Abstract
The relationship of hospital ownership and service composition to hospital charges was examined for 456 general acute hospitals in California. Ancillary services had higher profit margins, both gross and net profits, than daily hospital services. Ancillary services accounted for 55.3 percent of total patient revenue. Charges per day were 23 percent higher for ancillary services than for daily hospital services. Net profits for daily and ancillary services were lowest at county hospitals. Proprietary hospitals had the highest net profits for total ancillary services and the highest mean charges. Not-for-profit hospitals had the highest profit margins for daily hospital services. Neither direct nor total costs for ancillary services were significantly different among ownership groups, although direct costs for daily hospital services were significantly higher at proprietary hospitals.
Introduction
Hospital charges have become an area of widespread concern throughout the Nation. In 1982, it cost $4,566 for the average hospital stay in California (California Health Facilities Commission, 1983). Between 1981-82, hospital charges rose 21.3 percent, nearly twice the 12.6 percent increase nationally, and more than 3 times the rate of general inflation. Furthermore, charges are greatly varied among hospitals. In the increasingly competitive health care system now emerging, both consumers and third-party payers, particularly those contracting for services or negotiating rates, need more information regarding hospital charges. It is, therefore, important to identify and examine factors affecting hospital costs and charges.
Two of the factors affecting hospital charges are service composition and hospital ownership. Service composition refers to the number and type of services offered. Costs, charges, and profit margins greatly vary among services, so their distribution and intensity are important determinants of overall costs.
Ancillary and daily hospital services
Hospital services are traditionally grouped into two main categories—daily hospital services and ancillary services. Daily hospital services include room and board and nursing care. Examples of daily services are medical and surgical, intensive care, and pediatrics. Ancillary services include most nonroutine services such as pharmacy, laboratories, and radiology.
Ancillary services are producing an increasingly larger proportion of total hospital revenues, particularly for proprietary hospitals (Siafaca, 1981). The greater relative importance of ancillary services as revenue generators may be the result of several factors such as:
The emphasis of rate controls on routine rather than ancillary services.
The increased availability and utilization of ancillary services.
The relatively low cost of producing ancillary services when compared with daily hospital services.
The somewhat discretionary nature of ancillary service utilization.
The greater public scrutiny of costs for routine services than those for ancillary services.
Increased attention is now being given to ancillary services because of the concern about overutilization of these services. Variation in the use of ancillary services among physicians and hospitals indicates a lack of widespread standards for their use (Eisenberg, 1982).
Hospital ownership
Categories of hospital ownership include propriety, private nonprofit, and Government. Gross profits tend to be higher for proprietary hospitals than for nonprofit hospitals, indicating that costs are lower and/or charges are higher for these hospitals. For–profit hospitals have often been accused of “cream skimming” by selectively admitting only those patients who can be treated at acceptably high price-cost ratios. By such selective admissions, or by equipping themselves to provide only the most profitable services, hospitals could offer more competitive prices because they do not have to subsidize money-losing services (Bays, 1979).
Understanding the effects of hospital ownership on costs and pricing policies is becoming increasingly relevant. Proprietary hospitals have increased in number since the 1970's, and their growth is expected to continue. The effects of for–profit ownership are especially relevant in California because California has a larger number of investor-owned hospitals and beds than any other State in the country (White and Morse, 1981). A report on investor-owned and not-for–profit hospitals using 1979 California data concluded that costs and charges were higher in for–profit hospitals and that “for–profit chains have used aggressive marketing and price strategies to generate high rates of profitability and growth,”(Pattison and Katz, 1983).
Ownership effects may also become increasingly important as health care responsibilities become more decentralized. An illustration toward decentraling health care responsibilities is the shift of the California medically indigent adult program from the State to the county level, and State government contracting with particular hospitals under the California Medicaid (Medi-Cal) program. Ownership effects may have important implications in terms of the efficacy of direct provision of services versus contracting for services, and in the determination of the “best” settings for services to be provided.
