Abstract
Atrial fibrillation is associated with substantial morbidity and mortality rates. The incompletely understood pathogenesis of this cardiac dysrhythmia makes it difficult to improve approaches to primary and secondary prevention. Evidence has accumulated in regard to a relationship between inflammation and atrial fibrillation. Investigators have correlated the dysrhythmia with myocarditis, pericardiotomy, and C-reactive protein levels, suggesting that inflammation causes atrial fibrillation or participates in its onset and continuation. Conversely, other investigators suggest that atrial fibrillation induces an inflammatory response. In this review, we summarize and critically discuss the nature and clinical role of inflammation and C-reactive protein in atrial fibrillation.
Keywords: Atrial fibrillation/diagnosis/etiology/physiopathology/prevention & control; biological markers/blood; C-reactive protein/analysis/metabolism; disease management; heart conduction system/physiopathology; inflammation/complications/diagnosis/etiology; myocardial revascularization/adverse effects; polymorphism, genetic; primary prevention; risk factors
Atrial fibrillation (AF) is the sustained cardiac dysrhythmia most often encountered in clinical practice. Despite major advances in management and prophylaxis, AF continues to be associated with a high relative risk of death,1 and with increased morbidity, repeated hospitalization, and reduced quality of life. Moreover, the prevalence of AF becomes greater as the population ages.2 Therefore, improved primary and secondary AF prevention is needed to reduce the potentially enormous health burden. This requires a better understanding of the mechanisms underlying AF, with the premise that improved mechanistic insights will lead to innovative and more effective therapeutic approaches. Since the early 2000s, investigators have proposed that AF is caused by inflammatory processes. Study results have shown correlations between markers of inflammation, such as C-reactive protein (CRP), and the onset of AF. However, it remains debatable whether inflammation is only a consequence of left atrial remodeling, or whether inflammation is involved in the pathogenesis of the dysrhythmia. Herein, we summarize and critically discuss the relationship between AF and inflammation.
The Pathogenesis of Atrial Fibrillation
Atrial fibrillation can be induced and maintained by 3 kinds of mechanisms: 1) an irregular atrial response to a rapidly discharging, regularly firing driver that results from local ectopic activity; 2) an irregular atrial response to a rapid, regular discharge that results from a single localized reentry circuit; and 3) multiple functional reentry circuits that vary in time and space.3 Predisposing factors for all 3 mechanisms include cardiac aging, genotype, ischemic heart disease, and hyperthyroidism.4
Basic Mechanisms of Dysrhythmia
Ectopic Firing. Three basic mechanisms underlie ectopic firing: 1) “enhanced automaticity,” caused by a decrease in resting potassium (K+) permeability through the inward K+ current or by an increase in “funny current” (a pacemaker current manifested in normal human atrial cells during spontaneous phase 4 depolarization)5; 2) “early afterdepolarization,” a depolarization during the repolarization phase, promoted by action-potential prolongation that enables the L-type calcium (Ca) current to recover from inactivation; and 3) “delayed afterdepolarization,” an abnormal diastolic release of Ca from sarcoplasmic reticular Ca stores that causes a net depolarizing inward positive-ion movement.
Reentry. Reentry can maintain AF by producing a single-circuit reentry (a rapidly firing driver with fibrillatory propagation) or by producing multiple irregular reentry circuits. In both instances, the maintenance of continuous activity depends on atrial (substrate) anatomic and functional properties, with an appropriate balance between refractory and excitability determinants.
Atrial Remodeling. Atrial remodeling results from different kinds of persistent changes in atrial structure (structural remodeling) or function (electrical and neural/autonomic remodeling) that promote the occurrence or maintenance of AF. Inflammation might take part in both kinds of remodeling. Electrical remodeling consists of a shorter atrial effective refractory period, a loss of rate adaptation, and prolonged atrial conductivity.6 Accumulated Ca within atrial myocytes (related to AF) shortens the atrial effective refractory period and promotes wavelet-reentry circuits.7 The structural remodeling of the atria occurs in parallel with these changes of electrical remodeling. This process involves left atrial dilation and an increase in atrial fibrosis, particularly consequent to large deposits of collagen and fibronectin between individual cells. The deposition interferes with electrical continuity and slows conduction,8 whereas the fibroblasts, which can couple electrically to cardiomyocytes, promote reentry, ectopic activity, or both.9 Finally, autonomic neural remodeling promotes AF by means of vagal discharge that stimulates acetylcholine-dependent K current and reduces action-potential duration that stabilizes reentrant rotors,10 and by β-adrenoreceptor activation that increases diastolic Ca leak and promotes delayed depolarization-related ectopic firing by the hyperphosphorylating ryanodine receptor channel.11
Correlation between Atrial Fibrillation and Inflammation
The pathogenesis of AF is incompletely understood, but more knowledge should lead to new therapeutic approaches (Table I).12–41 It has been shown that the pathogenesis of several cardiovascular diseases—such as unstable angina and myocardial infarction42—involves inflammation. Substantial evidence also links inflammation to the initiation and perpetuation of AF, given the observed onset of AF in inflammatory states such as myocarditis43 and pericarditis,44 and the systemic inflammatory response induced by cardiac surgery and cardiopulmonary bypass.16 This observation was confirmed by histologic findings of atrial myocarditis in patients who had apparently lone AF, but not in persons who were in sinus rhythm.13 Inflammatory infiltrates, myocyte necrosis, and fibrosis—found in multiple atrial biopsy specimens from patients who had lone AF but no detectable organic heart disease or predisposing factors—were absent in biventricular biopsies of the same patients; this suggested a causative link between inflammation and AF. However, no viral, toxic, or autoimmune cause was established.13 Maixent and colleagues15 speculated on the possibility of an autoimmune process after finding circulating antimyosin autoantibodies in the serum of patients who had lone AF. Mandal and associates17 investigated the effects of heat-shock proteins (HSPs), a group of chaperone proteins that preserve cellular integrity by keeping proteins in their correctly folded state. Their study showed that the inflammation-induced expression of HSPs on the surface of myocytes might lead to cell lysis by circulating anti-HSP65 antibodies, with subsequent structural myocardial changes leading to AF after cardiac surgery. It is likely that the initiation of AF is a consequence of necrosis and fibrosis caused by inflammatory processes, which can trigger atrial dysrhythmias directly through fluctuations in membrane potential.44 This makes inflammation one of many possible cofactors of AF.
