Abstract
Background: Vascular endothelial growth factor (VEGF) induces proliferation of endothelial cells, stimulates angiogenesis, and increases vascular permeability, but information about its role in periodontal diseases is limited. The aim of this study is to determine the association between VEGF expression in healthy and periodontally diseased tissues of healthy and diabetic patients.
Materials and Methods: Seventeen systemically healthy and 17 Type 2 diabetic patients (DM), all diagnosed with periodontitis were enrolled into the study. Gingival samples were collected from both periodontal and healthy sites in all patients. Each patient served as his/her own control samples were subjected to immunohistochemical analysis.
Results: The diseased sites of diabetic subjects expressed higher level of VEGF when compared to diseased sites of non diabetic subjects with chronic periodontitis, VEGF was observed in healthy periodontal tissues of both diabetic and systemically healthy people with periodontitis and VEGF was intensely present in monocytes and macrophages.
Conclusion: The increased expression of VEGF in diseased sites of diabetic patients suggests that diabetes mellitus might have direct influence over VEGF expression.
Keywords: Diabetes mellitus, Heat induced enzyme retrievel, Vascular endothelial growth factor
Introduction
Angiogenesis occurs under pathological condition contributing to the degree of inflammation as a result the new blood vessels transport proinflammatory cells to the lesion and supply oxygen, nutrients to the inflamed tissues [1,2]. Numerous cytokines and growth factors are involved in the regulation of angiogenesis, including members of transforming growth factor α and β, Hepatocyte growth factor, Tumour necrosis factor, Interleukin-8. Of all, the most potent agent that acts specifically on vascular endothelium is vascular endothelial growth factor (VEGF) [1].
VEGF a 46 KD homodimeric glycoprotein is an endothelial – specific growth factor that potently increases microvascular permeability, stimulates endothelial cell proliferation, migration of monocytes, induces proteolytic enzyme expression, all of which are essential for angiogenesis [3]. VEGF stimulates interstitial collagenase production, von willebrand factor release, and enhanced procoagulant activity [1]. It induces permeability of fluids and proteins. It is 50,000 times more potent than histamine. VEGF is detectable in periodontal tissues within endothelial cells, plasma cells, macrophages and in junctional, sulcular and gingival epithelium [2].
Diabetes mellitus is considered as a systemic risk factor for periodontal disease. Various investigations revealed the contribution of diabetes mellitus to periodontitis and to the severity via its effects on vasculature, inflammatory and immune response, alterations in collagen synthesis and genetic predisposition. It has been demonstrated that diabetes mellitus results in increased expression of VEGF in numerous tissues as a response to both hyperglycemia and tissue ischemia [4].
Diabetes mellitus may have an inductive effect on VEGF levels in periodontal disease which may be an important factor in the onset of gingivitis and in its progression to periodontitis. With the increasing number of diabetics in an aging population the determination of VEGF levels in periodontally diseased tissues of diabetic patients may be beneficial [4].
Materials and Methods
The present study was conducted in the Division of Periodontics, Rajah Muthiah Dental College & Hospital, Annamalai University for a duration of one year. All the risks and benefits involved in the study were explained to the patients and informed consent was obtained and ethical clearance was sought. This study is a randomized clinical trial with a crossover design where each subject served as their own control.
A total of 34 patients all diagnosed as chronic periodontitis, based on the probing pocket depth,clinical attachment loss (CAL),plaque index,17 type II diabetic and 17 non diabetic patients with age group between 40 to 56 years, with mean HbA1c value ranging between 6 to 8 and duration not less than five years. Gingival samples were collected from healthy and diseased sites of all diabetic patients. Thus, each patient served as his/her own control. Healthy sites with probing pocket depth ≤3mm and disease sites with probing pocket depth ≥6mm. In non-diabetic patients with chronic periodontitis, gingival tissue samples were collected from periodontally diseased and healthy sites. All the patients were treated with initial preparatory phase consisting of instructions in proper plaque control, scaling and root planing. The gingival tissues were harvested from the sites with extensive involvement, from the tooth having hopeless prognosis or at the time of periodontal surgery, and were subjected for immunohistochemical analysis. Smokers, history of any systemic diseases and medications influencing the study were excluded from the study.
The following clinical parameters were recorded for all patients Plaque index (PI) Gingival index (GI), Probing pocket depth (PPD), Clinical attachment level (CAL).
