Abstract
Rationale
Paper-based medical record systems are known to have major problems of inaccuracy, incomplete data, poor accessibility, and challenges to patient confidentiality. They are also an inefficient mechanism of record-sharing for interdisciplinary patient assessment and management, and represent a major problem for keeping current and monitoring quality control to facilitate improvement. To address those concerns, national, regional, and local health care authorities have increased the pressure on oncology practices to upgrade from paper-based systems to electronic health records.
Objectives
Here, we describe and discuss the challenges to implementing a region-wide oncology information system across four independent health care organizations, and we describe the lessons learned from the initial phases that are now being applied in subsequent activities of this complex project.
Results
The need for change must be shared across centres to increase buy-in, adoption, and implementation. It is essential to establish physician leadership, commitment, and engagement in the process. Work processes had to be revised to optimize use of the new system. Culture change must be included in the change management strategy. Furthermore, training and resource requirements must be thoroughly planned, implemented, monitored, and modified as required for effective adoption of new work processes and technology. Interfaces must be established with multiple existing electronic systems across the region to ensure appropriate patient flow. Periodic assessment of the existing project structure is necessary, and adjustments are often required to ensure that the project meets its objectives.
Conclusions
The implementation of region-wide oncology information systems across different health practice locations has many challenges. Leadership is essential. A strong, collaborative information-sharing strategy across the region and with the supplier is essential to identify, discuss, and resolve implementation problems. A structure that supports project management and accountability contributes to success.
Keywords: Electronic medical records, oncology information systems, implementation
1. INTRODUCTION
Practice pattern variations are common in cancer care. To ensure best practice and to facilitate efficient health system administration, access to data about practice variation and treatment processes and outcomes is critical for health care providers, patients, and system administrators1. Oncology information systems (oiss) are essential tools for measuring the rate of adoption and the effectiveness of practice standards, for improving patient safety, and for facilitating research2–5. However, there is concern that oiss can lower productivity by requiring providers to enter data and clinical orders, and it has been suggested that system response and down time could jeopardize patient care6.
Paper-based systems are commonly inaccurate or incomplete and difficult to access; they offer poor protection of patient confidentiality; they are inefficient for record-sharing, interdisciplinary patient assessment, and management; and they are difficult to keep current. Furthermore, paper-based records can put patient safety at risk and limit the capacity to monitor and evaluate quality and effectiveness of care at a time when outcomes assessment has become an important measure7,8. In oncology, the ever-increasing volume of clinical data, the complexities of treatment and supportive care options, and the demand for near “real-time” outcomes underscore the need for an ois to access, organize, and manage clinical oncology data9 and potentially to realize true health benefits and to reduce costs10.
The regionalization of Ontario cancer services in regional cancer centres and local health integration networks provided an opportunity to standardize safe care processes and to improve efficiency and reduce costs while bringing care closer to home. The implementation of a regional oncology information system (rois) was felt to be a key aspect in the integration of the regional cancer program.
2. OBJECTIVE
This paper describes the challenges encountered in implementing a rois across four independent health care organizations and the lessons learned from the initial phases of the implementation process that are now being applied in the next phases of this complex project. The vision for the original initiative was to implement a common, integrated rois to support high-quality, standardized, safe, and efficient delivery of cancer care to patients in a region of southern Ontario.
The implementation of any new information technology (it) is often challenging. Some challenges are purely technical, such as integration of the new technology into existing systems; others are behavioural and require major shifts in how clinical practice is conducted. The implementation process is made more complex when it is undertaken with multiple players at a regional level and with organizations of different sizes and cultures.
