Abstract
Health care spending in the United States more than tripled between 1972 and 1982, increasing from $94 billion to $322 billion. This growth substantially outpaced overall growth in the economy. National health expenditures are projected to reach approximately $690 billion in 1990 and consume roughly 12 percent of the gross national product. Government spending for health care is projected to reach $294 billion by 1990, with the Federal Government paying 72 percent. The Medicare prospective payment system and increasing competition in the health services sector are providing incentives to integrate clinical practice patterns with improved management practices.
Introduction
External economic forces are limiting the ability of buyers to pay for increasingly costly health care. Major buyers of care such as the Federal Government, State and local governments, and corporate businesses, are putting mounting pressures on health care providers to reduce the rate of increase in health care costs without lowering the quality of care. Health care providers, in competing for these funding sources while providing quality care, will have to move toward integration of clinical practice patterns with modern techniques of finance, management, and information support systems. Competition among providers will be intensified so there will be additional incentives to integrate clinical practice styles with improved management practices.
The implementation of the Medicare prospective payment system (PPS) for hospital inpatient services by the Health Care Financing Administration (HCFA), the largest buyer of health care in America, will have a major impact on merging clinical medicine and quality of care issues with management, finance, and information support systems. Payment per case is fixed in advance and is linked to diagnostic related groups (DRG's). This PPS may be the most significant and pervasive change in Medicare since its passage in 1965, and no major part of our health care system is likely to be untouched by the direct and secondary effects of the PPS as it goes through various stages of evolution in the 1980's.
These questions are likely to surface with increasing intensity in the 1980's: What is good health? What is good quality health care? What is cost-effective health care? What can we (individual households, firms, State and local governments, and the Federal Government) afford to pay, given other demands on resources?
Managers, policymakers, and providers in the health care sector, as in all sectors, must incorporate estimates of future trends into today's decisions. Inflation, economic shocks, and unanticipated outcomes of policies over the last decade have intensified the need for periodic assessments of individual industries and their relationship to the larger economy. This article provides such an assessment for the health care industry by providing baseline current-law projections of national health expenditures through 1990.
Highlights
Highlights from this article include the following:
Economy-wide inflation is assumed to substantially moderate in the 1980's, resulting in a deceleration in health expenditure growth.
National health expenditures are projected to increase at an average annual rate of roughly 10 percent for the period 1982-90, a decline from the 13-percent average annual growth in the 1972-82 period.
The real gross national product is projected to increase at a faster rate for 1982-90 than in the previous decade, resulting in upward pressure for growth in real health spending as the ability to finance spending increases.
Growth in personal health expenditures per capita is projected to slow to an average annual rate of approximately 9 percent for the period 1982-90, a significant decline from the 12-13 percent growth rate for 1972-82.
Per capita expenditures for 1990 are projected to be approximately $2, 700 for total health care, $1, 200 for hospital care, and $525 for physicians' services.
Government spending for health care is projected to reach $294 billion by 1990, of which the Federal Government will finance roughly 72 percent.
Private spending in 1990 is estimated to reach $400 billion, 58 percent of all health care expenditures.
Medicare is projected to fund a higher proportion of health spending, even with the deceleration resulting from the prospective payment system.
The population 75 years of age or over is projected to increase four times as fast as the average annual rate for persons under 65 years of age, leading to upward pressure on expenditure growth, especially for long-term care.
Institutional care as a share of personal health expenditures will increase. By 1990, expenditures for hospital and nursing home care are expected to consume approximately 58 percent of personal health care spending compared with 45 percent in 1965.
Evolution of health care delivery and finance
The projections contained in this article are an evolution of past trends and tendencies (Gibson, et al., 1983) and assume no substantial departure from current health care delivery and finance institutions. The key assumption is that the present extensive third-party payment system will remain in place, including the PPS for Medicare hospital inpatient services (Health Care Financing Administration, 1983).
Other evolving patterns significant to the health care sector for the 1980's are:
Continued growth in new and expensive diagnostic and therapeutic technologies.
Reduced rate of growth of Government financing for social programs.
Increased rivalry and competition within and among various segments of the health care sector, taking many forms of price and nonprice competition, such as improved quality of services and products; expanded and intensified catchment area analyses1 to ascertain needs of potential patients and characteristics of competing providers; increased responsiveness to patients; more emphasis on clinical competency and personal effectiveness (bedside-manner); improved management information systems (MIS) that merge clinical (patient and provider) and financial data; greater use of medical records specialists, cost accountants, industrial engineers, and strategic planners; increased consumer health education and advertising; and greater substitution of cost-effective services and supplies.
Underlying the diminished growth in aggregate spending for health care will be substantial variation in the viability of individual health care providers and of medical equipment and supply firms. Providers and suppliers who respond effectively and in a timely fashion to the new realities will find many opportunities in markets that are growing significantly faster than average, as indicated by the projected rise in health care spending compared with the GNP. Providers and suppliers who do not respond effectively to the more intense competition will experience declines in market share; they will find the 1980's are not a repeat of the 1960's and 1970's.
Projection scenario
This article focuses on average annual rates of change, assuming no unanticipated events. This scenario serves as a baseline from which alternative scenarios can be constructed to meet the unique needs of individual managers, strategic planners, policymakers, and the like. Historical patterns in health spending are studied over three basic time periods: 1950-82, 1965-82, and 1972-82. The projection periods are short-term, 1982-84; midterm, 1982-87; and long-term, 1982-90.
The model incorporates economic, actuarial, statistical, demographic, and judgmental factors into a single, integrated framework. There are four major interrelated components of the model: (1) a five-factor formula of expenditure growth, (2) supply variables, (3) a channel of finance module; and (4) a net cost of private health insurance/program administration cost module.2
Presented first are the assumptions upon which the projections are based. Following this is an overview of projections for total health care costs and sources of financing. Health care expenditure growth is examined from an international vantage point, and some theories on the causes of health expenditure growth are presented. Also provided are projections of personal health spending per capita and projections for particular sectors of the health care industry.
Assumptions for current law projections
These current-law projections are based on a set of assumptions relating to the health care sector and to the economy as a whole. The fundamental assumption is that historical trends and relationships will continue into the future (which includes 1983, as complete information is not yet available for that year). Further, the following are assumed:
The competitive structure, conduct, and performance of the health care delivery system will continue to evolve along patterns followed during the historical period (from 1965 through 1982).
No federally mandated cost-containment program such as prospective payment for all payors, will be in effect. This is an assumption of the current-law projections, not a prediction.
No major new publicly-financed program of medical care, such as catastrophic National health insurance, will be implemented. This is an assumption of the current-law projections, not a prediction.
No major technological breakthrough in treatment of acute and chronic illnesses that would significantly alter evolving patterns of morbidity and mortality or health care delivery will occur.
Use of medical care, including intensity of services per case, will continue to grow in accordance with historical relationships and trends, reflecting clinical practice patterns and demand factors. The trends are modified to reflect current-law reimbursement incentives such as the Medicare prospective payment system, where such shifts can be discerned.
Population will grow as projected by the Office of the Actuary, Social Security Administration (Tables 1-3).
Health manpower will increase as projected by the Bureau of Health Professions (Table 4).
The GNP and the implicit price deflator for the GNP will grow as projected in economic assumptions incorporated in the Board of Trustees, 1983 Annual Report, Federal Old-Age and Survivors Insurance and Disability Trust Funds. Alternative II-B (intermediate) economic assumptions of the report were used (Table 1).3
Health care prices will vary with the implicit price deflator for the GNP, according to relationships established in the historical period studied.
Benefit outlays and administrative expenses for Medicare will grow as projected in the 1983 Annual Report, Federal Hospital Insurance Trust Fund, and the 1983 Annual Report Federal Supplementary Medical Insurance Trust Fund (Tables A and B).
Aggregate Federal Medicaid outlay increases are derived from the Health Care Financing Administration projections for the Midsession Review of the 1984 Budget, June 29, 1983 (Table C).
Table 1. Historical estimates and projections of gross national product, inflation, and population: Selected years 1950-90.
| Gross national product | Consumer Price1 2 Index—all items wage earners (1967 = 100.0) | Total3 population July 1 in thousands | |||
|---|---|---|---|---|---|
|
|
|||||
| Calendar year | Current dollars in billions | 1972 dollars in billions | Implicit price deflator (1972 = 100.0) | ||
| Historical estimates | |||||
| 1950 | $ 286.5 | $ 534.8 | 53.5 | 72.1 | 154,675 |
| 1955 | 400.0 | 657.5 | 60.8 | 80.2 | 168,385 |
| 1960 | 506.5 | 737.2 | 68.7 | 88.7 | 183,834 |
| 1965 | 691.0 | 929.3 | 74.4 | 94.5 | 197,876 |
| 1966 | 756.0 | 984.8 | 76.8 | 97.2 | 200,149 |
| 1967 | 799.6 | 1,011.4 | 79.0 | 100.0 | 202,334 |
| 1968 | 873.4 | 1,058.1 | 82.5 | 104.2 | 204,362 |
| 1969 | 944.0 | 1,087.6 | 86.8 | 109.8 | 206,369 |
| 1970 | 992.7 | 1,085.6 | 91.4 | 116.3 | 208,612 |
| 1971 | 1,077.7 | 1,122.4 | 96.0 | 121.3 | 211,256 |
| 1972 | 1,185.9 | 1,185.9 | 100.0 | 125.3 | 213,569 |
| 1973 | 1,326.4 | 1,254.3 | 105.7 | 133.1 | 215,665 |
| 1974 | 1,434.2 | 1,246.3 | 115.1 | 147.7 | 217,683 |
| 1975 | 1,549.2 | 1,231.7 | 125.7 | 161.2 | 219,890 |
| 1976 | 1,718.0 | 1,298.2 | 132.3 | 170.5 | 221,993 |
| 1977 | 1,918.3 | 1,369.7 | 140.0 | 181.5 | 224,225 |
| 1978 | 2,163.8 | 1,438.5 | 150.4 | 195.4 | 226,583 |
| 1979 | 2,417.8 | 1,479.4 | 163.4 | 217.7 | 229,061 |
| 1980 | 2,631.7 | 1,475.0 | 178.4 | 247.0 | 231,679 |
| 1981 | 2,954.1 | 1,513.8 | 195.1 | 272.3 | 233,988 |
| 1982 | 3,073.0 | 1,485.4 | 206.9 | 288.6 | 236,215 |
| Projections | |||||
| 1984 | 3,603.2 | 1,594.3 | 226.0 | 310.8 | 240,581 |
| 1987 | 4,575.4 | 1,757.1 | 260.4 | 358.0 | 247,136 |
| 1990 | 5,629.5 | 1,920.0 | 293.2 | 403.1 | 253,416 |
| Selected periods | Average annual percent change | ||||
| 1950-55 | 6.9 | 4.2 | 2.6 | 2.2 | 1.7 |
| 1955-60 | 4.8 | 2.3 | 2.5 | 2.0 | 1.8 |
| 1960-65 | 6.4 | 4.7 | 1.6 | 1.3 | 1.5 |
| 1965-70 | 7.5 | 3.2 | 4.2 | 4.3 | 1.1 |
| 1970-75 | 9.3 | 2.6 | 6.5 | 6.8 | 1.1 |
| 1975-80 | 11.2 | 3.7 | 7.3 | 8.9 | 1.0 |
| 1980-85 | 8.4 | 2.3 | 5.9 | 5.8 | 0.9 |
| 1985-90 | 7.4 | 3.0 | 4.3 | 4.3 | 0.9 |
| 1979-82 | 8.3 | 0.1 | 8.2 | 9.9 | 1.0 |
| 1982-84 | 8.3 | 3.6 | 4.5 | 3.8 | 0.9 |
| 1984-87 | 8.3 | 3.3 | 4.8 | 4.8 | 0.9 |
| 1987-90 | 7.2 | 3.0 | 4.0 | 4.0 | 0.8 |
| 1965-82 | 9.2 | 2.8 | 6.2 | 6.8 | 1.0 |
| 1972-82 | 10.0 | 2.3 | 7.5 | 8.7 | 1.0 |
| 1982-87 | 8.3 | 3.4 | 4.7 | 4.4 | 0.9 |
| 1982-90 | 7.9 | 3.3 | 4.5 | 4.3 | 0.9 |
Historical estimates are reported in Council of Economic Advisors, February 1983. Projection growth rates are from the 1983 Annual Report, Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds, ll-B Assumptions. The growth rates for 1983 for GNP and inflation were slightly modified to reflect partial year data available as of mid-1983. The average annual rate of growth in GNP for 1982-90 used in this projection is within 1 percentage point of the rate used by the private consulting firm of Data Resources, Inc. See U.S. Long-Term Review, Fall 1983 (Forecast: TRENDLONG2008B).
The CPI is shown for comparison only. The implicit price deflator for GNP is used in the projection process to reflect cost pressures external to health care industry.
Historical estimates of population are based on data from the Bureau of the Census. The estimates are reported in Gibson et al., (1983). Projected growth rates in population are from the Office of the Actuary, see Wilkin, (1983). Alternative II (intermediate) assumptions for population growth were used.
Table 3. Average annual percent change in the number of persons under 65 years of age, 65 years of age and over, and 75 years of age and over: Selected periods 1960-20001.
| Period | Under 65 years | 65 years and over | 75 years and over |
|---|---|---|---|
| 1960-65 | 1.4 | 2.0 | 3.6 |
| 1965-70 | 1.0 | 1.7 | 3.4 |
| 1970-75 | 0.7 | 2.3 | 2.4 |
| 1975-80 | 0.7 | 2.3 | 2.4 |
| 1980-85 | 0.8 | 2.2 | 3.1 |
| 1985-90 | 0.7 | 2.1 | 2.8 |
| 1990-95 | 0.7 | 1.4 | 2.6 |
| 1995-2000 | 0.6 | 0.7 | 2.4 |
| 1965-82 | 0.9 | 2.2 | 3.0 |
| 1972-82 | 0.8 | 2.5 | 2.8 |
| 1980-82 | 0.8 | 2.4 | 3.4 |
| 1982-84 | 0.8 | 2.0 | 2.8 |
| 1984-87 | 0.7 | 2.3 | 2.9 |
| 1987-90 | 0.7 | 2.0 | 2.8 |
| 1982-87 | 0.7 | 2.2 | 2.8 |
| 1982-90 | 0.7 | 2.1 | 2.8 |
Derived from data in Wilkin (1983). Alternative II (intermediate) assumptions for population growth were used.
Table 4. Historical estimates and projections of active physicians and dentists: Selected years 1950-901.
| Year | Number of active physicians (as of December 31) | Number of active dentists (as of December 31) | ||
|---|---|---|---|---|
|
| ||||
| Total | M.D.'s | D.O.'s | ||
| Historical estimates | ||||
| 1950 | 219,900 | 209,000 | 10,900 | 79,190 |
| 1955 | 240,200 | 228,600 | 11,600 | 84,370 |
| 1960 | 259,400 | 247,300 | 12,200 | 90,120 |
| 1965 | 288,700 | 277,600 | 211,100 | 95,900 |
| 1970 | 323,200 | 311,200 | 12,000 | 102,220 |
| 1972 | 345,200 | 332,400 | 12,800 | 105,400 |
| 1975 | 378,600 | 364,500 | 14,100 | 112,020 |
| 1980 | 449,500 | 432,400 | 17,100 | 126,240 |
| 1981 | 464,000 | 446,000 | 18,000 | 129,330 |
| 1982 | 478,900 | 460,000 | 18,900 | 132,590 |
| Projection | ||||
| 1984 | 508,300 | 487,600 | 20,700 | 138,620 |
| 1987 | 551,900 | 527,500 | 24,400 | 147,030 |
| 1990 | 591,200 | 563,300 | 27,900 | 154,760 |
| Selected periods | Average annual percent change | |||
| 1950-55 | 1.8 | 1.8 | 1.3 | 1.3 |
| 1955-60 | 1.6 | 1.6 | 1.0 | 1.3 |
| 1960-65 | 2.2 | 2.3 | 2−1.9 | 1.3 |
| 1965-70 | 2.3 | 2.3 | 1.6 | 1.3 |
| 1970-75 | 3.2 | 3.2 | 3.3 | 1.9 |
| 1975-80 | 3.5 | 3.5 | 3.9 | 2.4 |
| 1970-80 | 3.4 | 3.3 | 3.6 | 2.1 |
| 1980-90 | 2.8 | 2.7 | 5.0 | 2.1 |
| 1982-84 | 3.1 | 3.0 | 4.7 | 2.3 |
| 1984-87 | 2.8 | 2.7 | 5.6 | 2.0 |
| 1987-90 | 2.3 | 2.2 | 4.6 | 1.8 |
| 1982-87 | 2.9 | 2.8 | 5.2 | 2.2 |
| 1965-82 | 3.0 | 3.0 | 3.2 | 1.9 |
| 1972-82 | 3.3 | 3.3 | 4.0 | 2.3 |
| 1982-90 | 2.7 | 2.6 | 5.0 | 2.0 |
The decline in the number of active D.O.'s between 1960 and 1965 reflects the granting of approximately 2,400 M.D. degrees to osteopathic physicians who had graduated from the University of California College of Medicine at Irvine. These physicians are included with active M.D.'s beginning in 1962.
Table A. Medicare benefit payments, by type of service and administrative expenses: 1967-90.
| Benefit payments by type of service1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Calendar year | Benefits And administrative expenses | Total | Hospital care | Physicians' services | Other professional services2 | Eyeglasses and appliances | Nursing home care | Other personal health care | Administrative expenses |
|
| |||||||||
| Amount in billions | |||||||||
| Historical3 | |||||||||
| 1967 | $ 4.7 | $ 4.5 | $ 3.1 | $ 1.1 | (5) | (5) | $0.2 | (5) | $0.2 |
| 1968 | 6.0 | 5.7 | 3.8 | 1.4 | $0.1 | (5) | 0.4 | (5) | 0.3 |
| 1969 | 6.9 | 6.6 | 4.5 | 1.6 | 0.1 | (5) | 0.3 | (5) | 0.3 |
| 1970 | 7.5 | 7.1 | 5.1 | 1.6 | 0.1 | (5) | 0.3 | (5) | 0.4 |
| 1971 | 8.3 | 7.9 | 5.7 | 1.8 | 0.1 | $0.1 | 0.2 | (5) | 0.4 |
| 1972 | 9.1 | 8.6 | 6.4 | 2.0 | 0.1 | 0.1 | 0.2 | (5) | 0.5 |
| 1973 | 10.1 | 9.6 | 7.1 | 2.1 | 0.1 | 0.1 | 0.2 | (5) | 0.6 |
| 1974 | 13.1 | 12.4 | 9.3 | 2.6 | 0.1 | 0.1 | 0.2 | (5) | 0.7 |
| 1975 | 16.3 | 15.6 | 11.6 | 3.3 | 0.2 | 0.1 | 0.3 | (5) | 0.7 |
| 1976 | 19.3 | 18.4 | 13.8 | 3.9 | 0.3 | 0.1 | 0.3 | $0.1 | 0.9 |
| 1977 | 22.5 | 21.8 | 16.3 | 4.6 | 0.3 | 0.2 | 0.4 | 0.1 | 0.8 |
| 1978 | 25.9 | 24.9 | 18.4 | 5.4 | 0.5 | 0.2 | 0.3 | 0.1 | 1.0 |
| 1979 | 30.3 | 29.3 | 21.2 | 6.5 | 0.6 | 0.3 | 0.4 | 0.4 | 1.0 |
| 1980 | 36.8 | 35.7 | 26.0 | 7.8 | 0.7 | 0.4 | 0.4 | 0.5 | 1.1 |
| 1981 | 44.8 | 43.5 | 31.3 | 9.7 | 0.9 | 0.5 | 0.4 | 0.6 | 1.3 |
| 1982 | 52.2 | 50.9 | 36.3 | 11.4 | 1.3 | 0.6 | 0.5 | 0.8 | 1.3 |
| Projected4 | |||||||||
| 1984 | 67.9 | 66.5 | 46.1 | 15.9 | 1.9 | 1.0 | 0.5 | 1.0 | 1.4 |
| 1987 | 96.4 | 94.7 | 64.6 | 24.0 | 2.4 | 1.5 | 0.7 | 1.4 | 1.7 |
| 1990 | 133.6 | 131.5 | 88.7 | 34.6 | 3.2 | 2.1 | 0.9 | 2.0 | 2.0 |
Service categories used in this Table differ from those used in the annual reports of the Board of Trustees of the Federal Hospital Insurance and Supplementary Medical Insurance Trust Funds. For example, hospital-based home health services appear as hospital care rather than as home health services, which are included in other professional services.
Hospice benefits are included with other professional services. The benefit provision was effective November 1, 1983, and expires October 1, 1986.
Historical data are from Gibson et al. (1983).
Projections are derived from Assumptions II-B (intermediate) of the Board of Trustees' 1983 annual reports. However, growth rates for hospital inpatient expenses were modified by the Medicare actuaries to reflect minor changes associated with the implementation of the Medicare PPS. Projections of Medicare outlays are updated periodically through the year to reflect changes in regulations and revised forecasts of the economy.
Less than $50 million.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Table B. Average annual percent change in Medicare benefit payments, by type of service and administrative expenses: 1968-90.
| Benefit payments by type of service1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Calendar year | Benefits and administrative expenses | Total | Hospital care | Physicians' services | Other professional services2 | Eyeglasses and appliances | Nursing home care | Other personal health care | Administrative expenses |
|
| |||||||||
| Percent change | |||||||||
| Historical | |||||||||
| 1968 | 26.4 | 25.4 | 20.6 | 25.0 | 79.2 | 33.2 | 88.6 | 27.2 | 50.7 |
| 1969 | 15.8 | 16.0 | 20.1 | 14.4 | 16.7 | 20.2 | −17.8 | 23.7 | 10.5 |
| 1970 | 8.4 | 7.6 | 11.7 | 1.6 | 0.1 | 4.0 | −18.7 | 4.7 | 27.2 |
| 1971 | 10.5 | 10.9 | 13.0 | 12.3 | −17.7 | 18.4 | −31.2 | 17.6 | 2.6 |
| 1972 | 10.0 | 9.7 | 10.9 | 7.3 | 7.7 | 11.7 | −5.6 | 12.5 | 16.2 |
| 1973 | 11.2 | 10.9 | 11.9 | 7.2 | 28.0 | 11.4 | 11.7 | 10.7 | 16.0 |
| 1974 | 29.2 | 29.6 | 30.5 | 25.5 | 53.4 | 30.2 | 28.6 | 32.7 | 23.8 |
| 1975 | 24.6 | 25.5 | 25.3 | 25.8 | 43.6 | 34.1 | 17.7 | 33.4 | 6.8 |
| 1976 | 18.3 | 18.2 | 18.4 | 16.8 | 31.9 | 24.0 | 13.1 | 23.5 | 21.4 |
| 1977 | 16.7 | 18.2 | 18.2 | 17.6 | 32.9 | 24.6 | 9.6 | 25.0 | −14.7 |
| 1978 | 15.1 | 14.6 | 13.5 | 18.3 | 31.0 | 24.6 | −4.3 | 24.7 | 31.2 |
| 1979 | 17.0 | 17.6 | 15.0 | 20.4 | 24.1 | 27.4 | 4.3 | (4) | 1.5 |
| 1980 | 21.4 | 21.7 | 22.4 | 20.1 | 24.4 | 27.0 | 4.3 | 22.7 | 11.6 |
| 1981 | 21.6 | 21.8 | 20.6 | 24.7 | 27.5 | 34.9 | 15.5 | 24.1 | 15.8 |
| 1982 | 16.5 | 17.0 | 16.1 | 17.4 | 41.6 | 30.5 | 9.2 | 19.9 | −0.5 |
| Projected3 | |||||||||
| 1982-84 | 14.1 | 14.3 | 12.7 | 18.0 | 23.8 | 24.3 | 7.5 | 13.6 | 5.9 |
| 1984-87 | 12.4 | 12.5 | 11.9 | 14.8 | 7.8 | 15.7 | 8.7 | 13.0 | 6.0 |
| 1987-90 | 11.5 | 11.6 | 11.2 | 12.9 | 9.2 | 12.0 | 9.0 | 11.8 | 5.9 |
| 1982-87 | 13.1 | 13.2 | 12.2 | 16.1 | 13.9 | 19.0 | 8.2 | 13.3 | 5.9 |
| 1982-90 | 12.5 | 12.6 | 11.8 | 14.9 | 12.1 | 16.4 | 8.5 | 12.7 | 5.9 |
Service categories used in this table differ from those used in the annual reports of the Board of Trustees of the Federal Hospital Insurance and Supplementary Medical Insurance Trust Funds. For example, hospital-based home health services appear as hospital care rather than as home health services which are included in other professional services.
Hospice benefits are included with other professional services. This benefit provision was effective November 1, 1983, and expires October 1, 1986.
Projections are derived from assumptions II-B (intermediate) of the Board of Trustees' 1983 annual reports. However, growth rates for hospital inpatient expenses were modified by the Medicare actuaries to reflect minor changes associated with the implementation of the Medicare prospective payment system. Projections of Medicare outlays are updated periodically through the year to reflect changes in regulations and revised forecasts of the economy.
Expenditures for other personal health care were revised for the period beginning in 1979. Time-series data for 1968 through 1978 are not consistent.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Table C. Federal share of Medicaid benefits and administrative expenses: 1967-90.
| Benefits and administrative expenses | Benefits | Administrative expenses | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Calendar year | Amount in billions | Percent change | Amount in billions | Percent change | Amount in billions | Percent change |
| Historical1 | ||||||
| 1967 | $ 1.5 | --- | $ 1.4 | --- | $0.1 | --- |
| 1968 | 2.0 | 34.7 | 1.9 | 34.7 | 0.1 | 33.4 |
| 1969 | 2.4 | 21.7 | 2.3 | 21.7 | 0.1 | 23.4 |
| 1970 | 3.0 | 24.6 | 2.9 | 24.2 | 0.1 | 34.4 |
| 1971 | 3.8 | 28.0 | 3.7 | 28.6 | 0.2 | 15.8 |
| 1972 | 4.6 | 20.7 | 4.4 | 20.8 | 0.2 | 19.9 |
| 1973 | 5.5 | 17.8 | 5.2 | 17.3 | 0.2 | 30.5 |
| 1974 | 6.4 | 17.1 | 6.1 | 17.2 | 0.3 | 15.1 |
| 1975 | 7.9 | 24.1 | 7.6 | 23.8 | 0.4 | 29.1 |
| 1976 | 9.0 | 13.5 | 8.5 | 12.9 | 0.5 | 26.8 |
| 1977 | 10.0 | 11.5 | 9.5 | 11.1 | 0.5 | 17.8 |
| 1978 | 11.2 | 11.1 | 10.4 | 9.9 | 0.7 | 31.8 |
| 1979 | 13.0 | 16.7 | 12.2 | 17.0 | 0.8 | 13.0 |
| 1980 | 14.6 | 11.9 | 13.8 | 12.7 | 0.8 | −0.2 |
| 1981 | 17.3 | 18.4 | 16.2 | 17.7 | 1.1 | 30.0 |
| 1982 | 18.0 | 4.1 | 16.9 | 4.6 | 1.0 | −3.4 |
| Projected2, 3 | ||||||
| 1984 | 21.9 | --- | 20.7 | --- | 1.2 | --- |
| 1987 | 28.9 | --- | 27.4 | --- | 1.5 | --- |
| 1990 | 37.3 | --- | 35.6 | --- | 1.7 | --- |
Historical Medicaid financial data on outlays reflect changes in services incurred and cash flow adjustments (Gibson, et al., 1983).
The projections are derived from changes in Medicaid benefits and administrative expenses prepared by HCFA for the Midsession Review of the 1984 Budget, June 29, 1983. The Midsession Review projections extend through fiscal year 1988. Projections through calendar year 1990 were prepared for this report.
Projections of the Federal share of the Medicaid vendor payments are updated periodically through the year to reflect changes in regulations and revised forecasts of the economy.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The short-term outlook for the economy for the period 1982-84, compared with the period 1979-82, can be characterized by a substantial deceleration in inflation and a rebound in real growth in the economy in 1983 (Table 1). The gross national product (GNP) deflator, an economy-wide measure of inflation, is projected to increase at an average annual rate of 4.5 percent for the period 1982-84, compared with an 8.2 percent annual rate for the 1979-82 period. Real (inflation-adjusted) GNP increased at an average annual rate of only 0.1 percent for the period 1979-82. It is estimated to increase at an average annual rate of 3.6 percent for the period 1982-84.
For the midterm period 1982-87, GNP is projected to increase at an average annual rate of 8.3 percent, with the GNP deflator expected to increase at an average rate of 4.7 percent and real GNP increasing at an average rate of 3.4 percent. For 1987-90, the GNP deflator is expected to increase at an average annual rate of 4.0 percent and real GNP at a 3.0 percent rate.
For the entire projection period, 1982-90, the GNP deflator is expected to increase at an average annual rate of 4.5 percent. This is a significant deceleration from the last decade, 1972-82, when the GNP deflator increased at an average annual rate of 7.5 percent. Real and nominal GNP are projected to increase at an average annual rate of 3.3 and 7.9 percent for the 1982-90 period. This deceleration in economy-wide inflation has a significant impact on health care spending since approximately 60 percent of the growth in this spending can be accounted for by economy-wide inflation. Thus, projections of health care spending are very sensitive to relatively small errors in forecasting economy-wide inflation.
Shifts in the age composition of the population is one factor that will cause health expenditures to rise in the 1980's. Use of health care by the aged population is disproportionate to their numbers. The number of persons aged 75 and over is projected to increase at an average rate of 2.8 percent in the period 1982-90, compared with a 0.7 rate for the nonaged population (Table 3). During the 1972-82 period, the growth rates were essentially the same as for the projected period. The proportion of the total population 65 years of age or over will rise from 11.5 percent in 1982 to 12.6 percent in 1990 (Table 2). Total population is projected to increase at an average rate of 0.9 percent from 1982-90 (Table 1). The aging of the population will continue through this century with the proportion of people 75 years of age or over reaching 6.5 percent in the year 2000, an increase from 4.7 percent in 1982 (Table 2).
Table 2. Number of persons and proportions of the population under 65 years of age, 65 years of age and over, and 75 years of age and over. Selected years 1960-20001.
| Year | All ages | Under 65 years | 65 years and over | 75 years and over |
|---|---|---|---|---|
| Number of persons as of July 1 in thousands | ||||
| 1960 | 188,943 | 171,796 | 17,147 | 5,775 |
| 1965 | 203,032 | 184,080 | 18,952 | 6,879 |
| 1970 | 214,024 | 193,343 | 20,681 | 8,133 |
| 1972 | 218,849 | 197,239 | 21,610 | 8,624 |
| 1975 | 224,956 | 201,656 | 23,300 | 9,307 |
| 1980 | 236,417 | 210,096 | 26,321 | 10,573 |
| 1981 | 238,588 | 211,716 | 26,872 | 10,881 |
| 1982 | 241,058 | 213,444 | 27,614 | 11,312 |
| Projections | ||||
| 1984 | 245,495 | 216,724 | 28,771 | 11,949 |
| 1985 | 247,727 | 218,321 | 29,406 | 12,291 |
| 1987 | 252,174 | 221,407 | 30,767 | 13,012 |
| 1990 | 258,670 | 226,011 | 32,659 | 14,117 |
| 1995 | 268,590 | 233,513 | 35,077 | 16,039 |
| 2000 | 227,353 | 241,015 | 36,338 | 18,080 |
| Percent distribution | ||||
| 1960 | 100.0 | 90.9 | 9.1 | 3.1 |
| 1965 | 100.0 | 90.7 | 9.3 | 3.4 |
| 1970 | 100.0 | 90.3 | 9.7 | 3.8 |
| 1972 | 100.0 | 90.1 | 9.9 | 3.9 |
| 1975 | 100.0 | 89.6 | 10.4 | 4.1 |
| 1980 | 100.0 | 88.9 | 11.1 | 4.5 |
| 1981 | 100.0 | 88.7 | 11.3 | 4.6 |
| 1982 | 100.0 | 88.5 | 11.5 | 4.7 |
| Projections | ||||
| 1984 | 100.0 | 88.3 | 11.7 | 4.9 |
| 1985 | 100.0 | 88.1 | 11.9 | 5.0 |
| 1987 | 100.0 | 87.8 | 12.2 | 5.2 |
| 1990 | 100.0 | 87.4 | 12.6 | 5.5 |
| 1995 | 100.0 | 86.9 | 13.1 | 6.0 |
| 2000 | 100.0 | 86.9 | 13.1 | 6.5 |
Derived from data in Wilkin (1983). Alternative II (intermediate) assumptions for population growth were used. Social security aged population differs slightly in concept from the national health expenditure population concept. See Gibson et al. (1983) and Wilkin (1983).
The number of health professional workers is expected to increase substantially. The number of active physicians is projected to grow from 478, 900 in 1982 to 591, 200 in 1990 (Table 4), an aggregate increase of 23 percent, or more than three times the projected aggregate population growth. The number of active dentists is projected to increase from 132,590 in 1982 to 154,760 in 1990, a 17-percent increase (Table 4). This increase is approximately 2.5 times faster than aggregate population growth. As is the case with physicians, the growth in the number of dentists will decelerate during the 1980's, declining from the peak growth rate years of 1975-80 (Table 4).