In addition to having important policy implications, a better understanding of the effects that service composition and hospital ownership have on hospital charge structures can also be useful to the hospital industry itself, third-party payers, employers, consumers, and providers of health care. Among other things, such information would be valuable for hospital rate negotiations, the development of incentives for cost containment, and the determination of reimbursement policies.
Financial requirements
All hospitals, regardless of their ownership, must earn an excess of revenues over costs to continue operating. These “profits” are required to offset inflation, for technological improvements, expansion and/or change in services, allowance for working capital and changes in the physical plant. Charges must also exceed costs to help compensate for the often substantial deductions from revenue. Deductions from revenue include bad debts, charity care, and contractual allowances. They vary in size among hospitals depending on several factors, primarily the hospital's indigent population and its payer-mix composition.
Failure to distinguish operating costs from charges is a source of much confusion in discussions of hospital costs. Although “cost” is often used to refer to both, the words are not synonymous. “Costs” in this article refers to expenses incurred by the hospital. “Charges” is synonymous with gross revenues, or the amount billed to the patient, and usually exceeds the revenue actually received by the hospital (net revenue). As discussed later, the two do not necessarily vary directly nor do they have any uniform relationship.
Selective pricing
Potential profit is only one of several factors considered when deciding whether or not to offer a service and how to price it. Most hospitals practice selective pricing and use different criteria in the determination of charges for different departments and services. The vast majority of hospitals, both for–profit and nonprofit, provide some services for which gross revenue is less than costs. Among the reasons hospitals offer such money losing services are prestige, teaching and/or research functions, physician recruiting, attracting patients, or providing needed community services.
Methodology
Data
The data presented in this article were from sixth year hospital disclosure magnetic tapes. California hospitals are required by law to file these reports annually with the California Health Facilities Commission. The reports contain extensive financial and utilization information and are generally based on each facility's fiscal year. The sixth year disclosure reports are for fiscal years ending between June 30, 1980 and May 31, 1981.
Hospitals used in the analyses were general acute, short-term, and nonuniversity teaching facilities. Hospitals that changed ownership or filed incomplete reports were excluded. The total number of hospitals used in the analyses was 456, approximately 75 percent of California's general acute hospitals.
Services
Not all services for which data were provided were analyzed individually. The services chosen for individual analysis consisted of 8 of the 16 short-term daily hospital services and 15 of the 27 ancillary services.
Daily hospital services included in the article were medical and surgical, pediatric, psychiatric, obstetrics, intensive care, coronary intensive care, neonatal intensive care, and nursery. Those services excluded1 from the study were rehabilitation, definitive observation, pediatric intensive care, burn care, residential, psychiatric (adolescent and pediatric), other acute care, and psychiatric isolation.
Ancillary services included in the article were labor and delivery, surgery and recovery, anesthesiology, central services and supplies, pharmacy, clinical laboratories, electrocardiology, cardiac catheterization lab, diagnostic radiology, computed tomographic scanner, nuclear medicine, inhalation therapy, electroencephalography, physical therapy, and occupational therapy. Those services excluded were emergency, clinics, surgical day care, ambulance, home health, pathological laboratories, blood bank, therapeutic radiology, pulmonary laboratories, electromyography, and dialysis. Only the services with the largest and most prevalent utilization in California hospitals are presented in this article.
Ownership groups
Hospitals were separated into 4 ownership groups: private nonprofit, proprietary, district, and county. The district hospital group included both district and city hospitals, and the county hospital group included city as well as county hospitals. The sample was comprised of 207 nonprofit, 141 proprietary, 72 district, and 36 county hospitals.
