Abstract
In the early years of the Medicare program, proportionally more whites than non-whites among the aged used Medicare services. This article examines the use and reimbursement of Medicare services by the aged between 1967 and 1976 to determine if racial differences still exist. To do so, three measures are studied. The first, the number of persons reimbursed for Medicare services per 1,000 enrollees, measures access to Medicare's reimbursement system. The second, reimbursement per person using reimbursed services, measures the amount of reimbursement received after persons exceed Medicare deductibles. The third, reimbursement per enrollee, indicates the combined effect of access and reimbursement and represents a measure of equity for the population at risk. Analysis of the three measures by type of Medicare service found that the disparities in use and reimbursement of services by race decreased considerably between 1967 and 1976. This trend was found both at the national and at the regional level.
Overall, the decreases in the disparity measured are noteworthy. By type of service, proportionally more whites than non-whites still receive reimbursement. However, once non-whites exceed deductibles, the reimbursements per person using reimbursed services are generally comparable or higher than reimbursements to whites.
Background
Purpose
The Medicare program was established to lessen the financial burden of aged persons for medical care. The law states that the hospital insurance program “provides basic protection against the cost of hospital and post-hospital services,” (Section 1811 of The Social Security Act). The law also requires institutional providers of medical care to furnish services without discrimination in accordance with Title VI of the Civil Rights Act of 1964.
It was clearly the intent of the law that Medicare provide equal access to medical care regardless of race, income, or location of residence. In 1975, Karen Davis published an article entitled, “Equal Treatment and Unequal Benefits: The Medicare Program.” Davis found that in 1968, the second full year of the program, there were wide disparities by race in average Medicare reimbursements. The average reimbursement per enrollee for whites was significantly higher than that for non-whites. This paper analyzes Medicare data for 1967 through 1976 to determine if racial disparities have changed over time.
The data are examined at both the national and the regional level. It is important to consider regional data because both the distribution of the aged population and average Medicare reimbursements vary significantly by race and region. For instance, over half of the aged non-white population lives in the South. Thus, the South strongly affects national data.
Medicare Program Benefit Structure
Medicare is made up of two separate but complementary insurance programs: hospital insurance (HI) and supplementary medical insurance (SMI), (Medicare: Health Insurance for the Aged and Disabled, 1978). Persons 65 and over, if eligible, pay no insurance premiums for HI but are subject to a deductible and, in some instances, to co-insurance. Those aged not eligible for HI may enroll by paying a premium. SMI is a voluntary program requiring a monthly premium, a deductible, and coinsurance payments.
Reimbursements for covered SMI services after the annual $60 deductible is met ($50 deductible until 1973) are based on “reasonable” charges. For example, Medicare determines total covered charges for physicians' services by first eliminating items not covered by Medicare. Then the remainder may be reduced to “reasonable” charges. The $60 annuual deductible is then applied to the reasonable charges. Medicare then pays 80 percent of the reasonable charges and the person is liable for the $60 deductible and the 20 percent coinsurance.
When physicians do not accept assignment, the enrollee is liable for the difference between the total covered charge and the reasonable charge. In all cases, the enrollee is liable for any noncovered charges.
Total Medicare reimbursements for services incurred by the aged in 1976 are shown by type of service in Table 1. Hospital insurance benefits represented 73.1 percent of total reimbursements to the aged. Inpatient hospital services, by far the largest HI service, were 70.0 percent of total reimbursements to the aged. Reimbursements for the other HI benefits as a percent of total reimbursements to the aged were much smaller: skilled nursing facility, 1.8 percent, and home health agency, 1.2 percent. Total supplementary medical insurance benefits represented 26.9 percent of total Medicare reimbursements to the aged. The major SMI benefit was physicians' and other medical services, 23.2 percent. The remaining SMI benefits were: outpatient services, 3.3 percent, and home health benefits, 0.5 percent. Thus, in terms of importance, two services, inpatient hospital and physicians' and other medical services, accounted for 93.2 percent of total reimbursements. Though these two services are the most important, for completeness, each of the services in Table 1 is analyzed for racial disparities in usage and reimbursement.
Table 1. Amount of Medicare Reimbursements and Percent Distribution for the Aged by Type of Service, 1976.
| Type of Service | Reimbursement | |
|---|---|---|
|
| ||
| Amount (in millions) | Percent | |
| All Services (HI and/or SMI) | $15,680 | 100.0 |
|
|
|
|
| Hospital Insurance (HI) | 11,456 | 73.1 |
|
|
|
|
| Inpatient Hospital | 10,980 | 70.0 |
| Skilled Nursing Facility | 283 | 1.8 |
| Home Health Agency | 193 | 1.2 |
| Supplementary Medical Insurance (SMI) | 4,223 | 26.9 |
|
|
|
|
| Physician and Other Medical | 3,633 | 23.2 |
| Outpatient | 516 | 3.3 |
| Home Health Agency | 75 | .5 |
Definitions and Methods
This paper analyzes three relative measures. The first is a measure of usage of Medicare services; the other two are measures of average Medicare reimbursements. For ease in understanding, the measures are stated in this paper by using acronyms. The usage measure is as follows:
Persons served per 1,000 enrolled = (PS/E) (M) = PSM/E.
Persons served (PS) is defined as the number of aged Medicare beneficiaries who used covered services that exceeded Medicare deductibles and who were reimbursed. E stands for the number of enrollees under HI or under SMI or under HI and SMI. M stands for 1,000. Since persons served per enrollee is a fraction less than one, it is customarily multiplied by 1,000 for ease in presentation. For example, in 1967, for the aged Medicare population, there were 3,591,600 white persons served under the HI program and 17,385,350 white enrollees under HI. Thus, PSM/E = (3,591,600) (1,000)/17,385,350 = (.2066) (1,000) = 206.6.
The two measures of reimbursement are:
Reimbursement per person served = R/PS.
Reimbursement per enrollee = R/E.
Where R stands for the amount of reimbursement.
The relationship between the three measures is: (PS/E) (R/PS) ≡ R/E. The equation shows that R/E measures the combined effect of the other two variables. Thus, R/E represents the average Medicare reimbursement paid to enrollees (the population at risk). PS/E represents the proportion of the population at risk that had access to Medicare in that enrollees received reimbursement. R/PS represents the extent to which enrollees who exceeded the deductible were reimbursed. This paper presents tables showing each of these measures by race, type of HI and SMI benefit, and by the region in which enrollees live.
The method used in this report to measure racial disparity in use and reimbursement of Medicare services is to compute the ratio of whites to non-whites for each of the three measures in this study.
The letter D is used as an acronym (not as a mathematical symbol) to indicate the disparity in the ratio of whites to non-whites for each of the three measures. For example, D (PSM/E) represents the disparity of white to non-white persons served per 1,000 enrolled. To illustrate, in 1976, PSM/E for whites using HI and/or SMI services was 561 and the comparable figure for non-whites was 495, as shown in the following table:
Disparity Ratios of Whites to Non-Whites for HI and/or SMI Services, 1976.
| Race | Measures of Use and Reimbursement | |||
|---|---|---|---|---|
|
| ||||
| PSM/E | R/PS | R/E | ||
| White | 561 | $1212 | $680 | |
| Non-White | 495 | 1247 | 617 | |
|
|
||||
| Ratio of White to Non-White | ||||
|
|
||||
| D(PSM/E) | D(R/PS) | D(R/E) | ||
|
|
||||
| Disparity Ratios | 1.13 | .97 | 1.10 | |
The ratio of PSM/E of whites to PSM/E of non-whites, 561 to 495, was 1.13. Thus, D(PSM/E) in this example is 1.13, indicating that whites had a 13 percent higher proportion of persons served per 1,000 enrolled than did non-whites. Comparable disparity ratios are computed for the other two variables. Thus, D(R/PS) was .97 and indicates the disparity in the amount of reimbursement per person served for whites compared to non-whites. D(R/E) was 1.10, the disparity of whites to non-whites in the amount of reimbursement per enrollee.
D ratios greater than 1.00 indicate whites have higher PSM/E, R/PS, or R/E than non-whites. D ratios less than 1.00 indicate non-whites have lower PSM/E, R/PS, or R/E than whites. The D(R/PS) of .97 in the example indicated that the (R/PS) of whites was 97 percent of that of non-whites in 1976.
Having defined our terms and methods, we now summarize Davis' findings in terms of race. Davis found for HI and/or SMI services (total Medicare services) incurred in 1968:
D(PSM/E) = 1.35,
D(R/PS) = 1.04, and
D(R/E) = 1.40.
Davis also analyzed D(R/E), by type of service. The two largest disparities were for physicians' and other medical services with D(R/E) = 1.63, and for skilled nursing facility services, with D(R/E) = 2.17. While various measures indicated a decrease in the higher use of medical care by whites between 1965 and 1967, and a further decrease in 1968, the 1968 disparities were still sizeable (Lowenstein, 1971).
Source of Data
The primary data used in this paper are from a 5 percent sample of aged enrollees selected by their health insurance number from a computer file of all enrollees. The presence of the enrollee's health insurance number on every claim tabulated by Medicare's central record system makes possible a summary of each person's reimbursement (Medicare: Health Insurance for the Aged and Disabled, 1973-74). The sample is part of an annual data collection program that began with the start of Medicare. This sample provides data by type of service for the number of persons served and their reimbursements by age, race, sex, and residence. Enrollee counts, the denominator of persons served per 1,000 enrolled, are available from another annual report which provides counts of the number of aged enrollees on July 1 of a given year (Medicare: Health Insurance for the Aged and Disabled, 1976).
Race or color designation is obtained when persons apply for a social security number and fill out an application form. The form currently used asks the applicant to check a box marked “White,” “Negro”, or “other.” If no box is checked, the race category is classified as “race unknown.” Medicare program statistical tabulations group “Negro” and “other” into a class called “all other races.” Thus, this paper compares whites and all other races. All other races are referred to as non-whites in this report. The term non-whites is used rather than minorities because some minorities, for example, Hispanics, may choose any of the three race categories on the application form. Non-whites are primarily black persons except in the Western States where a sizeable proportion are Orientals and American Indians.
Other Medicare data sources are used to estimate the number of persons who used covered services but did not exceed the SMI deductible and were not reimbursed. Those aged who do not exceed the SMI deductible are excluded from the count of persons served. However, these excluded persons generally use some SMI services, even though they are not reimbursed. Therefore, data on persons using at least one covered physician's or hospital outpatient service, whether they were reimbursed or not, are also presented by race. A disparity ratio of white to non-white users of any of these two covered SMI services are then calculated. This measure provides information on the proportion using covered services whether or not they met the SMI deductible. The purpose is to determine if there is more racial equality in the proportion of the population using at least one covered SMI service in comparison to the proportion of the population exceeding the SMI deductible and receiving reimbursement.
Two sources of data are used to make these computations. One source is the Current Medicare Survey which provides data on the use of any covered physicians' service. This survey was based on a national probability sample of aged Medicare enrollees (Current Medicare Survey Report, June 1978). The other source is a 5 percent sample of aged Medicare enrollees which provides data on the use of any covered hospital outpatient service.1 All hospital outpatient bills, regardless of deductible status, are recorded in Medicare central records. The reimbursement of aged hospital outpatient users represented 86 percent of all outpatient reimbursements in 1975. These records are summarized for each individual.
The data, except for the Current Medicare Survey, are based on administrative records and are a by-product of the Medicare program. Administrative records lack information on many characteristics of enrollees such as health status, income, education, and use of services not covered by the Medicare program. Hence, these variables which may influence the trends noted in this paper are not accounted for in this analysis. Thus, racial disparities in usage may also be attributed to several variables other than the Medicare program. Accordingly, it is unknown to what extent the Medicare program is responsible for the decreases in racial disparity in the use and reimbursement of medical services.
