Abstract
Several States now use patient-based payments for skilled nursing facilities and intermediate care facilities; others are in the process of developing case-mix systems. The Health Care Financing Administration is working under congressional mandate to develop a prospective case-mix system for Medicare payments to skilled nursing facilities. If new payment methods follow the existing pattern, they will be based not on the patient's clinical characteristics but rather on a mixture of clinical characteristics and services delivered. As a result, innate incentives are contained in data collection systems which are cost-increasing at best and dangerous at worst. A preferable approach would be to develop payment schemes based on the patient's degree of dependence.
Overview
Government pricing of nursing home care appears to be undergoing a major change. Traditional methods, which offer an individual facility a single rate for all patients, have been widely criticized for making the heaviest care patients economically unattractive. Rapid rises in nursing home costs, coupled with demographic shifts that will further increase the demand for long-term care, making nursing home prices a topic of intense interest to State policymakers (Tynan, 1981). The high proportion of Medicaid dollars already consumed by institutional long-term care serves to make this interest even more intense (Spitz, 1981). Given the successful introduction of the Diagnosis-Related Groups (DRG's) methodology in the acute care setting, interest in the development of similar methods for skilled nursing facilities (SNF's) and intermediate care facilities (ICF's) is increasing.
The idea of adjusting nursing home payments to allow for variations in residents' needs is not new. Illinois uses a modification of such a system that was first introduced in 1969 (Walsh, 1979). Four other States use patient-based payments; at least two more have recently contracted with outside organizations to develop such systems. The Health Care Financing Administration is currently working under a congressional mandate to develop a prospective case-mix system for Medicare payments to SNF's.
The patient-related payment systems already in use have not been free of problems. Walsh (1979) describes the Illinois system as both expensive and inequitable. He goes on to note that “…patient-related reimbursement introduces in the reimbursement system all of the human elements of inconsistency, arbitrariness, and corruption.” Although troubles experienced in States other than Illinois have not been described in the literature, there is no reason to believe that the Illinois experience is unique. The aim of this paper is to analyze a central element in all patient-based systems: the incentives which arise from the instrument used for data gathered on patients.
Four case-based systems will be examined in this analysis. These include two State systems, Illinois and West Virginia, and two experimental models, those of Cameron and Knauf (1981) and Fries and Cooney (1983). The State systems were chosen because they are well established, well described in the literature, and typical of the State systems now in operation. The two research models were included because they represent the most recent work in the field, and they are the only long-term care systems reported to date that use AUTOGRP—the interactive statistical program from which DRG's were defined (Mills, 1976).
All four systems used for analysis are Medicaid only. The payment schemes of Illinois and West Virginia are used for Medicaid reimbursement, and they do not affect Medicare or private-pay prices. The data used for Cameron's research were collected entirely on nursing home residents covered by Medicaid, Fries and Cooney's data are based on a resident group that was 92 percent Medicaid and 8 percent Medicare. The conclusions reached in this article are therefore applicable only to residents covered by Medicaid, the vast majority of whom are expected to have long nursing home stays. Whether covered by Medicare, private pay, or Medicaid, residents with short nursing home stays are a very different population group and may well require a very different payment scheme. No case-mix system for the short-stay group is available for analysis at present.
The West Virginia system described here is, in Willemain's terms, “patient centered”: it assigns a specific price to a specific patient. Illinois, by contrast, recently changed to what Willemain would consider a true case-mix system in which a facility rate is developed from the characteristics of a random sample of patients (Willemain, 1980). The issues regarding patient information are of equal importance in both types of systems. Despite Willemain's careful distinction, the term “case-mix” is used by most authors (Stassen, 1983) to describe “…many approaches to adjusting reimbursement for differences in patient needs.” The term will therefore be used in its broadest sense throughout this paper to describe both patient-specific and facility-wide systems.
Why patient-based payments?
