Abstract
Although growing more slowly than in recent years, spending for health continued to account for an increasing share of the Nation's gross national product. In 1983, spending for health amounted to 10.8 percent of the gross national product, or $1,459 per person. Public programs financed 40 percent of all personal health care spending. Medicare and Medicaid expended $91 billion in benefits, 29 percent of all spending for personal health. New estimates of spending in calendar year 1983, along with revised measures of the benefits paid by private health insurers, are presented here.
The United States spent an estimated $355 billion for health in 1983, an amount equal to 10.8 percent of the gross national product. Highlights of the figures that underly this estimate include the following:
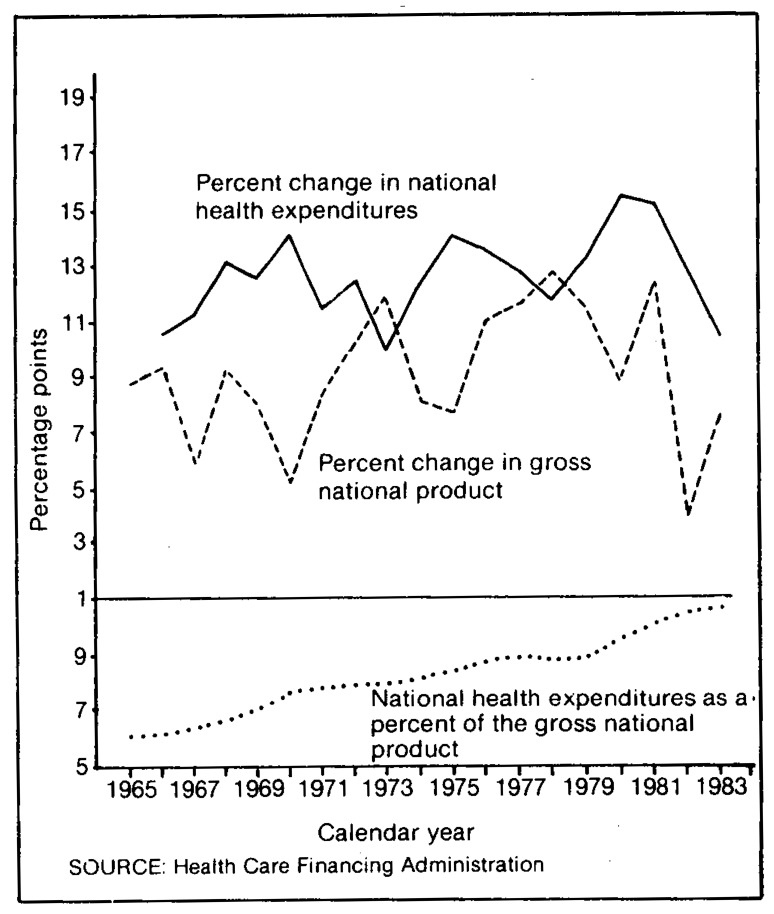
Health expenditures grew 10.3 percent between 1982 and 1983 (Figure 1).
Health expenditures amounted to $1,459 per person in 1983, $122 more than 1982. Of that amount, $611 came from public funds.
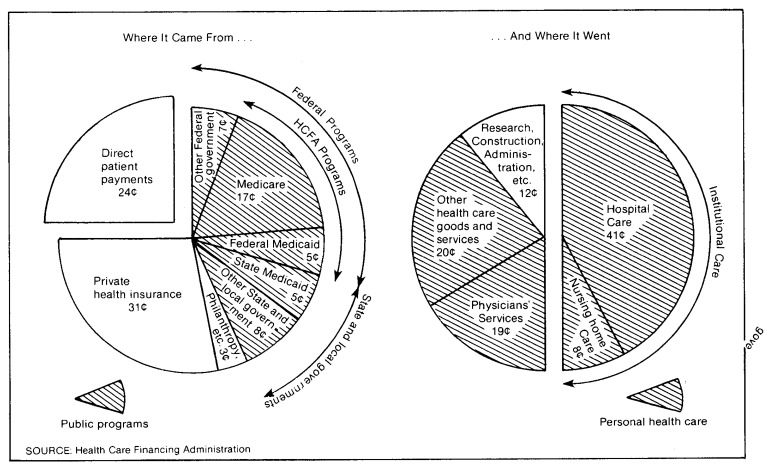
Hospital care accounted for 41 percent of total health care spending in 1983 (Figure 2). These expenditures rose to a level of $147 billion—an increase of 9.1 percent from 1982.
Spending for the services of physicians increased 11.7 percent to $69 billion—19 percent of all health care spending.
Public sources provided 42 cents of every dollar spent on health in 1983. Federal payments amounted to $103 billion, and $46 billion came from State and local governments.
Consumers paid $196 billion for health care in 1983, either directly or (together with employers) in the form of health insurance premiums.
All third parties combined—private health insurers, Government, private charities, and industry—financed 73 percent of the $313 billion spent for personal health care in 1983, covering 92 percent of hospital care services, 72 percent of physicians' services, and 44 percent of the remainder.
Outlays for health care benefits by the Medicare and Medicaid programs totaled $91 billion, including $54 billion for hospital care. The two programs combined paid for 29 percent of all personal health care in the Nation.
Figure 1. National health expenditures and gross national product and national health expenditures as a percent of the gross national product: 1965-1983.
Figure 2. The Nation's health dollar in 1983.
Overview
As shown in Table 1, expenditures for health reached $355 billion in 1983, an increase of 10.3 percent from 1982 and an amount equal to 10.8 percent of the gross national product (GNP). Although real growth—exclusive of price inflation—lagged behind the rest of the economy by a small margin, price inflation for health-related goods and services was much more rapid than that for other goods and services. The inflation effect being dominant, the share of our Nation's production accounted for by health increased from 10.5 percent in 1982 to 10.8 percent in 1983. Rapid growth of health costs, which places increasing financial strain on Federal programs such as Medicare, Medicaid, and the Veterans' Administration, as well as upon purchasers of private health insurance, has sparked a national debate of the philosophy and direction of health care financing.
Table 1. Aggregate and per capita national health expenditures, by source of funds and percent of gross national product: Selected calendar years, 1929-83.
| Item | 1983 | 1982 | 1981 | 1980 | 1979 | 1978 | 1977 | 1976 | 1975 | 1974 | 1973 | 1972 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| National health expenditures in billions | $355.4 | $322.3 | $285.8 | $248.0 | $215.1 | $190.0 | $170.2 | $150.8 | $132.7 | $116.3 | $103.4 | $93.9 |
| Percent of the Gross National Product | 10.8 | 10.5 | 9.7 | 9.4 | 8.9 | 8.8 | 8.9 | 8.8 | 8.6 | 8.1 | 7.8 | 7.9 |
| Source of funds in billions | ||||||||||||
| Private expenditures | $206.6 | $186.5 | $164.2 | $142.2 | $124.2 | $110.1 | $100.1 | $87.9 | $76.3 | $68.8 | $64.0 | $58.5 |
| Public expenditures | 148.8 | 135.8 | 121.7 | 105.8 | 90.9 | 79.9 | 70.1 | 62.8 | 56.4 | 47.6 | 39.4 | 35.4 |
| Federal expenditures | 102.7 | 93.3 | 83.5 | 71.1 | 61.0 | 53.8 | 47.4 | 42.6 | 37.1 | 31.0 | 25.2 | 22.9 |
| State and local expenditures | 46.1 | 42.6 | 38.1 | 34.8 | 29.8 | 26.1 | 22.7 | 20.3 | 19.3 | 16.6 | 14.2 | 12.5 |
| Per capita expenditures1 | $1,459 | $1,337 | $1,197 | $1,049 | $920 | $822 | $743 | $665 | $590 | $522 | $468 | $429 |
| Private expenditures | 848 | 774 | 688 | 601 | 531 | 476 | 437 | 388 | 340 | 309 | 290 | 268 |
| Public expenditures | 611 | 564 | 510 | 448 | 389 | 346 | 306 | 277 | 251 | 214 | 178 | 162 |
| Federal expenditures | 422 | 387 | 350 | 301 | 261 | 233 | 207 | 188 | 165 | 139 | 114 | 105 |
| State and local expenditures | 189 | 177 | 160 | 147 | 128 | 113 | 99 | 89 | 86 | 75 | 64 | 57 |
| Percent distribution of funds | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private funds | 58.1 | 57.9 | 57.4 | 57.3 | 57.7 | 57.9 | 58.8 | 58.3 | 57.5 | 59.1 | 61.9 | 62.3 |
| Public funds | 41.9 | 42.1 | 42.6 | 42.7 | 42.3 | 42.1 | 41.2 | 41.7 | 42.5 | 40.9 | 38.1 | 37.7 |
| Federal funds | 28.9 | 28.9 | 29.3 | 28.7 | 28.4 | 28.4 | 27.9 | 28.2 | 28.0 | 26.6 | 24.4 | 24.4 |
| State and local funds | 13.0 | 13.2 | 13.3 | 14.0 | 13.9 | 13.7 | 13.3 | 13.5 | 14.5 | 14.3 | 13.7 | 13.3 |
| Addenda | ||||||||||||
| Gross national product (billions) | $3,304.8 | $3,069.2 | $2,957.8 | $2,631.7 | $2,417.8 | $2,163.9 | $1,918.3 | $1,718.0 | $1,549.2 | $1,434.2 | $1,326.4 | $1,185.9 |
| Population in millions | 243.6 | 241.1 | 238.7 | 236.4 | 233.8 | 231.3 | 228.9 | 226.8 | 224.8 | 222.7 | 220.8 | 218.8 |
| Annual percent changes | ||||||||||||
| National health expenditures | 10.3 | 12.8 | 15.2 | 15.3 | 13.2 | 11.7 | 12.9 | 13.6 | 14.0 | 12.5 | 10.0 | 12.5 |
| Private expenditures | 10.8 | 13.6 | 15.5 | 14.5 | 12.8 | 10.0 | 13.8 | 15.2 | 11.0 | 7.4 | 9.3 | 12.9 |
| Public expenditures | 9.5 | 11.7 | 15.0 | 16.5 | 13.7 | 14.0 | 11.6 | 11.5 | 18.5 | 20.8 | 11.2 | 11.8 |
| Federal expenditures | 10.1 | 11.7 | 17.5 | 16.5 | 13.3 | 13.5 | 11.4 | 14.8 | 19.8 | 22.9 | 10.0 | 12.6 |
| State and local expenditures | 8.2 | 11.6 | 9.7 | 16.5 | 14.3 | 15.1 | 11.8 | 5.2 | 16.1 | 17.0 | 13.3 | 10.3 |
| Gross national product | 7.7 | 3.8 | 12.4 | 8.8 | 11.7 | 12.8 | 11.7 | 10.9 | 8.0 | 8.1 | 11.8 | 10.1 |
| Population | 1.1 | 1.0 | 1.0 | 1.1 | 1.1 | 1.0 | .9 | .9 | .9 | .8 | .9 | 1.0 |
| National health expenditures in billions | $83.5 | $75.0 | $65.6 | $58.2 | $51.5 | $46.3 | $41.9 | $26.9 | $17.7 | $12.7 | $4.0 | $3.6 |
| Percent of the Gross National Product | 7.7 | 7.6 | 7.0 | 6.7 | 6.4 | 6.1 | 6.1 | 5.3 | 4.4 | 4.4 | 4.0 | 3.5 |
| Sources of funds in billions | ||||||||||||
| Private expenditures | $51.8 | $47.2 | $40.7 | $36.1 | $32.5 | $32.7 | $30.9 | $20.3 | $13.2 | $9.2 | $3.2 | $3.2 |
| Public expenditures | 31.7 | 27.8 | 24.9 | 22.1 | 19.0 | 13.6 | 11.0 | 6.6 | 4.6 | 3.4 | .8 | .5 |
| Federal expenditures | 20.3 | 17.7 | 16.1 | 14.1 | 11.9 | 7.4 | 5.5 | 3.0 | 2.0 | 1.6 | NA | NA |
| State and local expenditures | 11.4 | 10.1 | 8.9 | 8.0 | 7.0 | 6.1 | 5.5 | 3.6 | 2.6 | 1.8 | NA | NA |
| Per capita expenditures1 | $386 | $350 | $310 | $278 | $248 | $225 | $207 | $146 | $105 | $82 | $30 | $29 |
| Private expenditures | 239 | 221 | 192 | 172 | 157 | 159 | 152 | 110 | 78 | 60 | 24 | 25 |
| Public expenditures | 146 | 130 | 118 | 105 | 91 | 66 | 54 | 36 | 27 | 22 | 6 | 4 |
| Federal expenditures | 94 | 83 | 76 | 67 | 57 | 36 | 27 | 16 | 12 | 10 | NA | NA |
| State and local expenditures | 52 | 47 | 42 | 38 | 34 | 30 | 27 | 20 | 15 | 12 | NA | NA |
| Percent distribution of funds | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Private funds | 62.1 | 63.0 | 62.0 | 62.0 | 63.2 | 70.7 | 73.8 | 75.3 | 74.3 | 72.8 | 79.7 | 86.4 |
| Public funds | 37.9 | 37.0 | 38.0 | 38.0 | 36.8 | 29.3 | 26.2 | 24.7 | 25.7 | 27.2 | 20.3 | 13.6 |
| Federal funds | 24.3 | 23.5 | 24.5 | 24.3 | 23.1 | 16.1 | 13.2 | 11.2 | 11.3 | 12.8 | NA | NA |
| State and local funds | 13.6 | 13.5 | 13.5 | 13.7 | 13.7 | 13.2 | 13.0 | 13.5 | 14.4 | 14.4 | NA | NA |
| Addenda | ||||||||||||
| Gross national product (billions) | $1,077.6 | $992.7 | $944.0 | $873.4 | $799.6 | $756.0 | $691.0 | $506.5 | $400.0 | $286.5 | $100.0 | $103.4 |
| Population in millions | 216.6 | 214.0 | 211.7 | 209.6 | 207.6 | 205.6 | 203.0 | 183.8 | 168.4 | 154.7 | 134.6 | 123.7 |
| Annual percent changes | ||||||||||||
| National health expenditures | 11.4 | 14.2 | 12.7 | 13.1 | 11.2 | 10.3 | 9.3 | 8.7 | 7.0 | 12.2 | .8 | NA |
| Private expenditures | 9.8 | 16.0 | 12.7 | 11.1 | .6 | 5.7 | 8.8 | 9.0 | 7.4 | 11.2 | .1 | NA |
| Public expenditures | 14.1 | 11.3 | 12.8 | 16.6 | 39.8 | 23.4 | 10.6 | 7.8 | 5.8 | 15.5 | 4.6 | NA |
| Federal expenditures | 15.0 | 9.8 | 14.0 | 18.4 | 60.1 | 34.5 | 12.9 | 8.5 | 4.3 | .0 | NA | NA |
| State and local expenditures | 12.5 | 14.0 | 10.8 | 13.6 | 15.1 | 12.1 | 8.5 | 7.2 | 7.0 | 8.4 | NA | NA |
| Gross national product | 8.6 | 5.2 | 8.1 | 9.2 | 5.8 | 9.4 | 6.4 | 4.8 | 6.9 | 11.1 | −.3 | NA |
| Population | 1.2 | 1.1 | 1.0 | 1.0 | 1.0 | 1.2 | 2.0 | 1.8 | 1.7 | 1.4 | .8 | NA |
Based on July 1 social security area population estimates.
NA = Data not available.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
The estimates presented in this article contain several revisions. Revisions to private health insurance benefit and premium levels and to the distribution of those benefits, discussed elsewhere in this issue (Arnett and Trapnell, 1984), have resulted in a substantially larger share of personal health care expenditures paid for by private health insurance. Estimates of total spending for hospital care have been revised upward as well, reflecting a more accurate method of converting fiscal year data to calendar year data. Minor changes have been made in the way public program benefit data are allocated to the types of services consumed. The net effect of these changes has been an overall decrease in the estimated level of direct patient payments, which is calculated as the remainder of total spending after all known third-party payments are deducted, and in the size of direct patient payments in each service category. Finally, official social security area population estimates have been used to calculate spending per capita. Because the figures in this report are based on provider and program aggregate data, per capita figures are an output of, rather than an input to, the estimates. The new population figures differ in concept from those used previously because of the addition of an estimate of the number of people missed by the census of population (Wade, 1984).