Statistical analysis
Examination of subgroup means was used as the primary method of determining the presence of statistically significant relationships among hospital groups. This statistical method, with the use of one way analysis of variance (ANOVA), was used to determine the statistical significance of the differences among subpopulation means. Bivariate analysis was also used to examine the effects of various factors while controlling for size differences. Hospital bed size was not found to be a confounding factor because when economies of scale were examined overall hospital size was not statistically significant (Eskoz, 1983). The computer analyses were performed using the statistical package for the social services (SPSS). The level of significance at which the null hypotheses were rejected was p<.01. Tables present only results which met this statistical criterion.
Limitations of study
One problem inherent in the study, which this article presents, was the complicating effects of patient case-mix differences among hospitals (i.e., the differences in severity of illness). Using hospital bed size as a proxy for case-mix intensity levels (i.e., holding bed size constant for comparisons) was examined, but was found to be inappropriate. Although university teaching hospitals, which have higher than average case-mix intensities, were excluded. No other adjustments were made to account for these case-mix differences. Another problem was the lack of conformity among hospital reporting periods (each Disclosure Report was based on the hospital's own fiscal year). These time differences, however, were assumed to have minimal effects on the findings.
The data presented were from California hospitals only, although we know of no reasons why the findings would not be similar for hospitals in other States or for the hospital industry as a whole. All the analyses used mean values for the dependent and independent variables. The findings are not necessarily true for each individual hospital, but rather are generalizations found to hold true on average.
Results
Service profit margins
Both the gross and net profit margins of services varied widely, as can be seen by the large standard deviations shown in Tables 1 and 2. As expected, ancillary services had the highest profit margins, and daily hospital services had the lowest. As Table 1 illustrates, the mean gross profit margins (gross profit divided by gross revenue) for the 23 services examined ranged from −88 percent for labor and delivery services to 54 percent for electrocardiology. Only 3 (38 percent) of the 8 daily hospital services (psychiatric, medical and surgical, and newborn intensive care) had positive gross profit margins, whereas 12 (80 percent) of the 15 ancillary services had positive gross profit margins. The 3 ancillary services for which gross profit margins were negative included labor and delivery (−88 percent), occupational therapy (−27.5 percent) and surgery and recovery (−4.8 percent).
Table 1. Mean gross profit margins for ancillary and daily hospital services and hospitals with positive gross profit margins by type of service.
| Type of service | Gross profit margins | Hospitals with positive gross profit margins | |
|---|---|---|---|
|
| |||
| Mean | Standard deviation | ||
|
| |||
| Percent | |||
| Electrocardiology | 54.2 | 24.2 | 98 |
| Pharmacy | 47.0 | 20.8 | 98 |
| Anesthesiology | 41.4 | 76.2 | 88 |
| Central services and supplies | 37.6 | 35.1 | 94 |
| Inhalation therapy | 33.3 | 44.6 | 95 |
| CT scanning1 | 30.8 | 43.5 | 83 |
| Clinical laboratory | 25.3 | 43.7 | 93 |
| Electroencephalography | 29.8 | 56.5 | 83 |
| Nuclear medicine | 17.3 | 52.2 | 79 |
| Diagnostic radiology | 16.4 | 52.9 | 86 |
| Cardiac catheterization | 15.5 | 40.1 | 81 |
| Psychiatric | 3.7 | 29.9 | 66 |
| Medical and surgical | 3.4 | 25.4 | 68 |
| Newborn intensive care | 0.8 | 66.2 | 67 |
| Physical therapy | 0.1 | 99.0 | 72 |
| Surgery and recovery | −4.8 | 49.9 | 59 |
| Coronary intensive care | −5.3 | 31.1 | 48 |
| Intensive care | −14.8 | 41.2 | 40 |
| Obstetrics | −17.1 | 235.0 | 44 |
| Nursery | −23.8 | 66.2 | 42 |
| Pediatrics | −25.4 | 90.3 | 42 |
| Occupational therapy | −27.5 | 195.0 | 56 |
| Labor and delivery | −88.1 | 132.0 | 18 |
Computed tomography scanning.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
Table 2. Mean net profit margins for ancillary and daily hospital services and hospitals with positive net profit margins, by type of service.
