ABSTRACT
Purpose
The primary healthcare setting is well placed for health screening. Tear fluid composition gives valuable information about the eye and systemic health, and there is now significant interest in the potential application of tears as a tool for health screening; however, the acceptability of tear collection in the primary healthcare setting as compared with other methods of human sample collection has not been previously addressed. The objective of this study was to evaluate the patient acceptability of tear collection in a primary healthcare setting.
Methods
This was a cross-sectional study on 383 adult patients seeking primary healthcare, who were not diabetic and were not attending for an eye-related complaint. Tear collection was done using Schirmer strips, and an interviewer-administered questionnaire was conducted to collate information on the pain score (0–10) of the Schirmer tear collection, as well as to score the pain associated with their previous experience of antecubital venous puncture and finger prick test.
Results
The pain score for Schirmer tear collection was significantly lower (p < 0.001) than antecubital venous puncture but higher (p < 0.001) than finger prick. The pain scores for all three procedures were significantly higher in participants of younger age, female gender, and higher education level. Among the participants, 70% did not mind their tears being collected to screen for eye problems, whereas only 38% did not mind this procedure being performed for general health screening. Nevertheless, 69% of the participants preferred tear to urine collection, and 74% of participants preferred tear to blood collection.
Conclusions
Tear collection using Schirmer strips is a highly acceptable form of investigation that has the potential for use in health screening in the primary healthcare setting. This study has implications on using tear collection as a method of ocular and systemic health screening in the primary healthcare setting.
Key Words: tear collection, eye, screening, outpatients, patient acceptance of healthcare, clinical study
Tear fluid is an extremely complex biological mixture containing proteins and peptides, electrolytes, lipids, and small molecule metabolites. New technologies, especially biological mass spectrometry, are dramatically influencing advances in tear analysis using large-scale, high-throughput, untargeted approaches, including proteomics, metabolomics, and lipidomics.1 Office-based devices such as the Agilent Bioanalyser2 can help in clinic diagnosis by quantifying major tear proteins. A rapid in-office kit that is patient administered is also available for tear proteins such as matrix metalloproteinase 9.3
The health status of the ocular surface and conditions of the lacrimal functional unit are reflected in the composition and quality of tear components. Tear collection can be useful in understanding eye conditions such as dry eye syndrome,4 Sjogren’s syndrome,5 microbial infections,6 allergic eye diseases,7 and blepharitis.8 For example, lacritin is one of a handful of tear proteins preliminarily reported to be downregulated in blepharitis and in two dry eye syndromes.9 Systemic diseases in which changes in tear proteins have been detected include diabetes mellitus and thyroid eye disease. In fact, tear proteomic pattern has also been linked to cancer, particularly breast cancer.10–12
Diabetes mellitus is a systemic disease which can be associated with eye complications and blindness. In patients with proliferative diabetic retinopathy, changes in major tear proteins found include a decrease in tear-specific pre-albumin as well as an increase in lysozyme,13 while autonomic nerve function has been shown to be impaired.14 Apolipoprotein AI concentrations in tears are significantly higher in patients with diabetes mellitus with retinopathy than those without.15 Also, levels of nerve growth factor (NGF) in both serum and tears were higher in proliferative diabetic retinopathy patients than in nonproliferative diabetic retinopathy patients and controls.16 Glycemic control can also be tracked with tear examination.17,18
Thyroid eye disease, also known as Graves’ ophthalmopathy, is a characteristic feature of Graves’ disease. It is associated with enlargement of lacrimal gland19 and ocular surface diseases such as dry eye.20 A raised tear IgA-to-lysozyme ratio was seen in patients with thyroid eye disease,21 which suggested the involvement of the lacrimal gland. This involvement occurred more often in patients with a long history of the disease. The levels of zinc-alpha2-glycoprotein and lactoferrin were increased in tears in patients with thyroid eye disease.22 The levels of NGF were also higher in patients with thyroid eye disease than in controls and significantly decreased after 2 to 4 weeks of steroid treatment.23
The Schirmer test is a popular method of collecting tear from humans. It is easily performed and is routinely used in the ophthalmology clinic as a standard clinical test, and can also be made available to primary care clinics. Another method of tear collection uses the glass capillary tube.24 Other less popular tear collection methods using absorbent materials or eye wash (eye flush) can also be used as alternative tear collection methods.
