Abstract
Since the beginning of the Medicare program in July 1966, the rate of hospitalizations for persons age 65 and over has risen steadily. The rate grew more for the aged than for younger age groups. Because of concern about the appropriateness and cost of hospital care, this article examines the increase in hospitalizations for the aged and attempts to identify factors that may explain why the discharge rate rose more for the aged than for younger persons.
The article shows that most of the increase in the discharge rate among the aged was associated with an increase in the percentage of persons using the hospital rather than with an increase in rate of multiple hospitalizations. There was also a large increase in the rate of hospital stays of short duration. Examination of changes in diagnostic and surgical case-mix showed that there was a large increase in vascular and cardiac surgeries. Changes in demographic composition and insurance coverage did not help explain the difference in the rate of growth of hospitalizations by age group.
The increase in the rate of the aged being cared for in the hospital raises the question of the necessity and quality of the care they receive. Additional studies should focus on the nature and appropriateness of the hospital services rendered to the elderly.
Introduction
Since the beginning of the Medicare program in July 1966, the rate of hospitalizations for Medicare enrollees has risen steadily. While the discharge rate (the number of discharges per 1,000 persons) for the population under age 65 grew by 11 percent from 1967 to 1979, the rate for persons age 65 and over—more than 90% of whom are Medicare enrollees—increased by 35 percent. A comparison of the proportion of the population hospitalized in each age group shows that the proportion of aged persons hospitalized annually increased more than that of younger age groups. Thus, in addition to greater increases in the discharge rate there has been a greater increase in the proportion of the aged who are exposed to the benefits and risks of hospital care. The steady but undramatic nature of the year-to-year rise in the hospital discharge rate for Medicare beneficiaries coupled with the fact that the number of days of care per 1,000 enrollees has not increased, are very likely the major reasons that the rise in the discharge rate has not received as much attention as the rise in hospital expenditures. Because of the influence of the increase in the discharge rate on expenditures and because of the questions it raises about changes in the nature of hospital care of the aged, the increase in the Medicare hospitalization rate must be examined.
An important reason to examine the rise in the Medicare discharge rate is provided by studies suggesting that some hospital admissions and days of care may be inappropriate (Zimmer, 1974, Restuccia and Holloway, 1976) and by studies finding large geographic variations in the incidence of surgery, apparently unrelated to variations in need (Lembcke, 1952; Lewis, 1969; Bunker, 1970; Wennberg and Gittlesohn, 1975).
This article focuses on trends in the discharge rate under Medicare for persons age 65 years and over and discusses certain components of the discharge rate that have played a role in the overall increase. It also explores some factors that may have influenced the discharge rate. The article examines changes in the number of persons hospitalized each year and changes in the rate of multiple stays. Then changes in the distribution of hospital stays and hospital charges by length-of-stay interval are examined. The article also focuses on trends in diagnostic and surgical case-mix and explores how the findings relate to changing patterns of medical practice. Finally, the article examines changes in hospital insurance coverage and changes in the supply of hospitals and physicians as these changes relate to the increases in the discharge rate for the aged.
Several earlier studies have analyzed aspects of the Medicare discharge rate. Pettengill (1972) studied the initial impact of Medicare on hospital use by comparing use before and after the program began. Using data from a variety of sources, he found a 5-7 percent increase in the discharge rate from the year before Medicare was implemented to the first year of the program. From 1967 to 1971, the discharge rate grew, although at a decreasing rate. The trend of slowly rising discharge rates, the author felt, may have stemmed from developments in medicine permitting treatment of disorders that could not be dealt with before. Gornick (1977) focused on geographic differences in hospital discharge rates among states using 1972-1973 data and found higher rates in rural states and greater variation in non-surgical discharges than discharges with surgery. An analysis of trends in Medicare hospital use from 1967 to 1976 (Helbing, 1980) showed higher discharge rates for men than women, and whites than non-whites (although the gap has been narrowing) and higher rates for older enrollees throughout the period.
Most studies exploring factors related to hospital use have focused on explaining cross-sectional variation across geographic areas rather than time trends. In their review of such studies Rothberg et al (1980) noted that they often arrived at contradictory results and that no study was able to explain differences in hospital use across census regions. Nevertheless, we believe that studies of cross-sectional variation at the national level have generally identified a set of variables related to hospital use despite differences in methods and units of analysis and time and population studied.1 Variables generally found positively correlated with admission or discharge rates include extent of hospital insurance coverage, hospital bed supply, age, and measures of rurality; and variables negatively correlated with admission rates include hospital occupancy and physician supply. Chiswick (1976) found a positive relation between admission rates and supply of surgeons, as opposed to other physicians. The studies did not agree on the role of race, income or the supply of nursing home beds.
The 1979 evaluation of the Professional Standards Review Organization (PSRO) program (United States Department of Health and Human Services, 1980) was one of the few studies that attempted to explain time trends rather than cross-sectional differences in hospital use. As part of an analysis of the impact of PSROs, the study examined the relationship between a number of factors and the change in discharge rates in PSRO areas in the four U.S. census regions between 1974 and 1978. However, except for a relationship between an increase in the supply of hospital beds and an increase in the discharge rate in two regions, no variable showed a consistent relationship with the change in the discharge rate in PSRO areas in two or more regions.
In contrast to most of the cited studies, this article examines national trends through time rather than cross-sectional geographic variations in one year. The study explores trends in some of the variables found related to the discharge rate in earlier studies—insurance coverage, hospital supply, and physician supply; and demographic variables like age, sex, and race. A multivariate analysis of the differential rise in the discharge rate between the aged and younger populations was not attempted because of the difficulty in identifying independent variables with differential impacts on the old and young.
It is important to observe that the continuing upward trend in the discharge rate affects Medicare payments to hospitals. In particular, this trend should be taken into account in the cost-containment strategies now being designed and tested. Many strategies involve case-mix based reimbursement schemes which would pay hospitals on a per-discharge basis, as opposed to the current retrospective cost basis. Clearly, if the current trend in the discharge rate continues, total reimbursements will increase despite the restraints such a system might impose.
Sources of the Data
The data used in this study were derived primarily from information which hospitals report to the Health Care Financing Administration through their fiscal intermediaries.2 Data were compiled and analyzed for a 20-percent probability sample of Medicare Part A (Hospital Insurance) enrollees aged 65 and over discharged from short-stay hospitals during the period covered by this study.3 Not included in the study are hospital stays of persons enrolled under the disability portion of the Medicare program which covers certain disabled persons under age 65. Since the data come from a sample of enrollees, the estimates are subject to sampling errors which are given in the Technical Note at the end of this report.
In addition, data from the Medicare program are supplemented by data from the National Center for Health Statistics (NCHS) National Hospital Discharge Survey, an annual survey of a probability sample of U.S. hospitals begun in 1965 and from the NCHS National Health Interview Survey, an annual survey of a probability sample of households in the U.S.
The NCHS National Hospital Discharge Survey is the source of data on longitudinal trends in discharges by diagnosis and surgical procedure. It was chosen over the Medicare Statistical System as a source of such data because it provides data on all ages and because data were more readily available for more years in the study period. The reliability of diagnostic and surgical data from both the National Hospital Discharge Survey and Medicare was studied by the Institute of Medicine (Institute of Medicine, 1977, 1980). In these studies, diagnostic and surgical information on a sample of cases was abstracted and coded by a trained field team. When their results were compared with the codes for the same cases in the files of the systems under study, serious discrepancies were found for many diagnoses and procedures. Thus, data on discharges by diagnosis or surgical procedure contain errors, and emphasis should be given to analysis of large differences persisting over time. We attempted to present the most recent data but, because of differences in data availability, not all data could be shown through 1979.
Findings
Changes in the Discharge Rate for Different Age Groups
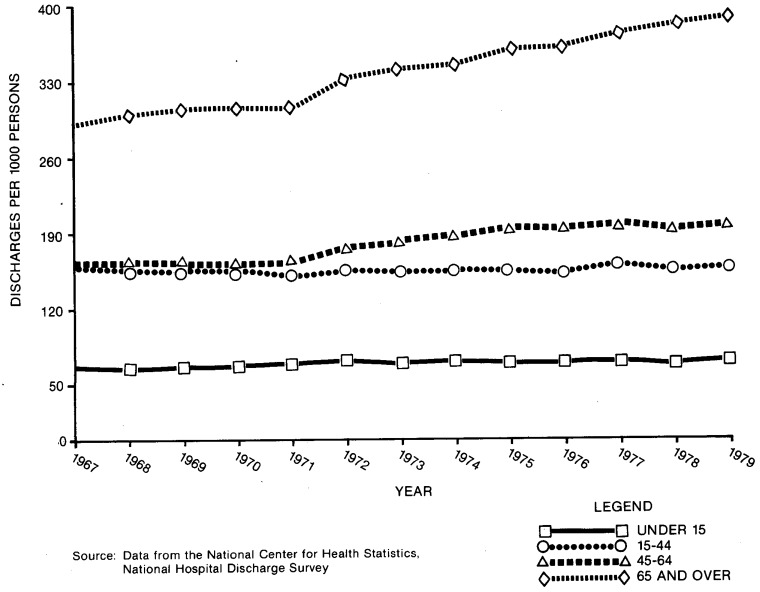
Table 1 and Figure 1 use data from the NCHS to contrast the increase in the discharge rate from short-stay hospitals for persons 65 years of age and over and for persons under age 65. From 1967 to 1979, the discharge rate for persons age 65 and over grew 35 percent, rising from 289 discharges per 1,000 persons to 389 discharges per 1,000 persons. The discharge rate for persons under age 65 grew only 11 percent, increasing from 130 discharges per 1,000 persons to 144 discharges per 1,000 persons from 1967 to 1979. The discharge rate for persons 45 to 64 increased by 22 percent; for persons age 15 to 44 the rate actually decreased by 4 percent, and for persons under age 15 the rate rose by 9 percent.4
Table 1. Number of Short-stay Hospital Discharges Per 1,000 Population, by Age, U.S., 1967, 1974, 1977 and 1979.
| Age | 1967 | 1974 | 1977 | 1979 | Percent Change, 1967-1979 |
|---|---|---|---|---|---|
| All Ages | 144 | 159 | 169 | 170 | 18 |
| Under 65, unadjusted | 130 | 138 | 145 | 144 | 11 |
| Under 65, adjusted1 | 109 | 119 | 124 | 121 | 11 |
| Under 15 | 67 | 72 | 73 | 73 | 9 |
| 15-44 | 162 | 155 | 160 | 156 | −4 |
| 15-44, excluding deliveries2 | 115 | 120 | 125 | 120 | 4 |
| 45-64 | 161 | 188 | 198 | 196 | 22 |
| 65 Years and Over | 289 | 346 | 374 | 389 | 35 |
The rates were adjusted first for the decrease in hospitalizations for deliveries due to the decline in the birth rate by excluding hospitalizations for deliveries.