Findings
Persons Served per 1,000 Enrolled (PSM/E)
All Services (Hospital Insurance and/or Supplementary Medical Insurance)
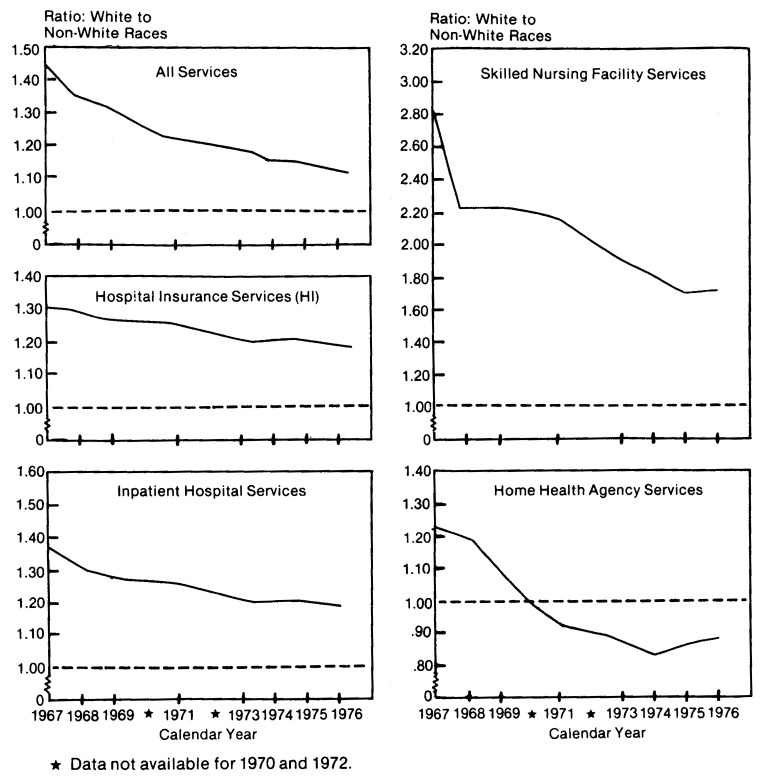
In 1967, the first full calendar year of Medicare, PSM/E for whites was 375, the comparable rate for non-whites was 261, thus, D(PSM/E) was 1.44 (Table 2). However, between 1967 and 1976, D(PSM/E) declined each year and by 1976 was only 1.13. Most of this decline took place from 1967 to 1971, the early years of the program (Figure 1). Similar findings are described next for each type of Medicare benefit shown in Table 2.
Table 2. Use of Medicare Services by the Aged: Persons Served Per 1,000 Enrolled by Type of Service and Race, 1967-19761.
| Type of Reimbursed Service | 1967 | 1968 | 1969 | 1971 | 1973 | 1974 | 1975 | 1976 |
|---|---|---|---|---|---|---|---|---|
| White | ||||||||
| Hospital Insurance and/or Supplementary Medical insurance | 375 | 407 | 435 | 432 | 474 | 501 | 535 | 561 |
| Hospital Insurance | 207 | 208 | 212 | 216 | 218 | 218 | 224 | 233 |
| Inpatient Hospital Services | 189 | 201 | 208 | 215 | 216 | 216 | 222 | 231 |
| Skilled Nursing Facility Services | 19 | 21 | 20 | 12 | 12 | 12 | 12 | 13 |
| Home Health Agency Services | 7 | 8 | 10 | 8 | 10 | 12 | 15 | 18 |
| Supplementary Medical Insurance | 372 | 403 | 434 | 460 | 474 | 505 | 541 | 569 |
| Physician and Other Medical Services | 367 | 395 | 425 | 448 | 462 | 491 | 526 | 553 |
| Outpatient Services | 70 | 72 | 84 | 107 | 123 | 144 | 170 | 194 |
| Home Health Agency Services | 7 | 7 | 7 | 4 | 5 | 6 | 7 | 8 |
| All Other Races | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 261 | 302 | 333 | 353 | 398 | 431 | 467 | 495 |
| Hospital Insurance | 159 | 162 | 167 | 174 | 180 | 183 | 188 | 196 |
| Inpatient hospital services | 138 | 154 | 165 | 173 | 178 | 180 | 185 | 193 |
| Skilled Nursing Facility Services | 7 | 9 | 9 | 6 | 6 | 7 | 7 | 8 |
| Home Health Agency Services | 5 | 7 | 9 | 9 | 11 | 14 | 17 | 20 |
| Supplementary Medical Insurance | 263 | 304 | 341 | 388 | 412 | 448 | 488 | 518 |
| Physician and Other Medical Services | 246 | 279 | 309 | 350 | 376 | 409 | 449 | 476 |
| Outpatient Services | 79 | 90 | 103 | 134 | 152 | 174 | 199 | 225 |
| Home Health Agency Services | 6 | 7 | 8 | 5 | 7 | 8 | 9 | 12 |
| Ratio: White to All Other Races | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.44 | 1.35 | 1.31 | 1.22 | 1.19 | 1.16 | 1.15 | 1.13 |
| Hospital Insurance | 1.30 | 1.29 | 1.27 | 1.25 | 1.21 | 1.20 | 1.20 | 1.19 |
| Inpatient Hospital Services | 1.36 | 1.31 | 1.27 | 1.25 | 1.21 | 1.20 | 1.20 | 1.19 |
| Skilled Nursing Facility Services | 2.83 | 2.22 | 2.23 | 2.16 | 1.90 | 1.81 | 1.70 | 1.72 |
| Home Health Agency Services | 1.23 | 1.20 | 1.08 | .93 | .87 | .83 | .86 | .88 |
| Supplementary Medical Insurance | 1.41 | 1.32 | 1.28 | 1.19 | 1.15 | 1.13 | 1.11 | 1.10 |
| Physician and Other Medical Services | 1.49 | 1.41 | 1.38 | 1.28 | 1.23 | 1.20 | 1.17 | 1.16 |
| Outpatient Services | .88 | .80 | .81 | .80 | .81 | .83 | .85 | .86 |
| Home Health Agency Services | 1.14 | 1.04 | .94 | .74 | .72 | .71 | .76 | .72 |
Data for 1970 and 1972 not available.
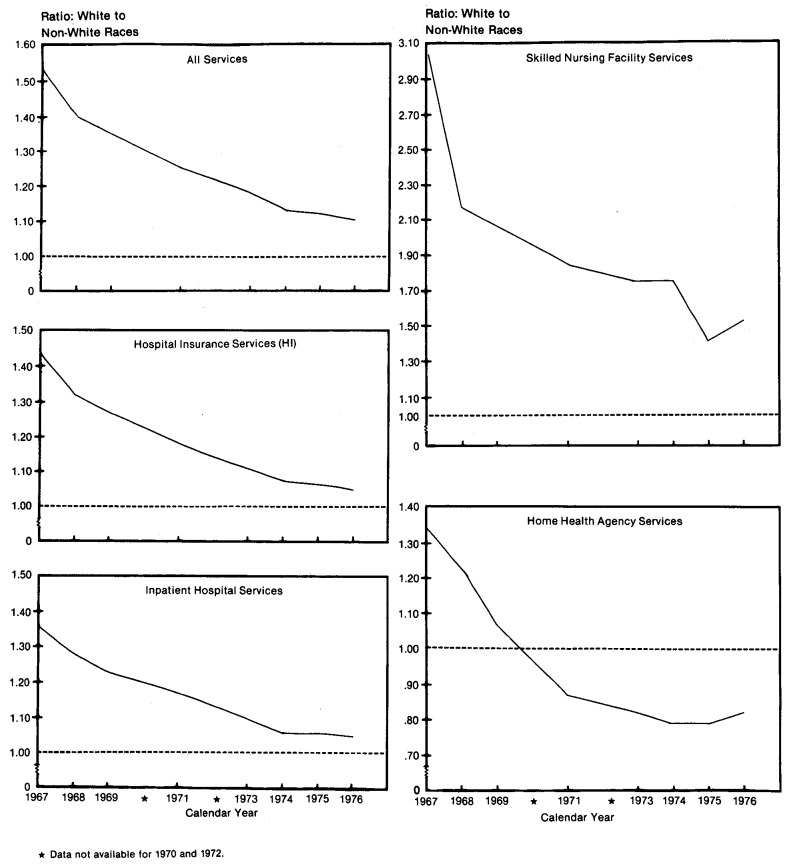
Figure 1. Use of All and HI Services by the Aged, Persons Served Per 1,000 Enrolled: Ratio of White to Non-White Races, 1967-1976.
Hospital Insurance
The number of persons served in inpatient hospitals and for all hospital insurance services are nearly the same. As a result, D(PSM/E) for both HI and inpatient hospital services are nearly identical (Table 2 and Figure 1). Therefore, this analysis of HI services begins with inpatient hospital services. For inpatient hospital services, D(PSM/E) was 1.36 in 1967 and fell to 1.19 in 1976 indicating a decline in the racial disparity. However, there has been little change in D(PSM/E) since 1973. Thus, D(PSM/E) for the major HI component, inpatient hospital services, indicates that relatively more whites receive inpatient hospital care under Medicare.
The largest D(PSM/E) for any type of service covered by Medicare was skilled nursing facility services; that difference was 2.83 in 1967, and in 1976 it was still 1.72. However, note that PSM/E for skilled nursing facility services by both whites and non-whites were very small, 13 and 8 per 1,000 in 1976, respectively (Table 2).
The D(PSM/E) for home health services in 1967 was 1.23, but by 1976 it had fallen to .88. However, for both races, PSM/E using home health services was small; 18 per 1,000 for whites and 20 per 1,000 for non-whites in 1976.
Supplementary Medical Insurance
Before examining the use of SMI services it is important to note the changes that have occurred in the SMI population. In 1967, the ratio of SMI to HI enrollment among whites was 92.7 percent, the comparable figure for non-whites was 83.2 percent. By 1976, the difference had narrowed. The white proportion was 98.1 and the non-white proportion was 96.3 percent.
The improvement of non-white coverage was most likely related to the growth in the State buy-in program, a provision of the Medicare law. This program permits States to pay SMI premiums for those aged receiving cash payments under public assistance programs. In 1967 only 27 States participated in this program. By 1976, 46 States and the District of Columbia participated. Of the 1.4 million aged persons covered by the State buy-in program in 1967, 8.2 percent were non-whites (Medicare: Health Insurance for the Aged and Disabled, 1976). By 1976, aged non-whites were 25 percent of the total State buy-in population.
This increase in the proportion of non-whites covered by SMI (because of the growth of the State buy-in program) is one likely reason for the relatively greater increase in the use of SMI services by non-whites in the 1967-1976 period. Persons qualify for the buy-in program because they cannot afford to pay the SMI premium. In addition, they may also qualify for Medicaid depending upon requirements in each State. If so, Medicaid will pay Medicare deductibles and co-insurance. Thus, non-whites covered under the buy-in program are likely to be above average users of Medicare services compared to non-whites who are able to pay the SMI premiums.
The distribution of reimbursements, as shown in Table 1, indicate that among SMI services, physicians' and other medical services was the major service category. By race, these were also the most important SMI services among the aged in 1976:
Distribution of SMI Reimbursements by Race, 1976.
| Type of SMI Service | Reimbursement | |
|---|---|---|
|
| ||
| Whites | Non-Whites | |
| Supplementary Medical Insurance | 100.0 | 100.0 |
| Physician and Other Medical | 87.0 | 74.4 |
| Outpatient | 11.4 | 22.5 |
| Home Health Agency | 1.6 | 3.1 |
Eighty-seven percent of reimbursements to whites for SMI services were for physicians' and other medical services compared to 74 percent for non-whites. Twenty-three percent of SMI reimbursements to non-whites were for outpatient services, while for whites they were 11 percent.