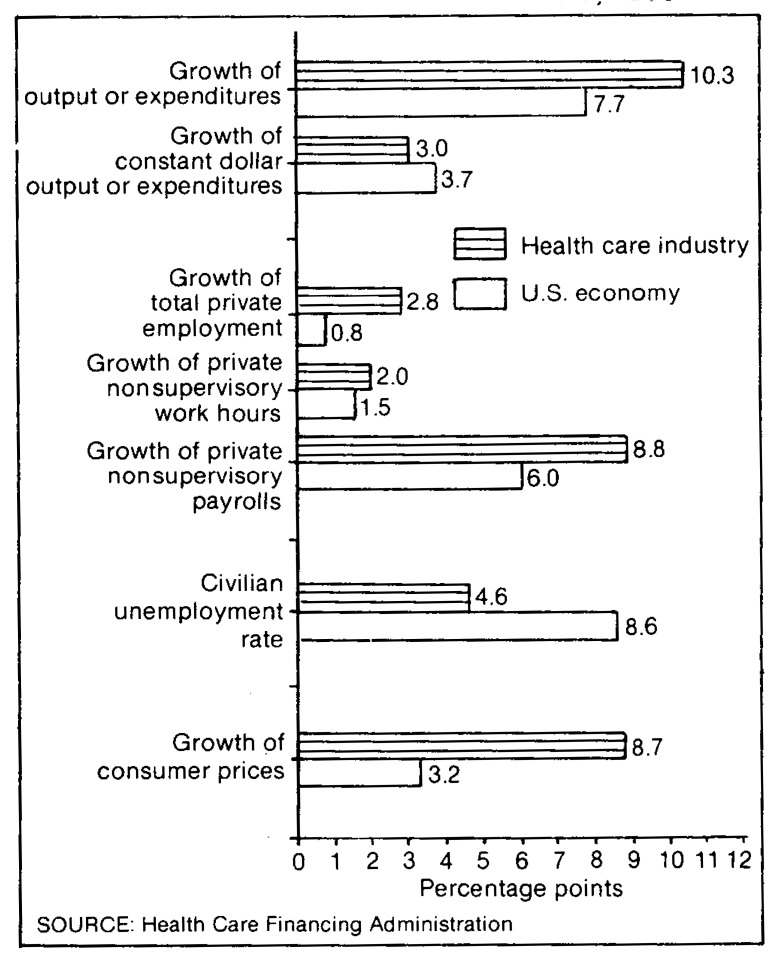
The health delivery industry is among the largest and strongest in the Nation (Figure 3). With over 7.2 million employees in 1983, it ranked second among industries — 1 in the United States in terms of employment or payroll. Output, measured by price-adjusted (“real”) personal health care expenditures, grew slightly less than real GNP, but for only the fourth time since 1966. The dollar value of output, including the effects of inflation, increased more rapidly than the GNP because consumer medical prices grew over 2½ times as fast as general consumer prices did. Employment in the private health industry grew three times as fast as that of the total private nonfarm economy, nonsupervisory work hours grew 1⅓ times as fast, and nonsupervisory payroll grew 1½ times as fast. The unemployment rate for health workers was lower than rates for comparably skilled workers in other areas, averaging somewhat more than half the rate of all experienced workers. All of these details point to a large and strong industry. When viewed over time, the data mentioned above described an industry that has been relatively insulated from the business cycle. Since 1972, nonsupervisory work hours in private health establishments have grown an average of 4.9 percent per year. Except for 1983, growth in a single year varied by no more than 1.7 percentage points from the average. In contrast, growth of non-supervisory work hours in all private nonagricultural establishments averaged 1.2 percent per year, varying in response to the business cycle by as much as 5.7 percentage points in a single year. A similar pattern can be seen in growth of nonsupervisory employment and average weekly earnings: Growth for the private health industry has been higher and has varied less than growth for the aggregate private nonfarm economy since 1972.
Figure 3. Measures of economic activity in the health care industry and in the United States as a whole, 1983.
There are a number of explanations for the difference in growth between health spending and the output of the general economy. First, it is generally accepted that, as an economy matures, consumers desire an increasing proportion of services, such as travel, health care, and dining. Second, economists theorize that industries with slower growing productivity may experience more rapid price inflation than industries with faster growing productivity. Health care, despite recent advances in technology, is still quite labor intensive; productivity growth is low, or even negative by some measures. Third, rapid development and dissemination of medical technology have expanded the treatment of disease to previously unattainable breadth and depth. This has resulted in more consumption of health care per capita, and it may also stimulate price inflation. Competition among providers in local medical markets to offer the latest technology can oversaturate the market and create excess capacity, thus raising costs. Fourth, the population of the United States gradually is aging. Although each age group is healthier than its counterparts in previous decades, one consequence of more older Americans is a need for more health care, because older people require more hospital and nursing-home care, for example, than younger people do (Waldo and Lazenby, 1984).
There are other reasons, financial in nature, for increases in the share of GNP going to health care. Two such reasons are the nature of third-party reimbursement and Government subsidies of health care spending.
Third-party reimbursement, as it has been practiced historically, leads to greater consumption of health care for two reasons. The first reason is that when a third party pays for a service, the act of consumption and the act of paying are separated in time and place: The consumer may not perceive the true cost of the service. Because the perceived price of consumption is lower than the actual price, consumers tend to use more health care services than they would otherwise use. Second, a great deal of third-party reimbursement is “cost based” or “retrospective” in nature. When the insurer pays a large proportion of costs, whatever those costs may be, there is little incentive for consumers or providers of care to be cost conscious. This feature reflects directly the original intent of health insurance, which was to guarantee access to health care regardless of cost. However, with consumption growing more rapidly than the supply of funds from which care is paid for, increasing pressure for reform of the cost-based aspect of third-party reimbursement has culminated in the conversion of part of Medicare to a prospective payment system.
Another important force acting on the financing of health care is the tax treatment of health insurance premiums and out-of-pocket payments for health care. Under current law, employer contributions for health insurance policies (more than three-quarters of the premiums earned by insurance companies in 1983) are excluded from employees' taxable income and from earnings subject to payroll taxes. In addition, until 1983 up to $150 of an employee's share of health insurance premiums could be deducted directly from taxable income. Today, only that part of health insurance premiums and other consumer medical expenses that exceeds 5 percent of adjusted gross income is tax deductible. The tax treatment of premiums alone cost the Federal Government $26 billion in foregone revenue in fiscal year 1983 (Congressional Budget Office, 1982). The tax-exempt status of health insurance premiums encourages employees, and does not discourage employers, to substitute more comprehensive insurance coverage for higher money wages. Many consumers view such expanded coverage as a “use-or-lose” benefit, and they tend to overconsume health care services, despite the fact that overconsumption raises the price of health insurance in the long run. The extensive third-party coverage of health care and the tax treatment of health care spending can be considered financial causes of rising health expenditures.
The broadest Government response to increasing health care expenditures, which comprised 11.9 percent of Federal outlays in 1983, was begun with the introduction of diagnosis-related hospital payments under Medicare, to take effect in stages between fiscal years 1984 and 1986. A hospital knows at the time of admission how much Medicare will pay for treatment of the patient. This form of prospective payment is expected to encourage providers of care to become more cost conscious. Evidence available at this time indicates that Medicare's prospective payment system has resulted in slower growth of spending for hospital care.
Goods and services purchased in 1983
“National health expenditures” are defined to include all spending for health care of individuals, the administrative costs of nonprofit and Government health programs, the net cost to enrollees of private health insurance, Government expenditures through public health programs, noncommercial health research, and construction of medical facilities. The definition excludes spending for environmental improvement and for subsidies and grants for health professional's education, categories which often are categorized with health in Federal budget documents.
National health expenditures are divided into two categories: Health services and supplies—expenditures related to current health—and research and construction of medical facilities—expenditures related to future health (Table 2). Health services and supplies, in turn, consist of personal health care (the direct provision of care), program administration and the net cost of insurance, and Government public health activities.
Table 2. National health expenditures, by type of expenditure: Selected years, 1929-83.
| Type of expenditure | 1983 | 1982 | 1981 | 1980 | 1979 | 1978 | 1977 | 1976 | 1975 | 1974 | 1973 | 1972 | 1971 | 1970 | 1969 | 1968 | 1967 | 1966 | 1965 | 1960 | 1955 | 1950 | 1940 | 1929 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||||||||
| Amount in billions | ||||||||||||||||||||||||
| Total | $355.4 | $322.3 | $285.8 | $248.0 | $215.1 | $190.0 | $170.2 | $150.8 | $132.7 | $116.3 | $103.4 | $93.9 | $83.5 | $75.0 | $65.6 | $58.2 | $51.5 | $46.3 | $41.9 | $26.9 | $17.7 | $12.7 | $4.0 | $3.6 |
| Health services and supplies | 340.1 | 308.1 | 272.7 | 236.1 | 204.6 | 180.2 | 161.0 | 141.8 | 124.3 | 108.9 | 96.5 | 87.4 | 77.4 | 69.6 | 60.8 | 54.1 | 47.6 | 42.6 | 38.4 | 25.2 | 16.9 | 11.7 | 3.9 | 3.4 |
| Personal health care | 313.3 | 284.7 | 253.4 | 219.1 | 189.6 | 167.4 | 149.1 | 132.8 | 117.1 | 101.5 | 89.0 | 80.5 | 72.2 | 65.4 | 57.1 | 50.3 | 44.5 | 39.7 | 35.9 | 23.7 | 15.7 | 10.9 | 3.5 | 3.2 |
| Hospital care | 147.2 | 134.9 | 117.9 | 101.3 | 87.0 | 76.2 | 68.1 | 60.9 | 52.4 | 45.0 | 38.9 | 35.2 | 31.0 | 28.0 | 24.2 | 21.1 | 18.4 | 15.8 | 14.0 | 9.1 | 5.9 | 3.9 | 1.0 | .7 |
| Physicians' services | 69.0 | 61.8 | 54.8 | 46.8 | 40.2 | 35.8 | 31.9 | 27.6 | 24.9 | 21.2 | 19.1 | 17.2 | 15.9 | 14.3 | 12.6 | 11.1 | 10.1 | 9.2 | 8.5 | 5.7 | 3.7 | 2.7 | 1.0 | 1.0 |
| Dentists' services | 21.8 | 19.5 | 17.3 | 15.4 | 13.3 | 11.8 | 10.5 | 9.4 | 8.2 | 7.4 | 6.5 | 5.6 | 5.1 | 4.7 | 4.2 | 3.7 | 3.4 | 3.0 | 2.8 | 2.0 | 1.5 | 1.0 | .4 | .5 |
| Other professional services | 8.0 | 7.1 | 6.4 | 5.6 | 4.7 | 4.1 | 3.6 | 3.2 | 2.6 | 2.2 | 2.0 | 1.8 | 1.6 | 1.6 | 1.5 | 1.4 | 1.3 | 1.2 | 1.0 | .9 | .6 | .4 | .2 | .3 |
| Drugs and medical sundries | 23.7 | 21.8 | 20.5 | 18.5 | 17.1 | 15.4 | 14.1 | 13.0 | 11.9 | 11.0 | 10.1 | 9.3 | 8.6 | 8.0 | 7.1 | 6.4 | 5.8 | 5.5 | 5.2 | 3.7 | 2.4 | 1.7 | .6 | .6 |
| Eyeglasses and appliances | 6.2 | 5.5 | 5.6 | 5.1 | 4.7 | 4.2 | 3.7 | 3.4 | 3.2 | 2.8 | 2.5 | 2.3 | 2.0 | 1.9 | 1.7 | 1.5 | 1.3 | 1.3 | 1.2 | .8 | .6 | .5 | .2 | .1 |
| Nursing home care | 28.8 | 26.5 | 23.9 | 20.4 | 17.4 | 15.1 | 13.0 | 11.3 | 10.1 | 8.5 | 7.2 | 6.5 | 5.6 | 4.7 | 3.8 | 3.4 | 2.8 | 2.4 | 2.1 | .5 | .3 | .2 | .0 | .0 |
| Other health services | 8.5 | 7.6 | 7.0 | 5.9 | 5.1 | 4.8 | 4.2 | 4.0 | 3.8 | 3.3 | 2.7 | 2.6 | 2.3 | 2.1 | 1.9 | 1.7 | 1.5 | 1.5 | 1.1 | 1.1 | .7 | .5 | .1 | .1 |
| Expenses for prepayment and administration | 15.6 | 13.4 | 10.6 | 9.2 | 8.6 | 7.5 | 7.5 | 5.1 | 4.0 | 4.7 | 5.3 | 4.8 | 3.5 | 2.8 | 2.5 | 2.7 | 2.2 | 2.1 | 1.7 | 1.1 | .8 | .5 | .2 | .1 |
| Government public health activities | 11.2 | 10.0 | 8.6 | 7.7 | 6.4 | 5.3 | 4.3 | 3.8 | 3.2 | 2.7 | 2.2 | 2.0 | 1.8 | 1.4 | 1.2 | 1.0 | .9 | .8 | .8 | .4 | .4 | .4 | .2 | .1 |
| Research and construction of medical facilities | 15.3 | 14.2 | 13.2 | 11.9 | 10.4 | 9.8 | 9.2 | 9.0 | 8.4 | 7.5 | 6.8 | 6.6 | 6.1 | 5.4 | 4.8 | 4.1 | 3.8 | 3.7 | 3.5 | 1.7 | .9 | 1.0 | .1 | .2 |
| Research1 | 6.2 | 5.9 | 5.6 | 5.4 | 4.7 | 4.4 | 3.9 | 3.7 | 3.3 | 2.8 | 2.5 | 2.4 | 2.1 | 2.0 | 1.9 | 1.9 | 1.8 | 1.6 | 1.5 | .7 | .2 | .1 | .0 | .0 |
| Construction | 9.1 | 8.3 | 7.6 | 6.5 | 5.7 | 5.3 | 5.3 | 5.3 | 5.1 | 4.7 | 4.3 | 4.2 | 4.0 | 3.4 | 2.9 | 2.3 | 2.1 | 2.1 | 2.0 | 1.0 | .7 | .8 | .1 | .2 |
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but they are included in the expenditure class in which the product falls.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Personal health care
A total of $313 billion was spent for personal health care in 1983 (Table 3), up 10.1 percent from the amount spent in 1982. In 1983, $1,286 was spent per capita for personal health care—an increase of 8.9 percent from the 1982 level.
Table 3. National health expenditures, by type of expenditure and source of funds: Calendar years 1981-83.
