Abstract
Health care spending in the United States more than tripled between 1971 and 1981, increasing from $83 billion to $287 billion. This growth in health sector spending substantially outpaced overall growth in the economy, averaging 13.2 percent per year compared to 10.5 percent for the gross national product (GNP). By 1981, one out of every ten dollars of GNP was spent on health care, compared to one out of every thirteen dollars of GNP in 1971. If current trends continue and if present health care financing arrangements remain basically unchanged, national health expenditures are projected to reach approximately $756 billion in 1990 and consume roughly 12 percent of GNP.
The focal issue in health care today is cost and cost Increases. The outlook for the 1980's is for continued rapid growth but at a diminished rate. The primary force behind this moderating growth is projected lower inflation. However, real growth rates are also expected to moderate slightly. The chief factors influencing the growth of health expenditures in the eighties are expected to be aging of the population, new medical technologies, increasing competition, restrained public funding, growth in real income, increased health manpower, and a deceleration in economy-wide inflation.
Managers, policy makers and providers in the health sector, as in all sectors, must include in today's decisions probable future trends. Inflation, economic shocks, and unanticipated outcomes of policies over the last decade have intensified the need for periodic assessments of individual industries and their relationship to the macro economy. This article provides such an assessment for the health care industry. Baseline current-law projections of national health expenditures are made to 1990.
Highlights
Highlights from this study include:
Economy-wide inflation is assumed to moderate in the 1980's resulting in a deceleration in health expenditure growth.
National health expenditures are projected to increase at an average annual rate of 11 to 12 percent for the period 1981-1990, a decline from the 13.2 percent average annual growth in the 1971-1981 interval.
Real GNP is assumed to increase faster in the 1982-1990 period than in the previous 8-year interval resulting in upward pressure for growth in real health spending.
Growth in total systems cost (personal health expenditures) per capita is projected to slow to an average annual rate of 10.6 percent for the period 1981-1990, a 1.7 percentage point decline in the growth rate from 1971 to 1981 (12.3 percent).
Per capita expenditures for 1990 are projected to be approximately $3000 for total health care, $1340 for hospital care, and $560 for physician services.
Total public spending for health care is projected to reach $325 billion by 1990, of which the Federal government will finance approximately 71 percent. Total private spending is expected to reach $431 billion in 1990 or approximately 57 percent of all health expenditures.
The population 75 years of age and over is projected to increase four times faster than the population of persons under age 65, leading to upward pressure on expenditure growth.
The institutional care share of personal health expenditures will increase and by 1990 hospital and nursing home care are expected to consume approximately 60 percent of personal health care spending.
The number of active physicians is projected to increase at an average annual rate of 2.7 percent in the projection period, a rate of increase triple that of population growth.
These projections are an evolution of historical trends and assume no abrupt or significant departure from current law. The key assumption is that the present extensive third party payment system will remain in place.
Other evolving patterns significant to the health care sector for the 1980's are:
Continued growth in new and expensive diagnostic and therapeutic technologies.
Slackening in growth of public financing for social programs.
Increased rivalry and competition within and among various segments of the health industry, taking many forms of price and nonprice competition such as: improved quality of services and products, expanded markets, increased advertising and greater substitution of services and goods (Porter, 1980). This increases the need to plan and adapt to changes in the health care sector.
The purpose of this baseline projection is to provide an evolution of health care spending under current law. This is a trend, or smooth growth projection scenario with focus on average annual rates of change.
Historical patterns in health spending are studied over three basic time intervals: 1950 to 1981, 1965 to 1981, and 1971 to 1981. The projection intervals are the short term, 1981 to 1983; the midterm, 1983 to 1985; and the long term, 1985 to 1990. The entire projection horizon, 1981 to 1990, is also examined.
We have developed a model which incorporates economic, actuarial, statistical, demographic and judgmental factors into a single integrated framework. There are four major interrelated components of the model: 1) a five-factor model of expenditures, 2) supply variables, 3) a channel of finance module and 4) a net cost of private health insurance/program administration cost module.
First, the assumptions upon which the projections are based are presented. An overview of projections for total health costs and sources of financing is given. We then examine health care expenditure growth from an international vantage point. Some theories on the causes of health expenditure growth are discussed. Projections of total systems cost per capita are presented. Finally, projections for particular health care sectors are presented. In addition, there are technical notes on methodology and data sources available from the author.
Assumptions for Current-Law Projections
These current-law projections are based on the fundamental assumption that historical trends and relationships will continue into the future. Further, it is assumed that:
The competitive structure, conduct, and performance of the health care delivery system will continue to evolve along patterns followed during the historical period 1965 through 1981.
No Federally mandated pro-competition health insurance plan or cost containment program, including prospective payment for all payers, will be in effect. This is an assumption of the current law projection, not a prediction.
No major, new, publicly-financed program of medical care such as catastrophic national health insurance will be legislated. This is an assumption of the current law projection, not a prediction.
No major technological breakthrough in treatment of acute and chronic illnesses that would significantly alter evolving patterns of morbidity and mortality will occur.
Use of medical care, including intensity of services per case (derived in part from new technologies) will continue to grow in accordance with historical relationships and trends.
Medical care prices will vary with the implicit price deflator for the GNP1 according to relationships established in the historical period studied.
Population will grow as projected by the Office of the Actuary, Social Security Administration (Tables A-1 through A-3).
Health manpower will increase as projected by the Bureau of Health Professions (Table A-4).
The GNP and the implicit price deflator for the Gross National Product will grow as projected in economic assumptions incorporated in the Board of Trustees, Federal Old-Age and Survivors Insurance and Disability Trust Funds, 1982 Annual Report, alternative II-B (intermediate) economic assumptions (Table A-1).
Benefit outlays for Medicare and total community hospital inpatient expenses and use will grow as projected in the 1982 Annual Report of the Federal Hospital Insurance Trust Fund and the 1982 Annual Report of the Federal Supplementary Medical Insurance Trust Fund. Projected growth rates were modified by the Medicare actuaries to account for factors and trends evident as of mid-1982.
Aggregate Federal Medicaid benefit outlay increases are consistent with the Health Care Financing Administration projections.
Provisional estimates of the effects of the Tax and Equity Fiscal Responsibility Act of 1982 (P.L. 92-248)(Health Care Financing Administration, September 13, 1982) have been factored into the projection estimates.
Table A-1. Historical Estimates and Projections of Gross National Product, Inflation, and Population, Selected Years, 1950-1990.
| Calendar Year | Gross National1 Product (billions) | Real Gross1 National Product (1972 dollars, billions) | Implicit1 Price Deflator, Gross National Product (1972= 100.0) | Consumer Price1 2 Index-All Items Wage Earners (1967=100.0) | Total3 Population (Thousands, July 1) |
|---|---|---|---|---|---|
|
|
|
|
|
|
|
| Historical Estimates | |||||
|
|
|||||
| 1950 | $ 286.5 | $ 534.8 | 53.5 | 72.1 | 154,675 |
| 1955 | 400.0 | 657.5 | 60.8 | 80.2 | 168,385 |
| 1960 | 506.5 | 737.2 | 68.7 | 88.7 | 183,834 |
| 1965 | 691.0 | 929.3 | 74.4 | 94.5 | 197,876 |
| 1966 | 756.0 | 984.8 | 76.8 | 97.2 | 200,149 |
| 1967 | 799.6 | 1,011.4 | 79.0 | 100.0 | 202,334 |
| 1968 | 873.4 | 1,058.1 | 82.5 | 104.2 | 204,362 |
| 1969 | 944.0 | 1,087.6 | 86.8 | 109.8 | 206,369 |
| 1970 | 992.7 | 1,085.6 | 91.4 | 116.3 | 208,612 |
| 1971 | 1,077.6 | 1,122.4 | 96.0 | 121.3 | 211,256 |
| 1972 | 1,185.9 | 1,185.9 | 100.0 | 125.3 | 213,569 |
| 1973 | 1,326.4 | 1,254.3 | 105.7 | 133.1 | 215,665 |
| 1974 | 1,434.2 | 1,246.3 | 115.1 | 147.7 | 217,683 |
| 1975 | 1,549.2 | 1,231.7 | 125.7 | 161.2 | 219,890 |
| 1976 | 1,718.0 | 1,298.2 | 132.3 | 170.5 | 221,993 |
| 1977 | 1,918.3 | 1,369.7 | 140.0 | 181.5 | 224,225 |
| 1978 | 2,163.8 | 1,438.5 | 150.4 | 195.4 | 226,583 |
| 1979 | 2,417.8 | 1,479.4 | 163.4 | 217.7 | 229,061 |
| 1980 | 2,633.1 | 1,474.0 | 178.6 | 247.0 | 231,679 |
| 1981 | 2,937.7 | 1,502.6 | 195.5 | 272.3 | 233,988 |
| Projections | |||||
|
|
|||||
| 1983 | 3,468.9 | 1,555.2 | 223.0 | 311.2 | 238,219 |
| 1985 | 4,207.4 | 1,654.8 | 254.3 | 356.2 | 242,526 |
| 1990 | 6,304.1 | 1,918.5 | 328.6 | 458.9 | 253,387 |
| Selected Periods | Average Annual Rates of Increase | ||||
|
|
|
||||
| 1950-1955 | 6.9% | 4.2% | 2.6% | 2.2% | 1.7% |
| 1955-1960 | 4.8 | 2.3 | 2.5 | 2.0 | 1.8 |
| 1960-1965 | 6.4 | 4.7 | 1.6 | 1.3 | 1.5 |
| 1965-1970 | 7.5 | 3.2 | 4.2 | 4.3 | 1.1 |
| 1970-1975 | 9.3 | 2.6 | 6.5 | 6.3 | 1.1 |
| 1975-1980 | 11.2 | 3.7 | 7.3 | 8.9 | 1.0 |
| 1980-1985 | 9.8 | 2.3 | 7.3 | 7.6 | 0.9 |
| 1985-1990 | 8.4 | 3.0 | 5.3 | 5.2 | 0.9 |
| 1981-1983 | 8.7 | 1.7 | 6.8 | 6.9 | 0.9 |
| 1983-1985 | 10.1 | 3.2 | 6.8 | 7.0 | 0.9 |
| 1970-1980 | 10.2 | 3.1 | 6.9 | 7.8 | 1.1 |
| 1980-1990 | 9.1 | 2.7 | 6.3 | 6.4 | 0.9 |
| 1971-1981 | 10.5 | 3.0 | 7.4 | 8.4 | 1.0 |
| 1981-1990 | 8.9 | 2.8 | 5.9 | 6.0 | 0.9 |
Historical estimates are reported in Economic Report of the President, February 1982. Projection growth rates are from Board of Trustees Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds, 1982 Annual Report, Washington, April 1, 1982. II-B assumptions were used. The growth rates for 1982 for GNP and inflation were slightly modified to reflect partial year data available as of mid 1982. The 1990 GNP used in this projection is within 3 percent of the GNP forecast by the private consulting firm of Data Resources, Inc. See Review of the U.S. Economy, October 1982 (forecast: TREND LONG 1082).
The CPI is shown for comparison only. The implicit price deflator for GNP is used in the projection process to reflect cost pressures external to health care industry.
Historical estimates of population are based on data from the Bureau of Census. The estimates are reported in Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982, pp. 1-36. Projected growth rates in population are from the Office of the Actuary, Social Security Area Population Projections, 1981, Actuarial Study No. 85, SSA Pub. No. 11-11532, U.S. Department of Health and Human Services, July 1981. Alternative II (intermediate) assumptions for population growth were used.
Table A-3. Proportions of the Population Ages Less than 65, 65 +, and 75 +, Selected Years, 1960-1990.
| Calendar Year | Total All Ages | Less than 65 | Equal to or Greater Than Age 65 | Equal to or Greater Than Age 75 |
|---|---|---|---|---|
|
|
|
|
|
|
| Historical Estimates | ||||
|
|
||||
| 1960 | 100.0% | 90.9% | 9.1% | 3.1% |
| 1965 | 100.0 | 90.7 | 9.3 | 3.4 |
| 1970 | 100.0 | 90.3 | 9.7 | 3.8 |
| 1971 | 100.0 | 90.2 | 9.8 | 3.9 |
| 1975 | 100.0 | 89.6 | 10.4 | 4.1 |
| 1979 | 100.0 | 89.0 | 11.0 | 4.3 |
| 1980 | 100.0 | 88.9 | 11.1 | 4.4 |
| 1981 | 100.0 | 88.7 | 11.3 | 4.5 |
| Projections | ||||
|
|
||||
| 1983 | 100.0 | 88.5 | 11.5 | 4.7 |
| 1985 | 100.0 | 88.1 | 11.9 | 4.9 |
| 1990 | 100.0 | 87.4 | 12.6 | 5.4 |
Derived from data in Office of the Actuary (1981). Alternative II (intermediate) assumptions for population growth were used.
Table A-4. Historical Estimates and Projections of Active Physicians and Dentists, Selected Years, 1950-19901.
| Year | Number of Active Physicians (as of December 31) |
Number of Active Dentists (as of December 31) |
||
|---|---|---|---|---|
|
|
|
|
||
| Historical Estimates | Total | M.D.'s | D.O.'s | |
|
|
|
|
|
|
| 1950 | 219,900 | 209,000 | 10,900 | 79,190 |
| 1955 | 240,200 | 228,600 | 11,600 | 84,370 |
| 1960 | 259,400 | 247,300 | 12,200 | 90,120 |
| 1965 | 288,700 | 277,600 | 11,1002 | 95,900 |
| 1970 | 323,200 | 311,200 | 12,000 | 102,220 |
| 1971 | 334,400 | 322,000 | 12,400 | 103,350 |
| 1975 | 378,600 | 364,500 | 14,100 | 112,020 |
| 1980 | 449,500 | 432,400 | 17,100 | 126,240 |
| 1981 | 464,000 | 446,000 | 18,000 | 129,330 |
| Projections | ||||
|
|
||||
| 1983 | 493,100 | 473,500 | 19,700 | 135,670 |
| 1985 | 523,900 | 502,000 | 21,900 | 141,500 |
| 1990 | 591,200 | 563,300 | 27,900 | 154,760 |
| Selected Periods | Average Annual Percent Increases | |||
|
|
|
|||
| 1950-1955 | 1.8% | 1.8% | 1.3% | 1.3% |
| 1955-1960 | 1.6 | 1.6 | 1.0 | 1.3 |
| 1960-1965 | 2.2 | 2.3 | −1.92 | 1.3 |
| 1965-1970 | 2.3 | 2.3 | 1.6 | 1.3 |
| 1970-1975 | 3.2 | 3.2 | 3.3 | 1.9 |
| 1975-1980 | 3.5 | 3.5 | 3.9 | 2.4 |
| 1980-1985 | 3.1 | 3.0 | 5.1 | 2.3 |
| 1985-1990 | 2.5 | 2.3 | 5.0 | 1.8 |
| 1970-1980 | 3.4 | 3.3 | 3.6 | 2.1 |
| 1980-1990 | 2.8 | 2.7 | 5.0 | 2.1 |
| 1981-1983 | 3.1 | 3.0 | 4.6 | 2.4 |
| 1983-1985 | 3.1 | 3.0 | 5.4 | 2.1 |
| 1981-1990 | 2.7 | 2.6 | 5.0 | 2.0 |
| 1971-1981 | 3.3 | 3.3 | 3.8 | 2.3 |
Division of Health Professions Analysis, Bureau of Health Professions, Third Report to the President and Congress on the Status of Health Professions Personnel in the United States, Health Resources Administration, U.S. Department of Health and Human Services, January 1982.
The decline in the number of active D.O.'s between 1960 and 1965 reflects the granting of approximately 2,400 M.D. degrees to osteopathic physicians who had graduated from the University of California College of Medicine at Irvine. These physicians are included with active M.D.'s beginning in 1962.
The short-term outlook for the economy for the period 1981 to 1983, compared to the period 1979 to 1981, can be characterized by a substantial deceleration in inflation and a rebound in real growth in the economy in 1983 (Table 1). Real GNP increased at an average annual rate of 0.8 percent for the period 1979 to 1981. It is expected to increase at an average annual rate of 1.7 percent for the period 1981-1983 reflecting negative growth in 1982, but a 4.2 percent increase in 1983. The GNP deflator, an economy-wide measure of inflation, is expected to increase at an average annual rate of 6.8 percent for the period 1981 to 1983, compared to a 9.4 percent annual rate for the 1979-1981 period.
Table 1. National Health Expenditures by Source of Funds and Percent of Gross National Product, Selected Calendar Years, 1950-1990.
| National Health Expenditures | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Calendar Year | Gross National Product (billions) | Total | Private | Public | ||||||||
|
|
|
|
||||||||||
| Amount (billions) | Per Capita | Percent of GNP | Amount (billions) | Percent of Total | Total | Federal | State & Local | |||||
|
|
|
|
||||||||||
| Amount (billions) | Percent of Total | Amount (billions) | Percent of Total | Amount (billions) | Percent of Total | |||||||
| Historical1 | ||||||||||||
| 1950 | $ 286.5 | $ 12.7 | $ 82 | 4.4% | $ 9.2 | 72.8% | $ 3.4 | 27.2% | $ 1.6 | 12.8% | $ 1.8 | 14.4% |
| 1960 | 506.5 | 26.9 | 146 | 5.3 | 20.3 | 75.3 | 6.6 | 24.7 | 3.0 | 11.2 | 3.6 | 13.5 |
| 1970 | 992.7 | 74.7 | 358 | 7.5 | 46.9 | 62.8 | 27.8 | 37.2 | 17.7 | 23.7 | 10.1 | 13.6 |
| 1971 | 1,077.7 | 83.3 | 394 | 7.7 | 51.6 | 62.0 | 31.7 | 38.0 | 20.3 | 24.4 | 11.3 | 13.6 |
| 1975 | 1,549.2 | 132.7 | 604 | 8.6 | 76.5 | 57.7 | 56.2 | 42.3 | 37.1 | 27.9 | 19.1 | 14.4 |
| 1979 | 2,417.8 | 215.0 | 938 | 8.9 | 124.4 | 57.9 | 90.6 | 42.1 | 61.0 | 28.4 | 29.5 | 13.7 |
| 1980 | 2,633.1 | 249.0 | 1,075 | 9.5 | 143.6 | 57.7 | 105.4 | 42.3 | 71.1 | 28.5 | 34.3 | 13.8 |
| 1981 | 2,937.7 | 286.6 | 1,225 | 9.8 | 164.1 | 57.3 | 122.5 | 42.7 | 83.9 | 29.3 | 38.6 | 13.5 |
| Projected | ||||||||||||
| 1983 | 3,468.9 | 362.3 | 1,521 | 10.4 | 211.2 | 58.3 | 151.1 | 41.7 | 104.2 | 28.8 | 46.9 | 12.9 |
| 1985 | 4,207.4 | 456.4 | 1,882 | 10.8 | 268.2 | 58.8 | 188.1 | 41.2 | 131.5 | 28.8 | 56.6 | 12.4 |
| 1990 | 6,304.1 | 755.6 | 2,982 | 12.0 | 430.9 | 57.0 | 324.7 | 43.0 | 231.6 | 30.7 | 93.1 | 12.3 |
Historical estimates are from Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September, 1982.
For the midterm period 1983-1985, GNP is projected to increase at an average annual rate of 10.1 percent, with economy-wide prices increasing at an average rate of 6.8 percent and real GNP increasing at an average rate of 3.2 percent. The GNP deflator is expected to increase at an average annual rate of 5.3 percent, and real GNP at a 3.0 percent rate for the 1985-1990 interval.
For the entire projection period 1981-1990, the GNP deflator is expected to increase at an average annual rate of 5.9 percent. During the last decade, 1971-1981, the GNP deflator increased at an average annual rate of 7.4 percent. Thus significant deceleration of inflation is assumed. Real GNP is expected to increase at an average annual rate of 2.8 percent for the 1981-1990 period. Nominal GNP is expected to increase at an average annual rate of 8.9 percent over the 1981-1990 horizon, reflecting the deceleration in inflation.
A shift in the age composition of the population is one factor which will cause health expenditures to rise in the 1980's. Use of medical care by the aged population is disproportionate to their numbers. The number of persons 75 years of age and over is projected to increase at an average rate of 3.1 percent in the period 1981-1990 compared to an increase of .7 for the nonaged population (Table A-2). During the 1971-1981 period, the growth rates were 2.4 percent and 0.7 percent respectively. The proportion of the total population 65 years of age and over will rise from 11.3 percent in 1981 to 12.6 percent in 1990 (Table A-3). Total population is projected to increase at an average annual rate of 0.9 percent from 1981 to 1990.
Table A-2. Average Annual Percent Increases in Numbers of Persons of Ages Less than 65,65 +, and 75 +, Selected Periods, 1960-19901.
| Selected Periods | Less Than Age 65 | Equal to or Greater Than Age 65 | Equal to or Greater Than Age 75 |
|---|---|---|---|
|
|
|
|
|
| 1960-1965 | 1.4% | 2.0% | 3.6% |
| 1965-1970 | 1.0 | 1.7 | 3.4 |
| 1970-1975 | 0.7 | 2.3 | 2.4 |
| 1975-1980 | 0.7 | 2.3 | 2.4 |
| 1980-1985 | 0.8 | 2.1 | 3.1 |
| 1985-1990 | 0.7 | 2.2 | 3.0 |
| 1960-1981 | 0.9 | 2.1 | 2.9 |
| 1965-1981 | 0.8 | 2.1 | 2.7 |
| 1971-1981 | 0.7 | 2.3 | 2.4 |
| 1981-1983 | 0.8 | 2.0 | 3.0 |
| 1983-1985 | 0.7 | 2.4 | 3.5 |
| 1981-1990 | 0.7 | 2.2 | 3.1 |
Derived from data in Office of the Actuary (1981). Alternative II (intermediate) assumptions for population growth were used.
Physicians are the key decision makers in the health sector. The number of active physicians is projected to grow from 464,000 in 1981 to 591,000 in 1990 (Table A-4), an aggregate increase of 27 percent, or more than three times the projected aggregate population growth.
The number of active dentists is projected to increase from 129,000 in 1981 to 155,000 in 1990, a 20-percent increase (Table A-4). This increase is approximately 2.5 times faster than aggregate population growth. As is the case with physicians, the growth in the number of dentists will decelerate during the 1980's declining from the peak growth rate years of 1975-1980 (Table A-4).
Overview of Projections
Total national health expenditures rose from $42 billion in 1965 to $287 billion in 1981, an average annual rate of growth of 12.8 percent (Table 1 and Table A-5). This rate implies a doubling of health spending every 5.8 years. There is variation around this average rate of increase. The lowest annual percent increase in this period was 10.3 percent in 1973, during the Economic Stabilization Program (ESP). The highest annual percent increase in this period was 15.8 percent in 1980.
Table A-5. National Health Expenditures by Source of Funds and Percent of Gross National Product, Selected Calendar Years, 1950-1990.
| Calendar Year | Gross National Product (billions) | National Health Expenditures | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Total | Private | Public | ||||||||||
|
|
|
|
||||||||||
| Total | Federal | State & Local | ||||||||||
| Amount (billions) | Per Capita | Percent of GNP | Amount (billions) | Percent of Total | Amount (billions) | Percent of Total | Amount (billions) | Percent of Total | Amount (billions) | Percent of Total | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Historical1 | ||||||||||||
|
|
||||||||||||
| 1950 | $286.5 | $ 12.7 | $ 82 | 4.4% | $ 9.2 | 72.8% | $ 3.4 | 27.2% | $1.6 | 12.8% | $1.8 | 14.4% |
| 1955 | 400.0 | 17.7 | 105 | 4.4 | 13.2 | 74.3 | 4.6 | 25.7 | 2.0 | 11.3 | 2.6 | 14.4 |
| 1960 | 506.5 | 26.9 | 146 | 5.3 | 20.3 | 75.3 | 6.6 | 24.7 | 3.0 | 11.2 | 3.6 | 13.5 |
| 1965 | 691.0 | 41.7 | 211 | 6.0 | 30.9 | 74.1 | 10.8 | 25.9 | 5.5 | 13.3 | 5.2 | 12.6 |
| 1966 | 756.0 | 46.1 | 230 | 6.1 | 32.5 | 70.6 | 13.6 | 29.4 | 7.4 | 16.1 | 6.1 | 13.3 |
| 1967 | 799.6 | 51.3 | 254 | 6.4 | 32.4 | 63.1 | 19.0 | 36.9 | 11.9 | 23.2 | 7.0 | 13.7 |
| 1968 | 873.4 | 58.2 | 285 | 6.7 | 36.1 | 62.0 | 22.1 | 38.0 | 14.1 | 24.3 | 8.0 | 13.7 |
| 1969 | 944.0 | 65.7 | 318 | 7.0 | 40.8 | 62.1 | 24.9 | 37.9 | 16.1 | 24.5 | 8.8 | 13.4 |
| 1970 | 992.7 | 74.7 | 358 | 7.5 | 46.9 | 62.8 | 27.8 | 37.2 | 17.7 | 23.7 | 10.1 | 13.6 |
| 1971 | 1,077.6 | 83.3 | 394 | 7.7 | 51.6 | 62.0 | 31.7 | 38.0 | 20.3 | 24.4 | 11.3 | 13.6 |
| 1972 | 1,185.9 | 93.5 | 438 | 7.9 | 58.1 | 62.1 | 35.4 | 37.9 | 22.9 | 24.5 | 12.5 | 13.4 |
| 1973 | 1,326.4 | 103.2 | 478 | 7.8 | 63.9 | 61.9 | 39.3 | 38.1 | 25.2 | 24.5 | 14.1 | 13.7 |
| 1974 | 1,434.2 | 116.4 | 535 | 8.1 | 69.3 | 59.5 | 47.1 | 40.5 | 30.4 | 26.2 | 16.6 | 14.3 |
| 1975 | 1,549.2 | 132.7 | 604 | 8.6 | 76.5 | 57.7 | 56.2 | 42.3 | 37.1 | 27.9 | 19.1 | 14.4 |
| 1976 | 1,718.0 | 149.7 | 674 | 8.7 | 86.7 | 57.9 | 62.9 | 42.1 | 42.6 | 28.5 | 20.3 | 13.6 |
| 1977 | 1,918.3 | 169.2 | 755 | 8.8 | 99.1 | 58.6 | 70.1 | 41.4 | 47.4 | 28.0 | 22.7 | 13.4 |
| 1978 | 2,163.8 | 189.3 | 836 | 8.8 | 109.8 | 58.0 | 79.5 | 42.0 | 53.9 | 28.4 | 25.7 | 13.6 |
| 1979 | 2,417.8 | 215.0 | 938 | 8.9 | 124.4 | 57.9 | 90.6 | 42.1 | 61.0 | 28.4 | 29.5 | 13.7 |
| 1980 | 2,633.1 | 249.0 | 1,075 | 9.5 | 143.6 | 57.7 | 105.4 | 42.3 | 71.1 | 28.5 | 34.3 | 13.8 |
| 1981 | 2,937.7 | 286.6 | 1,225 | 9.8 | 164.1 | 57.3 | 122.5 | 42.7 | 83.9 | 29.2 | 38.6 | 13.5 |
| Projections | ||||||||||||
|
|
||||||||||||
| 1983 | 3,468.9 | 362.3 | 1,521 | 10.4 | 211.2 | 58.3 | 151.1 | 41.7 | 104.2 | 28.8 | 46.9 | 12.9 |
| 1985 | 4,207.4 | 456.4 | 1,882 | 10.8 | 268.2 | 58.8 | 188.1 | 41.2 | 131.5 | 28.8 | 56.6 | 12.4 |
| 1990 | 6,304.1 | 755.6 | 2,982 | 12.0 | 430.9 | 57.0 | 324.7 | 43.0 | 231.6 | 30.7 | 93.1 | 12.3 |
| Selected Periods | Average Annual Percent Increases | |||||||||||
|
|
|
|||||||||||
| 1950-1955 | 6.9% | 6.9% | 5.2% | — | 7.4% | — | 5.8% | — | 4.6% | — | 7.6% | — |
| 1955-1960 | 4.8 | 8.7 | 6.8 | — | 9.0 | — | 7.8 | — | 8.5 | — | 6.7 | — |
| 1960-1965 | 6.4 | 9.2 | 7.6 | — | 8.8 | — | 10.2 | — | 12.9 | — | 7.6 | — |
| 1965-1970 | 7.5 | 12.4 | 11.2 | — | 8.7 | — | 20.8 | — | 26.1 | — | 14.0 | — |
| 1970-1975 | 9.3 | 12.2 | 11.0 | — | 10.3 | — | 15.1 | — | 16.0 | — | 13.6 | — |
| 1975-1980 | 11.2 | 13.4 | 12.2 | — | 13.4 | — | 13.4 | — | 13.9 | — | 12.5 | — |
| 1950-1980 | 7.7 | 10.4 | 8.9 | — | 9.6 | — | 12.1 | — | 13.5 | — | 10.2 | — |
| 1970-1980 | 10.2 | 12.8 | 11.6 | — | 11.8 | — | 14.3 | — | 14.9 | — | 13.0 | — |
| 1980-1990 | 9.1 | 11.7 | 10.7 | — | 11.6 | — | 11.9 | — | 12.5 | — | 10.5 | — |
| 1981-1983 | 8.7 | 12.4 | 11.4 | — | 13.4 | — | 11.1 | — | 11.4 | — | 10.3 | — |
| 1983-1985 | 10.1 | 12.2 | 11.2 | — | 12.7 | — | 11.6 | — | 12.3 | — | 9.9 | — |
| 1980-1985 | 9.8 | 12.9 | 11.9 | — | 13.3 | — | 12.3 | — | 13.1 | — | 10.5 | — |
| 1985-1990 | 8.4 | 10.6 | 9.6 | — | 9.9 | — | 11.5 | — | 12.0 | — | 10.4 | — |
| 1971-1981 | 10.5 | 13.2 | 12.0 | — | 12.3 | — | 14.5 | — | 15.2 | — | 13.1 | — |
| 1981-1990 | 8.9 | 11.4 | 10.4 | — | 11.3 | — | 11.4 | — | 11.9 | — | 10.3 | — |
Historical estimates are from Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982, pp. 1-36.
