Abstract
The private health insurance industry collected $47.1 billion in premiums in 1977 and returned $41.6 billion in benefits to their subscribers. Premiums rose 16.3 percent as a direct consequence of rapid claims growth in 1976. After operating expenses were deducted, the industry showed a small, $.4 billion underwriting loss. About 78 percent of the population were insured for hospital care, and about 76 percent for surgical services. Smaller percentages had coverage for other types of care. An estimated 61.8 percent of the aged bought private hospital insurance, and 47.1 percent bought surgical insurance, mostly to supplement Medicare benefits. About 12 percent of persons under age 65 had no protection against the cost of hospital care either through private insurance or a public program such as Medicare or Medicaid.
Extent of Health Insurance Coverage
Private Insurance Coverage of the Population
In 1977, 168 million persons—almost 4 million more persons than in 1976—were covered by private hospital insurance through an insurance company, a Blue Cross and/or a Blue Shield plan, or an independent prepaid or self-insured health plan. Surgical insurance was carried by 164 million persons—1.7 million more persons than in 1976. Thus the percentages of the privately insured population rose from 76.8 percent to 78.0 percent for hospital insurance and from 75.8 percent to 76.0 percent for private surgical insurance (Tables 1 and 2).
Table 1. Estimates of net number of different persons under private health insurance plans and percent of population covered, by age and specific type of care as of December 31, 1977.
| All ages | Under age 65 | Aged 65 and over | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Number (in thousands) | Percent of civilian population 1 | Number (in thousands) | Percent of civilian population 2 | Number (in thousands) | Percent of civilian population 3 | |
| Hospital care | 168,212 | 78.0 | 153,505 | 80.0 | 14,707 | 61.8 |
| Physicians' services | ||||||
| Surgical services | 163,864 | 76.0 | 152,651 | 79.6 | 11,213 | 47.1 |
| In-hospital visits | 156,607 | 72.6 | 146,327 | 76.3 | 10,280 | 43.2 |
| X-ray and laboratory examinations | 150,399 | 69.8 | 142,630 | 74.4 | 7,769 | 32.6 |
| Office and home visits | 121,711 | 56.4 | 115,697 | 60.3 | 6,014 | 25.3 |
| Dental care | 49,250 | 22.8 | 48,093 | 25.1 | 1,157 | 4.9 |
| Prescribed drugs (out-of-hospital) | 149,896 | 69.5 | 145,323 | 75.8 | 4,573 | 19.2 |
| Private duty nursing | 148,584 | 68.9 | 144,552 | 75.4 | 4,032 | 16.9 |
| Visiting nurse service | 151,788 | 70.4 | 147,063 | 76.7 | 4,725 | 19.9 |
| Nursing home care | 65,889 | 30.6 | 61,029 | 31.8 | 4,860 | 20.4 |
Based on Bureau of Census estimates of 215,618,000 as of Jan. 1, 1978.
Based on Bureau of Census estimate of 191,823,000 as of Jan. 1, 1978.
Based on Bureau of Census estimate of 23,795,000 as of Jan. 1, 1978.
Table 2. Estimates of net number of different persons under private health insurance plans and percent of population covered, by specified type of care, 1974, 1976 and 1977.
| Physicians' services | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| End of year | Hospital care | Surgical services | In-hospital visits | X-ray and laboratory examinations | Office and home visits | Dental care | Prescribed drugs (out-of- hospital) | Private duty nursing | Visiting nurse service | Nursing home care |
| Number (in thousands) | ||||||||||
|
|
||||||||||
| 1974 | 162,693 | 158,928 | 146,494 | 152,206 | 126,235 | 32,896 | 142,246 | 140,353 | 135,751 | 69,601 |
| 1976 | 164,235 | 162,179 | 155,548 | 150,897 | 134,124 | 46,578 | 150,222 | 147,311 | 145,863 | 70,422 |
| 1977 | 168,212 | 163,864 | 156,607 | 150,399 | 121,711 | 49,250 | 149,896 | 148,584 | 151,788 | 65,889 |
|
|
||||||||||
| Percent | ||||||||||
|
|
||||||||||
| 1974 | 77.3 | 75.5 | 69.6 | 72.3 | 59.5 | 15.6 | 67.5 | 66.6 | 64.5 | 33.0 |
| 1976 | 76.8 | 75.8 | 72.7 | 70.6 | 58.0 | 21.8 | 70.2 | 68.9 | 68.2 | 32.9 |
| 1977 | 78.0 | 76.0 | 72.6 | 69.8 | 56.4 | 22.8 | 69.5 | 68.9 | 70.4 | 30.6 |
A smaller percentage of the population was protected against the costs of other health care services. About 70 percent had private insurance to help pay the cost of out-of-hospital X-ray and laboratory examinations, prescribed drugs, and nursing services. Only 23 percent of the population had private dental insurance, and only 31 percent were insured for nursing home care. Private insurance provided some level of payment for doctors' home and office visits for only 56 percent of the population, a slight decline from 1976.
The fastest growth occurred in hospital insurance and in coverage for dental care and visiting nurse service. Both employer-related and individually-purchased hospital insurance coverage rose in the effort to meet expensive hospital bills. Collective bargaining settlements brought dental care to larger numbers of workers and their families. Visiting nurse services were added to many private insurance plans to help keep down the cost of hospital care.
Almost four-fifths of persons under age 65—the work force and their families—were insured for hospital-related services, and about three-fourths were protected against out-of-hospital X-ray and laboratory examinations, prescribed drugs (out-of-hospital, and nursing services. Many of the aged, virtually all of whom were covered by Medicare hospital insurance and supplementary medical insurance, also bought private insurance, most of it to supplement Medicare coverage. This coverage was purchased by individuals and to some extent by employers where unions had bargained for continued group coverage into retirement. Supplementary private insurance paid some or all of patient deductibles and co-insurance required by Medicare for hospital care, physicians' services, and nursing home care. Some insurance plans made partial payments for services excluded by Medicare—prescribed drugs and private duty nursing. The proportion of the aged population with private insurance coverage ranged from 62 percent for hospital care to 5 percent for dental care.
Gross Enrollments
Private insurers reported a record 218.6 million in enrollments for hospital care in 1977, of which 50.4 million or approximately 23 percent represented duplicate or multiple coverage (Table 3).
Table 3. Gross enrollment under private health insurance plans, by age, type of plan and specified type of care, as of December 31, 1977.
| [In thousands] | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Physicians' Services | |||||||||||
|
|
|||||||||||
| Type of plan | Hospital care | Surgical services | In-hospital visits | X-ray and laboratory examinations | Office and home visits | Dental care | Prescribed drugs (out- of-hospital) | Private duty nursing | Visiting nurse service | Nursing Home care | Vision care |
| All Ages | |||||||||||
|
|
|||||||||||
| Total | 218,607 | 200,568 | 197,548 | 189,549 | 153,986 | 49,734 | 163,486 | 161,415 | 162,403 | 69,429 | (1) |
|
|
|||||||||||
| Blue Cross and Blue Shield | 85,101 | 75,379 | 71,261 | 63,284 | 28,372 | 5,283 | 41,208 | 38,249 | 39,108 | 32,066 | 1,593 |
| Blue Cross | 83,153 | 4,848 | 4,017 | (1) | 2,327 | (1) | (1) | (1) | (1) | (1) | (1) |
| Blue Shield | 1,948 | 70,531 | 67,244 | (1) | 26,045 | (1) | (1) | (1) | (1) | (1) | (1) |
| Insurance companies | 117,906 | 106,313 | 108,026 | 108,026 | 108,026 | 32,215 | 108,026 | 108,026 | 108,026 | 27,567 | (1) |
| Group policies | 89,219 | 91,904 | 101,925 | 101,925 | 101,925 | 32,215 | 101,925 | 101,925 | 101,925 | 22,511 | (1) |
| Individual policies | 28,687 | 14,409 | 6,101 | 6,101 | 6,101 | 0 | 6,101 | 6,101 | 6,101 | 5,056 | (1) |
| Independent plans 2 | 15,600 | 18,876 | 18,261 | 18,239 | 17,588 | 12,236 | 14,252 | 15,140 | 15,269 | 9,796 | 12,574 |
| Consumer | 4,692 | 6,939 | 6,923 | 6,890 | 6,786 | 1,207 | 3,517 | 5,786 | 6,675 | 3,915 | 5,340 |
| Labor-Management | 10,355 | 11,237 | 10,763 | 10,774 | 10,206 | 5,028 | 10,381 | 8,933 | 8,109 | 5,420 | 3,498 |
| Health professional | 553 | 700 | 575 | 575 | 596 | 749 | 384 | 421 | 485 | 461 | 679 |
| Dental service corporation | ...... | ...... | ...... | ...... | ...... | 5,252 | ...... | ...... | ...... | ..... | ..... |
| Vision service corporation | ...... | ...... | ...... | ...... | ...... | ..... | ...... | ...... | ...... | ...... | 3,057 |
|
|
|||||||||||
| Under age 65 | |||||||||||
|
|
|||||||||||
| Total | 199,494 | 186,843 | 186,397 | 179,758 | 146,377 | 48,566 | 158,498 | 157,035 | 157,348 | 64,308 | (1) |
|
|
|||||||||||
| Blue Cross and Blue Shield | 76,228 | 67,170 | 63,766 | 57,187 | 24,353 | 5,147 | 39,631 | 37,156 | 37,496 | 28,038 | 1,575 |
| Blue Cross | 74,514 | 4,318 | 3,661 | (1) | 2,187 | (1) | (1) | (1) | (1) | (1) | (1) |
| Blue Shield | 1,713 | 62,852 | 60,105 | (1) | 22,166 | (1) | (1) | (1) | (1) | (1) | (1) |
| Insurance companies | 108,733 | 102,238 | 105,695 | 105,695 | 105,695 | 31,706 | 105,695 | 105,695 | 105,695 | 27,000 | (1) |
| Group policies | 87,104 | 89,808 | 97,766 | 99,766 | 99,766 | 31,706 | 99,766 | 99,766 | 99,766 | 22,091 | (1) |
| Individual policies | 21,629 | 12,430 | 5,929 | 5,929 | 5,929 | 0 | 5,929 | 5,929 | 5,929 | 4,909 | (1) |
| Independent plans 2 | 14,533 | 17,435 | 16,936 | 16,876 | 16,329 | 11,713 | 13,172 | 14,184 | 14,157 | 9,270 | 11,987 |
| Consumer | 4,455 | 6,457 | 6,444 | 6,420 | 6,324 | 1,184 | 3,296 | 5,477 | 6,254 | 3,721 | 5,000 |
| Labor-Management | 9,567 | 10,338 | 9,952 | 9,916 | 9,444 | 4,893 | 9,549 | 8,320 | 7,450 | 5,120 | 3,309 |
| Health professional | 511 | 640 | 540 | 540 | 561 | 694 | 327 | 387 | 453 | 429 | 629 |
| Dental service corporation | ...... | ...... | ...... | ...... | ...... | 4,942 | ...... | ...... | ...... | ..... | ..... |
| Vision service corporation | ...... | ...... | ...... | ...... | ...... | ..... | ...... | ...... | ...... | ..... | 3,049 |
|
|
|||||||||||
| Aged 65 and over | |||||||||||
|
|
|||||||||||
| Total | 19,113 | 13,725 | 11,151 | 9,791 | 7,609 | 1,168 | 4,988 | 4,380 | 3 5,055 | 3 5,121 | (1) |
|
|
|||||||||||
| Blue Cross and Blue Shield | 3 8,873 | 38,209 | 3 7,495 | 3 6,097 | 3 4,019 | 136 | 1,577 | 1,093 | 1,612 | 4,028 | 18 |
| Blue Cross | 3 8,638 | 3530 | 3 356 | (1) | 3140 | (1) | (1) | (1) | (1) | (1) | (1) |
| Blue Shield | 3235 | 3 7,679 | 37,139 | (1) | 33,879 | (1) | (1) | (1) | (1) | (1) | (1) |
| Insurance companies | 9,173 | 4,075 | 2,331 | 2,331 | 2,331 | 509 | 2,331 | 2,331 | 2,331 | 567 | (1) |
| Group policies | 2,115 | 2,096 | 2,159 | 2,159 | 2,159 | 509 | 2,159 | 2,159 | 2,159 | 420 | (1) |
| Individual policies | 7,058 | 1,979 | 172 | 172 | 172 | 0 | 172 | 172 | 172 | 147 | (1) |
| Independent plans2 | 1,067 | 1,441 | 1,325 | 1,363 | 1,259 | 523 | 1,080 | 956 | 1,112 | 526 | 587 |
| Consumer | 237 | 482 | 479 | 470 | 462 | 23 | 220 | 308 | 421 | 195 | 339 |
| Labor-Management | 788 | 899 | 810 | 858 | 762 | 134 | 832 | 614 | 659 | 300 | 189 |
| Health professional | 42 | 60 | 36 | 35 | 35 | 56 | 28 | 34 | 32 | 31 | 50 |
| Dental service corporation | ...... | ...... | ...... | ...... | ...... | 310 | ...... | ...... | ...... | ..... | ..... |
| Vision service corporation | ...... | ...... | ...... | ...... | ...... | ..... | ...... | ...... | ...... | ..... | 9 |
Data not available.