The problems inherent in existing payment methods for long-term care are somewhat different from those that led Congress to mandate DRG's. In hospital payment, some form of adjustment for the care needs of individual patients was seen as an essential element in effective control of costs. If tight control were simply exerted over the rise in average costs, hospitals caring for the healthier patients would be rewarded, and those caring for the sicker patients would be penalized. Since earlier attempts at cost control had been based on each facility's own historic costs, tight control in the absence of case-mix adjustments would have rewarded those institutions that had high historic costs as a result of inefficiency. DRG's were viewed as providing a fair means to control rising costs while allowing efficient hospitals more flexibility in managing their funds.
In long-term care the same problem exists, but at a different point in time. Although State payments for skilled and intermediate care facilities must, by law, be “cost related,” States have been able to devise a variety of methods for limiting the rise in these payments. The result in many States has been fairly effective control of daily costs coupled with the emergence of special problems related to the care of the sickest and/or most dependent patients. There seems to be little question that institutions choose among patients, leaving many of the sickest “backed up” in hospitals; the exact size of the problem is difficult to quantify however. The common wisdom is that these patients are those who are the most dependent or require the most intensive nursing care. One detailed study of “backup days” in New York City suggests that mental illness is also a common cause of such discrimination (NYCHSRO, 1982).
In addition to the problem of backup days, highly restrictive State payment systems raise the question of whether or not institutions can deliver adequate care to the sickest patients at the going rate. The impetus for case-mix payments is the need to adjust for the ill effects experienced as a result of cost controls that have previously made no adjustments for patient need. What was feared in the debate about hospital payment has, in fact, happened in nursing homes. The goal, therefore, of case-mix reimbursement for long-term care is to make the most dependent patients more attractive to nursing homes and to ensure that these patients receive adequate amounts of care once admitted.
Willemain, in arguing for payments that are facility-specific rather than patient-specific, assumes that there is an ideal amount of care that each patient should receive on a given day. He freely admits, however, that little empirical evidence is available to demonstrate what such ideal care is (Willemain, 1980). It seems preferable to regard case-mix payments in long-term care as we regard them in hospital care: prices that reflect patient need, allowing efficient institutions to deliver care of adequate quality to all of their residents.
There is a major difference between nursing homes and hospitals: the pervasive concern that nursing home care may not be of adequate quality. As a result, any payment method for long-term care facilities should be at best quality-enhancing and at worst as close to quality-neutral as possible. Since many commentators on long-term care would express concern that cost savings in this field can arise from poor care rather than efficiency, the incentives inherent in a case-mix system for long-term care should be well understood so that regulatory strategies can be developed to compensate for payment system weaknesses.
Inherent incentives
Incentives in any case-mix payment system are of two types: those that are inherent in the patient data collection methods used to compose the system and those that are structural, arising in the process of conversion from patient status to price. Inherent incentives arise directly from those patient characteristics and treatment processes that are included in the tool, leading to higher scores and, therefore, to higher prices. For example, an instrument that emphasizes mental illness will contain inherent incentives to admit and care for emotionally disturbed patients. Structural incentives contained in the pricing process may enhance or alter the inherent incentives in a variety of ways. If the payment system does not provide adequate funds to care for severely disturbed patients, then the inherent incentives will be obliterated. By contrast, if the payment system leads to a reduction in price as soon as a patient improves, then the inherent incentive to admit the mentally ill will persist, but it will be associated with a much more disturbing incentive of not encouraging these patients to recover.
The two types of incentives arise from different aspects of the payment mechanism, and they can be altered in different ways. Analyses of the nature of the resulting influences on institutions should therefore consider each type of incentive separately. Inherent incentives, which have received relatively little attention in the literature, are the primary focus of this analysis; they will first be described using the simplifying assumption that high scores will be rewarded. Later, the complexities introduced by structural design will be discussed briefly in order to illustrate the wide range of results that the translation to payment can impose on a data instrument.
