Abstract
The companion paper on nursing home levels of care (Bishop, Plough and Willemain, 1980) recommended a “split-rate” approach to nursing home reimbursement that would distinguish between fixed and variable costs. This paper examines three alternative treatments of the variable cost component of the rate: a two-level system similar to the distinction between skilled and intermediate care facilities, an individualized (“patient-centered”) system, and a system that assigns a single facility-specific rate that depends on the facility's case-mix (“case-mix reimbursement”). The aim is to better understand the theoretical strengths and weaknesses of these three approaches.
The comparison of reimbursement alternatives is framed in terms of minimizing reimbursement error, meaning overpayment and underpayment. We develop a conceptual model of reimbursement error that stresses that the features of the reimbursement scheme are only some of the factors contributing to over- and underpayment. The conceptual model is translated into a computer program for quantitative comparison of the alternatives.
The Concept of Reimbursement Error and Its Origins
Those who pay for long-term care services have a natural interest in paying the “right” amount for the services received by each resident. Paying too little creates hardship for residents or providers or both, while paying too much creates a hardship for the public at large. The concept of a “proper” rate is a powerful organizer for thinking about financing social services generally and certainly underlies many proposals for reform of payment for long-term care. Witness the statement of Walsh and Koetting (1978) regarding the motivation for the individualized reimbursement system implemented in Illinois:
“The alternative to an open-ended reimbursement policy is development of group rates or ceilings which, at least implicity, will define what level of care the payor expects. In developing such ceilings it is imperative that the level of care to be reimbursed is appropriate. Too high a level of reimbursement would generate excess profits, induce undesirable entries to the industry, and possibly provide an incentive to provide an excessive length of stay. Too low a level of reimbursement would provide a disincentive to adequate care, and may ultimately reduce entry and create a shortage of capacity.”
Perhaps the most difficult aspect of any attempt to set reimbursement rates or ceilings which are adequate, but not excessive, concerns the differentiation of payment by level of need of the patient being cared for. While most would agree that the overall level of reimbursement must be appropriate to prevent either excess or insufficient entry, it should be recognized that inadequate differentiation among patients will lead to the same undesirable consequences for sub-groups of patients. For example, a flat rate for all ICF patients would probably create a rush for patients who require little care, while placing more difficult to care for patients in a position of being unable to obtain adequate care.
Consider also the statement of Fulton (1976):
“(The Senate Committee on Finance) was concerned about the effect of both underpayment and overpayment on the quality of medical care of recipients. If facilities are underpaid … facilities will be under pressure to cut corners and provide lower quality care, or will be forced to make their non-Medicaid patients absorb some of the cost of Medicaid patients' care; at worst, facilities may refuse to accept Medicaid patients. If facilities are overpaid … there is little incentive for providers to employ the most efficient and economical methods of providing services, with the result that the State's Medicaid dollars do not go as far as they could to provide needed medical care.”
The urge to perfect reimbursement by linking payment tightly to resident need is powerful. However, in the companion paper we documented the problems of assessing resident condition, developing a consensus of professionals on the bundle of services recommended for the resident, and then eliciting a societal commitment to authorize those services. There is simply no “clean” way to proceed through those steps to determine the cost of an optimal service bundle and use that cost as the basis for reimbursement. Nevertheless, in this paper we will refer to a “proper”per diem rate, which we take to be equal to the (hypothetical) cost of an optimal service bundle. We will assume for purposes of analysis that it is conceptually possible to determine the cost of an optimal service bundle for each resident. Making this assumption will allow us to isolate the extent to which a system of classification involving levels of care can itself contribute to problems in reimbursement for services. We will not, however, assume that the proper rate is obvious in practice; in fact, one of the key elements of our analysis will be the extent to which the proper rate is only dimly perceived because of the difficulties of assessment and service planning.
