Abstract
In 1977-78 Medicaid recipients in Wayne County, Michigan had the option of joining health maintenance organizations (HMO's). This article presents an analysis of utilization levels and physician contact patterns prior to HMO enrollment and following HMO disenrollment. Medicaid families that had patterns of previous contacts with non-HMO physicians overwhelmingly choose the non-HMO option. Families with no physician contacts and very low utilization levels selected the HMO's. Also, higher than average utilization occurred during the 3 months following disenrollment from these HMO's.
Introduction
In recent years the rising costs of health care for Medicaid (Title XIX) recipients have become a serious problem. The people responsible for State budgets have been looking for ways to control these costs, while continuing to provide necessary health care to program recipients. Also, program expenses must be predictable, program monitoring must be kept to a minimum, and quality must be ensured.
One potential method for achieving these objectives is for the States to contract with health maintenance organizations (HMO's). The HMO's provide enrollees with a specified package of benefits in exchange for a fixed, prepaid, per capita premium. Prepayment of a predictable amount to HMO's allows for ease of payment for the State, and eliminates the need to process and pay individual claims for each of the services rendered to Medicaid recipients. Moreover, the Medicaid budget is more predictable, because maximum liability is established in advance for the HMO's. The need for program monitoring by the State also is reduced because a large portion of this responsibility is shifted to the HMO's, which accept the financial risk for their own enrollees. Thus, HMO contracts offer States several potential advantages over the fee-for-service system.
Experience with the performance of the early prepaid group practices, the prototype HMO's, had shown that such arrangements have resulted in reduced costs without lowering the quality of care and with less need for intense direct monitoring by the financing organization. Donabedian (1969) and Luft (1981) have reviewed the literature on HMO utilization. Both noted that most prepaid group practice plans experienced lower hospitalization rates than fee-for-service insurance plans, and surgical rates for many of the more discretionary procedures often were lower. The organizational features of the prepaid group practices and the financial incentives to their physicians encouraged the providers to eliminate care that was not medically necessary.
It should be noted that most of the studies of HMO performance have focused on employed populations, rather than Medicaid recipients. A medical care system that meets the needs of a middle-class group may not be effective in serving the poor. Reasons for joining or disenrolling from HMO's may be extremely different for Medicaid families, who do not need to weigh financial considerations when choosing a plan. Medicaid recipients ordinarily do not face premium differentials or out-of-pocket expenses (copayments or deductibles), regardless of the plan chosen. Therefore, one cannot generalize directly from the experience of HMO's serving employed populations to ones serving the poor. Still, HMO arrangements have seemed advantageous to many States for the reasons previously stated. Recent laws, such as the Omnibus Reconciliation Act of 1980 (Public Law 96-499), the Omnibus Reconciliation Act of 1981 (Public Law 97-35), and the Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA—Public Law 97-248), contain provisions to permit increased flexibility for State Medicaid programs. New options include provisions for a variety of reimbursement methods, and waivers of freedom of choice under certain conditions. Several States, including New York and California, have been able to implement competition in their Medicaid programs by allowing for choice among HMO's. As various State Medicaid programs become involved with HMO's, it is important to understand more about how Medicaid recipients choose and use HMO's.
The State of Michigan had already entered into agreements with two HMO's in Wayne County in the early 1970's, long before the Omnibus Reconciliation Acts and TEFRA. Under the terms of these agreements most Medicaid families in Wayne County were given the option of joining one of two HMO's or continuing to use their usual sources of care on a fee-for-service basis. It should be noted that there were no specific inducements for these Medicaid families to join these HMO's. Benefits were similar (and quite comprehensive) in all options. Copayments and deductibles were not required for any of the options. However, some Medicaid families were excluded from HMO eligibility because of their aid categories (families with crippled children or disabled persons).
One of these two HMO's was organized as a group practice. All patients were seen at a facility in Detroit's New Center area. During 1977 and 1978 this HMO had approximately 28,000 members, almost all of whom were Medicaid clients. Hospital care was furnished through the hospitals of the Detroit Medical Center and several other hospitals in the central city area. Salaried staff physicians provided primary care; specialists were retained on contracts on a part-time basis. The other HMO was an individual practice association (IPA) in which the physicians saw Medicaid HMO patients in their private offices, along with their other non-HMO patients. Most of the physicians in this association had offices in the inner city and had largely Medicaid patients in their private practices. These IPA physicians formed or joined the plan primarily because they had experienced billing and cash flow problems when dealing directly with the Medicaid program on a fee-for-service basis. One reason for forming the plan was to obtain a prepaid and predictable income when treating Medicaid patients. About 26,000 Medicaid enrollees were in this IPA plan during the period 1977-78.
State figures for fiscal year 1976 and later suggested that there were differences in hospital use between those Medicaid recipients who enrolled in these HMO's and those who used the fee-for-service option. Those enrolled in the HMO's were using less hospital care. These differentials in hospital use may have occurred for a variety of reasons, including the possibility that a lower-risk membership joined the HMO's. Another possibility is that the populations which chose the HMO's were similar to the group that did not, but the differentials in hospital utilization rates were accomplished by the HMO's, using a variety of mechanisms and controls. The HMO's may have used financial incentives (or disincentives); education programs and other informal organizational controls; or formal organizational controls. These controls could have resulted in reduction of hospital care through substitution of lower-cost services or through avoiding unnecessary care.
Because the capitation rate paid by the State of Michigan on behalf of the Medicaid enrollees was based on the assumption that the HMO enrollees had about the same health care needs as the Medicaid beneficiaries who used the fee-for-service option, it is important to know whether this was an accurate assumption. Even though preferred selection into the HMO's would have resulted in lower costs to the HMO's, this would not have translated into savings to Medicaid program. On the contrary, this situation may have resulted in additional costs to the State, because the HMO's were paid on the basis of estimates from a higher-risk population than was actually enrolled. Meanwhile, the non-HMO Medicaid population would have been left with a disproportionately large number of higher-risk persons, and therefore, would have had costs that were higher than expected if one used projections based on the combined population's use prior to introducing the HMO option.