| Type of expenditure | Total | Private | Public | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Total | Consumer | Other 1 | Total | Federal | State and local | ||||
|
| |||||||||
| Total | Direct | Insurance | |||||||
|
| |||||||||
| Amount in billions | |||||||||
| 1983 | |||||||||
| Total | $355.4 | $206.6 | $195.7 | $85.2 | $110.5 | $10.9 | $148.8 | $102.7 | $46.1 |
| Health services and supplies | 340.1 | 199.8 | 195.7 | 85.2 | 110.5 | 4.1 | 140.3 | 96.8 | 43.5 |
| Personal health care | 313.3 | 188.8 | 185.2 | 85.2 | 100.0 | 3.7 | 124.5 | 93.0 | 31.5 |
| Hospital care | 147.2 | 68.8 | 67.3 | 11.1 | 56.2 | 1.5 | 78.4 | 60.6 | 17.8 |
| Physicians' services | 69.0 | 49.7 | 49.7 | 19.6 | 30.1 | 3 | 19.3 | 15.6 | 3.7 |
| Dentists' services | 21.8 | 21.2 | 21.2 | 13.9 | 7.4 | --- | .6 | .3 | .3 |
| Other professional services | 8.0 | 5.6 | 5.5 | 3.3 | 2.1 | .1 | 2.5 | 1.9 | .5 |
| Drugs and medical sundries | 23.7 | 21.6 | 21.6 | 18.4 | 3.2 | --- | 2.1 | 1.1 | 1.1 |
| Eyeglasses and appliances | 6.2 | 5.2 | 5.2 | 4.5 | .7 | --- | 1.0 | .9 | .1 |
| Nursing home care | 28.8 | 14.9 | 14.7 | 14.4 | .3 | .2 | 14.0 | 8.1 | 5.9 |
| Other health services | 8.5 | 1.8 | --- | --- | --- | 1.8 | 6.6 | 4.5 | 2.1 |
| Program administration and net cost of insurance | 15.6 | 10.9 | 10.5 | --- | 10.5 | .5 | 4.6 | 2.6 | 2.0 |
| Government public health activities | 11.2 | --- | --- | --- | --- | --- | 11.2 | 1.2 | 10.0 |
| Research and construction of medical facilities | 15.3 | 6.8 | --- | --- | --- | 6.8 | 8.4 | 5.9 | 2.6 |
| Research2 | 6.2 | .4 | --- | --- | --- | .4 | 5.8 | 5.2 | .6 |
| Construction | 9.1 | 6.5 | --- | --- | --- | 6.5 | 2.6 | .7 | 2.0 |
| 1982 | |||||||||
| Total | $322.3 | $186.5 | $176.6 | $77.2 | $99.3 | $9.9 | $135.8 | $93.3 | $42.6 |
| Health services and supplies | 308.1 | 180.4 | 176.6 | 77.2 | 99.3 | 3.8 | 127.8 | 87.6 | 40.1 |
| Personal health care | 284.7 | 171.4 | 168.0 | 77.2 | 90.8 | 3.4 | 113.4 | 84.0 | 29.4 |
| Hospital care | 134.9 | 63.2 | 61.8 | 10.3 | 51.4 | 1.4 | 71.8 | 55.3 | 16.4 |
| Physicians' services | 61.8 | 44.9 | 44.9 | 17.8 | 27.1 | 3 | 16.9 | 13.4 | 3.5 |
| Dentists' services | 19.5 | 18.9 | 18.9 | 12.4 | 6.5 | --- | .6 | .3 | .3 |
| Other professional services | 7.1 | 5.1 | 5.1 | 3.1 | 2.0 | .1 | 2.0 | 1.5 | .5 |
| Drugs and medical sundries | 21.8 | 19.9 | 19.9 | 16.9 | 2.9 | --- | 1.9 | 1.0 | 1.0 |
| Eyeglasses and appliances | 5.5 | 4.7 | 4.7 | 4.1 | .6 | --- | .8 | .7 | .1 |
| Nursing home care | 26.5 | 13.1 | 12.9 | 12.7 | .2 | .2 | 13.4 | 7.7 | 5.7 |
| Other health services | 7.6 | 1.7 | --- | --- | --- | 1.7 | 5.9 | 4.1 | 1.8 |
| Program administration and net cost of insurance | 13.4 | 9.0 | 8.6 | --- | 8.6 | .4 | 4.4 | 2.4 | 1.9 |
| Government public health activities | 10.0 | --- | --- | --- | --- | --- | 10.0 | 1.2 | 8.8 |
| Research and construction of medical facilities | 14.2 | 6.1 | --- | --- | --- | 6.1 | 8.1 | 5.6 | 2.5 |
| Research2 | 5.9 | .3 | --- | --- | --- | .3 | 5.5 | 5.0 | .6 |
| Construction | 8.3 | 5.8 | --- | --- | --- | 5.8 | 2.5 | .6 | 1.9 |
| 1981 | |||||||||
| Total | $285.8 | $164.2 | $155.6 | $70.8 | $84.8 | $8.6 | $121.7 | $83.5 | $38.1 |
| Health services and supplies | 272.7 | 159.0 | 155.6 | 70.8 | 84.8 | 3.4 | 113.7 | 78.1 | 35.6 |
| Personal health care | 253.4 | 152.6 | 149.5 | 70.8 | 78.8 | 3.0 | 100.8 | 74.3 | 26.5 |
| Hospital care | 117.9 | 55.2 | 53.9 | 9.2 | 44.7 | 1.3 | 62.7 | 48.6 | 14.1 |
| Physicians' services | 54.8 | 39.7 | 39.7 | 16.3 | 23.4 | 3 | 15.0 | 11.7 | 3.3 |
| Dentists' services | 17.3 | 16.6 | 16.6 | 10.9 | 5.8 | --- | .7 | .4 | .3 |
| Other professional services | 6.4 | 4.8 | 4.7 | 3.1 | 1.6 | .1 | 1.6 | 1.2 | .4 |
| Drugs and medical sundries | 20.5 | 18.7 | 18.7 | 16.2 | 2.5 | --- | 1.9 | .9 | .9 |
| Eyeglasses and appliances | 5.6 | 4.9 | 4.9 | 4.5 | .5 | --- | .7 | 1.6 | .1 |
| Nursing home care | 23.9 | 11.1 | 10.9 | 10.7 | .2 | .2 | 12.8 | 7.2 | 5.7 |
| Other health services | 7.0 | 1.6 | --- | --- | --- | 1.6 | 5.4 | 3.7 | 1.7 |
| Program administration and net cost of insurance | 10.6 | 6.4 | 6.0 | --- | 6.0 | .4 | 4.2 | 2.5 | 1.7 |
| Government public health activities | 8.6 | --- | --- | --- | --- | --- | 8.6 | 1.3 | 7.3 |
| Research and construction of medical facilities | 13.2 | 5.2 | --- | --- | --- | 5.2 | 8.0 | 5.4 | 2.6 |
| Research2 | 5.6 | .3 | --- | --- | --- | .3 | 5.3 | 4.8 | .5 |
| Construction | 7.6 | 4.8 | --- | --- | --- | 4.8 | 2.7 | .7 | 2.1 |
Spending by philanthropic organizations, industrial inplant health services, and privately financed construction.
Research and development expenditures of drug companies and other manufacturers and providers of medical equipment and supplies are excluded from “research expenditures,” but they are included in the expenditure class in which the product falls.
Less than $50 million.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Third parties account for almost three-quarters of spending for personal health care. Private health insurance benefits amounted to $100 billion in 1983, and other private third-party benefits (philanthropy and industrial inplant health programs) amounted to $4 billion. The Federal Government expended $93 billion, most of it through Medicare and Medicaid; and State and local governments spent $32 billion, about half of which was channeled through Medicaid.
Although price inflation has been moderating, it still accounts for most of the growth in spending for personal health care. As shown in Figure 4, 70 percent of the increase in spending between 1982 and 1983 was due to price inflation; another 11 percent was due to population growth. The remainder was due to a variety of influences, among them the aging of the population, increased consumption per capita, and changes in the types of services provided.
Figure 4. Factors in the increase of personal health care expenditures, 1982-1983.
Personal health care consists of a number of different goods and services.
Physicians' services
Physicians are the most influential group in determining the size and shape of the health care sector. They affect personal health care expenditures much more than is indicated by the 22-percent share of spending devoted to their services. By some estimates, they influence 70 to 80 percent of health care spending (Blumberg, 1979; Somers and Somers, 1977). Physicians play a dominant role in determining who will be hospitalized and what type and quantity of services the hospital patient will receive; expenditures for prescription drugs are influenced similarly.
Expenditures for physicians' services reached $69 billion in 1983—an increase of 11.7 percent from the previous year. This spending accounted for 22.0 percent of personal health care expenditures and for 19.4 percent of all national health expenditures.
Third parties play a large role in the financing of physicians' services. The Federal Government financed slightly less than a quarter of such spending, 23 percent, and private health insurance benefits financed 44 percent of the total. State and local governments paid for 5 percent of the total; and the balance, some 28 percent, is assumed to have been paid by patients or their families.
Price inflation was a significant contributor to the growth of expenditures for physicians' services. Measured by the Consumer Price Index (CPI) physicians' fees rose 7.7 percent in 1983, compared with an increase of 3.2 percent in the CPI for all items.
Existing data convey differing implications concerning growth in the use of physicians' services. Physician visit data, available through 1981, indicate a slight long-run decline in visits per capita (National Center for Health Statistics: data from the Health Interview Survey). The number of surgical operations performed in community hospitals rose very little—0.5 percent in 1983, half the rate of growth of the population—and the number of inpatient days—presumably correlated with physician inpatient contacts—dropped 2.5 percent (American Hospital Association: data from the National Hospital Panel Survey). On the other hand, the decline in inpatient contacts probably has been offset by an increase in office-based contacts. As evidence, nonsupervisory work hours in offices of physicians and surgeons rose 5.7 percent in 1983 (Bureau of Labor Statistics: data from the Establishment Survey), data consistent with greater office activity. Part of the work hours growth may be due to the activity of physician-operated freestanding emergency and outpatient surgery centers; but the data suggest, nonetheless, a strong increase in physician contact outside the hospital.
In the National Health Accounts—the framework within which these estimates fit—expenditures for physician's services encompass the cost of all services and supplies provided in physicians' offices, the cost for services of private practitioners in hospitals and other institutions, and the cost of diagnostic work performed in independent clinical laboratories. The salaries of staff physicians are counted with expenditures for the services of the employing institution.
Hospital care
Expenditures for hospital care in 1983 were $147 billion—an increase of 9.1 percent from 1982. Hospital care accounted for 47.0 percent of the total personal health care expenditures and for 41.4 percent of the national health expenditures. The Federal Government paid for 41.1 percent of hospital care in 1983, private health insurance paid for 38.2 percent, and State and local governments paid for 12.1 percent. Thus, patients paid just 7.5 percent of the cost of hospital care directly.
Data on use of community hospitals (which account for over 80 percent of hospital spending) show a shift from inpatient to outpatient settings. Admissions were 0.5 percent lower in 1983 than in 1982, and inpatient days dropped 2.5 percent. By contrast, clinic visits rose 6.1 percent from 1982 to 1933, and other nonemergency outpatient visits increased 4.1 percent (American Hospital Association: data from the National Hospital Panel Survey).
Three-quarters of the increase in hospital spending between 1982 and 1983 was due to price inflation. General (economy-wide) inflation measured by the gross national product fixed-weight price index accounted for half of the increase; hospital price inflation over and above the general rate accounted for another quarter. Hospital-specific inflation measured by Health Care Financing Administration's National Hospital Input Price Index (Freeland, Anderson, and Schendler, 1979) dropped to 6.4 percent in 1983, the lowest rate in the last 10 years but still higher than the general rate of inflation.
The remaining quarter of the increase in hospital spending is attributable to population growth and to residual factors. The latter category—which includes such effects as the aging of the population, changes in the mix of hospital services provided, and changes in the amounts and mix of goods and services used to provide those services—accounted for 16 percent of the growth in spending.
In the National Health Accounts, hospital care includes all inpatient and outpatient care in public and private hospitals and all services and supplies provided by hospitals. Except for the services of hospital staff physicians, expenditures for physician care provided in hospitals are included in the physician category described above.
Nursing home care
In 1983, $29 billion was spent for nursing home care—an increase of 8.8 percent from the previous year. Such care amounted to 8.1 percent of total health spending and to 9.2 percent of personal health care expenditures.
In the National Health Accounts, nursing home services are those provided in skilled nursing facilities, in intermediate care facilities, and in personal care homes that provide nursing care. In addition, a majority of the care for mentally retarded Medicaid recipients provided in what are designated “intermediate care facilities for the mentally retarded” (ICFMR) is included as nursing home care. Nursing type care provided in hospitals (including ICFMR care) is included with expenditures for hospital care.
Part of the growth in spending for nursing home care is due to the rapid expansion in intermediate care facilities for the mentally retarded, a Medicaid benefit first offered in 1972. Currently, about $2.4 billion (60 percent of the total expenditures for ICFMR) is spent in nursing homes. ICFMR growth has been very rapid, averaging almost 40 percent per year since its inception. Despite its relatively small size and a slowing of growth in recent years, it continues to raise the growth rate of the total nursing home aggregate.
Growth in spending for nursing home care other than ICFMR has slowed considerably in recent years. Part of this slowdown is due to a deceleration of prices paid by nursing home: Health Care Financing Administration's National Nursing Home Input Price Index rose 5.8 percent in 1983, the smallest increase in the last 10 years. The share of nursing home care financed by public programs has declined since 1979, from 56 percent to 48 percent. Almost all of that decline was in Medicaid and Medicare shares. Reduced utilization of nursing home care by Medicaid and Medicare patients has been occurring. The explanation for this reduction is twofold. First, the shortage of nursing home beds in some areas allows nursing homes to selectively admit patients (Feder and Scanlon, 1981). Higher-paying private patients will be admitted before Medicaid or Medicare patients. This results in a large number of days spent in hospitals while patients await discharge to nursing homes. Second, the shortage of beds may be purposely induced in some States in order to minimize Medicaid expenditures. Tactics used by States include tightening of certificate of need requirements and keeping reimbursement rates low (Weissert, et al., 1984). Potential investors in the nursing home business may be discouraged by the low profitability of the industry, due primarily to these reimbursement policies. However, despite the reduction in spending by the public sector, and even excluding the effects of price inflation, constant dollar expenditures grew 2.9 percent in 1983; this was about the same rate of growth as for the population aged 75 years or over.
Drugs and medical sundries
This category, for which $24 billion was spent in 1983 (accounting for 7.6 percent of personal health care expenditures), includes spending for prescription drugs, over-the-counter drugs, and medical sundries dispensed through retail channels. Expenditures for drugs purchased or dispensed by hospitals, physicians, nursing homes, and other institutions and practitioners are counted elsewhere.
Spending for drugs and sundries is financed mostly by consumers directly: Of the $24 billion spent in 1983, $18 billion (or three-quarters of the total) was financed that way. Private health insurance paid approximately $3 billion, and Federal and State or local governments each paid about $1 billion.
Drug therapy constitutes a significant factor in the treatment of illness. An estimated 58 percent of the noninstitutionalized population received at least one prescription for medication in 1977 (Kasper, 1982). About 57 percent of all dollars spent for drugs and medical sundries is estimated to be spent for prescription drugs alone, and 31 percent is estimated to be spent for over-the-counter drug products.
Historically, spending for drugs and sundries has increased at a rate significantly below that of other health care goods and services. Over the last 10 years, for example, such spending increased 9.0 percent per year, compared with an annual growth of 13.4 percent in total personal health care spending.
Part of this phenomenon is due to a relatively low rate of price inflation for drugs. From 1964 to 1968, the Consumer Price Index (CPI) for prescription drugs actually declined, and it was not until 1974 that it recovered its 1964 level. From 1974 to 1980, the CPI for prescription drugs rose 7.0 percent per year, and from 1980 to 1983 it rose 11.4 percent annually.
Another reason drug spending has grown more slowly than spending for other forms of health care is that the amount of third-party coverage is much lower in this area. Private health insurance covered 13.6 percent of drug and sundry expenditures in 1983, and Government covered another 9 percent. These figures are far less than the 31.9 and 39.7 percent, respectively, of total personal health care spending financed by private insurance and by Government. One consequence of this greater reliance upon direct consumer financing is that spending varies with consumer purchasing power. Price-adjusted spending for drugs and sundries declined during the recent recession, and it has not yet returned to its 1979 level.
Other personal health care goods and services
Expenditures for all other types of personal health care goods and services were $44.5 billion in 1983—an increase of 12.1 percent. That spending amounted to 14 percent of all personal health care expenditures and to 13 percent of national health expenditures. Almost equal proportions of this group of services were financed through Government programs (24 percent) and private health insurance (23 percent) in 1983; consumers paid for 49 percent directly. Almost half of the expenditures in this category were for dentist's services, but the category also includes spending for services of other health professionals (including most home health agencies), for eyeglasses and orthopedic appliances, and for other health services (including the provision of care in industrial settings and school health). Growth of this composite component was influenced significantly by the growth of spending for dentists' services and, to some extent, by the growth of spending for other professional services.
Spending for dentists' services, which reached $22 billion in 1983, increased not only because of price inflation but also because of recent increases in the extent of third-party dental coverage. Traditionally, use of dental services fluctuated with the business cycle. However, despite a 12-percent increase in the CPI for dental care in 1980 and the recent economic recession, “price-deflated” expenditures per capita for dental services increased 4 percent per year between 1978 and 1983. This departure from tradition reflects the increased extent of third-party dental coverage. For example, private health insurance, which covered 1 percent of dental services in 1965, paid for one-third of all services received in 1983.
Other health services and supplies
The cost of operating third-party programs in 1983 rose 16.6 percent, to $15.6 billion. This estimate includes $4.6 billion in administrative expenses for those public programs that identified administrative expenses. Administrative costs associated with operating the Medicare and Medicaid programs amounted to $3.1 billion in 1983. Administrative expenses also included a small amount estimated to be the fundraising and administrative expenses of philanthropic organizations. The largest part of the component is the net cost of private health insurance, the difference between earned premiums and incurred claims. Estimated at $10.5 billion for 1983, net cost reflects administrative expenses, additions to loss reserves, and profits or losses of Blue Cross and Blue Shield plans, mutual and stock carriers, and prepaid and self-insured health plans.
Public health activities of various levels of Government amounted to $11.2 billion in 1983. Public health activities are those functions carried out by Federal, State, and local governments to support community health, in contrast with care delivered to individuals. Federal expenditures of $1.2 billion included the services of the Centers for Disease Control and the Food and Drug Administration, as well as grants to States.
Other National health expenditures
National health expenditures devoted to nonprofit research and to construction of medical facilities were $15 billion in 1983, an amount equal to 4.3 percent of total health spending.
Expenditures for noncommercial health care research and development were $6.2 billion in 1983. The Federal Government financed by far the largest amount for research, with funds totaling $5.2 billion, most of which was spent by the National Institutes of Health. Expenditures by State and local governments, exclusive of Federal grants, were $588 million, and private philanthropy funded an even smaller amount.
The $6.2 billion in spending for research in the National Health Accounts excludes research performed by drug companies and by other manufacturers and suppliers of health care goods and services, estimated to be $4 billion in 1983. As this type of research is treated as a business expense and is financed through sales of goods or services, its dollar value is implicitly included in personal health care expenditures; to include it again in this line would result in double counting.
Of the $9.1 billion spent on construction of medical facilities in 1983, 29 percent was funded from public sources. Grants from philanthropic organizations funded 4 percent, and the remainder came from internal funds or from the private capital market. This estimate does not include spending for capital equipment, because there is no source of data to yield a reliable, consistent time series of data on spending for equipment.
Financing health care
Health care can be financed directly by the consumer through out-of-pocket payments. Alternatively, consumers can reduce the risk of incurring major medical costs by acquiring third-party coverage. The third party may act as the financial intermediary between the health provider and the consumer of health care, or may reimburse the consumer for the cost of care, or may hire the provider of care. In any case, an insured consumer pays less or none of the cost of care at the time of service.
The health care market differs from the perfect market for goods and services depicted in standard economic theory. First, it is dominated by third-party payers: In 1983, 73 percent of personal health care expenditures were made by the Government or by private health insurance. Second, unlike most other markets, the consumers of health care lack full information when decisions are made to purchase health care. For example, hospital admission is usually made on the decision of a seller of health care (a physician) rather than by the consumer of hospital services (the patient), or by the purchaser of the service (the Government, private health insurers, or the patient). Whether the patient with complete information would choose the same types and quantities of care is an issue yet to be answered empirically. To the extent that the patient would not make the same choices, the industry plays a role in determining its “sales.”
