Abstract
A previous article in this journal (Coelen and Sullivan, 1981) reported new evidence that many State hospital prospective reimbursement (PR) programs have been successful in reducing hospital cost inflation. Limiting proliferation of redundant technologies and community services may be one method of reducing this cost inflation. Data compiled from a sample of over 2,500 hospitals in 15 rate-setting and other States between 1969 and 1978 were used to determine PR's effect on both service adoption and sharing.
Evidence indicates a consistent, retarding effect on all services for New York, the country's oldest, most stringent program. Several other States, notably Minnesota, Maryland, New Jersey, Washington, and Wisconsin showed retarding effects on costly rapidly diffusing services such as open heart surgery, intensive care units (ICUs), and social work, as well as accelerating the phasing-out of redundant services, such as the premature nursery. We found no consistent, significant effects on service sharing.
Introduction
The proliferation and duplication of hospital services are prime contributors to rapidly rising hospital costs. Many of the services diffusing rapidly in the past decade have involved advanced technologies, expensive to purchase and even more expensive to operate. For example, the use of intensive care units (ICUs) increased 32 percent: the performance of open heart surgery increased 43 percent; the use of radioisotopes increased 53 percent; the use of organ banks increased 50 percent; and the application of electroencephalograms (EEGs) increased 69 percent. (See the Data Base section for sources.) Moreover, several community-oriented services requiring costly labor and overhead support services were expanding even more rapidly: social work (124 percent); psychiatric emergency (75 percent); outpatient rehabilitation (64 percent); and outpatient abortion (225 percent).
Without denying the medical need for these services in general, one can question whether the most desirable diffusion levels are being observed. For example, the following questions should be considered. Should eight out of ten hospitals be equipped with an ICU; should one out of ten be equipped for open heart surgery; or should six out of ten have an EEG unit or a social work department? Widespread philanthropy and cost-based reimbursement modes seriously alter competitive market behavior, driving a wedge between use rates for individual services and revenues received., Hospital financial viability is now only loosely tied to need, as manifested in patient use. Thus, it is entirely possible that service expansion has proceeded at a rate beyond cost-effective levels.
Prospective rate-setting, by constraining hospital revenues, may deter hospitals from adopting new facilities and services. They may choose, instead, to share a service with another institution or to develop a patient referral network. Previous research (Coelen and Sullivan, 1981) indicates that some PR programs have been successful in reducing hospital expenditures as a whole. In this paper, we examine the cost-saving impact of rate-setting in retarding diffusion of services.
The next section provides a framework for analyzing reimbursement constraints on decision-making involving facilities and services. We give special emphasis to program characteristics most likely to impinge upon the hospital's capital investment behavior (for example, the age of a program). This section is followed by a brief overview of the data base, then a presentation of tabular and econometric findings. The final section includes a brief discussion of the findings in light of regulatory policy.
Analytic Framework
Logistic Diffusion Curve
Diffusion of innovation in industry has been scrutinized by economists and sociologists since Griliches' (1957) pioneering study of the diffusion of hybrid corn seed. In that study, the author found that diffusion of innovations tends to begin slowly, increases rapidly as individuals/groups become familiar with a particular technological improvement, and then decelerates as adoption of the innovation reaches a saturation point. (See also Mansfield, 1968.)
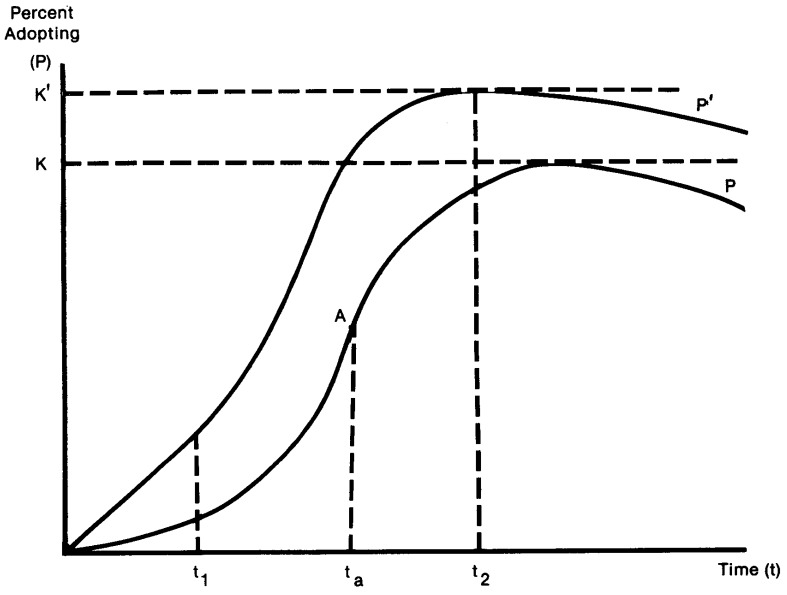
Considerable evidence now exists generally supporting an S-shaped diffusion curve for hospital services (Russell, 1979; Rapoport, 1974; Coleman et al., 1966; and Warner, 1974, 1975). Figure 1 displays a family of diffusion curves for selected values of parameters K, a, and b of the logistic diffusion curve
Figure 1. Logistic Diffusion Curves.
| (1) |
where Pt = the percentage of potential adopters who have actually adopted the service by time, t; K = maximum or equilibrium number of eventual adopters; a = constant of integration locating the curve on the time scale; b = rate of growth coefficient; and t = time. Up through time, ta, the diffusion rate is accelerating; beyond ta, it decelerates as fewer and fewer potential adopters are left. When the curve is very steep around A (the inflection point), diffusion proceeds rapidly, implying a high b coefficient. If b is low, the curve will never be very steep and diffusion will proceed slowly to some maximal level, K, usually less than 100 percent. Both b and K are of interest from a regulatory perspective. Over the short run we are concerned with the rate of proliferation of new, possibly redundant, services while in the long run it is the ultimate adoption level that determines average costs (and charges).
In determining the impact of rate-setting on diffusion of services, it is important to consider both the evaluation time period and the hospital mix. Services generally continue to expand over long time periods (Russell, 1979). These time periods are usually much longer than our evaluation period, 1969-1978. Where this period falls on the underlying diffusion curve for a geographic area will affect the estimated diffusion rate, as Figure 1 shows. If the evaluation period comes between t1 and ta, the diffusion rate will be high, but after t2, the rate will be low even before the introduction of prospective rate-setting. Because the American Hospital Association (AHA) begins recording the adoption of a new service only after some initial diffusion period, rates are often decreasing (although they are not necessarily negative). Hence, the observed diffusion rate, b, reported in AHA statistics will generally be an inverse function of the previous adoption level at any time t>ta, a fact that needs to be considered in making inter-area comparisons of diffusion rates.
Hospital mix is also going to vary—possibly systematically—with implementation of prospective rate-setting, which also can affect the results. Russell (1979), Rapoport (1974), Ginsburg (1977), and Kaluzny (1970), among others, have found a positive relationship between the timing and ultimate level of adoption of services and such hospital characteristics as the number of beds, ownership, teaching status, urbanization, and physician specialists. Hence, States with a greater percentage of teaching or large, voluntary hospitals can be expected to exhibit faster service adoption rates and higher equilibrium levels (see curve P′) than States with a majority of small, community hospitals, at least for the early diffusion years. Thus, for any given evaluation period, say, ta−t2, adoption levels will be higher in P′ States, but adoption rates may well be lower because diffusion has run its course. Structural aspects of the industry, including bed size distribution, teaching status, and ownership, must be accounted for—along with actual adoption levels—to avoid drawing erroneous conclusions with respect to rate-setting impacts.
Geographic variations in medical need should also influence adoption patterns. Areas with high proportions of elderly persons or with extensive insurance coverage should exhibit a stronger overall demand for care as well as for specific services (for example, open heart surgery, cancer therapy, psychiatric counseling), and can be represented as upward or downward shifts in the diffusion curve.
Finally, the possibility of hospitals “over-adopting,” then discontinuing a service has to be considered (Warner, 1974). Some institutions may have been too optimistic in their projected use rates, particularly during a phase of rapid diffusion. If many hospitals are now providing a new service to a fixed population, some hospitals may voluntarily or involuntarily decide to discontinue or share a service. Under truly competitive conditions the retrenching phase would come swiftly and surely, but widespread cost-based reimbursement seriously erodes the punitive incentive to over-expansion in the hospital industry. Prospective rate-setting may well reestablish this form of market penalty, explaining negative adoption rates in some PR States.
Time-related technical change also needs to be considered in the evaluation design. Cobalt therapy, for example, has replaced radium therapy as a safer, more cost-effective cancer treatment (Russell, 1979, p. 103).
Shared Services
Instead of investing in a new service individually, hospitals may choose to share the service with another institution or a group of hospitals. Service sharing is perceived as one method of reducing the institutional costs implicit in adopting a service, through economies of scale and shared overhead expenses. In addition to potential cost reductions, sharing arrangements can prevent the duplication of services in a particular geographic area, while improving the range and, perhaps, the quality of service made available to a particular population.
The majority of literature on shared services is devoted to organization and management studies.1 Kerr (1978), for example, discusses six types of organizational relationships, as presented below:
Purchased Services: The output of one hospital is marketed to one or more other institutions.
Joint Ventures: The creation of a corporation or partnership to meet the combined needs of two or more hospitals.
Freestanding Service Corporation: This type is similar to the Joint Venture model, but control is not vested solely in the participating hospitals. Rather, the corporation is governed by a Board of Directors structured to promote neutrality among participating hospitals and broad community involvement.
Trade Association Sponsorship: In general, this type involves a metropolitan or regional council or a State hospital association offering services for purchase by member institutions.
Commercial Supplier: This kind of arrangement is initiated by an established commercial or professional enterprise, or by a group of hospitals seeking private expertise.
Referred Service: Individual hospitals agree to refrain from providing a particular service and to refer requests for the service to another hospital that is able to provide it both efficiently and economically. (For our purposes, only formal referral agreements are included).
The particular type of sharing arrangement selected by a hospital can vary from service to service. In fact, the organizational types just described are in many ways interchangeable. Thus, the same service may be shared under a number of different organizational relationships. For example, a service like laundry/linen or biomedical engineering will probably be purchased by one institution from another, or perhaps a hospital will contract with a commercial organization that supplies the service. The “Joint Venture” model may be employed for services like nursing education, blood banking, laundry/linen, and laboratory. Dietary service sharing and shared drug and equipment purchasing appear likely to fall into the commercial supplier model. Finally, a referral agreement is probably the most common type of arrangement for critical care services such as intensive care, burn care, and open heart surgery. Generally, these services involve seriously ill/injured patients for whom transport is somewhat risky.