The focus of this article is on the enrollment and disenrollment patterns of Medicaid families. “Preferred selection” describes a situation where disproportionately more of the low utilizers and the nonutilizers from the Medicaid population joined the HMO's. “Selective disenrollment” describes a situation where those who anticipate higher than normal use leave the HMO's.
The first objective is to investigate whether at least part of the utilization differential could be a result of lower-risk persons enrolling in the HMO's or higher-risk people leaving the HMO's. A second objective is to determine the personal and family characteristics related to joining HMO's, by examining the differences between HMO-enrolled and non-HMO Medicaid recipients with respect to age distribution, geographic location, family size and race; health care utilization patterns; and relationships with HMO and non-HMO physicians. A third objective is to examine patterns of use following disenrollment from the HMO's.
Literature review
Although there have been many studies of choice of plan using employed populations, only a few studies have been done concerning choice of plans by Medicaid recipients. Bice (1975) did a prospective study in 1971 among residents of four housing projects in east Baltimore. Low-income families were classified as to whether or not they were eligible for Medicaid. Bice found that in the non-Medicaid low-income group the demographic characteristics and use patterns associated with higher-risk of becoming ill and needing care were positively related to joining the group practice plan; however this relationship was not found for the Medicaid population, who incurred no out-of-pocket costs irrespective of where they received care.
Aside from Bice's study, there has been little empirical research on choice of plan by Medicaid recipients. However, several descriptive articles have discussed problems in extending the marketing mechanisms of the private, prepaid plans to the poor. Spitz (1979) speculated that the decision to join an HMO is quite different for Medicaid clients, when compared to employed persons. He suggested that Medicaid enrollees may have tended to assume a more passive role due to low education, a lack of sophistication, low expectations, and the type of docile behavior encouraged by welfare agencies.
Along the same lines Goldberg (1975) described the marketing abuses that occurred in California in the 1970's, including misrepresentations by those who conducted door-to-door solicitations. He suggested that under such circumstances where marketing strategies were based on pressure and misrepresentation, the Medicaid recipients became passive captives in the marketing process. Goldberg discussed the “… characteristics of market solutions when the consumer has freedom of choice among private profit-seeking providers, but is a poor judge of quality… [and when] the government pays most of the costs, and the provider's costs (or the quality of the output) depend on the consumers attracted.” He emphasized the producer's role in influencing demand, saying that, “Enrollment in a PHP [prepaid health plan] is not viewed as the result of careful evaluation of the alternatives by the Medicaid recipients; rather it is considered to be primarily influenced by the calculated decisions of the PHPs in their marketing efforts and in their screening out of bad risks.”
Interesting as these insights seem, neither they nor Bice's study suffice for developing a theoretical framework for Medicaid enrollment decisions.
Considerably more research has been done on employed populations, but such research is only partially applicable to a Medicaid situation. Berki and Ashcraft (1980) have summarized the literature on choice of plans for employed populations, and they have also developed a model which is useful in analyzing enrollment decisions for employed families. In this model the economic characteristics and risk factors of a family unit are modified by its beliefs about medicine and its attribute preferences, (patient-physician relationships; concerns about quality; preference for certain settings). Expected utilization patterns and attribute preferences then may be modified by insurance characteristics and delivery system characteristics to determine choice of plan.
This choice model needs to be modified somewhat to explain the behavior of Medicaid clients. Because there was no financial risk for these Medicaid families, the families did not need to consider their vulnerability to expenses when choosing among plans. However, the patient-physician relationships may have become even more important in determining the choices of plans for Medicaid families. Tessler (1975) found evidence in employed populations of important differences in choice behavior when joining an HMO means leaving one's personal physician. Whereas employed people need to balance leaving their personal physician against financial concerns (premium differentials or differences in coverge), the Medicaid recipients in this study did not have to do so. Therefore, it would seem that the patient-physician relationship may be the main determinant of choice for these Medicaid recipients. Those Medicaid recipients who already had satisfactory ongoing relationships with non-HMO physicians had something to lose, but nothing to gain if they joined HMO's. Those who did not have such relationships may have decided that the HMO's would provide some access to health care providers. However, they would lose the freedom to use non-HMO providers if they joined an HMO.
Because the existence of a prior relationship with a personal physician is partially related to risk, these two factors should not be considered independently. Those people who have had serious illnesses are most likely to have ongoing relationships with physicians; those who have no illnesses are least likely to see physicians. Therefore, the lower-risk people may be more likely to enroll in HMO's, because they do not have to sever existing doctor-patient relationships to join an HMO. This bias, in turn, would lead to favorable self-selection into the HMO's.
Although the tendency toward preferred self-selection has not been documented for Medicaid populations, it has been noted for a Medicare population and for employed families. Eggers (1980) compared prior utilization of 887 Medicare enrollees to the use of care in a fee-for-service control population. Eggers found the Medicare group that enrolled in HMO's were lower utilizers than the people in the control group. He speculated that the healthier, lower-risk people may have been attracted to and selected HMO's.
Luft (1981) provided a summary of recent studies on self selection among the employed populations. He concluded that,
“All evidence points to the importance of the pre-existing patient-physician relationship. People with strong ties are unwilling to break them, and will prefer to retain their old coverage, unless an HMO is structured to change only the financial linkages rather than the personal ones… It seems to be the case that within an employed population strong physician-patient ties are associated with poorer health status. More precisely, employed people without a private physician as their usual source of care are usually healthier than average, or at least lower utilizers of care.”
Luft's conclusion may be applicable to Medicaid recipients as well.
Whereas it is apparent that little is known about Medicaid enrollment decisions, even less is known about Medicaid disenrollment decisions. There have been few studies of HMO disenrollment even among employed populations. Obviously the loss of eligibility is a major reason for disenrollment, and dissatisfaction with the plans is another important factor. The role of the HMO or the HMO physicians in encouraging higher-risk people to disenroll has not been explored; neither has the topic of selective disenrollment been studied.