Then the rates were age and sex adjusted by the direct method to the 1967 population using three age groups.
The decline in the discharge rate for the age group 15 to 44 reflects the substantial decline in deliveries. This line gives the discharge rate excluding hospitalizations for deliveries.
Source: National Center for Health Statistics, “Inpatient Utilization of Short-Stay Hospitals in Each Geographic Division, U.S.—1966-1968,” Vital and Health Statistics, Series 13, No. 10, “Utilization of Short-Stay Hospitals, Summary of Nonmedical Statistics, U.S.—1967,” Vital and Health Statistics, Series 13, No. 9, and “Utilization of Short-Stay Hospitals, Annual Summary of the United States,” Vital and Health Statistics, Series 13, No. 26, for 1974 and Series 13, No. 41 for 1977 and preliminary data from NCHS for 1979.
Figure I. Number of Discharges Per 1000 Persons by Age, U.S. 1967-1979.
Two major demographic changes in the population under age 65 from 1967 to 1979 have had opposite effects on the discharge rate for this group. The aging of the under 65 population tended to increase the rate. The lowered birth rate, which in turn reduced the rate of hospitalizations for deliveries, tended to decrease the rate. Using an age and sex adjusted discharge rate, and excluding hospitalizations for deliveries, the increase in the discharge rate for 1967 to 1979 for the under 65 population was shown to be 11 percent, the same as the increase in the unadjusted rate.
It is of interest to compare the aged population and the population under age 65 on trends in the two other summary measures of hospital use—average length of stay (ALOS) and days of care per 1,000 population. Table 2 shows that ALOS declined for all age groups and that the percentage decline was greater for the aged than for other age groups. Table 3 shows trends in the days of care rate by age.5 For most age groups the days of care rate decreased, but for the aged the rate increased slightly.
Table 2. Average Length of Stay (in days) in Short-stay Hospitals, by Age, U.S., 1967, 1974, 1977 and 1979.
| Age | 1967 | 1974 | 1977 | 1979 | Percent Change, 1967-1979 |
|---|---|---|---|---|---|
| All Ages | 8.4 | 7.7 | 7.3 | 7.2 | −14 |
| Under age 65 | 7.1 | 6.6 | 6.2 | 6.0 | −15 |
| Under 15 | 5.0 | 4.6 | 4.2 | 4.3 | −14 |
| 15-44 | 6.2 | 5.7 | 5.3 | 5.2 | −16 |
| 15-44, excluding deliveries | 6.8 | 6.2 | 5.7 | 5.7 | −16 |
| 45-64 | 10.1 | 9.0 | 8.5 | 8.2 | −19 |
| 65 Years and Over | 14.1 | 11.9 | 11.1 | 10.8 | −23 |
Source: National Center for Health Statistics, “Inpatient Utilization of Short-Stay Hospitals in Each Geographic Division, U.S.—1966-1968,” Vital and Health Statistics, Series 13, No. 10, “Utilization of Short-Stay Hospitals, Summary of Nonmedical Statistics, U.S.—1967,” Vital and Health Statistics, Series 13, No. 9, and “Utilization of Short-Stay Hospitals, Annual Summary of the United States,” Vital and Health Statistics, Series 13, No. 26, for 1974 and Series 13, No. 41 for 1977 and preliminary data from NCHS for 1979.
Table 3. Number of Days of Care in Short-stay Hospitals per 1,000 Population by Age, U.S., 1967, 1974, 1977 and 1979.
| Age | 1967 | 1974 | 1977 | 1979 | Percent Change, 1967-1979 |
|---|---|---|---|---|---|
| All Ages | 1,215 | 1,233 | 1,237 | 1,224 | 1 |
| Under age 65 | 920 | 913 | 894 | 864 | −6 |
| Under 15 | 333 | 328 | 308 | 315 | −5 |
| 15-44 | 1,000 | 892 | 849 | 818 | −18 |
| 15-44, excluding deliveries | 783 | 752 | 716 | 681 | −13 |
| 45-64 | 1,635 | 1,702 | 1,688 | 1,604 | −2 |
| 65 Years and Over | 4,086 | 4,107 | 4,156 | 4,182 | 2 |
Source: National Center for Health Statistics, “Inpatient Utilization of Short-Stay Hospitals in Each Geographic Division, U.S.—1966-1968,” Vital and Health Statistics, Series 13, No. 10, “Utilization of Short-Stay Hospitals, Summary of Nonmedical Statistics, U.S.—1967,” Vital and Health Statistics, Series 13, No. 9, and “Utilization of Short-Stay Hospitals, Annual Summary of the United States,” Vital and Health Statistics, Series 13, No. 26, for 1974 and Series 13, No. 41 for 1977 and preliminary data from NCHS for 1979.
Overall Trends in Medicare Hospital Use
Medicare data for 1967 to 1977 show that the discharge rate from short-stay hospitals for Medicare enrollees age 65 and over rose from 259 discharges per 1,000 enrollees to 335 discharges per 1,000, a 29 percent increase. (Table 4).
Table 4. Trends in Selected Measures of Short-stay Hospital Use by Medicare Enrollees Age 65 and Over, U.S., 1967, 1973 and 1977.
| Measure | 1967 | 1973 | 1977 | Change | Percent Change |
|---|---|---|---|---|---|
|
| |||||
| 1967-1977 | 1967-1977 | ||||
| Discharges per 1,000 enrollees, unadjusted | 259 | 303 | 335 | 76 | 29 |
| Discharges per 1,000 enrollees, adjusted* | 259 | — | 332 | 73 | 28 |
| Average Length of Stay | 13.8 | 11.7 | 10.9 | −2.9 | −21 |
| Median Length of Stay | 9.9 | 9.1 | 8.4 | −1.5 | −15 |
| Days of Care per 1,000 enrollees | 3575 | 3547 | 3651 | 76 | 2 |
The 1977 rate was adjusted for age, sex, and race to the 1967 enrollee population using the direct method using two race groups and eight age groups.
Year-by-year data (not shown) indicate that the discharge rate increased from 1967 to 1968, nearly leveled off from 1968 through 1971, and has been growing steadily ever since. In contrast, ALOS has dropped steadily from 13.8 in 1967 to 10.9 days in 1977, a 21 percent decline. These opposing trends in the discharge rate and ALOS have nearly offset each other with the result that the rate of days of care has not changed much from 1967 to 1977. The rate was 3,575 in 1967 and 3,651 in 1977.
Since the demographic characteristics of the Medicare population have changed from 1967 to 1977, with increases in the median age and the proportion of women and non-whites, the possible role of these changes in the growth of the discharge rate was examined. When the 1977 total discharge rate was adjusted by age, sex and race to the 1967 population, the 1977 rate changed slightly from 335 to 332 discharges per 1,000 enrollees, showing that the net effect of demographic changes has been small.
Table 5 shows the increase in the discharge rate by age group for Medicare enrollees. The youngest group of enrollees, age 65 to 74, experienced the greatest increase, 29 percent, followed by an increase of 27 percent for enrollees age 75 to 84 and an increase of 23 percent for enrollees age 85 and over.
Table 5. Number of Short-stay Hospital Discharges Per 1,000 Enrollees by Age for Medicare Enrollees Age 65 and Over, U.S., 1967, 1973 and 1977.
| Age | Discharges Per 1,000 Enrollees | Percent Change | ||
|---|---|---|---|---|
| 1967 | 1973 | 1977 | 1967-1977 | |
| 65 and over | 259 | 303 | 335 | 29 |
| 65-74 | 224 | 265 | 289 | 29 |
| 75-84 | 307 | 348 | 389 | 27 |
| 85 and over | 370 | 404 | 455 | 23 |
Two other population factors should be examined for their possible role in the increase in the Medicare discharge rate. The first is the mortality rate of Medicare enrollees. The discharge rate is much higher in the last year of life (Piro and Lutins, 1973; Lubitz et al, 1981). If the mortality rate increased, it would very likely have raised the discharge rate. However, the number of deaths per 1,000 enrollees actually decreased from 58 in 1967 to 53 in 1977, despite the aging of the Medicare population.
The second factor that could be related to the increase in the discharge rate is a change in the percent of deaths occuring in hospitals. This percent actually changed very little. In 1967, 44 percent of all deaths of Medicare enrollees occurred in a short-stay hospital; in 1977, 42 percent took place in a short-stay hospital. Thus, neither changes in the mortality rate nor changes in the percent of deaths that occur in hospitals were factors in the rise of the hospitalization rate.
Trends in User Rates and Stay Rates
The discharge rate can be expressed as the product of two measures—the user rate and the stay rate. The relationship between the discharge rate and (1) the user rate or proportion of enrollees hospitalized in a year; and (2) the stay rate or average number of hospital stays per year for each user can be expressed as:
D = U × S
| where | D = discharge rate (number of discharges per 1,000 enrollees). |
| U = user rate (number of persons hospitalized per 1,000 enrollees). | |
| S = stay rate (average number of stays per hospitalized person). |
In order for the discharge rate to increase, either the user rate and/or the stay rate must increase. Table 6 shows the user rates for both the population age 65 and over and the age groups under 65 years, using data from the National Health Interview Survey of NCHS. The National Health Interview Survey underestimates the hospital experience of the persons age 65 and over because the survey excludes deceased or institutionalized persons who account for a large percent of hospital discharges for the aged. Since 1967, National Health Interview Survey estimates of discharges for persons age 65 and over have averaged 21 to 32 percent less than estimates from the National Hospital Discharge Survey of NCHS (Lubitz, 1981). For this reason the data in Table 6 are more useful for comparing time trends by age group than for making comparisons across age groups for any one year.