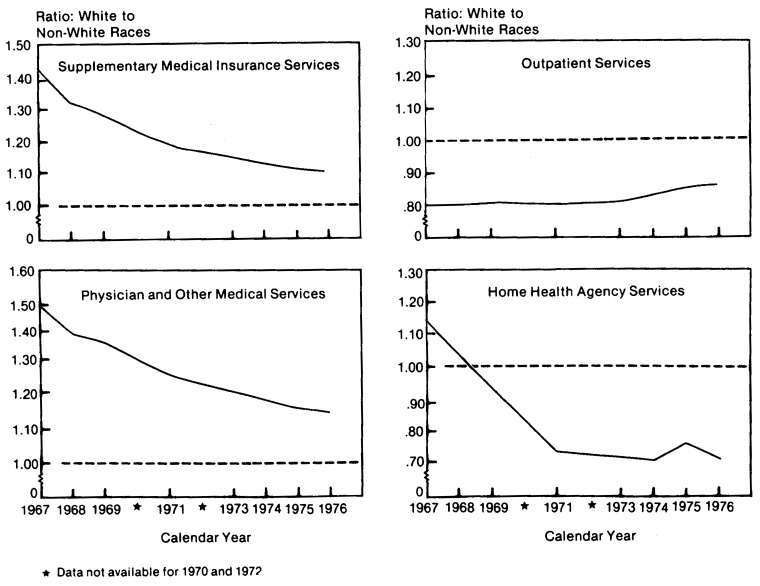
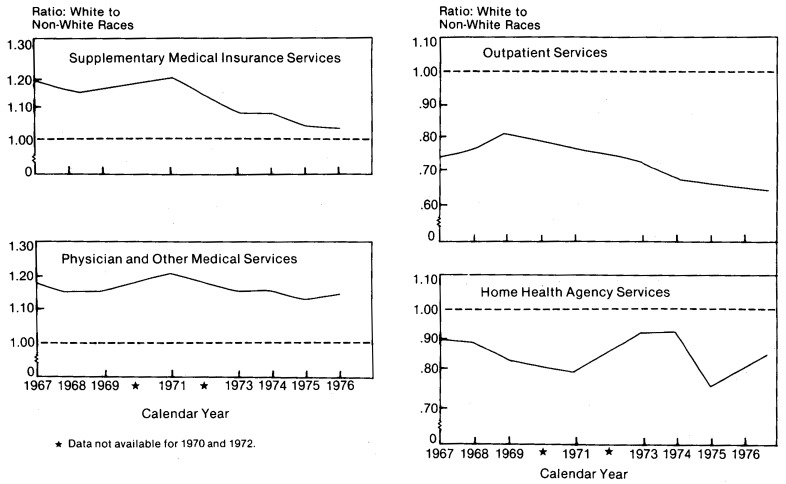
Returning to the analyses of D(PSM/E): for all SMI services D(PSM/E) fell from 1.41 to 1.10 in the 1967-1976 period (Table 2 and Figure 2).
Figure 2. Use of SMI Services by the Aged, Persons Served Per 1,000 Enrolled: Ratio of White to Non-White Races, 1967-1976.
Physicians' and Other Medical Services
For services of physicians and suppliers of medical services, D(PSM/E) was 1.49 in 1967 and fell to 1.16 in 1976. Though D(PSM/E) for physicians and suppliers of medical services (showing higher proportions of whites) has decreased over time, there were considerable differences in the type of physicians used by whites and non-whites for services rendered in 1975.2 Thus, according to a study of reimbursed physicians' services (excluding suppliers) by type of physician specialty, D(PSM/E) was much higher for aged whites than non-whites as follows:
Persons Served per 1,000 Enrolled by Race and Physician Specialty, 1975.
| Physician Specialty | PSM/E | ||
|---|---|---|---|
|
|
|||
| White | Non-White | D(PSM/E) | |
| All Physicians | 504 | 419 | 1.20 |
| General Practice | 223 | 202 | 1.10 |
| Internal Medicine | 224 | 168 | 1.33 |
| Radiology | 137 | 109 | 1.26 |
| General Surgery | 98 | 75 | 1.31 |
| Orthopedic Surgery | 47 | 20 | 2.35 |
Presumably, D(PSM/E) in the use of physician specialists indicates that white beneficiaries are receiving higher quality care.
Outpatient Services
Charges for outpatient services under the Medicare program are reimbursed for two types of services: diagnostic and therapeutic. Diagnostic services are examinations and tests which aid in assessing medical conditions or in identifying diseases. Covered outpatient diagnostic services include those of nurses, psychologists, and technicians. Drugs needed for diagnosis, and the use of supplies and equipment are also reimbursable to outpatients under SMI. Therapeutic services are those which aid physicians in treating patients and must be incident to physicians' services. They include the use of hospital facilities such as clinics and emergency rooms, the services of various hospital personnel, and the use of medical supplies and devices. Outpatient services under Medicare generally exclude charges by physicians except when physicians elect to have the hospital submit the bill for them. Physicians' charges are usually billed on a form separate from the outpatient billing form and reimbursements for their services are tabulated under physicians' and other medical services.
From the start of Medicare, D(PSM/E) for outpatient services has been less than 1.00. In 1976 the disparity ratio was .86.
Home Health Agency Services
For HHA services under the SMI program, D(PSM/E) was .72 in 1976, the lowest for any SMI service. Again, PSM/E for both races was small, 8 per 1,000 for whites and 12 per 1,000 for non-whites (Table 2).
Racial Differences in Total Users Per 1,000 Beneficiaries
The SMI services discussed so far have dealt solely with data of aged enrollees who exceeded the SMI deductible and were reimbursed. (We are concerned only with the SMI deductible because virtually all users of HI services exceed the HI deductible.) The Current Medicare Survey has indicated that about 300 aged enrollees per 1,000 who used SMI services in a year are excluded from a count of PSM/E because they did not exceed the SMI deductible and were not reimbursed. This raises the question, are there racial disparities in the number of “total users” of SMI services per 1,000 enrolled? Total users are defined as those persons who used at least one covered service whether or not they exceeded the SMI deductible and were reimbursed. To answer this question, data are available on the number of total users of covered physicians' services and covered hospital outpatient services.
Total Users of Physicians' Services
The Current Medicare Survey for 1976 reported that the percentage of aged persons using any SMI covered physicians' service were nearly equal for whites and non-whites. Among whites the total user rate was 809 per 1,000 enrolled and among non-whites 786 per 1,000 enrolled. The difference was not statistically significant. Thus, there was no disparity by race between the two groups in the total users of covered physicians' services per 1,000 enrolled. The comparable D(PSM/E) figures for 1976 for physicians' and other medical services were 553 per 1,000 for whites and 476 per 1,000 for non-whites or D(PSM/E) was 1.16 (Table 2).
What accounts tor D(PSM/E) still showing higher proportions of whites in the use of physicians' services? The study of reimbursed physicians' services used by aged persons under SMI during 1975 indicates a possible explanation (see footnote 2). The explanation is that for the United States, average reimbursement per physicians' services was higher for whites than non-whites. (Whites averaged $11.36 per service and non-whites $10.09). These differences in charges per service resulted in higher proportions of whites exceeding the SMI deductible than non-whites. Another possible factor, the number of physicians' services per person served was ruled out because for whites and non-whites they were nearly equal (22.0 services vs. 21.2 services, respectively).
Total Users of Covered Hospital Outpatient Services
The proportion of total users of covered outpatient services (hospital and non-hospital) may be approximated by data collected from Medicare hospital outpatient bills. Hospital outpatient reimbursements represented 86 percent of total outpatient reimbursements to the aged in 1975. These data provide a count of the number of white and black enrollees using covered hospital outpatient services whether or not they exceeded the SMI deductible.
For outpatient services, D(PSM/E) was .85 in 1975. The comparable disparity for total white and black users of hospital outpatient services whether or not they were reimbursed was similar, .91 (Table 3). In addition, average covered charges of blacks were higher, $140, than of whites, $96 (Table 3.) (Blacks represent 89 percent of the HI and/or SMI non-white population.) Presumably, the higher average charges of blacks resulted in higher proportions of them meeting the SMI deductible and, in turn, to D(PSM/E) showing higher proportions of non-whites using outpatient services.
Table 3. Persons 65 and Over Using Hospital Outpatient Services Per 1,000 Enrolled and Charges Per User by Race, United States, 1975.
| Users and Charges | White | Black | Ratio: White to Black |
|---|---|---|---|
| Total Users Per 1,000 Enrolled | 248.0 | 272.6 | 0.91 |
| Covered Charges Per User | $96.33 | $140.14 | .69 |
Source: Martin Ruther, Medicare: Use of Hospital Outpatient Services by the Aged, 1975, Office of Research, Demonstrations and Statistics, Health Care Financing Administration (in press).
Regional Analysis
Before examining the disparity in PSM/E by race and region it is important to note differences in the regional distribution of whites and non-whites. In 1976 about equal proportions of aged whites (26-29 percent) lived in the Northeast, North Central, and Southern regions, and 17 percent lived in the West (Table 4.) Among non-whites, 56 percent lived in the South, and 12-17 percent lived in the other regions. Non-whites represented 15 percent of the aged population in the South and ranged from 5 to 8 percent of the aged population in the remaining regions. An analysis of Medicare usage by region indicates the extent that regional differences affect racial disparity in the nation.
Table 4. Persons 65 years and Over Enrolled for Hospital Insurance Under Medicare by Race, Region and Type of County, July 1, 1976.
| Hospital Insurance | |||
|---|---|---|---|
|
| |||
| Region and Type of County | Total1 | White | All Other Races |
| Number | |||
| Census Region: | |||
| United States2 | 22,500,506 | 20,038,013 | 1,851,964 |
| Northeast | 5,576,039 | 5,146,231 | 279,862 |
| North Central | 6,183,466 | 5,706,878 | 311,864 |
| South | 7,089,902 | 5,864,485 | 1,031,357 |
| West | 3,631,862 | 3,306,499 | 227,183 |
| Residence:3 | |||
| Metropolitan | 14,989,437 | 13,669,261 | 1,320,176 |
| Nonmetropolitan | 6,865,069 | 6,336,755 | 528,314 |
| Percent Distribution | |||
| Census Region: | |||
| United States2 | 100.0 | 100.0 | 100.0 |
| Northeast | 24.8 | 25.7 | 15.1 |
| North Central | 27.5 | 28.5 | 16.8 |
| South | 31.5 | 29.3 | 55.7 |
| West | 16.1 | 16.5 | 12.3 |
| Residence:3 | |||
| Metropolitan | 66.6 | 68.2 | 71.3 |
| Nonmetropolitan | 30.5 | 31.6 | 28.5 |
| Percent Distribution | |||
| Census Region: | |||
| United States2 | 100.0 | 89.1 | 8.2 |
| Northeast | 100.0 | 92.3 | 5.0 |
| North Central | 100.0 | 92.3 | 5.0 |
| South | 100.0 | 82.7 | 14.5 |
| West | 100.0 | 91.0 | 6.3 |
| Residence:3 | |||
| Metropolitan | 100.0 | 91.2 | 8.8 |
| Nonmetropolitan | 100.0 | 92.3 | 7.7 |
Includes race unknown.
Includes residence unknown.
Excludes county unknown.
Since this report combines blacks and all other non-whites, a distribution of these two groups by region is presented to indicate the proportion of blacks in the non-white Medicare population (Table 5.) Aged black Medicare enrollees in the Northeast, North Central, and South accounted for about 90 to 98 percent of aged non-whites in 1977. However, in the West, blacks were only 42 percent of non-white beneficiaries. The 1970 Census found that about 10 percent of the aged non-whites living in the West were American Indians (Census of Population: 1970). The number of Indians covered by Medicare is unknown but “very few of them have worked long enough for social security coverage,” (Indian Health Care Improvement Act, 1975). Thus, they would be ineligible for HI and those not enrolled under the State buy-in program would likely not be able to afford SMI premiums. Further, the report states, “since most Indians reside on remote reservation lands, access to Medicare is severely limited.” Most Indians are probably eligible for services of the Indian Health Service (IHS). However, Medicare reimbursements to the IHS for services rendered by them to Medicare enrollees did not become effective until October 1976. Therefore, the racial disparities in the West in the period covered by this report may be somewhat overstated because non-white usage is understated in Medicare records.