A corollary to these theories is that the absence of the “usual” market forces that limit health care expenditures may generate political (nonmarket) bargaining between payers and providers. Where the Government is the payer, this takes the form of regulations or ratesetting (Feder and Spitz, 1980). In practice, those parts of the health care sector for which Government pays the highest proportion of costs (hospitals, for example) are also parts of the sector with the greatest degree of cost regulation.
Third-party financing
Unlike other goods or services for which the consumer pays the provider directly, health care payments often are handled by a financial agent—a “third party.” The details of the payment method may vary: The consumer may pay the provider and apply for reimbursement from the third party, or the provider may bill the third party directly, or the provider may be employed by the third party (as in the case of U.S. Department of Defense hospitals or industrial inplant services, for example). In the case of Medicare, institutional providers bill “financial intermediaries”—private health insurers acting as agents for the Federal Government—and physicians may bill either the financial intermediary or the patient.
The existing third-party coverage of health care may have contributed to a healthier population, but it has exacted a price as well. Insurance has increased access to care, resulting in treatment of patients who had been shut out of the orthodox medical market by price considerations. However, the historical structure of insurance benefits encourages use of inpatient rather than outpatient facilities, and it encourages overuse of tests and procedures rather than underuse. The financial incentives embedded in traditional reimbursement structures may encourage effective medical care, but not necessarily at the lowest cost.
Private health insurance
Blue Cross and Blue Shield plans, commercial insurance companies, and prepaid and self-insured plans paid an estimated $100 billion in medical benefits in 1983, an amount equal to 31.9 percent of personal health care expenditures. These benefit payments were 10.2 percent higher than the 1982 payments of $91 billion. Insurers received an estimated $110 billion in premiums, 56.5 percent of all consumer spending for health, resulting in a net cost to enrollees over $10.5 billion. The 1982 premiums and net cost were $99 billion and $8.6 billion, respectively.
The 1982 levels for insurance are substantially higher than those previously published (Table 4). The major source of revision stems from a new treatment of self-insured and insurance company data. New information, particularly new preliminary estimates of third-party administrator business, has also been incorporated. These revisions are discussed in detail elsewhere in this issue (Arnett and Trapnell, 1984).
Table 4. Revisions to private health insurance estimates.
| Year | Current estimates | Previously published | Difference | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Premiums | Benefits | Premiums | Benefits | Premiums | Benefits | |
|
| ||||||
| Amount in billions | ||||||
| 1965 | $10.0 | $8.7 | $10.0 | $8.7 | $ 0.0 | $0.0 |
| 1970 | 16.9 | 15.3 | 17.1 | 15.6 | −.2 | −.3 |
| 1975 | 33.2 | 31.2 | 32.4 | 30.1 | .8 | 1.1 |
| 1976 | 40.4 | 37.6 | 38.2 | 35.5 | 2.2 | 2.1 |
| 1977 | 48.0 | 43.0 | 44.6 | 40.0 | 3.4 | 3.0 |
| 1978 | 53.6 | 49.1 | 49.7 | 45.0 | 3.9 | 4.1 |
| 1979 | 62.0 | 56.9 | 55.9 | 50.2 | 6.1 | 6.7 |
| 1980 | 72.5 | 67.3 | 63.6 | 57.0 | 8.9 | 10.3 |
| 1981 | 84.8 | 78.8 | 73.2 | 66.8 | 11.6 | 12.0 |
| 1982 | 99.3 | 90.8 | 84.2 | 76.6 | 15.1 | 14.2 |
| 1983 | 110.5 | 100.0 | --- | --- | --- | --- |
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
The size of the private health insurance industry has been growing, reflecting the perceived desire for its services. By 1983, 53 percent of private expenditures for personal health care—the amount not covered by public programs—was reimbursed by private insurance. In 1982, three-quarters of the U.S. population was covered by private health insurance for hospital care, compared with one-half in 1950. The relatively rapid rate of growth of insurance premiums—14 percent per year since 1950, compared with an increase of 11 percent in total personal health care expenditures—reflects the desire for the prepayment and risk-sharing offered by private health insurance. Only a handful of the population has the financial resources to pay directly and fully for the medical costs of a major illness (Falk, et al., 1933).
Self-insured plans have been growing during the latter half of the seventies (Table 5). This growth has been stimulated by tax and other financial advantages to employers. Insurance companies have also contributed to this growth by providing administrative and stop-loss services that aid and protect self-insured plans. The prepaid plans category, comprised of health maintenance organizations and single-service plans, has also grown significantly in recent years, but it still remains a small part of overall insurance.
Table 5. Private health insurance benefits and percent distribution by type of insurer: United States, selected years 1965-83 (Amount in billions).
| Year | Total private health insurance1 | Insurance companies2 | Blue Cross and Blue Shield | Self-insured plans3 | Prepaid plans4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| Amount | Percent | Amount | Percent | Amount | Percent | Amount | Percent | Amount | Percent | |
| 1965 | $ 8.7 | 100.0 | $4.2 | 48.4 | $3.9 | 45.2 | $.3 | 3.9 | $.2 | 2.6 |
| 1970 | 15.3 | 100.0 | 7.1 | 46.4 | 7.0 | 46.1 | .7 | 4.3 | .5 | 3.2 |
| 1975 | 31.2 | 100.0 | 12.8 | 41.1 | 14.2 | 45.5 | 3.0 | 9.6 | 1.2 | 3.8 |
| 1976 | 37.6 | 100.0 | 15.0 | 39.8 | 16.2 | 43.2 | 4.9 | 13.2 | 1.5 | 3.9 |
| 1977 | 43.0 | 100.0 | 16.4 | 38.3 | 17.8 | 41.5 | 6.8 | 15.9 | 1.9 | 4.3 |
| 1978 | 49.1 | 100.0 | 19.1 | 38.8 | 19.5 | 39.7 | 8.3 | 16.9 | 2.3 | 4.6 |
| 1979 | 56.9 | 100.0 | 21.8 | 38.4 | 21.7 | 38.2 | 10.5 | 18.5 | 2.8 | 5.0 |
| 1980 | 67.3 | 100.0 | 25.6 | 38.0 | 25.5 | 37.8 | 12.7 | 18.8 | 4.4 | 5.6 |
| 1981 | 78.8 | 100.0 | 30.6 | 38.8 | 29.2 | 37.1 | 14.5 | 18.5 | 4.4 | 5.6 |
| 1982 | 90.8 | 100.0 | 37.1 | 40.9 | 32.1 | 35.4 | 16.2 | 17.8 | 5.3 | 5.9 |
| 1983 | 100.0 | 100.0 | 41.3 | 41.3 | 35.2 | 35.2 | 17.4 | 17.4 | 6.1 | 6.1 |
Detail may not add to totals because of rounding.
Includes minimum premium plans (MPP).
Includes administrative service only (ASO) plans.
Includes health maintenance organizations and other prepaid plans such as dental and vision.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
The advent of Medicare and Medicaid slowed the growth of the private health insurance share of personal health care expenditures. Private health insurance share of spending doubled between 1950 and 1965, reaching 24 percent (Table 6). Since 1967, this share has grown gradually, increasing to 32 percent in 1983. The change results from an increased breadth of services covered and an increasing depth of coverage in hospital and physician services, as well as increasing enrollment through 1977. By 1983, private health insurance was paying $100 billion in health benefits.
Table 6. Aggregate and per capita amount and percent distribution of personal health care expenditures, by source of funds: Selected years 1929-83.
| Year | Total | Patient direct payments | All third parties | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Total | Private | Public | ||||||
|
|
|
|||||||
| Health Insurance | Other | Total | Federal | State and local | ||||
| Amount in billions | ||||||||
| 1929 | $3.2 | $2.8 | $.4 | 1 | $.1 | $.3 | $.1 | $.2 |
| 1935 | 2.7 | 2.2 | .5 | 1 | .1 | .4 | .1 | .3 |
| 1940 | 3.5 | 2.9 | .7 | 1 | .1 | .6 | .1 | .4 |
| 1950 | 10.9 | 7.1 | 3.8 | $.9 | .3 | 2.4 | 1.1 | 1.3 |
| 1955 | 15.7 | 9.1 | 6.6 | 2.5 | .4 | 3.6 | 1.6 | 2.0 |
| 1960 | 23.7 | 13.0 | 10.7 | 5.0 | .5 | 5.2 | 2.2 | 3.0 |
| 1965 | 35.9 | 18.5 | 17.3 | 8.7 | .8 | 7.9 | 3.6 | 4.3 |
| 1966 | 39.7 | 19.6 | 20.0 | 9.1 | .8 | 10.1 | 5.3 | 4.9 |
| 1967 | 44.5 | 19.0 | 25.5 | 9.6 | .8 | 15.1 | 9.5 | 5.6 |
| 1968 | 50.3 | 20.7 | 29.6 | 10.9 | .9 | 17.8 | 11.4 | 6.4 |
| 1969 | 57.1 | 23.0 | 34.0 | 12.9 | .9 | 20.2 | 13.2 | 7.0 |
| 1970 | 65.4 | 26.5 | 38.9 | 15.3 | 1.1 | 22.4 | 14.5 | 7.9 |
| 1971 | 72.2 | 28.1 | 44.1 | 17.2 | 1.3 | 25.6 | 16.8 | 8.8 |
| 1972 | 80.5 | 30.6 | 49.9 | 19.0 | 2.0 | 28.8 | 18.9 | 9.9 |
| 1973 | 89.0 | 33.3 | 55.7 | 21.4 | 2.2 | 32.1 | 21.1 | 11.1 |
| 1974 | 101.5 | 35.8 | 65.6 | 25.1 | 1.5 | 39.0 | 26.3 | 12.7 |
| 1975 | 117.1 | 38.0 | 79.1 | 31.2 | 1.6 | 46.3 | 31.4 | 14.9 |
| 1976 | 132.8 | 42.0 | 90.8 | 37.6 | 1.8 | 51.4 | 36.1 | 15.3 |
| 1977 | 149.1 | 46.4 | 102.7 | 43.0 | 2.0 | 57.8 | 41.0 | 16.8 |
| 1978 | 167.4 | 50.6 | 116.7 | 49.1 | 2.1 | 65.6 | 46.4 | 19.2 |
| 1979 | 189.6 | 55.8 | 133.8 | 56.9 | 2.3 | 74.6 | 53.3 | 21.2 |
| 1980 | 219.1 | 62.5 | 156.7 | 67.3 | 2.6 | 86.7 | 62.5 | 24.2 |
| 1981 | 253.4 | 70.8 | 182.6 | 78.8 | 3.0 | 100.8 | 74.3 | 26.5 |
| 1982 | 284.7 | 77.2 | 207.5 | 90.8 | 3.4 | 113.4 | 84.0 | 29.4 |
| 1983 | 313.3 | 85.2 | 228.1 | 100.0 | 3.7 | 124.5 | 93.0 | 31.5 |
| Per capita amount2 | ||||||||
| 1929 | $26 | $23 | $3 | 1 | $1 | $2 | $1 | $2 |
| 1935 | 21 | 17 | 4 | 1 | 1 | 3 | 1 | 2 |
| 1940 | 26 | 21 | 5 | 1 | 1 | 4 | 1 | 3 |
| 1950 | 70 | 46 | 24 | $6 | 2 | 16 | 7 | 8 |
| 1955 | 93 | 54 | 39 | 15 | 3 | 21 | 10 | 12 |
| 1960 | 129 | 71 | 58 | 27 | 3 | 28 | 12 | 16 |
| 1965 | 177 | 91 | 85 | 43 | 4 | 39 | 18 | 21 |
| 1966 | 193 | 95 | 98 | 44 | 4 | 49 | 26 | 24 |
| 1967 | 214 | 91 | 123 | 46 | 4 | 73 | 46 | 27 |
| 1968 | 240 | 99 | 141 | 52 | 4 | 85 | 54 | 30 |
| 1969 | 270 | 109 | 161 | 61 | 4 | 95 | 62 | 33 |
| 1970 | 305 | 124 | 182 | 72 | 5 | 105 | 68 | 37 |
| 1971 | 333 | 130 | 203 | 79 | 6 | 118 | 77 | 41 |
| 1972 | 368 | 140 | 228 | 87 | 9 | 132 | 87 | 45 |
| 1973 | 403 | 151 | 252 | 97 | 10 | 146 | 95 | 50 |
| 1974 | 456 | 161 | 295 | 113 | 7 | 175 | 118 | 57 |
| 1975 | 521 | 169 | 352 | 139 | 7 | 206 | 140 | 66 |
| 1976 | 586 | 185 | 400 | 166 | 8 | 227 | 159 | 67 |
| 1977 | 651 | 203 | 449 | 188 | 9 | 253 | 179 | 74 |
| 1978 | 724 | 219 | 505 | 212 | 9 | 283 | 201 | 83 |
| 1979 | 811 | 239 | 572 | 243 | 10 | 319 | 228 | 91 |
| 1980 | 927 | 264 | 663 | 285 | 11 | 367 | 265 | 102 |
| 1981 | 1062 | 297 | 765 | 330 | 13 | 422 | 311 | 111 |
| 1982 | 1181 | 320 | 861 | 377 | 14 | 470 | 348 | 122 |
| 1983 | 1286 | 350 | 936 | 410 | 15 | 511 | 382 | 129 |
| Percent distribution | ||||||||
| 1929 | 100.0 | 88.4 | 11.6 | 1 | 2.6 | 9.0 | 2.7 | 6.3 |
| 1935 | 100.0 | 82.4 | 17.6 | 1 | 2.8 | 14.7 | 3.4 | 11.3 |
| 1940 | 100.0 | 81.3 | 18.7 | 1 | 2.6 | 16.1 | 4.1 | 12.0 |
| 1950 | 100.0 | 65.5 | 34.5 | 9.1 | 2.9 | 22.4 | 10.4 | 12.0 |
| 1955 | 100.0 | 58.1 | 41.9 | 16.1 | 2.8 | 23.0 | 10.5 | 12.5 |
| 1960 | 100.0 | 54.9 | 45.1 | 21.1 | 2.3 | 21.8 | 9.3 | 12.5 |
| 1965 | 100.0 | 51.6 | 48.4 | 24.2 | 2.2 | 22.0 | 10.1 | 11.9 |
| 1966 | 100.0 | 49.5 | 50.5 | 22.9 | 2.1 | 25.5 | 13.2 | 12.3 |
| 1967 | 100.0 | 42.6 | 57.4 | 21.6 | 1.9 | 33.9 | 21.3 | 12.6 |
| 1968 | 100.0 | 41.2 | 58.8 | 21.7 | 1.8 | 35.3 | 22.6 | 12.7 |
| 1969 | 100.0 | 40.4 | 59.6 | 22.7 | 1.6 | 35.3 | 23.1 | 12.3 |
| 1970 | 100.0 | 40.5 | 59.5 | 23.4 | 1.7 | 34.3 | 22.2 | 12.1 |
| 1971 | 100.0 | 38.9 | 61.1 | 23.8 | 1.8 | 35.5 | 23.2 | 12.3 |
| 1972 | 100.0 | 38.0 | 62.0 | 23.6 | 2.5 | 35.8 | 23.5 | 12.3 |
| 1973 | 100.0 | 37.4 | 62.6 | 24.0 | 2.5 | 36.1 | 23.7 | 12.4 |
| 1974 | 100.0 | 35.3 | 64.7 | 24.8 | 1.5 | 38.4 | 25.9 | 12.6 |
| 1975 | 100.0 | 32.5 | 67.5 | 26.7 | 1.3 | 39.5 | 26.8 | 12.7 |
| 1976 | 100.0 | 31.6 | 68.4 | 28.3 | 1.4 | 38.7 | 27.2 | 11.5 |
| 1977 | 100.0 | 31.1 | 68.9 | 28.8 | 1.3 | 38.8 | 27.5 | 11.3 |
| 1978 | 100.0 | 30.3 | 69.7 | 29.3 | 1.2 | 39.2 | 27.7 | 11.5 |
| 1979 | 100.0 | 29.4 | 70.6 | 30.0 | 1.2 | 39.3 | 28.1 | 11.2 |
| 1980 | 100.0 | 28.5 | 71.5 | 30.7 | 1.2 | 39.6 | 28.5 | 11.0 |
| 1981 | 100.0 | 27.9 | 72.1 | 31.1 | 1.2 | 39.8 | 29.3 | 10.4 |
| 1982 | 100.0 | 27.1 | 72.9 | 31.9 | 1.2 | 39.8 | 29.5 | 10.3 |
| 1983 | 100.0 | 27.2 | 72.8 | 31.9 | 1.2 | 39.7 | 29.7 | 10.1 |
Included with direct payments; separate data not available.
