Abstract
This article presents a detailed account of the incidence, prevalence, and survival experience of people with end-stage renal disease (ESRD) covered by Medicare. The number of new entrants into the ESRD program has risen since its inception. This increase is greatest for people whose cause of renal failure is primary hypertensive disease or diabetic nephropathy. The program incidence rates for black people is 2.8 times that of white people. Incidence is highest for persons 65 to 69 years of age. Total patient survival is 44 percent 5 years after renal failure onset. Total Medicare enrollment for ESRD quadrupled between the years 1974 and 1981.
Introduction
End-stage renal disease (ESRD) is the generic term used to describe a wide variety of diseases, trauma, and the like that result in the terminal failure of the kidneys to function sufficiently well to maintain an individual free of uremic symptoms. However, the body adapts to renal insufficiency exceptionally well. Fairly good health can be maintained despite the loss of 75 percent of the functioning capacity of the kidneys, which is typically described in terms of the filtration rate. Late chronic renal failure is said to occur when filtration approaches 10 percent of normal and end-stage renal failure becomes terminal, or life threatening, when filtration falls to about 5 percent of normal.
There are two basic treatments available to persons with end-stage renal disease, transplantation and dialysis. Transplantation dates back to 1956 when the first successful transplant was performed on identical twins. Successful transplants of kidneys from cadavers dates to the early 1960's. In 1982 there were over 5,300 kidney transplantations performed in the United States (HCFA, 1983). Of these, approximately 70 percent were transplants of kidneys from cadavers and 30 percent were from live, related donors. A successful kidney transplant relieves the patient of the necessity of dialysis and usually improves the quality of life, though for recipients of transplants from cadavers, it has not been shown that it improves length of life. However, the patient has a functioning kidney and is essentially free of maintenance renal therapy.
The second treatment available to ESRD patients is dialysis; hemodialysis is the most common form. It involves the circulation of the body's blood through a machine that cleans the blood of toxins. The first artificial kidney machine was developed in the early 1940's in Holland. The early machines could not maintain life for long because repeated treatments were not possible due to the lack of a means of repeatedly gaining access to the circulation. This problem was partially solved in 1960 when a subcutaneous cannulae-and-shunt apparatus was developed that permited the repeated access of patients to hemodialysis on a more or less permanent basis. Maintenance hemodialysis as a viable treatment for ESRD patients can be traced from this time. A typical hemodialysis patient will dialyze three times a week for about 4 hours per session. About 87 percent of current dialysis patients are on hemodialysis, either at a dialysis facility or at home (HCFA, 1983).
Another major form of dialysis is peritoneal dialysis. In this form, a dialysate solution is introduced into the peritoneal cavity. Osmatic pressure causes body wastes to pass from the bloodstream into the dialysate. After a time the dialysate solution containing the wastes is drained. Intermittent peritoneal dialysis (IPD) is done four times a week for a 10-hour period. A newer form of peritoneal dialysis is continuous ambulatory peritoneal dialysis (CAPD). Rather than use frequent exchanges of fluids over relatively brief interludes as in IPD, CAPD patients always have fluid present in their peritoneal cavity and use only four to five exchanges of fluid per day.
CAPD patients are home patients, that is, they do not have to travel to an ESRD facility for treatment. As such, CAPD allows the patient greater freedom of mobility than patients on hemodialysis and is a rapidly growing treatment modality. In 1979, CAPD was just starting to be used with a few patients. It has since grown by about 2,000 persons a year. Currently, about 7,500 patients are dialyzing by this method.
Determination of appropriate treatment therapy for ESRD patients is a complex process involving the patient's age, primary cause of renal failure, co-morbid conditions, and family support structure, as well as patient and physician preferences.
With the enactment of the Social Security Amendments of 1972 (Public Law 92-603, Sec. 299I), Congress extended Medicare coverage to most of the people suffering from ESRD. Coverage began on July 1, 1973. Since that time, there has been one major change to the program, the End-Stage Renal Disease Program Amendment of 1978 (Public Law 95-292). This amendment was designed to promote efficiency and economy in the delivery of services by encouraging home dialysis and transplantation for the maximum number of suitable patients. Changes implemented through this amendment included extension of eligibility from 1 to 3 years post-transplantation, increased coverage of kidney acquisition costs, 100-percent reimbursement for home dialysis equipment, and expanded coverage of home dialysis supplies.
Since the implementation of the original ESRD law, the program has experienced rapid growth both in the population served and in program costs. In 1974, Medicare expenditures for the 16,000 persons covered under the program were $250 million. By 1979, costs had risen to $1 billion and enrollment to 51,000. The 1982 expenditures are expected to be $1.8 billion and by 1986, costs are projected to reach $2.8 billion (HCFA, 1983).
This study provides a comprehensive description of the ESRD program from 1974 through 1979, focusing on the characteristics of the patient population. A wide array of tabulations have been generated to analyze changes in incidence and prevalence of ESRD, as well as variations in these measures by basic demographic characteristics (age, sex, and race) and by geographic area. Additional analyses focus on the primary diagnosis leading to renal failure, how these have changed over time, and variations in diagnoses by age, sex, and race. A second area of analysis examines the survival experience of the ESRD population during the initial years of the program. Finally, the implications of current incidence rates are explored by modeling the potential growth of the program.
Research on end-stage renal disease
Incidence and prevalence
There has been considerable effort devoted to determining the demographic factors that affect incidence and prevalence of ESRD. Race has been shown to be an important correlate of incidence (Wineman, 1981; Hiatt and Friedman, 1982; Mausner et al., 1978; Rostand et al., 1982: Relman, 1982; Esterling, 1977). The estimates of the overall ratio between incidence rates for black people and incidence rates for white people range from 3.2 (Hiatt and Friedman, 1982) to 4.2 (Rostand et al., 1982). Less well-publicized, but still apparent in the renal incidence literature, is the importance of sex as a determinant of renal failure (Hiatt and Friedman, 1982; Mausner et al., 1978; Rostand et al., 1982). The effect is not as large as is the case with race. Nevertheless, the reported incidence rates for males are between 30 percent to 40 percent higher than for females. Finally, age has been shown to be a critical factor in the studies of renal failure incidence rates (Hiatt and Friedman, 1982;Mausner et al., 1978; Rostand et al., 1982). Estimated rates per million range from under 10 for the population 0-14 years of age to 150 or even higher for the aged population (Hiatt and Friedman, 1982;Mausner et al., 1978; Rostand et al., 1982).
The United States has one of the highest rates in the world for treatment of people with ESRD. In a comparison of European and U.S. experience, Prottas et al. (1983) examined some of the reasons for national differences in the rate of dialysis treatment. The authors found that dialysis prevalence rates in 17 Western European Nations ranged from 31 per million to 144 per million. The U.S. rate was 209 per million (all rates were based on 1978 data). However, the authors estimate that about half the difference between U.S. and European rates can be attributed to racial differences. Black people, with the highest rates of renal failure, comprise a very small part of European populations. Many of the remaining differences can be attributed to eligibility restrictions in most European Nations that limit access to dialysis for the elderly and patients with significant medical complications. The United States has, essentially, no restrictions for access based on age or medical criteria.
Even within the United States there appears to be significant variation in the treatment of renal failure. Relman and Rennie (1980) examined State variation in dialysis prevalence, using the 1979 ESRD Facilities Survey Report. The authors found rates ranging from a low of 20 per million in Wyoming to a high of 383 per million in Hawaii. The authors concluded that, “Eight years after the enactment of a Federal law providing universal entitlement to treatment of ESRD, we find an extraordinary variation in the law's application.”
Readers quickly pointed out that there are many possible explanations for the seemingly unjustified variations in dialysis rates (Held et al., 1981; Evans and Blagg, 1981; Lowrie, 1981; Velez and Charlton, 1981; Lemann, 1981). Among the explanations suggested are racial composition, age composition, urbanization, physician supply, and per capita income. Analyses were presented indicating that indeed many of these variables did correlate with dialysis rates. There are other limitations in the data available to Relman and Rennie that were not addressed by the initial critics. First, the analysis centered on prevalence rather thn incidence. Thus, differences between States could be due in part to the maturity of the State program, as well as different rates of transplantation, patient survival, and patient movement after onset of renal failure. For instance, patients may well move to a new State if that State provides better coverage for the costs of treatment not covered by Medicare. For these reasons, the number of dialysis patients per million people in a State is an inaccurate measure of the rate of renal failure. Rather, the rate of newly treated cases each year, termed “incidence” in this article, is a more direct measure of the rate of renal failure.
Second, the Facilities Survey Report used by Relman and Rennie gives the number of patients with ESRD by place of dialysis rather than place of residence. Thus, the numerator (patients receiving dialysis within a State) is not precisely related to the denominator (people living in a State). The rate reported for the District of Columbia appears strikingly high when, in fact, many of the patients dialyzing there live in Maryland or Virginia.
Third, the incidence rate of renal failure is so low that a difference of a few cases from one year to the next can greatly affect the rate in a small State.
A final issue relates to medical practice. Apparently, there is considerable professional uncertainty about the efficacy of dialyzing elderly patients (those 65 years of age and over). This uncertainty could result in differences in medical practice that should not be construed as “good” or “bad.” However, such differences in practice could result in differing dialysis rates.
The present study addresses many of the issues raised by earlier analyses of incidence and prevalence. Detailed age, sex, and race incidence rates are calculated that indicate, much more precisely than was possible in other studies, the interrelationships of demographic factors in explaining variations in treatment of renal failure. Diagnostic-specific incidence rates are also provided that demonstrate the changes taking place in patient mix, as well as the age, sex, and race variations in causes of renal failure. Finally, an analysis is provided that examines State variations in treatment of renal failure, controlling for variables not available in earlier efforts.
Survival
Patient survival for the Medicare ESRD population is published each year in the ESRD annual report to Congress. These analyses, calculated by the National Cancer Institute, using HCFA's Medical Information System (MIS) data base, provide basic age, sex, and race variations in patient survival. The most recent analyses (HCFA, 1983) show that 81 percent of patients on dialysis can be expected to survive 1 year after onset of renal failure; 57 percent survive for 3 years, and patient survival at the end of 5 years is 38 percent. The analyses in the present study expand on the ESRD annual report by examining patient survival by primary diagnosis and by analyzing changes that may have occurred in patient survival since the program's inception.
Program data on survival of transplant patients has always been limited by the fact that patients with functioning grafts lose entitlement after 3 years. After losing entitlement, it becomes virtually impossible for the HCFA MIS to validate survival. Consequently, patient survival on transplant is necessarily limited to 3 years post transplantation.
Since the program's inception, 3-year survival for all transplanted patients is 82 percent. A recent analysis of Medicare transplants occurring since 1977 has shown 3-year patient survival of 78 percent for transplants of kidneys from cadavers and 91 percent for live, related donor transplants (Krakauer et al., 1983). The present study does not include analysis of transplant patients.
Projections
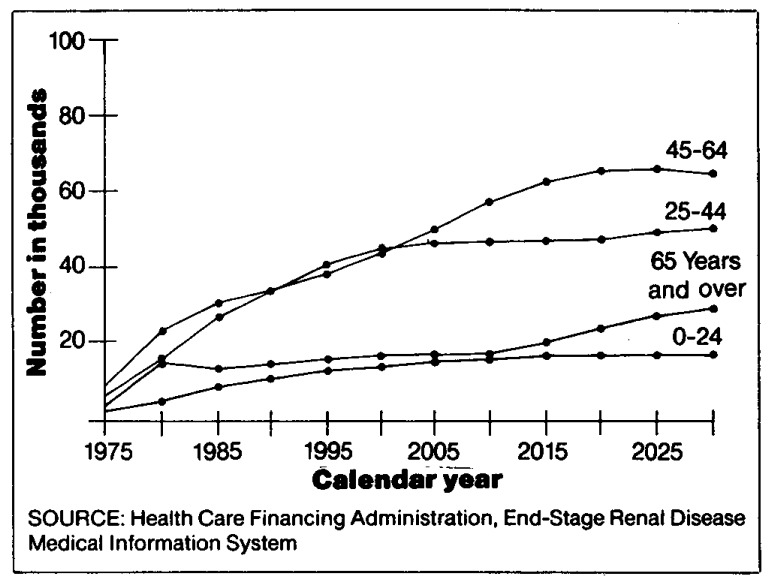
Projections as to the growth of a program such as the ESRD program are always subject to considerable error because of changes in treatment patterns, resource availability, and a myriad of unforeseen consequences. An early estimate of program growth (Klar, 1972) had the program growing to 35,000 persons within 5 years. In Congressional testimony in 1975, the Department of Health, Education, and Welfare projected a continuing growth of the program up to the range of 50,000 to 60,000 persons (Van Hoek, 1975). More recent projections reported in the literature estimate a leveling of the ESRD population at about 90,000 (Iglehart, 1982; Kolata, 1980). These figures apparently are based on estimates by HCFA's Office of the Actuary (Rettig and Marks, 1981) that project program enrollment to reach 90,000 by the year 1995. However, as long as the total population of the United States continues to grow, there should be at least a comparable growth in the ESRD program enrollment. This study projects program enrollment based on demographic changes and growth in the U.S. population.
