Abstract
In recent years non-communicable chronic diseases that are potentiated by sterile inflammation have replaced infectious diseases as the major threat to human health. Sterile inflammation that results from aberrant tissue damage plays pivotal roles in the pathogenesis of numerous acute and chronic inflammatory diseases including atherosclerosis, type 2 diabetes, cancer, obesity, and multiple neurodegenerative diseases. The cellular events and molecular signaling pathways that govern sterile inflammation currently remain poorly defined, however emerging data suggest central roles for IL-1 in driving autoimmune and inflammatory disease pathogenesis. Improved characterization of the immunological pathways that contribute to sterile inflammation are desperately needed to develop effective therapeutics to treat these devastating diseases. In this review we discuss recent advances in our understanding of how IL-1 is regulated in response to tissue damage. In particular, we highlight recent studies that describe novel roles for conventional cell death molecules in the regulation of IL-1β production.
Keywords: Sterile inflammation, interleukin-1, innate immunity, inflammasome, NOD-like receptor, autoinflammation
Introduction
Inflammation that is mediated by immune cells is vital for host protection against pathogens. In response to an infection, the immune system orchestrates a coordinated response to eradicate the pathogen and to restore tissue integrity. Innate immune cells constitute the first line of defense and are involved in recognizing the initial threat, containing the infection and promoting the recruitment of additional immune cells through the release of cytokines and chemokines. Adaptive immune cells, which comprise of T and B cells, then arrive at the site of invasion and promote the clearance of infected cells. An inability to mount protective responses against pathogens can have debilitating and even fatal consequences for the host and, as a result, the immune system has evolved an arsenal of effector mechanisms to combat infection.
However inflammation can be a double-edged sword, and the same inflammatory pathways that are required for host protection against microbes can also be provoked in response to tissue damage in the absence of apparent infection. Inflammation and tissue destruction that results from trauma, cellular and metabolic dysfunction, ischemia-reperfusion injury or environmental irritants typically ensues in the absence of infection and is commonly referred to as sterile inflammation [1]. Controlled immune responses to sterile stimuli are needed to neutralize and sequester the irritant, clear damaged cells, and to promote wound healing. Innate immune cells, including most prominently neutrophils and macrophages, are the major mediators of sterile inflammation [2–5]. Following tissue damage, neutrophils and macrophages are recruited into the area of injury where they play essential roles in the removal of the irritant and the induction of repair pathways. The process of immune cells aiding in the resolution of sterile tissue damage typically occurs in the absence of overt pathology. However, continuous exposure to an injurious agent can cause unrestrained inflammation, fibrosis and potentially organ failure. Mounting evidence indicates that unchecked immune responses are centrally involved in a spectrum of acute and chronic inflammatory disorders. Indeed, dysregulated production of proinflammatory cytokines, reactive oxygen species (ROS), growth factors and proteases by immune cells are known to cause the aberrant tissue destruction, collagen deposition and fibrosis that underlie inflammatory and autoimmune disease [6, 7].
Acute disorders that result from sterile inflammation include ischemia-reperfusion injury, trauma and particulate-induced lung injury. In these settings, rapid perturbations to tissue integrity cause inflammatory forms of cell death such as necrosis. Immune cells respond to danger-associated molecular patterns (DAMPs) released by necrotic cells and rapidly up-regulate factors to limit the spread of tissue damage and to promote wound-healing responses. Immune-based inflammatory responses that ensue in response to acute tissue damage are directly responsible for the pain, vasodilation and scarring that are associated with trauma, exposure to environmental irritants, and tissue hypoxia.
Dysregulated immune responses are also centrally responsible for driving inflammation and tissue destruction in chronic autoimmune and inflammatory diseases. For example, deposition of cholesterol crystals around arterial walls provokes inflammatory cytokine production by macrophages and this contributes to subsequent plaque formation in atherosclerosis [8]. Sterile inflammation is also involved in the pathogenesis of multiple neurodegenerative diseases including Alzheimer’s disease and amyotrophic lateral sclerosis (ALS). In these disorders, the buildup of amyloids and unfolded proteins in the central nervous system (CNS) incites the release of neurotoxic pro-inflammatory cytokines by microglial cells and other innate immune cells [9]. Further, immune cell-mediated inflammation is now recognized to contribute to the development and progression of obesity and associated metabolic disorders, which include type 2 diabetes and fatty liver disease [10–13]. In this context, saturated fatty acids and danger signals (e.g. islet amyloid polypeptide, uric acid and damaged mitochondria) produced as a result of metabolic dysfunction provoke inflammatory cytokine production and tissue damage.
Extensive work now shows that IL-1, in particular, plays overarching roles in the inflammatory process and, as a result, the immune system has evolved numerous mechanisms to regulate IL-1 production. Indeed, aberrant IL-1 signaling has been identified to underlie many monogenic and polygenic human inflammatory disorders including cryopyrin-associated periodic syndromes (CAPS) and familial Mediterranean fever (FMF). Generation of IL-1 by caspase-1 in canonical inflammasome complexes is by far the most well established mechanism for IL-1 production, however recent studies have implicated prominent roles for additional pathways and molecules in the regulation of IL-1 secretion. In this review we discuss that pivotal roles that IL-1 plays in inflammatory disease and draw attention to emerging pathways that are involved in the regulation of IL-1 production.
The IL-1 family cytokines: central mediators of inflammation
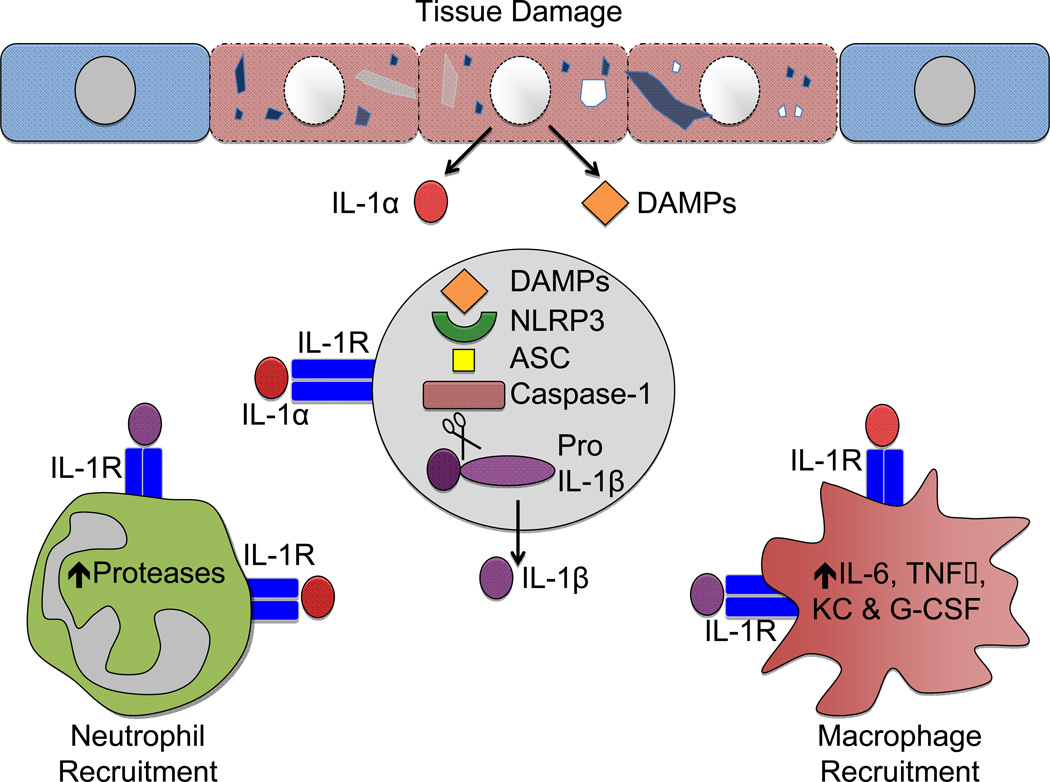
The IL-1 family cytokines, IL-1α and IL-1β, have been established to play key roles in infectious and sterile inflammatory diseases [1, 14–19]. Both IL-1α and IL-1β provoke potent proinflammatory events by engaging the IL-1 receptor (IL-1R). Following tissue damage, IL-1 release serves as the primary initiating signal to coordinate the mobilization of immune cells to the damaged area (Figure 1). Indeed, induction of IL-1 signaling results in dramatic production of chemokines and cytokines that function to orchestrate the expansion and recruitment of phagocytes to the site of damage. The early recruitment of neutrophils appears to be mediated primarily via IL-1-dependent production of granulopoietic factors including IL-6, KC and G-CSF [20–23]. The release of these mediators rapidly induces the expansion of neutrophils in the bone marrow (termed granulopoiesis) and also provides cues to direct the trafficking of neutrophils to the damaged tissue. IL-1 can also directly coordinate the mobilization and activation of macrophages during autoinflammatory responses by promoting the production of IL-12, M-CSF and IP-10 [23].
Figure 1. IL-1 signaling centrally regulates sterile inflammation.
Cell death that results from trauma, ischemia, environmental irritants and cellular stress provokes the recruitment and activation of immune cells in areas of tissue damage. Inflammatory forms of cell death that ensue as a result of these triggers provoke the release of IL-1α and danger-associated molecular patterns (DAMPs). DAMPs such as ATP, uric acid, and damaged mitochondria are recognized by the cytosolic sensor NLRP3 in surrounding cells and this initiates the recruitment of NLRP3, the adaptor protein ASC and caspase-1 into multiprotein complexes that are referred to as inflammasomes. Formation of inflammasome molecular platforms triggers self-cleavage and activation of caspase-1. Active caspase-1 subsequently cleaves the pro-forms of IL-1β and IL-18, which is required for their secretion and biological activity. This is in contrast to IL-1α, which does not require processing to elicit its inflammatory activity. Both IL-1α and mature IL-1β induce potent proinflammatory singling following engagement of the IL-1 receptor (IL-1R). IL-1-dependent signaling promotes the up-regulation of additional inflammatory cytokines such as IL-6, TNFα, KC and G-CSF in macrophages and neutrophils. The release of these inflammatory mediators helps to promote the removal of cellular debris and to instruct the recruitment of additional immune cells to damaged tissue. IL-1 also triggers the expression of proteases and growth factors, which are needed to restore tissue integrity in the damaged areas. Inflammatory responses that are mounted in response to aberrant cell death are required to restrain the insult, phagocytize damaged cells, and to promote wound healing. However, excessive or sustained sterile inflammation can adversely cause fibrosis and tissue destruction. As a result, immune responses that ensue in response to tissue damage are directly responsible for driving the inflammation and pathology that cause inflammatory and autoimmune disease.
In addition to acting on innate cells, IL-1 signaling is also known to influence aspects of the sterile inflammatory process by affecting adaptive cells [24, 25]. For instance, IL-1 secretion in the periphery directs recruitment of B and T cells out of circulation through the blood and lymphatic system and into the inflamed tissue [26, 27]. Once mobilized in inflamed organs, B cells can secrete antibodies that help to opsonize irritants and remove cellular debris [28]. Furthermore, B cells participate in sterile inflammatory responses by secreting cytokines (IL-10, IL-12 and IL-18) that are known to regulate the activity of macrophages and neutrophils in inflamed areas [29, 30]. T cells aid in the containment and removal of irritants and cell damage by secreting cytokines that further promote the recruitment of additional phagocytes to the injured area and by producing cytolytic factors that eliminate injurious agents [31]. T cells have also been found to centrally contribute to the wound healing process. In particular, the production of anti-inflammatory cytokines such as IL-10 and TGF-β by regulatory T cells (Tregs) is needed to facilitate effective resolution of inflammatory responses and to promote tissue repair [32]. Although T cells contribute to successful containment and resolution of tissue damage, unchecked T cell responses can also provoke tissue pathology. Interestingly, dysregulated IL-1 signaling has emerged as a major mechanism that promotes pathogenic T cells responses during autoinflammatory disease and work by multiple laboratories has clearly shown that IL-1 signaling in T cells markedly induces T cell expansion and promotes enhanced inflammatory cytokine production [33–35]. For example, IL-1R signaling promotes the generation of GM-CSF and IL-17 producing autoreactive T cells that are required to cause demyelinating neuroinflammatory disease in experimental autoimmune encephalomyelitis (EAE) [36, 37].
Historically, IL-1α and IL-1β have been considered to have overlapping functions. Despite their ability to evoke similar immunological outcomes, IL-1α and IL-1β differ substantially in their expression and regulation. Furthermore, non-redundant roles for IL-1α or IL-1β have recently been established in multiple inflammatory diseases [20, 21, 38–42]. Below we highlight the specific molecular pathways that are known to regulate IL-1α and IL-1β production and discuss their contributions to autoinflammatory disease.
