Abstract
Spending per capita for health care in the United States varies dramatically by State and region. In 1982, personal health care costs per capita ranged from a low of $857 in South Carolina to a high of $1,508 in Massachusetts. The focus of this article is State and regional variation in spending levels and the mix of health care services purchased. Possible causes for these differences are presented.
Introduction
Expenditures for personal health care include spending for hospital care, physicians' services, dentists' services, drugs, eyeglasses, and nursing home care. Levels of spending, growth in spending over time, and the mix of services purchased with the health care dollar vary considerably among States and regions. Health care prices and the extent of health care use have grown rapidly in recent years, placing severe strain on the ability of governments and individuals to finance that care. In an effort to contribute to an understanding of the problems faced by health care financers, estimates of personal health care spending by State for selected years from 1966 through 1982 are presented in this report, and some of the differences that exist in spending patterns by geographic area are examined.
National health expenditures (NHE) is a measure of the costs of health care in the United States (Gibson et al., 1984). NHE categories, or accounts, are constructed in a matrix showing expenditure levels and sources of payment for medical services and goods. NHE accounts include not only personal health care expenditures but also estimates of expenditures for public health programs, administration, research, and construction of health facilities. State expenditures for personal health care services presented in this report are directly linked to the NHE. Whenever possible, the same definitions, methods, and data sources are used for State estimates as for national estimates. (See “Definitions and methodology.”)
The data in this report are presented by economic region and State. The economic regions, which represent groups of economically interdependent States, were developed by the Bureau of Economic Analysis in the U.S. Department of Commerce. These regional groupings were chosen instead of administrative regions used by the Health Care Financing Administration or Bureau of the Census regions because the analysis of economically interdependent areas should demonstrate the strongest, most homogeneous spending patterns within regions.
The per capita estimates presented in this article, although useful in the determination of spending trends and levels, should not be interpreted as spending per resident. Per capita figures are derived by dividing total spending in a State by the State's population, but total spending in a State (“place of service”) does not necessarily equal total spending by residents of a State (“place of residence”).
The presentation of estimates by place of service is dictated by the availability of data. For the most part, estimates shown in this article are based on aggregations of providers' total incomes. By their nature, these aggregations group expenditures geographically by the location of the provider, because individual patient data are never reported.
Unfortunately, there are few sources of information that could lead to place-of-residence spending estimates. For the most part, financial data are reported by provider rather than by recipient. Surveys of recipients, such as the National Medical Care Expenditure Survey, are based on samples drawn principally to facilitate demographic comparisons rather than State comparisons. The one sample large enough to allow State comparisons to be made comes from the Medicare Statistical System (Lave, Dobson, and Walton, 1983).
Spending by place of residence can be higher or lower than spending by place of service, depending upon the relative size of “imports” (out-of-State spending by State residents) and “exports” (in-State spending by out-of-State residents). The relationship between place-of-service and place-of-residence spending is illustrated in Table 1. In this example, per capita figures by place of service are adjusted to a place-of-residence basis by excluding spending by out-of-State residents and including out-of-State spending by State residents. Using this method, per capita charges for short-stay hospital services rendered to aged Medicare beneficiaries in the District of Columbia declines from $2,061 on a place-of-service basis to $1,553 on a place-of-residence basis. Conversely, in Wyoming per capita charges rise from $715 on a place-of-service basis to $891 on a place-of-residence basis.
Table 1. Relationship of spending by place of service and place of residence for short-stay hospital covered charges of persons 65 years of age or over enrolled in Medicare Part A: District of Columbia and Wyoming, 1980.
| Statistic | District of Columbia | Wyoming |
|---|---|---|
| Amount in thousands | ||
| Spending by place of service | $136,990 | $26,921 |
| Less: spending in State by nonresidents | 43,579 | 1,903 |
| Subtotal | 93,411 | 25,018 |
| Plus: out-of-State spending by residents | 9,814 | 8,566 |
| Equals: spending by place of residence | 103,225 | 33,584 |
| Amount per enrollee | ||
| Place-of-service spending | 2,061 | 715 |
| Place-of-residence spending | 1,553 | 891 |
| Percent | ||
| Ratio of place-of-residence spending to place-of-service spending | 75.4 | 124.8 |
| Number | ||
| Aged hospital insurance enrollees, July 1980 | 66,467 | 37,659 |
NOTE: The District of Columbia and Wyoming have the lowest and highest ratios of place-of-residence to place-of-service spending and were chosen to illustrate the relationship.
SOURCE: Health Care Financing Administration: Medicare Statistical System, Inpatient Stay Record File.
Table 2 shows the relationship of Medicare-covered short-stay hospital charges for aged beneficiaries by place of service (column A) and by place of residence (column B) in 1980. The third column of the table shows the percentage of residents' care purchased in another State; it ranges from a low of 1.6 percent in California to a high of 25.5 percent in Wyoming. The fourth column shows the percentage of hospital care provided in a State but used by out-of-State residents. This ranges from 2.5 percent of Michigan hospital care services to 31.8 percent of District of Columbia hospital services. In the fifth column, place-of-residence spending is expressed as a percentage of place-of-service spending. Ratios range from 75.4 percent in the District of Columbia to 124.7 percent in Wyoming. Although the migration patterns of Medicare enrollees do not necessarily match those of the general population, Table 2 illustrates the type of variation one might expect to find when comparing hospital care expenditures by State on a place-of-service and place-of-residence basis.
Table 2. Place-of-service and place-of-residence statistics on short-stay hospital covered charges of persons 65 years of age or over enrolled in Medicare Part A, by State: 1980.
| State | Covered charges | Percent of column B purchased out of State | Percent of column A sold to out-of-State residents | Ratio of column B to column A (times 100) | |
|---|---|---|---|---|---|
|
| |||||
| By place of service (column A) | By place of residence (column B) | ||||
|
| |||||
| Thousands of dollars | |||||
| Alabama | $462,869 | $471,719 | 6.4 | 4.6 | 101.9 |
| Alaska | 10,163 | 10,989 | 14.7 | 7.8 | 108.1 |
| Arizona | 285,804 | 279,295 | 8.5 | 10.6 | 97.7 |
| Arkansas | 257,956 | 273,265 | 13.0 | 7.8 | 105.9 |
| California | 3,042,994 | 3,004,970 | 1.6 | 2.8 | 98.8 |
| Colorado | 261,601 | 250,002 | 4.4 | 8.7 | 95.6 |
| Connecticut | 332,615 | 337,736 | 6.2 | 4.8 | 101.5 |
| Delaware | 59,537 | 62,513 | 13.3 | 8.9 | 105.0 |
| District of Columbia | 136,990 | 103,225 | 9.5 | 31.8 | 75.4 |
| Florida | 1,774,101 | 1,735,760 | 7.2 | 9.2 | 97.8 |
| Georgia | 443,609 | 438,524 | 6.3 | 7.4 | 98.9 |
| Hawaii | 56,064 | 54,793 | 2.8 | 5.0 | 97.7 |
| Idaho | 62,819 | 70,495 | 16.9 | 6.7 | 112.2 |
| Illinois | 1,690,307 | 1,737,781 | 6.0 | 3.4 | 102.8 |
| Indiana | 533,240 | 534,503 | 7.4 | 7.2 | 100.2 |
| Iowa | 344,257 | 358,405 | 10.5 | 6.8 | 104.1 |
| Kansas | 307,776 | 330,808 | 12.1 | 5.5 | 107.5 |
| Kentucky | 320,882 | 335,794 | 9.8 | 5.6 | 104.6 |
| Louisiana | 389,053 | 385,673 | 4.1 | 5.0 | 99.1 |
| Maine | 137,961 | 144,018 | 8.4 | 4.4 | 104.4 |
| Maryland | 387,273 | 403,038 | 11.5 | 7.9 | 104.1 |
| Massachusetts | 940,143 | 909,240 | 2.6 | 5.8 | 96.7 |
| Michigan | 1,184,680 | 1,210,844 | 4.6 | 2.5 | 102.2 |
| Minnesota | 453,224 | 433,538 | 6.6 | 10.6 | 95.7 |
| Mississippi | 246,175 | 265,385 | 12.6 | 5.8 | 107.8 |
| Missouri | 771,565 | 737,933 | 5.2 | 9.3 | 95.6 |
| Montana | 69,848 | 73,435 | 10.4 | 5.8 | 105.1 |
| Nebraska | 206,005 | 202,442 | 8.3 | 9.9 | 98.3 |
| Nevada | 100,088 | 95,709 | 9.5 | 13.5 | 95.6 |
| New Hampshire | 86,623 | 91,411 | 18.7 | 14.2 | 105.5 |
| New Jersey | 936,611 | 1,001,530 | 10.5 | 4.3 | 106.9 |
| New Mexico | $90,181 | $98,080 | 15.0 | 7.6 | 108.8 |
| New York | 2,605,638 | 2,601,589 | 4.0 | 4.1 | 99.8 |
| North Carolina | 459,943 | 461,343 | 5.7 | 5.4 | 100.3 |
| North Dakota | 84,084 | 76,950 | 10.4 | 18.0 | 91.5 |
| Ohio | 1,274,036 | 1,272,930 | 4.6 | 4.7 | 99.9 |
| Oklahoma | 356,333 | 372,265 | 7.8 | 3.7 | 104.5 |
| Oregon | 268,830 | 264,722 | 5.3 | 6.7 | 98.5 |
| Pennsylvania | 1,957,056 | 1,935,744 | 3.6 | 4.6 | 98.9 |
| Rhode Island | 125,154 | 124,911 | 6.9 | 7.1 | 99.8 |
| South Carolina | 207,608 | 222,578 | 10.6 | 4.2 | 107.2 |
| South Dakota | 79,019 | 82,194 | 14.0 | 10.6 | 104.0 |
| Tennessee | 581,856 | 521,561 | 3.8 | 13.8 | 89.6 |
| Texas | 1,317,130 | 1,278,016 | 2.4 | 5.3 | 97.0 |
| Utah | 86,853 | 81,394 | 4.9 | 10.9 | 93.7 |
| Vermont | 46,495 | 51,753 | 21.9 | 13.0 | 111.3 |
| Virginia | 488,037 | 494,838 | 8.3 | 7.0 | 101.4 |
| Washington | 324,081 | 323,275 | 5.6 | 5.8 | 99.8 |
| West Virginia | 230,941 | 238,283 | 14.0 | 11.3 | 103.2 |
| Wisconsin | 521,622 | 527,473 | 6.1 | 5.1 | 101.1 |
| Wyoming | 26,921 | 33,584 | 25.5 | 7.1 | 124.7 |
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Medicare Statistical System.
These migration patterns apply to short-stay hospitals only. Preliminary evidence suggests a very different pattern of migration for skilled nursing care for elderly Medicare beneficiaries. One would expect that migration patterns for other services would vary as well.
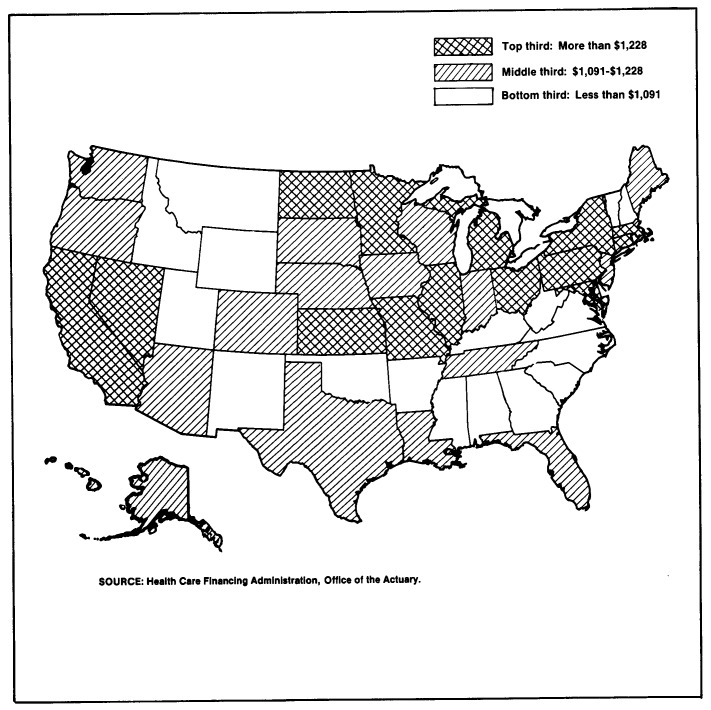
In this article, per capita estimates are presented to permit comparison of spending levels among States and regions (Figure 1), because the influences of population size and differential population growth are eliminated from such estimates. Per capita estimates for the District of Columbia are not presented or considered in discussions of State spending. In this small, totally metropolitan area, significant proportions of hospital, physician, and dental services, as well as durable and nondurable medical goods, are provided to residents of Maryland and Virginia. Per capita spending in the District of Columbia is thus significantly inflated by out-of-State health care purchases. However, these estimates are included in all regional-level calculations where interstate flows are not significant.
Figure 1. Per capita expenditures for personal health care, by State: Calendar year 1982.
National trends
From 1966 to 1982, personal health expenditures in the United States grew from $39.3 to $282.8 billion at an average annual rate of 13.1 percent. Increases in the proportion of spending for institutional services (those services included in NHE hospital and nursing home categories) dominated the health industry. The Nation's bill for hospital care grew at 14.4 percent per year and the bill for nursing homes at 16.3 percent per year through the 16-year period. In 1966, 45.7 percent of all personal care services went for institutional care. By 1982, hospital and nursing home spending accounted for 56.6 percent of all expenditures (Table 3). At the same time, the percentage of health expenditures for the purchase of drugs and medical sundries declined from 13.9 percent to 7.7 percent. Much of this decline can be attributed to a slower growth rate in drug prices than in prices for overall health care.
Table 3. Percent distribution of personal health care expenditures, by type of expenditure: Selected calendar years 1966-82.
| Type of expenditure | 1966 | 1969 | 1972 | 1976 | 1979 | 1982 |
|---|---|---|---|---|---|---|
|
| ||||||
| Percent distribution | ||||||
| Total personal health care | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| All institutional care | 45.7 | 49.1 | 51.8 | 54.3 | 55.0 | 56.6 |
| Hospital care | 39.7 | 42.4 | 43.6 | 45.7 | 45.7 | 47.3 |
| Nursing home care | 6.0 | 6.7 | 8.2 | 8.6 | 9.3 | 9.4 |
| Physicians' services | 23.4 | 22.4 | 21.5 | 21.0 | 21.4 | 21.8 |
| Dentists' services | 7.5 | 7.4 | 7.1 | 7.2 | 7.1 | 6.9 |
| Other professional services | 3.0 | 2.6 | 2.3 | 2.4 | 2.5 | 2.5 |
| Drugs and medical sundries | 13.9 | 12.7 | 11.7 | 9.9 | 9.1 | 7.7 |
| Eyeglasses and appliances | 3.3 | 3.0 | 2.8 | 2.6 | 2.5 | 1.9 |
| Other health services | 3.1 | 2.8 | 2.8 | 2.6 | 2.5 | 2.5 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Methods of financing health care shifted during the period 1966-82. In 1966, the consumer paid directly for one-half of all health care spending, with the other one-half financed about equally by insurance and public programs. By 1982, public programs accounted for almost 40 percent of all spending; insurance, 32 percent; and the consumer, 27 percent (Table 4).
Table 4. Percent distribution of personal health care expenditures, by source of funds: Selected calendar years 1966-82.
| Source of funds | 1966 | 1969 | 1972 | 1976 | 1979 | 1982 |
|---|---|---|---|---|---|---|
|
| ||||||
| Percent distribution | ||||||
| Personal health care | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Direct consumer payments | 49.5 | 40.4 | 38.0 | 31.6 | 29.4 | 27.1 |
| Private health insurance | 22.9 | 22.7 | 23.6 | 28.3 | 30.0 | 31.9 |
| Other private payments | 2.1 | 1.6 | 2.5 | 1.4 | 1.2 | 1.2 |
| Public payments | 25.5 | 35.3 | 35.8 | 38.7 | 39.3 | 39.8 |
| Federal Government | 13.2 | 23.1 | 23.5 | 27.2 | 28.1 | 29.5 |
| State and local government | 12.3 | 12.3 | 12.3 | 11.5 | 11.2 | 10.3 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
The shift of payment responsibility from the consumer to “third parties” such as government and insurance companies alters the interaction among supply, demand, and prices. The consumer, who pays only a fraction of the cost of most services at the point of purchase, perceives the price of services to be lower than it really is. In some cases, such as hospital care, services cost the consumer only a small proportion of the actual cost at the point of purchase, because public programs and private insurance pay most of the costs, 91 percent in 1982 (Gibson et al., 1984).
An example of this phenomenon can be seen in the increase in the proportion of health spending for institutional services that coincided with the implementation of the Medicaid and Medicare programs. These two programs combined, financing 36 percent of all hospital and 46 percent of all nursing home care in 1982, have been instrumental in the rapid increase in spending for institutional services.
Of particular concern in recent years is the rapid increase in Medicare funding of hospital care for the elderly and disabled. During the period 1969-82, hospital care financing by Medicare grew at a rate of 17.4 percent per year to a level of $36.7 billion, representing 27 percent of all hospital care spending. This dramatic growth prompted legislation to reform the Medicare reimbursement system through prospective payment. The prospective payment policy would allow the Medicare program to set the level of hospital reimbursement in advance and would be based primarily on the diagnosed illness of a patient. The aim of prospective payment is to force hospitals to choose the most cost-effective course of treatment but insure that quality care is delivered.