2.1. Setting
After external consultation and internal leadership workshops in 2009, the regional oncology clinical and administrative leadership agreed to implement a common rois at the four hospitals that provide ambulatory cancer services in a region serving a population of approximately 1.4 million residents. Systemic chemotherapy was administered at all four facilities, but at the time when the rois was first discussed, only one site provided radiotherapy. A second cancer centre for the region was planned to open in early 2013. There was agreement that the radiation program at this second site would open as part of an integrated program with the established radiotherapy centre (site A). Site A operated a large program (11,627 new patient visits during fiscal 2011–2012). It also provided 31,607 systemic therapy treatments and 76,333 radiation therapy treatments during the same period. The new cancer centre (site B) handled 1958 new patient visits and a total of 9686 systemic therapy treatments. Two smaller facilities (sites C and D) provided on-site consultation for 698 and 371 new cases respectively in 2011–2012 and delivered a total of 3083 systemic therapy treatments.
2.2. The “Burning Platform” for Change
Table i outlines details of the various systems used across the region to support patient care in the ambulatory oncology setting. These oiss operated independently and did not interface with their respective host hospital information systems (hiss), thereby creating potentially significant patient care and safety issues. The inability to transfer patient information electronically between sites meant that cancer patients receiving treatment in more than one location had to provide demographic information and medical history on multiple occasions. Photocopying and chart mirroring between active treatment sites was used, which created incremental work and the potential for incomplete or inconsistent paper-based information. Furthermore, patients were often asked to carry their own medical information when referred to a provider at another location. That practice negatively affected the patient experience, and the transport of paper records was a threat to patient confidentiality. In addition, data entered into one oncology system had to be transferred manually into other systems for reporting to the provincial cancer program. Those transfers in turn created the risk of data entry errors and inefficiencies in resource use.
TABLE I.
Regional systems that supported patient care in the ambulatory oncology setting
| Site | Systems in use | Key issues |
|---|---|---|
| A | Electronic system for radiation treatment planning and operation of radiotherapy equipment | System features not used to full capacity |
| Practice administration | Out of date, no longer supported by supplier | |
| Clinic functions | Paper charts in clinics | |
| Chemotherapy system | Computerized prescriber order entry (cpoe) as a separate system | |
| Integration with hospital information system (his) | Nonexistent | |
| B | Practice administration | Electronic medical record (emr) used was several versions out of date; not supported by supplier or hospital information technology department |
| Clinic functions | Paper charts supporting operations and many paper-based embedded functions | |
| Chemotherapy system | Electronic cpoe (same system as practice administration) | |
| Integration With Hospital his | None; registration of admission, discharge, and transfer (a/d/t) in his was a separate function from the oncology information system (ois) | |
| C | Practice administration | Used site A’s system; used his scheduling system |
| Clinic functions | Paper charts in clinics | |
| Chemotherapy system | Used site A’s electronic cpoe as a separate system | |
| Integration with his | None; registration of a/d/t in his was a separate function from ois; used his for scheduling | |
| D | Practice administration | Used site A’s system; used his scheduling system |
| Clinic functions | Paper charts in clinics | |
| Chemotherapy system | Used site A’s electronic cpoe as a separate system | |
| Integration with his | Registration of a/d/t in his was a separate function from ois; used his for scheduling |
2.3. Implementation Approach
For the rois to be successful, it was felt to be critical that all partners participate fully and collaboratively and function as a unified team. Guiding principles for decision-making were established by the leadership team. The decisions were to
be made in the best interest of patients;
support a standardized configuration of the rois and its use across the region;
take account of the most effective and efficient workflow processes;
avoid unnecessary duplication of existing processes, databases, and systems;
be informed by evidence, when available;
be made transparently and by consensus of the partner organizations; and
be communicated openly to all stakeholders.
In addition to those guiding principles, several criteria for the development of the project structure and associated work processes were followed:
Managers and supervisors were involved in reviewing and developing solutions.
Physicians and other clinicians were involved in reviewing, assessing, and approving new processes and functions before implementation.
Clear lines of accountability were established.
The Project Steering Committee (psc) that was initially created included representatives from sites A and B because of the priority represented by the existing radiotherapy system at site A and the need to convert an outdated ois at site B. The psc comprised senior administrative leaders at the vice-presidential level, directors of clinical programs and it, and managerial-level representatives who had intimate knowledge of the information systems.