Data sources
Data for this study were taken from two sources: the Medicare Statistical System (MSS) and the ESRD Medical Information System. The MSS is a by-product of the basic administrative data system used to determine eligibility and monitor program expenditures for the 30 million Medicare beneficiaries currently entitled to Medicare. The Master Beneficiary. Record, a part of the MSS, is used to maintain individual entitlement information and to provide the basic age, sex, race, residence, entitlement, and death information used in the analysis. From 1973 through 1979, approximately 100,000 different people were identified as Medicare beneficiaries with ESRD for some length of time. The analyses in this study are based on the universe of ESRD patients covered by Medicare during these years. Data in the MIS are taken from specific HCFA medical reporting forms; these include date of primary diagnosis and first dialysis (HCFA Form 2742), evidence of dialysis services (HCFA Form 2743), and date of transplantation (HCFA Form 600–1).
Prior to the creation of HCFA, the MIS was maintained by a private firm under contract to the Social Security Administration. In 1977, with the creation of HCFA and the centralization of ESRD functions into this single administrative unit, the data maintenance responsibilities were assumed by HCFA itself. Consequently, there has been a slight discontinuity in procedures and operation from the pre-1977 period to the post-1977 period. This does not greatly affect certain analyses, such as program enrollment and survival analyses, but it has made trends in incidence difficult to estimate. The analyses that follow take into account this discontinuity.
Results
End-stage renal disease program incidence
In this section, incidence (new cases) rates in the ESRD program are examined to determine what trends are taking place with regard to new entrants and how these trends will affect the program.1 As discussed earlier, the transition of the data system from contractor to HCFA in-house operation has resulted in a slight discontinuity between pre-1977 data and data thereafter. Therefore, the analyses in this section will highlight trends from 1978 onward.
The 3 years, 1978-80, show an increasing annual number of people with onset of renal failure and entitled to Medicare coverage (Table 1). In 1978 the Medicare program incidence was 15,584; by 1980 it had risen by 17 percent to 18,279. The largest increases occurred in the older age groups. For the groups 55-64, 65-74, and 75 years of age and over, the total increase in incidence was 21 percent, 21 percent, and 67 percent, respectively. The percent increase was identical for males and females. By race, the increase for white people was 16 percent; for black people, 19 percent; and for all other races (not black or white), 30 percent. In Table 2, the ESRD program incidence per million population is presented. Because of the growth in the U.S. population, the ESRD program incidence rate is growing somewhat more slowly than the actual number of new beneficiaries. In 1980 the overall program incidence rate was 82 per million. Incidence rose rapidly with age from 7 per million in the 0-14 years of age group to 241 per million in the 65-74 years of age group. For those 75 years of age and over, the rate dropped sharply to 153 per million. The incidence rate for males was 95 per million, or 36 percent higher than the 70 per million rate for females. White people had an incidence rate of 67 per million. The rate for black people was 2.8 times as high, at 185 per million. The rate for all other races was 140 per million, twice that of white people.2
Table 1. Medicare ESRD program incidence, by age, sex, and race: 1978-80.
| Age, sex, and race | 1978 | 1979 | 1980 | Percent change 1978-80 |
|---|---|---|---|---|
| Total | 15584 | 17243 | 18279 | 17 |
| Age | ||||
| 0-14 years | 309 | 302 | 345 | 12 |
| 15-24 years | 1076 | 1069 | 1013 | −6 |
| 25-34 years | 1793 | 1885 | 2088 | 16 |
| 35-44 years | 2076 | 2113 | 2221 | 7 |
| 45-54 years | 2789 | 3107 | 3097 | 11 |
| 55-64 years | 3580 | 4034 | 4334 | 21 |
| 65-74 years | 3096 | 3496 | 3739 | 21 |
| 75 years and over | 865 | 1237 | 1442 | 67 |
| Sex | ||||
| Male | 8755 | 9658 | 10256 | 17 |
| Female | 6829 | 7584 | 8023 | 17 |
| Race | ||||
| White | 10725 | 11568 | 12418 | 16 |
| Black | 3935 | 4593 | 4680 | 19 |
| All Other | 464 | 535 | 601 | 30 |
| Unknown | 460 | 547 | 580 | 26 |
Table 2. Medicare ESRD program incidence rates per million population, by age, sex, and race: 1978-80.
| Age, sex, and race | 1978 | 1979 | 1980 | Percent change 1978-80 |
|---|---|---|---|---|
| Total | 71 | 78 | 82 | 15 |
| Age | ||||
| 0-14 years | 6 | 6 | 7 | 17 |
| 15-24 years | 26 | 26 | 24 | −8 |
| 25-34 years | 53 | 54 | 58 | 9 |
| 35-44 years | 85 | 84 | 86 | 1 |
| 45-54 years | 120 | 135 | 136 | 13 |
| 55-64 years | 173 | 193 | 204 | 18 |
| 65-74 years | 208 | 230 | 241 | 16 |
| 75 years and over | 96 | 134 | 153 | 59 |
| Sex | ||||
| Male | 82 | 90 | 95 | 16 |
| Female | 61 | 67 | 70 | 15 |
| Race | ||||
| White | 59 | 63 | 67 | 15 |
| Black | 159 | 184 | 185 | 16 |
| All Other | 118 | 131 | 140 | 19 |
To show more clearly the relationships between age, sex, and race groups in ESRD program incidence, data for the 3 years, 1978-80, were combined; detailed age-specific incidence rates for white people and non-white people (all others) by sex, were calculated. The rates were then smoothed, using a moving average to control for minor fluctuations in rates across age groups resulting from small numbers of people.3 The results of this analysis are presented in Table 3.
Table 3. Medicare ESRD program incidence rates per million population, by age, sex, and race: 1978-80 average.
| Race | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| All persons | White | All other | |||||||
|
|
|||||||||
| Age | Total | Male | Female | Total | Male | Female | Total | Male | Female |
| Total | 77 | 89 | 66 | 63 | 74 | 52 | 169 | 186 | 154 |
| 0-4 years | 3 | 3 | 2 | 3 | 4 | 3 | 2 | 3 | 2 |
| 5-9 years | 6 | 7 | 6 | 6 | 7 | 6 | 6 | 7 | 5 |
| 10-14 years | 13 | 13 | 12 | 12 | 13 | 12 | 14 | 16 | 13 |
| 15-19 years | 21 | 23 | 19 | 19 | 21 | 17 | 30 | 32 | 27 |
| 20-24 years | 32 | 37 | 28 | 28 | 31 | 24 | 57 | 70 | 46 |
| 25-29 years | 46 | 55 | 37 | 38 | 44 | 31 | 94 | 122 | 70 |
| 30-34 years | 61 | 75 | 47 | 48 | 58 | 39 | 143 | 196 | 99 |
| 35-39 years | 76 | 95 | 58 | 59 | 72 | 46 | 196 | 266 | 138 |
| 40-44 years | 95 | 116 | 75 | 71 | 86 | 56 | 263 | 340 | 199 |
| 45-49 years | 119 | 140 | 99 | 88 | 105 | 72 | 345 | 413 | 286 |
| 50-54 years | 145 | 164 | 127 | 107 | 125 | 91 | 440 | 492 | 396 |
| 55-59 years | 174 | 197 | 153 | 130 | 153 | 109 | 547 | 586 | 514 |
| 60-64 years | 204 | 234 | 177 | 157 | 190 | 129 | 616 | 639 | 597 |
| 65-69 years | 220 | 265 | 183 | 175 | 224 | 135 | 633 | 646 | 623 |
| 70-74 years | 218 | 279 | 173 | 179 | 243 | 132 | 591 | 609 | 576 |
| 75-79 years | 183 | 256 | 136 | 154 | 228 | 107 | 496 | 532 | 469 |
| 80-84 years | 128 | 201 | 87 | 111 | 183 | 72 | 310 | 372 | 268 |
| 85 years and over | 43 | 84 | 25 | 40 | 82 | 21 | 71 | 99 | 56 |
Several important relationships become evident in this analysis. The first is the overriding importance of the effect of age on renal failure. For persons under age 10, the incidence rate is fewer than 10 per million. This incidence rate rises sharply in succeeding age groups, up to almost 100 per million in the 40-44 years of age group; this rate peaks in the 65-69 years of age group and the 70-74 years of age group at about 220 per million. After 75 years of age, the incidence drops sharply to the point where the incidence rate for persons 85 years of age and over is 43 per million. It is important to re-emphasize at this point that these are Medicare ESRD program incidence rates and thus reflect treated cases only. It is probable that the absolute rate of kidney failure continues to rise with age, but that the consensus among physicians is that dialysis will not prolong life for the oldest patients. It is likely that very few patients initiate dialysis therapy above the age of 90.
A second relationship is the effect of age on the racial differences in program incidence. Overall, non-white people have an incidence rate that is 2.7 times as great as for white people (169 and 63, respectively). This difference does not, however, appear until adulthood. From virtually no racial difference in the under 10 years of age group, the two groups diverge rapidly with increasing age. By the 20-24 years of age group, nonwhite people have twice the incidence of white people (57 and 28, respectively). The greatest racial difference is reached in the 55-59 years of age group where the rate for nonwhite people (547) is 4.2 times that of white people (130). Across the age groups of 45-64 years of age, the rate for nonwhite people is roughly four times the rate for white people. After 65 years of age the racial differences begin to lessen as both groups near the point where virtually no one initiates dialysis.
A third relationship is that between sex and race. For white and nonwhite races combined, males have incidence rates that are 35 percent higher than females. Among white people, the differential is 42 percent as compared with only 21 percent among non-white people. For white people, the difference between males and females increases with age up to the 35-39 years of age group (57 percent higher for males), at which point the difference tapers off slightly until 65 years of age. At this point, the male incidence rate increases to twice the female rate for persons 75 years of age and over. Among black people, the relative sex difference peaks in the 30-34 years of age group where the male incidence rate is roughly twice that of the female (196 per million and 99 per million, respectively). Following this, the female rate gradually approaches the male rate up to the 65-69 years of age group. Here the male rate peaks at 646 per million, which is only 4 percent higher than the female rate of 623 per million.
Some interesting issues in regard to prevention can be seen in Table 3. The age, sex, and racial variations in renal failure parallel trends in hypertension. Hypertension, defined as a systolic blood pressure of at least 160 millimeters of mercury or a diastolic blood pressure of at least 95 millimeters of mercury, has long been known to be more prevalent among black people, (Harburg, et al., 1978a; Harburg et al., 1978b; Keil et al., 1978; Tyroler and James, 1978). Recent data from the National Center for Health Statistics (Rowland and Roberts, 1982) show that the rate of hypertension among black people is 69 percent higher than among white people. Hypertension is 39 percent more prevalent among white males than white females, but among black people the rate of hypertension among females is slightly higher than among males. It is generally accepted that hypertension is a contributing causal factor in renal failure (as will be shown in the following section). Perhaps the historical discrepancies between black people and white people in access to health care (Aday et al., 1980; Dobson and Ruther, 1981; Andersen, 1980) have also contributed to the different renal failure rates. To the extent that differences between white people and black people are socially determined and not genetic in origin, vigorous preventive measures could help reduce future renal failure rates.
Geographic variation in incidence
The Medicare program incidence rates by State, averaged across the 3 years, 1978-1980, are shown in Table 4. The rates are presented for all persons and for the white population under 65 years of age.