| Type of service | Net profit margins | Hospitals with positive net profit margins | |
|---|---|---|---|
|
| |||
| Mean | Standard deviation | ||
| Electrocardiology | 16.5 | 24.1 | 82 |
| Pharmacy | 30.8 | 21.9 | 95 |
| Anesthesiology | 20.5 | 82.9 | 78 |
| Central services and supplies | 21.6 | 34.6 | 85 |
| Inhalation therapy | 17.0 | 43.5 | 87 |
| CT scanning1 | 5.0 | 44.8 | 64 |
| Clinical laboratory | 3.6 | 41.9 | 72 |
| Electroencephalography | −12.9 | 55.0 | 39 |
| Nuclear medicine | −13.5 | 50.5 | 42 |
| Diagnostic radiology | −13.1 | 53.4 | 36 |
| Cardiac catheterization | −6.4 | 48.8 | 56 |
| Psychiatric | −15.7 | 34.1 | 30 |
| Medical and surgical | −11.0 | 29.2 | 32 |
| Newborn intensive care | −22.8 | 52.1 | 33 |
| Physical therapy | −7.1 | 49.3 | 43 |
| Surgery and recovery | −20.2 | 49.5 | 37 |
| Coronary intensive care | −22.8 | 31.3 | 17 |
| Intensive care | −28.8 | 39.9 | 8 |
| Obstetrics | −48.3 | 76.6 | 18 |
| Nursery | −47.9 | 46.4 | 24 |
| Pediatrics | −32.6 | 76.1 | 25 |
| Occupational therapy | −29.9 | 31.6 | 35 |
| Labor and delivery | −127.0 | 459.0 | 7 |
Computed tomography scanning
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
The services with the highest gross profit margins were electrocardiology (54.2 percent), pharmacy (47.0 percent), anesthesiology (41.4 percent), central services and supplies (37.6 percent), and inhalation therapy (33.3 percent). The services with the lowest gross profit margins were labor and delivery (−88.1 percent), occupational therapy (−27.5 percent), pediatrics (−25.4 percent), and nursery (−23.8 percent). There were 10 services (all ancillary services) for which 80 percent or more of the hospitals had positive gross profit margins. The services for which the greatest percentage of hospitals had positive gross profit margins were pharmacy (98 percent), electrocardiology (98 percent), and inhalation therapy, (95 percent). The services for which the fewest hospitals had positive gross profit margins were labor and delivery (18 percent) and intensive care (40 percent).
It is interesting to note that there were no services for which all hospitals had positive gross profits. At least 2 percent of all the hospitals had negative gross profits (i.e., losses) for each of the services, even those with the highest gross profit margins such as electrocardiology and pharmacy.
Net profits, defined as gross profits minus deductions from revenue, showed a distribution similar to that of gross profits. Table 2 lists net profit margins, which ranged from −127 percent for labor and delivery to 21.6 percent for central services and supplies. Like gross profit margins, net profit margins were highest for ancillary services and lowest for daily hospital services. The average net profit margin for total daily hospital services was −14.1 percent, and was 9.3 percent for total ancillary services. There were no positive net profit margins for any of the daily hospital services. Of the 15 ancillary services, 7 services had positive net profit margins.
The mean charge per day was $232 for ancillary services and $ 188 for daily hospital services. Thus, 44.7 percent of total gross patient revenue came from daily hospital services and 55.3 percent from ancillary services, with charges per day being 23 percent higher for ancillary services than for daily hospital services. The larger percentage of patient revenue attributable to ancillary services than to daily hospital service, along with the large differences between profit margins of the 2 service categories, indicate that there is cross-subsidization between ancillary and daily hospital services.