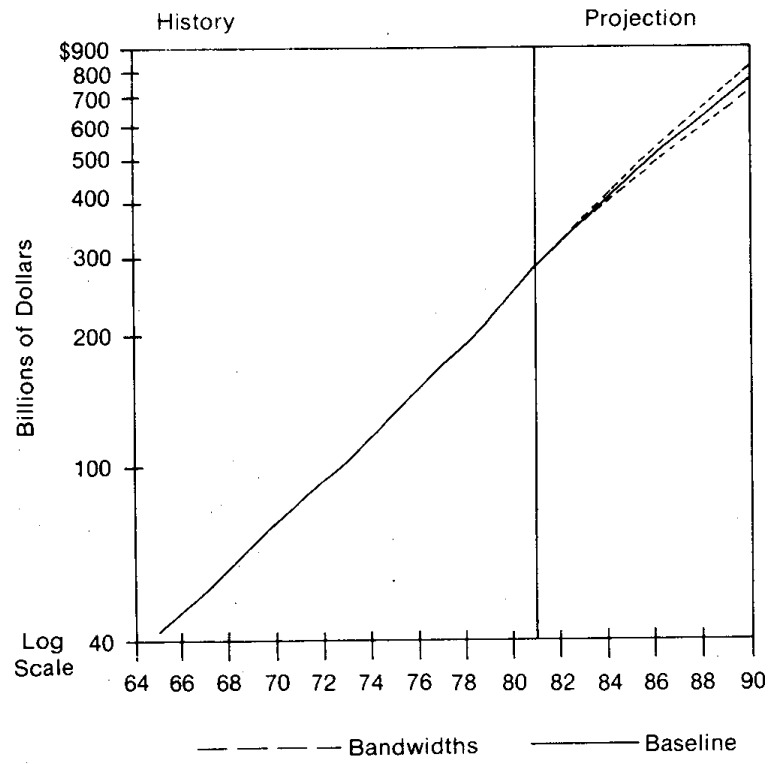
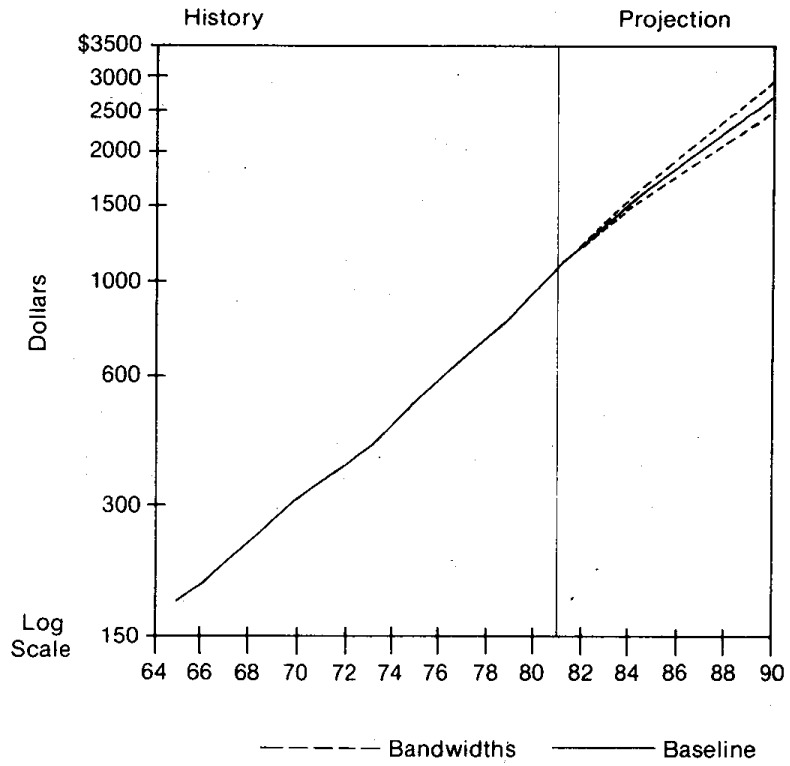
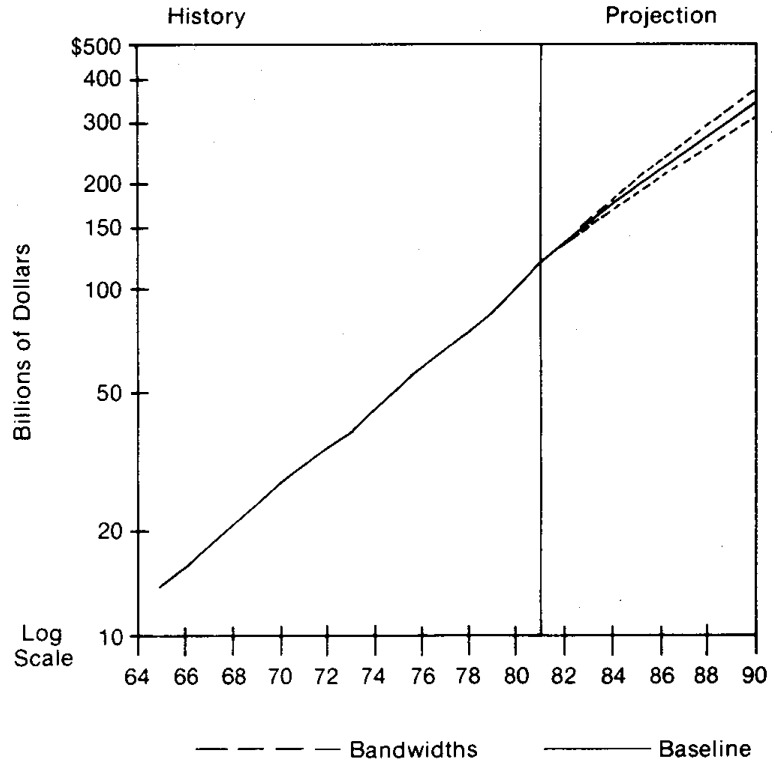
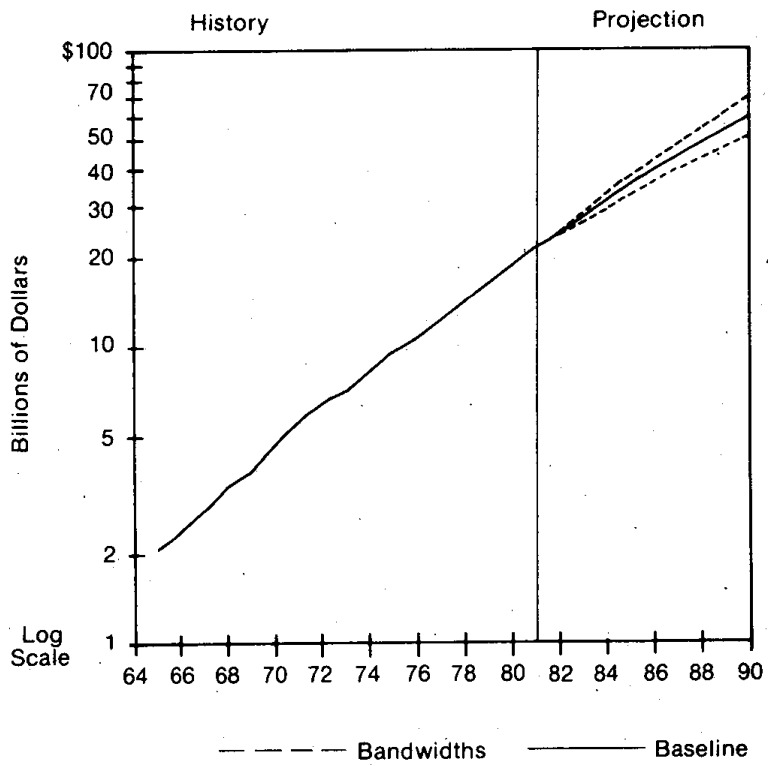
National health expenditures increased 33.3 percent and the GNP 21.5 percent during the 2-year period 1979-1981. Projected outlays for national health expenditures (Table 1 and Figure 1) are:
Figure 1. Total National Health Expenditures 1965 to 1990, with Bandwidth Intervals1.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in total national health expenditures for 1966-1981 (see Table A-12) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
$362 billion by 1983 or $1,521 per capita;
$456 billion by 1985 or $1,882 per capita;
$756 billion by 1990 or $2,982 per capita.
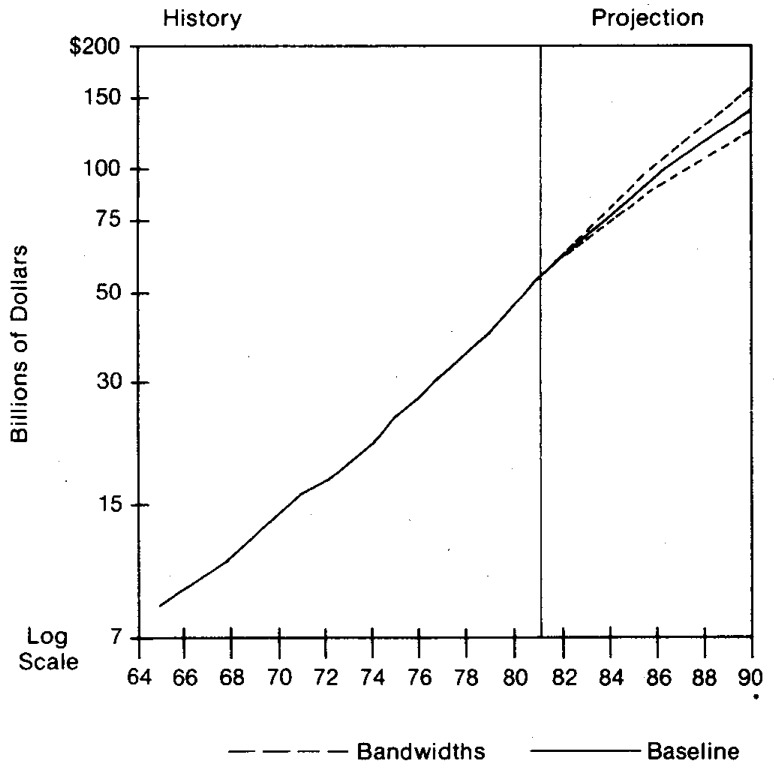
These projections reflect a gradual deceleration in expenditure growth, but the increases in health care spending are expected to continue to outpace growth in the Gross National Product (GNP). By 1983, the health sector share of the GNP is projected to increase to about 10.4 percent (Figure 2).
Figure 2. The Share National Health Expenditures are of GNP 1965 to 1990, with Bandwidth Intervals1.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in the ratio of national health expenditures to GNP for 1966-1981 (see Table A-11) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
The projected negative growth in real GNP in 1982 and the relatively fast growth in health care spending account for the rapid projected increase in the ratio of health spending to GNP for the period 1981-1983. Extensive third-party payments for health care and the necessary nature of much care, insulate growth in aggregate health care expenditures from short-term fluctuations in real GNP. On the other hand, some services which have shallow insurance coverage such as eyeglasses, drugs, and other professional services appear to be adversely affected by the recession.
We expect the upward trend in the health care sector's share of GNP to slow as the economy rebounds in 1983. A gradual increase in this share is projected for the remainder of the 1980's, reaching roughly 12.0 percent in 1990. Between 1965 and 1982, health's share of GNP increased at an average annual rate of 3.3 percent per year (partial year data were available for 1982 estimate). From 1982 to 1990 it is expected to increase at an average annual rate of 1.8 percent. From 1981 to 1990, health expenditure growth is expected to rise slower (average annual rate of 11.4 percent) than in the post-Medicare historical period 1971-1981 (average annual rate of 1.3.2 percent).
A projected decline in the general inflation rate leading to lower health care price increases will exert a downward pressure on health spending in the 1980s. Restrained growth in public financing of health care will exert further downward pressure. However, projected increases in real GNP, beginning in 1983, will exert an upward pressure as will aging of the population and new technologies. As the economy expands the fiscal tightness affecting government programs may tend to ease. We project that the net effect of these pressures will be a deceleration in the growth of health spending.
Government Funding of National Health Expenditures
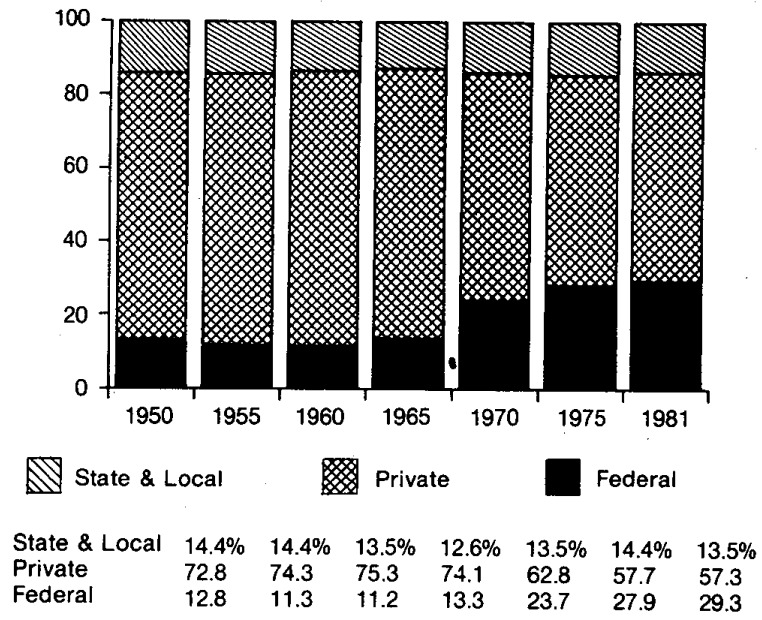
In 1981 the Federal share of spending was 29.3 percent (Figure 3 and Table 1), having increased its share 5 percentage points since 1973 (Table A-5). Due to a maturing of Federal health programs and the tight fiscal situation, the Federal share stabilizes at approximately 29 percent for 1983 and 1985. It rises to 31 percent by 1990 due to the aging of the population and the expanding revenue base accompanying the more robust economic growth.
Figure 3. Percent Distribution of Total National Health Expenditures by Source of Funds for Selected Years, 1950 to 1981.
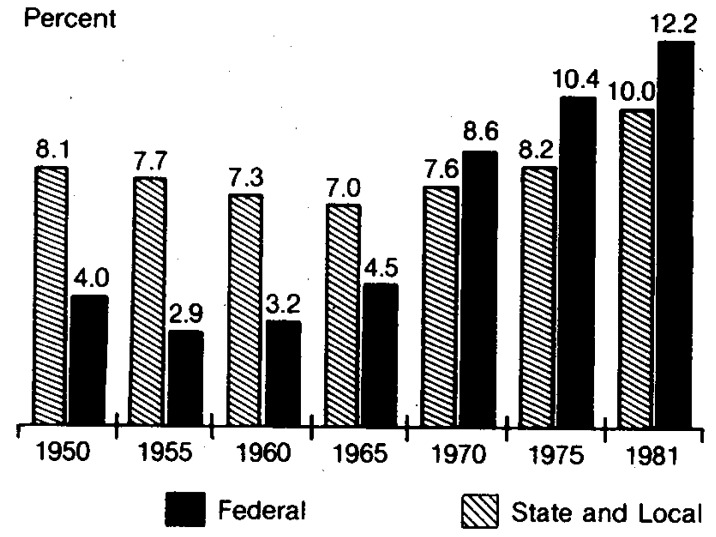
Federal outlays for national health expenditures, which were $1.6 billion in 1950, increased to $5.5 billion in 1965 and $83.9 billion in 1981 (Table A-5). Federal expenditures increased at an average annual rate of 18.5 percent for the period 1965-1981 (Table A-5). Federally financed health expenditures were 4.5 percent of total Federal government expenditures in 1965 and this percentage has risen to 12.2 percent in 1981 (Figure 4 and Table A-18).
Figure 4. National Health Expenditures as a Percent of Government Expenditures for Selected Years, 1950 to 1981.
Table A-18. Federally Financed Health Expenditures Relative to Total Federal Government Expenditures, and to Gross National Product, Selected Years, 1950-1981.
| Year | Health1 Expenditures Federally, Financed (Amounts in billions of dollars) |
Federal Government2 Expenditures (Amounts in billions of dollars) |
Health Expenditures Federally Financed As Percent of Federal Gov't Expenditures | Gross National Product2 (Amounts in billions of dollars) |
Federal Gov't Expenditures As Percent of Gross National Product | Health Expenditures Federally Financed As Percent of Gross National Product |
|---|---|---|---|---|---|---|
|
|
|
|||||
| 1950 | $1.6 | $40.8 | 3.9% | $286.5 | 14.2% | 0.6% |
| 1955 | 2.0 | 68.1 | 2.9 | 400.0 | 17.0 | 0.5 |
| 1960 | 3.0 | 93.8 | 3.2 | 506.5 | 18.4 | 0.6 |
| 1965 | 5.5 | 123.8 | 4.4 | 691.0 | 17.9 | 0.8 |
| 1966 | 7.4 | 143.8 | 5.2 | 756.0 | 19.0 | 1.0 |
| 1967 | 11.9 | 163.7 | 7.3 | 799.6 | 20.5 | 1.5 |
| 1968 | 14.9 | 180.5 | 7.8 | 873.4 | 20.7 | 1.6 |
| 1969 | 16.1 | 188.4 | 8.5 | 944.0 | 20.0 | 1.7 |
| 1970 | 17.7 | 204.3 | 8.7 | 992.7 | 20.6 | 1.8 |
| 1971 | 20.3 | 220.6 | 9.2 | 1,077.6 | 20.5 | 1.9 |
| 1972 | 22.9 | 244.3 | 9.4 | 1,185.9 | 20.6 | 1.9 |
| 1973 | 25.2 | 264.3 | 9.5 | 1,326.4 | 19.9 | 1.9 |
| 1974 | 30.4 | 299.4 | 10.2 | 1,434.2 | 20.9 | 2.1 |
| 1975 | 37.1 | 356.6 | 10.4 | 1,549.2 | 23.0 | 2.4 |
| 1976 | 42.6 | 384.8 | 11.1 | 1,718.0 | 22.4 | 2.5 |
| 1977 | 47.4 | 421.1 | 11.3 | 1,918.3 | 22.0 | 2.5 |
| 1978 | 53.9 | 461.1 | 11.7 | 2,163.8 | 21.3 | 2.5 |
| 1979 | 61.0 | 509.7 | 12.0 | 2,417.8 | 21.3 | 2.5 |
| 1980 | 71.1 | 602.1 | 11.8 | 2,633.1 | 22.9 | 2.7 |
| 1981 | 83.9 | 688.2 | 12.2 | 2,937.7 | 23.4 | 2.9 |
Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982.
Bureau of Economic Analysis, Survey of Current Business, U.S. Department of Commerce.
The short-term outlook is for Federal expenditures to rise to $104 billion in 1983, an increase of $20 billion over 1981. We project that Federal expenditures will reach $131 billion by 1985 and $232 billion by 1990. Federal outlays for national health expenditures are expected to increase at an average annual rate of 11.9 percent, a rate substantially below the 15.2 percent rate for the 1971-1981 period.
For the period 1950 to the mid-1970's State and locally financed health expenditures were 7-8 percent of total State and local government expenditures. By 1981 this ratio had risen to 10 percent (Figure 4 and Table A-19). State and local governments have consistently financed 13-14 percent of national health expenditures (Table 1 and Figure 3). The State and local share of spending is projected to drop slightly between 1981 and 1985 and then stabilize at 12-13 percent for the period 1985-1990.
Table A-19. State and Local Financed Health Expenditures Relative to Total State and Local Government Expenditures, and to Gross National Product, Selected Years, 1950-1981.
| Year | Health Expenditures State & Local Financed (Amount in billions of dollars)1 |
State & Local Gov't Expenditures (Amount in billions of dollars)2 |
Health Expenditures State and Local Financed As Percent of State and Local Gov't Expenditures | Gross National Product (Amount in billions of dollars) |
State and Local Expenditures as Percent of Gross National Product | Health Expenditures State & Local Financed as Percent of Gross National Product |
|---|---|---|---|---|---|---|
|
|
|
|||||
| 1950 | $1.8 | $22.5 | 8.1% | $286.5 | 7.9% | 0.6% |
| 1955 | 2.6 | 32.9 | 7.7 | 400.0 | 8.2 | 0.7 |
| 1960 | 3.6 | 49.8 | 7.3 | 506.5 | 9.8 | 0.7 |
| 1965 | 5.2 | 75.1 | 7.0 | 691.0 | 10.9 | 0.8 |
| 1966 | 6.1 | 84.3 | 7.2 | 756.0 | 11.2 | 0.8 |
| 1967 | 7.0 | 94.7 | 7.4 | 799.6 | 11.8 | 0.9 |
| 1968 | 8.0 | 107.2 | 7.5 | 873.4 | 12.3 | 0.9 |
| 1969 | 8.8 | 118.7 | 7.4 | 944.0 | 12.6 | 0.9 |
| 1970 | 10.1 | 133.5 | 7.6 | 992.7 | 13.5 | 1.0 |
| 1971 | 11.3 | 150.5 | 7.5 | 1,077.6 | 14.0 | 1.0 |
| 1972 | 12.5 | 164.8 | 7.6 | 1,185.9 | 13.9 | 1.1 |
| 1973 | 14.1 | 181.6 | 7.8 | 1,326.4 | 13.7 | 1.1 |
| 1974 | 16.7 | 204.5 | 8.2 | 1,434.2 | 14.3 | 1.2 |
| 1975 | 19.1 | 232.1 | 8.2 | 1,549.2 | 15.0 | 1.2 |
| 1976 | 20.4 | 251.3 | 8.1 | 1,718.0 | 14.6 | 1.2 |
| 1977 | 22.7 | 269.7 | 8.4 | 1,918.3 | 14.1 | 1.2 |
| 1978 | 25.7 | 297.4 | 8.6 | 2,163.8 | 13.7 | 1.2 |
| 1979 | 29.5 | 321.5 | 9.2 | 2,417.8 | 13.3 | 1.2 |
| 1980 | 34.3 | 357.8 | 9.6 | 2,633.1 | 13.6 | 1.3 |
| 1981 | 38.6 | 385.0 | 10.0 | 2,937.7 | 13.1 | 1.3 |
Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982.
Bureau of Economic Analysis, Survey of Current Business, U.S. Department of Commerce.
We project that State and local outlays will be $47 billion in 1983, $57 billion in 1985, and $93 billion in 1990. The average annual growth rate for health expenditures State and locally financed during 1981-1990 is 10.3 percent, a rate substantially below the 13.1-percent rate for the period 1971-1981.
Private Funding
The private sector financed 57.3 percent of expenditures in 1981, a decline from 62.8 percent in 1970 (Table 1 and Figure 3). The private share is projected to increase over the period 1981-1985 and drop slightly over the period 1985-1990 as the aging population and more robust economy contribute to a slightly larger share of public financing derived from an expanding revenue base.
Private expenditures for health care are expected to reach $211 billion by 1983 and $431 billion by 1990. For the period 1981-1990 private expenditures are expected to increase at an average annual rate of 11.3 percent, close to the 1965-1981 rate of 11.0 percent.
World-Wide Burgeoning Cost of Health Care
Relatively high rates of growth in health care expenditures are not unique to the United States. Economy-wide inflation, growth in real income, demographic shifts, and product-innovative technologies have been associated with rising health care costs in the western industrialized countries.
In one study of the rising cost of health care among nine industrialized countries, expenditures increased during 1969 to 1976 at average annual rates from a low of 12.5% (United States) to a high of 20.5% (Australia) (Table 2). In all nine countries health expenditures increased as a proportion of GNP. While the United States is among the highest, when ranked according to percent spent on health care, the Federal Republic of Germany topped the list with 9.7 percent of GNP spent on health care for the year 1975 (the latest available data in the study).
Table 2. National Health Expenditures in Nine Industrialized Countries, Average Annual Percent Increases, and as Percent of Gross National Product, 1969 and 19761.
| National Health Expenditures | |||
|---|---|---|---|
|
| |||
| Country (ranked by 1969-1976 increase in health expenditures) | Average Annual Rate of Increase, 1969-1976 | As Percent of GNP | |
|
| |||
| 1969 | 1976 | ||
| Australia | 20.5% | 5.6% | 7.7% |
| Finland | 18.9 | 6.0 | 7.2 |
| Netherlands | 18.4 | 6.0 | 8.5 |
| United Kingdom | 18.2 | 4.5 | 5.8 |
| Federal Republic of Germany | 17.7 | 6.3 | 9.72 |
| France | 16.5 | 6.3 | 8.2 |
| Sweden | 14.6 | 7.2 | 8.72 |
| Canada | 14.3 | 6.8 | 7.1 |
| United States3 | 12.5 | 7.0 | 8.7 |
Simanis and Coleman (1980).
National health expenditures as percent of gross national product were not available for 1976. The 1975 ratios are given. See Simanis and Coleman (1980).
Some analysts suggest that health spending as a proportion of GNP tends to grow in spurts. Countries appear to have relatively effective methods to stem the rise in health spending relative to GNP, then slippage in the system results in health spending escalating relative to GNP.
Nations implicitly or explicitly make judgments about the “correct” ratio of GNP allocated to health care. For example, Finland is reported to have earmarked 15 percent of GNP for health care under the assumptions that health care is socially desirable and that employment in the health sector is as good as any other type of employment (Perspective, 1982).
Why Health Expenditures Are Rising
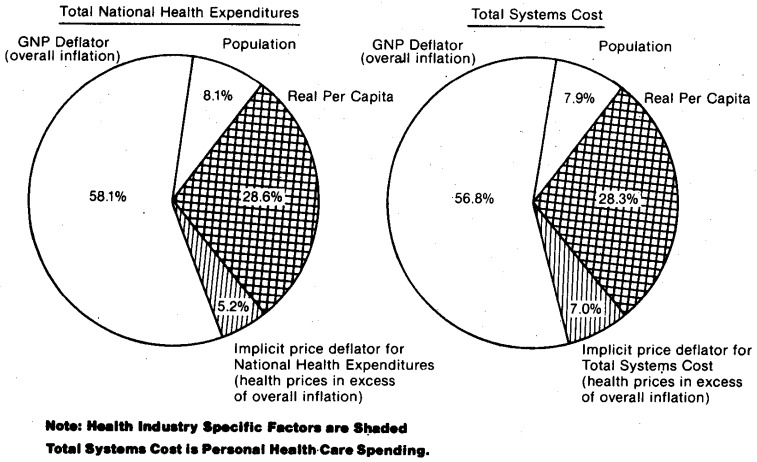
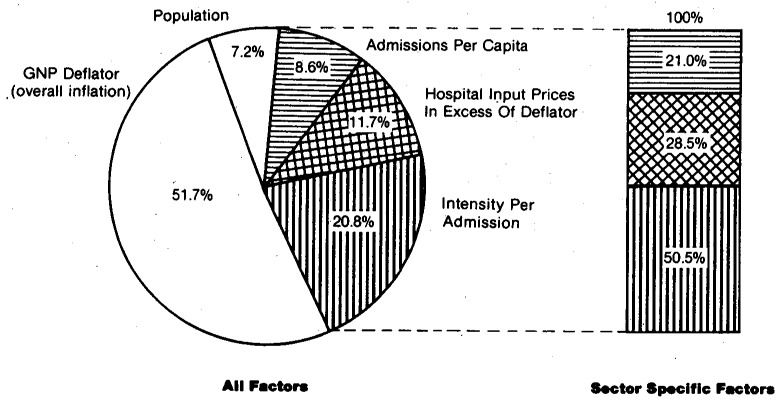
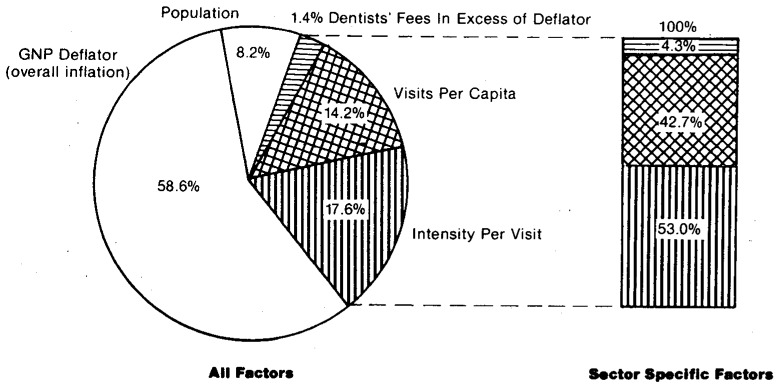
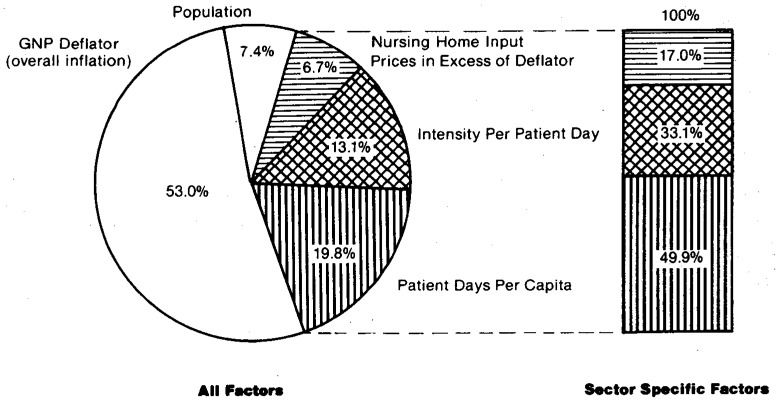
Many factors account for the rising cost of health care. The projection process uses a five-factor formula which accounts for how expenditures rise. The five components are changes in: (1) general inflation, (2) aggregate population, (3) medical-care prices in excess of overall price inflation (4) per capita visits and per capita patient days and (5) the mix and content of services and supplies per visit or per day. These five “how” factors (see Tables 3 and 4), two relating to the general economy and three specific to the health sector, account for all increases in expenditure growth since one factor (changes in the mix and content of services and supplies per visit or per patient day) is calculated as a residual. The five factors combine to form an accounting identity in the historical period.