Overview of projections
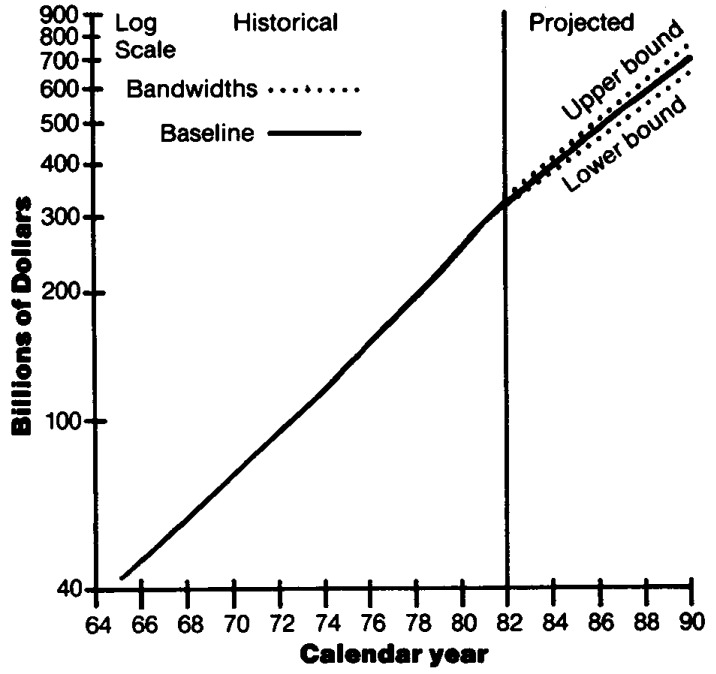
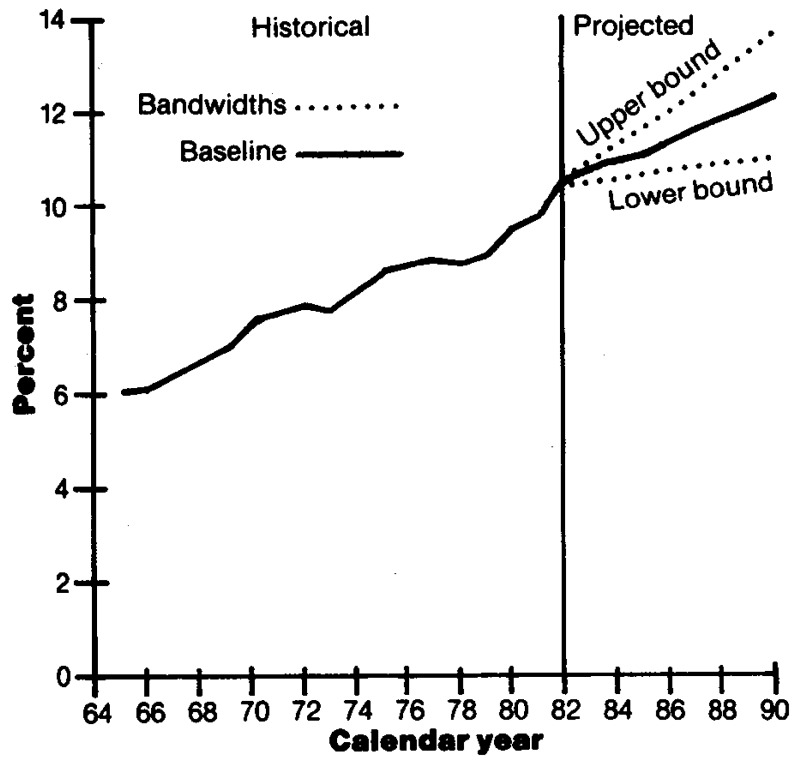
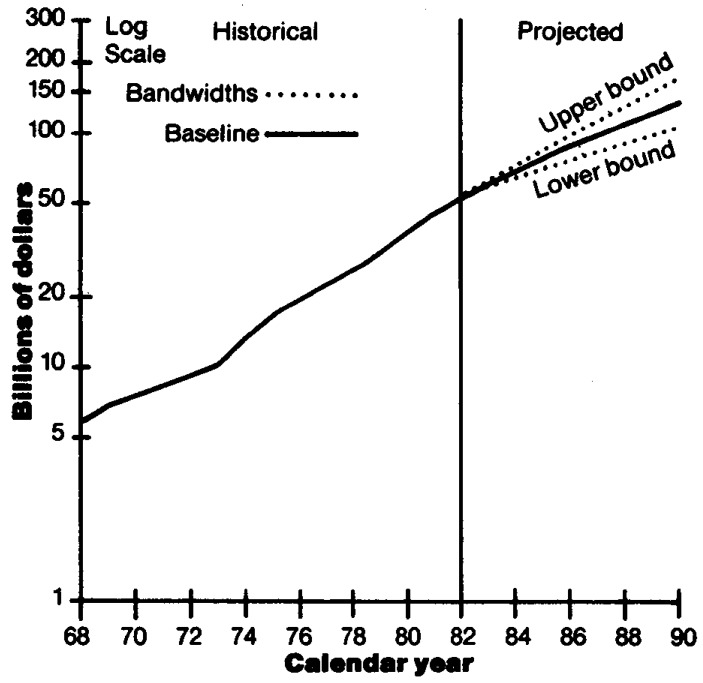
Total National health expenditures rose from $42 billion in 1965 to $322 billion in 1982, an average annual rate of growth of almost 13 percent (Table D). This rate implies a doubling of health care spending every 6 years. Total spending is projected to reach $690 billion and roughly 12 percent of GNP by 1990 (Figures 1 and 2). This increasing share of the GNP allocated to health is reflected by many indicators of economic activity—employment (Personick, 1983; Silvestri et al., 1983), consumption, real resource outlays, and payroll expense.
Table D. National health expenditures, and average annual percent change, by source of funds, and percent of gross national product (GNP): Selected calendar years 1950-90.
| Calendar year | Gross national product In billions | Total | Private | Public | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Total | Federal | State and local | ||||||||||
|
|
|
|
||||||||||
| Amount in billions | Per capita | Percent of GNP | Amount in billions | Percent of total | Amount in billions | Percent of total | Amount in billions | Percent of total | Amount in billions | Percent of total | ||
| Historical estimates1 | ||||||||||||
| 1950 | $ 286.5 | $ 12.7 | $ 82 | 4.4 | $ 9.2 | 72.8 | $ 3.4 | 27.2 | $ 1.6 | 12.8 | $ 1.8 | 14.4 |
| 1955 | 400.1 | 17.7 | 105 | 4.4 | 13.2 | 74.3 | 4.6 | 25.7 | 2.0 | 11.3 | 2.6 | 14.4 |
| 1960 | 506.5 | 26.9 | 146 | 5.3 | 20.3 | 75.3 | 6.6 | 24.7 | 3.0 | 11.2 | 3.6 | 13.5 |
| 1965 | 691.0 | 41.7 | 211 | 6.0 | 30.9 | 74.1 | 10.8 | 25.8 | 5.5 | 13.3 | 5.2 | 12.6 |
| 1966 | 756.0 | 46.1 | 230 | 6.1 | 32.5 | 70.6 | 13.6 | 29.4 | 7.4 | 16.1 | 6.1 | 13.3 |
| 1967 | 799.6 | 51.3 | 254 | 6.4 | 32.4 | 63.1 | 18.9 | 36.9 | 11.9 | 23.2 | 7.0 | 13.7 |
| 1968 | 873.4 | 58.2 | 285 | 6.7 | 36.1 | 62.0 | 22.1 | 38.0 | 14.1 | 24.2 | 8.0 | 13.7 |
| 1969 | 944.0 | 65.7 | 318 | 7.0 | 40.8 | 62.1 | 24.9 | 37.9 | 16.1 | 24.5 | 8.8 | 13.4 |
| 1970 | 992.7 | 74.7 | 358 | 7.5 | 46.9 | 62.8 | 27.8 | 37.2 | 17.7 | 23.7 | 10.1 | 13.5 |
| 1971 | 1,077.7 | 83.3 | 394 | 7.7 | 51.6 | 62.0 | 31.6 | 38.0 | 20.3 | 24.4 | 11.3 | 13.6 |
| 1972 | 1,185.9 | 93.5 | 438 | 7.9 | 58.1 | 62.1 | 35.4 | 37.9 | 22.9 | 24.5 | 12.5 | 13.4 |
| 1973 | 1,326.4 | 103.2 | 478 | 7.8 | 63.9 | 61.9 | 39.3 | 38.1 | 25.2 | 24.4 | 14.1 | 13.6 |
| 1974 | 1,434.2 | 116.4 | 535 | 8.1 | 69.3 | 59.5 | 47.1 | 40.5 | 30.4 | 26.2 | 16.6 | 14.3 |
| 1975 | 1,549.2 | 132.7 | 604 | 8.6 | 76.5 | 57.7 | 56.2 | 42.3 | 37.1 | 27.9 | 19.1 | 14.4 |
| 1976 | 1,718.0 | 149.7 | 674 | 8.7 | 86.7 | 57.9 | 62.9 | 42.1 | 42.6 | 28.4 | 20.3 | 13.6 |
| 1977 | 1,918.3 | 169.2 | 755 | 8.8 | 99.1 | 58.6 | 70.1 | 41.4 | 47.4 | 28.0 | 22.7 | 13.4 |
| 1978 | 2,163.8 | 189.3 | 836 | 8.7 | 109.8 | 58.0 | 79.5 | 42.0 | 53.9 | 28.4 | 25.7 | 13.6 |
| 1979 | 2,417.8 | 215.0 | 938 | 8.9 | 124.4 | 57.9 | 90.6 | 42.1 | 61.0 | 28.4 | 29.5 | 13.7 |
| 1980 | 2,631.7 | 249.0 | 1,075 | 9.5 | 143.6 | 57.7 | 105.4 | 42.3 | 71.1 | 28.6 | 34.3 | 13.8 |
| 1981 | 2,954.1 | 286.6 | 1,225 | 9.7 | 164.4 | 57.4 | 122.2 | 42.6 | 83.7 | 29.2 | 38.5 | 13.4 |
| 1982 | 3,073.0 | 322.4 | 1,365 | 10.5 | 185.6 | 57.6 | 136.8 | 42.4 | 93.2 | 28.9 | 43.7 | 13.5 |
| Projections | ||||||||||||
| 1984 | 3,603.2 | 392.7 | 1,632 | 10.9 | 226.7 | 57.7 | 166.0 | 42.3 | 115.5 | 29.4 | 50.4 | 12.8 |
| 1987 | 4,575.4 | 529.8 | 2,144 | 11.6 | 307.2 | 58.0 | 222.5 | 42.0 | 157.5 | 29.7 | 65.0 | 12.3 |
| 1990 | 5,629.5 | 690.4 | 2,724 | 12.3 | 396.8 | 57.5 | 293.5 | 42.5 | 211.4 | 30.6 | 82.1 | 11.9 |
| Average annual percent change | ||||||||||||
| Selected Periods | ||||||||||||
| 1950-55 | 6.9 | 6.9 | 5.1 | --- | 7.5 | --- | 6.2 | --- | 4.6 | --- | 7.6 | --- |
| 1955-60 | 4.8 | 8.7 | 6.8 | --- | 9.0 | --- | 7.5 | --- | 8.4 | --- | 6.7 | --- |
| 1960-65 | 6.4 | 9.2 | 7.6 | --- | 8.8 | --- | 10.4 | --- | 12.9 | --- | 7.6 | --- |
| 1965-70 | 7.5 | 12.3 | 11.2 | --- | 8.7 | --- | 20.8 | --- | 26.1 | --- | 14.0 | --- |
| 1970-75 | 9.3 | 12.2 | 11.0 | --- | 10.3 | --- | 15.1 | --- | 16.0 | --- | 13.6 | --- |
| 1975-80 | 11.2 | 13.4 | 12.2 | --- | 13.4 | --- | 13.4 | --- | 13.9 | --- | 12.5 | --- |
| 1950-80 | 7.7 | 10.4 | 9.0 | --- | 9.6 | --- | 12.1 | --- | 13.5 | --- | 10.3 | --- |
| 1970-80 | 10.2 | 12.8 | 11.6 | --- | 11.8 | --- | 14.3 | --- | 14.9 | --- | 13.0 | --- |
| 1980-90 | 7.9 | 10.7 | 9.7 | --- | 10.7 | --- | 10.8 | --- | 11.5 | --- | 9.1 | --- |
| 1979-82 | 8.3 | 14.5 | 13.3 | --- | 14.3 | --- | 14.7 | --- | 15.1 | --- | 13.9 | --- |
| 1982-84 | 8.3 | 10.4 | 9.4 | --- | 10.5 | --- | 10.1 | --- | 11.4 | --- | 7.5 | --- |
| 1984-87 | 8.3 | 10.5 | 9.5 | --- | 10.7 | --- | 10.3 | --- | 10.9 | --- | 8.8 | --- |
| 1987-90 | 7.2 | 9.2 | 8.3 | --- | 8.9 | --- | 9.7 | --- | 10.3 | --- | 8.1 | --- |
| 1972-82 | 10.0 | 13.2 | 12.0 | --- | 12.3 | --- | 14.5 | --- | 15.1 | --- | 13.3 | --- |
| 1982-87 | 8.3 | 10.4 | 9.4 | --- | 10.6 | --- | 10.2 | --- | 11.1 | --- | 8.3 | --- |
| 1982-90 | 7.9 | 10.0 | 9.0 | --- | 10.0 | --- | 10.0 | --- | 10.8 | --- | 8.2 | --- |
Historical estimates are from Gibson et al. (1983).
SOURCE: Office of Statistics and Data Management, Bureau of Data Management and Strategy, Health Care Financing Administration.
Figure 1. Total national health expenditures with bandwidths: 1965-901.
1The conditional bandwidths around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in total national health expenditures for 1966-82 was multiplied by a t-distribution value of 2.12 to derive the conditional “95 percent” bandwidths. The calculated bandwidths are approximate and are used as a rough guide in assessing variability and uncertainty. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no assurance that future variability will replicate historical variability.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Figure 2. National health expenditures as percent of gross national product with bandwidths: 1965-901.
1The conditional bandwidths around the baseline projection scenario provide one indicator of variability. The standard error associated with annual percent increases in the ratio of national health expenditures to gross national product for 1966-82 was multiplied by a t-distribution value of 2.12 to derive the conditional “95 percent” bandwidths. The calculated bandwidths are approximate and are used as a rough guide in assessing variability and uncertainty. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no assurance that future variability will replicate historical variability.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Over the period 1979-82, real GNP increased cumulatively less than 1 percent; whereas real National health care expenditures increased cumulatively nearly 13 percent (Table E). This rapid growth in inflation-adjusted spending for health care, relative to our ability to pay, was a factor that prompted Congress, States, and private industry to initiate alternative ways to pay for health care. Developing effective and efficient patterns of care that are clinically sound and humane are progressively becoming a necessity (Williamson and associates, 1982). There is potential for adopting cost-decreasing technologies and for making management improvements.
Table E. Annual percent change in real (inflation-adjusted) gross national product, health care spending, and Medicare benefits: 1980-82.
| Item | Per from cent change previous year | Cumulative growth 1979-82 | Price deflator used | ||
|---|---|---|---|---|---|
|
| |||||
| 1980 | 1981 | 1982 | |||
| Gross national product (GNP) | −0.3 | 2.6 | −1.9 | 0.4 | Implicit price deflator for GNP |
| National health expenditures (NHE) | 4.6 | 4.4 | 3.2 | 12.7 | Implicit price deflator for NHE |
| Community hospital inpatient services | 5.0 | 5.7 | 5.5 | 17.1 | National hospital input price index |
| Total Medicare benefits | 9.5 | 9.4 | 6.8 | 27.9 | Implicit price deflator for personal health care expenditures |
| Medicare hospital benefits | 9.7 | 7.8 | 5.9 | 25.2 | National hospital input price index |
| Medicare physician benefits | 8.6 | 12.3 | 7.3 | 30.9 | Consumer Price Index for physicians' services |
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The slow growth in the GNP and fast growth in health care spending account for the rapid increase in the ratio of health spending to GNP for the period 1979-82 (Table D and Figure 2). Growth in aggregate health care expenditures is insulated from short-term fluctuations in real GNP by both the pervasive system of third-party payments and the persistent need for medical care. On the other hand, some services that have relatively small proportions paid by insurance coverage (such as eyeglasses, drugs, and certain types of other professional services) appear to be adversely affected by recession. Growth in National health expenditures is relatively stable compared with GNP growth; this is indicated by negative growth in real GNP being associated with abnormally large annual increases in the ratio of National health expenditures to the GNP and atypically large increases in real GNP being associated with negative (or abnormally small) annual increases in the ratio of National health expenditures to the GNP (Freeland and Schendler, 1983). Growth in National health expenditures appears to be associated with growth in long-run “permanent” or expected GNP, rather than with current GNP.
Between 1965 and 1982, the health care sector's share of GNP increased at an average annual rate of 3.3 percent, rising from 6.0 percent of GNP in 1965 to 10.5 percent in 1982. From 1982 to 1990, the ratio of health care spending to the GNP is projected to increase at an average annual rate of 2 percent, a rate two-thirds as fast as the 1965 to 1982 rate. As the economy rebounds in 1983 and 1984, and as the effect of current-law reimbursement reform (for example, the Medicare PPS) takes hold, the health care sector's growth relative to GNP should decelerate. In 1984, National health expenditures are projected to be approximately 10.9 percent of GNP (Table D). A relatively gradual increase in this share is projected for the remainder of the 1980's, reaching roughly 12 percent in 1990.
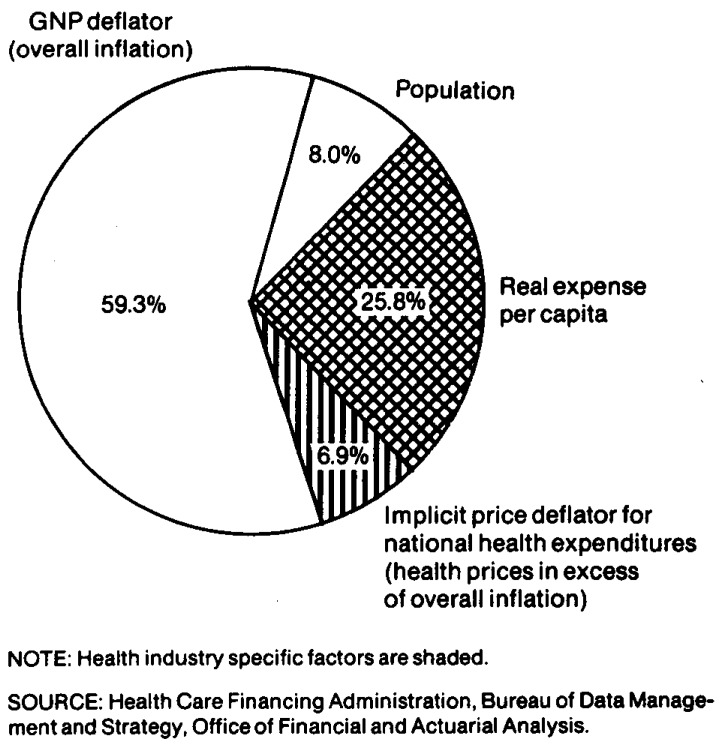
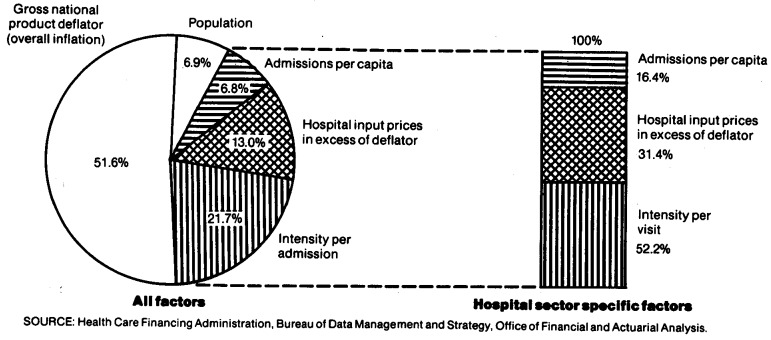
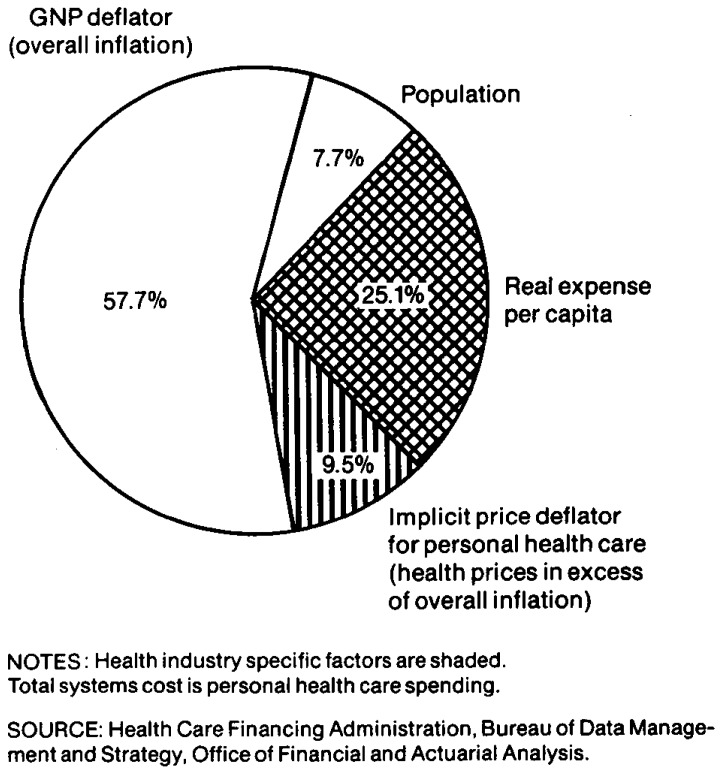
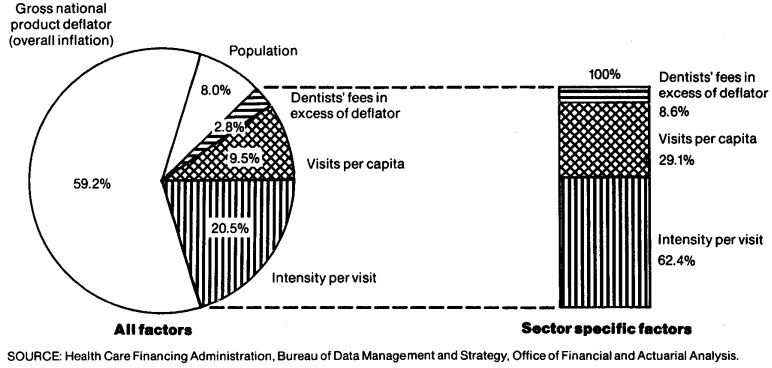
Five factors account for the 13-percent average annual increase in National health expenditures during 1972-82. Economy-wide inflation (GNP deflator) accounted for 59 percent of this growth (Figure 3). Health care sector prices (implicit price deflator for National health expenditures) in excess of economy-wide inflation accounted for 7 percent of the growth in spending. Growth in population accounted for 8 percent, and real expense per capita (intensity) accounted for the remaining 26 percent of increases in spending. The implicit price deflator for National health expenditures increased at an average annual rate of 8.5 percent during the period 1972-82, 1 percentage point faster than the GNP deflator and 1 percentage point lower than the Consumer Price Index (CPI) for medical care. Real spending for National health expenditures increased at an average annual rate of 4.3 percent for the 1972-82 period.
Figure 3. Factors accounting for growth in total national health expenditures: 1972-82.
Increases in National health care spending have fluctuated in the past according to policy factors, economic conditions, and other variables. The lowest annual percentage increase in the 1972-82 period, 10 percent, occurred during the Economic Stabilization Program (ESP) in 1973. The highest annual percentage increase in this period was 16 percent in 1980, the year in which the CPI for all items peaked with over a 13-percent increase. It is not possible to accurately predict the timing of turning points in health care sector activity; consequently, projections in this study are trend projections that reflect average tendencies.
During the 3-year period 1979-82, National health expenditures increased 50 percent and the GNP, 27 percent. Projected outlays are expected to increase at substantially lower rates, both absolutely and in relation to the GNP (Figures 1, 2 and Table D) as follows:
$393 billion by 1984, or $1,632 per capita.
$530 billion by 1987, or $2,144 per capita.
$690 billion by 1990, or $2,724 per capita.
Total spending is projected to increase at an average annual rate of 10 to 11 percent for the period 1982-84, down substantially from the 14 to 15 percent rate for the 1979-82 period. For the long-term period 1982-90, expenditures are expected to rise at an average annual rate of 10 percent, significantly below the 13-percent rate for the 1972-82 period.
A projected significant decline in the general inflation rate, leading to lower health care price increases, will exert substantial downward pressure on health spending in the 1980's. However, projected increases in real GNP, beginning in 1983, will exert an upward pressure, as will the aging of the population and the introduction of new cost-increasing technologies. Restrained growth in Government financing of health care, including the Medicare PPS, will exert downward pressure. As the economy expands, the fiscal restraint in Government programs may tend to ease. It is estimated that the net effect of these pressures will be a deceleration in the growth of health care spending.
There will be shifts in the relative share of health care spending going to various types of goods and services. Hospital care, physicians' services, other professional services (including home health services), and nursing home care are projected to increase at faster rates than other health care sectors (Tables 5 and 6). Reforms in payment systems for hospital care will result in some deceleration of spending increases relative to the last decade.
Table 5. National health expenditures by type of expenditure: Selected years 1950-90.
| Historical estimates1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Type of expenditure | 1950 | 1955 | 1960 | 1965 | 1970 | 1971 | 1972 | 1973 | 1974 | 1975 | 1976 |
|
| |||||||||||
| Amount in billions | |||||||||||
| Total | $ 12.7 | $ 17.7 | $ 26.9 | $ 41.7 | $ 74.7 | $ 83.3 | $93.5 | $103.2 | $116.4 | $132.7 | $149.7 |
| Health Services and Supplies | 11.7 | 16.9 | 25.2 | 38.2 | 69.3 | 77.2 | 86.9 | 96.3 | 108.9 | 124.3 | 140.6 |
| Personal Health Care | 10.9 | 15.7 | 23.7 | 35.8 | 65.1 | 72.0 | 80.2 | 88.7 | 101.0 | 116.8 | 131.8 |
| Hospital Care | 3.9 | 5.9 | 9.1 | 13.9 | 27.8 | 30.8 | 34.9 | 38.7 | 44.8 | 52.1 | 59.9 |
| Physicians' Services | 2.7 | 3.7 | 5.7 | 8.5 | 14.3 | 15.9 | 17.2 | 19.1 | 21.2 | 24.9 | 27.6 |
| Dentists' Services | 1.0 | 1.5 | 2.0 | 2.8 | 4.7 | 5.1 | 5.6 | 6.5 | 7.4 | 8.2 | 9.4 |
| Other Professional Services | 0.4 | 0.6 | 0.9 | 1.0 | 1.6 | 1.6 | 1.8 | 2.0 | 2.2 | 2.6 | 3.2 |
| Drugs and Medical Sundries | 1.7 | 2.4 | 3.7 | 5.2 | 8.0 | 8.6 | 9.3 | 10.1 | 11.0 | 11.9 | 13.0 |
| Eyeglasses and Appliances | 0.5 | 0.6 | 0.8 | 1.2 | 1.9 | 2.0 | 2.3 | 2.5 | 2.8 | 3.2 | 3.4 |
| Nursing Home Care | 0.2 | 0.3 | 0.5 | 2.1 | 4.7 | 5.6 | 6.5 | 7.1 | 8.5 | 10.1 | 11.4 |
| Other Health Services | 0.5 | 0.9 | 1.1 | 1.1 | 2.1 | 2.3 | 2.6 | 2.7 | 3.1 | 3.7 | 3.8 |
| Program Administration and Cost of Insurance | 0.5 | 0.6 | 1.1 | 1.6 | 2.7 | 3.4 | 4.7 | 5.4 | 5.2 | 4.4 | 5.0 |
| Government Public Health Activities | 0.4 | 0.4 | 0.4 | 0.8 | 1.4 | 1.8 | 2.0 | 2.2 | 2.7 | 3.2 | 3.8 |
| Research and Construction of Medical Facilities | 1.0 | 0.9 | 1.7 | 3.5 | 5.4 | 6.1 | 6.6 | 6.8 | 7.5 | 8.4 | 9.0 |
| Research | 0.1 | 0.2 | 0.7 | 1.5 | 2.0 | 2.1 | 2.4 | 2.5 | 2.8 | 3.3 | 3.7 |
| Construction | 0.8 | 0.7 | 1.0 | 2.0 | 3.4 | 4.0 | 4.2 | 4.3 | 4.7 | 5.1 | 5.3 |
| Historical estimates1 | Projections | ||||||||||
|
|
|||||||||||
| 1977 | 1978 | 1979 | 1980 | 1981 | 1982 | 1984 | 1987 | 1990 | |||
|
|
|||||||||||
| Total | $169.2 | $189.3 | $215.0 | $249.0 | $286.6 | $322.4 | $392.7 | $529.8 | $690.4 | ||
| Health Services and Supplies | 160.1 | 179.5 | 204.5 | 237.1 | 273.5 | 308.3 | 375.9 | 508.3 | 664.2 | ||
| Personal Health Care | 148.7 | 166.7 | 188.9 | 219.4 | 254.6 | 286.9 | 349.4 | 471.3 | 619.0 | ||
| Hospital Care | 67.8 | 75.7 | 86.1 | 100.4 | 118.0 | 135.5 | 165.7 | 226.7 | 303.6 | ||
| Physicians' Services | 31.9 | 35.8 | 40.2 | 46.8 | 54.8 | 61.8 | 76.1 | 102.5 | 133.5 | ||
| Dentists' Services | 10.5 | 11.8 | 13.3 | 15.4 | 17.3 | 19.5 | 23.7 | 30.9 | 38.9 | ||
| Other Professional Services | 3.6 | 4.1 | 4.7 | 5.6 | 6.4 | 7.1 | 8.9 | 12.3 | 16.1 | ||
| Drugs and Medical Sundries | 14.1 | 15.4 | 17.2 | 19.3 | 21.3 | 22.4 | 26.7 | 34.4 | 43.6 | ||
| Eyeglasses and Appliances | 3.7 | 4.1 | 4.6 | 5.1 | 5.7 | 5.7 | 6.8 | 8.7 | 10.9 | ||
| Nursing Home Care | 13.2 | 15.2 | 17.6 | 20.6 | 24.2 | 27.3 | 32.7 | 44.4 | 58.4 | ||
| Other Health Services | 4.1 | 4.5 | 5.1 | 6.0 | 6.9 | 7.6 | 8.8 | 11.3 | 14.1 | ||
| Program Administration and Cost of Insurance | 7.1 | 7.5 | 9.3 | 10.7 | 11.1 | 12.7 | 16.1 | 22.9 | 27.0 | ||
| Government Public Health Activities | 4.3 | 5.3 | 6.2 | 7.0 | 7.7 | 8.6 | 10.4 | 14.0 | 18.3 | ||
| Research and Construction of Medical Facilities | 9.2 | 9.8 | 10.5 | 11.8 | 13.1 | 14.1 | 16.8 | 21.5 | 26.2 | ||
| Research | 3.9 | 4.4 | 4.8 | 5.3 | 5.7 | 5.9 | 6.5 | 7.9 | 9.6 | ||
| Construction | 5.3 | 5.3 | 5.7 | 6.5 | 7.5 | 8.2 | 10.3 | 13.6 | 16.6 | ||
Historical estimates are reported in Gibson, et al., (1983).
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Table 6. National health expenditures, average annual percent change by type of expenditure: selected periods 1950-90.
| Average annual percent change | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||
| Type of expenditure | 1950-55 | 1955-60 | 1960-65 | 1965-70 | 1970-75 | 1975-80 | 1979-82 | 1982-84 | 1984-87 | 1987-90 | 1965-82 | 1972-82 | 1982-87 | 1982-90 |
| Total | 7.0 | 8.7 | 9.2 | 12.3 | 12.2 | 13.4 | 14.5 | 10.4 | 10.5 | 9.2 | 12.8 | 13.2 | 10.4 | 10.0 |
| Health Services and Supplies | 7.6 | 8.3 | 8.7 | 12.6 | 12.4 | 13.8 | 14.7 | 10.4 | 10.6 | 9.3 | 13.1 | 13.5 | 10.5 | 10.1 |
| Personal Health Care | 7.6 | 8.6 | 8.6 | 12.7 | 12.4 | 13.4 | 14.9 | 10.4 | 10.5 | 9.5 | 13.0 | 13.6 | 10.4 | 10.1 |
| Hospital Care | 8.9 | 9.0 | 8.8 | 14.9 | 13.4 | 14.0 | 16.3 | 10.6 | 11.0 | 10.2 | 14.3 | 14.5 | 10.8 | 10.6 |
| Physicians' Services | 6.1 | 9.0 | 8.3 | 11.1 | 11.7 | 13.4 | 15.4 | 11.0 | 10.5 | 9.2 | 12.4 | 13.7 | 10.6 | 10.1 |
| Dentists' Services | 9.4 | 5.6 | 7.3 | 11.1 | 11.6 | 13.3 | 13.5 | 10.3 | 9.2 | 7.9 | 12.1 | 13.2 | 9.6 | 9.0 |
| Other Professional Services | 7.3 | 8.9 | 3.7 | 9.1 | 10.4 | 16.5 | 14.4 | 11.7 | 11.4 | 9.5 | 12.0 | 14.7 | 11.6 | 10.7 |
| Drugs and Medical Sundries | 6.7 | 8.9 | 7.2 | 9.1 | 8.3 | 10.1 | 9.1 | 9.2 | 8.9 | 8.2 | 9.0 | 9.1 | 9.0 | 8.7 |
| Eyeglasses and Appliances | 4.2 | 5.1 | 8.6 | 10.7 | 10.1 | 10.2 | 6.9 | 9.5 | 8.7 | 7.7 | 9.7 | 9.6 | 8.8 | 8.5 |
| Nursing Home Care | 10.8 | 11.0 | 31.5 | 17.8 | 16.5 | 15.4 | 15.9 | 9.4 | 10.8 | 9.5 | 16.4 | 15.5 | 10.2 | 10.0 |
| Other Health Services | 11.9 | 3.7 | 0.7 | 12.5 | 12.2 | 10.4 | 14.3 | 7.5 | 8.6 | 7.8 | 11.8 | 11.3 | 8.3 | 8.0 |
| Program Administration and Net Cost of Insurance | 14.6 | 6.7 | 13.8 | 10.4 | 10.3 | 19.5 | 11.1 | 12.5 | 12.5 | 5.6 | 12.8 | 10.5 | 12.5 | 9.9 |
| Government Public Health Activities | 0.9 | 1.9 | 14.5 | 11.8 | 17.3 | 17.3 | 11.4 | 9.7 | 10.5 | 9.2 | 14.9 | 15.7 | 10.3 | 9.8 |
| Research and Construction of Medical Facilities | −2.2 | 14.7 | 15.5 | 9.1 | 9.3 | 7.1 | 10.3 | 9.2 | 8.6 | 6.8 | 8.5 | 7.9 | 8.8 | 8.1 |
| Research | 12.4 | 25.8 | 18.0 | 5.4 | 11.1 | 9.8 | 7.2 | 5.4 | 6.5 | 6.6 | 8.3 | 9.6 | 6.0 | 6.3 |
| Construction | −5.0 | 10.0 | 13.8 | 11.4 | 8.1 | 5.1 | 12.9 | 11.8 | 9.8 | 6.8 | 8.7 | 6.9 | 10.6 | 9.1 |
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Government financing
In 1982, the Federal share of health spending was 29 percent (Table D), an increase of 4 percentage points since 1973. Because of new reimbursement incentives—such as Medicare's PPS, the maturing of Federal health programs, and the tight fiscal situation—the Federal share is expected to increase at a slower pace over the 1982-90 period than during the 1972-82 period. The Federal share is projected to be approximately 29 percent in 1984, 30 percent in 1987, and 31 percent in 1990. The gradual rise in Federal share reflects primarily the aging of the population. Federal outlays for National health expenditures, which were $1.6 billion in 1950, increased to $23 billion in 1972 and $93 billion in 1982 (Table D). These expenditures increased at an average annual rate of 15 percent for the period 1972-82.
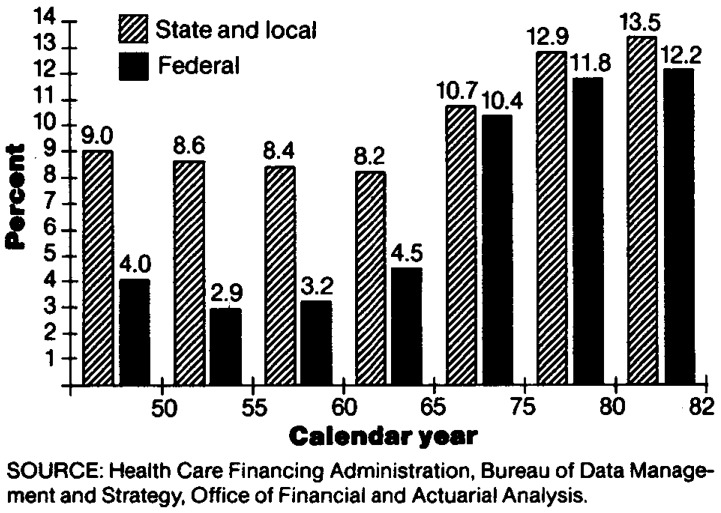
Health care outlays are becoming a larger slice of the Federal fiscal pie. Federally financed health expenditures made up between 4 and 5 percent of total Federal Government expenditures in 1965 (pre-Medicare and Medicaid); by 1982, this percentage rose to 12 percent (Figure 4).
Figure 4. Government expenditures for health as a percent of total government expenditures: Selected years 1950-82.
The near-term outlook has Federal expenditures rising to $116 billion in 1984, an increase of 24 percent over 1982. Federal outlays for National health expenditures are estimated to increase at an average annual rate of 11 percent from 1982-90, a rate substantially below the 15 percent rate for the 1972-82 period and slightly above the growth rate for total National health expenditures. It is projected that Federal expenditures will reach $158 billion by 1987 and $211 billion by 1990.
