Abstract
Purpose of review
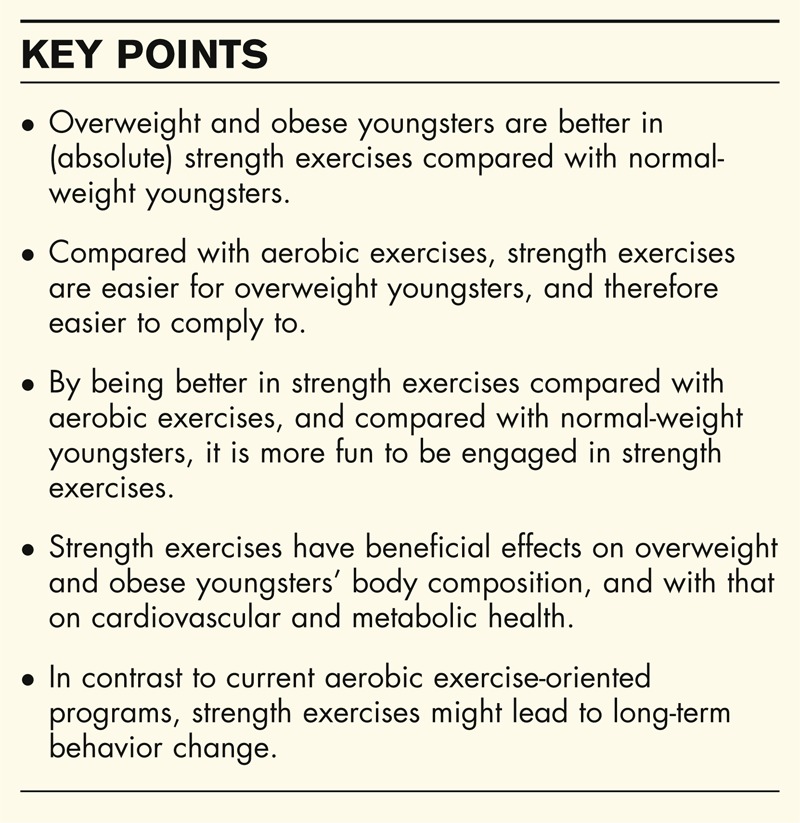
Optimizing the approach to combat childhood obesity, we emphasize the importance of combining both biological and psychological knowledge. In such an approach, strength exercises might be an important aspect in the treatment and prevention of childhood obesity.
Recent findings
Recent evidence indicates plausible effects of the role of resistance exercise in combating the negative health effects of childhood obesity. When looking at body composition, overweight youngsters do not only have a higher fat mass, but also a higher muscle mass compared with their normal-weight counterparts. With that, they are also stronger and better in exercises wherein the focus is on absolute strength, making them – under the right circumstances – more motivated to engage in resistance exercise and ultimately maintain a physically active lifestyle.
Summary
More and more children are obese, and obese children become obese adults. One reason that overweight youngsters are not physically active is that they are outperformed by normal-weight youngsters, and one reason they are overweight is because they are not physically active. To combat childhood obesity, strength exercise might be a solution to break the vicious cycle.
Keywords: body composition, childhood obesity, physical activity, resistance exercises, social comparison
INTRODUCTION
Nowadays, the news that the overweight and obesity prevalence is still rising [1,2] is not a revelation anymore. More and more children are obese, and obese children become obese adults [3,4]. The obesity ‘epidemic’ – and related noncommunicable diseases (NCDs) – are begging for action [5].
In the 2013 Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020 [6], a healthy diet and physical activity are recognized as factors that should be improved to reduce obesity and NCDs, especially in children. In the European Action Plan on Childhood Obesity 2014–2020 [7], the goal was stated to stop the rise in overweight and obesity in youngsters (0–18 years) by the year 2020 with, besides targeting nutrition, a greater focus on physical activity promotion. In this article, we focus on the physical activity aspect, and emphasize the importance of combining both biological and psychological knowledge.