Table 3. “How” Versus “Why” Medical Care Expenditures Rise1.
| “How” Medical Care Expenditures Rise | “Why” Medical Care Expenditures Rise | |
|---|---|---|
| Economy-Wide Factors | ||
| 1. | General Inflation | Montetary policies; fiscal policies relating to taxing, spending, and debt management; supply-side shocks such as energy price increases, food price increases caused by world-wide droughts, Social Security tax rate increases, and minimum wage increases; productivity changes; and monopoly powers of firms and unions over prices and wages. |
| 2. | Aggregate population growth | Birth rates, death rates, in migration, out migration. |
| “Health-Sector Specific” Factors | ||
|
| ||
| 3. | Growth in per capita patient visits and per capita patient days | Factors influencing the demand for and supply of medical care services such as: |
| ||
| 4. | Changes in the nature of services and supplies provided per visit or per patient day (product innovation, intensity of service, amenities, etc.)2 | Generally the same factors as in 3 above, however, the relative importance of particular factors may differ. |
| 5. | Medical care price increases relative to general price inflation | Generally the same factors as in 3 above, however, the relative importance of particular factors may differ and in some cases the sign of the factor may differ. For example, increasing the number of dentists relative to population in a given geographic area may cause dental prices to rise slower than would otherwise be the case and to expand utilization of dental services in the geographic area. In other words, expanding the supply of dentists, all other things constant, may have a negative impact on price increases but a positive impact on visits and intensity of services per visit. |
Martin Feldstein (1971) has made this distinction between “how” versus “why” medical care expenditures have risen. For analyses accounting for expenditure growth using the “how” approach, see M. Feldstein (1971,1981), P. Feldstein (1979), Klarman, Rice, Cooper, and Stettler (1970), and Mushkin (1979).
This factor is calculated as a residual by deflating current dollar expenditures per visit or per patient day by a relevant price index. This yields growth in “real services” per visit or per day.
Table 4. Factors Accounting for Growth in Expenditures for Selected Categories of Total Systems Cost, 1971 to 19811.
| Factors Accounting for “How” Medical Care Expenditures Rose | Community Hospital Care | Physicians' Services | Dentists' Services | Nursing Home Care Excluding ICF-MR | Total Systems Cost (Personal Health Care) | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| inpatient Expenses2 | Outpatient Expenses2 | |||||||
|
| ||||||||
| Inpatient Days | Admissions | |||||||
| Economy-Wide factors | ||||||||
| 1. | General inflation | 51.7% | 51.7% | 41.6% | 58.1% | 58.6% | 53.0% | 56.8% |
| 2. | Aggregate population growth | 7.2 | 7.2 | 5.6 | 8.1 | 8.2 | 7.4 | 7.9 |
| “Health-Sector Specific” Factors | ||||||||
| 3. | Growth in per capita visits or patient days | 4.2 | 8.6 | 17.9 | −3.4 | 14.2 | 19.8 | NA |
| 4. | Growth in real services per visit or per day (intensity) | 25.2 | 20.8 | 25.3 | 27.4 | 17.6 | 13.1 | NA |
| 5. | Medical care price increases relative to general price inflation3 | 11.7 | 11.7 | 9.6 | 9.8 | 1.4 | 6.7 | 7.0 |
| Addenda: Growth in real services per capita | — | — | — | — | — | — | 28.3 | |
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | |
NA = Not available
Total systems cost is called personal health care in Gibson and Waldo (1982).
Community hospital expenses are split into inpatient and outpatient expenses using the American Hospital Association (1982) procedure.
See Table A-13 for price variables.
From a behavioral or “why” point of view, the causal factors for each of the five “how” factors are analyzed (Table 3). During the projection process we determine our growth rates for the “how” factors by analyzing and evaluating the effects of the “why” factors. For example, in the nursing-home sector, we examine increases in the age 75 and over population, (a “why” factor) as one determinant of growth in nursing home days per capita (a “how” factor).
Understanding Health Care Expenditure Growth
General inflation, a “how” factor, accounted for approximately 57 percent of the increase in total systems cost (personal health care cost) for the period 1971-1981 (Table 4 and Figure 6). General inflation, a complex and volatile phenomenon, is caused by many factors including monetary policy, fiscal policy, supply-side shocks such as energy price increases, productivity changes, etc. (Table 3).
Figure 6. Factors Accounting for Growth in Total Health Costs 1971 to 1981.
While overall inflation is clearly the single most important factor accounting for expenditure growth, lowering the overall inflation rate will not reduce the ever-increasing amount of real resources flowing into the health sector. Health sector-specific factors relating to the demand for and supply of medical care services must be examined to understand the flow of real resources into the health sector relative to the rest of the economy.
Factors contributing to the rapid growth in health spending are numerous and interrelated (National Commission on the Cost of Medical Care, 1978). The interplay of demand pressures and supply incentives contribute to the growth in specific types of medical expenditures. Two factors are particularly note-worthy: first, a demand-side factor, the role of third party payments in increasing consumer demand for services, and second, a supply-side factor, the fee-for-service and cost-based reimbursement systems which lack incentives to provide medical care in the least expensive manner.
The third-party financing of medical care increases demand for services and incorporates cost-increasing incentives. Studies correlate increases in medical care prices and expenditures not only to increased insurance coverage, but also to the level of such coverage (National Commission on the Cost of Medical Care, 1978; Newhouse, 1978). As we approach the point where third parties finance 100 percent of the consumers' cost, providers and consumers of medical care appear to increasingly treat medical care as a free service at the time of decision-making, resulting in increased consumer demand for services. For example, in the hospital sector the proportion paid out of pocket has remained at roughly 10 percent from 1967 through 1981, yet community hospital revenues during this period have increased at an average annual rate of almost 16 percent. In the 2-year period 1979 to 1981, community hospital revenues rose 40 percent while a broad-based measure to finance such care, the GNP, rose 22 percent. Third-party payments play a very significant role in increasing access to quality care, but they also have the effect of divorcing utilization and price from ability to pay at the individual level and to a lesser extent at the aggregate level.
Third-party payment growth is stimulated by the provision of tax subsidies for private health insurance. These subsidies provide incentives to purchase more insurance (Congressional Budget Office, 1980; Feldstein 1981; Greenspan and Vogel, 1980). The additional insurance then encourages further use of medical care.
Third-party reimbursement systems incorporate incentives to increase costs (Enthoven, 1980). Retrospective cost-based reimbursement for hospitals and fee-for-service reimbursement for physicians reward those providers who supply larger quantities and more costly services with more revenues. An incentive is therefore provided to adopt new diagnostic and therapeutic procedures and techniques (product-innovative technologies) rather than to adopt new processes to more efficiently produce existing procedures and techniques (process-innovative technologies). (Altman and Blendon, 1979; Feldstein, 1981).
The diffusion of information relating to new techniques, procedures, and supplies (such as: implants, transplants, CT scans, life-saving drugs, etc.) can push up demand. First, as persons become aware of techniques, procedures, and supplies through the mass media they may pressure providers to make them available. Second, the consumer population purchases more comprehensive insurance at higher premium rates to reimburse for more expensive procedures and techniques (Feldstein, 1981). Political pressure may be applied to cover such innovations under public programs. Third, increased awareness can be associated with greater utilization of health services. Detailed physical examinations may diagnose conditions that cannot be cured with today's state-of-the-art medicine, but which may result in expensive maintenance programs.
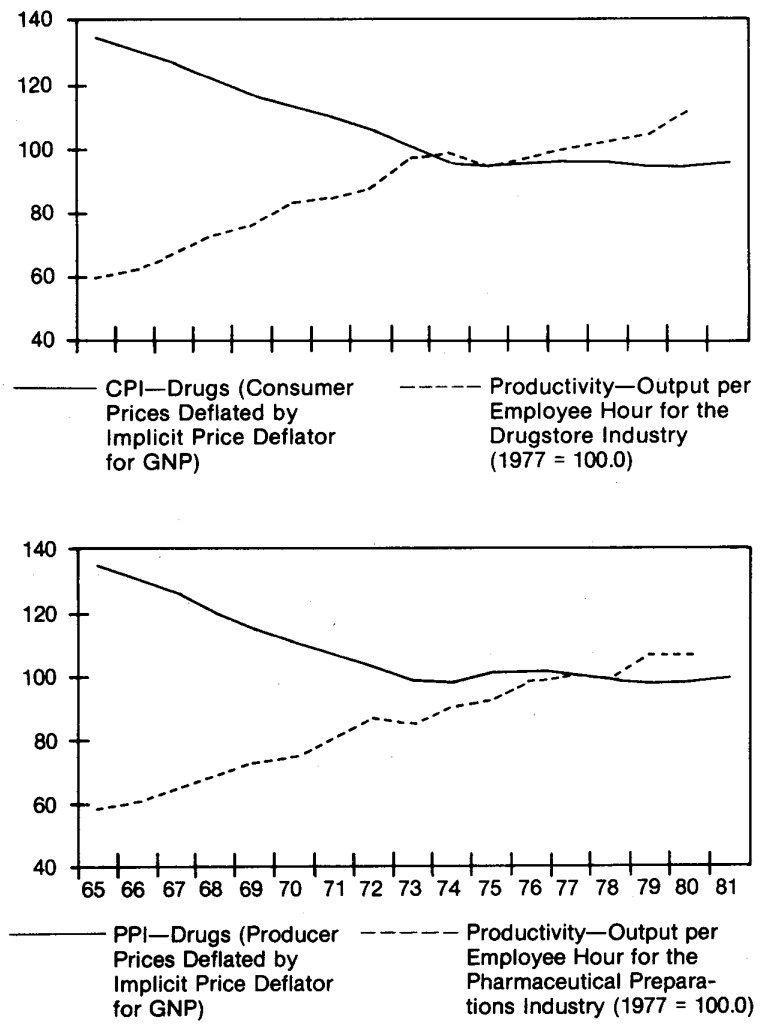
It has been suggested that productivity levels in the health-services sector are lower than in the overall economy; that the rate of increase in productivity is slower than in the private sector; and that significant increases can be made in current productivity levels. Baumol's model of unbalanced economic growth (1967) may have relevance for the health services sector (Mushkin et al., 1978).
Applying this to the health sector: If productivity or output per manhour increases faster in the nonhealth sector than in the health sector, and wages increase at the same rate in both sectors, then unit costs in the health sector must increase faster than in the nonhealth sector. Fragmentary evidence on wages, prices, and productivity is consistent with such an application of Baumol's model.
Between 1972 and 19812 wages in the health sector increased at an average annual rate of 8.3 percent compared to 7.8 percent in the total private economy (Bureau of Labor Statistics, Employment and Earnings). During the period 1969 to 1979, productivity in the health services industry is reported to have declined at an average annual rate of −1.4 percent per year while productivity in the private nonfarm economy increased at an average annual rate of 1.7 percent (Table A-24).3 For the same period as for wage increases above (1972-1981), the medical care services component of the Consumer Price Index rose at an average annual rate of 9.7 percent compared to the 8.1 percent rate for the fixed-weight personal consumption expenditure price index (Bureau of Economic Analysis, Survey of Current Business). Thus, medical care service prices increased at an average annual rate 20 percent faster than overall consumer prices. Price data were used, rather than unit-cost data, since cost data were not available for either the health-services sector or for the total private economy. If the percent mark-up of unit prices over unit costs is constant over time, the growth in both prices and unit costs will be the same. The difficulty in measuring output in the health services sector (Reder, 1969) has hampered efforts to measure price changes for a fixed unit of service over time. Some factors, such as the increasing sophistication of care that cannot be separated from a “fixed” unit of service over time, may result in medical care price statistics being biased upward over time. Other factors, such as separating services and procedures into finer components and billing individually for each service or procedure, may result in medical care price statistics being biased downward over time (Ginsberg, 1978; Showstack et al., 1979; Sobaski et al., 1975).
Table A-24. Average Annual Rate of Change in Productivity, Selected Industries, 1969-19791.
| Selected Industries | Productivity2 |
|---|---|
|
|
|
| Health Services | −1.4% |
| All Industries | 1.7 |
| Private Nonfarm Economy3 | 1.7 |
| Manufacturing | 2.7 |
| Transportation | 2.1 |
| Wholesale and Retail Trade | 1.4 |
| Finance, Insurance and Real Estate | 0.7 |
| All Services | 0.6 |
| Business Services | 0.7 |
| Other Services | 1.1 |
| Government and Government Enterprises | 0.7 |
Bureau of Industrial Economics (January 1982, p. 424).
Productivity is defined as gross product originating per hour worked. “Gross productivity originating” is constant dollar value added and represents that industry's contribution to real gross national product. “Productivity” is calculated by dividing gross product originating by hours worked. These measures differ from the Bureau of Labor Statistics' measures of productivity in the private nonfarm business sector, because of differences in coverage. See Bureau of Industrial Economics (January 1982, p. 424).
Excludes government and farms.
Relatively high price increases in the health services sector may be partially explained by lower productivity increases in the health care industry.4 The relatively high price increases, combined with an inelastic demand for medical care (Newhouse and Phelps, 1976; Newhouse et al., 1981), contributes to the increase in expenditures for health care relative to the GNP.
Another hypothesis relating to increasing costs is that physicians may be able to induce some demand for their service (Cotterill, 1979; Reinhardt, 1978). The patient's dependence upon the physician for technical decisions and the existence of third-party payments may provide the means for physicians to raise fees and increase intensity of services. According to the physician-induced demand and target-income models, increases in the number of physicians are associated with increases in expenditures for their services. This relationship becomes more important when the interaction of physicians' services and other related health services is noted (Blumberg, 1979; Pauly, 1980; Pauly and Redisch, 1973; Redisch, 1978). Blumberg estimates that the physician influences approximately 70 percent of total systems cost (personal health care expenditures). Thus, according to this hypothesis, the number of physicians is correlated not only with expenditures for physicians' services, but also with expenditures for hospital care, other professional services, drugs, and so forth.
Between 1965 and 1981, the number of active physicians increased at an average annual rate of 3.0 percent, triple the average annual rate for the population, 1.1 percent. For the period 1981 to 1990, the Bureau of Health Professions projects that the number of active physicians will increase at an average annual rate of 2.7 percent (Table A-4). This increase in the number of physicians is likely to be associated with increases in per capita and aggregate medical expenditures, especially for services significantly covered by third-party payments. If insurance pays all costs, a provider's pricing behavior has little effect on market shares (Congressional Budget Office, May 1982A). For example, if a market area has full insurance coverage (no consumer cost sharing), an individual physician can raise his fees without his services becoming less attractive (from a price point of view) at the time of purchase.
Increases in real income and shifts in the age distribution of the population toward the more aged segment expands demand (Denton and Spencer, 1975; Dresch et al., 1981; Fisher, 1980; Russell, 1981; Torrey, 1981; Torrey, 1982).
An Important factor that is sometimes overlooked is that achieving satisfaction in all areas of life is conditioned on and affected by one's subjective feeling of health status. If one does not feel well, other satisfactions (material and nonmaterial) are typically diminished and in some cases eliminated.
Psychological factors (expectations, motivations, past experiences, etc.) are important in understanding most all economic behavior (Alhadeff, 1982; Katona, 1975; Maital, 1982; Scitovsky, 1976), but such factors are especially important in understanding consumer and provider behavior in medical care markets. Pain, guilt, uncertainty, and subjective well-being (experienced in some cases by the patient, families, and physician) can put significant pressures on patients, their families, and providers to utilize quantities and qualities of medical care that may appear excessive when viewed from a strictly cost-benefit point of view.
A last theory is that some services once provided free by household members are now provided by health professionals (Fuchs, 1979). This factor contributes to growth in the health sector and is of particular importance for one of the fastest growing services, long-term care (Chiswick, 1976). The increasing proportion of females 16 years of age and over who are in the labor force, contributes to the shift in providing services. This proportion has increased from 39 percent in 1965 to 52 percent in 1981 (Council of Economic Advisors, 1982) resulting in a smaller number of persons available for productive, nonpaying work in the household. Because more women are working, the opportunity cost of providing unpaid personal-care services for relatives and friends has increased. In addition, the size of the average household decreased from 3.3 persons in 1965 to 2.7 in 1981, a decline of 18 percent (Bureau of Census, 1981). As average household size decreases due to social, economic and demographic forces, there are fewer household members to provide personal care.
As more women join the labor force and as the average household size decreases, some long-term care activities have been “pushed” out of the household and into the for-pay health sector. It is also likely that increased third-party payments for coverage of health services have increased this trend.
Total Systems Cost Per Capita (TSCPC)
The net effect of all the causal factors on spending for health care can be summarized in personal health care cost per capita. It is important to have a comprehensive definition of costs when evaluating a public program, regulatory policy, insurance benefit package or marketing strategy since each of these is likely to have direct and indirect effects on medical care utilization, quality, and price. Total systems cost per capita (TSCPC) provides such a measure.
Total systems cost per capita includes all medical care costs related to direct patient care: long-term and short-term, inpatient and ambulatory, covered and uncovered by third-party reimbursement. It includes all services and supplies included in personal health care (Gibson and Waldo, 1982) such as hospital care, physicians' services, drugs, nursing-home care, etc. (Table 5).
Table 5. Percentage Distribution of Total Systems Cost, by Type of Service, Selected Years, 1950-19901.
| Calendar Year | Total Systems Cost Per Capita Current Dollars | Total Systems Cost Current Dollars | Total Systems Cost | Hospital Care | Physicians' Services | Dentists' Services | Other Professional Services | Drugs and Medical Sundries | Eyeglasses and Appliances | Nursing-Home Care | Other Health Services |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Historical Estimates | (Amount in (dollars) | (Amount in (billions) | Percentage Distribution | ||||||||
| 1950 | $ 70 | $ 10.9 | 100.0% | 35.4% | 25.2% | 8.8% | 3.6% | 15.9% | 4.5% | 1.7% | 4.8% |
| 1960 | 129 | 23.7 | 100.0 | 38.4 | 24.0 | 8.3 | 3.6 | 15.4 | 3.3 | 2.2 | 4.7 |
| 1965 | 181 | 35.8 | 100.0 | 38.8 | 23.7 | 7.9 | 2.9 | 14.5 | 3.3 | 5.8 | 3.2 |
| 1970 | 312 | 65.1 | 100.0 | 42.6 | 22.0 | 7.3 | 2.4 | 12.3 | 3.0 | 7.2 | 3.2 |
| 1971 | 341 | 72.0 | 100.0 | 42.8 | 22.1 | 7.0 | 2.3 | 11.9 | 2.8 | 7.8 | 3.2 |
| 1975 | 531 | 116.8 | 100.0 | 44.6 | 21.4 | 7.1 | 2.2 | 10.2 | 2.7 | 8.6 | 3.2 |
| 1979 | 825 | 188.9 | 100.0 | 45.6 | 21.3 | 7.1 | 2.5 | 9.1 | 2.4 | 9.3 | 2.7 |
| 1980 | 947 | 219.4 | 100.0 | 45.8 | 21.4 | 7.0 | 2.6 | 8.8 | 2.3 | 9.4 | 2.7 |
| 1981 | 1090 | 255.0 | 100.0 | 46.3 | 21.5 | 6.8 | 2.5 | 8.4 | 2.2 | 9.5 | 2.8 |
| Projections | |||||||||||
| 1983 | 1359 | 323.6 | 100.0 | 47.8 | 21.6 | 6.7 | 2.4 | 7.7 | 1.8 | 9.4 | 2.6 |
| 1985 | 1683 | 408.2 | 100.0 | 48.2 | 21.5 | 6.6 | 2.5 | 7.4 | 1.8 | 9.5 | 2.5 |
| 1990 | 2701 | 684.4 | 100.0 | 49.7 | 20.7 | 6.2 | 2.5 | 6.9 | 1.6 | 9.8 | 2.5 |
Total systems cost is called personal health care expenditures in Gibson and Waldo (1982).
The TSCPC concept captures indirect effects and leakages. If, for example, hospital rate setting restrains hospital inpatient costs, but implicitly provides pressures to substitute ambulatory and nursing-home care, TSCPC will capture the leakage from one health sector to another health sector. There can be both leakage from one sector and significant savings when the total net effect is considered.
Some questions relating to TSCPC are:
What is the magnitude of the leakage?
Is the nature of the leakage socially desirable? That is, what services and payers are affected, and what happens to prices, utilization, quality, and access for various socioeconomic groups?
Does TSCPC increase or decrease as it is related to the specific policy, regulation, or marketing strategy?
To provide further insight on leakage and indirect effects, we examine the relationship of substitutes and complements to TSCPC. There are significant substitute and complement relationships among various components of TSCPC (Davis and Russell, 1972; Feldstein, 1970; Hellinger, 1977; Russell, 1973). An example of a complementary relationship occurs when a patient incurs a physician expense to obtain a prescription drug, to be admitted to a hospital, or to purchase orthopedic appliances covered by third-party reimbursements.
To some extent hospital care and nursing-home care are both substitutes and complements. Due to medical, family, and/or financial reasons some segments of the patient population may receive institutional care in a hospital rather than a nursing-home setting or vice versa. Hospital care and nursing-home care are substitutes in the above example. On the other hand, patients may consecutively stay in a hospital, a nursing home, and at home (with home health care) depending upon the level of care needed. This switching of modalities of care reflects the complementary nature of hospital care, nursing home care, and home care.
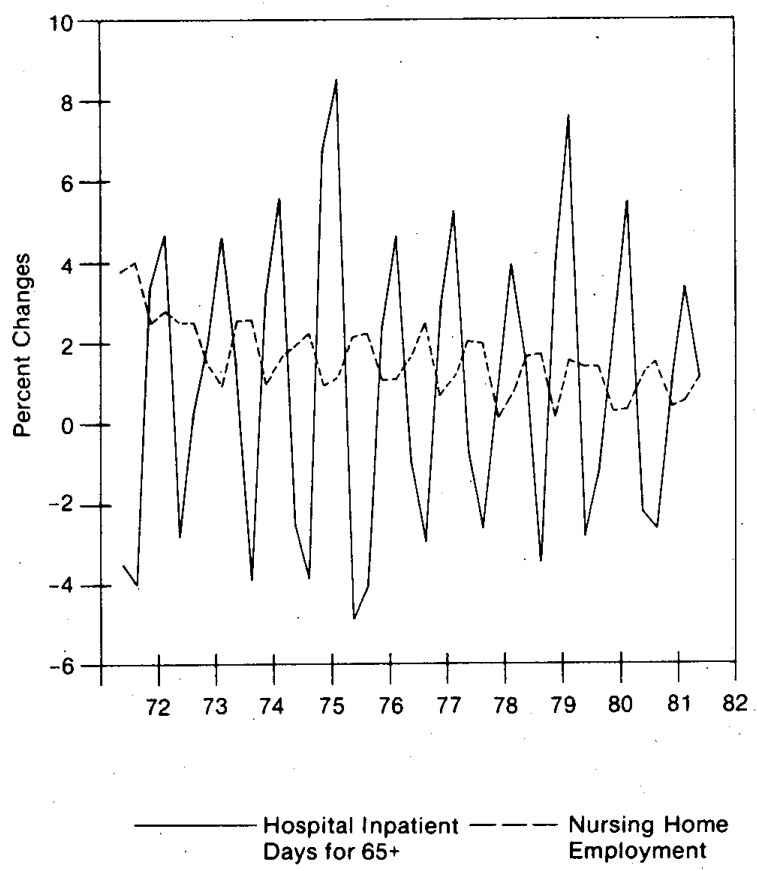
An inverse association between the nursing home sector and hospital care is illustrated in Figure 15. Over the period 1972 to mid-year 1982, quarter-to-quarter percent changes in community hospital inpatient days for the aged are negatively associated with quarter-to-quarter percent changes in total employment in the nursing-home sector.5 Quarterly nursing employment was used as a rough indicator of utilization of nursing home days (in the absence of utilization data). The causal factors (seasonal and nonseasonal) leading to this negative association need to be studied. Since a day in a community hospital costs 7 to 8 times as much as a day in a nursing home, it is important that patients be placed in the proper continuum of care.6
Figure 15. Quarterly Percent Changes in Community Hospital Inpatient Days for Aged and Nursing Home Employment, 1972 to 19821.
1Quarter-to-quarter percent changes are graphed, not percent changes from same quarter a year ago.
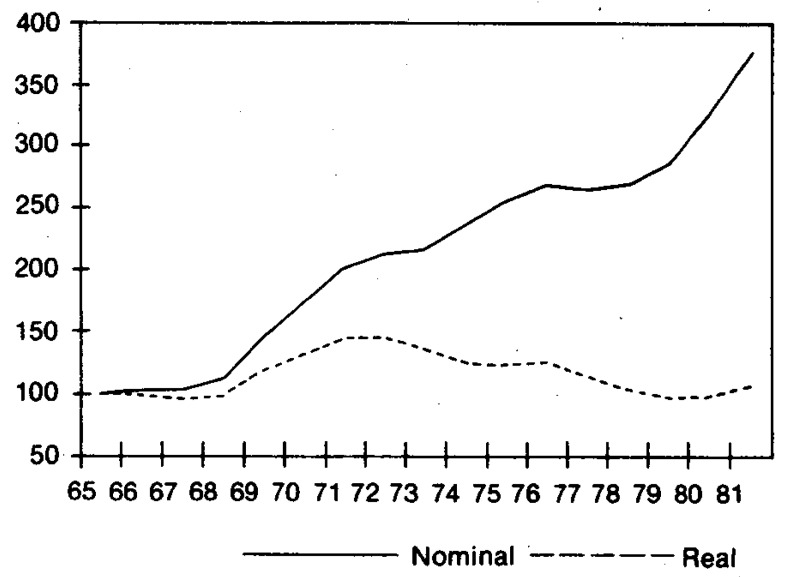
TSCPC: Historical Perspective
TSCPC has grown from $70 in 1950 to $1090 in 1981, an average annual rate of increase of 9.2 percent (Tables 5 and A-8). For the last decade (1971 to 1981) TSCPC increased at an average annual rate of 12.3 percent.
Table A-8. Average Annual Percent Increases in Per Capita Total Systems Cost and Per Capita GNP, Current Dollars and Constant Dollars, Selected Periods, 1950-1990.
| Selected Periods | Her capita Total Systems Cost1 | Per Capita GNP | Implicit Price Deflator for GNP | CPI-W3 | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Current Dollars | Constant Dollars2 | Current Dollars | Constant Dollars2 | |||
|
|
|
|
|
|
|
|
| Average Annual Rates of Increase | ||||||
|
|
||||||
| 1950-1955 | 5.8% | 3.1% | 5.1 % | 2.5% | 2.6% | 2.2% |
| 1955-1960 | 6.7 | 4.1 | 3.0 | 0.5 | 2.5 | 2.0 |
| 1960-1965 | 7.0 | 5.3 | 4.9 | 3.2 | 1.6 | 1.3 |
| 1965-1970 | 11.6 | 7.0 | 6.4 | 2.1 | 4.2 | 4.3 |
| 1970-1975 | 11.2 | 4.3 | 8.2 | 1.5 | 6.6 | 6.8 |
| 1975-1980 | 12.3 | 4.7 | 10.0 | 2.6 | 7.3 | 8.9 |
| 1980-1985 | 12.2 | 4.5 | 8.8 | 1.4 | 7.3 | 7.6 |
| 1985-1990 | 9.9 | 4.4 | 7.5 | 2.1 | 5.3 | 5.2 |
| 1950-1981 | 9.2 | 4.8 | 6.4 | 2.0 | 4.3 | 4.4 |
| 1950-1965 | 6.5 | 4.2 | 4.3 | 2.1 | 2.2 | 1.8 |
| 1965-1981 | 11.9 | 5.3 | 8.3 | 2.0 | 6.2 | 6.8 |
| 1971-1981 | 12.3 | 4.6 | 9.4 | 1.9 | 7.4 | 8.4 |
| 1979-1981 | 14.9 | 5.1 | 9.1 | −0.3 | 9.4 | 11.8 |
| 1981-1983 | 11.7 | 4.5 | 7.7 | 0.8 | 6.8 | 6.9 |
| 1983-1985 | 11.3 | 4.3 | 9.1 | 2.2 | 6.8 | 7.0 |
| 1981-1990 | 10.6 | 4.4 | 7.9 | 1.8 | 5.9 | 6.0 |
Per capita total systems cost is called per capita personal health care expenditures in Gibson and Waldo (1982).
Per capita total systems cost and GNP were each deflated by the implicit price deflator for GNP (1972 = 100.0).
“Consumer Price Index—all items, wage earners” is shown for comparison only.
The composition of TSCPC has significantly shifted over time. Two institutional services, hospital care7 and nursing-home care, have significantly increased their relative shares over the period 1950-1981 rising from a combined share of 37 percent in 1950 to 56 percent in 1981 (Table 5). All ambulatory services and medical supplies have decreased their relative shares and noninstitutional services and medical supplies as a share of TSCPC have dropped from 63 percent to 44 percent during this period. In the last decade expenditures for services of physicians, dentists, and other professionals have maintained their relative shares of TSCPC. Drugs and medical sundries, eyeglasses and appliances, and other health services have declined in relative importance during this decade.
Sources funding TSCPC have also shifted substantially during the 1950 to 1981 period (Table 6). In 1950, patient direct payments accounted for nearly two-thirds of the financing. The Federal government, private health insurance, and State and local governments financed roughly 10 percent each (Table 6). During the period 1950 to 1965 Federal and State and local shares were fairly constant, but private health insurance grew very rapidly. In 1950, private insurance paid 9 percent, in 1965 that share had almost tripled to 24 percent. By 1981, the share reached 26 percent.