The Medicaid populations' reasons for disenrolling from HMO's remain largely unexplained. Hester and Sussman (1974), in their description of the Martin Luther King Neighborhood Health Center in New York, state that disenrollment was a major difficulty in running the program. These authors speculated that it was difficult to attract and retain Medicaid recipients probably because there were no financial advantages to joining an HMO. On the other hand there were disadvantages insofar as the patients had to give up access to non-HMO providers.
Wollstadt et al. (1978), examined disenrollment at the East Baltimore Medical Plan during the period from 1970 through 1973 using an actuarial analysis. They found that there was an increased trend toward disenrollment among the younger women. In addition those who stayed enrolled used plan services far more often than those who voluntarily disenrolled. Less than one in five of those who voluntarily disenrolled had sought services from the plan during the time they were enrolled. This group of disenrollees also had low facility use. However, while in the HMO out-of-plan use was higher for this group, compared with other enrollees.
Unfortunately, these studies do not form the basis for a model of why people on Medicaid disenroll from HMO's. Obviously loss of Medicaid eligibility is a major factor. However, among those who maintained continuous eligibility the reasons for disenrolling still are unclear. This study will examine various factors related to Medicaid HMO enrollment and disenrollment in order to explore whether such models can be developed.
Model and hypotheses
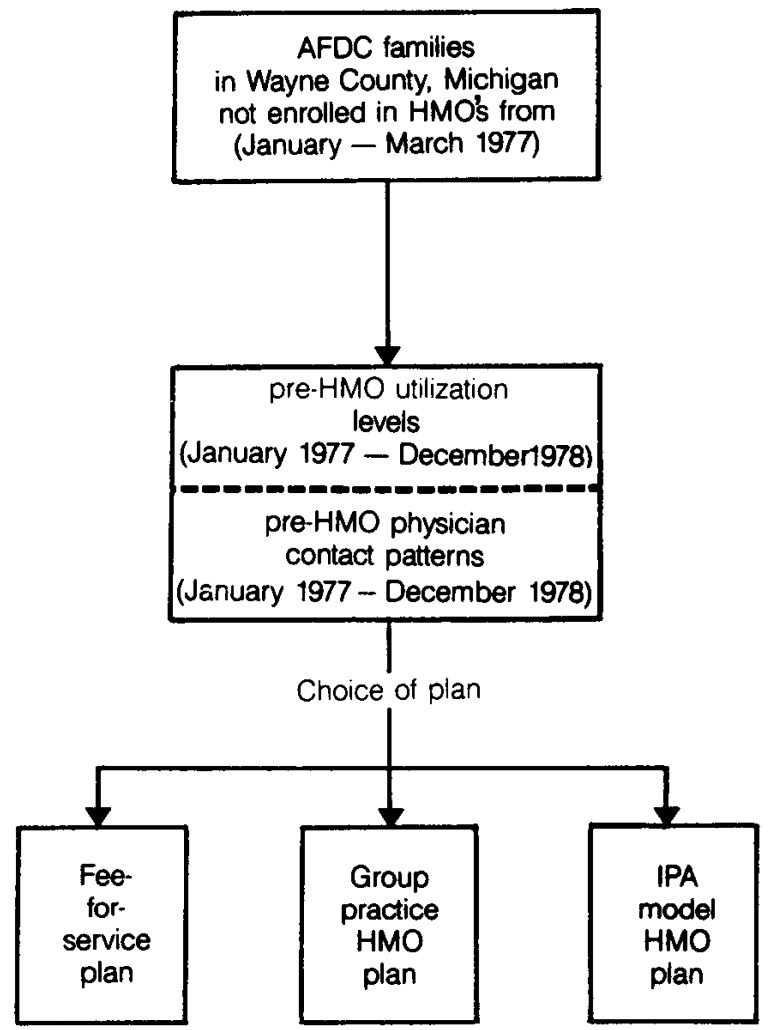
Figure 1 shows a schematic diagram for analyzing enrollment in HMO's. It should be emphasized again that the choice of plan had no economic consequences for these Medicaid recipients.
Figure 1. Model for analysis of enrollment in health maintenance organizations (HMO's).
The following hypotheses were tested:
H1: Those Medicaid families who enrolled in the HMO's have had lower utilization of medical care under Title XIX prior to enrollment, when compared to those who did not join HMO's.
H2: Among those Medicaid families who had contacts with non-HMO physicians, enrollment in HMO's is negatively related to health risk of the family.
H3: Those Medicaid families who had no physician contacts of any type would be most likely to join the HMO's.
H4: Among those families recently disenrolled from the HMO's, average expenses per person per month and average hospital utilization rates per person per month are higher than for those Medicaid families that had not been in HMO's.
-
H5: The following factors will be related to choice of HMO's:
Contacts with non-HMO physicians (negative).
High utilization patterns (negative).
Geographic location of residence in Detroit (positive).
Number of family members under 18 years of age (positive).
Geographic location inside Detroit and a large number of young family members are hypothesized to create access problems for the families. Therefore, the HMO may be chosen as a means of gaining access to care.
Method
A data file was created using records from the Michigan Department of Social Services on eligibility and utilization for all Aid to Families with Dependent Children (AFDC) cases in Wayne County that had continuous Medicaid eligibility between January, 1977 and December, 1978. All contacts with physicians were classified into categories by matching the identification numbers of the physicians to staff listings for each of the two HMO's.
A record was then created for each family unit—case. The data files on utilization, expenses, and contacts were generated through bills paid by Medicaid. Because the HMO's did not bill Medicaid on a fee-for-service basis, utilization data are absent while a family was enrolled in either HMO.
It should be noted that dollars are employed as a measure of utilization in order to standardize from one type of service to another. Thus, expenditures of various types can be added to arrive at a measure of utilization. A supplementary measure, hospital days, is also used, but cannot be combined with the other dollar measures.