Collection of Tissues Samples and Staining Procedure
Approximately 1mm of tissue samples were obtained from both healthy and diseased sites and were immediately placed in 10% neutral buffered formalin solution. Samples were embedded into paraffin blocks on the same day. Sections of four microns thickness were made in Poly-L-lysine pre-coated slides. The sections were incubated at 600C for one hour in hot plate, allowed to cool and then deparaffinised in xylene and brought to water through graded alcohols (100%, 90%, 70% and 50%). Antigen retrieval was done with HIER (heat induced enzyme retrieval) method using a pressure cooker for 10min.
Slides were washed twice in phosphate buffer solution (PBS) for 5min. Slides were incubated for 5min in 0.4% case in phosphate buffer solution to block non specific reaction.
Now, the slides were placed in the staining chamber and incubated with Polyclonal rabbit Anti-Vascular endothelial growth factor antibody (biogenex, USA) for 30min at room temperature and then incubated in 10% (V/V) animal serum in tris buffered saline for 30min and incubated with nova link polymer (anti mouse/rabbit IgG) for 30min at room temperature. Slides were further incubated with the substrate chromogen, 3, 3’ Diamino benzidine (DAB) solution for 5min and counter stained with 0.02%Mayer’s haematoxylin and mounted with Dibutyl Phthalate xylene. The negative controls slides were stained with all the above-mentioned steps except the primary antibody. Care was taken in every step to eliminate possible human errors. Sections were washed with phosphate buffer solution twice for 5min during each procedure.
Interpretation of Vegf Expression
The expression of VEGF in connective tissue especially in endothelial cells and monocytes were examined. The slides were viewed under low power (10 x) to identify areas of good expression. Then the slides were viewed under high power (40 x) to examine the intensity of expression in both endothelial cells and monocytes. The total number of cells were counted based degree of staining by using IMAGE J software.
Image J Standardisation
A stage micrometer (Erma, JAPAN) is mounted on the photomicrograph system (Nikon- Eclyror-E200) and a picture is captured with 40x magnification. A standardized setting is used to capture the photomicrograph of all the samples. The micrometer picture is opened in Image J software and the scale of the software is calibrated with the scale found in the micrometer.
Now each photomicrograph of the samples was opened in the Image J software and a square of measurement is projected on the photomicrograph. Now the cells inside the square are counted for positivity.
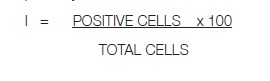 |
The sum of the staining intensity was used for total immunoreactivity. Immunoreactivity was scored on a scale of 0 to 4 as follows: [5]
Grade 0 - representing negative or less than 2% of positively stained cells,
Grade I – for 2-10% positive cells,
Grade II- representing 11-25% positive cells,
Grade III- for 26- 50% positive cells,
Grade IV – for more than 50% positively stained cells.
Results
The mean P1, G1, PPD, CAL of both the groups are presented in [Table/Fig-1]. The evaluation was based according to the brown staining within the cell cytoplasm which was accepted as positive staining. VEGF was intensely present in monocytes and pale intra cytoplasmic brown DAB staining was observed in endothelial cells in both diseased gingiva of diabetic and non-diabetic patients with chronic periodontitis [Table/Fig-2]. The demographic features and the results of immunohistochemical evaluation are presented in [Table/Fig-3].
[Table/Fig-1]:
Mean and standard deviation of baseline parameters
| Criteria | DM with Periodontitis | Non DM with Periodontitis | ANOVA | p- Value | ||
|---|---|---|---|---|---|---|
| HEALTHY SITES | ||||||
| MEAN± SD | ||||||
| PI | 0.54 ± 0.12 | 1.64 ±0.12 | 0.63 ±0.07 | 1.51 ±0.14 | 3.78 | ≤ 0.01 |
| GI | 0.57±0.22 | 2.72±1.13 | 0.61±0.76 | 2.14±0.14 | 516.421 | ≤0.01 |
| PPD | 2.382±0.51 | 9.097±0.57 | 3.218±0.62 | 9.025±0.714 | 682.15 | ≤0.01 |
| CAL | 11.162±1.1239 | 2.66 | <0.014 | |||
[Table/Fig-2]:
Mean and standard deviation of monocytes, endothelial cells, negative cells in diabetic and non diabetic patients with chronic periodontitis chronic periodontitis
| Diabetic with Chronic Periodontitis | Non Diabetic Chronic Periodontitis | f Value | p- Value | |||
|---|---|---|---|---|---|---|
| Healthy Sites | Diseased Sites | Healthy Sites | diseased sites | |||
| Endothelial Cells | 27.572±2085 | 27.752±2.602 | 21.645±1837 | 31.107±2.383 | 9.803 | 0.001 |
| Monocytes Cells | 18.928±2028 | 54.48±3.33 | 14.289±1978 | 41.347±2.85 | 673.45 | 0.001 |
