Abstract
A physician's Medicare assignment rate is one measure of his or her willingness to participate in the Medicare program. The assignment rate reflects the proportion of services provided to Medicare beneficiaries for which the physician accepts the Medicare reasonable fee as payment in full. Generally, Medicare reasonable fees are lower than the payment which a physician receives from providing the same service to a private patient or to a Medicare patient who is not treated on assignment. Because Medicare eligibles not treated on an assigned basis are financially liable for the difference between the physician's charge and the Medicare reasonable fee, the assignment rate is an indication of the out-of-pocket costs borne by Medicare eligibles.
One factor which may affect the willingness of physicians to accept patients on assignment is the difference between the reimbursement which he or she may receive in the private market and the fee received from treating Medicare eligibles on assignment. Throughout this paper we assume that the physician's private price or billed charge is equivalent to the level of reimbursement received from treating privately insured patients and Medicare non-assigned patients. Since the level of reimbursement is generally no greater than the billed charge and may be less, this assumption may overstate the actual reimbursement received by the physician. In all instances, reimbursement refers to the aggregate amount received by the physician from all sources for a given service. The lower a physician's Medicare reasonable fee relative to the private market fee the less willing he/she may be to participate in Medicare assignment. This paper examines the effect of changes in Medicare reimbursement on the assignment rates of physicians. It also predicts Medicare assignment rates under a policy option which would increase Medicare reasonable fees to the level of prevailing fees.
Medicare Reimbursement
Medicare legislation originally provided for reimbursement of physicians on the basis of their reasonable, customary, and prevailing charges. Physicians were paid by Medicare on the basis of their reasonable charge, which is the lowest of: (1) the actual charge for the service provided, (2) the physician's median (customary) charge for services rendered during the calendar year immediately preceding the fee screen year, or (3) the prevailing charge, set at the 75th percentile of all customary charges made for similar services in the same geographic area.1
Although the CPR methodology for determining the reasonable fee put some constraints on the amount which the Medicare program will pay physicians for their services to the elderly, it does not necessarily constrain the out-of-pocket costs of the elderly for medical care. Physicians participating in the Medicare program are permitted two billing options, assignment and non-assignment, which they may exercise on a claim-by-claim basis. When a claim is assigned, physicians submit their bills directly to the Medicare carrier for their area. Medicare pays the physician 80 percent of the reasonable charge for the service, less any unpaid deductible. The physician bills the patient for the 20 percent coinsurance and any unpaid deductible.
The second option is to bill on a non-assigned basis. Physicians choosing non-assignment must bill the patient directly for the full amount charged. The patient in turn pays the physician directly for the services rendered and secures reimbursement from Medicare for 80 percent of the reasonable charge, less any unpaid deductible. Patients who are treated on a non-assigned basis are liable for the entire difference between the billed and reasonable charges, as well as the coinsurance and the deductible. From the physician's perspective, treating non-assigned Medicare patients is equivalent to seeing private patients.
Physicians treating elderly patients who are also eligible for Medicaid do not have the same billing options. Joint Medicare/Medicaid claims are in practicality only taken on an assigned basis. The reimbursement levels are equivalent to the reasonable charge as determined by the Medicare carrier, and Medicaid picks up the coinsurance and the deductible on behalf of the patient. The only option the physician has in this case is to not treat the patient at all.
Because patients whose physicians do not accept assignment generally face larger out-of-pocket expenditures than those treated on assignment, the assignment rates of physicians provide one indication of the share of the cost borne by the beneficiaries. Increases in the assignment rates of physicians are desirable because (ceterus paribus) they may reduce costs of medical care for the elderly. By examining how the assignment rate changes when billed charges and reasonable fees change, this paper will provide evidence on the extent to which changes in Medicare reimbursement can be used to alter the assignment rate.
Analytic Framework
The conceptual framework to be used in analyzing the Medicare assignment decision has been developed by Sloan, Mitchell, and Cromwell (1978) and Sloan and Steinwald (1978) and extended by Hadley and Lee (1978). The analysis assumes that the physician firm is a monopolistic competitor. The demand curve facing a physician is therefore downward sloping, and a physician must set price and output accordingly. According to the model the physician treats five types of patients; private, Medicare non-assigned, Medicare assigned, joint Medicare/Medicaid (mandatory assigned patients), and Medicaid non-aged. In treating the five patient groups the physician will receive three different fees. For the private patients and Medicare non-assigned patients treated, the physician is reimbursed an amount equal to the billed charge. For treating Medicare assigned patients and joint Medicare/Medicaid eligibles, the physician is reimbursed an amount equal to the Medicare reasonable fee. For services rendered to the non-aged Medicaid eligibles, the physician is reimbursed at the Medicaid fee level. In general, a physician's billed charge is higher than his/her Medicare reasonable fee, which in turn is higher than the Medicaid fee.