Table 5. Aged Non-White HI and/or SMI Enrollees by Region, July 1, 1977.
| Region | Non-Whites | ||
|---|---|---|---|
|
| |||
| Total | Black | All Other | |
| United States | 100.0 | 89.0 | 11.0 |
| Northeast | 100.0 | 89.8 | 10.2 |
| North Central | 100.0 | 95.0 | 5.0 |
| South | 100.0 | 97.6 | 2.4 |
| West | 100.0 | 42.2 | 57.8 |
Source: Five percent sample of Medicare enrollees.
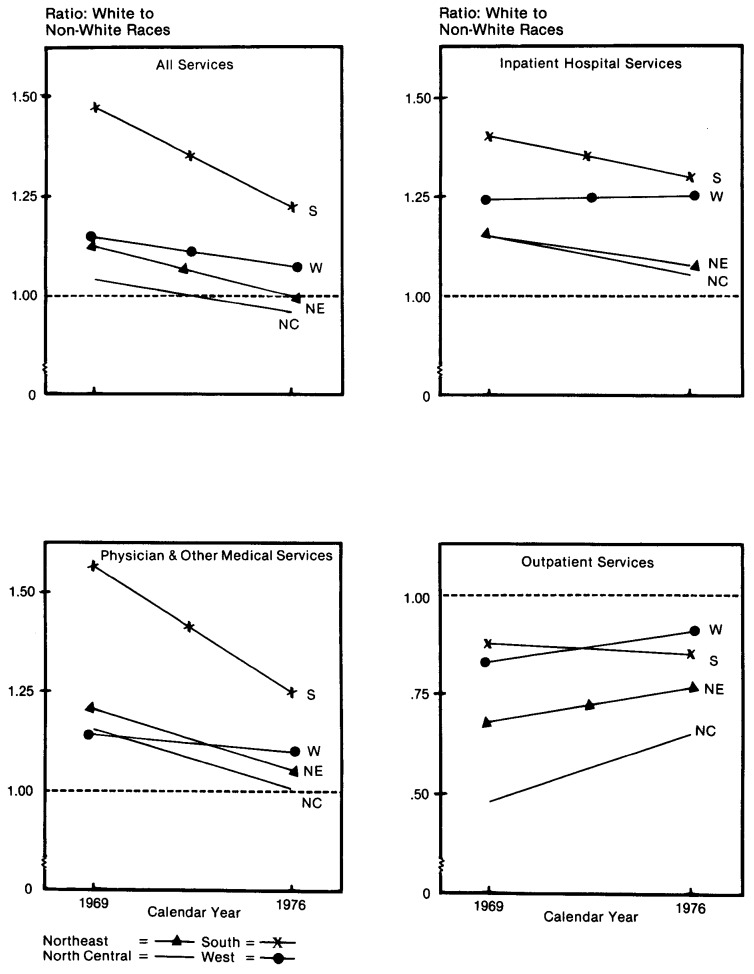
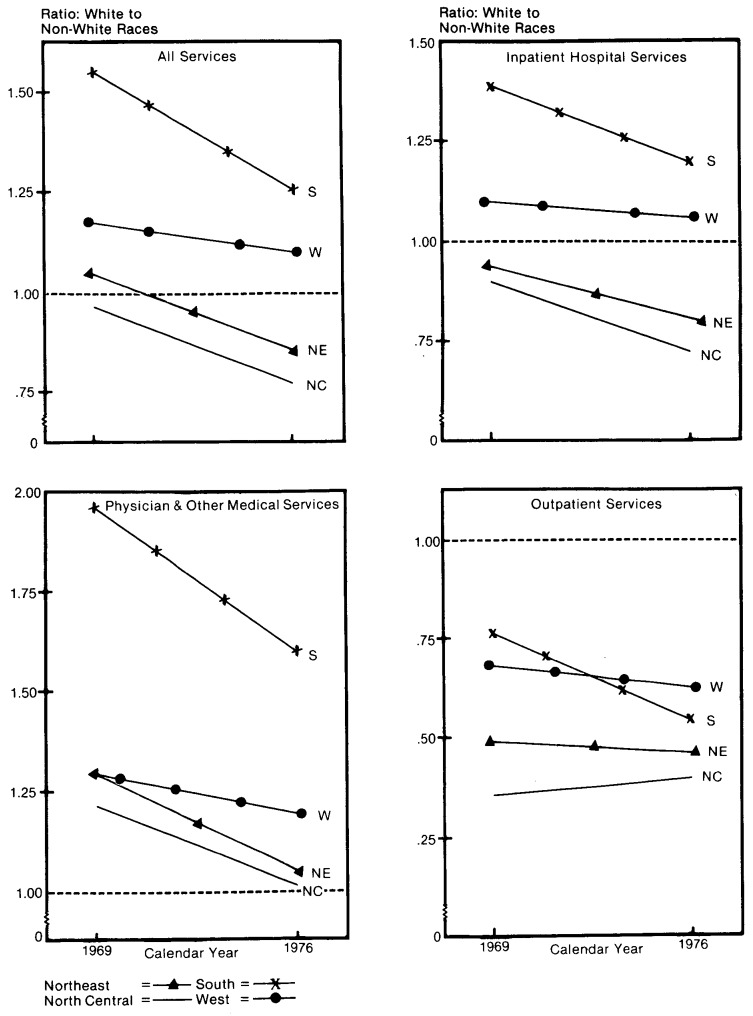
Between 1969 and 1976, for HI and/or SMI services there was a decrease in D(PSM/E) in all four regions (Table 6 and Figure 3). (Data by region were not available for 1967). However, D(PSM/E) in the South was still 1.22 by 1976 indicating considerable disparity showing higher proportions of whites. The comparable figures were 1.07 in the West, 1.00 in the Northeast and .96 in the North Central States.
Table 6. Use of Medicare Services by the Aged: Persons Served Per 1,000 Enrolled by Type of Service, Race, and Region, 1969 and 1976.
| All Areas | Northeast | North Central | South | West | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Reimbursed Service | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 |
| White | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 435 | 561 | 445 | 597 | 407 | 524 | 433 | 554 | 521 | 626 |
| Hospital Insurance | 212 | 233 | 189 | 219 | 224 | 244 | 231 | 251 | 215 | 220 |
| Inpatient Hospital Services | 208 | 231 | 184 | 216 | 220 | 243 | 228 | 249 | 209 | 218 |
| Skilled Nursing Facility Services | 20 | 13 | 19 | 15 | 17 | 12 | 18 | 9 | 36 | 21 |
| Home Health Agency Services | 10 | 18 | 13 | 26 | 8 | 13 | 7 | 15 | 13 | 18 |
| Supplementary Medical Insurance | 434 | 569 | 444 | 601 | 397 | 523 | 428 | 557 | 521 | 631 |
| Physician and Other Medical Services | 425 | 553 | 431 | 577 | 389 | 508 | 421 | 545 | 512 | 617 |
| Outpatient Services | 84 | 194 | 102 | 238 | 73 | 181 | 67 | 157 | 102 | 219 |
| Home Health Agency Services | 7 | 8 | 11 | 10 | 5 | 6 | 6 | 9 | 10 | 8 |
| All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 333 | 495 | 396 | 595 | 393 | 548 | 294 | 455 | 456 | 582 |
| Hospital Insurance | 167 | 196 | 164 | 204 | 194 | 232 | 164 | 195 | 174 | 176 |
| Inpatient Hospital Services | 165 | 193 | 160 | 200 | 191 | 229 | 162 | 192 | 169 | 174 |
| Skilled Nursing Facility Services | 9 | 8 | 9 | 7 | 13 | 10 | 7 | 6 | 20 | 15 |
| Home Health Agency Services | 9 | 20 | 14 | 26 | 13 | 26 | 7 | 18 | 10 | 18 |
| Supplementary Medical Insurance | 341 | 518 | 404 | 610 | 392 | 563 | 294 | 468 | 468 | 595 |
| Physician and Other Medical Services | 309 | 476 | 356 | 546 | 336 | 502 | 269 | 435 | 451 | 561 |
| Outpatient Services | 103 | 225 | 151 | 312 | 152 | 282 | 76 | 185 | 123 | 240 |
| Home Health Agency Services | 8 | 12 | 10 | 11 | 10 | 11 | 7 | 13 | 8 | 7 |
| Ratio: White to All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.31 | 1.13 | 1.12 | 1.00 | 1.04 | .96 | 1.47 | 1.22 | 1.14 | 1.07 |
| Hospital Insurance | 1.27 | 1.19 | 1.15 | 1.07 | 1.15 | 1.05 | 1.41 | 1.29 | 1.24 | 1.25 |
| Inpatient Hospital Services | 1.27 | 1.19 | 1.15 | 1.08 | 1.15 | 1.06 | 1.41 | 1.30 | 1.24 | 1.25 |
| Skilled Nursing Facility Services | 2.23 | 1.72 | 2.11 | 2.14 | 1.31 | 1.20 | 2.57 | 1.50 | 1.80 | 1.41 |
| Home Health Agency Services | 1.08 | .88 | .93 | 1.00 | .62 | .48 | 1.00 | .87 | 1.30 | .99 |
| Supplementary Medical Insurance | 1.28 | 1.10 | 1.10 | .99 | 1.01 | .93 | 1.46 | 1.19 | 1.11 | 1.06 |
| Physician and Other Medical Services | 1.38 | 1.16 | 1.21 | 1.06 | 1.16 | 1.01 | 1.57 | 1.25 | 1.14 | 1.10 |
| Outpatient Services | .81 | .86 | .68 | .76 | .48 | .64 | .88 | .85 | .83 | .91 |
| Home Health Agency Services | .94 | .72 | 1.10 | .91 | .50 | .53 | .86 | .71 | 1.25 | 1.10 |
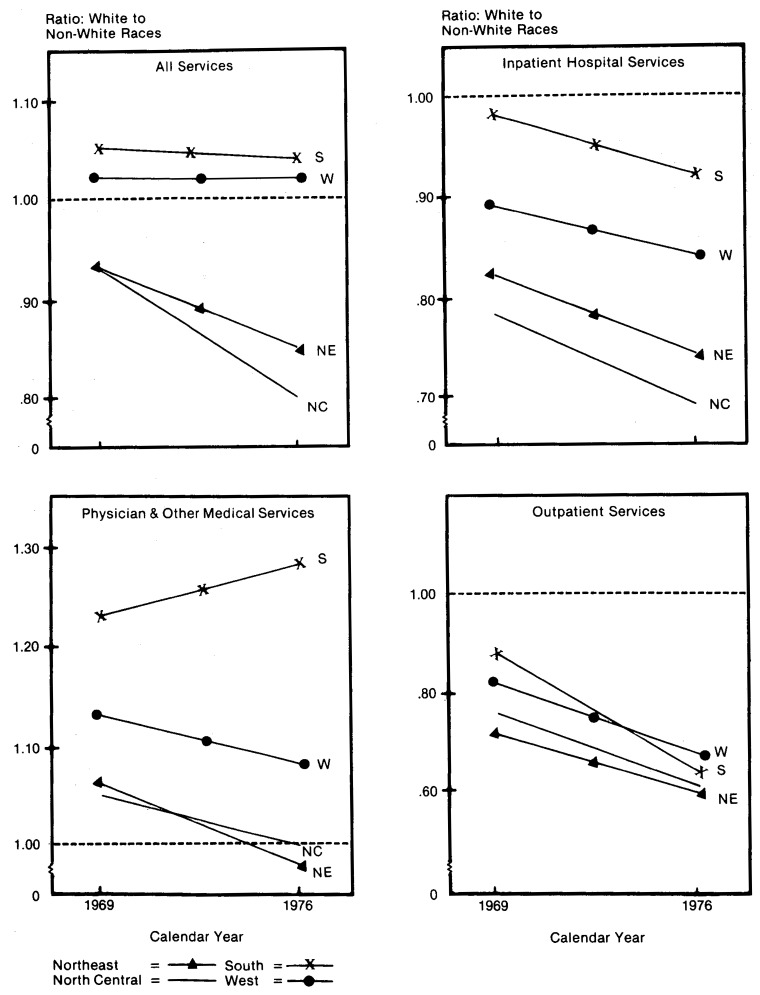
Figure 3. Selected Services under Medicare, Persons Served Per 1,000 Enrolled: Ratio of White to Non-White Races by Census Region, 1969 and 1976.