An institution's decision to share a service is primarily the product of two factors: the institution's goals, and the internal and external constraints that impede the achievement of its goals. Goals and constraints are determined, at one level, by certain institutional characteristics, such as bed size, teaching status, and ownership type. The impact of these institutional characteristics on the decision to share a service is less clear-cut than their impact on the decision to adopt a service. The AHA Shared Services surveys (see Astolfi and Matti, 1972; and Taylor, 1977, 1979) suggest that sharing is positively related to bed size and voluntary ownership. For example, large institutions and teaching hospitals each maintain broad, sophisticated service mixes. These hospitals may provide services to small hospitals on a contract or referral basis, particularly for costly clinical services that small hospitals cannot support independently. Voluntary and public nonfederal hospitals also appear more likely to engage in sharing as a method of distributing the financial burden of providing these services across a group of hospitals than for-profit institutions are (Lee and Weisbrod, 1974). Sharing may be a particularly attractive way of providing a service if the hospital is unable to subsidize an unprofitable service through cross-subsidization or philanthropy. Finally, as with service adoption, changes in sharing rates will likely depend on the amount of sharing a hospital currently does. Sharing rates are expected to vary inversely with sharing levels, although the opposite may well occur due to the very low levels observed for most hospitals.
Prospective Reimbursement
As one of many regulatory programs, prospective reimbursement exerts an indirect effect on service mix. Unlike capital expenditure regulation (for example, certificate of need (C/N) review), PR programs cannot directly prevent a hospital from adopting a particular service. Rather, PR programs regulate total or per diem revenue flows, leaving considerable leeway for hospitals to react. Most rate-setting programs control unit prices or charges which, other things being equal, should reduce total hospital revenues and raise operating deficits. Presuming hospitals cannot (or will not) incur continual losses, they will eventually respond by: 1) raising prices to other patients not covered by PR, promoting cross-subsidization; 2) increasing use where marginal costs are below the average, inducing demand; 3) lowering costs by being more efficient; or 4) cutting services.
To date very little is known about the hospital's short and long run responses to rate ceilings—particularly with regard to service expansion and sharing. In one of the few empirical studies, Cromwell (1976) did find that the percentage of patients under the New York PR program negatively affected the adoption of complexity-expanding services in smaller hospitals, while the larger institutions were apparently unaffected. The Economic Stabilization Program also appeared to have had significant negative impacts on service adoption in New York.2 A more recent study by Wagner et al. (1982) confirms the earlier findings on PR and adoption rates, at least for New York.
Hospitals have a number of responses open to them, and structural change in their service configuration is least likely to be affected over a short period of time (two to three years) unless the program is especially constraining. Even if services are affected, it will most likely be through a reduction in activity (for example, limiting the lab to two shifts, or employing fewer psychiatric counsellors) rather than through a complete discontinuation of the service. However, an important argument for a short run rate-setting effect on service expansion rests on cost avoidance. Hospital administrators do exert considerable influence on capital budgets (Cromwell, October 1976). Thus, if PR is effectively limiting revenues, it may reduce the amount of internal funds available to simultaneously expand services in several areas. It may be easier, in some sense, for the administrator to avoid incurring new service costs than to reduce the operating levels of existing services. In the final analysis this is an empirical question, and the answer depends on hospital preferences as well as the scope and stringency of the program.
If all State rate-setting programs were alike, we could expect a consistent response, at least within hospital groups. However, programs vary considerably in many important facets of rate determination as well as in the overall regulatory environment. With regard to service adoption or sharing, five program characteristics are worthy of special consideration: 1) program age, or maturity; 2) scope of revenues, or patients, covered; 3) mode of participation; 4) type of rate review; and 5) the presence of a complementary Certificate of Need Program.
Theory predicts, first, that older, more mature programs are more likely to show a constraining effect on service proliferation as hospitals exhaust short run options. Second, as scope of payer coverage under the program broadens, hospitals have less flexibility in circumventing the revenue ceiling by raising prices to excluded patients. Third, if hospital participation or compliance is voluntary, the program will probably have less impact than if hospitals face mandatory inclusion. Fourth, program rigor can be seen as a function of the type of review conducted, either formulary or budgetary. Under formulary review, a per diem rate is calculated by allowing a hospital's base year costs to be adjusted upward by some inflation factor. The budgetary review is a somewhat less rigid method, in that individual differences across hospitals are taken into consideration, and negotiation between rate-setters and hospital administrators is often an important part of the process. Budget review systems can be established either with or without formal cost and use screens. Generally, formulary systems are expected to be more rigorous; budget review systems without screens, are expected to be the least rigorous. Finally, program effectiveness may be influenced by the State's C/N program. C/N regulation directly addresses facility and service expansion. Rigorous C/N activity may result in a lower rate of service diffusion and an increase in shared service activity. In addition, the presence of a strong C/N program indicates a State political environment somewhat favorable to regulation. If the PR and C/N programs are supportive, both should benefit.
In summary, the most effective rate-setting programs should be the older, more mature ones, with a comprehensive scope of coverage, mandatory authority, a formulary method of review, and a rigorous Certificate of Need program in existence in the State. The least effective programs would appear to be those based on voluntary participation and compliance, in operation only a few years, and with limited coverage.
The 15 programs under examination are variations of these two extremes. Among these, the New York program should be the most effective at constraining service expansion. It is a mature program (12 years old) that now covers all payers except Medicare, it has mandatory authority to set rates using a formulary method, and a C/N program has been in place since 1966. The one major weakness of the program, which has now been corrected, was its narrow scope of coverage. Until 1976, only Blue Cross and Medicaid patients were under rate review, permitting hospitals to charge higher prices to charge-based payers.
Both the Washington and Maryland programs cover all sources of revenue, are mandatory, use a budget review system with screens, and have C/N programs; however, the PR programs have been in place only since 1975 and 1974, respectively. Hence, their effect on service diffusion may be somewhat limited over the 1969-1978 period for which we have data. A third group of programs consisting of New Jersey, Connecticut, and Massachusetts are also mandatory, with mature C/N programs, but all have limited coverage and are younger than the programs discussed above. Until very recently, New Jersey's program covered only Blue Cross and Medicaid, and it was not until 1975 that it was put under State auspices. Prior to 1982, the Massachusetts program excluded both Medicare and Blue Cross, the two principal hospital payers in the State, while Connecticut covers only commercially insured and self-pay patients. Both programs were first implemented in 1974. Colorado, Rhode Island, and Wisconsin are the remaining rate-setting programs with mandatory participation, but only for a single payer: Medicaid in Colorado and Blue Cross in the other States.
The sample group also contains a number of voluntary programs. By their very nature, these programs are expected to be somewhat less rigorous than the mandatory programs, although this is an empirical question. Indiana's program is the oldest in the sample group, having been implemented in 1959. The program is operated by Blue Cross and is totally voluntary. Nebraska's program was implemented in 1972 by the State hospital association. It also was completely voluntary before its termination in 1977. Other voluntary programs include Arizona and Minnesota (mandatory review, voluntary compliance); Western Pennsylvania (voluntary participation, mandatory review and compliance); Colorado (voluntary participation for Blue Cross); and Kentucky (voluntary review, mandatory compliance for Blue Cross).3
Predicting a priori which programs will have the greatest impact on service adoption and sharing is impossible without knowing more about program stringency or hospital reaction functions. Of the five characteristics, however, two may dominate: program age and mode of participation. Older, mandatory programs should have the best chance of altering the service structure of the industry. New York is unique in this regard, and if rate-setting has any impact, we should detect it here. Other possible candidates include Maryland and Washington, followed by New Jersey, Connecticut, and Massachusetts. If voluntary cost containment programs do have an impact on hospital service mix, we should also be in a position to document it in this study.
Data Base and Service Groupings
The data base used in this analysis is part of a larger one created for the National Hospital Rate-Setting Study. A 25 percent random sample was drawn from the 8,160 AHA hospitals reporting at least one year's data between 1970 and 1977. We expanded this sample to include all hospitals in the 15 PR study States. In total, the sample included 2,558 hospitals with observations covering all or part of the 10-year period beginning in 1969 and ending in 1978, a total of 23,576 hospital years. We then merged several demand and supply variables onto the file. In addition, each hospital recorded whether or not certain services were offered in a given year. (See Table 1 for a list of services in our sample.)
Table 1. Service Groupings for Adoption Analysis1.
| Supportive | Competitive | Diffusing | Peaked/Latent | |
|---|---|---|---|---|
| QUALITY-ENHANCING (7) | ||||
| Pharmacy-Full Time | X | X | ||
| Pharmacy-Part Time | X | X | ||
| Histopathology Lab | X | X | ||
| Organ Bank | X | |||
| Blood Bank | X | X | ||
| Premature Nursery | X | X | ||
| Postoperative Recovery | X | X | ||
| COMPLEXITY-EXPANDING (9) | ||||
| X-Ray Therapy | X | X | ||
| Cobalt Therapy | X | X | ||
| Radium Therapy | X | X | ||
| Therapeutic/Diagnostic Radioisotope | X | X | ||
| Electroencephalography | X | X | ||
| Burn Care | X | X | ||
| Physical Therapy | X | X | ||
| ICU/ICCU | X | X | ||
| Open Heart Surgery | X | X | ||
| COMMUNITY SERVICES (8) | ||||
| Outpatient Rehabilitation | X | X | ||
| Psychiatric Outpatient | ||||
| Psychiatric Emergency | X | X | ||
| Outpatient Department | X | X | ||
| Social Work Department | X | X | ||
| Family Planning Service | X | |||
| Home Care Department | X | |||
| Emergency Department | X | X |
Note that service totals do not add to 30, for a couple of reasons. First, four services were combined into two: therapeutic and diagnostic radioisotope and mixed/intensive cardiac care. Second, four services were dropped from the analysis. In- and outpatient hemodialysis and respiratory therapy were excluded due to an extensive problem with unreported data in the early years of the time series (specifically, 1969 through 1974 went unreported). Outpatient abortion service was excluded because it was not legalized until the early 1970s—in the middle of our time series.
One problem that required attention concerned missing and spurious data. Such data had to be supplied or replaced so as not to lose potentially meaningful variation in adoption levels. Services requiring missing value replacement included therapeutic radioisotope therapy, respiratory therapy, inpatient and outpatient hemodialysis, outpatient rehabilitation, outpatient and emergency psychiatric service, emergency department services, and outpatient abortion. A more serious problem involved bad or misreported data which resulted in year-to-year switches in service status. The problem varied in scope, with a range of 7 to 30 percent of the hospitals having at least one bad response. To avoid “overcorrecting” the data, we changed responses only if one year in mid-series was different from the rest.
We used a second data source for the service sharing analysis, namely, the AHA's Hospital Shared Services Participation Profile, a survey conducted in 1978 covering 7,060 hospitals. We gathered data on 48 services, including whether the service was shared and, if shared, the year the sharing arrangement began. This file had a missing values problem that involved unreported dates of initial sharing arrangements in about 40 percent of the cases. Correcting the problem required two steps. First, we regressed reported sharing dates based on hospital teaching status, bed size, and location, making it possible to impute a mean reported sharing date based on available data. Second, we adjusted the imputed sharing date by the independent variables determined to be statistically significant. For example, we created the Emergency Care sharing date through the following computation:
where ECYi is the predicted year sharing began for the i-th hospital, TEACH = teaching status, and REG1, REG2 = the East and South census regions, respectively. This process was repeated for each service selected for analysis.