Given these three different prices facing a physician, the model predicts that physicians will satisfy the demand for care for each higher fee market before treating patients in the lower fee market. The number of markets in which a physician participates will depend on the intersection of his marginal cost curve and the fee schedules. Individuals with higher marginal cost schedules might participate in only the private market. Those with low marginal cost schedules may participate in the private, Medicare, and Medicaid markets.2
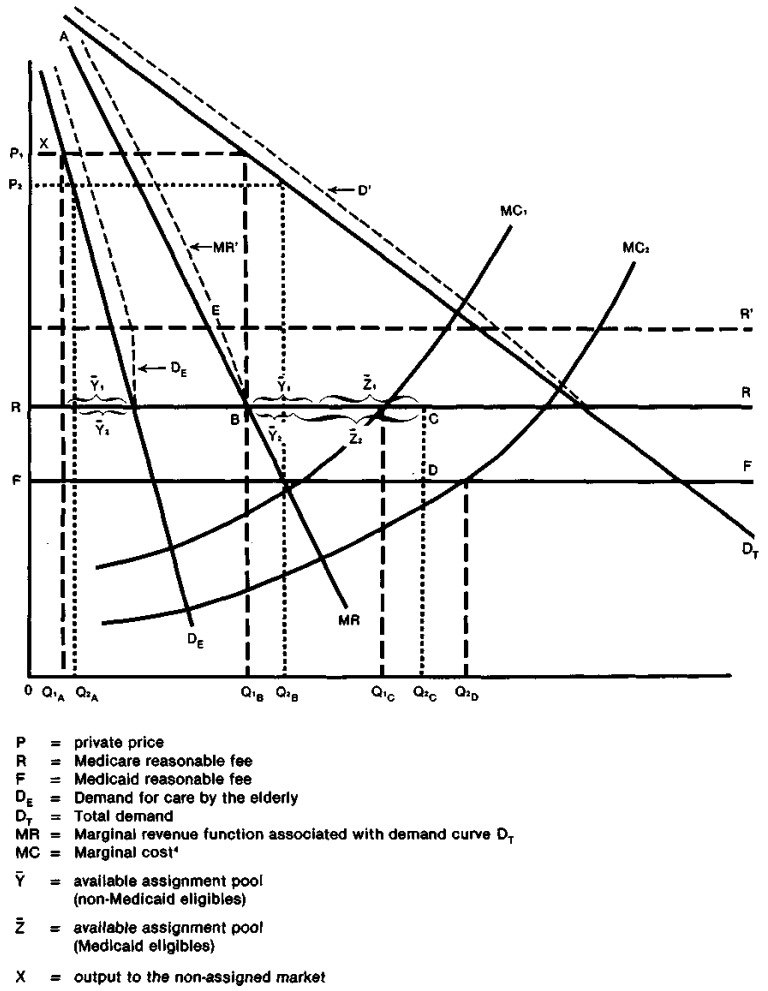
A graphic depiction of the problem is presented in Figure 1, in which the demand curves have been shifted to account for the coinsurance and deductibles. Due to the three separate markets, the physician's marginal revenue curve is kinked and discontinuous. The marginal revenue curve pertaining to the private market is labelled MR. When the marginal revenue curve intersects the Medicare reasonable fee at B, it becomes horizontal. This is because a physician will be able to satisfy all demand for Medicare assigned output at the exogenously determined reasonable fee R. Once a physician exhausts assigned demand at C, he/she will then drop down to the Medicaid market and supply output at the lower exogenous fee F. The marginal revenue curve follows ABCDF with a gap existing between C (the point at which Medicare assigned output is exhausted) and D.
Figure 1. Graphical Analysis of the Assignment Decision.
Given marginal cost curve MC1, to maximize profits the physician firm will produce total output of OQ1C. Of this amount, OQ1A will be provided to Medicare non-assigned patients and Q1AQ1B to private patients. For these two groups of patients the physician charges (and is reimbursed) price P1.3 At the Medicare reasonable fee R, an additional Y̅1 non-Medicaid eligible elderly are willing to purchase services. This is the available voluntary assignment pool. In addition, Z̅1 elderly Medicaid eligibles will also desire physician services at the zero price. It is useful to distinguish between the Medicaid eligible and non-eligible elderly population, since demand for care by joint Medicare/Medicaid beneficiaries is not responsive to changes in the reasonable fee (they face no out-of-pocket price), while demand by the voluntary assignment pool is a negative function of R. This has important implications for the responsiveness of total assigned demand to a change in the reasonable fee. All else constant, the larger the proportion of joint Medicare/Medicaid beneficiaries demanding assigned services, the less elastic the response of assigned demand to a change in reasonable fees. The physician will produce Q1BQ1C units of output for the Medicare assignment market. He or she will not, however, exhaust demand for Medicare assigned services, and therefore would not participate in Medicaid.5
Physicians with marginal cost schedule MC2will exhaust Medicare assigned demand and participate in the Medicaid market. Assuming, as in Figure 1, that all physicians face the same demand curve (differing only in their marginal cost schedules), those who participate in Medicaid should charge lower private prices and provide a greater amount of non-assigned output than the non-participants. A physician with marginal cost curve MC2 will provide OQ2A services to the Medicare non-assignment market. Q2AQ2B services will be provided to the private market. For these two groups of patients, the physician will charge price P2. This physician will provide Q2BQ2C services to the Medicare assignment market, exhausting demand for services among this group of patients. The physician will then drop down to the Medicaid market, providing Q2CQ2D output to this patient group and receiving the Medicaid fee F for these services.
A physician's net income can be written as follows:
y = (P)(PVT) + (P)(X) + (R)(Y) + (R)(Z) + (F)(MAID) − C(Q) where
P = private price
R = Medicare reasonable fee
F = Medicaid reasonable fee
PVT = quantity of services provided to the private market
X = quantity of services provided to Medicare non-assignment
Y = quantity of services provided to Medicare on voluntary assignment
Z = quantity of services provided to joint Medicare/Medicaid patients (mandatory assignment)
MAID = quantity of services provided to Medicaid non-elderly
Q = PVT + X + Y + Z+MAID
C(Q) = cost function
In this study we used two definitions of the assignment rate. The total assignment rate of physicians is defined as
and represents the percent of total Medicare RVS units which are taken on assignment. The voluntary assignment rate is defined as
and excludes mandatory assigned output from both the numerator and the denominator. Because it excludes services which must either be taken on assignment or not taken at all, the voluntary assignment rate provides an indication of a physician's willingness to assign claims over which he has the discretion to do so. Because both X and Y enter into the determination of the assignment rate, the response will depend on what happens to the quantity of both assigned and non-assigned output as the price variables change.
Let us first examine the impact of an increase in R.6 Because of coinsurance, an increase in reasonable fees will reduce the quantity of services demanded by patients currently on assignment. However, an increase in the reasonable charge will also decrease the out-of-pocket price of non-assigned patients by 80 percent of the change in the reasonable fee. This is equivalent to an outward shift in the demand curve facing the physician at prices above the reasonable fee. At the new, higher, reasonable fee and the old price, the quantity of non-assigned services demanded will increase (assuming all else is equal). The resulting impact on the assignment rate is not known and depends on the shape of the demand and supply curve of the physician. Because physicians who don't participate in Medicaid are able to increase supply to the assignment market, an increase in reasonable fees may increase the assignment rates of these physicians (as long as the supply elasticity is greater than demand elasticity). The assignment rates of physicians who do participate in Medicare are expected to decrease, since those physicians will redistribute output from the assigned to the non-assigned market.
The long run 7 impact of a change in reasonable fees on the assignment rate may differ from the short run impact. Among physicians who don't participate in Medicaid, an increase in reasonable fees will have two effects. First, it will directly increase the price at which the Medicare reasonable fee intersects the marginal revenue curve (raising it from B to E). Secondly, by reducing the out-of-pocket price faced by non-assigned patients, it will also shift the demand and marginal revenue curves facing the physician.8 Both of these effects will lead to an increase in private price. Medicaid participating physicians will only respond to the second effect since an increase in the Medicare reasonable will not directly affect the point at which the private marginal revenue curve intersects the Medicaid reasonable. Thus, we would expect a larger private price response to a change in the Medicare reasonable to occur among physicians not participating in Medicaid. Because physicians will eventually increase private price in response to an increase in Medicare reasonable fees, the long run effects of altering reasonable fees will be to move physicians to a higher price and a lower level of non-assigned output on the new demand curve. In the long run, non-assigned output may either increase or decrease in relation to the level before the change in the reasonable. The long run effect on the assignment rate will depend on the relative elasticities of demand and supply. The relationship between the Medicare reasonable fee and the assignment rate remains an empirical question.