TABLE I.
Current Understanding of Correlation between Inflammation and Atrial Fibrillation
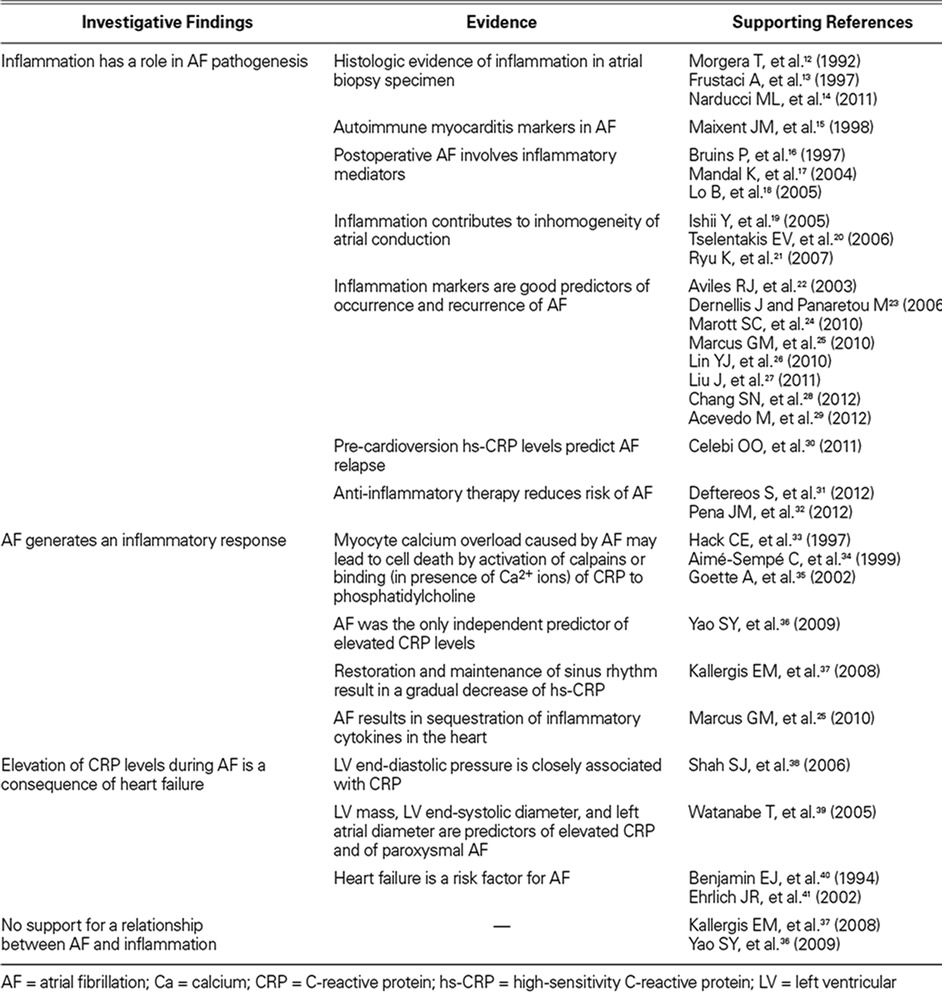
In perpetuating AF, inflammation might participate in the structural remodeling, inducing cellular degeneration, apoptosis, and subsequent atrial fibrosis and dilation. Watanabe and co-authors39 examined 50 consecutive patients who had paroxysmal AF and 50 control subjects without AF. The authors found that left ventricular mass, left ventricular end-systolic diameter, and left atrial diameter were predictors of elevated CRP and persistent AF. Similarly, Psychari and colleagues,45 after examining 90 patients with persistent and permanent AF, showed that CRP and interleukin (IL)-6 were positively related to left atrial diameter, and that a significant relationship existed between IL-6 levels and AF duration before cardioversion.
It is also likely that inflammation is involved during electrical remodeling, in particular by increasing the inhomogeneity of atrial conduction and consequently prolonging atrial conductivity. Ishii and associates19 examined 24 normal dogs and randomly divided them into 4 equal-sized groups: a control group that had anesthesia alone; a pericardiotomy group that had anesthesia and a pericardiotomy; an atriotomy group that underwent anesthesia, pericardiotomy, and a 5-cm lateral right atriotomy; and an anti-inflammatory group that underwent anesthesia, pericardiotomy, and a 5-cm lateral right atriotomy but with 2 mg/kg/d of methylprednisolone administered continuously for one week. Myocardial inflammation was quantified by myeloperoxidase activity, whereas inhomogeneous atrial conduction was quantified by the variation coefficient of the maximal local activation-phase difference. The authors found that inhomogeneous atrial conduction in the atriotomy and pericardiotomy groups was proportionally increased in comparison with the control group, and that anti-inflammatory therapy decreased the inhomogeneity after atriotomy. Moreover, AF duration was longer in the atriotomy and pericardiotomy groups than in the control and anti-inflammatory groups.19 Ryu and co-authors21 subjected 5 dogs to sterile pericarditis and showed that inflammation was associated with altered distribution of atrial connexins 40 and 43—major gap-junction proteins in the atrial myocardium that are responsible for cell-to-cell conduction of the action potential. Irregular production of these proteins might alter intercellular communication, reducing conduction within the atrial myocardium and creating an arrhythmogenic substrate for AF.46 This concept was supported by Sawaya and coworkers,47 who achieved the down-regulation of connexin 40 (but not of connexin 43) in 8 transgenic mice by means of targeted overexpression of tumor necrosis factor in the pericardium.