The AHA now reports over 50 hospital facilities and services. Many of these have appeared only in the last few years and are not amenable to time-series analysis. Nearly 30 services remain, far too many to analyze and present individually. We tried several grouping procedures, placing primary emphasis on a factor-analytic method first employed by Berry (1973). Using factor analysis, Berry discovered that a group of five basic services were adopted by most hospitals first: clinical laboratory; emergency room; operating, delivery, and recovery rooms; and diagnostic X-ray.4 The next group to be added are the quality-enhancing services, so named by Berry because the services tend to enhance the quality of the basic services. This group includes pharmacy, pathology lab, blood bank, premature nursery, and the like. Following the addition of quality-enhancing services, hospitals next tend to adopt services and facilities that expand the capacity to treat patients with widely varying problems. These complexity-expanding services, such as therapeutic X-ray, intensive care, cobalt therapy, and physical therapy, complete an institution's evolution into a sophisticated inpatient treatment center. At this stage of development, some hospitals begin adding another group of services, the community services, transforming the hospital into a full-service community medical care center. Included among these services are the outpatient department, home care, social work, and family planning. Table 1 provides a complete list.
A tripartite grouping into quality, complex, and community services accomplishes several analytic goals.5 First, policy concerns over hospital costs, quality, and service access clearly correspond to this aggregation scheme. Reductions in quality-enhancing services, for example, would be viewed quite differently from dropping certain expensive, often underused, high technology services. Second, previous research shows a systematic adoption relationship between these service groups and those services being added or dropped at the margin.
Other ways of grouping hospitals were considered as well. One can argue, for example, that hospitals under financial constraint might view the adoption of services in terms of their revenue-generating possibilities. If rate-setting renews competitive market forces, hospitals may have to compete more vigorously for patients by adopting services that attract new patients. To the extent this occurred, the diffusion-retarding effects of PR would be nullified. To test this hypothesis, we re-categorized the 24 services listed in Table 1 as either competitive or supportive. Competitive services expand the range of illnesses and hence, patients, a hospital can effectively treat, while supportive services merely complement the existing patient mix. A blood bank, for example, is a supportive service necessary to carry out a wide range of medical and surgical procedures. An organ bank, on the other hand, is a very specialized, expensive facility that permits hospitals to perform organ transplantation, thereby (marginally) expanding treatment modalities and patient use of other inpatient services. A high correlation exists between the competitive/supportive dimension of services and their complexity/community orientation, as Table 1 shows. Quality-enhancing services tend to be supportive, while complex and community services are generally competitive in the sense that they broaden hospital case-mix. Hence, it is unlikely that analysis of the competitive orientation of services will give results materially different from those using Berry's tripartite system.
A third way of grouping services considers actual diffusion rates over the period. If rate-setting is retarding adoption of services, this effect should be most pronounced on services diffusing rapidly nation-wide. Less, if any, effect should be found for services that either had not begun to diffuse rapidly (for example, burn care) or had already completed their diffusion pattern (for example, radium therapy and blood bank), although rate-setting could encourage a quicker discarding of obsolete services for newer technologies (for example, radium therapy being phased out in favor of cobalt therapy).
Table 1 illustrates that most of the rapidly diffusing services tend to be either new, competitive, medical technologies that focus on direct patient care and the treatment of heretofore incurable illnesses, or community outreach services addressing psycho-social problems. Thus, the competitive response to rate-setting, leading to an actual expansion of services, may offset some, if not all, of the diffusion-retarding aspects of prospective reimbursement. Which effect dominates can be determined only empirically.
The AHA's 1978 shared services survey reported inter-hospital sharing of 48 administrative and clinical services. Many of these were of marginal interest (for example, microfilm and public relations) or redundant with other services (for example, safety and security; employee health services, and medical/surgical services). Of the original 48 services, the following were selected for special study (1978 sharing rates for all short-term general hospitals are given in parentheses):
| Administrative (9) |
|---|
|
| Clinical (11) |
|---|
|
These groups cover a wide range of sharing percentages, with obstetrics and open heart surgery among the least shared services, (less than 4 percent), and medical/surgical supply (46.4 percent) and drug supply purchasing (38.9 percent) the two most frequently shared services. The 20 services also vary in terms of their complexity, in the level of patient involvement in the service, in ease of sharing, and in the organizational arrangement most likely to be employed if the service is shared. If rate-setting encourages hospitals to share more services in a significant effort to control costs, then it should show up in one or both groups.
Descriptive Findings
Service Adoption
Table 2 provides average adoption levels for quality-enhancing, complexity-expanding, and community-augmenting services by hospital bed size, ownership, and teaching status for the years 1970 and 1977. Although the terms “adoption” and “diffusion” are often used interchangeably, they mean something different here. By adoption level (or rate) we mean the number of services an individual hospital offers out of a given subset. This idea is in contrast to diffusion levels (and rates) which measure the number of hospitals in a geographic area offering a single service. While the two are clearly related, one (adoption level) uses the hospital as the analytic unit and sums across services, while the other (diffusion level) uses the geographic area as the unit and sums across hospitals. The figures presented in Table 2 should be interpreted, not as the usual diffusion rates seen in the literature, but rather as the level and rate at which hospitals with particular characteristics add new services.
Table 21. Level and Rate of Service Adoption, PR and Control Hospitals, 1970-1977.
| Number/% | Total Services | Quality Enhancing | Complexity Expanding | Community | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||
| 70 | 77 | %Δ | 70 | 77 | %Δ | 70 | 77 | %Δ | 70 | 77 | %Δ | ||
| PR(N) | 1440 | 9.4 | 10.5 | 11.7% | 3.6 | 3.6 | 0.0% | 3.3 | 3.8 | 15.2% | 2.5 | 3.0 | 20.0% |
| Bed Size | |||||||||||||
| <100 | 42% | 4.8 | 6.0 | 25.0 | 2.4 | 2.5 | 4.2 | 1.2 | 1.9 | 58.3 | 1.3 | 1.6 | 23.1 |
| 100-199 | 24 | 9.5 | 10.3 | 8.4 | 4.0 | 3.9 | −2.5 | 3.3 | 3.8 | 15.2 | 2.2 | 2.7 | 22.7 |
| 200-399 | 25 | 13.7 | 13.8 | .6 | 4.6 | 4.5 | −2.2 | 5.5 | 5.3 | −3.6 | 3.7 | 4.1 | 10.8 |
| 400+ | 10 | 17.4 | 17.4 | 0.0 | 5.0 | 4.9 | −2.0 | 7.1 | 6.8 | −4.2 | 5.3 | 5.7 | 7.5 |
| Ownership | |||||||||||||
| Public | 20 | 7.3 | 8.1 | 11.0 | 2.9 | 3.0 | 3.4 | 2.2 | 2.7 | 22.7 | 2.1 | 2.4 | 14.3 |
| Voluntary | 74 | 10.1 | 11.3 | 11.9 | 3.8 | 3.9 | 2.6 | 3.7 | 4.2 | 13.5 | 2.7 | 3.3 | 22.2 |
| Proprietary | 6 | 6.8 | 9.0 | 32.3 | 3.1 | 3.4 | 9.7 | 2.3 | 3.4 | 47.8 | 1.5 | 2.2 | 46.7 |
| Teaching Status | |||||||||||||
| Teaching | 11 | 17.1 | 16.8 | −1.8 | 4.9 | 4.8 | −2.0 | 6.8 | 6.5 | −4.4 | 5.4 | 5.6 | 3.7 |
| Nonteaching | 89 | 8.4 | 9.2 | 9.5 | 3.4 | 3.4 | 0 | 2.9 | 3.3 | 13.8 | 2.1 | 2.5 | 19.0 |
|
| |||||||||||||
| Control (N) | 879 | 7.7 | 9.0 | 16.9 | 3.1 | 3.3 | 6.5 | 2.8 | 3.4 | 21.4 | 1.8 | 2.3 | 27.8 |
| Bed Size | |||||||||||||
| <100 | 55% | 4.3 | 5.5 | 27.9 | 2.1 | 2.4 | 14.3 | 1.1 | 1.8 | 63.6 | 1.1 | 1.4 | 27.3 |
| 100-199 | 23 | 9.0 | 9.9 | 10.0 | 3.9 | 3.7 | −5.1 | 3.4 | 3.9 | 14.7 | 1.7 | 2.3 | 35.3 |
| 200-399 | 16 | 12.7 | 12.8 | .8 | 4.6 | 4.4 | −4.3 | 5.5 | 5.3 | −3.6 | 2.7 | 3.2 | 18.5 |
| 400+ | 6 | 17.2 | 17.2 | 0.0 | 5.1 | 4.9 | −3.9 | 7.4 | 7.3 | −1.4 | 4.8 | 5.0 | 4.2 |
| Ownership | |||||||||||||
| Public | 29% | 6.5 | 7.4 | 13.8 | 2.8 | 2.9 | 3.6 | 1.9 | 2.5 | 31.6 | 1.7 | 2.0 | 17.6 |
| Voluntary | 58 | 8.8 | 10.2 | 15.9 | 3.4 | 3.6 | 5.9 | 3.4 | 4.0 | 17.6 | 2.0 | 2.6 | 30.0 |
| Proprietary | 14 | 4.9 | 7.8 | 59.2 | 2.2 | 3.0 | 36.4 | 1.7 | 3.1 | 82.4 | 1.0 | 1.7 | 70.0 |
| Teaching Status | |||||||||||||
| Teaching | 7 | 15.9 | 16.4 | 3.1 | 4.9 | 4.8 | −2.0 | 6.6 | 6.6 | 0.0 | 4.4 | 5.0 | 13.6 |
| Nonteaching | 93 | 7.0 | 8.1 | 15.7 | 3.0 | 3.1 | 3.3 | 2.5 | 3.1 | 24.0 | 1.6 | 2.0 | 25.0 |
Numbers may be slightly off due to rounding error.
At the beginning of the previous decade, adoption levels among the 1440 PR study group hospitals were about 1.7(= 9.4−7.7) services higher (out of a total of 24 services) than the control group. This difference included .5 more quality-enhancing services, .5 more complexity-expanding services, and .7 more community services. Conversely, rates of increase tended to be higher among control group hospitals: 12 percent in PR study hospitals, compared with a 17 percent increase within the control group—a 50 percent difference, although overall adoption levels in PR States were still higher by 1977. This difference is consistent across the service groups. Quality-enhancing service levels remained constant among PR hospitals, versus a 6 percent increase in the control group; complexity-expanding service levels increased 15 and 21 percent in PR and control hospitals, respectively; and community service adoption levels increased 20 and 27 percent, respectively.
Part of these differences between study and control hospitals can be attributed to industry structure and initial adoption levels. First, as Table 2 shows, adoption levels clearly vary systematically by hospital bed size, teaching status, and ownership. Hospitals with more than 400 beds provide three to four times as many services as hospitals with under 100 beds; teaching hospitals offer twice as many services as nonteaching institutions; and voluntary hospitals provide 50 to 75 percent more services than proprietary institutions. Second, States with prospective reimbursement include more large, sophisticated, teaching hospitals than those States without PR, and these hospitals are more likely to offer a wider range of services as shown below:
Only 42 percent of PR study hospitals had less than 100 beds versus 55 percent of the control group;
10 percent of PR study hospitals had over 400 beds, versus 6 percent of non-PR hospitals;
11 percent of the PR hospitals were teaching hospitals versus 7 percent of the control group; and,
6 percent of the PR hospitals were for-profit hospitals versus 14 percent of the control group.