Table 6. Percentage Distribution of Total Systems Cost, by Source of Funds, Selected Years, 1950-19901.
| Calendar Year | Total Systems Cost Per Capita, Current Dollars | Total Systems Cost, Current Dollars | Total Systems Cost | Patient Direct Payments | All Third Parties | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total Private and Public | Private Health Insurance | Other Private | Public | |||||||
|
| ||||||||||
| Total | Federal | State and Local | ||||||||
|
| ||||||||||
| Historical Estimates | (Amount in dollars) | (Amount in billions) | Percentage Distribution | |||||||
|
|
|
|
|
|||||||
| 1950 | $ 70 | $ 10.9 | 100.0% | 65.5% | 34.5% | 9.1 % | 2.9% | 22.4% | 10.4% | 12.0% |
| 1960 | 129 | 23.7 | 100.0 | 54.9 | 45.1 | 21.1 | 2.3 | 21.8 | 9.3 | 12.5 |
| 1965 | 181 | 35.8 | 100.0 | 51.8 | 48.2 | 24.4 | 2.2 | 21.6 | 10.1 | 11.4 |
| 1970 | 312 | 65.1 | 100.0 | 39.9 | 60.1 | 24.0 | 1.6 | 34.5 | 22.3 | 12.2 |
| 1971 | 341 | 72.0 | 100.0 | 38.6 | 61.4 | 24.1 | 1.7 | 35.6 | 23.3 | 12.3 |
| 1975 | 531 | 116.8 | 100.0 | 33.4 | 66.6 | 25.8 | 1.4 | 39.5 | 26.9 | 12.6 |
| 1979 | 825 | 188.9 | 100.0 | 32.7 | 67.3 | 26.6 | 1.4 | 39.3 | 28.2 | 11.1 |
| 1980 | 947 | 219.4 | 100.0 | 32.9 | 67.1 | 26.0 | 1.4 | 39.7 | 28.6 | 11.2 |
| 1981 | 1090 | 255.0 | 100.0 | 32.1 | 67.9 | 26.2 | 1.4 | 40.4 | 29.3 | 11.1 |
| Projections | ||||||||||
| 1983 | 1359 | 323.6 | 100.0 | 32.1 | 67.9 | 26.3 | 1.4 | 40.2 | 29.2 | 11.0 |
| 1985 | 1683 | 408.2 | 100.0 | 32.2 | 67.8 | 26.4 | 1.4 | 40.0 | 29.5 | 10.5 |
| 1990 | 2701 | 684.4 | 100.0 | 30.9 | 69.0 | 26.1 | 1.3 | 41.6 | 31.5 | 10.1 |
Total systems cost is called personal health care expenditures in Gibson and Waldo (1982).
Medicare and Medicaid took effect in mid-1966 and by 1967 the Federal government's share of TSCPC advanced to 21 percent; the State and local government share stayed roughly constant at 13 percent; and patient direct payments dropped to 43 percent.
By 1981 the percentages paid by the major payers were as follows: patient direct payments, 32 percent; private health insurance, 26 percent; Federal government, 29 percent; and State and local governments, 11 percent (Table 6).
Inflation-adjusted8 TSCPC increased at an average annual rate of 4.8 percent for the period, 1950 to 1981 (Tables A-7 and A-8) and during the last ten years at a 4.6-percent rate. A higher annual rate of 5.1 was experienced in the period 1979 to 1981 while inflation-adjusted GNP per capita had a —0.3 average annual rate of change (Table A-8).
Table A-7. Per Capita Total Systems Cost, Nominal and Constant Dollar, Selected Years, 1950-1990.
| Calendar Year | Total Systems Cost Per Capita1 Current Dollars | Total Systems Cost Per Capita Constant Dollars2 | Gross National Product Per Capita, Current Dollars | Total Systems Cost as Percent of GNP |
|---|---|---|---|---|
|
|
|
|
|
|
| Historical Estimates | ||||
|
|
||||
| 1950 | $ 70 | $131 | $1,852 | 3.8% |
| 1960 | 129 | 187 | 2,755 | 4.7 |
| 1965 | 181 | 243 | 3,492 | 5.2 |
| 1970 | 312 | 342 | 4,759 | 6.6 |
| 1971 | 341 | 355 | 5,100 | 6.7 |
| 1975 | 531 | 422 | 7,045 | 7.5 |
| 1979 | 825 | 505 | 10,555 | 7.8 |
| 1980 | 947 | 530 | 11,365 | 8.3 |
| 1981 | 1,090 | 557 | 12,555 | 8.7 |
| Projections | ||||
|
|
||||
| 1983 | 1,359 | 609 | 14,562 | 9.3 |
| 1985 | 1,683 | 662 | 17,348 | 9.7 |
| 1990 | 2,701 | 822 | 24,879 | 10.9 |
Total systems cost per capita is called per capita personal health care expenditures in Gibson and Waldo (1982).
Per capita total systems cost was deflated by the implicit price deflator for GNP (1972= 100.0). See Table 1 for values of the deflator.
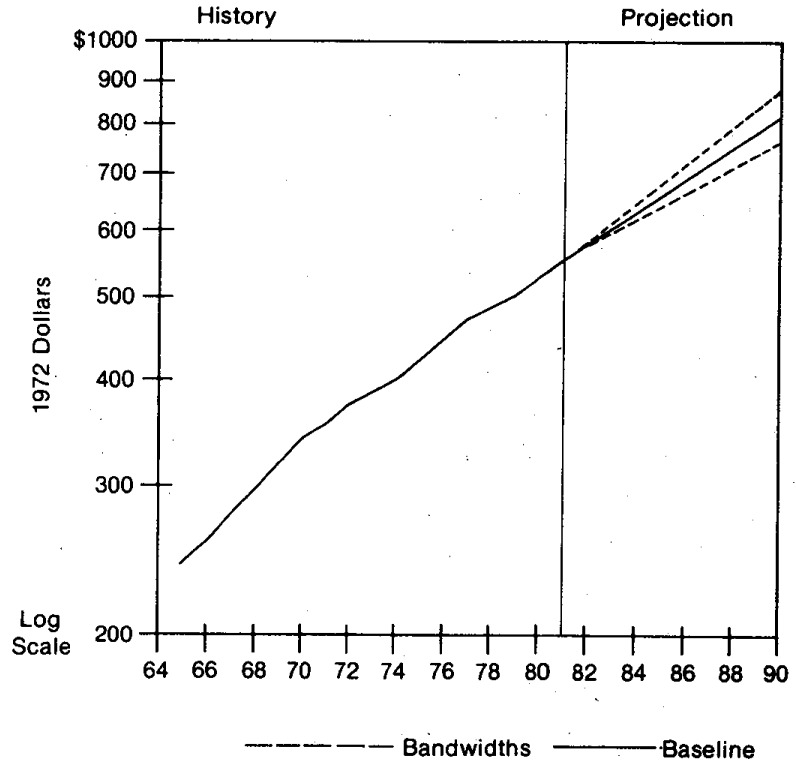
TSCPC Projections
In the baseline projections current dollar TSCPC rises at an average annual rate of 10.6 percent from 1981 to 1990 (Table A-8 and Figure 7), substantially below the 1971-1981 rate of 12.3 percent and reflecting significant deceleration of inflation. Inflation-adjusted TSCPC is expected to increase at an average annual rate of 4.4 percent during the 1981 to 1990 period with a range of approximately 3.6 percent to 5.2 percent. This range of estimates reflects historical variability in the growth of inflation-adjusted TSCPC (Table A-15 and Figure 8).
Figure 7. Total Systems Cost Per Capita 1965 to 1990, with Bandwidth Intervals1 2.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in total systems cost per capita for 1966-1981 (see Table A-15) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
2Total systems cost per capita is also referred to as personal health care spending per capita.
Table A-15. Measures of Central Tendency and Variability for Year-to-Year Changes in Total Systems Cost Per Capita and GNP Per Capita, 1966-19811.
| Variable | Measures of Variability2 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of Mean3 | ||
|
| |||||
| Mean | MEDIAN | ||||
| Total Systems Cost Per Capita, Current Dollars | 11.9% | 11.9% | 1.8% | 0.470% | 0.039 |
| Implicit Price Deflator for GNP | 6.3 | 5.6 | 2.2 | 0.560 | 0.090 |
| Total Systems Cost Per Capita Deflated by Implicit Price Deflator for GNP | 5.3 | 5.4 | 1.5 | 0.383 | 0.072 |
| Per Capita GNP, Current Dollars | 8.3 | 8.2 | 2.1 | 0.550 | 0.066 |
| Per Capita GNP, Constant Dollars | 2.0 | 1.9 | 2.4 | 0.625 | 0.312 |
| Total Systems Cost as a Percent of GNP | 3.3 | 2.7 | 2.8 | 0.732 | 0.222 |
There are 16 annual percent changes for the period 1966-1981.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of nonsampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
Figure 8. Constant Dollar Total Systems Cost Per Capita 1965 to 1990, with Bandwidth Intervals1 (Inflation-Adjusted to 1972 Dollars)2.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in constant dollar (inflation adjusted) total systems cost per capita for 1966-1981 (see Table A-15) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
2Total systems cost per capita (personal health care spending per capita) was deflated by the implicit price deflator for the GNP.
In the 1980's we expect to see a continuation of the historical pattern of institutional care increasing its share of TSCPC. We do expect some modifications in light of the underlying fiscal pressures, demographic shifts and new technologies.
Demographic shifts in the age composition of the population, fiscal pressures of the Federal and State and local governments, changes in the mix of services (see Table 5), and pressures on employers and individuals to increase deductibles and coinsurance on private health insurance plans (Lawson, 1982) all contribute to shifts in the expected sources of financing for TSCPC in the 1980's (Table 6).
In the following section, we will explore the impact of these factors on the various individual sectors of the health care industry.
Projection Trends by Type of Health Expenditures
In this section, we present highlights relating to projection trends for each of the 12 types of expenditures. First, we provide a historical perspective with commentary on factors influencing expenditure growth. Second, we present a synopsis of the short-term outlook and the long-term projections. Third, we include highlights of projections of sources of funds.
Hospital Care
Total Hospital Care: Historical Perspective
In this age of complex technologies and procedures, hospitals have become the focal point of the health industry. Hospital care as a percent of total system costs, increased from 35 percent in 1950 to 46 percent in 1981 and is expected to garner an increased share by 1990 (Table 5). The $118 billion spent on hospital care in 1981 (Table 7) comprises 4 percent of GNP. To put this expenditure amount into perspective, as it relates to services provided: in 1981 6,933 hospitals with 1.4 million beds handled 39.2 million admissions and provided 387 million patient days of service. In addition, 265 million outpatient visits were provided (American Hospital Association, 1982). Although the 10-percent proportion of the population with one or more hospital episodes has not changed in the last decade (Table A-20), the intensity and sophistication of care has increased substantially (Figure 5). We first examine total hospital costs and then present synopses of spending patterns in the major hospital components.
Table 7. National Health Expenditures by Type of Expenditure, Selected Years, 1950-1990.
| Historical Estimates | Projections | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| 1950 | 1960 | 1970 | 1971 | 1975 | 1979 | 1980 | 1981 | 1983 | 1985 | 1990 | |
| (amount in billions) | |||||||||||
| Total | $12.7 | $26.9 | $74.7 | $83.3 | $132.7 | $215.0 | $249.0 | $286.6 | $362.3 | $465.4 | $755.6 |
| Health Services and Supplies | 11.7 | 25.2 | 69.3 | 77.2 | 124.3 | 204.5 | 237.1 | 273.5 | 347.4 | 438.4 | 728.9 |
| Personal Health Care | 10.9 | 23.7 | 65.1 | 72.0 | 116.8 | 188.9 | 219.4 | 255.0 | 323.6 | 408.2 | 684.4 |
| Hospital Care | 3.9 | 9.1 | 27.8 | 30.8 | 52.1 | 86.1 | 100.4 | 118.0 | 154.7 | 196.7 | 340.1 |
| Physicians' Services | 2.7 | 5.7 | 14.3 | 15.9 | 24.9 | 40.2 | 46.8 | 54.8 | 69.8 | 87.9 | 141.9 |
| Dentists' Services | 1.0 | 2.0 | 4.7 | 5.1 | 8.2 | 13.3 | 15.4 | 17.3 | 21.6 | 26.8 | 42.3 |
| Other Professional Services | 0.4 | 0.9 | 1.6 | 1.6 | 2.6 | 4.7 | 5.6 | 6.4 | 7.9 | 10.1 | 17.4 |
| Drugs & Medical Sundries | 1.7 | 3.7 | 8.0 | 8.6 | 11.9 | 17.2 | 19.3 | 21.4 | 24.9 | 30.2 | 47.3 |
| Eyeglasses & Appliances | 0.5 | 0.8 | 1.9 | 2.0 | 3.2 | 4.6 | 5.1 | 5.7 | 6.0 | 7.3 | 11.2 |
| Nursing Home Care | 0.2 | 0.5 | 4.7 | 5.6 | 10.1 | 17.6 | 20.6 | 24.2 | 30.3 | 38.9 | 67.1 |
| Other Health Services | 0.5 | 1.1 | 2.1 | 2.3 | 3.7 | 5.1 | 6.0 | 7.2 | 8.5 | 10.3 | 17.3 |
| Program Admin. & Net Cost of Insurance | 0.5 | 1.1 | 2.7 | 3.4 | 4.4 | 9.3 | 10.7 | 11.2 | 16.0 | 20.8 | 27.8 |
| Government Public Health Activities | 0.4 | 0.4 | 1.4 | 1.8 | 3.2 | 6.2 | 7.0 | 7.3 | 7.8 | 9.4 | 16.7 |
| Research & Construction of Medical Facilities | 1.0 | 1.7 | 5.4 | 6.1 | 8.4 | 10.5 | 11.8 | 13.1 | 14.9 | 18.0 | 26.7 |
| Research | 0.1 | 0.7 | 2.0 | 2.1 | 3.3 | 4.8 | 5.3 | 5.7 | 5.8 | 6.5 | 9.7 |
| Construction | 0.8 | 1.0 | 3.4 | 4.0 | 5.1 | 5.7 | 6.5 | 7.5 | 9.1 | 11.5 | 17.0 |
Historical estimates are reported in Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982, pp. 1-36.
Table A-20. Percent of Persons with Hospitalization, Physician Visits, and Dental Visits, Selected Years 1968-19811.
| Type of Service | Calendar year | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1968 | 1969 | 1970 | 1971 | 1975 | 1979 | 1980 | 1981 | |
|
|
|
|||||||
| Hospitalization | ||||||||
|
|
||||||||
| Percent of persons with 1 hospital episode or more | 9.6% | 10.3% | 10.3% | 10.5% | 10.6% | 10.3% | 10.4% | 10.2% |
| Physician Visits | ||||||||
|
|
||||||||
| Percent of persons with visits in past year | 71.2 | 69.4 | 71.9 | 72.4 | 75.2 | 75.1 | 74.9 | 74.3 |
| Dental Visits | ||||||||
|
|
||||||||
| Percent of persons with visits in past year | N.A. | 45.0 | 46.8 | 47.1 | 50.3 | 50.2 | 49.9 | 50.0 |
N.A. = Not available
Source is various issues of Current Estimates From the Health Interview Survey: United States, National Center for Health Statistics, U.S. Department of Health and Human Services.
Figure 5. Factors Accounting for Growth in Expenditures for Community Hospital Inpatient Care 1971 to 1981.
The industry appears to be undergoing forms of productline expansion and horizontal integration in response to the increasing demand pressures on the sector. Hospitals are expanding services offered to include greater emphasis on ambulatory care (such as hemodialysis, physical therapy, treatment for alcoholism and chemical dependency); home health services; hospice care; and skilled nursing care. Horizontal integration appears to be taking place with the increased formation of multi-hospital chains. In addition there is a shift toward the for-profit sector. For the period 1971 to 1981 investor-owned (for-profit) community hospital beds increased at an average annual rate 3 to 4 times faster than total community hospital beds.
Total hospital expenditures in the last ten years increased at an average annual rate of 14.4 percent (Table 8). The 1981 hospital outlays of $118 billion were distributed to four major sectors: community hospital inpatient care (72.6 percent), community hospital outpatient care (11.2 percent), Federal hospital care (8.0 percent), and all other hospital care (8.2 percent).
Table 8. National Health Expenditures, Average Annual Percent Changes by Type of Expenditures, Selected Periods, 1950-1990.
| 1950-1955 | 1955-1960 | 1960-1965 | 1965-1970 | 1970-1975 | 1975-1980 | 1980-1985 | 1985-1990 | 1971-1981 | 1981-1990 | 1979-1981 | 1981-1983 | 1983-1985 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||
| Total | 7.0% | 8.7% | 9.2% | 12.3% | 12.2% | 13.4% | 12.9% | 10.6% | 13.2% | 11.4% | 15.5% | 12.4% | 12.2% |
| Health Services and Supplies | 7.6 | 8.3 | 8.7 | 12.6 | 12.4 | 13.8 | 13.1 | 10.7 | 13.5 | 11.5 | 15.7 | 12.7 | 12.3 |
| Personal Health Care | 7.6 | 8.6 | 8.6 | 12.7 | 12.4 | 13.4 | 13.2 | 10.9 | 13.5 | 11.6 | 16.2 | 12.7 | 12.3 |
| Hospital Care | 8.9 | 9.0 | 8.8 | 14.9 | 13.4 | 14.0 | 14.4 | 11.6 | 14.4 | 12.5 | 17.1 | 14.5 | 12.8 |
| Physicians' Services | 6.1 | 9.0 | 8.3 | 11.1 | 11.7 | 13.4 | 13.4 | 10.1 | 13.2 | 11.2 | 16.7 | 12.9 | 12.2 |
| Dentists' Services | 9.4 | 5.6 | 7.3 | 11.1 | 11.6 | 13.3 | 11.7 | 9.5 | 13.1 | 10.4 | 14.0 | 11.8 | 11.4 |
| Other Professional Services | 7.3 | 8.9 | 3.7 | 9.1 | 10.4 | 16.5 | 12.4 | 11.5 | 14.6 | 11.8 | 15.9 | 11.4 | 12.9 |
| Drugs & Medical Sundries | 6.7 | 8.9 | 7.2 | 9.1 | 8.3 | 10.1 | 9.4 | 9.4 | 9.6 | 9.2 | 11.4 | 7.8 | 10.2 |
| Eyeglasses & Appliances | 4.2 | 5.1 | 8.6 | 10.7 | 10.1 | 10.2 | 7.4 | 8.9 | 11.2 | 7.7 | 11.2 | 2.2 | 10.7 |
| Nursing Home Care | 10.8 | 11.0 | 31.5 | 17.8 | 16.5 | 15.4 | 13.5 | 11.5 | 15.7 | 12.0 | 17.4 | 11.9 | 13.3 |
| Other Health Services | 11.9 | 3.7 | 0.7 | 12.5 | 12.2 | 10.4 | 11.4 | 10.8 | 11.9 | 10.2 | 18.6 | 8.7 | 10.4 |
| Program Admin. & Net Cost of Insurance | 14.6 | 6.7 | 13.8 | 10.4 | 10.3 | 19.5 | 14.1 | 6.0 | 12.6 | 10.6 | 10.0 | 19.3 | 14.0 |
| Government Public Health Activities | 0.9 | 1.9 | 14.5 | 11.8 | 17.3 | 17.3 | 6.1 | 12.1 | 15.2 | 9.7 | 7.9 | 3.3 | 10.1 |
| Research & Construction of Medical Facilities | −2.2 | 14.7 | 15.0 | 9.1 | 9.3 | 7.1 | 8.7 | 8.2 | 7.9 | 8.2 | 11.9 | 6.5 | 9.8 |
| Research | 12.4 | 25.8 | 18.0 | 5.4 | 11.1 | 9.8 | 4.0 | 8.4 | 10.3 | 6.1 | 8.7 | 1.1 | 5.8 |
| Construction | −5.0 | 10.0 | 13.8 | 11.4 | 8.1 | 5.1 | 12.1 | 8.1 | 6.5 | 9.5 | 14.5 | 10.5 | 12.2 |
Total Hospital Care: Projections
The short-term outlook is for total hospital expenditures to rise from $118 billion in 1981 to $155 billion in 1983 (Table 7). Total hospital expenditures are expected to reach $197 billion in 1985 and $340 billion in 1990 (Figure 9).
Figure 9. Total Hospital Expenditures 1965 to 1990, with Bandwidth Intervals1.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in total hospital expenditures for 1966-1981 (see Table A-12) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
Over the period 1965 to 1981, growth in total hospital spending exhibited significant variation (Tables 8 and A-12) and it is likely that the 1981 to 1990 period will experience volatility and spurts in spending. However, the growth in total hospital spending is less volatile than growth in the GNP. The coefficient of variation for annual percent increases in hospital expenditure growth for 1966 to 1981 was .036 (Table A-12) whereas it was .058 for GNP growth (Table A-11).
Table A-12. Measures of Central Tendency and Variability for Year-to-Year Percent Changes in National Health Expenditures by Type of Expenditure, Current Dollars, 1966-19811.
| Type of National Health Expenditure | Measures of Variability2 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of The Mean3 | ||
|
| |||||
| Mean | Median | ||||
|
|
|
|
|
|
|
| Total | 12.8% | 12.8% | 1.5% | 0.377% | 0.029 |
| Personal Health Care (Total Systems Cost) |
13.1 | 13.0 | 1.8 | 0.467 | 0.036 |
| Hospital Care | 14.3 | 14.7 | 2.0 | 0.517 | 0.036 |
| Community Hospital Care | 15.8 | 16.6 | 2.8 | 0.716 | 0.045 |
| Inpatient | 15.5 | 16.2 | 2.8 | 0.732 | 0.047 |
| Outpatient | 19.0 | 19.3 | 3.6 | 0.919 | 0.048 |
| Federal Hospital Care | 11.1 | 11.8 | 3.2 | 0.819 | 0.074 |
| Physicians' Services | 12.4 | 11.9 | 2.9 | 0.742 | 0.060 |
| Dentists' Services | 12.1 | 12.5 | 2.8 | 0.725 | 0.060 |
| Other Professional Services | 12.2 | 12.6 | 5.1 | 1.309 | 0.108 |
| Drugs and Medical Sundries | 9.3 | 9.2 | 2.1 | 0.537 | 0.058 |
| Eyeglasses and Appliances | 10.5 | 11.9 | 5.1 | 1.317 | 0.125 |
| Nursing-Home Care | 16.7 | 16.5 | 3.3 | 0.862 | 0.052 |
| Nursing-Home Care Excluding ICF-MR | 15.9 | 15.1 | 3.5 | 0.905 | 0.057 |
| Other Health Services | 12.3 | 12.1 | 6.2 | 1.606 | 0.130 |
| Program Administration and Net Cost of Insurance | 13.8 | 14.6 | 15.3 | 3.949 | 0.286 |
| Government Public Health Activities | 14.8 | 15.5 | 6.4 | 1.648 | 0.111 |
| Research | 8.6 | 7.6 | 4.1 | 1.053 | 0.122 |
| Construction of Medical Facilities | 8.9 | 7.6 | 7.8 | 2.014 | 0.227 |
There are 16 annual percent changes for the period 1966-1981.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of nonsampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
Table A-11. Measures of Central Tendency and Variability for Year-to-Year Percent Changes in Gross National Product, National Health Expenditures, and National Health Expenditures as Percent of GNP, 1966-19811.
| Variable | Measures of Variability2 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of The Mean3 | ||
|
| |||||
| Mean | Median | ||||
|
|
|
|
|
|
|
| Gross National Product, Current Dollars | 9.5% | 9.3% | 2.1% | 0.550% | 0.058 |
| Implicit Price Deflator for GNP | 6.3 | 5.6 | 2.2 | 0.560 | 0.090 |
| Gross National Product, Constant Dollars | 3.1 | 3.1 | 2.4 | 0.632 | 0.205 |
| National Health Expenditures, Current Dollars | 12.8 | 12.8 | 1.5 | 0.377 | 0.029 |
| Implicit Price Deflator for National Health Expenditures | 7.0 | 7.2 | 2.2 | 0.569 | 0.082 |
| Real National Health Expenditures | 5.5 | 4.7 | 1.4 | 0.367 | 0.067 |
| National Health Expenditures as a percent of GNP | 3.1 | 3.0 | 2.5 | 0.640 | 0.208 |
There are 16 annual percent changes for the period 1966-1981.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of non-sampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
The Federal-financing share of total hospital spending, which has been relatively stable since 1976, is not expected to change substantially over the projection horizon.
Increasing deductibles and coinsurance (Lawson, 1982) contribute to the slightly rising proportion paid directly by the patient. The proportion paid out of pocket reached a low point in 1975 and has gradually risen since then.
State and local funding of hospital care is expected to decrease as a percentage of hospital expenditures. Continued cutbacks in long-term mental hospital care and restraining of community hospital cost increases under Medicaid contribute to the decline in the State and local share.
Community Inpatient Care: Historical Perspective
Community hospital inpatient care (almost three-fourths of total hospital spending in 1981) increased from $21 billion in 1971 to $86 billion in 1981, an average annual rate of increase of 15.2 percent. Large increases in community hospital inpatient expenses during the historical period are accounted for by several factors. Overall inflation in the economy, as measured by the GNP deflator, accounted for 51.7 percent of the growth (Figure 5). Increases in hospital input prices (Freeland et al., 1979; Freeland et al., 1981) in excess of the GNP deflator accounted for 11.7 percent. Growth in aggregate population accounted for 7.2 percent of the increase, and growth in admissions per capita accounted for 8.6 percent. Intensity (as measured by growth in real expense per admission) accounted for the remaining 20.8 percent. If we combine only the factors specific to the hospital industry: intensity per admission (which includes such factors as nursing hours per case, and diagnostic and therapeutic procedures per case); admissions per capita; and hospital input prices in excess of the GNP deflator, we find that growth in intensity per admission accounted for half of the increase (Figure 5). The primary force in the rapid growth in intensity is the demand for increased quality of care which is driven by comprehensive insurance coverage (low cost-sharing). This demand factor in turn interacts with our cost-based reimbursement system (piece work payment system) to fuel the growth in intensity of services.
Community Hospital Inpatient Expenditures: Projections
Spending for community hospital inpatient care is expected to rise to approximately $115 billion in 1983, representing a 2-year cumulative increase of 34 percent, a deceleration from the 1979-1981 period increase of 39 percent. Inpatient expenditures are expected to reach $148 billion in 1985 and $261 billion in 1990. The daily semi-private room charge is projected to rise from $165 in 1981 to approximately $213 dollars in 1983, $263 in 1985, and $413 in 1990 (Table 9). Expenses per inpatient stay tripled from $670 in 1971 to $2,155 in 1981 and are projected to rise to $5,955 by 1990 (Table 9).
Table 9. Expenses per Inpatient Stay and Daily Semi-Private Room Charges, Selected Years, 1965 to 1990.
| Year | Inpatient Stay1 2 | Room Charge3 |
|---|---|---|
| Historical Estimates | ||
| 1965 | $ 315 | $ 23 |
| 1970 | 608 | 49 |
| 1975 | 1,017 | 79 |
| 1979 | 1,618 | 127 |
| 1980 | 1,836 | 143 |
| 1981 | 2,155 | 165 |
| Projections | ||
| 1983 | 2,851 | 213 |
| 1985 | 3,570 | 263 |
| 1990 | 5,955 | 413 |
Historical data for community hospitals are from American Hospital Association. “Hospital Indicators”, Hospitals.
Costs are adjusted to eliminate expenses associated with outpatient care.
Health Insurance Association of America. Source Book of Health Insurance Data, 1981-1982. Washington D.C., 1982. Daily semi-private room charges reflect rates near the end of a calendar year. For example, the charge of $165 for 1981 reflects the U.S. daily charge as of January 1982.
An examination of inpatient days and admissions, both measures of inpatient hospital use, follows. Community hospital inpatient days are expected to increase at an average annual rate of 0.9 percent over the period 1981 to 1990. This rate is a little over half the 1.6 percent average annual rate of 1971 to 1981 and results in days growing at about the same rate as aggregate population. The aging of the population puts upward pressure on growth in days while substitution of ambulatory care and a more restrictive monitoring of admissions and length of stay, exerts down-ward pressure. Admissions are projected to rise at an average annual rate of 1.3 percent over the 1981 to 1990 interval. This rate of increase is slightly more than half the 1971 to 1981 average annual increase of 2.3 percent. As the less-sickly patients are channeled into ambulatory settings (such as physicians' offices, hospital outpatient departments) and into nursing homes, it is expected that the hospital case-mix severity may rise slightly compared to the average level of case-mix severity if such channeling had not occurred. Likewise, the average case-mix severity in ambulatory settings and nursing homes may rise since patients who previously were in hospitals will be served there.
We expect the hospital sector to be dynamic during the 1980's (Goldsmith, 1981). There is likely to be increased rivalry among existing hospitals, and there may be new entrants with more convenient locations and sophisticated services and amenities. Suppliers to the hospital industry (such as surgical supplies, pharmaceuticals, registered nurses, unionized employees, etc.) may attempt to strengthen their bargaining positions relative to the hospital industry. Buyers of hospital care, especially the Federal government, State and local governments, and the corporate sector are likely to negotiate more vigorously in the 1980's. Threats of substitute services such as ambulatory surgery and nursing home care are likely to become increasingly important. Even with increasing competition we expect continued rapid growth in the hospital sector in the 1980's due to the aging population, new technologies, and increased ability to pay.