Based on July 1 social security area population estimates.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
A large proportion of spending for hospital care and physicians' services is paid by private health insurance. In 1960, private insurance paid for 36 percent of hospital care, the first type of service to be covered extensively; that share reached 41 percent by 1965 (Table 7). When Medicare and Medicaid were established in 1966, hospital care spending increased dramatically, and the portion paid by private insurance, while growing in dollar terms, dropped to less than 34 percent by 1967. Since 1967, the insurance share of hospital financing has grown to 38 percent because consumers have sought more depth in their hospital coverage. In 1967, patient direct payments financed 10.6 percent of all hospital expenditures. By 1983, however, these payments had declined to 7.5 percent because private insurance picked up an increasing proportion of the expenditures. Extension of coverage beyond surgical procedures in recent years has led to a higher share of physicians' services being reimbursed by private insurance. This share rose from 31 percent in 1965 to 44 percent in 1983 (Table 8).
Table 7. Aggregate and per capita amount and percent distribution of expenditures for hospital care, by source of funds: Selected years 1950-83.
| Year | Total | Patient direct payments | All third parties | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Total | Private | Public | ||||||
|
|
|
|||||||
| Health insurance | Other | Total | Federal | State and local | ||||
| Amount in billions | ||||||||
| 1950 | $ 3.9 | $ 1.2 | $ 2.7 | $ .7 | $ .1 | $ 1.9 | 1 | 1 |
| 1955 | 5.9 | 1.3 | 4.6 | 1.7 | .2 | 2.7 | 1 | 1 |
| 1960 | 9.1 | 1.8 | 7.3 | 3.3 | .2 | 3.8 | 1 | 1 |
| 1965 | 14.0 | 2.3 | 11.6 | 5.7 | .3 | 5.6 | $ 2.4 | $ 3.1 |
| 1966 | 15.8 | 2.6 | 13.2 | 6.0 | .3 | 6.9 | 3.5 | 3.4 |
| 1967 | 18.4 | 1.9 | 16.4 | 6.2 | .3 | 10.0 | 6.3 | 3.7 |
| 1968 | 21.1 | 2.3 | 18.8 | 7.0 | .4 | 11.5 | 7.3 | 4.1 |
| 1969 | 24.2 | 2.6 | 21.6 | 8.2 | .3 | 13.1 | 8.5 | 4.6 |
| 1970 | 28.0 | 3.2 | 24.8 | 9.7 | .4 | 14.7 | 9.5 | 5.1 |
| 1971 | 31.0 | 3.1 | 27.9 | 10.9 | .5 | 16.5 | 10.9 | 5.6 |
| 1972 | 35.2 | 3.5 | 31.7 | 11.8 | 1.2 | 18.6 | 12.4 | 6.2 |
| 1973 | 38.9 | 3.9 | 35.0 | 13.1 | 1.4 | 20.6 | 13.7 | 6.9 |
| 1974 | 45.0 | 4.6 | 40.5 | 15.1 | .6 | 24.7 | 17.0 | 7.7 |
| 1975 | 52.4 | 4.1 | 48.3 | 18.8 | .6 | 28.9 | 20.2 | 8.8 |
| 1976 | 60.9 | 5.1 | 55.7 | 22.5 | .7 | 32.5 | 23.7 | 8.8 |
| 1977 | 68.1 | 5.4 | 62.8 | 25.5 | .7 | 36.6 | 27.0 | 9.6 |
| 1978 | 76.2 | 5.5 | 70.7 | 28.6 | .8 | 41.3 | 30.4 | 10.9 |
| 1979 | 87.0 | 6.4 | 80.6 | 33.0 | .9 | 46.7 | 34.9 | 11.8 |
| 1980 | 101.3 | 7.5 | 93.8 | 38.6 | 1.0 | 54.2 | 41.1 | 13.1 |
| 1981 | 117.9 | 9.2 | 108.7 | 44.7 | 1.3 | 62.7 | 48.6 | 14.1 |
| 1982 | 134.9 | 10.3 | 124.6 | 51.4 | 1.4 | 71.8 | 55.3 | 16.4 |
| 1983 | 147.2 | 11.1 | 136.1 | 56.2 | 1.5 | 78.4 | 60.6 | 17.8 |
| Percent distribution | ||||||||
| 1950 | 100.0 | 29.9 | 70.1 | 17.7 | 3.5 | 48.9 | 1 | 1 |
| 1955 | 100.0 | 22.3 | 77.7 | 28.5 | 3.0 | 46.2 | 1 | 1 |
| 1960 | 100.0 | 19.8 | 80.2 | 36.3 | 2.5 | 41.3 | 1 | 1 |
| 1965 | 100.0 | 16.8 | 83.2 | 41.1 | 2.2 | 39.9 | 17.4 | 22.5 |
| 1966 | 100.0 | 16.4 | 83.6 | 37.7 | 2.0 | 43.8 | 22.4 | 21.4 |
| 1967 | 100.0 | 10.6 | 89.4 | 33.5 | 1.6 | 54.3 | 34.2 | 20.1 |
| 1968 | 100.0 | 10.9 | 89.1 | 33.2 | 1.7 | 54.2 | 34.7 | 19.5 |
| 1969 | 100.0 | 10.7 | 89.3 | 33.9 | 1.3 | 54.0 | 35.2 | 18.8 |
| 1970 | 100.0 | 11.4 | 88.6 | 34.6 | 1.6 | 52.4 | 34.1 | 18.4 |
| 1971 | 100.0 | 10.1 | 89.9 | 35.0 | 1.7 | 53.1 | 35.0 | 18.1 |
| 1972 | 100.0 | 10.0 | 90.0 | 33.7 | 3.5 | 52.8 | 35.2 | 17.6 |
| 1973 | 100.0 | 10.1 | 89.9 | 33.5 | 3.5 | 52.9 | 35.3 | 17.6 |
| 1974 | 100.0 | 10.1 | 89.9 | 33.6 | 1.4 | 54.9 | 37.8 | 17.1 |
| 1975 | 100.0 | 7.9 | 92.1 | 35.9 | 1.1 | 55.2 | 38.5 | 16.7 |
| 1976 | 100.0 | 8.5 | 91.5 | 37.0 | 1.2 | 53.4 | 39.0 | 14.4 |
| 1977 | 100.0 | 7.9 | 92.1 | 37.4 | 1.1 | 53.7 | 39.6 | 14.0 |
| 1978 | 100.0 | 7.3 | 92.7 | 37.6 | 1.0 | 54.2 | 39.9 | 14.3 |
| 1979 | 100.0 | 7.3 | 92.7 | 38.0 | 1.0 | 53.7 | 40.1 | 13.6 |
| 1980 | 100.0 | 7.4 | 92.6 | 38.1 | 1.0 | 53.5 | 40.6 | 13.0 |
| 1981 | 100.0 | 7.8 | 92.2 | 37.9 | 1.1 | 53.2 | 41.2 | 12.0 |
| 1982 | 100.0 | 7.6 | 92.4 | 38.1 | 1.0 | 53.2 | 41.0 | 12.2 |
| 1983 | 100.0 | 7.5 | 92.5 | 38.2 | 1.0 | 53.3 | 41.1 | 12.1 |
Disaggregation not available.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Table 8. Aggregate and per capita amount and percent distribution of expenditures for physicians' services, by source of funds: Selected years 1950-83.
| Year | Total | Patient direct payments | All third parties | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Total | Private | Public | ||||||
|
|
|
|||||||
| Health insurance | Other | Total | Federal | State and local | ||||
| Amount in billions | ||||||||
| 1950 | $ 2.7 | $ 2.3 | $ .5 | $ .3 | 2 | $ .1 | 1 | 1 |
| 1955 | 3.7 | 2.6 | 1.1 | .9 | 2 | .2 | 1 | 1 |
| 1960 | 5.7 | 3.7 | 2.0 | 1.6 | 2 | .4 | 1 | 1 |
| 1965 | 8.5 | 5.2 | 3.3 | 2.7 | 2 | .6 | $ .2 | $ .4 |
| 1966 | 9.2 | 5.5 | 3.7 | 2.8 | 2 | .8 | .3 | .5 |
| 1967 | 10.1 | 5.1 | 5.0 | 3.0 | 2 | 2.0 | 1.4 | .7 |
| 1968 | 11.1 | 5.2 | 5.9 | 3.4 | 2 | 2.5 | 1.8 | .7 |
| 1969 | 12.6 | 5.8 | 6.8 | 4.0 | 2 | 2.8 | 2.0 | .7 |
| 1970 | 14.3 | 6.5 | 7.8 | 4.8 | 2 | 3.0 | 2.1 | .9 |
| 1971 | 15.9 | 7.1 | 8.8 | 5.3 | 2 | 3.5 | 2.5 | 1.0 |
| 1972 | 17.2 | 7.2 | 10.0 | 6.0 | 2 | 3.9 | 2.8 | 1.2 |
| 1973 | 19.1 | 7.8 | 11.3 | 6.9 | 2 | 4.4 | 3.1 | 1.4 |
| 1974 | 21.2 | 7.7 | 13.5 | 8.1 | 2 | 5.4 | 3.8 | 1.6 |
| 1975 | 24.9 | 8.5 | 16.4 | 9.9 | 2 | 6.6 | 4.7 | 1.9 |
| 1976 | 27.6 | 9.0 | 18.5 | 11.4 | 2 | 7.1 | 5.2 | 1.9 |
| 1977 | 31.9 | 10.8 | 21.1 | 13.0 | 2 | 8.1 | 6.0 | 2.1 |
| 1978 | 35.8 | 11.5 | 24.3 | 15.0 | 2 | 9.3 | 6.9 | 2.3 |
| 1979 | 40.2 | 12.4 | 27.8 | 17.1 | 2 | 10.7 | 8.1 | 2.6 |
| 1980 | 46.8 | 14.3 | 32.6 | 19.9 | 2 | 12.6 | 9.7 | 3.0 |
| 1981 | 54.8 | 16.3 | 38.5 | 23.4 | 2 | 15.0 | 11.7 | 3.3 |
| 1982 | 61.8 | 17.8 | 44.0 | 27.1 | 2 | 16.9 | 13.4 | 3.5 |
| 1983 | 69.0 | 19.6 | 49.5 | 30.1 | 2 | 19.3 | 15.6 | 3.7 |
| Percent distribution | ||||||||
| 1950 | 100.0 | 83.2 | 16.8 | 11.4 | 3 | 5.2 | 1 | 1 |
| 1955 | 100.0 | 69.8 | 30.2 | 23.2 | 2 | 6.7 | 1 | 1 |
| 1960 | 100.0 | 65.4 | 34.6 | 28.0 | 2 | 6.4 | 1 | 1 |
| 1965 | 100.0 | 61.6 | 38.4 | 31.4 | .1 | 6.9 | 1.8 | 5.1 |
| 1966 | 100.0 | 60.0 | 40.0 | 30.7 | .1 | 9.3 | 3.4 | 5.9 |
| 1967 | 100.0 | 50.3 | 49.7 | 29.4 | .1 | 20.2 | 13.6 | 6.6 |
| 1968 | 100.0 | 46.9 | 53.1 | 30.5 | .1 | 22.5 | 15.8 | 6.7 |
| 1969 | 100.0 | 46.2 | 53.8 | 31.8 | .1 | 21.9 | 16.2 | 5.8 |
| 1970 | 100.0 | 45.4 | 54.6 | 33.6 | .1 | 20.9 | 14.9 | 6.0 |
| 1971 | 100.0 | 44.8 | 55.2 | 33.4 | .1 | 21.7 | 15.5 | 6.3 |
| 1972 | 100.0 | 41.9 | 58.1 | 35.1 | .1 | 22.9 | 16.2 | 6.7 |
| 1973 | 100.0 | 40.7 | 59.3 | 36.0 | .1 | 23.3 | 16.1 | 7.1 |
| 1974 | 100.0 | 36.4 | 63.6 | 38.4 | .1 | 25.2 | 17.8 | 7.4 |
| 1975 | 100.0 | 34.1 | 65.9 | 39.5 | .1 | 26.4 | 18.8 | 7.6 |
| 1976 | 100.0 | 32.7 | 67.3 | 41.5 | .1 | 25.7 | 18.7 | 7.0 |
| 1977 | 100.0 | 33.8 | 66.2 | 40.8 | .1 | 25.4 | 18.7 | 6.7 |
| 1978 | 100.0 | 32.1 | 67.9 | 41.9 | .1 | 25.9 | 19.3 | 6.5 |
| 1979 | 100.0 | 30.9 | 69.1 | 42.4 | 3 | 26.6 | 20.2 | 6.5 |
| 1980 | 100.0 | 30.5 | 69.5 | 42.5 | 3 | 26.9 | 20.6 | 6.3 |
| 1981 | 100.0 | 29.7 | 70.3 | 42.8 | 3 | 27.4 | 21.4 | 6.0 |
| 1982 | 100.0 | 28.8 | 71.2 | 43.8 | 3 | 27.4 | 21.7 | 5.7 |
| 1983 | 100.0 | 28.3 | 71.7 | 43.7 | 3 | 28.0 | 22.6 | 5.3 |
Disaggregation not available.
Less than $50 million.
Less than 0.5 percent.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Insurance coverage for other health care services, while growing, has been more limited (Table 9). Dental care is one example. Enrollment for dental benefits rose over 50 percent between 1976 and 1979 to a total of 60.3 million persons (Carroll and Arnett, 1981). Insurance paid for about 34 percent of all dental expenditures in 1983. Vision care benefits, although not large in dollar terms, also has experienced significant growth in recent years.
Table 9. Aggregate and per capita amount and percent distribution of other personal health care expenditures,1 by source of funds: Selected years 1950-83.
| Year | Total | Patient direct payments | All third parties | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Total | Private | Public | ||||||
|
|
|
|||||||
| Health insurance | Other | Total | Federal | State and local | ||||
| Amount in billions | ||||||||
| 1950 | $ 4.3 | $ 3.7 | $ .6 | 2 | $ .2 | $ .4 | 3 | 3 |
| 1955 | 6.1 | 5.2 | .9 | 2 | .2 | .6 | 3 | 3 |
| 1960 | 8.9 | 7.5 | 1.4 | $ .1 | .3 | 1.0 | 3 | 3 |
| 1965 | 13.4 | 10.9 | 2.5 | .3 | .5 | 1.7 | $ 1.0 | $ .7 |
| 1966 | 14.7 | 11.5 | 3.2 | .3 | .5 | 2.4 | 1.4 | 1.0 |
| 1967 | 16.0 | 11.9 | 4.1 | .5 | .5 | 3.0 | 1.8 | 1.2 |
| 1968 | 18.1 | 13.2 | 4.9 | .5 | .6 | 3.8 | 2.3 | 1.5 |
| 1969 | 20.2 | 14.6 | 5.6 | .7 | .6 | 4.3 | 2.6 | 1.7 |
| 1970 | 23.1 | 16.8 | 6.3 | .8 | .6 | 4.8 | 2.9 | 1.9 |
| 1971 | 25.2 | 17.8 | 7.4 | 1.0 | .7 | 5.7 | 3.4 | 2.2 |
| 1972 | 28.2 | 19.9 | 8.2 | 1.2 | .8 | 6.3 | 3.8 | 2.5 |
| 1973 | 31.0 | 21.6 | 9.4 | 1.4 | .8 | 7.1 | 4.3 | 2.8 |
| 1974 | 35.2 | 23.6 | 11.6 | 1.9 | .9 | 8.9 | 5.4 | 3.5 |
| 1975 | 39.8 | 25.4 | 14.4 | 2.6 | 1.0 | 10.8 | 6.6 | 4.2 |
| 1976 | 44.4 | 27.8 | 16.6 | 3.7 | 1.1 | 11.8 | 7.2 | 4.6 |
| 1977 | 49.2 | 30.3 | 18.9 | 4.5 | 1.2 | 13.2 | 8.0 | 5.2 |
| 1978 | 55.3 | 33.6 | 21.7 | 5.4 | 1.3 | 15.0 | 9.0 | 6.0 |
| 1979 | 62.4 | 37.0 | 25.4 | 6.8 | 1.4 | 17.2 | 10.3 | 6.8 |
| 1980 | 71.0 | 40.7 | 30.3 | 8.8 | 1.6 | 19.9 | 11.8 | 8.1 |
| 1981 | 80.7 | 45.3 | 35.4 | 10.6 | 1.8 | 23.0 | 14.0 | 9.1 |
| 1982 | 88.0 | 49.1 | 38.9 | 12.2 | 1.9 | 24.7 | 15.3 | 9.4 |
| 1983 | 97.1 | 54.5 | 42.6 | 13.7 | 2.1 | 26.8 | 16.8 | 10.0 |
| Percent distribution | ||||||||
| 1950 | 100.0 | 86.2 | 13.8 | 2 | 4.2 | 9.6 | 3 | 3 |
| 1955 | 100.0 | 85.6 | 14.4 | 2 | 4.1 | 10.3 | 3 | 3 |
| 1960 | 100.0 | 83.9 | 16.1 | 1.1 | 3.3 | 11.6 | 3 | 3 |
| 1965 | 100.0 | 81.6 | 18.4 | 1.9 | 3.5 | 13.0 | 7.8 | 5.2 |
| 1966 | 100.0 | 78.4 | 21.6 | 2.2 | 3.4 | 16.1 | 9.6 | 6.5 |
| 1967 | 100.0 | 74.5 | 25.5 | 3.1 | 3.3 | 19.1 | 11.3 | 7.7 |
| 1968 | 100.0 | 73.1 | 26.9 | 2.9 | 3.1 | 21.0 | 12.6 | 8.3 |
| 1969 | 100.0 | 72.3 | 27.7 | 3.4 | 3.0 | 21.4 | 12.8 | 8.5 |
| 1970 | 100.0 | 72.9 | 27.1 | 3.6 | 2.8 | 20.8 | 12.4 | 8.3 |
| 1971 | 100.0 | 70.7 | 29.3 | 3.9 | 2.9 | 22.5 | 13.6 | 8.8 |
| 1972 | 100.0 | 70.7 | 29.3 | 4.1 | 2.8 | 22.4 | 13.4 | 9.0 |
| 1973 | 100.0 | 69.7 | 30.3 | 4.7 | 2.6 | 23.0 | 13.8 | 9.2 |
| 1974 | 100.0 | 66.9 | 33.1 | 5.3 | 2.5 | 25.3 | 15.5 | 9.8 |
| 1975 | 100.0 | 63.9 | 36.1 | 6.5 | 2.5 | 27.1 | 16.5 | 10.6 |
| 1976 | 100.0 | 62.7 | 37.3 | 8.2 | 2.5 | 26.6 | 16.3 | 10.3 |
| 1977 | 100.0 | 61.6 | 38.4 | 9.2 | 2.4 | 26.8 | 16.3 | 10.5 |
| 1978 | 100.0 | 60.7 | 39.3 | 9.8 | 2.4 | 27.1 | 16.3 | 10.8 |
| 1979 | 100.0 | 59.3 | 40.7 | 10.9 | 2.3 | 27.5 | 16.6 | 10.9 |
| 1980 | 100.0 | 57.3 | 42.7 | 12.4 | 2.2 | 28.0 | 16.6 | 11.4 |
| 1981 | 100.0 | 56.1 | 43.9 | 13.1 | 2.2 | 28.5 | 17.3 | 11.2 |
| 1982 | 100.0 | 55.8 | 44.2 | 13.9 | 2.2 | 28.1 | 17.3 | 10.7 |
| 1983 | 100.0 | 56.2 | 43.8 | 14.1 | 2.2 | 27.6 | 17.3 | 10.3 |
Dentists' services, other professional services, drugs and medical sundries, eyeglasses and appliances, nursing home care, and other personal health care.