The reported protein concentration in tears has been found to vary between studies (between 6 and 11 mg/mL),25 and this is hypothesized to be a result of different tear collection methods, the type of tears collected (i.e., nonstimulated versus reflex tears), and the protein assay method (Bradford or Lowry method). Schirmer strips tend to collect some cellular proteins which may come from epithelial cells from the corneal and conjunctival epithelium.24,26,27 Tear collection methods which cause ocular stimulation, for example the Schirmer test, can cause an increase in the levels of glucose in the collected tear sample.17 Sample processing could also introduce variability in sample composition of tear proteins collected with Schirmer strips.28
Tear collection using a glass capillary tube may be difficult for some patients without using a flush method. Also, it does not measure tear function simultaneously like the Schirmer test. Primary healthcare workers not accustomed to research may also be more wary about inserting a pointed object on the eye. Appropriate storage of tear sample is also an important consideration in the healthcare setting, as total protein concentration can be reduced significantly if samples are not stored under suitable conditions.29
Unlike urine collection, Schirmer tear collection can be carried out in a consult room, and unlike blood collection, it does not require universal precautions for the healthcare personnel administering the test and does not pose a risk of bruising or hematoma to the patient, which occur in about 12.3% of venous punctures.30 Tear collection also does not require specially trained healthcare personnel such as phlebotomists to administer. Despite these advantages of tear collection, there has not been any evaluation of its acceptability to patients as a form of primary health screening.
We chose to use Schirmer test in this study to collect tears because it is a commonly available technique that has been used in many tear protein studies.1 The advantages of the Schirmer test are that it is relatively convenient, easy to interpret, and tears from both eyes can be collected simultaneously. The Schirmer test is also by far the more pleasant method compared to the glass capillary tube method, which requires constant, well-practiced, and prolonged work on the open eye.31 It is also fairly cheap involving only the cost of the Schirmer strip.
The objective of this study was to investigate the acceptability toward tear collection using Schirmer test in primary healthcare adult patients.
METHODS
We conducted a cross-sectional study between November 2009 and March 2010 in Outram Polyclinic. A total of 383 participants completed an interviewer-administered questionnaire for this study. They were chosen by convenience sampling from a group of 1000 patients from whom tears were collected for the purpose of establishing a reference sample of human tear for tear proteomics profiling. All participants were adults above 21 years of age, did not have diabetes mellitus, were not attending for an eye-related complaint, and had given written informed consent. These participants were patients attending Outram Polyclinic, a primary healthcare clinic located centrally in Singapore. SingHealth Polyclinics is a group of nine primary healthcare polyclinics, including Outram Polyclinic, which saw 1.74 million patients in the year 2012.
A standard questionnaire was interviewer administered, in English, by a single interviewer, after the Schirmer tear collection. The questionnaire included sections on demographics, background medical history, eye medical history, pain score, and acceptability of tear collection. Pain score was graded on a scale of 0 to 10, with 0 indicating no pain and 10 the worst pain that one can experience. Pain scores recorded were based on the Schirmer tear collection done at that setting, as well as the participant’s previous experience with antecubital venous puncture and finger prick test. The questionnaire is available online as an Appendix, at http://links.lww.com/OPX/A158.
Tear collection was performed in each eye using Schirmer strips by the trial coordinator. During the Schirmer test collection, SNO strips (Bausch + Lomb, Montpellier, France) were folded along the notch and carefully placed in the lower fornix of each eyelid, between the middle and outer third of the eyelid. The participants were instructed to gently close the eyelids during the 5 minutes and the strips’ positions adjusted if there should be irritation felt.
The hypothesis was that the pain score from tear collection would be lower than the pain score from antecubital venous puncture. Considering a mean pain score of 1.98 (SD = 1.2) for the antecubital venous puncture in our database of 383 patients, a difference as small as 0.2 could be shown with 80% power and a type I error of 0.05.
For statistical analysis, as the pain scores were skewed, nonparametric tests were performed when appropriate. Firstly, the comparisons of antecubital venous puncture and finger prick test with the pain scores of Schirmer tear collection were analyzed using the Wilcoxon signed-rank test. Secondly, the association between pain score and each of its potential factors was studied. In the univariate analysis, the association was tested using Mann-Whitney for the two-group variables, Kruskal-Wallis for the variables with more than two groups, and Spearman correlation for the continuous variables. Then multivariate analysis using linear regressions where the pain was log-transformed was run. The associations between the questions regarding acceptability of tear collection with its factors were tested using chi-square test. In this analysis, all variables were treated as categorical variables including age (age below 50 years vs. age 50 years and above). Statistical analysis was performed using Statistical Package for the Social Sciences version 15. All statistical tests were two sided with significance level of 0.05.