The consumer continued to be the primary payer for drugs, eyeglasses, and appliances throughout the period 1969-82. The consumer paid directly for three-quarters of all drugs, eyeglasses, and appliances purchased in 1982. Although insurance has been financing increasing proportions of these expenditures, in 1982 less than 15 percent were covered by private insurance.
Personal health care
Expenditures per person for personal health care increased from $201 in 1966 to $1,220 in 1982 (Table 5). Per capita expenditures increased at a rate of 11.9 percent per year, while personal income per person, a measure of the financial resources available to individuals, grew at an average annual rate of 8.6 percent. Although government financed increasing proportions of health care throughout the period, the contrasting rates of growth of spending and income emphasize the ever-increasing amount of resources diverted to health care.
Table 5. Per capita personal health care expenditures, by region and State: Selected calendar years 1966-82.
| Region and State | 1966 | 1969 | 1972 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1982 |
|---|---|---|---|---|---|---|---|---|---|---|
| U.S. total | $201 | $280 | $381 | $605 | $673 | $747 | $838 | $958 | $1,097 | $1,220 |
| New England | 234 | 328 | 441 | 686 | 757 | 834 | 932 | 1,058 | 1,202 | 1,356 |
| Connecticut | 236 | 330 | 438 | 675 | 745 | 821 | 918 | 1,046 | 1,194 | 1,348 |
| Maine | 173 | 242 | 328 | 542 | 603 | 661 | 748 | 870 | 975 | 1,091 |
| Massachusetts | 253 | 360 | 489 | 760 | 844 | 930 | 1,037 | 1,175 | 1,333 | 1,508 |
| New Hampshire | 188 | 245 | 330 | 507 | 548 | 607 | 679 | 759 | 883 | 986 |
| Rhode Island | 231 | 315 | 413 | 672 | 743 | 831 | 931 | 1,062 | 1,199 | 1,351 |
| Vermont | 197 | 274 | 352 | 531 | 571 | 626 | 683 | 778 | 889 | 978 |
| Mideast | 228 | 320 | 430 | 667 | 730 | 802 | 900 | 1,028 | 1,173 | 1,322 |
| Delaware | 209 | 286 | 381 | 599 | 661 | 729 | 806 | 912 | 1,030 | 1,153 |
| District of Columbia | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Maryland | 190 | 273 | 390 | 609 | 668 | 747 | 840 | 957 | 1,096 | 1,232 |
| New Jersey | 192 | 264 | 355 | 578 | 643 | 694 | 776 | 877 | 1,004 | 1,115 |
| New York | 258 | 366 | 488 | 745 | 796 | 860 | 972 | 1,107 | 1,253 | 1,417 |
| Pennsylvania | 201 | 279 | 372 | 590 | 664 | 756 | 841 | 972 | 1,124 | 1,273 |
| Great Lakes | 203 | 278 | 378 | 610 | 681 | 759 | 851 | 978 | 1,119 | 1,249 |
| Illinois | 220 | 300 | 407 | 634 | 706 | 797 | 899 | 1,033 | 1,169 | 1,308 |
| Indiana | 182 | 252 | 337 | 542 | 610 | 673 | 751 | 861 | 987 | 1,101 |
| Michigan | 211 | 286 | 388 | 635 | 714 | 797 | 890 | 1,014 | 1,152 | 1,281 |
| Ohio | 195 | 264 | 361 | 597 | 664 | 738 | 822 | 958 | 1,110 | 1,247 |
| Wisconsin | 192 | 269 | 373 | 610 | 674 | 745 | 838 | 952 | 1,112 | 1,219 |
| Plains | 200 | 273 | 369 | 597 | 670 | 750 | 841 | 973 | 1,114 | 1,241 |
| Iowa | 197 | 265 | 351 | 563 | 643 | 728 | 820 | 935 | 1,068 | 1,176 |
| Kansas | 195 | 270 | 379 | 568 | 633 | 735 | 855 | 988 | 1,150 | 1,271 |
| Minnesota | 216 | 287 | 389 | 602 | 665 | 738 | 827 | 976 | 1,116 | 1,229 |
| Missouri | 198 | 273 | 365 | 627 | 709 | 785 | 866 | 997 | 1,134 | 1,285 |
| Nebraska | 195 | 268 | 371 | 598 | 658 | 739 | 827 | 948 | 1,085 | 1,216 |
| North Dakota | 197 | 273 | 367 | 676 | 771 | 825 | 906 | 1,034 | 1,180 | 1,325 |
| South Dakota | 181 | 241 | 327 | 522 | 587 | 667 | 763 | 887 | 1,027 | 1,154 |
| Southeast | $153 | $218 | $309 | $508 | $572 | $638 | $723 | $828 | $954 | $1,055 |
| Alabama | 145 | 210 | 300 | 501 | 567 | 631 | 708 | 809 | 929 | 1,033 |
| Arkansas | 142 | 198 | 284 | 470 | 523 | 583 | 661 | 766 | 889 | 994 |
| Florida | 184 | 264 | 377 | 623 | 698 | 770 | 869 | 975 | 1,119 | 1,228 |
| Georgia | 150 | 217 | 319 | 515 | 581 | 648 | 734 | 843 | 953 | 1,048 |
| Kentucky | 155 | 218 | 286 | 444 | 493 | 555 | 639 | 739 | 853 | 957 |
| Louisiana | 156 | 226 | 322 | 511 | 577 | 651 | 740 | 857 | 1,002 | 1,106 |
| Mississippi | 115 | 163 | 242 | 425 | 481 | 554 | 640 | 730 | 828 | 897 |
| North Carolina | 143 | 204 | 282 | 461 | 515 | 577 | 646 | 737 | 852 | 931 |
| South Carolina | 125 | 182 | 251 | 423 | 475 | 527 | 594 | 686 | 790 | 857 |
| Tennessee | 166 | 232 | 324 | 531 | 605 | 672 | 757 | 874 | 1,012 | 1,144 |
| Virginia | 151 | 213 | 301 | 493 | 564 | 629 | 712 | 811 | 943 | 1,054 |
| West Virginia | 161 | 227 | 313 | 508 | 556 | 618 | 699 | 808 | 935 | 1,057 |
| Southwest | 178 | 252 | 341 | 546 | 606 | 679 | 759 | 864 | 993 | 1,095 |
| Arizona | 190 | 271 | 376 | 582 | 628 | 703 | 777 | 882 | 1,004 | 1,112 |
| New Mexico | 157 | 214 | 282 | 458 | 506 | 573 | 627 | 722 | 829 | 904 |
| Oklahoma | 183 | 263 | 351 | 539 | 599 | 666 | 749 | 852 | 988 | 1,086 |
| Texas | 177 | 249 | 338 | 549 | 612 | 687 | 770 | 876 | 1,007 | 1,110 |
| Rocky Mountain | 194 | 262 | 344 | 529 | 582 | 642 | 723 | 822 | 944 | 1,046 |
| Colorado | 233 | 311 | 396 | 605 | 656 | 725 | 825 | 942 | 1,088 | 1,209 |
| Idaho | 153 | 210 | 292 | 455 | 514 | 558 | 615 | 695 | 791 | 868 |
| Montana | 175 | 236 | 325 | 510 | 582 | 638 | 701 | 801 | 916 | 1,036 |
| Utah | 158 | 211 | 286 | 458 | 506 | 563 | 636 | 714 | 815 | 896 |
| Wyoming | 200 | 268 | 327 | 451 | 495 | 549 | 615 | 710 | 811 | 873 |
| Far West | 234 | 327 | 439 | 691 | 777 | 865 | 963 | 1,094 | 1,252 | 1,380 |
| California | 242 | 340 | 460 | 727 | 818 | 912 | 1,016 | 1,152 | 1,319 | 1,451 |
| Nevada | 196 | 282 | 389 | 658 | 747 | 850 | 959 | 1,163 | 1,273 | 1,380 |
| Oregon | 197 | 274 | 364 | 587 | 663 | 730 | 806 | 912 | 1,044 | 1,165 |
| Washington | 219 | 297 | 390 | 584 | 649 | 720 | 799 | 915 | 1,045 | 1,165 |
| Alaska | 227 | 289 | 340 | 560 | 644 | 734 | 845 | 961 | 1,120 | 1,187 |
| Hawaii | 208 | 300 | 401 | 598 | 679 | 749 | 838 | 932 | 1,098 | 1,228 |
Per capita estimates for the District of Columbia are not presented in this report, because significant proportions of services rendered in the District of Columbia are purchased by out-of-State residents. However, these estimates are included in regional and U.S. totals.
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Per capita spending for health care in 1982 ranged from a low of $1,046 in the Rocky Mountain region to a high of $1,380 in the Far West region. Even greater diversity existed among States, with expenditures ranging from a low of $857 in South Carolina to a high of $1,508 in Massachusetts. The States of California and New York ranked second and third, with per capita spending higher than $1,400.
The choice of services purchased with the health care dollar varies by region and State (Tables 6 and 7). Nationwide almost one-half of all personal health care expenditures went toward the purchase of hospital care in 1982. Among States, however, Washington devoted the smallest proportion, 37 percent, to hospital care; in Massachusetts, 54 percent of all personal health spending purchased hospital care. (An even higher percentage of spending, 71 percent, was devoted to hospital care in the District of Coumbia; however, as noted before, a large portion of that spending can be attributed to purchases by out-of-State residents.)
Table 6. Percent distribution of personal health care expenditures, by type of expenditure, region, and State: Calendar year 1966.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Percent distribution | |||||||||
| U.S. total | 100.0 | 39.7 | 23.4 | 7.5 | 3.0 | 13.9 | 3.3 | 6.0 | 3.1 |
| New England | 100.0 | 43.1 | 20.9 | 7.3 | 3.4 | 11.3 | 3.4 | 8.4 | 2.8 |
| Connecticut | 100.0 | 38.4 | 23.6 | 8.2 | 4.2 | 12.3 | 2.5 | 7.9 | 3.0 |
| Maine | 100.0 | 42.6 | 21.0 | 5.5 | 3.0 | 13.2 | 4.3 | 8.5 | 1.8 |
| Massachusetts | 100.0 | 45.6 | 19.4 | 7.6 | 2.9 | 10.2 | 2.9 | 8.9 | 2.5 |
| New Hampshire | 100.0 | 39.0 | 23.0 | 6.0 | 4.5 | 12.1 | 3.0 | 8.3 | 4.0 |
| Rhode Island | 100.0 | 43.8 | 21.4 | 5.2 | 2.8 | 12.5 | 3.6 | 6.5 | 4.1 |
| Vermont | 100.0 | 43.4 | 18.7 | 6.2 | 3.9 | 12.1 | 4.0 | 9.8 | 1.9 |
| Mideast | 100.0 | 41.6 | 23.6 | 8.0 | 3.2 | 11.9 | 3.0 | 5.7 | 3.4 |
| Delaware | 100.0 | 43.8 | 20.6 | 5.5 | 3.6 | 15.9 | 2.8 | 3.6 | 4.2 |
| District of Columbia | 100.0 | 44.6 | 27.8 | 7.7 | 2.8 | 11.3 | 1.4 | 1.4 | 3.1 |
| Maryland | 100.0 | 44.4 | 21.0 | 6.8 | 2.8 | 14.4 | 2.9 | 4.8 | 3.0 |
| New Jersey | 100.0 | 36.7 | 25.6 | 8.8 | 3.3 | 14.5 | 2.8 | 5.0 | 3.3 |
| New York | 100.0 | 42.7 | 23.6 | 8.5 | 3.1 | 10.2 | 2.2 | 6.3 | 3.4 |
| Pennsylvania | 100.0 | 40.7 | 22.8 | 7.2 | 3.6 | 13.0 | 3.3 | 5.9 | 3.6 |
| Great Lakes | 100.0 | 39.7 | 23.6 | 7.1 | 2.6 | 14.5 | 3.4 | 5.9 | 2.9 |
| Illinois | 100.0 | 41.0 | 22.5 | 7.1 | 2.6 | 14.2 | 3.9 | 5.7 | 3.0 |
| Indiana | 100.0 | 34.8 | 25.7 | 6.5 | 2.1 | 16.9 | 4.8 | 6.6 | 2.6 |
| Michigan | 100.0 | 42.5 | 22.9 | 7.4 | 2.3 | 14.3 | 3.2 | 4.7 | 2.8 |
| Ohio | 100.0 | 37.8 | 24.7 | 7.0 | 2.8 | 14.9 | 3.9 | 6.2 | 2.7 |
| Wisconsin | 100.0 | 39.7 | 23.4 | 7.4 | 3.0 | 12.1 | 3.9 | 7.5 | 3.0 |
| Plains | 100.0 | 39.5 | 21.9 | 7.1 | 2.9 | 13.5 | 3.9 | 8.9 | 2.2 |
| Iowa | 100.0 | 34.9 | 23.9 | 7.3 | 3.0 | 13.2 | 4.7 | 11.3 | 1.8 |
| Kansas | 100.0 | 38.9 | 20.9 | 6.4 | 3.3 | 13.9 | 5.4 | 9.2 | 2.0 |
| Minnesota | 100.0 | 41.2 | 20.0 | 7.8 | 2.8 | 12.2 | 3.0 | 10.3 | 2.7 |
| Missouri | 100.0 | 40.8 | 22.9 | 6.9 | 3.3 | 14.5 | 3.3 | 6.0 | 2.3 |
| Nebraska | 100.0 | 38.5 | 22.8 | 7.7 | 2.0 | 14.0 | 4.2 | 8.6 | 2.2 |
| North Dakota | 100.0 | 42.1 | 21.9 | 5.3 | 1.9 | 13.1 | 4.9 | 9.5 | 1.3 |
| South Dakota | 100.0 | 41.6 | 18.2 | 6.8 | 2.2 | 13.1 | 6.2 | 10.2 | 1.8 |
| Southeast | 100.0 | 39.6 | 23.6 | 6.8 | 2.8 | 16.2 | 3.5 | 4.9 | 2.9 |
| Alabama | 100.0 | 41.9 | 23.6 | 6.5 | 2.5 | 15.1 | 2.7 | 5.4 | 2.3 |
| Arkansas | 100.0 | 39.4 | 20.9 | 5.7 | 2.0 | 16.2 | 3.9 | 9.3 | 2.5 |
| Florida | 100.0 | 35.8 | 23.6 | 8.1 | 4.3 | 17.4 | 2.5 | 5.9 | 2.4 |
| Georgia | 100.0 | 37.6 | 26.1 | 6.9 | 2.5 | 15.9 | 2.9 | 5.1 | 3.0 |
| Kentucky | 100.0 | 38.9 | 24.2 | 5.8 | 2.2 | 16.1 | 3.6 | 5.8 | 3.3 |
| Louisiana | 100.0 | 40.0 | 24.9 | 6.5 | 2.4 | 16.4 | 2.9 | 5.1 | 1.9 |
| Mississippi | 100.0 | 41.8 | 23.2 | 5.9 | 3.4 | 17.1 | 3.2 | 3.4 | 2.0 |
| North Carolina | 100.0 | 39.9 | 23.2 | 6.4 | 2.6 | 17.1 | 3.4 | 4.5 | 2.8 |
| South Carolina | 100.0 | 40.9 | 19.5 | 5.8 | 2.9 | 17.0 | 4.2 | 4.7 | 5.2 |
| Tennessee | 100.0 | 40.6 | 24.4 | 6.8 | 2.2 | 15.4 | 3.8 | 3.4 | 3.3 |
| Virginia | 100.0 | 41.9 | 22.0 | 7.3 | 2.6 | 14.7 | 3.5 | 4.1 | 3.9 |
| West Virginia | 100.0 | 43.6 | 24.6 | 5.7 | 2.0 | 14.4 | 3.9 | 2.1 | 3.7 |
| Southwest | 100.0 | 38.7 | 22.7 | 6.1 | 2.9 | 16.1 | 3.3 | 6.4 | 3.9 |
| Arizona | 100.0 | 40.8 | 25.6 | 6.8 | 2.8 | 15.1 | 2.1 | 4.2 | 2.6 |