Ownership differences
There were significant differences in service profit margins among types of hospital ownership. As is shown in Table 3, the mean net profits per unit differed significantly among ownership groups for both total daily hospital services and total ancillary services. Net profits for total ancillary services were highest at proprietary hospitals and lowest at county hospitals. Net profits for daily hospital services, which were actually losses because they were negative, were highest at not-for-profit hospitals and lowest at county hospitals.
Table 3. Average net profit margins for ancillary and daily hospital services, by type of hospital ownership and type of service.
| Type of service | Type of hospital ownership | Level of significance P | Standard deviation | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| All | Private nonprofit | For–profit | District | County | |||
|
| |||||||
| Percent | |||||||
| Daily hospital services | −15.8 | −10.9 | −20.6 | −16.0 | −24.8 | <0.001 | 23.2 |
| Total ancillary services1 | 9.3 | 8.2 | 17.3 | 7.3 | −12.1 | <0.001 | 22.4 |
Includes only the 15 ancillary services examined individually.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
Mean net profit per unit service for each of 4 ownership groups were analyzed. Although a high degree of variation with groups was evident, there were statistically significant differences for the net profits of the 9 individual services shown in Table 4. Proprietary hospitals had either the highest or lowest net profits per unit service for each of these 9 services. Proprietary hospitals' net profits per unit were lowest for 3 of the 4 daily hospital services, and were highest for 4 of the 5 ancillary services. The reverse was true for the remaining service in each service category where proprietary hospitals had the lowest net profit per unit for labor and delivery (−$244), and the highest net profit per day for psychiatric services ($3.36). There was no common ranking of profit margin among hospital ownership types for the daily hospital services. However, for the 5 ancillary services, net profits per unit ranked from highest to lowest among ownership groups in the following order—proprietary, private nonprofit, district, and county hospitals.
Table 4. Statistically significant1 differences in mean net profits per unit for ancillary and daily hospital services, by type of hospital ownership and type of service.
| Type of service | Type of hospital ownership | All hospitals | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Private nonprofit | Proprietary | District | County | Mean | Standard deviation | |
|
| ||||||
| Mean net profit | ||||||
| Medical and surgical | −$12 | −$31 | −$19 | −$30 | $20 | $42 |
| Psychiatric | −13 | 3 | −14 | −78 | −25 | 53 |
| Intensive care | −109 | −167 | −50 | −130 | −121 | 133 |
| Coronary intensive care | −66 | −157 | −40 | −114 | −86 | 104 |
| Labor and delivery | −158 | −244 | −145 | −209 | −177 | 173 |
| Central services and supplies | 7 | 17 | 7 | 1 | 10 | 12 |
| Pharmacy | 15 | 27 | 12 | 4 | 17 | 14 |
| Electrocardiology | 6 | 12 | 9 | 3 | 8 | 11 |
| Inhalation therapy | 5 | 6 | 3 | 0 | 5 | 9 |
Level of significance is p<.001.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
Costs
The higher net profit margin of ancillary services at proprietary hospitals was not related to significant differences in operating costs among ownership groups. Contrary to expectations, neither direct costs nor total costs per unit for total ancillary services differed significantly among types of ownership. Proprietary hospitals did not appear to be more cost efficient than hospitals of other ownership types as it is often claimed, and in fact this group had the highest mean costs for most of the services for which significant cost differences among types of ownership were found.
As seen in Table 5, differences in direct costs per unit among ownership groups were statistically significant for only 5 of the individual services. Only 2 of these were ancillary services (pharmacy and labor and delivery), and proprietary hospitals had the highest and second highest direct costs per unit, respectively, for these services.