The most support for correlation between AF and inflammation derives from studies that have related inflammatory biomarkers to the dysrhythmia. Among the first such observations was the correlation between postoperative AF and the degree of systemic inflammatory response after coronary artery bypass grafting (CABG). Lo and co-authors18 showed that high baseline CRP levels were associated with an increased risk of postoperative AF. Gaudino and colleagues48 showed that the promoter polymorphism –174G/C IL-6 gene influenced the inflammatory response to CABG and was associated with postoperative AF. In addition, CABG patients who had low IL-2 levels when undergoing CABG had a reduced incidence of postoperative AF.49 Marcus and associates,50 in studying 971 coronary heart disease participants in the Heart and Soul Study, found that high levels of IL-6 were associated with the risk of AF. Other investigators associated serum IL-6 levels with AF after CABG,51 after cardioversion,52 and after radiofrequency catheter ablation.53 Aviles and associates22 performed a cross-sectional study of 5,806 subjects and reported that baseline levels of CRP were higher in patients affected by AF even after adjustment for multiple variables potentially associated with AF, and that CRP level is a strong predictor of future AF. Among 5,491 patients included in the longitudinal study, 897 (16%) developed AF during the follow-up period (median duration, 7.8 yr). Patients in higher CRP quartiles at baseline had a higher risk of developing AF during the follow-up period.22 Marott and colleagues24 monitored 10,276 subjects from the Copenhagen City Heart Study for 12 to 15 years for incident AF; CRP levels in the upper versus lower quintiles were associated with a 2.19-fold increased risk of AF after adjustment for age, sex, and statin use.24 In a population-based cohort of 1,011 patients, Dernellis and Panaretou23 explored whether the CRP-related incidence of AF was modified by components of the complement systems C3 and C4, with 4 years of follow-up data. Patients with high CRP and high complement levels had a significantly higher risk of AF than did those with normal CRP and low complement levels; conversely, absent a high complement level, high CRP levels were not significantly associated with AF.23 Acevedo and co-authors29 compared the baseline CRP levels of 130 patients who had newly diagnosed nonvalvular AF with those of 20 healthy individuals and found that baseline CRP levels were significant and independent predictors of recurrent AF upon one-year follow-up examination, independent of other clinical and echocardiographic variables. Celebi and colleagues30 evaluated the prognostic value of before- and after-cardioversion CRP levels in predicting the long-term risk of AF. They enrolled 216 patients who had persistent AF; the CRP levels were before cardioversion. After 12 months, basal CRP levels were significantly higher in the patients who had an AF relapse than in those who did not. Other investigators found correlation between baseline CRP levels and the risk of recurrent AF after ablation attempts by circumferential pulmonary vein isolation27 and catheter ablation.26
Inflammation might be involved in the prothrombotic state during AF.54 Inflammatory cells such as monocytes, macrophages, and lymphocytes produce cytokines and chemokines and can trigger and sustain thrombosis in AF. Interleukin-6 and CRP levels were found to be elevated in patients who had a dilated left atrium and poorly functioning left atrial appendage,55 and CRP has been correlated with established clinical stroke-risk stratification scores such as CHADS2 and Stroke Prevention in Atrial Fibrillation. The highest CRP levels were found in patients who had a moderate-to-high risk of stroke.56 Interleukin-6 induces the expression of tissue factor, fibrinogen, factor VIII, and von Willebrand factor, mediating a prothrombotic state. In addition, endothelial function might contribute to inflammation and thrombosis in AF57: von Willebrand factor and soluble P-selectin, released by activated endothelial cells, contribute to the development of a proinflammatory and prothrombotic state that mediates the adhesion of leukocytes to the endothelium.
Atrial Inflammation: Cause or Effect?
Inflammatory processes have been associated with AF, but it is uncertain whether this represents the cause or the effect of inflammation. Moreover, it is unclear whether inflammation has the same effect in normal atria and in atria that have undergone substantial structural remodeling.58
Factors Favoring a Role of Inflammation in the Initiation of Atrial Fibrillation. Evidence implicating inflammation in the initiation of AF includes the following:
The prevalence of AF is higher in the presence of inflammatory states such as cardiac surgery, myocarditis, pericarditis, and sepsis.59
Baseline CRP levels predict the occurrence and recurrence of AF.