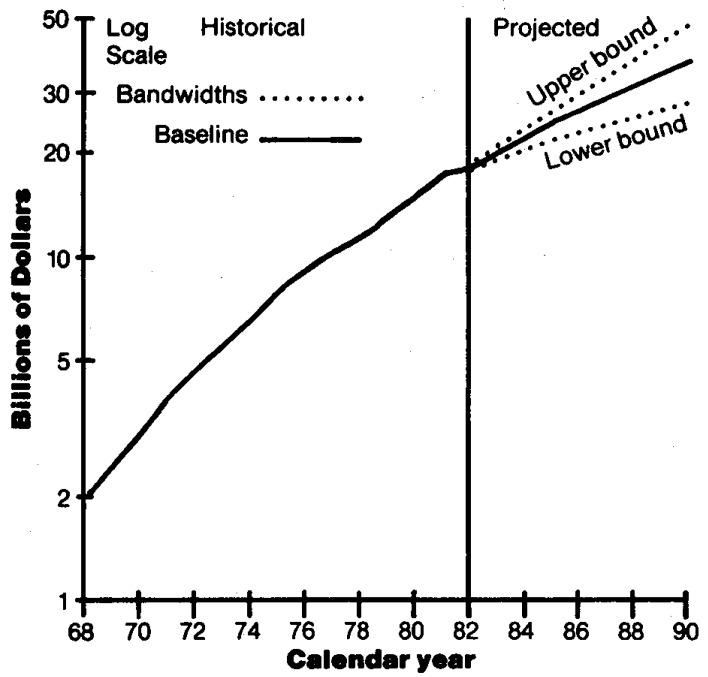
Medicare expenditures of $52 billion in 1982 (Table A) made up 60 percent of total Federal outlays for health care in 1982, compared with 40 percent in 1972. By 1990, Medicare is projected to account for 63 percent of Federal outlays for health care. In 1967 (the first full year of the Medicare program), total Medicare outlays were $4.7 billion, and these outlays increased at an average annual rate of 17 percent between 1967 and 1982, compared with an average annual increase of 13 percent for National health expenditures. By 1990, Medicare outlays are expected to reach $134 billion (Figure 5 and Table A), increasing at an average annual rate of between 12 and 13 percent for the 1982-90 period (Table B). The GNP is projected to increase at an average rate of 8 percent during this period. Thus, Medicare outlays represent an ever-increasing share of the real resources in the economy, and Medicare will finance an increasing share of National health expenditures, even under the PPS. This is expected for two reasons: (1) hospital and physician services are a high proportion of Medicare outlays (Table F), and costs of these services are projected to rise faster than most other service types; and (2) the aged population is growing three times faster than the nonaged population (Table 3).
Figure 5. Medicare outlays with bandwidths: 1968-901,2.
1Outlays include benefits plus administrative expenses.
2The conditional bandwidths around the baseline projections scenario provide one indicator of variability. The standard error associated with annual percentage increases in Medicare outlays for 1969-1982 was multiplied by a t-distribution value of 2.16 to derive the conditional “95 percent” bandwidths. The calculated bandwidths are approximate and are used as a rough guide in assessing variability and uncertainty. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no assurance that future variability will replicate historical variability.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Table F. Percent distribution of Medicare benefit payments by type of service: Selected years 1967-901.
| Calendar year | Per capita Medicare benefit payments | Total Medicare benefit payments in billions | Type of personal health care expenditure | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | Hospital care | Physicians' services | Other professional services2 | Eyeglasses and appliances | Nursing home care | Other health services | |||
|
| |||||||||
| Percent distribution | |||||||||
| Historical3 | |||||||||
| 1967 | $ 22 | $ 4.5 | 100.0 | 69.0 | 24.7 | 0.8 | 0.6 | 4.6 | 0.2 |
| 1970 | 34 | 7.1 | 100.0 | 71.4 | 22.9 | 1.1 | 0.6 | 3.7 | 0.2 |
| 1972 | 40 | 8.6 | 100.0 | 73.6 | 22.7 | 0.8 | 0.7 | 2.0 | 0.3 |
| 1975 | 71 | 15.6 | 100.0 | 74.5 | 21.3 | 1.3 | 0.7 | 1.9 | 0.3 |
| 1980 | 154 | 35.7 | 100.0 | 72.7 | 21.8 | 2.0 | 1.0 | 1.0 | 1.4 |
| 1981 | 186 | 43.5 | 100.0 | 72.0 | 22.4 | 2.1 | 1.1 | 1.0 | 1.5 |
| 1982 | 215 | 50.9 | 100.0 | 71.4 | 22.4 | 2.5 | 1.3 | 0.9 | 1.5 |
| Projected4 | |||||||||
| 1984 | 276 | 66.5 | 100.0 | 69.4 | 23.9 | 2.9 | 1.5 | 0.8 | 1.5 |
| 1987 | 383 | 94.7 | 100.0 | 68.2 | 25.4 | 2.6 | 1.6 | 0.7 | 1.5 |
| 1990 | 519 | 131.5 | 100.0 | 67.5 | 26.3 | 2.4 | 1.6 | 0.7 | 1.5 |
Service categories used in this table differ from those used in the annual reports of the Board of Trustees of the Federal Hospital Insurance and Supplementary Medical Insurance Trust Funds. For example, hospital-based home health services appear as hospital care rather than as home health services, which are included in other professional services.
Hospice benefits are included with other professional services. The benefit provision was effective November 1, 1983, and expires October 1, 1986.
Historical data are from Gibson et al. (1983).
Projections are derived from Assumptions II-B (intermediate) from the Board of Trustees (1983). However, growth rates for hospital inpatient expenses were modified by the Medicare actuaries to reflect minor changes associated with the implementation of the Medicare PPS. Projections of Medicare outlays are updated periodically through the year to reflect changes in regulations and revised forecasts of the economy.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Total Medicare outlays (including administrative expenses) are projected to reach $68 billion by 1984, $96 billion by 1987, and $134 billion by 1990. Under the Alternative II-B assumptions incorporated in this projection, the Medicare hospital insurance trust fund is expected to be able to finance total outlays until approximately 1990. With more pessimistic or optimistic assumptions, the hospital insurance trust fund will be depleted at an earlier or later date (Board of Trustees, Federal Hospital Insurance Trust Fund, 1983).
Federal Medicaid outlays (benefits plus administrative expenses) were $18 billion in 1982, compared with $4.6 billion in 1972 (Table C), an average annual rate of increase of almost 15 percent. Federal Medicaid outlays are projected to reach $22 billion in 1984, $29 billion in 1987, and $37 billion in 1990 (Figure 6 and Table C). These outlays are projected to increase at an average annual rate of approximately 10 percent over the period 1982-87, a rate approximately one-third lower than the 15 percent rate for the 1972-82 period. This is principally due to the assumption of lower inflation.
Figure 6. Federal Medicaid outlays, with bandwidths: 1968-901,2.
1Outlays include benefits plus administrative expenses.
2The conditional bandwidths around the baseline projections scenario provide one indicator of variability. The standard error associated with annual percent increases in Federal Medicaid outlays for 1969-1982 was multiplied by a t-distribution value of 2.16 to derive the conditional “95 percent” bandwidths. The calculated bandwidths are approximate and are used as a rough guide in assessing variability and uncertainty. It is important to keep in mind the potential dangers of extrapolating historical measures of variability into the future. That is, there can be no assurance that future variability will replicate historical variability.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
Federal health care outlays other than Medicare and Medicaid rose at an average annual rate of nearly 10 percent from 1972 to 1982 and are estimated to increase at a 7 percent annual rate from 1982 to 1990.
Health expenditures financed by State and local governments were 8 to 9 percent of their total expenditures for the years 1950-70 (Figure 4). By 1982, this percentage had risen to over 13 percent, forcing State and local governments to economize and reorder priorities. State and local governments have consistently financed 13-14 percent of national health expenditures (Table D). Between 1982 and 1990, this State and local share of spending is projected to drop slightly to approximately 12 percent.
Private financing
The private sector financed 58 percent of expenditures in 1982, a decline from 63 percent in 1970 (Table D). The private share is estimated to remain stable at approximately 58 percent over the projection period.
Private expenditures for health care are projected to reach $227 billion by 1984 and $397 billion by 1990. For the period 1982-90, private expenditures are estimated to increase at an average annual rate of approximately 10 percent.
Private health insurance premiums made up 45 percent of total private funding for National health care.4 Premiums have risen from $22 billion in 1972 to $84 billion in 1982, nearly a fourfold increase in only 10 years (Table 7). Premiums are projected to increase to $104 billion in 1984, $142 billion in 1987, and $183 billion in 1990.
Table 7. National health expenditures by type of expenditure and source of funds: Selected years 1972-90.
| Private | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Consumer | Public | ||||||||
|
|
|
||||||||
| Type of expenditure | Total | Total | Total | Patient direct | Health insurance | Other1 | Total | Federal | State and local |
|
| |||||||||
| Amount in billions | |||||||||
| 1972 | |||||||||
| Total | $ 93.5 | $ 58.1 | $ 53.4 | $ 31.0 | $ 22.4 | $ 4.7 | $ 35.4 | $ 22.9 | $12.5 |
| Health services and supplies | 86.9 | 54.8 | 53.4 | 31.0 | 22.4 | 1.5 | 32.1 | 20.6 | 11.4 |
| Personal health care | 80.2 | 51.4 | 50.1 | 31.0 | 19.1 | 1.3 | 28.8 | 18.9 | 9.9 |
| Hospital care | 34.9 | 16.3 | 15.8 | 3.8 | 12.0 | .5 | 18.6 | 12.4 | 6.2 |
| Physicians' services | 17.2 | 13.3 | 13.2 | 7.3 | 6.0 | (3) | 3.9 | 2.7 | 1.2 |
| Dentists' services | 5.6 | 5.3 | 5.3 | 5.0 | .3 | — | .3 | .2 | .1 |
| Other professional services | 1.8 | 1.5 | 1.5 | 1.2 | .3 | (3) | .3 | .2 | .1 |
| Drugs and medical sundries | 9.3 | 8.7 | 8.7 | 8.2 | .4 | — | .7 | .3 | 3 |
| Eyeglasses and appliances | 2.3 | 2.1 | 2.1 | 2.1 | (3) | — | .1 | .1 | (3) |
| Nursing home care | 6.5 | 3.4 | 3.4 | 3.4 | (3) | (3) | 3.0 | 1.7 | 1.4 |
| Other health services | 2.6 | .7 | — | — | — | .7 | 1.9 | 1.3 | .6 |
| Program administration and net cost of insurance | 4.7 | 3.5 | 3.3 | — | 3.3 | .2 | 1.2 | .7 | .5 |
| Government public health activities | 2.0 | — | — | — | — | — | 2.0 | 1.0 | 1.0 |
| Research and construction of medical facilities | 6.6 | 3.2 | — | — | — | 3.2 | 3.4 | 2.3 | 1.1 |
| Research2 | 2.4 | .2 | — | — | — | .2 | 2.1 | 1.9 | .2 |
| Construction | 4.2 | 3.0 | — | — | — | 3.0 | 1.2 | .4 | .9 |
| 1975 | |||||||||
| Total | $132.7 | $ 76.5 | $ 71.4 | $ 39.0 | $ 32.4 | $ 5.1 | $ 56.2 | $ 37.1 | $19.1 |
| Health services and supplies | 124.3 | 73.2 | 71.4 | 39.0 | 32.4 | 1.8 | 51.1 | 33.8 | 17.3 |
| Personal health care | 116.8 | 70.6 | 69.1 | 39.0 | 30.1 | 1.6 | 46.1 | 31.4 | 14.7 |
| Hospital care | 52.1 | 23.3 | 22.7 | 4.3 | 18.4 | .6 | 28.8 | 20.3 | 8.6 |
| Physicians' services | 24.9 | 18.4 | 18.4 | 9.0 | 9.4 | (3) | 6.5 | 4.6 | 1.9 |
| Dentists' services | 8.2 | 7.8 | 7.8 | 6.8 | 1.0 | — | .5 | .3 | .2 |
| Other professional services | 2.6 | 2.0 | 2.0 | 1.7 | .4 | (3) | .6 | .4 | .2 |
| Drugs and medical sundries | 11.9 | 10.9 | 10.9 | 10.2 | .7 | — | 1.0 | .5 | .5 |
| Eyeglasses and appliances | 3.2 | 2.9 | 2.9 | 2.8 | .1 | — | .2 | .2 | .1 |
| Nursing home care | 10.1 | 4.4 | 4.3 | 4.3 | .1 | .1 | 5.7 | 3.2 | 2.5 |
| Other health services | 3.7 | .9 | — | — | — | .9 | 2.8 | 2.0 | .8 |
| Program administration and net cost of health insurance | 4.4 | 2.6 | 2.4 | — | 2.4 | .2 | 1.8 | 1.2 | .7 |
| Government public health activities | 3.2 | — | — | — | — | — | 3.2 | 1.2 | 1.9 |
| Research and construction of medical facilities | 8.4 | 3.3 | — | — | — | 3.3 | 5.1 | 3.3 | 1.8 |
| Research2 | 3.3 | .3 | — | — | — | .3 | 3.1 | 2.8 | .3 |
| Construction of medical facilities | 5.1 | 3.1 | — | — | — | 3.1 | 2.0 | .5 | 1.5 |
| 1980 | |||||||||
| Total | $249.0 | $143.6 | $135.7 | $ 72.1 | $ 63.6 | $ 7.8 | $105.4 | $ 71.1 | $34.3 |
| Health services and supplies | 237.1 | 139.3 | 135.7 | 72.1 | 63.6 | 3.6 | 97.9 | 66.0 | 31.9 |
| Personal health care | 219.4 | 132.2 | 129.1 | 72.1 | 57.0 | 3.1 | 87.2 | 62.7 | 24.5 |
| Hospital care | 100.4 | 46.1 | 44.6 | 10.9 | 33.7 | 1.5 | 54.3 | 41.1 | 13.2 |
| Physicians' services | 46.8 | 34.3 | 34.3 | 17.8 | 16.5 | (3) | 12.5 | 9.5 | 3.0 |
| Dentists' services | 15.4 | 14.8 | 14.8 | 11.2 | 3.6 | — | .6 | .3 | .3 |
| Other professional services | 5.6 | 4.2 | 4.2 | 3.3 | .9 | .1 | 1.4 | 1.0 | .4 |
| Drugs and medical sundries | 19.3 | 17.7 | 17.7 | 15.7 | 2.0 | — | 1.6 | .8 | .8 |
| Eyeglasses and appliances | 5.1 | 4.6 | 4.6 | 4.3 | .3 | — | .5 | .5 | .1 |
| Nursing home care | 20.6 | 9.1 | 9.0 | 8.8 | .2 | .1 | 11.5 | 6.2 | 5.3 |
| Other health services | 6.0 | 1.4 | — | — | — | 1.4 | 4.6 | 3.2 | 1.4 |
| Program administration and net cost of insurance | 10.7 | 7.1 | 6.6 | — | 6.6 | .4 | 3.7 | 2.0 | 1.7 |
| Government public health activities | 7.0 | — | — | — | — | — | 7.0 | 1.3 | 5.7 |
| Research and construction of medical facilities | 11.8 | 4.3 | — | — | — | 4.3 | 7.5 | 5.1 | 2.4 |
| Research2 | 5.3 | .3 | — | — | — | .3 | 5.0 | 4.5 | .5 |
| Construction | 6.5 | 4.0 | — | — | — | 4.0 | 2.5 | .6 | 2.0 |
| 1981 | Amount in billions | ||||||||
| Total | $286.6 | $164.4 | $155.3 | $ 82.1 | $ 73.2 | $ 9.2 | $122.2 | $ 83.7 | $38.5 |
| Health services and supplies | 273.5 | 159.3 | 155.3 | 82.1 | 73.2 | 4.0 | 114.2 | 78.2 | 36.0 |
| Personal health care | 254.6 | 152.4 | 148.9 | 82.1 | 66.8 | 3.5 | 102.2 | 74.4 | 27.8 |
| Hospital care | 118.0 | 54.2 | 52.4 | 13.1 | 39.4 | 1.7 | 63.8 | 48.5 | 15.3 |
| Physicians' services | 54.8 | 39.7 | 39.7 | 20.7 | 19.0 | (3) | 15.1 | 11.7 | 3.3 |
| Dentists' services | 17.3 | 16.6 | 16.6 | 12.3 | 4.3 | — | .7 | .4 | .3 |
| Other professional services | 6.4 | 4.7 | 4.7 | 3.5 | 1.1 | .1 | 1.7 | 1.3 | .4 |
| Drugs and medical sundries | 21.3 | 19.5 | 19.5 | 17.1 | 2.4 | — | 1.9 | .9 | .9 |
| Eyeglasses and appliances | 5.7 | 5.1 | 5.1 | 4.7 | .3 | — | .7 | .6 | .1 |
| Nursing home care | 24.2 | 11.0 | 10.9 | 10.7 | .2 | .1 | 13.2 | 7.3 | 5.8 |
| Other health services | 6.9 | 1.6 | — | — | — | 1.6 | 5.3 | 3.7 | 1.7 |
| Program administration and net cost of insurance | 11.1 | 6.9 | 6.4 | — | 6.4 | .5 | 4.2 | 2.5 | 1.7 |
| Government public health activities | 7.7 | — | — | — | — | — | 7.7 | 1.3 | 6.4 |
| Research and construction of medical facilities | 13.1 | 5.1 | — | — | — | 5.1 | 8.0 | 5.5 | 2.6 |
| Research2 | 5.7 | .3 | — | — | — | .3 | 5.3 | 4.8 | .5 |
| Construction | 7.5 | 4.8 | — | — | — | 4.8 | 2.7 | .7 | 2.1 |
| 1982 | |||||||||
| Total | $322.4 | $185.6 | $174.7 | $ 90.4 | $ 84.2 | $10.9 | $136.8 | $ 93.2 | $43.7 |
| Health services and supplies | 308.3 | 179.5 | 174.7 | 90.4 | 84.2 | 4.8 | 128.7 | 87.5 | 41.2 |
| Personal health care | 286.9 | 171.2 | 167.0 | 90.4 | 76.6 | 4.2 | 115.7 | 83.7 | 32.0 |
| Hospital care | 135.5 | 63.5 | 61.3 | 16.4 | 44.9 | 2.2 | 72.0 | 54.6 | 17.4 |
| Physicians' services | 61.8 | 44.8 | 44.7 | 23.1 | 21.7 | (3) | 17.0 | 13.4 | 3.6 |
| Dentists' services | 19.5 | 18.7 | 18.7 | 13.4 | 5.2 | — | .8 | .4 | .4 |
| Other professional services | 7.1 | 4.9 | 4.9 | 3.6 | 1.3 | .1 | 2.2 | 1.7 | .5 |
| Drugs and medical sundries | 22.4 | 20.4 | 20.4 | 17.6 | 2.8 | — | 1.9 | .9 | 1.0 |
| Eyeglasses and appliances | 5.7 | 4.8 | 4.8 | 4.4 | .4 | — | .8 | .7 | .1 |
| Nursing home care | 27.3 | 12.3 | 12.2 | 11.9 | .2 | .2 | 15.0 | 7.9 | 7.1 |
| Other health services | 7.6 | 1.7 | — | — | — | 1.7 | 5.9 | 4.0 | 1.9 |
| Program administration and net cost of health insurance | 12.7 | 8.3 | 7.7 | — | 7.7 | .6 | 4.4 | 2.4 | 2.0 |
| Government public health activities | 8.6 | — | — | — | — | — | 8.6 | 1.4 | 7.3 |
| Research and construction of medical facilities | 14.1 | 6.0 | — | — | — | 6.0 | 8.1 | 5.7 | 2.4 |
| Research 2 | 5.9 | .3 | — | — | — | .3 | 5.6 | 5.0 | .5 |
| Construction of medical facilities | 8.2 | 5.7 | — | — | — | 5.7 | 2.5 | .7 | 1.9 |
| 1984 | |||||||||
| Total | $392.7 | $226.7 | $213.2 | $109.6 | $103.6 | $13.6 | $166.0 | $115.5 | $50.4 |
| Health services and supplies | 375.9 | 219.0 | 213.2 | 109.6 | 103.6 | 5.8 | 156.9 | 109.2 | 47.7 |
| Personal health care | 349.4 | 207.9 | 202.9 | 109.6 | 93.3 | 5.0 | 141.5 | 105.0 | 36.5 |
| Hospital care | 165.7 | 78.9 | 76.2 | 21.9 | 54.3 | 2.7 | 86.8 | 67.3 | 19.5 |
| Physicians' services | 76.1 | 53.5 | 53.5 | 27.7 | 25.8 | (3) | 22.5 | 18.3 | 4.3 |
| Dentists' services | 23.7 | 22.8 | 22.8 | 15.8 | 6.9 | 1.0 | .5 | .4 | |
| Other professional services | 8.9 | 5.7 | 5.6 | 3.9 | 1.7 | .1 | 3.2 | 2.5 | .7 |
| Drugs and medical sundries | 26.7 | 24.4 | 24.4 | 20.7 | 3.7 | — | 2.3 | 1.1 | 1.2 |
| Eyeglasses and appliances | 6.8 | 5.5 | 5.5 | 5.0 | .5 | — | 1.2 | 1.1 | .1 |
| Nursing home care | 32.7 | 15.1 | 14.9 | 14.6 | .3 | .2 | 17.6 | 9.4 | 8.2 |
| Other health services | 8.8 | 2.0 | — | — | — | 2.0 | 6.8 | 4.7 | 2.1 |
| Program administration and net cost of insurance | 16.1 | 11.1 | 10.3 | — | 10.3 | .8 | 5.0 | 2.8 | 2.3 |
| Government public health activities | 10.4 | — | — | — | — | — | 10.4 | 1.5 | 8.9 |
| Research and construction of medical facilities | 16.8 | 7.8 | — | — | — | 7.8 | 9.0 | 6.3 | 2.8 |
| Research2 | 6.5 | .4 | — | — | — | .4 | 6.2 | 5.6 | .6 |
| Construction | 10.3 | 7.4 | — | — | — | 7.4 | 2.9 | .7 | 2.2 |
| 1987 | Amount in billions | ||||||||
| Total | $529.8 | $307.2 | $288.9 | $147.4 | $141.5 | $18.3 | $222.5 | $157.5 | $65.0 |
| Health services and supplies | 508.3 | 296.6 | 288.9 | 147.4 | 141.5 | 7.7 | 211.7 | 150.0 | 61.7 |
| Personal health care | 471.3 | 279.7 | 273.0 | 147.4 | 125.7 | 6.7 | 191.6 | 145.0 | 46.6 |
| Hospital care | 226.7 | 110.1 | 106.4 | 33.0 | 73.4 | 3.7 | 116.6 | 92.2 | 24.4 |
| Physicians' services | 102.5 | 69.9 | 69.8 | 36.3 | 33.5 | (3) | 32.6 | 27.2 | 5.5 |
| Dentists' services | 30.9 | 29.7 | 29.7 | 20.0 | 9.8 | — | 1.2 | .6 | .5 |
| Other professional services | 12.3 | 7.9 | 7.8 | 5.4 | 2.5 | .1 | 4.3 | 3.4 | 1.0 |
| Drugs and medical sundries | 34.4 | 31.5 | 31.5 | 26.2 | 5.3 | — | 2.9 | 1.4 | 1.5 |
| Eyeglasses and appliances | 8.7 | 6.9 | 6.9 | 6.0 | .8 | — | 1.8 | 1.7 | .2 |
| Nursing-home care | 44.4 | 21.2 | 20.9 | 20.4 | .5 | .3 | 23.3 | 12.4 | 10.8 |
| Other health services | 11.3 | 2.5 | — | — | — | 2.5 | 8.8 | 6.1 | 2.7 |
| Program administration and net cost of insurance | 22.9 | 16.9 | 15.9 | — | 15.9 | 1.0 | 6.0 | 3.3 | 2.7 |
| Government public health activities | 14.0 | — | — | — | — | — | 14.0 | 1.6 | 12.4 |
| Research and construction of medical facilities | 21.5 | 10.7 | — | — | — | 10.7 | 10.9 | 7.6 | 3.3 |
| Research2 | 7.9 | .4 | — | — | — | .4 | 7.5 | 6.8 | .7 |
| Construction | 13.6 | 10.3 | — | — | — | 10.3 | 3.3 | .8 | 2.6 |
| 1990 | |||||||||
| Total | $690.4 | $396.8 | $373.8 | $190.5 | $183.3 | $23.0 | $293.5 | $211.4 | $82.1 |
| Health services and supplies | 664.2 | 383.7 | 373.8 | 190.5 | 183.3 | 9.9 | 280.5 | 202.2 | 78.3 |
| Personal health care | 619.0 | 363.9 | 355.4 | 190.5 | 164.8 | 8.5 | 255.0 | 196.5 | 58.6 |
| Hospital care | 303.6 | 148.7 | 143.7 | 46.4 | 97.3 | 5.0 | 154.9 | 124.7 | 30.2 |
| Physicians' services | 133.5 | 88.0 | 87.9 | 45.4 | 42.5 | (3) | 45.4 | 38.6 | 6.9 |
| Dentists' services | 38.9 | 37.5 | 37.5 | 24.7 | 12.8 | — | 1.4 | .7 | .6 |
| Other professional services | 16.1 | 10.1 | 9.9 | 6.5 | 3.4 | .1 | 6.0 | 4.6 | 1.5 |
| Drugs and medical sundries | 43.6 | 40.0 | 40.0 | 32.9 | 7.1 | — | 3.6 | 1.7 | 1.8 |
| Eyeglasses and appliances | 10.9 | 8.3 | 8.3 | 7.2 | 1.1 | — | 2.5 | 2.3 | .2 |
| Nursing home care | 58.4 | 28.4 | 28.0 | 27.3 | .7 | .4 | 30.1 | 16.1 | 14.0 |
| Other health services | 14.1 | 3.0 | — | — | — | 3.0 | 11.2 | 7.8 | 3.4 |
| Program administration and net cost of health insurance | 27.0 | 19.8 | 18.4 | — | 18.4 | 1.4 | 7.2 | 3.9 | 3.3 |
| Government public health activities | 18.3 | — | — | — | — | — | 18.3 | 1.8 | 16.4 |
| Research and construction of medical facilities | 26.2 | 13.1 | — | — | — | 13.1 | 13.0 | 9.2 | 3.8 |
| Research2 | 9.6 | .4 | — | — | — | .4 | 9.2 | 8.3 | .9 |
| Construction of medical facilities | 16.6 | 12.7 | — | — | — | 12.7 | 3.9 | .9 | 3.0 |
Spending by philanthropic organizations, industrial in-plant health services and privately financed construction.
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but are included in the expenditure class in which the product falls.
Less than $50 million.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
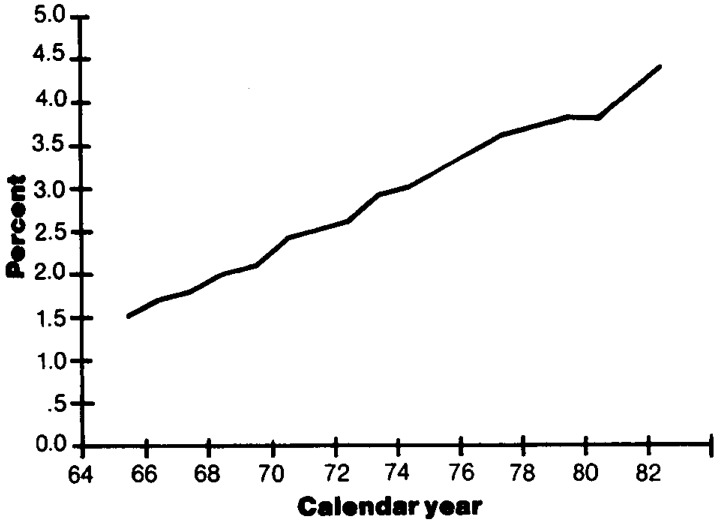
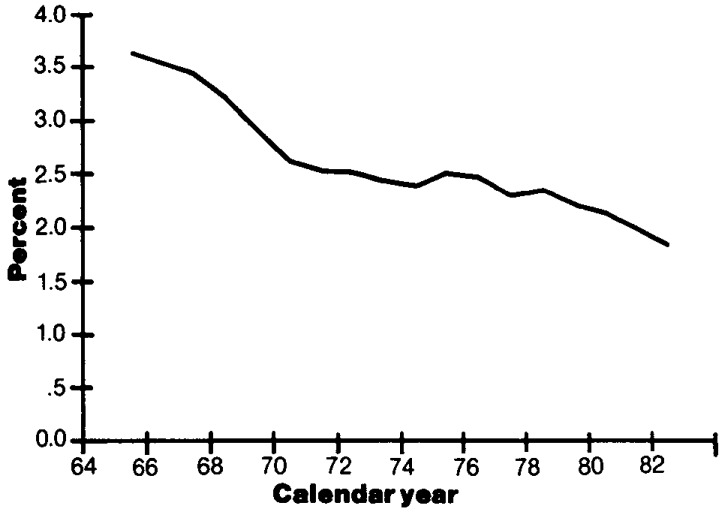
The employer share of private health insurance premiums has been an increasing cost to employers. Such premiums have risen at an average annual rate of 15 percent over the period 1972-82, reaching nearly $66 billion in 1982 (Table G). Employers also make contributions to the Medicare Hospital Insurance Trust Fund, and these contributions have risen from $2.7 billion in 1972 to $16.4 billion in 1982, an average annual rate of increase of nearly 20 percent. During this same period, total employee compensation increased at an average rate of only 10 percent, resulting in an increased share allocated to health costs. In 1950, the employer contribution to group health insurance was one-half of 1 percent of total employee compensation. By 1972, this share, adjusted to include the contributions to the Medicare Hospital Insurance Trust Fund, was 2.6 percent, and in 1982, the share had risen to 4.4 percent (Figure 7 and Table G).
Table G. Employer contributions for health insurance and total employee compensation: Selected years 1950-82.
| Employer contributions for health insurance | Employee compensation | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Calendar year | Private health insurance premiums | Federal hospital insurance, Medicare | Total | Wages and salaries | Supplements to wages and salaries | Total | Contributions for health insurance as percent of total compensation |
|
| |||||||
| Amount in billions | |||||||
| 1950 | $ 0.7 | (1) | $ 0.7 | $ 147.0 | $ 7.8 | $ 154.8 | 0.5 |
| 1955 | 1.7 | (1) | 1.7 | 211.7 | 13.2 | 224.9 | 0.8 |
| 1960 | 3.4 | (1) | 3.4 | 271.9 | 23.0 | 294.9 | 1.2 |
| 1965 | 5.9 | (1) | 5.9 | 362.0 | 34.6 | 396.6 | 1.5 |
| 1966 | 6.4 | $ 1.0 | 7.4 | 398.4 | 41.0 | 439.4 | 1.7 |
| 1967 | 6.9 | 1.5 | 8.4 | 427.0 | 44.4 | 471.4 | 1.8 |
| 1968 | 8.4 | 2.1 | 10.5 | 469.6 | 50.3 | 519.9 | 2.0 |
| 1969 | 9.9 | 2.3 | 12.2 | 515.7 | 57.2 | 572.9 | 2.1 |
| 1970 | 12.1 | 2.3 | 14.4 | 548.7 | 63.3 | 612.0 | 2.4 |
| 1971 | 13.7 | 2.4 | 16.1 | 581.5 | 70.7 | 652.2 | 2.5 |
| 1972 | 16.2 | 2.7 | 18.9 | 635.2 | 82.8 | 718.0 | 2.6 |
| 1973 | 18.0 | 5.3 | 23.3 | 702.6 | 98.7 | 801.3 | 2.9 |
| 1974 | 20.7 | 5.4 | 26.1 | 765.2 | 112.3 | 877.5 | 3.0 |
| 1975 | 24.0 | 5.6 | 29.6 | 806.4 | 125.0 | 931.4 | 3.2 |
| 1976 | 28.8 | 6.2 | 35.0 | 889.9 | 146.4 | 1,036.3 | 3.4 |
| 1977 | 34.5 | 6.9 | 41.4 | 983.2 | 168.9 | 1,152.1 | 3.6 |
| 1978 | 39.3 | 8.6 | 47.9 | 1,106.5 | 194.6 | 1,301.1 | 3.7 |
| 1979 | 44.2 | 10.6 | 54.8 | 1,237.4 | 220.7 | 1,458.1 | 3.8 |
| 1980 | 49.8 | 11.6 | 61.4 | 1,356.6 | 243.0 | 1,599.6 | 3.8 |
| 1981 | 57.3 | 15.9 | 73.2 | 1,493.2 | 276.0 | 1,769.2 | 4.1 |
| 1982 | 65.7 | 16.4 | 82.1 | 1,568.1 | 297.5 | 1,865.6 | 4.4 |
Not applicable.
SOURCE: Bureau of Economic Analysis (1981, 1983).
Figure 7. Employer contributions for health insurance as percent of total employee compensation: 1965-821.
1Employer contributions for private health insurance premiums and for Federal hospital insurance (Medicare) taxes are included. Also see Table G.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The increasing cost of employer-paid health costs relative to total compensation has led to numerous private sector initiatives to reduce the rate of increase of health care costs. Employers increasingly include cost-containment features in their group coverages. In one recent survey of new group policies, 79 percent of the employees had reimbursement for prescriptions on a generic basis; 76 percent had coverage for second opinions on surgery; 85 percent, for preadmission testing; and 85 percent, for outpatient surgery (Health Insurance Association of America, 1983b). Employers are also making increasing use of HMO's (Blostin and Marclay, 1983) and self-funding of health benefits (Cain, 1983; Harker, 1981). Major reasons for self-funding are these: elimination of State premium taxes, averaging 2 to 3 percent of premiums; improved cash flow (a one-shot, temporary factor); the earning of a higher interest rate on reserves held to pay benefits; and the availability of third-party administrators, many of whom claim to be able to monitor and control costs more effectively than traditional insurers.
International experience
Relatively high rates of growth in health care expenditures are not unique to the United States. Economy-wide inflation, growth in real income, demographic shifts, and innovative, but cost-increasing, technologies have been associated with rising health care costs in selected western industrialized countries studied.
In one such study of the rising cost of health care among nine industrialized countries for 1969-76, expenditures increased at average annual rates of less than 13 percent (United States) to over 20 percent (Australia) (Table H). In all nine countries, health expenditures increased as a proportion of GNP. While the United States is among the highest when ranked according to percentage of GNP spent on health care, the Federal Republic of Germany topped the list with nearly 10 percent of GNP spent on health care for the year 1975 (the latest available data in the study).
Table H. National health expenditures in nine industrialized countries, average annual percent change, and percent of gross national product: 1969 and 19761.
| National health expenditures | |||
|---|---|---|---|
|
|
|||
| Country (ranked by 1969-76 increase in health expenditures) | Average annual percent change 1969-76 | Percent of gross national product | |
|
| |||
| 1969 | 1976 | ||
| Australia | 20.5 | 5.6 | 7.7 |
| Finland | 18.9 | 6.0 | 7.2 |
| Netherlands | 18.4 | 6.0 | 8.5 |
| United Kingdom | 18.2 | 4.5 | 5.8 |
| Federal Republic of Germany | 17.7 | 6.3 | 29.7 |
| France | 16.5 | 6.3 | 8.2 |
| Sweden | 14.6 | 7.2 | 28.7 |
| Canada | 14.3 | 6.8 | 7.1 |
| United States3 | 12.5 | 7.0 | 8.7 |
National health expenditures as percent of gross national product were not available for 1976. The 1975 ratios are given. See Simanis and Coleman (1980).
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Growth in international health care spending is highly correlated with increases in income (Newhouse, 1977), and income appears to be a more important determinant of growth than whether the source of funding is public or private (Kleiman, 1974). Nations have financed these spending increases with different mixes of private and public spending, but the result has been approximately the same—higher incomes result in additional spending on health (Kleiman, 1974).
As health care garners an ever-increasing share of nations' incomes around the world, the nature of care appears to be shifting toward care that emphasizes the caring function, rather than the curing function—relieve anxiety, alleviate symptoms, and provide prognostic information (Newhouse, 1977).
The degree of inequality that nations accept in the distribution of health care is typically less than the degree of inequality found acceptable in the distribution of income (Kleiman, 1974; Tobin, 1970); because of this, the distribution of health care services usually has significant governmental involvement.