| New Mexico | 100.0 | 43.9 | 18.9 | 6.7 | 2.7 | 16.3 | 3.5 | 3.5 | 4.5 |
| Oklahoma | 100.0 | 34.3 | 24.1 | 6.0 | 2.2 | 14.5 | 3.6 | 10.5 | 4.9 |
| Texas | 100.0 | 38.9 | 22.2 | 6.0 | 3.0 | 16.6 | 3.4 | 6.0 | 3.8 |
| Rocky Mountain | 100.0 | 40.0 | 22.0 | 7.2 | 2.8 | 14.8 | 4.5 | 6.2 | 3.7 |
| Colorado | 100.0 | 42.8 | 20.3 | 6.8 | 3.0 | 12.8 | 2.5 | 6.3 | 5.5 |
| Idaho | 100.0 | 32.9 | 23.3 | 8.1 | 2.6 | 19.2 | 4.5 | 7.7 | 1.8 |
| Montana | 100.0 | 38.3 | 21.2 | 6.4 | 2.6 | 16.8 | 6.1 | 6.8 | 1.9 |
| Utah | 100.0 | 36.9 | 25.4 | 8.9 | 2.3 | 16.4 | 2.7 | 5.4 | 1.9 |
| Wyoming | 100.0 | 42.3 | 25.1 | 6.4 | 2.6 | 14.7 | 4.4 | 3.2 | 1.2 |
| Far West | 100.0 | 36.1 | 24.9 | 9.3 | 3.1 | 14.2 | 3.1 | 4.9 | 3.6 |
| California | 100.0 | 36.4 | 25.2 | 9.4 | 3.3 | 13.9 | 3.9 | 4.4 | 3.6 |
| Nevada | 100.0 | 34.8 | 23.5 | 7.4 | 3.0 | 21.3 | 3.2 | 3.3 | 3.5 |
| Oregon | 100.0 | 33.6 | 23.6 | 9.7 | 2.9 | 14.8 | 4.9 | 8.5 | 2.0 |
| Washington | 100.0 | 32.8 | 25.7 | 9.3 | 2.6 | 15.2 | 3.9 | 7.3 | 3.1 |
| Alaska | 100.0 | 65.5 | 12.6 | 4.6 | 1.7 | 10.2 | 2.2 | .6 | 2.6 |
| Hawaii | 100.0 | 38.1 | 22.5 | 9.6 | 2.1 | 13.0 | 2.8 | 2.8 | 9.2 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Table 7. Percent distribution of personal health care expenditures, by type of expenditure, region, and State: Calendar year 1982.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Percent distribution | |||||||||
| U.S. total | 100.0 | 47.3 | 21.8 | 6.9 | 2.5 | 7.7 | 1.9 | 9.4 | 2.5 |
| New England | 100.0 | 49.3 | 17.1 | 6.5 | 2.7 | 6.5 | 1.8 | 13.7 | 2.3 |
| Connecticut | 100.0 | 42.9 | 19.6 | 8.3 | 3.0 | 7.2 | 1.5 | 15.3 | 2.2 |
| Maine | 100.0 | 47.4 | 17.3 | 4.9 | 2.5 | 7.1 | 2.1 | 16.1 | 2.5 |
| Massachusetts | 100.0 | 53.7 | 15.4 | 5.8 | 2.7 | 5.7 | 1.8 | 12.8 | 2.1 |
| New Hampshire | 100.0 | 46.4 | 20.9 | 7.5 | 2.8 | 8.7 | 1.7 | 9.1 | 2.8 |
| Rhode Island | 100.0 | 46.1 | 18.8 | 6.1 | 2.2 | 6.2 | 2.1 | 15.9 | 2.6 |
| Vermont | 100.0 | 45.3 | 14.7 | 7.2 | 2.9 | 8.5 | 2.9 | 15.3 | 3.3 |
| Mideast | 100.0 | 49.7 | 19.2 | 6.5 | 3.4 | 6.6 | 1.5 | 10.4 | 2.7 |
| Delaware | 100.0 | 47.9 | 21.9 | 7.5 | 1.9 | 8.5 | 1.8 | 7.4 | 3.2 |
| District of Columbia | 100.0 | 71.2 | 14.6 | 2.5 | 1.5 | 4.2 | .9 | 2.0 | 3.2 |
| Maryland | 100.0 | 49.2 | 21.2 | 7.1 | 2.2 | 7.5 | 1.6 | 8.3 | 2.9 |
| New Jersey | 100.0 | 44.6 | 22.2 | 8.8 | 3.1 | 8.3 | 1.7 | 8.7 | 2.7 |
| New York | 100.0 | 47.9 | 18.6 | 6.1 | 4.4 | 5.9 | 1.3 | 13.0 | 2.9 |
| Pennsylvania | 100.0 | 53.0 | 18.2 | 6.2 | 2.7 | 6.6 | 1.8 | 9.1 | 2.4 |
| Great Lakes | 100.0 | 49.2 | 20.4 | 6.9 | 1.7 | 7.4 | 2.0 | 10.0 | 2.4 |
| Illinois | 100.0 | 53.5 | 18.7 | 6.4 | 2.0 | 6.4 | 2.2 | 8.3 | 2.5 |
| Indiana | 100.0 | 46.5 | 19.7 | 5.5 | 1.5 | 10.1 | 2.5 | 11.7 | 2.5 |
| Michigan | 100.0 | 49.0 | 20.7 | 8.5 | 1.5 | 7.8 | 1.6 | 8.3 | 2.5 |
| Ohio | 100.0 | 48.1 | 21.4 | 6.2 | 1.5 | 7.2 | 1.9 | 11.4 | 2.2 |
| Wisconsin | 100.0 | 44.2 | 22.3 | 7.9 | 2.1 | 6.6 | 2.3 | 12.3 | 2.3 |
| Plains | 100.0 | 47.7 | 19.3 | 6.2 | 2.2 | 6.8 | 2.3 | 13.8 | 1.7 |
| Iowa | 100.0 | 45.5 | 19.5 | 6.5 | 2.6 | 7.2 | 2.6 | 14.3 | 1.7 |
| Kansas | 100.0 | 46.7 | 21.1 | 5.8 | 2.0 | 6.8 | 3.3 | 12.8 | 1.6 |
| Minnesota | 100.0 | 44.0 | 17.2 | 7.8 | 2.0 | 6.3 | 1.9 | 19.1 | 1.6 |
| Missouri | 100.0 | 52.8 | 18.4 | 5.4 | 2.3 | 6.9 | 1.7 | 10.8 | 1.7 |
| Nebraska | 100.0 | 46.7 | 22.3 | 6.1 | 2.0 | 7.5 | 2.4 | 11.5 | 1.6 |
| North Dakota | 100.0 | 47.1 | 23.9 | 5.4 | 1.8 | 5.7 | 3.0 | 11.7 | 1.4 |
| South Dakota | 100.0 | 45.9 | 19.0 | 5.2 | 2.6 | 6.6 | 3.4 | 14.3 | 2.8 |
| Southeast | 100.0 | 47.8 | 23.4 | 5.9 | 1.9 | 9.3 | 1.8 | 7.6 | 2.3 |
| Alabama | 100.0 | 52.4 | 20.6 | 5.0 | 1.5 | 9.2 | 1.4 | 7.6 | 2.3 |
| Arkansas | 100.0 | 44.6 | 22.0 | 5.0 | 1.9 | 10.4 | 2.2 | 11.3 | 2.6 |
| Florida | 100.0 | 46.3 | 27.8 | 6.3 | 2.2 | 8.5 | 1.6 | 5.3 | 1.8 |
| Georgia | 100.0 | 47.0 | 24.2 | 6.1 | 1.5 | 9.5 | 1.6 | 7.5 | 2.7 |
| Kentucky | 100.0 | 45.3 | 21.4 | 5.6 | 2.5 | 9.9 | 2.2 | 10.9 | 2.3 |
| Louisiana | 100.0 | 49.7 | 22.6 | 5.3 | 2.0 | 8.7 | 1.6 | 8.0 | 2.0 |
| Mississippi | 100.0 | 48.0 | 21.2 | 4.5 | 2.4 | 9.7 | 1.6 | 10.0 | 2.6 |
| North Carolina | 100.0 | 46.0 | 21.7 | 6.6 | 1.7 | 11.6 | 2.0 | 8.1 | 2.5 |
| South Carolina | 100.0 | 46.3 | 20.1 | 5.9 | 1.6 | 11.3 | 2.4 | 8.9 | 3.6 |
| Tennessee | 100.0 | 50.5 | 22.7 | 5.6 | 2.0 | 8.4 | 2.1 | 6.7 | 2.0 |
| Virginia | 100.0 | 48.0 | 22.6 | 7.0 | 1.4 | 8.6 | 1.9 | 8.0 | 2.5 |
| West Virginia | 100.0 | 53.4 | 20.7 | 5.0 | 1.6 | 8.9 | 2.1 | 5.9 | 2.3 |
| Southwest | 100.0 | 45.0 | 24.8 | 6.4 | 2.0 | 9.2 | 2.2 | 7.7 | 2.6 |
| Arizona | 100.0 | 44.8 | 27.3 | 8.3 | 2.2 | 8.5 | 1.3 | 4.8 | 2.9 |
| New Mexico | 100.0 | 49.6 | 20.8 | 6.9 | 2.4 | 8.3 | 2.7 | 5.4 | 3.7 |
| Oklahoma | 100.0 | 45.9 | 21.6 | 5.6 | 1.8 | 9.5 | 2.6 | 10.2 | 2.8 |
| Texas | 100.0 | 44.6 | 25.3 | 6.1 | 2.0 | 9.3 | 2.2 | 8.0 | 2.5 |
| Rocky Mountain | 100.0 | 44.5 | 22.8 | 8.4 | 2.8 | 8.0 | 2.3 | 8.3 | 2.9 |
| Colorado | 100.0 | 46.1 | 21.7 | 8.2 | 3.0 | 6.9 | 2.1 | 8.6 | 3.5 |
| Idaho | 100.0 | 38.6 | 24.6 | 8.9 | 3.1 | 10.4 | 2.9 | 9.7 | 1.8 |
| Montana | 100.0 | 42.9 | 23.7 | 7.7 | 2.7 | 8.2 | 3.3 | 8.9 | 2.7 |
| Utah | 100.0 | 44.6 | 24.0 | 9.5 | 2.5 | 8.8 | 1.5 | 7.1 | 2.1 |
| Wyoming | 100.0 | 45.5 | 22.6 | 7.8 | 2.6 | 9.1 | 4.5 | 5.6 | 2.4 |
| Far West | 100.0 | 42.3 | 25.9 | 9.0 | 3.3 | 7.5 | 2.3 | 7.0 | 2.7 |
| California | 100.0 | 43.1 | 26.4 | 8.6 | 3.4 | 7.2 | 2.2 | 6.3 | 2.7 |
| Nevada | 100.0 | 45.6 | 26.0 | 7.7 | 2.3 | 9.1 | 1.8 | 5.9 | 1.5 |
| Oregon | 100.0 | 40.2 | 23.9 | 9.3 | 2.8 | 9.2 | 2.8 | 9.7 | 2.1 |
| Washington | 100.0 | 37.2 | 23.0 | 11.2 | 3.6 | 7.9 | 2.7 | 11.8 | 2.6 |
| Alaska | 100.0 | 46.5 | 22.9 | 10.5 | 2.6 | 8.7 | 1.7 | 2.2 | 4.9 |
| Hawaii | 100.0 | 39.0 | 30.6 | 10.9 | 1.7 | 7.6 | 1.8 | 5.1 | 3.3 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
The purchase of physicians' services, the second largest category of health expenditures, was responsible for 22 percent of all spending nationwide. The lowest proportion of spending was in Vermont, where less than 15 percent of the health dollar was expended for physicians' services; the highest occurred in Hawaii, where over 30 percent of every dollar went for physicians' services. Florida and Arizona rank second and third in the proportion of health care spending devoted to physicians' services. In these two States, over 27 percent of health care spending went for these services in 1982.
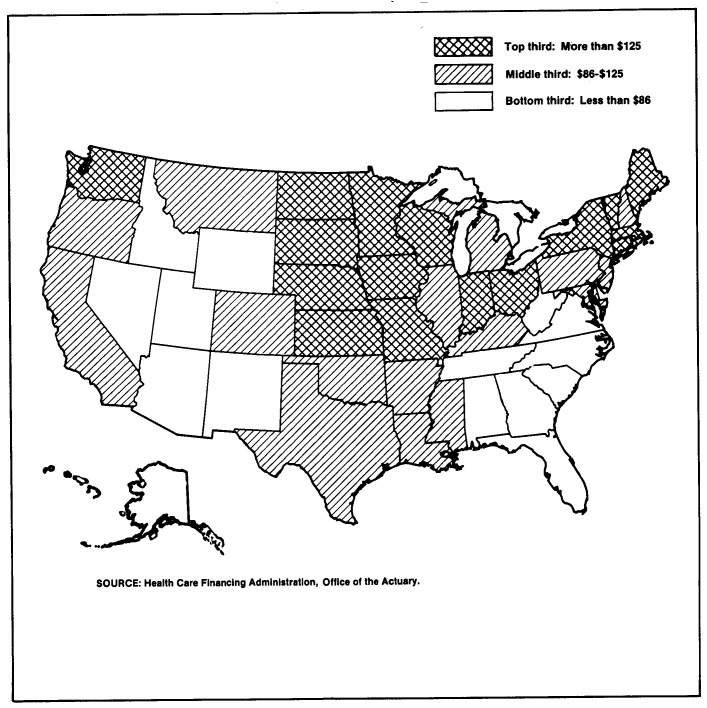
Expenditures for nursing home care in 1982 averaged over 9 percent of total personal health care expenditures. The highest levels of spending per capita occur in the colder climatic regions of the United States (Figure 2). The areas with rapidly growing, larger than average proportions of elderly people— Florida and Arizona—appear to be retirement havens for the “well” elderly, because only a small proportion of spending is devoted to nursing home care in those States (less than 6 percent in 1982). In these two States, higher than average proportions of spending for physicians' services offset lower than average spending for nursing home care.
Figure 2. Per capita expenditures for nursing home care, by State: Calendar year 1982.
Spending per capita for personal health care grew an average of 11.9 percent per year during the period 1966-82 (Table 8). Growth was most dramatic in the Southeast, where expenditures per capita grew 12.8 percent per year. Mississippi registered an average annual growth rate of 13.7 percent, the highest per capita growth in the region and the Nation. However, despite rapid growth, the per capita expenditure for personal health care in Mississippi remains among the lowest in the Nation.
Table 8. Average annual growth of per capita personal health care expenditures, by region and State: Calendar years 1966-82.
| Region and State | Average annual percent growth |
|---|---|
| U.S. total | 11.9 |
| New England | 11.6 |
| Connecticut | 11.5 |
| Maine | 12.2 |
| Massachusetts | 11.8 |
| New Hampshire | 10.9 |
| Rhode Island | 11.7 |
| Vermont | 10.5 |
| Mideast | 11.6 |
| Delaware | 11.3 |
| District of Columbia | 12.5 |
| Maryland | 12.4 |
| New Jersey | 11.6 |
| New York | 11.2 |
| Pennsylvania | 12.2 |
| Great Lakes | 12.0 |
| Illinois | 11.8 |
| Indiana | 11.9 |
| Michigan | 11.9 |
| Ohio | 12.3 |
| Wisconsin | 12.2 |
| Plains | 12.1 |
| Iowa | 11.8 |
| Kansas | 12.4 |
| Minnesota | 11.5 |
| Missouri | 12.4 |
| Nebraska | 12.1 |
| North Dakota | 12.7 |
| South Dakota | 12.3 |
| Southeast | 12.8 |
| Alabama | 13.1 |
| Arkansas | 12.9 |
| Florida | 12.6 |
| Georgia | 12.9 |
| Kentucky | 12.0 |
| Louisiana | 13.0 |
| Mississippi | 13.7 |
| North Carolina | 12.4 |
| South Carolina | 12.8 |
| Tennessee | 12.8 |
| Virginia | 12.9 |
| West Virginia | 12.5 |
| Southwest | 12.0 |
| Arizona | 11.7 |
| New Mexico | 11.6 |
| Oklahoma | 11.8 |
| Texas | 12.1 |
| Rocky Mountain | 11.1 |
| Colorado | 10.8 |
| Idaho | 11.5 |
| Montana | 11.7 |
| Utah | 11.5 |
| Wyoming | 9.6 |
| Far West | 11.7 |
| California | 11.8 |
| Nevada | 13.0 |
| Oregon | 11.7 |
| Washington | 11.0 |
| Alaska | 10.9 |
| Hawaii | 11.7 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
The slowest growing region in terms of health care spending was the Rocky Mountain region, with an average annual growth rate of 11.1 percent. Wyoming registered the slowest growth in personal health care expenditures per capita in the region and the Nation, with a 9.6-percent average annual growth. The slow growth rate can be explained, in part, by the large proportion of hospital services purchased out-of-State by Wyoming residents (Table 2). Growth in spending per capita in Wyoming appears artificially lower because it is estimated on a place-of-service basis rather than a place-of-residence basis.
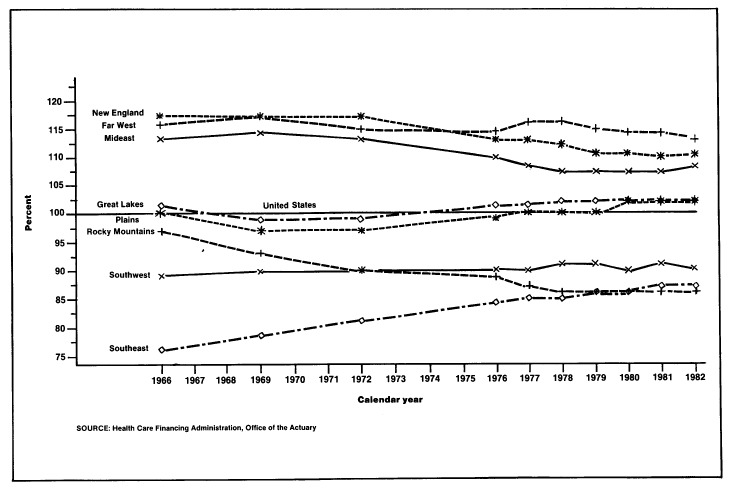
When per capita personal health care estimates for the States are divided by the national estimate, the resulting percentages show a pattern of convergence toward the U.S. average over the 16-year period (Table 9 and Figure 3). This pattern can be seen for a majarity of States, indicating that variations in health spending levels among most States and regions are narrowing. The most notable exception to this pattern is the Rocky Mountain region. In 1966, its proportion of the national average was 97 percent; by 1982, it had sunk to 86 percent. In addition, the rate of convergence may be slowing, particularly in the Southeast region. In the period 1966-76, personal health expenditures for the Southeast grew from 76 to 84 percent of the U.S. average. However, since 1976, the rate of increase appears to have slowed, reaching only 87 percent of the U.S. average in 1982.