This study was approved by the SingHealth Centralised Institutional Review Board and adhered to the tenets of the Declaration of Helsinki in human research.
RESULTS
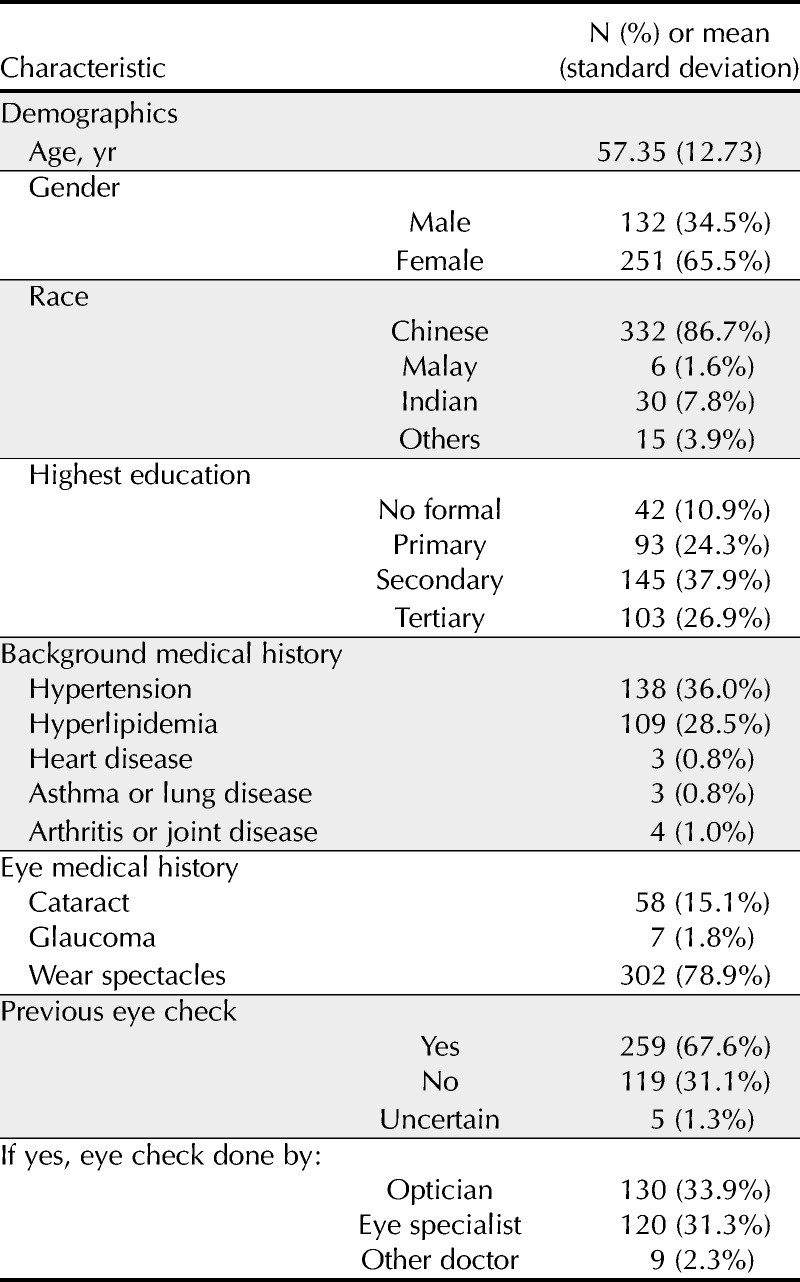
Sociodemographics and clinical characteristics of study participants are presented in Table 1. The study involved 383 patients, including 132 males and 251 females, with a mean age of 57.35 years (age range 21–92 years, standard deviation 12.73). Majority of the participants were Chinese at 86.7%, while Malays accounted for 1.6%, Indians 7.8%, and other races 3.9%. This reflects more or less the ethnic composition of Singapore except for a slight under-representation of Malays. In terms of education, 10.9% of the participants had no formal education, 24.3% had primary education, 37.9% had secondary education, and 26.9% had tertiary education. The background medical conditions of the participants include hypertension in 36.0%, hyperlipidemia in 28.5%, heart disease in 0.8%, asthma or lung disease in 0.8%, and arthritis or joint disease in 1.0%. As for eye medical conditions, 15.1% of the participants had a history of cataract, 1.8% had glaucoma, and 78.9% wore spectacles. Moreover, 67.6% of participants had had a previous eye check conducted, and among these, 33.9% had the check by an optician, 31.3% by an eye specialist, and 2.3% by other doctors.