Just as new technologies diffuse through national health care systems (Cromwell and Kanak, 1982; Russell, 1979), they also diffuse through the western industrialized countries and Japan (Banta and Russell, 1981). For example, the computerized axial tomography (CAT) scanner was developed in Britain, and techniques for renal dialysis were developed in the Netherlands (Banta and Russell, 1981).
The United States is a major contributor to this diffusion, exporting and importing substantial amounts of medical equipment. In 1982, the United States exported one-third of its domestic production of X-ray and electro-medical equipment (Table I). These exports have increased at an average annual rate of almost 30 percent for the period 1972-82 (Table I). On the other hand, nearly one-fifth of our domestic consumption of X-ray and electro-medical equipment in 1982 was imported (Table I). Over the last 10 years, imports of surgical and medical instruments, surgical appliances and supplies, and X-ray and electromedical equipment have each increased at average annual rates of 20 percent or more (Table I). Our major international trading partners leading to this technology diffusion are West Germany, Japan, the United Kingdom, Canada, and the Netherlands (Table J).
Table I. Exports and imports of medical equipment, supplies, and drugs: 1982.
| Category of equipment, supplies, or drugs | Estimated value of product shipments in millions | Estimated value of exports in millions | Estimated value of imports in millions | Exports as percent of shipments | Imports as percent of new supply1 | Imports as percent of apparent consumption2 | Average annual percent increase 1972-82 | ||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Value of product shipments | Value of exports | Value of imports | |||||||
| X-ray and electromedical equipment | $ 2,977 | $1,008 | $445 | 33.9 | 13.0 | 18.4 | 22.8 | 28.7 | 21.0 |
| Surgical and medical instruments | 3,537 | 632 | 213 | 17.9 | 5.7 | 6.8 | 13.6 | 16.2 | 22.9 |
| Surgical appliances and supplies | 4,283 | 388 | 113 | 9.1 | 2.6 | 2.8 | 14.1 | 17.6 | 20.2 |
| Dental equipment and supplies | 1,333 | 148 | 52 | 11.1 | 3.8 | 4.2 | 14.2 | 15.8 | 14.9 |
| Biological products | 1,840 | 416 | 31 | 22.6 | 1.6 | 2.1 | 14.0 | 21.8 | 16.0 |
| Medicinals and botanicals | 3,877 | 1,422 | 975 | 36.7 | 20.1 | 28.4 | 17.2 | 15.3 | 15.9 |
| Pharmaceutical preparations | 17,177 | 488 | 29 | 2.8 | 0.2 | 0.2 | 10.6 | 10.4 | 7.2 |
New supply is the sum of product shipments plus imports.
Apparent consumption is the sum of product shipments plus imports less exports.
SOURCE: Bandy (1983) and Mclntyre (1983).
Table J. Major international trading partners of the United States in medical and dental instruments and supplies: Trade shares in 1981.
| Country | Percent |
|---|---|
| U.S. exports | |
| Total | 100 |
| Canada | 14 |
| Japan | 11 |
| West Germany | 8 |
| The United Kingdom | 7 |
| The Netherlands | 6 |
| Other | 54 |
| U.S. imports | |
| Total | 100 |
| West Germany | 29 |
| Japan | 20 |
| The United Kingdom | 6 |
| Canada | 6 |
| The Netherlands | 5 |
| Other | 34 |
SOURCE: Bandy (1983).
The United States also exports and imports drugs and biological, botanical, and medicinal products. Approximately one-fifth of biological products and over one-third of medicinals and botanicals produced in the United States are exported, but U.S. international trade in pharmaceutical preparations is insignificant (Table I). However, U.S. firms have subsidiaries or other corporate operations abroad, and foreign firms have subsidiaries and corporate operations in the United States (Pharmaceutical Manufacturers' Association, 1981); therefore, the diffusion of information, laboratory techniques, and products is more pervasive than indicated by these international trade statistics. Some 30-40 percent of sales of major U.S. drug firms come from foreign operations (McIntyre, 1983).
This international diffusion of medical equipment, supplies, and drugs, combined with diffusion of biomedical research results, leads to potential linkages in medical practice patterns and cost-price spirals in the western industrialized world. However, the extent to which convergence among nations in medical practice is occurring because of this technology diffusion is difficult to ascertain.
Outside the western industrialized world, some factors in holding down costs can be discerned. In centrally planned economies such as the Soviet Union and China, costs are contained by use of low technologies and by payment of relatively low wages to health care sector employees (Davis, 1983; Dobson, 1981; Feshbach, 1983; Knaus, 1981). In the developing countries, health care spending is typically a much lower proportion of the GNP than in the western industrialized countries, and improvements in health status and medical practice patterns are increasingly viewed as an integral part of overall economic development. For development planners, this is a marked shift in thinking from the 1950's and 1960's when spending on health care was not considered so advantageous from a benefit-cost view of economic development (Golladay, 1980; Golladay and Liese, 1980). Emphasis is now being given to providing low-technology, low-wage primary health care to the masses. It is alleged that health status can be substantially improved with relatively low cost and that higher labor force participation, labor productivity, and the like will result.
Some analysts of international health care spending suggest that health care spending as a proportion of GNP tends to grow in spurts. Countries appear to employ relatively effective methods to stem the rise in health spending relative to GNP, and then slippage in the system results in health spending escalating relative to GNP.
Nations implicitly or explicitly make judgments as to the “correct” ratio of GNP allocated to health care. Finland is reported to have earmarked 15 percent of GNP for health care under the assumption that health care is socially desirable and that employment in the health sector is as beneficial to the general economy as any other type of employment (Perspective, 1982). On the other hand, several western industrialized countries have recently modified and restricted social programs covering the health care sector because of the excessive burden on public sector financing during sluggish economic growth (Zeiter, 1983); one study forecasts that health spending increases in the developed world will slow in the 1980's as cost-effective changes in health delivery systems and finance are incorporated (Predicasts, Inc., 1983).
Explaining the rise in expenditures
Many theories account for the rising cost of health care expenditures. The projection process uses a five-factor formula that accounts for how expenditures increase. The five how factors are changes in the following: 1) general inflation, 2) aggregate population, 3) medical care price increases in excess of general price inflation, 4) per capita visits and patient days, and 5) the mix and content of services and supplies per visit or day (the intensity factor). All increases may be attributed to one of these five factors (see Tables K and L and Figure 8)—two relating to the general economy and three specific to the health care sector. The last factor, changes in the mix and content of services and supplies per visit or patient day, is calculated as a residual, and the five factors combine to form an accounting identity.
Table K. How versus why medical care expenditures rise1.
| How medical care expenditures rise | Why medical care expenditures rise |
|---|---|
| Economy-wide factors | |
| 1. General inflation | 1. Monetary policies; fiscal policies relating to taxing, spending, and debt management; supply-side shocks such as energy price increases, food price increases caused by world-wide droughts, Social Security tax rate increases, and minimum wage increases; productivity changes; and monopoly powers of firms and unions over prices and wages. |
| 2. Aggregate population growth | 2. Birth rates, death rates, in-migration, out-migration. |
| Health sector-specific factors | |
| 3. Growth in per capita patient visits or per capita patient days | 3. Factors influencing the demand for and supply of medical care services:
|
| 4. Changes in the nature of services and supplies provided per visit or per patient day (product innovation, intensity of services, amenities, and so forth)2 | 4. Generally, the same factors as in (3) above; however, the relative importance of particular factors may differ. |
| 5. Medical care price increases relative to general price inflation (GNP deflator) | 5. This measures change in medical care prices relative to overall prices in the economy. It captures the interplay of (1) demand-pull inflationary forces (such as changes in deductibles and coinsurance); (2) cost pressures specific to the industry; (3) supply-side pricing behavior; (4) supply-side productivity behavior, and so on. In general, medical care prices increase faster than the GNP deflator. During periods of high growth in commodity and energy prices, the differential between medical care prices and economy-wide prices usually narrows. In addition, when overall price increases in the economy decelerate, medical care price increases typically decelerate with a marked lag. Generally, the same factors as in (3) cause the differential rates of price increase; however, the relative importance of particular factors may differ and, in some cases, the sign of the factor may differ. For example, increasing the number of dentists relative to population in a given geographic area may cause dental prices to rise more slowly than would otherwise be the case and to expand utilization of dental services in the geographic area. In other words, expanding the supply of dentists, all other things constant, may have a negative impact on price increases, but a positive impact on visits and intensity of services per visit. |
Martin Feldstein (1971) has made this distinction between how vs. why medical expenditures have risen. For analyses accounting for expenditure growth using the how approach, see M. Feldstein (1971, 1981); Klarman et al. (1970); and Mushkin (1979).
This factor is calculated as a residual by deflating current dollar expenditures per visit or per patient day by a relevant price index. This yields growth in real services or intensity per visit or per day. Since the five measured components (general inflation, aggregate population growth, growth in per capita visits or days, medical care price increases relative to general price inflation, and growth in total expenditures) are each subject to sampling variability and measurement error, it is important to interpret the residual category with caution. For example, if through unpackaging or unbundling of services (that is, separating services and procedures into finer components) and billing individually for each service or procedure, it may result in greater total revenues for a fixed volume and mix of services. Thus, effective price increases are greater than shown by National price measures, which do not reflect such unbundling or unpackaging. If the National price index (not reflecting unpackaging) is used to calculate the residual, it will result in lower price increases and higher residual growth than if the true (unbundled) price increases were used.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Table L. Factors accounting for growth in expenditures for selected categories of total systems cost: 1972-821 2.
| Factors accounting for how medical care expenditures rise | Community hospital care | Federal hospitals | Physicians' services | Dentists' services | Nursing home care excluding ICF-MR | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Inpatient expenses3 | Outpatient expenses3 | ||||||
|
| |||||||
| Inpatient days | Admissions | ||||||
|
| |||||||
| Percent | |||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Economy-wide factors | |||||||
| 1. General inflation | 51.5 | 51.6 | 42.4 | 67.6 | 57.3 | 59.2 | 55.3 |
| 2. Aggregate population growth | 6.9 | 6.9 | 5.7 | 9.1 | 7.7 | 8.0 | 7.4 |
| Health sector-specific factors | |||||||
| 3. Growth in per capita visits or patient days | 3.1 | 6.8 | 13.8 | 4−29.4 | −5.2 | 9.5 | 16.6 |
| 4. Growth in real services per visit or per day (intensity) | 25.4 | 21.7 | 27.4 | 543.8 | 27.4 | 20.5 | 13.8 |
| 5. Medical care price increases in excess of general price inflation (GNP deflator) | 13.0 | 13.0 | 10.7 | 9.0 | 12.8 | 2.8 | 6.8 |
For derivation of the method used to allocate factors, see Klarman et al., 1970.
Total systems cost is called “personal health care” in Gibson et al., 1983.
Community hospital expenses are split into inpatient and outpatient expenses using the American Hospital Association (1983) procedure.
Inpatient days is used as the indicator of per capita utilization.
Expenses associated with hospital outpatient care are included with this residual category.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Figure 8. Factors accounting for growth in expenditures for community hospital inpatient care: 1972-82.
From a behavioral (or why) point of view, the causal factors for each of the five how factors are analyzed (Table K). During the projection process, growth rates for the how factors are determined by analyzing and evaluating the effects of the why factors. For example, with nursing homes, increases in the aged 75 and over population (a why factor) was examined as one determinant of growth in nursing home days per capita (a how factor).
General inflation, a how factor, accounted for approximately 58 percent of the increase in total systems cost (personal health care) for the period 1972-82 (Figure 9 and Table 8). General inflation (an overall increase in prices) results from a combination of factors, including monetary policy, fiscal policy, and supply-side shocks, such as energy price increases, productivity changes, and so forth (Table K).
Figure 9. Factors accounting for growth in total systems cost: 1972-82.
Table 8. Factors accounting for growth in selected categories of national health expenditures: 1972-19821.
| Factors accounting for how medical care expenditures rise | Total personal health care | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Other health services | Public health activities | State-and local-financed Government public health activities | Medical research | Federally financed medical research |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Percent | |||||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Economy-wide factors | |||||||||
| General inflation | 57.7 | 53.3 | 83.6 | 79.4 | 68.8 | 50.0 | 37.0 | 79.8 | 75.0 |
| Aggregate population growth | 7.7 | 7.2 | 11.2 | 10.7 | 9.2 | 6.7 | 5.0 | 10.7 | 10.1 |
| Health sector-specific factors | |||||||||
| Growth in per capita visits or patient days | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Growth in real services per visit or per day (intensity) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Medical care price increases relative to general price inflation | 9.5 | 0.3 | −6.7 | −19.4 | 16.7 | −1.0 | −0.2 | 3.0 | 2.8 |
| Addenda: Growth in real services per capita | 25.1 | 39.3 | 11.9 | 29.3 | 5.3 | 44.3 | 58.2 | 6.5 | 12.1 |
See Table K for method used to calculate relative contributions.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Overall inflation is clearly the most important factor accounting for health care expenditure growth; however, health care sector-specific factors, relating to the demand for and supply of medical care services, must be examined to understand the flow of real resources into the health care sector relative to the rest of the economy.
Factors contributing to this rapid growth in health spending are numerous and interrelated (National Commission on the Cost of Medical Care, 1978). The interplay of demand pressures and supply incentives contribute to the growth in specific types of medical expenditures. Two factors are particularly noteworthy: first, a demand-side factor: the role of third-party payments in increasing consumer demand for services; and second, a supply-side factor: the fee-for-service and cost-based reimbursement systems that lack incentives to provide health care in the least expensive manner.
Third-party payments
The third-party financing of health care increases demand for services and incorporates incentives for increasing costs. Increases in health care prices and expenditures are not only correlated to increases in insurance coverage, but also to the levels of such coverage (National Commission on the Cost of Medical Care, 1978; Newhouse, 1978). As third-party payments cover larger proportions of consumers' costs, providers and consumers of health care appear to increasingly treat it as a free service at the time of decisionmaking; this results in increased consumer demand for services. For example, with hospitals, the proportion paid out-of-pocket has remained at roughly 10 percent from 1967 through 1982, yet community hospital revenues during this period have increased at an average annual rate of almost 16 percent. From 1979 to 1982, community hospital revenues rose 63 per cent, while a broad-based measure to finance such care, the GNP, rose 27 percent. Third-party payments play a very significant role in increasing access to quality care, but they also have the effect of divorcing utilization and price from ability to pay at the individual level and, to a lesser extent, at the aggregate level.
Third-party payment growth is stimulated by the provision of tax subsidies for private health insurance. These subsidies provide incentives to purchase more insurance than would otherwise be the case (Congressional Budget Office, 1980; Feldstein, 1981; Greenspan and Vogel, 1980). The additional insurance then encourages further use of health care.
Reimbursement incentives
Third-party reimbursement systems often incorporate incentives to increase costs (Enthoven, 1980). Retrospective cost-based reimbursement for hospitals and fee-for-service reimbursement for physicians reward those providers who supply larger quantities and more costly services. An incentive is, therefore, provided to adopt new diagnostic and therapeutic procedures and techniques (product-innovative technologies), rather than to adopt new processes to more efficiently produce existing procedures and techniques (process-innovative technologies) (Altman and Blendon, 1979; Feldstein, 1981). The Medicare PPS for hospital inpatient services is a major step in the direction of increasing efficiency and effectiveness. It rewards adoption of cost-decreasing technologies and penalizes adoption of cost-increasing technologies.
Information diffusion
The diffusion of information relating to new techniques, procedures, and supplies (for example, implants, transplants, CAT scans, life-saving drugs, and so forth) can push up demand. First, as consumers become aware of techniques, procedures, and supplies through the mass media, they may pressure providers to make them available. Second, consumers frequently purchase more comprehensive insurance at higher premium rates to get reimbursement for more expensive procedures and techniques (Feldstein, 1981). Political pressure may be applied to include such innovations under public programs. Third, increased awareness can be associated with greater utilization of health services. Detailed physical examinations may diagnose conditions that cannot be cured with today's state-of-the-art medicine, but which may result in expensive maintenance programs.
Productivity performance
It has frequently been alleged that productivity levels for the health services sector are lower than in the overall economy, that the rate of increase in productivity is slower than in the private sector, and that significant increases can potentially be made in current productivity levels. It is hard to document these assertions, but there is fragmentary evidence on health sector wages, prices, and productivity to suggest that relatively poor productivity performance contributes to health sector price increases.
If productivity or output per hour increases faster in the nonhealth sector than in the health sector, and wages increase at the same rate in both sectors, then unit costs in the health sector must increase faster than in the nonhealth sector (Mushkin et al., 1978). Between 1972 and 1982, wages in the health care sector increased at an average annual rate of 8.4 percent compared with 7.6 percent in the total private economy (Bureau of Labor Statistics, Employment and Earnings). During the period 1973-81, productivity in the health services industry declined at an average annual rate of 0.6 percent per year, while productivity in the private nonfarm economy increased at an average annual rate of 0.4 percent (Table M).5 The medical care services component of the Consumer Price Index rose at an average annual rate of 10 percent between 1972 and 1982, compared with an 8 percent rate for the fixed-weight personal consumption expenditure price index (Bureau of Economic Analysis, Survey of Current Business). Thus, medical care services prices increased at an average annual rate of 25 percent faster than overall consumer prices. Price data were used, rather than unit cost data, since cost data were not available for either the health care sector or for the total private economy.6
Table M. Average annual percent change in productivity, by selected industries: 1973-81 1.
| Selected industry | Percent change in productivity1 |
|---|---|
| Services | 0.1 |
| Health | −0.6 |
| Business | 0.1 |
| Other | 0.2 |
| Finance, insurance and real estate | 0.3 |
| Manufacturing | 1.1 |
| All private industries | 0.4 |
Productivity is calculated by dividing gross product originating (1972 dollars) by the number of persons engaged in production. “Gross product originating” represents each respective industry's contribution to the “gross domestic product.” See Bureau of Industrial Economics (January 1983, p. XXI).
High price increases in the medical care services segment may be partially explained by the lower productivity increases in the health care sector.7 The relatively high price increases, combined with an inelastic demand for medical care services (Newhouse and Phelps, 1976; Newhouse et al., 1981), contributes to the increase in expenditures for health care relative to the GNP.
Physician-induced demand
Another hypothesis relating to increasing costs is that some physicians may induce demand for their services (Cotterill, 1979; Reinhardt, 1978). The patient's dependence upon the physician for diagnostic and treatment decisions interacts with third-party payments to provide the means for physicians to raise fees and increase intensity of services. According to the physician-induced demand and target-income models, increases in the number of physicians are associated with increases in expenditures for their services. This relationship becomes more important when the interaction of physicians' services and other related health services is noted (Blumberg, 1979). Blumberg estimates that physicians influence approximately 70 percent of total systems cost (personal health care expenditures). Thus, according to this hypothesis, the number of physicians is correlated not only with expenditures for physicians' services, but also with expenditures for hospital care, other professional services, drugs, and so forth.
Between 1965 and 1982, the number of active physicians increased at an average annual rate of 3.0 percent, triple the rate for population increase. For the period 1982-90, the Bureau of Health Professions projects that the number of active physicians will increase at an average annual rate of 2.7 percent (Table 4). This increase in the number of physicians is likely to be associated with increases in per capita and aggregate health expenditures, especially for services significantly covered by third-party payments. If insurance pays all costs, the physician's pricing behavior has little effect on market shares (Congressional Budget Office, 1982). For example, if a market area has full insurance coverage (no consumer cost sharing), an individual physician can raise fees without services becoming less attractive (from a price point of view) at the time of purchase. Proposals to increase consumer cost sharing will thus induce increased price competition in the health care sector.
Income and demographics
Increases in real income and shifts in the age distribution of the population toward the more aged segment expands demand (Denton and Spencer, 1975; Dresch et al., 1981; Russell, 1981; Torrey, 1982).
Psychological factors
An important factor, sometimes overlooked, is that achieving satisfaction in all areas of life is conditioned on, and affected by, one's subjective feeling of health status. If one does not feel well, other satisfactions (material and nonmaterial) are typically diminished and, in some cases, eliminated. Psychological factors (attitudes, aspirations, expectations, motivations, past experiences, and so forth) are important in understanding economic behavior in general (Alhadeff, 1982; Katona, 1975; Maital, 1982; Scitovsky, 1976), but such factors are especially important in understanding consumer and provider behavior in health care markets. Pain, guilt, uncertainty, and the subjectivity of well-being (from the point of view of the patient, the family, and the physician) can put significant pressures on patients, their families, and providers to utilize quantities and qualities of health care that may appear excessive when viewed from a strictly cost-benefit point of view. Consequently, the increasing percent of the GNP allocated to health (historical and projected), in part, reflects this perceived linkage between our health care system and our physical and emotional well-being, indeed, life itself.
Monetization of household activities
Another factor is that some services once provided for free by household members are now provided by health professionals (Fuchs, 1979). This factor contributes to growth in the health care sector and is of particular importance for one of the fastest growing services, long-term care (Chiswick, 1976). The increasing proportion of females 16 years of age and over in the labor force contributes to the shift in providing services. This proportion has increased from 39 percent in 1965 to 53 percent in 1982 (Council of Economic Advisors, 1983), resulting in a smaller number of people available for productive, nonpaying work in the household. Because more women are working, the opportunity cost of providing unpaid personal care services for relatives and friends has increased. In addition, the size of the average household decreased from 3.3 persons in 1965 to 2.7 in 1982, a decline of 18 percent (Bureau of the Census, 1983). As average household size decreases because of social, economic, and demographic forces, there are fewer household members to provide personal care.
As more women join the labor force and as the average household size decreases, some long-term care activities have been pushed out of the household and into the for-pay health care sector. It is also likely that increased third-party payments for coverage of health services in nursing homes and hospitals have increased this trend.
Total systems cost per capita
When projecting health spending, estimating the costs of a public program (such as the Medicare PPS), and evaluating regulatory policy, an insurance benefit package, or a marketing strategy, it is important to have a comprehensive definition of costs. This is so because each of these analyses is likely to have direct and indirect effects on health care utilization, quality, and price. Total systems cost per capita (TSCPC) provides such comprehensive definition of costs.
Total systems cost per capita includes all health care costs related to direct patient care: long-term and short-term, inpatient and outpatient, and covered and noncovered by third-party reimbursement. TSCPC includes all services and supplies in the personal health care category (Gibson et al., 1983), such as hospital care, physicians' services, drugs, nursing home care, and so forth (Table N). Thus, the net effect of all the causal factors on spending for health care can be summarized in TSCPC.
Table N. Percent distribution of total systems cost, by type of service: Selected years 1950-90.
| Type of personal health care expenditure
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Calendar year | Current dollars
|
Total systems cost | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services | |
| Total systems cost per capita in dollars | Total systems cost in billions | ||||||||||
|
| |||||||||||
| Percent distribution | |||||||||||
| Historical estimates | |||||||||||
| 1950 | $ 70 | $ 10.9 | 100.0 | 35.4 | 25.2 | 8.8 | 3.6 | 15.9 | 4.5 | 1.7 | 4.8 |
| 1960 | 129 | 23.7 | 100.0 | 38.4 | 24.0 | 8.3 | 3.6 | 15.4 | 3.3 | 2.2 | 4.7 |
| 1965 | 181 | 35.8 | 100.0 | 38.8 | 23.7 | 7.9 | 2.9 | 14.5 | 3.3 | 5.8 | 3.2 |
| 1970 | 312 | 65.1 | 100.0 | 42.6 | 22.0 | 7.3 | 2.4 | 12.3 | 3.0 | 7.2 | 3.2 |
| 1972 | 376 | 80.2 | 100.0 | 43.6 | 21.4 | 7.0 | 2.2 | 11.6 | 2.8 | 8.1 | 3.3 |
| 1975 | 531 | 116.8 | 100.0 | 44.6 | 21.4 | 7.1 | 2.2 | 10.2 | 2.7 | 8.6 | 3.2 |
| 1980 | 947 | 219.4 | 100.0 | 45.8 | 21.4 | 7.0 | 2.6 | 8.8 | 2.3 | 9.4 | 2.7 |
| 1981 | 1,088 | 254.6 | 100.0 | 46.3 | 21.5 | 6.8 | 2.5 | 8.4 | 2.2 | 9.5 | 2.7 |
| 1982 | 1,215 | 286.9 | 100.0 | 47.2 | 21.5 | 6.8 | 2.5 | 7.8 | 2.0 | 9.5 | 2.7 |
| Projections | |||||||||||
| 1984 | 1,452 | 349.4 | 100.0 | 47.4 | 21.8 | 6.8 | 2.5 | 7.6 | 1.9 | 9.4 | 2.5 |
| 1987 | 1,907 | 471.3 | 100.0 | 48.1 | 21.8 | 6.6 | 2.6 | 7.3 | 1.8 | 9.4 | 2.4 |
| 1990 | 2,442 | 619.0 | 100.0 | 49.0 | 21.6 | 6.3 | 2.6 | 7.0 | 1.8 | 9.4 | 2.3 |
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The TSCPC shows significant geographic variation in levels and rates of change over time, although there appears to be a pattern of convergence toward the U.S. average of TSCPC, at least over the period 1966-78 (Levit, 1982). The Medicare PPS provides additional pressures toward convergence since the system will evolve toward National rates of payment per discharge (adjusted for area wages and case-mix).
The TSCPC concept captures indirect effects and leakages. If, for example, the Medicare PPS restrains growth in hospital inpatient costs, but implicitly provides pressures to substitute less expensive ambulatory and nursing home care, TSCPC will capture the leakage from one health service type to another. Leakage from one service type into others may result in significant savings when the total net effect is considered.
These are some questions relating to TSCPC:
What is the magnitude of the leakage?
Is the nature of the leakage socially desirable; that is, what services and payers are affected, and what happens to prices, utilization, quality, and access for various socio-economic groups?
Does TSCPC increase or decrease as it is related to the specific policy, regulation, or marketing strategy?
To provide further insight on leakage and indirect effects, good health, as a concept, is examined. This includes good health as the ultimate output of the health care sector and the substitutional and complementary relationships of various inputs used to produce good health. This concept is fundamental to understanding the intended and likely consequences of the Medicare PPS as its effects reverberate through our health care delivery system in the 1980's. Good health can be viewed as the primary output of the health care sector with various types of health services and supplies, environmental health programs, health education, lifestyle changes, and the like, as inputs used to produce this good health (Feldstein, 1979).
Two types of interdependent relationships, substitutability and complementarity, are critical to understand when analyzing cost-effective methods to produce quality health care with attendant improved health status. Substitute services and goods serve similar purposes so that the purchaser of care or the decision maker (for example, the physician) can choose from among the set of substitutes that meet his or her objectives. For example, organized hospital outpatient department services are a substitute for physician office services. Usually, substitutes are imperfect so the decision maker will not be indifferent as to choice. Complementary services and goods are used jointly to produce improved health status: prescription drugs and physicians' services; hospital board and room services and physicians' surgical procedures.
It is important to note that various services, such as nursing home care and hospital room and board services, may be either substitute or complementary inputs to improved health status, depending on the particular situation. For example, because of medical, family, or financial reasons, some segments of the patient population may receive institutional care in a hospital rather than a nursing home setting or vice versa. Hospital care and nursing home care serve similar purposes and are substitutes here. However, patients may consecutively stay in a hospital and then a nursing home, depending upon the intensity of care needed. This switching of modalities of care to jointly produce improved health reflects the complementary nature of hospital and nursing home care.
There are, then, significant substitute and complementary relationships between various components of total systems cost (Davis and Russell, 1972; Feldstein, 1970; Hammond, 1979; Hellinger, 1977; Interindustry Economics Division, 1979; Russell, 1973; and U.S. General Accounting Office, 1982); it is important to use cost-effective combinations of these services when producing quality health care with limited resources.
An inverse association between nursing homes and hospitals is illustrated in Figure 10 where quarter-to-quarter percent changes in community hospital inpatient days for the aged are graphed along with quarter-to-quarter percent changes in total employment in nursing homes.8 The quarterly nursing home employment data were used as a rough indicator of utilization of nursing home services (in the absence of utilization data). Causal factors (seasonal and nonseasonal) leading to this negative association need to be studied for possible clues in reducing total costs for combined hospital and nursing home care. The daily room charge in a community hospital is three to four times as much as the cost of a day in a nursing home, so it is important that patients be placed in the proper continuum of care.9
Figure 10. Interaction between nursing home and hospital sectors: Quarterly percent changes in community hospital inpatient days for aged and nursing home employment, 1972-831,2.
1Quarter-to-quarter percent changes are graphed, not percent changes from same quarter a year ago.
2Quarterly percent changes in nursing home employment was used as a rough indicator of changes in nursing home use (in the absence of use data).
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The substitutional and complementary relationships among nursing home care, based on needs for and availability of shelter, and various intensities of medical care and social services are well illustrated by Lane (Figure 11). The universal need for shelter can be met by a whole continuum of types of living arrangements, such as individual housing, multifamily housing, congregate housing, nursing homes, hospitals, and the like. Shelter services are complementary (jointly produced) with certain health services, and in some cases shelter services substitute for (serve similar purposes) as institutional services such as nursing home care.
Figure 11. Potential substitutions for nursing home care, based on needs for and availability of shelter, social services, and medical care.
People with higher degrees of severity of impairment have a greater tendency to be in institutions where there are higher intensities of medical services or social services available. And this higher intensity of services is associated with higher costs per day. Some nursing home residents in Area A can potentially be relocated to individual or multifamily housing if in-home (for example, home health services) or community-based support services are available. A portion of Area B nursing home residents can potentially be relocated to domiciliary care programs and to congregate social care facilities. Likewise, nursing home residents in Area C can potentially be relocated to empty hospital beds by creating swing beds or extended care beds. The various types of living arrangements and the various modalities of medical care substitute and complement each other in the production of improved health.
A major objective of the Medicare PPS is to provide incentives for increasing efficiency and effectiveness by channeling patients to a more cost-effective mix of institutional care, ambulatory care, home care, and community services, with due regard for case-mix characteristics and quality of care. The Lane schematic graphically illustrates the substitutional and complementary nature of shelter, medical services, and social services for people with various degrees of impairment or case-mix complexity. This schematic could be revised to focus on potential substitution and complementary relationships of hospital inpatient care with various types of shelter, social services, and medical care services. As trends and patterns of health care spending in the 1980's are examined in this study, some of these interrelationships will be traced.
Historical perspective for total systems cost per capita
Total Systems Cost Per Capita (TSCPC) has grown from $70 in 1950 to $1, 215 in 1982, an average annual rate of increase of 9 percent (Tables N and O). Inflation-adjusted TSCPC increased at an average annual rate of 4 percent over this 32-year period.
Table O. Current and constant dollar per capita total systems cost: Selected years 1950-901.
| Calendar year | Current dollars | Constant dollars2 |
|---|---|---|
| Historical estimates | ||
| 1950 | $ 70 | $209 |
| 1955 | 93 | 239 |
| 1960 | 129 | 288 |
| 1965 | 181 | 372 |
| 1970 | 312 | 503 |
| 1972 | 376 | 550 |
| 1975 | 531 | 623 |
| 1980 | 947 | 722 |
| 1981 | 1,088 | 746 |
| 1982 | 1,215 | 760 |
| Projections | ||
| 1984 | 1,452 | 798 |
| 1987 | 1,907 | 868 |
| 1990 | 2,442 | 942 |
| Selected periods | Average annual percent change | |
| 1950-82 | 9.3 | 4.1 |
| 1965-82 | 11.9 | 4.3 |
| 1972-82 | 12.5 | 3.3 |
| 1965-70 | 11.6 | 6.3 |
| 1970-75 | 11.2 | 4.4 |
| 1975-80 | 12.3 | 3.0 |
| 1982-84 | 9.3 | 2.5 |
| 1984-87 | 9.5 | 2.8 |
| 1987-90 | 8.6 | 2.7 |
| 1982-87 | 9.4 | 2.7 |
| 1982-90 | 9.1 | 2.7 |
Total systems cost per capita is called per capita personal health care expenditures in Gibson et al. (1983).
Total systems cost per capita was deflated by the implicit price deflator for total systems cost (1977 = 100.0).
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
During the decade ending in 1982, TSCPC grew at an average annual rate of between 12 and 13 percent, the implicit price deflator for TSCPC at a 9 percent rate, and inflation-adjusted TSCPC at a little over a 3 percent rate (Table O). Economy-wide inflation accounted for 58 percent of the growth in total systems cost during the last 10 years (Figure 9). Increases in prices in excess of economy-wide prices accounted for between 9 and 10 percent of the increase. Population accounted for nearly 8 percent of the growth, and 25 percent was due to increases in real spending per capita. This last factor includes changes in the number of diagnostic and therapeutic procedures provided per capita and changes in the mix of services.
Changes in mix of services
The composition of TSCPC has shifted significantly over time. Two institutional services, hospital care10 and nursing home care, have increased their relative shares over the period 1950-82, rising from a combined share of 37 percent in 1950 to 57 percent in 1982 (Table N). Noninstitutional services (and medical supplies as a share of TSCPC) have dropped from 63 to 43 percent during this period.
In the last decade, expenditures for services of physicians and dentists have maintained their relative shares of TSCPC; other health services, (as well as drugs and medical sundries and eyeglasses and appliances) have declined in relative importance. But other professional services have increased their share of TSCPC. This changing of the relative composition of TSCPC reflects the net effect of substitution and complementary relations, as well as a host of other factors described in this study.
Changes in sources of funding
Sources of funding TSCPC have also shifted substantially from the 1950-82 period (Table P). In 1950, patient-direct payments accounted for nearly two-thirds of the financing. In 1982, patient-direct payments represented one-third, while total third-party payments accounted for over two-thirds of the financing.
Table P. Percent distribution of total systems cost by source of funds: Selected years 1950-901.
| All third parties | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Calendar year | Current dollars | Total systems cost | Patient direct payments | Total private and public | Private health insurance | Other private | Public | |||
|
|
|
|||||||||
| Total systems cost per capita In dollars | Total systems cost in billions | Total | Federal | State and local | ||||||
| Historical estimates | Percent distribution | |||||||||
| 1950 | $ 70 | $ 10.9 | 100.0 | 65.5 | 34.5 | 9.1 | 2.9 | 22.4 | 10.4 | 12.0 |
| 1960 | 129 | 23.7 | 100.0 | 54.9 | 45.1 | 21.1 | 2.3 | 21.8 | 9.3 | 12.5 |
| 1965 | 181 | 35.8 | 100.0 | 51.8 | 48.2 | 24.4 | 2.2 | 21.6 | 10.1 | 11.4 |
| 1970 | 312 | 65.1 | 100.0 | 39.9 | 60.1 | 24.0 | 1.6 | 34.5 | 22.3 | 12.2 |
| 1972 | 376 | 80.2 | 100.0 | 38.6 | 61.4 | 23.8 | 1.6 | 36.0 | 23.6 | 12.4 |
| 1975 | 531 | 116.8 | 100.0 | 33.4 | 66.6 | 25.8 | 1.4 | 39.5 | 26.9 | 12.6 |
| 1980 | 947 | 219.4 | 100.0 | 32.9 | 67.1 | 26.0 | 1.4 | 39.7 | 28.6 | 11.2 |
| 1981 | 1,088 | 254.6 | 100.0 | 32.2 | 67.7 | 26.2 | 1.4 | 40.1 | 29.2 | 10.9 |
| 1982 | 1,215 | 286.9 | 100.0 | 31.5 | 68.5 | 26.7 | 1.5 | 40.3 | 29.2 | 11.1 |
| Projections | ||||||||||
| 1984 | 1,452 | 349.4 | 100.0 | 31.4 | 68.6 | 26.7 | 1.4 | 40.5 | 30.1 | 10.4 |
| 1987 | 1,907 | 471.3 | 100.0 | 31.3 | 68.8 | 26.7 | 1.4 | 40.7 | 30.8 | 9.9 |
| 1990 | 2,442 | 619.0 | 100.0 | 30.8 | 69.2 | 26.6 | 1.4 | 41.2 | 31.7 | 9.5 |
Total systems cost is called “personal health care expenditures” in Gibson, et al. (1983).