Included with direct payments; separate data not available.
Disaggregation not available.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Public expenditures
Government programs spent $124 billion for personal health care services in 1983, a 9.8 percent increase over 1982. Public programs financed almost 40 percent of all personal health care expenditures, including 53 percent of all hospital care, 28 percent of all physician services, and 48 percent of all nursing home care.
Federal expenditures of $93 billion for personal health care accounted for three-quarters of the public outlay and 30 percent of the total funding for personal health. Sixty-five percent of these Federal funds went towards purchases of hospital care; 17 percent, for physician services; and 9 percent, for nursing home care.
State and local governments financed $32 billion (10 percent) of personal health care services in 1983. Purchases of hospital services accounted for over half of the State and local expenditures; physician services, 12 percent; and nursing home care, 19 percent.
Public funding of personal health care changed dramatically with the advent of the Medicare and Medicaid programs. In 1965, 22 percent of all personal health care spending was publicly financed. Implementation of the Medicare and Medicaid programs rapidly boosted the proportion of public funding of personal health care to 34 percent in 1967. By 1980, public expenditures reached 40 percent and remained at that level through 1983. Federal funding has accounted for all of the growth in the proportion of public funds financing personal health care; the proportion of State and local funds actually declined over the period 1967 to 1983, from 13 percent to 10 percent.
From 1967 to 1983, the proportion of public funding to hospitals has remained stable (between 52 and 55 percent), with Federal funds (the Medicare program, specifically) accounting for a steadily increasing proportion of those public funds. During the same period, the proportion of public funding for physicians' services grew from 20 percent in 1967 to 28 percent in 1983. Once again, most of that increase can be attributed to the Medicare program.
Public financing of nursing home care grew from 34 percent in 1965 to 49 percent in 1967, peaked at 56 percent in 1975, and declined to 48 percent in 1983. Public financing for nursing home care comes predominantly through the Medicaid program, where costs are shared between the Federal and State and local governments.
Public financing for health care services comes from a number of Federal, State, and local programs (Table 10). Some, such as the Veterans' Administration and the U.S. Department of Defense, provide services directly through networks of hospitals, clinics, and nursing homes. The same agencies also pay public and private facilities to provide services. In the Medicare program, the Federal Government acts as an insurer, providing funds for medical care for eligible aged and disabled people. In other programs, Federal funds flow to State governments, which contribute additional funds. States may administer a medical program, as in the case of Medicaid, or may let funds flow through to local government agencies, as is done with maternal and child health and other community-related grants. States also fund health programs independently in State-run hospitals or through public assistance vendor payments for individuals not covered by Medicaid.
Table 10. Expenditures for health services and supplies under public programs, by program, type of expenditure, and source of funds: Calendar years 1982-83.
| Program area | Health services and supplies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Total | Personal health care | Administration | Public health activities | |||||||||
|
| ||||||||||||
| Total | Hospital care | Physicians' services | Dentists' services | Other professional services- | Drugs etc. | Eye glasses etc. | Nursing home care | Other care | ||||
|
| ||||||||||||
| Amount in billions | ||||||||||||
| 1983 | ||||||||||||
| Total health services and supplies | $340.1 | $313.3 | $147.2 | $69.0 | $21.8 | $8.0 | $23.7 | $6.2 | $28.8 | $8.5 | $15.6 | $11.2 |
| All public programs | 140.3 | 124.5 | 78.4 | 19.3 | .6 | 2.5 | 2.1 | 1.0 | 14.0 | 6.6 | 4.6 | 11.2 |
| Total Federal expenditures | 96.8 | 93.0 | 60.6 | 15.6 | .3 | 1.9 | 1.1 | .9 | 8.1 | 4.5 | 2.6 | 1.2 |
| Total State and local expenditures | 43.5 | 31.5 | 17.8 | 3.7 | .3 | .5 | 1.1 | .1 | 5.9 | 2.1 | 2.0 | 10.0 |
| Medicare1 (Federal) | 58.8 | 57.4 | 40.4 | 13.4 | --- | 1.5 | --- | .8 | .5 | .9 | 1.4 | --- |
| Medicaid2 | 35.6 | 34.0 | 13.6 | 2.9 | .5 | .8 | 1.9 | --- | 12.4 | 2.0 | 1.7 | --- |
| Federal expenditures | 19.2 | 18.1 | 6.9 | 1.6 | .3 | .4 | 1.0 | --- | 7.0 | 1.0 | 1.1 | --- |
| State and local expenditures | 16.4 | 15.8 | 6.7 | 1.4 | .2 | .4 | .9 | --- | 5.4 | .9 | .6 | --- |
| Other public assistance payments for medical care | 1.6 | 1.6 | .7 | .2 | .0 | .0 | .1 | --- | .5 | .1 | --- | --- |
| Federal | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| State and local | 1.6 | 1.6 | .7 | .2 | .0 | .0 | .1 | --- | .5 | .1 | --- | --- |
| Veterans' medical care | 7.7 | 7.6 | 6.3 | .1 | .0 | --- | .0 | .1 | .5 | .6 | .1 | --- |
| Department of defense medical care3 | 6.6 | 6.5 | 5.3 | .2 | .0 | --- | .0 | --- | --- | 1.0 | .1 | --- |
| Workers compensation | 6.4 | 5.0 | 2.6 | 2.1 | --- | .2 | .1 | .1 | --- | 1.4 | --- | |
| Federal employees | .3 | .3 | .2 | .1 | --- | .0 | .0 | .0 | --- | --- | .0 | --- |
| State and local programs | 6.1 | 4.8 | 2.4 | 2.0 | --- | .1 | .1 | .1 | --- | --- | 1.4 | --- |
| State and local hospitals4 | 7.9 | 7.9 | 7.9 | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| Other public expenditures for personal health care5 | 4.5 | 4.4 | 1.7 | .3 | .0 | .1 | .0 | .1 | --- | 2.2 | .1 | --- |
| Federal | 3.0 | 3.0 | 1.6 | .2 | .0 | .0 | .0 | .0 | --- | 1.1 | .0 | --- |
| State and local | 1.5 | 1.4 | .2 | .1 | .0 | .0 | .0 | .0 | --- | 1.1 | .1 | --- |
| Government public health activities | 11.2 | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 11.2 |
| Federal | 1.2 | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 1.2 |
| State and local | 10.0 | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 10.0 |
| Addenda: Medicare and Medicaid | 94.0 | 91.0 | 53.9 | 16.3 | .5 | 2.2 | 1.9 | .8 | 12.9 | 2.4 | 3.1 | --- |
| 1982 | ||||||||||||
| Total health services and supplies | $308.1 | $284.7 | $134.9 | $61.8 | $19.5 | $7.1 | $21.8 | $5.5 | $26.5 | $7.6 | $13.4 | $10.0 |
| All public programs | 127.8 | 113.4 | 71.8 | 16.9 | .6 | 2.0 | 1.9 | .8 | 13.4 | 5.9 | 4.4 | 10.0 |
| Total Federal expenditures | 87.6 | 84.0 | 55.3 | 13.4 | .3 | 1.5 | 1.0 | .7 | 7.7 | 4.1 | 2.4 | 1.2 |
| Total State and local expenditures | 40.1 | 29.4 | 16.4 | 3.5 | .3 | .5 | 1.0 | .1 | 5.7 | 1.8 | 1.9 | 8.8 |
| Medicare1 (Federal) | 52.4 | 51.1 | 36.7 | 11.4 | --- | 1.1 | --- | .6 | .5 | .8 | 1.3 | --- |
| Medicaid2 | 32.9 | 31.3 | 12.4 | 2.8 | .5 | .6 | 1.7 | --- | 11.7 | 1.6 | 1.6 | --- |
| Federal expenditures | 18.0 | 17.0 | 6.4 | 1.5 | .3 | .4 | .9 | --- | 6.7 | .9 | 1.0 | --- |
| State and local expenditures | 14.9 | 14.3 | 6.0 | 1.3 | .2 | .3 | .8 | --- | 5.0 | .7 | .6 | --- |
| Other public assistance payments for medical care | 2.0 | 2.0 | .8 | .2 | .0 | .0 | .1 | --- | .7 | .1 | --- | --- |
| Federal | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| State and local | 2.0 | 2.0 | .8 | .2 | .0 | .0 | .1 | --- | .7 | .1 | --- | --- |
| Veterans' medical care | 7.1 | 7.1 | 5.9 | .1 | .0 | --- | .0 | .1 | .5 | .5 | .1 | --- |
| Department of defense medical care3 | 5.7 | 5.7 | 4.6 | .2 | .0 | --- | .0 | --- | --- | .9 | .0 | --- |
| Workers compensation | 6.0 | 4.7 | 2.4 | 2.0 | --- | .1 | .1 | .1 | --- | --- | 1.3 | --- |
| Federal employees | .2 | .2 | .1 | .0 | --- | .0 | .0 | .0 | --- | --- | .0 | --- |
| State and local programs | 5.8 | 4.5 | 2.3 | 1.9 | --- | .1 | .1 | .1 | --- | --- | 1.3 | --- |
| State and local hospitals4 | 7.2 | 7.2 | 7.2 | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| Other public expenditures for personal health care5 | 4.4 | 4.4 | 1.8 | .3 | .0 | .1 | .0 | .1 | --- | 2.1 | .1 | --- |
| Federal | 3.1 | 3.0 | 1.6 | .2 | .0 | .0 | .0 | .0 | --- | 1.1 | .0 | --- |
| State and local | 1.4 | 1.3 | .1 | .1 | .0 | .0 | .0 | .0 | --- | 1.1 | .1 | --- |
| Government public health activities | 10.0 | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 10.0 |
| Federal | 1.2 | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 1.2 |
| State and local | 8.8 | --- | --- | --- | --- | --- | --- | --- | --- | --- | 8.8 | |
| Addenda: Medicare and Medicaid | 84.8 | 82.0 | 49.1 | 14.2 | .5 | 1.8 | 1.7 | .6 | 12.2 | 1.9 | 2.9 | --- |
Represents total expenditures from trust funds for benefits and administrative costs. Trust fund income includes premium payments paid by or on behalf of enrollees.
Includes funds paid into Medicare trust funds by states under “buy-in” agreements to cover premiums for public assistance recipients and for persons who are medically indigent.
Includes care for retirees and military dependents.
Expenditures for State and local government hospitals not offset by other revenues.
Includes program spending for maternal and child health; vocational rehabilitation medical payments; temporary disability insurance medical payments; Public Health Service and other Federal hospitals; Indian health services; alcoholism, drug abuse, and mental health; and school health.
Based on July 1 social security area population estimates.
SOURCE; Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Medicare and Medicaid
In 1983, Medicare and Medicaid financed 29 cents of every dollar spent for personal health care in the United States. The two programs expended $91 billion in benefits to 48 million people—one-fifth of the U.S. population. This figure does not include $404 million treated as a Medicaid expenditure which purchased Medicare supplementary medical insurance for eligible Medicaid recipients. To eliminate double counting, Medicaid “buy-in” premiums (income to Medicare) are subtracted, and only Medicare benefits received by these Medicaid eligible are counted when data from the two programs are presented together.
The introduction of these two programs, which accounted for almost three-quarters of all public spending in 1983, has dramatically increased the presence of the Federal Government in the health care market. Currently, the two programs pay 37 percent of all hospital expenditures, 24 percent of all physician expenditures, and 45 percent of all nursing home expenditures.
Over 30 million people, 90 percent of whom are 65 years of age or over, are enrolled in Medicare. The 1983 program expenditures totaled $58.8 billion: $57.4 billion was for benefit (personal health care) payments, and the remainder was for administrative expenses. About $2,900 per person was paid in 1983 for the 19.6 million people receiving benefits. Medicare spending for personal health care increased 12.4 percent in 1983, up $6.4 billion from 1982.
In 1983, Medicare spent an amount equal to 46.1 percent of the public share of personal health care expenditures and 18.3 percent of total spending for personal health care. Over 70 percent of Medicare benefits were for hospital care; another 23 percent were for physicians' services.
Medicare was created by Title XVIII of the Social Security Act. It began on July 1, 1966, as a Federal insurance program to protect the elderly from the high cost of health care. Rather than provide health care directly, Medicare reimbursed for care received from private sector providers. In July 1973, coverage was extended to permanently disabled workers and their dependents eligible for old age, survivors, and disability insurance (OASDI) benefits and to persons with end-stage renal disease.
Medicare has two parts, each with its own trust fund. The hospital insurance (HI) program, also called Part A, pays for inpatient hospital services, posthospital skilled nursing services, and home health services. A new benefit covering hospice care was introduced in October 1983. The supplementary medical insurance (SMI) program, also called Part B, covers physician services, medical supplies and services, home health services, outpatient hospital services and therapy, and a few other services.
Unlike other Federal health programs, Medicare is not financed solely by general revenues. In 1983, 84 percent of the income for the HI program (Table 11) came from a 1.3 percent payroll tax levied on employers and on employees for the first $35,700 of wages. Payroll contributions to the HI program increased 5.8 percent in fiscal year 1983, and HI benefit payments increased 10.9 percent.
Table 11. Payments into Medicare trust funds, by type of fund and source of income: Fiscal year 1983.
| Source of income | Total | Hospital insurance trust fund | Supplementary medical insurance trust fund | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Billions of dollars | Percent of total | Billions of dollars | Percent of total | Billions of dollars | Percent of total | |
| Total | $63.1 | 100.0 | $43.9 | 100.0 | $19.1 | 100.0 |
| Payroll taxes | 36.7 | 58.2 | 36.7 | 83.6 | --- | --- |
| General revenues | 18.81 | 29.8 | 4.51 | 10.3 | 14.2 | 74.4 |
| Premiums | 4.3 | 6.7 | .0 | .1 | 4.2 | 22.1 |
| Interest | 3.3 | 5.2 | 2.6 | 6.0 | .7 | 3.6 |
Includes a one-time lump sum transfer of $3.5 billion in military wage credits.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
The SMI program was financed by monthly premium payments of $12.20 per enrollee and by general revenues (appropriations from general tax receipts). The general revenue share of SMI receipts has grown significantly, from about 50 percent in 1971 to 74 percent in 1983 (Table 11). Through calendar year 1983, SMI premiums could not increase more than the increase in monthly cash retirement and survivors benefits, requiring a proportionately greater amount of general tax revenues to maintain the trust fund. Beginning in 1984, premiums were established so as to cover 25 percent of the costs incurred by the aged. Premiums for SMI rose to $14.60 per month in 1984 and will increase to $15.50 in 1985.