Table 4. Medicare ESRD program 1978-80 average incidence, by State, all persons, and white persons under age 65.
| All persons | White persons under age 65 | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| State | 1978 population in thousands | Average annual ESRD incidence | ESRD incidence per million | 1978 population in thousands | Average annual ESRD incidence | ESRD Incidence per million |
| U.S. total | 220,276 | 17,035.3 | 77 | 168,088 | 8,593.7 | 51 |
| Alabama | 3742 | 362.0 | 97 | 2355 | 152.7 | 65 |
| Alaska | 403 | 10.3 | 26 | 257 | 8.0 | 31 |
| Arizona | 2354 | 210.3 | 89 | 1701 | 125.3 | 74 |
| Arkansas | 2244 | 128.3 | 57 | 1446 | 71.7 | 50 |
| California | 22294 | 1830.7 | 82 | 16529 | 935.7 | 57 |
| Colorado | 2671 | 168.3 | 63 | 2165 | 120.7 | 56 |
| Connecticut | 3099 | 217.3 | 70 | 2580 | 121.7 | 47 |
| Delaware | 583 | 48.3 | 83 | 444 | 25.3 | 57 |
| District of Columbia | 674 | 125.0 | 185 | 152 | 9.7 | 64 |
| Florida | 8594 | 921.0 | 107 | 5457 | 381.7 | 70 |
| Georgia | 5084 | 482.0 | 95 | 3256 | 178.3 | 55 |
| Hawaii | 897 | 86.7 | 97 | 307 | 17.0 | 55 |
| Idaho | 878 | 38.3 | 44 | 684 | 29.3 | 43 |
| Illinois | 11243 | 807.3 | 72 | 8585 | 402.7 | 47 |
| Indiana | 5374 | 325.3 | 61 | 4416 | 205.0 | 46 |
| Iowa | 2915 | 155.3 | 53 | 2460 | 116.0 | 47 |
| Kansas | 2348 | 118.3 | 50 | 1873 | 72.7 | 39 |
| Kentucky | 3518 | 197.7 | 56 | 2748 | 124.3 | 45 |
| Louisiana | 3966 | 326.7 | 82 | 2377 | 107.7 | 45 |
| Maine | 1091 | 46.3 | 42 | 910 | 35.3 | 39 |
| Maryland | 4143 | 315.7 | 76 | 2986 | 128.3 | 43 |
| Massachusetts | 5774 | 405.0 | 70 | 4927 | 225.3 | 46 |
| Michigan | 9189 | 627.7 | 68 | 7247 | 304.0 | 42 |
| Minnesota | 4047 | 235.3 | 58 | 3394 | 137.7 | 41 |
| Mississippi | 2404 | 195.3 | 81 | 1309 | 62.0 | 47 |
| Missouri | 4880 | 302.0 | 62 | 3716 | 166.0 | 45 |
| Montana | 785 | 36.0 | 46 | 623 | 25.3 | 41 |
| Nebraska | 1585 | 91.0 | 57 | 1288 | 64.0 | 50 |
| Nevada | 663 | 59.3 | 89 | 470 | 35.3 | 75 |
| New Hampshire | 871 | 44.0 | 51 | 703 | 30.7 | 44 |
| New Jersey | 7327 | 709.3 | 97 | 5748 | 332.7 | 58 |
| New Mexico | 1212 | 96.7 | 80 | 913 | 54.7 | 60 |
| New York | 17748 | 1457.3 | 82 | 13842 | 665.0 | 48 |
| North Carolina | 5577 | 455.3 | 82 | 3712 | 180.0 | 48 |
| North Dakota | 652 | 33.7 | 52 | 544 | 25.0 | 46 |
| Ohio | 10749 | 710.0 | 66 | 8731 | 418.7 | 48 |
| Oklahoma | 2880 | 189.0 | 66 | 2072 | 111.3 | 54 |
| Oregon | 2444 | 118.0 | 48 | 1913 | 87.7 | 46 |
| Pennsylvania | 11750 | 938.7 | 80 | 9519 | 514.0 | 54 |
| Rhode Island | 935 | 78.3 | 84 | 828 | 42.3 | 51 |
| South Carolina | 2918 | 237.7 | 81 | 1722 | 80.7 | 47 |
| South Dakota | 690 | 36.7 | 53 | 557 | 22.7 | 41 |
| Tennessee | 4358 | 305.7 | 70 | 3082 | 156.3 | 51 |
| Texas | 13092 | 1053.3 | 80 | 9326 | 540.0 | 58 |
| Utah | 1308 | 69.0 | 53 | 1039 | 53.7 | 52 |
| Vermont | 487 | 28.3 | 58 | 413 | 19.7 | 48 |
| Virginia | 5150 | 481.0 | 93 | 3591 | 193.7 | 54 |
| Washington | 3774 | 217.7 | 58 | 2945 | 149.7 | 51 |
| West Virginia | 1860 | 113.0 | 61 | 1518 | 79.0 | 52 |
| Wisconsin | 4679 | 295.7 | 63 | 3877 | 196.3 | 51 |
| Wyoming | 424 | 15.3 | 36 | 311 | 10.7 | 34 |
As shown, average yearly Medicare program incidence for all people varies from a high of 185 per million in the District of Columbia to a low of 26 per million in Alaska. The National average was 77 per million. When the analysis is limited to the white population under 65 years of age, the National rate drops to 51 per million. Several of the States and the District of Columbia show a sharp decrease in incidence when only white people 65 years of age and over are included in the calculation: for example, Georgia, Louisiana, North Carolina and the District of Columbia with their large nonwhite populations, show a great decrease. Florida, the State with the highest percentage of people over 65 years of age, had an overall program incidence rate of 107 per million; the rate for white people under 65 years of age was 70 per million.
Grouping the States together in ranges of program incidence rates per million, more clearly illustrates the impact of removing the effects of race and age on incidence rates (see Table 5). The four groups, with ranges of 50-59, 60-69, 70-79, and 80-89 per million account for 38 of the 51 States (including the District of Columbia) in total program incidence. Thirteen States fall outside of this range, including seven States with rates in excess of 90 per million. When the analysis is limited to the white population, under 65 years of age, the States group together markedly: Two intervals, 40-49 and 50-59 per million, account for forty-one of the States. It is worth noting that the two outlying States, shown in Table 4, are Alaska (31 per million) and Nevada (75 per million). If Alaska had had 7 more cases of renal failure and if Nevada had had 23 fewer cases of renal failure in the entire 3-year period, both areas would have fallen into the 40-59 per million ranges. This indicates the extent to which a few cases can markedly change incidence rates for small populations.
Table 5. Medicare ESRD program incidence rates, by distribution of States: 1978-80 average.
| Number of states | ||
|---|---|---|
|
|
||
| Rate per million | All persons | White persons, under age 65 |
| Total | 51 | 51 |
| 20-29 | 1 | 0 |
| 30-39 | 1 | 4 |
| 40-49 | 4 | 23 |
| 50-59 1 | 12 | 18 |
| 60-69 | 8 | 3 |
| 70-79 2 | 5 | 3 |
| 80-89 | 13 | 0 |
| 90-99 | 5 | 0 |
| 100 or more | 2 | 0 |
U.S. total for white persons under 65 years of age is 51 per million.
U.S. total for all persons is 77 per million.
This analysis shows, therefore, that although geographic variation does exist in the incidence of renal failure, when adjusted for age and race, it is not so marked as suggested in the Relman and Rennie study.
Incidence by diagnosis
As mentioned earlier, HCFA has required a patient history form (HCFA 2742) to be completed for each new ESRD patient. Until recently, compliance has been a major problem. Through 1980, completed forms were received by HCFA for only about one-half of the newly entitled patients. Nevertheless, it is possible to examine the primary diagnoses reported on these forms to detect trends in ESRD incidence by diagnosis. Since it is unlikely that noncompliance in submitting this form is related to causes of renal failure, the distribution found each year should, more or less, reflect the distribution of causes of renal failure in the ESRD population. Future analyses of causes of renal failure should be more accurate because the required information will be captured on the entitlement form itself. This would not apply for aged persons whose reason for Medicare entitlement (age) is unrelated to renal failure.
Since the beginning of Medicare coverage of ESRD, there has been a distinct change in the recorded primary diagnosis leading to renal failure. The distribution of primary diagnoses from 1973 and prior years through 1980 is shown in Table 6. Several trends are evident. First, glomerulonephritis has declined from 36.4 percent of all reported cases through 1973 to 19.7 percent in 1980. (Many persons whose renal failure occurred prior to 1973 became entitled in 1973; patient histories were received for many of these patients.) There has been a concomitant rise in the relative proportion of renal failure cases attributed to primary hypertensive disease and diabetic nephropathy. Primary hypertensive disease has risen from 13.2 percent of all cases to 23.4 percent; diabetic nephropathy has risen from 7.0 percent to 21.8 percent. Other notable changes among frequently reported cases include a decline in polycystic kidney disease (8.7 percent to 5.9 percent) and a decline in “other interstitial nephritis” from 12.5 percent to 6.4 percent. One interesting change has occurred in the categories “other, unspecified,” and “etiology unknown.” From 1974 through 1976, these categories each accounted for about 12 percent of all reported causes. In 1977, the first year that the MIS was made into an in-house data operation, there was a noticeable drop in these codes. The drop in “other, unspecified” has continued to the point where this category accounts for only 5.0 percent of cases in 1980. In 1977, there was also a noticeable increase in some of the less frequently reported diagnoses (for example, analgesic abuse nephropathy and the obstructuve uropathies). Whether this amounts to an improvement in data coding or merely a change in assigning causes cannot be determined in this study.
Table 6. Primary diagnosis for newly entitled ESRD persons: 1973-80.
| Diagnosis | 1973 and prior | 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 |
|---|---|---|---|---|---|---|---|---|
| Number of persons | 13,320 | 6,553 | 6,805 | 6,245 | 7,226 | 7,505 | 8,315 | 9,310 |
| Percent distribution | ||||||||
| All causes | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Glomerulonephritis | 36.4 | 29.2 | 27.1 | 24.7 | 23.5 | 21.7 | 21.0 | 19.7 |
| Primary hypertensive disease | 13.2 | 13.9 | 15.0 | 15.8 | 20.4 | 22.2 | 22.1 | 23.4 |
| Diabetic nephropathy | 7.0 | 11.9 | 12.2 | 14.0 | 15.8 | 18.0 | 18.7 | 21.8 |
| Polycystic kidney disease | 8.7 | 7.5 | 6.5 | 7.0 | 6.7 | 6.4 | 6.1 | 5.9 |
| Collagen vascular disease | 1.5 | 2.0 | 1.8 | 1.8 | 1.3 | 1.7 | 1.4 | 1.4 |
| Interstitial nephritis, hereditary | 1.5 | 1.4 | 1.0 | 1.6 | 1.2 | .7 | 1.0 | 1.0 |
| Interstitial nephritis, other | 12.5 | 10.4 | 10.0 | 9.4 | 7.2 | 6.6 | 6.7 | 6.4 |
| Analgesic abuse nephropathy | ( 1) | .1 | ( 1) | .2 | 1.0 | 1.0 | 1.2 | 1.1 |
| Obstructive uropathy, acquired | .3 | .2 | .1 | .4 | 2.2 | 2.5 | 2.5 | 2.4 |
| Obstructive uropathy, congenital | .1 | .1 | .1 | .5 | 1.5 | 1.3 | 1.5 | 1.1 |
| Amyloidosis | ( 1) | ( 1) | ( 1) | .1 | .5 | .6 | .4 | .5 |
| Multiple Myeloma | .1 | ( 1) | .1 | .1 | .8 | 1.0 | 1.0 | 1.0 |
| Gouty nephropathy | ( 1) | ( 1) | ( 1) | ( 1) | .3 | .3 | .3 | .5 |
| Other, unspecified | 9.4 | 12.5 | 13.3 | 12.1 | 7.8 | 6.5 | 6.1 | 5.0 |
| Etiology unknown | 9.0 | 11.0 | 12.8 | 12.4 | 9.6 | 9.5 | 10.1 | 8.8 |
Less than .1 percent.
Given that incidence rates are rising, merely examining the distribution of diagnoses does not present an adequate picture of the actual trends. The distribution for causes of renal failure was used to calculate diagnosis specific incidence rates in Table 7. (This assumes that the distribution of causes of renal failure among unknown cases is similar to that for reported cases. In addition, incidence rates are calculated only for 1978 onward because, as noted earlier, the shift of data management in 1977 caused certain discontinuities, particularly in incidence.) These estimated incidence rates show that, for most reported causes of renal failure, there was little change in reported incidence rates in the 3-year period 1978 through 1980. Among the more common diagnoses, glomerulonephritis rose slightly from 15 per million to 16 per million (despite the fact that glomerulonephritis continues to decline as a percentage of new cases), while both polycystic kidney disease and other interstitial nephritis remained constant at 5 per million.