Table 9. Per capita personal health care expenditures as a percent of national average, by region and State: Selected calendar years 1966-82.
| Region and State | 1966 | 1969 | 1972 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1982 |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Percent | ||||||||||
| U.S. total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| New England | 117 | 117 | 116 | 113 | 113 | 112 | 111 | 111 | 110 | 111 |
| Connecticut | 117 | 118 | 115 | 112 | 111 | 110 | 110 | 109 | 109 | 110 |
| Maine | 86 | 86 | 86 | 90 | 90 | 88 | 89 | 91 | 89 | 89 |
| Massachusetts | 126 | 128 | 128 | 126 | 125 | 124 | 124 | 123 | 122 | 124 |
| New Hampshire | 94 | 87 | 87 | 84 | 82 | 81 | 81 | 79 | 81 | 81 |
| Rhode Island | 115 | 112 | 109 | 111 | 110 | 111 | 111 | 111 | 109 | 111 |
| Vermont | 98 | 98 | 93 | 88 | 85 | 84 | 82 | 81 | 81 | 80 |
| Mideast | 113 | 114 | 113 | 110 | 108 | 107 | 107 | 107 | 107 | 108 |
| Delaware | 104 | 102 | 100 | 99 | 98 | 98 | 96 | 95 | 94 | 94 |
| District of Columbia | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Maryland | 95 | 97 | 102 | 101 | 99 | 100 | 100 | 100 | 100 | 101 |
| New Jersey | 96 | 94 | 93 | 96 | 96 | 93 | 93 | 92 | 92 | 91 |
| New York | 129 | 131 | 128 | 123 | 118 | 115 | 116 | 116 | 114 | 116 |
| Pennsylvania | 100 | 99 | 98 | 98 | 99 | 101 | 100 | 102 | 102 | 104 |
| Great Lakes | 101 | 99 | 99 | 101 | 101 | 102 | 102 | 102 | 102 | 102 |
| Illinois | 109 | 107 | 107 | 105 | 105 | 107 | 107 | 108 | 107 | 107 |
| Indiana | 91 | 90 | 88 | 90 | 91 | 90 | 90 | 90 | 90 | 90 |
| Michigan | 105 | 102 | 102 | 105 | 106 | 107 | 106 | 106 | 105 | 105 |
| Ohio | 97 | 94 | 95 | 99 | 99 | 99 | 98 | 100 | 101 | 102 |
| Wisconsin | 96 | 96 | 98 | 101 | 100 | 100 | 100 | 99 | 101 | 100 |
| Plains | 100 | 97 | 97 | 99 | 100 | 100 | 100 | 102 | 102 | 102 |
| Iowa | 98 | 95 | 92 | 93 | 96 | 97 | 98 | 98 | 97 | 96 |
| Kansas | 97 | 96 | 99 | 94 | 94 | 98 | 102 | 103 | 105 | 104 |
| Minnesota | 107 | 103 | 102 | 100 | 99 | 99 | 99 | 102 | 102 | 101 |
| Missouri | 98 | 98 | 96 | 104 | 105 | 105 | 103 | 104 | 103 | 105 |
| Nebraska | 97 | 95 | 97 | 99 | 98 | 99 | 99 | 99 | 99 | 100 |
| North Dakota | 98 | 97 | 96 | 112 | 115 | 110 | 108 | 108 | 108 | 109 |
| South Dakota | 90 | 86 | 86 | 86 | 87 | 89 | 91 | 93 | 94 | 95 |
| Southeast | 76 | 78 | 81 | 84 | 85 | 85 | 86 | 86 | 87 | 87 |
| Alabama | 72 | 75 | 79 | 83 | 84 | 84 | 85 | 84 | 85 | 85 |
| Arkansas | 71 | 71 | 75 | 78 | 78 | 78 | 79 | 80 | 81 | 81 |
| Florida | 92 | 94 | 99 | 103 | 104 | 103 | 104 | 102 | 102 | 101 |
| Georgia | 75 | 77 | 84 | 85 | 86 | 87 | 88 | 88 | 87 | 86 |
| Kentucky | 77 | 78 | 75 | 73 | 73 | 74 | 76 | 77 | 78 | 78 |
| Louisiana | 78 | 80 | 84 | 85 | 86 | 87 | 88 | 90 | 91 | 91 |
| Mississippi | 57 | 58 | 64 | 70 | 72 | 74 | 76 | 76 | 76 | 73 |
| North Carolina | 71 | 73 | 74 | 76 | 77 | 77 | 77 | 77 | 78 | 76 |
| South Carolina | 62 | 65 | 66 | 70 | 71 | 71 | 71 | 72 | 72 | 70 |
| Tennessee | 83 | 83 | 85 | 88 | 90 | 90 | 90 | 91 | 92 | 94 |
| Virginia | 75 | 76 | 79 | 82 | 84 | 84 | 85 | 85 | 86 | 86 |
| West Virginia | 80 | 81 | 82 | 84 | 83 | 83 | 83 | 84 | 85 | 87 |
| Southwest | 89 | 90 | 90 | 90 | 90 | 91 | 91 | 90 | 91 | 90 |
| Arizona | 95 | 97 | 99 | 96 | 93 | 94 | 93 | 92 | 92 | 91 |
| New Mexico | 78 | 76 | 74 | 76 | 75 | 77 | 75 | 75 | 76 | 74 |
| Oklahoma | 91 | 94 | 92 | 89 | 89 | 89 | 89 | 89 | 90 | 89 |
| Texas | 88 | 89 | 89 | 91 | 91 | 92 | 92 | 92 | 92 | 91 |
| Rocky Mountain | 97 | 93 | 90 | 88 | 87 | 86 | 86 | 86 | 86 | 86 |
| Colorado | 116 | 111 | 104 | 100 | 97 | 97 | 98 | 98 | 99 | 99 |
| Idaho | 76 | 75 | 77 | 75 | 76 | 75 | 73 | 73 | 72 | 71 |
| Montana | 87 | 84 | 85 | 84 | 86 | 85 | 84 | 84 | 84 | 85 |
| Utah | 78 | 75 | 75 | 76 | 75 | 75 | 76 | 75 | 74 | 73 |
| Wyoming | 100 | 95 | 86 | 75 | 74 | 73 | 73 | 74 | 74 | 72 |
| Far West | 116 | 117 | 115 | 114 | 116 | 116 | 115 | 114 | 114 | 113 |
| California | 120 | 121 | 121 | 120 | 122 | 122 | 121 | 120 | 120 | 119 |
| Nevada | 98 | 100 | 102 | 109 | 111 | 114 | 114 | 121 | 116 | 113 |
| Oregon | 98 | 98 | 96 | 97 | 99 | 98 | 96 | 95 | 95 | 95 |
| Washington | 109 | 106 | 102 | 97 | 97 | 96 | 95 | 96 | 95 | 95 |
| Alaska | 113 | 103 | 89 | 93 | 96 | 98 | 101 | 100 | 102 | 97 |
| Hawaii | 104 | 107 | 105 | 99 | 101 | 100 | 100 | 97 | 100 | 101 |
Per capita estimates for the District of Columbia are not presented in this report, because significant proportions of services rendered in the District of Columbia are purchased by out-of-State residents. However, these estimates are included in regional and U.S. totals.
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Figure 3. Per capita expenditures for personal health care as a percent of U.S. average, by region: Calendar years 1966-82.
Hospital care
Hospital expenditures represent the single largest component of personal health care spending. In 1966, 39.7 percent of each personal health care dollar went for hospital care; by 1982, the share had risen to 47.3 percent. In 1982, 7.6 percent of all hospital expenditures came directly from consumers. The remainder was financed by private health insurance (38.1 percent), public programs (53.2 percent), and other private sources (1.0 percent) (Gibson et al., 1984).
In 1966, hospital care expenditures amounted to $80 per person (Table 10); by 1982, spending had risen sevenfold to $577 (Table 11). Regionally, New England and the Mideast ranked highest in hospital expenditures per person in 1982, with spending higher than $650; at $465, persons in the Rocky Mountain region expended the least.
Table 10. Per capita personal health care expenditures, by type of expenditure, region, and State: Calendar year 1966.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
| U.S. total | $201 | $80 | $47 | $15 | $6 | $28 | $7 | $12 | $6 |
| New England | 234 | 101 | 49 | 17 | 8 | 26 | 8 | 20 | 6 |
| Connecticut | 236 | 91 | 56 | 19 | 10 | 29 | 6 | 19 | 7 |
| Maine | 173 | 74 | 36 | 10 | 5 | 23 | 7 | 15 | 3 |
| Massachusetts | 253 | 116 | 49 | 19 | 7 | 26 | 7 | 22 | 6 |
| New Hampshire | 188 | 73 | 43 | 11 | 9 | 23 | 6 | 16 | 8 |
| Rhode Island | 231 | 101 | 50 | 12 | 7 | 29 | 8 | 15 | 9 |
| Vermont | 197 | 86 | 37 | 12 | 8 | 24 | 8 | 19 | 4 |
| Mideast | 228 | 95 | 54 | 18 | 7 | 27 | 7 | 13 | 8 |
| Delaware | 209 | 91 | 43 | 11 | 8 | 33 | 6 | 8 | 9 |
| District of Columbia | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Maryland | 190 | 84 | 40 | 13 | 5 | 27 | 5 | 9 | 6 |
| New Jersey | 192 | 71 | 49 | 17 | 6 | 28 | 5 | 10 | 6 |
| New York | 258 | 110 | 61 | 22 | 8 | 26 | 6 | 16 | 9 |
| Pennsylvania | 201 | 82 | 46 | 14 | 7 | 26 | 7 | 12 | 7 |
| Great Lakes | 203 | 81 | 48 | 14 | 5 | 29 | 7 | 12 | 6 |
| Illinois | 220 | 90 | 49 | 16 | 6 | 31 | 9 | 13 | 7 |
| Indiana | 182 | 63 | 47 | 12 | 4 | 31 | 9 | 12 | 5 |
| Michigan | 211 | 90 | 48 | 16 | 5 | 30 | 7 | 10 | 6 |
| Ohio | 195 | 74 | 48 | 14 | 6 | 29 | 8 | 12 | 5 |
| Wisconsin | 192 | 76 | 45 | 14 | 6 | 23 | 8 | 14 | 6 |
| Plains | 200 | 79 | 44 | 14 | 6 | 27 | 8 | 18 | 4 |
| Iowa | 197 | 69 | 47 | 14 | 6 | 26 | 9 | 22 | 4 |
| Kansas | 195 | 76 | 41 | 12 | 6 | 27 | 11 | 18 | 4 |
| Minnesota | 216 | 89 | 43 | 17 | 6 | 26 | 6 | 22 | 6 |
| Missouri | 198 | 81 | 45 | 14 | 7 | 29 | 7 | 12 | 5 |
| Nebraska | 195 | 75 | 44 | 15 | 4 | 27 | 8 | 17 | 4 |
| North Dakota | 197 | 83 | 43 | 10 | 4 | 26 | 10 | 19 | 2 |
| South Dakota | 181 | 75 | 33 | 12 | 4 | 24 | 11 | 18 | 3 |
| Southeast | $153 | $61 | $36 | $10 | $4 | $25 | $5 | $8 | $4 |
| Alabama | 145 | 61 | 34 | 9 | 4 | 22 | 4 | 8 | 3 |
| Arkansas | 142 | 56 | 30 | 8 | 3 | 23 | 6 | 13 | 4 |
| Florida | 184 | 66 | 43 | 15 | 8 | 32 | 5 | 11 | 4 |
| Georgia | 150 | 56 | 39 | 10 | 4 | 24 | 4 | 8 | 5 |
| Kentucky | 155 | 60 | 38 | 9 | 3 | 25 | 6 | 9 | 5 |
| Louisiana | 156 | 63 | 39 | 10 | 4 | 26 | 4 | 8 | 3 |
| Mississippi | 115 | 48 | 27 | 7 | 4 | 20 | 4 | 4 | 2 |
| North Carolina | 143 | 57 | 33 | 9 | 4 | 25 | 5 | 6 | 4 |
| South Carolina | 125 | 51 | 24 | 7 | 4 | 21 | 5 | 6 | 6 |
| Tennessee | 166 | 67 | 40 | 11 | 4 | 25 | 6 | 6 | 5 |
| Virginia | 151 | 63 | 33 | 11 | 4 | 22 | 5 | 6 | 6 |
| West Virginia | 161 | 70 | 40 | 9 | 3 | 23 | 6 | 3 | 6 |
| Southwest | 178 | 69 | 40 | 11 | 5 | 29 | 6 | 11 | 7 |
| Arizona | 190 | 78 | 49 | 13 | 5 | 29 | 4 | 8 | 5 |
| New Mexico | 157 | 69 | 30 | 11 | 4 | 26 | 5 | 5 | 7 |
| Oklahoma | 183 | 63 | 44 | 11 | 4 | 26 | 7 | 19 | 9 |
| Texas | 177 | 69 | 39 | 11 | 5 | 29 | 6 | 11 | 7 |
| Rocky Mountain | 194 | 78 | 43 | 14 | 5 | 29 | 9 | 12 | 7 |
| Colorado | 233 | 100 | 47 | 16 | 7 | 30 | 6 | 15 | 13 |
| Idaho | 153 | 50 | 36 | 12 | 4 | 29 | 7 | 12 | 3 |
| Montana | 175 | 67 | 37 | 11 | 4 | 30 | 11 | 12 | 3 |
| Utah | 158 | 58 | 40 | 14 | 4 | 26 | 4 | 9 | 3 |
| Wyoming | 200 | 85 | 50 | 13 | 5 | 30 | 9 | 6 | 2 |
| Far West | 234 | 84 | 58 | 22 | 7 | 33 | 7 | 11 | 8 |
| California | 242 | 88 | 61 | 23 | 8 | 34 | 9 | 11 | 9 |
| Nevada | 196 | 68 | 46 | 14 | 6 | 42 | 6 | 7 | 7 |
| Oregon | 197 | 66 | 46 | 19 | 6 | 29 | 10 | 17 | 4 |
| Washington | 219 | 72 | 56 | 20 | 6 | 33 | 9 | 16 | 7 |
| Alaska | 227 | 149 | 29 | 11 | 4 | 23 | 5 | 1 | 6 |
| Hawaii | 208 | 79 | 47 | 20 | 4 | 27 | 6 | 6 | 19 |
Per capita estimates for the District of Columbia are not presented in this report, because significant proportions of services rendered in the District of Columbia are purchased by out-of-State residents. However, these estimates are included in regional and U.S. totals.