TABLE 1.
Sociodemographic and clinical characteristics of study participants (N = 383)
The pain scores of the Schirmer tear collection, antecubital venous puncture, and finger prick test are compared in Fig. 1. The median pain score for Schirmer tear collection was 1 (interquartile range 0–2), 2 (interquartile range 1–3) for antecubital venous puncture, and 1 (interquartile range 0–1) for finger prick test. The pain score for Schirmer tear collection was significantly lower than that of an antecubital venous puncture (p < 0.001), while significantly higher than that of the finger prick test (p < 0.001).
FIGURE 1.
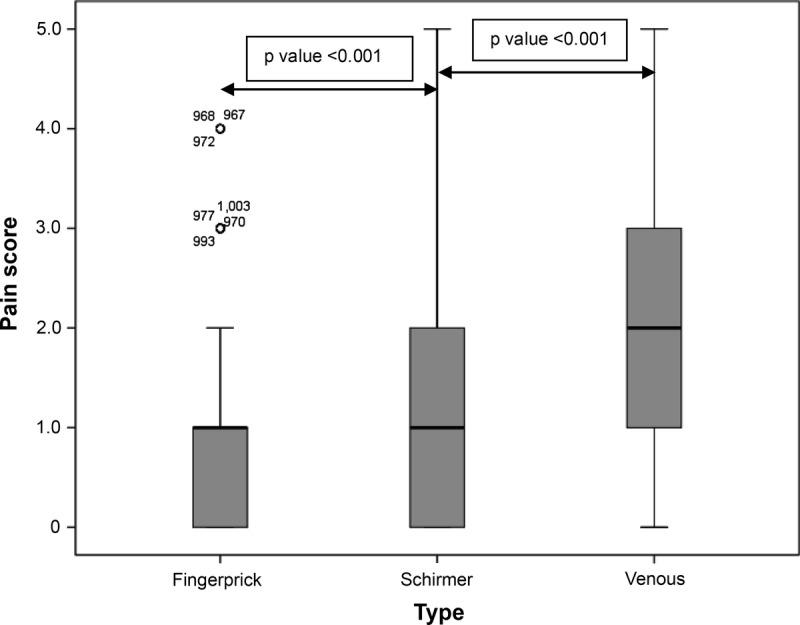
Boxplot of the pain scores for finger prick test, Schirmer tear collection, and antecubital venous puncture.
Factors affecting pain scores are presented in Table 2. For Schirmer tear collection, younger age was associated with an increased pain scores (p = 0.009). When stratified by gender, the pain scores for Schirmer tear collection for females was significantly higher than males (p = 0.014). Also when stratified by education level, the pain scores of Schirmer tear collection were significantly higher for better-educated participants (p = 0.002).
TABLE 2.