Table 6. Percent of Population with Short-stay Hospital Discharges, by Age, U.S., 1967, 1974 and 1977.
| Age | Percent of Population With Short-Stay Hospital Discharges (user rate) | Percent Change | ||
|---|---|---|---|---|
|
|
||||
| 1967 | 1974 | 1977 | 1967-1977 | |
| All Ages | 9.8 | 10.7 | 10.4 | 6 |
| Under 17 | 5.3 | 5.7 | 5.0 | −6 |
| 17-24 | 13.4 | 11.3 | 10.9 | −19 |
| 25-34 | 13.6 | 13.3 | 12.5 | −8 |
| 35-44 | 10.5 | 11.2 | 10.4 | −1 |
| 45-64 | 10.7 | 12.7 | 12.0 | 12 |
| 65 and over | 14.3 | 16.8 | 18.1 | 27 |
Source: National Center for Health Statistics, “Current Estimates from the Health Interview Survey, United States,” for 1967, 1974 and 1977, Series 10, Nos. 52, 100 and 106.
Note: The Health Interview Survey (NHIS) does not provide information on the deceased or institutionalized population. Thus, NHIS data tend to seriously underestimate hospital use for the 65 and over age group.
The table shows that from 1967 to 1977 the percent of the population with a hospital stay rose 6 percent from 9.8 to 10.4 percent. For all age groups up to age 44 the user rate actually declined. For persons age 45 to 64 the user rate increased 12 percent, and for persons age 65 and over it increased 27 percent. By 1977, 18.1 percent of persons age 65 and over were hospitalized at least once in contrast to 14.3 percent in 1967.
Table 7 uses data from the National Health Interview Survey to compare trends by age from 1967 to 1977 in the number of hospital discharges per person hospitalized (the stay rate). For all ages the stay rate increased from 1.25 stays per person hospitalized in 1967 to 1.34 stays per person hospitalized in 1977, a 7 percent increase. The greatest increases were found among persons age 35 to 44, showing a 13 percent increase, and persons age 65 and over, showing an 11 percent increase. Thus, aged persons experienced the greatest growth in the user rate and the second greatest growth in the stay rate among all age groups.
Table 7. Number of Short-stay Hospital Discharges Per Person Hospitalized, by Age, U.S., 1967, 1974 and 1977.
| Age | Number of Short-Stay Hospital Discharges Per Person Hospitalized (stay rate) | Percent Change | ||
|---|---|---|---|---|
|
|
||||
| 1967 | 1974 | 1977 | 1967-1977 | |
| All Ages | 1.25 | 1.32 | 1.34 | 7 |
| Under 17 | 1.22 | 1.24 | 1.26 | 3 |
| 17-24 | 1.22 | 1.24 | 1.25 | 3 |
| 25-34 | 1.15 | 1.20 | 1.24 | 8 |
| 35-44 | 1.22 | 1.35 | 1.38 | 13 |
| 45-64 | 1.32 | 1.37 | 1.38 | 4 |
| 65 and over | 1.37 | 1.51 | 1.52 | 11 |
Source: National Center for Health Statistics, “Current Estimates from the Health Interview Survey, United States,” for 1967, 1974 and 1977, Series 10, Nos. 52, 100 and 106.
Table 8 uses Medicare data to examine changes in the user rate and the stay rate by age for Medicare enrollees 65 and over from 1967 to 1977. The table shows that the largest increases in the user rate occurred among younger enrollees aged 65 to 74. In that age group there was a 21 percent increase, compared to a 15 percent increase among persons age 85 and over. The percent increase in the stay rate did not vary greatly by age.
Table 8. Percent of Enrollees With Short-stay Hospital Discharges and Number of Discharges Per Person Hospitalized, by Age, Medicare Enrollees Age 65 and Over, U.S., 1967, 1973 and 1977.
| Age | 1967 | 1973 | 1977 | Percent Change 1967-1977 |
|---|---|---|---|---|
| Percent of Enrollees With Short-stay Hospital Discharges (User Rate) | ||||
|
| ||||
| 65 and Over | 18.7 | 21.4 | 22.6 | 21 |
| 65-74 | 16.1 | 18.7 | 19.4 | 21 |
| 75-84 | 22.0 | 24.5 | 26.1 | 19 |
| 85 and Over | 27.4 | 29.4 | 31.5 | 15 |
|
| ||||
| Number of Short-stay Hospital Discharges Per Person Hospitalized (Stay Rate) | ||||
|
| ||||
| 65 and Over | 1.38 | 1.41 | 1.48 | 7 |
| 65-74 | 1.38 | 1.42 | 1.49 | 8 |
| 75-84 | 1.39 | 1.42 | 1.49 | 7 |
| 85 and Over | 1.35 | 1.37 | 1.44 | 7 |
The NCHS and Medicare data on trends in the discharge rate by age (Tables 1 and 5) and on trends by age in the user rate (Tables 6 and 8), when taken together, suggest that the greatest growth in both the discharge and the user rate occurred in the ages from 45 to 74. Later, we speculate that these age groups experienced the greatest increases in hospitalizations because they have high morbidity but are not too aged to risk certain medical interventions.
Since the discharge rate is a function of the user rate and the stay rate (D = U × S), the overall increase in the discharge rate for Medicare enrollees from 1967 to 1977 can be allocated to increases in each of its two components and the interaction of these two factors. The following relationship expresses this:
where Δ terms represent changes in the period 1967-1977 and subscripts represent the 1967 base year, and:
D = discharge rate
U = user rate
S = stay rate
Table 9 shows the result of allocating the change in the discharge rate to changes in its two components; the user rate and the stay rate and to an interaction factor. Of the total increase of 76 discharges per 1,000 enrollees from 1967 to 1977, 54 discharges per 1,000 enrollees (71 percent) were due to a growth in the proportion of Medicare enrollees hospitalized in a year, while an increase in the number of discharges per Medicare patient accounted for 19 discharges (25 percent). Thus, the greatest proportion of the increase in the discharge rate came from an increase in the rate of enrollees cared for in the hospital, rather than from an increase in the rate of multiple discharges.
Table 9. The Change in the Short-stay Hospital Discharge Rate Allocated to the Change in the User Rate and the Stay Rate, Medicare Enrollees Age 65 and Over, U.S., 1967 and 1977.
| Contribution to Change in Discharge Rate | ||||
|---|---|---|---|---|
|
|
||||
| Measure | 1967 | 1977 | Discharges per 1,000 Enrollees | Percent |
| Discharge Rate (Number of discharges per 1,000 enrollees) | 259 | 335 | 761 | 1001 |
|
| ||||
| User Rate (Number of persons hospitalized per 1,000 enrollees) | 187 | 226 | 54 | 71 |
|
| ||||
| Stay Rate (Number of discharges per user) | 1.38 | 1.48 | 19 | 25 |
|
| ||||
| Interaction Term | — | — | 4 | 5 |
Parts do not add to total due to rounding.
Note: The technique for ascribing the change in the discharge rate to its components is described in Clifford H. Springer, Robert E. Herlihy and Robert I. Beggs, Advanced Methods and Models, Vol. II of the Mathematics for Management Series, Richard D. Irwin, Inc., 1965, pp. 122-125.
Discharges by Length-of-Stay Interval
At the same time that the discharge rate was increasing, the distribution of discharges by length-of-stay intervals was changing significantly. The effect of this change is illustrated in Table 10. From 1967 to 1977 the distribution of discharges by length of stay shifted to shorter stays. In 1967, for example, stays of 2-3 and 4-5 days together accounted for 24 percent of all stays, and in 1977 they accounted for 31 percent. On the other hand, long stays of 29 days or more accounted for 10 percent of stays in 1967 but only 6 percent in 1977.
Table 10. Rate and Percent Distribution of Discharges by Length of Stay Interval for Medicare Enrollees Age 65 and Over, U.S., 1967 and 1977.
| 1967 | 1977 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Length of Stay (in days) | Discharges Per 1,000 Enrollees | Percent Distribution | Discharges Per 1,000 Enrollees | Percent Distribution | Percent Increase in Discharges Per 1,000 Enrollees 1967-1977 |
| All Stays | 259 | 100 | 335 | 100 | 29 |
| 1 day | 12 | 5 | 14 | 4 | 17 |
| 2-3 days | 29 | 11 | 50 | 15 | 72 |
| 4-5 days | 33 | 13 | 53 | 16 | 61 |
| 6-7 days | 32 | 12 | 45 | 13 | 41 |
| 8-14 days | 74 | 29 | 97 | 29 | 31 |
| 15-21 days | 35 | 14 | 41 | 12 | 17 |
| 22-28 days | 18 | 7 | 17 | 5 | −6 |
| 29 days and over | 26 | 10 | 19 | 6 | −27 |
As shown in Table 10, the incidence of hospital stays of one day increased 17 percent compared to the 29 percent growth in the overall discharge rate. Stays of 2-3 days grew 72 percent which was more than any other interval. The growth of stays of 4-5 and 6-7 days also far outpaced the overall increase, growing by 61 and 41 percent. Thus, the increase in shorter hospital stays contributed greatly to the increase in the overall discharge rate.
Stays of 8-14 and 15-21 days increased by 31 and 17 percent. The incidence of stays of 22-28 days showed a slight decrease of 6 percent, and the rate of very long stays of 29 days and over decreased by 27 percent.
The decrease in the incidence of long stays is of interest in view of the findings of studies that have examined the medical and socio-economic situation of long-staying patients. (Goldmann, 1959; National Capital Medical Foundation, 1977; Rosenfeld et al, 1957; and Van Dyke et al, 1963). The studies found that many long-staying patients did not need to be in an acute-care hospital. They were often persons with complex social and medical problems for whom post-hospital placement difficulties were frequently compounded by a shortage of appropriate long-term care facilities.