In earlier series, consumer plans were titled community, labor management plans were titled employer-employee-union, and health professional plans were titled private group clinic.
Includes disabled persons under age 65 who are eligible for Medicare.
Multiple coverage occurs when both spouses are employed and both have group insurance through their employer, when a person with group insurance purchases an individual policy or policies to supplement group coverage, or when a person not eligible for group insurance holds two or more individual policies in an effort to obtain some level of protection against the costs of health care.
The rate of duplication was lower for physicians' services (18 to 21 percent) and much lower for other types of care—8 percent for prescribed drugs and private duty nursing, 7 percent for visiting nurse service, 5 percent for nursing home care, and 1 percent for dental care. Rates of duplication were similar for both the under-age-65 and aged-65-and-over groups.
Table 3 also shows enrollments for the various kinds of health care, by type of private insurer and for each of the age groups.
Market Shares
Insurance Companies
Insurance companies continued to dominate the market for the work force and their families, insuring 54 percent of the hospital market. Persons covered by employer-related group policies for hospital care numbered 87.1 million; an additional 21.6 million had individual hospital policies for a total of 108.7 million persons, well above the 76.2 million hospital enrollments in Blue Cross and Blue Shield plans. Insurance companies covered 35 to 82 million more persons than did Blue Cross and Blue Shield plans for various physicians' services, and more than 66 million more for prescribed drugs and nursing services (Tables 3 and 4).
Table 4. Percentage distribution of total gross enrollment under private health insurance plans, by age, type of plan and specified type of care, as of December 31, 1977.
| Type of plan | Hospital care | Physicians' Services | Dental care | Prescribed drugs (out-of-hospital) | Private-duty nursing | Visiting nurse service | Nursing-home care | |||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Surgical services | In-hospital visits | X-ray and laboratory examinations | Office and home visits | |||||||
| All ages | ||||||||||
|
|
||||||||||
| Total | 100.0 | 100,0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Blue Cross and Blue Shield | 38.9 | 37.6 | 36.1 | 33.4 | 18.4 | 10.6 | 25.2 | 23.7 | 24.1 | 46.2 |
| Insurance companies | 53.9 | 53.0 | 54.7 | 57.0 | 70.2 | 64.8 | 66.1 | 66.9 | 66.5 | 39.7 |
| Group policies | 40.8 | 45.8 | 51.6 | 53.8 | 66.2 | 64.8 | 62.3 | 63.1 | 62.8 | 32.4 |
| Individual policies | 13.1 | 7.2 | 3.1 | 3.2 | 4.0 | .0 | 3.7 | 3.8 | 3.8 | 7.3 |
| Independent plans | 7.1 | 9.4 | 9.2 | 9.6 | 11.4 | 24.6 | 8.7 | 9.4 | 9.4 | 14.1 |
|
|
||||||||||
| Under age 65 | ||||||||||
|
|
||||||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Blue Cross and Blue Shield | 38.2 | 35.9 | 34.2 | 31.8 | 16.6 | 10.6 | 25.0 | 23.7 | 23.8 | 43.6 |
| Insurance companies | 54.5 | 54.8 | 56.7 | 58.8 | 72.2 | 65.3 | 66.7 | 67.3 | 67.2 | 42.0 |
| Group policies | 43.7 | 48.1 | 53.5 | 55.5 | 68.2 | 65.3 | 62.9 | 63.5 | 63.4 | 34.4 |
| Individual policies | 10.8 | 6.7 | 3.2 | 3.3 | 4.1 | .0 | 3.7 | 3.8 | 3.8 | 7.6 |
| Independent plans | 7.3 | 9.3 | 9.1 | 9.4 | 11.2 | 24.1 | 8.3 | 9.0 | 9.0 | 14.4 |
|
|
||||||||||
| Aged 65 and over | ||||||||||
|
|
||||||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Blue Cross and Blue Shield | 46.4 | 59.8 | 67.2 | 62.3 | 52.8 | 11.6 | 31.6 | 25.0 | 31.9 | 78.7 |
| Insurance companies | 48.0 | 29.7 | 20.9 | 23.8 | 30.7 | 43.6 | 46.7 | 53.2 | 46.1 | 11.1 |
| Group policies | 11.1 | 15.3 | 19.4 | 22.1 | 28.4 | 43.6 | 43.3 | 49.3 | 42.7 | 8.2 |
| Individual policies | 36.9 | 14.4 | 1.5 | 1.8 | 2.3 | .0 | 3.4 | 3.9 | 3.4 | 2.9 |
| Independent plans | 5.6 | 10.5 | 11.9 | 13.9 | 16.5 | 44.8 | 21.7 | 21.8 | 22.0 | 10.3 |
Insurance companies also made inroads in the insurance market for the elderly. For the first time they sold more coverage to this age group than did the Blue Cross and Blue Shield plans for hospital care, for prescribed drugs, and for visiting nurse service.
Blue Cross and Blue Shield Plans
The 69 Blue Cross plans enrolled 83.2 million persons—38 percent of the population that the plans served. About 85 percent of these persons were enrolled in groups. Of this number, 8.6 million persons aged 65 and over were enrolled for coverage beyond Medicare levels and/or for health care services not provided by Medicare. The 70 Blue Shield plans covered 70.5 million persons in 1977 (7.7 million of them aged 65 and over) or 33 percent of the population in the areas they served. Blue Cross and Blue Shield shares represented 46 percent of the hospital market for the elderly and 38 percent of the under-age-65 market. For surgical care, their shares accounted for 60 percent of the elderly market and 36 percent of the market for workers and their families. Blue Cross and Blue Shield plans continued to hold almost all the market for nursing home care, covering 4 million elderly, or 79 percent of the market.
Independent Plans
A small but growing share of the market is held by independent prepaid and self-insured health plans. These plans are not underwritten by Blue Cross or Blue Shield or an insurance company. They are sponsored by consumers, labor and/or management, and health professionals. Most are not for profit.
Most of these plans provided comprehensive health care services, providing coverage for about 7 percent of the market for hospital insurance and 9-11 percent for various physicians' services, prescribed drugs, and nursing services. Dental coverage (largely by the dental service corporations) represented 25 percent of all persons with dental insurance.
Administrative Service Only (ASO) Agreements and Minimum Premium Plans (MPP)
The count of the number of persons enrolled in insurance company plans includes a number who are also reported by independent plans and other health insurers. These persons are in plans with Administrative Service Only (ASO) agreements. Under ASO agreements, an insurance company provides services to another insurance company or another health insurance organization—an HMO or a self-insured plan, for example. These services include such things as marketing, claims monitoring, premium collection, accounting, computing, or consulting for a designated fee. These persons have already been reported by the independent prepaid or self-insured plan that was at risk for and provided directly or arranged for health care services for its members in return for a fixed, monthly fee. Additional duplication occurred when third party administrators or other companies provided administrative services in plan areas where the issuing companies do not have regional offices.
Acording to The Health Insurance Association of America (HIAA), an estimated 12 million persons were represented by ASO and MPP agreements. The 1979 HIAA survey of companies will provide statistics for each of these businesses so that HIAA can eliminate the duplication for ASO agreements, thereby allowing the Health Care Financing Administration (HCFA) to unduplicate the health insurance business written by the companies. The enrollment of the companies with respect to stop loss, catastrophic, or out-of-area cover-age can also be reported separately by HCFA.
Changes in the Industry
Growth in Total Enrollments
The growth in the number of enrollments reported by all private insurers for hospital care, surgical services, prescription drugs, and dental care is shown in Table 5. The growth of hospital and surgical insurance was most rapid in the fifties when the concept of health insurance was becoming an important fringe benefit in employer-employee negotiations. The growth rate moderated in the sixties when insurance for other types of care such as prescription drugs and dental care was being pursued in contract negotiations. The insurance companies experienced the same general trends in growth as the overall industry.
Table 5. Gross enrollment under private health insurance plans, by type of care and type of plan, 1950–1977.
| [In thousands] | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| End of year | All plans | Blue Cross and Blue Shield | Insurance companies | Independent plans | ||||
|
|
|
|||||||
| Total | Blue Cross | Blue Shield | Total | Group policies | Individual policies | |||
| Hospital care | ||||||||
|
|
||||||||
| 1950 | 81,691 | 37,645 | 37,432 | 210 | 39,601 | 22,305 | 17,296 | 4,445 |
| 1960 | 140,055 | 57,464 | 55,938 | 1,526 | 76,597 | 54,416 | 22,181 | 5,994 |
| 1970 | 190,758 | 75,464 | 72,942 | 2,522 | 107,163 | 80,505 | 26,658 | 8,131 |
| 1975 | 212,154 | 85,762 | 83,179 | 2,583 | 117,300 | 87,185 | 30,115 | 112,581 |
| 1976 | 208,575 | 85,528 | 83,054 | 2,474 | 113,820 | 86,825 | 26,996 | 114,091 |
| 1977 | 219,570 | 85,101 | 83,153 | 1,948 | 117,906 | 89,219 | 28,687 | 15,600 |
|
|
||||||||
| Surgical services | ||||||||
|
|
||||||||
| 1950 | 55,950 | 17,253 | 1,151 | 16,102 | 34,937 | 21,219 | 13,718 | 3,760 |
| 1960 | 127,091 | 48,266 | 3,773 | 44,493 | 71,489 | 55,464 | 16,025 | 7,336 |
| 1970 | 179,152 | 69,110 | 3,874 | 65,236 | 99,510 | 81,549 | 17,961 | 10,532 |
| 1975 | 195,624 | 77,803 | 4,699 | 73,104 | 106,426 | 87,958 | 18,468 | 115,435 |
| 1976 | 192,812 | 76,952 | 4,629 | 72,323 | 104,399 | 88,327 | 16,072 | 117,155 |
| 1977 | 200,568 | 75,379 | 4,848 | 70,531 | 106,313 | 91,904 | 14,409 | 18,876 |
|
|
||||||||
| Prescribed drugs (out-of-hospital) | ||||||||
|
|
||||||||
| 1950 | (2) | (2) | (2) | (2) | (2) | (2) | (2) | (2) |
| 1960 | 69,632 | 10,800 | (2) | (2) | 56,100 | 51,700 | 4,400 | 2,732 |
| 1970 | 105,885 | 25,627 | (2) | (2) | 75,437 | 70,396 | 5,041 | 4,821 |
| 1975 | 156,592 | 46,122 | (2) | (2) | 104,033 | 96,718 | 7,315 | 110,870 |
| 1976 | 157,591 | 46,253 | (2) | (2) | 105,027 | 98,355 | 6,672 | 112,561 |
| 1977 | 163,485 | 41,208 | (2) | (2) | 108,026 | 101,925 | 6,101 | 14,252 |
|
|
||||||||
| Dental care | ||||||||
|
|
||||||||
| 1950 | (2) | (2) | (2) | (2) | (2) | (2) | (2) | (2) |
| 1960 | 4,227 | 16 | (2) | (2) | 2,000 | 2,000 | ‥ | 2,211 |
| 1970 | 12,977 | 273 | (2) | (2) | 7,454 | 7,383 | 71 | 5,250 |
| 1975 | 34,815 | 3,320 | (2) | (2) | 19,020 | 18,936 | 84 | 110,289 |
| 1976 | 47,036 | 4,363 | (2) | (2) | 26,662 | 26,562 | 100 | 111,262 |
| 1977 | 49,734 | 5,283 | (2) | (2) | 32,215 | 32,215 | 0 | 12,236 |
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for earlier years are provided on a provisional basis and will be revised upon completion of the survey.