For inpatient hospital services, the major HI service, there was a decrease in D(PSM/E) in three regions and virtually no change in the West. However, in 1976, in all four regions the rates of whites still exceeded that of non-whites. The greatest disparities were in the South, 1.30, and the West, 1.25.
For the major SMI service, physicians' services, there were decreases in all regions in D(PSM/E). By 1976, D(PSM/E) in the South was 1.25, the largest contributor to racial disparity. For outpatient services, D(PSM/E) showed higher proportions of non-whites in all four regions in 1969 and increases in 1976 in all regions except the South where D(PSM/E) fell slightly from .88 to .85.
Thus, though regional disparities have diminished, for the major services (inpatient hospital and physician) the South continues to exhibit the highest D(PSM/E) showing proportionally higher rates by whites. This is particularly important because 56 percent of the nation's aged non-whites live in the South.
Reimbursement Per Person Served (R/PS)
HI and/or SMI Services
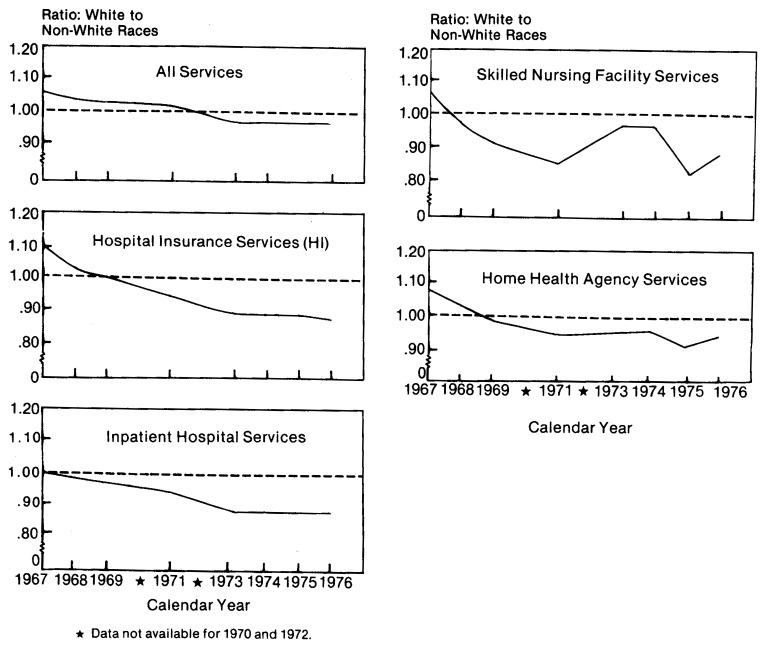
For all Medicare services, R/PS in 1967 for white persons was $593 and $557 for non-whites or D(R/PS) was 1.06 (Table 7 and Figure 4). By 1971, D(R/PS) fell to 1.02 and since 1973, the disparity leveled off at .97. Thus, once non-whites exceeded the deductible, their R/PS for HI and/or SMI was greater than that of whites. However, as will be shown, R/PS varies by type of service.
Table 7. Use of Medicare Services by the Aged: Reimbursement Per Person Served by Type of Service and Race, 1967-19761.
| Type of Reimbursed Service | 1967 | 1968 | 1969 | 1971 | 1973 | 1974 | 1975 | 1976 |
|---|---|---|---|---|---|---|---|---|
| White | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $593 | $670 | $697 | $781 | $850 | $917 | $1,053 | $1,212 |
| Hospital Insurance | 751 | 933 | 1,019 | 1,208 | 1,363 | 1,530 | 1,839 | 2,155 |
| Inpatient Hospital Services | 737 | 869 | 950 | 1,169 | 1,323 | 1,480 | 1,783 | 2,085 |
| Skilled Nursing Facility Services | 773 | 815 | 785 | 688 | 712 | 835 | 888 | 984 |
| Home Health Agency Services | 205 | 236 | 261 | 250 | 274 | 344 | 410 | 471 |
| Supplementary Medical Insurance | 196 | 205 | 211 | 221 | 237 | 265 | 297 | 334 |
| Physician and Other Medical Services | 192 | 199 | 203 | 212 | 224 | 247 | 270 | 299 |
| Outpatient Services | 29 | 39 | 47 | 56 | 66 | 77 | 95 | 112 |
| Home Health Agency Services | 144 | 162 | 176 | 157 | 222 | 294 | 336 | 378 |
| All Other Races | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $557 | $645 | $677 | $762 | $861 | $942 | $1,081 | $1,247 |
| Hospital Insurance | 682 | 907 | 1,019 | 1,277 | 1,486 | 1,716 | 2,070 | 2,438 |
| Inpatient Hospital Services | 739 | 890 | 975 | 1,247 | 1,458 | 1,677 | 2,015 | 2,379 |
| Skilled Nursing Facility Services | 721 | 837 | 849 | 803 | 776 | 863 | 1,069 | 1,102 |
| Home Health Agency Services | 191 | 229 | 266 | 266 | 289 | 363 | 449 | 503 |
| Supplementary Medical Insurance | 168 | 178 | 182 | 187 | 215 | 246 | 286 | 326 |
| Physician and Other Medical Services | 164 | 173 | 177 | 177 | 194 | 215 | 239 | 263 |
| Outpatient Services | 38 | 50 | 58 | 72 | 90 | 113 | 141 | 169 |
| Home Health Agency Services | 158 | 181 | 206 | 195 | 258 | 315 | 436 | 458 |
| Ratio: White to All Other Races | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.06 | 1.04 | 1.03 | 1.02 | .99 | .97 | .97 | .97 |
| Hospital Insurance | 1.10 | 1.03 | 1.00 | .95 | .92 | .89 | .89 | .88 |
| Inpatient Hospital Services | 1.00 | .98 | .97 | .94 | .91 | .88 | .88 | .88 |
| Skilled Nursing Facility Services | 1.07 | .97 | .92 | .86 | .92 | .97 | .83 | .89 |
| Home Health Agency Services | 1.08 | 1.03 | .98 | .94 | .95 | .95 | .91 | .94 |
| Supplementary Medical Insurance | 1.17 | 1.15 | 1.15 | 1.18 | 1.11 | 1.08 | 1.04 | 1.03 |
| Physician and Other Medical Services | 1.17 | 1.15 | 1.15 | 1.20 | 1.15 | 1.15 | 1.13 | 1.14 |
| Outpatient Services | .75 | .77 | .82 | .78 | .73 | .68 | .67 | .66 |
| Home Health Agency Services | .91 | .90 | .85 | .81 | .86 | .93 | .77 | .82 |
Data for 1970 and 1972 not available.
Figure 4. Use of All and HI Services by the Aged, Reimbursement Per Person Served: Ratio of White to Non-White Races, 1967-1976.
HI Services
Changes in the D(R/PS) for each of the three HI benefits—inpatient, SNF, and HHA services—were similar. In 1967, D(R/PS) was 1.00 for inpatient hospital services. By 1974, D(R/PS) fell to .88 and then leveled off for the next two years. Data for aged Medicare beneficiaries discharged from short-stay hospitals in 1976 provide an explanation of the higher average reimbursement of non-whites.3 Non-whites averaged 13 percent more covered days per discharge than whites (12.4 vs. 11.0). Another possible factor, the difference by race in reimbursements per covered day, was negligible. Non-whites during 1976 averaged $128 per day in reimbursements and whites $126 per day.
For SNF and HHA services the D(R/PS) was 1.07 and 1.08 in 1967. Two years later the D(R/PS) fell slightly below 1.00 for both services and has remained below 1.00. Based on discharge data from SNFs, aged non-whites had higher average reimbursements per covered day and higher average number of covered days per discharge. In 1976, reimbursements per day were $34.57 for non-whites, 8 percent more than the $32.13 average for whites (Skilled Nursing Facility Utilization, 1976). Covered days per discharge were 9 percent higher for non-whites, 28.8 days, contrasted with 26.5 days for whites.
For HHA services, the D(R/PS) was .94 in 1976. This difference probably resulted because non-whites had a higher average number of HHA visits per person served and higher reimbursements per visit. In 1976 non-whites averaged 23.8 visits per person served or 7 percent more than the 22.3 visits of whites.4 Reimbursements per visit were 8 percent higher for non-whites than whites, $23.26 and $21.54, respectively.
SMI Services
For supplementary medical insurance, D(R/PS) ranged from 1.15 to 1.18 in the 1967-1971 period and then fell to 1.03 in 1976 (Table 7 and Figure 5). For physicians' and other medical services, D(R/PS) averaged about 1.15 for the 1967-1976 period. As previously noted, D(R/PS) for physicians' services was higher for whites because their reimbursements per service were higher. For outpatient services, D(R/PS) has been stable at about .67. Medicare data on hospital outpatient services help explain why D(R/PS) indicated non-whites received higher reimbursements than whites for outpatient services. As noted earlier, in 1975, average covered charges of blacks using hospital outpatient services were nearly 50 percent higher than those of whites (Table 3). The major service accounting for this difference in average covered charges was hospital outpatient clinic services. In 1975, such services were 31 percent of all hospital outpatient charges for blacks but only 8 percent for whites. In addition, average covered charges per hospital outpatient clinic user for blacks exceeded whites, $97 to $80. The greater average number of visits per user by blacks accounted for this difference. Blacks averaged 5.2 hospital outpatient clinic visits per user in 1975 compared to 4.2 visits by whites.
Figure 5. SMI Services under Medicare, Reimbursement per Person Served: Ratio of White to Non-White Races, 1967-1976.
For HHA services under the SMI program, D(R/PS) was also consistently below 1.00 over the 1967-1976 period—showing higher average reimbursements for non-whites.
Regional Analysis
The pattern in the D(R/PS) was mixed in the four regions for HI and/or SMI services (Table 8 and Figure 6). In the Northeast and North Central States the D(R/PS) declined from .93 to .85 and .93 to .80, respectively. In the South and the West, D(R/PS) was 1.04 and 1.02 in 1976, virtually unchanged since 1969. For inpatient hospital services, the D(R/PS) in all four regions were below 1.00 in 1969 and declined even further in 1976—ranging from .92 in the South to .69 in the North Central States.