Table 7. Medicare ESRD program incidence rates per million population, by primary diagnosis: 1978-80.
| Diagnosis | 1978 | 1979 | 1980 |
|---|---|---|---|
| All causes | 71 | 78 | 82 |
| Glomerulonephritis | 15 | 16 | 16 |
| Primary hypertensive disease | 16 | 17 | 19 |
| Diabetic nephropathy | 13 | 15 | 18 |
| Polycystic kidney disease | 5 | 5 | 5 |
| Collagen vascular disease | 1 | 1 | 1 |
| Interstitial nephritis, hereditary | (1) | 1 | 1 |
| Interstitial nephritis, other | 5 | 5 | 5 |
| Analgesic abuse nephropathy | 1 | 1 | 1 |
| Obstructive uropathy, acquired | 2 | 2 | 2 |
| Obstructive uropathy, congenital | 1 | 1 | 1 |
| Amyloidosis | ( 1) | ( 1) | ( 1) |
| Multiple myeloma | 1 | 1 | 1 |
| Gouty nephropathy | ( 1) | ( 1) | ( 1) |
| Other, unspecified | 5 | 5 | 4 |
| Etiology unknown | 7 | 8 | 7 |
Less than 1 per million.
The two exceptions were primary hypertensive disease and diabetic nephropathy, both of which rose markedly. Primary hypertensive disease rose from 16 per million to 19 per million, a 19-percent rise in incidence, while diabetic nephropathy rose from 13 per million to 18 per million, a 38 percent rise in incidence.
The percent distribution of the 1980 reported primary diagnosis, broken into eight age categories, is presented in Table 8. It can be seen that the distribution of diagnoses varies greatly by age group. For the youngest age group, 37 percent are coded as glomerulonephritis, followed by 20 percent unspecified, and 18 percent with obstructive uropathy, congenital. None had primary hypertensive disease and less than 1 percent had diabetic nephropathy. Among the group 25-34 years of age, the two major causes of renal failure were glomerulonephritis (31 percent) and diabetic nephropathy (31 percent). In the older age groups, primary hypertensive disease increased in importance to the point of being the number one reported cause of renal failure among people 65 years of age and over.
Table 8. Medicare ESRD program incidence, by diagnosis and age: 1980.
| Diagnosis | 0-14 years | 15-24 years | 25-34 years | 35-44 years | 45-54 years | 55-64 years | 65-74 years | 75 years and over |
|---|---|---|---|---|---|---|---|---|
| Number of persons | 137 | 472 | 1060 | 1113 | 1530 | 2126 | 2065 | 807 |
| Percent distribution | ||||||||
| All causes | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Glomerulonephritis | 37.2 | 40.0 | 30.7 | 24.0 | 17.6 | 15.2 | 14.6 | 12.6 |
| Primary hypertensive disease | 0.0 | 5.9 | 11.9 | 20.0 | 24.4 | 25.0 | 29.1 | 36.7 |
| Diabetic nephropathy | 0.7 | 5.5 | 30.8 | 28.1 | 24.3 | 25.9 | 17.4 | 10.4 |
| Polycystic kidney disease | 6.6 | 1.1 | 2.3 | 7.5 | 10.7 | 7.4 | 4.5 | 2.0 |
| Collagen vascular disease | 2.2 | 4.7 | 2.5 | 2.1 | 1.4 | 0.6 | 0.8 | 0.4 |
| Interstitial nephritis, hereditary | 2.9 | 4.4 | 2.2 | 0.9 | 0.5 | 0.7 | 0.3 | 0.4 |
| Interstitial nephritis, other | 4.4 | 8.1 | 5.1 | 4.1 | 5.6 | 6.6 | 7.1 | 9.3 |
| Analgesic abuse nephropathy | 0.0 | 0.2 | 0.1 | 1.3 | 1.2 | 1.7 | 1.3 | 0.2 |
| Obstructive uropathy, acquired | 0.7 | 1.1 | 0.7 | 0.4 | 1.4 | 2.4 | 4.2 | 5.8 |
| Obstructive uropathy, congenital | 18.2 | 9.1 | 2.0 | 0.6 | 0.1 | 0.1 | 0.1 | 0.0 |
| Amyloidosis | 0.0 | 0.0 | 0.0 | 0.4 | 0.7 | 0.7 | 0.8 | 0.5 |
| Multiple myeloma | 0.0 | 0.0 | 0.0 | 0.4 | 0.6 | 1.3 | 1.9 | 2.1 |
| Gouty nephropathy | 0.7 | 0.2 | 0.2 | 0.2 | 0.7 | 0.5 | 0.6 | 0.7 |
| Other, unspecified | 20.4 | 13.1 | 6.4 | 3.6 | 3.5 | 4.3 | 12.7 | 4.2 |
| Etiology unknown | 5.8 | 6.6 | 5.2 | 6.5 | 7.2 | 7.7 | 4.4 | 14.6 |
Diagnostic specific incidence rates by age present a slightly different perspective, as shown in Table 9. Glomerulonephritis rises steadily with age from 3 per million for persons 0-14 years of age to 35 per million for persons 65-74 years of age. Primary hypertensive disease has a similar but steeper increase, rising from 0 incidence in the youngest to a rate that is double (70 per million) that of glomerulonephritis in the group 65-74 years of age. Diabetic nephropathy tends to peak a little more to the center of the age distribution. Its highest rate appears in the 55-64 age range (53 per million), although it is the most commonly reported cause of renal failure in three age groups: 35-44, 45-54, and 55-64 years of age.
Table 9. Medicare ESRD program incidence per million population, by diagnosis and age: 1980.
| Diagnosis | 0-14 years | 15-24 years | 25-34 years | 35-44 years | 45-54 years | 55-64 years | 65-74 years | 75 years and over |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Incidence per million | ||||||||
| All causes | 7 | 24 | 58 | 86 | 136 | 204 | 241 | 153 |
| Glomerulonephritis | 3 | 10 | 18 | 21 | 24 | 31 | 35 | 19 |
| Primary hypertensive disease | 0 | 1 | 7 | 17 | 33 | 51 | 70 | 56 |
| Diabetic nephropathy | ( 1) | 1 | 18 | 24 | 33 | 53 | 42 | 16 |
| Polycystic kidney disease | ( 1) | ( 1) | 1 | 6 | 15 | 15 | 11 | 3 |
| Collagen vascular disease | ( 1) | 1 | 1 | 2 | 2 | 1 | 2 | 1 |
| Interstitial nephritis, hereditary | ( 1) | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Interstitial nephritis, other | ( 1) | 2 | 3 | 4 | 8 | 13 | 17 | 14 |
| Analgesic abuse nephropathy | 0 | ( 1) | ( 1) | 1 | 2 | 3 | 3 | ( 1) |
| Obstructive uropathy, acquired | ( 1) | ( 1) | ( 1) | ( 1) | 2 | 5 | 10 | 9 |
| Obstructive uropathy, congenital | 1 | 2 | 1 | 1 | ( 1) | ( 1) | ( 1) | 0 |
| Amyloidosis | 0 | 0 | 0 | ( 1) | 1 | 1 | 2 | 1 |
| Multiple myeloma | 0 | 0 | 0 | ( 1) | 1 | 3 | 5 | 3 |
| Gouty nephropathy | ( 1) | ( 1) | ( 1) | ( 1) | 1 | 1 | 1 | 1 |
| Other, unspecified | 1 | 3 | 4 | 3 | 5 | 9 | 31 | 6 |
| Etiology unknown | ( 1) | 2 | 3 | 6 | 10 | 16 | 11 | 22 |
Less than 1 per million.
The incidence rates in 1980 by diagnosis are shown by sex in Table 10. Overall, males had an incidence rate which was 25 per million higher than females (95 per million and 70 per million, respectively). Most of this difference can be attributed to higher rates of glomerulonephritis and primary hypertensive disease. Males were also slightly more likely to have diabetic nephropathy. In two diagnostic categories, collagen vascular disease and other interstitial nephritis, females had higher incidence rates than males.
Table 10. Medicare ESRD program incidence and percent distribution, by diagnosis and sex: 1980.
| Diagnosis | Male | Female | Male | Female |
|---|---|---|---|---|
|
| ||||
| Incidence per million | Percent distribution | |||
| All causes | 95 | 70 | 100 | 100 |
| Glomerulonephritis | 20 | 12 | 21.5 | 17.3 |
| Primary hypertensive disease | 24 | 15 | 24.9 | 21.4 |
| Diabetic nephropathy | 19 | 17 | 20.1 | 24.1 |
| Polycystic kidney disease | 5 | 5 | 5.2 | 6.8 |
| Collagen vascular disease | ( 1) | 2 | 0.5 | 2.5 |
| Interstitial nephritis, hereditary | 1 | 1 | 1.1 | 0.8 |
| Interstitial nephritis, other | 5 | 6 | 4.8 | 8.4 |
| Analgesic abuse nephropathy | 1 | 1 | 0.6 | 1.6 |
| Obstructive uropathy, acquired | 3 | 1 | 3.5 | 1.1 |
| Obstructive uropathy, congenital | 1 | ( 1) | 1.5 | 0.7 |
| Amyloidosis | ( 1) | ( 1) | 0.5 | 0.6 |
| Multiple myeloma | 1 | 1 | 1.1 | 0.9 |
| Gouty nephropathy | 1 | ( 1) | 0.6 | 0.3 |
| Other, unspecified | 5 | 4 | 5.1 | 5.0 |
| Etiology unknown | 9 | 6 | 9.0 | 8.5 |
Less than 1 per million.
The incidence rates by diagnosis by race are presented in Table 11. It is immediately evident that primary hypertensive disease is much more likely to be reported as the cause of renal failure among black people (43 percent) than among either white people (17 percent) or other races (14 percent). This should be interpreted with some caution, however. It has been suggested that there is the possibility that physicians, when faced with black renal patients who are hypertensive, are more likely to attribute the renal failure to hypertension than when faced with white hypertensive patients. Nevertheless, it appears that there are distinctly different patterns of renal failure by race. Black people have a reported rate of renal failure resulting from hypertension (79 per million) that is 6.5 times as great as for white people (12 per million) and four times as great as for all other people (20 per million). This discrepancy in hypertensive renal failure is far greater than would be predicted based on the 65 percent higher rate of hypertension among black people cited earlier (Rowland and Roberts, 1982). The reason for this is not clear. Part of it could be caused by the presumed tendency of physicians to categorize renal failure among black people as resulting from hypertension. Another possibility is that hypertension is more severe among black people and has the more severe outcome of renal failure in a greater number of cases.
Table 11. Medicare ESRD program incidence and percent distribution, by diagnosis and race: 1980.
| Diagnosis | White | Black | Other | White | Black | Other |
|---|---|---|---|---|---|---|
|
| ||||||
| Incidence per million | Percent distribution | |||||
| All causes | 67 | 185 | 140 | 100 | 100 | 100 |
| Glomerulonephritis | 14 | 26 | 32 | 21.5 | 13.8 | 22.9 |
| Primary hypertensive disease | 12 | 79 | 20 | 17.4 | 42.5 | 14.0 |
| Diabetic nephropathy | 14 | 40 | 44 | 21.5 | 21.6 | 31.2 |
| Polycystic kidney disease | 5 | 3 | 3 | 7.5 | 1.8 | 2.4 |
| Collagen vascular disease | 1 | 3 | 3 | 1.2 | 1.6 | 2.4 |
| Interstitial nephritis, hereditary | 1 | ( 1) | 0 | 1.3 | 0.2 | 0.0 |
| Interstitial nephritis, other | 5 | 7 | 9 | 7.2 | 4.0 | 6.5 |
| Analgesic abuse nephropathy | 1 | 1 | 1 | 1.2 | 0.6 | 1.0 |
| Obstructive uropathy, acquired | 2 | 2 | 4 | 2.8 | 1.3 | 3.1 |
| Obstructive uropathy, congenital | 1 | ( 1) | ( 1) | 1.5 | 0.2 | 0.3 |
| Amyloidosis | ( 1) | ( 1) | ( 1) | 0.7 | 0.2 | 0.3 |
| Multiple myeloma | 1 | 1 | 0 | 1.3 | 0.5 | 0.0 |
| Gouty nephropathy | ( 1) | 1 | 0 | 0.5 | 0.4 | 0.3 |
| Other, unspecified | 4 | 5 | 8 | 5.8 | 2.7 | 5.5 |
| Etiology unknown | 6 | 16 | 14 | 8.8 | 8.6 | 9.9 |
Less than 1 per million.