IL-1α and inflammatory disease
Aberrant cell death that results from cellular stress, trauma, environmental insults and hypoxia are known trigger to inflammatory disease and, accordingly, the release of IL-1α under these conditions has been shown to prominently affect such disease [43]. Indeed, IL-1α has been discovered to be a central driver of immune responses that are generated in response to sterile tissue damage. Early studies demonstrated that IL-1α instigates the sterile inflammatory response to necrotic cells in mice [7, 44], and subsequent studies have shown that IL-1α critically regulates aspects of wound healing [45]. Following catastrophic tissue damage, IL-1α is released by cells and serves as an “alarmin” molecule to recruit other immune cells to the site of injury. IL-1α can also lead to potent up-regulation of inflammatory cytokines including proIL-1β, IL-6, and TNFα following IL-1R-mediated NF-κB signaling in nearby cells (Figure 1). IL-1α has been proposed to be an apical initiator of autoinflammatory responses due to the fact that it does not require up-regulation or processing to provoke inflammation once it is released. Indeed, IL-1α has been shown to centrally orchestrate the inflammatory responses that develop in response to ischemia-reperfusion injury, and altered IL-1 signaling has been identified to be a major culprit in the pathology of many ischemia-related diseases, including stroke and myocardial infarction [46–51].
IL-1α was also shown to centrally drive inflammatory immune responses in a mouse model of neutrophilic dermatosis [20]. Mutation in the phosphatase, SHP-1, causes a severe autoinflammatory syndrome that resembles neutrophilic dermatosis in humans and is characterized by persistent footpad swelling and suppurative inflammation [52–55]. Excessive production of inflammatory cytokines, neutrophilia and hyperactive T cell responses are associated with this SHP-1-mediated disease pathology [56, 57]. Genetic abrogation of IL-1R was found to protect SHP-1 mutant mice from cutaneous inflammation [58], suggesting that IL-1-mediated events potentiate disease. Surprisingly, inflammasome activation and IL-1β expression were dispensable for SHP-1-mediated footpad disease. In contrast, dysregulated IL-1α-mediated events were discovered to be responsible for chronic inflammation in this model, as genetic deletion of Il1α provided complete protection from disease [20]. IL-1α is also chiefly responsible for driving inflammation in models of trauma-induced skin damage [20], artery rejection [27], atherosclerosis [41], and DNA damage-induced senescence and tumorigenesis [21]. Additional studies that seek to characterize the discrete roles of IL-1α and IL-1β in sterile inflammation will provide much needed insight into the etiology of many inflammatory diseases.
Regulation of IL-1α
In comparison to IL-1β, our understanding of the roles and regulation of IL-1α in sterile inflammatory disease is severely limited. IL-1α is one of the few known cytokines that can exert transcriptional functions in the nucleus while also promoting immunological activities once it is released into the extracellular compartment. IL-1α possesses a nuclear localization sequence in its N-terminus, which allows it to translocate into the nucleus where it can affect transcription [59–61]. Interestingly, the only other two known dual function cytokines, IL-33 and HMGB1, have also been implicated to play instrumental roles in regulating inflammatory responses to tissue damage [62, 63]. In comparison to IL-1β, which requires cleavage to provoke its inflammatory activities, full-length IL-1α can incite inflammation without any modification and, thus, it is critical that cells employ protective measures to ensure that IL-1α is not released during cell death. Turnover of cells occurs at astounding rates in humans and it is estimated that one million cells die each second through a silent or non-inflammatory form of cell death known as apoptosis [64]. During homeostasis IL-1α exists both in the cytoplasm and nucleus, however following apoptotic signaling, IL-1α is rapidly shuttled into the nucleus to prevent its passive release during cell turnover [43, 65]. In contrast, the induction of catastrophic forms of cell death, including necrosis, can provoke the release of IL-1α and subsequent inflammation (Figure 1).
While IL-1α is constitutively expressed by both immune cells and parenchymal cells, IL-1β is not expressed at appreciable levels by circulating cells [66]. Rather, a priming step is required to up-regulate IL-1β before it can be processed and secreted. Once IL-1β has been expressed it requires cleavage to elicit its biological activity and secretion. In contrast, IL-1α does not require processing for it to be active and, as a result, IL-1α can promote inflammation in its full-form (precursor IL-1α) [67]. Precursor IL-1α can also be cleaved to generate two biologically active IL-1α species, which are known as the mature and propiece forms. The proteases that contribute to IL-1α cleavage and the generation of mature IL-1α remains a subject of debate. Multiple groups have reported that activators of caspase-1 in inflammasomes (see below for description of caspase-1 and inflammasomes) can promote the secretion of mature IL-α [68, 69]. In contrast, other studies suggest that calpain-like activities rather than inflammasomes are required for mature IL-1α processing [70–73]. Regardless, it is clear that additional studies are needed to ascertain the molecular players that coordinate IL-1α cleavage. Furthermore, the discrete biological functions of the three different forms of IL-1α (precursor, propiece and mature IL-1α) have not been fully characterized and this remains an important area of future investigation in the sterile inflammatory field.
The upstream pathways that regulate IL-1α production still remain poorly defined. However, in an inflammatory skin disease model it was found that the kinase RIP1 is centrally involved in driving IL-1α-mediated inflammation [20]. RIP1 has been established to play important roles in cell death pathways, however its ability to influence inflammatory responses has not been studied in detail. Additional studies are needed to unravel the signaling pathways that are involved in RIP1-dependent control of cytokine production and inflammation.
Inflammasome-mediated processing of IL-1β
IL-1β has also been established to play pathogenic roles in multiple major inflammatory and autoimmune diseases including type 2 diabetes, Alzheimer’s disease and obesity. A two-step process is required to generate and secrete biologically active IL-1β. Under steady state conditions, there is typically minimal expression of IL-1β by immune cells, thus the first step that is required for production of bioactive IL-1β is characterized by the up-regulation of IL-1β expression. This induction of IL-1β priming is typically mediated by NF-κB signaling. The most well characterized triggers that have been shown to facilitate IL-1β induction include TNF, IL-1α and Toll-like receptor (TLR)-ligands [66, 74, 75]. In the case of autoinflammatory and autoimmune disease, which typically occur in the absence of infection, it is likely that proinflammatory cytokines that are known to promote NF-κB activation (e.g. IL-1α, TNFα and IL-6) provide the necessary signal to promote IL-1β expression [75]. However, it is also possible that commensal bacteria that reside in the host can also mediate proIL-1β up-regulation by providing TLR signals. The second essential step for the generation of biologically active IL-1β involves the cleavage of precursor IL-1β by a protease.
The most well characterized mechanism for IL-1β processing is via activated caspase-1 in the canonical inflammasome complex. Canonical inflammasomes are multi-protein complexes that generally consist of three main components: a cytosolic sensor molecule, the enzyme caspase-1 and the adaptor protein ASC [14, 15, 74]. Members of the NOD-like receptor (NLR) and AIM2-like receptor (ALR) families are established cytosolic sensor molecules that mediate inflammasome formation. NLRs that have been identified to incite inflammasome activation include NLRP1, NLRP3, NLRP6, NLRP7, NLRP12 and NLRC4. NLRP1 and NLRC4 are primarily involved in initiating innate immune responses during infection. NLRP1b detects anthrax lethal toxin [76–78] and NLRC4 induces IL-1β secretion in response to certain bacterial flagellin and Type III secretion system-associated proteins [79–84]. NLRP6, NLRP7 and NLRP12 have also recently been suggested to coordinate inflammasome signaling under specific conditions. For instance, NLRP12 has been implicated in the regulation of IL-1β secretion in response to Yersinia pestis and malaria [85, 86], and NLRP7 was described to control inflammasome-mediated IL-1β by human macrophages following stimulation with microbial lipopeptides [87]. Interestingly, NLRP6 and NLRP12 also negatively regulate NF-κB signaling and inflammatory cytokine production in response to TLR activation [88–95]. Thus, additional studies are needed to clarify how these NLRs can exert both anti- and pro-inflammatory functions in different pathways. NLRP3, on the other hand, has been identified to be a central mediator of sterile inflammatory disease as a result of its unique ability to recognize a diverse array of endogenous danger signals that are released during aberrant cell death (ATP and uric acid), metabolic factors (saturated fatty acids and cholesterol crystals) and exogenous irritants (asbestos and silica).
Absent in melanoma 2 (AIM2) and interferon-inducible protein 16 (IFI16) are ALR (also known as pryin- and HIN-200 domain–containing proteins or PYHIN containing proteins) family molecules that have recently been described to incite inflammasome formation following detection of intracellular DNA [96–100]. The roles of AIM2 and IFI16 in autoinflammatory disease progression are currently poorly defined. Interestingly, the development of immune response to self-DNA is believed to contribute to the pathogenesis of multiple autoimmune disorders including systemic lupus erythematous (SLE) [101], psoriasis [102], type 1 diabetes [103], and polyarthritis [104]; thus it is feasible that ALRs will be discovered to contribute to autoinflammatory disease progression at some level.
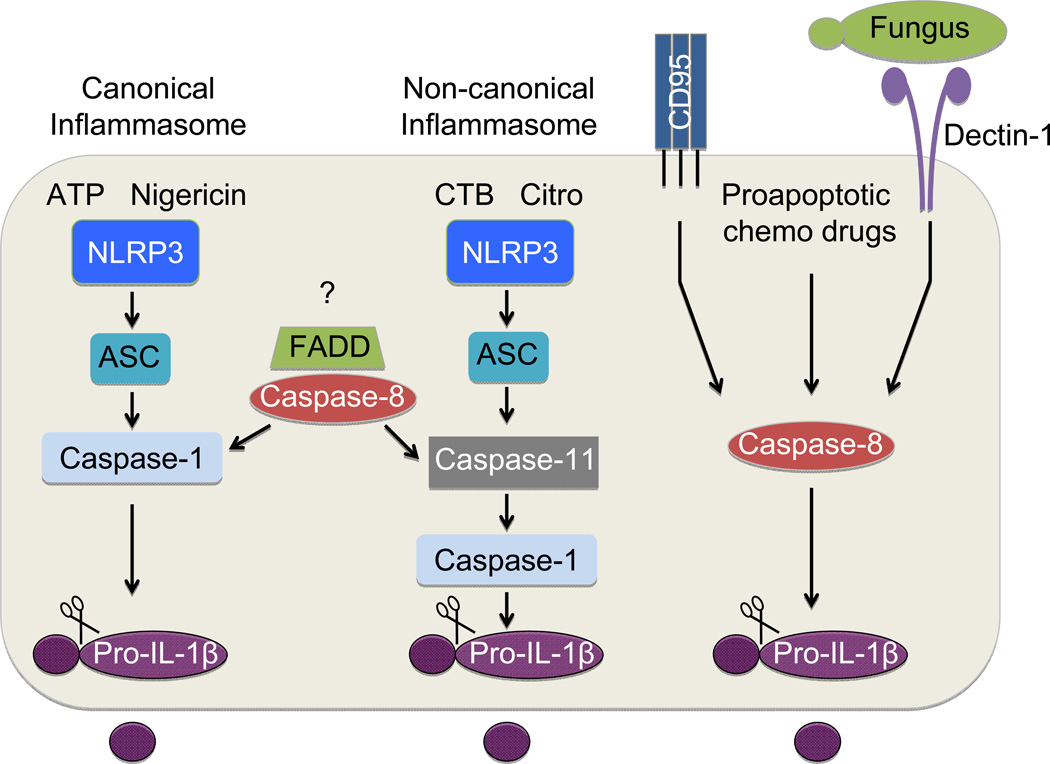
Recognition of pathogen- or danger-associated molecular patterns (PAMPs and DAMPs, respectively) by NLRs or ALRs promotes the recruitment of ASC and caspase-1 into the inflammasome complex, which is required to correctly orient caspase-1 for auto-cleavage and activation. Once activated, caspase-1 subsequently cleaves proIL-1β and proIL-18, which is required for their secretion and to elicit their inflammatory properties (Figure 2). Intriguingly, many of the danger- and stress-associated signals that have been widely proposed to trigger sterile inflammation have recently been discovered to provoke inflammasome-mediated IL-1β production. For instance, it was shown that man-made and environmental irritants (silica, asbestos, alum, alloy particles, and car exhaust), metabolic factors (cholesterol, amyloids, saturated fatty acids, and glucose) and endogenous danger signals that are released as a result of aberrant cell death (ATP, reactive oxygen species, and uric acid) can all trigger inflammasome-mediated IL-1β secretion. Furthermore, work from multiple groups has clearly shown that dysregulated inflammasome activation and downstream cytokine production centrally contributes to the development of inflammation and pathology in a spectrum of metabolic, autoimmune and inflammatory disorders.