Factors affecting pain score
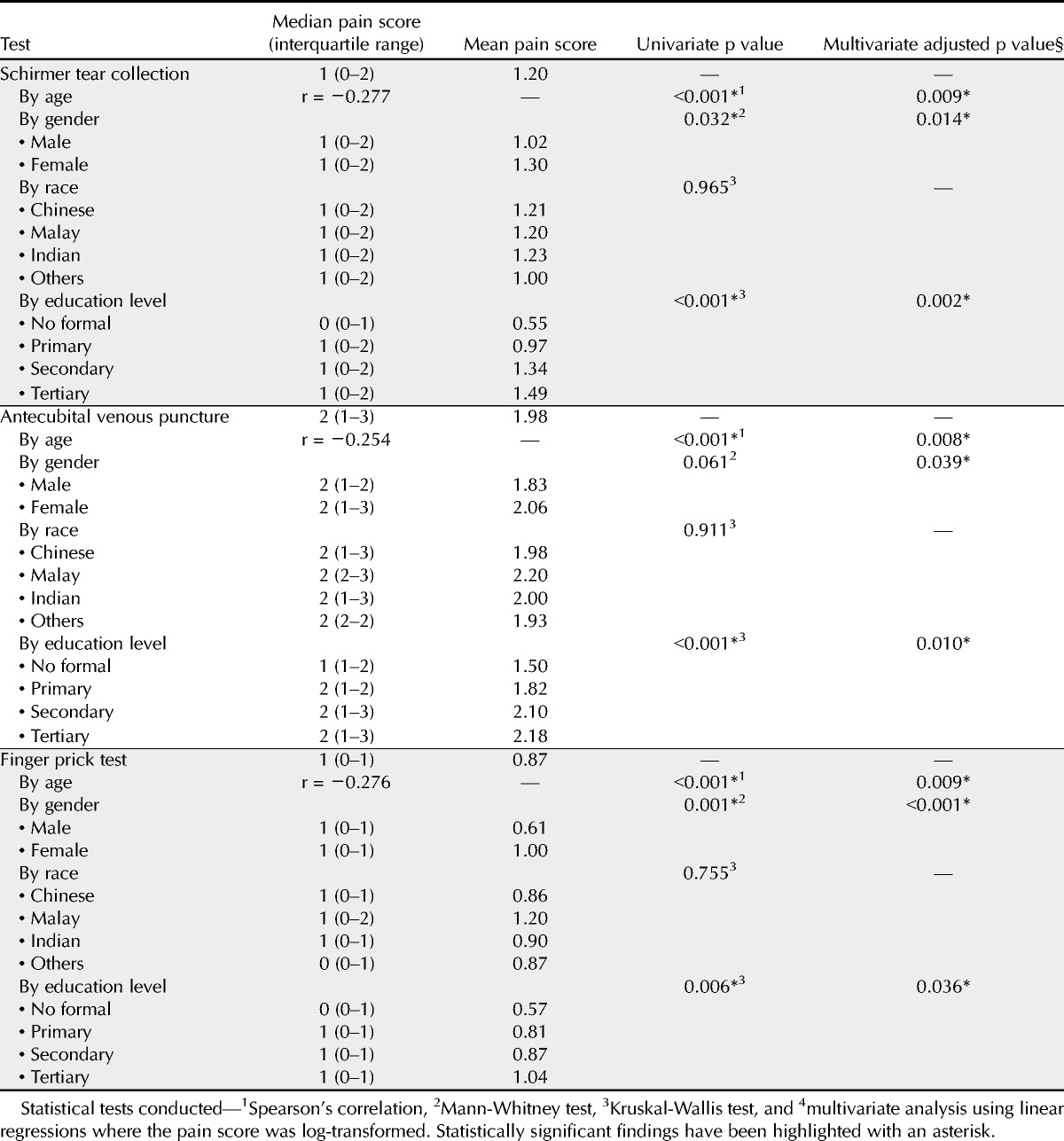
Similarly for antecubital venous puncture, younger age was associated with increased pain score (p = 0.008). When stratified by gender, the pain scores of antecubital venous puncture for females was significantly higher than males (p = 0.039). Also when stratified by education level, the pain scores of antecubital venous puncture were significantly higher for better-educated participants (p = 0.010).
For finger prick test, younger age was associated with increased pain scores (p = 0.009). When stratified by gender, the pain score of finger prick test for females was significantly higher than males (p < 0.001). Also when stratified by education level, the pain scores of finger prick test were significantly higher for better-educated participants (p = 0.036). For Schirmer tear collection, antecubital venous puncture, and finger prick test, there was no association of the pain score with race.
Acceptability of tear collection using Schirmer test is presented in Fig. 2A–D. The majority of participants (70%) agreed that they did not mind their tears being collected to screen for eye problems, whereas only 38% did not mind this procedure being performed for general health screening. Majority of the participants (69%) prefer tear collection to urine collection for health screening, as well as prefer tear collection to venous blood testing for health screening (74%). The acceptability of tear collection using Schirmer test from these four questions showed no significant association with age, gender, race, or education level.
FIGURE 2.