| Negative Cells | 53.500±3.551 | 17.764±2.852 | 54.659±3148 | 27.546±3.17 | 564.6 | 0.001 |
[Table/Fig-3]:
Demographic features and the results of immunohistochemical evaluation
| Diabetic patients | Age &Gender | VEGF | Non Diabetic patients | Age & Gender | VEGF | ||
|---|---|---|---|---|---|---|---|
| HG | DG | HG | DG | ||||
| 1 | 42/F | II | IV | 1 | 50/M | I | II |
| 2 | 50/M | II | IV | 2 | 53/M | I | II |
| 3 | 46/M | I | IV | 3 | 52/F | 0 | II |
| 4 | 45/M | II | IV | 4 | 40/M | I | II |
| 5 | 47//F | II | III | 5 | 53/M | I | III |
| 6 | 42/M | II | IV | 6 | 45/M | 0 | II |
| 7 | 45/M | II | III | 7 | 53/M | 0 | II |
| 8 | 48/M | I | IV | 8 | 45/F | I | III |
| 9 | 45/M | II | IV | 9 | 53/M | 0 | II |
| 10 | 47/F | II | IV | 10 | 53/F | 0 | III |
| 11 | 51/M | I | III | 11 | 49/M | 0 | III |
| 12 | 50/M | II | IV | 12 | 43/M | I | II |
| 13 | 48/M | I | III | 13 | 52/M | 0 | III |
| 14 | 44/F | II | IV | 14 | 52/M | 0 | II |
| 15 | 53/M | II | III | 15 | 54/M | I | II |
| 16 | 49/M | I | IV | 16 | 49/M | I | III |
| 17 | 53/M | II | IV | 17 | 55/M | 0 | III |
Discussion
In accordance to the study done by Booth et al., [6] our present study showed the expression of VEGF was found to be higher in the diseased sites of diabetic patients with chronic periodontitis when compared to their healthy sites. which was found to be statistically significant with p-value>0.001 as assessed by the degree of staining of monocytes and endothelial cells immunohistochemically [Table/Fig-2].
One of the prominent features of angiogenesis is the infiltration of monocytes in growing collateral vessels where monocytes are found to be prominent source of VEGF. The result of our present study was similar where the level of VEGF expression in the diseased sites of diabetic patients was high (grade IV) when compared to healthy sites of the same patients, but when compared to the diseased sites of non diabetic patients with chronic periodontitis patients the level of VEGF expression was till found to be higher (gradeIV) [7].
In our present study there was a high degree of positive staining of monocytes with an increase in the mean number of cells(50-60%) when compared to endothelial cells (22-33%) and was found to be statistically significant with p-value>0.001 which was in accordance to the study by Fisan et al., [8].
Walten berger et al., [9] in his study has isolated peripheral blood monocytes from both diabetic and non-diabetic individuals of similar age. The migratory response of monocytes was impaired towards a gradient of VEGF in diabetic individuals. Whereas, in our study it was assessed that the monocytes staining was significantly high in periodontal tissues of the diseased sites in diabetic patients with chronic periodontitis.
The presence of significant differences between VEGF values of healthy gingival tissues from diabetic patients and those of healthy gingival tissues of periodontal patients may indicate the possible effect of systemic conditions on the level of VEGF [9]. In our present study it was observed that the mean number of negative cells that had not expressed the VEGF was higher in healthy sites of diabetic patients with chronic periodontitis (53.5), than non diabetic patients
Lie et al., [10] has made a study to determine the association of chronic periodontitis and circulating endothelial progenitor cells (EPC). The results revealed that patients with moderate to severe periodontitis exhibited increase in endothelial progenitor cell count.
This was in accordance with our study, where the mean number of endothelial cells (31.107) was significantly high in diseased sites of non diabetic chronic periodontitis patients with p<0.001 when compared to diseased sites of diabetic chronic periodontitis patients (27.752). Another result of this study, the insignificant disparity between the periodontally diseased tissues of both diabetics and non-diabetics, seems to suggest the effect of periodontitis as an additional factor on the level of VEGF.
The study result was also in accordance to the study done by Aspriello SD [11]. He concluded that decreased endothelial VEGF expression and MVD in type ii diabetes mellitus patients that may be due to insulin resistance and endothelial and concluded that EMD induces proliferation and viability and angiogenesis of human microvacular cells and increase the angiogenesis in periodontal pockets [11]. An experimental animal study has been done to conclude Atrovastin used in the treatment of hypercholestremia can be used as a protective and therapeutic agent for periodontal disease based on immunoreactivity to vascular endothelial growth factor and MMP-9 [12].