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
The Federal Government, private health insurance, and State and local governments each financed roughly 10 percent of TSCPC in 1950 (Table P). From 1950-65, Federal, State, and local shares were fairly constant, but private health insurance grew very rapidly. Medicare and Medicaid took effect in mid-1966, and by 1967, the Federal Government's share of TSCPC advanced to 21 percent. Patient-direct payments dropped from 66 percent in 1950 to 43 percent in 1967. By 1982, the percentages paid by the major payors were as follows: patient-direct payments, 32 percent; Federal Government, 29 percent; private health insurance, 27 percent; and State and local governments, 11 percent (Table P).
Changes in mix of services for various sources of funding
Another way to look at sources of funding is to ask, “What fraction of each type of funding is allocated to various categories of services?” For example, Federal payments for hospital care as a portion of total Federal health spending remained fairly constant from 1965-82, about $2 out of $3. In contrast, Federal funding for physicians' services as a percent of total Federal payments increased fourfold over the same period, rising from 4 percent in 1965 to 16 percent in 1982 (Table 9).
Table 9. Percent distribution of Federal benefits and State and local benefits, by type of personal health care expenditures: Selected years 1965-1990.
| Type of personal health care expenditure | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Calendar year | Benefits per capita in dollars | Total benefits in billions | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses And appliances | Nursing home care | Other health services |
|
| |||||||||||
| Percent distribution | |||||||||||
| Federal Historical | |||||||||||
| 1965 | $ 18 | $ 3.6 | 100.0 | 67.0 | 4.2 | 0.9 | 0.3 | 3.3 | 0.3 | 12.7 | 11.2 |
| 1970 | 70 | 14.5 | 100.0 | 65.5 | 14.7 | 0.9 | 1.0 | 1.6 | 0.5 | 9.3 | 6.5 |
| 1972 | 89 | 18.9 | 100.0 | 65.5 | 14.5 | 1.0 | 0.8 | 1.8 | 0.6 | 8.8 | 7.0 |
| 1975 | 143 | 31.4 | 100.0 | 64.5 | 14.8 | 0.9 | 1.2 | 1.7 | 0.6 | 10.1 | 6.3 |
| 1980 | 271 | 62.7 | 100.0 | 65.6 | 15.2 | 0.6 | 1.6 | 1.3 | 0.7 | 9.9 | 5.1 |
| 1981 | 318 | 74.4 | 100.0 | 65.2 | 15.8 | 0.5 | 1.7 | 1.3 | 0.8 | 9.9 | 4.9 |
| 1982 | 354 | 83.7 | 100.0 | 65.2 | 16.0 | 0.5 | 2.0 | 1.1 | 0.9 | 9.4 | 4.8 |
| Projected | |||||||||||
| 1984 | 436 | 105.0 | 100.0 | 64.1 | 17.4 | 0.5 | 2.4 | 1.1 | 1.1 | 9.0 | 4.5 |
| 1987 | 587 | 145.0 | 100.0 | 63.6 | 18.7 | 0.4 | 2.3 | 1.0 | 1.2 | 8.6 | 4.2 |
| 1990 | 775 | 196.5 | 100.0 | 63.4 | 19.6 | 0.4 | 2.3 | 0.9 | 1.2 | 8.2 | 4.0 |
| State and local Historical | |||||||||||
| 1965 | 21 | 4.1 | 100.0 | 72.5 | 10.6 | 0.4 | 0.6 | 1.9 | 0.4 | 6.2 | 7.5 |
| 1970 | 38 | 7.9 | 100.0 | 65.0 | 10.8 | 1.2 | 1.0 | 3.1 | 0.4 | 11.8 | 6.7 |
| 1972 | 46 | 9.9 | 100.0 | 62.8 | 11.7 | 1.1 | 1.0 | 3.4 | 0.3 | 13.8 | 5.9 |
| 1975 | 67 | 14.7 | 100.0 | 58.2 | 12.8 | 1.3 | 1.3 | 3.4 | 0.3 | 17.0 | 5.6 |
| 1980 | 106 | 24.5 | 100.0 | 53.8 | 12.2 | 1.1 | 1.6 | 3.4 | 0.4 | 21.8 | 5.8 |
| 1981 | 119 | 27.8 | 100.0 | 55.0 | 11.9 | 1.1 | 1.5 | 3.3 | 0.4 | 20.9 | 6.0 |
| 1982 | 135 | 32.0 | 100.0 | 54.4 | 11.2 | 1.1 | 1.6 | 3.2 | 0.3 | 22.3 | 5.9 |
| Projected | |||||||||||
| 1984 | 152 | 36.5 | 100.0 | 53.5 | 11.7 | 1.2 | 1.8 | 3.3 | 0.3 | 22.4 | 5.9 |
| 1987 | 188 | 46.6 | 100.0 | 52.3 | 11.7 | 1.1 | 2.1 | 3.2 | 0.3 | 23.2 | 5.8 |
| 1990 | 231 | 58.6 | 100.0 | 51.5 | 11.8 | 1.1 | 2.5 | 3.1 | 0.3 | 23.9 | 5.7 |
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Under the Medicare program, in 1972, 96 percent of benefits were for hospital care and physicians' services, leaving only 4 percent for other services, such as other professional services and nursing home care (Table F). By 1982, services other than hospital care and physicians' services increased to 6 percent of total Medicare benefits. Although nursing home care has declined in relative importance, other professional services (which includes home health agency funding) have increased in relative importance.
Hospital care, physicians' services, dentists' services, and drugs have declined as a relative share of total Medicaid (Federal, State and local) benefit payments over the 1967-82 period (Table 10); at the same time, nursing home care, other professional services, and other health services have increased their relative shares of benefit payments.
Table 10. Percent distribution of Medicaid benefits, by type of personal health care expenditure: Selected years 1967-82.
| Type of personal health care expenditure | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Calendar year | Medicaid Benefits per capita in dollars | Total Medicaid benefits in billions | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Nursing home care | Other health services |
|
| ||||||||||
| Percent distribution | ||||||||||
| 1967 | $ 14 | $ 2.9 | 100.0 | 42.3 | 10.9 | 4.4 | 0.9 | 7.2 | 31.7 | 2.6 |
| 1970 | 25 | 5.2 | 100.0 | 42.9 | 13.3 | 3.2 | 1.4 | 7.9 | 27.2 | 4.1 |
| 1972 | 38 | 8.2 | 100.0 | 40.9 | 13.6 | 2.4 | 1.2 | 7.1 | 31.5 | 3.4 |
| 1975 | 62 | 13.5 | 100.0 | 34.9 | 13.9 | 2.7 | 1.8 | 6.6 | 36.0 | 4.1 |
| 1980 | 110 | 25.5 | 100.0 | 36.9 | 9.7 | 2.0 | 1.9 | 5.6 | 39.8 | 4.1 |
| 1981 | 124 | 29.0 | 100.0 | 36.3 | 9.6 | 2.0 | 1.9 | 5.6 | 39.9 | 4.7 |
| 1982 | 137 | 32.4 | 100.0 | 36.3 | 9.0 | 2.0 | 2.1 | 5.2 | 40.9 | 4.5 |
NOTE: Benefits include Federal, State, and Local shares.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
In 1982, State and local government benefit payments for hospital care and nursing home care made up 77 percent of the total, nearly the same as in 1965 (Table 9). However, nursing home costs were only 6 percent of benefits in 1965, but increased to 22 percent in 1982; and hospital outlays were 73 percent in 1965, but 54 percent in 1982.
Private health insurance benefit payments are skewed toward hospital care and physicians' services. In 1982, hospital care was only 47 percent of total systems costs (Table N), but 59 percent of private health insurance benefits (Table 11). Likewise, physician services represented 22 percent of total systems costs and 28 percent of private health insurance benefits. Spending for nursing homes made up 10 percent of total systems costs, but less than one-half of 1 percent of private insurance benefits (Table 11). Dental services, drugs, and eyeglasses and appliances are becoming increasing shares of health insurance benefits (Bureau of Labor Statistics, August 1983; Health Insurance Association of America, 1983a, 1983b).
Table 11. Percent distribution of private health insurance benefits: Selected years 1965-90.
| Calendar year | Private health insurance benefits per capita in dollars | Total private health insurance benefits in billions | Type of personal health care expenditure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | |||
|
| ||||||||||
| Percent distribution | ||||||||||
| Historical | ||||||||||
| 1965 | $ 44 | $ 8.8 | 100.0 | 66.2 | 30.6 | 0.5 | 1.2 | 1.5 | (1) | (1) |
| 1970 | 75 | 15.6 | 100.0 | 63.6 | 31.1 | 1.6 | 1.7 | 2.0 | (1) | 0.1 |
| 1972 | 89 | 19.1 | 100.0 | 62.8 | 31.3 | 1.7 | 1.8 | 2.2 | 0.1 | 0.1 |
| 1975 | 137 | 30.1 | 100.0 | 61.3 | 31.1 | 3.3 | 1.2 | 2.5 | 0.3 | 0.3 |
| 1980 | 246 | 57.0 | 100.0 | 59.1 | 28.9 | 6.2 | 1.5 | 3.5 | 0.5 | 0.3 |
| 1981 | 285 | 66.8 | 100.0 | 59.0 | 28.5 | 6.5 | 1.7 | 3.5 | 0.5 | 0.3 |
| 1982 | 324 | 76.6 | 100.0 | 58.7 | 28.3 | 6.9 | 1.6 | 3.7 | 0.5 | 0.3 |
| Projected | ||||||||||
| 1984 | 388 | 93.3 | 100.0 | 58.2 | 27.7 | 7.4 | 1.8 | 4.0 | 0.6 | 0.3 |
| 1987 | 509 | 125.7 | 100.0 | 58.4 | 26.7 | 7.8 | 2.0 | 4.2 | 0.6 | 0.4 |
| 1990 | 650 | 164.8 | 100.0 | 59.0 | 25.8 | 7.7 | 2.0 | 4.3 | 0.7 | 0.4 |
Less than 0.05 percent.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
Total systems cost per capita projections
The short-term outlook is for TSCPC to rise from $1,215 in 1982 to $1,452 in 1984 (Table N), an average annual rate of increase of over 9 percent. This is down significantly from the nearly 14 percent average annual rate of increase for the 1979-82 period. The baseline projections assume that current dollar TSCPC will rise at an average annual rate of 9 percent from 1982 to 1990 (Table O), substantially below the 1972-82 rate of between 12 and 13 percent. This reflects significant deceleration of inflation, tighter third-party payment incentives, and increases in efficiency and effectiveness in providing care.
Inflation-adjusted (implicit price deflator for total systems costs) TSCPC is expected to increase at an average annual rate of under 3 percent from 1982 to 1990, with a range of approximately plus or minus 1 percent. This compares with an average annual rate of over 3 percent during the 1972-82 period. The projected rate is roughly one-fifth lower in the 1982-90 period, in spite of real GNP growing significantly faster.
Changes in mix of services
In the 1980s it is expected that there will be a continuation of the historical pattern of institutional care (hospital and nursing home care combined), increasing its share of TSCPC. Some modifications in light of the underlying fiscal pressures, altered payment systems, demographic shifts, and new technologies are expected.
The aging of the population (Tables 2 and 3) slowly but powerfully increases the demand for health care, especially services and supplies associated with long-term care such as home health services, durable medical equipment, hospital care, physicians' services, drugs, and nursing home care.
Some analysts believe that disability and chronic disease prevalence will increase as life expectancy lengthens and the duration of disability and illness episodes increases (Gruenberg, 1977; Kramer, 1980; Kramer, 1981). Others, such as Fries (1980), argue that certain chronic diseases and disabilities can be eliminated or postponed so that smaller fractions of the human life span will be subjected to the need for increased health and social services. In any case, the aging process is a biomedically complex phenomenon that will have penetrating implications for the financers of health care in both the public and private sector (Manton, 1982).
Changes in sources of funding
Factors influencing patterns of growth in TSCPC include the Medicare PPS for inpatient services; fiscal pressures on Federal, State, and local governments leading to more cost-effective payment policies; pressures on employers and individuals to increase deductibles and coinsurance on private health insurance plans (Lawson, 1982); and increased use of private sector initiatives such as business coalitions and preferred provider organizations (PPO's). The net effect of the various forces is to shift the sources of funding for TSCPC (Table P). Medicare benefit payments for hospital services are expected to decline relative to Medicare benefit payments for physician services (Table F), given the current-law regulations as of mid-1983. State and local governments are expected to spend increasing shares for nursing home care and other professional services, such as home health services (Table 9). Private health insurance benefits are expected to continue to expand for dentists' services; other professional services; and drugs, eyeglasses, and durable medical equipment (Table 11), given current laws.
In this section, factors accounting for growth in TSCPC were discussed. In the following section, the impact of these factors on the various individual sectors of the health care sector will be explored.
Projection trends by type of health expenditure
In this section, highlights relating to projection trends by type of health expenditure are presented: first, a historical perspective with commentary on factors influencing expenditure growth; second, a synopsis of the short-term outlook and the long-term projection, including highlights of the projections by sources of funding.
Hospital care
Historical perspective
With complex technologies and procedures, specialization, and interrelatedness of treatments at various stages in episodes of illness, hospitals have become the focal point of the health care sector and, in some cases, hospitals are beginning to serve as the health care centers for communities by providing a wide array of services in addition to acute inpatient services. Such services may include organized outpatient clinics for the provision of nonemergency medical or dental services, home health services, outpatient hemodialysis, hospice care, skilled nursing care, self-care, pharmacy service, health education, and the like.
The Medicare PPS, effective with cost-reporting periods beginning after September 30, 1983, thoroughly revises the financial incentives associated with Medicare inpatient services. Implications of the new payment plan will directly affect community hospitals; the higher the proportion of the revenue mix for individual hospitals that is derived from Medicare inpatient benefits the greater the potential impact. The new payment plan may have indirect effects on other types of hospitals and on services other than those for Medicare inpatients.
Hospital care as a percentage of total systems costs increased from 35 percent in 1950 to 47 percent in 1982, and is expected to garner a larger share by 1990 (Table N). The $136 billion spent on hospital care in 1982 (Table 5) makes up 4 percent of GNP. To put this expenditure amount into perspective, 6,915 hospitals with 1.4 million beds handled 39.1 million admissions and 384 million patient days of service in 1982. In addition, 314 million outpatient visits were provided (American Hospital Association, 1983). Although the proportion of the population with one or more hospital episodes (10 percent) has not changed in the last decade, intensity and sophistication of care have increased substantially (Table Q and Figure 8).
Table Q. National Hospital input price index, expense per inpatient stay and per inpatient day (current dollars and intensity); 1965-82.
| National hospital input price index1(1977 = 100.0) | Expense per inpatient stay2 3 | Expense per inpatient day2 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Current dollars | Intensity (real expense per stay)4 | Current dollars | Intensity (real expense per day)4 | |||||||
|
|
|
|
|
|
||||||
| Calendar year | Level | Percent change | Level | Percent change | Level | Percent change | Level | Percent change | Level | Percent change |
| 1965 | 42.3 | --- | $ 315 | --- | $ 745 | --- | $ 41 | --- | $ 98 | --- |
| 1966 | 44.8 | 5.9 | 356 | 13.1 | 796 | 6.8 | 46 | 11.4 | 103 | 5.2 |
| 1967 | 48.4 | 8.0 | 425 | 19.1 | 877 | 10.3 | 53 | 15.3 | 110 | 6.7 |
| 1968 | 51.9 | 7.2 | 482 | 13.4 | 928 | 5.8 | 59 | 11.5 | 114 | 4.0 |
| 1969 | 54.5 | 5.0 | 552 | 14.5 | 1,012 | 9.1 | 68 | 15.4 | 126 | 9.9 |
| 1970 | 58.5 | 7.3 | 608 | 10.3 | 1,040 | 2.8 | 78 | 13.8 | 133 | 6.1 |
| 1971 | 62.3 | 6.5 | 670 | 10.1 | 1,075 | 3.4 | 88 | 12.3 | 140 | 5.4 |
| 1972 | 65.9 | 5.8 | 729 | 8.8 | 1,106 | 2.9 | 96 | 10.3 | 146 | 4.3 |
| 1973 | 69.9 | 6.1 | 784 | 7.5 | 1,121 | 1.4 | 105 | 9.2 | 151 | 3.0 |
| 1974 | 76.9 | 10.0 | 873 | 11.4 | 1,135 | 1.3 | 118 | 12.3 | 154 | 2.1 |
| 1975 | 85.0 | 10.5 | 1,017 | 16.5 | 1,196 | 5.4 | 138 | 16.4 | 162 | 5.3 |
| 1976 | 92.5 | 8.8 | 1,168 | 14.8 | 1,262 | 5.5 | 158 | 15.0 | 171 | 5.7 |
| 1977 | 100.0 | 8.1 | 1,312 | 12.3 | 1,312 | 3.9 | 181 | 14.3 | 181 | 5.8 |
| 1978 | 108.4 | 8.4 | 1,466 | 11.8 | 1,352 | 3.1 | 203 | 12.1 | 187 | 3.5 |
| 1979 | 119.3 | 10.1 | 1,618 | 10.4 | 1,356 | 0.3 | 226 | 11.5 | 190 | 1.3 |
| 1980 | 133.5 | 11.9 | 1,836 | 13.5 | 1,375 | 1.4 | 256 | 12.9 | 192 | 0.9 |
| 1981 | 149.7 | 12.1 | 2,155 | 17.4 | 1,440 | 4.7 | 299 | 16.9 | 200 | 4.3 |
| 1982 | 164.8 | 10.1 | 2,489 | 15.5 | 1,510 | 4.9 | 348 | 16.2 | 211 | 5.6 |
| Average annual percent change | ||||||||||
| Selected periods | ||||||||||
| 1972-82 | --- | 9.6 | --- | 13.1 | --- | 3.2 | --- | 13.7 | --- | 3.7 |
| 1965-82 | --- | 8.3 | --- | 12.9 | --- | 4.2 | --- | 13.3 | --- | 4.6 |
For information on derivation of the National Hospital Input price, see Freeland et al. (1979). For information on a related input price index to adjust Medicare PPS rates for inflation, see Health Care Financing Administration (1983).
Historical current dollar data are from American Hospital Association (1982).
Costs are adjusted by the American Hospital Association to eliminate expenses associated with outpatient care.
Intensity (or real expense per unit of service) is calculated by dividing current dollar expenses by the National Hospital Input Price Index. For example, in 1982, real expense per inpatient stay is .
Note that the decimal point on the input price index must be moved two places to the left.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
The 1982 hospital outlays of $135.5 billion were distributed to four major sectors: community hospital inpatient care (73 percent of total hospital), community hospital outpatient care (12 percent), Federal hospital care (7 percent), and all other hospital care (8 percent).
Total hospital expenditures in the last 10 years increased at an average annual rate of almost 15 percent (Table 6). Economy-wide inflation accounted for 54 percent of the growth in total hospital spending during the 1972-82 period. Hospital input prices in excess of economy-wide inflation accounted for 13 percent of the growth, and population increases accounted for 7 percent. Finally, increases in real spending per capita accounted for 25 percent of the growth in hospital spending.
Third-party payments play a very significant role in financing hospital care since only about one-tenth of this care is paid directly out-of-pocket by the patient. Private health insurance covers one-third of the outlays; Medicare covers over a quarter, and Medicaid's share is less than a tenth. Medicare's share has increased from 18 percent in 1972 to 27 percent in 1982, reflecting an average annual expenditure growth rate of 19 percent; total hospital outlays increased at an average annual rate of less than 15 percent during this same period. Other third-party payors experienced stable or declining shares.
Private health insurance benefit payments increased at nearly the same rate as total hospital outlays, over 14 percent, and major medical and daily hospital room and board benefits have increased substantially as hospital costs have escalated (Bureau of Labor Statistics, August 1983; Health Insurance Association of America, 1983b, 1983c).
Projections
Total hospital expenditures are expected to rise from $135.5 billion in 1982 to $166 billion in 1984, $227 billion in 1987, and $304 billion in 1990 (Table 5). From 1972-82, annual percent increases in total hospital spending exhibited substantial variation with a low of under 11 percent in 1973 (Economic Stabilization Program period) to a high of over 17 percent in 1981. It is likely that as we approach 1990, there will be volatility and spurts in spending as there have been historically.
Medicare benefit payments (inpatient and outpatient) are projected to increase in the 12 to 13 percent range through the mid-1980's, and in the 11 to 12 percent range for the latter part (Table B). This rate is substantially lower than the 19 percent for the 1972-82 period. Several factors account for this deceleration in spending growth: 1) Economy-wide inflation is projected to increase at substantially lower rates in the 1980's; 2) inpatient benefit payment increases will be restrained by the PPS (Board of Trustees, Federal Hospital Insurance Trust Fund, 1983), and 3) during the historical period 1972-82, certain disabled beneficiaries and persons with end-stage renal disease were added to those eligible for Medicare hospital insurance coverage.
The deceleration in Medicare benefit payment increases due to the PPS is projected to slow total hospital spending increases as hospitals are forced to economize to meet the predetermined payment rates of PPS. The Federal share of total hospital spending, which has been relatively stable since 1976 at 40 to 41 percent, is not projected to change substantially over the projected horizon. Demographic factors provide pressures to increase the Federal share, but the slowing of benefit increases due to PPS provides a counter force.
State and local funding of hospital care is expected to decrease as a percentage of hospital expenditures. Continued cutbacks in long-term mental hospital care and restraining of community hospital cost increases under Medicaid, contribute to the decline in the State and local share.
Community hospitals: Inpatient
Historical perspective
Community hospital inpatient care, from technological and financial perspectives, is the cornerstone of our Nation's health delivery system for complex, acute care services. In 1982, the 5,801 community hospitals, with 1.0 million beds, handled 36.4 million admissions. The average number of beds per hospital was 173, up 13 percent from 1972. The number of hospitals peaked in 1977 at 5,881 and has declined each year through 1982 (American Hospital Association, 1983).
Community hospital inpatient spending (almost three-fourths of total hospital spending in 1982) increased from $23 billion in 1972 to $99 billion in 1982, an average annual rate of increase of nearly 16 percent.
Large increases in community hospital inpatient expenses during the historical period 1972-82 are accounted for by several factors. Overall inflation in the economy, as measured by the GNP deflator, accounted for 52 percent of the growth (Figure 8): Increases in hospital input prices (Freeland et al., 1979; Freeland et al., 1981) in excess of the GNP deflator accounted for 13 percent (Figure 8 and Table 12). Growth in aggregate population accounted for 7 percent of the increase, as did growth in admissions per capita. Intensity (as measured by growth in real expense per admission) accounted for the remaining 22 percent. By combining only those factors specific to the hospital industry, it can be seen that growth in intensity per admission accounted for half of the increase (Figure 8): The factors are intensity per admission (includes nursing hours per case and diagnostic and therapeutic procedures per case), admissions per capita, and hospital input prices in excess of the GNP deflator.
Table 12. National hospital input price index compared with overall inflation in the economy: 1950-82.
| National Hospital Input Price Index1(1977 = 100.0) | Implicit price deflator for gross national product2(1972 = 100.00) | National Hospital Input Price Index deflated by implicit price deflator for GNP | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Calendar year | Level | Percent change | Level | Percent change | Level | Percent change |
| 1950 | 23.7 | --- | 53.5 | --- | 44.3 | --- |
| 1951 | 26.2 | 10.5 | 57.1 | 6.6 | 45.9 | 3.7 |
| 1952 | 27.7 | 5.7 | 57.9 | 1.4 | 47.8 | 4.2 |
| 1953 | 28.9 | 4.3 | 58.8 | 1.6 | 49.1 | 2.7 |
| 1954 | 29.5 | 2.1 | 59.5 | 1.2 | 49.5 | 0.8 |
| 1955 | 30.3 | 2.7 | 60.8 | 2.2 | 49.8 | 0.5 |
| 1956 | 30.9 | 2.0 | 62.8 | 3.2 | 49.2 | −1.2 |
| 1957 | 32.0 | 3.6 | 64.9 | 3.4 | 49.3 | 0.2 |
| 1958 | 33.5 | 4.7 | 66.0 | 1.7 | 50.7 | 3.0 |
| 1959 | 35.0 | 4.5 | 67.6 | 2.4 | 51.8 | 2.0 |
| 1960 | 36.4 | 4.0 | 68.7 | 1.6 | 53.0 | 2.3 |
| 1961 | 37.3 | 2.5 | 69.3 | 0.9 | 53.8 | 1.6 |
| 1962 | 38.5 | 3.2 | 70.6 | 1.8 | 54.5 | 1.3 |
| 1963 | 39.6 | 2.9 | 71.7 | 1.5 | 55.2 | 1.3 |
| 1964 | 40.7 | 2.8 | 72.8 | 1.5 | 55.9 | 1.2 |
| 1965 | 42.3 | 3.9 | 74.4 | 2.2 | 56.9 | 1.7 |
| 1966 | 44.8 | 5.9 | 76.8 | 3.2 | 58.4 | 2.6 |
| 1967 | 48.4 | 8.0 | 79.0 | 3.0 | 61.2 | 4.9 |
| 1968 | 51.9 | 7.2 | 82.5 | 4.4 | 62.9 | 2.7 |
| 1969 | 54.5 | 5.0 | 86.8 | 5.2 | 62.8 | −0.2 |
| 1970 | 58.5 | 7.3 | 91.4 | 5.4 | 64.0 | 1.9 |
| 1971 | 62.3 | 6.5 | 96.0 | 5.0 | 64.9 | 1.4 |
| 1972 | 65.9 | 5.8 | 100.0 | 4.1 | 65.9 | 1.6 |
| 1973 | 69.9 | 6.1 | 105.7 | 5.8 | 66.1 | 0.3 |
| 1974 | 76.9 | 10.0 | 115.1 | 8.9 | 66.8 | 1.1 |
| 1975 | 85.0 | 10.5 | 125.7 | 9.2 | 67.6 | 1.2 |
| 1976 | 92.5 | 8.8 | 132.3 | 5.2 | 69.9 | 3.4 |
| 1977 | 100.0 | 8.1 | 140.0 | 5.8 | 71.4 | 2.2 |
| 1978 | 108.4 | 8.4 | 150.4 | 7.4 | 72.1 | 1.0 |
| 1979 | 119.3 | 10.1 | 163.4 | 8.7 | 73.0 | 1.3 |
| 1980 | 133.5 | 11.9 | 178.4 | 9.2 | 74.8 | 2.5 |
| 1981 | 149.7 | 12.1 | 195.1 | 9.4 | 76.7 | 2.5 |
| 1982 | 164.8 | 10.1 | 206.9 | 6.0 | 79.7 | 3.8 |
| Average annual percent change | ||||||
| Selected periods | ||||||
| 1972-82 | --- | 9.6 | --- | 7.5 | --- | 1.9 |
| 1965-82 | --- | 8.3 | --- | 6.2 | --- | 2.0 |
For information on derivation of the National Hospital Input Price Index, see Freeland et al. (1979). Percent changes beginning with 1970 are presented in this article. Prior year percent changes have been estimated using available wage and price indicators.
The implicit price deflator for GNP is a widely used indicator of inflation for the overall economy.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
The primary force in the rapid growth in intensity is the demand for increased quality of care, which is driven by comprehensive insurance coverage (low cost-sharing). This demand factor interacts with cost-based reimbursement systems (piecework payment systems) to fuel the growth in intensity of services. The primary way in which the Medicare PPS is expected to decelerate the rate of increase in hospital costs is to slow the growth in intensity of services per case by setting predetermined rates of payment (per DRG), independent of the specific ancillary services used.
Projections
The PPS for Medicare inpatient services is intended to reduce forecasted deficits in the Hospital Insurance Trust Fund; the higher the proportion of Medicare revenues a hospital has, the greater the potential impact of PPS on that hospital. The financial incentives and medical records requirements that community hospitals face will be profoundly affected. Consequently, a brief synopsis of some major provisions and probable incentives of Medicare PPS are included here. It is important to note that this brief summary of provisions and incentives omits some significant characteristics, as well as details and exceptions. The interested reader should consult other sources to obtain such information (Board of Trustees, Federal Hospital Insurance Trust Fund, 1983; Grimaldi, August 1983; Grimaldi and Micheletti, 1983a, 1983b; and Health Care Financing Administration, 1983).
Beginning with cost-reporting periods after September 30, 1983, hospitals (except for psychiatric, long-term care, rehabilitative, and children's hospitals) will be paid by a prospectively determined amount per discharge, rather than by a retrospective, reasonable cost basis. Payment will vary by DRG's, of which there are approximately 470 based on principal diagnosis, principal operating-room procedure, other diagnoses and procedures, discharge status, sex, and age at admission. Capital-related costs will continue to be reimbursed on a retrospective, reasonable cost basis. However, Congress requires that the Secretary of Health and Human Services (HHS) examine methods to include capital-related costs in the rate for the PPS. Findings from this study are due in October 1984.
The plan will be phased in over a 4-year period to allow hospital administrators and staff time to adjust to policies and procedures appropriate for the revised financial incentives. During the first 3 years, a hospital's DRG payment rate will be a mixture of 1) each hospital's own cost base, 2) the regional DRG rate, and 3) the National DRG rate. Over time, there will be increased emphasis on National DRG rates so that by the fourth year (1986), the entire DRG rate will be determined from National averages (with adjustment for area wage-rate levels).
The DRG payment rates are updated annually based on a hospital input price index that reflects the price of goods and services used to produce hospital care. There is an additional 1 percent added to the DRG payment rate to permit quality and intensity increases. Included in this 1 percent allowance are the costs of new medical technology, new services and supplies, additional personnel, shifts in the mix of staff toward higher quality employees, and the like.
The Prospective Payment Assessment Commission will advise the Secretary of HHS on the need for changes in the 1) relative values of various DRG's due to changes in clinical practice patterns and technological advances, 2) inflation adjustment (hospital input price index), and 3) intensity allowance.
The Medicare PPS has financial incentives to 1) increase admissions, 2) shorten lengths of stay, 3) reduce ancillary services, and 4) assign patients to DRG's that will maximize Medicare payments (Grimaldi and Micheletti, 1983b). Payment is directly related to the number of admissions by DRG classification, and payment per discharge is independent of the specific quantity and quality of ancillary services provided and the specific length of stay. Congress and HHS were fully aware of these incentives when the PPS was designed and have, accordingly, designed utilization, quality, and DRG assignment review procedures to place strong emphasis on quality of care and valid DRG assignments.
How does the PPS reduce the rate of Medicare inpatient outlays? There are three main factors (Grimaldi, August 1983): 1) Hospital output is defined by number of discharges, rather than by days of care and quantity of ancillary services, as was previously the case. The old reimbursement system had incentives to increase length of stay and for overuse of ancillary services. 2) The PPS replaces retrospective cost-based reimbursement. Under cost-based reimbursement, hospitals were paid, in essence, what they spent. This was inherently inflationary and led to obvious inefficiencies. Competition among hospitals focused on sophisticated equipment and quality services that would attract physicians and patients. With the PPS, the intent is to reward hospitals financially for being cost-effective while at the same time assuring the continuation of high quality care. The DRG rates are fixed amounts independent of actual costs—hence, cost-effective hospitals become more financially viable, generate surpluses, and can expand services to meet community needs more effectively. 3) Reimbursable costs per discharge (by DRG) have a 1 percent ceiling in the annual rate of increase, after adjustment has been made for hospital input price inflation. As mentioned above, this allowance is for enhanced quality of care and for increases in intensity. From 1972 to 1982, intensity of services per admission has grown at an average annual rate of over 3 percent for community hospital inpatient services (Table Q). The slowing of growth in intensity per discharge, from about 3 percent annually to 1 percent annually, is the essence of the method used to reduce the rate of increase of Medicare outlays. Over time, billions of dollars can cumulatively be saved by slowing the rate of intensity growth. Over half of the increase in hospital-specific expenditure growth is accounted for by the rise in intensity per case (Figure 8). Each year, quality/intensity per discharge is permitted to rise, but at a rate that is slower than under inherently inflationary and inefficient cost-based reimbursement.
The PPS uncouples Medicare revenues to hospitals from expenses incurred to treat Medicare patients. Medicare outlays are projected to increase more slowly than would otherwise be the case since the growth in intensity is down from approximately 3 percent annually to 1 percent annually. The intent is to force hospitals to economize and adopt more cost-effective patterns of care while assuring quality of care. By increasing productivity and improving practice patterns, hospitals can increase real service output substantially in excess of the 1 percent allowance for intensity growth. Competition among hospitals will force such economizing behavior.
The DRG's are a patient classification system (Pettengill and Vertrees, 1982) that plays three vital roles in the Medicare PPS: 1) defining outputs for groups of discharges that are relatively hemogeneous in resource use; 2) distributing Medicare benefit payments among hospitals in accordance with resource intensity of DRG's, rather than in accordance with historical cost patterns that reflect inefficiencies and inflationary cost behavior; 3) facilitating communication among hospital medical staff, hospital administrators, Medicare intermediaries, Federal Government administrators, and other groups concerned about quality care produced with cost-effective patterns of care. The long-run viability of any program to reduce the rate of increase of hospital costs is highly dependent upon clear communication among the affected parties. Since output was not clearly defined in retrospective cost-based reimbursement, it was not feasible to develop fair and efficient methods of Medicare payment. Definitions of outputs that integrate concepts from clinical practice with finance, budget, and management information support systems are essential; these definitions permit finite hospital resources to be allocated in a more fair and cost-effective manner.
The communication fostered by the DRG classification system will likely result in management related groups (MRG's) (Lindner and Wagner, 1983). MRG's may include hospital managers, physicians, and staff from medical records (Nathanson, 1983), finance, information support systems, and various other departments. MRG's analyze data generated from the DRG information support system to improve quality of care and to increase efficiency and effectiveness, given the finite resources available. DRG information support systems that merge clinical and financial data ideally identify revenue and costs per discharge by DRG, by department, and for each physician on the medical staff (Grimaldi and Micheletti, 1983a; Lindner and Wagner, 1983). The importance of this physician-hospital cooperation in producing high-quality, cost-effective care under the Medicare PPS program has been endorsed by the American Medical Association (American Medical News, 1983).
The DRG's do not inherently slow the rate of increase in Medicare outlays (Grimaldi, August 1983). The slowing is accomplished by linking increases in Medicare payments per discharge to increases in hospital input prices plus the 1 percent add-on for intensity/quality, a feature first incorporated in the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982 (Grimaldi, Jan. 1983).
Spending for community hospital inpatient care is projected to rise from $99 billion in 1982 to approximately $123 billion in 1984. This represents a 2-year cumulative increase of 23 percent, a deceleration from the 1980 to 1982 period increase of 38 percent. Inpatient spending is projected to reach $168 billion in 1987 and $226 billion in 1990.
Expenses per inpatient stay tripled from $729 in 1972 to $2, 489 in 1982, and are projected to rise to over $5, 000 by 1990 (Table R). Expenses per inpatient day are projected to rise from $348 in 1982 to approximately $432 in 1984, $584 in 1987, and $771 in 1990 (Table R).
Table R. Expense per inpatient stay and per inpatient day, community hospitals: Selected years 1965-90.
| Calendar year | Expense per inpatient stay1, 2 | Expense per Inpatient day1, 2 |
|---|---|---|
| Historical estimates | ||
| 1965 | $ 315 | $ 41 |
| 1970 | 608 | 78 |
| 1972 | 729 | 96 |
| 1975 | 1,017 | 138 |
| 1980 | 1,836 | 256 |
| 1981 | 2, 155 | 299 |
| 1982 | 2,489 | 348 |
| Projections | ||
| 1984 | 3,013 | 432 |
| 1987 | 3,971 | 584 |
| 1990 | 5,114 | 771 |
Historical data for community hospitals are from American Hospital Association, (1982).
Costs are adjusted to eliminate expenses associated with outpatient care.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
These projections are lower than the comparable projections made last year for two major reasons. First, the projected economy-wide inflation rates are lower and, second, the Medicare PPS is projected to slow the growth in expense per discharge for the Medicare beneficiary population (Board of Trustees, Federal Hospital Insurance Trust Fund, 1983).