The strong race relationships for glomerulonephritis and diabetic nephropathy are also shown in Table 11. Glomerulonephritis as a cause of renal failure is nearly twice as common among black people (26 per million) than among white people (14 per million), and the rate among all other people is 2.3 times that of the rate for white people. For diabetic nephropathy, the rate among black people and other races (nonwhite) is approximately three times the rate among white people. As with hypertension, the racial differences in incidence for diabetic nephropathy is in the expected direction, but is of a greater magnitude than would have been predicted by rates of diabetes alone. The rate of diabetes among black people is 50 percent greater than among white people, and other races have a rate that is 69 percent greater than the rate for white people (National Center Health Statistics, 1979).
End-stage renal disease program survival analyses
This section describes the program experience with respect to patient survival from onset of renal failure. The analysis covers the period from July 1973 through December 1979, a 6 ½ -year time period. All persons with renal failure occurring after June 30, 1973, and before January 1, 1980, who were Medicare entitled and never received a transplant, were included in the analysis. The total number of persons included in the computation of survival rates was 74,547.
Survival rates were calculated using a standard modified life-table analysis (Cutler and Ederer, 1958). For each interval (each successive year following renal onset), the number of deaths occurring during the interval was divided by the number of persons exposed to risk to obtain the survival rate. The cumulative survival rate is simply the product of successive yearly survival rates.
These survival analyses are limited to the patients treated by dialysis only; transplant patients have been deleted from the analyses since they lose their entitlement to Medicare benefits after 3 years if their grafts continue to function. Thus, it has been virtually impossible to track these patients for more than 3 years post-transplant. Therefore, it was decided to emphasize the dialysis population, the group for whom survival can be estimated over the long term. One limitation to this analysis is the many unidentified transplant patients, who could not be identified as such because of the under-reporting of the transplantation form (HCFA 600-1). Since patients receiving transplants have higher survival rates than dialysis patients, these analyses will be biased upward to some extent (that is, estimates of patient survival will be higher than the true survival on dialysis). A sensitivity analysis was performed and showed that the effect of the inclusion of unidentified transplant patients in the calculation of dialysis survival rates could bias results upward by 1 or 2 percent for the groups under 55 years of age. There is essentially no bias in the older age groups because these patients so rarely receive transplants.
The results of the survival analysis for all Medicare persons with ESRD on dialysis are presented in Table 12. Eighty-one percent of all persons survived for 1 year after onset of kidney failure. The probability of survival shows a slight upward trend with each succeeding year of survival. For example, for persons who have survived 2 years, the probability of surviving an additional year is 85 percent; for those surviving 5 years, the probability of surviving through the sixth year is 89 percent.
Table 12. Year-to-year survival of Medicare ESRD dialysis patients, by age at renal failure onset during period 1973-79.
| Age at onset | Number of persons 1 | Year from onset | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
|
| |||||||
| Percent surviving from previous year | |||||||
| All persons | 74,547 | 81 | 83 | 85 | 88 | 88 | 89 |
| 0-14 years | 827 | 84 | 88 | 91 | 93 | 97 | 95 |
| 15-24 years | 3,638 | 88 | 90 | 91 | 93 | 96 | 95 |
| 25-34 years | 6,833 | 86 | 86 | 89 | 91 | 93 | 93 |
| 35-44 years | 9,179 | 86 | 85 | 88 | 91 | 91 | 91 |
| 45-54 years | 15,409 | 85 | 85 | 86 | 87 | 85 | 89 |
| 55-64 years | 19,897 | 83 | 82 | 84 | 84 | 85 | 88 |
| 65-74 years | 14,273 | 74 | 77 | 79 | 82 | 81 | 83 |
| 75 years and over | 4,491 | 64 | 72 | 72 | 82 | 81 | 91 |
The number of persons is the number of persons at risk at the beginning of the first year. Subsequent years are based on smaller numbers of cases.
One of the strongest determinants of survival among ESRD Medicare beneficiaries is the age of the beneficiary at renal onset. For the youngest group (0-14 years of age), first-year survival is 84 percent. Second-year survival rises to 88 percent, and survival in subsequent years is greater than 90 percent. Survival is highest for the group 15-24 years of age. Eighty-eight percent survive the first year, and survival in subsequent years is over 90 percent. Patients in the next three age groups (25-34, 35-44, and 45-54 years of age) have year-to-year survival rates that start in the mid-80 percent range and improve in later years to about 90 percent. Survival is lowest for the oldest age groups. Persons 65-74 years of age have a first-year survival of 74 percent. This improves to slightly more than 80 percent by the fourth year. Similarly, the oldest group (75 years of age and over) experience a 64-percent survival in the first year, which improves to more than 80 percent by the fourth year.
The cumulative effect of yearly survival rates is presented in Table 13. The net effect of the yearly survival rates is a rapidly declining cohort. About two-thirds (67 percent) of all patients can be expected to live for 2 years after the onset of renal failure. Fifty percent will survive for 4 years and, by the end of 6 ½ years, only 37 percent of ESRD beneficiaries can be expected to live.
Table 13. Cumulative survival rates of Medicare ESRD dialysis patients, by age at renal failure onset: 1973-79.
| Age at onset | Number of persons 1 | Year from renal failure onset | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 6½ | ||
|
| ||||||||
| Percent surviving | ||||||||
| All persons | 74,547 | 81 (.1) |
67 (.2) |
57 (.2) |
50 (.2) |
44 (.3) |
39 (.3) |
37 (.3) |
| 0-14 years | 827 | 84 (1.3) |
74 (1.7) |
67 (1.9) |
62 (2.1) |
60 (2.2) |
57 (2.5) |
57 (2.5) |
| 15-24 years | 3,638 | 88 (.5) |
79 (.7) |
72 (.9) |
67 (.9) |
64 (1.0) |
61 (1.2) |
61 (1.2) |
| 25-34 years | 6,833 | 86 (.4) |
74 (.6) |
66 (.7) |
60 (.7) |
56 (.8) |
52 (.9) |
51 (1.0) |
| 35-44 years | 9,179 | 86 (.4) |
73 (.5) |
64 (.6) |
58 (.6) |
53 (.7) |
48 (.8) |
46 (.9) |
| 45-54 years | 15,409 | 85 (.3) |
72 (.4) |
62 (.5) |
54 (.5) |
46 (.6) |
41 (.6) |
39 (.7) |
| 55-64 years | 19,897 | 83 (.3) |
68 (.4) |
57 (.4) |
48 (.5) |
41 (.5) |
36 (.6) |
33 (.6) |
| 65-74 years | 14,273 | 74 (.4) |
57 (.5) |
45 (.5) |
37 (.6) |
30 (.7) |
25 (.9) |
23 (1.1) |
| 75 years and over | 4,491 | 64 (.6) |
46 (.8) |
33 (.9) |
27 (.9) |
22 (1.5) |
20 (2.2) |
16 (3.7) |
The number of persons is the number of persons at risk at the beginning of the first year. Subsequent years are based on smaller numbers of cases.
NOTE: Standard errors are in parentheses.
At first glance, cumulative survival by age is striking. The highest survival is found in the group 15-24 years of age, where 61 percent survive for 6 ½ years. By the end of the 6 ½-year time period, 57 percent of the group 0-14 years of age can be expected to survive. This cumulative survival rate decreases steadily for the older age groups. For the group 75 years of age and over, only 16 percent can be expected to survive 6/2 years. Thus, relative to other people with ESRD, persons 0-14 and 15-24 years of age have the highest survival rates.
However, most of these differences by age are attributable to underlying age mortality, irrespective of renal disease. Relative to the death rate experienced by the total population in their age groups, the younger age groups' survival rate is much lower. In Table 14, the 5-year death rates by age for the ESRD population and for the entire U.S. population are shown. Among the general U.S. population under 35 years of age, death is a rare event. Less than one percent of people in these age groups can be expected to die over a 5-year period. By contrast, 36-44 percent of persons with ESRD in the three youngest age groups can be expected to die over a 5-year period. Thus, the excess mortality of ESRD patients in these age groups is quite high, with the mortality rate 60 to 80 times as great as for the total population of the same age. This relative mortality decreases for the older groups. Thus, while the oldest age group of ESRD beneficiaries (75 years of age and over) has a mortality rate of 78 percent during 5 years, this is three times as great as the mortality rate for all persons in this age group.
Table 14. Five-year mortality rates for the U.S. population and for Medicare ESRD dialysis patients, by age: 1973-79.
| Age | 5-year mortality | 5-year excess mortality | ||
|---|---|---|---|---|
|
|
|
|||
| Percent of total population | Percent of ESRD patients | Ratio of ESRD patients to total population | Percent difference of ESRD patients to total population | |
| 0-14 years | 0.5 | 40 | 80 | 39 |
| 15-24 years | 0.6 | 36 | 60 | 35 |
| 25-34 years | 0.7 | 44 | 63 | 43 |
| 35-44 years | 1.3 | 47 | 36 | 46 |
| 45-54 years | 3.1 | 54 | 17 | 51 |
| 55-64 years | 7.2 | 59 | 8 | 52 |
| 65-74 years | 14.8 | 70 | 5 | 55 |
| 75 years and over | 31.1 | 78 | 3 | 47 |
ESRD mortality, expressed in absolute differences from the total population rates as opposed to ratios, is also shown in Table 14. This provides a somewhat different perspective. Excess 5-year mortality for the youngest two age groups is 39 percent and 35 percent, respectively. This excess mortality increases with each advancing age group up to 65-74 years of age, at which point there is a 55 percent excess mortality for ESRD persons. Excess mortality then drops slightly for persons 75 years of age and over to about 47 percent.
The preceding analysis has shown that age at onset of renal failure has a strong effect on survival probabilities. Given this relationship, it was decided to age adjust all subsequent analyses. Survival rates for various subgroups were adjusted (by the direct method) to the age distribution of all ESRD persons (N = 74,547) included in the survival analyses.
The results of age-adjusted survival analysis by sex and by race are presented in Table 15. Females have a better survival pattern than do males. By the end of 6 ½ years, 39 percent of females with ESRD can be expected to survive as compared with 36 percent of males. This finding is consistent with the general relationship of sex to life expectancy. (Among the general population, for instance, females have a life expectancy more than 7 years greater than males, 76.7 years and 69.0 years, respectively. By 65 years of age, female life expectancy is still 4.3 years longer than males, 18.0 years and 13.7 years, respectively.) There are racial differences as well. Black people have the highest 6 ½ -year cumulative survival at 39 percent. This is followed by all other races (except white) at 38 percent and white people at 36 percent.
Table 15. Cumulative survival of Medicare ESRD dialysis patients, by sex and race, age adjusted: 1 1973-79.
| Sex and race | Number of persons 2 | Year from renal failure onset | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 6½ | ||
|
| ||||||||
| Surviving percent | ||||||||
| All persons | 74,547 | 81 (.1) |
67 (.2) |
57 (.2) |
50 (.2) |
44 (.3) |
39 (.3) |
37 (.3) |
| Sex | ||||||||
| Male | 41,827 | 82 (.2) |
67 (.3) |
57 (.3) |
49 (.3) |
43 (.3) |
38 (.4) |
36 (.4) |
| Female | 32,719 | 82 (.2) |
69 (.3) |
60 (.3) |
53 (.4) |
48 (.4) |
43 (.4) |
39 (.6) |
| Race | ||||||||
| White | 50,907 | 81 (.2) |
67 (.2) |
57 (.3) |
50 (.3) |
44 (.3) |
39 (.3) |
36 (.4) |
| Black | 19,414 | 84 (.3) |
70 (.4) |
60 (.4) |
53 (.5) |
46 (.5) |
42 (.6) |
39 (.8) |
| All Other | 2,001 | 83 (.9) |
69 (1.1) |
59 (1.3) |
51 (1.4) |
45 (1.6) |
41 (1.8) |
38 (2.4) |
| Unknown | 2,225 | 79 (.9) |
69 (1.1) |
62 (1.2) |
56 (1.4) |
52 (1.5) |
47 (1.8) |
43 (2.6) |
The rates have been adjusted to the age distribution of all ESRD beneficiaries.