Figure 2. Pathways involved in caspase-mediated IL-1β maturation.
IL-1β requires cleavage to elicit its biological activity and to promote its secretion. Multiple caspase-dependent pathways have been identified to promote IL-1β maturation. The best characterized of these pathways involves caspase-1 activation in inflammasome complexes. Recognition of pathogen- or danger-associated molecular patterns (PAMPs and DAMPs, respectively) by NOD-like receptors (NLRs) or AIM2-like receptors (ALRs) promotes the recruitment of caspase-1 into a multiprotein complex with the help of the adaptor protein ASC. Inflammasome complex formation orchestrates the self-cleavage and activation of caspase-1. Active caspase-1 subsequently cleaves the pro-form of IL-1β. Inflammasomes were originally thought to only require participation from a cytosolic sensor molecule, the adaptor protein ASC and caspase-1. However recent studies suggest that additional caspases and signaling molecules can directly impinge on pathways that coordinate IL-1β maturation. For instance, caspase-11 is required for efficient downstream caspase-1 and IL-1β activation in complexes that are now referred to as non-canonical inflammasomes. Caspase-11 is essential for inflammasome-induced IL-1β production in response to cholera toxin B and citrobacter rodentium. In contrast, other activators of inflammasome-dependent IL-1β maturation such as ATP and nigericin can trigger IL-1β cleavage via canonical inflammasomes in a fashion that is NLR/ASC/caspase-1 dependent and caspase-11 independent. The traditional cell death molecules, caspase-8 and FADD, have also been established to play major regulatory roles in both canonical and non-canonical inflammasome activation. However the upstream regulators of FADD and caspase-8 in these pathways still remain to be identified. Caspase-8 can also cleave IL-1β independently of caspase-1/11, and this has been suggested to contribute to IL-1β production that occurs in response to engagement of the death receptor CD95 (also known as FAS), fungal infection, and following treatment of cells with proapoptotic chemotherapeutic drugs.
For instance, inflammasome-mediated IL-1β has emerged as a major driver of the chronic low-grade inflammation that underlies obesity-associated diseases [105– 110]. In these studies NLRP3 inflammasome-mediated sensing of saturated fatty acids and associated metabolites (e.g. ceramide and palmitate) induced potent IL-1β secretion [107, 109]. Likewise, genetic deletion of central inflammasome molecules (caspase-1, ASC, NLRP3 and IL-1β) in mice that are fed a high-fat diet leads to reduced weight gain and improved glucose tolerance and insulin sensitivity [105–109, 111].
Inflammasome activation has also been discovered to incite IL-1β maturation in response to misfolded protein and amyloids; and, thus, caspase-1 has been implicated in driving the inflammation that causes tissue destruction in Alzheimer’s disease and type 2 diabetes. The deposition of amyloid β in the brain is believed to cause Alzheimer’s disease by provoking immune cell-mediated damage to CNS cells. Studies now show that recognition of amyloid β by microglia cells induces inflammasome-dependent IL-1β production [112]. Consistent with these in vitro findings, genetic abrogation of NLRP3 or caspase-1 in mice carrying mutations that are associated with familial Alzheimer’s disease (APP/SP1 mouse model) protects mice from loss of spatial memory and leads to enhanced phagocytosis of amyloid β by CNS phagocytes [113]. Accumulation of amyloids, and islet amyloid polypeptide (IAPP) in particular, is also associated with beta cell destruction in type 2 diabetes. IAPP has been described to initiate inflammasome-induced IL-1β production and this is believed to play pathogenic roles in type 2 diabetes [108].
Crystals and particulates that are of both environmental and endogenous origin have been historically linked to tissue damage and sterile inflammatory disease. For instance, the build-up of uric acid in joints is known to cause inflammatory joint destruction in gout, and the inhalation of irritants such as asbestosis and silica has been shown to cause chronic obstructive pulmonary disease (COPD) [114]. Recent studies now suggest that macrophage-mediated IL-1 production in response to particulates and crystals appears to be largely dependent on caspase-1 activation in inflammasomes [111, 115–118]. Collectively, these studies have helped to position inflammasome-mediated IL-1β as a key regulator of sterile inflammation. However, as discussed throughout this review, there are numerous important areas of both inflammasome and IL-1 biology that still require further investigation.
Regulation of IL-1β by new players in inflammasome activation
Over the last few years it has become increasingly apparent that inflammasome activation is not as simple as once thought, and additional caspases and modulators have been discovered to play critical roles in IL-1β cleavage and secretion. Interestingly, many of the newly identified contributors to inflammasome-mediated IL-1β maturation, including caspase-8 and caspase-11, have been previously described to potentiate sterile inflammatory disease through their established roles in regulating cell death. This emerging appreciation for the interface between traditional cell death pathways and IL-1β production has helped to identify new layers of complexity in IL-1β regulation.
Caspase-11
One of the first indications that additional caspases may be involved in inflammasome activation came from the important observation that the routinely studied caspase-1 knockout mouse is actually deficient in both caspase-1 and caspase-11 [119]. It turns out that embryonic stem cells from the 129 background mouse strain, which were used to target caspase-1 deletion, also lack expression of caspase-11 due to a 5-base-pair deletion that impairs exon splicing and, as a result, caspase-1 null mice also lack casp11. Previous work identified caspase-11 as an executioner caspase and found that caspase-11 was involved in promoting Fas-mediated apoptosis. Moreover, initial evaluation of inflammatory disease in caspase-11 deficient mice suggested that caspase-11 is involved in driving disease pathology through the regulation of cell death [120, 121]. To ascertain whether caspase-11 specifically influences the regulation of IL-1β production in the routinely studied Casp1‒/‒ mouse, which we now know lacks both caspase-1 and caspase-11, side-by-side comparisons of IL-1β secretion and caspase activation were conducted between singly deficient Casp1‒/‒ and Casp11‒/‒ cells. From these studies it was discovered that caspase-11 plays non-redundant roles in the generation of IL-1β production in response to specific activators of inflammasome activation. Namely, caspase-11 was found to be required for downstream activation of caspase-1 and subsequent IL-1β maturation in response to stimulation with cholera toxin B, E. coli, citrobacter rodentium, and others (Figure 2) [119, 122, 123]. Inflammasome platforms that are dependent on upstream caspase-11 activation are now referred to as non-canonical inflammasomes. In contrast, multiple known triggers of IL-1β production including ATP, silica, and nigericin were found to provoke IL-1β maturation independently of a role for caspase-11. These inflammasomes that do not require caspase-11 to trigger IL-1β processing have been coined canonical inflammasomes.
This discovery of a discrete role for caspase-11 in the regulation of IL-1β has been a fairly recent finding and additional studies are greatly needed to further dissect the unique roles of canonical vs. non-canonical inflammasomes in the regulation of disease. For instance, up until now our understanding of these separate inflammasome pathways comes primarily from studies performed on bone marrow-derived macrophages. Additional studies are required to formally address the distinct contributions of canonical and non-canonical inflammasomes in other cell types that are known to contribute to sterile inflammatory disease including dendritic cells, neutrophils, and tissue resident innate cells such as microglia. Recent advances have been made to highlight the specific roles of caspase-1 and caspase-11 under physiological settings. However, this work has been primarily done in infection models, thus far [124–128], and complete characterization of the distinct roles of caspase-1 and caspase-11 is still lacking in most autoimmune and sterile inflammatory disease models. Earlier in vivo studies that utilized singly deficient caspase-11 mice showed that caspase-11 could indeed influence tissue damage in autoinflammatory disease models, including EAE [121], and thus future studies that decipher discrete roles for caspase-1 and caspase-11 under physiologically settings are warranted. Furthermore, it is not known whether caspase-11 is required for the induction of IL-1β maturation in response to inflammasome triggers that have been identified to promote obesity-associated disease including amyloids, saturated fatty acids, and cholesterol crystals.
Caspase-8
Additional molecules that have been traditionally associated with the regulation of cell death have also recently been identified to modulate IL-1β maturation. For instance, multiple recent reports have established caspase-8 as a key regulator of IL-1β production. Caspase-8 has been extensively studied in the cell death field, where it is known to play important roles in regulating both cell survival and death. Caspase-8 is perhaps best known for its ability to drive extrinsic apoptosis in response to TNF receptor 1 (TNFR1) and CD95 (also known as Fas) activation [129]. Ligand binding to TNFR1 and CD95 promotes conformational changes in their cytoplasmic tails, which is necessary to allow for the docking of the FAS-associated death domain (FADD) adaptor protein to these death receptors. Under healthy conditions caspase-8 typically exists in a monomeric form as an inactive enzyme. However the binding of FADD to death receptors promotes the recruitment of monomeric caspase-8 zymogens, which in turn leads to homodimerization of caspase-8 and subsequent caspase-8 activation. Once activated caspase-8 directs apoptotic cell death by activating the downstream executioner caspase-3. In addition to performing its classic function in apoptosis, caspase-8 has also been demonstrated to play numerous non-apoptotic roles, including promoting NF-κB signaling, monocyte differentiation, cell survival and proliferation [129].
Multiple reports now show that caspase-8 can also influence IL-1β regulation and processing at multiple levels (Figure 2). In early in vitro studies, it was shown that recombinant caspase-8 is capable of cleaving proIL-1β at exactly the same site as caspase-1 [130]. Moreover, generation of biologically active IL-1β in response to poly(I:C)- and LPS-mediated stimulation was inhibited in the presence of caspase-8 inhibitors, CrmA (virally encoded caspase-8 inhibitor) or vFLIP expression (virally encoded caspase-8 inhibitor) [130]. These results helped to identify caspase-8 as a bona fide activator of IL-1β, however the embryonic lethality that is associated with caspase-8 deletion hampered complete mechanistic characterization of caspase-8 in the regulation of IL-1β maturation. Several recent genetic advancements have helped to reinvigorate interest in this area. These have included the discovery that the additional deletion of RIP3 in Casp8‒/‒ mice rescues embryonic lethality by limiting fatal necrosis/inflammation during development [131–133]. Utilization of Rip3‒/‒xCasp8‒/‒ cells and conditional targeting of the Casp8 allele has made it possible to unravel how caspase-8 influences IL-1β production at a molecular level. Genetic deletion of either caspase-8 or FADD on the Rip3‒/‒ background was found to markedly impair both canonical and non-canonical (caspase-11 dependent) inflammasome activation and downstream IL-1β processing [134]. This effect was not the result of RIP3 deletion, as Rip3‒/‒ cells secreted IL-1β at levels similar to wild-type cells in response to various inflammasome triggers. Rather, FADD and caspase-8 were shown to control the transcriptional priming of the NLRP3 inflammasome by regulating the expression of NLRP3 and proIL-1β. Furthermore, caspase-8 was specifically observed to dampen inflammasome activation at the post-translational level. This was accomplished by showing that treatment of wild-type macrophages with caspase-8 inhibitors following LPS priming still results in significant reductions in IL-1β secretion. To confirm that FADD/caspase-8 do in fact influence IL-1-mediated inflammatory responses under physiological settings, LPS-induced endotoxemia was induced in Rip3‒/‒xCasp8‒/‒ and Rip3‒/‒xFadd‒/‒ mice. Deletion of either caspase-8 or FADD on the RIP3 deficient background markedly dampened IL-1β and IL-1α release into the serum in response to LPS, which further confirms a role for the FADD-Caspase-8 axis in the regulation of IL-1β production.
Caspase-8 has also been proposed to directly promote IL-1β production through pathways that are completely independent of the critical inflammasome adaptor protein, ASC. For instance, it was found that endoplasmic reticulum (ER) stress induced IL-1β maturation is fully dependent on caspase-8 and does not require ASC expression [135]. Similar to other reports, they also found that caspase-8 is involved in the transcriptional regulation of proIL-1β. ER stress that results from the accumulation of unfolded proteins has been observed in multiple inflammatory disorders and is believed to spur inflammation and disease pathology. In particular, ER stress is frequently observed in obesity-associated diseases and diabetes, and the accumulation of unfolded proteins in the ER is thought to be linked to the chronic inflammation that underlies these diseases [136–139]. Future studies are required to elucidate whether caspase-8-mediated regulation of IL-1β secretion contributes to inflammation and tissue destruction in these disease settings.