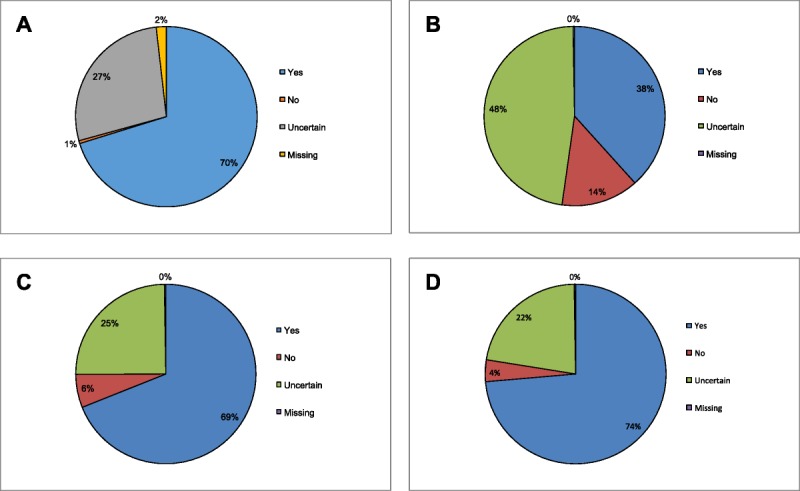
A, Responses to the question “Do you mind your tears being collected to screen for eye problems?” B, Responses to the question “Do you mind your tears being collected if it can detect other health problems?” C, Responses to the question “Would you prefer tear collection to urine collection for health screening?” D, Responses to the question “Would you prefer tear collection to venous blood testing for health screening?” A color version of this figure is available online at www.optvissci.com.
DISCUSSION
We have studied the acceptability of Tear collection using Schirmer strips and have found it to be highly acceptable with the potential for use in health screening in the primary healthcare setting. The discomfort of tear collection was between that of the finger prick and antecubital venous puncture. Also, most people prefer to have their tears collected instead of urine or blood, which are common investigations done in the primary care setting for health screening as well as monitoring of chronic medical conditions commonly managed including hypertension and diabetes mellitus. Schirmer tear collection (without anesthesia) in our study has been shown to have a higher pain score than the finger prick test. This is possibly because the Schirmer test can cause irritation when there is slight movement of the strip during the test, stimulating the nerves on the conjunctiva, thus causing some discomfort.
Tear collection has traditionally been used in the investigation of various eye conditions including dry eye. With newer technology and advanced knowledge of the composition of human tears and abnormalities in eye and systemic conditions, tear analysis has the potential to provide new knowledge through research. Proteomic composition of the tear film is a potentially rich and untapped reservoir of potential disease-specific protein biomarkers for emerging disease and diagnosis in clinical medicine.1,32
It is interesting that the pain score for Schirmer tear collection, antecubital venous puncture, and finger prick test was consistently higher in patients who were younger, female, and had higher education level. Other studies in the clinical setting have also shown that females report increased pain intensity compared to males.33 Better-educated individuals could also have a heightened awareness to pain. There is a decrease in the frequency and intensity of pain in adults of advanced age, but evidence has not determined whether the observed changes are caused by the aging process or reflect other age-associated effects, including an increased presence of comorbid disease, bioculture cohort effects, or altered psychosocial influences.34 Many diseases that can be screened for with tear analysis are common in elderly patients, and as the pain score in this group of patients is lower than younger patients as found in our study, the acceptability of the Schirmer test would be higher.
Strengths of this study include the uniformity of the data recorded, the prospective nature of the survey, and that a single research coordinator conducted both the tear collection and interview. Limitation of this study is that the sampling was by convenience sampling as compared to random sampling, which would have been more robust and less prone to bias. Another limitation is that the rating of pain was rated at the time of the procedure for the Schirmer test, and from memory for other tests including the finger prick and venous puncture. However, it would not have been ethical to include these tests in this study just to assess relative pain score for the various procedures.
Further studies could look into the cost effectiveness of using tear collection for screening and the reliability of screening for specific medical conditions including diabetes mellitus and thyroid conditions. Studies should also explore the acceptability of other methods of tear analysis using other methods such as microcapillary tubes.
In conclusion, tear collection using Schirmer strips is highly acceptable in the primary healthcare setting, and this study indicates a positive patient acceptance of using tear collection and analysis as a method.
Supplementary Material
Joanne Hui Min Quah
Outram Polyclinic, SingHealth Polyclinics
3 Second Hospital Avenue
Health Promotion Board Building, Level 2
Singapore 168937
Singapore
e-mail: joanne.quah.h.m@singhealth.com.sg
ACKNOWLEDGMENTS
This research is supported by the Singapore National Research Foundation under its clinician scientist award NMRC/CSA/013/2009 and administered by the Singapore Ministry of Health’s National Medical Research Council. This research is supported by the Singapore Ministry of Health’s National Medical Research Council under its Individual research grant NMRC/1206/2009 and center grant NMRC/CG/SERI/2010. The authors have no potential conflicts of interest to declare.