Data not available.
For Blue Cross-Blue Shield plans, however, the growth rate from 1950 to 1975 was slower, and in recent years they have actually experienced declines for many services. In 1977, enrollments fell for hospital care, physicians' services, and nursing home care, as the number of dependents in this age group declined because of fewer children and a growing number of complementary-to-Medicare contracts written. Growth was concentrated in the more recently negotiated health care fringe benefits for the work force and their dependents—dental care (18 percent), vision care (112 percent), and visiting nurse service (7 percent).
The biggest losses were incurred by Blue Shield plans covering persons under age 65; enrollments for surgical and physicians' in-hospital visits dropped 2 to 3.5 million, and 9 million for physicians' home and office visits, representing loss rates of 3 to 29 percent for these services. Hospital coverage, provided by 11 Blue Shield plans in the United States, also fell for the under-age-65 group (22 percent) as well as for persons aged 65 and over (14 percent).
Growth in the independent plans has been slow but steady. Beginning in the mid-seventies, enrollments have increased, as more employers have turned away from insurance company coverage and have self-insured for the health care costs of their employees. The enactment of the Health Maintenance Organization Act of 1973 has also stimulated the expansion of consumer-sponsored plans and plans sponsored by health professionals.
Growth in Net Coverage
The growth in net coverage from 1974 to 1977 is shown in Table 2 for 10 types of health care services. The estimates for hospital and surgical coverage are based on household surveys conducted biennially by the National Center for Health Statistics. Estimates for other types of care are developed by HCFA from data reported by the industry. Trends in the growth of net coverage have been similar to those in the total enrollments reported by the various insurers. (Further details on the methodology employed can be found in the Technical Note following this article.)
Major Medical Coverage
Major medical plans provide broad protection against a wide range of health care expenses as well as substantial protection for large, unpredictable medical expenses. Supplementary major medical plans supplement basic health care plans; comprehensive major medical plans combine in one plan both basic protection and coverage against catastrophic expenses. Major medical coverage has grown rapidly over the years. It has also extended the range of services covered and raised the benefit levels.
In 1977, an estimated 162 million persons or 75 percent of the population had major medical protection either through insurance company supplementary major medical or comprehensive major medical policies, through Blue Cross and Blue Shield major medical plans, or through comprehensive independent prepaid and self-insured health plans (Table 6). In 1970, the insurance companies and Blue Cross and Blue Shield plans covered 109 million persons; in 1960 only 31 million were covered. No comparable figures are available for independent comprehensive plans for years before 1977.
Table 6. Grots enrollment in supplementary major medical and comprehensive major medical policies of insurance companier, in Blue Cross and Blue Shield major medical plans and in comprehensive prepaid and self-insured independent plans, 1960–1977.
| [In thousands] | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| End of year | All plans | Insurance companies | Blue Cross and Blue Shield Supplementary Plans | Independent Plans | |||
|
| |||||||
| Total | Group Policies | Individual policies 1 | |||||
|
| |||||||
| Supplementary | Comprehensive | ||||||
| 1960 | (2) | 28,061 | 17,991 | 8,463 | 1,607 | 3 3,020 | (2) |
| 1965 | (2) | 59,868 | 42,450 | 12,962 | 4,456 | (2) | (2) |
| 1970 | (2) | 87,376 | 61,718 | 20,244 | 5,414 | 21,658 | (2) |
| 1975 | (2) | 104,033 | 67,310 | 29,408 | 7,315 | 39,172 | (2) |
| 1976 | (2) | 105,027 | 66,753 | 31,602 | 6,672 | 37,026 | (2) |
| 1977 | 161,835 | 108,026 | 68,349 | 33,576 | 6,101 | 39,390 | 12,419 |
Includes both supplementary major medical and comprehensive major medical policies.
Data not available.
Data jointly developed by Blue Cross Association and National Association of Blue Shield plans on unduplicated number of persons covered.
The growth of supplementary major medical coverage by Blue Cross and Blue Shield has been more rapid than that of insurance companies. In 1970 Blue Cross and Blue Shield had only a fourth of such coverage; in 1977 they had more than a third.
In its annual survey of group insurance policies, the Health Insurance Institute (HII) found that major medical insurance had more than doubled from 1976 to 1977 and that 91 percent of the persons with such insurance had maximum benefits of $100,000 or more, compared to less than 1 percent in 1972. HII also revealed that among the most typical size groups of employees (25-499), about half had benefits up to $1 million or unlimited benefits.
In 1977, group major medical policies provided for about 100 million persons under age 65 some level of benefits for physicians' in-hospital visits and home and office visits. These policies covered about 76 million persons for prescription drugs and private duty nursing, and about 21 million for skilled nursing care. Individual major medical insurance policies provided benefits for physicians' services for 5.9 million persons in this age group, some benefits for prescribed drugs and private duty nursing for 4.7 million persons, and comprehensive hospital and surgical expense coverage for 3.2 million persons. Thus, for the under-age-65 group, total major medical coverage by insurance companies for physicians' services ran about 106 million, for prescribed drugs and private duty nursing about 81 million.
Major medical policies covered 2.3 million of the aged. No separate figures for this age group are available for Blue Cross and Blue Shield plans or the independent plans.
Blue Cross generally offered in its basic policies many of the services found in major medical policies. Beyond their basic plans, Blue Cross offered supplementary coverage subject to deductibles and coinsurance with maximum benefits varying from $5,000 to an unlimited amount of extended benefits for the following services: physicians and other health care professionals, prescribed drugs, diagnostic x-rays and laboratory services, nursing home care, home health services, ambulance transportation, prosthetic and orthopedic devices, durable medical equipment, medical supplies, blood, psychiatric treatment, drug addiction, and alcoholism.
Blue Shield plans were comprehensive health care programs consisting of 20 broad benefit areas. Dental care, vision care, and hearing care were new areas of coverage being developed. A majority of the plans also offered supplementary major medical coverage to help pay for the costs of prolonged or catastrophic illnesses.
Independent prepaid and self-insured health plans generally offered a comprehensive range of health care services. Health maintenance organizations for the most part fall in this independent plan category. Because of their comprehensive range of benefits and the prepaid delivery of health care services as needed, independent plans are considered to provide major medical protection. With the rapid growth of self-insured labor-management plans and the increasing number of health maintenance organizations, the number of persons with major medical protection in independent plans reached approximately 12 million in 1977. Among this 12 million were 6.8 million members of prepaid group practice plans. The slow but steady growth of these plans over the years is shown in Table 7. Their growth was stimulated by the enactment of the Health Maintenance Organizations Act of 1973.
Table 7. Gross enrollment under independent group practice prepayment plans, by specified type of care, 1961-1977.
| [In thousands] | |||||
|---|---|---|---|---|---|
|
| |||||
| End of year | Hospital care | Physicians' services | Dental care | ||
|
| |||||
| Surgical services | In-hospital visits | Office, clinic or health center visits | |||
| 1961 | 2,586 | 3,484 | 3,643 | 3,643 | 398 |
| 1964 | 2,695 | 3,504 | 3,196 | 3,894 | 438 |
| 1967 | 3,060 | 4,130 | 3,760 | 4,480 | (1) |
| 1970 | 4,131 | 5,032 | 4,532 | 5,432 | 910 |
| 1972 | 3,984 | 5,080 | 4,553 | 5,476 | 791 |
| 1973 2 | 4,338 | 5,427 | 4,974 | 5,716 | 843 |
| 1974 2 | 4,692 | 5,774 | 5,394 | 5,956 | 896 |
| 1975 2 | 5,047 | 6,120 | 5,815 | 6,197 | 948 |
| 1976 2 | 5,401 | 6,467 | 6.235 | 6,437 | 1,001 |
| 1977 | 5.755 | 6.814 | 6,656 | 6.677 | 1,053 |
Data not available.
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for earlier years are provided on a provisional basis and will be revised upon completion of the survey.
Quality of Coverage
Coverage and enrollment statistics do not provide a total picture of health insurance protection. Coverage can mean a narrow or a comprehensive range of benefits, a large deductible and copayment, or 100 percent reimbursement by the insurer for health care costs. The range of services and the degree to which benefit payments meet the cost of these services provide a measure of the quality of insurance coverage. For some, the source of payment of insurance premiums is also an indicator of coverage quality.
Group Insurance Policies
The Health Insurance Institute's annual sample survey of group health insurance policies provides some measure of the quality of group policies sold by insurance companies. The sample included 33 companies that accounted for half the group business written in the United States in 1976. In 1977, 58 percent of the employees in the survey had their premiums paid entirely by their employers; 4 percent had to pay their own premiums. The cost was shared by the employer and the employee for the remaining 38 percent of the employees surveyed. This was a change from the previous year when employers paid the entire premium for 69 percent of the employees surveyed and only 31 percent had to pay all or part of their own premiums.
Probably most critical to the wage earner and his family is the level of insurance benefits for hospital room and board charges. Among all employees with hospital insurance who were surveyed only 3 percent had basic coverage only. Basic coverage insures a limited range of services and is generally characterized by minimum benefit levels. For example, the majority of those with only basic hospital coverage had a maximum daily room and board benefit of $49 or less. The maximum number of hospital days was under 40, and full reimbursement for miscellaneous hospital expense benefits was under $1,000. Thus, without major medical insurance the insured faced two risks: one, benefits provided might be exhausted, as for example the number of hospital days used might exceed the number of benefit days; and two, benefits paid by the basic plan might be less than actual charges for services.
The remaining 97 percent of the employees with hospital insurance had supplementary or comprehensive major medical coverage of hospital room and board expense. These persons were less likely to suffer catastrophic losses for these services. About half had full payment for semi-private room charges, but a number were subject to a maximum daily benefit of only $59 or less, a maximum of 39 days or less, or a maximum payment of $200 or less. For surgical services, the survey indicated that for 72 percent of employees with such insurance there were unlimited benefits, after a typical $100 deductible and 20 percent co-payments.
Another measure of the adequacy of group insurance policies for workers and their families is afforded by looking at the coverage reported by HII for groups of 25-499 employees. These groups are regarded as having typical benefit patterns. Sixty-one percent of those with hospital coverage received full payment at the semi-private room rate. The average daily room and board benefit for those who were not eligible for full payment was $67. Twenty-one percent of those with surgical coverage were reimbursed at the physician's reasonable and customary rate. For others, the average maximum scheduled surgical benefit was $1,141. The average maximum scheduled benefit for in-hospital physicians' visits was $9, and the most common diagnostic x-ray and laboratory benefit was $100.
Nervous and mental disorder benefits were provided for two out of three employees with comprehensive major medical coverage. Almost 70 percent of these employees had full plan benefits while confined in a hospital, but received reduced or limited benefits for out-of-hospital treatment.
Employees in groups of 25-499 had other benefit limitations as well. Only 54 percent had nursing home or extended care facility coverage, with more than a fourth of these subject to a maximum of less than 70 days coverage. While 92 percent of the employees in these groups had dependent-type coverage and 87 percent had medical care coverage, two out of five in the latter group had no maternity coverage and of those who did have such coverage more than a fourth were eligible for a flat benefit of less than $500.
Although the extent of dental coverage was limited—only 21 percent had this type of coverage—the level of benefits was somewhat better. Forty-six percent of those with dental insurance had comprehensive coverage subject to deductibles and co-insurance, but with a maximum annual benefit of $1,000 or more.
Individual Insurance Policies
Individual (nongroup) policies almost always provide less economic protection than that provided by group insurance. These policies are generally tied to hospitalization and pay fixed amounts per day in the hospital and/or fixed amounts per surgical procedure. As a result of low reimbursement limits and a narrow range of benefits, individual policy holders face relatively large out-of-pocket expenses.