Table 5. Statistically significant1 differences in mean direct costs per unit for ancillary and daily hospital services, by type of hospital ownership and type of service.
| Type of service | Type of hospital ownership | All hospitals | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Private nonprofit | Proprietary | District | County | Mean | Standard deviation | |
|
| ||||||
| Mean direct cost | ||||||
| Intensive care | $267 | $290 | $222 | $243 | $267 | $91 |
| Coronary intensive care | 251 | 289 | 196 | 265 | 253 | 81 |
| Pediatrics | 95 | 76 | 69 | 88 | 85 | 40 |
| Labor and delivery | 213 | 195 | 126 | 181 | 188 | 112 |
| Pharmacy | 10 | 14 | 10 | 8 | 11 | 7 |
The level of significance is p<.001.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
The differences among ownership groups were statistically significant for total daily hospital services' direct costs per day. These costs were highest at forprofit hospitals and lowest at district hospitals. The differences in total costs per unit among types of ownership were statistically significant for only 4 services; but after controlling for hospital bed size, the differences were no longer statistically significant.
Higher average costs at proprietary hospitals were also indicated by the relatively large average percentage of gross patient revenue represented by contractual allowances. Deductions from revenue were 10.1 percent at proprietary hospitals, the second highest percentage among the 4 ownership groups. Contractual allowances were highest at county hospitals, where they averaged 12.2 percent of gross revenue. The percent of total revenue derived from cost-based payers at proprietary institutions (30.2 percent), however, was similar to the average for all hospitals (30.5 percent). It appears that contractual allowances, relative to the percent of cost-based payers, were higher at proprietary hospitals. Large deductions from revenue are because either a large percentage of Medicare or Medi–cal patients, and/or to many disallowed costs. Because the average percent of revenue from cost-based payers was not significantly higher at proprietary hospitals, the high level of contractual allowances must have been the result of higher-than-average-costs and thus many disallowed costs.
Charges
Table 6 displays the differences in the mean charges per unit among ownership groups that were significant for both total daily hospital services and total ancillary services. For–profit hospitals ranked highest in mean charges. The contrast between proprietary and other groups is particularly wide for ancillary services. Proprietary hospitals averaged $303 per unit whereas the next highest group, nonprofit, averaged only $218 per unit.
Table 6. Mean charge per unit for ancillary and daily hospital services, by type of hospital ownership and type of service.
| Type of service | Type of hospital ownership | All hospitals | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Private nonprofit | Proprietary | District | County | Mean | Standard deviation | |
|
| ||||||
| Charge per unit | ||||||
| Total daily hospital services1 | $193 | $197 | $157 | $179 | $188 | $43 |
| Total ancillary services | 218 | 303 | 175 | 151 | 232 | 187 |
Statistical difference is p <.001.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
Table 7 shows the 15 services for which the differences in average charge per unit among types of ownership were significant. These included 7 of the 8 daily hospitals (psychiatric charges per day were not significantly different) and 8 ancillary services. The charges per unit for 3 services (nursery, anesthesiology, and obstetrics) were no longer statistically significant after controlling for hospital bed size. Average charges per unit were highest at proprietary hospitals for 16 of the 23 services. District hospitals had the lowest charges per unit for all 8 daily hospital services and for 2 ancillary services (labor and delivery, and surgery and recovery). County hospitals had the lowest charges per unit for 4 of 8 ancillary services where differences were found to be significantly different.
Table 7. Statistically significant1 differences in mean charges, per unit by type of hospital ownership and type of service.
| Type of service | Type of hospital ownership | All hospitals | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Private nonprofit | Proprietary | District | County | Mean | Standard deviation | |
|
|
|
|
|
|
|
|
| (N = 207) | (N = 141) | (N = 72) | (N = 36) | (N = 456) | ||
| Medical and surgical | $166 | $170 | $143 | $166 | $164 | $30 |
| Obstetrics2 | 164 | 158 | 141 | 162 | 158 | 47 |
| Pediatrics | 167 | 159 | 149 | 199 | 165 | 60 |
| Intensive care | 399 | 412 | 349 | 399 | 397 | 95 |
| Coronary intensive care | 412 | 430 | 332 | 436 | 407 | 109 |
| Newborn intensive care | 398 | 540 | 280 | 324 | 383 | 97 |
| Nursery2 | 105 | 96 | 85 | 105 | 99 | 30 |
| Labor and delivery | 269 | 198 | 189 | 254 | 237 | 124 |
| Surgery and recovery | 6 | 6 | 5 | 7 | 6 | 4 |
| Anesthesiology2 | 1 | 1 | 2 | 2 | 2 | 1 |
| Central services and supplies | 29 | 45 | 26 | 20 | 33 | 20 |
| Pharmacy | 44 | 70 | 35 | 28 | 49 | 26 |
| Electrocardiology | 45 | 55 | 41 | 33 | 47 | 20 |
| Diagnostic radiology | 10 | 13 | 9 | 9 | 1 | 11 |
| Inhalation therapy | 25 | 31 | 24 | 24 | 27 | 17 |
Level of significance is p <.001.