Appendix
The appendix, the study participant’s questionnaire, is available online at http://links.lww.com/OPX/A158.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.optvissci.com).
REFERENCES
- 1. Zhou L, Beuerman RW. Tear analysis in ocular surface diseases. Prog Retin Eye Res 2012; 31: 527– 50 [DOI] [PubMed] [Google Scholar]
- 2. Versura P, Bavelloni A, Blalock W, Fresina M, Campos EC. A rapid standardized quantitative microfluidic system approach for evaluating human tear proteins. Mol Vis 2012; 18: 2526– 37 [PMC free article] [PubMed] [Google Scholar]
- 3. Kaufman HE. The practical detection of mmp-9 diagnoses ocular surface disease and may help prevent its complications. Cornea 2013; 32: 211– 6 [DOI] [PubMed] [Google Scholar]
- 4. Grus FH, Podust VN, Bruns K, Lackner K, Fu S, Dalmasso EA, Wirthlin A, Pfeiffer N. SELDI-TOF-MS ProteinChip array profiling of tears from patients with dry eye. Invest Ophthalmol Vis Sci 2005; 46: 863– 76 [DOI] [PubMed] [Google Scholar]
- 5. Tomosugi N, Kitagawa K, Takahashi N, Sugai S, Ishikawa I. Diagnostic potential of tear proteomic patterns in Sjogren’s syndrome. J Proteome Res 2005; 4: 820– 5 [DOI] [PubMed] [Google Scholar]
- 6. Ananthi S, Chitra T, Bini R, Prajna NV, Lalitha P, Dharmalingam K. Comparative analysis of the tear protein profile in mycotic keratitis patients. Mol Vis 2008; 14: 500– 7 [PMC free article] [PubMed] [Google Scholar]
- 7. Nomura K, Takamura E. Tear IgE concentrations in allergic conjunctivitis. Eye (Lond) 1998; 12 (Pt. 2): 296– 8 [DOI] [PubMed] [Google Scholar]
- 8. Koo BS, Lee DY, Ha HS, Kim JC, Kim CW. Comparative analysis of the tear protein expression in blepharitis patients using two-dimensional electrophoresis. J Proteome Res 2005; 4: 719– 24 [DOI] [PubMed] [Google Scholar]
- 9. McKown RL, Wang N, Raab RW, Karnati R, Zhang Y, Williams PB, Laurie GW. Lacritin and other new proteins of the lacrimal functional unit. Exp Eye Res 2009; 88: 848– 58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lebrecht A, Boehm D, Schmidt M, Koelbl H, Schwirz RL, Grus FH. Diagnosis of breast cancer by tear proteomic pattern. Cancer Genomics Proteomics 2009; 6: 177– 82 [PubMed] [Google Scholar]
- 11. Bohm D, Keller K, Pieter J, Boehm N, Wolters D, Siggelkow W, Lebrecht A, Schmidt M, Kolbl H, Pfeiffer N, Grus FH. Comparison of tear protein levels in breast cancer patients and healthy controls using a de novo proteomic approach. Oncol Rep 2012; 28: 429– 38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Evans V, Vockler C, Friedlander M, Walsh B, Willcox MD. Lacryglobin in human tears, a potential marker for cancer. Clin Experiment Ophthalmol 2001; 29: 161– 3 [DOI] [PubMed] [Google Scholar]
- 13. Stolwijk TR, Kuizenga A, van Haeringen NJ, Kijlstra A, Oosterhuis JA, van Best JA. Analysis of tear fluid proteins in insulin-dependent diabetes mellitus. Acta Ophthalmol (Copenh) 1994; 72: 357– 62 [DOI] [PubMed] [Google Scholar]
- 14. Clark CV. Ocular autonomic nerve function in proliferative diabetic retinopathy. Eye (Lond) 1988; 2 (Pt. 1): 96– 101 [DOI] [PubMed] [Google Scholar]
- 15. Kawai S, Nakajima T, Hokari S, Komoda T, Kawai K. Apolipoprotein A-I concentration in tears in diabetic retinopathy. Ann Clin Biochem 2002; 39: 56– 61 [DOI] [PubMed] [Google Scholar]
- 16. Park KS, Kim SS, Kim JC, Kim HC, Im YS, Ahn CW, Lee HK. Serum and tear levels of nerve growth factor in diabetic retinopathy patients. Am J Ophthalmol 2008; 145: 432– 7 [DOI] [PubMed] [Google Scholar]