Comparing rates of change within hospital category partially adjusts for differences in industry structure and initial adoption levels. Reading across the rows in Table 2, we can see that most of the difference between PR and control hospitals is found in small bed size groupings and among proprietary hospitals generally. In the study period, small (< 100 bed) hospitals in the PR group added new services at a rate 3 percentage points lower than similar control group hospitals, while for-profit hospitals under rate-setting added services at a rate 27 percentage points lower than proprietaries in the control group.
Further analysis of Table 2 actually shows negative adoption rates for large, teaching hospitals in the PR study group, particularly in the quality-enhancing and complexity-expanding service groups. Net increases in community services only partially offset decreases in the other two groups, although even for these services rates of change in PR hospitals are much lower among the three smallest bed size groups. However, this occurrence may simply reflect higher initial adoption levels among the PR hospitals.
Tables 3 and 4 present adoption levels for the individual services that make up each of the three service groups, broken down by bed size, ownership, and teaching status. Information contained in these tables shows which of the individual services fluctuated the most during the time period studied. For example, the declines in quality-enhancing services among the three largest bed size categories reported in Table 2 can be traced primarily to a drop in the adoption levels for premature nurseries. This decline presumably reflects a discontinuation of maternity services in response to decreasing birth rates. The tables also show a decline in the complexity-expanding services, X-ray and radium therapy. These declines are partially offset, however, by increases in adoption levels for ICUs, EEGs, and diagnostic/therapeutic radioisotopes. Rapidly increasing community services can be attributed primarily to increases in psychiatric emergency units, social work departments, and abortion services.
Table 3. Adoption Levels for All Services, by Hospital Bed Size.
| Bed Size Less than 100 |
Bed size 100-199 |
Bed Size 200-399 |
Bed Size Greater Than 400 |
|||||
|---|---|---|---|---|---|---|---|---|
| 70 | 77 | 70 | 77 | 70 | 77 | 70 | 77 | |
| Quality Enhancing | ||||||||
| Post Operative Recovery Room | .60 | .73 | .97 | .99 | 1.00 | 1.00 | 1.00 | 1.00 |
| Blood Bank | .50 | .55 | .80 | .79 | .90 | .89 | .94 | .94 |
| Pharmacy Full Time | .23 | .37 | .90 | .94 | .99 | 1.00 | 1.00 | 1.00 |
| Premature Nursery | .22 | .12 | .47 | .29 | .75 | .57 | .90 | .83 |
| Pharmacy Part Time | .47 | .46 | .09 | .05 | .04 | .00 | .02 | .00 |
| Histopathology | .19 | .22 | .75 | .76 | .95 | .94 | .98 | .97 |
| Organ Bank | .00 | .00 | .01 | .00 | .04 | .04 | .17 | .15 |
| Complexity-Expanding | ||||||||
| ICU | .37 | .62 | .79 | .95 | .97 | 1.00 | 1.00 | 1.00 |
| Physical Therapy | .40 | .67 | .83 | .94 | .95 | .98 | .99 | .99 |
| X-Ray Therapy | .09 | .09 | .41 | .25 | .74 | .49 | .92 | .83 |
| Therapeutic Radioisotope | .08 | .22 | .47 | .77 | .92 | .98 | .99 | .97 |
| EEG | .09 | .20 | .34 | .64 | .79 | .93 | .99 | .99 |
| Radium Therapy | .04 | .02 | .31 | .17 | .67 | .48 | .89 | .84 |
| Cobalt Therapy | .01 | .01 | .08 | .07 | .28 | .27 | .69 | .65 |
| Open Heart Surgery | .00 | .00 | .00 | .02 | .13 | .14 | .55 | .58 |
| Burn Care | .00 | .00 | .01 | .01 | .04 | .03 | .16 | .16 |
| Community | ||||||||
| Emergency Dept. | .91 | .90 | .96 | .94 | .99 | .98 | .99 | .99 |
| Outpatient Dept. | .15 | .11 | .25 | .22 | .55 | .46 | .84 | .75 |
| Social Work | .06 | .29 | .34 | .75 | .72 | .91 | .89 | .98 |
| Psychiatric Emergency | .03 | .05 | .13 | .21 | .31 | .43 | .58 | .64 |
| Psychiatric Outpatient | .02 | .02 | .07 | .09 | .23 | .25 | .57 | .56 |
| Family Planning | .01 | .01 | .04 | .03 | .16 | .13 | .41 | .34 |
| Rehabilitation-Outpatient | .02 | .01 | .07 | .08 | .20 | .23 | .49 | .55 |
| Home Care | .02 | .04 | .09 | .08 | .19 | .16 | .25 | .24 |
| Abortion-Outpatient | .00 | .04 | .03 | .10 | .05 | .16 | .20 | .36 |
Table 4. Adoption Levels for All Services, by Hospital Ownership Type, and by Teaching Status.
| Government, Nonfederal |
Voluntary | Proprietary | Nonteaching | Teaching | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 70 | 77 | 70 | 77 | 70 | 77 | 70 | 77 | 70 | 77 | |
| Quality-Enhancing | ||||||||||
| Post Operative Recovery Room | .71 | .78 | .85 | .93 | .70 | .89 | .78 | .87 | .99 | 1.00 |
| Blood Bank | .60 | .63 | .74 | .78 | .55 | .66 | .66 | .70 | .92 | .91 |
| Pharmacy Full Time | .41 | .48 | .69 | .80 | .48 | .80 | .57 | .67 | 1.00 | 1.00 |
| Premature Nursery | .40 | .28 | .50 | .39 | .19 | .14 | .41 | .27 | .81 | .77 |
| Pharmacy Part Time | .38 | .37 | .21 | .15 | .25 | .13 | .28 | .24 | .04 | .00 |
| Histopathology | .36 | .38 | .63 | .69 | .38 | .53. | .50 | .53 | .95 | .96 |
| Organ Bank | .03 | .02 | .03 | .03 | .01 | .00 | .01 | .01 | .17 | .14 |
| Complexity-Expanding | ||||||||||
| ICU | .52 | .71 | .72 | .88 | .42 | .73 | .61 | .80 | .98 | .99 |
| Physical Therapy | .52 | .72 | .74 | .90 | .40 | .77 | .63 | .82 | .97 | .99 |
| X-Ray Therapy | .23 | .20 | .44 | .36 | .20 | .19 | .33 | .23 | .78 | .71 |
| Therapeutic Radioisotope | .22 | .38 | .51 | .70 | .29 | .62 | .37 | .55 | .95 | .96 |
| EEG | .20 | .32 | .44 | .65 | .28 | .59 | .31 | .49 | .93 | .97 |
| Radium Therapy | .16 | .13 | .37 | .32 | .17 | .17 | .26 | .17 | .79 | .72 |
| Cobalt Therapy | .09 | .08 | .16 | .19 | .07 | .08 | .09 | .09 | .56 | .52 |
| Open Heart Surgery | .06 | .06 | .09 | .12 | .01 | .07 | .02 | .03 | .52 | .48 |
| Burn Care | .04 | .05 | .02 | .02 | .01 | .01 | .01 | .01 | .15 | .14 |
| Community | ||||||||||
| Emergency Dept. | .97 | .93 | .96 | .95 | .78 | .84 | .94 | .93 | .96 | .97 |
| Outpatient Dept. | .22 | .20 | .36 | .35 | .18 | .15 | .26 | .20 | .85 | .80 |
| Social Work | .20 | .39 | .41 | .72 | .09 | .52 | .27 | .56 | .89 | .97 |
| Psychiatric-Emergency | .15 | .17 | .17 | .29 | .02 | .11 | .11 | .18 | .53 | .63 |
| Psychiatric-Outpatient | .11 | .10 | .14 | .18 | .01 | .05 | .08 | .08 | .52 | .55 |
| Family Planning | .09 | .07 | .09 | .09 | .00 | .00 | .04 | .03 | .43 | .36 |
| Rehabilitation-Outpatient | .09 | .09 | .12 | .17 | .03 | .04 | .07 | .07 | .41 | .51 |
| Home Care | .06 | .04 | .12 | .13 | .01 | .03 | .08 | .07 | .26 | .24 |
| Abortion-Outpatient | .04 | .10 | .04 | .12 | .03 | .12 | .02 | .07 | .20 | .36 |
These findings suggest that the relatively slower service growth in quality-enhancing and community service adoption among PR hospitals may be due to a faster phasing-out of services such as premature nursery, X-ray and radium therapy, the outpatient department, and the family planning department, and slower diffusion of rapidly growing services such as ICUs, EEGs, social work, and psychiatric emergency.
Service Sharing
Table 5 provides average sharing levels for 20 administrative and clinical services by hospital bed size, ownership, and teaching status, also for the years 1970 and 1977. Sharing levels, like adoption levels shown previously, are generally higher among PR hospitals. At the beginning of the previous decade, PR hospitals shared .5 more services than control hospitals shared, equally divided between the two service categories. Rates of change, on the other hand, are higher among control group hospitals. Over the study period, non-PR hospitals increased sharing levels by 93 percent, compared to 89 percent for PR hospitals, a slight difference entirely due to a higher rate of increase in shared administrative services. Indeed, the rate of change in the clinical group was slightly higher among PR study hospitals.
Table 5. Level and Rate of Service Sharing, PR and Control Hospitals, 1970-1977.