Immunosuppressive therapy with glucocorticoids reduces AF recurrence, and this antiarrhythmic effect correlates with a decrease in plasma CRP levels. Ho and Tan60 performed a meta-analysis of 3,323 patients from 50 randomized controlled clinical trials in which corticosteroids were compared with placebo or an equal volume of normal saline solution, initiated before or at the time of cardiopulmonary bypass. The authors found that corticosteroid prophylaxis reduces the risk of AF in comparison with placebo (25.1% vs 35.1%; P <0.01) and that the prophylaxis was associated with reduced concentrations of IL-6 and high-sensitivity CRP 24 hours after surgery.60 Similar results have been found with the use of colchicine to reduce AF recurrence after pulmonary vein isolation.31
Statins have anti-inflammatory properties. In the Jupiter trial, 17,120 individuals without prior histories of arrhythmia were selected for underlying inflammation (high-sensitivity CPR, >2 mg/L) and were randomized to receive either 20 mg/d of rosuvastatin or a placebo. When compared with placebo, allocation to rosuvastatin was associated with a 27% reduction in the relative risk of developing AF during the trial period.32 Beyond this, a series of studies revealed the efficacy of statins in reducing AF in patients undergoing CABG, to the point that these drugs became a class IIa recommendation in the 2010 European Society of Cardiology Guidelines for CABG.61
Inflammatory cytokines have an arrhythmogenic effect on atrial myocardium. Tselentakis and colleagues20 quantified the conduction properties of 6 normal canine right atrial appendages as a function of the direction of impulse propagation with and without 80 μM of arachidonic acid. The inflammatory mediator produced an anisotropic and rapidly reversible decrease in conduction velocity, transverse to the long axis only.
Does C-Reactive Protein Have a Direct Role in the Generation of Atrial Fibrillation?
Marott and colleagues24 concluded that elevated plasma CRP in itself does not increase the risk of AF. When individuals underwent genotyping for 4 CRP gene polymorphisms, positive results were associated with as much as a 63% increase in plasma CRP levels, but not with an increased risk of AF. Conversely, a direct role of CRP is supported by Narducci and associates.14 By means of immunohistochemical analysis, they found the intracytoplasmic localization of CRP in isolated atrial cardiomyocytes in 13 of 23 atrial specimens from patients with AF and in no atrial specimens from a control group. Furthermore, CRP in human atrial tissue was unrelated to serum CRP levels in AF patients, which would explain why the results of this study14 differed from those of Marott and colleagues. It is likely that AF involves a sequestration of inflammatory cytokines in atrial tissue: Marcus and associates25 found that the difference between left atrial and coronary sinus CRP levels was significantly greater in patients who had AF at the time of the blood draw than in patients who were in sinus rhythm during that time. Chang and coworkers28 showed that changes in the promoter region regulated the CRP gene that influences the risk of AF: the –390A variant was associated with greater CRP gene-promoter activity, a higher plasma CRP level, and a higher risk of AF. Further analysis showed that CRP significantly increased the inward L-type Ca current in atrial myocytes with no changes in other ionic currents and without affecting expressions of gene-encoding pro-collagens in atrial fibroblasts. This suggests that CRP increases the risk of the AF-increasing Ca influx in atrial myocytes, but not because of atrial fibrosis.28
Factors Not Favoring a Role of Inflammation in the Pathogenesis of Atrial Fibrillation. Evidence against a primary role of inflammation in AF includes the following:
The restoration and maintenance of sinus rhythm results in a gradual decrease in CRP levels. Kallergis and colleagues37 examined 52 patients whose AF had persisted for 3 months and measured their CRP levels before and after successful electrical cardioversion. Those who were in sinus rhythm one month later had significantly lower CRP levels than at baseline; conversely, subjects whose AF recurred had no differences in CRP levels during the study, suggesting that AF by itself induces inflammation.
No significant difference was found in CRP levels between persistent AF and episodes of AF in paroxysmal AF, and between the absence of AF in paroxysmal AF and its absence in control subjects. Yao and associates36 enrolled 411 patients who had lone AF and found that the presence of AF was the only independent predictor of elevated CRP levels.
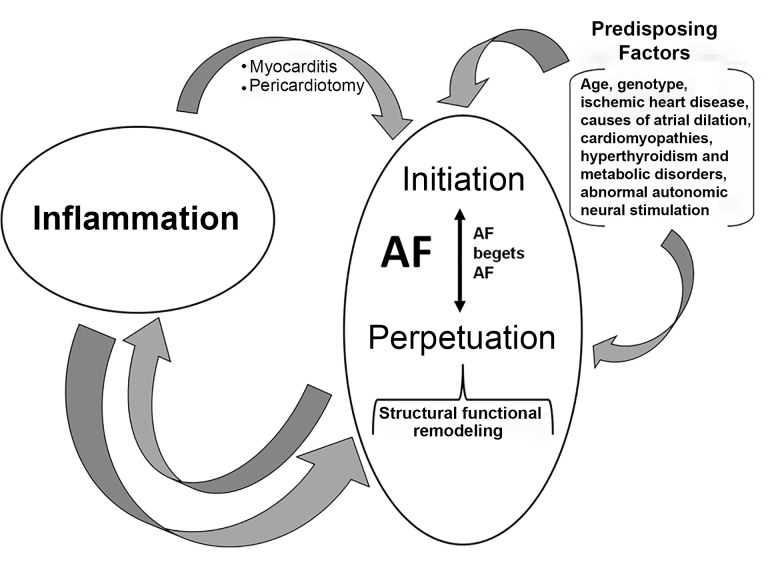
Although the mechanisms by which AF might cause inflammation are unknown (Fig. 1), it has been hypothesized that the myocyte Ca overload caused by AF leads to cell death34 mediated by the activation of calpains35 or by the binding (in the presence of Ca2+ ions) of CRP to phosphatidylcholine-generating long-chain acylcarnitines and lysophosphatidylcholines. These mechanisms lead to cellular membrane dysfunction, energy depletion, and apoptosis,33 and might induce a low-grade inflammatory response—including healing and repair that bring about adverse structural and electrical changes and might also explain the significant difference in CRP levels during AF in the left atrium and coronary sinus.14
Fig. 1.