Efforts to curb rapidly growing Medicare expenditures resulted in changes in reimbursement policies late in 1982. The limits on daily routine inpatient hospital costs were replaced by limits on total inpatient costs per admission. In addition, Congress permitted prospective per capita payments to health maintenance organizations and other medical programs that contracted to provide comprehensive medical services to Medicare beneficiaries. Beginning in October 1983, further initiatives in prospective payment were implemented in the form of predetermined reimbursement rates for over 400 different diagnosis-related groups (DRG's). Under DRG's, hospitals will be paid based on the diagnosis group into which a patient falls, regardless of services provided or of length of stay (Grimaldi and Michelleti, 1984). The aim of DRG's is to encourage hospitals and attending physicians to consider the economic consequences of prescribed courses of treatment—a facet from which they often are insulated. Efforts to curtail the rapid growth in physician services were implemented in July 1984 with a 15-month freeze on physician fees. At the same time, the laboratory fee schedule will be changed to reimburse independent labs and physicians for 60 percent of prevailing charges. The freeze, coupled with lab fee change, is expected to save Medicare $105 million during the last 3 months of fiscal 1984 and $485 million during fiscal 1985.
In addition to reimbursement reforms, other changes are being made in the Medicare programs. Coverage of Federal employees became effective in January 1983, and mandatory coverage of employees of nonprofit organizations occurred in 1984. Also in 1984, self-employed people were required to contribute the equivalent of both the employer's share and the employee's share of the HI tax, doubling their contribution to the HI trust fund. Beginning in 1984, certain working aged and their spouses can elect to have primary insurance coverage through an existing employer plan or through Medicare. Employers will no longer be able to eliminate health coverage for employees 65-69 years of age (or employees with spouses aged 65 to 69) who choose to be covered.
When Medicare began in 1966, 9.4 percent of the population was 65 years of age or over. By 1983, the U.S. Bureau of the Census estimated that 11.7 percent of the population was elderly. Because of this shift toward an older population, the percentage of the total population potentially eligible for Medicare on the basis of age has increased 24 percent. That increase in the proportion of the population eligible for Medicare, coupled with significant rises in medical care prices, has put the solvency of the Medicare HI trust fund in jeopardy. The Medicare trustees believe that unless additional changes in the program are instituted, the HI trust fund will be unable to meet its obligations by 1991 (Board of Trustees, 1984).
From 1977 to 1982, Medicare hospital expenditures grew at an average annual rate of 18.0 percent, in contrast to a 14.6 percent increase in overall hospital spending. In 1983, growth in Medicare hospital expenditures slowed to 10.0 percent, slightly higher than the increase of 9.1 percent in total expenditures for hospital care. The reduced rate of growth for all hospital expenditures and for Medicare hospital expenditures resulted from lower hospital price inflation. Medicare growth was further curtailed with the fiscal 1983 implementation of limits on inpatient costs per admission and the fiscal 1984 implementation of the diagnosis-related group prospective payment regulations.
The diagnosis-related group prospective payment encourages shorter lengths of stay by paying hospitals a fixed, predetermined price independent of length of stay. Preliminary data on community hospitals from the American Hospital Association indicate a decline in length of stay for the aged of 4 percent in 1983, the largest decline in the past 10 years. Admissions for the elderly increased in 1983 by 4.7 percent, slightly less than the average increase over the past 10 years. The overall result is an increase of .1 percent in utilization measured in patient days for the population 65 years of age or over, significantly less than the average annual increase of 3.5 percent registered between 1974 and 1982.
Average annual growth in physician expenditures reimbursed by Medicare has exceeded the growth in overall expenditures for physician services by over 40 percent during the last 6 years. Growth in Medicare spending for physician services continued unabated into 1983 at a rate of 17.6 percent, half again as great as the growth in overall physician expenditures.
Medicare payments for care in a skilled nursing facility as a percent of total nursing home revenues have declined in recent years. In 1968, Medicare provided more than one-tenth of total nursing home revenues; by 1983, that share had dropped to less than 2 percent. Most of the decrease occurred between 1969 and 1971, following a reinterpretation of Medicare nursing care coverage.
Medicare reimbursement for home health agency services has grown significantly, increasing at an average annual rate of 24 percent since 1968. Home health care reimbursements in fiscal 1983 were $1.5 billion, compared with $60 million spent for home health care in fiscal year 1968. Growth in Medicare home health services accelerated in fiscal year 1983, increasing 30 percent over 1982. The growth stems, in part, from the elimination of the prior hospitalization requirement for coverage of home health care under the HI program, as well as the removal of the 100-visit limit. In addition, growth may be attributed to home health services being used to complement shorter hospital stays encouraged by Medicare reimbursement policies and by an easing of certification requirements for proprietary home health agencies. Most of Medicare payments for home health agency care are included in “other professional services.” The remainder, which was used to reimburse care provided by hospital based agencies, is reported under “hospital care.”
Beginning in October 1983, Medicare expanded hospital insurance benefits to include coverage of hospice care for terminally ill Medicare beneficiaries. Expenditures, estimated to be $148 million in fiscal year 1984, are categorized as “other professional services” within the national health expenditures.
In 1983, Medicaid cost $35.6 billion in combined Federal and State funds, providing benefits equal to 10.8 percent of personal health care spending. Medicaid expenditures for personal health care were 8.6 higher than in 1982. Hospital care accounted for 40 percent of program benefit expenditures, and nursing home care accounted for almost 36 percent.
During fiscal year 1983, Medicaid paid an average of $1,500 in benefits for each of its 21.5 million recipients. Two-thirds of the recipients qualify for Medicaid through their eligibility as members of families with dependent children; these recipients consume approximately one-quarter of all Medicaid financed services. Aged and disabled eligible recipients, accounting for 28 percent of recipients, consume 70 percent of all Medicaid financed services.
Medicaid was established in 1966 by Title XIX of the Social Security Act as a joint Federal-State program to provide medical assistance to certain categories of low-income people. These include aged, blind, and disabled people and members of families with dependent children. The program is run by the State, but the Federal Government, through what are called “matching funds,” contributes a portion of the cost of providing medical benefits to the categorically eligible. In addition, if the States chooses, Federal matching funds are available for medical benefits for the “medically needy”—people in one of the categories listed above who have incomes too high to qualify for cash assistance but not adequate to pay their medical bills. The basic Federal share of Medicaid payments to a State is based on a formula that incorporates the State's per capita personal income. The Federal formula match ratio currently ranges from 50 to 78 percent, 83 percent being the maximum payable by law.
Federal law requires that States participating in Medicaid provide a minimum set of services for their recipients. These services include inpatient and outpatient hospital care; laboratory and X-ray services; skilled nursing home care and home health services for those 21 years of age or over; early and periodic screening, diagnosis, and treatment for individuals under 21; family planning services; and rural health clinic services.
The Omnibus Budget Reconciliation Act of 1981 (OBRA) implemented a reduction in Federal Medicaid reimbursement to States of 3 percent in fiscal year 1982 and 4 percent in fiscal year 1983. Legislation extended OBRA through 1984, with a 4.5-percent reduction for that year. States could regain or “offset” one of those percentage points for each of three conditions: 1) if the State operated a hospital cost review program, 2) if the State had an unemployment rate 1½ times the national average, or 3) if the State operated a fraud and abuse program that recovered at least 1 percent of the Federal payment. In addition to these three offsets, a State could regain up to the original loss of Federal money by reducing the growth of its program expenditures to a target rate. It is estimated that these OBRA reductions will save the Federal Government $455 million in fiscal year 1984, costs that will have to be borne by the States.
Medicaid finances more long-term, nonacute, institutional care than Medicare does. Long-term care is provided by nursing facilities, psychiatric hospitals, and home health agencies. Long-term care benefit expenditures amounted to almost half of all 1983 Medicaid program spending. Nursing facility expenditures include spending in skilled nursing facilities, intermediate care facilities for the mentally retarded (ICFMR), and all other intermediate care facilities.
ICFMR has been the most rapidly growing benefit financed by Medicaid. The aim of ICFMR is to provide rehabilitative services to develop mentally disabled individuals in whom developmental progress is deemed possible.
Since 1973, expenditures for ICFMR have increased at a rate of almost 40 percent per year. By 1983, over 11 of all Medicaid dollars went for the purchase of ICFMR care. This rapid growth has occurred as a result of changes in the financing mechanism used by States to pay for the care of their developmentally disabled population—a change from funding under the supplemental security income (SSI) program to Medicaid.
A University of Minnesota study (Hill and Lakin, 1984) indicates that the mentally retarded population in residential care facilities in the United States declined slightly between 1977 and 1982, from 247,800 to 243,700. During the same period, the number of ICFMR-certified beds increased 40 percent to 138,738 beds. This increase occurred as it became more advantageous to finance care through Medicaid than through SSI. As costs for ICFMR increased (from $41.96 per resident day in 1977 to $79.53 in 1982), the payments under SSI covered a smaller proportion of services, with States financing the remainder. Under Medicaid, the maximum contribution by States could be limited to between 17 and 50 percent, depending on the State's formula match ratio. As costs rose, more States opted for Medicaid financing, resulting in rapid increases in expenditures for ICFMR.
The rapid growth of ICFMR will probably slow over the next 2 years, as the pool of beds eligible for Medicaid certification dwindles.
Data reported by Hill and Lakin show other trends affecting the mentally retarded population. The number of small, group residential facilities doubled between 1977 and 1982. At the same time, the number of mentally retarded residents in large public facilities declined by 20 percent, mostly from the mildly and moderately retarded group. There is an increase in the percent of profoundly retarded in large, public institutions, contributing to a doubling of the average per diem cost per resident in public institutions between 1977 and 1982.
Health Care for Veterans
The Veterans' Administration (VA) provides compensation and pensions for military veterans and their survivors, as well as medical care for veterans. Nearly 28.2 million people are eligible to receive some medical care from the VA, although not all of them apply for benefits. In fiscal year 1983, hospital and other medical care for veterans accounted for almost 31 percent of the $24.9 billion in outlays of the VA. In the 1983 National Health Accounts, VA expenditures for personal health care are estimated at $7.6 billion. Of that amount, $6.3 billion, or 83 percent, was spent to provide care in 172 VA medical centers (and other hospitals). VA medical centers provided care for 1.3 million inpatients and supplied care during 18.5 million outpatient visits.
In fiscal year 1983, 24.3 million inpatient days of care were financed by the Veterans' Administration in VA and non-VA hospitals. An additional 9.5 million inpatient days were provided in VA nursing homes or financed by the VA in State or community operated nursing facilities.
Over the next 20 years, the VA will have to address the issue of rapidly increasing demands on their health care systems. During this period, the total number of veterans will decline. However, the average age of veterans will increase, and the number of veterans 65 years of age and older will more than double between 1983 and 1995 (Veterans' Administration, 1983). Since the aged use more services and more expensive services per capita than the nonaged population, the costs of medical care provided by the VA are expected to accelerate.
Health Care for the Military and Dependents
The U.S. Department of Defense (DOD) assumes responsibility for the health care needs of the Nation's active and retired military forces and their dependents and survivors. Approximately $6.5 billion (10.5 percent of DOD outlays for salaries and benefits) was spent for health care in fiscal year 1983, including care for more than 2.1 million active personnel. The DOD health care system includes 168 hospitals that provided 5.3 million inpatient days of care in fiscal year 1983. Civilian Health and Medical Program of the Uniformed Services, the program that finances care required outside the DOD facilities (primarily for dependents and retirees), financed another 2.3 million inpatient days of care.
Indian Health Service
The Federal Indian Health Service provides personal health care and public health services to approximately 888,000 Indians and Alaskan natives through a network of hospitals and clinics. In 1983, $517 million was spent by the Indian Health Service in the delivery of health services.
Health Block Grants
During fiscal year 1982, Federal block grants were introduced for maternal and child health; preventive health; and alcohol, drug abuse, and mental health. A fourth health block grant, primary care, is scheduled for implementation in fiscal year 1984, furnishing grants for community health centers to provide care for the medically needy population. A total of $1.1 billion in fiscal year 1981 health expenditures were consolidated into three block grants amounting to $887 million in fiscal year 1982. This represents an 18-percent decrease in spending. The objective of these block grants is to moderate the levels of Federal funding and to reduce regulatory involvement while offering States flexibility in responding to their diverse health needs and priorities.
Despite the reduction in Federal appropriations for these block grants programs, the full reduction in Federal outlays is yet to be seen in all programs. Many of the health programs falling under block grants awarded project grants during the last quarter of fiscal year 1981, funding projects for up to 12 months under fiscal year 1981 budget authority. In addition, emergency jobs bill legislation increased maternal and child health appropriations in late 1983, most of which will be expanded in fiscal 1984. These extensions of Federal outlays have eased, and will continue to ease, the transition to block grants for many States.
Maternal and child health programs promote the health of medically underserved mothers and children and of crippled children. State and local governments spent $1.0 billion, including Federal block and special project grants of $425 million, for a variety of physician and other clinical services and for infant intensive care.
Federal preventive health block grants are included in Federal public health expenditures, funding various prevention and detection programs. This grant program requires a 20-percent match in funds by States, which is included in State and local public health activities.
The alcohol, drug abuse, and mental health block grants provide funds for prevention, treatment, and rehabilitative programs. Outlays for block grants and special projects, along with funding for St. Elizabeth's hospital in Washington, D.C., amounted to $581 million in 1983.
A report to Congress (General Accounting Office, 1982) indicates that a few program changes occurred during the early part of fiscal year 1982 as a result of the health block grants. States relied on the same mechanisms to handle block grants as were used in the supplanted categorical programs, because States had little time or money to institute change. States began to reexamine their needs, prioritize expenditures, and shift funds within the health sector in response to reduced Federal funding and to increased State budget constraints.
Programs such as maternal and child health and crippled children's services that affected a broad segment of the population received continued high priority compared with more narrowly defined programs such as the one to prevent lead paint poisoning (also included in the maternal and child health block grant). Programs where State involvement was minimal under the old categorical grant setup received lower priority under block grants. Increased public participation in setting priorities for block grant funds has been noted (General Accounting Office, 1984).
Workers' Compensation
Except for the program for Federal workers, workers' compensation programs are independent State-administered income maintenance programs that provide benefits for work-related disability and death. Approximately 29 percent of the benefits paid by these programs in 1980 was for medical services for workers, and the remaining 71 percent was for income-loss payments for workers and survivors (Price, 1984). Health and medical benefits amounted to $5.0 billion in 1983. Since workers' compensation programs are required by law, they are treated as public programs in the National Health Accounts. In some States, workers' compensation is run by private insurance under State oversight; others use State operated insurance funds or a combination of both (Price, 1980, 1981, 1984).
State and Local Government Hospitals
State and local governments traditionally have operated hospitals in order to provide health care to their citizens. In 1983, the cost of providing that care, after deduction of receipts from Medicare, Medicaid, other Government programs, and patient payments, was $7.9 billion.
Medicare and Medicaid have altered significantly the financing patterns of these hospitals, providing reimbursement for services that would have been provided previously as charity care. Thus, the net cost of care in State and local hospitals declined from 61 percent of total operating expenses in 1965 to 25 percent in 1977, and it has remained at about that level since then.
Approximately 1,700 community hospitals, accounting for 21 percent of all community hospital beds (American Hospital Association, 1983), are operated by State and local governments (primarily local). The American Hospital Association (AHA) reported that expenditures for services in these hospitals amounted to $19.9 billion in 1982, having increased at an average annual rate of almost 14 percent since 1973.
State governments and some large local governments care for the mentally ill in psychiatric hospitals, where 1982 AHA-reported expenses amounted to $5.5 billion. Care for the chronically mentally ill has undergone substantial change since 1955. A shift toward community-oriented care reduced the resources devoted to psychiatric hospitals. From 1964 to 1982, spending in these hospitals increased at a 7.5-percent annual rate—substantially below the rate for hospitals as a whole (American Hospital Association, 1983). In 1955, the 275 State and county mental hospitals had 559,000 resident patients. That number fell to 338,000 in 1970, to 216,000 in 1974 (National Institute of Mental Health, 1977), and to 126,000 in 1981. Operation of these hospitals is financed mostly from State and local governments' own funds, with relatively little patient revenue.
Other State and Local Government Programs
State spending for medical care for the poor who are not eligible for Medicaid and State spending that is not eligible for Federal matching funds are classified as “other public assistance payments for medical care.” In 1983, this spending amounted to $1.6 billion. Another $.9 billion was spent in 1983 through temporary disability insurance, school health, and vocational rehabilitation programs.
Philanthropy and industrial inplant services
Some health care is provided to industrial employees through inplant health services. Expenditures for these services, classified as “other health services,” are estimated at $1.8 billion for 1983. Funds for personal health care from private philanthropic organizations are classified by type of care and totaled over $1.8 billion in 1983. Administrative and fundraising expenses of private charities and philanthropic support of research and construction are included with the respective expenditure categories.
Direct patient payments
People must pay some of the cost of health care themselves, because third parties in general do not cover all the expenses of such care. These expenditures, called “direct patient payments” in the National Health Accounts, have grown more slowly than total personal health care expenditures have, and they are concentrated more in some types of services than in others.
Direct patient payments include a variety of expenditures. They include coinsurance and deductible amounts incurred under private or Government health insurance coverage. They also include uncovered services and amounts paid to providers of care over and above the usual, customary, or reasonable charges reimbursed by such insurance. The category does not include health insurance premiums, because some or all of those premiums are returned in the form of benefits during the year.