Charges by Length-of-Stay Interval
Table 11 shows average charge per day for discharges of differing lengths of stay for 1967 and 1976. For both years one to three day stays have a charge per day considerably above the average. In part, this is due to the variable costs of a hospital stay, such as routine tests and other ancillary charges being spread over fewer days. Higher daily charges for short stays may also be due to a high proportion of serious emergency admissions and admissions ending in death. Medicare data (not shown) indicate that a much higher than average percent of 1-3 day stays end in death than do other stays.
Table 11. Average Charge Per Day in Short-stay Hospitals, by Length of Stay, Medicare Patients Age 65 and Over, 1967 and 1976.
| Length of Stay (in days) | Average Charge Per Day | |
|---|---|---|
|
| ||
| 1967 | 1976 | |
| All Stays | $49 | $169 |
| 1-3 days | 72 | 231 |
| 4-7 days | 54 | 167 |
| 8-14 days | 51 | 163 |
| 15-21 days | 51 | 169 |
| 22-28 days | 50 | 172 |
| 29-40 days | 49 | 171 |
| 41 days and over | 40 | 167 |
Table 11 also shows that the pattern of average charge per day for stays beyond 40 days changed from 1967 to 1976. In 1967, the average daily charge for stays of more than 40 days was $40, considerably less than the overall average of $49. The average daily charge for stays of 41 days and over in 1976 of $167 was very close to the overall average of $169 per day.
The contrast between the average charge per day for stays over 40 days between 1967 and 1976 very likely reflects a change in patterns of hospital practice. The lower average daily charge for stays over 40 days in 1967 may reflect the presence of a large proportion of chronically ill, long-staying patients requiring a lesser intensity of services. Perhaps by 1976 many of these types of patients were being discharged to other facilities, and the role of the hospital had shifted to caring for more acutely ill patients. The lack of a significant drop in average daily charges for stays beyond 40 days in 1976 may mean that hospitals had a higher proportion of acutely ill patients and a lower proportion of chronically ill patients than in 1967. This would mean an increase in hospital revenues even if occupancy remained unchanged.
These findings are also in line with Feldstein and Taylor's (1977) analysis of the rising cost of hospital care. They concluded that, due to the influence of hospital insurance, the character of a hospital day had changed as the intensity and sophistication of hospital services increased. They found that most of the growth in average cost per hospital day in excess of the rise in the general price level was due to an increased number of employees and non-labor inputs per patient day. Other studies have quantified the spread of technically sophisticated services (such as intensive care units or coronary care units) which increased the cost and complexity of hospital care (Russell, 1979), (Goldfarb et al, 1980).6 The increased intensity and complexity of services in a hospital stay, taken together with the growth in the rate of short hospital stays and the growth in the user rate, indicate a trend among the elderly of more persons using the hospital but having shorter stays with a higher intensity of services.
The Role off Changes in Case—Mix in the Increasing Discharge Rate
The increase in the discharge rate for persons age 65 and over from 1967 to 1977 raises the question of the role of changes in diagnostic and surgical case—mix. Data from both NCHS and Medicare are used to examine this increase. Data on specific diagnoses or surgeries are limited to the period 1970-1977 because of a change in 1970 in the diagnostic and surgical coding system used by NCHS.
Table 12 uses NCHS data and shows the discharge rates in the major diagnostic categories and individual diagnostic groups with the highest frequency for persons age 65 and over. As compared with the overall 22 percent increase in the discharge rate between 1970-77, there were no strikingly different increases in any major diagnostic category. Hospitalizations in the categories of neoplasms, diseases of the nervous system and sense organs, and diseases of the musculoskeletal system increased by 32; 34 and 31 percent, somewhat more than the overall 22 percent increase. The leading cause of hospitalization, diseases of the circulatory system, grew by 227 discharges per 10,000 persons or 26 percent. This increase of 227 discharges per 10,000 persons accounted for one-third of the total increase of 676 discharges per 10,000 in the discharge rate from 1970 to 1977. When the increase in discharges for diseases of the circulatory system (227 discharges per 10,000) is taken together with the increase of 89 discharges per 10,000 in the category of malignant neoplasms, the combined increase of 316 discharges accounts for about one-half of the overall increase in the discharge rate. Thus, from a diagnostic case-mix point of view, the increase in the discharge rate is characterized by moderate increases in the major categories, rather than very large percentage increases in a few groups.
Table 12. Number of Discharges Per 10,000 Population by Selected Leading First-Listed Diagnostic Groups for Persons Age 65 and Over, U.S., 1970, 1972, 1975 and 19771.
| Diagnostic Group and ICDA-8 Code | Number of First-Listed Diagnoses Per 10,000 Population | Change in Rate 1970-1977 (Discharges Per 10,000 Persons) | Percent Change (1970-1977) | |||
|---|---|---|---|---|---|---|
|
|
||||||
| 1970 | 1972 | 1975 | 1977 | |||
| All Conditions | 3068 | 3330 | 3593 | 3744 | 676 | 22 |
| Neoplasms (140-239) | 310 | 336 | 385 | 409 | 99 | 32 |
| Malignant neoplasms (140-209) | 271 | 294 | 338 | 360 | 89 | 33 |
| Endocrine, nutritional and metabolic diseases (240-279) | 114 | 120 | 123 | 122 | 8 | 7 |
| Diabetes mellitus (250) | 89 | 94 | 93 | 91 | 2 | 2 |
| Diseases of the nervous system and sense organs (320-389) | 160 | 174 | 197 | 214 | 54 | 34 |
| Cataract (374) | 82 | 90 | 108 | 111 | 29 | 35 |
| Disease of the circulatory system (390-458) | 882 | 982 | 1047 | 1109 | 227 | 26 |
| Acute myocardial infarction (410) | 84 | 93 | 87 | 93 | 9 | 11 |
| Chronic ischemic heart disease (412) | 290 | 316 | 322 | 324 | 34 | 12 |
| Congestive heart failure (427.0) | 59 | 73 | 88 | 104 | 45 | 76 |
| Cerebrovascular disease (430-438) | 194 | 207 | 202 | 205 | 11 | 6 |
| Diseases of the respiratory system (460-519) | 301 | 320 | 349 | 352 | 51 | 17 |
| Pneumonia, all forms (480-486) | 96 | 103 | 112 | 110 | 11 | 14 |
| Diseases of the digestive system (520-577) | 429 | 459 | 490 | 482 | 53 | 12 |
| Cholelithiasis, cholecystitis and cholangitis (574, 575) | 80 | 82 | 78 | 73 | −7 | −9 |
| Diseases of the genitourinary system (580-629) | 249 | 254 | 265 | 281 | 32 | 13 |
| Hyperplasia of prostate (600) | 76 | 75 | 73 | 81 | 5 | 7 |
| Diseases of the musculoskeletal system (710-738) | 130 | 151 | 157 | 170 | 40 | 31 |
| Arthritis, all forms (710-718) | 68 | 78 | 85 | 88 | 20 | 29 |
| Accidents, poisonings and violence (800-999) | 266 | 279 | 301 | 315 | 49 | 18 |
| Fractures, neck of femur (820) | 63 | 61 | 67 | 70 | 7 | 11 |
| Other fractures (800-819, 821-829) | 91 | 97 | 94 | 101 | 10 | 11 |
| Other conditions (Residual) | 227 | 255 | 279 | 290 | 63 | 28 |
The diagnostic categories and diagnostic groups were selected because they were the most frequent for persons age 65 and over in 1975.
Source: 1970 and 1977, unpublished tables from NCHS; 1972 and 1975, NCHS, “Inpatient Utilization of Short-Stay Hospitals by Diagnosis, United States” for 1972 and 1975.
Among individual diagnostic groups the rate of discharges for congestive heart failure showed by far the largest percentage increase, 76. The rate of discharges for cataract and malignant neoplasms showed larger than average increases of 35 and 33 percent.
Just as the overall hospitalization rate has been growing at a faster pace for persons aged 65 and over than for the rest of the population, so the incidence of surgeries has been increasing faster for the aged. As shown in Table 13, from 1965 to 1977 the number of surgeries per 1,000 population increased more for older persons. Persons aged 65 and over experienced a 58 percent increase in the rate of operations as compared with a 24 percent increase for persons under age 65. It has been suggested that the increase in surgery among the aged may be due in part to, “technological advances that make surgery safer and more effective,” (Machlin and Kleinman, 1980).
Table 13. Number of Surgical Operations Per 1,000 Population by Age, U.S., 1965, 1970, 1975 and 1977.
| Age | 1965 | 1970 | 1975 | 1977 | Percent Change 1965-1977 |
|---|---|---|---|---|---|
| All Ages | 77 | 78 | 96 | 100 | 30 |
| Under 65 | 74 | 74 | 89 | 92 | 24 |
| Under 15 | 41 | 40 | 41 | 41 | 0 |
| 15-44 | 89 | 86 | 102 | 105 | 18 |
| 45-64 | 99 | 96 | 123 | 125 | 26 |
| 65 and over | 105 | 123 | 155 | 166 | 58 |
Note: The data in this table refer to “all-listed” operations in contrast to Table 15 which presents data on “first-listed” operations. The NCHS uses “all-listed” operations to include all operations coded for a discharge.
Source: NCHS, “Surgical Operations in Short-Stay Hospitals, United States, 1975,” Vital and Health Statistics, Series 13, Number 34, April 1978, p. 16, and unpublished tables from NCHS.
One notable example of the effect of technological advances on the surgical rate is extraction of lens (cataract). Technical improvements reduced the complexity of the procedure, and its incidence grew from 53 operations per 10,000 persons age 65 and over in 1965 to 112 in 1975 (Ranofsky, 1978)7 while the average length of stay for cataract operations dropped from 7.9 days to 4.7 days from 1969 to 1977 for Medicare enrollees. Some other technical advances which may have influenced the incidence of surgeries are the introduction of new materials for prostheses, new cements in the field of orthopedics, and advances in cardiology including bypass surgery and heart pacemakers.