Diagram shows the relationship between atrial fibrillation (AF) and inflammation. Inflammation might contribute to initiating AF (as in myocarditis and pericardiotomy) and perpetuating AF (as one of many cofactors that together contribute to remodeling). On the other hand, AF might generate an inflammatory response, as shown by the normalization of C-reactive protein levels after cardioversion.
In some cases, both the elevation of CRP and the onset of AF might be consequences of heart failure; indeed, Shah and colleagues38 have shown, in 98 patients undergoing cardiac catheterization, that left ventricular end-diastolic pressure is closely associated with CRP level. On the other hand, heart failure is a recognized risk factor for AF.40,41
Future Directions
Understanding the pathogenesis of AF and the relationships between inflammation and AF is of both academic and clinical interest, because insights might lead to better prevention and treatment of this common but dangerous dysrhythmia. The detailed imaging of inflammation by positron emission tomographic or molecular means62 might help to clarify the role of inflammation in AF, and microRNA could prove to be of substantial value in the study of tissue and circulating biomarkers.63 If and when a causal link between inflammation and AF is proved, novel approaches to targeting inflammation, including anti-IL-1 and tumor necrosis factor-α antibodies and microRNA antagonists or mimics,64–66 might lead to better therapeutic options.
Conclusion
Despite the evidence linking inflammation with AF, the role of inflammation as an initiating event in the development of AF remains debatable. However, on the basis of the current evidence, it is likely that inflammation is involved in electrophysiologic and structural atrial remodeling—processes integral to the development and perpetuation of AF—and that the dysrhythmia subsequently generates an inflammatory response that contributes to remodeling. We need a better understanding of the pathophysiology of AF in order to develop new therapeutic approaches.
Footnotes
From: Institute of Cardiology, Catholic University of the Sacred Heart, 00168 Rome, Italy
Dr. Galea is now at the Department of Cardiovascular Sciences, University of Milan, Milan, Italy.
This paper's source of funding is grant number 7021526 from the Catholic University of Rome.
References
- 1.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98(10):946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82(8A):2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- 3.Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124(20):2264–74. doi: 10.1161/CIRCULATIONAHA.111.019893. [DOI] [PubMed] [Google Scholar]
- 4.Camm AJ, Al-Khatib SM, Calkins H, Halperin JL, Kirchhof P, Lip GY et al. A proposal for new clinical concepts in the management of atrial fibrillation. Am Heart J. 2012;164(3):292–302.e1. doi: 10.1016/j.ahj.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 5.Stillitano F, Lonardo G, Zicha S, Varro A, Cerbai E, Mugelli A, Nattel S. Molecular basis of funny current (If) in normal and failing human heart. J Mol Cell Cardiol. 2008;45(2):289–99. doi: 10.1016/j.yjmcc.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Hertervig EJ, Yuan S, Carlson J, Kongstad-Rasmussen O, Olsson SB. Evidence for electrical remodelling of the atrial myocardium in patients with atrial fibrillation. A study using the monophasic action potential recording technique. Clin Physiol Funct Imaging. 2002;22(1):8–12. doi: 10.1046/j.1475-097x.2002.00384.x. [DOI] [PubMed] [Google Scholar]
- 7.Lau CP, Tse HF. Electrical remodelling of chronic atrial fibrillation. Clin Exp Pharmacol Physiol. 1997;24(12):982–3. doi: 10.1111/j.1440-1681.1997.tb02734.x. [DOI] [PubMed] [Google Scholar]
- 8.Kostin S, Klein G, Szalay Z, Hein S, Bauer EP, Schaper J. Structural correlate of atrial fibrillation in human patients. Cardiovasc Res. 2002;54(2):361–79. doi: 10.1016/s0008-6363(02)00273-0. [DOI] [PubMed] [Google Scholar]
- 9.Yue L, Xie J, Nattel S. Molecular determinants of cardiac fibroblast electrical function and therapeutic implications for atrial fibrillation. Cardiovasc Res. 2011;89(4):744–53. doi: 10.1093/cvr/cvq329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kneller J, Zou R, Vigmond EJ, Wang Z, Leon LJ, Nattel S. Cholinergic atrial fibrillation in a computer model of a two-dimensional sheet of canine atrial cells with realistic ionic properties. Circ Res. 2002;90(9):E73–87. doi: 10.1161/01.res.0000019783.88094.ba. [DOI] [PubMed] [Google Scholar]
- 11.Dobrev D, Voigt N, Wehrens XH. The ryanodine receptor channel as a molecular motif in atrial fibrillation: pathophysiological and therapeutic implications. Cardiovasc Res. 2011;89(4):734–43. doi: 10.1093/cvr/cvq324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgera T, Di L, enarda A, Dreas L, Pinamonti B, Humar F, Bussani R et al. Electrocardiography of myocarditis revisited: clinical and prognostic significance of electrocardiographic changes. Am Heart J. 1992;124(2):455–67. doi: 10.1016/0002-8703(92)90613-z. [DOI] [PubMed] [Google Scholar]