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Table 11. Per capita personal health care expenditures, by type of expenditure, region, and State: Calendar year 1982.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
| U.S. total | $1,220 | $577 | $267 | $84 | $31 | $94 | $24 | $114 | $30 |
| New England | 1,356 | 669 | 232 | 88 | 37 | 88 | 24 | 186 | 31 |
| Connecticut | 1,348 | 578 | 264 | 112 | 40 | 98 | 21 | 206 | 30 |
| Maine | 1,091 | 517 | 189 | 54 | 28 | 78 | 23 | 176 | 27 |
| Massachusetts | 1,508 | 810 | 232 | 87 | 40 | 86 | 27 | 192 | 32 |
| New Hampshire | 986 | 458 | 206 | 74 | 28 | 86 | 17 | 90 | 27 |
| Rhode Island | 1,351 | 623 | 254 | 82 | 30 | 84 | 28 | 214 | 36 |
| Vermont | 978 | 443 | 144 | 70 | 28 | 83 | 28 | 149 | 32 |
| Mideast | 1,322 | 657 | 254 | 86 | 45 | 87 | 20 | 138 | 36 |
| Delaware | 1,153 | 552 | 252 | 86 | 22 | 98 | 21 | 86 | 37 |
| District of Columbia | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) | (1) |
| Maryland | 1,232 | 606 | 262 | 87 | 27 | 92 | 20 | 102 | 36 |
| New Jersey | 1,115 | 498 | 247 | 98 | 35 | 92 | 19 | 97 | 30 |
| New York | 1,417 | 679 | 264 | 86 | 62 | 84 | 18 | 184 | 40 |
| Pennsylvania | 1,273 | 675 | 232 | 79 | 34 | 84 | 22 | 116 | 30 |
| Great Lakes | 1,249 | 615 | 254 | 86 | 22 | 92 | 25 | 125 | 30 |
| Illinois | 1,308 | 700 | 245 | 83 | 27 | 83 | 28 | 109 | 33 |
| Indiana | 1,101 | 512 | 216 | 60 | 17 | 111 | 27 | 129 | 27 |
| Michigan | 1,281 | 628 | 265 | 109 | 20 | 100 | 20 | 106 | 32 |
| Ohio | 1,247 | 599 | 267 | 77 | 19 | 90 | 24 | 143 | 27 |
| Wisconsin | 1,219 | 539 | 272 | 97 | 26 | 80 | 28 | 150 | 28 |
| Plains | 1,241 | 592 | 240 | 77 | 27 | 84 | 28 | 172 | 21 |
| Iowa | 1,176 | 536 | 230 | 76 | 31 | 85 | 30 | 168 | 20 |
| Kansas | 1,271 | 593 | 269 | 73 | 26 | 86 | 41 | 163 | 20 |
| Minnesota | 1,229 | 540 | 212 | 96 | 25 | 78 | 23 | 235 | 20 |
| Missouri | 1,285 | 679 | 237 | 69 | 29 | 89 | 22 | 139 | 22 |
| Nebraska | 1,216 | 568 | 271 | 74 | 24 | 91 | 29 | 140 | 19 |
| North Dakota | 1,325 | 624 | 316 | 72 | 24 | 76 | 40 | 154 | 18 |
| South Dakota | 1,154 | 530 | 219 | 60 | 30 | 77 | 40 | 165 | 33 |
| Southeast | $1,055 | $505 | $247 | $62 | $20 | $98 | $19 | $80 | $24 |
| Alabama | 1,033 | 541 | 213 | 51 | 16 | 95 | 14 | 79 | 24 |
| Arkansas | 994 | 443 | 219 | 49 | 19 | 103 | 22 | 112 | 26 |
| Florida | 1,228 | 569 | 342 | 77 | 27 | 105 | 20 | 65 | 23 |
| Georgia | 1,048 | 492 | 253 | 64 | 16 | 100 | 17 | 79 | 28 |
| Kentucky | 957 | 433 | 205 | 54 | 24 | 95 | 21 | 104 | 22 |
| Louisiana | 1,106 | 549 | 250 | 59 | 22 | 96 | 18 | 89 | 22 |
| Mississippi | 897 | 431 | 190 | 40 | 22 | 87 | 15 | 90 | 23 |
| North Carolina | 931 | 428 | 202 | 61 | 16 | 108 | 18 | 75 | 23 |
| South Carolina | 857 | 397 | 172 | 51 | 13 | 97 | 20 | 76 | 31 |
| Tennessee | 1,144 | 578 | 259 | 64 | 23 | 96 | 25 | 76 | 23 |
| Virginia | 1,054 | 506 | 238 | 74 | 15 | 90 | 20 | 85 | 26 |
| West Virginia | 1,057 | 564 | 219 | 53 | 17 | 94 | 22 | 62 | 25 |
| Southwest | 1,095 | 493 | 272 | 70 | 22 | 100 | 24 | 85 | 29 |
| Arizona | 1,112 | 498 | 304 | 92 | 24 | 94 | 14 | 53 | 32 |
| New Mexico | 904 | 449 | 188 | 62 | 22 | 75 | 24 | 49 | 34 |
| Oklahoma | 1,086 | 498 | 234 | 61 | 20 | 103 | 28 | 111 | 30 |
| Texas | 1,110 | 495 | 281 | 68 | 23 | 103 | 25 | 88 | 27 |
| Rocky Mountain | 1,046 | 465 | 238 | 88 | 30 | 83 | 24 | 87 | 30 |
| Colorado | 1,209 | 557 | 262 | 99 | 36 | 84 | 25 | 104 | 42 |
| Idaho | 868 | 335 | 213 | 78 | 27 | 90 | 25 | 84 | 16 |
| Montana | 1,036 | 445 | 245 | 80 | 28 | 85 | 34 | 92 | 27 |
| Utah | 896 | 399 | 215 | 85 | 22 | 79 | 14 | 63 | 19 |
| Wyoming | 873 | 398 | 197 | 68 | 23 | 80 | 39 | 49 | 21 |
| Far West | 1,380 | 584 | 358 | 124 | 45 | 104 | 31 | 97 | 37 |
| California | 1,451 | 626 | 383 | 125 | 49 | 105 | 32 | 91 | 40 |
| Nevada | 1,380 | 630 | 359 | 106 | 32 | 126 | 25 | 82 | 20 |
| Oregon | 1,165 | 468 | 279 | 109 | 32 | 108 | 32 | 113 | 24 |
| Washington | 1,165 | 434 | 268 | 131 | 42 | 92 | 31 | 137 | 30 |
| Alaska | 1,187 | 552 | 272 | 125 | 31 | 104 | 21 | 26 | 58 |
| Hawaii | 1,228 | 479 | 376 | 133 | 21 | 93 | 23 | 63 | 40 |
Per capita estimates for the District of Columbia are not presented in this report, because significant proportions of services rendered in the District of Columbia are purchased by out-of-State residents. However, these estimates are included in regional and U.S. totals.
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Dramatic variations in 1982 spending by State are also apparent. Per capita spending in Massachusetts ($810 per person) was almost 2½ times spending in Idaho ($335 per person). Illinois ($700 per capita), Missouri, and New York (both $679 per capita) ranked second through fourth in hospital spending levels. Along with Idaho, South Carolina, Wyoming, and Utah, all with spending levels below $400 per person, ranked lowest in the United States in hospital spending.
During the period 1966-82, expenditures per capita for hospital care increased at an average annual rate of 13.2 percent. Expenditures in the Southeast increased at 14.2 percent per year, and in the Rocky Mountain region they increased 11.8 percent. Variations were wider among States, ranging from a high growth rate of 14.9 percent per year in Nevada to a low of 8.5 percent per year in Alaska. Eleven States— Nevada, Alabama, Mississippi, Louisiana, Georgia, Florida, Tennessee, Missouri, Pennsylvania, Indiana, and Ohio—registered average annual growth rates in per capita spending for hospital care of 14 percent or greater.
Some of the variation in expenditures for hospital care can be attributed to the computation of per capita expenditures by place of service. In 1980, 17 percent of community hospital1 charges attributable to aged Medicare recipients living in Idaho were for services rendered in other States. On the other hand, almost 6 percent of the Massachusetts estimate of community hospital charges for aged Medicare recipients was for services rendered to out-of-State residents. Thus, the estimate of per capita spending in Massachusetts is inflated by utilization by nonresidents. Purchase of services in other States leads to underestimates of per capita spending by Idaho residents. (See the earlier discussion of place of residence and place of service.)
Variations in the price of hospital care and in utilization practices among States account for additional differences in spending levels. Salaries, fringe benefits, and nonlabor costs vary among regions, affecting the price structure for hospital services. The admission rate and length of stay, affected by the severity and frequency of illness and by historical patterns of medical practice, influence the quantity of hospital services utilized. Interacting with these factors are the amount of services provided per employee, the supply of hospital beds that the area supports, occupancy rates, types of hospitals in the area, number of physicians, and the per capita personal income and age structure of the population.
One area of growing concern involves physician practice patterns related to wide variations in the rates of performance of specific procedures. For certain conditions, insufficient information exists relating to treatment options and outcomes. Regional variations tend to emerge in physician practice patterns when there is no clinical evidence to cause physicians to prefer one treatment option over another (Wennberg, 1984). Current research studies are aimed at determining the extent to which differences in regional patterns exist and the extent to which physician practices can be altered (Office of Technology Assessment, 1983).
Expenditures for care in community hospitals represent 86 percent of all spending for hospital care. Because they account for such a sizable share of total hospital spending, data for community hospitals will be examined in some detail.
In Table 12, some of the factors that influenced the per capita spending levels for community hospitals in 1982 are presented. These factors are useful in examining causes for regional differences in spending for hospital care.
Table 12. Community hospital statistics, by region and State: 1982.
| Region and State | Expenditure per capita | Number of hospitals | Expense per day of care | Labor expense per day of care | Salary per employee | Days of care per employee | Admission rate per 1,000 population | Expense per admission | Length of stay in days | Beds per 1,000 population | Occupancy rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| U.S. total | $495 | 5,801 | $327 | $186 | $15,319 | 96.9 | 157 | $2,883 | 7.6 | 4.4 | 75.3 |
| New England | 546 | 250 | 348 | 207 | 15,586 | 88.4 | 144 | 3,564 | — | 4.1 | — |
| Connecticut | 465 | 37 | 354 | 219 | 16,957 | 92.0 | 133 | 3,328 | 7.8 | 3.5 | 81.9 |
| Maine | 458 | 43 | 296 | 173 | 14,317 | 95.5 | 151 | 2,810 | 7.7 | 4.4 | 71.9 |
| Massachusetts | 661 | 113 | 370 | 216 | 15,696 | 85.1 | 152 | 4,105 | 8.9 | 4.5 | 82.8 |
| New Hampshire | 378 | 27 | 288 | 164 | 13,542 | 95.6 | 138 | 2,487 | 7.1 | 3.6 | 73.9 |
| Rhode Island | 485 | 14 | 332 | 211 | 14,947 | 83.9 | 134 | 3,380 | 8.5 | 3.7 | 84.9 |
| Vermont | 369 | 16 | 256 | 154 | 13,432 | 100.3 | 143 | 2,478 | 8.2 | 4.3 | 75.1 |
| Mideast | 545 | 688 | 314 | 184 | 16,010 | 102.7 | 153 | 3,315 | — | 4.5 | — |
| Delaware | 427 | 8 | 302 | 184 | 15,717 | 100.8 | 133 | 2,957 | 8.2 | 3.5 | 85.0 |
| District of Columbia | (1) | 12 | 459 | 269 | 18,700 | 81.0 | (1) | 4,612 | 8.7 | (1) | 82.8 |
| Maryland | 453 | 55 | 329 | 190 | 15,213 | 94.2 | 129 | 3,210 | 8.3 | 3.6 | 81.9 |
| New Jersey | 427 | 97 | 280 | 161 | 15,573 | 112.6 | 145 | 2,712 | 8.4 | 4.1 | 81.8 |
| New York | 574 | 272 | 312 | 188 | 16,657 | 105.8 | 149 | 3,607 | 9.7 | 4.5 | 87.3 |
| Pennsylvania | 577 | 244 | 320 | 182 | 15,256 | 98.3 | 166 | 3,194 | 8.5 | 4.8 | 80.5 |
| Great Lakes | 556 | 902 | 334 | 197 | 15,891 | 95.1 | 163 | 3,090 | — | 4.7 | — |
| Illinois | 632 | 241 | 369 | 213 | 16,872 | 92.8 | 168 | 3,351 | 8.0 | 5.0 | 73.6 |
| Indiana | 461 | 114 | 287 | 162 | 13,946 | 100.4 | 162 | 2,592 | 7.8 | 4.4 | 78.1 |
| Michigan | 571 | 205 | 357 | 214 | 16,635 | 92.3 | 154 | 3,351 | 8.0 | 4.4 | 77.2 |
| Ohio | 547 | 203 | 325 | 194 | 15,492 | 94.5 | 169 | 3,007 | 8.1 | 4.7 | 79.0 |
| Wisconsin | 469 | 139 | 283 | 169 | 14,951 | 103.0 | 157 | 2,724 | 8.3 | 5.0 | 71.3 |
| Plains | 518 | 799 | 280 | 160 | 14,247 | 102.5 | 179 | 2,630 | — | 5.8 | — |
| Iowa | 480 | 128 | 260 | 146 | 13,579 | 107.5 | 182 | 2,361 | 8.0 | 5.7 | 69.4 |
| Kansas | 500 | 146 | 292 | 166 | 14,107 | 97.2 | 177 | 2,600 | 7.8 | 5.8 | 65.4 |
| Minnesota | 484 | 169 | 257 | 156 | 14,503 | 107.9 | 159 | 2,730 | 9.4 | 5.7 | 72.2 |
| Missouri | 598 | 148 | 328 | 185 | 14,950 | 93.4 | 186 | 2,915 | 8.0 | 5.5 | 73.4 |
| Nebraska | 501 | 99 | 260 | 141 | 13,584 | 110.1 | 189 | 2,448 | 8.4 | 6.4 | 68.8 |
| North Dakota | 520 | 52 | 244 | 139 | 13,559 | 111.1 | 205 | 2,277 | 8.6 | 7.2 | 67.3 |
| South Dakota | 403 | 57 | 217 | 123 | 12,508 | 115.1 | 178 | 2,059 | 8.7 | 6.3 | 67.3 |
| Southeast | $431 | 1,467 | $285 | $153 | $13,551 | 102.6 | 171 | $2,294 | — | 4.5 | — |
| Alabama | 468 | 129 | 276 | 145 | 12,834 | 103.6 | 191 | 2,174 | 7.2 | 5.1 | 74.2 |
| Arkansas | 384 | 92 | 253 | 139 | 12,737 | 105.3 | 187 | 1,859 | 6.6 | 5.0 | 68.4 |
| Florida | 503 | 216 | 335 | 177 | 14,840 | 97.9 | 167 | 2,780 | 7.5 | 4.6 | 74.1 |
| Georgia | 399 | 162 | 284 | 154 | 12,923 | 97.0 | 170 | 2,156 | 6.7 | 4.4 | 70.6 |
| Kentucky | 382 | 106 | 261 | 142 | 13,504 | 109.4 | 180 | 1,974 | 6.7 | 4.2 | 78.3 |
| Louisiana | 471 | 138 | 337 | 175 | 14,169 | 92.5 | 176 | 2,412 | 6.3 | 4.4 | 70.1 |
| Mississippi | 367 | 108 | 227 | 122 | 11,928 | 112.8 | 184 | 1,772 | 7.0 | 5.1 | 69.5 |
| North Carolina | 356 | 132 | 258 | 145 | 13,070 | 104.0 | 149 | 2,196 | 7.5 | 4.0 | 77.0 |
| South Carolina | 312 | 71 | 251 | 136 | 12,973 | 110.3 | 138 | 2,134 | 7.4 | 3.7 | 76.0 |
| Tennessee | 518 | 146 | 275 | 146 | 12,923 | 103.3 | 207 | 2,176 | 7.2 | 5.5 | 74.7 |
| Virginia | 404 | 102 | 282 | 152 | 14,107 | 108.2 | 142 | 2,575 | 7.9 | 4.0 | 77.8 |
| West Virginia | 501 | 65 | 271 | 153 | 13,731 | 107.0 | 202 | 2,248 | 7.2 | 5.3 | 75.2 |
| Southwest | 415 | 716 | 322 | 172 | 14,067 | 94.3 | 160 | 2,397 | — | 4.0 | — |
| Arizona | 419 | 59 | 410 | 213 | 15,307 | 84.0 | 131 | 3,101 | 6.5 | 3.3 | 71.0 |
| New Mexico | 347 | 42 | 317 | 169 | 14,573 | 98.5 | 124 | 2,626 | 6.7 | 3.2 | 71.0 |
| Oklahoma | 422 | 120 | 333 | 182 | 13,916 | 88.5 | 166 | 2,425 | 6.5 | 4.2 | 70.2 |
| Texas | 419 | 495 | 307 | 164 | 13,847 | 97.1 | 167 | 2,272 | 6.6 | 4.2 | 72.0 |
| Rocky Mountain | 379 | 250 | 314 | 180 | 15,325 | 98.1 | 140 | 2,462 | — | 3.7 | — |
| Colorado | 428 | 80 | 336 | 197 | 16,618 | 96.2 | 142 | 2,782 | 7.1 | 3.8 | 71.8 |
| Idaho | 301 | 46 | 266 | 151 | 13,211 | 103.6 | 133 | 2,072 | 6.5 | 3.6 | 65.9 |
| Montana | 387 | 60 | 226 | 131 | 14,635 | 128.2 | 163 | 2,152 | 8.3 | 5.6 | 67.0 |
| Utah | 350 | 37 | 376 | 210 | 14,192 | 80.5 | 130 | 2,384 | 5.4 | 2.7 | 71.4 |
| Wyoming | 311 | 27 | 303 | 169 | 14,686 | 99.7 | 141 | 2,009 | 5.5 | 3.6 | 59.1 |
| Far West | 506 | 729 | 476 | 264 | 17,971 | 82.1 | 128 | 3,574 | — | 3.3 | — |
| California | 546 | 496 | 507 | 280 | 18,611 | 80.6 | 128 | 3,886 | 6.5 | 3.3 | 68.5 |
| Nevada | 579 | 19 | 493 | 255 | 17,898 | 85.2 | 144 | 3,500 | 6.3 | 3.6 | 68.8 |
| Oregon | 411 | 74 | 382 | 224 | 15,578 | 83.1 | 137 | 2,660 | 5.9 | 3.4 | 66.5 |
| Washington | 367 | 105 | 376 | 214 | 15,617 | 84.9 | 131 | 2,524 | 5.7 | 2.9 | 71.1 |
| Alaska | 370 | 16 | 508 | 302 | 23,594 | 92.2 | 93 | 3,633 | 5.9 | 2.3 | 65.4 |
| Hawaii | 343 | 19 | 307 | 168 | 14,758 | 103.1 | 102 | 2,780 | 8.3 | 2.9 | 80.8 |
Per capita estimates for the District of Columbia are not presented in this report, because significant proportions of services rendered in the District of Columbia are purchased by out-of-State residents. However, these estimates are included in regional and U.S. totals.
NOTE: Per capita expenditures in community hospitals are estimated by the Health Care Financing Administration, Office of the Actuary.
SOURCE: (American Hospital Association, 1977-83b).
In the United States in 1982, $495 per capita was spent for community hospital services. The Great Lakes region, with per capita expenditures of $556, had the highest spending level, followed closely by New England ($546) and the Mideast ($545). The Rocky Mountain region trailed all other regions in community hospital spending with $379 per capita. Expense per day of community hospital care ranged from a regional high of $476 in the Far West to regional lows of $280 in the Plains and $285 in the Southeast regions. The U.S. average was $327 per day. Labor expense accounted for 57 percent of total hospital expenses. The Southeast maintained the lowest labor expense at $153 per day of care; in the Far West labor costs per day amounted to $264. Labor expense nationwide amounted to $186 per day.