Established regulators of cell death have also been discovered to potentiate IL-1β production through caspase-8. For example, it was shown that CD95 (also known as Fas) engagement provokes caspase-8-dependent IL-1β maturation in myeloid cells in a fashion that is not dependent on caspase-1 or RIP3 [140]. CD95 activation is known to play pathogenic roles in many inflammatory and autoimmune disorders, however whether this is directly due to CD95/caspase-8-mediated regulation of IL-1β still remains to be formally investigated. Cell death pathways that are induced by blocking the inhibitors of apoptosis proteins (IAPs) also regulate IL-1β production at least partially through caspase-8 activation. IAPs (namely XIAP, cIAP1 and cIAP2) are a family of molecules that limit the formation of the cell death inducing “ripoptosome” complex (RIP1-FADD-caspase-8-cFLIP) [141, 142]. Treatment of cells with the smac-mimetic compound A inhibits IAP activity and results in RIP3-mediated ROS production. This Smac-mimetic induced mitochondrial ROS production has been suggested to provoke both caspase-1- and caspase-8-mediated IL-1β secretion in a recent study [143]. However, a separate study arrived at opposite conclusions and found that deficiency in either cIAP1 or cIAP2 results in impaired in caspase-1 activation [144]. Further studies are thus required to ascertain the exact role(s) of IAPs in the regulation of IL-1.
Caspase-8 was also recently implicated in IL-1β secretion that can result in response to treatment with chemotherapeutic drugs such as doxorubicin (Dox) or staurosporine (STS) [145]. Many chemotherapeutic drugs rely on their ability to promote apoptosis in tumorigenic cells to limit the spread of cancer. However, proapoptotic chemotherapeutic drugs, such as Dox and STS, have also been reported to incite IL-1 production by immune cells. This induction of IL-1β maturation in response to proapoptotic chemotherapeutic drugs was found to specifically require caspase-8 activation. Furthermore, it appears that caspase-8-triggered IL-1β processing proceeds independently of a role for caspase-1 or caspase-11, as it was shown that Dox and STS treatment of Casp1‒/‒Casp11‒/‒ dendritic cells results in secretion of IL-1β at levels that were comparable to WT cells. In addition to helping to illuminate how proapoptotic drugs influence immune responses, these findings also have great implications for the field of sterile inflammation, where apoptosis and caspase-8 activation are hallmarks of disease pathogenesis.
Consistent with these findings, caspase-8 has also been discovered to directly regulate IL-1β production during infection [146]. For example, caspase-8 has emerged as a key inducer of IL-1β maturation in response fungal infection. The importance of IL-1-dependent signaling in the generation of protective anti-fungal responses has been widely appreciated for many years, and IL-1β has been established to be required for the induction of TH1 and TH17-mediated clearance [147–150]. However, the mechanism responsible for IL-1β maturation during various forms of fungal infection has remained a matter of debate since caspase-1/11 has been reported to be dispensable to mount protective responses [151, 152]. Recent findings now show that dectin-1 recognition of fungi on dendritic cells promotes caspase-8-induced cleavage of IL-1β [146]. Interestingly, IL-1β secretion in response to fungal stimulation did not require caspase-1 or NLRP3 participation, but rather involved the recruitment of the MALT1-Bcl-10-Card9 scaffold into a complex with caspase-8. Salmonella infection was also recently demonstrated to lead to caspase-8-dependnent modulation of IL-1β production in macrophages [153]. In these studies it was found that caspase-8 could be recruited into a complex with ASC independently of caspase-1, and that caspase-8 is an important driver of proIL-1β synthesis. Collectively these studies further demonstrate that caspase-8 can indeed functionally impinge on IL-1β secretion, however future studies are needed to evaluate the contributions of caspase-8-mediated IL-1β in the generation of effector responses and pathogen clearance.
It should also be noted that a recent study suggests that caspase-8 can also repress IL-1β secretion by blocking RIP3-mediated activation of the NLRP3 inflammasome under certain conditions. In this study, the authors found that conditional deletion of caspase-8 in dendritic cells using the CD11c-Cre deleter results in exacerbated IL-1β production and inflammatory disease in response to LPS stimulation [154]. Deletion of RIP3 or pharmacological inhibition of RIP1 was found to rescue hyperinflammatory responses in Casp8fl/flxCD11c-Cre+ mice and this was suggested to occur through RIP1/RIP3-mediated regulation of NLRP3 inflammasome activation and not by influencing cell death. It is clear from recent studies that caspase-8 is indeed a central regulator of IL-1β maturation, however additional studies are needed to further characterize the molecular underpinnings of caspase-8-regulated IL-1β production. Such future investigation should help reconcile how under certain conditions caspase-8 promotes IL-1β secretion, whereas in other situations it has been suggested to block IL-1β production.
Inflammasome-independent sources of IL-1β
Although caspase-mediated processing of IL-1β is the most widely characterized mechanism of IL-1-mediated inflammation and disease, emerging data also suggest pivotal roles for inflammasome-independent IL-1β in autoimmune and inflammatory disease pathogenesis. Indeed, caspase-1/11-independent IL-1β has been described to play crucial roles in osteomyelitis [38, 39], particulate-induced lung inflammation [155], osteoarthritis [156, 157], acidosis-provoked inflammation [158], host defense against certain pathogens [146, 159], and other inflammatory diseases [160]. Moreover, genetic deletion of caspase-1/11 does not lead to complete abrogation of IL-1β production or disease progression in numerous IL-1-dependent disease models [111, 115, 117, 152, 160, 161], suggesting that inflammasome-independent sources of IL-1β can also potentiate disease pathology in some settings. A number of additional serine proteases including cathepsin B, cathepsin C, cathepsin G, proteinase-3 (PR3), elastase, granzyme-A, chymase, matrix metalloproteinase 9, and chymotrypsin have also been shown to cleave proIL-1β under in vitro conditions [19, 162–167]. The molecular mechanisms that orchestrate the activation of IL-1β by these proteases are just beginning to be elucidated under physiological settings and not much is currently known. Furthermore, whether these serine proteases contribute to IL-1β secretion and subsequent inflammatory disease in vivo is just beginning to be elucidated.
Recently, it was shown that inflammasome-independent IL-1β production is responsible for driving inflammatory bone destruction in a mouse model of osteomyelitis [38, 39]. In these studies, it was discovered that IL-1 signaling and IL-1β production were required to spur this osteoimmunological disorder; however, genetic abrogation of critical inflammasome components including caspase-1/11, ASC and NLRP3 did not rescue aberrant IL-1β production or osteolytic disease. These studies suggest that inflammasome-autonomous IL-1 signaling contributes to osteomyelitis, however future studies are needed to formally identify the alternative protease that is responsible for driving excessive IL-1β processing during this disease.
IL-1β-dependent responses to necrotic cells and silica crystals have also been found to occur largely in the absence of inflammasomes [7, 160]. Although silica-induced IL-1β production by macrophages, neutrophils and mast cells appears to require inflammasome activation under in vitro conditions, treatment of caspase-1/11 doubly deficient mice with either silica crystals or necrotic cells still results in substantial peritonitis. It was found that cathepsin C uniquely regulates inflammasome-independent IL-1β production in these settings, and genetic deletion of cathepsin C was found to markedly diminish myeloid cell recruitment and IL-1β levels in the peritoneal cavity of mice that received silica crystals or necrotic cells [160]. Cathepsin C is known to control the downstream activation of cathepsin G, elastase and proteinase-3 by removing two inhibitory amino acids from the N terminus of these zymogens [164, 166]. Thus, the exact nature of the serine protease that promotes IL-1β generation in response to necrotic cells and silica crystal still requires formal identification. It is possible that there may be functional redundancy between the specific proteases and that combined deletion is required to have a biological effect. Regardless, these findings highlight prominent roles for inflammasome-independent IL-1β production during responses to tissue damage and crystalline particulates. Furthermore, they also underscore the important point that in vitro settings do not always completely recapitulate the complexity of in vivo IL-1 regulation, and thus it is imperative to characterize IL-1 processing in physiological settings.
Caspase-1/11-independent IL-1β production has also been described to drive joint inflammation and disease in two separate models of arthritis [156, 157]. In the K/BxN serum transfer model of arthritis, it was shown that inflammatory joint destruction is dependent on IL-1 signaling. However, genetic deletion of caspase-1/11 in mice did not provide significant protection against joint destruction and caspase-1/11 deficient neutrophils and mast cells were found to secrete potent amounts of IL-1β even in the absence of inflammasomes. Instead, pharmacological inhibition of elastase and chymase were discovered to dampen aberrant IL-1β production and to limit the development of arthritis [157]. Inflammasome-independent IL-1β production has also been suggested to centrally promote disease in the streptococcal cell wall (SCW)-induced model of arthritis. In this study it was shown that wild-type and caspase-1 deficient mice develop inflammatory joint swelling to a similar extent in the SCW-arthritis model, and that genetic and pharmacological inhibition of the neutrophil serine protease PR3 is capable of attenuating IL-1β-mediated inflammation [156]. Collectively these studies indicate that IL-1β production by neutrophils and mast cells is not exclusively dependent on inflammasome activation, and that additional serine proteases can promote IL-1β-mediated inflammatory disease by processing proIL-1β.
Concluding Remarks
Infection and cellular injury are the two principal stimuli that provoke inflammatory disease. Much attention in recent years has been paid to define the receptors and signaling pathways that are responsible for pathogen recognition and subsequent inflammatory immune responses. In comparison, less is known about the molecular pathways that regulate sterile inflammatory responses. Sterile inflammation that results from aberrant cell death plays pivotal roles in the pathogenesis of numerous acute and chronic inflammatory diseases including atherosclerosis, multiple sclerosis, type 2 diabetes, myocardial infarction, arthritis, and multiple neurodegenerative diseases. Non-communicable chronic diseases that are potentiated by sterile inflammation have recently surpassed infectious diseases as the leading cause of worldwide morbidity and mortality. Thus, improved understanding of the sterile inflammatory process has emerged as one of the most important areas of biomedical investigation.
The identification of the central role of IL-1 signaling in inflammatory disease progression and the discovery of the specific danger signals that trigger IL-1-mediated inflammation has provided an important foundation in our understanding of the etiology of many human diseases. Although caspase-1 activation in canonical inflammasomes is the most well established mechanism for IL-1 production in many disease settings, recent studies now clearly demonstrate critical roles for additional pathways in IL-1-medated inflammation. For instance, aberrant IL-1α release that occurs in the absence of caspase-1/11 has been shown to specifically cause inflammation and tissue destruction in multiple disease models. Mounting evidence also suggests that IL-1β secretion is not solely dependent on caspase-1, and new regulators of IL-1β processing including caspase-8, caspase-11 and cathepsins have recently been described. Continued identification of novel pathways that contribute to non-canonical inflammasome activation and the discovery of additional mechanisms that contribute to inflammasome-independent IL-1 production will undoubtedly aid in the discovery of novel therapeutics to treat autoimmune and inflammatory disease.
Acknowledgements
We apologize to authors whose work could not be referenced in this review due to space limitations. We thank Prajwal Gurung and Si Ming Man for their helpful discussions. This work was supported by: the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR056296 (T.-D.K); the National Cancer Institute, part of the National Institutes of Health, under Award Number CA163507 (T.-D.K); the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health, under Award Number AI101935 (T.-D.K); and ALSAC.
Abbreviations
- IL
interleukin
- PAMPs
pathogen-associated molecular patterns
- DAMPs
danger-associated molecular patterns
- IL-1R
IL-1 receptor
- NLR
NOD-like receptor
- ALR
AIM2-like receptor
- TLR
Toll-like receptor
- CNS
central nervous system
- EAE
experimental autoimmune encephalomyelitis
- ALS
amyotrophic lateral sclerosis
- Tregs
regulatory T cells
- IAPP
islet amyloid polypeptide
- SLE
systemic lupus erythematosus
- RIP
receptor-interacting protein
- FADD
FAS-associated death domain
- TNFR1
TNF receptor 1
- IAPs
inhibitors of apoptosis proteins
- COPD
chronic obstructive pulmonary disease
- ER
endoplasmic reticulum
Footnotes
Competing interests statement
The authors declare no competing financial interests.