- 13.Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo MA, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997;96(4):1180–4. doi: 10.1161/01.cir.96.4.1180. [DOI] [PubMed] [Google Scholar]
- 14.Narducci ML, Pelargonio G, Dello Russo A, Casella M, Biasucci LM, La Torre G et al. Role of tissue C-reactive protein in atrial cardiomyocytes of patients undergoing catheter ablation of atrial fibrillation: pathogenetic implications. Europace. 2011;13(8):1133–40. doi: 10.1093/europace/eur068. [DOI] [PubMed] [Google Scholar]
- 15.Maixent JM, Paganelli F, Scaglione J, Levy S. Antibodies against myosin in sera of patients with idiopathic paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 1998;9(6):612–7. doi: 10.1111/j.1540-8167.1998.tb00942.x. [DOI] [PubMed] [Google Scholar]
- 16.Bruins P, te Velthuis H, Yazdanbakhsh AP, Jansen PG, van Hardevelt FW, de Beaumont EM et al. Activation of the complement system during and after cardiopulmonary bypass surgery: postsurgery activation involves C-reactive protein and is associated with postoperative arrhythmia. Circulation. 1997;96(10):3542–8. doi: 10.1161/01.cir.96.10.3542. [DOI] [PubMed] [Google Scholar]
- 17.Mandal K, Jahangiri M, Mukhin M, Poloniecki J, Camm AJ, Xu Q. Association of anti-heat shock protein 65 antibodies with development of postoperative atrial fibrillation. Circulation. 2004;110(17):2588–90. doi: 10.1161/01.CIR.0000136825.96029.A5. [DOI] [PubMed] [Google Scholar]
- 18.Lo B, Fijnheer R, Nierich AP, Bruins P, Kalkman CJ. C-reactive protein is a risk indicator for atrial fibrillation after myocardial revascularization. Ann Thorac Surg. 2005;79(5):1530–5. doi: 10.1016/j.athoracsur.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Ishii Y, Schuessler RB, Gaynor SL, Yamada K, Fu AS, Boineau JP, Damiano RJ., Jr. Inflammation of atrium after cardiac surgery is associated with inhomogeneity of atrial conduction and atrial fibrillation. Circulation. 2005;111(22):2881–8. doi: 10.1161/CIRCULATIONAHA.104.475194. [DOI] [PubMed] [Google Scholar]
- 20.Tselentakis EV, Woodford E, Chandy J, Gaudette GR, Saltman AE. Inflammation effects on the electrical properties of atrial tissue and inducibility of postoperative atrial fibrillation. J Surg Res. 2006;135(1):68–75. doi: 10.1016/j.jss.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 21.Ryu K, Li L, Khrestian CM, Matsumoto N, Sahadevan J, Ruehr ML et al. Effects of sterile pericarditis on connexins 40 and 43 in the atria: correlation with abnormal conduction and atrial arrhythmias. Am J Physiol Heart Circ Physiol. 2007;293(2):H1231–41. doi: 10.1152/ajpheart.00607.2006. [DOI] [PubMed] [Google Scholar]
- 22.Aviles RJ, Martin DO, Apperson-Hansen C, Houghtaling PL, Rautaharju P, Kronmal RA et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108(24):3006–10. doi: 10.1161/01.CIR.0000103131.70301.4F. [DOI] [PubMed] [Google Scholar]
- 23.Dernellis J, Panaretou M. Effects of C-reactive protein and the third and fourth components of complement (C3 and C4) on incidence of atrial fibrillation. Am J Cardiol. 2006;97(2):245–8. doi: 10.1016/j.amjcard.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 24.Marott SC, Nordestgaard BG, Zacho J, Friberg J, Jensen GB, Tybjaerg-Hansen A, Benn M. Does elevated C-reactive protein increase atrial fibrillation risk? A Mendelian randomization of 47,000 individuals from the general population. J Am Coll Cardiol. 2010;56(10):789–95. doi: 10.1016/j.jacc.2010.02.066. [DOI] [PubMed] [Google Scholar]
- 25.Marcus GM, Smith LM, Ordovas K, Scheinman MM, Kim AM, Badhwar N et al. Intracardiac and extracardiac markers of inflammation during atrial fibrillation. Heart Rhythm. 2010;7(2):149–54. doi: 10.1016/j.hrthm.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin YJ, Tsao HM, Chang SL, Lo LW, Tuan TC, Hu YF et al. Prognostic implications of the high-sensitive C-reactive protein in the catheter ablation of atrial fibrillation. Am J Cardiol. 2010;105(4):495–501. doi: 10.1016/j.amjcard.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 27.Liu J, Fang PH, Dibs S, Hou Y, Li XF, Zhang S. High-sensitivity C-reactive protein as a predictor of atrial fibrillation recurrence after primary circumferential pulmonary vein isolation. Pacing Clin Electrophysiol. 2011;34(4):398–406. doi: 10.1111/j.1540-8159.2010.02978.x. [DOI] [PubMed] [Google Scholar]
- 28.Chang SN, Tsai CT, Wu CK, Lee JK, Lai LP, Huang SW et al. A functional variant in the promoter region regulates the C-reactive protein gene and is a potential candidate for increased risk of atrial fibrillation. J Intern Med. 2012;272(3):305–15. doi: 10.1111/j.1365-2796.2012.02531.x. [DOI] [PubMed] [Google Scholar]
- 29.Acevedo M, Corbalan R, Braun S, Pereira J, Gonzalez I, Navarrete C. Biochemical predictors of cardiac rhythm at 1 year follow-up in patients with non-valvular atrial fibrillation. J Thromb Thrombolysis. 2012;33(4):383–8. doi: 10.1007/s11239-012-0690-1. [DOI] [PubMed] [Google Scholar]