| Number | Total Sharing | Administrative Service | Clinical Services | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| 70 | 77 | %Δ | 70 | 77 | %Δ | 70 | 77 | %Δ | ||
| PR(N) | 1446 | 1.9 | 3.6 | 89.4% | 1.0 | 2.3 | 130.0% | .9 | 1.3 | 44.4% |
| Bed Size | ||||||||||
| <100 | 40% | 1.6 | 3.5 | 118.8 | .6 | 2.1 | 250.0 | 1.0 | 1.4 | 40.0 |
| 100-199 | 24 | 1.7 | 3.4 | 100.0 | .9 | 2.4 | 166.7 | .8 | 1.0 | 25.0 |
| 200-399 | 25 | 2.3 | 3.6 | 56.5 | 1.5 | 2.5 | 66.7 | .8 | 1.1 | 37.5 |
| 400 + | 11 | 3.1 | 4.4 | 41.9 | 1.9 | 2.7 | 42.1 | 1.2 | 1.7 | 41.7 |
| Ownership | ||||||||||
| Public | 21 | 1.8 | 3.5 | 94.4 | .6 | 2.0 | 233.3 | 1.2 | 1.5 | 25.0 |
| Voluntary | 74 | 2.1 | 3.8 | 81.0 | 1.2 | 2.5 | 108.3 | .9 | 1.3 | 44.4 |
| Proprietary | 5 | .6 | 1.2 | 100.0 | .4 | .9 | 125.0 | .2 | .3 | 50.0 |
| Teaching Status | ||||||||||
| Teaching | 15 | 3.2 | 4.4 | 37.5 | 2.0 | 2.8 | 40.0 | 1.2 | 1.7 | 41.7 |
| Nonteaching | 85 | 1.8 | 3.4 | 88.9 | .9 | 2.2 | 144.4 | .9 | 1.2 | 33.3 |
|
| ||||||||||
| Control (N) | 911 | 1.4 | 2.7 | 92.9 | .7 | 1.7 | 142.9 | .7 | 1.0 | 42.9 |
| Bed Size | ||||||||||
| <100 | 52% | 1.1 | 2.3 | 109.1 | .4 | 1.4 | 250.0 | .6 | .9 | 50.0 |
| 100-199 | 23 | 1.2 | 2.6 | 100.0 | .6 | 1.8 | 200.0 | .6 | .8 | 33.3 |
| 200-399 | 17 | 1.5 | 3.0 | 100.0 | 1.0 | 2.1 | 110.0 | .6 | .9 | 50.0 |
| 400 + | 7 | 2.9 | 4.4 | 51.7 | 1.6 | 2.6 | 62.5 | 1.3 | 1.8 | 38.5 |
| Ownership | ||||||||||
| Public | 30 | 1.0 | 2.4 | 140.0 | .4 | 1.5 | 275.0 | .6 | .9 | 50.0 |
| Voluntary | 56 | 1.6 | 3.2 | 100.0 | .8 | 2.1 | 162.5 | .8 | 1.1 | 37.5 |
| Proprietary | 14 | .7 | 1.3 | 85.7 | .3 | .9 | 200.0 | .3 | .5 | 66.7 |
| Teaching Status | ||||||||||
| Teaching | 9 | 2.7 | 4.2 | 55.6 | 1.4 | 2.5 | 78.5 | 1.3 | 1.8 | 38.5 |
| Nonteaching | 91 | 1.2 | 2.5 | 108.3 | .6 | 1.6 | 166.7 | .6 | .9 | 50.0 |
Numbers may be slightly off due to rounding error.
Similar to adoption levels, sharing levels and rates of change vary systematically by bed size category, ownership and teaching status. Large (400+ beds) hospitals shared twice as many services in 1970 as the hospitals with the smallest number of beds, (although the gap narrowed considerably after 1970); teaching hospitals shared nearly twice as much as nonteaching hospitals, and voluntary hospitals shared two to three times as many services as proprietary hospitals. Thus, the more sophisticated hospital mix in PR States partially explains, not only higher adoption levels, but the more extensive sharing observed as well.
Still, base year sharing levels are so low that the rates of change recorded are extremely high when compared to adoption figures presented earlier. For example, nonteaching hospitals in the PR group shared slightly less than one administrative service in 1970 and slightly more than two in 1977. This addition of an average of just 1.3 shared services is a 144 percent increase in sharing.
Comparing the rates of change by hospital size and type, it appears that any difference between PR and control hospitals comes in non-profit and teaching institutions with 200-400 beds. The rate of change among control hospitals with 200-400 beds was almost twice as great as similar PR hospitals, while rates of change were 20-45 percentage points higher among non-profit hospitals in the control group than in the PR group.
Rates of change were much higher among administrative services despite frequently higher base year sharing levels. This finding reflects a comparatively greater inclination among hospitals to share the administrative, non-patient-related services. Besides the lower rates of change, the clinical services did not always exhibit the monotonic increases in sharing levels from smallest to largest bed size that occurred in the administrative service group.
Econometric Findings
We used multivariate econometric techniques in an attempt to isolate the effects of rate-setting from other, confounding influences. The following estimates are based on a reduced-form specification of a structural model explaining hospital service mix and sharing (discussed in the preceding theoretical section).
Dependent Variables
We used ten service aggregates based on the service groupings previously described: the percent change in the total number of 1) quality-enhancing; 2) complexity-expanding; and 3) community-oriented services; plus 4) the total of 1, 2, and 3; two alternative service aggregates 5) supportive versus 6) competitive; and 7) rapidly diffusing versus 8) peaked or declining; and finally, the percent change in the number of 9) administrative and 10) clinical services shared by a hospital. Respiratory therapy, hemodialysis and outpatient abortion services had to be dropped due to non-reporting and other missing values problems.
We calculated annualized rates of change in service levels using the average number of services during the year as a base. For example, the rate of change in the S-th service aggregate in year t = [St − St−1/(St + St−1)/2]·100. Thus, for a hospital adding its first service, the rate of change would be 200 percent (=100·(1 − 0)/(1 + 0)/2). Using this formula avoids the problem of dividing by zero if base period levels were used in the denominator.
In addition to the service aggregates, we also analyzed selected services individually using a 0, 1 adoption dummy as a dependent variable. This analysis allowed us to go behind the aggregate results to see exactly where rate-setting was having its greatest effect. We used the same independent variable specification for both the aggregated and disaggregated dependent variables (except for the exclusion of a lagged dependent variable in the 0, 1 specification).
Independent Variables
We included the independent variable list to control for other, exogenous changes in medical and economic conditions that might be confounded with the implementation of rate-setting at the State level. Demand-side variables include those affecting medical need and ability-to-pay, while supply-side factors reflect the hospitals' willingness and ability to provide a broader scope of services. We will discuss each of the four categories briefly.
Medical need is measured by:
The percent of Aid to Families with Dependent Children (AFDC) recipients in a county (AFDC);
Births per 10,000 population in a county (BIRTH);
Crimes per 100,000 population in a county in 1975 (CRIME);
Population and population density per square mile in a county (P, POPDENS);
The percent of the population enrolled in Medicare Part A in a county (MEDCAR);
The percent of the white population in a county (WHITE); and
SMSA/Rural location (DSMSA).
A large number of AFDC recipients and areas with high birth rates should place greater demands on hospital outpatient services and lesser demands on the more complex technologies oriented to the middle-aged and elderly. High crime areas are likely to require more of all services—particularly complex services like ICUs. Elderly populations are also likely to need more of all services, such as cancer therapies, ICUs, and home care. Non-whites are also more likely than whites to need hospital care, especially community services that substitute for lack of primary care physicians, although many studies have shown less hospital inpatient use for blacks (U.S.DHEW, 1979; Cromwell and Schurman, 1981). Finally, large, dense, urban areas in general present a tense, fast-paced style of living that can result in greater need, due to accidents, heart attacks, neuroses, and psychoses.
Ability-to-pay is captured by:
Income per capita in the county (INCOME);
The percent of the population with commercial or Blue Cross insurance in a county (COMMINS);
Average years-of-schooling per person in a county (EDUC);
The unemployment rate (UNEMRT); and
AFDC, MEDCAR.
Wealthier, better insured populations should be able to afford a wider variety of hospital services. COMMINS, together with AFDC and MEDCAR, provides a comprehensive measure of insurance coverage. Better educated populations may or may not demand more services, depending on their use of preventive care, work and life styles, and their living standards. High unemployment rates should be inversely correlated with ability-to-pay, although lower time prices may encourage elective hospital use.
Factors affecting hospital willingness and ability to provide a broader scope of service include:
Ownership status—for-profit, private, and public voluntary (PROF, NONPROF, GOV);
Bed size (0-100 beds, BEDSZ1; 100-200, BEDSZ2; 200-400, BEDSZ3; 400 +, BEDSZ4);
Teaching status (MAPP5);
The number of active physicians per capita in a county (MDPOP);
Ratio of specialty to total physicians in a county (SPMD);
The number of community hospitals in a county (NHOSPS);
The number of for-profit hospitals in a county (NPROF);
The number of government-operated hospitals in a county (NGOVT); and
The percent of community hospitals in a county with medical school affiliation (TEACH);
plus two regulatory variables affecting service expansion directly or indirectly:
Professional Standards Review Organization (PSRO) binding review (PSRO = 1 for years covered, else = 0); and
Certificate of Need binding review (CN = 1 for years covered, else = 0).
For-profit hospitals in general provide a narrower scope of services due to negative incentives to cross-subsidization. The only reasons a proprietary hospital would continue to provide an unprofitable service would be if it were a necessary complement to other, profitable services or if the hospital wanted to maintain an image of a high quality community institution. Public voluntaries—city and county hospitals—on the other hand, attempt to fill service gaps left by the private sector. Larger hospitals will also provide a broader mix, other things being equal, because of the diversity of illnesses treated and because of scale economies. Teaching hospitals should provide a broader mix for educational reasons—particularly complex services involving the latest technologies. Both bed size and teaching status of a hospital could be considered endogenous to rate-setting over several years. To minimize this problem, hospitals have been placed in bed size groupings. Furthermore, instead of using a continuous measure of teaching status, such as the number of interns and residents, we used a dichotomous, 0-1 affiliation measure; presumably very few hospitals will have completely given up their affiliation because of rate-setting within the evaluation period.
Physician concentration in a market area—particularly specialists—should place a greater demand on hospitals to treat a variety of illnesses, both of residents and in-migrants. Their effect may be less, however, on the perceived need for community services.
We have included four additional variables to reflect the extent of inter-hospital competition. For a given population, two offsetting competitive effects are at work. A concentration of hospital beds in fewer institutions would permit each institution to broaden its mix by capturing a greater percentage of the market (the concentration effect). With fewer providers, however, pressure may be lessened to add new services to maintain a target occupancy rate (the competitive effect). Provider competition would also be shaped by the mix of hospitals in the area. Greater for-profit dominance should dampen service competition, while more teaching hospitals could conceivably foster competition unless nonteaching hospitals limited their competition by specializing in community-oriented services.6
PSROs, if effective, could indirectly affect service expansion by curtailing demand for care—mostly through admissions review. Certificate of Need should have a direct, negative effect on unnecessary expansion. In addition to these regulatory activities, we included several variables reflecting State rate-setting programs to test for the impact of revenue control on service diffusion and sharing. (See the following section for a discussion.)
Functional Specification and Estimation
While hospitals may adopt services in continuous packages (subject to minimum investment levels), the AHA reports only whether the service is offered or not. If, in addition, hospitals adopt only one or at most, two, services in any given year due to the expense involved, a reciprocal, inverse relationship is established between current adoption rates and previous adoption levels. That is, adding the first service implies an infinite adoption rate (which we have scaled down to a 200 percent increase) while the eleventh service represents only a 10 percent change. To account for this algebraic relationship between base period levels and rates of change, the lagged service level was included as an independent variable along with the other variables listed above. The following specification was used.7
| (2) |
where %ΔYt = percent change in adoption or sharing in hospital j (subscript suppressed) in year t; Yt−1 = lagged service level; Xit = vector of i exogenous variables; Tt = annual time dummy (a separate dummy for each year); DCt = 0, 1 dummy for study-control group (referred to as NONPR in the following regression list); DSt = 0, 1 dummy for individual States in the PR study group; and DSAt = 0, 1 dummy for the years in which a PR program is operational in a particular State. Incorporating time and PR-non-PR dummies in this fashion establishes a powerful, four-way, pre/post, study/control evaluation design. Adding other exogenous variables and lagged service levels further reinforces our confidence that no important omitted variables may result in spurious correlations between rate-setting activity and service diffusion/sharing.