Let us now investigate the impact of a change in P. First of all, let us assume that an increase in price is motivated by an outward shift in demand by the non-elderly. If the demand curve of the elderly remains stationary, an increase in price will decrease non-assigned output and will lead to a substitution of private output for output in the fixed fee markets. Physicians not participating in Medicaid would reduce their Medicare assigned output. Since both assigned and non-assigned output will decrease, the impact on the assignment rate is not known and depends on the elasticity of demand. Among physicians who participate in Medicaid, an increase in private price will shift the distribution of Medicare output toward more assigned output.
Description of Data Base and Empirical Specifications
Data Base
The data file used in this analysis consists of all claims paid by Medicare and Medicaid to a cohort of northern California physicians during the second quarter of each of the years 1972 through 1975. All of the physicians in the sample are solo practicioners who were eligible for reimbursement by California Blue Shield (the Medicare carrier) and who did not move during the study period. Information available from Blue Shield consists of the number and type of services provided to Medicare non-assigned, Medicare assigned, joint Medicare/Medicaid, and Medicaid patients. Information on the physician's date of graduation from medical school and country of medical education was also available. Additional information on the characteristics of the county in which the physician practices was available from public sources.
Since the major concern of this paper is to estimate the impact of private price and Medicare reasonable fees on the overall assignment rate, it was necessary to devise some method of aggregating physician prices and output. To deal with this problem we have defined Medicare output as the number of California Relative Value Scale (CRVS) units provided by the physician.9 Previous research has shown that for surgical procedures, the number of CRVS units is highly correlated with the amount of surgeon time required to perform the procedure (Hughes, 1972). In addition, the relative value scale has been in effect since 1969 and is well known among California physicians. Given the decision to use this definition of output, we then defined our price and reasonable variables as billed charge and reasonable fees per RVS unit.
The principal question of interest is the extent to which the assignment rate is sensitive to changes in the Medicare reasonable fee and in the price which the physician receives in the private market. Underlying this relationship between prices and output levels is a set of structural equations expressing the determinants of the supply of and demand for medical care. Demand for physician visits can be written as
D = f(NP, NPALT, Y, H, T)
NP = net price of the service (including time price)
NPALT = net price of alternatives
Y = family income
H = health status
T = vector of taste variables.
The supply of services by a physician is:
S = f(P, CL, Cc, W)
P = price per unit of service
CL = cost of labor inputs
Cc = cost of capital inputs
W = physician's implicit wage
In this type of structural model, both output and price are endogenous (determined within the model) variables.
The reasonable charge may be viewed as dependent upon previous values of the endogenous variables and therefore may be treated as exogenous (determined outside the model). Because of the simultaneous determination of price and output, the instrumental variable approach is an appropriate regression technique to use. The predicted price variable is then substituted for the observed billed charge in the second stage equation which estimates the determinants of the assignment rate.
Variable Definitions
Dependent Variable
The dependent variable in the analysis is the physician's Medicare assignment rate. As discussed previously, we will use two different definitions of the assigment rate, the voluntary assignment rate (which excludes joint Medicare/Medicaid claims) and the total assignment rate. One problem with using the voluntary assignment rate however, is that the available data do not permit one to distinguish voluntary assigned claims in 1974.10 Therefore, in estimating the voluntary assignment rate regressions we will only use data for 1972, 1973 and 1975. The total assignment rate regressions will use data from all four years.
Because we are using a regression framework for our empirical analysis, the estimated coefficient represents the change in the dependent variable with respect to a change in the independent variable, holding the value of all other independent variables constant. The coefficient on the reasonable fee therefore represents the short run effect on the assignment rate from an increase in R (i.e., P is held constant). As outlined in the previous section, an increase in the reasonable fee will have an ambiguous effect on the assignment rates of non-Medicaid participating physicians. The increase in reasonable fees is expected to reduce the assignment rates of physicians who participate in Medicaid. An increase in private price will also have an ambiguous effect on the assignment rates of non-Medicaid participating physicians, while increasing the assignment rates of physicians participating in Medicaid.
Cost Variables
The location of the physician's marginal cost curve will determine the markets in which he or she chooses to participate and the amount of output supplied to each market. Wages and salaries paid to office employees comprise one input to the firm's cost curve. Wage data are available by county and represent the cost of labor to the physician firm. The wage variable is defined by county and is a measure of the average salary of physicians' office employees. Firms with higher costs are less likely to participate in Medicare assignment and should have lower assignment rates.
Perhaps the most important factor which affects the marginal cost curve is the physician's implicit wage rate. Two variables are available as proxies for this wage: a dummy variable (FMG), which equals one if the physician graduated from a medical school outside of the United States, and the number of years since graduation from medical school (EXP). FMG status is expected to be negatively associated with the physician's implicit wage rate and therefore should increase his willingness to accept Medicare patients on assignment, consequently increasing the assignment rate. The experience variable is expected to be positively associated with the implicit wage and therefore would reduce both willingness to accept assignment and the assignment rate.
The relationship between the physician's specialty and the assignment rate is somewhat ambiguous. From 1972 through 1975, California Blue Shield did not reimburse physicians on a specialty specific basis. To the extent that internists and general surgeons have higher implicit wages one would expect that they would be less willing to take patients on assignment. However, general surgeons tend to provide more complex and expensive services than either general practitioners or internists. Previous research has shown that assignment rates are positively correlated with the price of the service being rendered (Health Insurance Benefits Council, 1973). If the probability of reimbursement under non-assignment varies with the size of the bill, it may be reasonable to take the higher priced procedures on assignment to avoid the risk of non-payment. This should increase general surgeons' incentives to accept assignment.
Other Variables
The number of physicians per aged population (DOCSA) is an indication of the availability of medical care in an area. As such, it may reflect the length of the mandatory assigned portion of the demand curve. The greater the number of physicians per population, the smaller the mandatory assigned demand facing each physician, and the lower will be the total assignment rate.