At site A, a major upgrade to the radiation ois system was successfully undertaken without significant issues in February 2012. Clinicians and staff at site B had experience in the use of a different ois. Its leadership perceived that site B would experience few differences in their work processes. Site B was moving to a new facility and any significant changes were therefore suspended for 1 year before the move, as directed by leadership at that site.
Site B lacked the capacity to develop new processes and to design process maps identified by current and future state analyses. Informatics leadership at site A took on that responsibility. In addition, the rois supplier provided extensive group and one-onone education over a long period of time with various educators. Site B asked the educators to focus on functionality rather than on processes, because clinicians and staff at that site had not been involved in the process redesign.
Data conversion from the site B ois to the new rois was another key step in the transition. Conversion requires a careful process of data cleaning and matching in advance of the conversion process. The site B ois came from a different supplier and was several versions out of date. The fields in which some of the data elements were located were not well defined, and many key fields were maintained in text format rather than as discrete elements, making translation and conversion difficult, if not impossible. In addition, the original supplier of software to site B did not assist with data access to facilitate the conversion.
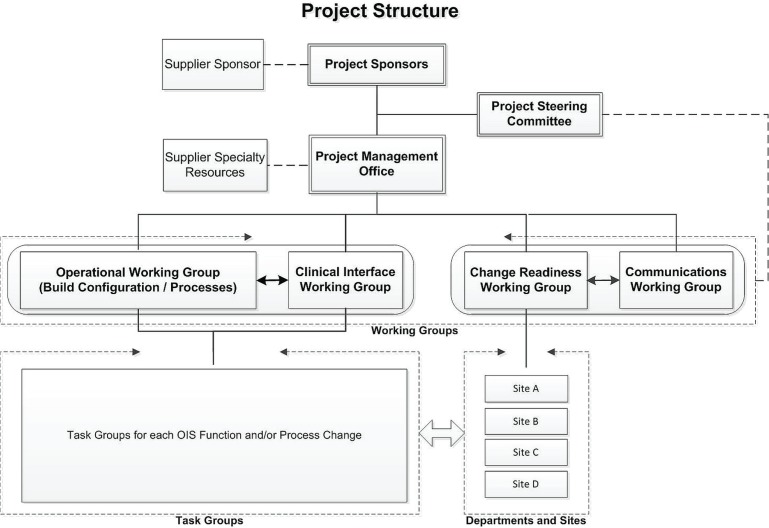
The server for the new cancer centre at site B was located at site A. An algorithm was created to describe the escalation process and steps to address system problems when they occurred. Implementation of the rois at site B failed to occur smoothly: it was characterized by multiple system crashes, physician and staff frustration with new work processes and increased time occupied with “computer work,” loss of clinical productivity, and resentment toward a system that was seen to be imposed from the outside. That experience led the leadership for the rois initiative to pause and reconsider how best to undertake the next steps in the implementation process and how to resolve the issues experienced at site B. Figure 1 illustrates the project structure used to guide the reboot of the rois.
FIGURE 1.
The revised project structure used to guide implementation of the regional oncology information system (ois).
Now, in the revised project structure, the project sponsors (the regional chief information officer and the head of the regional cancer program) have ultimate accountability for the project’s success. They co-chair the psc, which includes the clinical vice-presidents from the three other hospitals implementing the rois. The psc has provided oversight, strategic planning, and guidance to the project. Representation by senior leadership has also served to facilitate access to resources across the region when needed. The psc has maintained communication with the supplier on the status of implementation issues and has made the final decisions with regard to “Go Live” events. The project management office (pmo) and four working groups support the psc. The psc continues to meet monthly with the pmo team and the working group leads to receive updates about the status of their respective activities.
The pmo oversees all aspects of the project and supports the working groups in their decision-making and communication across the four sites. The pmo is the primary conduit for reports to the psc from the working groups. The pmo also maintains and updates the master project plan, ensures sign-off by the “most responsible person” and appropriate documentation of decisions and processes, and establishes protocols for issues management, risk management, change management, and communications.