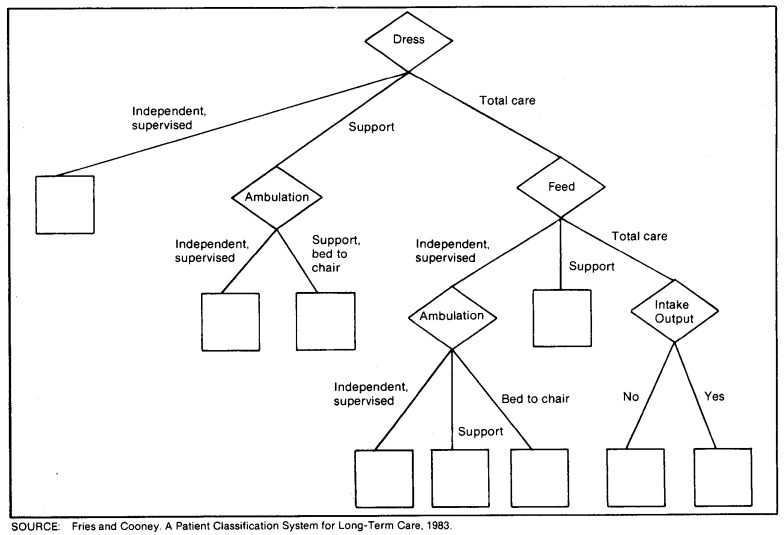
Table 1 lists the patient and service characteristics common to the Illinois and West Virginia systems, and lists characteristics unique to each system. Figure 1 shows an AUTOGRP-based system proposed by Fries and Cooney. The system subdivides patients using a single variable at each branching point to create the split. The end result is nine patient groups with distinct resource use. Four characteristics have been used to create these groups. Table 2 displays Cameron's results using AUTOGRP on a different data base. This study creates 13 patient groups, with 9 characteristics serving to distinguish among groups.
Table 1. Patient and service characteristics used by the States of Illinois and West Virginia.
| Common characteristics | |
|---|---|
| Illinois | West Virginia |
| Patient characteristics | Patient characteristics |
| Bathing | Personal hygiene |
| Clothing | Eating |
| Eating | Mobility |
| Mobility | Continence |
| Continence | Mental status or behavior |
| Behavior | |
| Mental status | |
| Service characteristics | Service characteristics |
| Appliances | Appliances |
| Catheterization | Catheterization |
| Douche or enema | Douche or enema |
| Dressings | Dressings |
| Injections | Injections |
| Intravenous | Intravenous |
| Medications | Medications |
| Ostomy care | Ostomy care |
| Restorative nursing | Restorative nursing |
| Unique characteristics | |
| Illinois | West Virginia |
| Service characteristics | Service characteristics |
| Decubitus care | Oxygen |
| Diets | Suction tracheostomy |
| Laboratory or specimen service | |
| Language rehabilitation | |
| Medication monitoring | |
| Occupational rehabilitation | |
| Physical rehabilitation | |
| Respiratory therapy | |
| Social rehabilitation | |
| Special health monitoring | |
| Suctioning or posturing | |
| Tube feeding | |
Figure 1. Resource utilization groups.
Table 2. Proposed groupings and variable costs, Cameron and Knauf's Grouping Method.
