faecal techniques including FLOTAC for copromicroscopic detection of first stage larvae of Angiostrongylus vasorum. Parasitol Res. 2011;109:63–69. doi: 10.1007/s00436-010-2221-3. [DOI] [PubMed] [Google Scholar]
- 77.Barçante JM, Barçante TA, Ribeiro VM, Oliveira-Junior SD, Dias SR, Negrão-Corrêa D, Lima WS. Cytological and parasitological analysis of bronchoalveolar lavage fluid for the diagnosis of Angiostrongylus vasorum infection in dogs. Vet Parasitol. 2008;158:93–102. doi: 10.1016/j.vetpar.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 78.Schnyder M, Tanner M, Webster P, Barutzki D, Deplazes P. An ELISA for sensitive and specific detection of circulating antigen of Angiostrongylus vasorum in serum samples of naturally infected dogs. Vet Parasitol. 2011;179:152–158. doi: 10.1016/j.vetpar.2011.01.054. [DOI] [PubMed] [Google Scholar]
- 79.Schnyder M, Schaper R, Pantchev N, Kowalska D, Szwedko A, Deplazes P. Serological detection of circulating Angiostrongylus vasorum antigen and parasite-specific antibodies in dogs from Poland. Parasitol Res. 2013;112:109–117. doi: 10.1007/s00436-013-3285-7. [DOI] [PubMed] [Google Scholar]
- 80.Schucan A, Schnyder M, Tanner I, Barutzki D, Traversa D, Deplazes P. Detection of specific antibodies in dogs infected with Angiostrongylus vasorum. Vet Parasitol. 2012;185:216–224. doi: 10.1016/j.vetpar.2011.09.040. [DOI] [PubMed] [Google Scholar]
- 81.Cury MC, Lima WS, Vitor RWA. Enzyme-linked immunosorbent assay (ELISA) for the diagnosis of Angiostrongylus vasorum (Baillet, 1866) infection in dogs. Revue Med Vet. 1996;147:525–530. [Google Scholar]
- 82.Cury MC, Guimarães MP, Lima WS, Vitor RWA. Western blot analysis of the humoral response of dogs experimentally infected with Angiostrongylus vasorum (Baillet, 1866) Vet Parasitol. 2002;106:83–87. doi: 10.1016/S0304-4017(02)00031-6. [DOI] [PubMed] [Google Scholar]
- 83.Jefferies R, Morgan ER, Shaw SE. A SYBR green real-time PCR assay for the detection of the nematode Angiostrongylus vasorum in definitive and intermediate hosts. Vet Parasitol. 2009;166:112–118. doi: 10.1016/j.vetpar.2009.07.042. [DOI] [PubMed] [Google Scholar]
- 84.De Oliveira Vasconcelos V, De Almeida Vitor R, Dos Santos Lima W. Identification of stage-specific proteins of Angiostrongylus vasorum (Baillet, 1866) Kamensky. Parasitol Res. 2008;102:389–395. doi: 10.1007/s00436-007-0774-6. [DOI] [PubMed] [Google Scholar]
- 85.Jefferies R, Morgan ER, Helm J, Robinson M, Shaw SE. Improved detection of canine Angiostrongylus vasorum infection using real-time PCR and indirect ELISA. Parasitol Res. 2011;109:1577–1583. doi: 10.1007/s00436-011-2414-4. [DOI] [PubMed] [Google Scholar]
- 86.Al-Sabi MNS, Deplazes P, Webster P, Willesen JL, Davidson RK, Kapel CMO. PCR detection of Angiostrongylus vasorum in faecal samples of dogs and foxes. Parasitol Res. 2010;107:135–140. doi: 10.1007/s00436-010-1847-5. [DOI] [PubMed] [Google Scholar]
- 87.Søland J, Bolt G. Hypovolaemic shock after anthelmintic treatment of canine angiostrongylosis. J Small Anim Pract. 1996;37:594–596. doi: 10.1111/j.1748-5827.1996.tb02337.x. [DOI] [PubMed] [Google Scholar]
- 88.Mealey KL, Bentjen SA, Gay JM, Cantor GH. Ivermectin sensitivity in collies is associated with a deletion mutation of the mdr1 gene. Pharmacogenetics. 2001;11:727–733. doi: 10.1097/00008571-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 89.Schnyder M, Fahrion A, Ossent P, Kohler L, Webster P, Heine J, Deplazes P. Larvicidal effect of imidacloprid/moxidectin spot-on solution in dogs experimentally inoculated with Angiostrongylus vasorum. Vet Parasitol. 2009;166:326–332. doi: 10.1016/j.vetpar.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 90.Böhm C, Schnyder M, Thamsborg SM, Thompson CM, Trout C, Wolken S, Schnitzler B. Assessment of the combination of spinosad and milbemycin oxime in preventing the development of canine Angiostrongylus vasorum infections. Vet Parasitol. 2014;199:272–277. doi: 10.1016/j.vetpar.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 91.Braga FR, Carvalho RO, Araujo JM, Silva AR, Araújo JV, Lima WS, Tavela AO, Ferreira SR. Predatory activity of the fungi Duddingtonia flagrans, Monacrosporium thaumasium, Monacrosporium sinense and Arthrobotrys robusta on Angiostrongylus vasorum first-stage larvae. J Helminthol. 2009;83:303–308. doi: 10.1017/S0022149X09232342. [DOI] [PubMed] [Google Scholar]
- 92.Jefferies R, Morgan ER, Shaw SE, Heesom K. Identification of immuno-reactive adult Angiostrongylus vasorum proteins using mass spectrometry. Mol Biochem Parasitol. 2011;180:56–61. doi: 10.1016/j.molbiopara.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 93.Gasser RB, Jabbar A, Mohandas N, Schnyder M, Deplazes P, Littlewood DT, Jex AR. Mitochondrial genome of Angiostrongylus vasorum: comparison with congeners and implications for studying the population genetics and epidemiology of this parasite. Infect Genet Evol. 2012;12:1884–1891. doi: 10.1016/j.meegid.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 94.Ansell BR, Schnyder M, Deplazes P, Korhonen PK, Young ND, Hall RS, Mangiola S, Boag PR, Hofmann A, Sternberg PW, Jex AR, Gasser RB. Insights into the immuno-molecular biology of Angiostrongylus vasorum through transcriptomics-prospects for new interventions. Biotechnol Adv. 2013;31:1486–1500. doi: 10.1016/j.biotechadv.2013.07.006. [DOI] [PubMed] [Google Scholar]