Annual salary per employee provides an indication of the wage levels of an area and the differences in cost of living that exist among States and regions. Nationwide an average of $15,319 was paid to community hospital employees. The Far West region paid the highest salaries and wages in the Nation, $17,971. The Southeast region paid the lowest, $13,551. Alaska paid the highest average salaries to their community hospital employees, $23,594. This amount was $4,894 higher than that paid in the District of Columbia, which recorded the second highest level of salaries and wages.
The days of care provided per full-time equivalent employee is a rough indicator of the intensity of service rendered. Also, the fewer the days of care for which each employee is responsible, the higher the cost is likely to be. In the Mideast, Plains, and Southeast regions, 103 days of care were provided per employee each year. In contrast, 82 days of care per employee were provided in the Far West.
Nationwide, the admission rate per 1,000 population was 157 in 1982. The rate of 179 admissions per 1,000 population in the Plains States contrasted with the Far West's 128 admissions per 1,000 population.
Expenses per admission averaged $2,883 in the United States. The Far West and New England regions led all other regions, with almost $3,600 in expenses per admission. The Southeast and Southwest regions trailed all other regions, with expenses per admission less than $2,400. Community hospitals in the District of Columbia and Massachusetts incurred the highest expenses per admission—$4,612 and $4,105, respectively. Mississippi ($1,772) and Arkansas ($1,859) registered the lowest expenses per admission, less than one-half that of the highest States.
The Plains region outpaced the Nation in community hospital beds maintained, with 5.8 beds per 1,000 population. In the Plains region, because of low population density and a larger-than-average proportion of elderly people, more beds per resident need to be available in order to offer easy access to the scattered population. The Far West maintained 3.3 beds per 1,000 residents, the lowest ratio maintained by any region.
Massachusetts' per capita community hospital spending of $661, the highest in the Nation, can be evaluated in the context of these community hospital statistics. Community hospital services in that State cost $370 per patient per day, the ninth highest daily expense in the Nation. Labor costs amounted to $216 per day. In days of care per employee, Massachusetts ranked eighth lowest at 85.1 days of care per employee. The length of stay in Massachusetts' community hospitals was the highest in the New England region and the third highest in the Nation. The combination of these factors led to the second highest expense per admission in the Nation.
One explanation for Massachusetts' high per capita hospital spending may be that Boston serves as the major medical center for northern New England, providing more specialized medical services than are available in most local community hospitals in the region. Admissions per 1,000 population are higher because nonresidents are attracted to the State for these specialized services. More complicated medical conditions are also likely to require labor-intensive services and longer than average lengths of stay. The combination of high cost per day, long length of stay, and the intense use of employees per day of care produces high expenses per admission.
The Great Lakes region had the highest per capita community hospital spending in the Nation in 1982. In the Far West, expense per day of community hospital care was $142 higher than the expense in the Great Lakes region. The Far West also had a lower number of days of care per employee and a labor expense per day over $65 higher than that in the Great Lakes region. Yet, per capita expenditures were $50 less in the Far West than in the Great Lakes. The significant factors in creating high costs in the Great Lakes appear to be a high admission rate (163 admissions per 1,000 population as opposed to 128 in the Far West) and a long average length of stay. Differences in the age structure and health status of the two populations contribute to the disparity in admission rates and lengths of stay. Variations in input prices, such as fuel, wages, and fringe benefits, could produce regional differences. Finally, differences in historical regional patterns of medical treatment that require hospital care and defined lengths of stay for particular medical procedures could affect per capita expenditures.
Physicians' services
From 1966 through 1982, 21-24 percent of every dollar spent on personal health care went for physicians' services, the second largest component of personal health care expenditures. Physicians' influence on the level of health care spending is even higher than data on physician expenditures indicate. Physicians prescribe and direct many medical services, including hospitalization and prescription drugs.
With the exception of the Far West region, where consumers spent $358 per person, variation in regional expenditures per capita for physician services was minimal, ranging from $272 in the Southwest region to $232 in the New England region (Table 11).
On a State-by-State basis, spending differences were more pronounced, ranging from a low of $144 per capita in Vermont to highs of $383 in California and $376 in Hawaii. Throughout the period 1966-82, California spending per person for this category of care has been the highest in the Nation. In five of the six States with high per capita spending for physicians' services, a large percentage of the total personal health care dollar goes for physician services. At least partially offsetting the high proportion devoted to physician care is a low proportion devoted to nursing home care. This is particularly noteworthy in Florida, which has the highest proportion of residents 65 years of age or over in the Nation.
The mix of reimbursement systems (fee-for-service, health maintenance organization, prepaid group practice, and insurance), standard of living, historical medical practices, and the concentration of physicians in each geographic area introduce different variables into physician expenditure patterns.
Per capita expenditures for physicians' services are related to the concentration of physicians in an area. An increase in the number of physicians tends to increase the amount of money spent for physician care, because more physicians' services have become available for purchase.
Table 13 shows the wide range in the number of non-Federal, office-based physicians per 10,000 population among the States and regions. The rate grew from 9.1 physicians per 10,000 population in 1969 to 12.4 physicians in 1981. For the same period, the Far West, and California specifically, maintained the lead over all other regions and States in concentration of physicians. (California also leads the Nation in physician expenditures per capita.) The lowest concentration of physicians in 1981 occurred in the Southeast (10.8 per 10,000 population), the Southwest (10.9), and the Plains (10.9) regions. In Mississippi, the rate of physicians per 10,000 population was the lowest in the Nation in 1981, at 8.3, and expenditures per capita for physician services were the third lowest in the Nation.
Table 13. Number of physicians, percent change, and rate per 10,000 population in 1969 and 1981, by region and State.
| Region and State | Number of physicians | Percent change 1969-81 | Physicans per 10,000 population | ||
|---|---|---|---|---|---|
|
|
|
||||
| 1969 | 1981 | 1969 | 1981 | ||
| U.S. total | 183,119 | 284,313 | 55.3 | 9.1 | 12.4 |
| New England | 12,122 | 17,816 | 47.0 | 10.3 | 14.4 |
| Connecticut | 3,343 | 4,699 | 40.6 | 11.1 | 15.1 |
| Maine | 757 | 1,261 | 66.6 | 7.6 | 11.1 |
| Massachusetts | 5,996 | 8,766 | 46.2 | 10.6 | 15.2 |
| New Hampshire | 694 | 1,161 | 67.3 | 9.6 | 12.4 |
| Rhode Island | 876 | 1,237 | 41.2 | 9.4 | 13.0 |
| Vermont | 456 | 692 | 51.8 | 10.4 | 13.4 |
| Mideast | 44,717 | 59,593 | 33.3 | 10.6 | 14.1 |
| Delaware | 472 | 699 | 48.1 | 8.7 | 11.7 |
| District of Columbia | 1,461 | 1,715 | 17.4 | 19.2 | 27.1 |
| Maryland | 3,392 | 6,479 | 91.0 | 8.8 | 15.2 |
| New Jersey | 6,627 | 9,487 | 43.2 | 9.3 | 12.8 |
| New York | 22,253 | 26,561 | 19.4 | 12.3 | 15.1 |
| Pennsylvania | 10,512 | 14,652 | 39.4 | 9.0 | 12.3 |
| Great Lakes | 32,013 | 46,141 | 44.1 | 8.0 | 11.1 |
| Illinois | 9,324 | 13,769 | 47.7 | 8.5 | 12.0 |
| Indiana | 3,838 | 5,224 | 36.1 | 7.5 | 9.5 |
| Michigan | 6,512 | 9,643 | 48.1 | 7.4 | 10.5 |
| Ohio | 8,754 | 11,928 | 36.3 | 8.3 | 11.1 |
| Wisconsin | 3,585 | 5,577 | 55.6 | 8.2 | 11.8 |
| Plains | 12,620 | 18,879 | 49.6 | 7.8 | 10.9 |
| Iowa | 2,026 | 2,661 | 31.3 | 7.2 | 9.1 |
| Kansas | 1,657 | 2,654 | 60.2 | 7.4 | 11.1 |
| Minnesota | 3,391 | 5,261 | 55.1 | 9.0 | 12.8 |
| Missouri | 3,456 | 5,217 | 51.0 | 7.5 | 10.6 |
| Nebraska | 1,180 | 1,739 | 47.4 | 8.0 | 11.0 |
| North Dakota | 473 | 715 | 51.2 | 7.6 | 10.8 |
| South Dakota | 437 | 632 | 44.6 | 6.5 | 9.1 |
| Southeast | 32,069 | 57,688 | 79.9 | 7.4 | 10.8 |
| Alabama | 2,172 | 3,688 | 69.8 | 6.3 | 9.4 |
| Arkansas | 1,249 | 2,201 | 76.2 | 6.5 | 9.6 |
| Florida | 5,885 | 13,463 | 128.8 | 8.9 | 13.2 |
| Georgia | 3,227 | 5,758 | 78.4 | 7.1 | 10.3 |
| Kentucky | 2,303 | 3,699 | 60.6 | 7.2 | 10.1 |
| Louisiana | 2,825 | 4,447 | 57.4 | 7.8 | 10.3 |
| Mississippi | 1,383 | 2,125 | 53.7 | 6.2 | 8.3 |
| North Carolina | 3,530 | 6,014 | 70.4 | 7.0 | 10.1 |
| South Carolina | 1,627 | 2,937 | 80.5 | 6.3 | 9.2 |
| Tennessee | 3,002 | 5,052 | 68.3 | 7.7 | 10.9 |
| Virginia | 3,606 | 6,438 | 78.5 | 7.8 | 11.8 |
| West Virginia | 1,260 | 1,866 | 48.1 | 7.2 | 9.5 |
| Southwest | 13,139 | 23,890 | 81.8 | 8.1 | 10.9 |
| Arizona | 1,581 | 3,519 | 122.6 | 9.1 | 12.5 |
| New Mexico | 725 | 1,464 | 101.9 | 7.2 | 11.0 |
| Oklahoma | 1,827 | 2,957 | 61.9 | 7.2 | 9.5 |
| Texas | 9,006 | 15,950 | 77.1 | 8.2 | 10.8 |
| Rocky Mountain | 4,639 | 8,073 | 74.0 | 9.4 | 11.9 |
| Colorado | 2,284 | 4,002 | 75.2 | 10.5 | 13.4 |
| Idaho | 554 | 910 | 64.3 | 7.8 | 9.4 |
| Montana | 599 | 937 | 56.4 | 8.6 | 11.8 |
| Utah | 941 | 1,765 | 87.6 | 9.0 | 11.6 |
| Wyoming | 261 | 459 | 75.9 | 7.9 | 9.3 |
| Far West | 31,800 | 52,233 | 64.3 | 11.9 | 15.7 |
| California | 25,045 | 39,987 | 59.7 | 12.7 | 16.5 |
| Nevada | 407 | 990 | 143.2 | 8.5 | 11.7 |
| Oregon | 2,052 | 3,716 | 81.1 | 10.0 | 13.9 |
| Washington | 3,355 | 5,732 | 70.8 | 10.0 | 13.5 |
| Alaska | 168 | 405 | 141.1 | 5.7 | 9.7 |
| Hawaii | 773 | 1,403 | 81.5 | 10.3 | 14.3 |
NOTE: Counts of physicians represent non-Federal, office-based physicians involved in patient care.
SOURCE: (American Medical Association, 1969, 1982).
During the period 1969-81, the number of physicians in the Mideast increased by 33 percent. During the same time period, the Southwest and Southeast regions experienced the largest percentage gains in number of physicians in the Nation: 82 and 80 percent, respectively. The variation in percentage change in the number of physicians among States has been dramatic, ranging from a low of 19 percent in New York to a high of 143 percent in Nevada. Alaska, Florida, Arizona, and New Mexico exhibited the next largest percentage increases in the United States, with 141, 129, 123, and 102 percent increases, respectively.
The States and regions experiencing large percentage increases in the number of physicians were also areas of large population growth. The net result was little change from 1969 to 1981 in regional and State rankings by physician concentration. The exceptions included Maryland and Alaska, which rose in physician concentration rank by at least 10 States, and Wyoming and Idaho, which dropped in physician concentration rank by at least 10 States.
Several precautions should be observed when using data from Table 13. First, the physicians in a State render services to nonresidents as well as residents, and residents may seek physicians' services in other States. States with major cities situated on their borders are particularly vulnerable to inflated physician-to-population ratios, because patients are likely to come from other States. Conversely, States adjoining out-of-State metropolitan areas may register lower physician-to-population ratios than actually exist, as residents receive physician care in other States.
A low physician-to-population ratio, by itself, should not be interpreted as an indication that an area is “underserved.” The needs of an area with low physician concentration could be met through the use of paraprofessionals, such as physician assistants and nurse practitioners. Similarly, a high physician-to-population ratio might exist in a geographic area, yet definite needs of the population might not be met. Examples exist where physician concentrations are high in wealthy areas of a State or city and low in poor areas. High physician concentration could also exist because of high concentrations of specialty care physicians, masking the need for general practitioners.
Another precaution related to physician density involves the age structure of an area and the health status associated with each age group. A younger population tends to require fewer health services than an older population does. Because physicians direct a large proportion of health services, one would expect areas with older populations to require greater concentrations of physicians. Florida's high concentration of elderly people supports a higher than average concentration of physicians. Conversely, States where the elderly population is a small proportion of the total population, such as Alaska and Wyoming, have lower physician concentration ratios.
Nursing home care
In 1982, nursing home expenditures accounted for 9.4 percent of personal health care expenditures, or $114 per capita nationwide. Distinct regional patterns in spending exist: from a high of $186 per person in New England to a low of $80 in the Southeast. Minnesota's expenditures were the highest in the Nation at $235 per capita. In Alaska, the smallest amount was spent per person for nursing home care, only $26 (Table 11).
The supply of nursing home beds provides an indication of the historical demand for these services; recently, certificate-of-need requirements in some States have affected the supply. The elderly use nursing home services more extensively than other age groups do. The concentration of beds per population 65 years or age or over shows regional variations in the availability of this service to the population most likely to use it.
The greatest supply of nursing home beds occurs in the Plains region, where 83 beds exist for each 1,000 persons 65 years of age or older (Table 14). The Plains region also has the greatest concentration of elderly people in the Nation, with over 13 percent of the population 65 years of age or over. In addition, per capita spending for nursing home care in the Plains region is the second highest in the Nation at $172 per person, well above the $114 per capita nationwide.
Table 14. Number of nursing home beds and number of beds per 1,000 population 65 years of age or over, by region and State: 1980.
| Region and State | Number of beds | Beds per 1,000 aged population |
|---|---|---|
| U.S. total | 1,537,338 | 60.2 |
| New England | 104,846 | 68.9 |
| Connecticut | 21,244 | 58.2 |
| Maine | 11,317 | 80.3 |
| Massachusetts | 52,254 | 71.9 |
| New Hampshire | 6,672 | 64.8 |
| Rhode Island | 8,653 | 68.1 |
| Vermont | 4,706 | 81.1 |
| Mideast | 244,120 | 48.0 |
| Delaware | 2,530 | 42.9 |
| District of Columbia | 3,180 | 43.0 |
| Maryland | 20,726 | 52.3 |
| New Jersey | 37,825 | 44.0 |
| New York | 103,952 | 48.1 |
| Pennsylvania | 75,907 | 49.6 |
| Great Lakes | 339,103 | 75.5 |
| Illinois | 88,383 | 70.0 |
| Indiana | 44,511 | 76.1 |
| Michigan | 80,082 | 87.8 |
| Ohio | 76,280 | 65.3 |
| Wisconsin | 49,847 | 88.4 |
| Plains | 182,558 | 83.0 |
| Iowa | 34,641 | 89.3 |
| Kansas | 25,208 | 82.4 |
| Minnesota | 41,931 | 87.4 |
| Missouri | 46,691 | 72.1 |
| Nebraska | 18,990 | 92.2 |
| North Dakota | 6,450 | 80.6 |
| South Dakota | 8,647 | 95.0 |
| Southeast | 265,897 | 42.8 |
| Alabama | 20,651 | 46.9 |
| Arkansas | 19,238 | 61.7 |
| Florida | 36,122 | 21.4 |
| Georgia | 30,041 | 58.1 |
| Kentucky | 26,265 | 64.1 |
| Louisiana | 21,672 | 53.6 |
| Mississippi | 12,253 | 42.4 |
| North Carolina | 32,173 | 53.4 |
| South Carolina | 11,990 | 41.8 |
| Tennessee | 21,692 | 41.9 |
| Virginia | 27,377 | 54.2 |
| West Virginia | 6,423 | 27.0 |
| Southwest | 140,813 | 64.9 |
| Arizona | 9,309 | 30.3 |
| New Mexico | 3,075 | 26.5 |
| Oklahoma | 27,101 | 72.1 |
| Texas | 101,328 | 73.9 |
| Rocky Mountain | 34,128 | 59.7 |
| Colorado | 17,310 | 70.1 |
| Idaho | 4,355 | 46.3 |
| Montana | 5,652 | 66.5 |
| Utah | 5,052 | 46.3 |
| Wyoming | 1,759 | 47.5 |
| Far West | 225,873 | 68.4 |
| California | 163,482 | 67.7 |
| Nevada | 2,022 | 30.6 |
| Oregon | 17,382 | 57.4 |
| Washington | 39,153 | 90.6 |
| Alaska | 1,029 | 85.8 |
| Hawaii | 2,805 | 36.9 |
SOURCE: (Sirrocco, 1983).