Differences are not statistically significant when hospital size is held constant.
SOURCE: California Health Facilities Commission, Hospital Financial Disclosure Tape, Sixth Reporting Year, Fiscal Year June 30, 1980, to May 31, 1981.
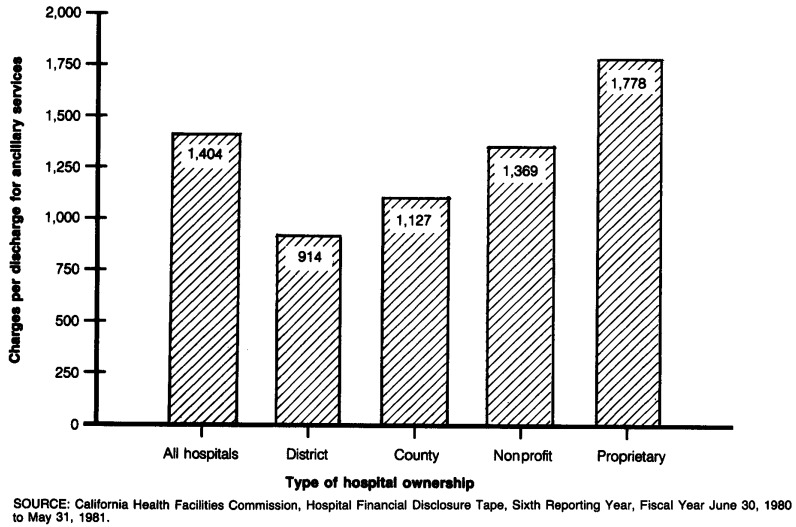
The average charge per discharge for ancillary services differed significantly among ownership types. Figure 1 illustrates the variation among ownership types with respect to their dependence on ancillary services as a source of revenue. Ancillary service charges per discharge were highest at proprietary hospitals ($1,778) and lowest at district hospitals ($914), which represents nearly a twofold difference. As shown in Table 8, charges per discharge increased with hospital bed size with proprietary hospitals significantly higher in all categories.
Figure 1. Charges per discharge for ancillary services, by type of hospital ownership.
Table 8. Mean total ancillary service charges per discharge, by type of hospital ownership and hospital size.
| Hospital size | Type of hospital ownership | All hospitals | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Private nonprofit | Proprietary | District | County | Mean2 | Standard deviation | |
| Total | $1,369 | $1,778 | $ 914 | $1,127 | $1,404 | $687 |
| Less than 150 beds | 1,187 | 1,679 | 868 | 1,012 | 1,296 | 735 |
| 150 - 400 beds | 1,471 | 2,005 | 1,108 | 1,094 | 1,544 | 579 |
| 400 beds or more | 1,762 | 12,947 | 918 | 1,461 | 1,623 | 602 |
There was only one proprietary hospital in the sample with 400 beds or more.
Difference in means is significant at p <.001.