- 30.Celebi OO, Celebi S, Canbay A, Ergun G, Aydogdu S, Diker E. The effect of sinus rhythm restoration on high-sensitivity C-reactive protein levels and their association with long-term atrial fibrillation recurrence after electrical cardioversion. Cardiology. 2011;118(3):168–74. doi: 10.1159/000327998. [DOI] [PubMed] [Google Scholar]
- 31.Deftereos S, Giannopoulos G, Kossyvakis C, Efremidis M, Panagopoulou V, Kaoukis A et al. Colchicine for prevention of early atrial fibrillation recurrence after pulmonary vein isolation: a randomized controlled study. J Am Coll Cardiol. 2012;60(18):1790–6. doi: 10.1016/j.jacc.2012.07.031. [DOI] [PubMed] [Google Scholar]
- 32.Pena JM, MacFadyen J, Glynn RJ, Ridker PM. High-sensitivity C-reactive protein, statin therapy, and risks of atrial fibrillation: an exploratory analysis of the JUPITER trial. Eur Heart J. 2012;33(4):531–7. doi: 10.1093/eurheartj/ehr460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hack CE, Wolbink GJ, Schalkwijk C, Speijer H, Hermens WT, van den Bosch H. A role for secretory phospholipase A2 and C-reactive protein in the removal of injured cells. Immunol Today. 1997;18(3):111–5. doi: 10.1016/s0167-5699(97)01002-5. [DOI] [PubMed] [Google Scholar]
- 34.Aime-Sempe C, Folliguet T, Rucker-Martin C, Krajewska M, Krajewska S, Heimburger M et al. Myocardial cell death in fibrillating and dilated human right atria. J Am Coll Cardiol. 1999;34(5):1577–86. doi: 10.1016/s0735-1097(99)00382-4. [DOI] [PubMed] [Google Scholar]
- 35.Goette A, Arndt M, Rocken C, Staack T, Bechtloff R, Reinhold D et al. Calpains and cytokines in fibrillating human atria. Am J Physiol Heart Circ Physiol. 2002;283(1):H264–72. doi: 10.1152/ajpheart.00505.2001. [DOI] [PubMed] [Google Scholar]
- 36.Yao SY, Chu JM, Chen KP, Tang M, Fang PH, Wang FZ, Zhang S. Inflammation in lone atrial fibrillation. Clin Cardiol. 2009;32(2):94–8. doi: 10.1002/clc.20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kallergis EM, Manios EG, Kanoupakis EM, Mavrakis HE, Kolyvaki SG, Lyrarakis GM et al. The role of the post-cardioversion time course of hs-CRP levels in clarifying the relationship between inflammation and persistence of atrial fibrillation. Heart. 2008;94(2):200–4. doi: 10.1136/hrt.2006.108688. [DOI] [PubMed] [Google Scholar]
- 38.Shah SJ, Marcus GM, Gerber IL, McKeown BH, Vessey JC, Jordan MV et al. High-sensitivity C-reactive protein and parameters of left ventricular dysfunction. J Card Fail. 2006;12(1):61–5. doi: 10.1016/j.cardfail.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Watanabe T, Takeishi Y, Hirono O, Itoh M, Matsui M, Nakamura K et al. C-reactive protein elevation predicts the occurrence of atrial structural remodeling in patients with paroxysmal atrial fibrillation. Heart Vessels. 2005;20(2):45–9. doi: 10.1007/s00380-004-0800-x. [DOI] [PubMed] [Google Scholar]
- 40.Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271(11):840–4. [PubMed] [Google Scholar]
- 41.Ehrlich JR, Nattel S, Hohnloser SH. Atrial fibrillation and congestive heart failure: specific considerations at the intersection of two common and important cardiac disease sets. J Cardiovasc Electrophysiol. 2002;13(4):399–405. doi: 10.1046/j.1540-8167.2002.00399.x. [DOI] [PubMed] [Google Scholar]
- 42.Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid A protein in severe unstable angina. N Engl J Med. 1994;331(7):417–24. doi: 10.1056/NEJM199408183310701. [DOI] [PubMed] [Google Scholar]
- 43.Spodick DH. Arrhythmias during acute pericarditis. A prospective study of 100 consecutive cases. JAMA. 1976;235(1):39–41. [PubMed] [Google Scholar]
- 44.Klein RM, Vester EG, Brehm MU, Dees H, Picard F, Niederacher D et al. Inflammation of the myocardium as an arrhythmia trigger [in German] Z Kardiol. 2000;89(Suppl 3):24–35. [PubMed] [Google Scholar]
- 45.Psychari SN, Apostolou TS, Sinos L, Hamodraka E, Liakos G, Kremastinos DT. Relation of elevated C-reactive protein and interleukin-6 levels to left atrial size and duration of episodes in patients with atrial fibrillation. Am J Cardiol. 2005;95(6):764–7. doi: 10.1016/j.amjcard.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 46.Chaldoupi SM, Loh P, Hauer RN, de Bakker JM, van Rijen HV. The role of connexin40 in atrial fibrillation. Cardiovasc Res. 2009;84(1):15–23. doi: 10.1093/cvr/cvp203. [DOI] [PubMed] [Google Scholar]
- 47.Sawaya SE, Rajawat YS, Rami TG, Szalai G, Price RL, Siva-subramanian N et al. Downregulation of connexin40 and increased prevalence of atrial arrhythmias in transgenic mice with cardiac-restricted overexpression of tumor necrosis factor. Am J Physiol Heart Circ Physiol. 2007;292(3):H1561–7. doi: 10.1152/ajpheart.00285.2006. [DOI] [PubMed] [Google Scholar]