In the section of the study that deals with enrollment behavior, those AFDC cases that were already enrolled in HMO's during months 1-3 were excluded, because behavior prior to enrollment could not be observed using the available data set. Similarly, for the disenrollment section of the study those families disenrolled during months 22-24 were excluded, because behavior following their disenrollment could not be observed. Those families that joined HMO's more than one time during this 24-month period are analyzed only in terms of their first enrollment after month 3 and their first disenrollment up to month 21. However, because HMO enrollees were locked in for a minimum of 6 months after joining this switching did not occur too frequently.
Physician contact patterns were observed for these AFDC families during the 3 months prior to HMO enrollment. Because it is necessary to have a sufficient observation period prior to joining the HMO, those families who were already enrolled prior to the first month of the study and those who joined an HMO in months 1-3 were excluded from the enrollment analysis.
For those families who enrolled in an HMO some time during months 4-24, physician contacts were observed during the 3 months prior to joining. This definition requires at least one billing for a service for any member of the family with at least one physician of the specified type or types during the 3 months prior to joining the HMO. This measure has the advantage of differentiating contact patterns with only one type of provider from mixed contact patterns. A disadvantage is the inability to measure intensity of contacts. It should be emphasized that all of these families in the study had continuous eligibility during the 24-month time period of this study.
For those families who did not join HMO's, different methods were used to measure physician contact patterns. The entire 24-month study period was used to observe contact and utilization patterns for these families, because any attempt to influence enrollment in HMO's could have occurred at any time during this period. Average utilization and contacts per person per month were calculated for each family. All health care costs billed to Medicaid were included.
For those families who enrolled in HMO's, a 3-month time period was used for observing utilization levels and contact patterns prior to joining. To standardize for differences in family size, this variable was measured as the average Medicaid dollars spent per person per month for each family unit.
For the disenrollment analysis the 3-month time period immediately following disenrollment was used. Average utilization per person per month was calculated. Measures used were total Medicaid dollars, hospital days, physician dollars, and outpatient hospital dollars. Post-disenrollment contact patterns were observed, to determine if the disenrollees continued to see HMO physicians following disenrollment. At least one family member must have had at least one bill from a physician in a given category for that family to be coded into that group.
Because the measurements for some families occurred at later times during the 24-month time period, it was necessary to standardize the dollars for inflation and for changes that occurred in Medicaid payment policy during the period 1977-78. Therefore, the Medicaid payments were adjusted to a base time period, using the medical care component of the Consumer's Price Index for the Detroit, Michigan area. Although the mix of services used in this index may not reflect precisely the mix used by Medicaid recipients, this provides a useful approximation for standardizing dollars over this 24-month time period. During the last 6 months of 1978 the Michigan Medicaid Program changed its reimbursement policy and, as a cost reduction measure, physician's services were paid at 95 percent of the amount billed. Therefore, the data on physician payments have been adjusted to compensate for this reduction. Because of these adjustments, the average amount of Medicaid expenses per month should be a stable and valid measure of utilization.
Several different types of statistical analysis were used to examine the associations between the variables. Contingency tables were used to examine the relationship of each of the contact and utilization variables to choice of plan for the enrollment hypotheses. Contingency tables were also used to look at utilization patterns following disenrollment from the HMO's. Analysis of variance and t-tests were used to compare groups of families who joined HMO's and those who did not, with respect to preenrollment expenditures. These techniques were used to compare levels of post-disenrollment expenditures for subgroups with various contact patterns. In addition, a discriminant analysis was used. Discriminant analysis is a statistical technique that allows the analyst to study the differences between two or more groups with respect to several variables simultaneously.
Several limitations should be recognized:
Measuring the predicted expenditures of family units based on past expenditure levels may result in problems. Various nonrecurrent past episodes, especially those involving hospital use, may misrepresent the future health risk of some family units. However, for a group this size this should not be a serious problem.
The use of family averages may distort individual use patterns. However, this should not create a serious problem, because families were required to enroll in/ disenroll from HMO's as units. Therefore, some averaging of families' expenses and utilization may be appropriate.
Measures of physician contacts and utilization are not independent, because utilization necessarily requires contacts. This means that the non-users are without contacts. This correlation between these independent variables may result in a less useful multivariate model.
Different operational definitions of the observation period of use were used for those families that joined and did not join HMO's. The use of the 3 and 24-month definitions resulted in unequal variances in the two groups. An alternate method was tried as a check, using 3-month observation time periods that were selected at random for each family that did not join HMO's. The results were not substantially different from those reported in this article.
Results
Records for 35,933 Medicaid AFDC families were analyzed for the hypotheses on enrollment. This included all families that did not join HMO's at all during the 24-month period, and those that joined HMO's in months 4-24. Families that joined HMO's in months 1-3 were excluded from the enrollment analysis, because sufficient data on preenrollment utilization patterns and physician contacts were not available; however, these cases were used in the disenrollment analysis when appropriate.
Contingency tables were used to examine the association between previous utilization levels, physician contact patterns, and choice of plan. In order to classify the Medicaid families according to previous utilization, the average Medicaid expenses per person per month were calculated for each family. Quartile values also were calculated for this measure. The 3 months prior to enrollment were observed for those families that joined HMO's in months 4-24. The entire 24-month time period was used for those families that did not join HMO's during this time period.
Table 1 displays the relationship of previous utilization level to choice of plan. These differences are highly significant, and indicate that the families in the very low previous utilization category enrolled in HMO's in disproportionately large numbers. Whereas 59 percent of the very low families joined HMO's, less than 10 percent of the families in any of the other (higher utilization) categories did so.