Box 1.
no caption available
PHYSICAL ACTIVITY RECOMMENDATIONS AND OBESITY
For 5–17 year olds (in general), the World Health Organization recommends at least 60 min of moderate-to-vigorous-intensity physical activity per day, mostly aerobic [8]. Lee et al.[9] argue that health is affected substantially when those recommendations are not met. We believe that these guidelines are not effective enough for overweight and obese 5–17 year olds. We argue that when it comes to physical activity, we have to bear in mind that overweight and obese youngsters are not ‘general normal–weight’ youngsters and hence different guidelines will apply. First, although it is a commonly accepted fact that in the treatment of obesity the physical activity guidelines should be met, less than 20% of US adolescents meet those guidelines with even lower rates among obese 12–17 year olds [10]. Other studies also report that obese youngsters often have more difficulties in meeting the physical activity guidelines compared with normal-weight people [11,12]. Second, although the WHO recommendations state that the emphasis should be on aerobic exercises, overweight and obese are not only physically limited by their weight when it comes to the performance of aerobic exercises [13], but they also have higher risks of injuries with aerobic exercises [14]. Third, to stimulate overweight people to be more physically active, and for long-term compliance, it is important not to focus on what overweight youngsters have to do, but on what they like to do [15▪,16]. Humans have the tendency to compare their own abilities with others’ abilities to value themselves: social comparison [17▪▪]. With that, people gain in self-worth when they appear to be better on a certain dimension (e.g., ‘I am faster’) and lose in self-worth when they are outperformed (e.g., for overweight and obese youngsters when it comes to aerobic exercises). As a consequence, they might focus on a different dimension to compare themselves favorably with similar others (e.g. ‘I am better in computer games’ or ‘I am better in Geography’) [18]. At the end of the day, a vicious cycle appears. One reason that overweight people are not physically active is that they are outperformed by normal-weight people, and one reason they are overweight is because they are not physically active.
BREAKING THE CYCLE
To break this vicious cycle, we first have to shift our focus away from body weight adjusted for height (BMI) as an individual metabolic and mental health measure. BMI is a good tool for risk estimates in large populations, but not the right tool for individual evaluations [19]. One's BMI is a bad predictor of one's body composition, and focusing on BMI might have stigmatizing effects on one's health in later life [4]. Furthermore, instead of the focus on making overweight people leaner – which might be stigmatizing – there should be a focus on improvement of body composition in all youngsters.
Finally, instead of focusing on the present physical activity guidelines, with poor compliance [10–12], it might be more appropriate to focus on health behaviors people like to do. From a metabolic perspective, physical activity can be distinguished in an aerobic subdimension and a resistance subdimension. Although normal-weight youngsters perform better on aerobic exercises, overweight and obese youngsters will perform better on strength exercises, and as a consequence gain self-worth (‘I am stronger’) (G.A. ten Hoor et al., unpublished observation). To break the cycle, these resistance exercises might be the solution.
PHYSIOLOGICAL AND PSYCHOLOGICAL BENEFITS OF RESISTANCE TRAINING
When looking at body composition, overweight youngsters do not only have a higher fat mass, but also a higher muscle mass compared with their normal-weight counterparts (G.A. ten Hoor et al., unpublished observation). With that, they are also stronger and better in exercises where the focus is on absolute strength (G.A. ten Hoor et al., unpublished observation) [20], making them under the right circumstances more motivated to engage in resistance exercises [21] and ultimately maintain a physically active lifestyle.
There is increasing evidence to shift focus from rapid short-term weight loss to gaining long-term health. Quickly losing weight may have short-term successes, but one often ends up in a fast weight regain because of several mechanisms (the so-called ‘yoyo effect’, for detailed information about known mechanisms, see [22▪,23]). By quickly losing weight by caloric restriction, amongst others, one's energy expenditure also adjusts to a lower energy intake making long-term dieting a necessity for the maintenance of lost weight [24]. At the same time, a proportionally high decrease of leptin levels (the ‘satiety hormone’), increased Ghrelin levels (induces hunger), decreased peptide YY3–36, and cholecystokinin (induce satiety), and increased neural responsivity make people who quickly lose weight often surrender to a higher energy intake [22▪]. Furthermore, another hypothesized cause of a fast weight regain is that by quickly losing weight, the size but not the number of fat cells reduces. The adipocytes get ‘stressed’, and try to compensate by an increased uptake of glucose and fatty acids [23]. Obviously, to achieve long-term health effects, quickly losing weight is not the answer.