The supplier supports the project tasks, timelines, and accountabilities through discussion with the pmo. The supplier’s resources have included expertise in it and information systems application functionality and in clinical process redesign. The supplier’s experiences with installations at other sites in the province, nationally, and internationally were shared and used, as needed, to help support system configuration, workflow processes, and decision-making.
Table ii outlines the major working groups and their roles in the implementation process.
TABLE II.
The project working groups and their roles in the implementation process
| Key working groupsa | Rolesb |
|---|---|
| Operations working group (owg) | Ensure that the regional oncology information system (rois) is built and configured to specifications before Go Live events. Ensure that process changes reflect clinic and administrative requirements. Recommend nature, type, order, and sequencing of incremental Go Live events. Oversee multidisciplinary task groups to ensure sign-off on agreed decisions. |
| Clinical Interface working group (ciwg) | Represent all areas of clinical activity. Ensure that the rois can be successfully adopted for use at all sites. Engage clinical leaders and communicate issues and decisions across clinical teams at all sites. Provide input to all clinical components of the system build and design, including readiness for Go Live events. |
| Change Readiness working group (crwg) | Ensure that each site and functional area is prepared to adopt and implement the Go Live elements of the rois. Provide guidance to sites and managers to prepare staff for Go Live events. Plan for change events. Develop change-readiness templates and materials. Use surveys, formal and informal interviews, liaison with key clinical and “super-users” to assess site readiness for Go Live events. |
| Communications working group (cwg) | Develop and implement a communications plan for all point-of-service staff to ensure their awareness of the changes about to occur and the potential effects. Develop needs assessment tools. Develop a communications toolkit for information-sharing to all levels of each organization. Organize celebratory events. |
| Task groups (multidisciplinary teams that report to owg and ciwg) | Work on specific aspects of the rois configuration or workflow processes. Provide recommendations to the owg and ciwg for ratification. |
Provide oversight and facilitate decision-making for the system build and configuration.
Working group lead accountable through the Project Management Office to the Project Steering Committee.
Just as the Operational and Clinical Interface working groups have to work closely together, so too do the Change Readiness and Communications working groups, because communication and management of this major change are critical to a successful implementation.
Because cancer care is delivered through functional departments at each location, it is essential that directors, managers, and supervisors are sufficiently prepared for Go Live events. Change readiness assessments are prepared periodically, and department and site managers are accountable for ensuring that their teams are prepared for the Go Live events, including process changes and development of policies and procedures.
3. ROIS IMPLEMENTATION
3.1. Challenges and Lessons Learned
The rois implementation is still a work in progress. It has had successes, but the project has also had its share of challenges and lessons learned. A regional implementation project involving four institutions and the replacement of two legacy systems, with upgrades to an existing system, is a very significant undertaking, but the magnitude was not fully understood by many of the stakeholders.
Although the radiation oncology program at site A successfully completed a major upgrade without incident, their experience might have made the implementation team overconfident about the project’s subsequent implementation activities. This initial phase of the project succeeded because a small group of clinical and administrative staff were pre-selected as “super users” to create a detailed upgrade plan, with the supplier contributing recommendations and substantial resources. In addition, a central project team worked with a small group of clinical staff to create a checklist of required tasks. During the Go Live event, members of both the clinical and the administrative staff were present over a weekend for final education and testing of the clinical system before the system was switched on. Information technology resources were available from the supplier, both on site and remotely, to assist the weekend turnover. During the first 2 weeks of the upgrade, super users and supplier resources both provided additional on-site and remote support as required. A key lesson learned from that experience was that a committed, engaged, and accountable multidisciplinary team, combined with supplier resources, can achieve positive results.
The radiation oncology upgrade was a relatively small component of the much larger rois implementation plan. The need for a common rois had been widely embraced, including these key elements for success:
Establishing the need for change
Establishing physician leadership and engagement in the change process
Revising work processes to optimize use of the ois
Identifying all education and resource needs required for implementation
Establishing appropriate interfaces to other hospital and regional systems to better integrate patient care
Despite acknowledging those critical success factors, numerous missteps occurred.