Table 1. Pre-health maintenance organization (HMO) utilization level and type of plan selected: 1977-78.
| Previous utilization level | Total number of families | Type of plan selected | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Non-HMO | IPA1-HMO | Staff-HMO | |||||
|
|
|
|
|||||
| Number | Percent | Number | Percent | Number | Percent | ||
| Very low-less than $6.002 | 9,021 | 3,681 | 40.8 | 2,456 | 27.2 | 2,884 | 32.0 |
| Low-$6.00-18.99 | 9,373 | 8,537 | 91.9 | 382 | 4.1 | 454 | 4.8 |
| High $19.00-$41.99 | 8,748 | 8,268 | 94.5 | 225 | 2.6 | 255 | 2.9 |
| Very high-more than $42.00 | 8,791 | 8,347 | 94.9 | 202 | 2.3 | 242 | 2.8 |
Individual practice association.
Figures in this column represent average Medicaid expenses per person per month for these families. These are quartile values.
NOTE: Chi-square = 11,867; significance at .001; number = 35,933.
To understand more about the behavior of these very low use families, it is helpful to subdivide them further, as follows:
Those families with at least one physician contact during their observation period of use.
Those families with no physician contacts during their observation period of use.
Table 2 displays the results of this subdivision, showing different patterns of choice of plan among those families that had no physician contact during the use observation time period, compared to those families with contacts. Contacts are defined to mean that at least one family member had at least one physician service billed to Medicaid during the observation period of use. Among those families with no physician contacts, 90 percent chose HMO's. Tables 1 and 2 show that the Medicaid families that chose the HMO's were predominantly those in the very low-risk category, and mainly those without any physician contacts prior to joining.
Table 2. Pre-health maintenance organization (HMO) utilization level, presence of physician contacts, and type of plan selected: 1977-78.
| Previous utilization level/contacts | Total number of families | Type of plan selected | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Non-HMO | IPA1-HMO | Staff-HMO | |||||
|
|
|
|
|||||
| Number | Percent | Number | Percent | Number | Percent | ||
| Very low utilization | |||||||
| No physician contact | 5,352 | 511 | 9.5 | 2,219 | 41.5 | 2,622 | 49.0 |
| Some contact | 3,669 | 3,170 | 86.4 | 237 | 6.5 | 262 | 7.1 |
| All utilization levels | |||||||
| No physician Contact | 5,489 | 567 | 10.3 | 2,261 | 41.2 | 2,661 | 48.5 |
| Some contact | 30,444 | 28,266 | 92.8 | 1,004 | 3.3 | 1,174 | 3.9 |
Individual practice association.
Table 3 presents data on the relationship between pre-enrollment contact patterns and choice of plan.
Table 3. Pre-health maintenance organization (HMO) physician contact patterns and type of plan selected: 1977-78.
| Previous physician contact pattern | Total number of families | Type of plan selected | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Non-HMO | IPA1-HMO | Staff-HMO | |||||
|
|
|
|
|||||
| Number | Percent | Number | Percent | Number | Percent | ||
| None | 5,489 | 567 | 10.3 | 2,261 | 41.1 | 2,661 | 48.4 |
| IPA1-HMO2 | 6,472 | 6,145 | 94.9 | 195 | 3.0 | 132 | 2.0 |
| Staff-HMO2 | 2,702 | 2,653 | 98.1 | 17 | 0.6 | 32 | 1.1 |
| Non-HMO2 | 30,231 | 28,193 | 93.2 | 920 | 3.0 | 1,118 | 3.7 |
Individual practice association.
Note that families may appear in more than one of these categories. In fact, the vast majority of those with HMO contacts also had contacts with non-HMO physicians.
It is clear from Table 3 that when some physician contact occurred the families overwhelmingly chose the non-HMO option; when no contacts occurred the HMO's were chosen. Because the families with mixed contact patterns (contacts with more than one group of provider) are counted in more than one category in Table 3, it is not possible to do a chi-square test; nevertheless this pattern is quite clear.
There were relatively few families that had exclusive contact patterns with HMO physicians while using the fee-for-service option. Still, it is informative to examine the behavior of those with exclusive HMO contact patterns for comparison with those who had both HMO and non-HMO contacts. Table 4 separates those families with exclusive preenrollment contact patterns from those with mixed contact patterns.
Table 4. Previous physician contact patterns and type of health maintenence organization (HMO) plan selected for those with exclusive and mixed contact patterns during the observation period of use: 1977-78.
| Previous physician contact pattern | Total number of families | Type of plan selected | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Non-HMO | IPA1-HMO | Staff-HMO | |||||
|
|
|
|
|||||
| Number | Percent | Number | Percent | Number | Percent | ||
| IPA1-HMO physicians (exclusively) | 194 | 62 | 31.9 | 80 | 41.2 | 52 | 26.8 |
| Staff-HMO physicians (exclusively) | 18 | 10 | 55.5 | 4 | 22.2 | 4 | 22.2 |
| Non-HMO physicians (exclusively) | 21,947 | 20,140 | 91.7 | 794 | 3.5 | 1,013 | 4.6 |
| None | 5,489 | 567 | 10.3 | 2,261 | 44.2 | 2,261 | 48.4 |
| Mixed patterns | 8,285 | 8,054 | 97.2 | 126 | 1.5 | 105 | 1.2 |
Individual practice association.
Those families with no physician contacts while under the fee-for-service option were the ones who were most likely to join the HMO's. The results found on Table 3 are somewhat different than on Table 4. Families with exclusive HMO contact patterns while using the fee-for-service option were more likely to subsequently enroll in HMO's, compared to those who had mixed contact patterns that included HMO physicians. Probably those with mixed contact patterns were more reluctant to join HMO's, because doing so would require them to give up at least some of their physician-patient relationships. However, those with exclusive HMO contacts would not face this conflict.
A discriminant analysis also was used to study the various factors related to choice of plan. Discriminant analysis is a statistical technique that allows the analyst to study the differences between two or more groups of objects with respect to several variables simultaneously. The Statistical Package for the Social Sciences (SPSS) was used to derive a canonical discriminant function, which is a linear combination of the independent variables.