The HIAA reported an estimated 18 million enrollment under age 65 in 1977 in individual basic hospital policies, and an estimated 9 million in basic surgical expense policies. An additional 5.9 million carried major medical coverage for these types of care, either in the form of supplementary major medical insurance or comprehensive major medical policies. These 5.9 million were unlikely to suffer catastrophic losses for hospital-related care and had some level of protection against the cost of physicians' office visits, x-ray and laboratory exams, prescribed drugs, and nursing services. It should be noted, however, that where major medical policies place no limit on policyholder cost-sharing, catastrophic expenses may be incurred through high co-payments. Heavy expenses may also be incurred for noninsured services such as nursing home care, psychiatric care, dental care, or prescribed drugs.
Blue Cross and Blue Shield plans
Blue Cross basic contracts provided service benefits rather than cash indemnities, i.e., hospitals and other providers were paid directly by the plan in lieu of payment to the subscriber of a fixed dollar amount. In addition, most Blue Cross plans provided extended benefits with variable front-end deductibles and 80 percent co-insurance for physicians' services and other professional services, nursing home care, home health services, prescription drugs, durable medical equipment, nursing services, x-ray and laboratory services, blood transfusions, and treatment of mental conditions, alcoholism, and drug addiction.
Blue Shield plans covered more than half of their enrollees under their Usual, Customary and Reasonable (UCR) program, in which payments to physicians are based upon their usual and customary fee in the locality in which they practice, as opposed to the traditional indemnity payment—the allowance of a fixed dollar amount toward the physician's charge. Payments by these Blue Shield plans were usually subject to deductibles and coinsurance payments, however.
Persons Without Private Health Insurance
The Under-Age-65 Group
It is estimated that in 1977 about 38 million persons under age 65 had no private insurance against the costs of hospital-related illnesses. A large number of these persons were self-employed and chose not to buy insurance; others worked for small, low wage-paying employers and could not afford to buy insurance on their own; others were in bad health and could not obtain insurance. Some were unemployed or were receiving assistance in meeting their medical expenses through such public programs as Medicare, Medicaid, Champus, the Veterans Administration, and Workers' Compensation.
The Medicaid program made medical assistance payments to 20.2 million persons in fiscal year 1977. Medicare covered 2.6 million disabled persons for hospital insurance and 2.4 million disabled for supplementary medical insurance in 1977. State and federal workers' compensation programs covered 72.1 million persons for work-related medical expenses in 1977.
According to the 1976 Household Interview Survey conducted by the National Center for Health Statistics (NCHS), 22.8 million persons under age 65 had no public or private coverage of any kind.
The Elderly
An estimated 9 million of the aged had no private hospital insurance; 13 million had no private surgical insurance. As previously noted, virtually all of the aged had coverage for these services under the Medicare program. For prescription drugs or private duty nursing, more than 19 million (80 percent) of the aged had no insurance protection, either through private insurance or through the Medicare program. The NCHS Survey showed only 437,000 aged with no public or private protection at all.
Financial Experience
The discussion that follows provides financial information on three major types of insurers: insurance companies that sell health insurance, Blue Cross and Blue Shield plans, and independent prepayment and self-insured or self-funded plans. Health maintenance organizations that provide and are at risk for health care services to their members are included in the independent plans category.1
Claims expense and operating expenses are measured against premium and subscription income to show the net underwriting gain or loss and other operating results—the proportion of premiums returned as benefits (the claims ratio) and the amount retained for operating expenses, additions to reserves, and profits. Available data on investment income provide some insight into the net income of the insurers. All data are on an incurred or accrual basis.
Industrywide Experience
In 1977, the private health insurance industry collected $47.1 billion in premiums and subscriptions, a 16.3 percent increase over the $40.5 billion collected in 1976 (Table 8). An estimated $36 billion, or 77.1 percent, represented employer contributions in 1977 compared with 74.9 percent contributed by employers in 1976. The insurers returned 88.3 percent of the 1977 premium total in the form of $41.6 billion in benefits, a drop from the 94.8 percent claims ratio in 1976. Operating expenses for 1977 were $5.9 billion and when added to benefit expenditures resulted in a relatively small ($.4 billion) net underwriting loss, an improvement over the $3.1 billion net underwriting loss of 1976. The net underwriting loss in 1975 was also large—$2.5 billion.
Table 8. Financial experience of private insurance organizations, 1975–1977.
| [In millions] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Type of plan | Total income | Subscription or premium -income | Claims expense | Operating expense | Net underwriting gain | Net income | ||||
|
| ||||||||||
| Amount | Percent of premium income | Amount | Percent of premium income | Amount | Percent of premium income | Amount | Percent of total income | |||
| 1977 | ||||||||||
|
|
||||||||||
| Total | (1) | $47,120.0 | $41,594.9 | 88.3 | $5,933.0 | 12.6 | $ —407.9 | —.9 | (1) | (1) |
|
|
||||||||||
| Blue Cross and Blue Shield | $19,857.8 | 19,553.4 | 17,626.2 | 90.1 | 1,330.3 | 6.8 | 596.9 | 3.1 | $ 901.3 | 4.5 |
| Blue Cross | 13,801.6 | 13,606.3 | 12,473.7 | 91.7 | 693.9 | 5.1 | 438.7 | 3.2 | 634.0 | 4.6 |
| Blue Shield | 6,056.2 | 5,947.1 | 5,152.5 | 86.6 | 636.4 | 10.7 | 158.2 | 2.7 | 267.3 | 4.4 |
| Insurance companies | (1) | 22,958.0 | 19,514.3 | 85.0 | 4,286.0 | 18.6 | —836.3 | —3.6 | (1) | (1) |
| Group policies | (1) | 19,375.0 | 17,591.9 | 90.8 | 2,638.6 | 13.6 | —855.5 | —4.4 | (1) | (1) |
| Individual policies | (1) | 3,583.0 | 1,922.4 | 53.7 | 1,641.4 | 45.8 | 19.2 | .5 | (1) | (1) |
| Independent plans 2,3 | 4,938.2 | 4,608.6 | 4,454.0 | 96.6 | 322.7 | 7.0 | —168.1 | —3.6 | 161.5 | 3.3 |
| Consumer | 1,551.0 | 1,445.0 | 1,375.4 | 95.2 | 102.9 | 7.1 | —33.3 | —2.3 | 72.7 | 4.7 |
| Labor-Management | 2,918.3 | 2,706.9 | 2,672.4 | 98.7 | 106.6 | 5.9 | —126.1 | —4.7 | 85.3 | 2.9 |
| Health Professional | 219.2 | 212.6 | 187.0 | 88.0 | 31.7 | 14.9 | —6.1 | —2.9 | .5 | .2 |
| Dental service corporation | 201.7 | 196.2 | 178.2 | 90.8 | 21.1 | 10.8 | —3.1 | —1.6 | 2.4 | 1.2 |
| Vision service corporation | 48.0 | 47.9 | 41.0 | 85.6 | 6.4 | 13.4 | .5 | 1.0 | .6 | 1.3 |
|
|
||||||||||
| 1976 | ||||||||||
|
|
||||||||||
| Total | (1) | $40,505.9 | $38,418.4 | 94.8 | $5,161.3 | 12.7 | $—3.073.8 | —7.6 | (1) | (1) |
|
|
||||||||||
| Blue Cross and Blue Shield | $17,560.1 | 17,268.1 | 16,226.5 | 94.0 | 1,192.8 | 6.9 | —151.2 | —.9 | $ 140.8 | .8 |
| Blue Cross | 12,242.9 | 12,037.4 | 11,624.9 | 96.6 | 623.3 | 5.2 | —210.8 | —1.8 | —5.3 | —.0 |
| Blue Shield | 5,317.2 | 5,230.7 | 4,601.6 | 88.0 | 569.5 | 10.9 | 59.6 | 1.1 | 146.1 | 2.7 |
| Insurance companies | (1) | 19,267.0 | 18,365.0 | 95.3 | 3,689.0 | 19.1 | —2,787.0 | —14.5 | (1) | (1) |
| Group policies | (1) | 15,985.0 | 16,633.8 | 104.1 | 2,154.3 | 13.5 | —2,803.1 | —17.5 | (1) | (1) |
| Individual policies | (1) | 3,282.0 | 1,731.2 | 52.7 | 1,534.7 | 46.8 | 16.1 | .5 | (1) | (1) |
| Independent plans 2,3 | (1) | 3,970.8 | 3,826.9 | 96.4 | 279.5 | 7.0 | —135.6 | —3.4 | (1) | (1) |
| Consumer | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Labor-Management | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Health Professional | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Dental service corporation | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Vision service corporation | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
|
|
||||||||||
| 1975 | ||||||||||
|
|
||||||||||
| Total | (1) | $33,811.4 | $31,917.3 | 94.4 | $4,373.0 | 12.9 | $—2,478.9 | —7.3 | (1) | (1) |
|
|
||||||||||
| Blue Cross and Blue Shield | $14,684.7 | 14,446.4 | 14,192.0 | 98.2 | 1,063.0 | 7.4 | —808.6 | —5.6 | $—570 | —3.9 |
| Blue Cross | 10,225.0 | 10,060.5 | 10,075.9 | 100.2 | 557.1 | 5.5 | —572.5 | —5.7 | —408.0 | —4.0 |
| Blue Shield | 4,459.7 | 4,385.8 | 4,116.1 | 93.9 | 505.9 | 11.5 | —236.2 | —5.4 | —162.3 | —3.6 |
| Insurance companies | (1) | 16,032.0 | 14,525.6 | 90.6 | 3,073.8 | 19.2 | —1,567.4 | —9.8 | (1) | (1) |
| Group policies | (1) | 12,962.0 | 12,956.6 | 100.0 | 1,658.5 | 12.8 | —1,653.1 | —12.8 | (1) | (1) |
| Individual policies | (1) | 3,070.0 | 1,569.0 | 51.1 | 1,415.3 | 46.1 | 85.7 | 2.8 | (1) | (1) |
| Independent plans 2,3 | (1) | 3,333.0 | 3,199.7 | 96.0 | 236.2 | 7.1 | —102.9 | —3.1 | (1) | (1) |
| Consumer | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Labor-Management | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Health Professional | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Dental service corporation | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Vision service corporation | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
Data not available.
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for earlier years are provided on a provisional basis and will be revised upon completion of the survey.
In earlier series, consumer plans were titled community, labor-management plans were titled employer-employee-union, and health professional plans were titled private group clinic.
The 1977 recovery was caused primarily by a slowing in the growth of benefits, which increased by only 8.3 percent as compared to a 20.4 percent increase in 1976 and a 23.4 percent increase in 1975. Premiums showed a somewhat different trend from 1975 to 1977 with increases in growth of 16.4, 19.8 and 16.3 percent, respectively. Operating expenses as a percent of premiums were fairly steady with a slight downward trend (12.9, 12.7, 12.6 percent) for the 1975-77 period. Net cost, the difference between premiums and benefits, increased by a dramatic 164.7 percent in 1977, going from $2.1 billion in 1976 to $5.5 billion in 1977. This kind of difference is normal in a recovery period when premium increases are outpacing benefit increases by a large margin.
Insurance Companies
Insurance companies reported a total of $23.0 billion in premium income in 1977, almost half (48.7 percent) of the industry total and a 19.2 percent increase over their 1976 premium earnings of $19.3 billion. Group policy premiums, which comprised 84.4 percent of the insurance company premium total, increased at an even faster pace (21.2 percent). Individual policy business rose 9.2 percent, a significant increase over the 1976 growth of 6.9 percent.
Conversely, insurance company claims slowed very little growth in 1977. The overall claims in 1977 were $19.5 billion with group claims of $17.6 billion and individual claims of $1.9 billion. The respective growth rates over 1976 were 6.3, 5.8 and 11.0 percent for all policies, group policies, and individual policies.2
The weak growth rate in claims contrasted strongly with the strong growth in premiums in 1977. Nonetheless, insurance companies suffered a net underwriting loss in 1977. When claims expenses were combined with $4.3 billion in operating expenses and deducted from premiums, the result was a net underwriting loss of $.8 billion. However, 1977 was a distinct improvement over the $2.8 billion underwriting loss in 1976 and the $1.6 billion loss in 1975. Operating expenses rose at a rate of 16.0 percent between 1976 and 1977, yet actually declined as a percent of premiums from 19.1 in 1976 to 18.6 in 1977.