Two additional variables have been included in the regression equations to capture any additional variations not captured by the revenue or cost variables. The population (POP) in the county where the physician practices may be positively associated with the cost of providing services, due to rural-urban differences in costs which are not captured by other cost variables. In addition, year dummies11 are included in the analysis to capture any year to year effects not captured by the price variables. These might include the speed with which claims are processed between Medicare and Medicaid, shifts in eligibility requirements, or the effects of price controls.
Equation Specification and Estimation Method
To estimate the impact of private prices and Medicare reasonable fees on physicians' Medicare assignment rates, we posited a regression framework of the following form:
where Y represents the Medicare assignment rate, A is a constant term, P and R refer to the billed price and Medicare reasonable, the χi are the other independent variables, u is the error term, and α, γ, and the βi are the estimated regression coefficients.12 The coefficients on the price and reasonable fee variables are interpreted as elasticities.
Since private price and output are simultaneously determined, ordinary least squares is not an appropriate statistical tool. An instrumental variable approach was therefore used to obtain estimates of a predicted billed price.13 This predicted price was then input into the second stage regression which estimated the determinants of the assignment rate.
Empirical Results
Table 1 presents the means and standard deviations for the two samples of data. The predicted price per RVS unit is about 15 to 20 percent higher than the Medicare reasonable fee. Among physicians not participating in Medicaid, the average price (billed charge) per RVS unit was $.72, compared to a reasonable fee of $.61 per RVS unit. The average prices and reasonable fees for physicians participating in Medicaid were $.68 and $.59 respectively.
Table 1. Means and Standard Deviations of the Independent Variables.
| Voluntary Assignment Rate | Total Assignment Rate | |||
|---|---|---|---|---|
|
|
|
|||
| Mean | Standard Deviation | Mean | Standard Deviation | |
| PRICE | .693 | .112 | .694 | .109 |
| REASONABLE | .595 | .082 | .593 | .081 |
| SURGEON | .266 | — | .269 | — |
| INTERNIST | .287 | — | .286 | — |
| FMG | .086 | — | .088 | — |
| EXP | 25.159 | 9.821 | 25.277 | 9.809 |
| DOSCA | 13.605 | 5.510 | 13.591 | 5.520 |
| POP | 485.906 | 302.396 | 489.482 | 304.889 |
| WAGE | 2.464 | .749 | 2.548 | .697 |
| Y73 | .312 | — | .232 | — |
| Y74 | — | — | .255 | — |
| Y75 | .344 | — | .257 | — |
| N=3127 | N=4199 | |||
| Medicaid Non-Participants | ||||
| PRICE | .718 | .087 | .718 | .109 |
| REASONABLE | .608 | .115 | .605 | .087 |
| N=963 | N = 1312 | |||
| Medicaid Participants | ||||
| PRICE | .683 | .110 | .683 | .107 |
| REASONABLE | .589 | .079 | .588 | .078 |
| N=2164 | N = 2887 | |||
Voluntary Assignment Rates Segmented by Medicaid Participation/Non-Participation
The dependent variable for the first set of regressions is the voluntary assignment rate. The results are presented in Table 2. The first column presents the coefficients and t-statistics for those physicians who were not Medicaid participants. The second column reports the results for Medicaid participants.
Table 2. Voluntary Assignment Rate Supply Function.
| Dependent Variable = LN (Voluntary Assignment Rate) (t-statistics in parentheses) | ||
|---|---|---|
|
| ||
| Medicaid Non-Participants | Medicaid Participants | |
| LN(BILLED) | − 5.959 17 (3.64) | − 2.796 17 (2.97) |
| LN(REASONABLE) | 5.101 17 (3.38) | 1.654 16 (1.74) |
| SURGEON 15 | .691 17 (3.91) | .402 17 (3.29) |
| INTERNIST 15 | −.128 (.70) | −.001 (0.00) |
| WAGE | −.029 (.16) | .116 (1.40) |
| FMG | −.019 (.07) | .298 16 (1.80) |
| EXP | −.015 16 (1.89) | −.019 17 (3.46) |
| POP (000,000) | −.379 (1.38) | .699 17 (3.83) |
| DOCSAGED | −.016 (1.08) | − .036 17 (3.61) |
| YEAR 73 | .649 16 (3.41) | .134 (1.12) |
| YEAR 75 | 1.435 16 (3.93) | .764 17 (4.10) |
| CONSTANT | −2.331 | − 2.381 |
| R̅2 | .05 | .03 |
| Standard error | 2.24 | 2.17 |
| N
|
963 | 2164 |
General Practitioners represent the omitted specialty.
Significant at the .10 level
Significant at the .05 level
As predicted by the model, the voluntary assignment rate of physicians not participating in Medicaid is sensitive to changes in private prices and Medicare reasonable fees. An increase in reasonable fees of one percent results in a five percent increase in the voluntary assignment rate for Medicaid non-participants. This implies that the increased quantity of assigned output provided more than offsets the increase in non-assigned output, resulting in an increase in the assignment rate. (An increase in R reduces the out-of-pocket price for Medicare patients not on assignment, thereby increasing the quantity demanded. It also increases physician willingness to supply output to the assignment market. The net effect of these two phenomena is an increase in the assignment rate.)
The positive coefficient on the Medicare reasonable fee for Medicaid participants is contrary to the model. Without knowing something about the response of total assigned and non-assigned output, it is not possible to determine whether the increase in the assignment rates is due to an ability to increase assigned output or to a shift in output from non-assignment to assignment. If there are significant problems in collecting payment from non-assigned patients, an increase in the reasonable fee would raise the expected payment for assigned claims relative to non-assigned claims and may cause physicians to shift to more assigned output. Alternatively, if physicians are able to induce demand, or if they have not exhausted assigned demand,14 an increase in reasonable fees could result in an increase in their assignment rate.
The physician's private price is negatively related to his/her assignment rate. A one percent increase in private price is associated with a six percent decrease in the assignment rate of physicians not participating in Medicaid and a 2.8 percent decrease in the rate of Medicaid participants. The reduction in assigned output more than offsets any decrease in non-assigned output, resulting in a decrease in the assignment rate.
In all of the analysis presented it must be remembered that the coefficient on the reasonable fee represents the effect of the reasonable fee on the assignment rate, assuming that price remains constant. As our theoretical model indicated, increases in reasonable fees will motivate increases in the private price of services. Since the coefficient on private price is negative, the long run effect of raising reasonable fees will be partially offset by the price increase. The extent of the offset will depend on the relative size of the private price and reasonable charge coefficients and the elasticity of price with respect to changes in reasonable fees. In the simulations, we will predict assignment rate responses to policy changes, using differing assumptions of the elasticity of price to reasonable fees.