Data on the rate and percent of discharges with surgery for Medicare enrollees are shown in Table 14. The table shows that the rate of discharges with surgery has increased along with the overall discharge rate. Discharges with surgery have comprised about 30 percent of all discharges since the Medicare program began. The data show that the percent of discharges with surgery dropped slightly after 1967, the first full year of the program, and then began to rise slightly after 1971. In 1971, 30 percent of discharges had surgery; in 1977 the percent with surgery had risen to 34. This trend, though slight, may signal a tendency to treat a larger proportion of cases with surgery.
Table 14. Number of Discharges With and Without Surgery Per 1,000 Medicare Enrollees, U.S., 1967-1977.
| Year | Discharges Per 1,000 Enrollees | Percent Distribution | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total | With Surgery | Without Surgery | Total | With Surgery | Without Surgery | |
| 1967 | 259 | 83 | 177 | 100 | 32 | 68 |
| 1968 | 284 | 86 | 198 | 100 | 30 | 70 |
| 1969 | 295 | 90 | 205 | 100 | 30 | 70 |
| 1970 | 293 | 90 | 203 | 100 | 31 | 69 |
| 1971 | 288 | 87 | 201 | 100 | 30 | 70 |
| 1972 | 299 | 93 | 207 | 100 | 31 | 69 |
| 1973 | 303 | 97 | 206 | 100 | 32 | 68 |
| 1976 | 327 | 103 | 223 | 100 | 32 | 68 |
| 1977 | 335 | 113 | 222 | 100 | 34 | 66 |
Note: Data for 1974 and 1975 are not available.
The changes in the rate of discharges in major surgical categories, and in the most common surgical groups within these categories from 1970 to 1977 for persons age 65 and over are shown in Table 15. Overall, discharges with surgery grew by 292 discharges per 10,000 persons, increasing from 896 to 1188 discharges per 10,000 persons.
Table 15. Number of Selected First-Listed Surgical Operations Per 10,000 Population, Persons Age 65 and Over, U.S., 1970, 1972, 1975 and 19771.
| Surgical Group and ICDA-8 Code | Number of First-Listed Operations Per 10,000 Population | Change in Rate 1970-1977 |
Percent Change 1970-1977 |
|||
|---|---|---|---|---|---|---|
|
| ||||||
| 1970 | 1972 | 1975 | 1977 | |||
| All operations | 896 | 957 | 1190 | 1188 | 292 | 33 |
| Neurosurgery (01-05) | 14 | 15 | 21 | 22 | 8 | 57 |
| Ophthalmology (06-14) | 106 | 117 | 137 | 146 | 40 | 38 |
| Extraction of lens (14.4-14.6) | 83 | 90 | 110 | 110 | 27 | 33 |
| Otorhinolaryngology (16-21) | 24 | 22 | 25 | 26 | 2 | 8 |
| Vascular and cardiac surgery (24-30) | 48 | 61 | 88 | 121 | 73 | 152 |
| Insertion or replacement of electronic heart device (30.4-30.5) | 14 | 21 | 29 | 39 | 25 | 179 |
| Thoracic surgery (32-35) | 17 | 24 | 28 | 29 | 12 | 71 |
| Abdominal surgery (38-48) | 190 | 196 | 213 | 207 | 17 | 9 |
| Repair of inguinal hernia (38.2-38.3) | 44 | 45 | 51 | 44 | 0 | 0 |
| Exploratory laparotomy or celiotomy (39.1) | 23 | 24 | 26 | 23 | 0 | 0 |
| Cholecystectomy (43.5) | 38 | 40 | 42 | 42 | 4 | 11 |
| Resection of small intestine or colon (47.4-47.6) | 18 | 21 | 24 | 26 | 8 | 44 |
| Proctological surgery (50-52) | 22 | 24 | 22 | 27 | 5 | 23 |
| Urological surgery (54-61) | 145 | 147 | 165 | 176 | 31 | 21 |
| Local excision and destruction of lesion of bladder (56.1-56.2) | 17 | 19 | 23 | 24 | 7 | 41 |
| Prostatectomy (58.1-58.3) | 69 | 68 | 70 | 79 | 10 | 14 |
| Breast surgery (65) | 15 | 18 | 23 | 22 | 7 | 43 |
| Mastectomy (65.2-65.6) | 14 | 17 | 22 | 20 | 6 | 43 |
| Gynecological surgery (67-72) | 49 | 45 | 48 | 49 | 0 | 0 |
| Orthopedic surgery (80-90) | 145 | 158 | 177 | 191 | 46 | 32 |
| Closed reduction of fracture without fixation (82.0) | 28 | 26 | 23 | 24 | −4 | −14 |
| Reduction of fracture with fixation (82.2) | 56 | 60 | 65 | 71 | 15 | 27 |
| Plastic surgery (92-94) | 47 | 47 | 50 | 52 | 5 | 11 |
| Excision of lesion of skin and subcutaneous tissues (92.1-92.2) | 26 | 29 | 28 | 31 | 5 | 19 |
| Biopsy (A1-A2) | 58 | 69 | 96 | 102 | 44 | 76 |
| Other (Residual) | 15 | 16 | 17 | 18 | 3 | 20 |
The surgical categories and surgical groups were selected because they were the most frequent for persons age 65 and over in 1975.
Source: Data for 1970, 1972 and 1977 are from unpublished tabulations from NCHS, 1975 data are from NCHS “Surgical Operations in Short-Stay Hospitals, United States, 1975,” Vital and Health Statistics, Series 13, No. 34, April 1978.
By far the largest increase in the discharge rate for a major surgical category was in vascular and cardiac surgeries which grew 152 percent from 1970 to 1977. The increase of 73 discharges per 10,000 persons in this category represented one quarter of the overall increase of 292 discharges with surgery per 10,000 persons. No other surgical category showed nearly the rate of increase shown by vascular and cardiac surgeries. Table 16 shows that the rate of vascular and cardiac surgeries also increased rapidly for persons age 45-64 in the same period. The next largest percentage increases in the surgical rates in major categories for the aged were found for biopsies and thoracic surgery (Table 15) which increased 76 and 71 percent. Among individual surgical groups, insertion or replacement of electronic heart device showed the largest increase of 186 percent. This operation accounts for about one third of all first-listed vascular and cardiac surgeries for the aged.8
Table 16. Number of First-Listed Surgical Operations for Vascular and Cardiac Surgery (ICDA-8 Codes 24-30) Per 10,000 Persons, by Age, U.S., 1970, 1972, 1975, 1977.
| Age | 1970 | 1972 | 1975 | 1977 | Change 1970-1977 | |
|---|---|---|---|---|---|---|
|
| ||||||
| Operations Per 10,000 Persons | Percent | |||||
| All Ages | 20 | 24 | 32 | 40 | 20 | 100 |
| Under Age 15 | 6 | 7 | 8 | 8 | 2 | 33 |
| 15-44 | 14 | 14 | 15 | 16 | 2 | 14 |
| 45-64 | 37 | 52 | 72 | 89 | 52 | 140 |
| 65 Years and Over | 48 | 61 | 88 | 121 | 73 | 152 |
Source: Data for 1970, 1972 and 1977 are from unpublished tabulations from NCHS, data for 1975 are from “Surgical Operations in Short-Stay Hospitals, United States, 1975,” Vital and Health Statistics, Series 13, No. 34, April 1978.
Data on surgeries involving the heart, as opposed to all cardiac and vascular surgeries, are shown in Table 17. The data show a large percentage increase in the rate of heart operations for persons age 65 and over and an even larger increase among persons 45 to 64 years.9
Table 17. Number of Selected First-Listed Surgical Operations for Selected Operations Involving the Heart* Per 10,000 Persons, by Age, U.S., 1970, 1972, 1975, 1977.
| Age | 1970 | 1972 | 1975 | 1977 | Change 1970-1977 | |
|---|---|---|---|---|---|---|
|
| ||||||
| Operations Per 10,000 Persons | Percent | |||||
| AAll Ages | 6.4 | 9.8 | 15.2 | 21.2 | 14.8 | 231 |
| Under Age 15 | 3.2 | 3.6 | 4.1 | 4.9 | 1.7 | 53 |
| 15-44 | 3.4 | 3.9 | 5.6 | 6.1 | 2.7 | 79 |
| 45-64 | 11.2 | 22.7 | 37.1 | 52.8 | 41.6 | 371 |
| 65 Years and Over | 18.6 | 25.8 | 40.4 | 61.9 | 43.3 | 233 |
- Operations On valves of heart (29.2-29.4)
- Cardiac revascularization (29.8)
- Cardiac catheterization (30.2)
- Insertion or replacement of electronic heart device (30.4, 30.5)
Source: Data for 1970, 1972 and 1977 are from unpublished tabulations from NCHS, data for 1975 are from “Surgical Operations in Short-Stay Hospitals, United States, 1975,” Vital and Health Statistics, Series 13, No. 34, April 1978.
The large increase in the rate of heart surgeries among the 45-64 and 65 and over age groups raises the question of its relation to the decline in mortality from heart disease, the leading cause of death in the United States. Table 18 shows the death rate from heart disease for the age groups with the highest mortality from heart disease. For all ages the age-adjusted death rate from heart disease decreased 16 percent from 1970 to 1977. For persons age 45 to 64, the death rate from heart disease declined 17 percent. For persons age 65 and over, the decline from 1970 to 1977 was 13 percent.
Table 18. Number of Deaths from Diseases of the Heart Per 10,000 Persons by Age, U.S., Selected Years 1950 to 1977.
| Change, 1950-1970 | Change, 1970-1977 | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Age | 1950 | 1970 | 1977 | Deaths Per 10,000 Persons | Percent | Deaths Per 10,000 Persons | Percent |
| All Ages (age adjusted)1 | 31 | 25 | 21 | −6 | −19 | −4 | −16 |
| All Ages, crude | 36 | 36 | 33 | ||||
| 45-64 | 53 | 42 | 35 | −11 | −21 | −7 | −17 |
| 65 Years and Over | 284 | 268 | 233 | −16 | −6 | −35 | −13 |
Age adjusted by the direct method to the total population of the United States in 1940, using 11 age groups.