Administrative Service Only Agreements (ASO) and Mini-Premium Plans (MPP)
Insurance company premiums and claims data reported by HIAA for the years 1975 and later include Administrative Service Only Agreements and Minimum Premium Plans.
As explained earlier, under ASO agreements the insurance company provides administrative services to another health insurance organization, but it is not at risk for the provision of health benefits to the persons covered by that plan. Minimum premium plans are risk sharing agreements under which an insurance company assumes responsibility for another health insurance organization's health care costs, at some pre-determined point, in return for an actuarially-determined premium payment. Or, the company may underwrite the cost of out-of-area services for a health plan. This type of coverage is typically used by relatively small health plans to protect against some unusually heavy loss or for out-of-area services.
The inclusion of ASO business results in an over-statement of the private health insurance premiums and claims. The companies count the enrollees of the prepaid or self-insured plans and/or the enrollees of the insurance company plans they administer as regularly insured and report the business of such persons under their ASO business. These persons are also reported by the administered plans and/or companies as part of their income and expense. The result is double accounting for the industry as a whole.
As noted earlier in this article, for the years 1975, 1976, and 1977 ASO business was not separated from MPP business in reports by the companies to HIAA. Beginning in 1978, reports from the companies are expected to make this distinction, and the ASO business will not be duplicated in HCFA reports.
For the purpose of measuring the companies' health insurance benefits, it is appropriate to include MPP premiums and benefits for that portion of the risk borne by the carriers. By the same standard, ASO should not be included in the insurance companies' premium and benefit totals because no health coverage risk is involved with these services.
Although it began in the mid-sixties, the ASO-MPP business has not been significant for insurance companies until recent years when it grew very rapidly. For the period 1975 through 1977 ASO-MPP represented 8.2, 14.3, and 17.2 percent of insurance company premium earnings for hospital-medical expenses policies as reported by HIAA. Between 1975 and 1976 the ASO-MPP business grew at a rate of 109.9 percent, and from 1976 to 1977 it grew at a rate of 43.1 percent. ASO-MPP claims showed the same trends as premiums, comprising 8.5, 13.6, and 18.8 percent of insurance company benefits for the 1975-77 period and growing at 102.3 percent from 1975 to 1976 and 46.8 percent from 1976 to 1977.
While it is not yet possible to measure ASO separately from MPP, ASO is reported to be much the larger of the two. Assuming that to be true, its impact on insurance company experience can be gleaned by comparing company data with and without ASO-MPP. The following comparison shows that both income and expense grew faster with the ASO-MPP data included.
| Insurance Company Premium Income | ||||
|---|---|---|---|---|
|
| ||||
| Including ASO-MPP | Percent Change | Excluding ASO-MPP | Percent Change | |
|
| ||||
| 1975 | $16,032 | $14,721 | ||
| 1976 | 19,267 | 20.2 | 16,515 | 12.2 |
| 1977 | 22,958 | 19.2 | 19,019 | 15.2 |
|
|
||||
| Insurance Company Claims Expense | ||||
|
| ||||
| Including ASO-MPP | Percent Change | Excluding ASO-MPP | Percent Change | |
|
| ||||
| 1975 | $14,525.6 | $13,204.6 | ||
| 1976 | 18,365.0 | 26.4 | 15,711.0 | 19.0 |
| 1977 | 19,514.3 | 6.3 | 15,611.3 | −0.6 |
|
| ||||
The ASO-MPP values are large enough to affect the overall health insurance industry premium and benefit totals, as shown below:
Premium and Benefit Growth Rates With and Without ASO-MPP.
| All private insurers | ||||
|---|---|---|---|---|
|
| ||||
| Premiums | Benefits | |||
|
| ||||
| With ASO-MPP | Less ASO-MPP | With ASO-MPP | Less ASO-MPP | |
| 1975 | — | — | — | — |
| 1976 | 19.8 | 16.2 | 20.4 | 16.9 |
| 1977 | 16.3 | 14.4 | 8.3 | 5.4 |
As in the case of insurance companies alone, when ASO-MPP is removed from the industry totals the growth rates of both premiums and benefits are significantly attenuated. As discussed earlier, it is appropriate to include MPP premiums and benefits for that portion of risk insured. The effect on the industry totals will be mitigated when it is possible to remove only the ASO business.
Profits of the Insurance Companies
It is difficult to determine the profits made by the commercial carriers from the health insurance segment of their business. Carriers typically sell a package of insurance (health, life, accident, death and dismemberment, and wage loss), and determining the cost of selling and the income from reserves for health insurance alone is not possible. In addition, company reports to the State insurance departments are not required to separate hospital and medical expense business from loss of income insurance business.
For these reasons it is useful to look at the overall operating results of the companies to determine the net income from underwriting gain and income from investment of reserves. HCFA analyzed the 1974-77 financial experience of 20 of the top 30 insurers representing 56 percent of the industry (based on earned premiums in 1977). The sample reflected the industry-wide split between group and individual policywriters.
As shown in the following table, earned premiums for health and wage loss insurance combined rose 38.2 percent while benefits incurred rose 33.6 percent The companies showed a net gain in all years except 1975.
Claims ratios went from 88.3 percent in 1975 (a net loss year) to 81.0 percent in 1977 (a profitable year). Operating expenses remained stable relative to earned premiums and fluctuated between 15.1 and 15.2 percent. (About 60 percent of operating expense can be attributed to general insurance expenses—underwriting, policy issues, premium collection, claims processing, and legal fees. The remaining 40 percent consists of commissions, state premium taxes, licenses, and fees.)
Net gain (after dividends and income tax) went from a loss of 1.4 percent of earned premiums in 1975 to a gain of 1.9 percent in 1977. When additions to reserves were added to net gain, however, the net loss in 1975 was eliminated. This measure of profitability—the increase in reserves plus the net gain—shows a high of 5.2 percent of earned premiums in 1977. When analyzing profit margins, however, there is a concern in valuating additions to reserves. There are no hard regulations established for determining reserves; the rapidly changing nature of claims negates retrospective experience in calculating prospective reserves, and the States have varying reserve requirements. Thus the valuation of reserves tends to rely on actuarial computations that do not have standardized guidelines.
Health Plus Wage-loss Financial Statistics of Selected Commercial Health Insurers, 1974-77 1.
| Item | Amounts in Millions | |||
|---|---|---|---|---|
|
| ||||
| 1974 | 1975 | 1976 | 1977 | |
| Income, total | 10,658.9 | 11,948.8 | 13,309.4 | 14.841.3 |
| Premiums | 10,326.4 | 11,590.0 | 12,874.6 | 14,269.2 |
| Investment income | 309.6 | 301.8 | 343.5 | 414.6 |
| Other income | 22.9 | 57.0 | 91.3 | 157.5 |
| Benefit expense, total | 8,744.4 | 10,227.3 | 11,032.0 | 11,929.2 |
| Benefits incurred | 8,648.8 | 10,231.0 | 10,723.7 | 11,556.1 |
| Increases in reserves | 184.8 | 192.7 | 153.7 | 463.3 |
| Other loss items | 16.1 | 17.3 | 232.1 | (27.1) |
| Transfers | (75.3) | (213.7) | (77.5) | (63.1) |
| Operating expense | 1,567.7 | 1,744.6 | 1,947.8 | 2,165.3 |
| Gain before dividends | 346.7 | (23.1) | 329.6 | 746.8 |
| Dividends | 97.2 | 71.7 | 169.1 | 324.8 |
| Gain after dividends before income taxes | 249.5 | (94.8) | 160.5 | 422.0 |
| Income tax | 76.5 | 69.5 | 109.2 | 146.9 |
| Net gain | 173.0 | (164.3) | 51.3 | 275.1 |
| Aggregate reserves | 2,451.6 | 2,645.6 | 2,769.5 | 2,701.5 |
20 of top 30 commercial health insurers representing 56 percent of the industry based on earned premiums for 1977. (National Underwriter, June 17, 1978).
In 1977, the net underwriting gain of the 20 companies was 3.8 percent of earned premiums. Income from reserves after Federal income taxes was 1.9 percent of premiums, giving the companies an estimated profit rate after taxes of 5.7 percent. Thus, 5.7 cents plus the 1 cent profit paid to the government as Federal income tax, accounted for about 7 cents of each premium dollar. In 1976 the profit rate for the 20 companies was an estimated 3.4 percent, and in 1975 there was a loss rate of 1.3 percent. Over the 3-year period the profit rate averaged 2.6 percent.
Blue Cross and Blue Shield Plans
The Blue Cross and Blue Shield experience was somewhat different from the remainder of the industry. Their slight enrollment decline was accompanied by an attenuation in the growth of both subscription income and claims expense. In 1977, Blue Cross and Blue Shield plans received a combined total of $19.6 billion from subscribers, which was 41.5 percent of all premiums and subscriptions collected by the industry for the year. In 1977, subscription income increased 13.2 percent over the 1976 total, while in 1976 it increased 19.5 percent over the 1975 total.
Blue Cross and Blue Shield plans incurred claims expenses of $17.6 billion in 1977, or 90.1 percent of their subscription income. In 1976 their benefit payments were 94.0 percent of subscriptions, and in 1975 their claims ratio was 98.2 percent. Both 1975 and 1976 were underwriting loss years for these plans.
The 1977 administrative expense of Blue Cross and Blue Shield plans totaled $1.3 billion or 6.8 percent of subscription income. The 1976 administrative expense ratio was almost the same—6.9 percent. After deducting claims and administrative expenses from subscription income, Blue Cross and Blue Shield plans were left with a net underwriting gain of $.6 billion in 1977, while the remainder of the industry was still experiencing losses. Their 1977 gain is an improvement over their underwriting loss of $.2 billion in 1976, a year when insurance companies experienced heavy underwriting losses.
Independent Plans
The 1977 independent plan data have been estimated on the basis of a new survey sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Final data from the survey are not yet available; the 1977 estimates are therefore preliminary. Also preliminary are the revisions made to the data for the 1973 to 1976 period. Thus, the year to year comparisons shown here represent only general trends.
The independent plan subscription income was $4.6 billion in 1977, up 16.1 percent from the 1976 level of $4.0 billion. Benefit expense, $4.5 billion, grew slightly faster at 16.4 percent. The independent plans' benefits ratio was the highest in the industry in 1977 at 96.6 percent. Benefits ($4.5 billion) combined with an operating expense of $.3 billion and deducted from premium income resulted in a net underwriting loss of $.2 billion in 1977. However, net income for 1977 was on the plus side at about $.2 billion. Independent plans did almost 10 percent of all health insurance business in 1977. Within the plan types, labor-management plans grew most rapidly and in 1977 represented 58.7 percent of the business done by independent plans.
Claims Ratios
Both the Blue Cross and Blue Shield plans and the insurance companies showed a decline in their claims ratios in 1977. The insurance companies' drop was particularly strong, going from 95.3 percent in 1976 to 85.0 in 1977, while Blue Cross and Blue Shield moved from 94.0 percent to 90.1 for the same years. These changes were caused by a sharp deceleration in the growth of benefit payments rather than any major change in premium growth. The claims ratio for the independent plans remained at a high level—96.6 percent.