Conclusion
This study investigates the association between VEGF, DM and periodontitis. The level of expression of VEGF was higher in diabetic patients with periodontitis when compared to non diabetic patients with chronic periodontitis. It has shown that periodontal disease might have influence on VEGF levels. This study also demonstrates VEGF levels are prominent even in the healthy gingival samples of controlled diabetic patients.
Therefore, in order to investigate the relationship between VEGF and progression of periodontitis in diabetic patients, more research on a larger sample must be provided.
Financial or Other Competing Interests
None.
References
- [1].Ferrara N. Molecular and biological properties of vascular endothelial growth factor. J Mol Med. 1999;77(7):527–43. doi: 10.1007/s001099900019. [DOI] [PubMed] [Google Scholar]
- [2].Lucarini G, Zizzi A, Aspriello SD, Ferrante L, Tosco E, Lo Muzio L, et al. Involvement of vascular endothelial growth factor, CD44 and CD133 in periodontal disease and diabetes: an immunohistochemical study. J Clin Periodontol. 2009;36(1):3–10. doi: 10.1111/j.1600-051X.2008.01338.x. [DOI] [PubMed] [Google Scholar]
- [3].Sakalliolu EE, Aliyev E, Lütfiolu M, Yavuz U, Açikgöz G. Vascular endothelial growth factor (VEGF) levels of gingiva and gingival crevicular fluid in diabetic and systemically healthy periodontitis patients. Clin Oral Investig. 2007;11(2):115–20. doi: 10.1007/s00784-006-0097-5. [DOI] [PubMed] [Google Scholar]
- [4].Mealey BL, Oates TW. American Academy of Periodontology. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77(8):1289–303. doi: 10.1902/jop.2006.050459. [DOI] [PubMed] [Google Scholar]
- [5].Markopoulos AK, Poulopoulos AK, Kayavis I, Papanayotou P. Immun- ohistochemical detection of insulin-like growth factor-I in the labial salivary glands of patients with + Sjögren’s syndrome. Oral Dis. 2000;6(1):31–34. doi: 10.1111/j.1601-0825.2000.tb00318.x. [DOI] [PubMed] [Google Scholar]
- [6].Booth V, Young S, Cruchley A, Taichman NS, Paleolog E. Vascular endothelial growth factor in human periodontal disease. J Periodont Res. 1998;33(8):491–99. doi: 10.1111/j.1600-0765.1998.tb02349.x. [DOI] [PubMed] [Google Scholar]
- [7].Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995;1(1):27–31. doi: 10.1038/nm0195-27. [DOI] [PubMed] [Google Scholar]
- [8].Güneri P, Ünlü F, Yeilbek B, Bayraktar F, Kokuludag A, Hekimgil M. Vascular Endothelial Growth Factor in Gingival Tissues and Crevicular Fluids of Diabetic and Healthy Periodontal Patients. Journal of Periodontology. 2004;75(1):91–97. doi: 10.1902/jop.2004.75.1.91. [DOI] [PubMed] [Google Scholar]
- [9].Walten berger J. Impaired collateral vessel development in diabetes: potential cellular mechanisms and therapeutic implications. Cardiovasc Res. 2001;49(3):554–60. doi: 10.1016/s0008-6363(00)00228-5. [DOI] [PubMed] [Google Scholar]
- [10].Tse HF, Yiu KH, Jia N, Chen H, Li LSW, et al. Increased levels of circulating endothelial progenitor cells in subjects with moderate to severe chronic periodontitis. J Clin Periodontol. 2009;36(11):933–39. doi: 10.1111/j.1600-051X.2009.01481.x. [DOI] [PubMed] [Google Scholar]
- [11].Balli U, Keles GC, Cetinkaya BO, Mercan U, Ayas B, Erdogan D. Assessment of vascular endothelial growth factor and matrix metalloproteinase-9 in the periodontium of rats treated with atorvastatin. J Periodontol. 2014;85(1):178–87. doi: 10.1902/jop.2013.130018. [DOI] [PubMed] [Google Scholar]
- [12].Aspriello SD, Zizzi A, Spazzafumo L, Rubini C, Lorenzi T, Marzioni D, et al. Effects of enamel matrix derivative on vascular endothelial growth factor expression and microvessel density in gingival tissues of periodontal pocket: a comparative study. J Periodontol. 2011;82(4):606–12. doi: 10.1902/jop.2010.100180. [DOI] [PubMed] [Google Scholar]