3.2. Establishing the Need for Change
The literature on change management clearly defines the need for a “burning platform” for change and effective communication of that need for change to all stakeholders11. The time required to identify and choose the most appropriate ois, to assess the effects on workflow processes, to purchase and implement the new system, to learn the system, and to integrate it into practice cannot be understated. A lack of participation in the decision-making process for the proposed system change can contribute to change resistance. Inadequate communication about why the organization has chosen to adopt a new information system and about the potential benefits can result in a lack of commitment to the change process, which can, in turn, result in a lack of commitment to new work processes. The fallout can be poor data entry, increased time spent problem-solving and communicating solutions, and challenges in accessing and reporting data12.
Communicating the “burning platform” to employees at multiple facilities is challenging. Although the administrative leadership was fully committed to the vision of a larger integrated cancer system, the clinical leadership had competing perspectives, including a strong emotional loyalty to their host institution with its embedded processes and culture. The point-of-care staff showed much good will at the start of the project, but little knowledge of, or relationship with, their counterparts at the other institutions. Relationships are important. More work could have been done to ensure better communication and opportunities for successful collaboration, including getting to know one another’s work environments, so that, as problems emerged, the focus would be on joint problem-solving. Decisions to freeze it initiatives to support the site B move created a “burning platform,” but one with insufficient time for key initiatives such as data clean-up in the legacy system.
3.3. Establishing Physician Leadership and Engagement in the Change Process
Change in physician behaviour and shifts in culture have been extensively studied. Lack of change readiness occurs largely because experienced physicians and other health care workers have entrenched working styles and routines that suit their personal practice styles. Practitioners also develop workarounds based on the real or perceived deficiencies of a new process or electronic system, and such practices can be difficult to eradicate.
The value proposition of an ois change has to emphasize efficiencies and better patient outcomes; however, physicians and other staff must make a material and human resource investment, and the benefits of adopting innovative technologies must be seen to outweigh the work and costs of implementation. If either or both of the change process and technology are difficult to learn, adoption will likely be difficult. Enabling factors such as intuitive user interfaces, communication of a clear understanding of how work processes will change, and provision of education and training in the new work processes are essential. Reinforcing a culture of continuous learning can also significantly improve success. Physicians are busy professionals. Learning how to use new technologies requires a significant time investment, and if an understanding of the value of the technology and its potential positive return on the investment of that time is not communicated, uptake can be negatively affected. Benefits such as less time, efficient access to test results, availability of information resources, and improved quality of patient care can be strong motivators. Recognition by peers and improvement in billing practice are also factors that can contribute to adoption in some settings. Similar arguments can be made for other clinical providers and for clerical and management staff. To facilitate uptake and optimal use, each group has to be comfortable with the new rois.
Negative attitudes toward the replacement of an existing system, with changes in work processes, have been reported to be particularly common among physicians who are unfamiliar with it and computer environments. Those individuals require leadership, champions, practical education, follow-on support, and ongoing encouragement to adopt the change13.
Manager and supervisor commitment to review, develop, and sign-off on new policies and procedures facilitates success. Establishing clear lines of accountability for leaders of task groups and working groups is also important for the success of any rois implementation project.
3.4. Revising Work Processes to Optimize Use of the ROIS
The rois project involved significant evaluation of current processes and proposed future requirements. The time required to review and assess workflow, to choose appropriate programs, to implement and learn how to use the software, to enter current and past patient data, to scan relevant images, and to learn how to access information all disrupted “normal” workflow. The care providers, it staff, and information systems supplier had to jointly consider how work would be done in the future to take best advantage of the software for care delivery and patient safety. That discussion should have been the catalyst for change within the organization. Unfortunately, relatively less work was invested in process re-engineering for the rois, and that work was not performed collaboratively with all sites. Site A took the lead on process redesign because site B had less capacity. Sites C and D participated in the process review and redesign of work processes, but as a result of limited time and resources, requested to be left out of the larger implementation process until closer to their Go Live dates. The result was that site B did not feel ownership of the new work-process maps. When the new software was implemented, some of the site B personnel continued to work as though their work processes had not changed, or they worked around the new software’s perceived inadequacies, which negatively affected overall adoption of the new system.