Paying more or less than the underlying proper rate constitutes error in reimbursement. Levels of care constitute only one of several sources of error. Others are the inability to discern the proper rate, fluctuation in resident status over time, and differences among the residents within a nursing home (if all were alike, the problem of customizing reimbursement would disappear). Our focus will be linking levels of care to payment error in ways that account for the simultaneous influence of other sources of error. This comprehensive perspective will allow us both to better assess the gains achievable by reforming level of care policies and to identify situations in which one type of reform is preferable to another. While we do not believe that “need” is a unidimensional attribute, this analysis will allow us to examine the patient-centered approach within the conceptual framework of reimbursement error usually used to justify it.
Alternative Reimbursement Schemes
We will consider three alternative reimbursement schemes:
Two resident classes, each reimbursed at its own fixed rate and each containing half the resident population;
A system in which rates are computed individually for each resident (“patient-centered reimbursement”); and
A system in which the care of every resident in a nursing home is paid for at the same rate; this rate is equal to the average of the patient-centered rates for a sample of patients in that home (“case-mix reimbursement”).
The first alternative corresponds to the present system in that it uses two levels. The second alternative is included to assess the impact of the ultimate refinement in which there are no groupings of residents into classes; each is treated individually. The third alternative is included to assess the impact of a cheaper and “weaker” use of individual resident assessments. Depending on the way these alternatives are implemented and the environment in which they are implemented, any one of them can be the most preferred.
Simulation of Alternatives
The technique of Monte Carlo simulation (Hillier and Lieberman, 1967) will be used to produce numerical comparisons. This methodology is commonly used when the complexity of a problem is such that other approaches would be inadequate or too cumbersome to be practical. The Monte Carlo method uses the speed of the computer to “play out” what would happen to many hypothetical residents under each of the alternatives.
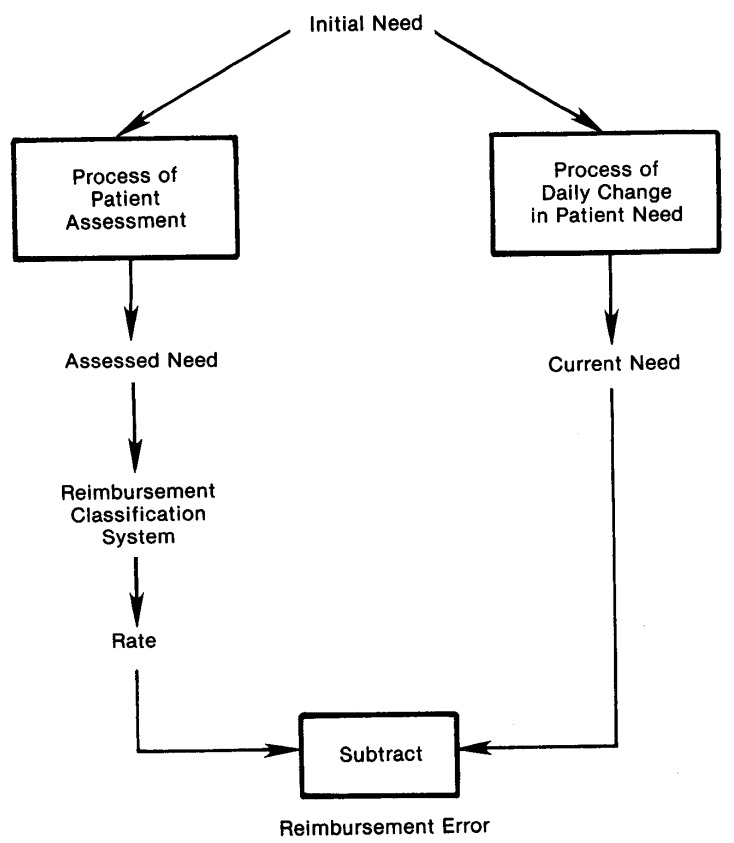
Refer to Figure 1 for a depiction of the steps in the simulation. Each hypothetical resident is assigned an initial need (expressed in dollars) drawn from a probability distribution; the initial need represents the cost of an optimal bundle of services for that resident. Then the resident's assessed need is determined by adding to the initial need a random number representing error in the assessment process. This assessed need is next converted into a reimbursement rate according to whatever reimbursement alternative is being analyzed. With a two level system, the rate is the fixed rate of the level appropriate to the resident's assessed need. With patient-centered reimbursement, the assessed need is the rate. With case-mix reimbursement, the rate is the average of the assessed needs of a sample of residents.