| Group | Characteristics | Direct care costs |
|---|---|---|
| 1 | Neuro diagnosis, tube feeding | $97.97 |
| 2 | Neuro diagnosis, continent, no catheter | 24.17 |
| 3 | Neuro diagnosis, incontinent, no mobility | 34.93 |
| 4 | Neuro diagnosis, incontinent, mobile | 29.44 |
| 5 | Neuro diagnosis, catheter, no mobility | 55.62 |
| 6 | Neuro diagnosis, catheter, mobile | 39.81 |
| 7 | Nonneuro diagnosis, decubitus stage II, III, IV | 41.49 |
| 8 | Nonneuro diagnosis, catheter | 33.40 |
| 9 | Nonneuro diagnosis, incontinent, totally dependent feeding | 29.56 |
| 10 | Nonneuro diagnosis, incontinent, not totally dependent feeding | 22.56 |
| 11 | Nonneuro diagnosis, continent, dependent walking | 21.00 |
| 12 | Nonneuro diagnosis, continent, independent walking, with special treatment | 21.62 |
| 13 | Non-neuro diagnosis, continent, independent walking, without special treatment | 15.04 |
A review of the characteristics listed in Table 1 shows that they fall into two categories: patient characteristics and service characteristics. The first seven elements in the Illinois scheme, which have been consolidated into five in West Virginia, measure patient qualities that will be unaffected by treatment in the shortrun and in many patients will be unaffected by longrun treatment as well. These include mental status, the level of independence in bathing, dressing, eating, and walking, as well as the presence or absence of incontinence and behavior problems. The 21 additional characteristics in the Illinois scheme and the 11 additional in West Virginia all reflect service patterns: whether injections are used, how many medications are given, and the type and level of rehabilitation services. In the experimental grouping systems, Cameron and Knauf's nine characteristics include three service and nine clinical; Fries and Cooney's four characteristics include one service and three patient.
The Illinois assessment manual assigns specific points to each characteristic: a total of 23 points arise from patient characteristics, and an additional 36 are attributable to treatments. In West Virginia, the maximum number of minutes that could be earned through patient status characteristics is 210; treatment can earn another 204. In Cameron's scheme, direct care costs by group range from a high of $97.97 for group 1 to a low of $15.04 for group 13. Of the six highest-priced groups, four are defined by the use of a service. Of the seven lowest priced groups, only one is defined by the use of a service.
The incentives that result are both clear and strong: more service means more money.
Control over and effects of services
The use of service characteristics to define case mix is not peculiar to long-term care. A major grouping variable in the construction of DRG's is the presence or absence of a surgical procedure performed in an operating room. Pettengill and Vertrees (1982) have discussed the problem of the inclusion of procedures in the design of hospital case-mix systems. They conclude that excessive encouragement of surgery is unlikely because the physician, not the hospital, makes the decision regarding surgery. They note that the doctor's choice of treatment “…is likely to be more strongly influenced by the relative risks to the patient and the economic incentives imbedded in the physician fee structure than by any effects of hospital reimbursement.”
There are important differences between surgery and the kinds of services used in long-term care case-mix systems. In a hospital, the responsible physician makes the decision to perform surgery and then performs it himself or herself. In a nursing home, however, the physician writes an order for a service that is then performed, usually in the physician's absence, by nursing staff. In practice, decisions such as the insertion of a urinary catheter, the initiation of tube feedings, or the administration of tranquilizers are usually negotiated between nursing staff and the responsible physician. Nursing staff, who must manage the patient for long periods in the physician's absence and will therefore be much more affected by treatment decisions than the physician, often effectively control the negotiations. As a result, the decision to do a given procedure is in the hands of nursing home employees, which is in sharp contrast to the decision to perform surgery that is made by a physician who is usually independent of the affected hospital.
The degree of local control over the kinds of nursing procedures used to determine payment is varied and is dependent on both the patient's condition and the nature of the treatment. A chronic, indwelling urinary catheter, for example, is unavoidable in a patient with outlet obstruction for whom surgical correction is infeasible. In many other patients the catheter is used as a convenient way to deal with chronic incontinence; its use for incontinence is judgmental and will depend on institutional and individual attitudes. Even when a clinical condition requires some treatment, such as dressings for foot ulcers or medication for uncontrollable diabetes, the local physician and nurses have considerable discretion as to how often dressings are changed or what kind of medication is used.
The effects of treatments used on patients with little medical indication are also variable. At one extreme are “benign” treatments, such as laboratory tests and social rehabilitation, that only waste money if used unnecessarily. At the other extreme are treatments, such as the urinary catheter, that increase risk, cause discomfort, and reduce independence. Because catheters are associated with increased infection rates, and may discourage or prevent ambulation, their use in judgmental situations should be discouraged, not rewarded. The same is true of tube feedings. Although such feedings are unavoidable in the unresponsive patient, there are a number of patients who can be hand fed with patience and coaxing. Optimal care involves avoiding the use of tube feeding for this group. Other service elements that are rewarded in the schemes described above and have a harmful effect if used inappropriately include douche or enemas, injections, intravenous feedings, complex medication programs, and the use of oxygen.