Source: For all ages and for persons age 65 and over; Health, United States, 1980, USDHHS, Public Health Service, Office of Health Research, Statistics and Technology, DHHS Pub. No. (PHS) 81-1232, Hyattsville, MD, 1980, p. 138. Rates for persons age 45 to 64 were computed using Vital Statistics of the United States, 1950, Vol. Ill, Table 52, and Vital Statistics of the United States for 1970 and 1977, Vol. II—Mortality, Part B, Section 7, Table 34.
Population data for 1950 are from U.S. Bureau of the Census, Statistical Abstract of the United States: 1955, Washington, D.C., 1955.
Population data for 1970 are from U.S. Bureau of the Census, Statistical Abstract of the United States: 1980, Washington, D.C., 1980.
Population data for 1977 are from U.S. Bureau of the Census, Current Population Reports: Population Estimates and Projections, “Estimates of the Population of States by Age, July 1, 1971 to 1979,” Series P-25, No. 875, 1980.
Some studies have attempted to relate the decline in mortality from heart disease to certain improvements in treatment such as coronary care units and by-pass surgery and to changes in risk factors such as hypertension, smoking, or serum cholesterol levels. Definite conclusions have not been reached, but it is generally believed that the role of improvements in treatment has been less than the role of changes in risk factors. (Kleinman et al, 1979; Stallones, 1980; Stern, 1979). The data presented here showing large increases in heart operations suggest the need to further examine the benefits of these operations and any relation between the decline in deaths from heart disease and the increase in heart operations.
Hospital Insurance Coverage for Persons Under and Over Age 65
Could differences in trends in insurance coverage for hospital care between persons under age 65 and 65 years of age and over help explain the differences in the increases in discharge rates between these age groups? The percentage of persons age 65 and over with hospital insurance hardly changed during the study period since most were covered by Medicare. Data from the National Health Interview Survey, shown in Table 19, indicate that the percentage of persons under age 65 with private hospital insurance also remained almost unchanged.
Table 19. Percent of Persons with Private or Medicare Hospital Insurance by Age, U.S., 1968, 1970, 1972 and 1974.
| Year | Age | |
|---|---|---|
|
| ||
| Under Age 65 | 65 Years and Over | |
| 1968 | 78 | 95 |
| 1970 | 78 | 96 |
| 1972 | 77 | 96 |
| 1974 | 78 | 97 |
| 1976 | 78 | 96 |
Note: The data for persons under age 65 are for private hospital insurance coverage and the data for persons age 65 years and over are for Medicare and/or private health insurance. Data on Medicaid coverage for both age groups and on Medicare coverage for the under 65 population (under the Medicare coverage for certain disabled persons begun in 1973) are not shown because they were not available for all years.
Source: Charles S. Wilder, “Hospital and Surgical Insurance Coverage, United States, 1974.” Vital and Health Statistics, Series 10, No. 17, DHEW Pub. No. (HRA) 77-1545, 1977, p.5 and Larry S. Corder, “Health Care Coverage: United States, 1976,” Advance Data, No. 44, National Center for Health Statistics, DHEW, 1979.
Another measure of insurance coverage is the percent of total personal health care expenditures paid by third-parties (primarily, private health insurance and government). Table 20 shows that from 1967 to 1977 third-party payments as a percentage of total expenditures actually grew more for persons under age 65 than for persons age 65 and over. Thus, differences in insurance coverage by age do not appear to explain differences in the increase in hospitalization rates between the aged and the rest of the population.
Table 20. Third Party Payments (Private Health Insurance, Government and Philanthropy and Industry) as a Percent of Personal Health Care Expenditures by Age, U.S., 1967-1977.
| Fiscal Year | Age | |
|---|---|---|
|
| ||
| Under Age 65 | 65 Years and Over | |
| 1967 | 52 | 63 |
| 1968 | 54 | 72 |
| 1969 | 56 | 72 |
| 1970 | 57 | 67 |
| 1971 | 59 | 66 |
| 1972 | 62 | 64 |
| 1973 | 62 | 65 |
| 1974 | 61 | 72 |
| 1975 | 64 | 74 |
| 1976 | 65 | 74 |
| 1977 | 68 | 74 |
|
| ||
| Percent Change | ||
|
| ||
| 1967-1977 | 31 | 17 |
Source: Robert M. Gibson and Charles R. Fisher, “Age Differences in Health Care Spending, Fiscal Year 1977,” Social Security Bulletin, Vol. 42, No. 1, January 1979 pp. 3-16.
Robert M. Gibson, Marjorie Smith Mueller and Charles R. Fisher, “Age Differences in Health Care Spending, Fiscal Year 1976,” Social Security Bulletin, Vol. 40, No. 8, August 1977, pp. 3-14.
Marjorie Smith Mueller and Robert M. Gibson, “Age Differences in Health Care Spending, Fiscal Year, 1974,” Social Security Bulletin, Vol. 38, No. 6, June 1975, pp. 3-16.
The Supply of Hospitals and Physicians
Another factor which may be related to the increase in the Medicare discharge rate is the supply of hospitals and physicians. Table 21 presents data on the number of hospitals and number of hospital beds certified for participation in Medicare. The number of hospitals changed little, but the number of beds increased 21 percent as average hospital size grew. In relation to the entire population the bed supply grew from 3.9 to 4.4 beds per 1,000 persons, but the number of beds per 1,000 aged Medicare enrollees changed little because the Medicare population and the number of beds grew at the same rate. With the supply of beds per Medicare population constant, the decrease in Medicare ALOS noted earlier, created more room for the increase in the discharge rate.
Table 21. Number of Participating Short-stay Hospitals Under Medicare, Number of Medicare Beds, Number of Medicare Beds per 1,000 U.S. Population and Per 1,000 Aged Medicare Enrollees, 1967-1976.
| Short-Stay Hospitals Under Medicare | ||||
|---|---|---|---|---|
|
|
||||
| Year | Number | Number of Certified Beds | Beds Per 1,000 U.S. Population | Beds Per 1,000 Aged Medicare Enrollees |
| 1967 | 6,299 | 779,908 | 3.9 | 40 |
| 1968 | 6,276 | 780,454 | 3.9 | 39 |
| 1969 | 6,345 | 823,703 | 4.1 | 41 |
| 1970 | 6,332 | 847,838 | 4.1 | 42 |
| 1971 | 6,301 | 854,388 | 4.1 | 41 |
| 1972 | 6,301 | 877,200 | 4.2 | 42 |
| 1973 | 6,262 | 895,600 | 4.3 | 42 |
| 1974 | 6,257 | 912,731 | 4.3 | 41 |
| 1975 | 6,213 | 921,800 | 4.3 | 41 |
| 1976 | 6,168 | 946,500 | 4.4 | 41 |
Source: Helbing, 1980.
The number of physicians increased 28 percent from 1968 to 1978 (Table 22). In relation to the number of Medicare enrollees, the supply of physicians increased from 14.7 physicians per 1,000 enrollees in 1968 to 15.5 in 1978. (Data not shown in table). An earlier study (Pine et al, 1981) showed that internal medicine and surgery were the two large specialty groups ranking highest in percent of total income derived from Medicare patients. Thus, it is interesting to observe that internal medicine experienced the largest growth of the major specialties. The growth in the number of internists is a part of the overall increase in the percentage of physicians who are specialists as opposed to general practitioners; an increase that parallels the increasing technological sophistication of hospital care mentioned previously.
Table 22. Number of Professionally Active Physicians by Selected Primary Specialty, U.S., Selected Years 1968-1978.
| Year | Total | General Practice1 | Internal Medicine2 | Surgical Specialties3 | Obstetrics Gynecology | Pediatrics | Psychiatry | All Other Specialties |
|---|---|---|---|---|---|---|---|---|
| 1968 | 290,750 | 60,258 | 48,922 | 62,731 | 17,655 | 16,282 | 19,697 | 65,205 |
| 1970 | 304,926 | 56,804 | 53,527 | 66,047 | 18,498 | 17,505 | 20,901 | 71,644 |
| 1972 | 315,522 | 54,357 | 58,575 | 69,846 | 19,820 | 19,176 | 22,319 | 71,429 |
| 1974 | 325,567 | 53,152 | 63,005 | 71,516 | 20,607 | 20,277 | 23,075 | 73,935 |
| 1976 | 343,876 | 54,631 | 70,253 | 75,508 | 21,908 | 22,108 | 24,196 | 75,272 |
| 1978 | 371,343 | 55,414 | 78,295 | 77,625 | 23,591 | 24,140 | 25,379 | 86,899 |
|
| ||||||||
| Percent Change 1968 to 1978 | ||||||||
|
| ||||||||
| 28 | −8 | 60 | 24 | 34 | 48 | 29 | 33 | |
Includes general and family practice.
Includes internal medicine and the sub-specialties of gastroenterology, pulmonary diseases, allergy and cardiovascular.
Source: USDHEW, Public Health Service, Health, United States, 1978, p. 340, and Health, United States, 1980, p. 190.
Excludes obstetrics and gynecology.
Discussion and Conclusions
If we could be confident that the increased number of people hospitalized means more Medicare enrollees are receiving needed care, then the first 13 years of Medicare have seen many of the Medicare program's goals being met. Access has increased; shorter ALOS could indicate that care is provided more efficiently, and a steady days-of-care rate means hospital services were provided to more Medicare beneficiaries without increased pressure on hospital occupancy or the need for additional hospital beds per 1,000 aged persons. The increased Medicare enrollment in the past 10 years would naturally add to the need for additional hospital capacity.
At present, concern about equity of access has been replaced to some extent by concern about rising burden of health care costs and concern about unnecessary services. Such concerns stem partly from studies of the large geographic differences in use of services and from recognition of the professional uncertainty about the indications for many common surgical procedures. (See Gornick, 1977; Lewis, 1969; Wennberg and Gittleson, 1975; Wennberg et al, 1980). The findings presented here show increased numbers of aged people using the hospital from 1967 to 1979. This also raises the question of the appropriateness of hospital care. The essential focus must now be whether such services are appropriate in terms of benefit to the patient.