Our results also show that surgeons have somewhat higher assignment rates than general practitioners. In part, this could result from differences in the type of procedures performed by surgeons. Because surgeons are most likely to provide services with high RVS values and high prices, they risk greater loss of revenue if the patient defaults than do physicians in other specialties. To minimize expected losses they may choose higher assignment rates.
Because we did not have accurate estimates of actual practice costs, we used a number of variables as proxies for the input price vector. The wage (WAGE) of personnel in physicians' offices proved not to be a significant determinant of the assignment rate. Similarly, graduation from a foreign medical school (FMG) did not affect the voluntary assignment rate. The physician's level of experience however, was significantly related to the assignment rate among those participating in Medicaid. We hypothesized that the estimated coefficient would have a negative sign, reflecting the higher implicit wage of experienced physicians. Our results confirm this hypothesis. The population of the county in which the physician practices (POP) was found to have a negative sign in the regression for Medicaid participants and was not significant among the non-participants. Inability to accurately capture the practice costs by these variables may be partly responsible for the lack of significance on some of the coefficients. In addition, the theoretical implication that physicians who participate in either of the fixed fee markets will set marginal cost equal to the fixed fee suggests that Medicaid participation status may account for a large part of the difference in marginal cost among physicians. The coefficients on the other proxy variables may therefore not be significant.18
The number of physicians per aged population has a negative impact on the voluntary assignment rate. There are two possible reasons for this. A charity motive could cause physicians living in underserved areas to treat more patients than profit maximization would dictate. Since these patients are less likely to be able to afford the price of services than the more affluent patients, a higher assignment rate would result. Also, areas with relatively high physician to population ratios are more affluent, and the lower assignment rate may represent a demand phenomenon.
Total Assignment Rates Segmenting by Medicaid Participation/Non-Participation
The second series of regressions which we estimated used the total Medicare assignment rate as the dependent variable. Table 3 presents the results of this analysis segmenting the sample by Medicaid participation.
Table 3. Total Assignment Rate Supply Function.
| Dependent Variable = LN (Total Assignment Rate) (t-statistics in parentheses) | ||
|---|---|---|
|
| ||
| Medicaid Non-Participants | Medicaid Participants | |
|
|
|
|
| LN(BILLED) | −2.03621 (3.43) | −.58321 (2.51) |
| LN(REASONABLE) | 1.35221 (2.47) | .087 (.36) |
| SURGEON19 | −.14121 (2.14) | −.23121 (6.94) |
| INTERNIST19 | −.41121 (5.98) | −.27121 (8.44) |
| WAGE | .060 (.83) | .04921 (2.00) |
| FMG | .17520 (1.75) | .22921 (5.11) |
| EXP | −.00821 (2.82) | −.00421 (2.71) |
| POP (000,000) | −.074 (.70) | .11321 (2.28) |
| DOCSAGED | −.02521 (4.36) | −.02021 (7.27) |
| YEAR 73 | .122 (1.49) | −.034 (.90) |
| YEAR 74 | .097 (.09) | −.024 (.57) |
| YEAR 75 | .24120 (1.68) | .01020 (1.92) |
| CONSTANT | −.826 | −.624 |
| R̅2 | .07 | .08 |
| Standard error | .98 | .69 |
| N | 1312 | 2887 |
General practitioners represent the omitted specialty
Significant at the .10 level
Significant at the .05 level
The assignment rate of non-Medicaid participants is significantly affected by billed prices and Medicare reasonable fees. A 1 percent increase in billed charge results in a 2 percent decrease in the assignment rate. The elasticity of the assignment rate with respect to the reasonable fee is 1.4. In general, the elasticity for the total assignment rate is considerably smaller than it was for the voluntary assignment rate. In part, this results from the fact that total assignment rates are greater than the voluntary assignment rates, so an absolute change is being applied to a much larger base. Among Medicaid participants, increases in reasonable fees are not related to increases in the assignment rate. Increases in billed charges have a significant negative impact on assignment rates, but the size of the coefficient is much smaller than it is for non-participants.
One notable difference between the results of the voluntary and total assignment rate regressions is in the coefficients on the specialty dummies. Surgeons and internists have significantly lower total assignment rates than general practitioners. This would result if specialists were less willing to treat joint Medicare/Medicaid patients than general practitioners. Available evidence for 1975 indicates that mandatory assignment rates are also substantially lower among internists and surgeons than among general practitioners. The proportion of assigned cases that are voluntarily assigned is higher among specialists than it is among general practitioners. Part of this may be the result of locational differences between the specialties, with general practitioners locating in lower income areas.
Generally, the remaining coefficients were similar in terms of significance to those found in the voluntary assignment regressions. Experience is negatively associated with the assignment rate. The salaries of employees in physicians' offices are not significantly related to the assignment rate, and FMG status is significant only among Medicaid participants. The number of physicians per aged population is negatively associated with the assignment rate, as it was in the voluntary assignment rate regressions.
Assignment Rate Simulations
The empirical results of the previous section provided estimates of the responsiveness of Medicare assignment rates to changes in reasonable fees and billed charges. The results indicate that the assignment rate is sensitive to changes in the revenue variables. This section of the paper will simulate the effect on the Medicare assignment rate of increasing reasonable charges for all physicians to the level of Medicare prevailing charges. This policy alternative will be evaluated in terms of its impact on both the voluntary and total assignment rate for Medicare services. We will base our simulations on the estimated coefficients of the assignment rate equations.
Because this policy strategy entails increasing the Medicare reasonable fee, it will be necessary to make some assumptions regarding the relationship between private prices and Medicare reasonable charges. The results of our predicted price equations and our model support the hypothesis of a positive relation between price and reasonable fees. However, our predicted price equations cannot indicate the magnitude of this relationship. It is reasonable to expect that the longer the time period, the greater the price response. In addition, our theoretical model predicted that the price response to a change in reasonable fees will be greater among physicians who do not participate in Medicaid than among those who do because of the effect which a change in reasonable fees has on the intersection of the physician's marginal revenue curve with the fee received in the fixed fee market. We have therefore simulated the assignment response under four alternative assumptions:
An increase in reasonable fees will have no effect on private prices.
A 1 percent increase in the reasonable fee will result in a .25 percent increase in billed charges.