The projections in this study assume that the Medicare PPS is in effect through 1990 and that other payors do not shift to DRG-type PPS's. The Medicare PPS represents a significant and pervasive change, and it is not possible, given the lack of historical precedent, to accurately project its effects, direct and indirect (Board of Trustees, Federal Hospital Insurance Trust Fund, 1983). As experience under the PPS develops and is quantified and analyzed, it will be possible to make more accurate projections.
Historically, there has been significant regional and local variation in levels and rates of change in hospital costs (American Hospital Association, 1983; Health Insurance Association of America, 1983c; Levit, 1982; Wennberg and Gittelsohn, 1982). Geographic variability in hospital costs is expected to continue, but the Medicare PPS provides an incentive for convergence on levels of cost per discharge (when adjustment has been made for area wage levels and case-mix complexity) compared with the pre-PPS period. Geographic areas that have high expenses per discharge compared with the Medicare PPS standards are expected to have relatively lower increases per discharge in the 1980's. Areas with relatively low expenses per discharge are expected to have relatively higher increases.
Community hospital inpatient days are expected to increase at an average annual rate of one-half of 1 percent from 1982 to 1990. This rate is one-third the average annual rate for 1972-82, and results in days growing slower than aggregate population. The aging of the population puts upward pressure on growth in days, while substitution to less expensive types of care (home health, hospital outpatient, physician office, and nursing home) and a more restrictive monitoring of admissions and length of stay, exerts downward pressure. The Medicare PPS is expected to reduce average length-of-stay and thus contribute to this slower growth in days.
Admissions are projected to rise at an average annual rate of between 1 and 2 percent over the 1982-90 period. This rate of increase is somewhat less than the 1972-82 average annual increase of 2 percent. The reduced rate of increase reflects recent historical experience and the increased competition from ambulatory facilities projected to further develop in the 1980's. As the less sick are channeled into ambulatory settings (for example, physicians' offices and hospital outpatient departments) and into nursing homes, it is expected that the hospital case-mix severity may rise slightly compared with the average level of case-mix severity if such channeling had not occurred. Likewise, the average case-mix severity in ambulatory settings and nursing homes may rise, since some patients will be served there who previously were in hospitals.
Intensity of services per admission is projected to rise at an average annual rate of between 2 and 3 percent a year or at a rate 40 percent slower than for the 1965-82 period (Table Q). Growth in intensity of services per day is projected to decelerate, but not to the same extent. As length-of-stay is shortened, the average intensity per day tends to rise since most ancillary services are provided near the beginning of the admission. The quantity and mix of ancillary services are expected to be modified as practice patterns change so that quality care can be provided at prices that third-party payors are willing and able to pay.
Hospitals are expected to put more emphasis on recruiting, credentialing, and reappointing staff physicians, since financial viability and solvency will increasingly be at stake. Physicians who provide high quality care with cost-effective patterns of care should be in highest demand.
In summary, the hospital sector is expected to be dynamic during the 1980's (Goldsmith, 1981). There is likely to be increased rivalry among existing hospitals, and there will be new entrants with more convenient locations and sophisticated cost-effective services. Suppliers to hospitals (for example, surgical supply companies, pharmaceutical companies, registered nurses, unionized employees, and so forth) may attempt to strengthen their bargaining positions relative to hospitals. Buyers of hospital care, such as the Federal Government and the corporate sector, are likely to negotiate more vigorously in the 1980's. Competition with substitute services, such as ambulatory surgery and nursing home care, are likely to be significant. Even with increasing competition and payment reforms, continued rapid growth in the hospital sector is expected to continue in the 1980's because of the aging population, new technologies, and greater ability to pay.
Community hospitals: Outpatient
Historical perspective
The community hospital emergency department and organized outpatient department are significant elements of the health delivery network. The emergency department is intended to diagnose and treat certain types of acute conditions such as injuries, burns, poisonings, and the like. The organized outpatient department, on the other hand, is expected to provide primary and secondary care, much like freestanding ambulatory clinics. In this section, services of emergency departments and organized outpatient departments are combined.
Expenditures for community hospital outpatient services grew from $2.6 billion in 1972 to $15.5 billion in 1982, an average annual rate of 19 percent. This is one of the fastest growing components of total systems cost, rising from about 3 percent of the total in 1972 to almost 5 percent in 1982. The proportion of community hospitals reporting organized outpatient departments has more than doubled in the last decade (American Hospital Association, 1973, 1983), and the array of services has proliferated. Rehabilitation services, occupational therapy, physical therapy, speech pathology, hemodialysis, genetic counseling, alcoholism/chemical dependency services, dental services, and so forth are some of the services available on an outpatient basis, which contribute to hospitals functioning as health care centers in some communities.
Outpatient visits increased at an average annual rate of between 3 and 4 percent during the 1972-82 interval. However, visits in offices of physicians showed almost no change over this same period. Economy-wide inflation accounted for 42 percent of growth in spending (Table L); changes in visits per capita accounted for 14 percent, and increases in intensity of services per visit accounted for 27 percent of the growth.
Projections
The substantial growth in services and revenues is expected to continue, but to be modified by several forces: an increasing supply of office-based physicians relative to the population, the growth in freestanding emergency care centers and in preferred provider organizations (PPO's), the implementation of the Medicare PPS for inpatient services and possible spinoffs to other third-party payors, and increasing scrutiny by third-party payors into the case-mix complexity of hospital outpatient services.
Hospital outpatient services can substitute for or complement office visits. For example, a physician may request that a patient go to a hospital outpatient or emergency department for diagnostic tests not available in the physician's office. Here, the hospital ambulatory services complement the physician's services to jointly produce improved health. The increasing physician-population ratio in the projection period will provide pressures on physicians to make their services relatively more attractive compared with hospital outpatient services than was the case during the 1970's. Some office-based physicians will find it to their advantage to provide more ancillary services, both in quantity and intensity in their offices or clinics. This will enable them to service a portion of the patients who were formerly seen in hospital outpatient or emergency departments where there is typically more equipment available.
The growth in freestanding emergency care centers and PPO's will make some hospital outpatient services less attractive from a competitive price point of view. In 1982, the average revenue per outpatient visit was roughly $70. This is substantially higher than the average revenue per visit in most ambulatory facilities. While there is no doubt that the case-mix complexity (and, thus, cost) of emergency room visits is significantly more severe than that of office-based physician visits, there is growing evidence that the case-mix complexity of hospital outpatient department (not including emergency department) visits may be only slightly more severe than for visits in offices of physicians in private practice (Dutton, 1979; Lion and Altman, 1982).
There is likely to be significant interest in the development of case-mix and DRG-type measures for hospital outpatient services (Fetter, 1980; Office of Research and Demonstrations, 1983). The advisability of using such case-mix measures as a fairer and more efficient way to reimburse for outpatient services will be studied and debated. The timing of implementing such a system, if, indeed, one is implemented in the foreseeable future, is conjectural.
The implementation of the Medicare PPS may have dual effects on outpatient services. On the one hand, hospitals find it to their financial advantage to admit more patients for inpatient services11, since there is a predetermined price per discharge that is independent of length of stay or services provided. On the other hand, hospitals may find it to their financial advantage to provide certain services on an outpatient basis rather than inpatient, since Medicare still has retrospective cost-based reimbursement for outpatient care. Some patients may be discharged earlier than would otherwise be the case, with follow-up outpatient services provided on a reasonable cost basis. Utilization and quality control peer review organizations (PRO's) will provide medical review and admission pattern monitoring to identify and alter inappropriate behavior.
To the extent that other third-party payors adopt DRG-type prospective payment plans, the effects of the Medicare plan on patterns of outpatient care will be intensified. In addition, the management information system that links clinical and financial data for Medicare inpatient services is sure to have spillover effects that alter behavior of the hospital staff and administrators.
Hospitals will develop strategies to be more competitive for outpatients (including expansion of outpatient facilities and services) so that the outpatient services will be a feeder system for inpatient services. There are likely to be careful analyses made of the hospital outpatient catchment areas to identify needs of the various demographic, ethnic, and income groups. Services will be developed to meet these shifting needs, backed by effective demand. Mergers, acquisitions, and the joining of multihospital systems will accelerate the timing and impact of some of the forces discussed above.
Several of the factors shaping the future of hospital outpatient sector can be anticipated, but not quantified in magnitude or time. Because of this, the difficulties inherent in projecting patterns of spending for this sector are clear.
The short-term outlook is for outpatient spending to reach $20 billion in 1984, an average annual rate of increase of 15 percent from 1982. Spending is expected to reach $30 billion in 1987 and $42 billion in 1990. Economy-wide inflation is projected to account for 35 percent of the growth in spending over the 1982-90 interval. Inflation-adjusted (real) output is projected to grow at an average annual rate of 6 percent over the 1982-90 period. This rate is substantially higher than for community hospital inpatient services or physicians' services, but only two-thirds the rate of real output growth for the last decade. Increasing competition from ambulatory services and more stringent payment, more closely linked to case-mix complexity, will have dampening influences on the hospital outpatient sector.
Federal hospitals
Historical perspective
There are 346 Federal hospitals operated by the Veterans' Administration, Department of Defense, Department of Justice, and Public Health Service (including the Indian Health Service). In 1982, these hospitals had 114,000 beds, handled 2 million admissions, and provided 33 million patient days of service. They also provided 56 million outpatient visits (American Hospital Association, 1983). Since 1972, there has been a decrease in the number of hospitals (by 55), the average number of beds per hospital, and the average length of stay. The number of admissions and outpatient visits have risen. The case-mix of Federal hospitals is shifting toward a higher proportion of short-term acute care patients. This is consistent with the rapid rise in intensity of services provided per patient day from 1972-82.
Expenditures reached $10.2 billion in 1982 (Gibson et al, 1983), increasing at an average annual rate of 11 percent since 1972. Economy-wide inflation accounted for two-thirds of this increase (Table L). A 21 percent decline in patient days, from 41.6 million in 1972 to 33.0 million in 1982, had a retarding effect on growth. The rise in services and supplies provided per patient day (including more outpatient services, since they cannot be separated out) had a strong positive effect on the rise in spending for Federal hospitals.
These hospitals have a substantially higher proportion of total expenses attributable to labor costs than community hospitals; however, comparing the Federal hospitals with the community hospitals, the Federal hospitals have a lower ratio of full-time equivalent personnel to average daily census. Federal hospital payroll expenses per full-time equivalent worker are higher than in community hospitals, but have experienced lower rates of increase during the 1972-82 period.
Projections
It is expected that growth in Federal hospital spending will be slowed in the 1982-90 period because of lower economy-wide inflation, the closing of some Federal hospitals, budget constraints on the growth in total Federal spending, and more effective payment strategies that attempt to link payments more closely to case-mix complexity.
One component of the Federal hospital sector, Veterans' Administration (VA) hospital, is likely to experience pressures to expand in the 1980's. The number of war veterans aged 75 and over is expected to increase at an average annual rate of approximately 8 percent during the 1982-90 period (Langberg and Maloy, 1982; Veterans' Administration, 1982). The aged 75-and-over war veterans will receive services through non-Veterans' Administration (VA) contract hospitals, as well as in the VA facilities. There is likely to be pressure to use a higher proportion of non-VA contract hospitals' services to handle the increased need.
Historically, Federal hospital spending growth showed considerable variability (Freeland and Schendler, 1983), and this is likely to continue. Given current trends and assumptions, expenditures in Federal hospital facilities will be approximately $19 billion in 1990.
Physicians' services
Historical perspective
The physicians' services industry has a much greater impact than is indicated by the nearly 22 percent of total systems cost that this sector consumes (Table N). Physicians control a substantial proportion of the total process of care. In Victor Fuchs' 1974 edition of Who Shall Live?, a major theme and title of a chapter is “The Physician: The Captain of the Team.” In his 1983 edition of the same book, Fuchs states that a more appropriate chapter title would be “Physician: The Co-Captain of the Team.” He explains that one of the most significant developments in medical care delivery in the past decade is the growth of management in clinics, hospitals, and other health care organizations. He emphasizes the need for physicians to share control and power with managers in order to work out compromises that meet the interests of all parties: society, patients, management, and health professionals. The implementation of the Medicare PPS will accelerate this important trend toward integration of clinical medicine with management.
The non-Federal, office-based physicians' services industry is large and complex, with spending totaling $62 billion in 1982 (Table 5). This amount is 2 percent of the GNP and is almost two-thirds of the $99 billion dollars spent on community hospital inpatient services.
In 1982, there were 478,900 active physicians (Table 4), approximately 1 active physician for each 500 persons in the United States. Ninety-six percent of the active physicians are M.D.'s, and the remaining 4 percent are osteopaths (D.O.'s). The major activity of approximately two-thirds of all active physicians is non-Federal, office-based practice. The other one-third are involved in hospital-based care, government service, teaching, research, administration, and so forth. There were roughly 1.3 billion physician visits in 1982 by approximately 75 percent of the population. There were about 5.7 visits per capita, including physician-billed hospital inpatient visits.
Expenditures for physicians' services increased from $17 billion in 1972 to $62 billion in 1982 (Table 5), an annual growth rate of about 14 percent. Of this expenditure growth, increases in overall inflation (GNP deflator) accounted for 57 percent (Table L); the CPI for physicians' fees, in excess of the GNP deflator, accounted for 13 percent; visits accounted for 3 percent; and intensity per visit (as measured by real expense per visit) for 27 percent (Figure 12). Excluding economy-wide factors (GNP deflator and population) and focusing on physician service-specific factors (physician fees in excess of overall inflation, visits per capita, and intensity per visit), intensity accounted for 78 percent of expenditure growth.
Figure 12. Factors accounting for growth in expenditures for physicians' services: 1972-82.
It is important to note that intensity per visit is calculated as a residual. Average revenue per physician visit is deflated by a fixed-weight price index for a constant composition of care (the CPI for physicians' services). To the extent there are measurement or conceptual errors in any variables (total business receipts, total visits, and CPI for physicians' services), there will be compensating errors in the residual calculated variable of growth in real services per visit (intensity). If physicians unbundle services (separate services and procedures into finer components and bill individually for each service or procedure) and charge more for the unbundled services than they had previously charged for the same services bundled, it results in actual prices rising faster than the Bureau of Labor Statistics' fixed-weight constant composition price index for physicians' services. If actual prices are, in fact, rising faster than the CPI for physicians' services, this manifests itself as growth in the residual intensity factor. Unfortunately, there do not seem to be any national data to determine whether actual prices are rising faster or slower than the CPI for physicians' services. In any case when third-party payors adopt revised procedural coding systems that unbundle services, or when physicians unbundle services themselves, there is potential for prices to rise faster than if such unbundling did not take place.
The rapid growth in intensity is indicated by various measures—both direct and indirect. Real services (intensity) per visit include such factors as shifts in mix of services, out-of-hospital laboratory tests, surgical procedures, minutes of direct patient care, and staffing per visit. Specific examples include the following: 1) the volume of out-of-hospital laboratory tests increased at an average annual rate of nearly 10 percent between 1975 and 1978 (Laboratory Management, 1979); 2) the number of surgical operations, as indicated in the American Hospital Association Panel Survey, increased from 15.2 million in 1972 to 19.7 million in 1982, an average annual rate of growth of 2.6 percent (this growth rate is 2½ times that of aggregate population growth, and is substantially faster than the 0.3 average annual growth rate for total physician visits); 3) the average number of minutes of direct physician patient care per visit rose from 20 in 1970 to 24 in 1980, an increase of almost 20 percent (Freeland and Schendler, 1983); and 4) the Bureau of Labor Statistics (Employment and Earnings) indicates that for the period 1972-82, total employment (supervisory and nonsupervisory) in offices of physicians and surgeons increased 84 percent. During this same period, the number of non-Federal office-based physicians increased 50 percent.12 Nonphysician staff (secretaries, nurses, and so forth) increased faster than the number of physicians, and both categories of employment grew faster than visits. Thus, the staffing associated with each visit has increased.
Increases in intensity of services per visit is caused, in part, by demand for increased quality of care which, in turn, is driven by insurance coverage (low cost-sharing) and the fee-for-service/usual-customary-reasonable reimbursement system (Delbanco et al., 1979; Roe, 1981; Showstack et al., 1979; Sloan and Steinwald, 1975).
Per capita expenditures for physicians' services are nearly three times greater for the population aged 65 and over than for the nonaged. Both the number of physician visits per capita and intensity of services per visit are relatively higher for the aged (Fisher, 1980). The continued aging of the population will contribute to growth in expenditures for physicians' services.
Between 1972 and 1982, the number of active physicians increased at an average annual rate of over 3 percent, while the population increased at a 1 percent rate. In the projected period, the annual rate of growth of physicians is slightly less than 3 percent (Table 4). Under current analyses are the effects of projected increases in active M.D.'s and D.O.'s (Bloom, 1980) relative to population on intensity per visit; fees; visits per capita; distribution by specialty, income, and geographic area; and the like (Graduate Medical Education National Advisory Committee, 1980; Hendrickson, 1980; Schwartz et al., 1980; Sloan and Schwartz, 1983).
Real per capita expenditures for physicians' services rose at an average annual rate of 3 percent, and real services per physician declined an average of almost 1 percent per year for the 1972-82 period (Table 13). These data indicate that the large increase in the number of active physicians relative to population has been associated with more real services provided per capita, but with a relatively constant or declining volume of real services per physician.
Table 13. Average income per physician and per capita expenditures for physicians' services, current and real dollars: 1972 and 1982.
| Selected variables | Year | Average annual percent change | |
|---|---|---|---|
|
| |||
| 1972 | 1982 | ||
| Per capita expenditures for physicians' services, current dollars1 | $ 80 | $ 262 | 12.5 |
| Real per capita expenditures for physicians' services2 | $ 60 | $ 80 | 2.9 |
| Professional expense per physician, current dollars3 | $31,318 | $ 78,400 | 9.6 |
| Real professional expense per physician4 | $31,318 | $ 36,773 | 1.6 |
| Net income from medical practice per physician, current dollars3 | $47,240 | $ 99,500 | 7.7 |
| Real net income from medical practice per physician4 | $47,240 | $ 46,670 | −0.1 |
| Gross income per physician, current dollars3 | $78,558 | $177,900 | 8.5 |
| Real service output per physician5 | $58,713 | $ 54,394 | −0.8 |
| CPI for physicians' services | 133.8 | 327.1 | 9.3 |
| Fixed-weight price index for personal consumption expenditures6 | 100.0 | 213.2 | 7.9 |
| Real CPI for physicians' services4 | 133.8 | 153.4 | 1.4 |
Deflated by the CPI for physicians' services.
Deflated by the fixed-weight price index for personal consumption expenditures. See Bureau of Economic Analysis, (1983).
Real service output is approximated by deflating gross income per physician by the CPI for physicians' services.
While average net income from medical practice rose at an average annual rate of nearly 8 percent in nominal terms, real income, after adjusting for inflation, was flat for 1972-82 (Table 13). Average total tax-deductible professional expenses per physician increased at an average annual rate of almost 10 percent, faster than the 8 percent average annual inflation rate measured by the fixed-weight personal consumption price index. A portion of the relatively fast growth in expenses and slow growth in net income may reflect physicians' putting increasing amounts of their income into deferred compensation pension programs. Thus, what formerly was included as net income is included as professional expenses (American Medical Association, 1980).
The increasing incidence of malpractice suits in the 1970's has affected expenditures in two ways (Greenspan, 1979; Henderson, 1979): 1) fees were raised to reflect increased costs from higher malpractice insurance premiums, and 2) the quantity of services provided increased as physicians became more thorough in response to the threat of malpractice suits. In the projected period, this threat will continue to be a factor in physicians' practice costs, but not as significant a cost determinant as it was in the 1970's.
The Federal Government paid out $13 billion for physicians' services in 1982 (Table 7), most of it under Medicare. Medicare outlays increased nearly twice as fast as Federal Medicaid outlays from 1972 to 1982—physicians' services are a declining proportion of Federal Medicaid benefits and a constant proportion of Medicare benefits (Tables F and 10). Private health insurance pays 28 percent of its benefits for physicians' services (Table 11) and the extent of coverage varies greatly among different policies and contracts (Bureau of Labor Statistics, August 1983; Health Insurance Association of America, 1983a).
Projections
Expenditures for physicians' services are projected to rise from $62 billion in 1982 to $76 billion in 1984. Physician fees, as measured by the CPI, are projected to substantially decelerate to a 7 percent annual rate during this period, compared with the over 10 percent average annual increase over the 1979 to 1982 interval. In 1987, expenditures are expected to reach $103 billion and by 1990, $134 billion. The average annual rate of increase from 1982 to 1990 is expected to be 10 percent.
The lack of public funds will dampen the growth of expenditures, but the projected increase in real income for the 1982-90 period is expected to bolster demand for services. A continued upward trend in intensity of services per visit is projected, partially reflecting growth in technologies. The number of patient contacts per physician is projected to continue declining, with physicians spending more time per contact. Competition between office-based physicians and hospital outpatient departments for increasing market shares of patients is projected to intensify.
The Medicare PPS has a fixed payment rate per hospital discharge that is independent of length-of-stay and ancillary services and, as previously discussed, the incentive will be to reduce length-of-stay and economize on ancillary services that are not medically necessary. Non-Federal, office-based physicians receive a substantial portion of their gross receipts from services provided in hospitals rather than in their office. Since under the Medicare PPS, use of ancillary services is constrained in hospitals but not, in an analogous way, in offices and clinics, physicians have an incentive to provide more ancillary services in the office setting. In addition, to the extent that office-based physicians gain a larger share of the patient services that previously were provided by hospitals,13 their average case-mix complexity may rise and contribute to the growth in intensity of services. This will put upward pressure on the demand for surgical and medical instruments, appliances, and supplies in offices and clinics (Bandy, 1983; Cassack, 1983; Interindustry Economics Division, 1979).
In the 1980's, there will be competitive pressures to make careful assessments of catchment areas so that unique needs can be met. Freestanding emergency, primary care, and ambulatory surgery centers will be competing aggressively to develop their niche in the market (Trauner et al., 1982). PPO's and health maintenance organizations (HMO's) will also be expanding.
There is substantial research on, and discussion of, the advisability and feasibility of extending DRG-type payment systems to the services of physicians (McIlrath, 1983; Office of Research and Demonstrations, 1983). Irrespective of whether such a system is developed and used, the perverse cost-increasing incentives of our current fee-for-service/usual-customary-reasonable systems are well known, and some modification to our current payment systems is likely in the 1980's.
Under current Medicare law, including PPS for inpatient services, benefit payments for physicians' services are projected to rise substantially faster than for inpatient hospital services (Tables B and F). These projected increases, combined with the 1979-82 experience of very rapid increases in Medicare physician benefit payments (Table E), are sure to raise questions on the ability to finance such increases for extended periods into the future.
Dentists' services
Historical perspective
The prevention and control of dental disease was a $20 billion industry in 1982, and made up approximately ½ percent of the GNP. Some 133,000 active dentists (approximately one dentist per 1,800 persons) provided roughly 400 million visits in 1982. Nine-tenths of active dentists were in non-Government, office-based practice in the year. About half the population had one or more visits, and the per capita visit rate was approximately 1.7. By contrast, in 1972, 47 percent of the population had one or more dental visits, and the per capita visit rate was 1.5.
Expenditures for dentists' services increased an average of 13 percent annually in the 1972-82 period (Table 6), more than tripling from $6 billion in 1972 to $20 billion in 1982. During this period, the number of active dentists increased at a rate more than twice as fast as the total population (Table 4).
Overall inflation accounted for 59 percent of the growth in expenditures for dentists' services from 1972 to 1982 (Figure 13 and Table L). Growth of dentists' fees in excess of overall inflation accounted for only 3 percent of the expenditure growth. This better price performance of the dental services sector relative to some other health sectors such as physicians' services, reflects, in part, more consumer cost sharing, competitive forces within the industry, better productivity performance, and the relative reduction in demand for dental services associated with more extensive use of fluoridation (Feldstein, 1974; Medicus Systems, 1980).
Figure 13. Factors accounting for growth in expenditures for dentists' services: 1972-82.
Intensity (as measured by real expense per visit) accounted for 21 percent of expenditure growth in the last decade. When focusing on factors specific to dental services, intensity contributed 62 percent (Figure 13). Intensity includes providing more services and procedures per visit (for example, high-speed drill use increases the average number of cavities filled during one visit), as well as shifts in the mix of services and procedures (for example, a greater proportion of expensive procedures, such as orthodontics and periodontal work).
The staffing associated with each visit has increased, contributing to the growth in intensity of service per visit. Bureau of Labor Statistics (Employment and Earnings) data indicate that total employment (supervisory and nonsupervisory) in offices of dentists approximately doubled for the period 1972-82. The number of dentists increased 26 percent during this same period (Table 4).14 Nondentist staff (clerical, dental auxiliaries, and so forth) are increasing faster than the number of dentists, while the number of dentists is growing at about the same rate as dental visits.
There is little relationship between changes in the age-sex mix of the population and changes in the number of dental visits per capita (Russell, 1981); however, the aged spend slightly less for dental services (Fisher, 1980) per capita than the nonaged.
Projections
The short-term projected expenditures for dentists' services are expected to rise from $20 billion in 1982 to $24 billion in 1984 (Table 5), an average annual rate of growth of 10 percent. Aggregate demand for dental services appears strong in mid-1983. The number of nonsupervisory employees (a rough indicator of demand) in offices of dentists was 6 percent higher in July 1983, compared with the same month a year earlier (Bureau of Labor Statistics, Employment and Earnings). The fast growth in dental insurance (Employee Benefit Plan Review, 1981) is a factor fueling the demand for dental services. In some cases, switches from mental health coverage, which provides significant benefits to a relatively small proportion of the covered population, to dental insurance coverage, which provides some benefits to a large proportion of the insured population, has contributed to the growth in dental insurance coverage.
Although aggregate National demand is strong (as measured by employment growth and price increases for dental services in excess of economy-wide inflation) practitioners in selected geographic areas with high unemployment are experiencing the negative impact of prolonged recession. As disposable household income declines and loss of employment-related insurance occurs, use of dental services declines. As the economy recovers and robust growth occurs, there will be additional growth in economy-wide employment, dental insurance and use of dental services.
Expenditures for dentists' services are expected to reach $31 bilion by 1987 and $39 billion by 1990 (Table 5). The annual rate of growth from 1982 to 1990 is expected to be 9 percent, substantially below the 13 percent annual rate for the 1971-82 period, when there was very rapid growth in dental insurance and higher economy-wide inflation.
Private health insurance is expected to finance an increasing share of benefits for dentists' services in the next decade (Bell, 1980; Employee Benefit Plan Review,1981), but at a slower rate of increase. It is assumed that the majority of dental plans will have deductibles, coinsurance, and maximum benefit amounts (Bureau of Labor Statistics, 1983; Health Insurance Association of America, 1983a, 1983b), so that consumer cost-consciousness will be a factor in restraining demand. Faster growth in real income for 1982-90 is expected to put upward pressure on the growth in demand for dentist's service.
In the 1980's, there is expected to be a continuation of a trend in the dental case-mix—a decline of cavities in children and an increased retention of natural teeth in adults (American Dental Association, 1983). The prevention, diagnosis, and treatment of periodontal disease will take on increasing importance as the population retains their natural teeth (American Dental Associations, 1982).
There are expected to be increases in the intensity of services provided, and these will augment the demand for dental equipment and supplies (Bandy, 1983; Cassack, 1983.)
There is wide dispersion in per capita spending for dental services among the States. Spending in Mississippi and Kentucky was about 50 percent of the National average in 1978; spending in Washington was approximately 50 percent more than the National average in 1978 (Levit, 1982). The increasing supply of dentists relative to the population may induce some dentists to locate in areas with low densities of practitioners. This may be a geographic equalizing force to increase access and use among underserved areas.
An important factor to watch in the 1980's is the growing trend toward “department store dentistry, ” with its emphasis on advertising, competitive prices, evening and weekend hours, and walk-in services (Cole, 1981; Trauner et al., 1982). There is likely to be intensified pressure to integrate clinical skills with modern techniques of management, catchment area analysis, and finance, so that costs (and, thus, prices) and services are competitive with other dentists in the catchment area.
The vast, unmet need for dental services is well documented. For example, the average American has lost 5 teeth and has 11 dental caries by age 35 (American Dental Association, 1983). However, converting this unmet need into effective demand may be difficult if the growth in dental insurance decelerates.
Other professional services
Historical perspective
Services of optometrists, podiatrists, chiropractors, registered and practical nurses engaged in independent practice, occupational therapists, clinical psychologists, freestanding home health agencies and the like are an increasingly significant component of our health care delivery system. The burgeoning growth in home health services is a significant contributor to the rise in spending for these services. Expenditures for other professional services have grown from nearly $2 billion in 1972 to over $7 billion in 1982, an average annual rate of increase of nearly 15 percent (Tables 5 and 6). Economy-wide inflation accounts for 53 percent of this increase, and growth in real services per capita accounts for nearly 40 percent of this increase (Table 8).
There appears to be more intense price competition and advertising in the sector of other professional services than in the physicians' and dentists' services sectors. Direct, out-of-pocket payments accounted for about 50 percent of the professional services outlays in 1982, with insurance playing a relatively smaller role in consumer demand than for other types of services (Table 7). The pricing behavior of other professional services reflects this competitive environment. From 1978-82 (the period of the newly available price index for other professional services), other professional fees (mostly for services of optometrists) rose at an average annual rate of about 8 percent; whereas physicians' fees rose at an average rate of 10 percent and dentists' fees, an average rate of 9 percent.
Projections
Expenditures for other professional services are projected to reach $9 billion in 1984, $12 billion in 1987, and $16 billion in 1990 (Table 5). Real expenditures are projected to rise rapidly at rates significantly exceeding both real GNP and real National health expenditures.
The implementation of the Medicare PPS is expected to increase demand for home health agency services, one component of other professional services. Since hospitals receive a predetermined price, independent of length-of-stay or services provided, per Medicare discharge, a financial motivation is present to discharge patients earlier than would be the case under retrospective cost-based reimbursement. Some of these discharged patients will need more home health services than was previously the case. In addition, the temporary Medicare hospice benefits permits patients diagnosed as terminally ill to live their last months at home, under the supervision of a hospice organization. Demand for this component of home care will be augmented by the Medicare benefit.
Because of the substitute and complementary relationships between other professional services and medical care services such as that provided by hospital, physician, and nursing home, it is difficult to accurately project this expenditure category. Alternative scenarios can produce projections that are significantly different. The situation is complicated by the fact that home health agency services can substitute for and complement personal care services provided by household members (U.S. General Accounting Office, 1982). If reimbursement regulations for nursing home care are significantly changed, it will influence the need for personal care services provided by household members and shift the demand for home health services.
As competition increases in the medical care services sector, the role of other professional services may change substantially. Home health services provide a cheaper alternative for some hospital, nursing home, and physician services. Optometrists, podiatrists, and chiropractors provide services that can sometimes substitute for or complement physicians' services. If consumer cost-sharing increases (including deductibles), increased use of other professional services can be expected, as consumers become more sensitive to prices and substitute cheaper alternatives.
Drugs and medical sundries
Historical perspective
Given the significant power of drugs to alter the course of illness, Fuchs (1983) has stated that this could well be called the “drug age.” Drugs and medical sundries dispensed through retail channels are less than 8 percent of total systems cost (Table N), but the effectiveness of other segments of the health care sector would be vitally impaired without the use of drugs dispensed in outpatient settings. The deinstitutionalization, through the use of psychotropic drugs, of a significant portion of the mental hospital population is an example of the cost-effective use of drug therapy.
In 1982, there were 1.5 billion prescriptions written in outpatient settings (Pharmacy Times, 1983). This is nearly 6.5 prescriptions per capita and underscores the widespread use of prescription drugs. About three-fourths of 1 percent of the GNP is spent on drugs and medical sundries. This category includes expenditures for prescription drugs (57 percent), over-the-counter drugs (31 percent), and medical sundries (12 percent).15
According to U.S. Department of Commerce data, expenditures for drugs and medical nondurables, dispensed through retail channels, have grown from $9 billion in 1972 to $22 billion in 1982, an average annual growth rate of 9 percent (Table 6). Seventy-seven percent of this increase in spending was accounted for by the rise in prices of drugs and medical sundries. Drug prices (in the CPI for medical commodities) rose at a slower rate than economy-wide inflation during this period (Table 8). Growth in population and real spending per capita each accounted for between 11 and 12 percent of the growth.
Aged persons spend more than twice as much per capita for drugs and medical sundries as the nonaged (Fisher, 1980). The aged use significantly more prescriptions per capita than the nonaged and pay a higher average price per prescription, reflecting larger dosages per prescription (Trapnell, 1979).
The pharmaceutical preparations industry and the drugstore industry are notable for extraordinary productivity increases (Brand, 1974; Cocks, 1983; Friedman, 1980). From 1965 to 1974, output per hour increased at an average annual rate of about 5 percent for all employees in the pharmaceutical preparations industry and at an almost 6 percent rate for all employees in the drugstore industry (Bureau of Labor Statistics, December 1982) (Figure 14). For the most recent 7-year period for which there are complete data, 1974-81, productivity increased but at substantially lower rates than previously—about 2 percent average annual rate for pharmaceutical preparations and about 1 percent rate for drugstores (Bureau of Labor Statistics, July 1983).
Figure 14. Drug industry trends for productivity and inflation-adjusted prices (consumer and producer): 1965-82.
Prices of drugs at both the producer and consumer levels of distribution rose at rates significantly lower than the overall inflation rate for the period 1965-74. During this period, the implicit price deflator for GNP rose at an average annual rate of 5 percent; whereas producer prices for drugs (Producer Prices and Price Indexes, Code 063, drugs and pharmaceuticals) and consumer prices (CPI Detailed Report, medical care commodities) rose at average annual rates of about 1 percent. After adjusting for economy-wide inflation, producer and consumer prices decreased at a rate of approximately 4 percent.
Since 1974, consumer and producer drug prices have increased at an average annual rate of 8 percent, about 0.5 percentage point higher than economy-wide inflation. Figure 14 indicates that during periods of substantial productivity increases in the manufacture of pharmaceuticals, such as 1965-74, inflation-adjusted producer prices for drugs declined at significant rates. As productivity increases decelerated, as during the 1974-81 period, inflation-adjusted producer prices increased, compared with the higher productivity period of 1965-74. This same productivity/inflation-adjusted price association also applies at the retail level, when drugstore productivity is compared with inflation-adjusted consumer prices for drugs.
Consumer prices for drugs tend to move in tandem with producer prices, indicating that the markup of retail prices over producer prices has been fairly stable in spite of significant productivity increases in drugstores (Figure 14). In 1982, however, consumer prices rose 10.3 percent, compared with an 8.6 percent increase in producer prices. Productivity in drugstores dropped 1.3 percent in 1982 (Bureau of Labor Statistics, July 1983). When producer price increases are adjusted upward to reflect rises in unit costs in drugstores, because of the decline in productivity for drugstores as a whole, the two series increase essentially at the same rate (10.3 percent for consumer prices and 10.0 percent for producer prices, adjusted upward for negative productivity at the retail level).
The drug industry, in both retail and producer segments, illustrates the inverse relationship between productivity increases and price increases. As previously discussed, one purpose of the Medicare PPS is to increase productivity in the hospital segment so that hospital prices will increase at a slower rate than would otherwise be the case. The drug industry from 1965 to 1974 exemplifies this productive economizing behavior with attendant favorable price performance (Figure 14).
Projections
The short-term outlook is for expenditures for drugs and medical sundries to rise from $22 billion in 1982 to $27 billion in 1984, an average annual rate of increase of 9 percent. Drug prices rose faster relative to overall inflation (in the CPI for all items) in the 12 months ending September 1983 than for any calendar year in the 1965-82 period. For the 12 months ending September 1983, the CPI for prescription drugs rose over 11 percent; the CPI for medical care commodities (mostly drugs) rose 9 percent; the CPI for internal and respiratory over-the-counter drugs rose over 8 percent; and overall inflation (in the CPI for all items) was 3 to 4 percent.