The dependent variable is defined as the families' choice of plan, with two possible values: HMO and non-HMO. Using this technique the independent variables were entered in the following order:
Mean previous utilization level per person per month.
Preenrollment contacts with non-HMO physicians.
Preenrollment contacts with IPA-HMO.
Preenrollment contacts with Staff-HMO.
Location (Detroit; other Wayne County).
Number of family members under 18 years of age.
The standardized canonical discriminant function coefficients and Wilks' Lambda for the discriminant function variables are shown in Table 5. The standardized canonical discriminant function coefficients give the relative contribution of each variable to the function if the signs are ignored; the signs indicate whether the variable is making a positive or negative contribution. Wilks' Lambda is an inverse measure, where values near zero indicate high discrimination between groups, and values near one (maximum value) indicate that the group centroids are identical (no discrimination). Table 5 gives these values for the discriminating variables. The standardized canonical discriminant function coefficients show that the variable that makes the greatest (negative) contribution to joining an HMO is the percentage of months with non-HMO contacts. This means that choosing the HMO option is least likely for those families with intense non-HMO contacts. Other variables (more family members under 18 years of age, living in Detroit) are related in a positive way to choosing HMO's. It should be noted that while the percentage of months with HMO contacts has a negative relationship to choosing the HMO option, these contacts are not defined here as exclusive contacts with HMO physicians. In Table 4, virtually all of these HMO contacts are actually part of mixed contact patterns.
Table 5. Standardized canonical discriminant function coefficients and Wilks' Lambda for the discriminant function variables; entry order of independent variables assigned by user: 1977-78.
| Variable name | Wilks' Lambda | Standardized canonical discriminant function coefficients1 |
|---|---|---|
| Mean Medicaid dollar per person/month | .958 | + .170 |
| Percent of months with non-HMO contacts | .673 | −.988 |
| Percent of months with IPA-HMO contacts | .660 | −.250 |
| Percent of months with staff-HMO contacts | .656 | −.131 |
| Geographic location in Detroit | .640 | + .249 |
| Number of persons under 18 years of age | .624 | + .257 |
Relationship to choice of HMO option.
Mean Medicaid dollars per family member per month has a positive sign, although it is clear that families with the higher previous utilization levels chose the non-HMO option. The positive sign in the discriminant analysis is present because this variable, mean Medicaid dollars per family member per month, is correlated with another variable in the same function, percent of months with non-HMO contacts. The contribution of the previous utilization variable is reversed and partially cancelled by the relatively strong contribution of the non-HMO contact variable. This occurs because each of the standardized coefficients takes into consideration the simultaneous contribution of all the other variables.
Using this method 92.30 percent of the cases were classified correctly with respect to the dependent variable (HMO; non-HMO), compared to an a priori probability of 79.67 percent. This a priori probability is based on the overall proportion of families that did not join HMO's. Table 6 displays these figures. Chi-square, with 7 and 31,340 degrees of freedom, equals 14,775, which is significant at .0001. This indicates significant differences in the centroids of the two groups resulting from this function.
Table 6. Discriminant analysis with entry order of independent variables assigned by user: 1977-78.
| Actual group membership | Total number of families | Predicted group membership | |||
|---|---|---|---|---|---|
|
| |||||
| Group 1 joined HMO1 | Group 2 did not join HMO | ||||
|
|
|
||||
| Number | Percent | Number | Percent | ||
| Group 1 (joined HMO) |
6,373 | 4,561 | 71.6 | 1,812 | 28.4 |
| Group 2 (did not join HMO) |
24,975 | 602 | 2.4 | 24,373 | 97.6 |
Health maintenance organization.
The discriminant analysis thus was quite successful in developing an equation that predicts enrollment behavior. This multivariate model predicts 92.30 percent of the cases correctly, based on the values of the independent variables. The variable that makes the greatest contribution to this function is contact with non-HMO physicians.
Another version of the discriminant analysis was also used. This model, which separated the two HMO's, was unsuccessful. A scatter plot showing the centroids for the groups confirmed this interpretation. Group centroids for the two HMO's were almost identical.
Utilization levels following disenrollment
The 3 months immediately following disenrollment were used as an observation time period in order to assess the utilization patterns of those families recently disenrolled from HMO's. The objective was to discover if those families who disenrolled were higher than average in terms of risk. Here subsequent utilization was used as an indicator of risk.
There were 1,052 families who disenrolled from HMO's between months 1 and 21 of the study period, with 506 of them coming from the IPA-HMO and 546 from the staff-HMO. Families that disenrolled in months 22-24 had to be excluded, because there was not sufficient time to observe their post-disenrollment utilization patterns. Average Medicaid post-disenrollment expenses per person per month were calculated for these 1,052 families, for comparison with those families who were not in HMO's. All types of expenses paid by the Medicaid program (hospital, physician, drugs, etc.) were included.
An analysis of variance was performed to test whether the differences in post-disenrollment expenses were significant. When all families that disenrolled from HMO's are grouped together and compared to the families that had not been in HMO's, it is clear that average post-disenrollment expenses are higher. The differences are significant at .0166, with F= 5.74.
The same pattern of higher use was found for post-disenrollment hospital utilization (Table 7). An analysis of variance was performed to test the statistical significance of these differences. With F = 12.749 the differences are significant at .001.
Table 7. Average use of hospital days per family member per month, by enrollment status: 1977-78.
| Enrollment status | Mean monthly hospital days per family member | Standard deviation | Number of families |
|---|---|---|---|
| IPA-HMO1 disenrolled | .0810 (post disenrollment) |
.3922 | 506 |
| Staff-HMO disenrollees | .0733 (post disenrollment) |
.3611 | 546 |
| Non-HMO | .0393 (24-month period) |
.2326 | 28,333 |
Individual practice association-health maintenance organization.
Further analysis showed that most of the disenrolled families either used non-HMO physicians or received no care in the time period immediately following their disenrollment.