Table 8. Use of Medicare Services by the Aged: Reimbursement Per Person Served by Type of Service, Race, and Religion, 1969 and 1976.
| All Areas | Northeast | North Central | South | West | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Reimbursed Service | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 |
| White | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $ 697 | $1,212 | $ 734 | $1,319 | $715 | $1,243 | $628 | $1,091 | $ 701 | $1,210 |
| Hospital Insurance | 1,019 | 2,155 | 1,237 | 2,667 | 979 | 2,064 | 813 | 1,753 | 1,153 | 2,389 |
| Inpatient Hospital Services | 950 | 2,085 | 1,158 | 2,568 | 925 | 2,014 | 763 | 1,696 | 1,039 | 2,305 |
| Skilled Nursing Facility Services | 785 | 984 | 899 | 1,254 | 798 | 960 | 683 | 895 | 750 | 768 |
| Home Health Agency Services | 261 | 471 | 226 | 422 | 229 | 380 | 282 | 612 | 337 | 453 |
| Supplementary Medical Insurance | 211 | 334 | 217 | 354 | 189 | 295 | 206 | 319 | 234 | 387 |
| Physician and Other Medical Services | 203 | 299 | 210 | 314 | 183 | 265 | 200 | 291 | 220 | 340 |
| Outpatient Services | 47 | 112 | 41 | 119 | 41 | 98 | 45 | 93 | 69 | 143 |
| Home Health Agency Services | 176 | 378 | 160 | 323 | 164 | 355 | 175 | 439 | 218 | 364 |
| All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $ 677 | $1,247 | $ 791 | $1,544 | $ 769 | $1,552 | $597 | $1,053 | $ 688 | $1,185 |
| Hospital Insurance | 1,019 | 2,438 | 1,458 | 3,526 | 1,234 | 2,998 | 806 | 1,887 | 1,270 | 2,818 |
| Inpatient Hospital Services | 975 | 2,379 | 1,419 | 3,471 | 1,183 | 2,934 | 775 | 1,834 | 1,166 | 2,729 |
| Skilled Nursing Facility Services | 849 | 1,102 | 892 | 1,580 | 856 | 1,090 | 751 | 1,011 | 1,012 | 982 |
| Home Health Agency Services | 266 | 503 | 251 | 465 | 218 | 470 | 272 | 549 | 361 | 441 |
| Supplementary Medical Insurance | 182 | 326 | 201 | 395 | 175 | 326 | 167 | 283 | 214 | 387 |
| Physician and Other Medical Services | 177 | 263 | 198 | 320 | 174 | 265 | 163 | 228 | 194 | 315 |
| Outpatient Services | 58 | 169 | 57 | 198 | 54 | 160 | 52 | 146 | 84 | 212 |
| Home Health Agency Services | 206 | 458 | 229 | 391 | 191 | 448 | 192 | 481 | 273 | 399 |
| Ratio: White to All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.03 | .97 | .93 | .85 | .93 | .80 | 1.05 | 1.04 | 1.02 | 1.02 |
| Hospital Insurance | 1.00 | .88 | .85 | .76 | .79 | .69 | 1.01 | .93 | .91 | .85 |
| Inpatient Hospital Services | .97 | .88 | .82 | .74 | .78 | .69 | .98 | .92 | .89 | .84 |
| Skilled Nursing Facility Services | .92 | .89 | 1.01 | .79 | .93 | .88 | .91 | .89 | .74 | .78 |
| Home Health Agency Services | .98 | .94 | .90 | .91 | 1.05 | .81 | 1.04 | 1.11 | .93 | 1.03 |
| Supplementary Medical Insurance | 1.15 | 1.03 | 1.08 | .90 | 1.08 | .90 | 1.23 | 1.13 | 1.09 | 1.00 |
| Physician and Other Medical Services | 1.15 | 1.14 | 1.06 | .98 | 1.05 | 1.00 | 1.23 | 1.28 | 1.13 | 1.08 |
| Outpatient Services | .82 | .66 | .72 | .60 | .76 | .61 | .87 | .64 | .82 | .68 |
| Home Health Agency Services | .85 | .82 | .70 | .83 | .86 | .79 | .91 | .91 | .80 | .91 |
Figure 6. Selected Services under Medicare, Reimbursement per Person Served: Ratio of White to Non-White Races by Census Region, 1969 and 1976.
In 1976, the D(R/PS) for physician services in the South was 1.28, in the West, 1.08, and about 1.00 in the other regions. In 1976 in all four regions the D(R/PS) for outpatient services varied from .60 to .68. This showed even greater average reimbursements for non-whites than in 1969; the overall D(R/PS) in 1969 was .82 and fell to .66 in 1976.
Reimbursement Per Enrollee (R/E)
HI and/or SMI Services
As explained earlier, R/E is considered a summary measure of the combined effect of PS/E and R/PS. It is thus the best single measure of the equity in the use of Medicare benefits because it combines the joint effect of access to Medicare reimbursements and the amount of reimbursement. For HI and SMI services there was a considerable decrease in D(R/E) from 1.53 in 1967 to 1.10 in 1976 (Table 9 and Figure 7).
Table 9. Use of Medicare Services by the Aged: Reimbursement Per Enrollee by Type of Service and Race, 1967-19761.
| Type of Reimbursed Service | 1967 | 1968 | 1969 | 1971 | 1973 | 1974 | 1975 | 1976 |
|---|---|---|---|---|---|---|---|---|
| White | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $222.47 | $272.63 | $303.43 | $337.03 | $402.49 | $459.49 | $563.01 | $680.49 |
| Hospital Insurance | 155.09 | 194.10 | 216.36 | 261.50 | 296.79 | 333.78 | 412.67 | 502.47 |
| Inpatient Hospital Services | 138.92 | 175.00 | 197.91 | 251.34 | 285.56 | 319.64 | 396.14 | 481.55 |
| Skilled Nursing Facility Services | 14.48 | 17.03 | 15.97 | 8.16 | 8.55 | 10.11 | 10.57 | 12.69 |
| Home Health Agency Services | 1.34 | 1.97 | 2.48 | 1.99 | 2.68 | 3.99 | 5.94 | 8.28 |
| Supplementary Medical Insurance | 72.96 | 82.70 | 91.47 | 101.69 | 112.59 | 133.72 | 160.59 | 190.26 |
| Physician and Other Medical Services | 70.36 | 78.76 | 86.22 | 95.11 | 103.44 | 121.00 | 142.11 | 165.48 |
| Outpatient Services | 2.03 | 2.81 | 3.96 | 5.96 | 8.12 | 11.05 | 16.07 | 21.65 |
| Home Health Agency Services | .93 | 1.15 | 1.30 | .62 | 1.04 | 1.65 | 2.39 | 3.13 |
| All Other Races | ||||||||
| Hospital insurance and/or Supplementary Medical Insurance | $145.13 | $194.68 | $225.31 | $268.55 | $342.46 | $406.01 | $504.68 | $617.20 |
| Hospital Insurance | 108.62 | 146.59 | 170.43 | 221.92 | 267.72 | 313.09 | 388.31 | 478.36 |
| Inpatient Hospital Services | 102.25 | 136.98 | 160.35 | 215.20 | 259.65 | 302.15 | 373.38 | 460.10 |
| Skilled Nursing Facility Services | 4.75 | 7.84 | 7.75 | 4.42 | 4.89 | 5.78 | 7.49 | 8.27 |
| Home Health Agency Services | 1.00 | 1.60 | 2.33 | 2.29 | 3.27 | 5.04 | 7.55 | 10.10 |
| Supplementary Medical Insurance | 44.11 | 54.20 | 62.13 | 72.62 | 88.47 | 110.07 | 139.57 | 168.59 |
| Physician and Other Medical Services | 40.45 | 48.44 | 54.57 | 61.92 | 73.06 | 87.86 | 107.40 | 125.36 |
| Outpatient Services | 3.00 | 4.50 | 5.93 | 9.65 | 13.73 | 19.73 | 28.09 | 37.96 |
| Home Health Agency Services | .90 | 1.23 | 1.63 | 1.05 | 1.68 | 2.49 | 4.10 | 5.27 |
| Ratio: White to All Other Races | ||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.53 | 1.40 | 1.35 | 1.25 | 1.18 | 1.13 | 1.12 | 1.10 |
| Hospital Insurance | 1.43 | 1.32 | 1.27 | 1.18 | 1.11 | 1.07 | 1.06 | 1.05 |
| Inpatient Hospital Services | 1.36 | 1.28 | 1.23 | 1.17 | 1.10 | 1.06 | 1.06 | 1.05 |
| Skilled Nursing Facility Services | 3.05 | 2.17 | 2.06 | 1.85 | 1.75 | 1.75 | 1.41 | 1.53 |
| Home Health Agency Services | 1.34 | 1.23 | 1.06 | .87 | .82 | .79 | .79 | .82 |
| Supplementary Medical Insurance | 1.65 | 1.53 | 1.47 | 1.40 | 1.27 | 1.21 | 1.15 | 1.13 |
| Physician and Other Medical Services | 1.74 | 1.63 | 1.58 | 1.54 | 1.42 | 1.38 | 1.32 | 1.32 |
| Outpatient Services | .68 | .62 | .67 | .62 | .59 | .56 | .57 | .57 |
| Home Health Agency Services | 1.03 | .93 | .80 | .59 | .62 | .66 | .58 | .59 |
Data for 1970 and 1972 not available.
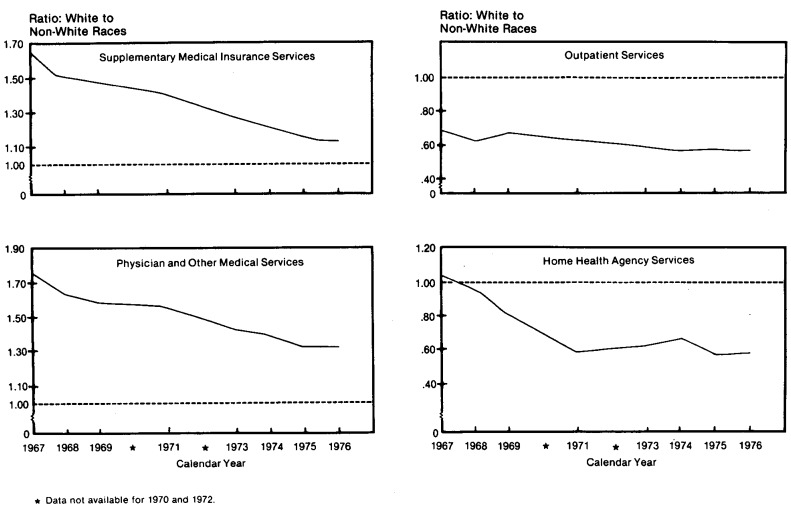
Figure 7. Use of All and HI Services by the Aged, Reimbursement per Enrollee: Ratio of White to Non-White Races, 1967-1976.
HI Services
HI services also showed a steady decrease: D(R/E) fell from 1.43 to only 1.05 in the same period. Inpatient hospital services, the major HI component, had a similar pattern, falling from 1.36 to 1.05. Similar changes in inpatient hospital disparities were found in data of aged Medicare enrollees discharged from short-stay hospitals in 1967 and 1976 (Medicare: Health Insurance for the Aged, 1967). The ratio of whites to non-whites in reimbursement per discharged enrollee is the product of total days of care per discharged enrollee and reimbursement per total days of care as shown in the following table.
Discharge Rates of Whites to Non-Whites, 1967 and 1976.
| Discharged Enrollees | 1967 | 1976 |
|---|---|---|
| Ratio of Whites to Non-whites: | ||
| Total Days of Care Per Enrollee | 1.29 | 1.10 |
| Reimbursements Per Total Days of Care | 1.06 | .98 |
| Reimbursement Per Enrollee | 1.37 | 1.08 |
Thus, the ratio of whites to non-whites for reimbursement per discharged enrollee fell from 1.37 in 1967 to 1.08 in 1976. This is comparable to the decline in the D(R/E) for inpatient hospital services of 1.36 to 1.05.
In 1976, total days of care per 1,000 enrolled among whites, 3,664, was greater than the comparable figures for non-whites, 3,343 per 1,000 (1.10 in the text table). To explain this disparity, it is important to note that the average length of stay of whites was less, 11.0 days, than that of non-whites, 12.4 days, but this was more than offset by a higher discharge rate per 1,000 enrolled: 333 for whites compared to 270 for non-whites. Thus, while whites have a higher frequency of hospital episodes than non-whites (1.23) their stays in the hospital are shorter (.89).
For skilled nursing facility services the D(R/E) was 3.05 in 1967 and fell to 1.53 in 1976. Though a relatively little used service, it was the service with the greatest disparity showing higher average reimbursements to whites.
For home health agency services D(R/E) fell from 1.34 in 1967 to .82 in 1976. Thus, among HI benefits in 1976, only the D(R/E) for home health agency services showed higher reimbursements to non-whites.