A 1 percent increase in the reasonable fee will result in a .50 percent increase in private price.
A 1 percent increase in the reasonable fee will result in a .75 percent increase in private price.
Calculating the resulting assignment rate under each of the four assumptions will provide an indication of the sensitivity of results to the relationship between private prices and Medicare reasonable fees.
We will perform separate simulations for each of the three specialties in our sample. Specialty-specific simulations are of interest, since Medicare assignment rates and output levels differ dramatically by specialty. Table 4 indicates the percentage increase in reasonable fees which would occur if reasonable charges were increased to the level of prevailing ones.
Table 4. Percent Increase in Reasonable Fees for Policy Option (1975 data).
| Raise Reasonable Fees to Level of Prevailing Fees (in percents) |
|
|---|---|
|
|
|
| General Practitioners | |
| Medicaid non-participants | 16.1 |
| Medicaid participants | 19.1 |
| General Surgeons | |
| Medicaid non-participants | 12.3 |
| Medicaid participants | 10.6 |
| Internists | |
| Medicaid non-participants | 12.6 |
| Medicaid participants | 14.6 |
In calculating the changes in assignment rate which would occur in such a situation, we estimated the equivalent percent increase in reasonable fees for each physician. Using our estimated regression coefficients, we simulated the new assignment rate for each physician. The aggregate assignment rate is a weighted average of the assignment rates of each physician, where the weight is the physician's total Medicare output for 1975.
Table 5 presents the simulated assignment rates of general practitioners, general surgeons, and internists for each assumption regarding the relationship of prices and reasonable fees. The simulations indicate that the assignment rates will increase the most if we assume that prices will not respond to an increase in the reasonable charge. Assuming the elasticity of price with respect to reasonable fee of .5 among all physicians, we find that increasing reasonable fees to the level of prevailing ones will increase the voluntary assignment rates of general practitioners not participating in Medicaid from 18.1 to 24.9 percent. It will increase their total assignment rate from 33.4 to 35.4 percent. The voluntary assignment rates of general practitioners participating in Medicaid will increase from 42.4 to 44.6 percent. Due to the larger coefficient on price, and assuming a .5 elasticity, an increase in reasonable fees will actually decrease the total assignment rates of general practitioners who do participate in Medicaid.
Table 5. Simulations of Medicare Assignment Rates.
| Raise Reasonable Fees to Level of Prevailing Fees | Voluntary Assignment Rate | Total Assignment Rate | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Medicaid non-participants | Medicaid Participants | Total | Medicaid non-participants | Medicaid Participants | Total | |
| General Practitioners | ||||||
| Case 1 (no price response) | 34.4 | 56.5 | 53.2 | 41.5 | 64.5 | 61.1 |
| Case 2 (.25 elasticity) | 29.7 | 50.6 | 43.0 | 38.5 | 62.7 | 59.1 |
| Case 3 (.50 elasticity) | 24.9 | 44.6 | 41.6 | 35.4 | 61.0 | 57.2 |
| Case 4 (.75 elasticity) | 20.1 | 38.6 | 32.8 | 32.5 | 59.2 | 55.2 |
| Actual 1975 Assignment Rate | 18.1 | 42.4 | 38.8 | 33.4 | 63.7 | 59.2 |
| General Surgeons | ||||||
| Case 1 | 47.6 | 53.7 | 51.9 | 43.9 | 56.6 | 53.8 |
| Case 2 | 40.9 | 49.1 | 46.6 | 40.7 | 55.4 | 51.0 |
| Case 3 | 34.2 | 44.6 | 41.5 | 37.3 | 54.2 | 49.1 |
| Case 4 | 27.5 | 40.1 | 36.3 | 34.1 | 53.0 | 47.3 |
| Actual 1975 Assignment Rate | 24.7 | 42.9 | 37.4 | 35.2 | 55.9 | 49.7 |
| Internists | ||||||
| Case 1 | 27.3 | 38.4 | 35.2 | 31.0 | 47.0 | 42.4 |
| Case 2 | 23.9 | 34.5 | 31.4 | 29.1 | 45.8 | 41.0 |
| Case 3 | 20.5 | 30.7 | 27.7 | 27.2 | 44.6 | 39.6 |
| Case 4 | 17.1 | 26.9 | 24.1 | 25.3 | 43.5 | 38.2 |
| Actual 1975 Assignment Rate | 15.7 | 29.3 | 25.4 | 25.8 | 46.1 | 40.2 |
Again assuming a .5 elascticity of price with respect to reasonable fees, we find that increasing them to the level of prevailing fees will increase the voluntary assignment rates of general surgeons not participating in Medicaid from 24.7 to 34.2 percent. Their total assignment rates would increase 6 percent (from 35.2 to 37.3 percent). General surgeons participating in Medicaid would increase their assignment rates from 42.9 to 44.6 percent. Aggregating both the Medicaid participants and non-participants, we find that the voluntary assignment rate would increase slightly. The total assignment rate would decrease slightly under such a policy. Since the estimated coefficients in the regression model were the same for each specialty, the differences in the simulated assignment rates reflect the different specialty-specific assignment rates prior to the policy change as well as specialty differences in the percent increase in reasonable fees from each policy alternative.
Among internists, the voluntary assignment rates of physicians not participating in Medicaid will increase from 15.7 to 20.5 percent (assuming an elasticity of .5) if reasonable fees were raised to the level of prevailing ones. The total assignment rate would increase much more moderately, from 25.8 to 27.2 percent. As with the other specialties, the majority of internists participate in Medicaid. Thus, the aggregate assignment rate response will be much smaller than the response for physicians who don't participate.
For all of the simulations, we are assuming that the price response to a change in reasonable fees is the same for both Medicaid participants and non-participants. As our theoretical model pointed out however, those not participating in Medicaid are expected to exhibit a larger price response to a change in reasonable fees than are participants. In reality therefore, we might exhibit a price elasticity response of .75 for non-Medicaid participants and one of .25 for the Medicaid participants. The .50 elasticity may thus represent an understatement of the assignment rate response of Medicaid participants and an overstatement of the response of non-participants.