Trends
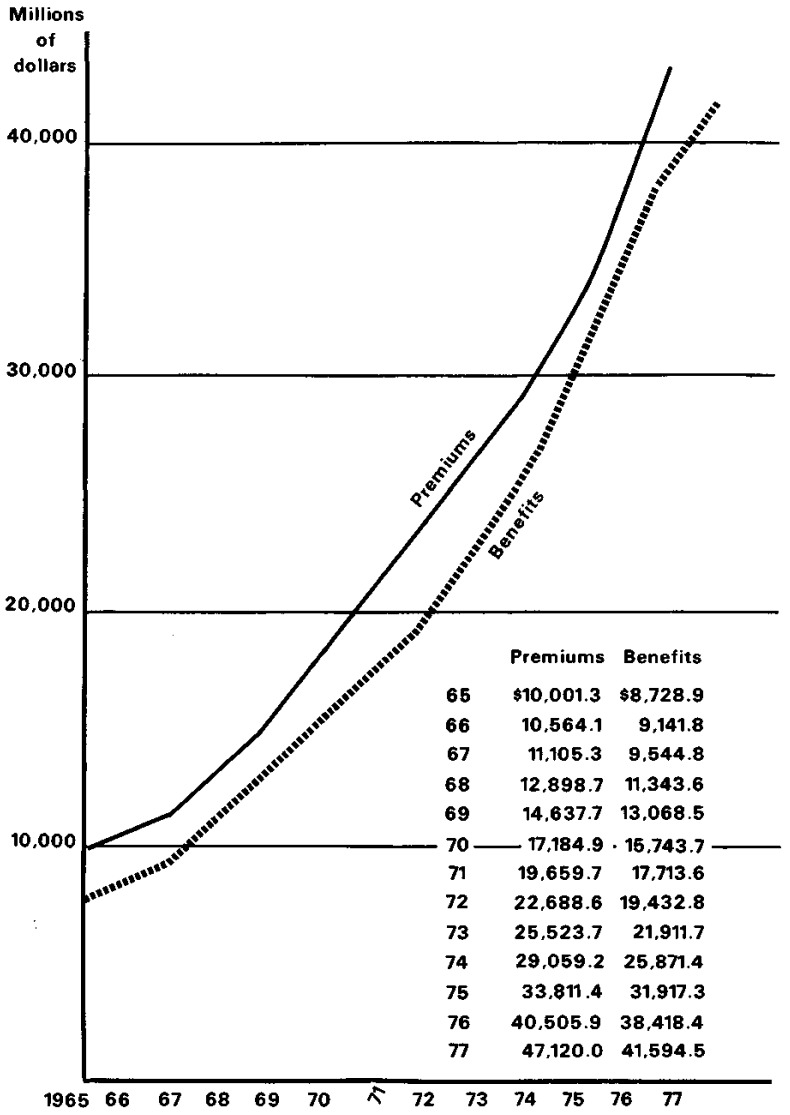
Benefit expenditures grew from $8.7 billion in 1965 to $41.6 billion in 1977, an annual average growth rate of 13.9 percent (Table 9). Chart 1 illustrates the behavior of premiums and benefits from 1965 to 1977. As shown in the table below, in the three years prior to 1977, the rates were 18.1, 23.4, and 20.4 percent. The growth rate of 8.3 percent in 1977 is considerably slower than that of immediately preceding years and also slower than the 12.9 percent 1977 growth in overall health expenditures. The reasons for the significant deceleration are not apparent.
Table 9. Subscription or premium income and benefit expenditures of private health insurance organizations, 1970-1977.
| [In millions] | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Year | All plans | Blue Cross and Blue Shield | Insurance Companies | Independent plans 1 | ||||
|
| ||||||||
| Total | Blue Cross | Blue Shield | Total | Group policies | Individual policies | |||
| Income | ||||||||
|
|
||||||||
| 1950 | $ 1,291.5 | $ 574.0 | $ 436.7 | $ 137.3 | $ 605.0 | $ 333.0 | $ 272.0 | $ 112.5 |
| 1955 | 3,149.6 | 1,292.4 | 910.7 | 381.7 | 1,626.9 | 1,022.5 | 604.4 | 230.3 |
| 1960 | 5,841.0 | 2,482.0 | 1,773.0 | 709.1 | 3,027.0 | 2,104.0 | 923.0 | 331.9 |
| 1965 | 10,001.3 | 4,169.0 | 2,993.7 | 1,175.3 | 5,224.0 | 3,665.0 | 1,559.0 | 608.3 |
| 1966 | 10,564.1 | 4,327.8 | 3,085.9 | 1,241.9 | 5,595.0 | 3,987.0 | 1,608.0 | 641.3 |
| 1967 | 11,105.3 | 4,555.3 | 3,230.0 | 1,325.3 | 5,858.0 | 4,270.0 | 1,588.0 | 692.0 |
| 1968 | 12,898.7 | 5,187.1 | 3,665.0 | 1,522.1 | 6,933.0 | 5,159.0 | 1,774.0 | 778.6 |
| 1969 | 14,657.7 | 6,155.6 | 4,365.2 | 1,790.4 | 7,569.0 | 5,685.0 | 1,884.0 | 933.1 |
| 1970 | 17,184.9 | 7,370.9 | 5,147.1 | 2,223.8 | 8,746.1 | 6,774.1 | 1,972.0 | 1,067.9 |
| 1971 | 19,659.7 | 8,790.2 | 6,239.6 | 2,550.6 | 9,601.6 | 7,231.6 | 2,370.0 | 1,267.9 |
| 1972 | 22,688.6 | 9,923.3 | 7,066.9 | 2,856.4 | 11,345.7 | 8,617.7 | 2,728.0 | 1,419.6 |
| 1973 | 25,523.7 | 11,059.1 | 7,862.1 | 3,197.0 | 12,407.2 | 9,414.2 | 2,993.0 | 2,057.4 |
| 1974 | 29,059.2 | 12,367.0 | 8,647.6 | 3,719.4 | 13,997.0 | 10,720.0 | 3,277.0 | 2,695.2 |
| 1975 | 33,811.4 | 14,446.4 | 10,060.5 | 4,385.8 | 16,032.0 | 12,962.0 | 3,070.0 | 3,333.0 |
| 1976 | 40,505.9 | 17,268.1 | 12,037.4 | 5,230.7 | 19,267.0 | 15,985.0 | 3,282.0 | 3,970.8 |
| 1977 | 47,120.0 | 19,553.4 | 13,606.3 | 5,947.1 | 22,958.0 | 19,375.0 | 3,583.0 | 4,608.6 |
|
|
||||||||
| Benefit expenditures | ||||||||
|
|
||||||||
| 1950 | $ 991.9 | $ 490.6 | $ 382.9 | $ 107.7 | $ 400.0 | $ 257.0 | $ 143.0 | $ 101.3 |
| 1955 | 2,535.7 | 1,146.7 | 832.2 | 314.5 | 1,179.0 | 858.0 | 321.0 | 210.0 |
| 1960 | 4,996.3 | 2,287.1 | 1,646.2 | 640.9 | 2,389.0 | 1,901.0 | 488.0 | 320.2 |
| 1965 | 8,728.9 | 3,912.9 | 2,853.4 | 1,059.5 | 4,265.0 | 3,413.0 | 852.0 | 551.0 |
| 1966 | 9,141.8 | 3,975.4 | 2,882.2 | 1,093.2 | 4,585.0 | 3,711.0 | 874.0 | 581.4 |
| 1967 | 9,544.8 | 4,082.8 | 2,963.1 | 1,119.7 | 4,837.0 | 3,998.0 | 839.0 | 625.0 |
| 1968 | 11,343.6 | 4,840.6 | 3,529.2 | 1,311.4 | 5,791.0 | 4,841.0 | 950.0 | 712.0 |
| 1969 | 13,068.5 | 5,903.1 | 4,271.4 | 1,631.7 | 6,306.0 | 5,349.0 | 957.0 | 859.4 |
| 1970 | 15,743.7 | 7,060.2 | 5,009.3 | 2,050.9 | 7,656.1 | 6,510.1 | 1,146.0 | 1,027.4 |
| 1971 | 17,713.6 | 8,178.7 | 5,906.9 | 2,271.8 | 8,341.5 | 7,067.5 | 1,274.0 | 1,193.4 |
| 1972 | 19,432.8 | 8,990.9 | 6,501.3 | 2,489.6 | 9,123.6 | 7,757.5 | 1,366.0 | 1,318.3 |
| 1973 | 21,911.7 | 10,004.2 | 7,187.3 | 2,816.9 | 9,962.1 | 8,405.9 | 1,556.2 | 1,945.4 |
| 1974 | 25,871.4 | 11,639.5 | 8,311.1 | 3,328.4 | 11,659.3 | 10,125.8 | 1,533.5 | 2,572.6 |
| 1975 | 31,917.3 | 14,192.0 | 10,075.9 | 4,116.1 | 14,525.6 | 12,956.6 | 1,569.0 | 3,199.7 |
| 1976 | 38,418.4 | 16,226.5 | 11,624.9 | 4,601.6 | 18,365.0 | 16,633.8 | 1,731.2 | 3,826.9 |
| 1977 | 41,594.5 | 17,626.2 | 12,473.7 | 5,152.5 | 19,514.3 | 17,591.9 | 1,922.4 | 4,454.0 |
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for 1973 to 1976 are provided on a provisional basis and will be revised upon completion of the survey.
Chart 1. All Private Health Insurance Premiums and Benefits 1966 - 77.
Premium and Claims Growth Rates.
| Industry Totals | Insurance Companies | Blue Cross Blue Shield | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Premiums | Claims | Premiums | Claims | Premiums | Claims | |
| 1974 | 13.9 | 18.1 | 12.8 | 17.0 | 11.8 | 16.3 |
| 1975 | 16.4 | 23.4 | 14.5 | 24.6 | 16.8 | 21.9 |
| 1976 | 19.8 | 20.4 | 20.2 | 26.4 | 19.5 | 14.3 |
| 1977 | 16.3 | 8.3 | 19.2 | 6.3 | 13.2 | 8.6 |
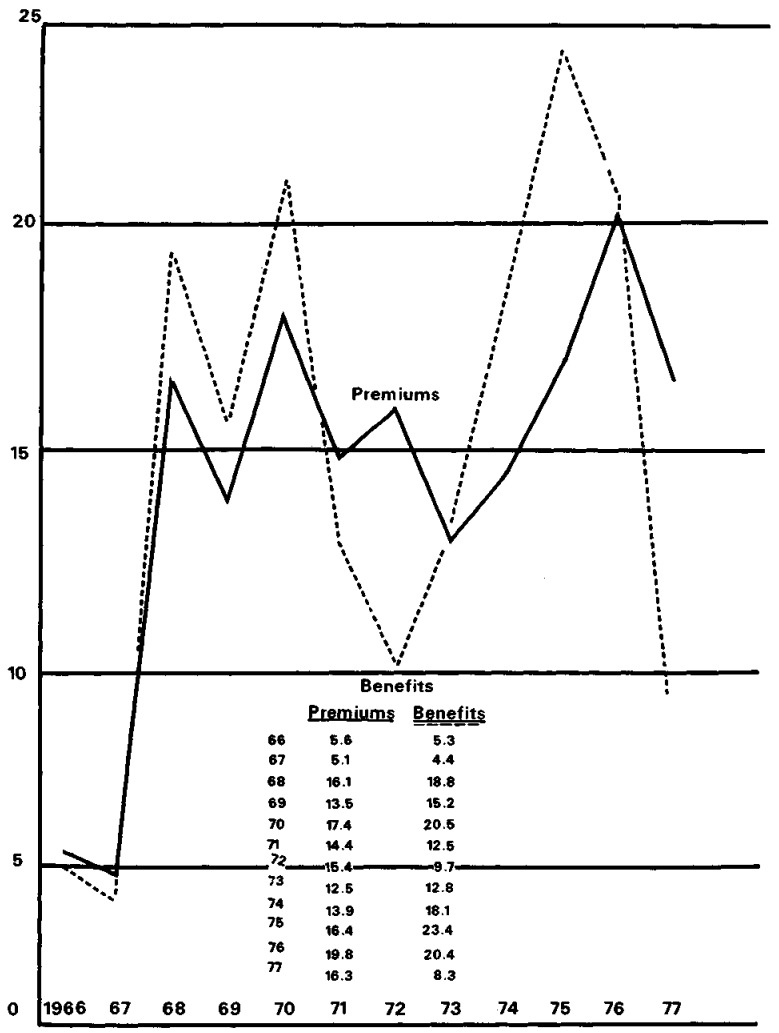
Premium growth outpaced claims growth in 1977 for the first year since 1973 (See Chart 2). Premium growth is a natural consequence of rapidly growing claims, which in turn reflect health care costs and an increase in the range of health care benefits covered by insurance. Though premiums grew faster than benefits in 1977, the industry in general still suffered a net underwriting loss. Thus, it may be expected that premiums, particularly for insurance companies, will show strong growth relative to benefits again in 1978. However, if the moderation in price increases continues, as shown in the table below, then premiums may show some deceleration in growth rate for 1978.