We can easily generalize the PR specification to account for multiple programs within a State or time-related program changes simply by creating a new PR dummy covering a particular hospital subset or time period. The New York program, for example, introduced some significant changes in 1976, five years after the first formula went into effect. This effect is captured by two New York rate-setting dummies: DNY71 = 1 for all New York hospitals from 1971-1978, else 0; and DNY76 = 1 for New York only beginning in 1976. We can derive total program impact in overlapping years from the addition of the two associated regression coefficients.
We used ordinary least squares regression on a pooled cross-section of time-series on over 2,500 hospitals for 10 years, 1969-1978, to test for the rate-setting effect on service adoption and sharing.8 (To calculate percent changes, the first year of the series, 1969, had to be dropped.) We specified all variables in linear terms, and coefficients can be interpreted as marginal contributions to the annual percent change in the dependent variable. Employment of annual time and State-specific dummies along with PR dummies for particular years in study States permits a direct interpretation of the rate-setting effect. That is, we can interpret a significant PR coefficient as the additional impact rate-setting had in a particular State over and above the national time trend in diffusion, trends in the control group, and trends in the State itself prior to PR. Negative PR coefficients imply slower (but not necessarily negative) adoption rates in rate-setting States when examining various service aggregates. For particular services that are being phased out, such as radium therapy, negative coefficients imply even faster discontinuation in PR States.
Econometric Results: Service Adoption
Tables 6 and 7 present results for the eight adoption aggregates: the percent change in total services (CTOT); quality-enhancing services (CQUALEN); complex services (CCMPLEX2); community services (CCOMMUN2); supportive services (CSUPP); competitive services (CCOMPET); rapidly diffusing services (CDIFFUS); and peaked services (CPEAK). Because of the long independent variable list, only explanatory variables with t-ratios exceeding 1.46 (an 85 percent confidence level) in any equation have been displayed. (All others were entered but proved completely insignificant by any standard.) The list begins with demand and supply factors, followed by regulatory dummies (if at all significant), a study-control group dummy (State dummies are not shown for purposes of brevity), and, finally, the PR-specific variables, identified by two digit numbers following the State's initials, (for example, DAZ 74 represents the Arizona PR program beginning in 1974).
Table 6. Regression Results: Total, Quality, Complex, and Community Service Aggregates.
| Dependent Variable: CTOT R2 = .065 F(94, 20454) = 17.8 |
Dependent Variable: CQUALEN R2 = .08 F(94, 20630) = 23.5 |
Dependent Variable: CCMPLEX2 R2 = .07 F(94, 20630) = 19.5 |
Dependent Variable: CCOMMUN2 R2 = .064 F(94, 20454) = 17.6 |
|
|---|---|---|---|---|
| Explanatory Variable | Estimated Coefficient | Estimated Coefficient | Estimated Coefficient | Estimated Coefficient |
| Intercept | 0.57** | −0.51** | ||
| Lag | −0.027** | −0.11** | −0.09** | −0.09** |
| D73 | 0.03** | |||
| D75 | 0.016* | 0.023* | ||
| D78 | 0.034** | |||
| AFDC | 0.004** | |||
| BIRTH | −0.017** | −0.02† | −0.02* | |
| CRIME (per Capita) | 0.23† | 0.39** | ||
| P(millions) | 0.013† | 0.028* | ||
| POPDENS(1000/sqmi.) | 0.14** | 0.09* | 0.118* | 0.24** |
| MEDCAR | −0.32** | −0.45** | −0.336** | −0.29** |
| WHITE | 0.065** | 0.18** | ||
| INCOME(000) | −0.008* | 0.007† | ||
| COMMINS | 0.074* | |||
| EDUC | 0.011** | |||
| UNEMRT | −0.28** | −0.266† | −0.446* | |
| NONPR | 0.29** | 0.32† | 0.76** | |
| PROF | −0.045** | −0.055** | −0.047** | −0.049** |
| GOV NONFED | 0.016** | |||
| BEDSZ1 | −0.21** | −0.187** | −0.33** | −0.20** |
| BEDSZ2 | −0.128** | −0.081** | −0.216** | −0.13** |
| BEDSZ3 | −0.067** | −0.039** | −0.113** | −0.071** |
| MAPP5 | 0.056** | 0.029** | 0.074** | 0.073** |
| SPMD | 0.001** | 0.001** | 0.001** | 0.001** |
| NPROF | 0.001** | |||
| TEACH | −0.33** | −0.059** | −0.061** | 0.031† |
| MDPOP | 8.266** | |||
| NHOSPS | −0.001 * | |||
| DAZ74(AZ 74-8) | 0.072** | |||
| DKY75(KY 75-8) | 0.066** | |||
| DWI73(WI 73-8) | 0.062** | |||
| DMNA75(MN 75-8) | −0.042** | −0.079** | ||
| DNY71(NY 71-8) | −0.036** | −0.07** | ||
| DNY76(NY 76-8) | −0.034* | |||
| DWA78 | −0.086† |
Significant at the 85% confidence level.
Significant at the 90% confidence level.
Significant at the 95% confidence level.
Table 7. Regression Results: Supportive, Competitive, Diffusing, and Peaked Service Aggregates.
| Dependent Variable: CSUPP R2 = .07 F(94, 20652) = 19.91 |
Dependent Variable: CCOMPET R2 = .05 F(94, 20454) = 13.66 |
Dependent Variable: CDIFFUS R2 = .08 F(94, 20456) = 20.82 |
Dependent Variable: CPEAK R2 = .08 F(94, 20456) = 22.03 |
|
|---|---|---|---|---|
| Explanatory Variable | Estimated Coefficient | Estimated Coefficient | Estimated Coefficient | Estimated Coefficient |
| Intercept | ||||
| Lag | −0.07** | −0.05** | −0.08** | −0.06** |
| D71 | −0.04** | |||
| D72 | −0.01* | |||
| D73 | −0.02* | 0.02** | ||
| D75 | 0.02* | 0.03* | ||
| AFDC | 0.002* | |||
| BIRTH | −0.02† | |||
| CRIME (per capita) | 0.42** | |||
| P (millions) | 0.01† | 0.02† | 0.01* | |
| POPDENS (1000/sqmi.) | 0.10** | 0.16** | 0.20** | 0.08** |
| MEDCAR | −0.41** | −0.33** | −0.42** | −0.31** |
| WHITE | 0.06* | 0.096** | 0.05** | |
| COMMINS | −0.10** | |||
| EDUC | 0.01** | |||
| UNEMRT | −0.35† | −0.21† | ||
| NONPR | 0.30** | |||
| PROF | −0.06** | −0.04** | −0.05** | −0.04** |
| GOV NONFED | 0.01† | |||
| BEDSZ1 | −0.19** | −0.24** | −0.32** | −0.18** |
| BEDSZ2 | −0.08** | −0.17** | −0.19** | −0.12** |
| BEDSZ3 | −0.03** | −0.10** | −0.10** | −0.06** |
| MAPP5 | 0.03** | 0.086** | 0.09** | 0.40** |
| SPMD | 0.001** | 0.001** | 0.002** | 0.001** |
| NPROF | 0.001* | 0.001** | ||
| TEACH | −0.06** | −0.03** | ||
| MDPOP | 7.14* | 4.55† | ||
| NHOSPS | −0.001* | |||
| DC072 | 0.05† | 0.09** | ||
| DMNA75(MN 75-8) | −0.05* | −0.09** | ||
| DNY71(NY 71-8) | −0.076** | −0.08** | ||
| DWPVPR(WT. PA. PR) | −0.04* | |||
| DMNB78 | 0.10* | 0.72† | ||
| DWA78 | − 0.08* | −0.10* | 0.52† |
Significant at the 85% confidence level.
Significant at the 90% confidence level.
Significant at the 95% confidence level.
All eight medical need variables proved to be significant in one or more equations, but not all with the predicted sign. The urbanization variable was positively related to all eight adoption rates, while the crime, population, percent of population that is white, and AFDC variables were positively associated with various subsets of the eight groups. The population variable, for example, was positively correlated with to-total, complexity-expanding, supportive, diffusing, and peaked service groupings. The elderly population and birth rate variables, conversely, were usually negatively related to adoption rates. The AFDC variable was postively correlated with community and competitive services. This finding is interesting, given that the diffusing and competitive groups contain many of the same services, and it suggests a more intensive use of outpatient facilities by the poor.
Ability-to-pay variables were much less successful in explaining adoption rates. Unemployment rates were negatively associated with adoption, as predicted; per capita income positively related to community services only, and commercial insurance negatively related to competitive services. Finally, education levels were positively related to the complex and diffusing service groups.
Among the variables that characterize the individual hospital and the hospital market area, for-profit hospitals and hospitals in the three smallest bed size categories (the over 400 bed size category is the omitted category) were negatively correlated with all eight service groups. Government, non-Federal hospitals tend to adopt community services rapidly, while teaching hospitals exhibited high adoption rates for all types of services. Physician specialty mix showed a strong positive correlation with service adoption since specialists make use of a wide variety of sophisticated medical technologies and community-oriented outpatient services. Holding the specialist mix constant, the number of physicians per capita was positively associated only with quality-enhancing and supportive services and not those competitive services that continue to diffuse rapidly.
Industry variables provide mixed results as well. The total number of hospitals in an area was negatively correlated with complexity-expanding services, suggesting a dominance of the concentration over the competitive effect: that is, fewer, more concentrated providers have less competitive pressure to add services but a broader patient base to support them. However, the number of for-profit hospitals in an area was positively correlated with adoption rates for competitive, complexity-expanding services, possibly due to a lagged competitive effect. Finally, the percent of teaching hospitals in an area was negatively correlated with adoption, reflecting greater opportunities for referrals to tertiary institutions (a specialization effect).
Turning to the regulatory variables, we discovered no impact for either PSROs or Certificate of Need programs in curtailing service adoption in any grouping. Individual programs may well be successful but not as a group across broad geographic boundaries. PSROs were not expected to exert much influence on service mix given the indirect chain of causation, but C/N programs have a direct mandate to discourage the proliferation of redundant services. Previous work by Salkever and Bice (1976) and Policy Analysis (1982) found no C/N effect either; all of the impact occurred in the elimination of underused beds. Our null findings confirm their results.
While many PR programs influenced diffusion, only a few attained statistical significance by conventional standards. Because of the quality of data, we relaxed confidence levels to 15 percent levels (t = 1.46), keeping in mind the tentativeness of the findings.
Referring again to Table 6, our findings indicate that two of the fifteen State programs showed significant retarding effects on all 24 services as a group (CTOT). The 1975 Minnesota program, a voluntary initiative, showed an overall negative effect on adoption, stemming from a significant retarding of complex, competitive, rapidly diffusing services. The 1971 mandatory New York program also exhibited an overall limiting effect on the adoption of the quality-enhancing, community, supportive, and rapidly diffusing services. In addition, although no other program had a statistically significant effect on all services together, the 1978 Washington program apparently reduced adoption rates for the complex, competitive, rapidly diffusing services. This effect apparently was offset, however, by a positive correlation in the peaked service grouping.