For most health care goods and services, the proportion of expenditures borne directly by patients and their families has declined over time. Direct patient payments of $85 billion in 1983 accounted for 27.2 percent of total personal health care expenditures, down from 37.4 percent 10 years earlier. Much of this decline is attributable to growth of private health insurance coverage and to steady increases in public program expenditures, particularly for hospital care and physicians' services. One exception to this trend is nursing home care, where reductions in Medicaid reimbursement have resulted in a larger proportion of private-pay patients. Direct patient payments as a fraction of total nursing home expenditures rose from 42.7 percent in 1979 to 49.9 percent in 1983.
The share of expenditures borne directly by the consumer varies by type of service (Table 12). In 1983, direct patient payments accounted for 7.5 percent of spending for hospital care and for 28.3 percent of spending for physicians' services. Almost half of nursing home care expenditures (49.9 percent) were paid directly by consumers. At the upper end of the range, the direct patient payment share of spending for eyeglasses and appliances was 72.5 percent in 1983, and the share of spending for drugs and sundries was 77.4 percent.
Table 12. Personal health care expenditures by selected third-party payers and type of expenditure: Calendar years 1981-83.
| Source of payment | Personal care | Hospital care | Physicians services | Dentists' services | Other Professional services | Drugs etc. | Eye- glasses etc. | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in billions | |||||||||
| 1983 | |||||||||
| Total | $313.3 | $147.2 | $69.0 | $21.8 | $8.0 | $23.7 | $6.2 | $28.8 | $8.5 |
| Direct payments | 85.2 | 11.1 | 19.6 | 13.9 | 3.3 | 18.4 | 4.5 | 14.4 | --- |
| Third-party payments | 228.1 | 136.1 | 49.5 | 7.9 | 4.7 | 5.4 | 1.7 | 14.4 | 8.5 |
| Private health insurance | 100.0 | 56.2 | 30.1 | 7.4 | 2.1 | 3.2 | .7 | .3 | --- |
| Philanthropy and industrial in plant | 3.7 | 1.5 | .0 | --- | .1 | --- | --- | .2 | 1.8 |
| Government | 124.5 | 78.4 | 19.3 | .6 | 2.5 | 2.1 | 1.0 | 14.0 | 6.6 |
| Federal | 93.0 | 60.6 | 15.6 | .3 | 1.9 | 1.1 | .9 | 8.1 | 4.5 |
| Medicare1 | 57.4 | 40.4 | 13.4 | --- | 1.5 | --- | .8 | .5 | .9 |
| Medicaid2 | 18.1 | 6.9 | 1.6 | .3 | .4 | 1.0 | --- | 7.0 | 1.0 |
| Other | 17.4 | 13.3 | .6 | .0 | .1 | .1 | .1 | .5 | 2.6 |
| State and local | 31.5 | 17.8 | 3.7 | .3 | .5 | 1.1 | .1 | 5.9 | 2.1 |
| Medicaid2 | 15.8 | 6.7 | 1.4 | .2 | .4 | .9 | --- | 5.4 | .9 |
| Other | 15.7 | 11.1 | 2.3 | .0 | .2 | .2 | .1 | .5 | 1.2 |
| 1982 | |||||||||
| Total | $284.7 | $134.9 | $61.8 | $19.5 | $7.1 | $21.8 | $5.5 | $26.5 | $7.6 |
| Direct payments | 77.2 | 10.3 | 17.8 | 12.4 | 3.1 | 16.9 | 4.1 | 12.7 | --- |
| Third-party payments | 207.5 | 124.6 | 44.0 | 7.1 | 4.0 | 4.9 | 1.4 | 13.8 | 7.6 |
| Private health insurance | 90.8 | 51.4 | 27.1 | 6.5 | 2.0 | 2.9 | .6 | .2 | --- |
| Philanthropy and industrial in plant | 3.4 | 1.4 | .0 | --- | .1 | --- | --- | .2 | 1.7 |
| Government | 113.4 | 71.8 | 16.9 | .6 | 2.0 | 1.9 | .8 | 13.4 | 5.9 |
| Federal | 84.0 | 55.3 | 13.4 | .3 | 1.5 | 1.0 | .7 | 7.7 | 4.1 |
| Medicare1 | 51.1 | 36.7 | 11.4 | --- | 1.1 | --- | .6 | .5 | .8 |
| Medicaid2 | 17.0 | 6.4 | 1.5 | .3 | .4 | .9 | --- | 6.7 | .9 |
| Other | 16.0 | 12.2 | .5 | .0 | .1 | .0 | .1 | .5 | 2.5 |
| State and local | 29.4 | 16.4 | 3.5 | .3 | .5 | 1.0 | .1 | 5.7 | 1.8 |
| Medicaid2 | 14.3 | 6.0 | 1.3 | .2 | .3 | .8 | --- | 5.0 | .7 |
| Other | 15.0 | 10.4 | 2.2 | .1 | .2 | .2 | .1 | .7 | 1.1 |
| 1981 | |||||||||
| Total | $253.4 | $117.9 | $54.8 | $17.3 | $6.4 | $20.5 | $5.6 | $23.9 | $7.0 |
| Direct payments | 70.8 | 9.2 | 16.3 | 10.9 | 3.1 | 16.2 | 4.5 | 10.7 | --- |
| Third-party payments | 182.6 | 108.7 | 38.5 | 6.4 | 3.3 | 4.4 | 1.2 | 13.2 | 7.0 |
| Private health insurance | 78.8 | 44.7 | 23.4 | 5.8 | 1.6 | 2.5 | .5 | .2 | --- |
| Philanthropy and industrial in plant | 3.0 | 1.3 | .0 | --- | .1 | --- | --- | .2 | 1.6 |
| Government | 100.8 | 62.7 | 15.0 | .7 | 1.6 | 1.9 | .7 | 12.8 | 5.4 |
| Federal | 74.3 | 48.6 | 11.7 | .4 | 1.2 | .9 | .6 | 7.2 | 3.7 |
| Medicare1 | 43.5 | 31.3 | 9.7 | --- | .8 | --- | .5 | .4 | .6 |
| Medicaid2 | 16.2 | 6.1 | 1.5 | .3 | .3 | .9 | --- | 6.3 | .8 |
| Other | 14.7 | 11.2 | .5 | .1 | .1 | .0 | .1 | .4 | 2.3 |
| State and local | 26.5 | 14.1 | 3.3 | .3 | .4 | .9 | .1 | 5.7 | 1.7 |
| Medicaid2 | 12.8 | 4.8 | 1.2 | .2 | .2 | .7 | --- | 4.9 | .6 |
| Other | 13.7 | 9.3 | 2.1 | .0 | .2 | .2 | .1 | .7 | 1.1 |
Represents total expenditures from trust funds for benefits. Trust fund income includes premium payments paid by or on behalf of enrollees.
Includes funds paid into Medicare trust funds by States under “buy-in” agreements to cover premiums for public assistance recipients and for persons who are medically indigent.
SOURCE: Office of Financial and Actuarial Analysis, Bureau of Data Management and Strategy, Health Care Financing Administration.
Because of the way in which estimates of national expenditures are made, direct patient payments include other items as well as those intended to be there—specifically, statistical error and nonpatient revenue of hospitals and nursing homes.
Direct patient payments are calculated as a residual and, thus, contain the net effect of data errors. The national health expenditure estimates are not based on a sample of patients but on aggregate provider and payer records. Many of these aggregations are subject to sample variability or errors of measurement. From estimates of total spending, estimates of the pieces paid by all known third parties have been deducted. Again, the estimates of these pieces are subject to sample and measurement errors. The residual, direct patient payments by definition, contains the net effect of these errors. If the magnitude of this type of error has not changed over time relative to that of expenditures, the movement of direct patient payments will be correct, even if the level is not correct.
Another result of the way in which direct patient payments are calculated is the inclusion of nonpatient revenues of hospitals and nursing homes. Surplus income from such sources as gift shops and parking lots and income from endowments and investments are used, in part, to offset losses from patient operations. Historical estimates of the magnitude of these items are not available. Based on data reported to the American Hospital Association, it would appear that about 5½ percent of community hospital revenue in 1982 came from these sources and from philanthropic donations for operating expenses. Assuming that noncommunity hospitals receive a smaller share of total revenue from these sources, about 5 percent of total hospital spending reported under personal health care expenditures was received from these sources. Subtracting the 1 percent share explicitly allocated to philanthropy in the 1983 National Health Accounts, the implication is that about 4 percent of the 7.5 percent “direct patient payments” share of total hospital spending is attributable to nonpatient, nonphilanthropic receipts; patient payments themselves amounted to about 3½ percent of the total. Using data for nursing homes (National Center for Health Statistics, 1979), it is estimated that about 4 percent of nursing home revenue also was attributable to nonpatient revenue, lowering the actual patient share of total spending for this type of care to about 46 percent.
The National Health Accounts: Definitions, concepts, and data sources
This report is the latest update of the national health expenditure estimates from the National Health Accounts. Provisional estimates of spending for health care in the Nation are presented for calendar year 1983, with selected historical data extending back to 1929. Revisions to estimates for 1965 through 1982 have been incorporated. These revisions affect primarily private insurance and direct patient payments.
The National Health Accounts provide a framework to help understand the nature of spending for health care. Going beyond a simple collection of numbers, the accounts employ a classification matrix with a consistent set of definitions to categorize health care goods and services and the manner in which their purchase is financed.
The framework of the National Health Accounts provides a more definitive picture of health care spending than other systems do, such as the National Income and Product Accounts (source of the GNP). However, care is taken to assure that the classifications used and estimates of levels generated are consistent with those underlying the GNP (Cooper, et al. 1982).
Different aspects of the National Health Accounts are explored in other work performed in HCFA (Arnett and Trapnell, 1984; Freeland and Schendler, 1984; Levit, 1982; Waldo and Lazenby, 1984).
For information concerning the definitions, concepts, and data sources used in this report, refer to “National Health Expenditures, 1982” (Gibson, Waldo, and Levit, 1982).
Footnotes
Reprint Requests: M. Carol Pearson, Division of National Cost Estimates, Room 2-C-7, Meadows East Building, 6325 Security Boulevard, Baltimore, Md. 21207.
This article continues a series of reports begun in the Department of Health, Education, and Welfare (Reed and Rice, 1964). The serires, now the responsibility of the Health Care Financing Administration, presents the National Health Accounts of the United States.
Industries are defined at the two-digit level of the 1972 Standard Industrial Classification, Government and private employment and payroll were combined for education (the largest industry) and for health care (Statistical Policy Division, 1978).
References
- American Hospital Association. Hospital Statistics, 1983 Edition. Chicago: 1983. [Google Scholar]
- Arnett RH, Trapnell GA. Health Care Financing Review. Washington: U.S. Government Printing Office; Winter. 1984. Private health insurance, New estimates of a dynamic industry. HCFA Pub. No. 03177. Office of Research and Demonstrations, Health Care Financing Administration. [Google Scholar]
- Blumberg MS. Provider price changes for improved health care use. In: Chacko GK, editor. Health Handbook. Amsterdam, Holland: North Holland Press; 1979. [Google Scholar]
- Board of Trustees, Federal Hospital Insurance Trust Fund. 1984 Annual Report of the Board of Trustees of the Federal Hospital Insurance Trust Fund. Washington: U.S. Government Printing Office; Apr. 1984. House Document 98-199. [Google Scholar]
- Carroll MS, Arnett RH. Health Care Financing Review. Washington: U.S. Government Printing Office; Sept. 1981. Private health insurance plans in 1978 and 1979: A review of coverage, enrollment, and financial experience. HCFA Pub. No. 03123. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Congressional Budget Office. Containing Medical Care Costs through Market Forces. Congress of the United States; May, 1982. [Google Scholar]
- Cooper BS, Gibson RM, Rice DP. U.S. national health accounts: Historical perspectives, current issues, and future projections. In: Levy E, editor. Accounting for Health. Paris, France: Economica; 1982. [Google Scholar]
- Falk IS, Klem MC, Sinai N. The Incidence of Illness and the Receipt and Costs of Medical Care Among Representative Families. Chicago: University of Chicago Press; 1933. [Google Scholar]
- Feder J, Scanlon W. Medicare and Medicaid Patients' Access to Skilled Nursing Facilities. Washington, D.C.: The Urban Institute; 1981. [Google Scholar]
- Feder J, Spitz B. The politics of hospital payment. In: Feder J, Holahan J, Marmor T, editors. National Health Insurance: Conflicting Goals and Policy Choices. Washington, D.C.: The Urban Institute; 1980. [Google Scholar]
- Freeland MS, Anderson G, Schendler CE. Health Care Financing Review. Washington: U.S. Government Printing Office; Summer. 1979. National hospital input price index. HCFA Pub. No. 03002. Office of Research, Demonstrations, and Statistics, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Freeland MS, Schendler CE. Health Care Financing Review. Washington: U.S. Government Printing Office; Spring. 1984. Health spending in the 1980's: Integration of clinical practice patterns with management. HCFA Pub. No. 03169. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- General Accounting Office. Report to Congress, Early Observations on Block Implementation. Washington: General Accounting Office; Aug. 1982. GAO/GGO-82-79. [Google Scholar]
- General Accounting Office. Report to Congress: Maternal and Child Health Block Grant: Program Changes Emerging Under State Administration. Washington: U.S. Government Accounting Office; May, 1984. GAO/HRD-84-35. [Google Scholar]
- Gibson R, Waldo DR, Levit KR. Health Care Financing Review. Washington: U.S. Government Printing Office; Sept. 1983. National health expenditures, 1982. HCFA Pub. No. 03154. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Grimaldi PL, Micheletti JA. Medicare's Prospective Payment Plan. Chicago: Pluribus Press, Inc.; 1984. [Google Scholar]
- Hill BK, Lakin KC. Trends in Residential Services for Mentally Retarded People: 1977-1982. Minneapolis: Center for Residential and Community Services, University of Minnesota, Department of Educational Psychology; Jun, 1984. Brief No. 23. [Google Scholar]
- Kasper JA. Prescribed Medicines: Use, Expenditures and Source of Payment. National Center for Health Services Research, Office of Health Research, Statistics, and Technology, Public Health Service; Hyattsville, Md.: Apr. 1982. DHHS Publication No. (PHS) 82-3320. [Google Scholar]
- Levit KR. Health Care Financing Review. Washington: U.S. Government Printing Office; Dec. 1982. Personal health care expenditures by State, selected years 1966-1978. HCFA Pub. No. 03149. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Van Nostrand J, et al. National Center for Health Statistics. Vital and Health Statistics. No. 43. Washington: U.S. Government Printing Office; Jul, 1979. The National Nursing Home Survey, 1977 Summary for the United States. (13). DHEW Pub. No. (PHS) 79-1794. Public Health Service. [PubMed] [Google Scholar]
- National Institute of Mental Health. Psychiatric Services and the Changing Institutional Scene, 1950-1985. Washington: U.S. Government Printing Office; 1977. DHEW Pub. No. (ADM) 77-433. [Google Scholar]
- Price DN. Social Security Bulletin. Washington: U.S. Government Printing Office; May, 1980. Workers' compensation program in the 1970's. SSA Pub. No. 13-11700. Office of Policy, Social Security Administration. [PubMed] [Google Scholar]
- Price DN. Social Security Bulletin. Washington: U.S. Government Printing Office; Sept. 1981. Workers' compensation, Coverage, benefits and costs. SSA Pub. No. 13-11700. Office of Policy, Social Security Administration. [Google Scholar]
- Price DN. Social Security Bulletin. Washington: U.S. Government Printing Office; Jul, 1984. Workers' compensation, 1976-80 benchmark revision. SSA Pub. No. 13-11700 Office of Policy, Social Security Administration. [PubMed] [Google Scholar]
- Reed LS, Rice DP. National health expenditures: Object of expenditures and source of funds, 1962. Social Security Bulletin. 1964 Aug. [Google Scholar]
- Somers AR, Somers HR. Health and Health Care. Germantown, Md.: Aspen Systems; 1977. [Google Scholar]
- Statistical Policy Division. Standard Industrial Classification Manual, 1972. Washington: U.S. Government Printing Office; 1978. Executive Office of the President, Office of Management and Budget. [Google Scholar]
- Veterans' Administration. Veteran Population Projections, by Age and Period of Service, Selected Years 1984-2030. Washington: Office of Reports and Statistics, Statistical Policy and Research Service; Apr. 1983. [Google Scholar]
- Wade AH. Social Security Area population projections, 1984, Actuarial Study No 92. Washington: U.S. Government Printing Office; May, 1984. Social Security Administration Pub. No. 11-11539. Office of the Actuary, Social Security Administration. [Google Scholar]
- Waldo DR, Lazenby H. Health Care Financing Review. Washington: U.S. Government Printing Office; Fall. 1984. Demographic characteristics and health care use and expenditure by the aged in the United States: 1977-1984. HCFA Pub. No. 03176. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Weissert WG, Scanlon WJ, Wan TTH, Skinner DE. Health Care Financing Review. Washington: U.S. Government Printing Office; Spring. 1984. Care for the chronically ill: Nursing home incentive payment experiment. HCFA Pub. No. 03168. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]