Chart 2. Percent Change In Private Health Premiums and Benefits 1966 - 77.
Annual Percentage Change for Selected Consumer Price Indexes 1.
| Year | 1973 | 1974 | 1975 | 1976 | 1977 | 1978 |
|---|---|---|---|---|---|---|
| All items | 6.2 | 11.0 | 9.1 | 5.8 | 6.5 | 7.7 |
| Medical care | 3.9 | 9.3 | 12.0 | 9.5 | 9.6 | 8.4 |
| Medical care services | 4.4 | 10.3 | 12.6 | 10.1 | 9.9 | 8.6 |
| Professional service | 3.3 | 8.7 | 11.0 | 9.1 | 8.2 | 7.6 |
| Physicians' services | 3.3 | 9.2 | 12.3 | 11.3 | 9.3 | 8.3 |
| Dental services | 3.1 | 7.6 | 10.3 | 6.4 | 7.5 | 7.0 |
| Other medical care services | 5.7 | 12.0 | 14.3 | 11.0 | 11.8 | 9.6 |
| Hospital room | 4.7 | 10.7 | 17.2 | 13.8 | 11.5 | 11.0 |
Based on data from the Bureau of Labor Statistics. Department of Labor.
Benefit Expenditures
Blue Cross and Blue Shield plans had the largest amount of hospital care expenditures in 1977, 46.8 percent of the $24.6 billion total (Table 10). Insurance companies expended almost as much, with 45.8 percent of the total. Independent plans had 7.4 percent of total insurance for hospital care. For physicians' care, the companies' expenditures represented 47.6 percent of the industry total of $12.5 billion; Blue Cross and Blue Shield plans had 38.6 percent; and independent plans supplied the remaining 13.8 percent. Independent plans had an even larger share of the $1.1 billion expended in 1977 by the industry for prescribed drugs (out-of-hospital), with 25.2 percent of the total. Blue Cross and Blue Shield plans had a 31.3 percent share of drug expenditures, and insurance companies had the largest share for drug expenditures with 43.5 percent of the total.
Table 10. Benefit expenditures of private health insurance organizations, by specified type of care, 1977.
| [In millions] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Type of plan | Total | Hospital care | Physicians' services | Dental care | Prescribed Drugs (out-of-hospital) | Private Duty nursing | Visiting Nurse service | Nursing Home care | Vision care | Other types of care |
| Total | $41,594.5 | $24,570.8 | $12,535.4 | $2,245.9 | $1,132.3 | $236.7 | $22.6 | $98.4 | $110.8 | $641.6 |
| Blue Cross and Blue Shield | 17,626.2 | 11,505.2 | 4,834.6 | 237.4 | 354.0 | 25.6 | 15.7 | 33.9 | 11.5 | 608.3 |
| Blue Cross | 12,473.7 | 11,280.2 | 451.3 | 96.7 | 210.2 | 21.7 | 14.1 | 31.0 | 4.0 | 364.5 |
| Blue Shield | 5,152.5 | 225.0 | 4,383.3 | 140.7 | 143.8 | 3.9 | 1.6 | 2.9 | 7.5 | 243.8 |
| Insurance companies | 19,514.3 | 11,244.9 | 5,970.3 | 1,531.5 | 492.6 | 201.7 | (1) | 54.9 | (1) | 18.4 |
| Group policies | 17,591.9 | 9,983.2 | 5,356.1 | 1,531.5 | 488.2 | 186.3 | (1) | 30.5 | (1) | 16.1 |
| Individual policies | 1,992.4 | 1,261.7 | 614.2 | 0 | 4.4 | 15.4 | (1) | 24.4 | (1) | 2.3 |
| Independent plans 2,3 | 4,454.0 | 1,820.7 | 1,730.5 | 477.0 | 285.7 | 9.4 | 6.9 | 9.6 | 99.3 | 14.9 |
| Consumer | 1,375.4 | 441.4 | 786.6 | 35.3 | 72.3 | 4.3 | 1.3 | .6 | 23.2 | 10.4 |
| Labor-Management | 2,672.4 | 1,315.6 | 864.2 | 232.7 | 207.6 | 4.8 | 5.5 | 8.9 | 29.1 | 4.0 |
| Health Professional | 187.0 | 63.7 | 79.7 | 30.8 | 5.8 | .3 | .1 | .1 | 6.0 | .5 |
| Dental service corporation | 178.2 | ...... | ...... | ..... | .... | .... | ... | ... | ... | .... |
| Vision service corporation | 41.0 | ...... | ...... | 178.2 | .... | .... | ... | ... | 41.0 | .... |
Included in “other types of care.”
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA.
In earlier series, consumer plans were titled community, labor-management plans were titled employer-employee-union, and health professional plans were titled private group clinic.
Dental care benefits in 1977 were $2.2 billion. Of this total, insurance companies accounted for 68.2 percent. Independent plans were next with 21.2 percent of the total, and Blue Cross and Blue Shield accounted for the remainder, 10.6 percent. Finally, for all other types of care in 1977, the industry total of $1.1 billion was shared at $.7, $.3 and $.1 billion respectively for Blue Cross and Blue Shield plans, insurance companies, and independent plans. They represented 62.6, 24.8, and 12.6 percent of the total expenditures on all other types of care in 1977.
No new trends have appeared in the percent distribution of benefit expenditures (Table 11). Almost ninety percent (89.2) of all benefit expenditures in 1977 went for hospital (59.1) and physicians' care (30.1). Another five percent (5.4) was paid for dental care, and almost three percent (2.7) was paid for prescribed drugs (out-of-hospital). The remaining three percent (2.7) went for private duty nursing (.6), visiting nurse services (.1), nursing home care (.2), vision care (.3), and other types of health care (1.5).
Table 11. Amount and percentage distribution of benefit expenditures of all private health insurance organizations, by specified type of care, 1950-1977.
| Year | Total | Hospital care | Physicians' services | Prescribed drugs(out-of-hospital) | Dental care | Other types of care |
|---|---|---|---|---|---|---|
| Amount (in millions) | ||||||
|
|
||||||
| 1950 | $ 992 | $ 680 | $ 312 | (1) | (1) | (2) |
| 1955 | 2,536 | 1,679 | 857 | (1) | (1) | (2) |
| 1960 | 4,996 | 3,304 | 1,593 | (1) | (1) | $ 99 |
| 1965 | 8,729 | 5,790 | 2,680 | (1) | (1) | 259 |
| 1966 | 9,142 | 5,993 | 2,831 | (1) | (1) | 318 |
| 1967 | 9,545 | 6,134 | 2,964 | (1) | (1) | 447 |
| 1968 | 11,344 | 7,329 | 3,477 | (1) | (1) | 538 |
| 1969 | 13,069 | 8,356 | 4,029 | (1) | (1) | 684 |
| 1970 | 15,744 | 10,008 | 4,908 | $ 310 | $ 240 | 278 |
| 1971 | 17,713 | 11,279 | 5,430 | 402 | 304 | 298 |
| 1972 | 1.9,429 | 12,162 | 6,062 | 427 | 389 | 389 |
| 1973 3 | 21,912 | (1) | (1) | (1) | (1) | (1) |
| 1974 3 | 25,871 | (1) | (1) | (1) | (1) | (1) |
| 1975 3 | 31,917 | 19,207 | 9,845 | 768 | 1,421 | 676 |
| 1976 3 | 38,418 | 22,954 | 11,495 | 981 | 2,087 | 901 |
| 1977 | 41,594 | 24,571 | 12,535 | 1,132 | 2,246 | 1,110 |
|
|
||||||
| Percentage distribution | ||||||
|
|
||||||
| 1950 | 100.0 | 68.5 | 31.5 | (1) | (1) | (2) |
| 1955 | 100.0 | 66.2 | 33.8 | (1) | (1) | (2) |
| 1960 | 100.0 | 66.1 | 31.9 | (1) | (1) | 2.0 |
| 1965 | 100.0 | 66.3 | 30.7 | (1) | (1) | 3.0 |
| 1966 | 100.0 | 65.5 | 31.0 | (1) | (1) | 3.5 |
| 1967 | 100.0 | 64.3 | 31.0 | (1) | (1) | 4.7 |
| 1968 | 100.0 | 64.6 | 30.7 | (1) | (1) | 4.7 |
| 1969 | 100.0 | 63.9 | 30.8 | (1) | (1) | 5.3 |
| 1970 | 100.0 | 63.6 | 31.2 | 2.0 | 1.5 | 1.8 |
| 1971 | 100.0 | 63.7 | 30.7 | 2.3 | 1.7 | 1.7 |
| 1972 | 100.0 | 62.6 | 31.2 | 2.2 | 2.0 | 2.0 |
| 1973 | 100.0 | (1) | (1) | (1) | (1) | (1) |
| 1974 | 100.0 | (1) | (1) | (1) | (1) | (1) |
| 1975 | 100.0 | 60.2 | 30.8 | 2.4 | 4.5 | 2.1 |
| 1976 | 100.0 | 59.7 | 29.3 | 2.6 | 5.4 | 2.3 |
| 1977 | 100.0 | 59.1 | 30.1 | 2.7 | 5.4 | 2.7 |
Data not available.
Included in “physicians' services.”
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for earlier years are provided on a provisional basis and will be revised upon completion of the survey.
Although hospital care continued its gradual decline as a share of total expenditures, it still accounted for almost sixty percent of total benefits in 1977. Prescribed drugs (out-of-hospital) and dental care continued to gain in their shares of the expenditure distribution, while physicians' care remained fairly constant. Nonhospital, nonphysician care has grown from 5.3 percent in 1970 to 10.8 percent in 1977, reflecting the increased coverage for these types of care.
Like benefit expenditures in general, each type of benefit showed a deceleration in growth rate in 1977, as the table below shows.
| 1976 | 1977 | |
|---|---|---|
| Total | 20.4 | 8.3 |
| Hospital care | 19.5 | 7.0 |
| Physicians' services | 16.8 | 9.0 |
| Prescribed drugs (out-of-hospital) | 27.8 | 15.4 |
| Dental care | 46.8 | 7.6 1 |
| Other types of care | 33.3 | 23.2 |
The sharp drop in dental care is accentuated by a correction in the 1977 data from Delta Dental Association. The data for earlier years included significant amounts of reimbursements from public programs. Efforts are being made to remove the public money from the years prior to 1977, but for now an inconsistency exists.
It is not clear how the 1978 moderation in medical care price increases indicated by the Consumer Price Index for medical care will affect the distribution of benefit expenditures in the future. At this point there is no reason to expect any major shift.
Operating Expense Ratios
Although operating expenses in dollars rose at a 15.0 percent rate in 1977, as a percent of premium income it continued the gradual declining trend begun in 1975 (Table 12). This decline was not surprising in view of the rapid growth of premium income in recent years.
Table 12. Operating expense of private health organizations as a percentage of premium income, 1970–1977.
| Type of plan | 1970 | 1971 | 1972 | 1973 | 1974 | 1975 | 1976 | 1977 |
|---|---|---|---|---|---|---|---|---|
| Total | 14.0 | 13.3 | 14.2 | 13.8 | 13.9 | 12.9 | 12.7 | 12.6 |
| Blue Cross and Blue Shield | 7.2 | 6.9 | 6.9 | 7.0 | 7.4 | 7.4 | 6.9 | 6.8 |
| Blue Cross | 5.6 | 5.3 | 5.2 | 5.2 | 5.4 | 5.5 | 5.2 | 5.1 |
| Blue Shield | 11.0 | 10.5 | 11.3 | 11.5 | 11.8 | 11.5 | 10.9 | 10.7 |
| Insurance companies | 20.4 | 19.9 | 21.5 | 20.9 | 21.0 | 19.2 | 19.1 | 18.6 |
| Group policies | 12.8 | 12.7 | 13.4 | 13.0 | 13.0 | 12.8 | 13.5 | 13.6 |
| Individual policies | 46.6 | 47.1 | 47.0 | 47.0 | 47.0 | 46.1 | 46.8 | 45.8 |
| Independent plans 1,2 | 7.7 | 7.5 | 7.0 | 7.3 | 7.2 | 7.1 | 7.0 | 7.0 |
| Consumer | 7.2 | 6.7 | 6.9 | (3) | (3) | (3) | (3) | 7.1 |
| Labor-Management | 7.7 | 7.8 | 6.0 | (3) | (3) | (3) | (3) | 5.9 |
| Health Professional | (3) | (3) | (3) | (3) | (3) | (3) | (3) | 14.9 |
| Dental service corporation | (3) | (3) | (3) | (3) | (3) | (3) | (3) | 10.8 |
| Vision service corporation | (3) | (3) | (3) | (3) | (3) | (3) | (3) | 13.4 |
In earlier series, consumer plans were titled community, labor-management plans were titled employer-employee-union, and health professional plans were titled private group practice.