Discussion
The findings of this study confirm the importance of the preexisting doctor-patient relationships in determining choice of plan. Juba (1980) and Ashcraft (1978) have discussed a tendency of those with preexisting patient-physician ties to be higher utilizers. Because families with physician ties are the ones least likely to sever these ties in order to join HMO's, this combination can result in preferred selection of the lower-risk families into the HMO's. The findings of this study are consistent with these observations. The majority of those with ties to non-HMO physicians did not join HMO's; the majority of the Medicaid families that had no previous physician contacts joined the HMO's. One plausible explanation for their joining was to gain access to an organized group of physicians.
Even though there is good evidence of preferred selection by Medicaid families, there is no evidence that the HMO physicians attempted to actively influence these decisions. It was suggested by some people that the IPA physicians, who saw both Medicaid HMO and Medicaid fee-for-service patients in their office practices, might try to selectively influence their higher utilizers to choose the fee-for-service option and their lower utilizers to choose the IPA-HMO. This could result in financial advantage for these physicians. Analysis showed that this pattern was not occurring. Instead, it would seem that the preferred selection occurred because the HMO's were more successful in attracting those families that did not have ongoing relationships with non-HMO physicians. Because those without physicians were probably healthier than average, this led to preferred self-selection (or, from another perspective, favorable recruitment by the HMO's).
The data in this study show higher than average use following disenrollment from HMO's. Nevertheless, the higher-risk disenrollees did not continue to retain their relationships with HMO physicians once they disenrolled. Because the study population only included families with continuous Medicaid eligibility during the entire 24-month study period, all disenrollments were voluntary. Therefore, loss of eligibility could not account for disenrollment. Many other reasons for the disenrollment patterns are possible. One explanation is that there was really no selective disenrollment. Instead, those families who disenrolled had health care needs which were normal. However, when they began to see non-HMO physicians (whom they had never seen before, or whom they had not seen for the time they were locked in to the HMO) then these physicians might have done extensive testing, X-rays, and other procedures in order to determine their new patients' conditions. The problem with this explanation is that it does not account for the higher than average hospital utilization that occurred following disenrollment. Even though the new physicians may have done a greater than average amount of testing or X-rays, it is unlikely that hospital stays would occur simply because new physicians were seeing recently disenrolled persons. Another explanation is that those HMO enrollees who required the most care had more opportunities to become dissatisfied with their HMO's. These higher-risk people may have disenrolled in order to have access to other physicians.
Some of this disenrollment may have resulted from situations where HMO enrollees had the need for surgical or childbirth care, but wanted these services performed by physicians whom they had known before joining the HMO. Freidson (1961) found that one of the major reasons for out-of-plan use among (non-Medicaid) Health Insurance Plan of Greater New York (HIP) enrollees was the desire to use physicians who were known to the enrollees before they joined HIP. This out-of-plan use was most frequent for childbirth or surgical procedures. Given the fact that most Medicaid HMO members could not afford out-of-plan use, the only way they could return to their non-HMO physicians for surgery or childbirth care would be to disenroll from the HMO. This explanation would be consistent with the data from this study, where both higher than average hospital expenses and use of non-HMO physicians were found among the recently disenrolled families.
Another possible explanation for the disenrollment of higher-risk enrollees is that they were pushed out by the HMO physicians. This could have happened for a variety of reasons. The HMO physicians may have referred higher users to outside specialists, whom the patients preferred to see as their regular physicians; HMO physicians may have neglected to satisfy some of the higher users' demands, and thereby left them dissatisfied, or HMO physicians may have deliberately influenced some of the higher users to disenroll, in order to lower their expenses (or their HMO's expenses) for providing care to these people. It is obvious that the disenrollment data that were available were inadequate for examining whether families were pushed out. To understand this behavior better, one would have to look at encounter forms or medical records to see what was wrong with these patients. There was no evidence that the HMO physicians influenced higher users to disenroll so that they could be seen as private patients on a fee-for-service basis. Those disenrollees who continued to use HMO physicians following disenrollment had lower than average expenses. It is clear that factors related to disenrollment need to be explored further using more direct methods, such as medical records or interviews with people at the time they disenroll or shortly afterwards. It is only through such methods that the reasons for disenrollment can be explored adequately.
In determining the proper level of reimbursement for Medicaid recipients enrolled in HMO's, it is important to know if favorable selection is occurring. In theory, it would seem that favorable selection should occur because those individuals who already have strong ties with physicians would not be expected to enroll, and they probably have poorer than average health status. Because there are no expected financial advantages associated with HMO enrollment for Medicaid families (no differentials in out-of-pocket or premium costs), financial considerations would not motivate the higher utilizers to join HMO's. Because ties with non-HMO physicians would have to be severed to join HMO's, one would expect those families with strong ties to non-HMO physicians to reject the option of HMO enrollment. This would result in the favorable self-selection of Medicaid recipients into the HMO's.
The findings of this study support this formulation. To some extent the research is similar to the work done by Eggers (1980) on Medicare beneficiaries. Going beyond Egger's analysis, this study has identified some possible causes of the self-selection of the lower-risk beneficiaries into HMO's. In particular, the possible roles of the patient-physician relationships were examined, insofar as they may have had an impact on favorable self-selection. Relationships with non-HMO physicians were found to be clearly and strongly associated with preferred selection for the HMO, insofar as the existence of these ties apparently prevented many higher-risk families from joining the HMO's. Finally, the lack of ties to any physicians were associated with low utilization levels and also with a tendency to join the HMO's. This resulted in preferred selection into the HMO's.
It would seem that these findings can be generalized to other situations where potential Medicaid HMO enrollees are offered a choice between two or more comprehensive health care plans, with no financial consequences associated with choice of plan. Assuming that other aspects of the options were similar (perceived quality, access, the attractiveness of the facilities, etc.) then existing patient-physician relationships (or the lack of such relationships) will be the major determinant of choice of plan. Preferred selection can be expected because of the correlation between risk levels and contact patterns. This pattern also might be generalized to certain non-Medicaid populations, providing the conditions described above are met. By eliminating differentials in potential financial loss, the risk-vulnerability considerations will become inoperative.