References
- 1.Lukens JR, Gross JM, Kanneganti TD. IL-1 family cytokines trigger sterile inflammatory disease. Front Immunol. 2012:3–315. doi: 10.3389/fimmu.2012.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson DM, Ross R. The neutrophilic leukocyte in wound repair a study with antineutrophil serum. J Clin Invest. 1972;51(8):2009–2023. doi: 10.1172/JCI107007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dovi JV, Szpaderska AM, DiPietro LA. Neutrophil function in the healing wound: adding insult to injury? Thromb Haemost. 2004;92(2):275–280. doi: 10.1160/TH03-11-0720. [DOI] [PubMed] [Google Scholar]
- 4.Lucas T, Waisman A, Ranjan R, Roes J, Krieg T, Muller W, Roers A, Eming SA. Differential roles of macrophages in diverse phases of skin repair. J Immunol. 2010;184(7):3964–7397. doi: 10.4049/jimmunol.0903356. [DOI] [PubMed] [Google Scholar]
- 5.Brancato SK, Albina JE. Wound macrophages as key regulators of repair: origin, phenotype, and function. The American journal of pathology. 2011;178(1):19–25. doi: 10.1016/j.ajpath.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rock KL, Latz E, Ontiveros F, Kono H. The sterile inflammatory response. Annu Rev Immunol. 2010;28:321–342. doi: 10.1146/annurev-immunol-030409-101311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med. 2007;13(7):851–856. doi: 10.1038/nm1603. [DOI] [PubMed] [Google Scholar]
- 8.Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12(3):204–212. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- 9.Lucin KM, Wyss-Coray T. Immune activation in brain aging and neurodegeneration: too much or too little? Neuron. 2009;64(1):110–122. doi: 10.1016/j.neuron.2009.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanneganti TD, Dixit VD. Immunological complications of obesity. Nat Immunol. 2012;13(8):707–712. doi: 10.1038/ni.2343. [DOI] [PubMed] [Google Scholar]
- 11.Lukens JR, Dixit VD, Kanneganti TD. Inflammasome activation in obesity-related inflammatory diseases and autoimmunity. Discov Med. 2011;12(62):65–74. [PMC free article] [PubMed] [Google Scholar]
- 12.Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. 2011;29:415–445. doi: 10.1146/annurev-immunol-031210-101322. [DOI] [PubMed] [Google Scholar]
- 13.Osborn O, Olefsky JM. The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med. 2012;18(3):363–374. doi: 10.1038/nm.2627. [DOI] [PubMed] [Google Scholar]
- 14.Kanneganti TD. Central roles of NLRs and inflammasomes in viral infection. Nat Rev Immunol. 2010;10(10):688–698. doi: 10.1038/nri2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lupfer C, Kanneganti TD. The role of inflammasome modulation in virulence. Virulence. 2012;3(3) doi: 10.4161/viru.20266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamkanfi M, Vande Walle L, Kanneganti TD. Deregulated inflammasome signaling in disease. Immunol Rev. 2011;243(1):163–173. doi: 10.1111/j.1600-065X.2011.01042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Z, Zaki MH, Vogel P, Gurung P, Finlay BB, Deng W, Lamkanfi M, Kanneganti TD. Role of inflammasomes in host defense against Citrobacter rodentium infection. J Biol Chem. 2012;b287(20):16955–16964. doi: 10.1074/jbc.M112.358705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw PJ, McDermott MF, Kanneganti TD. Inflammasomes and autoimmunity. Trends Mol Med. 2011;17(2):57–64. doi: 10.1016/j.molmed.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dinarello CA. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117(14):3720–3732. doi: 10.1182/blood-2010-07-273417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lukens JR, Vogel P, Johnson GR, Kelliher MA, Iwakura Y, Lamkanfi M, Kanneganti TD. RIP1-driven autoinflammation targets IL-1alpha independently of inflammasomes and RIP3. Nature. 2013 doi: 10.1038/nature12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orjalo AV, Bhaumik D, Gengler BK, Scott GK, Campisi J. Cell surface-bound IL-1alpha is an upstream regulator of the senescence-associated IL-6/IL-8 cytokine network. Proc Natl Acad Sci U S A. 2009;106(40):17031–17036. doi: 10.1073/pnas.0905299106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Paolo NC, Miao EA, Iwakura Y, Murali-Krishna K, Aderem A, Flavell RA, Papayannopoulou T, Shayakhmetov DM. Virus binding to a plasma membrane receptor triggers interleukin-1 alpha-mediated proinflammatory macrophage response in vivo. Immunity. 2009;31(1):110–121. doi: 10.1016/j.immuni.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rider P, Carmi Y, Guttman O, Braiman A, Cohen I, Voronov E, White MR, Dinarello CA, Apte RN. IL-1alpha and IL-1beta recruit different myeloid cells and promote different stages of sterile inflammation. J Immunol. 2011;187(9):4835–4843. doi: 10.4049/jimmunol.1102048. [DOI] [PubMed] [Google Scholar]
- 24.Chu E, Rosenwasser LJ, Dinarello CA, Lareau M, Geha RS. Role of interleukin 1 in antigen-specific T cell proliferation. J Immunol. 1984;132(3):1311–1316. [PubMed] [Google Scholar]
- 25.Falkoff RJ, Muraguchi A, Hong JX, Butler JL, Dinarello CA, Fauci AS. The effects of interleukin 1 on human B cell activation and proliferation. J Immunol. 1983;131(2):801–805. [PubMed] [Google Scholar]
- 26.McCandless EE, Budde M, Lees JR, Dorsey D, Lyng E, Klein RS. IL-1R signaling within the central nervous system regulates CXCL12 expression at the blood-brain barrier and disease severity during experimental autoimmune encephalomyelitis. J Immunol. 2009;183(1):613–620. doi: 10.4049/jimmunol.0802258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao DA, Eid RE, Qin L, Yi T, Kirkiles-Smith NC, Tellides G, Pober JS. Interleukin (IL)-1 promotes allogeneic T cell intimal infiltration and IL-17 production in a model of human artery rejection. The Journal of experimental medicine. 2008;205(13):3145–3158. doi: 10.1084/jem.20081661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishio N, Ito S, Suzuki H, Isobe K. Antibodies to wounded tissue enhance cutaneous wound healing. Immunology. 2009;128(3):369–380. doi: 10.1111/j.1365-2567.2009.03119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lund FE. Cytokine-producing B lymphocytes-key regulators of immunity. Curr Opin Immunol. 2008;20(3):332–328. doi: 10.1016/j.coi.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalampokis I, Yoshizaki A, Tedder TF. IL-10-producing regulatory B cells (B10 cells) in autoimmune disease. Arthritis Res Ther. 2013;15(Suppl 1):S1. doi: 10.1186/ar3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Toulon A, Breton L, Taylor KR, Tenenhaus M, Bhavsar D, Lanigan C, Rudolph R, Jameson J, Havran WL. A role for human skin-resident T cells in wound healing. The Journal of experimental medicine. 2009;206(4):743–750. doi: 10.1084/jem.20081787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burzyn D, Kuswanto W, Kolodin D, Shadrach JL, Cerletti M, Jang Y, Sefik E, Tan TG, Wagers AJ, Benoist C, Mathis D. A special population of regulatory T cells potentiates muscle repair. Cell. 2013;155(6):1282–1295. doi: 10.1016/j.cell.2013.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutton C, Brereton C, Keogh B, Mills KH, Lavelle EC. A crucial role for interleukin (IL)-1 in the induction of IL-17-producing T cells that mediate autoimmune encephalomyelitis. J Exp Med. 2006;203(7):1685–1691. doi: 10.1084/jem.20060285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chung Y, Chang SH, Martinez GJ, Yang XO, Nurieva R, Kang HS, Ma L, Watowich SS, Jetten AM, Tian Q, Dong C. Critical regulation of early Th17 cell differentiation by interleukin-1 signaling. Immunity. 2009;30(4):576–587. doi: 10.1016/j.immuni.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matsuki T, Nakae S, Sudo K, Horai R, Iwakura Y. Abnormal T cell activation caused by the imbalance of the IL-1/IL-1R antagonist system is responsible for the development of experimental autoimmune encephalomyelitis. Int Immunol. 2006;18(2):399–407. doi: 10.1093/intimm/dxh379. [DOI] [PubMed] [Google Scholar]
- 36.Sutton CE, Lalor SJ, Sweeney CM, Brereton CF, Lavelle EC, Mills KH. Interleukin-1 and IL-23 induce innate IL-17 production from gammadelta T cells, amplifying Th17 responses and autoimmunity. Immunity. 2009;31(2):331–341. doi: 10.1016/j.immuni.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Lukens JR, Barr MJ, Chaplin DD, Chi H, Kanneganti TD. Inflammasome-derived IL-1beta regulates the production of GM-CSF by CD4(+) T cells and gammadelta T cells. J Immunol. 2012;188(7):3107–3115. doi: 10.4049/jimmunol.1103308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lukens JR, Gross JM, Calabrese C, Iwakura Y, Lamkanfi M, Vogel P, Kanneganti TD. Critical role for inflammasome-independent IL-1beta production in osteomyelitis. Proc Natl Acad Sci U S A. 2014;111(3):1066–1071. doi: 10.1073/pnas.1318688111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cassel SL, Janczy JR, Bing X, Wilson SP, Olivier AK, Otero JE, Iwakura Y, Shayakhmetov DM, Bassuk AG, Abu-Amer Y, Brogden KA, Burns TL, Sutterwala FS, Ferguson PJ. Inflammasome-independent IL-1beta mediates autoinflammatory disease in Pstpip2-deficient mice. Proc Natl Acad Sci U S A. 2014;111(3):1072–1077. doi: 10.1073/pnas.1318685111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yazdi AS, Guarda G, Riteau N, Drexler SK, Tardivel A, Couillin I, Tschopp J. Nanoparticles activate the NLR pyrin domain containing 3 (Nlrp3) inflammasome and cause pulmonary inflammation through release of IL-1alpha and IL-1beta. Proc Natl Acad Sci U S A. 2010;107(45):19449–19454. doi: 10.1073/pnas.1008155107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freigang S, Ampenberger F, Weiss A, Kanneganti TD, Iwakura Y, Hersberger M, Kopf M. Fatty acid-induced mitochondrial uncoupling elicits inflammasome-independent IL-1alpha and sterile vascular inflammation in atherosclerosis. Nat Immunol. 2013;14(10):1045–1053. doi: 10.1038/ni.2704. [DOI] [PubMed] [Google Scholar]
- 42.Barry KC, Fontana MF, Portman JL, Dugan AS, Vance RE. IL-1alpha signaling initiates the inflammatory response to virulent Legionella pneumophila in vivo. J Immunol. 2013;190(12):6329–6339. doi: 10.4049/jimmunol.1300100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen I, Rider P, Carmi Y, Braiman A, Dotan S, White MR, Voronov E, Martin MU, Dinarello CA, Apte RN. Differential release of chromatin-bound IL-1alpha discriminates between necrotic and apoptotic cell death by the ability to induce sterile inflammation. Proc Natl Acad Sci U S A. 2010;107(6):2574–2579. doi: 10.1073/pnas.0915018107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berda-Haddad Y, Robert S, Salers P, Zekraoui L, Farnarier C, Dinarello CA, Dignat-George F, Kaplanski G. Sterile inflammation of endothelial cell-derived apoptotic bodies is mediated by interleukin-1alpha. Proc Natl Acad Sci U S A. 2011;108(51):20684–20689. doi: 10.1073/pnas.1116848108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lukens JR, Vogel P, Johnson GR, Kelliher MA, Iwakura Y, Lamkanfi M, Kanneganti TD. RIP1-driven autoinflammation targets IL-1alpha independently of inflammasomes and RIP3. Nature. 2013;498(7453):224–227. doi: 10.1038/nature12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boutin H, LeFeuvre RA, Horai R, Asano M, Iwakura Y, Rothwell NJ. Role of IL-1alpha and IL-1beta in ischemic brain damage. J Neurosci. 2001;21(15):5528–5534. doi: 10.1523/JNEUROSCI.21-15-05528.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thornton P, McColl BW, Greenhalgh A, Denes A, Allan SM, Rothwell NJ. Platelet interleukin-1alpha drives cerebrovascular inflammation. Blood. 2010;115(17):3632–3639. doi: 10.1182/blood-2009-11-252643. [DOI] [PubMed] [Google Scholar]