Figure 1. Conceptual Model of Reimbursement Error for an Individual Resident.
As time passes in the simulation, the hypothetical resident's level of need changes. On any given day, the current need is the sum of the initial need and the accumulated daily changes in need (again expressed in dollars). The reimbursement error is the difference between the rate and the current need. At fixed intervals the hypothetical resident's need is reassessed. After many simulated days and many simulated residents, a statistical picture emerges of the distribution of over- and underpayment under each alternative. This distribution of reimbursement error serves as the basis for comparing the alternatives.
In the simulation of payment error, assessment error is assumed to have a normal distribution (bell-shaped curve), the mean value of which represents any bias in the assessment process and the variance of which summarizes the precision of assessment. The daily change in need is likewise assumed to have a normal distribution, where the mean represents the general drift toward deterioration or improvement and the variance represents the volatility of the resident's status. Since the daily change in need has a normal distribution, so will the net accumulated change in need on any given day after an assessment. The distribution of initial need is assumed to be normal, with the mean representing the average debility of residents in the facility and the variance summarizing their diversity.
This model of resident need is similar to a physical model of particle motion known as “Brownian motion with drift.” Like any conceptual model, it contains simplifications. One is that the daily changes in need of an individual are independent and identically distributed over time. A second is that the distribution of daily change in need is independent and identically distributed in cross-section. A third is that the distribution of assessment error does not depend on the level of initial need. There are others, such as the assumption that the distributions are normal. It would be quite easy to repeat the simulations described below using different assumptions if we thought it necessary. In fact, we did repeat several simulations using uniform rather than normal distributions and obtained similar results. We regard the findings as relatively robust on both theoretical and empirical grounds. Their main value is the support they provide for the qualitative conclusions of the analysis.
Plan of Analysis
One of the difficulties with simulation studies is managing the large volume of numbers in the computer simulation program. The complex interplay of factors affecting reimbursement error is indicated by the need to specify the number of residents in the home, the time between assessments, and the means and standard deviations of the distributions of initial need, daily change in need, and assessment error.
To compare alternatives, we also required a summary measure of reimbursement error. A simple summary statistic like a mean or median would be inadequate, since we might rightly be as concerned about the possibility of large errors as about the typical size of an error, and because we might not react to a large underpayment in the same way as to an equally large overpayment. To fully assess alternatives and use all the information provided by the simulations, we must take better account of the entire distribution of reimbursement error and yet still have a compact summary. The solution we adopted was to create a loss function for reimbursement error which differentially weights each part of the distribution of error and produces a single-number summary called the expected loss. The proper crafting of such a loss function will embody policymakers' views about the relative importance of over- and underpayment. We chose to use three simple stereotypical loss functions that treat errors of the same sign with a seriousness proportional to their size (a $10 overpayment, for example, is twice as serious as a $5 overpayment) and that weight underpayments relative to overpayments by factors of 10:1, 1:1, and 1:10. Thus, perspectives ranging from extreme concern for underpayment to extreme concern for overpayment can be applied to the distributions of error resulting from each alternative.
We will compare the alternatives in terms of expected loss in different environments. The elements of the environment which we will vary are the case-mix found in a facility, the uncertainty in assessing needs, and the relative concern for overpayment and under-payment (the “error of primary concern”). As seen in Table 1, there will be three categories of each environmental variable, making a total of 3×3×3=27 comparisons.