Lately, the short-term and long-term benefits of youth resistance exercises become more and more evident (for an elaborate overview, see [25▪▪]). Although resistance exercises do not meet one's desire of a decreased weight or BMI per se [26], they can increase one's fat-free mass [27,28▪], body composition, strength, and energy balance on the long term [25▪▪,29▪,30▪]. Instead of losing weight, providing feedback about body composition can be a solid and sufficient motivator for continuing resistance exercise [31▪].
The benefits of an improved body composition are not only a higher energy balance (also a higher postexercise oxygen consumption [30▪] and decreased leptin levels [32▪]), but also improved insulin sensitivity, lower chances on cardiovascular disease, blood pressure, and cholesterol levels [29▪,30▪,33▪]. After a 3-month strength training exercise program, Vasquez et al.[29▪] for example found improvements of obese children's cholesterol levels (increase in high-density lipoprotein cholesterol, and decrease in total cholesterol). One's increased strength can also improve one's motor skills [25▪▪].
From a psychological point of view, there is only limited information about the mental health effects of strength training in overweight or obese people [25▪▪,27]. In a recent literature review, positive effects of resistance training in overweight people on quality of life-related outcomes and beliefs were found (G.A. ten Hoor et al., unpublished observation).
OTHER CONSIDERATIONS AND MISCONCEPTIONS
Although resistance exercises may have both biological and psychological benefits in the obesity ‘challenge’ [27,34▪▪], other factors need to be considered in implementing this approach. Without parental support, (overweight) youngsters will not engage in resistance exercises [35]. In a recent study about parental opinions about their child's physical activity behavior, we found that about one-third of the parents of 12–15 year olds would not allow their child to perform resistance exercises (G.A. ten Hoor et al., unpublished observation). The most mentioned reasons against resistance exercises were that their child was too young, and that at their age, strength exercises were considered unhealthy. The idea that strength exercises are unhealthy is a persistent misperception. As long as they are performed under qualified supervision, it can even prevent injuries and cause a rapid rehabilitation from injuries [25▪▪].
Another important point is that youngsters should not become little body builders, nor should aerobic components be completely banned. An important consideration for social comparison – which might trigger overweight people to become more physically active when there is a strength aspect involved – is not only that overweight youngsters are better than normal weight youngsters, but also that overweight and normal-weight youngsters exercise together, and that there is a mutual appreciation between the youngsters in each other's performance. It is evident that when normal-weight and overweight youngsters are not physically active together, there is no social comparison, as overweight youngsters will not find out that they in fact perform better than normal-weight youngsters. Also, when there is no mutual appreciation (e.g., normal-weight youngsters attribute the better strength performance of overweight youngster to ‘because they are heavy’ and not to ‘because they are strong’), the positive effects of the social comparison are devaluated. A possible manner to accomplish this is to develop a physical activity team-task with both aerobic and (absolute) strength components, wherein the team (and not the individual) will be evaluated per task at the level of the best team member (which is most satisfying for all group members, [17▪▪]). Because youngsters work in teams, the focus is on performance and not on weight. With that, the level of stigmatization is limited to a minimum [4].
CONCLUSION
Obesity is a multidisciplinary problem, and a multidisciplinary approach is needed. Therefore, it is not only important that scientists with expertise in different areas work together, but also governments and industries collaborate. We do not have to solve obesity per se, but obesity-related health issues. On many levels, strength exercises might contribute to this solution. The approach proposed here has the abilities to make overweight youngsters more (motivated to be) physically active, and more healthy by means of a healthier body composition; not by focusing on the current aerobic-focused physical activity guidelines, one's BMI, or the idea that overweight youngsters have to lose weight, but by focusing on their strength and on what overweight youngsters like to do.