The effect of this differential response by physicians is unclear. Medicaid-participating physicians account for a larger share of the Medicare market, not only in terms of numbers but also in terms of Medicare output per physician. Their assignment rates are less responsive to a change in reasonable fees than are the assignment rates of physicians not participating in Medicaid. Thus one would initially expect a relatively small increase in assignment rates from all physicians, when a large proportion of them participate in Medicaid and when they account for a large proportion of total output. However, private price response to a given change in reasonable fees should be lower among physicians participating in Medicaid than among those not participating. The effect on reducing non-assigned demand (and hence part of the denominator of the assignment rate) from a given increase in reasonable fees should therefore be greater among physicians who do not participate in Medicaid than among those who do. (Non-assigned demand will decline more as the elasticity of price with respect to a change in reasonable fees increases). Given these results, it is not possible to determine which group of physicians will experience a larger increase in price from a given change in reasonable fees.
Summary and Conclusions
This paper has investigated the effect of private prices and Medicare reasonable fees on both the voluntary and total Medicare assignment rates of physicians. Because Medicare assignment rates are an important indicator of the out-of-pocket cost burden for medical services on the elderly, increases in assignment rates are desirable, since they reduce this burden.
Using a simple theoretical model which viewed the physician firm as a monopolistic competitor, we were able to predict the assignment rate responses of certain groups of physicians to changes in private prices and Medicare reasonable fees. The theoretical model was useful in pointing out that physicians participating in both Medicaid and Medicare should exhibit different responses to changes in the price variables than physicians who participate only in the Medicare market. In brief, the assignment rates of Medicaid participating physicians were not expected to respond positively to increases in reasonable fees.
A second important implication of the model was that increases in reasonable fees would induce physicians to increase the private price of their services. The magnitude of this response depends on the elasticity of the demand curve facing the physician. Because of the relationship between price and reasonable charges, any effort to close the gap between the two revenue variables by raising reasonable charges will be met by further increases in price.
Finally, the model pointed out that a change in reasonable fees will affect demand for services as well as supply. Assuming price is constant, increasing reasonable fees will reduce quantity demanded among assigned patients and increase the quantity of physicians services demanded by non-assigned patients. The assignment rate is dependent on the relative sizes of assigned and non-assigned output. Thus, assignment rates may rise or fall in response to an increase in reasonable fees, depending on what happens to both assigned and non-assigned output. The uncertain response of price to the increase in reasonable fees further complicates the issue.
Our empirical model estimated the elasticity of the assignment rate to private prices and reasonable fees. We estimated assignment rate regressions using as a dependent variable the physicians' Medicare assignment rate defined in terms of RVS units. Our results indicate that the RVS assignment rates of physicians not participating in Medicaid are positively related to the Medicare reasonable fee. A 1 percent increase in reasonable fees will induce a 5.1 percent increase in the voluntary assignment rates of these physicians and a 1.4 percent increase in their total assignment rate. A similar increase in billed charge will reduce the voluntary assignment rate by 6.0 percent and the total assignment rate by 2.0 percent. Assignment rates of physicians participating in Medicaid exhibit a much smaller response to changes in the revenue variables, although the response is in the same direction. A 1 percent increase in reasonable fees will increase the voluntary assignment rate by 1.7 percent but will not significantly affect the total assignment rate of these physicians. An equivalent increase in billed charge will reduce the voluntary assignment rate by 2.8 percent and the total assignment rate by .6 percent.
Using the regression results from our RVS assignment rate equations, and assuming a number of different relationships between prices and reasonable fees, we predicted specialty-specific assignment rates under a policy option which would raise reasonable fees to the level of prevailing ones. Given the simulation results, it appears that physicians would not increase their assignment rates substantially if reasonable fees increase between 11 and 20 percent. In addition, such an increase would increase Medicare program costs significantly. It would also increase the out-of-pocket cost to Medicare voluntary-assigned beneficiaries because of the coinsurance rate. This should lead to a decline in the amount of services demanded at the reasonable fee. An increase in the reasonable charge will initially lower the out-of-pocket costs of non-assigned beneficiaries. However, this reduction in out-of-pocket costs will be limited because of the relationship between prices and reasonable fees.
Although the simulation results do not predict a substantial increase in the assignment rate from raising reasonable fees to the level of prevailing ones, improvements in medical care access among the elderly may still occur. Increasing the Medicare reasonable fee should increase physician willingness to participate in the Medicare program and may therefore increase Medicare output. Because an increase in reasonable fees will also reduce the price of non-assigned services, both assigned and non-assigned output may increase. The result could be little or no change in the assignment rate, although access might be improved considerably.
Also, since the time period covered by this study, there has been a significant change in the determination of reasonable fees. The economic index went into effect in 1976 and acts to constrain the rate of increase in Medicare prevailing fees. (Thus the difference between reasonable fees and the effective prevailing fee is smaller than it is in this study). Assuming physicians increase their private fees at a rate greater than that permitted by the index, the result will be a movement toward the use of a fee schedule in the Medicare market. The index will also modify the relationship between a physician's private price and his/her reasonable fee, so that current increases in private prices will have a smaller impact on the future value of a physician's Medicare reasonable fee than was the case under the CPR system. The long run impact of a Medicare fee schedule on the availability of Medicare services will depend on the Medicare fee level relative to the physician's private market price. In areas where the gap between the fee schedule and private price widens considerably, we may see a decline in the willingness of physicians to provide Medicare services on assignment.
The simulations in this paper have been performed assuming that any policy changes which increase Medicare reasonable fees would be applied to all Medicare claims. Another alternative is to apply a bonus to claims taken on assignment only. In terms of the model, such a policy would eliminate the increase in non-assigned demand resulting from an increase in reasonable fee. This effect would, in turn, reduce the price response to a reasonable fee change among physicians not participating in Medicaid, and should eliminate any response among Medicaid participants. The result would be a larger increase in assignment rates at a lower total cost to the program than that which would occur when reasonable fees are raised for all Medicare services.
In this paper, we have focused exclusively on the Medicare assignment rate and how changing reasonable fees would affect it. While we currently do not know the private price impact of increasing reasonable fees, or the behavior of physicians under some of these alternative policy measures, this study has furthered our understanding of the nature and complexity of the problem. By understanding the impact that a variety of different factors have on altering the distribution between assigned and non-assigned output, we gain additional insight into the response of physicians to alternative reimbursement strategies and the effect that changes in policy will have on the medical care cost burden of the elderly.
Acknowledgments
The author wishes to thank her colleagues Jack Hadley, John Holahan, Robert Lee, and William Scanlon for their helpful comments and suggestions. She also thanks Jon Gabel, Peter McMenamin, and Ira Burney of HCFA for comments on a previous draft. Patty Tigue contributed excellent research assistance.