Table 1. Environmental Variables for Comparison of Alternatives.
| Environmental Variable | Category | Model |
|---|---|---|
| Case Mix | Light | Normal with mean $15, standard deviation $3 |
| Representative | Normal with mean $20, standard deviation $5 | |
| Heavy | Normal with mean $25, standard deviation $3 | |
| Assessment Uncertainty | Low | Normal with standard deviation $1 |
| Moderate | Normal with standard deviation $3 | |
| High | Normal with standard deviation $10 | |
| Error of Primary Concern | Overpayment | Underpayment counts 1/10 time as much as overpayment |
| Both | Underpayment counts 1 time as much as over-payment | |
| Underpayment | Underpayment counts 10 times as much as overpayment |
We will hold other factors constant as follows. We assume a 100-bed facility. The daily change in need is normal with mean $0.01 and standard deviation $0.10. Resident assessments occur every 30 days; the assessment error is normal with mean $0 (that is, no bias). Initial need is normal in the entire institutionalized population with mean $20 and standard deviation $5. (The distribution in any particular home need not be representative of the distribution across all homes.)
Two of the alternatives must also be described parametrically. In the case of the scheme with two levels, the parameters are the location of the dividing line between levels—taken to be $20—and the fixed rates within each level—taken to be $15 and $25. For case-mix rate adjustment, we assume that a 10 percent sample will be used to determine the average case-mix intensity. In the case of patient-centered rates, no further definition is necessary.
Results
The results of the simulations are summarized in Table 2. The three alternatives are compared by expected loss per resident for each of the 27 combinations of environmental factors. The most important conclusion is that there is no categorically superior alternative: environment matters. When there is little uncertainty about resident assessment, the fine-grained, patient-centered approach is clearly dominant. When assessment uncertainty is moderate, the other alternatives are superior for some combinations of case-mix and error of primary concern, but patient-centered reimbursement continues to be generally attractive. When assessment uncertainty is high, patient-centered reimbursement is always dominated by the other alternatives because it relies too heavily on poor information. In contrast, a two-level system makes distinctions more commensurate with the amount of “noise” (that is, uncertainty or error) in the assessment data, while the case-mix approach responds to the noise by averaging the assessments.
Table 2. Results of Simulated Comparison of Alternatives.
| Simulation | Environment | Average Loss (Standard Error) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Assessment Uncertainty | Case-Mix | Error of Primary Concern | Case-Mix | Two Levels | Patient-Centered | |
| 1 | Low | Light | Overpayment | 2.00 (.21) | 1.60 (.19) | .40 (.06)* |
| 2 | Both | 2.74 (.20) | 2.41 (.17) | .82 (.06)* | ||
| 3 | Underpayment | 10.15(1.52) | 10.53(1.28) | 5.02 (.54)* | ||
| 4 | Representative | Overpayment | 3.18 (.35) | 1.41 (.17) | .40 (.06)* | |
| 5 | Both | 4.49 (.34) | 2.76 (.19) | .82 (.06)* | ||
| 6 | Underpayment | 17.56(2.58) | 16.24(1.97) | 5.02 (.54)* | ||
| 7 | Heavy | Overpayment | 2.00 (.21) | .93 (.11) | .40 (.06)* | |
| 8 | Both | 2.74 (.20) | 2.50 (.18) | .82 (.06)* | ||
| 9 | Underpayment | 10.15(1.52) | 18.20(2.09) | 5.02 (.54)* | ||
| 10 | Moderate | Light | Overpayment | 2.62 (.24) | 1.96 (.23) | 1.19 (.17)* |
| 11 | Both | 3.09 (.23) | 2.73 (.21) | 2.24 (.17)* | ||
| 12 | Underpayment | 7.84(1.22)* | 10.52(1.43) | 12.75(1.49) | ||
| 13 | Representative | Overpayment | 3.76 (.38) | 1.61 (.21) | 1.19 (.17)* | |
| 14 | Both | 4.77 (.36) | 3.20 (.23) | 2.24 (.17)* | ||
| 15 | Underpayment | 14.82(2.28) | 19.12(2.30) | 12.75(1.49)* | ||
| 16 | Heavy | Overpayment | 2.62 (.24) | .83 (.10)* | 1.19 (.17) | |
| 17 | Both | 3.09 (.23) | 2.89 (.23) | 2.24 (.17)* | ||