- 48.Luheshi NM, Kovacs KJ, Lopez-Castejon G, Brough D, Denes A. Interleukin-1alpha expression precedes IL-1beta after ischemic brain injury and is localised to areas of focal neuronal loss and penumbral tissues. J Neuroinflammation. 2011;8:186. doi: 10.1186/1742-2094-8-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shito M, Wakabayashi G, Ueda M, Shimazu M, Shirasugi N, Endo M, Mukai M, Kitajima M. Interleukin 1 receptor blockade reduces tumor necrosis factor production, tissue injury, and mortality after hepatic ischemiareperfusion in the rat. Transplantation. 1997;63(1):143–148. doi: 10.1097/00007890-199701150-00026. [DOI] [PubMed] [Google Scholar]
- 50.Abbate A, Salloum FN, Vecile E, Das A, Hoke NN, Straino S, Biondi-Zoccai GG, Houser JE, Qureshi IZ, Ownby ED, Gustini E, Biasucci LM, Severino A, Capogrossi MC, Vetrovec GW, Crea F, Baldi A, Kukreja RC, Dobrina A. Anakinra, a recombinant human interleukin-1 receptor antagonist, inhibits apoptosis in experimental acute myocardial infarction. Circulation. 2008;117(20):2670–2683. doi: 10.1161/CIRCULATIONAHA.107.740233. [DOI] [PubMed] [Google Scholar]
- 51.Pomerantz BJ, Reznikov LL, Harken AH, Dinarello CA. Inhibition of caspase 1 reduces human myocardial ischemic dysfunction via inhibition of IL-18 and IL-1beta. Proc Natl Acad Sci U S A. 2001;98(5):2871–2876. doi: 10.1073/pnas.041611398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Green MC, Shultz LD. Motheaten an immunodeficient mutant of the mouse. I. Genetics and pathology. J Hered. 1975;66(5):250–258. doi: 10.1093/oxfordjournals.jhered.a108625. [DOI] [PubMed] [Google Scholar]
- 53.Shultz LD, Coman DR, Bailey CL, Beamer WG, Sidman CL. "Viable motheaten," a new allele at the motheaten locus. I. Pathology. Am J Pathol. 1984;116(2):179–1792. [PMC free article] [PubMed] [Google Scholar]
- 54.Shultz LD, Schweitzer PA, Rajan TV, Yi T, Ihle JN, Matthews RJ, Thomas ML, Beier DR. Mutations at the murine motheaten locus are within the hematopoietic cell protein-tyrosine phosphatase (Hcph) gene. Cell. 1993;73(7):1445–1454. doi: 10.1016/0092-8674(93)90369-2. [DOI] [PubMed] [Google Scholar]
- 55.Tsui HW, Siminovitch KA, Souza Lde, Tsui FW. Motheaten and viable motheaten mice have mutations in the haematopoietic cell phosphatase gene. Nat Genet. 1993;4(2):124–129. doi: 10.1038/ng0693-124. [DOI] [PubMed] [Google Scholar]
- 56.Abram CL, Roberge GL, Pao LI, Neel BG, Lowell CA. Distinct roles for neutrophils and dendritic cells in inflammation and autoimmunity in motheaten mice. Immunity. 2013;38(3):489–501. doi: 10.1016/j.immuni.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nesterovitch AB, Szanto S, Gonda A, Bardos T, Kis-Toth K, Adarichev VA, Olasz K, Ghassemi-Najad S, Hoffman MD, Tharp MD, Mikecz K, Glant TT. Spontaneous insertion of a b2 element in the ptpn6 gene drives a systemic autoinflammatory disease in mice resembling neutrophilic dermatosis in humans. Am J Pathol. 2011;178(4):1701–1714. doi: 10.1016/j.ajpath.2010.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Croker BA, Lawson BR, Rutschmann S, Berger M, Eidenschenk C, Blasius AL, Moresco EM, Sovath S, Cengia L, Shultz LD, Theofilopoulos AN, Pettersson S, Beutler BA. Inflammation and autoimmunity caused by a SHP1 mutation depend on IL-1, MyD88, and a microbial trigger. Proc Natl Acad Sci U S A. 2008;105(39):15028–15033. doi: 10.1073/pnas.0806619105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, Zurawski G, Moshrefi M, Qin J, Li X, Gorman DM, Bazan JF, Kastelein RA. IL-33 an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23(5):479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 60.Buryskova M, Pospisek M, Grothey A, Simmet T, Burysek L. Intracellular interleukin-1alpha functionally interacts with histone acetyltransferase complexes. J Biol Chem. 2004;279(6):4017–4026. doi: 10.1074/jbc.M306342200. [DOI] [PubMed] [Google Scholar]
- 61.Werman A, Werman-Venkert R, White R, Lee JK, Werman B, Krelin Y, Voronov E, Dinarello CA, Apte RN. The precursor form of IL-1alpha is an intracrine proinflammatory activator of transcription. Proc Natl Acad Sci U S A. 2004;101(8):2434–2439. doi: 10.1073/pnas.0308705101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139–162. doi: 10.1146/annurev-immunol-030409-101323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ali S, Mohs A, Thomas M, Klare J, Ross R, Schmitz ML, Martin MU. The dual function cytokine IL-33 interacts with the transcription factor NF- kappaB to dampen NF-kappaB-stimulated gene transcription. J Immunol. 2011;187(4):1609–1616. doi: 10.4049/jimmunol.1003080. [DOI] [PubMed] [Google Scholar]
- 64.Ravichandran KS. Find-me and eat-me signals in apoptotic cell clearance: progress and conundrums. The Journal of experimental medicine. 2010;207(9):1807–1817. doi: 10.1084/jem.20101157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Luheshi NM, McColl BW, Brough D. Nuclear retention of IL-1 alpha by necrotic cells: a mechanism to dampen sterile inflammation. Eur J Immunol. 2009;39(11):2973–2980. doi: 10.1002/eji.200939712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, MacDonald K, Speert D, Fernandes-Alnemri T, Wu J, Monks BG, Fitzgerald KA, Hornung V, Latz E. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol. 2009;183(2):787–791. doi: 10.4049/jimmunol.0901363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim B, Lee Y, Kim E, Kwak A, Ryoo S, Bae SH, Azam T, Kim S, Dinarello CA. The Interleukin-1alpha Precursor is Biologically Active and is Likely a Key Alarmin in the IL-1 Family of Cytokines. Front Immunol. 2013;4:391. doi: 10.3389/fimmu.2013.00391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fettelschoss A, Kistowska M, LeibundGut-Landmann S, Beer HD, Johansen P, Senti G, Contassot E, Bachmann MF, French LE, Oxenius A, Kundig TM. Inflammasome activation and IL-1beta target IL-1alpha for secretion as opposed to surface expression. Proc Natl Acad Sci U S A. 2011;108(44):18055–18060. doi: 10.1073/pnas.1109176108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, Newton K, Qu Y, Liu J, Heldens S, Zhang J, Lee WP, Roose-Girma M, Dixit VM. Non-canonical inflammasome activation targets caspase-11. Nature. 479(7371):117–121. doi: 10.1038/nature10558. [DOI] [PubMed] [Google Scholar]
- 70.Kobayashi Y, Yamamoto K, Saido T, Kawasaki H, Oppenheim JJ, Matsushima K. Identification of calcium-activated neutral protease as a processing enzyme of human interleukin 1 alpha. Proc Natl Acad Sci U S A. 1990;87(14):5548–5552. doi: 10.1073/pnas.87.14.5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carruth LM, Demczuk S, Mizel SB. Involvement of a calpain-like protease in the processing of the murine interleukin 1 alpha precursor. J Biol Chem. 1991;266(19):12162–12167. [PubMed] [Google Scholar]
- 72.Gross O, Yazdi AS, Thomas CJ, Masin M, Heinz LX, Guarda G, Quadroni M, Drexler SK, Tschopp J. Inflammasome activators induce interleukin-1alpha secretion via distinct pathways with differential requirement for the protease function of caspase-1. Immunity. 2012;36(3):388–400. doi: 10.1016/j.immuni.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 73.Zheng Y, Humphry M, Maguire JJ, Bennett MR, Clarke MC. Intracellular interleukin-1 receptor 2 binding prevents cleavage and activity of interleukin-1alpha, controlling necrosis-induced sterile inflammation. Immunity. 2013;38(2):285–295. doi: 10.1016/j.immuni.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kanneganti TD, Ozoren N, Body-Malapel M, Amer A, Park JH, Franchi L, Whitfield J, Barchet W, Colonna M, Vandenabeele P, Bertin J, Coyle A, Grant EP, Akira S, Nunez G. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 2006;440(7081):233–236. doi: 10.1038/nature04517. [DOI] [PubMed] [Google Scholar]
- 75.Franchi L, Eigenbrod T, Nunez G. Cutting edge: TNF-alpha mediates sensitization to ATP and silica via the NLRP3 inflammasome in the absence of microbial stimulation. J Immunol. 2009;183(2):792–796. doi: 10.4049/jimmunol.0900173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Van Opdenbosch N, Gurung P, Vande Walle L, Fossoul A, Kanneganti TD, Lamkanfi M. Activation of the NLRP1b inflammasome independently of ASC-mediated caspase-1 autoproteolysis and speck formation. Nat Commun. 2014;5:3209. doi: 10.1038/ncomms4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frew BC, Joag VR, Mogridge J. Proteolytic processing of Nlrp1b is required for inflammasome activity. PLoS Pathog. 2012;8(4):e1002659. doi: 10.1371/journal.ppat.1002659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nour AM, Yeung YG, Santambrogio L, Boyden ED, Stanley ER, Brojatsch J. Anthrax lethal toxin triggers the formation of a membrane-associated inflammasome complex in murine macrophages. Infect Immun. 2009;77(3):1262–1271. doi: 10.1128/IAI.01032-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qu Y, Misaghi S, Izrael-Tomasevic A, Newton K, Gilmour LL, Lamkanfi M, Louie S, Kayagaki N, Liu J, Komuves L, Cupp JE, Arnott D, Monack D, Dixit VM. Phosphorylation of NLRC4 is critical for inflammasome activation. Nature. 2012;490(7421):539–542. doi: 10.1038/nature11429. [DOI] [PubMed] [Google Scholar]
- 80.Zhao Y, Yang J, Shi J, Gong YN, Lu Q, Xu H, Liu L, Shao F. The NLRC4 inflammasome receptors for bacterial flagellin and type III secretion apparatus. Nature. 2011;477(7366):596–600. doi: 10.1038/nature10510. [DOI] [PubMed] [Google Scholar]
- 81.Mariathasan S, Newton K, Monack DM, Vucic D, French DM, Lee WP, Roose-Girma M, Erickson S, Dixit VM. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 2004;430(6996):213–218. doi: 10.1038/nature02664. [DOI] [PubMed] [Google Scholar]
- 82.Miao EA, Alpuche-Aranda CM, Dors M, Clark AE, Bader MW, Miller SI, Aderem A. Cytoplasmic flagellin activates caspase-1 and secretion of interleukin 1beta via Ipaf. Nat Immunol. 2006;7(6):569–575. doi: 10.1038/ni1344. [DOI] [PubMed] [Google Scholar]
- 83.Franchi L, Amer A, Body-Malapel M, Kanneganti TD, Ozoren N, Jagirdar R, Inohara N, Vandenabeele P, Bertin J, Coyle A, Grant EP, Nunez G. Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1beta in salmonella-infected macrophages. Nat Immunol. 2006;7(6):576–582. doi: 10.1038/ni1346. [DOI] [PubMed] [Google Scholar]