Footnotes
The assignment rate simulations and the empirical work on the RVS assignment rate equations were supported by Contract No. 600-76-0054. Extensions of the theoretical model to consideration of the assignment rate, some of the procedure specific empirical work, and additional related research not presented in this paper were supported by Grant No. 18-P-9700813-01. Both the contract and grant are from the Health Care Financing Administration, USDHEW.
While the customary, prevailing, and reasonable charge (CPR) methodology was in force at the time of our study, the imposition of fee controls during the Economic Stabilization Program (ESP) caused the determination of reasonable charges to diverge from the stated methodology. The price controls under the ESP permitted reasonable charges to increase by only a fraction of what their increase would have been using the CPR methodology. Because the controls on Medicare fees were stricter than those placed on private prices, the divergence between Medicare reasonables and private prices increased during the control years. The controls were lifted in 1974. However, since reasonable charges for 1974 and 1975 were based on actual charge data from 1972 and 1973, the increase in reasonable charges in the two years after controls was limited. In addition, since 1976 the rate of increase in prevailing charges has been constrained by the imposition of an economic index. This index permits prevailing fees to increase at some weighted average of 2 components; 1) the increase in the general earnings level of workers and 2) increases in the expenses of the kind incurred by physicians in office practice.
In the analysis presented here we assume that the physician faces no additional costs from treating non-assigned patients, and that the probability of payment does not vary for assigned and non-assigned claims. However, since physicians must collect the full price of their services from non-assigned patients but are assured 80 percent payment for services provided on assignment, they may take payment probabilities into account in their assignment decision. While no empirical evidence on payment default is available, it seems reasonable to assume that such default is a function of patient characteristics (income, supplemental health insurance) and size of bill. If this is the case, then we might observe higher assignment rates on expensive services and a higher propensity to assign services to low income, poorly insured patients. Thus, physicians would not provide non-assigned services to all who demand them but only to those where the expected payments are larger than 80 percent of the Medicare reasonable fee. The rest of the output would be provided on assignment.
Our analysis assumes that physicians charge only one price to private and Medicare non-assigned patients. Empirical evidence supporting this assumption can be found in Bluck and Lee, 1977; and Sloan, Cromwell, and Mitchell, 1977.
The marginal cost schedules are arbitrarily drawn to reflect the market participation of two different physicians. Likewise, the value of Z is arbitrarily selected for graphical purposes.
In practice, non-participation in Medicaid may not be equivalent to zero Medicaid output. Due to emergencies or a charity motive, physicians who do not participate in Medicaid may still provide some Medicaid services. In our empirical work we have arbitrarily chosen 500 RVS units of output provided to Medicaid as the cut-off value between participants and non-participants.
This analysis assumes that the physician's marginal cost curve remains stationary and that the physician's implicit wage is exogenous. However, it is possible that a physician's implicit wage might rise with increases in prices and reasonable fees. If this occurs, the long run effect of a change in R on the assigned output of non-Medicaid participating physicians is indeterminate. Similarly, this model has not dealt explicitly with the labor/leisure choice of physicians. Using a utility maximizing framework, it would be possible to predict a decline in output as prices rise if the physician is on the backward bending portion of his labor supply curve.
Long run and short run impacts are distinguished by whether private price has responded to the new reasonable fee. In the short run we assume such adjustment has not yet occurred.
The change in out-of-pocket price represents a movement along the consumers' demand curve, since that curve is defined in terms of the out-of-pocket price. This same phenomenon is represented by an outward shift in the demand curve facing the physician, since at the same price P he/she can provide more services.
CRVS assigns a unit value to a medical procedure. Unit value is determined by the price and complexity of the procedure.
An additional problem in using the voluntary assignment rate in our empirical work is that the variable is measured with error, because the data did not directly identify which assigned claims were voluntarily assigned. Rather, the number of voluntary assigned claims was computed as the difference between total assigned claims and mandatory assigned claims. Mandatory assigned (Joint Medicare/Medicaid) claims must first pass through Medicare for payment before being submitted to Medicaid. Due to the time lag between payment from the two programs, it is possible that the number of mandatory assigned claims recorded by Medicare in a time period would differ from those recorded by Medicaid. Since the data from Blue Shield are based on date of claim payment rather than date of service, and since our information on mandatory assigned claims was provided by Medicaid while the total of assigned and non-assigned claims was provided by Medicare, it is possible that the number of voluntary assigned claims is measured with error. The direction of measurement error is not known, but will depend on the flow of claims through Medicare to Medicaid and the time lag between payment from the two programs.
Year dummies are variables which assume the value of 0 or 1, depending on the year. The omitted year in the regression is 1972.
Initially we posited a linear relationship between the assignment rate and prices and reasonable fees. However, inspection of the error term indicated that a multiplicative specification was superior in providing a random distribution of the error term across all values of the predicted dependent variable.
Regressions for the predicted price equations can be found in Lynn Paringer, “The Medicare Assignment Rates of Physicians: Their Responses to Changes in Reimbursement Policy.” Urban Institute Working Paper 1250-1, March 1979.
If physicians have not exhausted assigned demand, the level of Medicaid output at which we segmented our sample is not sufficiently high to select out those physicians who cannot increase output to Medicare as the reasonable fee rises.
This is because participation in one or both markets largely reflects the position of the physician's marginal cost curve, and additional variables will not greatly enhance the ability to trace out the MC curve. If we could perfectly separate out those physicians who are unable to increase Medicare output in response to an increase in reasonable fees (i.e., Medicaid participants), then we should exclude the proxy marginal cost variables from the assignment rate equations of these physicians, since the assignment rate should respond to demand conditions only.
References
- Hadley Jack, Lee Robert. Urban Institute Working Paper 998-8. The Urban Institute; Washington, D.C.: Apr, 1978. Physicians Price and Output Decisions: Theory and Evidence. [Google Scholar]
- Health Insurance Benefits Advisory Council. A Report on the Results of the Study of Methods of Reimbursement for Physicians' Services Under Medicare. HIBAC. 1973 Jul;II Appendix A. [Google Scholar]
- Hughes Edward. Surgical Workloads in a Community Practice. Surgery. 1972;7:315–72. [PubMed] [Google Scholar]
- Sloan Frank, Mitchell Janet, Cromwell Jerry. Physician Participation in State Medicaid Programs. Journal of Human Resources. 1978;(XIII):211–245. [PubMed] [Google Scholar]
- Sloan Frank, Steinwald Bruce. Physician Participation in Health Insurance Plans: Evidence on Blue Shield. Journal of Human Resources. 1978 Spring;XIII(No. 2):237–263. [PubMed] [Google Scholar]