The decline in very long stays and the change in the pattern of charges by length of stay probably reflects a change in the role of the hospital, with more hospital days being devoted to rendering high-level acute care and less to caring for the long-staying, chronically ill, multiple problem cases who do not need acute hospital services. Once again, the data suggest that a goal of the Medicare program, to provide care for the chronically ill less in the acute hospital and more in other settings, has been achieved. The question of the type and quality of care received outside the acute hospital by the kinds of cases that would have been cared for in the hospital in the past remains to be answered.
The continuing trend for the discharge rate to increase has implications for prospective reimbursement systems proposed to replace the current cost-based reimbursement system now used by Medicare to pay hospitals. One such scheme, begun in New Jersey on an experimental basis in 1980, is reimbursement per-case based on a diagnostic adjusted case-mix index. In that scheme, the number of cases becomes a multiplier, so that total reimbursement is directly proportional to the number of cases. The data presented show that, if case mix remains unchanged, such a system instituted nationwide will lead to increased payments to hospitals if the number of cases (discharges) increases in the future as it has in the past. Those making policy about hospital reimbursement have already recognized that each system presents varying incentives for hospitals to alter utilization parameters (admissions, ALOS, case-mix); the present study indicates they should also take into account the well-established secular trends in utilization over which hospitals may have little control.
The upward trend in the discharge rate also has implications for the design of utilization review programs. Utilization review and Professional Standards Review Organizations (PSRO) have often emphasized review of length of stay over review of the necessity of admission. Length of stay review may have little effect on the rate of admissions; utilization review programs may need to strengthen monitoring of admissions. However, given the professional uncertainty regarding indications for admission, guidelines based on current thinking are not likely to change admission patterns (Wennberg et al, 1981).
The analyses in this article have, for the most part, examined how the Medicare discharge rate has grown rather than why it has grown. The reason the rate has increased more for the Medicare population than for the population under age 65 is still not clear. Changes in the demographic composition and mortality experience were shown not to be factors in the increase for Medicare beneficiaries. The rate of discharges with surgery increased from 1967 to 1977, but the rate of discharges without surgery increased as well. Changes in insurance coverage are probably not a factor in the increase since the aged were covered by Medicare throughout the study period, and the percent of persons under age 65 covered by private hospital insurance also remained virtually the same. In fact, from 1967 to 1977 the percent of personal health care expenditures paid by third parties as opposed to percent of persons with coverage grew more for persons under age 65 than for persons age 65 and over. The supply of physicians and hospital beds also increased during the study period, but the rate of increase was close to the rate of increase in the number of Medicare enrollees.
One might speculate that the increase in the discharge rate is due to a number of interrelated factors. The initial effect of Medicare coverage in 1966 freed patients and physicians from concern about the costs of hospital care. Then, as suggested by Feldstein and Taylor, Medicare coverage may have provided an impetus for patients, physicians and hospitals to seek and provide more frequent and sophisticated services.
There are economic rewards to hospitals and physicians from increased hospitalizations. The current Medicare payment mechanism is such that amounts reimbursed to hospitals are highest per day for the first few days of a stay, reflecting the more concentrated use of ancillary services during the beginning of a stay. The trend for a greater number of short, but more care-intensive stays, and the decline in long stays of a semi-custodial nature has probably meant increased income for hospitals.
From the physician's point of view increased hospitalization can mean increased income. The physician in most cases decides whether or not to admit a patient. Pauley and Redisch (1973) emphasize the role of physicians in making decisions about the provision of hospital care and propose that such decisions are made by physicians to maximize their income.
But why would not these same factors have caused the discharge rate for the under-65 population to rise at the same rate? One reason might be that the under-65 population has less leisure time to spend seeking and receiving care. A more important reason might be that the over-65 population has more ailments for which medical treatment might be sought. There is only so much care that might be appropriate for a 25 year old person, while a 70 year old person might have a number of ailments for which medical care might offer hope of relief. In addition, technical advances, perhaps spurred by the advent of Medicare coverage, may have been adopted at a more rapid rate for conditions common among the elderly than for other conditions. We noted the large increase in the number of internists, a specialty often involved in the care of older persons. We also noted the discharge rate for persons age 45-64 also increased significantly, though not as much as the rate for persons age 65 and over. Persons in this age group would also have a higher morbidity and thus more reasons to seek care.
There are certainly risks associated with hospital care. Studies at individual hospitals of nosocomial bacteremias, iatrogenic illnesses and surgical mishaps have shown some of the risks. (Spengler, 1978; Steel et al, 1981; Couch et al, 1981). Other authors suggest excess mortality in areas with high surgery rates (Wennberg et al, 1980). As more Medicare enrollees are exposed to these risks, the undesirable, as well as the desirable, aspects of hospitalization increase. As the data show, the trend is for more enrollees to be hospitalized and for more multiple hospitalizations.
The central conclusion of this article—that more Medicare enrollees are being cared for with shorter hospital stays—leads to the important topic of the necessity and quality of the care they receive. The next generation of studies should begin to focus on the nature and appropriateness, as well as the cost, of the hospital services rendered to Medicare beneficiaries.
Technical Note: Reliability of Estimates
Medicare data in this report are estimates based on a 20-percent sample of the enrolled population and hence are subject to sampling errors. Table A shows estimated standard errors for discharges per 1,000 persons enrolled, the most frequently used estimate in this paper. Readers requiring standard errors for other types of estimates should contact the author. Use of Table A requires knowledge of the number of persons enrolled. This can be obtained from HCFA's annual enrollment series of publications.
Table A. Approximate Standard Error of Discharges Per 1,000 Enrolled.
| Estimated Discharges Per 1,000 Enrolled | Base of Rate (Number of Persons Enrolled in Thousands) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| 25 | 50 | 100 | 250 | 500 | 750 | 1,000 | 2,500 | 5,000 | 10,000 | 25,000 | |
| 10 | 2.0 | 1.4 | .97 | .61 | .43 | .35 | .30 | .19 | .13 | .092 | .058 |
| 20 | 2.7 | 1.9 | 1.4 | .85 | .60 | .49 | .42 | .26 | .19 | .13 | .081 |
| 30 | 3.4 | 2.4 | 1.7 | 1.0 | .73 | .59 | .51 | .32 | .23 | .16 | .099 |
| 40 | 3.9 | 2.7 | 1.9 | 1.2 | .84 | .68 | .59 | .37 | .26 | .18 | .11 |
| 50 | 4.3 | 3.0 | 2.1 | 1.3 | .94 | .76 | .66 | .41 | .29 | .20 | .13 |
| 100 | 6.1 | 4.3 | 3.0 | 1.9 | 1.3 | 1.1 | .92 | .58 | .41 | .29 | .18 |
| 150 | 7.4 | 5.2 | 3.6 | 2.3 | 1.6 | 1.3 | 1.1 | .71 | .50 | .35 | .22 |
| 200 | 8.5 | 6.0 | 4.2 | 2.6 | 1.8 | 1.5 | 1.3 | .81 | .57 | .40 | .25 |
| 250 | 9.5 | 6.7 | 4.7 | 2.9 | 2.1 | 1.7 | 1.4 | .91 | .64 | .45 | .28 |
| 300 | 10.0 | 7.3 | 5.1 | 3.2 | 2.3 | 1.8 | 1.6 | .99 | .70 | .49 | .31 |
| 350 | 11.0 | 7.9 | 5.5 | 3.5 | 2.4 | 2.0 | 1.7 | 1.1 | .75 | .53 | .33 |
| 400 | 12.0 | 8.4 | 5.9 | 3.7 | 2.6 | 2.1 | 1.8 | 1.1 | .80 | .56 | .35 |
| 450 | 13.0 | 8.9 | 6.2 | 3.9 | 2.8 | 2.2 | 1.9 | 1.2 | .85 | .60 | .38 |
| 500 | 13.0 | 9.4 | 6.6 | 4.1 | 2.9 | 2.4 | 2.0 | 1.3 | .90 | .63 | .40 |
| 550 | 14.0 | 9.8 | 6.9 | 4.3 | 3.0 | 2.5 | 2.1 | 1.3 | .94 | .66 | .41 |
A number of approximations were required to derive estimates of standard errors that would be applicable to a wide variety of items. As a result, the standard errors presented provide a general order of magnitude rather than the exact standard error for any specific item.
Sampling errors for data from the NCHS Hospital Discharge Survey and Health Interview Survey can be obtained from the publications listed in the sources to the tables in this paper.
Acknowledgments
The authors are indebted to HCFA's Office of Statistics and Data Management, under the direction of Carol Walton, who develop and maintain the Medicare Statistical System and to the Hospital Care Statistics Branch, Mary Moien, Chief, of the National Center for Health Statistics for their help in obtaining data for this study. The authors would like also to thank Jill Hare and Kay Barrett for their aid in preparing this paper. They would also like to thank Marian Gornick for her many helpful suggestions and Allen Dobson and Judith Lave for their careful review.
Footnotes
Such studies include Chiswick's (1976) multi-equation model examining factors related to the variation in admission rates, hospital occupancy and hospital beds per capita among Standard Metropolitan Statistical Areas (SMSAs) in 1967 and Anderson's (1981) examination of factors related to admission rates, length of stay, and hospital expenses per day among health service areas (HSAs) in 1978. Studies of variations in hospital use by Medicare enrollees, as opposed to the entire population, include Gornick's analyses (1981 and 1977) of 1979 PSRO level and 1972 and 1973 state level data and the analyses by Deacon et al (1980) and Lintzeris et al (1981) of 1976 data at the PSRO area and HSA levels.
Data used for this paper were developed especially for this study; some figures may differ slightly from those in other reports about Medicare hospital use. In no case would any conclusions be affected by the differences.
Short-stay hospitals are hospitals with an average length of stay of less than 30 days.
Data for 1953, 1958, 1963 and 1970 from household surveys suggest that the trend for admission rates to increase faster for older than younger persons began as early as the 1950's. For more information see; Ronald Andersen, Joanna Lion, and Odin Anderson, Two Decades of Health Services: Social Survey Trends in Use and Expenditure, Ballinger, Cambridge, MA, 1976, pp. 34 and 51.
The days of care rate is the product of the discharge rate and ALOS.