The number of persons is the number of persons at risk at the beginning of the first year. Subsequent years are based on smaller numbers of cases.
NOTE: Standard errors are in parentheses.
The underlying cause of renal failure can also be a determinant of survival. In Table 16, the results of the age-adjusted survival analysis for various primary diagnoses is presented. It is apparent that the reported cause of renal failure has an impact on survival. The best survival experience is shown by persons with polycystic kidney disease, with 52 percent surviving for 6 ½ years. A number of categories group at the 40-percent range for 6 ½-year survival. These include glomerulonephritis (41 percent), primary hypertensive disease (40 percent), other interstitial nephritis (42 percent), and etiology unknown (39 percent). The worst 6 ½-year survival is experienced by persons whose reported cause of renal failure is collagen vascular disease (30 percent) and persons with diabetic nephropathy (17 percent). This analysis illustrates some of the impact a changing case mix is likely to have on the ESRD population. For instance, the rapid rise in treatment for persons whose renal failure is due to diabetic nephropathy should be accompanied by a less rapid growth in program enrollment.
Table 16. Cumulative survival of Medicare ESRD dialysis patients, by primary diagnosis, age adjusted: 1973-79 1.
| Diagnosis | Number of persons 2 | Year from renal failure onset | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 6 ½ | ||
|
| ||||||||
| Surviving percent | ||||||||
| Glomerulonephritis | 8,006 | 87 (.4) |
73 (.5) |
63 (.6) |
54 (.7) |
47 (.7) |
42 (.8) |
41 (.9) |
| Primary hypertensive disease | 6,823 | 84 (.5) |
69 (.6) |
59 (.7) |
51 (.8) |
45 (.9) |
41 (1.0) |
40 (1.3) |
| Diabetic nephropathy | 5,512 | 73 (.6) |
51 (.7) |
37 (.8) |
28 (.8) |
21 (.9) |
18 (.9) |
17 (1.3) |
| Polycystic kidney disease | 2,528 | 92 (.5) |
82 (.8) |
74 (1.0) |
65 (1.2) |
58 (1.4) |
53 (1.7) |
52 (2.1) |
| Collagen vascular disease | 601 | 78 (1.7) |
61 (2.1) |
53 (2.3) |
45 (2.5) |
37 (2.7) |
30 (3.1) |
30 (3.1) |
| Other, interstitial nephritis | 3,040 | 86 (.7) |
73 (.9) |
61 (1.0) |
53 (1.1) |
47 (1.2) |
43 (1.3) |
42 (1.4) |
| Other, unspecified | 3,410 | 77 (.8) |
61 (.8) |
50 (.9) |
43 (1.0) |
37 (1.0) |
35 (1.2) |
32 (1.5) |
| Etiology unknown | 4,114 | 85 (.6) |
71 (.8) |
60 (.9) |
52 (.9) |
46 (1.0) |
41 (1.2) |
39 (1.4) |
Survival was not calculated for diagnoses in which there were few observations or for which the age distribution was so different from the total as to make direct age adjustment impractical.
The number of persons is the number of persons at risk at the beginning of the first year. Subsequent years are based on smaller numbers of cases.
NOTE: Standard errors are in parentheses.
It is also of interest to know if the survival of ESRD beneficiaries has changed during the course of the program. In Table 17, first-year survival rates of Medicare ESRD beneficiaries is shown for each year's cohort of new patients by age at renal failure onset. It appears that the greatest progress in patient survival has occurred at the extremes of the age distribution. In 1974, there was a 78-percent survival for persons 0-14 years of age. By 1979, this had risen to 90 percent. Persons 15-24 years of age at renal failure onset had a 6-percent increase in survival, from 86 percent to 92 percent. For persons 75 years of age and over, the first year's survival increased from 52 percent in 1974 to 65 percent in 1979. These three age groups, however, account for only 12 percent of all new ESRD patients. The majority of the ESRD population did not experience a large increase in survival. The two groups of 55-64 and 65-74 years of age actually had a slight decline in first-year survival during this 6-year period. These two age groups accounted for 46 percent of all new patients during these years. The net result is that there has been little change in aggregate survival for the ESRD population. From 1974 through 1977, the first-year survival remained constant at 81 percent. First-year survival rose by 1 percent in 1978, to 82 percent, and 1 percent in 1979, to 83 percent. Future analyses will show whether this represents a trend or is a short-term deviation in the survival rate.
Table 17. Medicare ESRD dialysis patient survival, by age and year of renal failure.
| Year | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Age at renal failure | 1974 | 1975 | 1976 | 1977 | 1978 | 1979 |
| All patients | 81 (.4) |
81 (.4) |
81 (.4) |
81 (.4) |
82 (.4) |
83 (.4) |
| Percent surviving 1 year | ||||||
| 0-14 years | 78 (3.7) |
80 (4.0) |
76 (3.9) |
90 (3.3) |
89 (2.8) |
90 (2.9) |
| 15-24 years | 86 (1.5) |
89 (1.4) |
88 (1.5) |
86 (1.6) |
91 (1.3) |
92 (1.4) |
| 25-34 years | 86 (1.2) |
82 (1.3) |
85 (1.1) |
84 (1.2) |
87 (1.0) |
89 (1.1) |
| 35-44 years | 86 (1.0) |
83 (1.1) |
87 (.9) |
85 (1.0) |
86 (.9) |
90 (1.0) |
| 45-54 years | 85 (.8) |
84 (.8) |
84 (.7) |
85 (.8) |
85 (.7) |
86 (.9) |
| 55-64 years | 84 (.8) |
83 (.8) |
81 (.7) |
82 (.7) |
80 (.7) |
83 (.8) |
| 65-74 years | 74 (1.3) |
74 (1.3) |
72 (.8) |
74 (.9) |
73 (.8) |
72 (1.0) |
| 75 years and over | 52 (3.7) |
59 (3.4) |
62 (1.3) |
64 (1.8) |
64 (1.6) |
65 (1.7) |
ESRD program enrollment (prevalence)
In Table 18, the number of Medicare enrollees with ESRD (prevalence) is shown by age, sex, and race for the years 1974-81. In 1974, there were nearly 16,000 such persons entitled to Medicare. By 1981, this had risen to a little over 64,000, an increase of 300 percent, representing an annual increase of almost 22 percent. The increase has not been uniform across all groups, however. By age, the largest increases have come in the groups 25-34 and 55-64 years of age, both with annual increases of 25 percent or more. The groups 15-24 and 65 years of age and over had annual increases of a little less than 20 percent. Not much difference was found in the rate of growth for males and females, although the rate for females was slightly higher; with regard to race, the rate for the non-white (black and all other) populations grew faster than that for the white population. The differential increases have produced small changes in the composition of the ESRD population. Females have increased from 43 percent of the treated population in 1974 to 45 percent in 1981, and black people have increased from 22 percent to 25 percent.
Table 18. Medicare ESRD program enrollment, by age, sex, and race: 1974-81 1.
| Age, sex, and race | Year | Percent change | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1974-81 | Yearly average | |
| Total | 15993 | 22674 | 28941 | 34778 | 43125 | 50829 | 57818 | 64063 | 301 | 21.9 |
| Age | ||||||||||
| 0-14 years | 211 | 315 | 363 | 402 | 401 | 605 | 695 | 815 | 286 | 21.3 |
| 15-24 years | 1075 | 1543 | 1900 | 2166 | 2562 | 3146 | 3583 | 3836 | 257 | 19.9 |
| 25-34 years | 1774 | 2688 | 3387 | 4196 | 5070 | 6283 | 7345 | 8485 | 378 | 25.0 |
| 35-44 years | 2161 | 3127 | 4009 | 4787 | 5989 | 7279 | 8277 | 9248 | 328 | 23.1 |
| 45-54 years | 3069 | 4509 | 5652 | 6697 | 8103 | 9284 | 10489 | 11550 | 276 | 20.8 |
| 55-64 years | 2836 | 4394 | 5879 | 7353 | 9101 | 10742 | 12399 | 14018 | 394 | 25.6 |
| 65 years and over | 4868 | 6097 | 7751 | 9178 | 11899 | 13490 | 15030 | 16111 | 231 | 18.6 |
| Sex | ||||||||||
| Male | 9071 | 12597 | 15920 | 19063 | 23806 | 27989 | 31804 | 35168 | 288 | 21.4 |
| Female | 6921 | 10077 | 13021 | 15715 | 19316 | 22837 | 26010 | 28891 | 317 | 22.6 |
| Race | ||||||||||
| White | 11738 | 16411 | 20693 | 24620 | 30068 | 35201 | 39459 | 43266 | 269 | 20.5 |
| Black | 3560 | 5139 | 6871 | 8496 | 10834 | 12867 | 15028 | 16927 | 375 | 24.9 |
| All other | 384 | 580 | 746 | 886 | 1177 | 1432 | 1716 | 1956 | 409 | 26.2 |
| Unknown | 311 | 544 | 631 | 776 | 1046 | 1329 | 1615 | 1914 | 515 | 29.6 |
Enrollment was measured as of July 1 each year.
It is interesting to note that the increase in the covered population has not progressed at a uniform rate (see Table 19). In the year between 1974 and 1975, there was a 42-percent growth in the population. Increases in the subsequent 3 years ranged from 20 percent to 28 percent. Then, in the most recent 3 years, the rate of growth has slowed to below 20 percent, reaching a low of 11 percent in the most recent year (1980-81). This general pattern of a slowing in growth is evident across all age, sex, and race groups. The pattern of rapid growth, which gradually tapers off, is to be expected with a program such as ESRD. Before Medicare funding, when rationing of scarce dialysis resources was the rule, the ESRD population did not grow because the vast majority of ESRD patients could not get services and died. With the implementation of the program, these patients received care and lived 2, 3, 4, 5, and more years, thus increasing the population markedly. Eventually, an equilibrium point is likely to be reached in which new entrants to the program are balanced by deaths. However, as will be illustrated in the following section, the changing demographic characteristics of the U.S. population make it unlikely that an equilibrium point will be reached in the near future.
Table 19. Annual percent change in Medicare ESRD program enrollment, by age, sex, and race: 1974-81.
| Annual percent change | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Age, sex, and race | 1974-75 | 1975-76 | 1976-77 | 1977-78 | 1978-79 | 1979-80 | 1980-81 |
| Total | 41.8 | 27.6 | 20.2 | 24.0 | 17.9 | 13.8 | 10.8 |
| Age | |||||||
| 0-14 years | 49.3 | 15.2 | 10.7 | −.2 | 50.9 | 14.9 | 17.3 |
| 15-24 years | 43.5 | 23.1 | 14.0 | 18.3 | 22.8 | 13.9 | 7.1 |
| 25-34 years | 51.5 | 26.0 | 23.9 | 20.8 | 23.9 | 16.9 | 15.5 |
| 35-44 years | 44.7 | 28.2 | 19.4 | 25.1 | 21.5 | 13.7 | 11.7 |
| 45-54 years | 46.9 | 25.3 | 18.5 | 21.0 | 14.6 | 13.0 | 10.1 |
| 55-64 years | 54.9 | 33.8 | 25.1 | 23.8 | 18.0 | 15.4 | 13.1 |
| 65 years and over | 25.2 | 27.1 | 18.4 | 29.6 | 13.4 | 11.4 | 7.2 |
| Sex | |||||||
| Male | 38.9 | 26.4 | 19.7 | 24.9 | 17.6 | 13.6 | 10.6 |
| Female | 45.6 | 29.2 | 20.7 | 22.9 | 18.2 | 13.9 | 11.1 |
| Race | |||||||
| White | 39.8 | 26.1 | 19.0 | 22.1 | 17.1 | 12.1 | 9.6 |
| Black | 44.4 | 33.7 | 23.7 | 27.5 | 18.8 | 16.8 | 12.6 |
| All other | 51.0 | 28.6 | 18.8 | 32.8 | 21.7 | 19.8 | 14.0 |
| Unknown | 74.9 | 16.0 | 23.0 | 34.8 | 27.1 | 21.5 | 18.5 |
The prevalence of Medicare ESRD coverage per million population in the U.S. is shown in Table 20. Comparing the prevalence rates across demographic characteristics, one sees the importance of age as a correlate of renal failure. By 1981, in the youngest group, 0-14 years of age, only 16 persons per million population were Medicare ESRD patients. This rate jumps almost sixfold in the next age group, 15-24 years of age, to 93 per million. The rate of Medicare-covered ESRD people continues to increase with age up to the group 55-64 years of age, with over 650 Medicare ESRD beneficiaries per million population. This rate remains essentially the same for the group 65 years of age and over. Males have a prevalence rate that is 28 percent higher than females (322 per million and 251 per million, respectively). By race, it can be seen that black people have a prevalence rate of 658 per million, which is 2.9 times that of white people (231 per million). People of all other races have a prevalence rate that is 90 percent higher than white people (437 per million).