- 17. Baca JT, Finegold DN, Asher SA. Tear glucose analysis for the noninvasive detection and monitoring of diabetes mellitus. Ocul Surf 2007; 5: 280– 93 [DOI] [PubMed] [Google Scholar]
- 18. Chen L, Zhou L, Chan EC, Neo J, Beuerman RW. Characterization of the human tear metabolome by LC-MS/MS. J Proteome Res 2011; 10: 4876– 82 [DOI] [PubMed] [Google Scholar]
- 19. Chang TC, Huang KM, Chang TJ, Lin SL. Correlation of orbital computed tomography and antibodies in patients with hyperthyroid Graves’ disease. Clin Endocrinol (Oxf) 1990; 32: 551– 8 [DOI] [PubMed] [Google Scholar]
- 20. Versura P, Campos EC. The ocular surface in thyroid diseases. Curr Opin Allergy Clin Immunol 2010; 10: 486– 92 [DOI] [PubMed] [Google Scholar]
- 21. Khalil HA, De Keizer RJ, Bodelier VM, Kijlstra A. Secretory IgA and lysozyme in tears of patients with Graves’ ophthalmopathy. Doc Ophthalmol 1989; 72: 329– 34 [DOI] [PubMed] [Google Scholar]
- 22. Baker GR, Morton M, Rajapaska RS, Bullock M, Gullu S, Mazzi B, Ludgate M. Altered tear composition in smokers and patients with graves ophthalmopathy. Arch Ophthalmol 2006; 124: 1451– 6 [DOI] [PubMed] [Google Scholar]
- 23. Yoon JS, Choi SH, Lee JH, Lee SJ, Lee SY. Ocular surface inflammation, and nerve growth factor level in tears in active thyroid-associated ophthalmopathy. Graefes Arch Clin Exp Ophthalmol 2010; 248: 271– 6 [DOI] [PubMed] [Google Scholar]
- 24. Stuchell RN, Feldman JJ, Farris RL, Mandel ID. The effect of collection technique on tear composition. Invest Ophthalmol Vis Sci 1984; 25: 374– 7 [PubMed] [Google Scholar]
- 25. Ng V, Cho P, To C. Tear proteins of normal young Hong Kong Chinese. Graefes Arch Clin Exp Ophthalmol 2000; 238: 738– 45 [DOI] [PubMed] [Google Scholar]
- 26. Prause JU. Immunoelectrophoretic determination of tear fluid proteins collected by the Schirmer I test. Acta Ophthalmol (Copenh) 1979; 57: 959– 67 [DOI] [PubMed] [Google Scholar]
- 27. Green-Church KB, Nichols KK, Kleinholz NM, Zhang L, Nichols JJ. Investigation of the human tear film proteome using multiple proteomic approaches. Mol Vis 2008; 14: 456– 70 [PMC free article] [PubMed] [Google Scholar]
- 28. Denisin AK, Karns K, Herr AE. Post-collection processing of Schirmer strip-collected human tear fluid impacts protein content. Analyst 2012; 137: 5088– 96 [DOI] [PubMed] [Google Scholar]
- 29. Sitaramamma T, Shivaji S, Rao GN. Effect of storage on protein concentration of tear samples. Curr Eye Res 1998; 17: 1027– 35 [DOI] [PubMed] [Google Scholar]
- 30. Galena HJ. Complications occurring from diagnostic venipuncture. J Fam Pract 1992; 34: 582– 4 [PubMed] [Google Scholar]
- 31. Posa A, Brauer L, Schicht M, Garreis F, Beileke S, Paulsen F. Schirmer strip vs. capillary tube method: non-invasive methods of obtaining proteins from tear fluid. Ann Anat 2013; 195: 137– 42 [DOI] [PubMed] [Google Scholar]
- 32. Sariri R, Ghafoori H. Tear proteins in health, disease, and contact lens wear. Biochemistry (Mosc) 2008; 73: 381– 92 [DOI] [PubMed] [Google Scholar]
- 33. Ruau D, Liu LY, Clark JD, Angst MS, Butte AJ. Sex differences in reported pain across 11,000 patients captured in electronic medical records. J Pain 2012; 13: 228– 34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gibson SJ, Helme RD. Age-related differences in pain perception and report. Clin Geriatr Med 2001; 17: 433– 56 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