Furthermore, converting from a paper-based medical record (with some level of electronic record use) to “paperless” (or near-paperless) delivery can be tremendously challenging. With paper systems, adjustments to care plans or practice notes can be made easily; by contrast, accessing a computer and entering data online was challenging for some users. In addition, not everyone who was expected to work with the rois had the same level of computer or keyboarding skills. Moreover, a paper-based system can have inherent prompts for the steps that are to follow, which might no longer exist in an electronic environment. Thus, if the OIS workflow does not include the prompts with which providers are familiar, confusion may result, and the system users might not know which action or actions are to follow, even if the OIS includes other prompts to alert actions.
Introduction of the rois into a paper environment, and “mixed environments” that combine both electronic and paper systems, required that old health records (or selected key data elements) and some current documentation be scanned so that the current patient record would be complete. Scanning processes are labour- and time-intensive and might have resulted in unnecessary materials being scanned. It is essential to create policies and procedures that specify the documents that have to be scanned and to provide sufficient resources for the work. The project’s leadership determined that it was not essential that all historical patient records be scanned, but that selected patients (those currently on active treatment, for example) have a core set of clinical information scanned, particularly if there was a need to transfer information between provider sites. Nevertheless, information in scanned format cannot be easily retrieved using electronic search strategies, a circumstance that makes it vital that standards be created for what is to be scanned and where the scanned documents are to be consistently maintained within the electronic record.
3.5. Identifying Education and Resource Needs to Support Implementation
The early stage of a new information system implementation process generally requires substantial resources for education in activities such as how to log into the system and how to type, scan, enter, and transfer data; otherwise, acceptance can be in jeopardy. Table iii summarizes the relevant education and other resource needs.
TABLE III.
Education and other resources needed during the early stages of implementing a new information system
| Need | Required support | Key elements |
|---|---|---|
| Login Data entry |
Training sessions tailored to the specific needs of each professional group | Must use standardized methodology and format across all locations Training should be standardized based on workflow processes so that trainer-based fluctuations can be controlled |
| Work processes | Process maps and education sessions for each professional group | Each professional has to understand their personal role—and those of others—in relation to orders, data entry, edit, and correction processes |
| Practice system for individual training and for interprofessional process simulation | A fully functional practice system for use well before “Go Live,” for training, education, and practice purposes | Regular reset of training system to allow for practice with data elements (for example, lab results for management) Realistic simulation of work processes that can manage data in a “learning laboratory” |
| Assessment of user readiness | Surveys, polls, and direct and indirect feedback with key user representatives and “super-users” to regularly assess the level of acceptance of the new system by the various user groups | Use of “traffic light” indicators to assess readiness of users and to focus training efforts with respect to the nature, type, and effort of training required for key groups |
| Supplier-based best-practice options | A test system based on initial site reviews and process re-engineering expertise that key users can work with to refine needs Refinements to the initial test system to meet regional requirements |
Gain acceptance of key users for standardized protocols and work processes Disseminate best-practice learnings from other sites globally to for local use |
| Key internal resource development | Cooperation with the vendor to achieve full competency training for members of the key resource team who will be responsible for system maintenance and who will participate in ongoing system development | Create a multidisciplinary group of users from across all locations Determine the key resources—both technical (Information Technology) and developmental (reports, information flow)—to be trained |
A key learning was that software applications can be customized to meet needs, but that standardized, consistent education of end users is essential. The supplier’s education staff often presented too many different techniques for accomplishing the same end, which ultimately confused clinicians and staff and undermined confidence in the quality of the processes and data that would be captured.