Data for 1977 are based on a new sample drawn from the 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans being conducted by HCFA. Data for earlier years are provided on a provisional basis and will be revised upon completion of the survey.
Data not available.
As in years past, there was wide variation in the operating expense ratio for the various types of insurers. Such features as the complexity of claims processed, acquisition costs, and other expenses of doing business—commissions, taxes, licenses and fees—caused these differences. Blue Cross plans have historically had the lowest operating expense ratio, just above 5 percent for all of the seventies, largely because hospital claims are not as complex as other kinds of claims, and hospital claims comprise most of the Blue Cross business. Blue Shield, which handles surgical-medical claims, has consistantly had an expense ratio about twice as large as that of Blue Cross.
The operating expense ratio of insurance company group business continued to be slightly higher than Blue Shield's, the difference stemming from the taxes the companies pay. The operating expense ratio of insurance company individual policy business was the highest for the industry at 45.8 percent. The reason for this high operating expense ratio is that individual policies are expensive to sell and administer. The operating expenses of independent plans have always been relatively low (7.0 percent of subscription income in 1977) primarily because they tend to deal with group situations which are less costly to administer.
The Consumer
Consumer Net Cost
Private health insurance cost consumers $5.5 billion above the amounts they received from insurers for claims or benefits in 1977. This $5.5 billion was retained by insurers to cover operating expenses, profits, and additions to reserves. As the table below shows, the 1977 net costs were more than double the 1976 level. Preliminary estimates for 1978 indicate that the same trend will continue, although not as strongly. The series shown below also indicates that net cost fluctuates quite a bit over time, usually reflecting the general business conditions in the health insurance industry, and in turn affecting the yearly increases in reserves and net gain of the insurers.
| Year | Total | Blue Cross and Blue Shield | Insurance companies | Independent plans |
|---|---|---|---|---|
| 1970 | 1,441.2 | 310.7 | 1,090.0 | 40.5 |
| 1971 | 1,946.1 | 611.5 | 1,260.1 | 74.5 |
| 1972 | 3,255.8 | 932.4 | 2,222.1 | 101.3 |
| 1973 | 3,612.0 | 1,054.9 | 2,445.1 | 112.0 |
| 1974 | 3,187.8 | 727.5 | 2,337.7 | 122.6 |
| 1975 | 1,894.1 | 254.4 | 1,506.4 | 133.3 |
| 1976 | 2,087.5 | 1,041.6 | 902.0 | 143.9 |
| 1977 | 5,525.5 | 1,927.2 | 3,443.7 | 154.6 |
Portion of Consumer Expenditures Met by Insurance
Private health insurance met 45.5 percent of the $89.1 billion spent by consumers in 1977 for health care, a drop from the 47.0 percent covered in 1976. The remaining 54.5 percent was direct out-of-pocket expense for noncovered and partially covered personal health care services. Employer payments for health insurance premiums are counted here as consumer expenses since the payments are considered to be part of employee income.
As the table below shows, the drop in the percent of consumer health care paid for by private health insurance was most notable in hospital care where the percent went from 84.6 to 79.3. This is the lowest percent since 1974 and the largest decline in the period from 1960 to 1977. The reason for this decline can be seen in Table 11. Benefit expenditures for hospital care increased only 7.0 percent in 1977 compared to a 19.5 percent increase in 1976. Physicians' services, which showed a slight drop in the percent of cost met by private health insurance (53.1 to 52.9), shows a benefit expenditure trend similar to hospital care; growth slowed from 16.8 in 1976 to 9.0 percent in 1977. The drop in overall costs met by insurance in 1977 is explained by these two types of care which comprise almost ninety percent of all benefit expenditures.
The portion of consumer expenditures for dental care met by insurance has risen to 20.2 percent, a trend of steady growth since 1965 when virtually no costs (1.6 percent) were paid by insurance. While the insurance share of payments for drugs and all other types of care have also grown over time, consumer out-of-pocket expenditures are still 92.1 and 91.2 percent, respectively, for these two types of care.
| Year | Total | Hospital care | Physicians' services | Prescribed drugs (out-of-hospital) | Dental care | Other types of care |
|---|---|---|---|---|---|---|
| 1950 | 12.2 | 37.1 | 12.0 | (1) | (1) | (1) |
| 1960 | 27.8 | 64.7 | 30.0 | (1) | (1) | 5.0 |
| 1965 | 30.5 | 70.1 | 34.0 | 2.4 | 1.6 | 2.0 |
| 1966 | 30.4 | 71.0 | 34.0 | 2.7 | 2.0 | 2.2 |
| 1967 | 31.8 | 76.7 | 36.7 | 3.5 | 2.5 | 3.4 |
| 1968 | 34.5 | 78.8 | 40.5 | 3.6 | 3.1 | 3.8 |
| 1969 | 35.5 | 77.7 | 41.1 | 4.0 | 3.9 | 4.7 |
| 1970 | 37.2 | 77.7 | 43.7 | 3.9 | 5.3 | 4.9 |
| 1971 | 39.1 | 80.9 | 43.7 | 4.9 | 6.3 | 5.3 |
| 1972 | 39.0 | 76.5 | 45.8 | 5.0 | 7.2 | 5.4 |
| 1973 | 39.0 | 75.4 | 46.0 | 5.6 | 8.1 | 6.1 |
| 1974 | 41.4 | 77.3 | 49.8 | 6.2 | 11.0 | 7.2 |
| 1975 | 45.0 | 82.6 | 51.3 | 6.7 | 15.8 | 7.2 |
| 1976 | 47.0 | 84.6 | 53.1 | 7.9 | 19.6 | 8.2 |
| 1977 | 45.5 | 79.3 | 52.9 | 7.9 | 20.2 | 8.8 |
Source: Robert Gibson, the Division of National Cost Estimates, Office of Financial and Actuarial Analysis.
Technical Note
Sources of Gross Enrollment Data
Gross enrollment figures are total enrollments reported by the various insurers, by type of care. No deductions are made for duplication among insurers or for both group and individual policies of insurance companies.
Blue Cross and Blue Shield data were supplied by the Blue Cross and Blue Shield Associations from data reported to them by their various plans in the United States. Gross enrollments for hospital and surgical care, for physicians' in-hospital visits, and home and office visits were provided separately by Blue Cross and Blue Shield plans for two age groups: (1) Regular membership (under age 65), and (2) coverage complementary to Medicare (for those aged 65 and over and disabled members under age 65 eligible for Medicare). For all other types of care, enrollments were reported jointly by the Blue Cross and Blue Shield Associations. Major-medical coverage was also reported jointly, but information was available only for the combined age groups. The Office of Research, Demonstrations, and Statistics (ORDS) of HCFA adjusted the data to exclude enrollments for underwritten welfare programs.
The data for insurance companies were compiled by the Health Insurance Association of America (HIAA) from its annual survey of the number of persons in the United States covered under group and individual insurance policies. Gross enrollments for hospital, surgical, regular medical, and major-medical (supplementary and comprehensive) policies were reported for persons under age 65 and those aged 65 and over. The enrollments for persons under age 65 included some 12 million persons covered under insurance company administrative service agreements and minimum premium plans.
Since 1974, HIAA has used the gross enrollments under major-medical plans for both age groups to represent gross enrollments for prescribed drugs and nursing services. Major-medical coverage is also the primary determinant of enrollment of persons under age 65 and aged 65 and over for the following services: physicians' inhospital visits and home and office visits, and x-ray and laboratory examinations. Dental enrollment was reported by HIAA for the combined age groups.
For the independent health insurance plans, the 1977 data were based on estimates from the ORDS annual survey of such plans. The 1978 Nationwide Survey of Independent Prepaid and Self-insured Health Plans has served as the sampling frame for this year's survey. A stratified, random sample of 151 plans was drawn based on enrollment size. When the 1978 survey is complete it will serve as a benchmark for the years between 1972 and 1977. As a temporary measure, data for 1973 through 1976 have been adjusted to the 1978 sample level by a linear interpolation.
ORDS Estimates of Net Coverage
Net figures are enrollments by type of care after deductions for duplicate coverage for persons protected by more than one type of insurer or by more than one insurance company plan. Net coverage has been projected on the basis of the 1976 to 1977 movement in gross enrollment. The 1976 net enrollment used as the base for the projection was developed from the National Center for Health Statistics (NCHS) household interview data, from HCFA's Current Medicare Survey, and from other sources. The assumption underlying the use of gross enrollment for the 1977 estimates is that a strong correlation exists between gross and net enrollments.
The split for net enrollment of those under age 65 and those age 65 and over was also estimated on the basis of gross enrollments. The exception to this method was physicians' in-hospital visits, which was estimated by using data on net regular medical-expense coverage for HIAA.
Sources of Financial Data
The data for Blue Cross and Blue Shield plans shown in Table 8 are based on financial statements supplied by the Blue Cross and Blue Shield Associations for all plans. Duplication resulting from the fact that 22 joint Blue Cross-Blue Shield plans report identical data to both national organizations has been eliminated. Data for Health Services, Inc., and for Medical Indemnity of America, Inc. (insurance companies owned by the Blue Cross and Blue Shield Associations, respectively) have been included.
Data on premium income and benefit expense of insurance companies were provided by HIAA, based on figures published by the National Underwriter Company. The data are adjusted by HIAA to eliminate premiums and estimated losses for accidental death and dismemberment insurance and to include any companies that do not appear in the National Underwriter figures.
Premium income and claims reported by HIAA for 1975, 1976, and 1977 include business for administrative service agreements and minimum premium plans. In previous years, only portions of this business were included in HIAA statistics, but a new data-collection mechanism initiated by HIAA in 1975 makes fuller reporting possible. The HIAA has estimated the premiums for this category of business (for companies reporting these items) at about $1.3, $2.8 and $3.9 billion in 1975, 1976, and 1977 respectively. Benefits for those years were $1.3, $2.7, and $3.9 billion.
Operating expenses were estimated by applying the ratio of operating expense to premium income derived from the National Underwriter aggregates to the figures for premium income provided by HIAA. 1
The data for independent plans are ORDS estimates based on its 1978 survey.
Acknowledgments
Robert J. Henkel, Summer Intern from the University of Pittsburgh, contributed to this article.
Footnotes
The 1973-76 data for independent plans are provisional estimates subject to revisions after completion of the 1978 Nationwide Survey of Independent Prepaid and Self-insured plans.
Insurance company claims are reported by HIAA on a paid rather than incurred basis. Claims incurred in any given year are equal to the claims paid for that year plus thirty percent of the difference between claims paid in the current year and in the preceding years. HIAA developed and derived this conversion method based on several years of data. It is subject to the variability inherent in a static formula applied to a dynamic environment.
National Underwriter Company, 1978 Argus Chart of Health Insurance, 1978, page 3.
Contributor Information
Marjorie Smith Carroll, Marjorie Smith Carroll is a social science research analyst with the Health Care Financing Administration's Division of National Cost Estimates, Office of Financial and Actuarial Analysis.
Ross H. Arnett, III, Ross H. Arnett III is an economist in the Health Care Financing Administration's Division of National Cost Estimates, Office of Financial and Actuarial Analysis.