Community Hospital Outpatient: Historical Perspective
Expenditures for community hospital outpatient services grew from $2.3 billion in 1971 to $13.2 billion in 1981, an average annual rate of 19.2 percent. During this period overall inflation accounted for 41.6 percent of the growth; aggregate population—5.6 percent; hospital input prices in excess of overall inflation—9.6 percent; outpatient visits per capita—17.9 percent; and intensity of services per outpatient visit—25.3 percent (Table 4).
Community Hospital Outpatient: Projections
The short-term outlook is for community hospital outpatient expenditures to reach $18 billion in 1983. Expenditures are projected to reach $23 billion in 1985 and $42 billion in 1990. Historical community outpatient expenditure growth has exhibited considerable variability (Table A-12). This variability in combination with the increasing competition in the provision of ambulatory services in the 1980's, makes it difficult to project this sector.
Hospital outpatient services are a substitute and complement for physician office visits and for some hospital inpatient services. The market share of revenues for hospital outpatient services relative to community hospital (inpatient and outpatient) and physician revenues combined, is expected to continue to rise in the eighties.
Community hospital outpatient visits are projected to rise faster than physician office visits in the 1981 to 1990 period, but the differential growth rate between the two sectors is expected to narrow as both groups of providers compete for the same pool of consumers using ambulatory services. The increasing physician-population ratio in the projected period is likely to provide an incentive for physicians to make their services more attractive compared to hospital outpatient services than was the case during the 1970's.
Federal Hospital: Historical Perspective
Expenditures for services in Federal hospitals increased from $3 billion in 1971 to $9.5 billion in 1981, an average annual rate of increase of 12.1 percent. During this period, overall inflation in the economy accounted for 62 percent of the expenditure growth; Federal hospital input price increases in excess of overall inflation accounted for 10 percent of the growth; and increases in real service volume (days and intensity per day combined) accounted for the remaining 28 percent of the expenditure growth.
Federal Hospital: Projections
It is expected that growth in Federal hospital spending will be slowed in the 1981 to 1990 period due to the closing of some Federal hospitals and reduced availability of Federal revenues. One component of the Federal hospital sector, Veteran's hospitals, is likely to experience pressures to expand in the 1980's. The number of veterans age 75 and over is expected to increase at an average annual rate of approximately 8 percent during the 1981 to 1990 period (Langberg and Maloy, 1982; Veterans Administration, 1982). The age 75 and over war veterans will receive services through non-VA contract hospitals as well as in the VA facilities.
In the historical period 1965 to 1981 Federal hospital spending growth showed considerable variability (Table A-12). Given current trends we project that expenditures in Federal hospital facilities will be roughly $20 billion in 1990.
Physicians' Services
Historical Perspective
The non-Federal office-based physicians' services industry is large and complex, with spending totaling $55 billion in 1981. This amount is nearly 2 percent of the GNP and almost two-thirds of the $86 billion dollars spent on community hospital inpatient services.
In 1981 there were 464,000 active physicians (Table A-4), approximately one active physician for each 500 persons in the United States. Ninety-six percent of the active physicians are M.D.'s and the remaining 4 percent are osteopaths (D.O.'s). The major activity of approximately two-thirds of all active physicians is non-Federal office-based practice. The other one-third are involved in hospital-based care, government service, teaching, research, administration, etc.
In 1981 there were approximately 1.4 billion physician visits with approximately 75 percent of the population seeing the physician one or more times (Table A-20). There were 5.8 visits per capita, including physician-billed hospital inpatient visits (Table A-21).
Table A-21. Number of Physician and Dental Visits Per Person Per Year. Selected Years. 1968-1990.
| Calendar Year | Number of Visits Per Person Per Year | |||
|---|---|---|---|---|
|
|
|
|||
| Physician | Dental | |||
|
|
|
|||
| Historical Estimates | Excluding Hospital Inpatient1 | Hospital Inpatient2 | Total | Total |
|
|
|
|
|
|
| 1968 | 4.2 | 1.1 | 5.3 | 1.3 |
| 1969 | 4.3 | 1.1 | 5.4 | 1.5 |
| 1970 | 4.6 | 1.1 | 5.8 | 1.5 |
| 1971 | 4.9 | 1.1 | 6.0 | 1.5 |
| 1972 | 5.0 | 1.1 | 6.1 | 1.5 |
| 1973 | 5.0 | 1.1 | 6.1 | 1.6 |
| 1974 | 4.9 | 1.1 | 6.1 | 1.7 |
| 1975 | 5.1 | 1.1 | 6.2 | 1.6 |
| 1976 | 4.9 | 1.1 | 6.1 | 1.6 |
| 1977 | 4.8 | 1.1 | 6.0 | 1.6 |
| 1978 | 4.8 | 1.1 | 5.9 | 1.6 |
| 1979 | 4.7 | 1.1 | 5.9 | 1.7 |
| 1980 | 4.8 | 1.2 | 5.9 | 1.7 |
| 1981 | 4.6 | 1.2 | 5.8 | 1.7 |
| Projections | ||||
|
|
||||
| 1983 | 4.5 | 1.2 | 5.7 | 1.7 |
| 1985 | 4.6 | 1.2 | 5.8 | 1.8 |
| 1990 | 4.7 | 1.2 | 5.9 | 1.9 |
Historical estimates are from various issues of Current Estimates from the Health Interview Survey. See, for example, Jack (1981).
American Hospital Association panel survey data on inpatient days in community hospitals are used to approximate hospital inpatient physician visits. It is assumed that each inpatient day is associated with one inpatient physician visit. See Wilson and Begun, (1977).
Expenditures for physicians' services increased from $16 billion in 1971 to $55 billion in 1981 (Table A-9), an annual growth rate of 13.2 percent. Of this expenditure growth, increases in: overall inflation (GNP deflator) accounted for 58 percent (Table 4); the CPI for physicians' fees in excess of the GNP deflator accounted for 10 percent; visits accounted for 5 percent and intensity per visit (as measured by real expense per visit) accounted for 27 percent. When controlling for physician service specific factors (physician fees in excess of overall inflation, visits per capita, and intensity per visit), intensity accounted for more than 80 percent of expenditure growth.
Table A-9. National Health Expenditures by Type of Expenditure, Selected Years, 1950-1990.
| Historical Estimates1 | Projections | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||||||||
| 1950 | 1955 | 1960 | 1965 | 1970 | 1971 | 1972 | 1973 | 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1983 | 1985 | 1990 | |
|
|
|||||||||||||||||||
| (amount in billions) | |||||||||||||||||||
| Total | $12.7 | $17.7 | $26.9 | $41.7 | $74.7 | $83.3 | $93.5 | $103.2 | $116.4 | $132.7 | $149.7 | $169.2 | $189.3 | $215.0 | $249.0 | $286.6 | 362.3 | 465.4 | 755.6 |
| Health Services and Supplies | 11.7 | 16.9 | 25.2 | 38.2 | 69.3 | 77.2 | 86.9 | 96.3 | 108.9 | 124.3 | 140.6 | 160.1 | 179.5 | 204.5 | 237.1 | 273.5 | 347.4 | 438.4 | 728.9 |
| Personal Health Care | 10.9 | 15.7 | 23.7 | 35.8 | 65.1 | 72.0 | 80.2 | 88.7 | 101.0 | 116.8 | 131.8 | 148.7 | 166.7 | 188.9 | 219.4 | 255.0 | 323.6 | 408.2 | 684.4 |
| Hospital Care | 3.9 | 5.9 | 9.1 | 13.9 | 27.8 | 30.8 | 34.9 | 38.7 | 44.8 | 52.1 | 59.9 | 67.8 | 75.7 | 86.1 | 100.4 | 118.0 | 154.7 | 196.7 | 340.1 |
| Physicians' Services | 2.7 | 3.7 | 5.7 | 8.5 | 14.3 | 15.9 | 17.2 | 19.1 | 21.2 | 24.9 | 27.6 | 31.9 | 35.8 | 40.2 | 46.8 | 54.8 | 69.8 | 87.9 | 141.9 |
| Dentists' Services | 1.0 | 1.5 | 2.0 | 2.8 | 4.7 | 5.1 | 5.6 | 6.5 | 7.4 | 8.2 | 9.4 | 10.5 | 11.8 | 13.3 | 15.4 | 17.3 | 21.6 | 26.8 | 42.3 |
| Other Professional Services | 0.4 | 0.6 | 0.9 | 1.0 | 1.6 | 1.6 | 1.8 | 2.0 | 2.2 | 2.6 | 3.2 | 3.6 | 4.1 | 4.7 | 5.6 | 6.4 | 7.9 | 10.1 | 17.4 |
| Drugs & Medical Sundries | 1.7 | 2.4 | 3.7 | 5.2 | 8.0 | 8.6 | 9.3 | 10.1 | 11.0 | 11.9 | 13.0 | 14.1 | 15.4 | 17.2 | 19.3 | 21.4 | 24.9 | 30.2 | 47.3 |
| Eyeglasses & Appliances | 0.5 | 0.6 | 0.8 | 1.2 | 1.9 | 2.0 | 2.3 | 2.5 | 2.8 | 3.2 | 3.4 | 3.7 | 4.1 | 4.6 | 5.1 | 5.7 | 6.0 | 7.3 | 11.2 |
| Nursing Home Care | 0.2 | 0.3 | 0.5 | 2.1 | 4.7 | 5.6 | 6.5 | 7.1 | 8.5 | 10.1 | 11.4 | 13.2 | 15.2 | 17.6 | 20.6 | 24.2 | 30.3 | 38.9 | 67.1 |
| Other Health Services | 0.5 | 0.9 | 1.1 | 1.1 | 2.1 | 2.3 | 2.6 | 2.7 | 3.1 | 3.7 | 3.8 | 4.1 | 4.5 | 5.1 | 6.0 | 7.2 | 8.5 | 10.3 | 17.3 |
| Program Admin. & Net Cost of Insurance | 0.5 | 0.6 | 1.1 | 1.6 | 2.7 | 3.4 | 4.7 | 5.4 | 5.2 | 4.4 | 5.0 | 7.1 | 7.5 | 9.3 | 10.7 | 11.2 | 16.0 | 20.8 | 27.8 |
| Government Public Health Activities | 0.4 | 0.4 | 0.4 | 0.8 | 1.4 | 1.8 | 2.0 | 2.2 | 2.7 | 3.2 | 3.8 | 4.3 | 5.3 | 6.2 | 7.0 | 7.3 | 7.8 | 9.4 | 16.7 |
| Research & Construction of Medical Facilities | 1.0 | 0.9 | 1.7 | 3.5 | 5.4 | 6.1 | 6.6 | 6.8 | 7.5 | 8.4 | 9.0 | 9.2 | 9.8 | 10.5 | 11.8 | 13.1 | 14.9 | 18.0 | 26.7 |
| Research | 0.1 | 0.2 | 0.7 | 1.5 | 2.0 | 2.1 | 2.4 | 2.5 | 2.8 | 3.3 | 3.7 | 3.9 | 4.4 | 4.8 | 5.3 | 5.7 | 5.8 | 6.5 | 9.7 |
| Construction | 0.8 | 0.7 | 1.0 | 2.0 | 3.4 | 4.0 | 4.2 | 4.3 | 4.7 | 5.1 | 5.3 | 5.3 | 5.3 | 5.7 | 6.5 | 7.5 | 9.1 | 11.5 | 17.0 |
Historical estimates are reported in Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981,” Health Care Financing Review, September 1982, pp. 1-36.
The rapid growth in intensity is indicated by various measures. Real services per visit (intensity) includes such factors as shifts in mix of services, out-of-hospital laboratory tests, surgical procedures, minutes of direct patient care, and staffing per visit. The volume of out-of-hospital laboratory tests increased at an average annual rate of 9.9 percent between'1975 and 1978 (Laboratory Management, 1979). The number of surgical operations as indicated in the American Hospital Association National Panel Survey, increased from 14.7 million to 19.7 million from 1971 to 1981, an average annual rate of growth of 3 percent. This growth rate is triple that of aggregate population growth and is 5 times faster than the 0.6 average annual growth rate for total physician visits. The average number of minutes of direct physician patient care per visit rose from 20.2 in 1970 to 23.8 in 1980, an increase of 17.8 percent (Table A-22). For the period 1972 to 1981 total employment (supervisory and nonsupervisory) in offices of physicians and surgeons increased 75 percent (Bureau of Labor Statistics, Employment and Earnings). During this same period the number of non-Federal office-based physicians increased 42 percent9. Nonphysician staff (secretaries, nurses, etc.) increased faster than the number of physicians and both categories of employment grew faster than visits. Thus, the staffing associated with each visit has increased. Increases in intensity of services per visit are caused in part by demand for increased quality of care, which, like hospital intensity, is driven by insurance coverage (low cost-sharing) and the fee-for-service reimbursement system (Delbanco et al., 1979; Showstack et al., 1979; Sloan and Steinwald, 1975).
Table A-22. Average Number of Minutes of Direct Physician Patient Care Per Visit, 1970 and 1980.
| Calendar Years | |||
|---|---|---|---|
|
|
|||
| 1970 | 1980 | 1980 as a Percent of 1970 | |
|
|
|||
| Average Number of Hours of Direct Patient Care Per Week Per Physician | 44.7 | 44.5 | −0.5% |
| Average Number of Total Patient Visits Per Week Per Physician | 132.5 | 112.0 | −15.5% |
| Average Number of Minutes of Direct Patient Care Per Visit | 20.2 | 23.8 | 17.8% |
American Medical Association, Profile of Medical Practice, AMA center for Health Services Research and Development, 1981.
Per capita expenditures for physicians' services are nearly three times greater for the age 65 and over population than for the nonaged population. Both the number of physician visits per capita and intensity of services per visit are relatively higher for the aged (Fisher, 1980). The continued aging of the population will contribute to growth in expenditures for physicians' services.
Between 1971 and 1981 the number of active physicians increased at an average annual rate of 3.3 percent while the population increased at a 1.0 percent rate. In the projected period, the annual rate of growth of physicians is slightly less, 2.7 percent (Table A-4). The effect of projected increases in active M.D.'s and D.O.'s (Bloom 1980) per capita on fees; visits per capita; intensity per visit; distribution by speciality, income and geographic area, etc. is under current analysis (Graduate Medical Education Naaional Advisory Committee, 1980; Hendrickson, 1980; Scheffler et al., 1979; Schwartz et al., 1980).
During the 1971-1981 period, real per capita expenditures for physicians' services rose at an average annual rate of 3.0 percent; and real services per physician declined −0.2 percent per year on the average (Table 10). These data indicate that the large increase in the number of active physicians relative to population have been associated with more real services provided per capita, but with a relatively constant volume of real services per physician.
Table 10. Average Income Per Physician and Per Capita Expenditures for Physicians' Services, Nominal and Real, 1971 and 1981.
| Selected Variables | Year | Average Annual Percent Change | |
|---|---|---|---|
|
| |||
| 1971 | 1981 | ||
| Per Capita Expenditures for Physicians' Services1 | $ 75 | $ 234 | 12.0% |
| Per Capita Expenditures for Physicians' Services Deflated by the CPI for Physicians' Services | $ 58 | $ 78 | 3.0 |
| Average Gross Income per Physician2 | $74,197 | $167, 000 | 8.5 |
| Average Gross Income per Physician Deflated by the CPI for Physicians' Services | $57,163 | $ 55,853 | −0.2 |
| Average Total Tax Deductible Professional Expense per Physician2 | $28,919 | $ 74,000 | 9.9 |
| Average Total Tax Deductible Professional Expense per Physician Deflated by the Fixed-Weight Price Index for Personal Consumption Expenditures3 | $29,937 | $ 36,616 | 2.0 |
| Average Net Income from Medical Practice per Physician | $45,278 | $ 93,000 | 7.5 |
| Average Net Income from Medical Practice per Physician Deflated by the Fixed Weight Price Index for Personal Consumption Expenditures3 | $46,872 | $ 46,017 | −0.2 |
| CPI for Physicians' Services (1967 = 100.0) | 129.8 | 299.0 | 8.7 |
| Fixed Weight Price Index for Personal Consumption Expenditures (1972= 100.0)3 | 96.6 | 202.1 | 7.7 |
| CPI for Physicians' Services Deflated by Fixed-Weight Price Index for Personal Consumption Expenditures3 | 134.4 | 147.9 | 1.0 |
Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981”, Health Care Financing Review, September, 1982.
American Medical Association, Profile of Medical Practice, 1981 and American Medical Association, SMS Report, AMA Center for Health Policy Research, 1982.
The fixed-weight price index for personal consumption expenditures is reported in Bureau of Economic Analysis, Survey of Current Business, U.S. Department of Commerce.
It is noteworthy that while average net income from medical practice rose at an average annual rate of 7.5 percent in nominal terms (Table 10), real income—after adjusting for inflation—declined at an average annual rate of −0.2 percent. Average total tax deductible professional expenses per physician increased at an average annual rate of 9.9 percent, faster than the 7.7 percent average annual inflation rate measured by the fixed-weight personal consumption price index. A portion of the relatively fast growth in expenses and slow growth in net income may reflect that physicians are putting increasing amounts of their income into deferred compensation pension programs. Thus, what formerly was included as net income is included as professional expenses (American Medical Association, 1980).
The increasing incidence of malpractice suits in the 1970's has affected expenditures in two ways (Greenspan, 1979; Henderson, 1979; Rottenberg, 1978): 1) fees were raised to reflect increased costs from higher malpractice insurance premiums, and 2) the quantity of services provided increased as physicians became more thorough in response to the threat of malpractice suits. In the projected period, this threat will continue to be a factor in physicians' practice costs but may not be as significant a cost determinant as it was in the 1970's.
Projections
The short-term outlook is for expenditures for physicians' services to rise from $55 billion in 1981 to $70 billion in 1983. Physician fees as measured by the CPI are projected to substantially decelerate during this period compared to the 10.8 percent average annual increase over the 1979 to 1981 interval. We expect that by 1985 expenditures will reach $88 billion and by 1990, $142 billion. The average annual rate of increase over the period 1981 to 1990 is 11.2 percent. As the projection horizon lengthens, the uncertainty associated with the expenditure growth widens (Figure 10).
Figure 10. Expenditures for Physicians' Services 1965 to 1990, with Bandwidth Intervals1.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in expenditures for physicians' services for 1966-1981 (see Table A-12) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
While scarcity of public funds will damp the growth of expenditures, projected increase in real income for the 1983-1990 period is expected to bolster demand for services. A continued upward trend in intensity of services per visit, partially reflecting growth in technologies, is projected. The number of patient contacts per physician, per week, is projected to continue declining, with the physician spending more time per contact. Competition between office-based physicians and hospital outpatient departments for increasing market shares of patients will intensify in the projection period.
To the extent that office-based physicians get a larger share of the patient segment that previously received care in hospital outpatient and hospital inpatient settings, their average case-mix complexity may rise and contribute to the growth in intensity of services. This will put upward pressure on the demand for surgical and medical instruments, appliances, and supplies (Bandy, 1982; Interindustry Economics Division, 1979; and Cassack, 1982).
Due in part to the aging of the population, the Federal share of outlays for physicians' services is projected to increase. The proportion paid out of pocket is expected to rise in the early eighties (Table A-10) partly due to the increase in deductibles and coinsurance rates on private health insurance plans (Lawson, 1982).
Table A-10. National Health Expenditures by Type of Expenditure and Source of Funds, Selected Years 1965-1990 (Amounts in Billions of Dollars).
| Total | Private | Public | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Total | Consumer | Other1 | |||||||
|
|
|
||||||||
| Total | Patient Direct | Health Insurance | Total | Federal | State & Local | ||||
| 1965 | |||||||||
|
|
|||||||||
| Total | $41.7 | $31.0 | $28.5 | $18.5 | $10.0 | $2.4 | $10.8 | $5.5 | $5.3 |
| Health Services and Supplies | 38.2 | 29.5 | 28.5 | 18.5 | 10.0 | 1.0 | 8.8 | 4.0 | 4.8 |
| Personal Health Care | 35.8 | 28.0 | 27.3 | 18.5 | 8.7 | .8 | 7.7 | 3.6 | 4.1 |
| Hospital Care | 13.9 | 8.5 | 8.2 | 2.4 | 5.8 | .3 | 5.4 | 2.4 | 3.0 |
| Physicians' Services | 8.5 | 7.9 | 7.9 | 5.2 | 2.7 | .0 | .6 | .2 | .4 |
| Dentists' Services | 2.8 | 2.8 | 2.8 | 2.7 | .0 | — | .0 | .0 | .0 |
| Other Professional Services | 1.0 | 1.0 | 1.0 | .9 | .1 | .0 | .0 | .0 | .0 |
| Drugs and Medical Sundries | 5.2 | 5.0 | 5.0 | 4.8 | .1 | — | .2 | .1 | .1 |
| Eyeglasses and Appliances | 1.2 | 1.1 | 1.1 | 1.1 | .0 | — | .0 | .0 | .0 |
| Nursing-home care | 2.1 | 1.4 | 1.3 | 1.3 | .0 | .0 | .7 | .5 | .3 |
| Other Personal Health Care | 1.1 | .4 | — | — | — | .4 | .7 | .4 | .3 |
| Program Administration and Net Cost of Health Insurance | 1.7 | 1.4 | 1.3 | — | 1.3 | .2 | .2 | .0 | .2 |
| Government Public Health Activity | .8 | — | — | — | — | — | .8 | .3 | .5 |
| Research and Construction of Medical Facilities | 3.5 | 1.5 | — | — | — | 1.5 | 2.0 | 1.6 | .5 |
| Research2 | 1.5 | .2 | — | — | — | .2 | 1.3 | 1.2 | .1 |
| Construction | 2.0 | 1.3 | — | — | — | 1.3 | .7 | .3 | .4 |
|
|
|||||||||
| 1970 | |||||||||
|
|
|||||||||
| Total | $74.7 | $46.9 | $43.1 | $26.0 | $17.1 | $3.8 | $27.8 | $17.7 | $10.1 |
| Health Services and Supplies | 69.3 | 44.3 | 43.1 | 26.0 | 17.1 | 1.2 | 25.0 | 15.7 | 9.2 |
| Personal Health Care | 65.1 | 42.7 | 41.6 | 26.0 | 15.6 | 1.0 | 22.5 | 14.5 | 7.9 |
| Hospital Care | 27.8 | 13.1 | 12.7 | 2.8 | 9.9 | .4 | 14.7 | 9.5 | 5.2 |
| Physicians' Services | 14.3 | 11.3 | 11.3 | 6.5 | 4.9 | .0 | 3.0 | 2.1 | .9 |
| Dentists' Services | 4.7 | 4.5 | 4.5 | 4.3 | .2 | — | .2 | .1 | .1 |
| Other Professional Services | 1.6 | 1.4 | 1.4 | 1.1 | .3 | .0 | .2 | .1 | .1 |
| Drugs and Medical Sundries | 8.0 | 7.5 | 7.5 | 7.2 | .3 | — | .5 | .2 | .2 |
| Eyeglasses and Appliances | 1.9 | 1.8 | 1.8 | 1.8 | .0 | — | .1 | .1 | .0 |
| Nursing-home care | 4.7 | 2.4 | 2.4 | 2.4 | .0 | .0 | 2.3 | 1.3 | .9 |
| Other Personal Health Care | 2.1 | .6 | — | — | — | .6 | 1.5 | .9 | .5 |
| Program Administration and Net Cost of Health Insurance | 2.7 | 1.6 | 1.5 | — | 1.5 | .2 | 1.1 | .6 | .5 |
| Government Public Health Activity | 1.4 | — | — | — | — | — | 1.4 | .6 | .8 |
| Research and Construction of Medical Facilities | 5.4 | 2.6 | — | — | — | 2.6 | 2.8 | 2.0 | .9 |
| Research2 | 2.0 | .2 | — | — | — | .2 | 1.8 | 1.6 | .2 |
| Construction of Medical Facilities | 3.4 | 2.3 | — | — | — | 2.3 | 1.1 | .4 | .7 |
|
|
|||||||||
| 1971 | |||||||||
|
|
|||||||||
| Total | $83.3 | $51.6 | $47.3 | $27.8 | $19.5 | $4.3 | $31.7 | $20.3 | $11.3 |
| Health Services and Supplies | 77.2 | 48.7 | 47.3 | 27.8 | 19.5 | 1.5 | 28.4 | 18.2 | 10.2 |
| Personal Health Care | 72.0 | 46.4 | 45.1 | 27.8 | 17.3 | 1.2 | 25.6 | 16.8 | 8.8 |
| Hospital Care | 30.8 | 14.4 | 13.9 | 2.8 | 11.1 | .5 | 16.5 | 10.9 | 5.6 |
| Physicians' Services | 15.9 | 12.5 | 12.4 | 7.1 | 5.3 | .0 | 3.5 | 2.5 | 1.0 |
| Dentists' Services | 5.1 | 4.8 | 4.8 | 4.5 | .3 | — | .3 | .2 | .1 |
| Other Professional Services | 1.6 | 1.4 | 1.4 | 1.1 | .3 | .0 | .2 | .1 | .1 |
| Drugs and Medical Sundries | 8.6 | 8.0 | 8.0 | 7.6 | .4 | — | .6 | .3 | .3 |
| Eyeglasses and Appliances | 2.0 | 1.9 | 1.9 | 1.9 | .0 | — | .1 | .1 | .0 |
| Nursing-home care | 5.6 | 2.8 | 2.8 | 2.8 | .0 | .0 | 2.8 | 1.7 | 1.1 |
| Other Personal Health Care | 2.3 | .7 | — | — | — | .7 | 1.6 | 1.1 | .6 |
| Program Administration and Net Cost of Health Insurance | 3.4 | 2.4 | 2.2 | — | 2.2 | .2 | 1.1 | .6 | .5 |
| Government Public Health Activity | 1.8 | — | — | — | — | — | 1.8 | .8 | .9 |
| Research and Construction of Medical Facilities | 6.1 | 2.9 | — | — | — | 2.9 | 3.2 | 2.1 | 1.1 |
| Research2 | 2.1 | .2 | — | — | — | .2 | 1.9 | 1.7 | .2 |
| Construction of Medical Facilities | 4.0 | 2.7 | — | — | — | 2.7 | 1.4 | .4 | .9 |
|
|
|||||||||
| 1975 | |||||||||
|
|
|||||||||
| Total | $132.9 | $76.7 | $71.5 | $39.1 | $32.4 | $5.1 | $56.2 | $37.1 | $19.1 |
| Health Services and Supplies | 124.5 | 73.3 | 71.5 | 39.1 | 32.4 | 1.8 | 51.1 | 33.8 | 17.3 |
| Personal Health Care | 116.9 | 70.8 | 69.2 | 39.1 | 30.1 | 1.6 | 46.1 | 31.4 | 14.7 |
| Hospital Care | 52.1 | 23.3 | 22.7 | 4.3 | 18.4 | .6 | 28.8 | 20.3 | 8.6 |
| Physicians' Services | 24.9 | 18.4 | 18.4 | 9.0 | 9.4 | .0 | 6.5 | 4.6 | 1.9 |
| Dentists' Services | 8.2 | 7.8 | 7.8 | 6.8 | 1.0 | — | .5 | .3 | .2 |
| Other Professional Services | 2.6 | 2.0 | 2.0 | 1.7 | .4 | .0 | .6 | .4 | .2 |
| Drugs and Medical Sundries | 11.9 | 10.9 | 10.9 | 10.2 | .7 | — | 1.0 | .5 | .5 |
| Eyeglasses and Appliances | 3.2 | 2.9 | 2.9 | 2.8 | .1 | — | .2 | .2 | .1 |
| Nursing-home care | 10.2 | 4.5 | 4.5 | 4.4 | .1 | .1 | 5.7 | 3.2 | 2.5 |
| Other Personal Health Care | 3.7 | .9 | — | — | — | .9 | 2.8 | 2.0 | .8 |
| Program Administration and Net Cost of Health Insurance | 4.4 | 2.6 | 2.4 | — | 2.4 | .2 | 1.8 | 1.2 | .7 |
| Government Public Health Activity | 3.2 | — | — | — | — | — | 3.2 | 1:2 | 1.9 |
| Research and Construction of Medical Facilities | 8.4 | 3.3 | — | — | — | 3.3 | 5.1 | 3.3 | 1.8 |
| Research2 | 3.3 | .3 | — | — | — | .3 | 3.1 | 2.8 | .3 |
| Construction of Medical Facilities | 5.1 | 3.1 | — | — | — | 3.1 | 2.0 | .5 | 1.5 |
|
|
|||||||||
| 1979 | |||||||||
|
|
|||||||||
| Total | $215.0 | $124.4 | $117.7 | $61.8 | $55.9 | $6.7 | $90.6 | $61.0 | $29.5 |
| Health Services and Supplies | 204.5 | 120.6 | 117.7 | 61.8 | 55.9 | 3.0 | 83.8 | 56.4 | 27.4 |
| Personal Health Care | 188.9 | 114.6 | 112.0 | 61.8 | 50.2 | 2.6 | 74.3 | 53.3 | 21.0 |
| Hospital Care | 86.1 | 39.8 | 38.7 | 8.5 | 30.1 | 1.2 | 46.3 | 34.8 | 11.5 |
| Physicians' Services | 40.2 | 29.5 | 29.5 | 15.0 | 14.6 | .0 | 10.7 | 8.1 | 2.6 |
| Dentists' Services | 13.3 | 12.8 | 12.8 | 9.9 | 2.9 | — | .5 | .3 | .2 |
| Other Professional Services | 4.7 | 3.5 | 3.5 | 2.8 | .7 | .1 | 1.2 | .9 | .3 |
| Drugs and Medical Sundries | 17.2 | 15.8 | 15.8 | 14.2 | 1.6 | — | 1.4 | .7 | .7 |
| Eyeglasses and Appliances | 4.6 | 4.2 | 4.2 | 4.0 | .2 | — | .4 | .4 | .1 |
| Nursing-home care | 17.6 | 7.7 | 7.6 | 7.4 | .1 | .1 | 9.9 | 5.5 | 4.4 |
| Other Personal Health Care | 5.1 | 1.3 | — | — | — | 1.3 | 3.8 | 2.7 | 1.2 |
| Program Administration and Net Cost of Health Insurance | 9.3 | 6.0 | 5.7 | — | 5.7 | .3 | 3.3 | 1.9 | 1.4 |
| Government Public Health Activity | 6.2 | — | — | — | — | — | 6.2 | 1.2 | 5.0 |
| Research and Construction of Medical Facilities | 10.5 | 3.8 | — | — | — | 3.8 | 6.7 | 4.6 | 2.2 |
| Research2 | 4.8 | .3 | — | — | — | .3 | 4.5 | 4.0 | .4 |
| Construction of Medical Facilities | 5.7 | 3.5 | — | — | — | 3.5 | 2.3 | .5 | 1.7 |
|
|
|||||||||
| 1980 | |||||||||
|
|
|||||||||
| Total | $249.0 | $143.6 | $135.7 | $72.1 | $63.6 | $7.8 | $105.4 | $71.1 | $34.3 |
| Health Services and Supplies | 237.1 | 139.3 | 135.7 | 72.1 | 63.6 | 3.6 | 97.9 | 66.0 | 31.9 |
| Personal Health Care | 219.4 | 132.2 | 129.1 | 72.1 | 57.0 | 3.1 | 87.2 | 62.7 | 24.5 |
| Hospital Care | 100.4 | 46.1 | 44.6 | 10.9 | 33.7 | 1.5 | 54.3 | 41.1 | 13.2 |
| Physicians' Services | 46.8 | 34.3 | 34.3 | 17.8 | 16.5 | .0 | 12.5 | 9.5 | 3.0 |
| Dentists' Services | 15.4 | 14.8 | 14.8 | 11.2 | 3.6 | — | .6 | .3 | .3 |
| Other Professional Services | 5.6 | 4.2 | 4.2 | 3.3 | .9 | .1 | 1.4 | 1.0 | .4 |
| Drugs and Medical Sundries | 19.3 | 17.7 | 17.7 | 15.7 | 2.0 | — | 1.6 | .8 | .8 |
| Eyeglasses and Appliances | 5.1 | 4.6 | 4.6 | 4.3 | .3 | — | .5 | .5 | .1 |
| Nursing-home care | 20.6 | 9.1 | 9.0 | 8.8 | .2 | .1 | 11.5 | 6.2 | 5.3 |
| Other Personal Health Care | 6.0 | 1.4 | — | — | — | 1.4 | 4.6 | 3.2 | 1.4 |
| Program Administration and Net Cost of Health Insurance | 10.7 | 7.1 | 6.6 | — | 6.6 | .4 | 3.7 | 2.0 | 1.7 |
| Government Public Health Activity | 7.0 | — | — | — | — | — | 7.0 | 1.3 | 5.7 |
| Research and Construction of Medical Facilities | 11.8 | 4.3 | — | — | — | 4.3 | 7.5 | 5.1 | 2.4 |