Table 20. Medicare ESRD program enrollment rates per million population, by age, sex, and race: 1974-81 1.
| Age, sex, and race | Year | Percent change | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1974-81 | Yearly average | |
|
| ||||||||||
| Enrollment per million | ||||||||||
| Total | 76 | 106 | 135 | 160 | 197 | 231 | 260 | 286 | 276 | 20.8 |
| Age | ||||||||||
| 0-14 years | 4 | 6 | 7 | 8 | 8 | 12 | 14 | 16 | 300 | 21.9 |
| 15-24 years | 27 | 39 | 47 | 52 | 62 | 76 | 86 | 93 | 244 | 19.3 |
| 25-34 years | 60 | 87 | 106 | 127 | 149 | 179 | 203 | 226 | 277 | 20.9 |
| 35-44 years | 95 | 137 | 174 | 203 | 246 | 290 | 322 | 352 | 271 | 20.6 |
| 45-54 years | 129 | 190 | 239 | 286 | 350 | 405 | 462 | 512 | 249 | 21.8 |
| 55-64 years | 145 | 222 | 293 | 360 | 440 | 513 | 585 | 655 | 352 | 24.0 |
| 65 years and over | 223 | 272 | 338 | 392 | 497 | 552 | 603 | 635 | 185 | 16.1 |
| Sex | ||||||||||
| Male | 88 | 121 | 152 | 180 | 224 | 261 | 294 | 322 | 266 | 20.4 |
| Female | 64 | 92 | 118 | 141 | 173 | 202 | 228 | 251 | 292 | 21.6 |
| Race | ||||||||||
| White | 65 | 91 | 114 | 134 | 163 | 190 | 212 | 231 | 255 | 19.8 |
| Black | 151 | 215 | 284 | 345 | 436 | 512 | 591 | 658 | 336 | 23.4 |
| All other | 123 | 172 | 208 | 235 | 298 | 348 | 399 | 437 | 255 | 19.8 |
Enrollment was measured as of July 1 each year.
Given the changing incidence rates by diagnosis, it is also interesting to examine prevalence rates by diagnosis. Changes in diagnostic prevalence will take place more slowly than incidence because survivors from previous incidence distributions will mute changes in recent incidence. In Table 21, the Medicare ESRD program prevalence by diagnostic category is shown. As expected, there has been less change in prevalence than in incidence rates. From 1974 through 1981, persons with glomerulonephritis have decreaed from 35 percent of the total to 29 percent. Primary hypertensive disease has increased only 5 percent, from 14 percent to 19 percent of the total renal population. Finally, despite the large increase in incidence, persons with diabetic nephropathy have only increased by about 4 percent (7.7 percent to 11.8 percent). This is because of the inherent lag of prevalence behind incidence as well as the considerably lower survival rates of persons with diabetic nephropathy as compared with those whose renal failure was due to other causes. How the percent distribution of diagnoses translates into rates per million is shown in Table 22. All diagnostic categories experienced an increase in prevalence from 1974 to 1981. Among the major categories, diabetic nephropathy had the largest increase in prevalence, 6 per million to 34 per million, a 470 percent increase. Primary hypertensive disease also increased more than 400 percent (10 per million to 54 per million). Glomerulonephritis increased by 320 percent, from 26 per million to 82 per million and remains the largest single diagnostic category of ESRD patients.
Table 21. Medicare ESRD program enrollment, by diagnosis: 1974-81.
| Diagnosis | Year | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | |
|
| ||||||||
| Percent distribution | ||||||||
| All causes | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Glomerulonephritis | 34.7 | 33.4 | 32.5 | 31.2 | 30.2 | 30.1 | 29.5 | 28.6 |
| Primary hypertensive disease | 13.5 | 13.9 | 14.3 | 15.5 | 16.8 | 17.0 | 18.2 | 19.0 |
| Diabetic nephropathy | 7.7 | 8.2 | 8.6 | 9.6 | 10.3 | 10.4 | 10.5 | 11.8 |
| Polycystic kidney disease | 8.7 | 8.4 | 8.4 | 8.3 | 8.2 | 8.3 | 8.6 | 8.4 |
| Collagen vascular disease | 1.7 | 1.7 | 1.7 | 1.6 | 1.7 | 1.6 | 1.6 | 1.6 |
| Interstitial nephritis, heredity | 1.6 | 1.5 | 1.6 | 1.6 | 1.5 | 1.6 | 1.5 | 1.5 |
| Interstitial nephritis, other | 11.8 | 11.4 | 11.0 | 10.1 | 9.5 | 9.3 | 8.7 | 8.2 |
| Analgesic abuse nephropathy | 0.1 | 0.1 | 0.1 | 0.3 | 0.4 | 0.6 | 0.7 | 0.8 |
| Obstructive uropathy, acquired | 0.3 | 0.3 | 0.3 | 0.8 | 1.2 | 1.3 | 1.4 | 1.5 |
| Obstructive uropathy, congenital | 0.1 | 0.1 | 0.2 | 0.6 | 0.8 | 1.0 | 1.2 | 1.3 |
| Amyloidosis | ( 1) | ( 1) | 0.1 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 |
| Multiple myeloma | 0.1 | 0.1 | 0.1 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 |
| Gouty nephropathy | ( 1) | ( 1) | ( 1) | 0.1 | 0.2 | 0.2 | 0.2 | 0.3 |
| Other, unspecified | 9.9 | 10.3 | 10.4 | 9.5 | 8.8 | 8.4 | 8.0 | 7.4 |
| Etiology unknown | 9.8 | 10.5 | 10.7 | 10.2 | 9.9 | 9.8 | 9.4 | 9.1 |
Less than .1 percent.
Table 22. Medicare ESRD program enrollment per million population, by diagnosis: 1974-81.
| Diagnosis | 1974 | 1975 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Enrollment per million | ||||||||
| All causes | 76 | 106 | 135 | 160 | 197 | 231 | 260 | 286 |
| Glomerulonephritis | 26 | 35 | 44 | 50 | 59 | 70 | 77 | 82 |
| Primary hypertensive disease | 10 | 15 | 19 | 25 | 33 | 39 | 47 | 54 |
| Diabetic nephropathy | 6 | 9 | 12 | 15 | 20 | 24 | 27 | 34 |
| Polycystic kidney disease | 7 | 9 | 11 | 13 | 16 | 19 | 22 | 24 |
| Collagen vascular disease | 1 | 2 | 2 | 3 | 3 | 4 | 4 | 5 |
| Interstitial nephritis, heredity | 1 | 2 | 2 | 3 | 3 | 4 | 4 | 4 |
| Interstitial nephritis, other | 9 | 12 | 15 | 16 | 19 | 21 | 23 | 23 |
| Analgesic abuse nephropathy | ( 1) | ( 1) | ( 1) | ( 1) | 1 | 1 | 2 | 2 |
| Obstructive uropathy, acquired | ( 1) | ( 1) | ( 1) | 1 | 2 | 3 | 4 | 4 |
| Obstructive uropathy, congenital | ( 1) | ( 1) | ( 1) | 1 | 2 | 2 | 3 | 4 |
| Amyloidosis | ( 1) | ( 1) | ( 1) | ( 1) | ( 1) | ( 1) | 1 | 1 |
| Multiple myeloma | ( 1) | ( 1) | ( 1) | ( 1) | 1 | 1 | 1 | 1 |
| Gouty nephropathy | ( 1) | ( 1) | ( 1) | ( 1) | ( 1) | ( 1) | 1 | 1 |
| Other, unspecified | 8 | 11 | 14 | 15 | 17 | 19 | 21 | 21 |
| Etiology unknown | 7 | 11 | 14 | 16 | 20 | 23 | 24 | 26 |
Less than .1 percent.
Future program growth
Given the observed rates of incidence and survival and the current enrollment of the Medicare ESRD program, it is possible to project the potential growth of this program. It has been widely reported that the American population will undergo a large shift in its age structure during the next 50 years (U.S. Bureau of the Census, 1977). From 1980 to 2030, the Census Bureau projects an increase in total population of 35 percent, reflecting a 28 percent increase in the white population and an 83-percent increase in the population of all races other than white. Concurrently, there will be a very large increase in older Americans, those most susceptible to renal failure. The number of Americans 65 years of age and over is expected to increase 121 percent by the year 2030. These population trends will have a direct impact on the Medicare ESRD program as shown in the following analysis.4
The 3-year average ESRD incidence rates (as shown in Table 3) and average ESRD termination rates over the same time period were used in conjunction with Census population projections to calculate future Medicare ESRD enrollments. Terminations are the sum of deaths and termination of Medicare benefits, usually due to successful transplantation. The estimates are based upon three assumptions: unchanging incidence rates for all age, sex, and race groups; unchanging termination rates; and accurate Census projections. If incidence rates rise, then the projections will be too low. To the extent that improvements in transplant success are made, or decreases in mortality rates are achieved, the estimates will change accordingly.
The estimates of Medicare ESRD program enrollment for the years 1980 through 2030 by age, sex, and race categories are presented in Table 23. Total ESRD enrollment is estimated to rise from 57,800 in 1980 to 162,100 in 2030, an increase of 180 percent. Under the stated assumptions, male enrollment will increase by 176 percent and female enrollment by 186 percent; the enrollment of white people will increase by 118 percent and the enrollment of all nonwhite people will increase by 327 percent. The large increase among non-white people is caused by not only their total growth in the general population, but also their (nonwhites) greater relative shift from young to old. Finally, the greatest increase by age will be among the group 0-24 years of age (279 percent) and the smallest enrollment increase will be among the aged, 65 years of age and over (100 percent). The reason that the aged enrollment will not increase to a greater extent, despite having the largest increase in total population, is the much higher mortality rates among aged ESRD Medicare beneficiaries. The mortality rates for the over-65 ESRD population are more than twice as great as for the under-25 population. A second reason is that most of the increase in the over-65 population will occur in the “older aged,” those 75 years of age and over. And, as was shown, treated incidence declines rapidly after 75 years of age.
Table 23. Projected Medicare ESRD program enrollment, by age, sex, and race: 1980-2030.
| Year | Percent change in ESRD population 1980-2030 | Percent change in U.S. population | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1980 | 1990 | 2000 | 2010 | 2020 | 2030 | |||
| Number of persons | ||||||||
| All persons | 57,800 | 94,400 | 117,200 | 136,700 | 152,800 | 162,100 | 180 | 35 |
| Age | ||||||||
| 0-24 years | 4,300 | 10,800 | 13,100 | 14,900 | 15,700 | 16,300 | 279 | 11 |
| 25-44 years | 15,600 | 34,100 | 44,400 | 46,500 | 47,800 | 50,600 | 224 | 24 |
| 45-64 years | 22,900 | 34,700 | 43,300 | 57,700 | 66,100 | 65,200 | 185 | 53 |
| 65 years and over | 15,000 | 14,800 | 16,400 | 17,600 | 23,200 | 30,000 | 100 | 121 |
| Sex | ||||||||
| Male | 31,800 | 51,800 | 64,600 | 75,000 | 83,100 | 87,700 | 176 | 34 |
| Female | 26,000 | 42,600 | 52,600 | 61,700 | 69,700 | 74,400 | 186 | 37 |
| Race | ||||||||
| White | 40,600 | 62,100 | 72,900 | 80,800 | 86,500 | 88,600 | 118 | 28 |
| All Other | 17,200 | 32,300 | 44,300 | 55,900 | 66,300 | 73,500 | 327 | 83 |
| Average annual percent increase | ||||||||
| — | 5.0 | 2.2 | 1.6 | 1.1 | 0.6 | — | — | |
The projected growth in the ESRD Medicare population is illustrated in Figure 1. The effect of the post-World War II baby boom is evident in this graph. Most of the growth in the groups 0-24 and 24-44 years of age will occur by the year 2000, after which it will level off somewhat. The group 45-64 years of age will start to experience its greatest growth between the years 2000 and 2015, as the baby boom segment of the population reaches this age range. Finally, as the baby boom population leaves the group 45-64 years of age and enters the group 65 years of age and over, (around 2015), there will be a subsequent rise in the over-65 ESRD population.