- 84.Kofoed EM, Vance RE. Innate immune recognition of bacterial ligands by NAIPs determines inflammasome specificity. Nature. 2011;477(7366):592–595. doi: 10.1038/nature10394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ataide MA, Andrade WA, Zamboni DS, Wang D, Mdo CSouza, Franklin BS, Elian S, Martins FS, Pereira D, Reed G, Fitzgerald KA, Golenbock DT, Gazzinelli RT. Malaria-induced NLRP12/NLRP3-dependent caspase-1 activation mediates inflammation and hypersensitivity to bacterial superinfection. PLoS Pathog. 2014;10(1):e1003885. doi: 10.1371/journal.ppat.1003885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vladimer GI, Weng D, Paquette SW, Vanaja SK, Rathinam VA, Aune MH, Conlon JE, Burbage JJ, Proulx MK, Liu Q, Reed G, Mecsas JC, Iwakura Y, Bertin J, Goguen JD, Fitzgerald KA, Lien E. The NLRP12 inflammasome recognizes Yersinia pestis. Immunity. 2012;37(1):96–107. doi: 10.1016/j.immuni.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Khare S, Dorfleutner A, Bryan NB, Yun C, Radian AD, Almeida Lde, Rojanasakul Y, Stehlik C. An NLRP7-containing inflammasome mediates recognition of microbial lipopeptides in human macrophages. Immunity. 2012;36(3):464–476. doi: 10.1016/j.immuni.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Anand PK, Malireddi RK, Lukens JR, Vogel P, Bertin J, Lamkanfi M, Kanneganti TD. NLRP6 negatively regulates innate immunity and host defence against bacterial pathogens. Nature. 2012;488(7411):389–393. doi: 10.1038/nature11250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zaki MH, Man SM, Vogel P, Lamkanfi M, Kanneganti TD. Salmonella exploits NLRP12-dependent innate immune signaling to suppress host defenses during infection. Proc Natl Acad Sci U S A. 2014;111(1):385–390. doi: 10.1073/pnas.1317643111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zaki MH, Vogel P, Malireddi RK, Body-Malapel M, Anand PK, Bertin J, Green DR, Lamkanfi M, Kanneganti TD. The NOD-like receptor NLRP12 attenuates colon inflammation and tumorigenesis. Cancer Cell. 2011;20(5):649–660. doi: 10.1016/j.ccr.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Allen IC, Wilson JE, Schneider M, Lich JD, Roberts RA, Arthur JC, Woodford RM, Davis BK, Uronis JM, Herfarth HH, Jobin C, Rogers AB, Ting JP. NLRP12 suppresses colon inflammation and tumorigenesis through the negative regulation of noncanonical NF-kappaB signaling. Immunity. 2012;36(5):742–754. doi: 10.1016/j.immuni.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Normand S, Delanoye-Crespin A, Bressenot A, Huot L, Grandjean T, Peyrin-Biroulet L, Lemoine Y, Hot D, Chamaillard M. Nod-like receptor pyrin domain-containing protein 6 (NLRP6) controls epithelial self-renewal and colorectal carcinogenesis upon injury. Proc Natl Acad Sci U S A. 2011;108(23):9601–9606. doi: 10.1073/pnas.1100981108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Elinav E, Strowig T, Kau AL, Henao-Mejia J, Thaiss CA, Booth CJ, Peaper DR, Bertin J, Eisenbarth SC, Gordon JI, Flavell RA. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell. 2011;145(5):745–757. doi: 10.1016/j.cell.2011.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen GY, Liu M, Wang F, Bertin J, Nunez G. A functional role for Nlrp6 in intestinal inflammation and tumorigenesis. J Immunol. 2011;186(12):7187–7194. doi: 10.4049/jimmunol.1100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hu B, Elinav E, Huber S, Strowig T, Hao L, Hafemann A, Jin C, Wunderlich C, Wunderlich T, Eisenbarth SC, Flavell RA. Microbiota-induced activation of epithelial IL-6 signaling links inflammasome-driven inflammation with transmissible cancer. Proc Natl Acad Sci U S A. 2013;110(24):9862–9867. doi: 10.1073/pnas.1307575110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fernandes-Alnemri T, Yu JW, Datta P, Wu J, Alnemri ES. AIM2 activates the inflammasome and cell death in response to cytoplasmic DNA. Nature. 2009;458(7237):509–513. doi: 10.1038/nature07710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hornung V, Ablasser A, Charrel-Dennis M, Bauernfeind F, Horvath G, Caffrey DR, Latz E, Fitzgerald KA. AIM2 recognizes cytosolic dsDNA and forms a caspase-1-activating inflammasome with ASC. Nature. 2009;458(7237):514–518. doi: 10.1038/nature07725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Roberts TL, Idris A, Dunn JA, Kelly GM, Burnton CM, Hodgson S, Hardy LL, Garceau V, Sweet MJ, Ross IL, Hume DA, Stacey KJ. HIN-200 proteins regulate caspase activation in response to foreign cytoplasmic DNA. Science. 2009;323(5917):1057–1060. doi: 10.1126/science.1169841. [DOI] [PubMed] [Google Scholar]
- 99.Kerur N, Veettil MV, Sharma-Walia N, Bottero V, Sadagopan S, Otageri P, Chandran B. IFI16 acts as a nuclear pathogen sensor to induce the inflammasome in response to Kaposi Sarcoma-associated herpesvirus infection. Cell Host Microbe. 2011;9(5):363–375. doi: 10.1016/j.chom.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Unterholzner L, Keating SE, Baran M, Horan KA, Jensen SB, Sharma S, Sirois CM, Jin T, Latz E, Xiao TS, Fitzgerald KA, Paludan SR, Bowie AG. IFI16 is an innate immune sensor for intracellular DNA. Nat Immunol. 2010;11(11):997–1004. doi: 10.1038/ni.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365(22):2110–2021. doi: 10.1056/NEJMra1100359. [DOI] [PubMed] [Google Scholar]
- 102.Dombrowski Y, Peric M, Koglin S, Kammerbauer C, Goss C, Anz D, Simanski M, Glaser R, Harder J, Hornung V, Gallo RL, Ruzicka T, Besch R, Schauber J. Cytosolic DNA triggers inflammasome activation in keratinocytes in psoriatic lesions. Sci Transl Med. 2011;3(82):82ra38. doi: 10.1126/scitranslmed.3002001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Diana J, Simoni Y, Furio L, Beaudoin L, Agerberth B, Barrat F, Lehuen A. Crosstalk between neutrophils, B-1a cells and plasmacytoid dendritic cells initiates autoimmune diabetes. Nat Med. 2013;19(1):65–73. doi: 10.1038/nm.3042. [DOI] [PubMed] [Google Scholar]
- 104.Kawane K, Ohtani M, Miwa K, Kizawa T, Kanbara Y, Yoshioka Y, Yoshikawa H, Nagata S. Chronic polyarthritis caused by mammalian DNA that escapes from degradation in macrophages. Nature. 2006;443(7114):998–1002. doi: 10.1038/nature05245. [DOI] [PubMed] [Google Scholar]
- 105.Stienstra R, Joosten LA, Koenen T, Bvan Tits JA, van Diepen SA, van den Berg PC, Rensen PJ, Voshol G, Fantuzzi A, Hijmans S, Kersten M, Muller WB, van den Berg N, van Rooijen N, Wabitsch M, Kullberg BJ, van der Meer JW, Kanneganti T, Tack CJ, Netea MG. The inflammasome-mediated caspase-1 activation controls adipocyte differentiation and insulin sensitivity. Cell Metab. 2010;12(6):593–605. doi: 10.1016/j.cmet.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stienstra R, Diepen JAvan, Tack CJ, Zaki MH, van de Veerdonk JA, Perera D, Neale GA, Hooiveld GJ, Hijmans A, Vroegrijk I, van den Berg S, Romijn J, Rensen PC, Joosten LA, Netea MG, Kanneganti TD. Inflammasome is a central player in the induction of obesity and insulin resistance. Proc Natl Acad Sci U S A. 2011;108(37):15324–15329. doi: 10.1073/pnas.1100255108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, Ravussin E, Stephens JM, Dixit VD. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17(2):179–188. doi: 10.1038/nm.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Masters SL, Dunne A, Subramanian SL, Hull RL, Tannahill GM, Sharp FA, Becker C, Franchi L, Yoshihara E, Chen Z, Mullooly N, Mielke LA, Harris J, Coll RC, Mills KH, Mok KH, Newsholme P, Nunez G, Yodoi J, Kahn SE, Lavelle EC, O'Neill LA. Activation of the NLRP3 inflammasome by islet amyloid polypeptide provides a mechanism for enhanced IL-1beta in type 2 diabetes. Nat Immunol. 2010;11(10):897–904. doi: 10.1038/ni.1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wen H, Gris D, Lei Y, Jha S, Zhang L, Huang MT, Brickey WJ, Ting JP. Fatty acid-induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Nat Immunol. 2011;12(5):408–415. doi: 10.1038/ni.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Henao-Mejia J, Elinav E, Jin C, Hao L, Mehal WZ, Strowig T, Thaiss CA, Kau AL, Eisenbarth SC, Jurczak MJ, Camporez JP, Shulman GI, Gordon JI, Hoffman HM, Flavell RA. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature. 2012;482(7384):179–185. doi: 10.1038/nature10809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nunez G, Schnurr M, Espevik T, Lien E, Fitzgerald KA, Rock KL, Moore KJ, Wright SD, Hornung V, Latz E. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464(7293):1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Halle A, Hornung V, Petzold GC, Stewart CR, Monks BG, Reinheckel T, Fitzgerald KA, Latz E, Moore KJ, Golenbock DT. The NALP3 inflammasome is involved in the innate immune response to amyloid-beta. Nat Immunol. 2008;9(8):857–865. doi: 10.1038/ni.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Heneka MT, Kummer MP, Stutz A, Delekate A, Schwartz S, Vieira-Saecker A, Griep A, Axt D, Remus A, Tzeng TC, Gelpi E, Halle A, Korte M, Latz E, Golenbock DT. NLRP3 is activated in Alzheimer's disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493(7434):674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Barnes PJ. New anti-inflammatory targets for chronic obstructive pulmonary disease. Nat Rev Drug Discov. 2013;12(7):543–559. doi: 10.1038/nrd4025. [DOI] [PubMed] [Google Scholar]
- 115.Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440(7081):237–241. doi: 10.1038/nature04516. [DOI] [PubMed] [Google Scholar]
- 116.Hornung V, Bauernfeind F, Halle A, Samstad EO, Kono H, Rock KL, Fitzgerald KA, Latz E. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat Immunol. 2008;9(8):847–856. doi: 10.1038/ni.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dostert C, Petrilli V, Bruggen RVan, Steele C, Mossman BT, Tschopp J. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science. 2008;320(5876):674–677. doi: 10.1126/science.1156995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cassel SL, Eisenbarth SC, Iyer SS, Sadler JJ, Colegio OR, Tephly LA, Carter AB, Rothman PB, Flavell RA, Sutterwala FS. The Nalp3 inflammasome is essential for the development of silicosis. Proc Natl Acad Sci U S A. 2008;105(26):9035–9040. doi: 10.1073/pnas.0803933105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, Newton K, Qu Y, Liu J, Heldens S, Zhang J, Lee WP, Roose-Girma M, Dixit VM. Non-canonical inflammasome activation targets caspase-11. Nature. 2011;479(7371):117–121. doi: 10.1038/nature10558. [DOI] [PubMed] [Google Scholar]
- 120.Furuya T, Hayakawa H, Yamada M, Yoshimi K, Hisahara S, Miura M, Mizuno Y, Mochizuki H. Caspase-11 mediates inflammatory dopaminergic cell death in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson's disease. J Neurosci. 2004;24(8):1865–1872. doi: 10.1523/JNEUROSCI.3309-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hisahara S, Yuan J, Momoi T, Okano H, Miura M. Caspase-11 mediates oligodendrocyte cell death and pathogenesis of autoimmune-mediated demyelination. The Journal of experimental medicine. 2001;193(1):111–122. doi: 10.1084/jem.193.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gurung P, Malireddi RK, Anand PK, Demon D, Vande Walle L, Liu Z, Vogel P, Lamkanfi M, Kanneganti TD. Toll or interleukin-1 receptor (TIR) domain-containing adaptor inducing interferon-beta (TRIF)-mediated caspase-11 protease production integrates Toll-like receptor 4 (TLR4) protein- and Nlrp3 inflammasome-mediated host defense against enteropathogens. J Biol Chem. 2012;287(41):34474–34483. doi: 10.1074/jbc.M112.401406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rathinam VA, Vanaja SK, Waggoner L, Sokolovska A, Becker C, Stuart LM, Leong JM, Fitzgerald KA. TRIF licenses caspase-11-dependent NLRP3 inflammasome activation by gram-negative bacteria. Cell. 2012;150(3):606–619. doi: 10.1016/j.cell.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aachoui Y, Leaf IA, Hagar JA, Fontana MF, Campos CG, Zak DE, Tan MH, Cotter PA, Vance RE, Aderem A, Miao EA. Caspase-11 protects against bacteria that escape the vacuole. Science. 2013;339(6122):975–978. doi: 10.1126/science.1230751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hagar JA, Powell DA, Aachoui Y, Ernst RK, Miao EA. Cytoplasmic LPS activates caspase-11: implications in TLR4-independent endotoxic shock. Science. 2013;341(6151):1250–1253. doi: 10.1126/science.1240988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kayagaki N, Wong MT, Stowe IB, Ramani SR, Gonzalez LC, Akashi-Takamura S, Miyake K, Zhang J, Lee WP, Muszynski A, Forsberg LS, Carlson RW, Dixit VM. Noncanonical inflammasome activation by intracellular LPS independent of TLR4. Science. 2013;341(6151):1246–1249. doi: 10.1126/science.1240248. [DOI] [PubMed] [Google Scholar]