| Research2 | 5.3 | .3 | — | — | — | .3 | 5.0 | 4.5 | .5 |
| Construction of Medical Facilities | 6.5 | 4.0 | — | — | — | 4.0 | 2.5 | .6 | 2.0 |
|
|
|||||||||
| 1981 | |||||||||
|
|
|||||||||
| Total | $286.6 | $164.1 | $154.9 | $81.7 | $73.2 | $9.2 | $122.5 | $83.9 | $38.6 |
| Health Services and Supplies | 273.5 | 159.0 | 154.9 | 81.7 | 73.2 | 4.0 | 114.5 | 78.4 | 36.1 |
| Personal Health Care | 255.0 | 152.1 | 148.5 | 81.7 | 66.8 | 3.5 | 102.9 | 74.6 | 28.3 |
| Hospital Care | 118.0 | 53.9 | 52.1 | 12.8 | 39.4 | 1.7 | 64.1 | 48.7 | 15.4 |
| Physicians' Services | 54.8 | 39.8 | 39.8 | 20.8 | 19.0 | .0 | 15.0 | 11.6 | 3.3 |
| Dentists' Services | 17.3 | 16.6 | 16.6 | 12.3 | 4.3 | — | .7 | .4 | .3 |
| Other Professional Services | 6.4 | 5.0 | 4.9 | 3.8 | 1.1 | .1 | 1.4 | 1.1 | .3 |
| Drugs and Medical Sundries | 21.4 | 19.5 | 19.5 | 17.1 | 2.4 | — | 1.9 | 1.0 | .9 |
| Eyeglasses and Appliances | 5.7 | 5.1 | 5.1 | 4.7 | .3 | — | .7 | .6 | .1 |
| Nursing-home care | 24.2 | 10.6 | 10.5 | 10.3 | .2 | .1 | 13.6 | 7.5 | 6.1 |
| Other Personal Health Care | 7.2 | 1.6 | — | — | — | 1.6 | 5.6 | 3.8 | 1.8 |
| Administration, and Net Cost of Health Insurance | 11.2 | 6.9 | 6.4 | — | 6.4 | .5 | 4.3 | 2.5 | 1.8 |
| Government Public Health Activity | 7.3 | — | — | — | — | — | 7.3 | 1.3 | 6.0 |
| Research and Construction | 13.1 | 5.1 | — | — | — | 5.1 | 8.0 | 5.5 | 2.6 |
| Noncommercial Research2 | 5.7 | .3 | — | — | — | .3 | 5.3 | 4.8 | .5 |
| Construction of Medical Facilities | 7.5 | 4.8 | — | — | — | 4.8 | 2.7 | .7 | 2.1 |
|
|
|||||||||
| 1983 | |||||||||
|
|
|||||||||
| Total | $362.3 | $211.2 | $199.0 | $103.8 | $95.2 | $12.1 | $151.1 | $104.2 | $46.9 |
| Health Services and Supplies | 347.4 | 204.2 | 199.0 | 103.8 | 95.2 | 5.2 | 143.2 | 98,7 | 44.5 |
| Personal Health Care | 323.6 | 193.6 | 189.1 | 103.8 | 85.3 | 4.5 | 130.0 | 94.6 | 35.5 |
| Hospital Care | 154.7 | 72.9 | 70.6 | 19.3 | 51.3 | 2.3 | 81.8 | 62.0 | 19.8 |
| Physicians' Services | 69.8 | 50.3 | 50.3 | 27.1 | 23.1 | 0.0 | 19.5 | 15.4 | 4.1 |
| Dentists' Services | 21.6 | 20.8 | 20.8 | 15.2 | 5.6 | 0.0 | 0.8 | 0.5 | 0.4 |
| Other Professional Services | 7.9 | 6.0 | 6.0 | 4.5 | 1.5 | 0.1 | 1.9 | 1.5 | 0.4 |
| Drugs and Medical Sundries | 24.9 | 22.7 | 22.7 | 19.6 | 3.0 | 0.0 | 2.2 | 1.1 | 1.1 |
| Eyeglasses and Appliances | 6.0 | 5.1 | 5.1 | 4.7 | 0.4 | 0.0 | 0.9 | 0.8 | 0.1 |
| Nursing-home care | 30.3 | 13.9 | 13.7 | 13.4 | 0.3 | 0.2 | 16.4 | 8.9 | 7.5 |
| Other Personal Health Care | 8.5 | 2.0 | — | — | — | 2.0 | 6.5 | 4.4 | 2.1 |
| Program Administration and Net Cost of Health Insurance | 16.0 | 10.6 | 10.0 | — | 10.0 | 0.6 | 5.4 | 2.9 | 2.4 |
| Government Public Health Activity | 7.8 | — | — | — | — | — | 7.8 | 1.2 | 6.6 |
| Research and Construction of Medical Facilities | 14.9 | 7.0 | — | — | — | 7.0 | 7.9 | 5.5 | 2.4 |
| Research2 | 5.8 | 0.4 | — | — | — | 0.4 | 5.4 | 4.9 | 0.5 |
| Construction of Medical Facilities | 9.1 | 6.6 | — | — | — | 6.6 | 2.5 | 0.6 | 1.9 |
|
|
|||||||||
| 1985 | |||||||||
|
|
|||||||||
| Total | $456.4 | $268.2 | $252.8 | $131.5 | $121.3 | $15.4 | $188.1 | $131.5 | $56.6 |
| Health Services and Supplies | 438.4 | 259.2 | 252.8 | 131.5 | 121.3 | 6.4 | 179.2 | 125.3 | 53.8 |
| Personal Health Care | 408.2 | 244.9 | 239.3 | 131.5 | 107.8 | 5.6 | 163.3 | 120.5 | 42.7 |
| Hospital Care | 196.7 | 94.2 | 91.3 | 26.1 | 65.3 | 2.9 | 102.4 | 78.7 | 23.8 |
| Physicians' Services | 87.9 | 62.4 | 62.4 | 34.0 | 28.3 | 0.1 | 25.4 | 20.4 | 5.0 |
| Dentists' Services | 26.8 | 25.8 | 25.8 | 18.6 | 7.2 | 0.0 | 1.0 | 0.6 | 0.4 |
| Other Professional Services | 10.1 | 7.7 | 7.6 | 5.7 | 1.9 | 0.1 | 2.4 | 1.9 | 0.5 |
| Drugs and Medical Sundries | 30.2 | 27.6 | 27.6 | 23.5 | 4.0 | — | 2.6 | 1.3 | 1.3 |
| Eyeglasses and Appliances | 7.3 | 6.2 | 6.2 | 5.6 | 0.6 | — | 1.1 | 1.0 | 0.1 |
| Nursing-home care | 38.9 | 18.6 | 18.4 | 18.0 | 0.4 | 0.2 | 20.3 | 11.1 | 9.1 |
| Other Personal Health Care | 10.3 | 2.3 | — | — | — | 2.3 | 8.0 | 5.5 | 2.5 |
| Program Administration and Net Cost of Health Insurance | 20.8 | 14.3 | 13.5 | — | 13.5 | 0.7 | 6.5 | 3.5 | 3.0 |
| Government Public Health Activity | 9.4 | — | — | — | — | — | 9.4 | 1.3 | 8.1 |
| Research and Construction of Medical Facilities | 18.0 | 9.0 | — | — | — | 9.0 | 8.9 | 6.1 | 2.8 |
| Research2 | 6.5 | 0.4 | — | — | — | 0.4 | 6.1 | 5.5 | 0.6 |
| Construction of Medical Facilities | 11.5 | 8.7 | — | — | — | 8.7 | 2.9 | 0.6 | 2.2 |
|
|
|||||||||
| 1990 | |||||||||
|
|
|||||||||
| Total | $755.6 | $430.9 | $407.2 | $211.6 | $195.6 | $23.7 | $324.7 | $231.6 | $93.1 |
| Health Services and Supplies | 728.9 | 417.5 | 407.2 | 211.6 | 195.6 | 10.3 | 311.5 | 222.5 | 89.0 |
| Personal Health Care | 684.4 | 399.4 | 390.2 | 211.6 | 178.6 | 9.2 | 285.1 | 215.8 | 69.3 |
| Hospital Care | 340.1 | 159.0 | 154.0 | 43.5 | 110.5 | 5.0 | 181.1 | 142.6 | 38.5 |
| Physicians' Services | 141.9 | 95.8 | 95.8 | 52.3 | 43.5 | 0.1 | 46.0 | 38.0 | 8.0 |
| Dentists' Services | 42.3 | 40.9 | 40.9 | 28.6 | 12.3 | — | 1.4 | 0.8 | 0.6 |
| Other Professional Services | 17.4 | 13.5 | 13.3 | 9.9 | 3.4 | 0.2 | 3.9 | 3.1 | 0.8 |
| Drugs and Medical Sundries | 47.3 | 43.4 | 43.4 | 36.2 | 7.2 | — | 4.0 | 2.0 | 2.0 |
| Eyeglasses and Appliances | 11.2 | 9.4 | 9.4 | 8.5 | 0.9 | — | 1.8 | 1.6 | 0.2 |
| Nursing-home care | 67.1 | 33.9 | 33.5 | 32.7 | 0.8 | 0.4 | 33.2 | 18.2 | 15.0 |
| Other Personal Health Care | 17.3 | 3.5 | — | — | — | 3.5 | 13.8 | 9.6 | 4.2 |
| Program Administration and Net Cost of Health Insurance | 27.8 | 18.1 | 17.0 | — | 17.0 | 1.1 | 9.7 | 5.0 | 4.7 |
| Government Public Health Activity | 16.7 | — | — | — | — | — | 16.7 | 1.7 | 15.0 |
| Research and Construction of Medical Facilities | 26.7 | 13.4 | — | — | — | 13.4 | 13.3 | 9.2 | 4.1 |
| Research2 | 9.7 | 0.5 | — | — | — | 0.5 | 9.2 | 8.3 | 0.9 |
| Construction of Medical Facilities | 17.0 | 12.9 | — | — | — | 12.9 | 4.1 | 0.9 | 3.2 |
Spending by philanthropic organizations, industrial in-plant health services and privately financed construction.
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but are included in the expenditure class in which the product falls.
Dentists' Services
Historical Perspective
About $17 billion was spent for dental services in 1981. About half the population had one or more dental visits (Table A-20) and the per capita visit rate was 1.7 (Table A-21). By contrast in 1971, 47 percent of the population had one or more dental visits and the per capita visit rate was 1.5. About 129,000 active dentists (approximately one dentist per 1800 persons) provided 395 million visits in 1981. Nine-tenths of active dentists are in nongovernment office-based practice.
Expenditures for dentists' services increased an average of 13.1 percent annually in the 1971-1981 period (Table 8), more than tripling from $5 billion in 1971 to $17 billion in 1981. During this period, the number of active dentists increased at a faster annual rate, (2.3 percent) than total population (1.0 percent).
From 1971 to 1981, overall inflation accounted for nearly 59 percent of the growth in expenditures for dentists' services (Figure 11). Growth of dentists fees in excess of overall inflation accounted for only 1 percent of the expenditure growth. The CPI for dentist fees increased at a 7.6 percent annual rate for this same period. The better price performance of the dental-services sector relative to the physicians'-services sector may in part reflect more consumer cost sharing; competitive forces within the industry; better productivity performance; and the relative reduction in demand for dental services associated with more extensive use of fluoridation (Douglas and Cole, 1979; Feldstein, P., 1974; Medicus Systems, 1980; Millenson, 1980).
Figure 11. Factors Accounting for Growth in Expenditures for Dentists' Services 1971 to 1981.
Intensity (as measured by real expense per visit) accounted for 18 percent of expenditure growth in the last decade. When focusing on factors specific to the dental-service sector, intensity contributed 53 percent (Figure 11). Intensity includes providing more services and procedures per visit (for example, high speed drill usage increases the average number of cavities filled during one visit) as well as shifts in the mix of services and procedures (for example, a greater proportion of expensive procedures such as orthodontics). For the period 1972 to 1981, total employment (supervisory and nonsupervisory) in offices of dentists increased 91 percent (Bureau of Labor Statistics, Employment and Earnings). During this same period the number of dentists increased 23 percent (Division of Health Professions Analysis, 1982).10 Nondentist staff (clerical, dental auxiliaries, etc.) is increasing faster than the number of dentists, while the number of dentists is growing at about the same rate as dental visits. Thus, the staffing associated with each visit has increased, contributing to the growth in intensity of services per visit.
There is little relationship between changes in the age-sex mix of the population and changes in number of dental visits per capita (Russell, 1981). The aged spend slightly less for dental services (Fisher, 1980) per capita than the nonaged.
Projections
In the short-term, 1981 to 1983, projected expenditures for dentists' services are expected to rise from $17 billion in 1981 to $22 billion in 1983 (Table 7), an average annual rate of growth of 11.8 percent. Increases in the CPI for dentists' fees of 11.8 percent in 1980 and 9.6 percent in 1981 significantly contributed to growth in expenditures in the 1979 to 1981 period. By mid-1982, dentists' pricing patterns appear to reflect the effects of decelerating inflation. In August 1982, dental fees were 6.1 percent higher than for the same month a year earlier.
Aggregate demand for dental services appears strong in mid-1982 in spite of the recession. The number of nonsupervisory employees (a rough indicator of demand) in offices of dentists was 7.3 percent higher in August 1982 compared to the same month a year ago (Bureau of Labor Statistics, Employment and Earnings). The fast growth in dental insurance (Employee Benefit Plan Review, 1981) may be the factor fueling the demand for dental services during the current recessionary, period. In some cases switches from mental health coverage, which provides significant benefits to a relatively small proportion of the covered population, to dental insurance coverage, which provides some benefits to a large proportion of the insured population, may have contributed to the fast growth in dental insurance coverage. While aggregate national demand seems fairly strong, particular geographic areas and some individual practitioners in other areas, appear to be experiencing the negative impact of the recession. As consumer disposable income declines and loss of employment-related dental insurance occurs, utilization of dental services declines.
Expenditures for dentists' services are expected to reach $27 billion by 1985 and $42 billion by 1990 (Table 7). The annual rate of growth from 1981 to 1990 is expected to be 10.4 percent. This is substantially below the 13.1 percent annual rate for the 1971 to 1981 period, a period of very rapid growth in dental insurance.
Private health insurance is expected to finance an increasing share of benefits for dentists' services in the next decade (Bell, 1980; Employee Benefit Plan Review, 1981), but at a slower rate of increase. Faster growth in real income for 1983-1990 is expected to put upward pressure on the growth in demand for dentists' services compared to the 1973-1982 period (all other factors held constant).
An important factor to watch in the 1980's is the growing trend toward department store dentistry with its emphasis on competitive prices, evening and weekend hours, and walk-in services (Cole, 1981).
Other Professional Services
Historical Perspective
Expenditures for other professional services (for example, optometrists, podiatrists, chiropractors, private-duty nurses, and home health agency services which are not hospital-based) have grown from $1.6 billion in 1971 to $6.4 billion in 1981 (Table 7), an average annual rate of growth of 14.6 percent (Table 8).
The use of home health services by the aging population is a factor contributing to the growth in expenditures for this service. Aged persons spend three times as much per capita for other professional services as nonaged persons (Fisher, 1980).
The role of other professional services in the increasing competition in the health services sector should not be underestimated. Home health services provide a cheaper alternative for some hospital, nursing home, and physician services. Optometrists, podiatrists, and chiropractors provide services which can substitute for and/or complement physicians' services in some instances. If consumer cost-sharing increases (including deductibles), we can expect increased utilization of other professional services as consumers become more sensitive to prices and substitute cheaper alternatives.
Projections
We project that expenditures for other professional services will reach $8 billion in 1983, $10 billion in 1985, and $17 billion in 1990 (Table 7). Expenditures are projected to increase at an average annual rate of 11.8 percent between 1981 and 1990 (Table 8).
Because of the substitution and complementary relationships between other professional services and other health services such as hospital, physician, and nursing home care, it is difficult to accurately project this expenditure category. Alternative scenarios can produce projections that are significantly different. The situation is complicated by the fact that home health services can substitute for and complement personal care services provided by household members. If reimbursement regulations for nursing home care are significantly changed, it will influence the need for personal care services provided by household members and change the demand for home health services.
Drugs and Medical Sundries
Historical Perspective
Expenditures for drugs and medical nondurables dispensed through retail channels have grown from $9 billion in 1971 to $21 billion in 1981 (Table 7), an average annual growth rate of 9.6 percent. About three-fourths of one percent of the GNP is spent on drugs and medical sundries. This category includes expenditures for prescription drugs (57 percent), over-the-counter drugs (31 percent) and medical sundries (12 percent).11
Aged persons spend more than twice as much per capita for drugs and medical sundries as the nonaged (Fisher, 1980). The aged use significantly more prescriptions per capita than the nonaged and pay a higher average price per prescription reflecting larger dosages per prescription (Trapnell, 1979).
The pharmaceutical preparations industry (Brand, 1974; Bureau of Labor Statistics, April 1982) and the drugstore industry (Bureau of Labor Statistics, April 1982; Friedman, 1980) are notable for extraordinary productivity increases (Cocks, 1974). From 1965 to 1974, output per hour increased at an average annual rate of 4.9 percent for all employees in the pharmaceutical preparations industry and at a 5.6 percent rate for all employees in the drugstore industry (Figure 12). For the period 1974-1980, productivity increased significantly but at substantially lower rates than previously for both industries—2.8 percent average annual rate for pharmaceutical preparations and 2.2 percent average annual rate for drugstores.
Figure 12. Drug Industry Trends for Productivity and Inflation-Adjusted Prices (Consumer and Producer), 1965 to 1981.
Prices of drugs at both the producer and consumer levels of distribution rose at rates significantly lower than the overall inflation rate for the period 1965-1974. During this period the implicit price deflator for GNP rose at an average annual rate of 5.0 percent, whereas producer prices for drugs (Producer Prices and Price Indexes, Code 063, drugs and pharmaceuticals) rose at an average annual rate of 1.3 percent, and consumer prices (CPI Detailed Report, medical care commodities) rose at an average annual rate of 1.0 percent. After adjusting for economy-wide inflation, producer prices decreased at an average annual rate of −3.5 percent per year and consumer prices decreased at an average annual rate of −3.8 percent per year (Figure 12).
Since 1974, drug prices have increased at about the same rate as overall inflation, about 7.9 percent. Figure 12 indicates that during periods of substantial productivity increases in the manufacture of pharmaceuticals, such as 1965 to 1974, inflation-adjusted producer prices for drugs declined at significant rates. As productivity increases decelerated, as during the 1974-1980 period, inflation-adjusted producer prices increased compared to the higher productivity period of 1965 to 1974. This same productivity/inflation-adjusted price association also applies at the retail level when drugstore productivity is compared to inflation-adjusted consumer prices for drugs. Consumer prices for drugs tend to move in tandem with producer prices, indicating that the mark-up of retail prices over producer prices has been fairly stable in spite of significant productivity increases in drugstores (Figure 12).
Projections
The short-term outlook is for expenditures for drugs and medical sundries to rise from $21 billion in 1981 to $25 billion in 1983, an average annual rate of increase of 7.8 percent. Relative to overall inflation (CPI all items) drug prices rose faster in the 12 months ending September 1982 than for any calendar year in the 1965-1981 period. For the 12 months ending September 1982 the CPI for prescription drugs rose 11.9 percent; the CPI for internal and respiratory over-the-counter drugs rose 11.1 percent; the CPI for medical care commodities (mostly drugs) rose 10.6 percent; and overall inflation (CPI all items) was 7.4 percent. The sharp increases in drug prices relative to other goods and services (price incentive to utilize fewer drugs), combined with the negative growth in real GNP, contributed to the negative growth in real consumption of drugs and medical sundries reported by the Commerce Department for the first three quarters of 1982.
Real income is projected to increase sharply in 1983 and grow steadily from 1984 to 1990; this is expected to increase demand for drugs and medical sundries. Expenditures are projected to reach $30 billion in 1985 and $47 billion in 1990 (Table 7). For the period 1981-1990 expenditures are projected to increase at an average annual rate of 9.6 percent.
In 1981 private health insurance benefits financed 11 percent of outlays for drugs and medical sundries (Gibson and Waldo, 1982), and the public sector financed another 9 percent, leaving 80 percent financed by direct consumer payments. The projections assume moderate growth in private health insurance coverage (Table A-10), but assume no significant expansion of benefits through a national health insurance program (Trapnell, 1979) or the addition of a Part B drug benefit under Medicare.
It is difficult to project expenditures for drugs in the 1980's due to the changes in productivity and pricing practices in the industry since 1974, and due to the potential new product lines including biotechnologies which may significantly alter prescribing patterns (Magnet, 1981; Mclntyre, 1982). It is also difficult to assess full implications of the Food and Drug Administration (FDA) procedural changes to reduce the time and expense associated with introducing drugs into the market.
Eyeglasses and Appliances
Historical Perspective
Consumer expenditures for ophthalmic products and durable medical equipment have almost tripled in the period 1971-1981, increasing from $2 billion to $5.7 billion in 1981 (Table 7), at an average annual growth rate of 11.2 percent. These expenditures are primarily for ophthalmic products. The usual pattern of the aged spending significantly more per capita than the nonaged is evident with aged persons spending about 1½ times as much per capita as non-aged persons (Fisher, 1980).
Compared to most health services and supplies industries, this industry is quite competitive (Benham, 1972; Feldman and Begun, 1978), as evidenced by its considerable price competition and advertising. Direct, out-of-pocket payments accounted for 82 percent of outlays for eyeglasses and appliances in 1981 (Gibson and Waldo, 1982), with public and private insurance exercising a relatively smaller role in consumer demand for these services.
These factors appear to be reflected in pricing behavior in the industry. For the period 1965-197712, the Consumer Price Index for Examining, Prescribing and Dispensing of Eyeglasses increased at an average annual rate of 5.1 percent while the GNP deflator increased 5.4 percent. Thus, after accounting for overall inflation in the economy, the CPI for this sector decreased at an average annual rate of −0.3 percent.
For the period 1978 to 1981, the new CPI for eyeglasses has increased at an annual rate of 7.1 percent compared to an overall inflation (GNP deflator) rate of 9.1 percent during this period. The CPI for eyeglasses has decreased at an average annual rate of −1.8 percent when adjustment is made for economy-wide inflation.
Projections
The short-term outlook is for expenditures for eyeglasses and appliances to grow from $5.7 billion in 1981 to $6 billion in 1983. Consumption of eyeglasses and durable medical equipment appears to have been sharply curtailed in 1982 according to partial-year U.S. Department of Commerce data. Third-party payments finance a small proportion of the expenditures. Consumers may delay or even forego purchase of eyeglasses and appliances during a recession. Real consumption is expected to decline substantially in 1982, but to rebound in 1983 as the economy expands. Retailers of eyeglasses appear to have reacted to the decline in demand by decelerating price increases. In September 1982, eyeglasses prices were only 3.9 percent higher than for the same month a year ago. By contrast, in calendar year 1981 the price of eyeglasses rose 6.9 percent.
By 1985 we expect that expenditures will reach $7.3 billion and by 1990, $11 billion. The projections assume that real consumption will rise substantially faster than real GNP over the 1982 to 1990 horizon and that consumer prices for eyeglasses will continue to rise slower than economy-wide prices.
Private health insurance benefits are projected to increase slightly faster than outlays in total for this sector, thus financing a higher proportion of the expenses (see Bell, 1980; Carroll and Arnett, 1981).
The appliances portion of eyeglasses and appliances includes durable medical equipment. The growth in durable medical equipment (walkers, traction equipment, wheelchairs, oxygen, hospital beds, etc.) is associated with growth in home health services (Cassack, 1982; Janssen and Saffran, 1981) which is included in the HCFA expenditure category of other professional services. The future expenditure growth for durable medical equipment (Cassack, 1982; Bandy, 1982) will partially be a function of reimbursement policies of Medicare, Medicaid, and private health insurance of both home health services and durable medical equipment.
Nursing Home Care
Historical Perspective
The $24 billion spent on nursing home care in 1981 comprised almost 1 percent of GNP. Nursing home care has risen from 1.7 percent of total systems cost in 1950 to 9.5 percent in 1981 (Table 5) reflecting expenditure growth at a phenomenal average annual rate of 17 percent. The only other total systems cost category that increased in relative importance over this period, hospital care (see Table 5), increased at an average of 11.7 percent annually.
Spending for nursing home care includes expenditures in all facilities (excluding hospital-based) that provide nursing care at some level. Skilled nursing facilities (SNFs) certified by Medicare and/or Medicaid and intermediate care facilities (ICFs) for regular patients and for the mentally retarded (ICF-MR) certified by Medicaid are included. In addition, all other homes that provide nursing care at some level are included, even though the facilities are not certified by Medicare and/or Medicaid.
Medicare and Medicaid finance half of all outlays for nursing home care. In January 1982, there were 7,850 skilled nursing facilities with 687,000 beds participating in Medicare and/or Medicaid; 11,157 intermediate care facilities with 961,000 beds participating in the Medicaid program;13 and an additional 1,453 institutions for the mentally retarded participating in the Medicaid program (Table A-23).
Table A-23. Number of Participating Long Term Care Facilities and Beds, Medicare and/or Medicaid, January 19821.
| Type of Facility | Number of Participating Facilities2 | Number of Beds2 |
|---|---|---|
|
|
|
|
| Skilled Nursing Facilities | ||
| Medicare and Medicare/Medicaid | 5,295 | 463,715 |
| Medicaid only | 2,555 | 223,450 |
| Intermediate Care Facilities (Medicaid) | 11,157 | 961,628 |
| Institutions for the Mentally Retarded (Medicaid) | 1,453 | NA |
NA = Not available
Statistical Information Services Branch, “Health Facilities Participating in HCFA Programs, 1982,” Health Care Spending Bulletin, Office of Statistics and Data Management, Bureau of Data Management and Strategy, Health Care Financing Administration, April 1982.
Facilities and beds that are dually certified under Medicaid as SNF and ICF are reported separately under both classifications. Double counting results if dually certified facilities and beds are added.
Expenditures for total nursing home care increased at an average annual rate of 15.7 percent for the period 1971 to 1981 (Table 8). Expenditures for the ICF-MR component have been increasing at a faster rate. For the period 1976-1981, expenditures for ICF-MR increased at an average annual rate of approximately 34 percent compared to 15 percent for nursing home care expenditures excluding ICF-MR.
This fast growth of expenditures for nursing home care is due to an interplay of demand and supply factors (Dunlop, 1978; Scanlon, 1978). Demand factors include a demographic shift toward the aged (Table A-3) (Dresch et al., 1981; Russell, 1981); growth in real income—each succeeding age cohort of residents has higher real income; expanded Medicaid benefits; including the addition of the ICF-MR benefit in 1973 (see Allard and Toff, 1980; Copeland and Iverson, 1980; and Trapnell et al., 1982); and the “transfer” of patients from mental hospitals to nursing homes (Bassuk and Gerson, 1978). Supply factors include: the increase in number of nursing home beds (Statistical Information Services Branch, 1982); and increases in prices paid for inputs (Data Resources, Inc., 1981; Fisher and Schendler, 1980; Health Care Financing Trends, quarterly).