Real income is projected to increase sharply in 1983 and grow steadily from 1984 to 1990; this is expected to increase demand for drugs and medical sundries. Expenditures are projected to reach $34 billion in 1987 and $44 billion in 1990 (Table 5). For the period 1982-90, expenditures are projected to increase at an average annual rate of roughly 9 percent.
Private health insurance benefits financed 12 percent of outlays for drugs and medical sundries in 1982, and the public sector financed another 9 percent, leaving 79 percent financed by direct consumer payments. The projections assume moderate growth in private health insurance coverage (Table 7), but assume no significant expansion of benefits through a National health insurance program (Trapnell, 1979) or the addition of the Part B drug benefit under Medicare.
The Medicare PPS system will force hospital materials managers to be more cost-conscious (Long, 1983). Hospitals may drive a harder bargain in their purchasing decisions relating to drugs: quantity, quality, generic vs. brand name, and price and quantity discounts. If profit margins and volume of sales are squeezed on hospital sales, manufacturers and distributors may try to compensate by raising profit margins and expanding sales to retail trade outlets.
The application of computer information support systems is expected to expand in the 1980's (American Druggist, 1983; Wertheimer, 1983). Patient drug history profiles, in combination with patient information on major conditions, are being used to enhance quality of care and reduce the possibility of errors in prescribing patterns.
It is difficult to project expenditures for drugs in the 1980's, given the changes in productivity and pricing practices in the industry since 1974 (discussed earlier) and the potential new product lines, including biotechnologies, which may significantly alter prescribing patterns (Hoff, 1983; American Druggist, 1983; Institute for Alternative Futures, 1983; McIntyre, 1983). It is also difficult to assess full implications of the Food and Drug Administration (FDA) procedural changes to reduce the time and expense associated with introducing drugs into the market.
Eyeglasses and appliances
Historical perspective
Consumer expenditures for ophthalmic products and durable medical equipment increased from $2.3 billion in 1972 to $5.7 billion in 1982 (Table 5), an average annual growth rate of nearly 10 percent. These expenditures are primarily for ophthalmic products.
Relative to most health services and supplies sectors, the market for ophthalmic goods is quite competitive (Benham, 1972; Feldman and Begun, 1978), as evidenced by its considerable price competition and advertising. Direct, out-of-pocket payments accounted for 78 percent of outlays for eyeglasses and appliances in 1982, with public and private insurance exercising a relatively small role in consumer demand.
From 1978 to 1982, the new CPI for eyeglasses increased at an annual rate of about 6 percent, compared with an overall inflation (GNP deflator) rate of 8 percent during this period. The CPI for eyeglasses has decreased at an average annual rate of nearly 2 percent, when adjustment is made for economy-wide inflation. In addition, for this same period, the new CPI for nonprescription medical equipment and supplies increased at an annual rate of 8 percent, approximately the same as economy-wide inflation.
The low price increases for eyeglasses, relative to overall inflation, had a negative impact on growth in current dollar spending (Table 8), but this lower relative price probably increased demand and sales. Real sales volume increased at a much faster rate than real GNP from 1972 to 1982. Growth in real services per capita accounted for 29 percent of the expenditure increases (Table 8).
Projections
Expenditures for eyeglasses and appliances are expected to grow from about $6 billion in 1982 to nearly $7 billion in 1984. Consumption of eyeglasses and durable medical equipment appears to have been sharply curtailed in 1982, based on U.S. Department of Commerce data. Third-party payments finance a small proportion of the expenditures, and consumers delay or even forego/purchase of eyeglasses and appliances during a recession. Retailers of eyeglasses reacted to the decline in demand by decelerating price increases. Real consumption in 1983 is rebounding smartly, according to partial-year U.S. Department of Commerce data. After reaching a low point in June 1983, the price of eyeglasses began to accelerate. As demand is picking up, prices are rising, but with a lag.
By 1990, it is expected that expenditures will reach $11 billion. The projections assume that real consumption will rise substantially faster than real GNP between 1982 and 1990, and that consumer prices for eyeglasses will continue to rise slower than economy-wide prices based on the competitive market conditions.
Competition is likely to intensify for various types of contact lenses—soft, semi-soft, and hard—and more variety is on the way (Hughey, 1982). There is a large market that chains and individual practitioners are competing for. Extended-wear and gas-permeable lenses are two of the specialty types of lenses in which the competition is expected to be especially intense. Private health insurance benefits are projected to increase faster than outlays in total for eyeglasses and appliances, thus financing a higher proportion of the expenses (Table 7) (Bell, 1980; Carroll and Arnett, 1981).
“Appliances” as used here include durable medical equipment. The growth in durable medical equipment (walkers, traction equipment, wheelchairs, oxygen, hospital beds, and so forth) is associated with growth in home health services (Cassack, 1983; Janssen and Saffran, 1981), which is included in the HCFA expenditure category of other professional services. The future expenditure growth for durable medical equipment (Bandy, 1983; Cassack, 1983) will partially be a function of reimbursement policies of Medicare, Medicaid, and private health insurance of both home health services and durable medical equipment. The Medicare PPS is expected to encourage short lengths of stay for inpatient hospital services. This should expand the demand for home health services. This, in turn, increases the demand for durable medical equipment, a complement of and integral component of home health services.
Nursing home care
Historical perspective
The $27 billion spent on nursing home care in 1982 made up nearly 1 percent of GNP. Nursing home care has risen dramatically, from less than 2 percent of total systems cost in 1950 to over 9 percent in 1982 (Table N), reflecting expenditure growth at an average annual rate of 17 percent. The only other total systems cost category that increased in relative importance over this period, hospital care (Table N), increased at an annual average of 12 percent.
Spending for nursing home care refers to expenditures in all facilities (excluding hospital-based) that provide nursing care. This includes skilled nursing facilities (SNF's), certified by Medicare or Medicaid, and intermediate care facilities (ICF's) for regular patients and for the mentally retarded (ICF-MR), certified by Medicaid. In addition, all other homes that provide nursing care at some level are included, even though the facilities are not certified by Medicare or Medicaid.
Medicaid (49 percent) and Medicare (2 percent) finance half of all outlays for nursing home care. In January 1983, there were 8,080 SNF's, with 727,000 beds, participating in Medicare or Medicaid; 11,304 ICF's, with 977,000 beds, participating in the Medicaid program16; and, an additional 1,445 ICF's-MR participating in the Medicaid program (Bureau of Data Management and Strategy, 1983).
Expenditures for total nursing home care increased at an average annual rate of over 15 percent from 1972 to 1982 (Table 6). Expenditures for the ICF-MR component have been increasing at a faster rate. From 1976 to 1982, expenditures for ICF-MR increased at an average annual rate of over 30 percent, compared with a 14 percent rate for nursing home care excluding ICF-MR.
This fast growth of nursing home care expenditures is due to an interplay of demand and supply factors (Birnbaum et al., 1982; Dunlop, 1978; Liu et al., 1983; Scanlon, 1978; U.S. General Accounting Office, 1983). Demand factors include a demographic shift toward the aged (Tables 2 and 3) (Russell, 1981); increases in real income—each succeeding age cohort of residents has higher real income; expanded Medicaid benefits, including the addition of the ICF-MR benefit in 1973 (Allard and Toff, 1980; Copeland and Iverson, 1980; and Trapnell et al., 1981); and, the transfer of patients from mental hospitals to nursing homes (Bassuk and Gerson, 1978). Supply factors include two increases: in number of nursing home beds (Bureau of Data Management and Strategy, 1983; U.S. General Accounting Office, 1983) and in prices paid for inputs (Table 14) (Data Resources Inc., 1983; Fisher and Schendler, 1980).
Table 14. National nursing home input price index compared with overall inflation in the economy: 1972-82.
| National Nursing Home Input Price Index1(1977 = 100.0) | Implicit price deflator for gross national product2(1972 = 100.0) | National nursing home input price index deflated by implicit price deflator for GNP | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Calendar year | Level | Percent change | Level | Percent change | Level | Percent change |
| 1972 | 68.1 | ---- | 100.0 | --- | 68.1 | --- |
| 1973 | 71.9 | 5.6 | 105.7 | 5.8 | 68.0 | −0.2 |
| 1974 | 79.3 | 10.3 | 115.1 | 8.9 | 68.9 | 1.3 |
| 1975 | 86.9 | 9.6 | 125.7 | 9.2 | 69.1 | 0.3 |
| 1976 | 93.4 | 7.5 | 132.3 | 5.2 | 70.6 | 2.1 |
| 1977 | 100.0 | 7.1 | 140.0 | 5.8 | 71.4 | 1.2 |
| 1978 | 108.8 | 8.8 | 150.4 | 7.4 | 72.4 | 1.3 |
| 1979 | 118.6 | 9.0 | 163.4 | 8.7 | 72.6 | 0.3 |
| 1980 | 130.4 | 9.9 | 178.4 | 9.2 | 73.1 | 0.7 |
| 1981 | 143.6 | 10.1 | 195.1 | 9.4 | 73.6 | 0.7 |
| 1982 | 154.6 | 7.6 | 206.9 | 6.0 | 74.7 | 1.5 |
| Average annual percent change | ||||||
| Selected period | ||||||
| 1972-82 | --- | 8.5 | --- | 7.5 | --- | 0.9 |
For information on derivation of the National Nursing Home Input Price Index, see Fisher and Schendler (1980). For information on a related input price index used for Medicare reimbursement, see Health Care Financing Administration (1982).
The implicit price deflator for GNP is a widely used indicator of inflation for the overall economy.
SOURCE: Bureau of Data Management and Strategy, Health Care Financing Administration.
The growth of nursing home expenditures (excluding ICF-MR) from 1972 to 1982 is accounted for in terms of five factors (Table L17): growth in economy-wide inflation (GNP deflator), 55 percent; increases in nursing home days per capita18, 17 percent; increases in real expenses per day (intensity), 14 percent; and growth in total population (all ages) and nursing home input prices in excess of overall inflation (Table 14) each accounted for 7 percent.
For the period 1978-82, aggregate nursing home days (excluding ICF-MR) are estimated to increase at an average annual rate of between 2 and 3 percent, or at roughly the same rate of increase as in the population aged 75 and over.
Projections
The short-term outlook, 1982-84, is for total nursing home care expenditures to rise from $27 billion to $33 billion (Table 5), an average annual rate of increase of 9 percent. For the long-term outlook, expenditures are projected to rise to $44 billion in 1987 and $58 billion in 1990. Excluding ICF-MR, nursing home expenditures are expected to reach $52 billion in 1990, more than double the $24 billion in 1982. Higher prices paid for inputs to produce nursing home services and the aging of the population (Table 2) account for most of the projected increases—aged persons spend more than 30 times as much per capita for nursing home care than nonaged persons (Fisher, 1980).
Nursing home care is difficult to project since it is but one component of our long-term care system. Hospital care, nursing home care, home health services, domicilliary care, congregate housing, continuing-care retirement homes, and personal care services provided by relatives and friends are all part of the network of long-term care that can be viewed as a system of substitutes and complements (Figures 10 and 11). To the extent that increasing amounts of nursing home care are transferred to domicilliary care homes, continuing-care community retirement homes, and the like, nursing home care will not be included as health spending by HCFA. Changes in reimbursement regulations that have a direct impact on one area of the health care sector can significantly influence other areas. The Medicare PPS is expected to reduce hospital length-of-stay, and some portion of the discharged patients will be transferred to nursing homes. Fewer third-party funds available for nursing home care could increase demand for home health services, congregate housing, hospital services, and personal services of relatives and friends.
There is significant interest in developing DRG-type PPS's for nursing home care services (Office of Research and Demonstrations, 1983). This will accelerate the integration of clinical practice aspects of nursing home care with management and finance so that care can be provided on a more cost-effective basis. Added attention will be given to the measurement and review of quality and to proper placement by level of care (Bishop et al., 1980; Kane et al., 1981; Medical Care Licensing and Certification Division, 1980; Mitchell, 1978; Kurowski and Shaughnessy, 1983; Willemain, 1980).
Third parties (Medicare, Medicaid, Veterans' Administration, and so forth) financed approximately 56 percent of nursing home expenditures in 1982. This proportion may decrease in the 1980's because of a tightening of Federal, State, and local budgets. Thus, an increasing proportion of out-of-pocket expenses may have to be financed by Social Security and private pension payments, investment income, savings, assets, and contributions of friends and relatives (Olson et al., 1981; Scholen and Chen, 1980).
Other personal health care
Historical perspective
Other personal health care makes up less than 3 percent of the total health care systems cost (Table N), but the $7.6 billion spent in 1982 plays a critical role in providing health services for certain groups in the population. Approximately one-fifth of spending was for onsite industrial health services, the only privately financed expenditures in other personal health care. Such onsite facilities play an important role in occupational safety and health, preventive care, and emergency services (Roemer, 1981). Government spending accounted for $6 billion and included, among other services, 1) care provided in Federal units other than hospitals, such as freestanding outpatient facilities; 2) school health services; 3) family-planning services; 4) ambulance services; and 5) health-care spending for which no service type can be identified.
Expenditures for other personal health care increased at an average annual rate of 11 percent during the last decade. Price increases, as approximated by the CPI for medical care (in the absence of a more appropriate price indicator), accounted for nearly 86 percent of the increase (Table 8). Population growth accounted for 9 percent of the increase, and growth in real services per capita accounted for the remaining 5 percent of the growth.
Federal programs other than Medicare and Medicaid, such as programs of the Veterans' Administration and the Department of Defense, financed one-third of the spending in 1982. Medicaid and Medicare paid for 20 and 11 percent of outlays, respectively.
Projections
Given the heterogeneous nature of other personal health care, including major categories of spending for which no service type can be identified, it is difficult to project spending patterns for the 1980's. In addition, this category of spending has exhibited a higher degree of volatility in growth than any other category of total health care cost (Freeland and Schendler, 1983). This volatility, in part, reflects evolving data collection and categorization processes that alter which expenditures are allocated to other personal health care. Given these caveats, projected spending will reach roughly $9 billion by 1984, $11 billion by 1987, and $14 billion by 1990.
Government is expected to finance an increasing share of other health services in the 1980's, continuing a trend from the 1970's. However, the growth in the Government's share is projected to decelerate in the 1980's relative to the previous decade. At this time, it is not clear what role corporations and business coalitions will play in altering the relative importance of industrial onsite health services for their employees, compared with facilities outside the plant. Onsite care may potentially diminish use of sick leave, decrease workmen's compensation claims, and reduce employer-paid health insurance premiums. However, the costs of providing quality onsite care will need to be weighed against the potential benefits.
Program administration and net cost of insurance
Historical perspective
Expenses for program administration and net cost of insurance include three components: 1) prepayment costs (including operating expenses) of private health insurance organizations (Blue Cross and Blue Shield, commercial companies, and independent plans); 2) administrative expenses of Government-financed health programs; and 3) nonpersonal health expenditures of private voluntary health organizations for lobbying, fund-raising, and so forth.
For private health insurance organizations, prepayment cost reflects the difference between the earned premiums (subscription income) and incurred benefit payments (claims). It represents the net cost to the consumer and is retained by the insurance organizations for additions to reserves, profits, and operating expenses. The operating-expenses component is a function of a number of factors, including these: marketing costs, State premium taxes, the incidence of claims per enrollee, the quantity and quality of effort used to monitor and control claims costs, the complexity of the benefits package, productivity improvements associated with automation, and wage growth for employees in the industry. The operating expenses component has been a fairly stable proportion of premium income (Carroll and Arnett, 1981). The additions to reserves and profits components, on the other hand, are volatile and cyclical. It is difficult to project these two components since both the length and depth of the cycle are variable.
Program administration and net cost of insurance expenses have risen from $4.7 billion in 1972 to $12.7 billion in 1982, an average annual rate of growth of almost 11 percent (Tables 5 and 6). Because of the cyclical nature of the net cost of insurance (caused by changes in reserves and profits components of prepayment costs), caution must be exercised in interpreting average annual growth rates (Table 6). Use of slightly different time periods can result in significantly different annual rates of growth.
Administrative expenses of the Medicare program increased from $0.5 billion in 1972 to $1.3 billion in 1982, an average annual rate of increase of between 10 and 11 percent (Table A). Increases in enrollment (including the disabled and end-stage renal dialysis beneficiaries, in 1974), claims per enrollee, and wages for employees of intermediaries and carriers accounted for most of the rise in Medicare administrative expenses.
Federal Medicaid administrative expenses rose from $200 million in 1972 to $1.0 billion in 1982 (Table C). Administrative expenses rose from 4.3 percent of benefits in 1972 to 6 percent in 1982.
Projections
There will be pressures in the early to mid-1980's to raise premiums relative to benefits so that net underwriting gains can improve. When operating expenses are added to benefits and this sum is divided by premiums, a combined ratio of approximately 104 is estimated for 1982. This implies negative net underwriting gains since, for each $100 of premium income, there is approximately $104 paid out in benefits and operating expenses. Of course, interest earned on reserves held to play claims offsets some of this net underwriting loss.
As interest rates decline in the early 1980's, it will put additional pressures to raise premiums relative to benefits. The lower interest rates imply there will be less investment income to offset underwriting losses. In other words, the extent of cash-flow underwriting, in which premium rates are set at levels that imply net underwriting losses, is likely to diminish in the early 1980's. With lower economy-wide inflation and interest rates and, thus, lower yielding financial instruments, it will be more difficult to recoup net underwriting losses.
Program administration and net cost of insurance expenses are projected to reach $16 billion in 1984, $23 billion in 1987, and $27 billion in 1990 (Table 5).
Benefits and premiums (to a lesser degree) exhibit relatively volatile growth over time, relating to fluctuations in medical care prices and use, changes in enrollment and coverage, and regulatory premium rate review procedures. Benefit growth is more volatile than premium growth (Carroll and Arnett, 1981; Freeland and Schendler, 1983). This is so because insurance carriers absorb a portion of unanticipated high benefit increases in the form of reduced profits or reserves. Likewise, when benefit increases are lower than expected, profits or reserves are enhanced.19
Thus, aggregate premium growth is more steady than aggregate benefit growth, and net cost of insurance shows substantial fluctuations; from its statistical analyses, HCFA concludes that it is not possible to accurately forecast the timing of fluctuations in the net cost of insurance (earned premiums minus incurred benefits), given the complexity of the underlying behavioral processes. The premium/benefit relationships incorporated in this projection reflect an assumption that over the period 1982-90, as a whole, the Blue Cross and Blue Shield Plans, commercial insurance companies, and independent plans will each be in approximate equilibrium and financially viable. In any one year, there will not be equilibrium. The timing of premium increases relative to benefit increases should be interpreted as a working assumption, not as a forecast.
Competition in the private health insurance industry is expected to intensify in the 1980's along three dimensions. First, corporate chief executive officers and employee-benefit specialists are becoming more knowledgeable and aggressive in their quest for cost-effective benefit plans. They will be asking penetrating questions and will switch to more attractively priced plans or self-insure if their needs are not met. Second, alternative delivery systems, such as PPO's and HMO's will be enlarging their market share, and the private health insurance industry will be actively involved. Third, employers and other payors of care are going to expect carriers to use more sophisticated techniques to control the rise in benefit claims costs. Information support systems that are case-mix based are expected to become more prevalent. The integration of concepts of clinical medicine with claims management and review will become increasingly important. The enhanced claims control effort is expected to put upward pressure on operating expenses, as will increased advertising and promotion. More efficient computer routines to process and analyze claims will put downward pressure on operating expenses. A major objective of improved claims control is to reduce benefit payments by substantially more than the increased administrative cost of monitoring and controlling claims payments. Competitive pressures in the insurance industry will work toward this end.
Government public health activities
Historical perspective
Public health activities are provided to improve and protect the well-being and health of the entire Nation. Preventive community health services are the focal point, and emphasis is placed on the interaction of social, cultural, economic, political, and biological dimensions of community health problems (Hanlon and Picket, 1984). In addition, groups of people who are at risk for particular diseases and groups of people with limited access to care in the private medical sector are also the focal point of many public health activities.
Federal health activities include health planning, disease prevention and control, consumer safety, and occupational safety and health. National priorities are set by the Federal Government, and financial support by means of block grants and intergovernmental transfers is provided to the 55 State and territorial health agencies and to the over 3,000 local health departments. These local health departments provide direct community health services such as public health nursing, home health care, immunization, venereal disease control, chronic disease screening, consumer protection, and the like.
Expenditures for public health activities have risen from $2.0 billion in 1972 to $8.6 billion in 1982 (Table 5). This reflects an average annual rate of growth of nearly 16 percent. Economy-wide inflation accounted for about half of this increase (Table 8). A weighted average of wages and salaries for certain Federal, State, and local government employees increased at an average annual rate of 7.4 percent, just under the 7.5 percent annual rate for economy-wide inflation. Thus, the increase in the cost of producing public health services, assuming the wage variables are a reasonable approximation, was about the same as economy-wide inflation. Growth in population accounted for about 7 percent of spending increases, and growth in real services per capita accounted for the remaining 44 percent of the increased spending.
State and local spending increased much faster than Federal spending from 1972-82. The State and local share rose from 52 percent in 1972 to 84 percent in 1982.
Projections
The short-term outlook is for expenditures for public health activities to rise to $10.4 billion in 1984. This is a marked slowdown in growth due to restrictive Government fiscal positions. Expenditures are projected to reach $14 billion in 1987 and $18 billion in 1990.
The tight revenue conditions at all levels of Government, combined with wage-rate increases for public health employees, are projected to squeeze growth in real service output in the 1982-90 period relative to the 1972-82 period. Historical growth in public health spending has been characterized by volatility and spurts (Freeland and Schendler, 1983). This, in part, reflects the complex inter-Governmental relationships that link our public health system (Kaufman, 1966; Tilson, 1981). This volatility is likely to continue in the 1980's as the public health sector and the private health sector define and redefine their unique and, in some areas, converging roles (Blendon, 1981). The expansion of public and private insurance for home health services may result in the private health sector enlarging its role relative to the public sector in this segment. On the other hand, the possible resurgence of some communicable diseases and an increased awareness of the importance of social and behavioral sciences in preventing and dealing with major health problems (such as chronic diseases, mental illness, suicide, accidents, drug and alcohol abuse, homocide, and sexually transmitted diseases)20 may augur more resources allocated to public health activities than would otherwise be the case.
Research
Historical perspective
Biomedical research into the diagnosis, treatment, and prevention of disease has significance well beyond its small proportion of National health spending21. Biomedical research has resulted in extraordinary accomplishments in the past (Fuchs, 1983; Mushkin, 1979) and promises incalculable benefits for the future. A classic example of such exceptional achievement was the development of polio vaccine (a preventive technological breakthrough) to replace the iron lung (a half-way technology). The life-enhancing and cost-reducing effect of this research is unmistakable.
For the 1965-82 period, expenditures for research increased at the slowest rate of the 12 HCFA categories of expenditures, resulting in the proportion of National health expenditures spent on research declining from 3.6 percent in 1965 to 1.8 percent in 1982 (Figure 15).
Figure 15. Expenditures for medical research as percent of national health expenditures: 1965-821.
1Medical research expenditures of drug companies and manufacturers of medical supplies and equipment are excluded from the Health Care Financing Administration category of “medical research” but are included in the expenditure category in which the product falls.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy, Office of Financial and Actuarial Analysis.
From 1972 to 1982, spending for research increased at an average annual rate of less than 10 percent, significantly slower than the 13 percent rate for total health care spending. Economy-wide inflation accounted for 80 percent of this increase in spending for research from 1972 to 1982 (Table 8).
The biomedical research and development price index (Copeland, 1982) increased marginally faster than economy-wide inflation and accounted for only 3 percent of the growth in spending. Population growth accounted for nearly 11 percent and increases in real spending per capita accounted for the remaining 7 percent of the growth in total spending (Table 8).
The Federal Government increased its share of research funding from 80 percent in 1972 to 85 percent in 1982. State and local governments financed 9 percent, and private organizations financed 6 percent of total spending in 1982.
Projections
Short-term expenditures for biomedical research and research on the delivery of health services are projected to increase from $5.9 billion in 1982 to $6.5 billion in 1984, $8 billion in 1987, and $10 billion in 1990.
The implementation of the Medicare PPS will result in more accurate financial and diagnostic information, which should improve research data bases relating to the practice patterns of clinical medicine and the delivery of hospital care. Diagnosis-specific research is expected to increase in relative importance, and this could lead to improvements in the diagnosis, treatment, and prevention of illness using more cost-effective patterns of care.
There is likely to be greater emphasis in the 1980's on using research findings as a means for decreasing the rate of increase in health spending. Many technologies are cost-increasing rather than cost-decreasing (Feldstein, 1981), and future research is likely to focus more on this issue out of economic necessity.
There may be increased emphasis on diagnosing, treating, and preventing chronic illness, impairments, and disabilities with relatively less emphasis on mortality. In other words, research relating to prevention of chronic illness and to quality of life for persons with chronic illness and disability (rather than length of life, per se) may take on increased relative importance.
Construction of medical facilities
Historical perspective
Expenditures for construction of medical facilities have doubled from 1972 to 1982 (Table 5), reflecting an average annual rate of growth of 7 percent. However, the price of construction materials, as measured by the Department of Commerce Composite Construction Cost Index, rose at an average annual rate of 9 percent, implying that real expenditures declined at an average annual rate of 2 percent.
These data and several studies suggest there has been an erosion of the health care sector's capital position in the 1970's (Bradford et al., 1982; ICF Inc., 1983; Ting and Valiante, 1982). Technological improvements and high inflation have exacerbated this erosion and obsolescence of capital.
There has been relatively fast growth in beds compared with increases in real spending per bed for renovation and modernization, especially for the 1971-79 period. According to the American Hospital Association Panel Survey, community hospital beds increased at an average annual rate of almost 2 percent from 1971 to 1979. Real construction spending during this period declined from $6.6 billion in 1971 to $4.5 billion in 1979, an average annual rate of decrease of 5 percent. Beginning in 1980, real construction expenditures started to rise, and in 1981 and 1982, real spending rose 9 percent and 8 percent, respectively, despite high interest rates and tight credit conditions.
Projections
The short-term projection is for current dollar construction expenditures to rise from $8 billion in 1982 to $10 billion in 1984. Data available, as of mid-1983, on authorized hospital construction and on the value of construction contracts are consistent with this projection (Bureau of Industrial Economics, July/August 1983). Expenditures are projected to reach $14 billion in 1987 and $17 billion in 1990. The price of goods and services used in construction of medical facilities is expected to rise at a slower rate in the 1980's because of a moderating of overall inflation, but real growth is expected to rise faster than in the 1970's.
During the 1950's and 1960's, Hill-Burton funds financed the building of a substantial number of beds, and in the 1980's and 1990's, much of this equipment and plant may require replacement or modernization. Several studies indicate that there will be great pressures in the last two decades of this century to modernize, renovate, replace, and build new hospital plant and equipment (Bradford et al., 1982; Phillips, 1982; Ting and Valiante, 1982). Shifts in geographic and age distributions of the population will also increase demand for new beds and facilities. Because of these pressures, future real growth in construction may not be an extrapolation of real growth in the 1970's.
Financing will derive from internal sources such as net income and depreciation allowances and from external sources including philanthropic gifts, government grants, and debt. Private sources of funding are expected to pay an increasing share of medical facility construction costs in the 1980's (Table 7).
The projected spending for construction in the 1982-90 period (Table 5) is roughly in line with the middle case of hospital capital requirements developed by ICF Inc. (1983). Higher and lower capital requirements were also developed by ICF Incorporated, using alternative assumptions for projected utilization, HMO enrollment, planning guidelines, length of renovation cycle, construction costs, inflation, and technology changes. Capital requirements were sensitive to alternative assumptions—the high case was more than double the middle case, and the low case was less than half of the middle case.
The Medicare PPS excludes capital-related costs from the prospective payment rates, and these costs continue to be reimbursed on a retrospective, reasonable cost basis. However, the PPS regulations require the Secretary of HHS to study the feasibility of adding capital-related costs to the prospective rates and to report the findings to Congress by October 1984. If, by October 1, 1986, capital-related costs are still excluded from the prospective rates, Medicare will only pay for new projects in which the State has a Section 1122 program that has approved the hospital's costs. When information becomes available on the findings of the congressionally-mandated study on adding capital-related costs to the prospective rates, it will be possible to develop some scenarios on construction spending for the remainder of the 1980's. In the private sector, Anderson and Ginsburg (1983) and Cohodes and Kinkead (1982) have discussed options for prospective payment for hospital capital outlays. These and other options will be intensively discussed in the 1980's.
The ability to finance and carry out new construction, renovation, and modernization is vital to the competitive position and financial viability of medical care institutions. This is especially true in an era of increasing competition and shifts in our delivery system. It will be important for institutions to develop viable strategies to make capital-related decisions in the 1980's that take into account financial and regulatory constraints, as well as market opportunities. The intensification of competition in the 1980's will put a premium on medical facility location, cost of service, and product/service differentiation—all capital-related attributes.
Summary
Projections of National health expenditures by type of expenditure and source of finance have been presented for 1984, 1987, and 1990. It is assumed that historical trends and relationships, modified for the effects of current-law regulations such as the Medicare PPS, will continue. It is also assumed that neither an all-payor PPS nor National health insurance will be in effect. (These are assumptions of the current-law projection, not predictions.) These baseline projections incorporate HCFA's projections of Medicare and Medicaid outlays, the Bureau of Health Professions' projections of active physicians and dentists, and the 1983 Board of Trustees' (Federal Old-Age and Survivors Insurance and Disability Insurance Trust Funds) projections of the GNP and overall inflation.
Health-spending increases are projected to decelerate, primarily because of lower projections of economy-wide inflation, implementation of the Medicare PPS, and the integration of clinical practice patterns with improved management practices, but spending is expected to continue to rise substantially faster than GNP. Significant implications for the economy arise as the health care sector continues to absorb larger percentages of the GNP. The major implication is that, as more labor and capital are drawn into the health care sector, relatively fewer resources are available for producing goods and services in other sectors.
There seem to be few demand or supply incentives to significantly retard the growth of health expenditures under current institutional arrangements except for the following: competitive forces inducing improved management (including more cost-effective clinical practice patterns), fragmented efforts by States to moderate hospital cost increases, and the Medicare PPS for inpatient services. As the population ages and as new health technologies are adopted, health costs increase. As health costs increase, so do the risks of financial burden to consumers with inadequate health insurance coverage. As the risks increase, the demand for public programs and private health insurance also rises. Moreover, tax subsidies for health insurance premiums add to this increased demand by encouraging the purchase of more comprehensive insurance. As the coinsurance rate (proportion paid out-of-pocket by consumers) declines with the additional insurance, both consumers and providers increasingly tend to treat health care services as a free good at the time of purchase. The ensuing increased demand for medical care interacts with our predominant fee-for-service and retrospective cost-based reimbursement systems to further increase costs; that is, more services and more costly services reward providers with additional revenues from third-party payors. The reimbursement policy provides an incentive for providers to adopt product-innovative technologies, which increase costs. There is relatively less incentive to adopt process-innovative technologies, which are associated with increased productivity and decreased costs. The Medicare PPS for inpatient services tends to modify these inflationary forces for its segment of the market.
Our current, primary institutional arrangement of third-party payments, with fee-for-service and retrospective cost-based reimbursement, evolved out of an interaction between providers, third-party payors, and consumers, based on their economic, social, and political needs and demands at the time the current health care financing system was begun, in the 1950's and 1960's. The cost-increasing incentives inherent in this system became increasingly evident in the 1970's and early 1980's, and questions are being raised as to its long-run desirability and viability.
What is good health? What is good quality of care? What is cost-effective care? What can we (individual households, firms, Government) afford to pay, given other demands? These questions will increasingly surface in the 1980's as we evolve toward a payment system that better balances the legitimate needs of patients, providers, taxpayers, and other buyers of care, such as corporations. Nevertheless, until alternative institutional arrangements are devised (that better meet the conflicting needs and demands placed on the current system), the affected parties may resist significant changes to the current system.
There is uncertainty as to the future ability to finance growth in health expenditures as reflected in GNP growth, and there is uncertainty as to the proportion of the GNP that will be allocated to the health care sector. The current-law projection of National health expenditures presented in this study is a baseline from which alternative scenarios can be constructed to meet the unique needs of individual managers, strategic planners, policy makers, and the like. Making a baseline projection does not imply that National health expenditures can be forecasted with precision, and the inherent difficulties in making short-term forecasts and long-term projections should not be underestimated. All that can be stated with assurance is that 1) as health expenditures consume an ever larger proportion of the GNP, there will be ever more intensive efforts by the financers of such care to slow the growth, and 2) as new effective and expensive technologies become available to diagnose and treat conditions, there will be pressures by patients, their families, and the providers to use such technologies. Assuming that the current incentive mechanisms and constraints affecting the demand for and supply of medical care are not significantly modified, and that the projected growth in inflation and GNP is accurate, the projections of health expenditures presented in this study are a reasonable approximation of what can be expected for the next decade.
Acknowledgments
The authors particularly want to thank George I. Kowalczyk, Director of the Division of National Cost Estimates, and Helen Lazenby, Division of National Cost Estimates for their extensive suggestions. Helpful comments and suggestions on all or selected portions of the report were made by Charles Fisher, Director of the Division of Information Analysis; Roland King, Fellow of the Society of Actuaries and Director of the Office of Financial and Acturial Analysis; and Gordon R. Trapnell, Fellow of the Society of Actuaries, Actuarial Research Corporation, Falls Church, Virginia. Significant contributions to the article were made by Ross H. Arnett, III, Robert M. Gibson, Katharine R. Levit, Brenda Maple, Patricia McDonnell, Deborah B. Miller, and Daniel R. Waldo, all of the Division of National Cost Estimates. Philip Buri and Jeffrey Coombs of Data Resources, Inc., provided technical support. The authors are grateful to Carol Pearson, Division of Medicare Cost Estimates, for outstanding secretarial assistance.
Footnotes
Reprint requests: Mark S. Freeland, Room 2-C-7 Meadows East Building, 6325 Security Boulevard, Baltimore, MD. 21207.
A catchment area is the geographic area serviced by a health care facility.
An explanation of methodology used to prepare this article is available from the authors.
The implicit price deflator for the gross national product (GNP) is a widely used indicator of inflation that takes into consideration not only changes in price of the various components of the GNP (consumer goods and services, such as food, health care, and the like, plus Government services, investment, and net exports), but also the changing mix of the economy's output. The GNP deflator measures price changes of a wider group of goods than does the Consumer Price Index (CPI), which excludes Government services, investment, and net exports.
Premiums (and subscription income) for private health insurance are listed at the intersection of the column for health insurance and the row for health services and supplies in Table 7. Total benefit payments are shown at the intersection of the column for health insurance and the row for personal health care.
Unfortunately, productivity data could not be located for the same time period as the wage and price data. The period 1973-81 was one of very low productivity growth by historical standards. For the period 1947-73, output per hour of all persons in the nonfarm business sector increased at an average annual rate of 2.5 percent (Council of Economic Advisors, 1983). One indicator of rates of change in productivity over one period of time is provided in Table M. It says nothing about the productivity levels of one industry compared with another, nor does it say anything about potential for improving future productivity levels for one industry compared with another. For example, because of years of retrospective cost-based and fee-for-service reimbursement, the Federal Government may have provided incentives to decrease productivity increases relative to most other industries. Efficiency, not effectiveness, is referred to in Table M. Efficiency measures output per unit of input and gets at this question: “Could the same output have been accomplished with fewer resources or with a different mix of resources?” Effectiveness compares the organization's objectives with its actual accomplishments. Effectiveness refers to this question: “Are we doing the right thing?” (Suver and Neumann, 1981). The Medicare PPS provides incentives to improve both efficiency and effectiveness. For example, altering clinical practice patterns to be more effective is an important objective of PPS.