Structural incentives
Inherent incentives may be enhanced, altered, or even obliterated by pricing structure. As Pettengill and Vertrees have noted, the price attached to a procedure must be at least equal to the institution's cost in order for any incentive to exist (Pettengill, 1982). With many of the procedures described here, the amount of nursing time used and, therefore, the cost of the procedure to the nursing home can vary widely from the ideal or standard on which price is based. The use of a urinary catheter can be made more economical by avoiding time-consuming efforts to reduce infections. Dressing changes, which are usually done two or three times a day, are far less costly if done daily or even less often. In short, unless careful attention is paid to the design of the payment system, the resulting incentive may be not only to do more nursing procedures but to do them badly.
Holahan and Cohen, for example, note that in Illinois during the period between 1978 and 1980 the true incentive was to attract needier patients while offering them less care. This arose because increased payments were based on the State's case-severity measure, regardless of the facility's actual costs. Their analysis shows that institutions responded to this incentive: average case complexity of Medicaid patients increased with no associated “increase in resources used to treat these patients commensurate with the reported increase in case-mix” (Holahan, 1983). This outcome is avoided in West Virginia, where case-mix adjustment is used as a cap on allowable costs (Cohen, 1983).
A key structural incentive is that created by the timing of reassessments. Many commentators fear case-mix based payment for long-term care because of the possibility that higher payment for more intensive care may encourage homes to keep patients dependent. In fact, the exact incentives associated with recovery are determined by the speed with which payments are adjusted downward as a patient improves and by the institutional costs associated with recovery. If the adjustment is very rapid, the institution will have no incentive to foster recovery. If, on the other hand, adjustment is slow and the price difference between dependent and independent patients is great, then there will be an incentive to admit sick patients who can be rehabilitated rapidly. During the recovery period, as patients improve and the cost of care decreases, the institution will be able to retain profits. The concept of fostering recovery by allowing institutions to retain a payment level related to the patient's dependency on admission is currently being tested in a reimbursement experiment in Southern California (Weissert, 1983; Meiners, 1983).
Operational problems
In addition to containing perverse incentives, case-mix definitions oriented toward service characteristics rather than patient characteristics present operational difficulties. Lengthy data collection instruments, such as those used by Illinois and West Virginia, are at once expensive and subject to problems with reliability. Walsh (1979) notes that both problems had proved severe in the version of the Illinois system then in use. A state-wide cost of $4 million was attributed to the case-mix system. In addition, testing demonstrated a 15-percent variation among the regions of the State that was interpreted as indicating poor instrument reliability rather than actual variation in patient characteristics. Walsh goes on to note that minor changes in the cumulative point count can mean substantial differences in income for a facility. Attempts to influence caseworker judgment are therefore likely. Caseworkers have a natural incentive to maximize the initial point count in order to insure placement and to maintain high point counts for those facilities they perceive to be deserving of reward (Walsh, 1979).
Illinois has dealt with these problems by moving to a system based on a sample of a facility's patients, by decreasing the frequency of reassessment to every 6 months for all patients, and by using nurses instead of social workers to conduct the assessments. Little has been done, however, to test or improve the basic reliability of the instrument itself. Many characteristics are scored on the basis of judgments, such as whether a patient requires “special monitoring” of medications or is receiving respiratory therapy that is “complex due to the nature of the resident's condition.” Variations in interpretation of the use of such characteristics are highly likely; such variations have been demonstrated in the closely-related area of coverage decisions for Medicare's skilled nursing benefit (Smits, 1982).