We account for growth of nursing home expenditures (excluding ICF-MR) during the period 1971-1981, in terms of the five factors (Figure 13).14 Growth in nursing home days per capita15 accounted for 20 percent; growth in economy-wide inflation (GNP deflator) accounted for 53 percent; growth in real expenses per day (intensity) accounted for 13 percent; and growth in total population (all ages) and nursing home input prices in excess of overall inflation each accounted for 7 percent.
Figure 13. Factors Accounting for Growth in Expenditures for Nursing Home Care (Excluding ICF-MR) 1971 to 1981.
For the period 1978 to 1981 we estimate that aggregate nursing home days (excluding ICF-MR) increased at an average annual rate of approximately 3 percent, or at roughly the same rate of increase as in the age 75 and over population.
Projections
The short-term outlook, 1981 to 1983, is for total nursing home care expenditures to rise from $24 billion to $30 billion (Table 7), an average annual rate of increase of 11.9 percent. For the longer term, we project that expenditures will rise to $39 billion in 1985, and $67 billion in 1990. Excluding ICF-MR, we expect nursing home expenditures to reach $60 billion in 1990, up from $22 billion in 1981 (Figure 14). Higher prices paid for inputs to produce nursing home services and the aging of the population account for most of the projected increases. Aged persons spend more than 30 times as much per capita for nursing home care than nonaged persons (Fisher, 1980).
Figure 14. Expenditures for Nursing Home Care (Excluding ICF-MR) 1965 to 1990, with Bandwidth Intervals1.
1The bandwidth intervals around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in expenditures for nursing home services (excluding ICF-MR) for 1966-1981 (see Table A-12) was multiplied by a t-distribution value of 2.131 to derive the bandwidth intervals. The calculated bandwidth intervals are approximate and are used as a rough guide in assessing variability and uncertainty.
It is difficult to project nursing home care in the 1980's since nursing home care is but one component of our long-term care “system.” Hospital care, nursing home care, home health services, congregate housing, and personal care services provided by relatives and friends are all part of the network of long-term care that can be viewed as a system of substitutes and complements (see Figure 15). Changes in reimbursement regulations that directly impact on one sector of the total system can significantly influence other parts of the system. For example, less third-party funds available for nursing home care, could increase demand for home health services, congregate housing, hospital services, and personal services of relatives and friends.
Third parties (Medicare, Medicaid, Veterans Administration, etc.) financed approximately 58 percent of nursing home expenditures in 1981 (Table A-10). This proportion may decrease in the eighties due to a tightening of Federal, and State and local budgets. Thus, an increasing proportion of out-of-pocket expenses may have to be financed by Social Security and private pension payments, investment income, savings, assets, and contributions of friends and relatives (Marsh, 1981; Olson et al., 1981; Scholen and Chen, 1980).
Other Health Services
Historical Perspective
Other health services is a catch-all category which captures residual amounts of public program expenditures that are not classified elsewhere. It includes among other services: (1) care provided in Federal units other than hospitals; (2) School health services; and (3) industrial in-plant services (Gibson and Waldo, 1982). Expenditures for other health services were $7 billion in 1981 and comprised 2.8 percent of total systems cost (Table 5).
Projections
We project that expenditures for other health services will reach $8.5 billion by 1983, $10.3 billion in 1985, and $17.3 billion in 1990.
Program Administration and Net Cost of Insurance
Historical Perspective
Expenses for program administration and net cost of insurance include three components: (1) prepayment costs (including operating expenses) of private health insurance organizations (Blue Cross and Blue Shield plans, commercial insurance companies, independent plans), 2) administrative expenses of Federally-financed health programs, and 3) nonpersonal health expenditures of private voluntary health organizations for health education, lobbying, fund raising, etc. (Gibson and Waldo, 1982).
For private health insurance organizations, prepayment costs reflect the difference between the earned premiums or subscription income and incurred benefit payments (claims) and represents the net cost to the consumer. This amount is retained by private health insurance organizations for additions to reserves, profits, and operating expenses. The operating expense component is a function of competitive forces within the industry, the size of the enrolled population, the incidence of claims per enrollee, productivity improvements associated with automation, and wage growth for employees in the industry (Bureau of Labor Statistics, 1965; Bureau of Labor Statistics, 1979; Hays, 1982; Vogel and Blair, 1975). Operating expenses have been a fairly stable proportion of premium income (Carroll and Arnett, 1981); however, the additions to reserves and profits component are volatile and cyclical. It is difficult to project this component since both the length of the cycle and the depth of the cycle are variable.
Program administration and net cost of insurance expenses have risen from $3.4 billion in 1971 to $11.2 billion in 1981 for an average annual rate of growth of 12.6 percent (Table 8). Due to the cyclical nature of net cost of insurance expenses (caused by changes in reserves and profits component of prepayment costs) caution must be exercised in interpreting average annual growth rates (see Tables A-12 and A-16). Use of slightly different time periods can result in significantly different average annual rates of growth.
Table A-16. Measures of Central Tendency and Variability for Year-to-Year Percent Changes in Private Health Insurance Premiums, Benefits, Operating Expenses and Net Cost, 1966-19811.
| Variable4 | Measures of Variability2 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of Mean3 | ||
|
| |||||
| Mean | Median | ||||
| Aggregate Earned Premiums | 13.3% | 14.0% | 3.6% | 0.934% | 0.070 |
| Blue Cross/Blue Shield | 13.3 | 13.1 | 4.7 | 1.214 | 0.091 |
| Commercial Companies | 11.1 | 10.2 | 3.7 | 0.961 | 0.086 |
| Independent Plans | 22.5 | 22.1 | 10.3 | 2.668 | 0.119 |
| Aggregate Incurred Benefits | 13.7 | 13.2 | 4.8 | 1.248 | 0.091 |
| Blue Cross/Blue Shield | 13.6 | 15.0 | 5.9 | 1.514 | 0.111 |
| Commercial Companies | 11.6 | 10.9 | 6.2 | 1.591 | 0.137 |
| Independent Plans | 22.4 | 23.1 | 10.8 | 2.789 | 0.125 |
| Aggregate Operating Expenses | 10.7 | 12.7 | 8.5 | 2.188 | 0.205 |
| Blue Cross/Blue Shield | 15.1 | 14.2 | 2.8 | 0.712 | 0.047 |
| Commercial Companies | 8.9 | 10.4 | 10.0 | 2.579 | 0.289 |
| Independent Plans | 25.2 | 25.2 | 15.1 | 3.901 | 0.155 |
| Aggregate Net Cost of Insurance | 13.5 | 14.5 | 25.5 | 6.594 | 0.489 |
| Blue Cross/Blue Shield | 29.0 | 16.2 | 84.7 | 21.869 | 0.755 |
| Commercial Companies | 14.3 | 2.2 | 36.1 | 9.325 | 0.651 |
| Independent Plans | 33.4 | 24.6 | 52.3 | 13.497 | 0.404 |
There are 16 annual percent changes for the period 1966-1981.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of nonsampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
For definitions and detailed analysis of the private health insurance industry, see Carroll and Arnett (1981).
Projections
There will be substantial pressures in the early 1980's to raise premiums relative to benefits so that net underwriting gains can improve. The aggregate premium/benefit ratio (times 100) was estimated to be approximately 110 in 1981. That is, premiums were 10 percent greater than benefit outlays in 1981 (see Table A-17). The average for this ratio in the 1965 to 1981 period was approximately 113. When operating expenses are added to benefits, and this sum is divided by premiums, a combined ratio of approximately 105 is estimated for 1981. This implies negative net underwriting gains since benefit outlays plus operating expenses exceed premiums by approximately 5 percent.
Table A-17. Private Health Insurance Subscription or Premium Income, Benefit Expenditures, Personal Health Expenditures, and Gross National Product, Selected Years, 1950-1990.
| Year | Subscription or Premium Income1
2 (billions) |
Benefit Expenditures1
2 (billions) |
Personal Health Expenditures (billions) |
Benefit Expenditures As Percent of Personal Health Expenditures | Gross National Product (billions) |
Subscription or Premium Income as Percent of Gross National Product |
|---|---|---|---|---|---|---|
|
|
|
|||||
| Historical | ||||||
|
|
||||||
| 1950 | $ 1.3 | $ 1.0 | $10.9 | 9.2% | $286.5 | 0.5% |
| 1955 | 3.1 | 2.5 | 15.7 | 15.9 | 400.0 | 0.8 |
| 1960 | 5.8 | 5.0 | 23.7 | 21.1 | 506.5 | 1.1 |
| 1965 | 10.0 | 8.7 | 35.8 | 24.3 | 691.0 | 1.4 |
| 1966 | 10.6 | 9.1 | 39.6 | 23.0 | 756.0 | 1.4 |
| 1967 | 11.1 | 9.6 | 44.4 | 21.6 | 799.6 | 1.4 |
| 1968 | 12.9 | 11.0 | 50.2 | 21.9 | 873.4 | 1.5 |
| 1969 | 14.6 | 13.0 | 56.9 | 22.8 | 944.0 | 1.5 |
| 1970 | 17.1 | 15.6 | 65.1 | 24.0 | 992.7 | 1.7 |
| 1971 | 19.5 | 17.3 | 72.0 | 24.0 | 1,077.6 | 1.8 |
| 1972 | 22.4 | 19.1 | 80.2 | 23.8 | 1,185.9 | 1.9 |
| 1973 | 24.8 | 21.1 | 88.7 | 23.8 | 1,326.4 | 1.9 |
| 1974 | 27.8 | 24.5 | 101.0 | 24.3 | 1,434.2 | 1.9 |
| 1975 | 32.4 | 30.1 | 116.8 | 25.8 | 1,549.2 | 2.1 |
| 1976 | 38.2 | 35.5 | 131.8 | 26.9 | 1,718.0 | 2.2 |
| 1977 | 44.6 | 40.0 | 148.7 | 26.9 | 1,918.3 | 2.3 |
| 1978 | 49.7 | 45.0 | 166.7 | 27.0 | 2,163.8 | 2.3 |
| 1979 | 55.9 | 50.2 | 188.9 | 26.5 | 2,417.8 | 2.3 |
| 1980 | 63.6 | 57.0 | 219.4 | 26.0 | 2,633.1 | 2.4 |
| 1981 | 73.2 | 66.8 | 255.0 | 26.2 | 2,937.7 | 2.5 |
| Projections | ||||||
|
|
||||||
| 1983 | 95.2 | 85.3 | 323.6 | 26.3 | 3,468.9 | 2.7 |
| 1985 | 121.3 | 107.8 | 408.2 | 26.4 | 4,207.4 | 2.9 |
| 1990 | 195.6 | 178.6 | 684.4 | 26.1 | 6,304.1 | 3.1 |
| Selected Periods | Average Annual Percent Increases | |||||
|
|
|
|||||
| 1950-1955 | 19.5% | 20.7% | 7.6% | — | 6.9% | — |
| 1955-1960 | 13.2 | 14.5 | 8.6 | — | 4.8 | — |
| 1960-1965 | 11.3 | 11.8 | 8.6 | — | 6.4 | — |
| 1965-1970 | 11.3 | 12.3 | 12.7 | — | 7.5 | — |
| 1970-1975 | 13.7 | 14.0 | 12.4 | — | 9.3 | — |
| 1975-1980 | 14.4 | 13.6 | 13.4 | — | 11.1 | — |
| 1950-1980 | 13.9 | 14.4 | 10.5 | — | 7.7 | — |
| 1970-1980 | 14.1 | 13.8 | 12.9 | — | 10.2 | — |
| 1980-1990 | — | 9.4 | — | |||
| 1981-1983 | 14.1 | 13.0 | 12.7 | — | 8.7 | — |
| 1983-1985 | 12.9 | 12.4 | 12.3 | — | 10.1 | — |
| 1980-1985 | 13.8 | 13.6 | 13.2 | — | 9.8 | — |
| 1985-1990 | 10.0 | 10.6 | 10.9 | — | 8.4 | — |
| 1971-1981 | 14.2 | 14.5 | 13.5 | — | 10.5 | — |
| 1981-1990 | 11.5 | 11.5 | 11.5 | — | 6.9 | — |
Blue Cross and Blue Shield Plans, Commercial Insurance Company Plans, and Independent Health Plans.
Majorie Smith Carroll and Ross H. Arnett III, “Private Health Insurance Plans in 1978 and 1979: A Review of Coverage, Enrollment, and Financial Experience,” Health Care Financing Review, September, 1981, pp. 55-87 and Robert M. Gibson and Daniel R. Waldo, “National Health Expenditures, 1981” Health Care Financing Review, September, 1982, pp. 1-36.
As interest rates decline in the early 1980's, there will be additional pressures to raise premiums relative to benefits. The lower interest rates imply there will be less investment income to offset underwriting losses. In other words, the extent of “cash-flow underwriting” in which premium rates are set at levels that imply net underwriting losses is likely to diminish in the early 1980's. With lower economy-wide inflation and interest rates and thus lower yielding financial instruments, it will be more difficult to recoup net underwriting losses. Program administration and net cost of insurance expenses are projected to reach $16 billion in 1983, $21 billion in 1985 and $28 billion in 1990.
Government Public Health Activities
Historical Perspective
Government public health activities include: surveillance, detection, and control through immunization and quarantines of epidemic diseases; and activities aimed at prevention and control of health problems and diseases (examples are drug abuse, mental health, and venereal disease programs).
Expenditures for government public health activities have risen from $1.8 billion in 1971 to $7.3 billion in 1981 (Table 7). This reflects an average annual rate of growth of 15 percent. During this period, State and local governments financed a large share, increasing from 53 percent of the total in 1971 to 82 percent in 1981. (Table A-10)
Projection
The short-term outlook is for expenses for government public health activities to rise to $7.8 billion by 1983. This is a marked slowdown in growth due to restrictive government fiscal positions. Expenses are projected to reach $9.4 billion in 1985 and $16.7 billion in 1990.
The tight revenue conditions at all government levels combined with wage rate increases for public health employees is projected to squeeze growth in real service output in the 1981-1990 period relative to the 1971-1981 period.
Research
Historical Perspective
Expenditures for medical research increased from $1.5 billion in 1965 to $5.7 billion in 1981. Research expenditures have been getting a smaller share of total health spending, declining from 3.6 percent of the total in 1965 to 2.0 percent in 1981. Research as a percent of the GNP declined also.
Projection
In the short term, we project that expenditures for medical research will increase to $5.8 billion in 1983. For the medium term, expenditures are projected to reach $6.5 billion in 1985 and $9.7 billion in 1990. In 1981 the federal government financed 85 percent of research expenditures and we expect this share to remain relatively stable over the projection horizon.
Construction of Medical Facilities
Historical Perspective
Expenditures for construction of medical facilities have risen from $2.0 billion in 1965 to $7.5 billion in 1981 (Table 7 and Figure 16). This reflects an average annual rate of growth of 8.6 percent. The price of construction materials, as measured by the U.S. Department of Commerce Composite Construction Cost Index, rose at an average annual rate of 8.1 percent during this period and implies that real construction expenditures rose at an average annual rate of only 0.4 percent.
Figure 16. Index of Nominal and Real Expenditures for Construction of Medical Facilities, 1965 to 1981 (1965 = 100.0).
Data suggest an erosion of the health sector's capital position. There has been relatively fast growth in beds compared to increases in real spending per bed for renovation and modernization. High inflation and technological change have contributed to this erosion and obsolesence of capital. According to the American Hospital Association Panel Survey, from 1965 to 1981 community hospital beds grew at an average annual rate of 1.9 percent, and nursing home beds are estimated to have grown at an average annual rate of roughly 6 percent. A significant portion of the nursing home bed growth occurred in the 1965-1971 period. Real expenditures declined from $6.6 billion in 1971 to $4.5 billion in 1979, an average annual rate of decrease of −4.8 percent. Beginning in 1980, real construction expenditures started to rise and in 1981 they increased 8.5 percent despite high interest rates and tight credit conditions (Figure 16). In July 1982 real construction spending was 3 percent higher than for the same month a year ago. This real growth in 1982 starkly contrasts with the 21 percent reduction in total nonresidential building construction forecasted by Dodge Construction Potentials (Christie, 1982) for 1982.
Projections
The short-term outlook is for current dollar construction expenditures to rise from $7.5 billion in 1981 to $9.1 billion in 1983. Expenditures are projected to reach $11.5 billion in 1985 and $17 billion in 1990. The price of goods and services used in construction of medical facilities is expected to rise at a slower rate in the 1980's due to a moderating of overall inflation, but real growth is expected to rise significantly faster than in the 1970's.
During the 1950's and 1960's Hill-Burton funds financed the building of a substantial number of beds. By the 1980's and 1990's much of this fixed equipment and plant will require replacement or modernization. Several studies indicate that there will be great pressures in the last two decades of this century to modernize, renovate, replace and build new hospital plant and fixed equipment (Bradford et al., 1982; Hernandez and Valimahomed, 1981; Kelling and Williams, 1978; Lightle and Plomann, 1981; Phillips, 1982; Ting and Valiante, 1982). Shifts in geographic and age distributions of the population will also increase demand for new beds and facilities. Due to these pressures, future real growth in construction will not be an extrapolation of real growth in the 1970's.
Financing is expected to derive from internal sources such as net income and depreciation allowances and from external sources including philanthropic gifts, government grants, and debt. Private sources of funding are expected to pay an increasing share of medical facility construction costs in the 1980's (Table A-10).
It will be important for institutions to develop viable strategies to make capital-related decisions in the 1980's which account for financial and regulatory constraints as well as market opportunities. The intensification of competition in the 1980's will put a premium on medical facility location, cost of service, and product/service differentiation—all capital-related attributes.
Summary
Projections of national health expenditures by type of expenditures and source of finance have been presented for 1983, 1985 and 1990. The projections assumed, among other factors, that historical trends and relationships will continue and that neither a mandatory cost containment program nor national health insurance will be in effect. These baseline current-law projections incorporated the Health Care Financing Administration's projections of Medicare benefit outlays and total community hospital inpatient expenses; the Bureau of Health Professions' projections of active physicians and dentists; and the 1982 Board of Trustees' (Board of Trustees, Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds, 1982) projections of the GNP and overall inflation.
There are significant implications for the economy as the health sector continues to absorb larger percentages of the GNP. The major one being, as more labor and capital are drawn into the health sector, relatively fewer resources are available for producing goods and services in other sectors (Cameron and Kirkland, 1980).
There seem to be few demand or supply incentives to significantly retard the growth of health expenditures under current institutional arrangements. As the population ages and as new health technologies are adopted, health costs increase. As health costs increase, so does the risk of financial burden to consumers with inadequate health insurance coverage. As this risk increases, the demand for public programs and private health insurance also rises. More-over, tax subsidies for health insurance premiums add to this increased demand by encouraging the purchase of more comprehensive insurance. As the proportion paid out-of-pocket by consumers (coinsurance rate) declines with the additional insurance, both consumers and providers increasingly tend to treat health care services as a free good at the time of purchase. The ensuing increased demand for medical care interacts with our fee-for-service and retrospective cost-based reimbursement systems to further increase costs. That is, more services and more costly services reward providers with additional revenues from third-party payers. The reimbursement policy provides an incentive for providers to adopt product-innovative technologies, which increase costs. There is relatively less incentive to adopt process-innovative technologies, which are associated with increased productivity and decreased costs.
Our current institutional arrangement of third-party payments, with fee-for-service and retrospective cost-based reimbursement, has evolved out of an interaction among providers, third party payers, and consumers, based on their economic, social, and political needs and demands. Until an alternative institutional arrangement is devised that better meets the often conflicting needs and demands placed on the current system, the affected parties may resist significant changes to the current arrangement.
Assuming that the current incentive mechanisms and constraints affecting the demand for and supply of medical care are not significantly modified, and that the projected growth in inflation and GNP is accurate, the projections of health expenditures presented in this paper are a reasonable approximation of what can be expected for the next decade.
An explanation of methodology used to prepare this article is available from the authors. Requests should be mailed to Room 4440 HHS Building; 330 Independence Avenue, S.W.; Washington, D.C. 20201.
Table A-6. Annual Percent Changes in Nominal and Constant Dollar GNP and National Health Expenditures, 1950-1981.
| Year | Gross National Product | Real Gross National Product (1972 Dollars) | Implicit Price Deflator GNP | National Health Expenditures | National Health Expenditures as Percent of GNP | National Health Expenditures in 1972 Dollars1 |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
| 1950 | 10.9% | 8.7% | 2.0% | 9.4% | −1.4% | 7.2% |
| 1951 | 15.5 | 8.3 | 6.6 | 10.5 | −4.3 | 3.6 |
| 1952 | 5.2 | 3.7 | 1.4 | 7.1 | 1.8 | 5.6 |
| 1953 | 5.4 | 3.8 | 1.6 | 5.1 | −0.3 | 3.4 |
| 1954 | 0.0 | −1.2 | 1.2 | 6.7 | 6.7 | 5.4 |
| 1955 | 9.1 | 6.7 | 2.2 | 5.6 | −3.2 | 3.4 |
| 1956 | 5.4 | 2.1 | 3.2 | 8.5 | 2.9 | 5.1 |
| 1957 | 5.3 | 1.8 | 3.4 | 9.7 | 4.2 | 6.1 |
| 1958 | 1.3 | −0.4 | 1.7 | 8.2 | 6.9 | 6.5 |
| 1959 | 8.5 | 6.0 | 2.4 | 8.9 | 0.3 | 6.3 |
| 1960 | 3.8 | 2.2 | 1.6 | 8.1 | 4.1 | 6.4 |
| 1961 | 3.6 | 2.6 | 0.9 | 7.0 | 3.3 | 6.1 |
| 1962 | 7.7 | 5.8 | 1.8 | 8.7 | 0.9 | 6.8 |
| 1963 | 5.6 | 4.0 | 1.5 | 7.1 | 1.4 | 5.5 |
| 1964 | 6.9 | 5.3 | 1.5 | 11.7 | 4.5 | 10.1 |
| 1965 | 8.4 | 6.0 | 2.2 | 11.4 | 2.8 | 9.0 |
| 1966 | 9.4 | 6.0 | 3.2 | 10.5 | 1.0 | 7.0 |
| 1967 | 5.8 | 2.7 | 3.0 | 11.4 | 5.3 | 8.2 |
| 1968 | 9.2 | 4.6 | 4.4 | 13.4 | 3.9 | 8.7 |
| 1969 | 8.1 | 2.8 | 5.2 | 12.9 | 4.4 | 7.3 |
| 1970 | 5.2 | −0.2 | 5.4 | 13.6 | 8.0 | 7.8 |
| 1971 | 8.6 | 3.4 | 5.0 | 11.5 | 2.8 | 6.3 |
| 1972 | 10.0 | 5.7 | 4.1 | 12.3 | 2.0 | 7.8 |
| 1973 | 11.8 | 5.8 | 5.8 | 10.3 | −1.3 | 4.3 |
| 1974 | 8.1 | −0.6 | 8.9 | 12.8 | 4.3 | 3.6 |
| 1975 | 8.0 | −1.2 | 9.2 | 14.0 | 5.6 | 4.4 |
| 1976 | 10.9 | 5.4 | 5.2 | 12.8 | 1.7 | 7.2 |
| 1977 | 11.7 | 5.5 | 5.8 | 13.1 | 1.3 | 6.9 |
| 1978 | 12.8 | 5.0 | 7.4 | 11.9 | −0.5 | 4.2 |
| 1979 | 11.7 | 2.8 | 8.7 | 13.5 | 1.4 | 4.5 |
| 1980 | 8.9 | −0.4 | 9.3 | 15.8 | 6.5 | 5.9 |
| 1981 | 11.6 | 1.9 | 9.4 | 15.1 | 3.3 | 5.2 |
Deflated using the implicit price deflator for GNP.
Table A-13. Measures of Central Tendency and Variability for Year-to-Year Percent Changes in Various Health Sector Prices. 1966-19811.
| Type of National Health Expenditure | Price Variable | Measures of Variability2 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of The Mean3 | |||
|
| ||||||
| Mean | Median | |||||
|
|
|
|
|
|
|
|
| Total | Implicit Price Deflator National Health Expenditures | 7.0% | 7.2% | 2.2% | 0.569% | 0.082 |
| Personal Health Care (Total Systems Cost) | Implicit Price Deflator Total Systems Cost | 7.2 | 7.1 | 2.5 | 0.645 | 0.090 |
| Hospital Care | Implicit Price Deflator Hospital Care | 8.1 | 7.8 | 2.0 | 0.529 | 0.065 |
| Community Hospital Care | National Hospital Input Price Index | 8.2 | 8.1 | 2.1 | 0.549 | 0.067 |
| Inpatient | National Hospital Input Price Index | 8.2 | 8.1 | 2.1 | 0.549 | 0.067 |
| Outpatient | National Hospital Input Price Index | 8.2 | 8.1 | 2.1 | 0.549 | 0.067 |
| Federal Hospital Care | Federal Hospital Input Price Index | 7.3 | 8.2 | 3.0 | 0.770 | 0.105 |
| Physicians' Services | CPI Physicians'Services | 8.0 | 7.9 | 2.6 | 0.676 | 0.085 |
| Dentists'Services | CPI Dental Services | 6.8 | 6.7 | 2.4 | 0.608 | 0.089 |
| Other Professional Services | CPI Professional Services | 7.5 | 7.3 | 2.3 | 0.582 | 0.078 |
| Drugs and Medical Sundries | CPI Medical Care Commodities | 4.0 | 2.8 | 3.7 | 0.953 | 0.237 |
| Eyeglasses and Appliances | CPI Eyeglasses | 4.7 | 4.7 | 1.7 | 0.440 | 0.093 |
| Nursing Home Care | National Nursing-Home Input Price Index | 7.9 | 7.8 | 1.5 | 0.391 | 0.049 |
| Nursing-Home Care Excluding ICF-MR | National Nursing-Home Input Price Index | 7.9 | 7.8 | 1.5 | 0.391 | 0.049 |
| Other Health Services | CPI Medical Care | 7.8 | 7.7 | 2.5 | 0.657 | 0.085 |
| Program Administration and Net Cost of Insurance | Implicit Price Deflator for Program Administration and Net Cost of Insurance | 6.5 | 6.3 | 1.9 | 0.499 | 0.077 |
| Government Public Health Activities | Wages and Salaries per Employee in Civilian Federal Government and in State and Local Government | 7.2 | 7.2 | 1.6 | 0.409 | 0.057 |
| Research | Biomedical Research and Development Price Index | 6.7 | 6.3 | 1.8 | 0.462 | 0.069 |
| Construction of Medical Facilities | Department of Commerce Composite Construction Cost Index | 8.2 | 7.1 | 3.8 | 0.987 | 0.120 |
There are 16 annual percent changes for the period 1966-1981.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of nonsampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
Table A-14. Measures of Central Tendency and Variability for Year-to-Year Percent Changes in Real National Health Expenditures by Type of Expenditure, 1966-19811 2.
| Type of Real National Health Expenditure | Measures of Variability3 | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measures of Central Tendency | Standard Deviation | Standard Error | Coefficient of Variation of The Mean4 | ||
|
| |||||
| Mean | Median | ||||
|
|
|
|
|
|
|
| Total | 5.5% | 4.7% | 1.4% | 0.367% | 0.067 |
| Personal Health Care (Total Systems Cost) |
5.5 | 4.8 | 1.5 | 0.386 | 0.070 |
| Hospital Care | 5.7 | 5.4 | 1.8 | 0.454 | 0.079 |
| Community Hospital Care | 7.0 | 6.4 | 2.3 | 0.605 | 0.086 |
| Inpatient | 6.7 | 5.9 | 2.4 | 0.624 | 0.093 |
| Outpatient | 9.9 | 10.3 | 3.2 | 0.835 | 0.084 |
| Federal Hospital Care | 3.6 | 3.0 | 4.6 | 1.186 | 0.328 |
| Physicians' Services | 4.1 | 4.2 | 1.9 | 0.493 | 0.119 |
| Dentists' Services | 5.0 | 4.4 | 3.0 | 0.764 | 0.154 |
| Other Professional Services | 4.4 | 5.8 | 4.0 | 1.022 | 0.234 |
| Drugs and Medical Sundries | 5.2 | 5.3 | 3.4 | 0.879 | 0.170 |
| Eyeglasses and Appliances | 5.6 | 6.5 | 5.3 | 1.375 | 0.246 |
| Nursing-Home Care | 8.1 | 7.9 | 2.9 | 0.749 | 0.093 |
| Nursing-Home Care Excluding ICF-MR | 7.4 | 6.8 | 3.3 | 0.842 | 0.114 |
| Other Health Services | 4.3 | 3.3 | 5.9 | 1.524 | 0.357 |
| Program Administration and Net Cost of Insurance | 7.1 | 7.5 | 15.3 | 3.943 | 0.558 |
| Government Public Health Activities | 7.1 | 7.2 | 6.0 | 1.549 | 0.217 |
| Research | 1.8 | 1.8 | 3.5 | 0.895 | 0.495 |
| Construction of Medical Facilities | 0.8 | −0.6 | 8.0 | 2.067 | 2.733 |
There are 16 annual percent changes for the period 1966-1981.
Real health expenditures were calculated by deflating current-dollar health expenditures by the price variables displayed in Table A-13.
ln textbook examples, measures of variability typically measure sampling variability, that is, variations that might occur by chance because a sample of the population is surveyed. As calculated in this paper (and for typical applied time-series analyses) measures of variability also reflect variability associated with evolving causal structures and variability associated with various types of nonsampling errors such as data processing mistakes, nonresponse, misreporting by respondents, etc. The calculated measures are approximate and are meant as a general guide. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no guarantee that future variability will replicate historical variability.
For cautions in using the coefficient of variation when the mean of the variable measures change, see Kish (1965, pp. 47-49).