- 48.Gaudino M, Andreotti F, Zamparelli R, Di C, astelnuovo A, Nasso G, Burzotta F et al. The -174G/C interleukin-6 polymorphism influences postoperative interleukin-6 levels and postoperative atrial fibrillation. Is atrial fibrillation an inflammatory complication? Circulation. 2003;108(Suppl 1):II195–9. doi: 10.1161/01.cir.0000087441.48566.0d. [DOI] [PubMed] [Google Scholar]
- 49.Hak L, Mysliwska J, Wieckiewicz J, Szyndler K, Siebert J, Rogowski J. Interleukin-2 as a predictor of early postoperative atrial fibrillation after cardiopulmonary bypass graft (CABG) J Interferon Cytokine Res. 2009;29(6):327–32. doi: 10.1089/jir.2008.0082.2906. [DOI] [PubMed] [Google Scholar]
- 50.Marcus GM, Whooley MA, Glidden DV, Pawlikowska L, Zaroff JG, Olgin JE. Interleukin-6 and atrial fibrillation in patients with coronary artery disease: data from the Heart and Soul Study. Am Heart J. 2008;155(2):303–9. doi: 10.1016/j.ahj.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaireviciute D, Blann AD, Balakrishnan B, Lane DA, Patel JV, Uzdavinys G et al. Characterisation and validity of inflammatory biomarkers in the prediction of post-operative atrial fibrillation in coronary artery disease patients. Thromb Haemost. 2010;104(1):122–7. doi: 10.1160/TH09-12-0837. [DOI] [PubMed] [Google Scholar]
- 52.Henningsen KM, Therkelsen SK, Bruunsgaard H, Krabbe KS, Pedersen BK, Svendsen JH. Prognostic impact of hs-CRP and IL-6 in patients with persistent atrial fibrillation treated with electrical cardioversion. Scand J Clin Lab Invest. 2009;69(3):425–32. doi: 10.1080/00365510802676848. [DOI] [PubMed] [Google Scholar]
- 53.Henningsen KM, Nilsson B, Bruunsgaard H, Chen X, Pedersen BK, Svendsen JH. Prognostic impact of hs-CRP and IL-6 in patients undergoing radiofrequency catheter ablation for atrial fibrillation. Scand Cardiovasc J. 2009;43(5):285–91. doi: 10.1080/14017430802653676. [DOI] [PubMed] [Google Scholar]
- 54.Conway DS, Buggins P, Hughes E, Lip GY. Relationship of interleukin-6 and C-reactive protein to the prothrombotic state in chronic atrial fibrillation. J Am Coll Cardiol. 2004;43(11):2075–82. doi: 10.1016/j.jacc.2003.11.062. [DOI] [PubMed] [Google Scholar]
- 55.Tousoulis D, Zisimos K, Antoniades C, Stefanadi E, Siasos G, Tsioufis C et al. Oxidative stress and inflammatory process in patients with atrial fibrillation: the role of left atrium distension. Int J Cardiol. 2009;136(3):258–62. doi: 10.1016/j.ijcard.2008.04.087. [DOI] [PubMed] [Google Scholar]
- 56.Lip GY, Patel JV, Hughes E, Hart RG. High-sensitivity C-reactive protein and soluble CD40 ligand as indices of inflammation and platelet activation in 880 patients with nonvalvular atrial fibrillation: relationship to stroke risk factors, stroke risk stratification schema, and prognosis. Stroke. 2007;38(4):1229–37. doi: 10.1161/01.STR.0000260090.90508.3e. [DOI] [PubMed] [Google Scholar]
- 57.Raviele A, Ronco F. Endothelial dysfunction and atrial fibrillation: what is the relationship? J Cardiovasc Electrophysiol. 2011;22(4):383–4. doi: 10.1111/j.1540-8167.2010.01954.x. [DOI] [PubMed] [Google Scholar]
- 58.Kourliouros A, Savelieva I, Kiotsekoglou A, Jahangiri M, Camm J. Current concepts in the pathogenesis of atrial fibrillation. Am Heart J. 2009;157(2):243–52. doi: 10.1016/j.ahj.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 59.Arora S, Lang I, Nayyar V, Stachowski E, Ross DL. Atrial fibrillation in a tertiary care multidisciplinary intensive care unit--incidence and risk factors. Anaesth Intensive Care. 2007;35(5):707–13. doi: 10.1177/0310057X0703500508. [DOI] [PubMed] [Google Scholar]
- 60.Ho KM, Tan JA. Benefits and risks of corticosteroid prophylaxis in adult cardiac surgery: a dose-response meta-analysis. Circulation. 2009;119(14):1853–66. doi: 10.1161/CIRCULATIONAHA.108.848218. [DOI] [PubMed] [Google Scholar]
- 61.European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery. Camm AJ, Kirchhof P, Lip GY, Schotten U et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC) [published erratum appears in Eur Heart J 2011;32(9):1172] Eur Heart J. 2010;31(19):2369–429. doi: 10.1093/eurheartj/ehq278. [DOI] [PubMed] [Google Scholar]
- 62.Wu C, Li F, Niu G, Chen X. PET imaging of inflammation biomarkers. Theranostics. 2013;3(7):448–66. doi: 10.7150/thno.6592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Biasucci LM, Cardillo MT. MicroRNA and myocardial infarction: a mystery turning into glory? J Am Coll Cardiol. 2013;62(11):999–1001. doi: 10.1016/j.jacc.2013.03.084. [DOI] [PubMed] [Google Scholar]
- 64.Ridker PM. Targeting inflammatory pathways for the treatment of cardiovascular disease. Eur Heart J. 2014;35(9):540–3. doi: 10.1093/eurheartj/eht398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marini MG, Sonnino C, Previtero M, Biasucci LM. Targeting inflammation: impact on atherothrombosis. J Cardiovasc Transl Res. 2014;7(1):9–18. doi: 10.1007/s12265-013-9523-7. [DOI] [PubMed] [Google Scholar]
- 66.Caroli A, Cardillo MT, Galea R, Biasucci LM. Potential therapeutic role of microRNAs in ischemic heart disease. J Cardiol. 2013;61(5):315–20. doi: 10.1016/j.jjcc.2013.01.012. [DOI] [PubMed] [Google Scholar]