Since we obtained only limited results using various service aggregates, our next step was to examine individual services. Toward this end, we selected 13 of the 24 services for individual analysis. The services selected included two quality-enhancing, seven complexity-expanding, and four community services. Selection was based primarily on whether the service was rapidly diffusing or being eliminated, in order to measure any additional impact that PR had on the ongoing diffusion process. We ran ordinary least squares (OLS) regressions using a 0, 1 (or 0, 1, 2 for radium + X-ray therapy) dependent variable for each service using the same specification as we described previously (without lagged levels).9 Table 8 presents the results, providing only statistically significant PR coefficients. Full regressions, including the other explanatory variables, are available from the authors upon request.
Table 8. Rate-Setting Regression Coefficients, Selected Facilities and Services.
| State Program | Complex Services | Quality Enhancing | Community Services | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Radio-therapy | ICU | Open Heart | EEG | Radio-isotopes | Burn Care | Physical Therapy | Premature Nursery | Pathology Lab | Social Work | Outpatient Department | Emergency Department | Psychiatric Emergency | |
| Arizona | |||||||||||||
| Voluntary (Vol.), 1974-78 | .10** | −.06* | −.06† | −.05† | |||||||||
| Connecticut | |||||||||||||
| Voluntary (Vol.), 1969-72 | −.11* | .1.0* | |||||||||||
| Mandatory (Man.), 1975-78 | −.11** | ||||||||||||
| Kentucky | |||||||||||||
| Voluntary (Vol.), 1975-78 | .05* | −.04† | .03† | −.05* | −.03† | −.04* | |||||||
| Maryland | |||||||||||||
| Mandatory (Man.), 1975-78 | −.12† | −.15** | .17** | −.13* | −.14** | ||||||||
| Mandatory (Man.), 1976-78 | −.13** | −.10** | |||||||||||
| Massachusetts | |||||||||||||
| Mandatory (Man.), 1975-78 | −.07* | −.06† | −.06† | ||||||||||
| Mandatory (Man.), 1976-78 | −.06† | ||||||||||||
| Minnesota | |||||||||||||
| Voluntary (Vol.), | −0.7** | −.04† | −.04† | −.08** | |||||||||
| Mandatory (Man.), 1978 | −.09* | −.07† | |||||||||||
| Mandatory (Man.), Rev. 78 | −.15** | −.09† | |||||||||||
| Nebraska | |||||||||||||
| Voluntary (Vol.), 1973-78 | −.08* | .07** | .14** | ||||||||||
| New Jersey | |||||||||||||
| Mandatory (Man.), 1975-78 | −.08** | −.10** | .04† | −.03* | −.05† | −.08** | −.06* | ||||||
| New York | |||||||||||||
| Mandatory (Man.), 1971-78 | −.04** | −.04* | −.04† | .03* | |||||||||
| Mandatory (Man.), 1976-78 | −.06** | −.03† | −.03** | −.04** | −.02† | −.02** | .05** | −.05** | −.03** | ||||
| Rhode Island | |||||||||||||
| Mandatory (Man.), 1973-78 | −.14† | ||||||||||||
| Western Pennsylvania | |||||||||||||
| Voluntary (Vol.), 1971-78 | −.14** | −.08** | .06† | −.02* | −.08** | .06* | |||||||
| Washington | |||||||||||||
| Mandatory (Man.), 1976-78 | .02* | ||||||||||||
| Mandatory (Man.), 1978 | −.10** | .02* | −.05† | ||||||||||
| Wisconsin | |||||||||||||
| Mandatory (Man.), 1973-78 | −.06† | −.05** | −.08** | −.09** | −.04* | .05** | |||||||
Significant at the 85% confidence level.
Significant at the 90% confidence level.
Significant at the 95% confidence level.
Unlike the more aggregated findings, these results indicate that many PR programs are having an effect in the desired direction, as evidenced by the negative correlations with rapidly diffusing services, such as intensive care, open-heart surgery, social work, physical therapy, and EEG. Further, several programs are negatively correlated with premature nursery, a service that is declining nationally, indicating an even more rapid phasing-out in PR States. Although premature nursery can be considered a quality-enhancing service, it is unlikely that hospitals are simply dropping this particular service. Rather, the negative coefficient indicates the discontinuation of maternity care itself, a natural response to declining birth rates. Although the New York program, arguably the most stringent in the country, is positively correlated with the adoption of this service, this paradoxical finding does not indicate that premature nurseries are diffusing in New York. In fact, premature nurseries were provided by 48 percent of New York hospitals in 1969, falling to only 41 percent by 1978. This figure compares to a nationwide decrease from 50 to 34 percent over the same time period.
Among the individual programs, New York's exhibits the most consistent, significant negative effects. The program appears to have had the greatest influence on selected complexity-expanding services, as evidenced by the negative correlations for six of the eight services in the group. New York also retarded the diffusion of social work departments, one of the most rapidly diffusing community services across the nation.
The Minnesota program, a voluntary program implemented in 1975 and made mandatory in 1978, shows a negative correlation with the complexity-expanding group as a whole that stems from the program's retarding effects on ICU, EEG, and physical therapy. Besides influencing these complex services, the Minnesota program also apparently retarded the diffusion of pathology labs and social work departments.
Besides New York and Minnesota, several other programs, including New Jersey, Maryland, Massachusetts, and Wisconsin, exhibited slower adoption rates for many services. That these programs do not show negative effects for the various service aggregates can be attributed to: (1) limited impact on only a few services, or (2) offsetting unexplained positive impact in a few instances (for example, EEG in New Jersey).
Econometric Results: Service Sharing
Table 9 presents the results for two service sharing aggregates: the percent change in administrative (CADMIN) and clinical (CCLIN) services. Because so few of the clinical services are ever shared, the list was narrowed to the four most often shared: blood bank, lab/pathology, physical therapy, and diagnostic radiology.
Table 9. Regression Results, Administrative, and Clinical Service Sharing.
| Dependent Variable: CADMIN R2 = .05 (F94, 20658) = 14.32 |
Dependent Variable: CCLIN R2 = .02 (F94, 20658) = 4.72 |
|
|---|---|---|
| Explanatory Variable | Estimated Coefficient | Estimated Coefficient |
| Intercept | −.644** | |
| Lag | −.058** | −.027** |
| D71 | −.063** | |
| D72 | .05** | .025** |
| D73 | .088** | −.019** |
| D74 | −.09* * | .018** |
| D78 | −.05** | −.026** |
| AFDC | −.002† | |
| CRIME (per capita) | .3** | |
| POPDENS(1000/sqmi.) | −.02** | |
| WHITE | .087* | .05* |
| INCOME (000) | −.01** | |
| COMMINS | .048† | |
| EDUC | .012** | |
| UNEMRT | −.80** | |
| NONPR | .073** | |
| PROF | −.128** | −.045** |
| GOV NONFED | −.029** | |
| BEDSZ1 | −.036** | |
| BEDSZ2 | −.028** | |
| BEDSZ3 | −.013† | |
| C/N | .021* | .009† |
| TEACH | −.04* | −.021† |
| MDPOP | 8.50† | 6.23* |
| DAZ74(AZ 74-8) | .10** | |
| DCT75(CT 75-8) | −.12* | |
| DKY75(KY 75-8) | −.03* | |
| DRI73(RI 73-8) | .439** | |
| DWI73(WI 73-8) | .039** | |
| DMD76(MD 76-8) | −.125* | |
| DNY71(NY 71-8) | −.056† |
Significant at the 85% confidence level.
Significant at the 90% confidence level.
Significant at the 95% confidence level.
Summarizing, first, the effects of the exogenous variables, only a few of the medical need variables show significant effects, primarily in the sharing of administrative services. The crime rate and white population variables show a positive correlation with the administrative group. The AFDC and population density variables are negatively correlated with the administrative group.
The ability-to-pay variables exhibit no easily identifiable trends. The income and unemployment rate variables correlate negatively with administrative sharing, while the education variable is positively related. The insurance coverage variable is positively correlated with clinical service sharing, an effect that is counter-intuitive. Higher income, better insured populations were expected to discourage sharing, particularly for clinical services.
As for specific hospital characteristics, proprietary and public hospitals appear to enter sharing arrangements less often, holding other things such as the number of hospital beds constant. Very small hospitals (those with under 100 beds) also showed a negative correlation with administrative service sharing, while the 100-400 bed size hospitals evidently share fewer clinical services, compared to larger institutions. The number of teaching hospitals in an area also discouraged sharing of both administrative and clinical services, while physician density showed a positive association with sharing in general. In marked contrast to the adoption results, C/N showed a positive sharing effect on both service groups.
PR-specific effects are rather limited. Two programs exhibit positive correlations: Arizona for administrative services; and Wisconsin for the clinical group. A few rate-setting programs are actually negatively correlated with service sharing: Connecticut, Maryland, and New York, with the administrative group; and Kentucky and Rhode Island with the clinical group. Negative signs do not necessarily indicate that sharing is falling in absolute terms. Rather, sharing may be increasing in these States but at a slower rate than in the rest of the country. However, the finding that New York does not show a positive PR effect on sharing, given the earlier findings on adoption, Is further reason to doubt the presence of any meaningful PR effect on hospitals' willingness to enter sharing arrangements.
This does not mean that rate-setting never leads to greater hospital sharing in a few cases for selected services. Nonetheless, while the data are crude, aggregated measures which may hide some of the effect, it is unlikely for a large PR effect on sharing to go undetected. Of the many possible responses to effective revenue constraints, hospitals would seem more likely to internalize the changes in the first instance (for example, reducing staff, or cross-subsidizing), and leave for later any active program for sharing services above and beyond that which would occur naturally (for example, EDP remote terminal sharing).
Conclusions and Policy Implications
Many high technology, complex services continued to diffuse rapidly during the past decade. Most of these services add significantly to the costs of hospital care, and their cost-effectiveness can legitimately be questioned in certain instances where use is low or a lower cost modality is available, such as a free-standing neighborhood clinic. New services spawned by new technologies (CAT scanning and catheterization) appear constantly on the horizon, making the issue of service coordination an increasingly salient one. From a regulatory perspective, the question is whether the hospital industry will, when confronted with externally imposed revenue constraints, rationalize the service mix by phasing out underused or obsolete services.
Our findings regarding the impact of hospital rate-setting suggest cautious optimism. Diffusion rates in States with mandated rate-setting are definitely lower than elsewhere. Complex services were diffusing at only about three-fourths the rate in PR study hospitals, as compared with a random sample of hospitals nationwide (15.2 percent versus 21.4 percent); community services were diffusing at only two-thirds the control-group rate (20 percent versus 28 percent).
Care should be taken in interpreting such differences, however. Only two States, Minnesota and New York, show retarding effects on service proliferation once other influential variables are held constant. If rate-setting does have an indirect, lagged effect on adoption, we should see it in New York, which has the oldest, most stringent program in the country-Why Minnesota's program has had such a broad effect is unexplained by the program's relative immaturity and voluntary nature prior to 1978; health maintenance organization (HMO) expansion may be the key to the explanation.