Acknowledgments
The authors are indebted to Charles R. Fisher, Acting Director of the Division of National Cost Estimates; Roland King, Fellow of the Society of Actuaries, Director of the Office of Financial and Actuarial Analysis; and to Gordon R. Trapnell, Fellow of the Society of Actuaries, Actuarial Research Corporation, Falls Church, Virginia, for their helpful comments and suggestions. Significant contributions to the article were made by Ross H. Arnett, III, Marjorie S. Carroll, Robert M. Gibson, Katharine R. Levit, Stephen H. Siegel, and Daniel R. Waldo, all of the Office of Financial and Actuarial Analysis. Jeffrey Coombs of Data Resources, Inc. provided technical support. The authors are grateful to Joanie L. Henderson and Roszetta C. Holmes for secretarial assistance.
Footnotes
The implicit price deflator for GNP is a widely used indicator of inflation that takes into consideration not only changes in price of the various components of the GNP (consumer goods and services such as food, health care, and the like, plus government services, investment, and net exports), but also the changing mix of the economy's output. The GNP deflator measures price changes of a wider group of goods than does the Consumer Price Index (CPI), which does not include investment, net exports, and the government sector.
The earliest year for which data are available for average hourly earnings of employees in the health services sector is 1972 (Bureau of Labor Statistics, July 1979).
Unfortunately, productivity data could not be located for the same time interval as the wage and price data.
Figure 12 indicates that high productivity increases can be associated with price increases that are substantially below economy-wide inflation, as was the case for the drug industry for the period 1965-1973.
These quarterly percent changes represent contiguous quarters, not percent changes from same quarters a year ago.
It is important to note that it cannot be discerned from Figure 15 the extent to which patients remain in hospitals beyond the optimal time for discharge because placement in a nursing home is not available.
Hospital care includes some ambulatory care in providing outpatient services.
An economy-wide measure of inflation, the GNP deflator, was used to adjust TSCPC for inflation.
Different data collection methods are used for the total employment and the non-Federal office-based physician series.
Different data collection methods are used for these two data series.
Medical sundries such as bandages and iodine are classified as medical nondurables. Medical durables such as crutches and bedpans are included in the HCFA expenditure category of eyeglasses and appliances. Spending for drugs dispensed or purchased by hospitals, physicians, dentists, and nursing homes is excluded from the HCFA category of drugs and medical sundries. Such spending for drugs is included in the respective HCFA categories of hospital care, physicians' services, dentists' services and nursing home care.
1977 is the last calendar year for which a continuous CPI times series is available for eyeglasses and related services.
Facilities and beds that are dually certified under Medicaid as SNF and ICF are reported separately under both classifications. Double counting results if dually certified facilities and beds are added.
Reliable annual data does not exist for aggregate nursing home days, beds, charges per day, etc. There are several data sources, relating to the nursing home industry that are available on a current or periodic basis. These data sources are synthesized by HCFA to develop a consistent time-series of the nursing home industry. It is with these caveats in mind that one must interpret the factors accounting for growth in the nursing home industry shown in Figure 13.
lt must be emphasized that this is growth in nursing home days relative to total population (all ages).
References
- Alhadeff David A. Microeconomics and Human Behavior: Toward a New Synthesis of Economics and Psychology. Berkeley, California: University of California Press; 1982. [Google Scholar]
- Allard Mary Ann, Toff Gail. Current and Future Development of Intermediate Care Facilities for the Mentally Retarded: A Survey of State Officials. Washington, D.C.: George Washington University; Aug, 1980. Intergovernmental Health Policy Project. [Google Scholar]
- Altman Drew, Greene Richard, Sapolsky Harvey M. Health Planning and Regulation: The Decision-Making Process. Ann Arbor, Michigan: Health Administration Press; 1981. [Google Scholar]
- Altman Stuart H, Blendon Robert., editors. Proceedings of the 1977 Sun Valley Forum on National Health. 1979. Medical Technology: The Culprit Behind Health Care Costs? pp. 79–3216. DHEW Publication No. (PHS) [Google Scholar]
- American Hospital Association. Hospital Statistics. Chicago: 1982. [Google Scholar]
- American Medical Association. Profile of Medical Practice. AMA Center for Health Services Research and Development, 1980; 1981. [Google Scholar]
- American Medical News. Medicine's Future Uncertain Says AMA Executive. American Medical News. 1980 Oct 24;:9. [Google Scholar]
- Armstrong J Scott. Long-Range Forecasting. John Wiley and Sons; 1978. [Google Scholar]
- Ascher William. Forecasting, An Appraisal for Policy-Makers and Planners. Johns Hopkins University Press; 1978. [Google Scholar]
- Bandy W Claude. 1982 US Industrial Outlook for 200 Industries with Outlook for 1985. U.S. Department of Commerce, Bureau of Industrial Economics; Jan, 1982. Medical and Dental Instruments and Supplies; pp. 361–369. [Google Scholar]
- Bassuk Ellen L, Gerson Samuel. Deinstitutionalization and Mental Health Services. Scientific American. 1978 Feb;238:45–53. doi: 10.1038/scientificamerican0278-46. [DOI] [PubMed] [Google Scholar]
- Bell Donald R. Dental and Vision Care Benefits in Health Insurance Plans. Monthly Labor Review. 1980 Jun;:22–26. [PubMed] [Google Scholar]
- Benham L. The Effect of Advertising on the Price of Eyeglasses. Journal of Law and Economics. 1972 Oct;:337–352. [Google Scholar]
- Berman Howard J, Weeks Lewis W. The Financial Management of Hospitals. Ann Arbor, Michigan: Health Administration Press; 1982. [Google Scholar]
- Biles Brian, Schramm Carl J, Atkinson J Graham. Hospital Cost Inflation understate Rate-Setting Programs. New England Journal of Medicine. 1980 Sep 18;:664–668. doi: 10.1056/NEJM198009183031203. [DOI] [PubMed] [Google Scholar]
- Birnbaum Howard, Lee A James, Bishop Christine E, Jensen Gail A. Public Pricing of Nursing Home Care. Cambridge, Mass: Abt Books; 1982. [Google Scholar]
- Board of Trustees. 1982 Annual Report. Washington: Apr 1, 1982. Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds. [Google Scholar]
- Bradford Charles, Caldwell George, Goldsmith Jeff. The Hospital Capital Crisis: Issues for Trustees. Harvard Business Review. 1982 Sep-Oct;:56–68. [PubMed] [Google Scholar]
- Brand Horst. Productivity in the Pharmaceutical Industry. Monthly Labor Review. 1974 Mar;:9–14. [Google Scholar]
- Bromberg Michael. Review. Federation of American Hospitals; Jul-Aug. 1982. New Financing Arrangements; p. 5. [PubMed] [Google Scholar]
- Bureau of Census. Statistical Abstract of the United States 1981. U.S. Department of Commerce; 1981. [Google Scholar]
- Bureau of Economic Analysis. Survey of Current Business. U.S. Department of Commerce; [Google Scholar]
- Bureau of Labor Statistics. Employment and Earnings, United States 1909-78. U.S. Department of Labor; Jul, 1979. Bulletin 1312-11. [Google Scholar]
- Bureau of Labor Statistics. Impact of Office Automation in the Insurance Industry. U.S. Department of Labor; 1965. BLS Bulletin 1468. [Google Scholar]
- Bureau of Labor Statistics. Productivity Measures for Selected Industries, 1954-1980. U.S. Department of Labor; Apr, 1982. Bulletin 2128. [Google Scholar]
- Bureau of Labor Statistics. Technology and Labor in Five Industries. U.S. Department of Labor; 1979. BLS Bulletin 2033. [Google Scholar]
- Business Week. Which Inflation Rate Should Business Use? Business Week. 1980 Apr 7;:94–97. [Google Scholar]
- Cameron Juan, Kirkland Richard I., Jr Five Burdens That Make a Rich U.S. Feel Poor. Fortune. 1980 Jan 14;:72–79. [Google Scholar]
- Cantor Samuel C. The National Underwriter. Life and Health Insurance; Aug 19, 1981. ‘Age of Entitlement’ May be Ending; p. 11. [Google Scholar]
- Carroll Marjorie Smith, Arnett Ross H., III Private Health Insurance Plans in 1978 and 1979: Coverage, Enrollment, and Financial Experience. Health Care Financing Review. 1981;3(No. 1):55–87. [PMC free article] [PubMed] [Google Scholar]
- Cassack David. Forecast 1982. Surgical Business. 1982 Jan;:20–35. [PubMed] [Google Scholar]
- Chambers Thomas C, Stern Alfred R. The Staggering Cost of Prolonging Life. Business Week. 1981 Feb 23;:19–20. [PubMed] [Google Scholar]
- Christie George A. The Data Resources Review of the US Economy. Lexington, Mass: Aug, 1982. 1982 Dodge/Sweets' Construction Outlook; pp. 1.14–1.20. [Google Scholar]
- Cocks Douglas L. The Measurement of Total Factor Productivity for a Large U.S. Manufacturing Corporation. Business Economics. 1974 Sept.:7–20. [Google Scholar]
- Coelen Craig, Sullivan Daniel. An Analysis of the Effects of Prospective Reimbursement Programs on Hospital Expenditures. Health Care Financing Review. 1981;2(No. 3):1–40. [PMC free article] [PubMed] [Google Scholar]
- Cole Leonard A. A New Look in American Dentistry. The New York Times Magazine. 1981 Apr 5;:86–94. [Google Scholar]
- Congressional Budget Office. An Analysis of the Presidents' Budget Proposals for Fiscal Year 1983. Congress of the United States; Feb, 1982. [Google Scholar]
- Congressional Budget Office. Containing Medical Care Costs Through Market Forces. Congress of the United States; May, 1982A. [Google Scholar]
- Congressional Budget Office. Interactions Among Programs Providing Benefits to Individuals: Secondary Effects on the Budget. Congress of the United States; May, 1982B. [Google Scholar]
- Congressional Budget Office. Catastrophic Health Insurance. Jan, 1977. Budget Issue Paper. [Google Scholar]
- Congressional Budget Office. Tax Subsidies for Medical Care: Current Policies and Possible Alternatives. Jan, 1980. Background Paper. [Google Scholar]
- Copeland William C, Iverson Iver A. Medicaid Funding for the Continuum of Care for MDIDD Persons. Hubert H. Humphrey Institute of Public Affairs, University of Minnesota; Minneapolis: Mar 11, 1980. [Google Scholar]
- Cotterill Phillip G. The Physician-Induced Demand and Target-Income Models: A Survey of The Issues. In: Gaffney John C., editor. Profile of Medical Practice, 1978. Revised Edition. American Medical Association; 1979. pp. 83–94. [PubMed] [Google Scholar]
- Council of Economic Advisors. Economic Report of the President. 1982. [Google Scholar]
- Crichton Anne. Health Policy Making. Ann Arbor, Michigan: Health Administration Press; 1981. [Google Scholar]
- Data Resources, Inc. Health Care Costs. Washington, D.C.: monthly. [Google Scholar]
- Davis Karen, Russell Louise B. The Substitution of Hospital Outpatient Care for Inpatient Care. Review of Economics and Statistics. 1972;54:109–120. [Google Scholar]
- Dean Joel. Managerial Economics. Englewood Cliffs, N.J.: Prentice-Hall, Inc.; 1951. [Google Scholar]
- Delbanco TL, Meyers KC, Segal EA. Paying the Physician's Fee: Blue Shield and the Reasonable Charge. New England Journal of Medicine. 1979;301:1314–1320. doi: 10.1056/NEJM197912133012404. [DOI] [PubMed] [Google Scholar]
- Denton Frank T, Spencer Byron G. Health Care Costs When the Population Changes. The Canadian Journal of Economics. 1975 Feb;:34–48. [Google Scholar]
- Division of Health Professions Analysis, Bureau of Health Professions. Third Report to the President and Congress on the Status of Health Professions Personnel. Health Resources Administration, U.S. Department of Health and Human Services; Jan, 1982. [Google Scholar]
- Douglas C, Cole K. The Supply of Dental Manpower in the United States. Journal of Dental Education. 1979;43:5. [PubMed] [Google Scholar]
- Douglas CW, Day JM. Cost and Payment of Dental Services in the United States. Journal of Dental Education. 1979 Jul;:330–348. [PubMed] [Google Scholar]
- Dresch Stephen P, Garvey Nancy A, Waldenberg Adair. The Aged: Population Composition and Health Care Utilization, 1979 to 2015. New Haven, Connecticut: Institute for Demographic and Economic Studies; Feb, 1981. [Google Scholar]
- Drury Patricia, Enthoven Alain. Competition and Health Care Costs. In: Boskin Michael J., editor. The Economy in the 1980's: A Program for Growth and Stability. San Francisco: Institute of Contemporary Studies; 1980. pp. 393–417. [Google Scholar]
- Duesenberry James S. Income, Saving, and the Theory of Consumer Behavior. Cambridge, Mass: Harvard University Press; 1949. [Google Scholar]
- Dunlop Burton. Understanding the Growth in Nursing Home Care, 1964-1974. Washington, D.C.: The Urban Institute; Apr, 1978. [Google Scholar]
- Eckstein Otto. Core Inflation. Englewood Cliffs: Prentice-Hall; 1981. [Google Scholar]
- Ellwein Linda Krane, Gregg David D. Review. Federation of American Hospitals; Jul-Aug. 1982. InterStudy Researchers Trace Progress of PPOs, Provide Insight into Future Growth; pp. 20–25. [PubMed] [Google Scholar]
- Employee Benefit Plan Review. Employee Benefit Plan Review. Nov, 1981. Dental Insurance is Fastest Growing Benefit; p. 88. [Google Scholar]
- Enthoven Alain C. Health Plan: The Only Practical Solution to the Soaring Cost of Medical Care. Reading, Mass: Addison-Wesley; 1980. [Google Scholar]
- Feldman R, Begun JW. The Effects of Advertising, Lessons from Optometry. Journal of Human Resources. 1978;(Supplement):247–262. [PubMed] [Google Scholar]
- Feldstein Martin S. An Econometric Model of the Medicare System. Quarterly Journal of Economics. 1970 May; [Google Scholar]
- Feldstein Martin S. Cambridge, Mass: Harvard University Press; 1981. Hospital Costs and Health Insurance. [Google Scholar]
- Feldstein Martin S. The Rising Cost of Hospital Care. Washington, D.C.: Informatin Resources Press; 1971. [Google Scholar]
- Feldstein P. A Review of Productivity in Dentistry. In: Rafferty J, editor. Health Manpower and Productivity. Lexington, Mass: D.C. Heath; 1974. [Google Scholar]
- Feldstein Paul. Health Associations and the Demand for Legislation: The Political Economy of Health. Lexington Mass: Ballinger Publishing Co.; 1977. [Google Scholar]
- Fetter RB, Shin Youngsoo, Freeman Jean L, et al. Case Mix Definition by Diagnosis-Related Groups. Medical Care. 1980 Feb;(Supplement) [PubMed] [Google Scholar]
- Fisher Charles R. Differences by Age Groups in Health Care Spending. Health Care Financing Review. 1980;1(4):65–90. [PMC free article] [PubMed] [Google Scholar]
- Fisher Charles R, Schendler Carol Ellen. National Nursing Home Input Price Index. Division of National Cost Estimates, Office of Financial and Actuarial Analysis, Health Care Financing Administration. 1980 Nov; unpublished. [Google Scholar]
- Freeland Mark S, Anderson Gerard, Schendier Carol Ellen. National Hospital Input Price Index. Health Care Financing Review. 1979;1(1):37–61. [PMC free article] [PubMed] [Google Scholar]
- Freeland Mark S, Schendler Carol Ellen, Anderson Gerard. Regional Hospital Input Price Indexes. Health Care Financing Review. 1981;3(2):25–48. [PMC free article] [PubMed] [Google Scholar]
- Friedman Brian L. Productivity Gains in the Drugstore Industry, 1958-79. Monthly Labor Review. 1980 Nov;:18–22. [Google Scholar]
- Friedman Milton. A Theory of the Consumption Function. Princeton, N.J.: Princeton University Press; 1957. [Google Scholar]
- Fuchs Victor R, Kramer Marcia J. Determinants of Expenditures for Physician Services in the United States, 1948-68. Dec, 1972. DHEW Publication No. (HSM) 73-30. [Google Scholar]
- Gibson Robert M, Waldo Daniel R. National Health Expenditures, 1981. Health Care Financing Review. 1982;4(Number 1):1–35. [PMC free article] [PubMed] [Google Scholar]
- Ginsburg DH. Medical Care Services in the Consumer Price Index. Monthly Labor Review. 1978 Aug;:35–39. [PubMed] [Google Scholar]
- Goldsmith Jeff C. Can Hospitals Survive? The New Competitive Health Care Market. Homewood, Illinois: Dow Jones-Irwin; 1981. [Google Scholar]
- Graduate Medical Education National Advisory Committee (GMENAC) Report of Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services. Sept. 1980. [Google Scholar]
- Greenspan Nancy T. A Descriptive Analysis of Medical Malpractice Insurance Premiums, 1974-1977. Health Care Financing Review. 1979;1(2):65–71. [PMC free article] [PubMed] [Google Scholar]
- Greenspan Nancy T, Vogel Ronald J. Taxation and Its Effect Upon Public and Private Health Insurance and Medical Demand. Health Care Financing Review. 1980;1(4):39–45. [PMC free article] [PubMed] [Google Scholar]
- Grimaldi Paul L, Micheletti Julie A. DRGs: A Practitioner's Guide. Chicago, Illinois: Pluribus; 1982. [Google Scholar]
- Grimaldi Paul L. Inflation Factors and Nursing Home Reimbursement. Long Term Care and Health Services Administration Quarterly. 1980 Spring;:16–28. [PubMed] [Google Scholar]
- Havighurst Clark. Deregulating the Health Care Industry: Planning for Competition. Cambridge, Mass: Ballinger Publishing Co.; 1982. [Google Scholar]
- Hays Robert D. Differential Organizational Patterns of Blue Cross-Blue Shield and Commercial Insurers for Competition in the Market for Group Health Insurance. Nashville: Vanderbilt University Press; 1982. [Google Scholar]
- Health Care Financing Administration. Health Care Financing Trends. Fall. 1979. various quarterly issues, beginning. [Google Scholar]
- Health Care Financing Administration. HCFA Legislative Summary. Office of Legislation and Policy; Sep 13, 1982. Tax Equity and Fiscal Responsibility Act of 1982 (P.L 97-248) [Google Scholar]
- Hellinger Fred J. Substitutability Among Different Types of Care Under Medicare. Health Services Research. 1977 Spring;:11–18. [PMC free article] [PubMed] [Google Scholar]
- Henderson Sharon R. The Malpractice Insurance Situation and Its Effects on Medical Practice. In: Gaffney John C., editor. Profile of Medical Practice, 1978. Revised Edition. American Medical Association; 1979. pp. 3–16. [Google Scholar]
- Hendrickson Robert M. Hard Times Ahead for Physicians. American Medical News. 1980 Jul 25; [PubMed] [Google Scholar]
- Hernandez Michael D, Valimahomed Salim A. The Capital Formation Environment of the 1980's. In: Jaeger B Jon., editor. Hospital Corporate Planning. Durham, N.C.: Department of Health Administration, Duke University; 1981. pp. 107–120. National Forum on Hospital and Health Affairs. [PubMed] [Google Scholar]
- Interindustry Economics Division, Bureau of Economic Analysis. The Detailed Input-Output Structure of the US Economy: 1972. I and II. U.S. Department of Commerce; 1979. [Google Scholar]
- Janssen Theodore J, Saffran G Theodore. Reimbursement for Durable Medical Equipment. Health Care Financing Review. 1981;2(3):85–96. [PMC free article] [PubMed] [Google Scholar]
- Katona George. Psychological Economics. New York: Elsevier; 1975. [Google Scholar]
- Kelling RS, Jr, Williams Paul C. Health Care Capital: Competition and Control. Cambridge, Mass: Ballinger Publishing Co.; 1978. The Projected Response of the Capital Markets to Health Facilities Expenditures; pp. 319–347. [Google Scholar]
- Laboratory Management. National Survey of Hospital and Non-Hospital Clinical Laboratories. Laboratory Management. 1979 Mar;:34–48. [Google Scholar]
- Langberg Robert, Maloy William A. The Aging Veteran: Statistical Analyses at the Veterans Administration. Paper presented at the American Statistical Association meetings in Cincinnati; Ohio. Aug, 1982. [Google Scholar]
- Lawson James C. Firms Hiking Health Plan Deductibles: Study. Business Insurance. 1982 Oct 11;:3. [PubMed] [Google Scholar]
- Lewis John P, Turner Robert C. Business Conditions Analysis. McGraw-Hill: 1967. [Google Scholar]
- Lightle Mary Alice, Plomann Marilyn P. Hospital Capital Financing Entering Phase Four. Hospitals. 1981 Aug 1;:61–63. [PubMed] [Google Scholar]
- Magnet Myron. The Scramble for the Next Superdrug. Fortune. 1981 Oct 19;:94–112. [Google Scholar]
- Maital Shlomo. Minds, Markets and Money: Psychological Foundations of Economic Behavior. New York: Basic Books, Inc.; 1982. [Google Scholar]
- Marsh Robert E. Income and Resources of the Elderly in 1978. Social Security Bulletin. 1981 Dec;:3–11. [PubMed] [Google Scholar]
- Mclntyre Leo. 1982 US Industrial Outlook for 200 Industries with Outlook for 1985. U.S. Department of Commerce, Bureau of Industrial Economics; Jan, 1982. Drugs; pp. 165–172. [Google Scholar]
- McNees Stephen K. The Recent Record of Thirteen Forecasters. New England Economic Review. 1981 Sep-Oct;:5–21. [Google Scholar]
- Medicus Systems. A Review and Evaluation of Health Manpower Productivity. Washington, D.C.: 1980. [Google Scholar]
- Millenson Leslie Joan. Increasing Demand for Dental Care: Motivating New Behavior. General Dentistry. 1980 Sep-Oct;:20–38. [Google Scholar]
- Mushkin Selma J, Smelker Mary, Wyss David, et al. Cost of Disease and Illness in the United States in the Year 2000. Public Health Reports. 1978 Sep-Oct;:493–588. [PMC free article] [PubMed] [Google Scholar]
- National Commission on the Cost of Medical Care. I and II. Chicago: American Medical Association; 1978. [Google Scholar]
- Newhouse Joseph P. The Erosion of the Medical Market Place. Dec, 1978. Rand Corporation, R-2141-1-HEW. [Google Scholar]
- Newhouse Joseph P, Phelps Charles E. New Estimates of Price and Income Elasticities. In: Rosett Richard., editor. The Role of Health Insurance in the Health Services Sector. New York: National Bureau of Economic Research; 1976. [Google Scholar]
- Newhouse Joseph P, Manning Willard G, Morris Carl N, et al. Some Interim Results from A Controlled Trail of Cost Sharing in Health Insurance. New England Journal of Medicine. 1981 Dec 17;:1501–1507. doi: 10.1056/NEJM198112173052504. [DOI] [PubMed] [Google Scholar]
- Office of Technology Assessment. Congress of the United States. The Implications of Cost-Effectiveness Analysis of Medical Technology. Washington, D.C.: Aug, 1980. [Google Scholar]
- Okun Arthur M. Prices and Quantities: A Macroeconomic Analysis. Washington, D.C.: Brookings Institution; 1981. [Google Scholar]
- Olson Lawrence, Caton Christopher, Duffy Martin. The Elderly and the Future Economy. D.C. Heath and Company; 1981. [Google Scholar]
- Pauly Mark V. Chicago: University of Chicago Press; 1980. Doctors and Their Workshops. [Google Scholar]
- Pauly Mark, Redisch Michael. The Not-for-Profit Hospital as a Physicians' Cooperative. American Economic Review. 1973 Mar;:87–99. [Google Scholar]
- Pechman Joseph A., editor. Setting National Priorities, the 1983 Budget. Washington, D.C.: Brookings; 1982. [Google Scholar]
- Perspective. Perspective. The Blue Cross and Blue Shield Magazine; Fall. 1982. GNP/Health: Can America Determine Their Appropriate Relationship? pp. 1–12. [Google Scholar]
- Pettengill J, Vertrees J. New Uses for Old Data: A Medicare Hospital Case Mix Index. New Challenges for Vital and Health Records; proceedings of the 18th National Meeting of the Public Health Conference on Records and Statistics; Washington, D.C.. 1980. U.S. Department of Health and Human Services, National Center for Health Statistics, Publication No (PHS) 81-1214. [Google Scholar]
- Phillips George. Capital Outlook: Some Encouragement, Much Concern, Many Changes. Hospitals. 1982 Apr 16;:69–71. [PubMed] [Google Scholar]
- Porter Michael E. Competitive Strategy: Techniques for Analyzing Industries and Competitors. New York: The Free Press; 1980. [Google Scholar]
- Ramsey James, Wascow Bernard. A Re-evaluation of Supply and Demand Concepts in Physician Care. Washington, D.C.: Health Resources Administration; 1981. DHPA Report No. 81-8. [Google Scholar]
- Redisch Michael A. Physician Involvement in Hospital Decision Making. In: Zubkoff M, Raskin I, Hanft R, editors. Hospital Cost Containment: Selected Notes for Future Policy. New York: Milbank Memorial Fund, PRODIST; 1978. pp. 217–243. [Google Scholar]
- Reinhardt U. Comment on ‘Competition Among Physicians’. In: Greenberg W, editor. Competition in the Health Care Sector: Past, Present, and Future. Bureau of Economics, Federal Trade Commission; Mar, 1978. pp. 156–190. [Google Scholar]
- Ricardo-Campbell Rita. The Economics and Politics of Health. Chapel Hill, N.C.: University of North Carolina Press; 1982. [Google Scholar]
- Rottenberg Simon., editor. The Economics of Medical Malpractice. American Enterprise Institute for Public Policy Research; Washington, D.C.: 1978. [Google Scholar]
- Russell Louise B. An Aging Population and the Use of Medical Care. Medical Care. 1981 Jun;:633–643. doi: 10.1097/00005650-198106000-00006. [DOI] [PubMed] [Google Scholar]
- Russell Louise, B. The Impact of the Extended Care Facility Benefit on Hospital Use and Reimbursement Under Medicare. Journal of Human Resources. 1973 Winter; [Google Scholar]
- Scanlon William J. Aspects of the Nursing Home Market Private Demand, Total Utilization and Investment. Washington, D.C.: The Urban Institute; 1978. [Google Scholar]
- Scheffler Richard M, Yoder Sunny G, Weisfeld Neil, Ruby Gloria. Physicians and New Health Practitioners: Issues for the 1980's. Inquiry. 1979 Fall;:195–229. [PubMed] [Google Scholar]
- Scitovsky Tibor. The Joyless Economy. New York: Oxford University Press; 1976. [Google Scholar]
- Scholen Ken, Chen Yung-Ping. Unlocking Home Equity for the Elderly. Cambridge, Mass: Ballinger; 1980. [Google Scholar]
- Showstack Jonathan, Blumberg Bart, Schwartz Judy, Schroeder Steven A. Fee-for-Service Physician Payment: Analysis of Current Methods, and Their Development. Inquiry. 1979 Fall;:230–246. [PubMed] [Google Scholar]
- Sloan Frank, Steinwald Bruce. The Role of Health Insurance in the Physician Services Market. Inquiry. 1975 Dec;:275–299. [PubMed] [Google Scholar]
- Smith David Barton. Long-Term Care in Transition: The Regulation of Nursing Homes. Ann Arbor, Mich: Health Administration Press; 1981. [Google Scholar]
- Sobaski WJ, Scitovsky A, McCall N. Health Policy Program Discussion Paper. San Francisco: University of California; 1975. The 1969 California Relative Value Studies and Costs of Physician Office Visits: Two Studies. [Google Scholar]
- Statistical Information Services Branch. Health Care Spending Bulletin. Office of Statistics and Data Management, Bureau of Data Management and Strategy, Health Care Financing Administration; Apr, 1982. Health Facilities Participating in HCFA Programs, 1982. [Google Scholar]
- Ting Harold M, Valiante John D. Future Capital Needs of Community Hospitals. Health Affairs. 1982 Summer;:14–27. doi: 10.1377/hlthaff.1.3.14. [DOI] [PubMed] [Google Scholar]
- Torrey Barbara Boyle. Guns vs. Canes: The Fiscal Implications of an Aging Population. American Economic Review. 1982 May;:309–313. [Google Scholar]
- Torrey Barbara Boyle. Technical Details on the Projection of Federal Outlays for the Older Population. Washington: Office of Management and Budget; 1981. [Google Scholar]
- Trapnell Gordon R. A Comparison of the Cost of Major National Health Insurance Proposals. National Technical Information Service; 1976. [Google Scholar]
- Trapnell Gordon R. National Health Insurance Issues: The Cost of a National Prescription Program. Roche Laboratories; 1979. [Google Scholar]
- Trapnell Gordon R, Chang YL, King EC, et al. Develop An Actuarial Model for Medicaid Cost Estimating: Final Report. Actuarial Research Corporation; Falls Church, VA: Apr 18, 1982. [Google Scholar]
- Veterans Administration. Medical and Construction Appropriations and Funds, Fiscal Year 1983. 1982 Feb;II of IV [Google Scholar]
- Vogel Ronald J, Blair Roger D. Health Insurance Administrative Costs. Social Security Administration; Oct, 1975. Office of Research and Statistics Staff Paper No. 21. [Google Scholar]
- Waldman Barry H. The Reaction of the Dental Profession to Changes in the 1970s. American Journal of Public Health. 1980 Jun;:619–624. doi: 10.2105/ajph.70.6.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner Kenneth E, Luce Bryan R. Cost-Benefit and Cost-Effectiveness Analysis in Health Care: Principles, Practice, and Potential. Ann Arbor, Mich: Health Administration Press; 1982. [Google Scholar]