SMI Services
Like HI services, the D(R/E) for all SMI services combined, showed whites receiving higher average reimbursements, though the disparity declined each year (Table 9 and Figure 8). D(R/E) fell from 1.65 in 1967 to 1.13 by 1976. Most of this improvement was for services of physicians and other suppliers: D(R/E) fell from 1.74 in 1967 to 1.32 in 1976. This service kept D(R/E) higher for whites for total SMI services, though the other two SMI services were higher for non-whites. Outpatient D(R/E) fell from .68 to .57 beetween 1967 and 1976 and D(R/E) for home health services fell from 1.03 to .59 in the same period.
Figure 8. Use of SMI Services by the Aged, Reimbursement per Enrollee: Ratio of White to Non-White Races, 1967-1976.
Regional Analysis
For HI and/or SMI services there were decreases in every region in the D(R/E) between 1969 and 1976 (Table 10 and Figure 9). In 1976 in the South, the D(R/E) was 1.26 and accounted for most of the disparity between races in the nation. In the West, the comparable figure was 1.10. In the other two regions, D(R/E) was .86 in the Northeast and .77 in the North Central region.
Table 10. Use of Medicare Services by the Aged: Reimbursement Per Enrollee by Type of Service, Race, and Region, 1969 and 1976.
| All Areas | Northeast | North Central | South | West | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Reimbursed Service | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 | 1969 | 1976 |
| White | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $303.43 | $680.49 | $326.48 | $787.89 | $291.15 | $651.18 | $271.93 | $604.81 | $365.25 | $756.82 |
| Hospital Insurance | 216.36 | 502.47 | 233.55 | 584.79 | 219.05 | 504.46 | 187.81 | 439.72 | 247.81 | 525.78 |
| Inpatient Hospital Services | 197.91 | 481.55 | 213.35 | 555.25 | 203.67 | 488.48 | 173.95 | 422.47 | 216.95 | 501.86 |
| Skilled Nursing Facility Services | 15.97 | 12.69 | 17.25 | 18.56 | 13.56 | 11.14 | 12.01 | 7.97 | 26.63 | 15.75 |
| Home Health Agency Services | 2.48 | 8.28 | 2.94 | 10.94 | 1.82 | 4.78 | 1.84 | 9.37 | 4.23 | 8.11 |
| Supplementary Medical Insurance | 91.47 | 190.26 | 96.21 | 212.85 | 74.94 | 154.34 | 88.07 | 117.37 | 121.99 | 243.94 |
| Physician and Other Medical Services | 86.22 | 165.48 | 90.31 | 181.21 | 71.11 | 134.60 | 84.09 | 158.74 | 112.83 | 209.66 |
| Outpatient Services | 3.96 | 21.65 | 4.23 | 28.36 | 2.98 | 17.64 | 3.02 | 14.61 | 7.06 | 31.41 |
| Home Health Agency Services | 1.30 | 3.13 | 1.67 | 3.29 | .85 | 2.10 | .97 | 3.99 | 2.10 | 2.88 |
| All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | $225.31 | $617.20 | $312.89 | $918.41 | $302.05 | $850.35 | $175.72 | $478.87 | $313.38 | $690.07 |
| Hospital Insurance | 170.43 | 478.36 | 239.17 | 718.92 | 239.82 | 696.38 | 131.92 | 367.60 | 221.23 | 495.89 |
| Inpatient Hospital Services | 160.35 | 460.10 | 227.57 | 694.98 | 225.81 | 673.13 | 125.20 | 352.35 | 197.47 | 473.52 |
| Skilled Nursing Facility Services | 7.75 | 8.27 | 8.21 | 11.53 | 11.28 | 10.90 | 4.89 | 5.56 | 20.12 | 14.24 |
| Home Health Agency Services | 2.33 | 10.10 | 3.39 | 12.23 | 2.73 | 12.31 | 1.83 | 9.61 | 3.64 | 7.98 |
| Supplementary Medical Insurance | 62.13 | 168.59 | 81.17 | 240.87 | 68.69 | 183.47 | 49.27 | 132.22 | 100.29 | 230.29 |
| Physician and Other Medical Services | 54.57 | 125.36 | 70.28 | 174.84 | 58.60 | 133.18 | 43.97 | 99.16 | 87.76 | 176.67 |
| Outpatient Services | 5.93 | 37.96 | 8.62 | 61.76 | 8.21 | 45.29 | 3.96 | 26.88 | 10.37 | 50.68 |
| Home Health Agency Services | 1.63 | 5.27 | 2.27 | 4.26 | 1.89 | 4.98 | 1.34 | 6.21 | 2.17 | 2.88 |
| Ratio: White to All Other Races | ||||||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.35 | 1.10 | 1.04 | .86 | .96 | .77 | 1.55 | 1.26 | 1.17 | 1.10 |
| Hospital Insurance | 1.27 | 1.05 | .98 | .81 | .91 | .72 | 1.42 | 1.20 | 1.12 | 1.06 |
| Inpatient Hospital Services | 1.23 | 1.05 | .94 | .80 | .90 | .73 | 1.39 | 1.20 | 1.10 | 1.06 |
| Skilled Nursing Facility Services | 2.06 | 1.53 | 2.10 | 1.61 | 1.20 | 1.02 | 2.46 | 1.43 | 1.32 | 1.11 |
| Home Health Agency Services | 1.06 | .82 | .87 | .89 | .67 | .39 | 1.01 | .98 | 1.16 | 1.02 |
| Supplementary Medical Insurance | 1.47 | 1.13 | 1.19 | .88 | 1.09 | .84 | 1.79 | .89 | 1.22 | 1.06 |
| Physician and Other Medical Services | 1.58 | 1.32 | 1.29 | 1.04 | 1.21 | 1.01 | 1.91 | 1.60 | 1.29 | 1.19 |
| Outpatient Services | .67 | .57 | .49 | .46 | .36 | .39 | .76 | .54 | .68 | .62 |
| Home Health Agency Services | .80 | .59 | .74 | .77 | .45 | .42 | .72 | .64 | .97 | 1.00 |
Figure 9. Selected Services under Medicare, Reimbursement Per Enrollee: Ratio of White to Non-White Races by Census Region, 1969 and 1976.
For inpatient hospital services in 1976, the D(R/E) was 1.20 in the South, the only region where average reimbursements were markedly higher for whites. The West registered a D(R/E) of 1.06 while the D(R/E) was .80 in the Northeast and in the North Central States, .73.
By 1976 there were sizeable decreases in D(R/E) for physicians' services in every region. In the Northeast and North Central States D(R/E) was nearly equal to 1.00 or racial equity. However, in the South, D(R/E) was 1.60 and in the West, 1.19. For outpatient services D(R/E) ranged from .39 in the North Central region to .62 in the West, strongly showing higher average reimbursements for non-whites.
Summary and Conclusions
In this section, the three measures used in this article are contrasted for the nation for 1967 and 1976 (Table 11). The three measures are further contrasted by region (Table 12). First, some conclusions are made about what has caused changes in disparities by race in each of the three measures in the 1967-1976 period. The conclusions are, of necessity, conjectural because the data used were designed neither to provide an explanation of what caused change nor to predict future changes (Link, unpublished).5
Table 11. Ratio of White to All Other Races: Persons Served Per Enrollee, Reimbursement Per Person Served, and Per Enrollee, by Type of Service, 1967 and 1976.
| Type of Reimbursed Service | 1967 | 1976 | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Persons Served Per Enrollee | Reimbursement | Persons Served Per Enrollee | Reimbursement | |||
|
|
|
|||||
| Per Person Served | Per Enrollee | Per Person Served | Per Enrollee | |||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.44 | 1.06 | 1.53 | 1.13 | 0.97 | 1.10 |
| Hospital Insurance | 1.30 | 1.10 | 1.43 | 1.19 | .88 | 1.05 |
| Inpatient Hospital Services | 1.36 | 1.00 | 1.36 | 1.19 | .88 | 1.05 |
| Skilled Nursing Facility Services | 2.83 | 1.07 | 3.05 | 1.72 | .89 | 1.54 |
| Home Health Agency Services | 1.23 | 1.08 | 1.34 | .88 | .94 | .82 |
| Supplementary Medical Insurance | 1.41 | 1.17 | 1.65 | 1.10 | 1.03 | 1.13 |
| Physician and Other Medical Services | 1.49 | 1.17 | 1.74 | 1.16 | 1.14 | 1.32 |
| Outpatient Services | .80 | .75 | .60 | .86 | .66 | .57 |
| Home Health Agency Services | 1.14 | .91 | 1.03 | .72 | .82 | .60 |
Table 12. Ratio of White to All Other Races: Persons Served Per Enrollee, Reimbursement Per Person Served, and Per Enrollee, for Selected Services, by Region, 1969 and 1976.
| Type of Reimbursed Service | 1969 | 1976 | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Persons Served Per Enrollee | Reimbursement | Persons Served Per Enrollee | Reimbursement | |||
|
|
|
|||||
| Per Person Served | Per Enrollee | Per Person Served | Per Enrollee | |||
| All Areas | ||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.31 | 1.03 | 1.35 | 1.13 | 0.97 | 1.10 |
| Inpatient Hospital Services | 1.27 | .97 | 1.23 | 1.19 | .88 | 1.05 |
| Physician and Other Medical Services | 1.38 | 1.15 | 1.58 | 1.16 | 1.14 | 1.32 |
| Outpatient Services | .81 | .82 | .67 | .86 | .66 | .57 |
| Northeast | ||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.12 | .93 | 1.04 | 1.00 | .85 | .86 |
| Inpatient Hospital Services | 1.15 | .82 | .94 | 1.08 | .74 | .80 |
| Physician and Other Medical Services | 1.21 | 1.06 | 1.29 | 1.06 | .98 | 1.04 |
| Outpatient Services | .68 | .72 | .49 | .76 | .60 | .46 |
| North Central | ||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.04 | .93 | .96 | .96 | .80 | .77 |
| Inpatient Hospital Services | 1.15 | .78 | .90 | 1.06 | .69 | .73 |
| Physician and Other Medical Services | 1.16 | 1.05 | 1.21 | 1.01 | 1.00 | 1.01 |
| Outpatient Services | .48 | .76 | .36 | .64 | .61 | .39 |
| South | ||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.47 | 1.05 | 1.55 | 1.22 | 1.04 | 1.26 |
| Inpatient Hospital Services | 1.41 | .98 | 1.39 | 1.30 | .92 | 1.20 |
| Physician and Other Medical Services | 1.57 | 1.23 | 1.91 | 1.25 | 1.28 | 1.60 |
| Outpatient Services | .88 | .87 | .76 | .85 | .64 | .54 |
| West | ||||||
| Hospital Insurance and/or Supplementary Medical Insurance | 1.14 | 1.02 | 1.17 | 1.07 | 1.02 | 1.10 |
| Inpatient Hospital Services | 1.24 | .89 | 1.10 | 1.25 | .84 | 1.06 |
| Physician and Other Medical Services | 1.14 | 1.13 | 1.29 | 1.10 | 1.08 | 1.19 |
| Outpatient Services | .83 | .82 | .68 | .91 | .68 | .62 |
The Medicare program was partially responsible for the decreasing disparity by race among the aged for three reasons. First, the program increased access to medical care among aged persons by providing “free” hospital insurance for those entitled to social security. The program also offered voluntary supplementary medical insurance (SMI) to the aged and Medicare shared the cost of the SMI premium. Many of those unable to afford the SMI premium obtained free coverage through the State buy-in program. Second, Medicare reduced out-of-pocket medical costs by paying 80 percent of SMI reasonable charges and a substantial part of HI charges. Further, Medicaid eligibles entitled to Medicare do not have to pay their Medicare coinsurance and deductibles—these are paid by Medicaid. Third, institutional providers of medical care to Medicare enrollees are required to furnish services without discrimination. These three factors probably increased the use of medical care by non-whites more than by whites. The reason for this is: non-whites benefited more because a lower-proportion of them probably had private health insurance than whites. The State buy-in program and probably the Medicaid program has disproportionate numbers of non-white eligibles.