An alternative approach
Case-mix measures that depend on the use of services contain inherent incentives that tend to be perverse. The treatment elements used are often under the control of the nursing home. When unneeded treatments are induced by payment schemes, the result is at best wasteful and at worst dangerous to patients. In addition, service-related scoring is complex, leading both to high system cost and to problems with instrument reliability.
The most promising solution to these difficulties would be the use of objective patient characteristics, rather than service characteristics, as the primary basis for case mix payments. Such a choice has a sound theoretical base. A wide variety of studies have linked patient characteristics, such as those used by Illinois and West Virginia to the use of resources, particularly nursing time. These include McCaffree's work (McCaffree, 1979), the “debility index” of Skinner and Yett, (Skinner, 1973), Parker's “geriatric index” (Parker, 1971), Swearingen's grouping method (Swearingen, 1978) and the study by Fries and Cooney described here. Although these studies use varied approaches and reach somewhat different conclusions, they have an overall conceptual consistency: all authors agree that feeding, ambulation, dressing, and continence are major determinants of the need for and cost of care.
These characteristics are all found in the best known of the available functional indexes: Katz' index of the Activities of Daily Living (ADL's). First reported in 1963, this simple index has been used widely by many researchers studying the elderly and disabled. The characteristics in Katz' scale are bathing, dressing, toileting, transfers, continence, and feeding (Katz, 1963).
The actual development of a clinically-based scoring system for payment must depend on a demonstrated association between the patient characteristics and the resources used or needed to deliver satisfactory care. Because of strong intercorrelations among the characteristics in Katz' scale, all six may not be needed as a basis for payment. The addition of elements relating to mental status and behavior may be necessary to accurately define institutional service needs. The classification scheme of Fries and Cooney demonstrates how very few characteristics can be used to develop groups of patients with distinct resource use. Their grouping variables include only dressing, ambulation, feeding, and the monitoring of intake and output. The last is not a suitable characteristic for a payment scheme because it is so easily manipulated by institutions. The authors noted this problem and developed one possible alternative grouping using the original reason for placement as the fourth variable.
Fries and Cooney did not attempt to price their Resource Utilization Groups (RUG's). These authors have, however, demonstrated that very simple patient characteristics can be used to create a grouping scheme that accurately reflects differences in resource use. A payment scheme based on a classification arrangement similar to the RUGs would fill all of the criteria for a satisfactory case-mix measure in long-term care described in a recent review by Stassen and Bishop (Stassen, 1983). The number of groups is manageable, and the distinctions are clinically valid and possess sufficient clarity to be easily understood by providers. Finally, the measures are feasible to construct, data collection and scoring development would be straightforward particularly when compared with existing service oriented schemes.
Katz' scale has proved reliable across a wide variety of research settings; it can be administered by an individual without extensive training. Because so few characteristics are used, training can focus on problems such as the precise definition of “assistance” with an activity such as dressing, thus enhancing reliability still further. Another important advantage of a functional scale is that State personnel would not need to rely exclusively on patient records for information but could instead observe samples of patients directly in order to verify institutional reports of dependence. The activities to be recorded are relatively simple ones, allowing a single observer to score a number of patients by direct observation in a relatively short time. Finally, the patient characteristics suggested here cannot easily be altered by a nursing home at short notice. It is no easy task to convince an elderly resident who usually eats independently to submit to hand feeding the day the inspectors arrive. Surprise inspections for scoring purposes could also serve to insure that institutions do not increase staff, and therefore the appearance of patient dependency, at the time of scoring.
No payment system for long-term care will be problem free. The greatest drawback of dependency-based pricing is the obvious one that nursing homes may be encouraged not only to admit very dependent patients but to keep them that way. One approach to this problem is that used in the Southern California experiment: to continue the high rate of payment indefinitely, thus creating a significant bonus for recovery. Such a solution, however, creates its own problems. First, there is no guarantee that the recovery bonus will be sufficient to cover the costs of rehabilitation and no certainty therefore that any incentive exists or that it exists for all patients. Second, if the bonus is small compared with rehabilitation costs, facilities will be encouraged to expend rehabilitation resources only on those patients who have a high likelihood both of recovering and of staying in the institution for a period of time post recovery. Rehabilitation of the patient with a terminal illness, or of the very fragile patient who appears likely to have a new stroke or heart attack, will in fact be discouraged. A final problem could arise from the institution's desire to retain bonus-paying patients, a desire that may discourage discharge to the community and that could also lead to an inappropriate, and possibly dangerous, deferring of hospitalization. Even if it were possible to solve all of these problems, a major obstacle to such an arrangement still exists in the form of State reluctance to continue indefinitely to pay bonuses which would eventually be perceived as unnecessary.