Acknowledgements
This project is sponsored by ZonMw (Netherlands organization for health research and development; Grant nr 525001004).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Seidell JC. In: Worldwide prevalence of obesity in adults. Bray GA, Bouchard C. editors. Handbook of obesity: epidemology, etiology, and physiopathology. Florida: Taylor & Francis Ltd; 2014. 47–54 [Google Scholar]
- 2.Mirza NM, Yanovski JA. In: Prevalence and consequences of pediatric obesity. Bray GA, Bouchard C. Handbook of obesity: epidemology, etiology, and physiopathology. Florida: Taylor & Francis Ltd; 2014. 55–74 [Google Scholar]
- 3.Kelsey MM, Zaepfel A, Bjornstad P, Nadeau K. Age-related consequences of childhood obesity. Gerontology 2014; 60:222–228 [DOI] [PubMed] [Google Scholar]
- 4.Hunger JM, Tomiyama AJ. Research letter: weight labeling and obesity: a longitudinal study of girls aged 10 to 19 years. JAMA Pediatr 2014; 168:579–580 [DOI] [PubMed] [Google Scholar]
- 5.Alwan A. Global status report on noncommunicable diseases. Geneva, Switzerland: World Health Organization; 2011 [Google Scholar]
- 6.Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020. WHO Ministerial Conference on Nutrition and Noncommunicable Diseases in the Context of Health 2020 2013 [Google Scholar]
- 7.EuropeanCommission. EU Action Plan on Childhood Obesity; 2014-2020 [Google Scholar]
- 8.WHO. Global Recommendations on Physical Activity for Health: 5-17 year olds; 2011 [Google Scholar]
- 9.Lee I-M, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major noncommunicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012; 380:219–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song M, Carroll DD, Fulton JE. Meeting the 2008 physical activity guidelines for americans among US youth. Am J Prevent Med 2013; 44:216–222 [DOI] [PubMed] [Google Scholar]
- 11.Wafa SW, Hamzaid H, Talib RA, Reilly JJ. Objectively measured habitual physical activity and sedentary behaviour in obese and nonobese Malaysian children. J Tropical Pediatr 2013; fmt093 [DOI] [PubMed] [Google Scholar]
- 12.Kann L. Obesity and other correlates of physical activity and sedentary behaviors among US high school students. J Obes 2013; [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pataky Z, Armand S, Müller-Pinget S, et al. Effects of obesity on functional capacity. Obesity 2014; 22:56–62 [DOI] [PubMed] [Google Scholar]
- 14.McHugh M. Oversized young athletes: a weighty concern. Brit J Sports Med 2010; 44:45–49 [DOI] [PubMed] [Google Scholar]
- 15▪.Kok G, Bartholomew LK, Parcel GS, et al. Finding theory- and evidence-based alternatives to fear appeals: Intervention Mapping. Int J Psychol 2014; 49:98–107 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides a framework for the development of theory and evidence based health promotion programs.
- 16.Ekkekakis P, Lind E. Exercise does not feel the same when you are overweight: the impact of self-selected and imposed intensity on affect and exertion. Int J Obes 2006; 30:652–660 [DOI] [PubMed] [Google Scholar]
- 17▪▪.Forsyth DR. Group dynamics; 6th ed Wadsworth: Cengage Learning; 2014, p113, p346 [Google Scholar]; From page 112 on, a summary of social comparison theory and evidence.
- 18.Van Knippenberg A, Wilke H, De Vries N. Social comparison on two dimensions. Eur J Social Psychol 1981; 11:267–283 [Google Scholar]
- 19.Bogin B, Varela Silva MI. The body mass index: the good, the bad, and the horrid. Bulletin de la société Suisse d’Anthropologie 2012; 18:5–11 [Google Scholar]
- 20.Colella D, Morano M, Robazza C, Bortoli L. Body image, perceived physical ability, and motor performance in nonoverweight and overweight Italian children. Percept Mot Skills 2009; 108:209–218 [DOI] [PubMed] [Google Scholar]
- 21.Patall EA, Sylvester BJ, Han C. The role of competence in the effects of choice on motivation. J Experiment Soc Psychol 2014; 50:27–44 [Google Scholar]
- 22▪.Ochner CN, Barrios DM, Lee CD, Pi-Sunyer FX. Biological mechanisms that promote weight regain following weight loss in obese humans. Physiol Behav 2013; 120:106–113 [DOI] [PMC free article] [PubMed] [Google Scholar]; This is an elaborate overview of mechanisms promoting weight regain following weight loss.