The Medicare program was not the only factor accounting for decreases in racial disparity. However, data of causation factors other than Medicare are not available from the Medicare statistical collection program. These factors include the civil rights movement, more positive attitudes of non-whites toward the use of medical care, and the relative increase in income among white and non-white aged. Some factors that are available but were found to be of minor importance were age and sex differences among whites and non-whites. Finally, some factors in the Medicare law are likely to continue to cause racial disparities, for example, the increasing gap between total charges and reasonable charges, regional differences in charges, and the purchase of private insurance to cover costs not covered by Medicare. Factors resulting in improvements for non-whites and for persistence of racial disparities are discussed next in detail.
First, those factors that are difficult to measure. One such factor, the civil rights movement, was at its peak during the period covered by this article. That movement probably helped the Medicare program provide services without discrimination. Another such factor may have been a change in attitude by non-whites that resulted in their increased use of health care.
A factor easier to quantify but not available from the Medicare data collection program is the relative change in the income of the two aged racial groups. According to the Census Bureau, the median family income of all non-whites relative to whites between 1967 and 1974 has varied little (U.S. Bureau of the Census, 1790-1978). In 1967 the median non-white family income was 62 percent that of whites. It rose to 64 percent in 1970 and fell back to 62 percent in 1974. Income of all persons 65 years old and over was not measured by the Census Bureau, but they did find that the proportion of aged whites and blacks below the poverty level declined. In 1969, the Census Bureau estimated that 50 percent of black persons 65 and over were below the poverty level compared to 23 percent of whites, or a ratio of 2.2 more blacks than whites. The figures for 1974 were 36 percent of blacks and 14 percent of whites, or a ratio of 2.6 more blacks than whites. This sketchy data appears to show that the relative income of aged non-whites to whites did not improve over the observation period. Therefore, it is unlikely that relative changes in income accounted for the changes in racial disparity noted in this paper.
However, Davis, in her paper, found income directly related to the use of physicians' services. This was probably reflected in the disparity by race in the use and reimbursement of physicians' services noted in the early years of the Medicare program. Link, Long, and Settle adjusted for income using 1969, 1974, and 1976 Health Interview Survey data of the National Center for Health Statistics (Link, unpublished). They found after adjusting for income that black-white disparity, as measured by the number of physician visits by the total aged population in the South, declined between 1969 and 1976. Their results are consistent with our findings of reduced D(PSM/E) in physicians' services, though we did not adjust for income.
There are other important factors with unknown effect on the relative change in the use of medical services by race. One such factor may be changes in the educational level of the aged Medicare population. (Because of high death rates the aged population changes greatly in a decade.) Other factors are the increased number of physicians and greater availability of hospital beds. Also of interest is the possible change in how whites and non-whites respond to such Medicare provisions as: the $60 deductible, the 20 percent coinsurance, and the difference between reasonable and actual charges. An example of the response to Medicare provisions is the assignment method. When a physician does not accept assignment (the reasonable charge paid by Medicare) the enrollee is liable for the difference between reasonable and total charges. In regard to accepting assignment, a higher proportion of non-whites than whites use physicians who accept assignment. For services incurred in 1975, among white aged beneficiaries, only 45 percent of covered charges were from physicians accepting assignment compared to 79.3 percent among non-whites (Ferry, 1980). Lack of similar data for other years makes it impossible to determine the effect of the assignment method on the use of physicians' services by whites and non-whites.
This article does not make adjustments for two known factors—age and sex composition—that affect disparities by race. Whites live longer than non-whites, but the median age of white enrollees 65 and over, 73.0 years, is only slightly more than that of non-whites, 72.5. Thus, adjustments for differences in age composition would account for little of the disparity by race noted here.
There is also a slightly higher proportion of aged white women enrollees, 59.5 percent, than non-white women, 56.3 percent. Though aged women have a higher PSM/E than men, adjusting for differences in sex composition would have little effect in comparing differences by race.
There are some factors that appear likely to account for the continued disparity by race found in this paper. The rise in the proportion of aged persons having private insurance supplementing Medicare probably causes whites to use more medical services. Since they have higher incomes, they are more likely to be able to afford this insurance which pays the coinsurance and perhaps the deductibles. Differences in regional prices and costs of SMI services may result in increasing the disparity by race with higher proportions of whites using services. Greater proportions of whites live in regions where prices and costs (as evidenced by regional reimbursements) are higher. Thus, whites would be more likely to exceed the SMI deductible and be reimbursed.
One final point on disparity by race: since aged non-whites are considered to be less healthy than whites, the three measures studied would logically be expected to show greater use by and higher reimbursements to non-whites because their medical needs are greater. This point was stressed in the Davis paper.
To summarize, numerous factors have probably contributed to the changes in disparity. The question of what each factor's influence has been is not answered in this paper. However, the decreases are large and likely are related to the success of the Medicare program in reducing the cost of care over the observation period.
Disparity in Persons Served Per 1,000 Enrollees D(PSM/E)
In a sense, the D(PSM/E) is an indicator of access to the Medicare reimbursement system. It represents the extent that enrollees seek care, exceed deductibles, and are reimbursed. The D(PSM/E) in hospital and physicians' services, which are the major services of entry to the health care system, shows greater use by whites (Table 11). These differences are not offset by the D(PSM/E) which shows non-whites using more of the minor services—outpatient and home health agency services. Outpatient care has been criticized by Davis and others as fragmented and impersonal. Another criticism is that using outpatient clinics for routine medical care is expensive.
Though the D(PSM/E) for physicians' services shows greater use by whites, it has decreased. Also, Figure 2 indicates this decrease in D(PSM/E) has continued year by year. Whether or not the decrease in disparity for physicians' services will continue toward equality is unknown. Reimbursement for physicians' services depends upon exceeding the deductible. Ferry, et al., have shown that regional differences in SMI reimbursements are marked and likely to continue under present Medicare reimbursement practices (Ferry, 1980). The South has a lower PSM/E than the Northeast and West. Since the majority of non-whites live in the South and if present Medicare reimbursement practices remain the same, the D(PSM/E) for physicians' services for the nation will likely continue to show higher use by whites.
Disparity in Reimbursement Per Person Served, D(R/PS)
In 1967, for every type of service, the disparities by which whites exceeded non-whites were smaller for D(R/PS) than for D(PSM/E) as shown in Table 11. Thus, once Medicare enrollees exceeded the deductible (for every service except physicians') the average reimbursements per person served (by race) were about equal. By 1976, D(R/PS) actually showed higher reimbursements for non-whites, except for physicians' services. Perhaps once non-whites exceed the deductible their poorer health requires more care and the result is higher average reimbursements. This may, for example, explain the longer hospital stays of non-whites. However, most of the decreases in the D(R/PS) for inpatient hospital services occurred between 1967 and 1973. Since then, D(R/PS) has been relatively stable. In contrast, the D(R/PS) for physicians' and other medical services has persistently shown higher average reimbursements for whites in the 1967-1976 period and has exhibited a slow and irregular decline (Figure 5).
Disparity in Reimbursement Per Enrollee, D(R/E)
The declines in the disparities in the two measures above were reflected in the D(R/E). The D(R/E) declined for every service between 1967 and 1976. By 1976, the D(R/E) for physicians' services was the major service that still showed whites receiving higher average reimbursements. Where D(R/E) still shows higher reimbursements for whites, the higher D(PSM/E) rather than the D(R/PS) accounts for most of the difference.
A Regional Summary
Between 1969 and 1976, in the Northeast and North Central States, there were decreases in both the D(PSM/E) and the D(R/PS) in inpatient hospital, and physicians' services (Table 12). As a result, in these regions, the D(R/E) in inpatient services showed higher reimbursements for non-whites. By race, reimbursements were about equal for physicians' services. The South and West experienced some decrease in both the D(PSM/E) and in the D(R/PS) for inpatient and physicians' services. However, in the South the D(R/E) was still considerably higher for whites for both services, and in the West for physicians' services. The South, where over half the non-white aged live, seems to be the largest contributor to disparities in terms of the three measures, but even here disparity by race has diminished markedly over time.
In conclusion, while considerable decreases in the three measures have occurred since the Davis study, the D(PSM/E) still shows higher proportions of white persons served. Specifically, lower access to physicians and hospitals by non-whites persist, especially in the South. However, once non-whites meet the deductible, the D(R/PS) is favorable for all services except physicians' services.
Acknowledgments
The authors would like to thank Judith Lave for her numerous reviews of this paper and for her valuable suggestions concerning the interpretation of the findings.
Footnotes
This 5 percent sample represents the same persons as the 5 percent sample used to generate the data used in this study. The difference is that the hospital outpatient services data base is a separate record providing unique information on covered hospital outpatient services.
Unpublished data from a one percent sample of beneficiaries. Data are based on bills submitted for services of physicians.
Unpublished data from 1976 Medicare Hospital Stay Record Controls, a 20 percent sample of short-stay hospital covered discharges.
Unpublished data of a 40 percent sample of enrollees. The source of the data are billing forms from home health agencies.
For another discussion of these issues see Link, Charles R., Stephen H. Long, and Russell F. Settle, “Equity and the Utilization of Health Care Services by the Medicare Elderly,” forthcoming in the Journal of Human Resources. This work was funded under HCFA Grant #18-19-97162/2, and was provided to the authors in unpublished form.
References
- Davis Karen. Equal Treatment and Unequal Benefits: The Medicare Program. Milbank Memorial Fund Quarterly: Health and Society. 1975 Fall; [PubMed] [Google Scholar]
- Ferry Thomas P, Gornick Marian, Newton Marilyn, Hackerman Carl. Health Care Financing Review. Health Care Financing Administration; Winter. 1980. Physicians' Charges Under Medicare: Assignment Rates and Beneficiary Liability. [PMC free article] [PubMed] [Google Scholar]
- Health Care Financing Administration. Medicare: Health Insurance for the Aged and Disabled, 1973-74. Washington, D.C.: 1978. Section 1.2, Summary. [Google Scholar]
- Health Care Financing Administration. Medicare: Health Insurance for the Aged and Disabled, 1976. Section 2, Enrollment, in press. [Google Scholar]
- Health Care Financing Administration. Medicare: Health Insurance for the Aged and Disabled, 1978. Section 1.1, Reimbursement by State and County. [Google Scholar]
- Link Charles R, Long Stephen H, Settle Russell F. The Journal of Human Resources. University of Wisconsin Press; Equity and the Utilization of Health Care Services by the Medicare Elderly. accepted for publication. [PubMed] [Google Scholar]
- Loewenstein Regina. Social Security Bulletin. Dept. of Health, Education, and Welfare, Social Security Administration; Apr, 1971. Early Effects of Medicare on the Health Care of the Aged. [Google Scholar]
- Moskowitz Edwin, Mitchell Robert. Supplementary Medical Insurance: Utilization and Charges for the Aged, 1974. Current Medicare Survey Report. 1978 Jun; [PubMed] [Google Scholar]
- Skilled Nursing Facility Utilization, 1976, Health Care Financing Administration, Office of Research, Demonstrations and Statistics, (in preparation).
- Social Security Administration, Office of Research and Statistics. Medicare: Health Insurance for the Aged, 1967. Short-Stay Hospital Utilization; Washington, D.C.: 1975. Section 4.1. [Google Scholar]
- The Social Security Act, Title XVIII, Section 1811.
- U.S. Bureau of Census. Census of Population: 1970 Detailed Characteristics, Final Report, PC(1)-D-1, United States Summary. Table 270. [Google Scholar]
- U.S. Bureau of the Census. (Special Studies Series P-23).The Social and Economic Status of the Black Population in the United States: An Historical View, 1790-1978 Current Population Reports. (No. 80) [Google Scholar]
- U.S. Senate Committee on Interior and Insular Affairs, Indian Health Care Improvement Act, May 13, 1975, pgs. 37 and 128.