An alternative reimbursement strategy to deal with the dependency incentive would be to segregate payment methods for patients who are engaged in active rehabilitation programs from those who are not. All of the work on the association between functional status and costs has been based on data collected about patients who are largely or entirely long-stay and stable. In addition, most of the studies cited here have not measured the costs of rehabilitation. There is no method at present to define an association between the characteristics of rehabilitation patients and the costs of caring for them. An ideal case-mix scheme for short-stay, recuperating nursing home patients would probably be a hybrid of the concepts embodied in hospital case mix and those used in long-term care. Even though dependence as measured by ADL's would still be an important influence on costs, the diagnosis leading to the need for rehabilitation is likely to be more useful in predicting cost than diagnoses have proved in long-stay patients. At present, in the absence of research on which to base a case-mix payment scheme for short-stay rehabilitation patients, some form of cost payments would appear to be the only practical solution.
If payments for active rehabilitation, or more precisely for all patients with significant recovery potential, are made on a different basis, then functional status case mix could comfortably be used for the vast majority of stable long-stay Medicaid patients in nursing homes. A finely tuned reimbursement system might provide for a single and significant bonus for the patient who makes an unanticipated recovery and might also include rewards for the prevention of deterioration. An alternative approach would be to accept the weakness in the payment system and simply focus regulatory efforts on ensuring the delivery of rehabilitative services aimed at the long-stay patient. For the vast majority of Medicaid patients, however, the absence of a significant incentive towards recovery woud appear to carry relatively little risk, particularly when compared with the significant and often unnoted perversities in existing case-mix systems.
Summary
Illinois began patient-related payments to nursing homes in 1969. Other States, aware of the problems inherent in the Illinois system, showed little or no interest in case-mix adjustments for almost a decade. By the late 1970's increasing problems with nursing home patients backed up in hospitals demonstrated that some adjustment for care needs was essential to permit placement and ongoing care for the most costly patients. Four States have recently adopted case-mix systems and at least two more are publicly committed to doing so. Enthusiasm for such payment methods has been enhanced by the adoption of DRG payments for hospitals and by recent research demonstrating associations between patients' functional status and the amount of resources used to deliver care.
Case-mix systems will solve some old problems but they wil also create new ones. One particularly important new problem is that of incentives. All case-mix systems used to date in long-term care contain perverse incentives that encourage the use of expensive services, many of which are potentially dangerous to patients when used unnecessarily. The use of functional status as a basis for case mix would be an important first step towards the design of a payment method in which all incentives are clear, well understood by both the State and its nursing homes, and beneficial to patients.
Acknowledgments
The author is indebted to Drs. Larry McMahon, Mark Meiners, and William Scanlon as well as two anonymous reviewers for their thoughtful criticisms of earlier drafts of this article.
Footnotes
Reprint requests: Helen L. Smits, Room 206, 12 Prospect Place, New Haven, Connecticut 06510.