These findings have important policy implications. The existence of a preferred selection process by Medicaid recipients has significance for assessing HMO reimbursement methods and levels. Based on the findings of this study, the rate-setting process should include consideration of the relative health risk of the HMO Medicaid enrollees, compared to those Medicaid beneficiaries who do not enroll in HMO's. Thomas (1983) and others have been working on adjustments based on risk differentials. Treiger (1981) suggests that, “The basic issue boils down to how complicated a risk reimbursement methodology one wishes to develop to minimize unknown factors.”
In addition to developing a satisfactory risk reimbursement methodology, it is important to monitor the self-selection of people into HMO's. Program monitoring should combine different methods, including:
Comparisons of prior utilization of HMO enrollees and a comparison group.
Monitoring of HMO utilization rates and non-HMO utilization rates.
Comparisons of post-disenrollment utilization (during the time period immediately following HMO disenrollment) for those recently disenrolled and for a comparison group.
Post-disenrollment interviews of samples of Medicaid recipients who had disenrolled from HMO's and analysis of their medical records.
The first and third methods can be approached in a manner similar to that used in this study. The second method is more complex, because HMO's often have achieved appropriate reductions in the utilization of hospital services. While lower hospital utilization rates would not, in and of themselves, prove that lower-risk families had enrolled in the HMO's, such reductions might still justify adjustments in premiums. It is important to monitor hospitalization rates for Medicaid recipients enrolled in HMO's so that changes in aggregate rates over time can be investigated further. Then utilization of individual families can be followed over time as they switch from one option to another. The fourth method, post-disenrollment interviews and review of medical records, is essential if one wishes to gain a better understanding of why Medicaid families leave HMO's.
The findings are also important as various State and Federal programs attempt to enroll more Medicaid recipients into HMO's to control program costs. In the 1970's, the Medicaid policy had been to allow for voluntary choice of plan, rather than requiring Medicaid recipients to use HMO's. However, recent Federal laws have given States more flexibility in administering their Medicaid programs. One option includes the waiver of freedom of choice of provider. If people are forced into HMO arrangements against their wishes, serious dissatisfaction may result. Both the patients and the providers may find such situations difficult, or even intolerable. However, given the findings of this study, it is apparent that complete freedom of choice will likely result in preferred selection into HMO's when choice of plan results in no financial consequences to the consumer. This could result in a situation when HMO's have a very limited potential to control costs for the Medicare/Medicaid programs. More attention should be given to developing both economic and noneconomic incentives to attract more medium and high-risk people into HMO's.
Footnotes
Reprint requests: Susan I. DesHarnais, University of Michigan-Flint, Health Care Program, Flint. Michigan, 48502-2186.
References
- Ashcraft MLF. The Impact of Previous Medical Care Experiences on Enrollment in Prepaid Group Health Plans. PhD Dissertation. The University of Michigan; 1978. [Google Scholar]
- Berki SE, Ashcraft MLF. HMO enrollment: Who joins what and why: A review of the literature. Milbank Memorial Fund Quarterly/Health and Society. 1980 Fall;:588–631. [PubMed] [Google Scholar]
- Bice TW. Risk vulnerability and enrollment in a prepaid group practice. Med Care. 1975 Aug.:698–703. doi: 10.1097/00005650-197508000-00011. [DOI] [PubMed] [Google Scholar]
- Donabedian A. An evaluation of prepaid group practice. Inquiry. 1969 Sept.:3–27. [Google Scholar]
- Eggers P. Health Care Financing Review. Washington: U.S. Government Printing Office; Winter. 1980. Risk differential between Medicare beneficiaries enrolled and not enrolled in an HMO. HCFA Pub. No. 03027. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Friedson E. Patient's views of medical practice. New York: Russell Sage Foundation; 1961. pp. 115–123. [Google Scholar]
- Goldberg VP. Some emerging problems of prepaid health plans in the Medi-Cal System 57-58. Policy Analysis. 1975 Winter;1:57–58. [PubMed] [Google Scholar]
- Hester J, Sussman E. Medicaid prepayment: Concept and implementation. Milbank Memorial Fund Quarterly/Health and Society. 1974 Fall;:415–444. [PubMed] [Google Scholar]
- Juba DA, Lave JR, Shaddy J. An analysis of the choice of health benefit plans. Inquiry. 1980 Spring;:62–71. [PubMed] [Google Scholar]
- Luft HS. Health maintenance organizations: Dimensions of performance. New York: John Wiley and Sons, Inc.; 1981. [Google Scholar]
- Spitz B. When a solution is not a solution: Medicaid and health maintenance organizations. Journal of Health Politics, Policy and Law. 1979 Winter; doi: 10.1215/03616878-3-4-497. [DOI] [PubMed] [Google Scholar]
- Tessler R, Mechanic D. Factors affecting the choice between prepaid group practice and alternative insurance programs. Milbank Memorial Fund Quarterly/Health and Society. 1975 Spring;:149–172. [PubMed] [Google Scholar]
- Thomas JW, Lichtenstein R, Wyszewianski L, Berki SE. Increasing Medicare enrollment in HMO's: The need for capitation rates adjusted for health status. Inquiry. 1983 Fall;:227–239. [PubMed] [Google Scholar]
- Trieger S, Galblum TW, Riley G. HMO's: Issues and alternatives for Medicare and Medicaid. Vol. 16. Department of Health and Human Services, Health Care Financing Administration, Office of Research, Demonstrations, and Statistics; [Google Scholar]
- Wollstadt LJ, Shapiro S, Bice TW. Disenrollment from a prepaid group practice: An actuarial and demographic description. Inquiry. 1978 Jun;:142–150. [PubMed] [Google Scholar]