| 18 | Underpayment | 7.84(1.22)* | 23.52(2.56) | 12.75(1.49) | ||
| 19 | High | Light | Overpayment | 5.46 (.30) | 3.53 (.37)* | 4.04 (.56) |
| 20 | Both | 5.54 (.29) | 4.12 (.34)* | 7.36 (.58) | ||
| 21 | Underpayment | 6.37 (.50)* | 10.03(1.35) | 40.50(4.87) | ||
| 22 | Representative | Overpayment | 6.32 (.46) | 2.19 (.28)* | 4.04 (.56) | |
| 23 | Both | 6.70 (.43) | 3.92 (.30)* | 7.36 (.58) | ||
| 24 | Underpayment | 10.49(1.34)* | 21.27(2.69) | 40.50(4.87) | ||
| 25 | Heavy | Overpayment | 5.46 (.30) | .92 (.10)* | 4.04 (.56) | |
| 26 | Both | 5.54 (.29) | 4.52 (.36)* | 7.36 (.58) | ||
| 27 | Underpayment | 6.37 (.50)* | 40.58(3.98) | 40.50(4.87) | ||
best alternative
We assumed in the simulations that the case-mix rate calculation was based on a sample of only 10 residents in a 100-bed home. Using a larger sample improves the estimate (although in practice it would also increase the cost of implementation); in at least three of the environments (simulations 19, 20 and 26), the case-mix method outperformed its competitors when the sample size was increased. A more general comparison of case-mix and patient-centered reimbursement appears in Willemain (1980), which reviews empirical evidence on assessment uncertainty and argues the superiority of the case-mix approach.
Summary
The design of nursing home reimbursement systems is a challenging task demanding both a sense of how to do the job well and a knowledge of how to assemble components into an effective system. A common analytical framework for assessing system performance is reimbursement error. A systematic view of reimbursement error recognizes that the performance of any payment mechanism depends on the environment in which it operates. Key elements of the environment are the bias and precision of resident assessment techniques, the diversity and volatility of resident need, and policymakers' sensitivities to over- and underpayment.
Comparisons of alternatives should be careful to specify the environment within which a payment system will operate. System design should not proceed on the basis of “obvious” characterizations such as: “Schemes based on two levels of care are too crude; patient-centered schemes are efficient and responsive.” This statement is appropriate for some environments and inappropriate for others, as illustrated by the Monte Carlo simulations.
Ultimately, the designer of a reimbursement system must reach beyond the theoretical considerations raised here to confront issues of feasibility and durability so important to implementation. Still, the concepts of “reimbursement error” and “environment” and the simulation of model systems make design less doctrinaire and point the way for empirical followup. For instance, it is clear from the simulation study that a critical empirical issue is the degree of uncertainty in resident assessment. Furthermore, the models provide a way to evaluate assessment technologies, since we can estimate how precise resident assessment must be in order to support patient-centered reimbursement. We have also discovered a promising alternative to patient-centered reimbursement that uses the same information more modestly and—in some environments—more effectively: case mix reimbursement.
Acknowledgments
The author acknowledges the assistance of Alonzo Plough, Christine Bishop, Stanley Wallack, and Joseph Ferreira in the preparation of this paper.
References
- Bishop Christine, Plough Alonzo, Willemain Thomas. Nursing Home Levels of Care: Problems and Alternatives. Health Care Financing Review. 1980;2 [PMC free article] [PubMed] [Google Scholar]
- Fulton Robert. Federal Register. 1976;41:27300–27308. [Google Scholar]
- Hillier Frederick, Lieberman Jerald. Introduction to Operations Research. San Francisco: Holden-Day; 1967. [Google Scholar]
- Walsh Thomas, Koetting Michael. Patient Related Reimbursement for Long-Term Care. 1978 Unpublished. [Google Scholar]
- Willemain Thomas. A Comparison of Patient-Centered and Case-Mix Reimbursement for Nursing Home Care. Health Services Research. 1980 Winter; forthcoming. [PMC free article] [PubMed] [Google Scholar]