If the percent markup of unit prices over unit costs is constant over time, the growth in both prices and unit costs will be the same. The difficulty in measuring output in the medical care services sector (Reder, 1969) has hampered efforts to measure price changes for a fixed unit of service over time. Some factors, such as the increasing sophistication of care that cannot be separated from a fixed unit of service over time, may result in medical care services price statistics being biased upward over time. Other factors, such as separating services and procedures into finer components and billing individually for each service or procedure (that is, unbundling), may result in medical care services price statistics being biased downward over time (Ginsburg, 1978; Showstack et al., 1979; and Sobaski et al., 1975).
High productivity increases can be associated with price increases that are substantially below economy-wide inflation, as was the case for the drug industry for the period 1965-74. This is detailed in the Drugs and medical sundries section of this article.
These quarterly percent changes represent contiguous quarters, not percent changes, from the same quarter a year ago.
It is important to note that the extent to which patients remain in hospitals beyond the optimal time for discharge, because placement in a nursing home is not available, cannot be discerned from Figure 10.
Hospital care includes some ambulatory care in providing outpatient services.
This assumes that the payment rate for the specific DRG is in excess of costs for this DRG at the particular hospital.
Different data, collection methods are used for the total employment and the non-Federal office-based physician series.
If length-of-stay is reduced or ambulatory surgery, rather than inpatient surgery, is performed, some services that were formerly provided on an inpatient basis can be provided in an office setting.
Note, however, that different data collection methods are used for these two data series.
Medical sundries, such as bandages and iodine, are classified as medical nondurables (medical durables such as crutches and bedpans are included in the HCFA expenditure category of eyeglasses and appliances). Note that spending for drugs dispensed or purchased by hospitals, physicians, dentists, and nursing homes are excluded from the HCFA category of drugs and medical sundries. Such spending for drugs is included in the respective HCFA categories of hospital care, physicians' services, dentists' services, and nursing home care.
Facilities and beds that are dually certified under Medicaid as SNF and ICF are reported separately under both classifications. Double counting results if dually certified facilities and beds are added.
Reliable annual data do not exist for aggregate nursing home days, beds, charges per day, and so forth. There are several data sources relating to the nursing home industry that are available on a current or periodic basis. These data sources are synthesized by HCFA to develop a consistent time-series of the nursing home industry. It is with these caveats in mind that one must interpret the factors accounting for growth in the nursing home industry shown in Table L.
It must be emphasized that this is growth in nursing home days relative to total population (all ages).
This may be the case in 1983, given the substantial deceleration in hospital cost increases.
public health has a long tradition of integration of social and behavioral sciences with biological sciences to deal more effectively with community health problems.
Expenditures for research by medical supply and drug companies are excluded from the HCFA medical research category because such spending is included in the expenditure category in which the product falls.
References
- Alhadeff DA. Microeconomics and Human Behavior: Toward a New Synthesis of Economics and Psychology. Berkeley, California: University of California Press; 1982. [Google Scholar]
- Allard MA, Toff G. Intergovernmental Health Policy Project. Washington, D.C.: George Washington University; Aug. 1980. Current and Future Development of Intermediate Care Facilities for the Mentally Retarded: A Survey of State Officials. [Google Scholar]
- Altman SH, Blendon R, editors. Medical Technology: The Culprit Behind Health Care Costs? Proceedings of the 1977 Sun Valley forum on national health; 1979. pp. 79–3216. DHEW Pub. No. (PHS) [Google Scholar]
- American Dental Association, Bureau of Economic and Behavioral Research. Changes in the prevalence of dental disease. Journal of the American Dental Association. 1982 Jul;105(1):75–79. [PubMed] [Google Scholar]
- American Dental Association, Special Committee on the Future of Dentistry. Strategic Plan, Report of the American Dental Association's Special Committee on the Future of Dentistry. Chicago: American Dental Association; Jul, 1983. [Google Scholar]
- American Druggist. Giant technological strides loom in RX drug industry. American Druggist. 1983 Jun;70 [Google Scholar]
- American Hospital Association. Hospital Statistics. Chicago: 1973, 1983. [Google Scholar]
- American Hospital Association. Hospital indicators. Hospitals. 1982 [Google Scholar]
- American Medical Association. Profile of Medical Practice. Monroe, Wisc.: Center for Health Services Research and Development, American Medical Association; 1980, 1981. [Google Scholar]
- American Medical Association. SMS Report. Monroe, Wisc.: Center for Health Policy Research, American Medical Association; Jul, 1983. [Google Scholar]
- American Medical News. MD-hospital cooperation essental under DRGs. American Medical News. 1983 Oct.4 [Google Scholar]
- Anderson G, Ginsburg P. Prospective capital payments to hospitals. Health Affairs. 1983 Fall;2(3) doi: 10.1377/hlthaff.2.3.52. [DOI] [PubMed] [Google Scholar]
- Bandy WC. 1983 US Industrial Outlook for 250 Industries With Projections for 1987. Bureau of Industrial Economics, U.S. Department of Commerce; Washington: Jan. 1983. Medical and dental instruments and supplies. [Google Scholar]
- Banta HD, Russell L. Policies toward medical technology, an international review. International Journal of Health Services. 1981;2(4):631–656. doi: 10.2190/CWE9-ETJC-1XXR-Y3RP. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Gerson S. Deinstitutionalization and mental health services. Scientific American. 1978 Feb.238:45–53. doi: 10.1038/scientificamerican0278-46. [DOI] [PubMed] [Google Scholar]
- Bell DR. Dental and vision care benefits in health insurance plans. Monthly Labor Review. 1980 Jun;103(6):22–26. [PubMed] [Google Scholar]
- Benham L. The effect of advertising on the price of eyeglasses. Journal of Law and Economics. 1972 Oct.:337–352. [Google Scholar]
- Birnbaum H, Lee AJ, Bishop CE, et al. Public Pricing of Nursing Home Care. Cambridge, Mass.: Abt Books; 1982. [Google Scholar]
- Bishop CE, Plough A, Willemain T. Health Care Financing Review. Washington: U.S. Government Printing Office; Dec. 1980. Nursing home levels of care, problems and alternatives. HCFA Pub. No. 03068. Office of Research Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ. The prospects for state and local governments playing a broader role in health care in the 1980s. American Journal of Public Health. 1981 Jan.71(1):9–14. doi: 10.2105/ajph.71.1_suppl.9. Supplement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom M. The DO's growing pains. Medical World News. 1980 Oct. [PubMed] [Google Scholar]
- Blostin A, Marclay W. HMOs and other health plans, coverage and employee premiums. Monthly Labor Review. 1983 Jun;106(6):28–33. [PubMed] [Google Scholar]
- Blumberg MS. Provider price changes for improved health care use. In: Chacko GK, editor. Health Handbook. Amsterdam, Holland: North Holland Press; 1979. [Google Scholar]
- Board of Trustees. 1983 Annual Report, Federal Old-Age and Survivors Insurance and Disability insurance Trust Fund. Washington: U.S. Government Printing Office; Jun 27, 1983. House Document No. 98-74. [Google Scholar]
- Board of Trustees. 1983 Annual Report, Federal Hospital Insurance Trust Fund. Washington: U.S. Government Printing Office; Jun 28, 1983. House Document No. 98-75. [Google Scholar]
- Board of Trustees. 1983 Annual Report, Federal Supplementary Medical Insurance Trust Fund. Washington: U.S. Government Printing Office; Jun 28, 1983. House Document No. 98-76. [Google Scholar]
- Bradford C, Caldwell G, Goldsmith J. The hospital capital crisis: issues for trustees. Harvard Business Review. 1982 Sep-Oct; [PubMed] [Google Scholar]
- Brand H. Productivity in the pharmaceutical industry. Monthly Labor Review. 1974 Mar;97(3) [Google Scholar]
- Bureau of the Census. Statistical Abstract of the United States 1984. 104th. Washington: U.S. Government Printing Office; 1983. U.S. Department of Commerce. [Google Scholar]
- Bureau of Data Management and Strategy. Health Care Spending Bulletin. 4. Vol. 83. Health Care Financing Administration; Mar. 1983. Health facilities participating in HCFA programs, 1983. [Google Scholar]
- Bureau of Economic Analysis. The National Income and Product Accounts of the United States, 1929-76s Statistical Tables. Washington: U.S. Government Printing Office; Sept. 1981. U.S. Department of Commerce. [Google Scholar]
- Bureau of Economic Analysis. Survey of Current Business. 7. Vol. 63. Washington: U.S. Government Printing Office; Jul, 1983. U.S. Department of Commerce. [Google Scholar]
- Bureau of Industrial Economics. 1983 US Industrial Outlook for 250 Industries with Projections for 1987. U.S. Department of Commerce; Washington: Jan. 1983. [Google Scholar]
- Bureau of Industrial Economics. Construction Review. 4. Vol. 29. Washington: U.S. Government Printing Office; Jul-Aug. 1983. U.S. Department of Commerce. [Google Scholar]
- Bureau of Labor Statistics. BLS Bulletin. Washington: U.S. Government Printing Office; Aug. 1983. Benefits in medium and large firms, 1982. No. 2176. US Department of Labor. [Google Scholar]
- Bureau of Labor Statistics. Employment and Earnings. U.S. Department of Labor; Washington: [Google Scholar]
- Bureau of Labor Statistics. USDL News. U.S. Department of Labor; Washington: Jul 25, 1983. Productivity declines in 1982 reported for most industries measured. No. 83-314. [Google Scholar]
- Bureau of Labor Statistics. BLS Bulletin 2155. Washington: U.S. Department of Labor; Dec. 1982. Productivity measures for selected industries. [Google Scholar]
- Cain C. Self-insurance: soft property/casualty rates slow self-funding growth—but everybody is self-funding health insurance benefits. Business Insurance. 1983 Jan. [Google Scholar]
- Cameron J, Kirkland RI. Five burdens that make a rich U.S. feel poor. Fortune. 1980 Jan.:72–79. [Google Scholar]
- Carroll MS, Arnett RH. Health Care Financing Review. Washington: U.S. Government Printing Office; Sept. 1981. Private health insurance plans in 1978 and 1979: Coverage, enrollment, and financial experience. HCFA Pub. No. 03123. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Cassack D. Forecast '83 and the year in review. Health Industry Today. 1983 Jan.46(1):18–38. [PubMed] [Google Scholar]
- Chiswick BR. The demand for nursing home care, an analysis of the substitution between institutional and noninstitutional care. Journal of Human Resources. 1976 Summer; [Google Scholar]
- Cocks DL. Economic and competitive aspects of the pharmaceutical industry. In: Smith MC, editor. Principles of Pharmaceutical Marketing. 3rd. Philadelphia: Lea and Febiger; 1983. [Google Scholar]
- Cohodes DR, Kinkead RM. Princeton; New Jersey: Aug. 1982. Hospital Capital Formation in the 1980s: Is there a crisis? Prepared for Robert Wood Johnson Foundation. [Google Scholar]
- Cole LA. A new look in american dentistry. The New York Times Magazine. 1982 Apr 5;:86–94. [Google Scholar]
- Congressional Budget Office. Containing Medical Care Costs Through Market Forces. Congress of the United States; May, 1982. [Google Scholar]
- Congressional Budget Office. Tax Subsidies for Medical Care: Current Policies and Possible Alternatives. Congress of the United States; Jan. 1980. Background Paper. [Google Scholar]
- Copeland WC, Iverson IA. Medicaid Funding for the Continuum of Care for MD/DD Persons. Hubert H. Humphrey Institute of Public Affairs, University of Minnesota; Mar 11, 1980. [Google Scholar]
- Copeland WL. Program Analysis Note. No. 4. Office of Program Planning and Evaluation, Office of the Director, National Institutes of Health; Washington: Jan. 1982. Measuring inflation of biomedical research costs. [Google Scholar]
- Cotterill PG. The physician-induced demand and target-income models: a survey of the issues. In: Gaffney JC, editor. Profile of Medical Practice, 1978. Revised edition. American Medical Association; Monroe, Wisc.: 1979. [PubMed] [Google Scholar]
- Council of Economic Advisors. Economic Report of the President. 1983 [Google Scholar]
- Cromwell J, Kanak J. Health Care Financing Review. US Government Printing Office; Washington: Dec, 1982. The effects of prospective reimbursement programs on hospital adoption and service sharing. HCFA Pub. No. 03149 Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Health Care Costs. Washington, D.C.: Data Resources, Inc. monthly. [Google Scholar]
- Davis C. Joint Economic Committee Print No 99-5790. Washington: U.S. Government Printing Office; 1983. The economics of the Soviet health system. In Soviet economy in the 1980s: Problems and Prospects, Part 2; pp. 228–264. Congress of the United States. [Google Scholar]
- Davis K, Russell LB. The substitution of hospital outpatient care for inpatient care. Review of Economics and Statistics. 1972;54:109–120. [Google Scholar]
- Delbanco TL, Meyers KC, Segal EA. Paying the physician's fee: Blue Shield and the reasonable charge. New England Journal of Medicine. 1979;301:1314–1320. doi: 10.1056/NEJM197912133012404. [DOI] [PubMed] [Google Scholar]
- Denton FT, Spencer BG. Health care costs when the population changes. The Canadian Journal of Economics. 1975 Feb.:34–48. [Google Scholar]
- Division of Health Professions Analysis, Bureau of Health Professions. Third Report to the President and Congress on the Status of Health Professions Personnel. Health Resources Administration, U.S. Department of Health and Human Services; Jan. 1982. [Google Scholar]
- Dobson A. Health Care Financing Review. Washington: U.S. Government Printing Office; Mar. 1981. Health care in China after Mao. HCFA Pub. No. 03090. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Dresch SP, Garvey NA, Waldenberg A. The Aged: Population Composition and Health Care Utilization, 1979 to 2015. New Haven, Connecticut: Institute for Demographic and Economic Studies; Feb. 1981. [Google Scholar]
- Dunlop B. Understanding the Growth in Nursing Home Care 1964-1974. Washington, D.C.: The Urban Institute; Apr, 1978. [Google Scholar]
- Dutton D. Patterns of ambulatory health care in five different delivery systems. Medical Care. 1979 Mar;17(3):221–243. doi: 10.1097/00005650-197903000-00001. [DOI] [PubMed] [Google Scholar]
- Employee Benefit Plan Review: Dental insurance is fastest growing benefit. Employee Benefit Plan Review. 1981 Nov.88 [Google Scholar]
- Enthoven AC. Health Plan: The Only Practical Solution to the Soaring Cost of Medical Care. Reading, Mass.: Addison-Wesley; 1980. [Google Scholar]
- Feldman R, Begun JW. The effects of advertising, lessons from optometry. Journal of Human Resources. 1978:247–262. Supplement. [PubMed] [Google Scholar]
- Feldstein MS. An econometric model of the Medicare system. Quarterly Journal of Economics. 1970 May; [Google Scholar]
- Feldstein MS. The Rising Cost of Hospital Care. Washington, D.C.: Information Resources Press; 1971. [Google Scholar]
- Feldstein MS. Hospital Costs and Health Insurance. Cambridge, Mass.: Harvard University Press; 1981. [Google Scholar]
- Feldstein P. A review of productivity in dentistry. In: Rafferty J, editor. Health Manpower and Productivity. Lexington, Mass.: D.C. Health; 1974. [Google Scholar]
- Feldstein PJ. Health Care Economics. New York: John Wiley & Sons; 1979. [Google Scholar]
- Feshbach M. Joint Economic Committee Print No 99-5790. Washington: U.S. Government Printing Office; 1983. Issues in Soviet health problems. In Soviet economy in the 1980s: Problems and Prospects, Part 2; pp. 203–227. Congress of the United States. [Google Scholar]
- Fetter RB. Ambulatory Patient Related Groups. New Haven: Yale University; 1980. [Google Scholar]
- Fisher CR. Health Care Financing Review. Washington: U.S. Government Printing Office; Spring. 1980. Differences by age groups in health care spending. HCFA Pub. No. 03045. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Fisher CR, Schendler CE. National Nursing Home Input Price Index. Division of National Cost Estimates, Office of Financial and Actuarial Analysis, Health Care Financing Administration. 1980 Nov. unpublished. [Google Scholar]
- Freeland MS, Anderson G, Schendler CE. Health Care Financing Review. Washington: U.S. Government Printing Office; Summer. 1979. National hospital input price index. HCFA Pub. No. 03002. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Freeland MS, Schendler CE, Anderson G. Health Care Financing Review. Washington: U.S. Government Printing Office; Dec. 1981. Regional hospital input price indexes. HCFA Pub. No. 03139. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Freeland MS, Schendler CE. Health Care Financing Review. Washington: U.S. Government Printing Office; Mar, 1983. National health expenditure growth in the 1980s: an aging population, new technologies, and increasing competition. HCFA Pub. No. 03149. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Friedman BL. Productivity gains in the drugstore industry, 1958-79. Monthly Labor Review. 1980 Nov.103(11):18–22. [Google Scholar]
- Fries JF. Aging, natural death, and the compression of morbidity. New England Journal of Medicine. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- Fuchs VR. The economics of health in a post-industrial society. Public Interest. 1979 Summer; [PubMed] [Google Scholar]
- Fuchs VR. Who Shall Live? Health, Economics, and Social Choice. New York: Basic Books, Inc.; 1983. [Google Scholar]
- Gibson R, Waldo DR, Levit KR. Health Care Financing Review. Washington: U.S. Government Printing Office; Sept. 1983. National health expenditures, 1982. HCFA Pub. No. 03154. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Ginsburg DH. Medical care services in the consumer price index. Monthly Labor Review. 1978 Aug.101(8):35–39. [PubMed] [Google Scholar]
- Goldsmith JC. Can Hospitals Survive? The New Competitive Health Care Market. Homewood, Illinois: Dow Jones-Irwin; 1981. [Google Scholar]
- Golladay F, Liese B. World Bank Staff Working Paper No 412. Washington, D.C.: World Bank; 1980. Health Problems and Policies in the Developing Countries. [Google Scholar]
- Golladay F. Health Sector Policy Paper. Washington, D.C.: World Bank; 1980. [Google Scholar]
- Graduate Medical Education National Advisory Committee (GMENAC) Report of Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services. 1980 Sept. [Google Scholar]
- Greenspan NT. Health Care Financing Review. 2. Vol. 1. Washington: U.S. Government Printing Office; Fall. 1979. A descriptive analysis of medical malpractice insurance premiums, 1974-1977; pp. 65–71. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Greenspan NT, Vogel RJ. Health Care Financing Review. Washington: U.S. Government Printing Office; Spring. 1980. Taxation and its effect upon public and private health insurance and medical demand. HCFA Pub. No. 03045. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Grimaldi PL. Adjusting to medicare DRG indexes and target ceilings. Hospital Progress. 1983 Jan. [PubMed] [Google Scholar]
- Grimaldi PL. Prospective payment scheme overhauls hospitals' financial incentives. Hospital Progress. 1983 Aug. [PubMed] [Google Scholar]
- Grimaldi PL, Micheletti JA. DRGs: A Practitioner's Guide. Chicago, Illinois: Pluribus Press, Inc.; 1983a. [Google Scholar]
- Grimaldi PL, Micheletti JA. DRG Update: Medicare's Prospective Payment Plan. Chicago: Pluribus Press, Inc.; 1983b. [Google Scholar]
- Gruenberg EM. The failures of success. Milbank Memorial Fund Quarterly/Health and Society. 1977;55(1):3–24. [PubMed] [Google Scholar]
- Hammond J. Home health care cost effectiveness: an overview of the literature. Public Health Reports. 1979;94:309. [PMC free article] [PubMed] [Google Scholar]
- Hanlon JJ, Pickett GE. Public Health Administration and Practice. St. Louis: Times Mirror/Mosby; 1984. [Google Scholar]
- Harker C. Self-Funding of Welfare Benefits. Brookfield, Wisconsin: International Foundation of Employee Benefit Plans; 1981. [Google Scholar]
- Health Care Financing Administration: Medicare Program. Federal Register 42901-42902. Washington: General Services Administration; Sept. 1982. Schedule of Limits on Skilled Nursing Facility Inpatient Routine Service Costs. [PubMed] [Google Scholar]
- Health Care Financing Administration: Medicare Program. Federal Register 39752-39890. Washington: General Services Administration; Sept. 1983. Prospective Payment for Medicare Inpatient Hospital Services; Interim Final Rule with Comment Period. [PubMed] [Google Scholar]
- Health Insurance Association of America. A Profile of Group Medical Expense Insurance in the United States. Washington, D.C.: Health Insurance Association of America; 1983a. [Google Scholar]
- Health Insurance Association of America. New Group Health Insurance, 1982. Washington, D.C.: Health Insurance Association of America; 1983b. [Google Scholar]
- Health Insurance Association of America. Source Book of Health Insurance Data, 1982-1983. Washington, D.C.: Health Insurance Association of America; 1983c. [Google Scholar]
- Hellinger FJ. Substitutability among different types of care under Medicare. Health Services Research. 1977 Spring;:11–18. [PMC free article] [PubMed] [Google Scholar]
- Henderson SR. The malpractice insurance situation and its effect on medical practice. In: Gaffney JC, editor. Profile of Medical Practice, 1978. Revised edition. American Medical Association; Monroe, Wisc.: 1979. [Google Scholar]
- Hendrickson RM. Hard times ahead for physicians. American Medical News. 1980 Jul 25; [PubMed] [Google Scholar]
- Hoff L. In our future: call receptors, recombinant DNA, hybridoma technology. American Druggist. 1983 Jan. [Google Scholar]
- Hughey A. Contact lens competition gets heated. Wall Street Journal. 1982 Nov. [Google Scholar]
- ICF, Inc. Assessment of Recent Estimates of Hospital Capital Requirements. Washington, D.C.: ICF, Inc.; Jun, 1983. Contract No. HHS-100-82-0077. [Google Scholar]
- Institute for Alternative Futures. Pharmaceuticals in the Year 2000. In: Bezold C, editor. The Changing Context for Drug R&D. Alexandria, Virginia: Institute for Alternative Futures; 1983. [Google Scholar]
- Interindustry Economics Division, Bureau of Economic Analysis. The Detailed Input-Output Structure of the US Economy: 1972. 1 and II. Washington: U.S. Department of Commerce; 1979. [Google Scholar]
- Janssen TJ, Saffran GT. Health Care Financing Review. Washington: U.S. Government Printing Office; Winter. 1981. Reimbursement for durable medical equipment. HCFA Pub. No. 03090. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Kane RL, Rubenstein LZ, Brook RH, et al. Utilization review in nursing homes: making implicit level-of-care judgments explicit. Medical Care. 1981;19:3–31. doi: 10.1097/00005650-198101000-00002. [DOI] [PubMed] [Google Scholar]
- Katona G. Psychological Economics. New York: Elsevier; 1975. [Google Scholar]
- Kaufman J. The political ingredient of public health services, a neglected area of research. Milbank Memorial Fund Quarterly. 1966 Oct.44(13) [PubMed] [Google Scholar]
- Klarman HE, Rice DP, Cooper BS, et al. ORS Staff Paper. No. 4. Office of Research and Statistics, Social Security Administration; Washington: Apr, 1970. Sources of increase in selected medical care expenditures, 1929-1969. [Google Scholar]
- Kleiman E. The determinants of national outlay on health. In: Perlman M, editor. The Economics of Health and Medical Care. London: MacMillan; 1974. [Google Scholar]
- Knaus W. Inside Russian Medicine. New York: Everest House; 1981. [Google Scholar]
- Kramer M. The rising pandemic of mental disorders and associated chronic diseases and disabilities. Acta Psychiatrica Scandinavica. 1980;285(62) [Google Scholar]
- Kramer M. The Increasing Prevalence of Mental Disorders: Implications for the Future. Presented at the National Conference on the Elderly Deinstitutionalized Patient in the Community; Arlington, Virginia. May 28, 1981. [Google Scholar]
- Kurowski BD, Shaughnessy PD. The measurement and assurance of quality. In: Vogel RJ, Palmer HC, editors. Long-Term Care, Perspectives From Research and Demonstration. Washington: U. S. Government Printing Office; 1983. Health Care Financing Administration. [Google Scholar]
- Laboratory Management. National survey of hospital and non-hospital clinical laboratories. Laboratory Management. 1979 Mar; [Google Scholar]
- Lane LF. The nursing home: weighing investment decisions. Hospital Financial Management. 1981 May; [PubMed] [Google Scholar]
- Langberg R, Maloy WA. The Aging Veteran: Statistical analyses at the Veterans Administration. Paper presented at the American Statistical Association meetings; Cincinnati, Ohio. Aug. 1982. [Google Scholar]
- Lawson JC. Firms hiking health plan deductibles: study. Business Insurance. 1982 Oct. [PubMed] [Google Scholar]
- Levit KR. Health Care Financing Review. Washington: U. S. Government Printing Office; Dec. 1982. Personal health care expenditures by state. HCFA Pub. No. 03149. Office of Research and Demonstrations, Health Care Financing Administration. [Google Scholar]
- Lindner J, Wagner DA. DRGs spur management related groups. Modern Healthcare. 1983 May; [PubMed] [Google Scholar]
- Lion J, Altman S. Health Care Financial Review. Washington: U. S. Government Printing Office; Sept. 1982. Case-mix differences between hospital outpatient departments and private practice. HCFA Pub. No. 03146. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Liu K, Manton KG, Allison WS. Demographic and epidemiologic determinants of expenditures. In: Vogel RJ, Palmer HC, editors. Long-Term Care, Perspectives From Research and Demonstrations. Washington: U. S. Government Printing Office; 1983. Health Care Financing Administration. [Google Scholar]
- Long CW. Materials managers told to be bottom line conscious in new system. Federation of American Hospitals Review. 1983 Sep-Oct; [PubMed] [Google Scholar]
- Maital S. Minds, Markets and Money Psychological Foundations of Economic Behavior. New York: Basic Books, Inc.; 1982. [Google Scholar]
- Manton KG. Changing concepts of morbidity and mortality in the elderly population. Milbank Memorial Fund Quarterly/Health and Society. 1982 Spring;60(2):183–244. [PubMed] [Google Scholar]
- Mcllrath S. Are DRGs for physicians available? American medical News. 1983 Oct 7; [PubMed] [Google Scholar]
- Mclntyre LR. 1983 U S Industrial Outlook for 250 Industries With Projections for 1987. Bureau of Industrial Economics, U. S. Department of Commerce; Washington: Jan. 1983. Drugs. [Google Scholar]
- QC Factors, A Relationship Between Computerization, Patient Care and the Regulatory Process. Denver: Colorado Department of Health; 1980. Medical Care Licensing and Certification Division. [Google Scholar]
- Medicus Systems. A Review and Evaluation of Health Manpower Productivity. Washington, D.C.: 1980. [Google Scholar]
- Mitchell JB. Patient outcome in alternative long-term care settings. Medical Care. 1978 Jun;XVI:439–452. doi: 10.1097/00005650-197806000-00001. [DOI] [PubMed] [Google Scholar]
- Mushkin SJ, Smelker M, Wyss D, et al. Cost of disease and illness in the United States in the year 2000. Public Health Reports. 1978 Sep-Oct;:493–588. [PMC free article] [PubMed] [Google Scholar]
- Mushkin SJ. Biomedical Research: Costs and Benefits. Cambridge, Massachusetts: Ballinger Publishing Co.; 1979. [Google Scholar]
- Nathanson M. Medical records' new financial role dramatically shifts hospital priorities. Modern Healthcare. 1983 Apr; [PubMed] [Google Scholar]
- National Commission on the Cost of Medical Care. 1 and II. Chicago: American Medical Association; 1978. [Google Scholar]
- Newhouse JP, Phelps CE. New estimates of price and income elasticities. In: Rosett R, editor. The Role of Health Insurance in the Health Services Sector. New York: National Bureau of Economic Research; 1976. [Google Scholar]
- Newhouse JP. Medical care expenditure; a cross-national survey. The Journal of Human Resources. 1977 Winter;XII(1):115–125. [PubMed] [Google Scholar]
- Newhouse JP. The Erosion of the Medical Market Place. Santa Monica, Calif.: Rand Corporation; Dec. 1978. Contract No. R-2141-1-HEW. [Google Scholar]
- Newhouse JP, Manning WG, Morris CN, et al. Some interim results from a controlled trail of cost sharing in health insurance. New England Journal of Medicine. 1981 Dec.:1501–1507. doi: 10.1056/NEJM198112173052504. [DOI] [PubMed] [Google Scholar]
- Office of Research and Demonstrations. Health Care Financing Status Report, Research and Demonstrations in Health Care Financing. Baltimore: Health Care Financing Administration; Oct. 1983. HCFA Pub. No. 03165. [Google Scholar]
- Olson L, Caton C, Duffy M. The Elderly and the Future Economy. Lexington, Mass.: D.C. Heath and Company; 1981. [Google Scholar]
- Personick V. The job outlook through 1995: industry output and employment. Monthly Labor Review. 1983 Nov.106(11):24–36. [PubMed] [Google Scholar]
- Perspective. The Blue Cross and Blue Shield Magazine; Fall. 1982. Perspective: GNP/Health: Can America determine their appropriate relationship? [Google Scholar]
- Pettengill J, Vertrees J. Health Care Financing Review. Washington: U.S. Government Printing Office; Dec. 1982. Reliability and validity in hospital case-mix measurement. HCFA Pub. N. 03149. Office of Reserach and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Pharmaceutical Manufacturers Association. Annual Survey Report PMA 1979-1980. Washington, D.C.: Pharmaceutical Manufacturers Association; 1981. [Google Scholar]
- Pharmacy Times. Apr, 1983. [Google Scholar]
- Phillips G. Capital outlook: some encouragement, much concern, many changes. Hospitals. 1982 Apr 16; [PubMed] [Google Scholar]
- Predicasts, Inc. Industry Study. 300. Cleveland, Ohio: Predicasts, Inc.; Jun, 1983. World health spending. [Google Scholar]
- Reder MW. Some problems in the measurement of productivity in the medical care industry. In: Fuchs VR, editor. Production and Productivity in the Service Industry. New York: Columbia University; 1969. [Google Scholar]
- Reinhardt U. Comment on competition among physicians. In: Greenberg W, editor. Competition in the Health Care Sector: Past, Present, and Future. Bureau of Economics, Federal Trade Commission; Mar, 1978. [Google Scholar]
- Roe BB. The UCR boondoggle, a death knell for private practice? The New England Journal of Medicine. 1981 Jul 2;305(1):41–45. doi: 10.1056/NEJM198107023050108. [DOI] [PubMed] [Google Scholar]
- Roemer MI. Ambulatory Health Services in America, Past, Present, and Future. Rockville, Maryland: Aspen Systems Corporation; 1981. [Google Scholar]
- Russell LB. The impact of the extended care facility benefit on hospital use and reimbursement under Medicare. Journal of Human Resources. 1973 Winter; [Google Scholar]
- Russell L. Washington, D.C.: The Brookings Institution; 1979. Technology in Hospitals: Medical Advances and Their Diffusion. [Google Scholar]
- Russell LB. An aging population and the use of medical care. Medical Care. 1981 Jun;XIX(6):633–643. doi: 10.1097/00005650-198106000-00006. [DOI] [PubMed] [Google Scholar]
- Scanlon WJ. Aspects of the Nursing Home Market, Private Demand, Total Utilization and Investment. Washington, D.C.: The Urban Institute; 1978. [Google Scholar]
- Scholen K, Chen Y. Unlocking Home Equity for the Elderly. Cambridge, Mass.: Ballinger; 1980. [Google Scholar]
- Schwartz WB, Newhouse JP, Bennett BW, et al. The changing geographic distribution of board-certified physicians. The New England Journal of Medicine. 1980 Oct 30;:1032–1038. doi: 10.1056/NEJM198010303031803. [DOI] [PubMed] [Google Scholar]
- Scitovsky T. The Joyless Economy. New York: Oxford University Press; 1976. [Google Scholar]
- Showstack J, Blumberg B, Schwartz J, et al. Fee-for-service physician payment: analysis of current methods, and their development. Inquiry. 1979 Fall;:230–246. [PubMed] [Google Scholar]
- Silvestri GT, et al. Occupational employment projections through 1995. Monthly Labor Review. 1983 Nov.106(11):37–49. [PubMed] [Google Scholar]
- Simanis JG, Coleman JR. Social Security Bulletin. 1. Vol. 43. Washington: U.S. Government Printing Office; Jan. 1980. Health care expenditures in nine industrialized countries, 1960-76; pp. 3–8. SSA Pub. No. 13-11700. Office of Research and Statistics, Social Security Administration. [PubMed] [Google Scholar]
- Sloan F, Steinwald B. The role of health insurance in the physician services market. Inquiry. 1975 Dec.:275–299. [PubMed] [Google Scholar]
- Sloan FA, Schwartz WB. More doctors: What will they cost? Journal of American Medical Association. 1983 Feb.249(6):766–769. [PubMed] [Google Scholar]
- Sobaski WJ, Scitovsky A, McCall N. Health Policy Program Discussion Paper. San Francisco: University of California; 1975. The 1969 California Relative Value Studies and Costs of Physician Office Visits: Two Studies. [Google Scholar]
- Suver JD, Neumann BR. Management Accounting for Health Care Organizations. Oak Brook, Illinois: Hospital Financial Management Association; 1981. [Google Scholar]
- Tilson HH. Intergovernmental relationships: more different or more the same? American Journal of Public Health. 1981 Oct.71(10):1103. [Google Scholar]
- Ting HM, Valiante JD. Future capital needs of community hospitals. Health Affairs. 1982 Summer;:14–27. doi: 10.1377/hlthaff.1.3.14. [DOI] [PubMed] [Google Scholar]
- Tobin J. On limiting the domain of equality. Journal of Law and Economics. 1970 Oct.:263–277. [Google Scholar]
- Torrey BB. Guns vs. canes: the fiscal implications of an aging population. American Economic Review. 1982 May;:309–313. [Google Scholar]
- Trapnell GR. National Health Insurance Issues: The Cost of a National Prescription Program. New York: Hoffman-Laroche, Inc.; 1979. [Google Scholar]
- Trapnell GR, Chang YL, King EC, et al. Develop An Actuarial Model for Medicaid Cost Estimating: Final Report. Actuarial Research Corporation; Falls Church, Va.: Apr 18, 1982. [Google Scholar]
- Trauner JB, Luft HS, Robinson JO. Contract with Federal Trade Commission. San Francico, Calif.: Institute for Health Policy Studies, University of California; Jul, 1982. Entrepreneurial Trends in Health Care Delivery: The Development of Retail Dentistry and Freestanding Ambulatory Services. [Google Scholar]
- U.S. General Accounting Office. The Elderly Should Benefit From Expanded Home Health Care But Increasing These Services Will Not Insure Cost Reductions. 1982 Dec.83(1) GAO/IPE. [Google Scholar]
- U.S. General Accounting Office. Medicaid and Nursing Home Care: Cost Increases and the Need for Services are Creating Problems for States and the Elderly. 1983 Oct.84(1) GAO/IPE. [Google Scholar]
- Veterans Administrtion. Medical and Construction Appropriations and Funds, Fiscal Year 1983. 1982 Feb.II of IV [Google Scholar]
- Wennberg J, Gittelsohn A. Variation in medical care among small areas. Scientific American. 1982 Apr;:120–134. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- Wertheimer AI. A prescription is not a simple matter anymore. American Journal of Public Health. 1983 Aug.73(8):844–845. doi: 10.2105/ajph.73.8.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkin JC. Actuarial Study No 88. Washington: U.S. Government Printing Office; Aug. 1983. Social Security area population projections, 1983. SSA Pub. No. 11-11535. Office of the Actuary, Social Security Administration. [Google Scholar]
- Willemain TR. Health Care Financing Review. Washington: U.S. Government Printing Office; Fall. 1980. Nursing home levels of care: reimbursement of resident specific costs. HCFA Pub. No. 03068. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Williamson JW. Teaching Quality Assurance and Cost Containment in Health Care. San Francisco: Jossey-Boss, Inc.; 1982. and associates. [Google Scholar]
- Zeiter IR. Social Security Bulletin. 3. Vol. 46. Washington: U.S. Government Printing Office; Mar, 1983. Social Security trends and developments in industrialized countries; pp. 52–62. SSA Pub. No. 13-11700. Office of Research and Statistics, Social Security Administration. [PubMed] [Google Scholar]