Conclusion
Both service composition and type of ownership have significant relationships on hospital charges and should continue to be examined in cost containment efforts. The composition of ancillary services should be of particular interest. The finding that 55.3 percent of total gross patient revenues came from ancillary services and the larger differences in profit margins for these services may have important policy implications for both cost containment and utilization review. Because ancillary services make up the majority of the average hospital bill, they are the area where cost containment efforts should focus more attention. In addition to the greater relative costliness of ancillary services, utilization of these services is more discretionary than that of daily hospital services and can potentially be more easily influenced by cost controls and incentives. The greater profit margin and variation in utilization of ancillary services also imply that there is an important role for utilization review for these services. In addition to higher charges, overutilization of ancillary services has several other important implications for the patient such as greater risk of nosocomial infections, increased inconvenience, and psychological and/or physical discomfort.
The increased competitiveness and changes in public and private reimbursement policies will result in major changes in the practices of hospitals. The sources of revenue, in terms of the number and types of services, will likely change. Some of these recent changes in the reimbursement system provide incentives for lower ancillary service utilization. All-inclusive rates, such as per diem rates or those based on diagnostic-related groups (DRG's), which are used for Medicare inpatient reimbursement, should serve to discourage overutilization of services. Because proprietary hospitals as a group are the most dependent on ancillary services and higher-than-average charges for revenue services, they may be most affected by the recent changes in reimbursement. It will be of interest to monitor changes in the proportion of total patient revenue derived from ancillary services after these non-cost-based reimbursement mechanisms take effect.
Preferred provider organizations (PPO's) and other rate-negotiating organizations should be aware of the potential differences in charges among ownership groups as well as the significance of ancillary services as revenue generators. If significant differences in charges or utilization of ancillary services exist, then it will be ineffective to solely rely on discounted rates based on a fixed percent of charges. A comparative analysis of overall charges within each local area is necessary because even discounted charges of some hospitals may be higher than undiscounted charges of other hospitals. Ancillary services as well as routine daily services must be considered in rate negotiations and utilization reviews of hospitals.
Under prospective reimbursement systems, hospital charges will not be as important as they were previously, because fewer and fewer patients will pay on the basis of undiscounted or other nonprospectively–set rates. Those who continue to pay on the basis of charges, however, may face even greater than usual charge increases because hospitals may find it necessary to offset revenue lost from prospectively-set rates, and there will be fewer charge paying patients among which to allocate increased revenue needs. The likely “victims” will be small insurance companies and self-insured employers too small to effectively negotiate discounted rates.
Footnotes
Reprint requests: K. Michael Peddecord, Assistant Professor, Graduate School of Public Health, College of Human Services, San Diego State University, San Diego, California 92182.
All services were included in the averages for total daily hospital services and total ancillary services, unless otherwise specified.
References
- Bays C. Cost companions of for-profit and nonprofit hospitals. Social Science and Medicine. 1979;13C(4):311–321. doi: 10.1016/0160-7995(79)90003-0. [DOI] [PubMed] [Google Scholar]
- California Health Facilities Commission. Financial and Utilization Data, Fourth Quarter. Sacramento, Calif.: 1982. Apr 14, 1983. [Google Scholar]
- Eisenberg J. The use of ancillary services: A role for utilization review? Med Care. 1982;20(8):849–861. doi: 10.1097/00005650-198208000-00009. [DOI] [PubMed] [Google Scholar]
- Eskoz R. Masters thesis. San Diego State University; San Diego, Calif.: 1983. The function of ancillary services in hospital charge structures. [Google Scholar]
- Pattison RV, Katz HM. Investor-owned and not-for-profit hospitals: A comparsion based on California data. N Engl J Med. 1983;309(6):347–353. doi: 10.1056/NEJM198308113090606. [DOI] [PubMed] [Google Scholar]
- Siafaca E. Investor-owned Hospitals and Their Role in the Changing US Health Care System. New York: F and S Press, A Division of Frost and Sullivan; 1981. [Google Scholar]
- White C, Morse L. Hospital Fact Book, 1981. California Hospital Association; Sacramento, Calif.: 1981. [Google Scholar]