The supply of nursing home beds for the elderly population is lowest in the Southeast region, where the rate of beds per 1,000 elderly residents is just over one-half that of the Plains region. Despite the fact that the concentration of elderly people in the Southeast is greater than the U.S. average, the supply of nursing home care is small, reflected both in available beds per population 65 years of age or over and in the per capita spending for nursing home services.
Climate appears to play a role in the demand for nursing home care. Figure 2 illustrates the areas where high per capita spending for this service exists. Clearly, higher per capita spending exists in areas where more severe climatic conditions exist.
Drugs and medical sundries
Drug expenditures consitute the fourth largest component of personal health care expenditures. In 1982, spending for drugs amounted to $94 per capita nationwide.
Throughout the 16-year period 1966-82, the Far West region and the State of Nevada maintained the highest per capita spending patterns for regions and States, with 1982 spending levels for drugs and medical sundries of $104 and $126, respectively. The Rocky Mountain and Plains regions registered the lowest per capita expenditures, with $83 and $84, respectively, in 1982. For the same year, New Mexico's expenditures of $75 per capita were the lowest in the Nation (Table 11).
Dentists' services
In 1982, $84 per person was spent on dental care. This amount represents 6.9 percent of personal health care expenditures. Spending ranged from a low of $40 per person in Mississippi, to highs of $133 per person in Hawaii and $131 in Washington. Regionally, the Southeast spent the least per person on dental care, with an average expenditure of $62 in 1982. At the other extreme, $124 worth of dental services were purchased per person in the Far West.
Other personal health care
The remaining portions of personal health care expenditures—other professional services, eyeglasses and appliances, and other health services—comprised 6.9 percent of personal health care expenditures in 1982. Their impact on regional and State spending patterns is minimal. Over the 16-year period, these categories declined in importance, dropping from 9.4 percent of personal health care expenditures in 1966 to the 1982 level of 6.9 percent. Nationwide, $84 per capita was spent for these services. Per capita spending ranged from a low of $54 in Alabama and Utah to a high of $121 in New York and California.
Economic and demographic factors
Many factors affect regional and state levels of health care spending. Foremost among those factors are the income with which care can be purchased and the size and age composition of the population consuming care.
Personal income
Personal income comprises income from all sources less personal contributions to social insurance programs such as social security, Medicare, and government retirement programs, but before removal of Federal, State, and local taxes. It includes wages and salaries, employer contributions to health and welfare funds, employer payments in kind, and income from self-employment, dividends, interest, rents, and royalties as well as transfer payments such as Social Security and Medicare benefits.
Variations in per capita personal income act as a barometer of the level of spending on health care. As disposable income levels change, consumers may choose to vary the amount allocated to health care spending. At higher levels of income, consumers can opt for more intense usage of health care services, such as private hospital rooms, cosmetic surgery, and discretionary purchases of prescription eyeglasses and contact lenses, without infringing on income used to purchase necessities.
In addition, wages, the largest component of personal income, are a major expense item in the labor-intensive health care sector. As wages rise (reflected in rises in personal income), prices charged for health services must increase to cover the added cost of labor.
Finally, the level of per capita personal income in an area influences the “target” level of income for health professionals. The prices charged by some health professionals may reflect their desire to reach a preconceived level of income in relation to other incomes in the area.
In 1982 per capita personal income in the United States amounted to $11,113. During the period 1966-82, per capita personal income rose at an average annual rate of 8.6 percent.
Leading the United States in per capita income in 1982 was the Far West region, with income of $12,314 per person. The Southeast, with per capita personal income of $9,657, was lower than any other region in personal income by more than $1,000 per person (Table 15).
Table 15. Per capita personal income, by region and State: Selected calendar years 1966-82.
| Region and State | 1966 | 1969 | 1972 | 1976 | 1977 | 1978 | 1979 | 1980 | 1981 | 1982 |
|---|---|---|---|---|---|---|---|---|---|---|
| U.S. total | $2,980 | $3,713 | $4,515 | $6,367 | $6,984 | $7,772 | $8,651 | $9,491 | $10,544 | $11,113 |
| New England | 3,248 | 4,048 | 4,849 | 6,625 | 7,231 | 8,027 | 8,958 | 10,032 | 11,193 | 12,118 |
| Connecticut | 3,792 | 4,664 | 5,465 | 7,446 | 8,187 | 9,100 | 10,241 | 11,546 | 12,895 | 13,937 |
| Maine | 2,457 | 3,040 | 3,710 | 5,344 | 5,774 | 6,305 | 6,971 | 7,770 | 8,621 | 9,267 |
| Massachusetts | 3,231 | 4,073 | 4,948 | 6,703 | 7,306 | 8,108 | 9,034 | 10,115 | 11,286 | 12,286 |
| New Hampshire | 2,883 | 3,590 | 4,261 | 5,962 | 6,553 | 7,372 | 8,239 | 9,145 | 10,215 | 11,130 |
| Rhode Island | 3,019 | 3,690 | 4,435 | 6,183 | 6,755 | 7,436 | 8,257 | 9,232 | 10,245 | 10,930 |
| Vermont | 2,666 | 3,302 | 3,948 | 5,363 | 5,754 | 6,576 | 7,275 | 7,957 | 9,025 | 9,519 |
| Mideast | 3,340 | 4,169 | 5,043 | 6,911 | 7,500 | 8,268 | 9,148 | 10,151 | 11,260 | 12,056 |
| Delaware | 3,527 | 4,289 | 5,150 | 7,008 | 7,535 | 8,254 | 9,118 | 10,076 | 11,079 | 11,912 |
| District of Columbia | 3,590 | 4,434 | 5,683 | 8,094 | 8,889 | 9,934 | 11,058 | 12,282 | 13,666 | 14,740 |
| Maryland | 3,172 | 4,020 | 4,963 | 7,016 | 7,590 | 8,465 | 9,399 | 10,397 | 11,546 | 12,281 |
| New Jersey | 3,550 | 4,405 | 5,381 | 7,368 | 8,025 | 8,883 | 9,819 | 10,977 | 12,203 | 13,164 |
| New York | 3,540 | 4,408 | 5,264 | 7,008 | 7,568 | 8,308 | 9,168 | 10,199 | 11,347 | 12,204 |
| Pennsylvania | 2,940 | 3,684 | 4,477 | 6,375 | 6,962 | 7,666 | 8,511 | 9,370 | 10,323 | 10,928 |
| Great Lakes | 3,223 | 3,930 | 4,698 | 6,673 | 7,388 | 8,168 | 9,042 | 9,726 | 10,602 | 10,985 |
| Illinois | 3,529 | 4,287 | 5,138 | 7,311 | 8,014 | 8,815 | 9,766 | 10,465 | 11,598 | 12,027 |
| Indiana | 2,998 | 3,647 | 4,324 | 6,224 | 6,814 | 7,531 | 8,291 | 8,928 | 9,810 | 10,020 |
| Michigan | 3,271 | 3,970 | 4,794 | 6,717 | 7,555 | 8,411 | 9,222 | 9,827 | 10,455 | 10,751 |
| Ohio | 3,097 | 3,815 | 4,505 | 6,405 | 7,094 | 7,811 | 8,670 | 9,416 | 10,221 | 10,660 |
| Wisconsin | 2,917 | 3,564 | 4,310 | 6,169 | 6,867 | 7,681 | 8,659 | 9,379 | 10,262 | 10,774 |
| Plains | 2,856 | 3,507 | 4,366 | 6,156 | 6,824 | 7,631 | 8,558 | 9,200 | 10,400 | 10,873 |
| Iowa | 3,010 | 3,586 | 4,416 | 6,303 | 6,972 | 7,900 | 8,697 | 9,238 | 10,524 | 10,635 |
| Kansas | 2,869 | 3,523 | 4,548 | 6,543 | 7,140 | 7,983 | 9,193 | 9,883 | 11,160 | 11,848 |
| Minnesota | 2,901 | 3,636 | 4,430 | 6,308 | 7,160 | 7,915 | 8,874 | 9,674 | 10,725 | 11,289 |
| Missouri | 2,823 | 3,462 | 4,236 | 5,925 | 6,570 | 7,278 | 8,163 | 8,821 | 9,819 | 10,402 |
| Nebraska | 2,863 | 3,560 | 4,467 | 6,201 | 6,736 | 7,531 | 8,458 | 8,899 | 10,450 | 10,887 |
| North Dakota | 2,535 | 3,137 | 4,350 | 5,927 | 6,126 | 7,372 | 8,006 | 8,642 | 10,766 | 10,862 |
| South Dakota | 2,457 | 2,930 | 3,895 | 5,106 | 5,844 | 6,628 | 7,499 | 7,808 | 9,014 | 9,339 |
| Southeast | $2,321 | $2,998 | $3,807 | $5,430 | $5,957 | $6,662 | $7,400 | $8,138 | $9,105 | $9,657 |
| Alabama | 2,113 | 2,699 | 3,424 | 5,079 | 5,572 | 6,231 | 6,864 | 7,464 | 8,234 | 8,684 |
| Arkansas | 2,047 | 2,556 | 3,267 | 4,865 | 5,400 | 6,022 | 6,653 | 7,124 | 8,019 | 8,444 |
| Florida | 2,604 | 3,474 | 4,439 | 5,938 | 6,544 | 7,407 | 8,296 | 9,205 | 10,388 | 10,929 |
| Georgia | 2,406 | 3,107 | 3,930 | 5,446 | 5,944 | 6,659 | 7,350 | 8,007 | 8,947 | 9,636 |
| Kentucky | 2,255 | 2,878 | 3,587 | 5,266 | 5,798 | 6,380 | 7,127 | 7,688 | 8,603 | 9,122 |
| Louisiana | 2,290 | 2,854 | 3,489 | 5,356 | 5,914 | 6,638 | 7,460 | 8,395 | 9,565 | 10,064 |
| Mississippi | 1,798 | 2,339 | 3,072 | 4,444 | 4,964 | 5,474 | 6,078 | 6,570 | 7,261 | 7,732 |
| North Carolina | 2,326 | 2,999 | 3,785 | 5,336 | 5,760 | 6,445 | 7,084 | 7,775 | 8,658 | 9,148 |
| South Carolina | 2,127 | 2,756 | 3,490 | 4,994 | 5,431 | 6,051 | 6,712 | 7,378 | 8,170 | 8,612 |
| Tennessee | 2,268 | 2,896 | 3,658 | 5,216 | 5,688 | 6,414 | 7,061 | 7,714 | 8,553 | 9,028 |
| Virginia | 2,652 | 3,441 | 4,376 | 6,258 | 6,897 | 7,643 | 8,483 | 9,404 | 10,554 | 11,353 |
| West Virginia | 2,212 | 2,735 | 3,575 | 5,341 | 5,830 | 6,365 | 7,099 | 7,770 | 8,396 | 8,966 |
| Southwest | 2,518 | 3,239 | 3,967 | 5,922 | 6,534 | 7,298 | 8,270 | 9,179 | 10,491 | 11,042 |
| Arizona | 2,529 | 3,367 | 4,287 | 5,704 | 6,211 | 7,080 | 8,011 | 8,821 | 9,819 | 10,053 |
| New Mexico | 2,315 | 2,839 | 3,589 | 5,307 | 5,789 | 6,523 | 7,190 | 7,923 | 8,777 | 9,285 |
| Oklahoma | 2,441 | 3,085 | 3,770 | 5,687 | 6,298 | 6,953 | 8,003 | 8,996 | 10,332 | 11,070 |
| Texas | 2,553 | 3,292 | 3,991 | 6,070 | 6,713 | 7,484 | 8,477 | 9,400 | 10,807 | 11,380 |
| Rocky Mountain | 2,708 | 3,303 | 4,224 | 6,044 | 6,581 | 7,420 | 8,260 | 9,112 | 10,176 | 10,675 |
| Colorado | 2,891 | 3,569 | 4,573 | 6,504 | 7,097 | 8,028 | 9,080 | 10,105 | 11,446 | 12,237 |
| Idaho | 2,479 | 3,078 | 3,907 | 5,650 | 6,092 | 6,827 | 7,382 | 8,091 | 8,948 | 9,012 |
| Montana | 2,653 | 3,144 | 4,093 | 5,774 | 6,171 | 7,022 | 7,565 | 8,345 | 9,251 | 9,616 |
| Utah | 2,499 | 2,960 | 3,729 | 5,293 | 5,805 | 6,436 | 7,082 | 7,630 | 8,322 | 8,696 |
| Wyoming | 2,830 | 3,462 | 4,392 | 6,766 | 7,508 | 8,607 | 9,804 | 10,937 | 12,114 | 12,230 |
| Far West | 3,413 | 4,181 | 4,943 | 7,083 | 7,767 | 8,743 | 9,775 | 10,756 | 11,822 | 12,314 |
| California | 3,494 | 4,282 | 5,062 | 7,154 | 7,862 | 8,859 | 9,951 | 10,998 | 12,105 | 12,617 |
| Nevada | 3,327 | 4,335 | 5,146 | 7,019 | 7,810 | 8,985 | 9,942 | 10,768 | 11,777 | 11,917 |
| Oregon | 2,927 | 3,520 | 4,343 | 6,352 | 6,976 | 7,829 | 8,643 | 9,300 | 9,939 | 10,149 |
| Washington | 3,293 | 3,969 | 4,524 | 6,815 | 7,424 | 8,464 | 9,429 | 10,231 | 11,255 | 11,694 |
| Alaska | 3,450 | 4,253 | 5,327 | 10,514 | 10,814 | 11,074 | 11,598 | 12,933 | 14,976 | 16,872 |
| Hawaii | 3,162 | 4,152 | 5,046 | 6,884 | 7,598 | 8,338 | 9,113 | 10,113 | 11,089 | 11,587 |
SOURCE: (Bureau of Economic Analysis, 1984a).
These regional differences in the levels of per capita personal income nevertheless represent a substantial narrowing of regional variation since 1929. The trend toward convergence of income is basically a result of the narrowing of regional differences in industrial distribution, in the percent of working-age population, and in wage rates (Garnick, 1982). Similarly, narrowing of differences in personal health care expenditures per capita over time can be observed (Figure 3).
In 1982, Alaska recorded the highest per capita personal income of any State—$16,872 per person. This high level of income was caused by the direct disbursement to State residents of taxes paid by the oil industry for depletion of that natural resource. Personal income per capita in Alaska exceeded that of the next highest State, Connecticut, by almost $3,000. At the opposite end of the scale, 1982 per capita personal income in Mississippi ($7,732), Arkansas ($8,444), and South Carolina ($8,612) remained the lowest in the Nation.
Measurement of the correlation between State personal health expenditures and State personal income is not appropriate for several reasons. In the first place, estimates of per capita personal income are produced on a location-of-residence basis, but personal health expenditures are calculated to reflect location of service.
Secondly, the concept of personal income excludes many public program payments for personal health care; only Medicare and workers' compensation benefits are included. Vendor payment programs (including Medicaid and State public assistance), health services provided directly by the Veterans' Administration and Department of Defense, and all other Federal, State, and local programs accounted for more than 20 percent of personal health care financing in 1982. However, they are excluded from the personal income measures.
Finally, public program health expenditures, by their nature, imply a redistribution of income. Federal Government funds are not necessarily allocated to States in the same proportions as they are received by the Federal Treasury in the form of tax revenues. In some cases, such as Medicare and workers' compensation, distribution of funds is based on age or disability. In other cases, distribution formulas based on the inverse of personal income are used, so the lowest income States (which generate the least tax revenue) receive the greatest proportion of the funds. Examples include grant programs such as Medicaid and Maternal and Child Health.
For these reasons, personal income provides only a partial indication of the ability to consume personal health care. Federal, State, and local programs, which accounted for 40 percent of all personal health care financing in 1982, are meant to make health care available regardless of income.
Population
During the period 1966-82, personal health expenditures in the United States grew at an annual rate of 13.1 percent. Population growth is an important factor affecting personal health care spending: As population increases, expenditures for health care grow as the demand for services for more people is met. From 1966 to 1982, the resident population of the United States grew from 195.5 million to 231.8 million persons (Bureau of the Census, 1984b).
The present change in the population structure, “aging” of the population, is another source of increased utilization: Health expenditures grow because of the larger number of older individuals, who require more frequent and expensive medical services (Waldo and Lazenby, 1984). The most recent estimate of personal health care spending by age indicates that, in 1978, elderly people accounted for 7.1 times the amount of per capita personal health care spending than did the population 18 years of age or under. Per capita purchases of personal health care goods and services for the age cohort 19-64 years amounted to 2.7 times the amount for the population 18 years of age or under (Fisher, 1980).
Despite the overall growth in population, an absolute decline occurred in the population under the age of 18 years. In 1966, 36.1 percent of the total population consisted of individuals under 18 years of age; by 1982, the percentage had dropped to 27.1, a decline of 12.5 percent. The cohort 18-64 years of age registered the largest absolute gains during the period, growing from 54.5 to 61.3 percent of total population. The cohort 65 years of age or over exhibited the highest growth rate, increasing by 45.3 percent—from 9.4 percent of total population in 1966 to 11.6 percent in 1982 (Table 16).