Figure 1. Projected Medicare End-stage Renal Disease program enrollment, by age: 1975-2030.
It should be noted that, in spite of the seemingly large increase in total ESRD enrollment compared with the growth in the U.S. population, this projection does reflect a continuation of the decrease (shown in Table 20) in percentage growth of the beneficiary population. From 1980-90, the projected annual growth rate is only 5 percent. In subsequent decades it declines even further so that in the decade 2020-30, the projected annual growth rate is less than 1 percent. Thus, the rate of growth in program enrollment is likely to level off, even if absolute enrollment continues to grow.
This estimate of future ESRD population growth is markedly different from previous estimates, which had the population leveling off at about 90,000 ( Iglehart, 1982; Klar, 1972; Kolata, 1980). The major differences between this and other projections are, first, higher incidence rates than previously suspected and, second, the factoring of the aging of the overall population into the model. In addition, the Office of Financial and Actuarial Analysis in HCFA never predicted a leveling off of program enrollment. Many authors apparently assumed that the actuaries' projection indicated level-off points. Nevertheless, this projection is likely to be a conservative estimate of future enrollment. It appears that incidence rates are not remaining unchanged, but, in fact, may be increasing (see Table 2). If this is so, then future Medicare ESRD enrollment will be greater than estimated in Table 23.
Summary and conclusions
The analyses presented in this paper bring to light several aspects of the Medicare ESRD program. First, program enrollment has been, and continues to be, growing rapidly. From 1974 through 1981, program enrollment quadrupled. Although this is a cause of concern to policymakers and legislators, who must deal with escalating program costs, it is also a measure of the program's success. Prior to Medicare funding of ESRD services, thousands of people each year died because there was no funding source for dialysis and transplantation. The 64,000 people covered by the program as of 1981 represent the truly lifesaving accomplishments of this program. It is important to note, as well, that the program is growing at a declining rate. Yearly increases in the early days of the program regularly exceeded 20 percent. That growth rate has now dropped to a little more than 10 percent.
A second finding is that, given the demographic characteristics of ESRD program incidence and the projections of the U.S. population, there is no reason to expect that program enrollment will level off during the immediate future. In fact, the recent incidence and mortality experience suggest the program will continue to grow with a 180-percent increase in enrollment during the next 50 years, although the growth rate is likely to continue to drop. However, the aging of the U.S. population and the projected relative increase in the U.S. population of all races other than white will combine to push program enrollment higher.
A third important finding is the changing mix of new entrants into the program. Program incidence continues to rise, a fact that underlines the conservative nature of the projections of future enrollments. The increase in incidence is higher among females and among all races other than white. In terms of diagnoses, the biggest increase in incidence are for persons whose reported cause of renal failure is either primary hypertensive disease or diabetic nephropathy.
A fourth finding concerns the complex relationship between age, sex, race, and ESRD program incidence. The fact that sex and race differences in incidence do not appear until adulthood underscores the potential benefits that prevention could have on this program. To the extent that diabetes and hypertension can be controlled, there could be substantial residual benefits in terms of lower incidence of renal failure.
The survival analyses showed that, for all the life-saving benefits of dialysis, end-stage renal disease remains a serious life-threatening disease. Fewer than one-half of people with renal failure can expect to survive 5 years. Age is a significant factor in survival, with persons aged 15-24 having a 64 percent 5 year survival rate; persons 75 years of age and over have a 5 year survival of only 22 percent. Much of this difference, however, is because of underlying age-specific mortality. Adjusting for overall mortality rates reduces much of the apparent age impact on ESRD survival. Race and sex are small determinants of survival in the population. Females survive at a rate 3 percent greater than males. Survival for black people is 3 percent greater than for white people. A critical determinant of survival is the principle cause of renal failure. People whose renal failure was caused by polycystic kidney disease have the best survival experience; those whose renal failure was caused by diabetic nephropathy have the worst.
This article describes a program in flux—one still growing but with a changing patient population. In the future, there is need for an updated study to determine if current trends in incidence, prevalence, and mortality are continuing. In particular, the increasing incidence rate is a real cause of concern. Presumably, the increase will stabilize at some level. However, it has exceeded initial expectations by a considerable amount and, as yet, there is little indication that a leveling off is occurring.
Footnotes
Reprint requests: Paul W. Eggers, Health Care Financing Administration, 2-C-13 Oak Meadows Building, 6325 Security Boulevard, Baltimore, MD 21207.
This section deals with Medicare ESRD program incidence and not total incidence of renal failure in an epidemiological sense. About 7 percent of all treated renal failure is not Medicare covered and is, of necessity, excluded from this analysis (HCFA, 1981). In addition, an unknown amount of renal failure will not be treated each year because of age, poor prognosis, or misdiagnosis.
In this and all subsequent analysis involving the calculation of rates by race, people of unknown race were assigned to the race categories in direct proportion to the distribution of known codes. For example, if 80 percent of people with known rates were white people, then 80 percent of the unknowns were included in the count of white people.
The moving average was calculated as the weighted average across three age groups. Thus the average incidence rate shown for white males 40-44 years of age is actually the weighted average of white males 35-39, 40-44, and 45-49 years of age. For a discussion of the use of and problems of moving averages, see Wallis and Roberts (1956).
The following analysis does not constitute official HCFA projections of ESRD Medicare enrollment since these projections were done in HCFA's Office of Research. Official HCFA projections are routinely produced by the Office of Financial and Actuarial Analysis in HCFA.
References
- Aday LA, Andersen R, Fleming CV. Health Care in the US, Equitable for Whom? Beverly Hills: Sage Publications; 1980. [Google Scholar]
- Andersen R. Health service distribution and equity. In: Andersen R, et al., editors. Equity in Health Services: Empirical Analyses in Social Policy. Cambridge, Massachusetts: Ballinger Publishing Company; 1980. [Google Scholar]
- Cutler SJ, Ederer F. Maximum utilization of the life table method in analyzing survival. Journal of Chronic Diseases. 1958;8:699–712. doi: 10.1016/0021-9681(58)90126-7. [DOI] [PubMed] [Google Scholar]
- Dobson A, Ruther M. Health Care Financing Review. Washington: U.S. Government Printing Office; Winter. 1981. Equal treatment and unequal benefits: a re-examination of the use of Medicare services by race, 1967-1976. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. HCFA Pub. No. 03090. [PMC free article] [PubMed] [Google Scholar]
- Esterling RE. Racial factors in the incidence and causation of end-stage renal disease. Transactions of the American Society for Artificial Internal Organs. 1977;(23):28–32. doi: 10.1097/00002480-197700230-00008. [DOI] [PubMed] [Google Scholar]
- Evans RW, Blagg CR. Correspondence. New England Journal of Medicine. 1981 Feb.304(6):357. [Google Scholar]
- Harburg E, Gleibermann L, Roeper P, Schork MA, Schull WJ. Skin color, ethnicity, and blood pressure 1: Detroit blacks. American Journal of Public Health. 1978a Dec.68:1177–1182. doi: 10.2105/ajph.68.12.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harburg E, Gleibermann L, Ozzoren F, Roeper P, Schork MA. Skin color, ethnicity, and blood pressure II: Detroit whites. American Journal of Public Health. 1978b Dec.68(12):1184–1188. doi: 10.2105/ajph.68.12.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Care Financing Administration. End-Stage Renal Disease Report to Congress. 1981. HCFA Pub. No. 82-02144. [Google Scholar]
- Health Care Financing Administration. End-Stage Renal Disease Report to Congress. 1983. in press. [Google Scholar]
- Held PJ, Pauly MV, Smits HL. Correspondence. New England Journal of Medicine. 1981;304(6):355. [Google Scholar]
- Hiatt RK, Friedman GO. Characteristics of patients referred for treatment of end-stage renal disease in a defined population. American Journal of Public Health. 1982 Aug.72(8):829–833. doi: 10.2105/ajph.72.8.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglehart JK. Funding the end-stage renal disease program. New England Journal of Medicine. 1982 Feb.306(8):492–496. doi: 10.1056/NEJM198202253060828. [DOI] [PubMed] [Google Scholar]
- Keil JE, Tyroler HA, Sandpiper SH, Boyle E., Jr Hypertension: effects of social class and racial admixture. American Journal of Public Health. 1977 Jul;67(7):634–639. doi: 10.2105/ajph.67.7.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klar R. Cost-Treatment of Chronic Renal Disease. DHEW Memorandum to Assistant Secretary for Health. 1972 [Google Scholar]
- Kolata GB. NMC thrives selling dialysis. Science. 1980 May;208:25. doi: 10.1126/science.7367865. [DOI] [PubMed] [Google Scholar]
- Krakauer H, Grauman JS, McMullan MR, Creede CC. The recent U.S. experience in the treatment of end-stage renal disease by dialysis and transplantation. New England Journal of Medicine. 1983 Jun;308(1) doi: 10.1056/NEJM198306303082603. [DOI] [PubMed] [Google Scholar]
- Lemann J. Correspondence. New England Journal of Medicine. 1981 Feb.304(6):355–356. [Google Scholar]
- Lowrie EE. Correspondence. New England Journal of Medicine. 1981 Feb.304(6):356. [Google Scholar]
- Mausner JS, Clark JK, Coles BI, Menduke H. An areawide survey of treated end-stage renal disease. American Journal of Public Health. 1978 Feb.68(2):166–169. doi: 10.2105/ajph.68.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Unpublished data from the Division of Health Interview Statistics, National Health Interview Survey. 1979. [Google Scholar]
- Prottas J, Segal M, Sapolsky HM. Cross-national differences in dialysis rates. Health Care Financing Review. 1983 Mar;4(3):91–104. [PMC free article] [PubMed] [Google Scholar]
- Relman AS. Race and End-Stage Renal Disease. New England Journal of Medicine. 1982 May;306(21):1290–1291. doi: 10.1056/NEJM198205273062109. [DOI] [PubMed] [Google Scholar]
- Relman AS, Rennie D. Treatment for End-Stage Renal Disease: Free But Not Equal. New England Journal of Medicine. 1980 Oct.303(17):996–998. doi: 10.1056/NEJM198010233031708. [DOI] [PubMed] [Google Scholar]
- Rettig RA, Marks EL. Implementing the End-Stage Renal Disease Program of Medicare. Washington: U.S. Government Printing Office; 1981. HCFA Pub. No. 03085, Office of Research, Demonstrations and Statistics, Health Care Financing Administration. [Google Scholar]
- Rostand SG, Kirk KA, Rutsky EA, Pate BA. Racial Differences in the Incidence of Treatment of End-Stage Renal Disease. New England Journal of Medicine. 1982 May;306(21):1276–1279. doi: 10.1056/NEJM198205273062106. [DOI] [PubMed] [Google Scholar]
- Rowland M, Roberts J. Advance Data From Vital and Health Statistics. No. 84. Washington: U.S. Government Printing Office; Oct. 1982. Blood pressure and hypertension in persons Aged 6-74 years: United States 1976-80. DHHS Pub. No. (PHS) 82-1250. National Center for Health Statistics, Public Health Service. [PubMed] [Google Scholar]
- Tyroler HA, James SA. Blood pressure and skin color. American Journal of Public Health. 1978 Dec.68(12):1170,1171–1172. doi: 10.2105/ajph.68.12.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Bureau of the Census. Projections of the Population of the United States: 1977 to 2050. No. 704. U.S. Department of Commerce; 1977. (P-25). [Google Scholar]
- Van Hoek R. Testimony before the Oversight Committee on Ways and Means. Jun 24 30, Jul 24 30, 1975. [Google Scholar]
- Velez R, Charlton J. Correspondence. New England Journal of Medicine. 1981 Feb.304(6):356–7. [Google Scholar]
- Wallis WA, Roberts H. Statistics: A New Approach. New York: Free Press of Glencoe; 1956. [Google Scholar]
- Wineman RJ. End-stage kidney disease: Trends in statistics. In: McNeil BJ, Cavalho EG, editors. Critical Issues in Medical Technology. Boston, Massachusetts: Auburn House; 1981. [Google Scholar]