- 23.Mariman EC. Human biology of weight maintenance after weight loss. J Nutrigenet Nutrigenom 2012; 5:13–25 [DOI] [PubMed] [Google Scholar]
- 24.Tremblay A, Royer M, Chaput J, Doucet E. Adaptive thermogenesis can make a difference in the ability of obese individuals to lose body weight. Int J Obes 2013; 37:759–764 [DOI] [PubMed] [Google Scholar]
- 25▪▪.Lloyd RS, Faigenbaum AD, Stone MH, et al. Position statement on youth resistance training: The 2014 International Consensus. Brit J Sports Med 2013; bjsports-2013-092952 [Accessed 17 July 2014] [DOI] [PubMed] [Google Scholar]; This is the current position statement on youth resistance training
- 26.Kelley GA, Kelley KS. Effects of exercise in the treatment of overweight and obese children and adolescents: A systematic review of meta-analyses. J Obes 2013; [online] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schranz N, Tomkinson G, Olds T. What is the effect of resistance training on the strength, body composition and psychosocial status of overweight and obese children and adolescents? A systematic review and meta-analysis. Sports Medicine 2013; 43:893–907 [DOI] [PubMed] [Google Scholar]
- 28▪.Cloutier G, Forman D, Lindegger N, et al. Effects of a short-term heavy resistance training in young and older adults for strength and body composition. FASEB J 2014; 28:1028–1031 [Google Scholar]; This study shows positive effects of resistance training.
- 29▪.Vasquez F, Diaz E, Lera L, et al. Impact of a strength training exercise program on body composition and cardiovascular risk factors in a group of obese schoolchildren by pubertal stage. Am J Sports Sci Med 2014; 2:40–47 [Google Scholar]; This study shows positive effects of resistance training.
- 30▪.Paoli A, Moro T, Bianco A. Lift weights to fight overweight. Clin Physiol Functional Imag 2014; doi: 10.1111/cpf.1213633. [Accessed 17 July 2014] [DOI] [PubMed] [Google Scholar]; This study shows positive effects of resistance training.
- 31▪.Pescud M, Pettigrew S, McGuigan MR, Newton RU. Factors influencing overweight children's commencement of and continuation in a resistance training program. BMC Public Health 2010; 10:709. [DOI] [PMC free article] [PubMed] [Google Scholar]; Study on children's commencement of and continuation in a resistance training program.
- 32▪.Mohebbi H, Fatahi A, Faraji H, Mohseni MM. The effect of upper and lower limb resistance training on leptin in overweight men. Int J Sport Studies 2013; 3:1318–1324 [Google Scholar]; This study shows positive effects of resistance training.
- 33▪.Tibana R, Pereira G, Navalta J, et al. Acute effects of resistance exercise on 24-h blood pressure in middle aged overweight and obese women. Int J Sports Med 2013; 34:460–464 [DOI] [PubMed] [Google Scholar]; This study shows positive effects of resistance training.
- 34▪▪.Schranz N, Tomkinson G, Parletta N, et al. Can resistance training change the strength, body composition and self-concept of overweight and obese adolescent males? A randomised controlled trial. Brit J Sports Med 2013; doi:10.1136/bjsports-2013-092209 [Accessed 17 July 2014] [DOI] [PubMed] [Google Scholar]; Schranz and colleagues are also advocates for resistance training for overweight youngsters
- 35.Davison KK, Mâsse LC, Timperio A, et al. Physical activity parenting measurement and research: challenges, explanations, and solutions. Childhood Obes 2013; 9: S-103-S-109 [DOI] [PMC free article] [PubMed] [Google Scholar]