An extensive evaluation process, including a staff survey, was undertaken with staff at sites A, C, and D to improve upon the user experience encountered at site B. The survey was pilot-tested with a group of key interdisciplinary people. It was then distributed to all staff. An overall response rate of 45% was achieved. To ensure that staff were more comfortable with the changes being implemented, key learnings (highlighted in Table iv) were used to focus the training and process change tasks.
TABLE IV.
Key findings from the staff survey about the new regional oncology information system (rois) implementation
| Finding | Comments |
|---|---|
| Perceptions | |
| Potential increase in workload with new rois | Nurses, followed by physicians, were significantly more likely than other professional staff to believe that the rois implementation would increase workload. |
| Documentation for care improved | Nurses were significantly more likely than physicians and others to believe that the new rois functionality would improve how care was documented. |
| Improvements in efficiency with rois | Fewer than half the respondents (44%) believed that the rois would not improve their efficiency, but more than 50% indicated that the rois was an essential part of improving efficiency. |
| Identified needs | |
| Training a key requirement | Training was customized to each user group and presented in modules. |
| Group training was identified as the preferred model, with one-on-one second and self-study third. | |
| Cheat sheets and process maps | Resources were developed as part of the training program. |
| A personalized “passport” for training, developed for each user type, highlighted the key learning requirements and provided “test” samples to gauge competency with the modules. | |
| Access to computers | Migration from paper charts necessitated a significant increase in the number of devices available within the clinics and elsewhere to ensure that all appropriate staff could access the rois as required without delay. |
| Expert users | Cadres of “super-users” were developed to facilitate training and to act as reference staff during implementation. The super-users were drawn from clinical and nonclinical areas at all four sites. |
| Keyboarding skills | Simple Web-based keyboarding practice tools were provided to all staff who felt that their keyboarding skills were not up to par, a feeling that was both a psychological impediment to implementation and a practical one as older staff struggle with computerized technology. |
| Practice time outside of work hours | All staff were actively encouraged to practice their new skills on the training system outside of their work hours. |
| Computer response time | The amount of information available within the rois (20+ years of patient history) meant that processing time lags of 5–10 seconds occurred in some transactions. |
3.6. Establishing Interfaces with Other Information Systems
The goal of integration of the rois with other hiss required consideration of how best to harmonize processes, data, and reporting. The key steps to achieving that goal included
developing a vision for the integration of the information systems.
fully documenting the systems that would be required for post-implementation integration.
ensuring the presence of it staff experienced with each system for which an interface would be required.
harmonizing data transmission protocols.
performing system-wide, integrated testing.
ensuring communication and collaboration by it resources across all sites.
performing intensive data mapping.
creating operational reports to share across sites.
redesigning processes so that the interfaces supported clinical activity.
Given the four separate his installations, significant complications arose with respect to a “complete” integration approach with the rois. The definition of the “source of truth” for validation of patients across the separate systems proved daunting. Further, the costs of purchasing the generic interfaces from the his suppliers across the four sites, and the costs to customize and maintain them were large. In the end, it was determined that the prime goal was to ensure that the admission, discharge, and transfer his would send information unidirectionally to the rois to keep it current.
Many system slowdowns and “crashes” occurred because of interactions with other software applications such as antiviral software. Those occurrences underscored the need for better communication between it departments with regard to any system changes that might affect the region-wide system. Also, the region-wide configuration was handled by a central group, which (it was learned over time) had not been provided with complete information about all the systems operating at the various sites. Furthermore, no mechanism existed to standardize the policies and processes for system configuration and implementation across the region. The lack of such a mechanism was not an rois issue, but became one because of the interaction of the rois with all the hiss.
The complexity of an implementation increases when interfaces are required across multiple sites with standalone technologies and with disparate policies on data ownership, privacy, and confidentiality (such as who is responsible for releasing information to a patient or to a provider). The need for a higher level of coordination between the it departments of the region’s hospitals was a catalyst for the creation of a regional ois group to work collaboratively on resolving many of the interface and system standardization issues.