References
- Cameron J, Knauf R. Long-Term Care Facilities Study, Final Report, Health Systems Research, Inc. California Department of Health Services; Dec. 1981. Prepared for. Contract No. 80-64741. [Google Scholar]
- Cohen J, Holahan J. Nursing Home Reimbursement in West Virginia—Effects on Cost Control, Access and Case-Mix. Washington, D.C.: The Urban Institute; 1983. Report No. 3172-06. [Google Scholar]
- Fetter B, et al. Case-mix definition by diagnosis related groups. Med Care. 1980 Feb.18(2 Supplement) [PubMed] [Google Scholar]
- Fries E, Cooney LM. A Patient Classification System for Long-Term Care. New Haven, Conn.: Yale School of Organization and Management; 1983. Report to HCFA. [Google Scholar]
- Holahan J, Cohen J. Nursing Home Reimbursement in Illinois—Effects on Cost Control, Access and Case-Mix. Washington, D.C.: The Urban Institute; 1983. Report No. 3172-01. [Google Scholar]
- Katz S, et al. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:94–100. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- McCaffree KM, Winn S, Bennett CA. Final Report of Cost Data Reporting System for Nursing Home Care. Health Care Study Center, Battelle Human Affairs Research Centers; Seattle, Wash.: Oct. 1976. [Google Scholar]
- McCaffree KM, Baker J, Perrin E. Long-Term Care Case Mix Employee Time and Costs. Health Care Study Center, Battelle Human Affairs Research Centers; Seattle, Wash.: Feb. 1979. [Google Scholar]
- Meiners MR, Heinemann GD, Jones BJ. An Evaluation of Nursing Home Payments Designed to Encourage Appropriate Care for the Chronically Ill: Some Preliminary Findings. Paper presented at the annual meeting of the American Economic Association; Dec. 1982. [Google Scholar]
- Mills R, et al. AUTOGRP, An Interactive Computer System for the Analysis of Health Care Data. Med Care. 1976;14:603–615. doi: 10.1097/00005650-197607000-00005. [DOI] [PubMed] [Google Scholar]
- New York County Health Services Review Organization. Nursing Home Bed Shortage: Myth or Reality. N.Y.: NYCHSRO; 1982. [Google Scholar]
- Parker R, Boyd J. A comparison of discriminate versus a clustering analysis of a patient classification for chronic disease care. Med Care. 1974 Nov.12:944–957. doi: 10.1097/00005650-197411000-00006. [DOI] [PubMed] [Google Scholar]
- Pettengill J, Vertrees J. Health Care Financing Review. No. 2. Vol. 4. Washington: U.S. Government Printing Office; Dec. 1982. Reliability and validity in hospital case-mix measurement. HCFA Pub. No. 03149. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Skinner DE, Yett DE. Debility index for long term care patients. In: Berg RL, editor. Health Status Indexes. Chicago: Hospital Research and Educational Trust; 1973. [Google Scholar]
- Spitz B. State Guide to Medicaid Cost Containment. Washington, DC: Intergovernmental Health Policy Project; 1981. [Google Scholar]
- Stassen M, Bishop E. Incorporating Case Mix in Prospective Reimbursement for Skilled Nursing Facility Care under Medicare—Critical Review of Relevant Research. Waltham, Mass.: Center for Health Policy Analysis and Research, Brandeis University; 1983. Report to HCFA. [Google Scholar]
- Swearingen C, et al. A Methodology for Finding, Classifying and Comparing Costs for Services in Long-Term Care Settings. Cambridge, Mass.: ABT Associates; 1978. [Google Scholar]
- Tynan E, Daniel H, Schlenker R. A Synthesis of Research on Nursing Home Reimbursement. Denver, Colo.: University of Colorado Health Sciences Center; 1981. [Google Scholar]
- Walsh TJ. Patient-Related Reimbursement for Long-Term Care. In: LaPorte V, Ruben J, editors. Reform and Regulation in Long-Term Care. NY: Piaeger; 1979. [Google Scholar]
- Weissert W, Scanlon W, Wan T, Skinner D. Health Care Financing Review. No. 2. Vol. 5. Washington: U.S. Government Printing Office; Feb. 1983. Care for the chronically ill: Nursing home incentive payment experiment. HCFA Pub. No. 03168. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Willemain TR. A comparison of patient centered and case-mix reimbursement for nursing home care. Health Services Research. 1980 Winter; [PMC free article] [PubMed] [Google Scholar]