When services are analyzed individually, we do find retarding effects in otherwise rapidly diffusing services in many States: New Jersey, Washington, Maryland, Wisconsin, and Massachusetts. ICUs, open heart surgery, EEGs, radioisotopes, physical therapy, and the social work department appear to be the most affected by rate-setting. Except for the outpatient department in New Jersey and the emergency department in New York and Kentucky, we found no PR effect on these two key outpatient services, and even this finding is qualified by the fact that in New York, 98 out of every 100 hospitals still offer some form of emergency care.
Prospective reimbursement programs differ greatly in key factors: some require mandatory hospital participation, others do not; some cover a majority of patients, others cover only one or two groups; some use rigorous screens, others minimize the role of inter-hospital comparisons; and finally, some are simply older, more mature programs with a longer regulatory history. New York typifies the mature, comprehensive system with mandatory participation and formulistic screens. Thus, it is not surprising to find the most dramatic effects on service diffusion in New York. And, along with the extension of the program to more payers and the implementation of even tighter screens, we see even greater declines in service proliferation.
Evidence from the other programs suggests that of the key characteristics, mandatory participation, broad payer scope, and time for hospitals to accept and structurally respond to rate-setting are most salient in depressing service adoption rates. New Jersey and Maryland, which are most like New York, show only limited effects on diffusion, possibly because of the few years a comprehensive, mandatory program has been in place, at least as of 1978.
When it comes to sharing services, rate-setting appears to have little or no influence. Of 20 key administrative and clinical services, PR hospitals shared only 3.6 in 1977. While this is one service more than the number shared among control hospitals, we can attribute no systematic difference to the introduction of rate-setting. Very narrow case studies of particular services in selected States may be required to isolate a PR effect on sharing.
We found no overall impact on diffusion or sharing for either the Certificate of Need or the PSRO program. This does not mean individual programs are not truly effective; PR programs as a whole have little influence on either diffusion or sharing. But the primary focus of this evaluation was rate-setting, not C/N or PSROs. It is quite possible that in States where PR does show a retarding effect, some joint C/N-rate-setting impact is being measured. New York's C/N program may well share materially in the credit for reductions in service proliferation, but because C/N has been in effect longer than our evaluation period, it is statistically impossible for us to separate out its effect from other factors unique to the State of New York.
As to the diffusion of services in the hospital industry generally, one final point seems relevant to public policy. Because industry structure and physician mix have major, long run impacts on diffusion, one long run policy approach to controlling the spread of unnecessary services involves limiting the number and distribution of new specialists, thereby reducing competitive pressures among hospitals for the latest technologies. With fewer specialists and more primary care physicians in a community, preventive care may also receive more emphasis, further reducing the need for more ICUs and other esoteric technologies.
Acknowledgments
Support for this study comes from HCFA Contract No. 500-78-0036.
Footnotes
Examples of the approach include: Kerr (1978); Maloney and Lasky (1979); Rice (1979); Ellis (1978); Brown (1976); Vraciu and Zuckerman (1979); Gilbertson (1977); and Townsend and Lucas (1979).
For discussion of the non-empirical literature on rate-setting and service diffusion, see Warner (1978).
For a more detailed review of program characteristics, see Coelen (1981), and the State case studies of the NHRS Study referenced by authors.
Berry's groupings were approximated, in that emergency department and diagnostic radioisotope, two basic services, were placed in the community service and complex service categories, respectively.
We did not examine basic services since they form the basic core of all hospitals.
For a model of segmented market competition, see Lee (1971).
This functional specification does not correspond to the logistic curve discussed in the theory section, although it draws from the same theoretical roots. We could not estimate a true logistic curve because of the lack of adoption information for all hospitals in a market area; we had data only on a random, unclustered, national sample. Thus, the hospital, rather than the market area, had to be the unit of analysis. Variables that influence area-wide adoption rates, however, should be the same as those influencing individual hospitals (for example, teaching hospitals should adopt sooner and more often).
The lagged dependent variable proved uncorrelated with the error term in the regressions, obviating the need for more complicated adjustments for serial correlation.
OLS is not the most efficient procedure for analyzing binary data with a concentration of values at zero. Other techniques, such as probit, were not practical, however, on such a large data base. Russell (1979) also used OLS techniques to predict adoption, arguing for the asymptotic properties of larger samples to eliminate serious, abnormal sampling errors.
References
- Astolfi A, Matti L. Survey Profiles Shared Services. Hospitals. 1972 Sep 16;46 [PubMed] [Google Scholar]
- Berry RE., Jr On Grouping Hospitals for Economic Analysis. Inquiry. 1973 Dec;10:5–12. [PubMed] [Google Scholar]
- Boland J, Reilly H. Vol I of “National Hospital Rate Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Arizona. [Google Scholar]
- Brown M, editor. Topics in Health Care Financing-Shared Services. 1976 Summer;2 [Google Scholar]
- Coelen C, Sullivan D. An Analysis of the Effects of Prospective Reimbursement Programs on Hospital Cost. Health Care Financing Review. 1981 Winter;2(3) [PMC free article] [PubMed] [Google Scholar]
- Coleman J, Katz E, Menzel H. Medical Innovation-A Diffusion Study. New York: Bobbs-Merrill Company; 1966. [Google Scholar]
- Cromwell J, et al. Analysis of Prospective Payment Systems for Upstate New York. 1976 Final report prepared for DHHS under Contract No. HEW-OS-74-261. [Google Scholar]
- Cromwell J. The Impact of Rate Regulation on the Diffusion of New Technologies in Hospitals. Cambridge, Massachusetts: Abt Associates, Inc.; Oct, 1976. Discussion Paper No. HCSA-1. [Google Scholar]
- Cromwell J, Schurman R. Tennessee PSRO/Medicaid Analysis. 1981 Report prepared for the Health Care Financing Administration under contract #500-79-0037. [Google Scholar]
- Ellis B. New Sharing Arrangements Meet Hospitals' Technical Support Needs. Hospitals. 1978 Aug 16;52(16):108–110. [PubMed] [Google Scholar]
- Gaumer G, et al. Vol II of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Connecticut. [Google Scholar]
- Gilbertson E. Shared Clinical Services Provide a Chance for Specialties to Thrive. Hospitals. 1977 Mar 1;51:89–93. [PubMed] [Google Scholar]
- Ginsburg P. The Diffusion of Hospital Technology. Feb, 1977. unpublished paper. [Google Scholar]
- Griliches Z. Hybrid Corn: An Exploration in the Economics of Technological Change. Econometrica. 1957 Oct;25:501–522. [Google Scholar]
- Hamilton D, et al. Vol VIII of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Washington. [Google Scholar]
- Hamilton D, et al. A Comparative Review of Nine Prospective Rate-Setting Programs. 1980 Jan; First Annual Report of the National Hospital Rate-Setting Study prepared for DHHS under Contract No. HCFA-500-78-0036. [Google Scholar]
- Hamilton D, Kamens G. Vol VII of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in New York. [Google Scholar]
- Kaluzny A, et al. Diffusion of Innovative Health Care in the United States: A Study of Hospitals. Medical Care. 1970 Nov-Dec;8:447–487. doi: 10.1097/00005650-197011000-00005. [DOI] [PubMed] [Google Scholar]
- Kerr F. The Myth and Reality of Shared Services. Trustee. 1978 Nov;31(11):28–30. [PubMed] [Google Scholar]
- Kimberly J. Hospital Adoption of Innovation: The Role of Integration into External Informational Environments. Journal of Health and Social Behavior. 1978 Dec;19:361–373. [PubMed] [Google Scholar]
- Lee J, Weisbrod B. Collective Goods and the Voluntary Sector: The Case of the Hospital Industry. Center for Medical Sociology and Health Services Research, University of Wisconsin; Madison: Aug, 1974. [Google Scholar]
- Lee J, Weisbrod B, Jensen G. Vol V of “National Hospital Rate-Setting Study/” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Minnesota. [Google Scholar]
- Lee ML. A Conspicuous Production Function Theory of Hospital Behavior. Southern Economic Journal. 1971 Jul;:48–58. [Google Scholar]
- Maloney S, Lasky P. Shared Services Arrangements. American Health Care Association Journal. 1979 Mar;:3–8. [PubMed] [Google Scholar]
- Mansfield E. Industrial Research and Technological Innovation. New York: W. W. Norton and Company; 1968. [Google Scholar]
- Policy Analysis, Inc. Evaluation of the Effects of Certificate of Need Programs. 1981 Jan; Final report prepared for DHHS/HRA under Contract No. 231-77-0114. [Google Scholar]
- Rapoport J. Diffusion of Technological Innovation in Hospitals: A Case Study of Nuclear Medicine. National Center for Health Services Research; 1974. unpublished monograph. [Google Scholar]
- Rice J. Hospitals Must Follow Strategy to Lead Regional Sharing Efforts. Hospitals. 1979 Mar 1;53:59–61. [PubMed] [Google Scholar]
- Russell L. Technology in Hospitals: Medical Advances and their Diffusion. The Brookings Institution; 1979. [Google Scholar]
- Salkever D, Bice T. The Impact of Certificate of Need on Hospital Investment. Inquiry. 1976 Spring; [PubMed] [Google Scholar]
- Sumner M, Gaumer G. Vol IX of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Western Pennsylvania. [PubMed] [Google Scholar]
- Taylor E. Participation in Shared Programs Up Sharply, Survey Discloses. Hospitals. 1977 Jul 16;51:192–198. [PubMed] [Google Scholar]
- Taylor E. Survey Shows Who is Sharing Which Services. Hospitals. 1979 Sep 16;53 [PubMed] [Google Scholar]
- Townsend J, Lucas F. Six-Year Program Shows Benefits of Shared Laboratory Services. Hospitals. 1979 Mar 16;53:107–112. [PubMed] [Google Scholar]
- U.S. Department of Health, Education and Welfare. Health: United States 1979. DHEW Publication No. (PHS) 80-1232. [Google Scholar]
- Vraciu R, Zuckerman H. Legal and Financial Contraints on the Development and Growth of Multiple Hospital Arrangements. Health Care Management. 1979 Winter;:39–47. [PubMed] [Google Scholar]
- Wagner J, et al. A Study of the Impact of Reimbursement Strategies on the Diffusion of Medical Technologies. 1982 Jun; Final report prepared for DHHS/HCFA under Grant No. 18-P-97113/3-01. [Google Scholar]
- Walter R, DeMarco J. Vol IV of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Massachusetts. [Google Scholar]
- Warner K. The Need for Some Innovative Concepts of Innovation: An Examination of Research on the Diffusion of Innovations. Policy Sciences. 1974;5:433–451. [Google Scholar]
- Warner K. unpublished doctoral dissertation. Yale University; 1975. The Diffusion of Leukemia Chemotherapy: A Study in the Non-Market Economics of Medical Care. [Google Scholar]
- Warner K. Hospital Cost-Containment Effects on Development and Use of Medical Technology. Milbank Memorial Fund Quarterly. 1978 Spring;:187–211. [PubMed] [Google Scholar]
- Worthington N, et al. Vol III of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement in Maryland. [Google Scholar]
- Worthington N, et al. Vol VI of “National Hospital Rate-Setting Study.” Health Care Financing Grants and Contracts Report. Apr, 1980. Case Study of Prospective Reimbursement In New Jersey. [Google Scholar]