4. CONCLUSIONS
The implementation of a new institutional information system is challenging at the best of times, but implementation on a region-wide basis brings new challenges. Strong leadership is required to articulate a clear vision and the need for major change. Active participation by all key leaders who will be affected by the change ensures adequate input to, and ownership of, the work processes necessary to achieve the desired project results. To facilitate commitment to an implementation that will ultimately affect the future work they will do and how they will do it, the need for change must be clearly and repeatedly communicated to all front-line staff. A plan for the overall implementation process and its subcomponents must be communicated in an understandable form to the relevant constituencies.
All institutions have their own cultures and ways of doing business, which can be challenging when it is essential that they standardize their work processes to a single approach. Senior executives from each participating institution must jointly steer the process and commit to a standardized approach. Clinical and point-of-care staff from all partner organizations must also participate in developing the new standard work-process maps, because the system will be configured according to those maps, and education must be standardized to the new work processes. In this respect, strong support from the supplier, working in a close partnership with the clients both in the education of users and in informing the client about best practices from prior implementations, can help to ensure the overall success of a multi-site ois implementation.
5. CONFLICT OF INTEREST DISCLOSURES
WKE is the former ceo of the regional cancer program and has no financial conflicts of interest. AS is the former project director of the rois, hired by the regional cancer program. FDA and JP are consultants contracted by the ois supplier and regional cancer program to evaluate implementation of the rois. GLH is the former general manager and senior vice-president, Elekta, supplier of the ois; he also owns stock in Elekta.
6. REFERENCES
- 1.Ashbury FD, Madlensky L, Raich P, et al. Antidepressant prescribing in community cancer care. Supportive Care Cancer. 2003;11:278–85. doi: 10.1007/s00520-003-0446-8. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW. Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–6. doi: 10.1007/s11606-010-1252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kralj B, Iverson DC, Hotz K, Ashbury FD. The impact of computerized clinical reminders on physician prescribing behavior. Am J Med Qual. 2003;18:197–203. doi: 10.1177/106286060301800504. [DOI] [PubMed] [Google Scholar]
- 4.Deutscher D, Hart DL, Dickstein R, Horn SD, Gutvirtz M. Implementing an integrated electronic outcomes and electronic health record process to create a foundation for clinical practice improvement. Phys Ther. 2008;88:270–85. doi: 10.2522/ptj.20060280. [DOI] [PubMed] [Google Scholar]
- 5.Kanas G, Morimoto L, Mowat F, O’Malley C, Fryzek J, Nordyke R. Use of electronic medical records in oncology outcomes research. Clinicoecon Outcomes Res. 2010;2:1–14. doi: 10.2147/CEOR.S8411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klumpp TR. Electronic medical records and quality of cancer care. Curr Oncol Rep. 2013;15:588–94. doi: 10.1007/s11912-013-0347-z. [DOI] [PubMed] [Google Scholar]
- 7.Dick RS, Steen EB, Dether DE, editors. The Computer-Based Patient Record: An Essential Technology for Health Care. 2nd ed. Washington DC: The National Academies Press; 1997. [PubMed] [Google Scholar]
- 8.Fletcher RD, Dayhoff RE, Wu CM, Graves A, Jones RE. Computerized medical records in the Department of Veterans Affairs. Cancer. 2001;91(suppl):1603–6. doi: 10.1002/1097-0142(20010415)91:8+<1603::AID-CNCR1173>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 9.Englebardt SP, Nelson R. Health Care Informatics: An Interdisciplinary Approach. St. Louis, MO: Mosby; 2001. [Google Scholar]
- 10.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings and costs. Health Aff (Millwood) 2005;24:1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 11.Kotter JP. Leading change: why transformation efforts fail. Harv Bus Rev. 2007:123–31. [Google Scholar]
- 12.Lai JK, Lau F, Shaw N. A study of information technology use and implementation of electronic medical record systems in BC medical practices. B C Med J. 2009;51:114–21. [Google Scholar]
- 13.Terry AL, Thorpe CF, Giles G, et al. Implementing electronic health records: key factors in primary care. Can Fam Physician. 2008;54:730–6. [PMC free article] [PubMed] [Google Scholar]