- 127.Case CL, Kohler LJ, Lima JB, Strowig T, Zoete MRde, Flavell RA, Zamboni DS, Roy CR. Caspase-11 stimulates rapid flagellin-independent pyroptosis in response to Legionella pneumophila. Proc Natl Acad Sci U S A. 2013;110(5):1851–1856. doi: 10.1073/pnas.1211521110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Broz P, Ruby T, Belhocine K, Bouley DM, Kayagaki N, Dixit VM, Monack DM. Caspase-11 increases susceptibility to Salmonella infection in the absence of caspase-1. Nature. 2012;490(7419):288–291. doi: 10.1038/nature11419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Oberst A, Green DR. It cuts both ways: reconciling the dual roles of caspase 8 in cell death and survival. Nat Rev Mol Cell Biol. 2011;12(11):757–763. doi: 10.1038/nrm3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Maelfait J, Vercammen E, Janssens S, Schotte P, Haegman M, Magez S, Beyaert R. Stimulation of Toll-like receptor 3 and 4 induces interleukin-1beta maturation by caspase-8. The Journal of experimental medicine. 2008;205(9):1967–1973. doi: 10.1084/jem.20071632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kaiser WJ, Upton JW, Long AB, Livingston-Rosanoff D, Daley-Bauer LP, Hakem R, Caspary T, Mocarski ES. RIP3 mediates the embryonic lethality of caspase-8-deficient mice. Nature. 2011;471(7338):368–372. doi: 10.1038/nature09857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dillon CP, Oberst A, Weinlich R, Janke LJ, Kang TB, Ben-Moshe T, Mak TW, Wallach D, Green DR. Survival function of the FADD-CASPASE-8-cFLIP(L) complex. Cell Rep. 2012;1(5):401–407. doi: 10.1016/j.celrep.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Oberst A, Dillon CP, Weinlich R, McCormick LL, Fitzgerald P, Pop C, Hakem R, Salvesen GS, Green DR. Catalytic activity of the caspase-8-FLIP(L) complex inhibits RIPK3-dependent necrosis. Nature. 2011;471(7338):363–367. doi: 10.1038/nature09852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gurung P, Anand PK, Malireddi RK, Vande Walle L, Opdenbosch NVan, Dillon CP, Weinlich R, Green DR, Lamkanfi M, Kanneganti TD. FADD and Caspase-8 Mediate Priming and Activation of the Canonical and Noncanonical Nlrp3 Inflammasomes. J Immunol. 2014;192(4):1835–1846. doi: 10.4049/jimmunol.1302839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shenderov K, Riteau N, Yip R, Mayer-Barber KD, Oland S, Hieny S, Fitzgerald P, Oberst A, Dillon CP, Green DR, Cerundolo V, Sher A. Cutting Edge: Endoplasmic Reticulum Stress Licenses Macrophages To Produce Mature IL-1beta in Response to TLR4 Stimulation through a Caspase-8- and TRIF-Dependent Pathway. J Immunol. 2014 doi: 10.4049/jimmunol.1302549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kawasaki N, Asada R, Saito A, Kanemoto S, Imaizumi K. Obesity-induced endoplasmic reticulum stress causes chronic inflammation in adipose tissue. Sci Rep. 2012;2:799. doi: 10.1038/srep00799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cnop M, Foufelle F, Velloso LA. Endoplasmic reticulum stress, obesity and diabetes. Trends Mol Med. 2012;18(1):59–68. doi: 10.1016/j.molmed.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 138.Ozcan U, Cao Q, Yilmaz E, Lee AH, Iwakoshi NN, Ozdelen E, Tuncman G, Gorgun C, Glimcher LH, Hotamisligil GS. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004;306(5695):457–461. doi: 10.1126/science.1103160. [DOI] [PubMed] [Google Scholar]
- 139.Ozcan U, Yilmaz E, Ozcan L, Furuhashi M, Vaillancourt E, Smith RO, Gorgun CZ, Hotamisligil GS. Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science. 2006;313(5790):1137–40. doi: 10.1126/science.1128294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bossaller L, Chiang PI, Schmidt-Lauber C, Ganesan S, Kaiser WJ, Rathinam VA, Mocarski ES, Subramanian D, Green DR, Silverman N, Fitzgerald KA, Marshak-Rothstein A, Latz E. Cutting edge: FAS (CD95) mediates noncanonical IL-1beta and IL-18 maturation via caspase-8 in an RIP3-independent manner. J Immunol. 2012;189(12):5508–5512. doi: 10.4049/jimmunol.1202121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gyrd-Hansen M, Meier P. IAPs: from caspase inhibitors to modulators of NF-kappaB, inflammation and cancer. Nat Rev Cancer. 2010;10(8):561–574. doi: 10.1038/nrc2889. [DOI] [PubMed] [Google Scholar]
- 142.Silke J, Meier P. Inhibitor of apoptosis (IAP) proteins-modulators of cell death and inflammation. Cold Spring Harb Perspect Biol. 2013;5(2) doi: 10.1101/cshperspect.a008730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Vince JE, Wong WW, Gentle I, Lawlor KE, Allam R, O'Reilly L, Mason K, Gross O, Ma S, Guarda G, Anderton H, Castillo R, Hacker G, Silke J, Tschopp J. Inhibitor of apoptosis proteins limit RIP3 kinase-dependent interleukin-1 activation. Immunity. 2012;36(2):215–227. doi: 10.1016/j.immuni.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 144.Labbe K, McIntire CR, Doiron K, Leblanc PM, Saleh M. Cellular inhibitors of apoptosis proteins cIAP1 and cIAP2 are required for efficient caspase-1 activation by the inflammasome. Immunity. 2011;35(6):897–907. doi: 10.1016/j.immuni.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 145.Antonopoulos C, Sanadi CEl, Kaiser WJ, Mocarski ES, Dubyak GR. Proapoptotic chemotherapeutic drugs induce noncanonical processing and release of IL-1beta via caspase-8 in dendritic cells. J Immunol. 2013;191(9):4789–4803. doi: 10.4049/jimmunol.1300645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gringhuis SI, Kaptein TM, Wevers BA, Theelen B, van der Vlist M, Boekhout T, Geijtenbeek TB. Dectin-1 is an extracellular pathogen sensor for the induction and processing of IL-1beta via a noncanonical caspase-8 inflammasome. Nat Immunol. 2012;13(3):246–254. doi: 10.1038/ni.2222. [DOI] [PubMed] [Google Scholar]
- 147.Bellocchio S, Montagnoli C, Bozza S, Gaziano R, Rossi G, Mambula SS, Vecchi A, Mantovani A, Levitz SM, Romani L. The contribution of the Toll-like/IL-1 receptor superfamily to innate and adaptive immunity to fungal pathogens in vivo. J Immunol. 2004;172(5):3059–3069. doi: 10.4049/jimmunol.172.5.3059. [DOI] [PubMed] [Google Scholar]
- 148.Vonk AG, Netea MG, Krieken JHvan, Iwakura Y, van der Meer JW, Kullberg BJ. Endogenous interleukin (IL)-1 alpha and IL-1 beta are crucial for host defense against disseminated candidiasis. J Infect Dis. 2006;193(10):1419–1426. doi: 10.1086/503363. [DOI] [PubMed] [Google Scholar]
- 149.Conti HR, Shen F, Nayyar N, Stocum E, Sun JN, Lindemann MJ, Ho AW, Hai JH, Yu JJ, Jung JW, Filler SG, Masso-Welch P, Edgerton M, Gaffen SL. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. The Journal of experimental medicine. 2009;206(2):299–311. doi: 10.1084/jem.20081463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hernandez-Santos N, Gaffen SL. Th17 cells in immunity to Candida albicans. Cell Host Microbe. 2012;11(5):425–435. doi: 10.1016/j.chom.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mencacci A, Bacci A, Cenci E, Montagnoli C, Fiorucci S, Casagrande A, Flavell RA, Bistoni F, Romani L. Interleukin 18 restores defective Th1 immunity to Candida albicans in caspase 1-deficient mice. Infect Immun. 2000;68(9):5126–5131. doi: 10.1128/iai.68.9.5126-5131.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fantuzzi G, Ku G, Harding MW, Livingston DJ, Sipe JD, Kuida K, Flavell RA, Dinarello CA. Response to local inflammation of IL-1 beta-converting enzyme- deficient mice. J Immunol. 1997;158(4):1818–1824. [PubMed] [Google Scholar]
- 153.Man SM, Tourlomousis P, Hopkins L, Monie TP, Fitzgerald KA, Bryant CE. Salmonella infection induces recruitment of Caspase-8 to the inflammasome to modulate IL-1beta production. J Immunol. 2013;191(10):5239–5246. doi: 10.4049/jimmunol.1301581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kang TB, Yang SH, Toth B, Kovalenko A, Wallach D. Caspase-8 blocks kinase RIPK3-mediated activation of the NLRP3 inflammasome. Immunity. 2013;38(1):27–40. doi: 10.1016/j.immuni.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 155.Provoost S, Maes T, Pauwels NS, Berghe TVanden, Vandenabeele P, Lambrecht BN, Joos GF, Tournoy KG. NLRP3/caspase-1-independent IL-1beta production mediates diesel exhaust particle-induced pulmonary inflammation. J Immunol. 2011;187(6):3331–3337. doi: 10.4049/jimmunol.1004062. [DOI] [PubMed] [Google Scholar]
- 156.Joosten LA, Netea MG, Fantuzzi G, Koenders MI, Helsen MM, Sparrer H, Pham CT, van der Meer JW, Dinarello CA, van den Berg WB. Inflammatory arthritis in caspase 1 gene-deficient mice: contribution of proteinase 3 to caspase 1-independent production of bioactive interleukin-1beta. Arthritis Rheum. 2009;60(12):3651–3662. doi: 10.1002/art.25006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Guma M, Ronacher L, Liu-Bryan R, Takai S, Karin M, Corr M. Caspase 1-independent activation of interleukin-1beta in neutrophil-predominant inflammation. Arthritis Rheum. 2009;60(12):3642–3650. doi: 10.1002/art.24959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Edye ME, Lopez-Castejon G, Allan SM, Brough D. Acidosis drives damage-associated molecular pattern (DAMP)-induced interleukin-1 secretion via a caspase-1-independent pathway. J Biol Chem. 2013;288(42):30485–30494. doi: 10.1074/jbc.M113.478941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mayer-Barber KD, Barber DL, Shenderov K, White SD, Wilson MS, Cheever A, Kugler D, Hieny S, Caspar P, Nunez G, Schlueter D, Flavell RA, Sutterwala FS, Sher A. Caspase-1 independent IL-1beta production is critical for host resistance to mycobacterium tuberculosis and does not require TLR signaling in vivo. J Immunol. 2010;184(7):3326–3330. doi: 10.4049/jimmunol.0904189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kono H, Orlowski GM, Patel Z, Rock KL. The IL-1-dependent sterile inflammatory response has a substantial caspase-1-independent component that requires cathepsin C. J Immunol. 2012;189(7):3734–3740. doi: 10.4049/jimmunol.1200136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lukens JR, Barr MJ, Chaplin DD, Chi H, Kanneganti TD. Inflammasome-derived IL-1beta regulates the production of GM-CSF by CD4(+) T cells and gammadelta T cells. J Immunol. 2012;188(7):3107–3115. doi: 10.4049/jimmunol.1103308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Schonbeck U, Mach F, Libby P. Generation of biologically active IL-1 beta by matrix metalloproteinases: a novel caspase-1-independent pathway of IL-1 beta processing. J Immunol. 1998;161(7):3340–3346. [PubMed] [Google Scholar]
- 163.Kawasaki Y, Xu ZZ, Wang X, Park JY, Zhuang ZY, Tan PH, Gao YJ, Roy K, Corfas G, Lo EH, Ji RR. Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nat Med. 2008;14(3):331–336. doi: 10.1038/nm1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.McGuire MJ, Lipsky PE, Thiele DL. Generation of active myeloid and lymphoid granule serine proteases requires processing by the granule thiol protease dipeptidyl peptidase I. J Biol Chem. 1993;268(4):2458–2467. [PubMed] [Google Scholar]
- 165.Mizutani H, Schechter N, Lazarus G, Black RA, Kupper TS. Rapid and specific conversion of precursor interleukin 1 beta (IL-1 beta) to an active IL-1 species by human mast cell chymase. The Journal of experimental medicine. 1991;174(4):821–825. doi: 10.1084/jem.174.4.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Pham CT, Ley TJ. Dipeptidyl peptidase I is required for the processing and activation of granzymes A and B in vivo. Proc Natl Acad Sci U S A. 1999;96(15):8627–8632. doi: 10.1073/pnas.96.15.8627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Netea MG, Simon A, van de Veerdonk F, Kullberg BJ, Van der Meer JW, Joosten LA. IL-1beta processing in host defense: beyond the inflammasomes. PLoS Pathog. 2010;6(2):e1000661. doi: 10.1371/journal.ppat.1000661. [DOI] [PMC free article] [PubMed] [Google Scholar]