The Goldfarb et al article contains a comprehensive review of possible causes of the increases in intensity and sophistication of services.
The data cited are for “all-listed” cataract operations in contrast to the data in Table 15 on “first-listed” operations. See the note to Table 13.
As noted above, from 1965 to 1975 cataract operations increased 111 percent. Since much of the increase occurred from 1965 to 1970, cataract surgery does not show an unusually large increase in Table 15. There were 53 all-listed cataract operations per 10,000 persons age 65 and over in 1965, 84 in 1970 and 112 in 1975 (Ranofsky, 1978). As explained above, data on most surgeries before 1970 were not available in a comparable form to data for 1970 and after because of a coding system change.
Data on surgeries involving the heart were selected from surgical groups in the NCHS category of “vascular and cardiac surgery” to separate operations involving the heart from those on blood vessels and the lymphatic system.
References
- Anderson Gerard USDHHS, Office of Assistant Secretary for Planning and Evaluation. Variations in Per Capita Community Hospital Expenditures. processed, paper presented at the December 1981 meeting of the American Economic Association. [Google Scholar]
- Bunker John P. A Comparison of Operations and Surgeons in the United States and in England and Wales. The New England Journal of Medicine. 1970 Jan 15;282(No. 3):135–144. doi: 10.1056/NEJM197001152820306. [DOI] [PubMed] [Google Scholar]
- Chiswick Barry R. Hospital Utilization: An Analysis of SMSA Differences in Occupancy Rates, Admission Rates, and Bed Rates. Explorations in Economic Research. 1976 Summer;3(No. 3):326–369. [Google Scholar]
- Couch Nathan P, et al. The High Cost of Low-Frequency Events: The Anatomy and Economics of Surgical Mishaps. The New England Journal of Medicine. 1981 Mar 12;304(No. 11):634–637. doi: 10.1056/NEJM198103123041103. [DOI] [PubMed] [Google Scholar]
- Deacon Ronald, et al. Analysis of Variations in Hospital Use by Medicare Patients in PSRO Areas, 1974-1977. Health Care Financing Review. 1979 Summer;1(1):79–107. [PMC free article] [PubMed] [Google Scholar]
- Feldstein Martin, Taylor Amy. The Rapid Rise of Hospital Costs. Staff Report, Executive Office of the President, Council on Wage and Price Stability. 1977 [Google Scholar]
- Goldfarb Marsha G, et al. Health, United States 1980. National Center for Health Statistics; Hyattsville, MD: 1980. Health Care Expenditures; pp. 101–116. DHHS Pub. No. (PHS)81-1232. [Google Scholar]
- Goldmann Franz. Prolonged Stay in General Hospitals. Geriatrics. 1959 Dec;14:789–800. [Google Scholar]
- Gornick Marian. Trends and Regional Variations in Hospital Use Under Medicare. Health Care Financing Review. 1981 Mar;3(3):41–73. [PMC free article] [PubMed] [Google Scholar]
- Gornick Marian. Medicare Patients: Geographic Differences in Hospital Discharge Rates and Multiple Stays. Social Security Bulletin. 1977 Jun;40(No. 6):22–41. [PubMed] [Google Scholar]
- Helbing Charles. Health Care Financing Research Report. USDHHS, Health Care Financing Administration; 1980. Ten Years of Short-Stay Hospital Utilization and Costs Under Medicare: 1967-1976. HCFA Pub. No. 03053. [Google Scholar]
- Institute of Medicine. Reliability of Medicare Hospital Discharge Records. Washington, D.C.: Nov, 1977. [Google Scholar]
- Institute of Medicine. Reliability of National Hospital Discharge Survey Data. Washington, D.C.: 1980. [Google Scholar]
- Kleinman Joel C, Feldman Jacob J, Monk Mary A. The Effects of Changes in Smoking Habits on Coronary Heart Disease Mortality. American Journal of Public Health. 1979 Aug;69(No. 8):795–802. doi: 10.2105/ajph.69.8.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembcke Paul A. Measuring the Quality of Medical Care Through Vital Statistics Based on Hospital Service Areas: 1. Comparative Study of Appendectomy Rates. American Journal of Public Health. 1952 Mar;42:276–286. doi: 10.2105/ajph.42.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis Charles E. Variations in the Incidence of Surgery. New England Journal of Medicine. 1969 Oct 16;281(No. 16):880–884. doi: 10.1056/NEJM196910162811606. [DOI] [PubMed] [Google Scholar]
- Lintzeris George, Lubitz James, Deacon Ronald. Health Care Financing Monograph. Health Care Financing Administration; 1981. Medicare: Hospital Use Rates of Aged Enrollees by Health Service Area, 1974-1977. [Google Scholar]
- Lubitz James. Different Data Systems, Different Conclusions? Comparing Hospital Use Data for the Aged from Four Data Systems. Health Care Financing Review. 1981 Spring;2(No. 4):41–60. [PMC free article] [PubMed] [Google Scholar]
- Lubitz James, Gornick Marian, Prihoda Ronald. Internal Working Paper. DHHS, Health Care Financing Administration; Sep, 1981. Use and Costs of Medicare Services in the Last Year of Life. Processed. [Google Scholar]
- Machlin Steven R, Kleinman Joel C. Health, United States 1980. National Center for Health Statistics; Hyattsville, MD: 1980. Regional and Income Differentials in Surgery; pp. 51–55. DHHS Pub. No. (PHS) 81-1232. [Google Scholar]
- National Capital Medical Foundation. Washington, D.C.: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health, Education, and Welfare; 1977. Inappropriate Hospital Stays, 1976. Processed. Study financed in part by contract No. HEW-100-77-0013. [Google Scholar]
- Pauly Mark, Redisch Michael. The Not-For-Profit Hospital as a Physicians' Cooperative. American Economic Review. 1973 Mar;63(No. 1):87–99. [Google Scholar]
- Pettengill Julian K. Trends in Hospital Use by the Aged. Social Security Bulletin. 1972 Jul;35(No. 7):3–15. [Google Scholar]
- Pine Penelope, et al. Analysis of Services Received Under Medicare by Specialty of Physician. Health Care Financing Review. 1981 Sep;3(No. 1):89–116. [PMC free article] [PubMed] [Google Scholar]
- Piro Paula A, Lutins Theodore. Health Insurance Statistics. USDHEW, Social Security Administration; 1973. Utilization and Reimbursements Under Medicare for Persons Who Died in 1967 and 1968. (HI-51), DHEW Pub. No. (SSA) 74-11702. [Google Scholar]
- Ranofsky Abraham. Vital and Health Statistics. No. 34. Hyattsville, MD: 1978. Surgical Operations in Short-Stay Hospitals, United States, 1975. (13). DHEW Pub. No. (PHS) 78-1785. [PubMed] [Google Scholar]
- Restuccia Joseph D, Holloway Don C. Barriers to Appropriate Utilization of an Acute Facility. Medical Care. 1976 Jul;14(No. 7):559–573. doi: 10.1097/00005650-197607000-00002. [DOI] [PubMed] [Google Scholar]
- Rosenfeld Leonard S, Goldmann Franz, Kaprio Leo A. Reasons for Prolonged Hospital Stay. Journal of Chronic Diseases. 1957 Aug;6:141–152. doi: 10.1016/0021-9681(57)90048-6. [DOI] [PubMed] [Google Scholar]
- Rothberg David L, Pinto Jennifer, Gertman Paul M. Medicare Utilization in the United States: PSRO and Regional Impacts. Health Services Research. 1980 Fall;15(No. 3):249–270. [PMC free article] [PubMed] [Google Scholar]
- Russell Louise. Technology in Hospitals. The Brookings Institution; Washington, D.C.: 1979. [Google Scholar]
- Spengler Robert F, Greenough William B., III Hospital Costs and Mortality Attributed to Nosocomial Bacteremias. Journal of The American Medical Association. 1978 Nov 24;240(No. 22):2455–2458. [PubMed] [Google Scholar]
- Stallones Reuel A. The Rise and Fall of Ischemic Heart Disease. Scientific American. 1980 Nov;243(No. 5):53–59. doi: 10.1038/scientificamerican1180-53. [DOI] [PubMed] [Google Scholar]
- Steel Knight, et al. Iatrogenic Illness on a General Medical Service at a University Hospital. The New England Journal of Medicine. 1981 Mar 12;304(No. 11):638–642. doi: 10.1056/NEJM198103123041104. [DOI] [PubMed] [Google Scholar]
- Stern Michael P. The Recent Decline in Ischemic Heart Disease Mortality. Annals of Internal Medicine. 1979 Oct;91(No. 4):630–640. doi: 10.7326/0003-4819-91-4-630. [DOI] [PubMed] [Google Scholar]
- Van Dyke Frank, Brown Virginia, Thorn Ann-Marie. Long Stay Hospital Care. Columbia University School of Public Health and Administrative Medicine; New York: 1963. [Google Scholar]
- Wennberg John, Barnes Benjamin, Zubkoff Michael. Professional Uncertainty and the Problem of Supplier-Induced Demand. Social Science and Medicine. doi: 10.1016/0277-9536(82)90234-9. forthcoming. [DOI] [PubMed] [Google Scholar]
- Wennberg John, Bunker John, Barnes Benjamin. The Need for Assessing the Outcome of Common Medical Practices. Annual Review of Public Health. 1980;1:277–295. doi: 10.1146/annurev.pu.01.050180.001425. [DOI] [PubMed] [Google Scholar]
- Wennberg John, Gittelsohn Alan. Health Care Delivery in Maine I: Patterns of Use of Common Surgical Procedures. Journal of the Maine Medical Association. 1975 May;66(No. 5):123–130. 149. [PubMed] [Google Scholar]
- USDHHS, Health Care Financing Administration. Professional Standards Review Organization 1979 Program Evaluation. USDHHS, Health Care Financing Administration; 1980. HCFA Pub. No. 03041. [Google Scholar]
- Zimmer James G. Length of Stay and Hospital Bed Misutilization. Medical Care. 1974 May;12(No. 5):453–462. doi: 10.1097/00005650-197405000-00007. [DOI] [PubMed] [Google Scholar]