Table 16. Percent distribution of resident population in 1966 and 1982 and percent change 1966-82, by age.
| Age | 1966 | 1982 | Percent change 1966-82 |
|---|---|---|---|
|
| |||
| Percent distribution | |||
| Total | 100.0 | 100.0 | 18.6 |
| Under 18 years | 36.1 | 27.1 | −12.5 |
| 18-64 years | 54.5 | 61.3 | 33.0 |
| 65 years or over | 9.4 | 11.6 | 45.3 |
SOURCE: U.S. Department of Commerce, Bureau of the Census.
The Southwest and Rocky Mountain regions had the largest gains in population from 1966 to 1982 (Table 17), each increasing more than 46 percent. The Mideast and Great Lakes regions grew the least, exhibiting increases of 2.4 and 6.8 percent, respectively.
Table 17. Resident population, percent of population under 18 years of age, and percent of population 65 years of age or over in 1966 and 1982 and average annual percent change 1966-82.
| Region and State | All ages | Under 18 years | 65 years or over | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Number in thousands | Average annual percent change 1966-82 | Percent | Average annual percent change 1966-82 | Percent | Average annual percent change 1966-82 | ||||
|
|
|
|
|||||||
| 1966 | 1982 | 1966 | 1982 | 1966 | 1982 | ||||
| U.S. total | 195,499 | 231,786 | 1.1 | 36.1 | 27.1 | −.7 | 9.4 | 11.6 | 2.4 |
| New England | 11,430 | 12,433 | .5 | 34.5 | 25.1 | −1.4 | 10.7 | 12.8 | 1.7 |
| Connecticut | 2,903 | 3,126 | .5 | 34.6 | 24.8 | −1.6 | 9.3 | 12.4 | 2.3 |
| Maine | 999 | 1,136 | .8 | 36.2 | 27.3 | −.9 | 11.6 | 12.9 | 1.6 |
| Massachusetts | 5,535 | 5,750 | .2 | 34.2 | 24.5 | −1.7 | 11.3 | 13.1 | 1.3 |
| New Hampshire | 681 | 948 | 2.1 | 35.4 | 26.7 | .4 | 11.2 | 11.5 | 2.3 |
| Rhode Island | 899 | 953 | .4 | 33.1 | 24.3 | −1.5 | 10.7 | 13.9 | 2.0 |
| Vermont | 413 | 520 | 1.5 | 36.3 | 27.1 | −.3 | 11.5 | 11.7 | 1.6 |
| Mideast | 41,360 | 42,369 | .2 | 33.8 | 25.4 | −1.6 | 9.9 | 12.4 | 1.6 |
| Delaware | 516 | 600 | .9 | 37.5 | 26.3 | −1.2 | 7.8 | 10.5 | 2.9 |
| District of Columbia | 791 | 626 | −1.5 | 34.2 | 21.7 | −4.3 | 8.6 | 11.8 | .4 |
| Maryland | 3,695 | 4,270 | .9 | 37.1 | 26.0 | −1.1 | 7.2 | 9.9 | 3.1 |
| New Jersey | 6,851 | 7,427 | .5 | 33.9 | 25.6 | −1.3 | 9.3 | 12.1 | 2.2 |
| New York | 17,843 | 17,567 | −.1 | 33.1 | 25.5 | −1.8 | 10.4 | 12.5 | 1.0 |
| Pennsylvania | 11,664 | 11,879 | .1 | 33.7 | 25.2 | −1.7 | 10.4 | 13.5 | 1.8 |
| Great Lakes | 38,951 | 41,581 | .4 | 36.7 | 27.7 | −1.3 | 9.3 | 11.3 | 1.6 |
| Illinois | 10,836 | 11,466 | .4 | 35.5 | 27.4 | −1.2 | 9.7 | 11.4 | 1.4 |
| Indiana | 4,999 | 5,482 | .6 | 36.9 | 28.2 | −1.1 | 9.5 | 11.2 | 1.7 |
| Michigan | 8,512 | 9,116 | .4 | 38.0 | 28.3 | −1.4 | 8.4 | 10.6 | 1.9 |
| Ohio | 10,330 | 10,772 | .3 | 36.7 | 27.5 | −1.6 | 9.1 | 11.4 | 1.6 |
| Wisconsin | 4,274 | 4,745 | .7 | 37.3 | 27.5 | −1.1 | 10.7 | 12.4 | 1.8 |
| Plains | 15,888 | 17,344 | .5 | 36.2 | 27.3 | −1.2 | 11.5 | 13.1 | 1.3 |
| Iowa | 2,762 | 2,906 | .3 | 35.9 | 27.4 | −1.4 | 12.4 | 13.8 | 1.0 |
| Kansas | 2,200 | 2,408 | .6 | 35.6 | 26.8 | −1.4 | 11.2 | 13.1 | 1.3 |
| Minnesota | 3,617 | 4,133 | .8 | 38.0 | 27.6 | −1.1 | 10.9 | 12.1 | 1.5 |
| Missouri | 4,523 | 4,942 | .6 | 34.5 | 26.7 | −1.1 | 11.6 | 13.5 | 1.4 |
| Nebraska | 1,456 | 1,589 | .5 | 36.4 | 27.8 | −1.1 | 12.1 | 13.3 | 1.2 |
| North Dakota | 647 | 672 | .2 | 38.6 | 28.9 | −1.5 | 9.8 | 12.5 | 1.8 |
| South Dakota | 683 | 694 | .1 | 38.7 | 29.1 | −1.6 | 11.5 | 13.5 | 1.2 |
| Southeast | 42,257 | 54,354 | 1.6 | 37.2 | 27.3 | −.4 | 8.9 | 12.1 | 3.5 |
| Alabama | 3,464 | 3,941 | .8 | 37.9 | 28.6 | −1.0 | 8.4 | 11.7 | 2.8 |
| Arkansas | 1,899 | 2,307 | 1.2 | 36.4 | 28.3 | −.6 | 11.0 | 14.0 | 2.6 |
| Florida | 6,104 | 10,466 | 3.4 | 34.4 | 23.3 | 1.1 | 12.5 | 17.3 | 5.8 |
| Georgia | 4,379 | 5,648 | 1.6 | 38.1 | 28.9 | −.3 | 7.4 | 9.7 | 3.3 |
| Kentucky | 3,147 | 3,692 | 1.0 | 36.6 | 28.4 | −.6 | 10.0 | 11.5 | 1.8 |
| Louisiana | 3,550 | 4,383 | 1.3 | 40.2 | 30.8 | −.5 | 7.6 | 9.6 | 2.7 |
| Mississippi | 2,245 | 2,569 | .8 | 40.2 | 31.3 | −1.0 | 8.8 | 11.6 | 2.3 |
| North Carolina | 4,896 | 6,019 | 1.3 | 37.2 | 26.8 | −.9 | 7.4 | 10.8 | 3.6 |
| South Carolina | 2,520 | 3,227 | 1.6 | 39.4 | 28.9 | −.6 | 6.6 | 9.6 | 3.8 |
| Tennessee | 3,822 | 4,656 | 1.2 | 35.7 | 27.1 | −.6 | 9.1 | 11.7 | 2.8 |
| Virginia | 4,456 | 5,485 | 1.3 | 36.6 | 26.2 | −.8 | 7.3 | 9.8 | 3.1 |
| West Virginia | 1,775 | 1,961 | .6 | 35.3 | 27.8 | −1.0 | 10.4 | 12.6 | 1.7 |
| Southwest | 15,567 | 22,814 | 2.4 | 38.0 | 29.3 | .7 | 8.4 | 10.1 | 3.4 |
| Arizona | 1,614 | 2,892 | 3.7 | 39.9 | 28.4 | 1.5 | 7.7 | 11.8 | 6.5 |
| New Mexico | 1,007 | 1,367 | 1.9 | 43.8 | 31.1 | −.2 | 6.1 | 9.2 | 4.5 |
| Oklahoma | 2,454 | 3,226 | 1.7 | 34.2 | 27.8 | .4 | 11.0 | 12.1 | 2.2 |
| Texas | 10,492 | 15,329 | 2.4 | 38.0 | 29.7 | .7 | 8.2 | 9.4 | 3.2 |
| Rocky Mountain | 4,735 | 6,933 | 2.4 | 38.9 | 30.7 | 1.0 | 8.5 | 8.8 | 2.7 |
| Colorado | 2,007 | 3,071 | 2.7 | 37.3 | 27.2 | .8 | 8.8 | 8.6 | 2.6 |
| Idaho | 689 | 977 | 2.2 | 38.7 | 32.2 | .9 | 9.0 | 10.3 | 3.0 |
| Montana | 707 | 805 | .8 | 38.5 | 28.8 | −1.0 | 9.4 | 11.2 | 2.0 |
| Utah | 1,009 | 1,571 | 2.8 | 42.4 | 37.3 | 2.0 | 6.8 | 7.5 | 3.4 |
| Wyoming | 323 | 509 | 2.9 | 38.4 | 31.0 | 1.6 | 9.1 | 7.7 | 1.9 |
| Far West | 25,311 | 33,958 | 1.9 | 35.7 | 26.5 | .0 | 8.7 | 10.4 | 3.0 |
| California | 18,858 | 24,697 | 1.7 | 35.5 | 26.2 | −.1 | 8.6 | 10.3 | 2.9 |
| Nevada | 446 | 876 | 4.3 | 37.7 | 26.0 | 2.1 | 5.5 | 8.8 | 7.6 |
| Oregon | 1,969 | 2,668 | 1.9 | 34.6 | 26.8 | .3 | 10.4 | 12.1 | 2.9 |
| Washington | 3,057 | 4,276 | 2.1 | 35.6 | 26.9 | .3 | 9.7 | 10.8 | 2.8 |
| Alaska | 271 | 444 | 3.1 | 43.8 | 32.0 | 1.3 | 1.9 | 2.9 | 6.2 |
| Hawaii | 710 | 997 | 2.1 | 39.6 | 28.0 | −.2 | 4.9 | 8.5 | 5.5 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary. Population figures supplied by U.S. Department of Commerce, Bureau of the Census.
The most dramatic increases in total population during the period 1966-82 occurred in the States of Nevada (96 percent), Arizona (79 percent), and Florida (71 percent). Each of these States also recorded large increases in the aged population, with population in the group 65 years of age or over growing 200 percent or more.
In contrast, the District of Columbia and New York lost population from 1966 to 1982. Pennsylvania, South Dakota, Massachusetts, and North Dakota had population gains of 4 percent or less.
Population growth and “aging” of the population influence personal health care expenditure growth by region and State. Although these two factors accounted for a small percentage of the national growth rate in personal health expenditures from 1966-78 (the last period for which spending data for all age groups are available), their impact on the variation in expenditure growth among regions and States was more dramatic. When the effects of population growth and “aging” are removed from the growth in personal health expenditures, the range in growth rates narrows considerably, clustering more closely around the U.S. average. Population gains and losses and the age composition of States and regions seems to account for a large proportion of the variations that occur in personal health care expenditure growth rates (Levit, 1982).
Definitions and methodology
The per capita estimates presented in this report are based on estimates of personal health expenditures shown in Tables 18 through 22. In the following descriptions of the methods used to estimate personal health expenditures by State, distributors by type of service are developed and then adjusted to equal NHE service totals. The validity of this method of estimating is predicated on the assumption that estimates of health expenditures for the Nation provide a more accurate level of spending than does the summation of any available State data used to produce State estimates.
Table 18. Personal health care expenditures, by type of expenditure, region, and State: Calendar year 1966.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in millions | |||||||||
| U.S. total | $39,267.5 | $15,603.4 | $9,175.3 | $2,964.1 | $1,159.4 | $5,462.4 | $1,314.7 | $2,356.0 | $1,232.2 |
| New England | 2,677.1 | 1,152.7 | 558.8 | 195.4 | 90.1 | 301.5 | 90.6 | 225.0 | 73.7 |
| Connecticut | 684.9 | 263.1 | 161.7 | 56.0 | 28.7 | 84.2 | 17.0 | 53.9 | 20.3 |
| Maine | 172.9 | 73.7 | 36.3 | 9.5 | 5.2 | 22.9 | 7.4 | 14.7 | 3.2 |
| Massachusetts | 1,402.2 | 639.5 | 271.6 | 106.4 | 41.3 | 143.0 | 40.9 | 124.3 | 35.1 |
| New Hampshire | 128.0 | 50.0 | 29.5 | 7.7 | 5.8 | 15.5 | 3.8 | 10.6 | 5.2 |
| Rhode Island | 207.7 | 91.0 | 44.5 | 10.8 | 5.8 | 26.0 | 7.5 | 13.6 | 8.5 |
| Vermont | 81.3 | 35.3 | 15.2 | 5.0 | 3.2 | 9.8 | 3.3 | 7.9 | 1.5 |
| Mideast | 9,413.3 | 3,914.7 | 2,221.4 | 756.7 | 301.5 | 1,119.4 | 284.7 | 536.8 | 319.8 |
| Delaware | 107.7 | 47.1 | 22.2 | 5.9 | 3.9 | 17.2 | 3.0 | 3.9 | 4.5 |
| District of Columbia | 339.9 | 151.5 | 94.6 | 26.1 | 9.4 | 38.3 | 4.7 | 4.8 | 10.4 |
| Maryland | 703.6 | 312.1 | 147.9 | 47.6 | 19.7 | 101.2 | 20.1 | 34.1 | 21.0 |
| New Jersey | 1,316.7 | 483.8 | 337.1 | 115.4 | 43.3 | 191.0 | 36.3 | 66.0 | 43.9 |
| New York | 4,606.8 | 1,967.7 | 1,087.2 | 393.4 | 141.4 | 468.2 | 102.8 | 290.8 | 155.3 |
| Pennsylvania | 2,338.6 | 952.6 | 532.3 | 168.3 | 83.8 | 303.6 | 76.2 | 137.2 | 84.6 |
| Great Lakes | 7,920.6 | 3,142.4 | 1,870.1 | 561.2 | 204.5 | 1,146.4 | 271.9 | 466.6 | 226.0 |
| Illinois | 2,380.4 | 974.8 | 535.6 | 168.0 | 62.9 | 337.3 | 93.5 | 136.9 | 71.4 |
| Indiana | 909.9 | 316.9 | 233.5 | 59.4 | 19.5 | 153.3 | 43.3 | 59.9 | 24.1 |
| Michigan | 1,796.5 | 763.0 | 411.6 | 132.3 | 40.6 | 256.9 | 56.8 | 84.4 | 50.9 |
| Ohio | 2,013.2 | 762.0 | 496.9 | 140.5 | 56.8 | 299.8 | 77.7 | 124.3 | 55.2 |
| Wisconsin | 820.6 | 325.8 | 192.4 | 61.0 | 24.7 | 99.0 | 32.1 | 61.2 | 24.4 |
| Plains | 3,182.6 | 1,257.3 | 695.7 | 226.7 | 92.8 | 428.8 | 123.6 | 283.9 | 70.4 |
| Iowa | 545.1 | 190.0 | 130.2 | 39.7 | 16.3 | 71.9 | 25.4 | 61.5 | 10.0 |
| Kansas | 428.4 | 166.6 | 89.6 | 27.3 | 14.0 | 59.7 | 23.2 | 39.4 | 8.5 |
| Minnesota | 780.3 | 321.5 | 156.1 | 60.7 | 21.8 | 95.1 | 23.5 | 80.1 | 21.4 |
| Missouri | 894.6 | 365.1 | 204.9 | 61.9 | 29.8 | 129.6 | 29.4 | 53.7 | 20.4 |
| Nebraska | 283.3 | 109.1 | 64.5 | 21.9 | 5.7 | 39.6 | 11.9 | 24.4 | 6.3 |
| North Dakota | 127.2 | 53.5 | 27.9 | 6.8 | 2.4 | 16.7 | 6.2 | 12.1 | 1.6 |
| South Dakota | 123.8 | 51.5 | 22.5 | 8.5 | 2.7 | 16.2 | 7.7 | 12.6 | 2.2 |
| Southeast | $6,464.8 | $2,559.4 | $1,524.3 | $437.4 | $180.0 | $1,044.8 | $229.0 | $319.4 | $189.8 |
| Alabama | 501.9 | 210.3 | 118.2 | 32.8 | 12.6 | 75.8 | 13.6 | 27.2 | 11.3 |
| Arkansas | 268.9 | 106.0 | 56.2 | 15.3 | 5.5 | 43.6 | 10.5 | 25.1 | 6.7 |
| Florida | 1,125.1 | 403.2 | 265.1 | 91.3 | 48.6 | 195.6 | 28.4 | 66.5 | 26.4 |
| Georgia | 658.1 | 247.3 | 171.8 | 45.6 | 16.2 | 104.7 | 19.0 | 33.7 | 19.8 |
| Kentucky | 488.4 | 190.1 | 118.1 | 28.5 | 10.8 | 78.7 | 17.7 | 28.4 | 16.1 |
| Louisiana | 555.3 | 221.9 | 138.1 | 36.2 | 13.5 | 90.8 | 16.0 | 28.4 | 10.4 |
| Mississippi | 257.4 | 107.5 | 59.7 | 15.3 | 8.6 | 44.0 | 8.3 | 8.7 | 5.3 |
| North Carolina | 701.0 | 279.6 | 162.5 | 45.1 | 18.1 | 120.2 | 24.0 | 31.8 | 19.7 |
| South Carolina | 314.8 | 128.8 | 61.3 | 18.1 | 9.0 | 53.5 | 13.1 | 14.7 | 16.3 |
| Tennessee | 633.9 | 257.7 | 154.7 | 43.4 | 14.2 | 97.4 | 24.3 | 21.5 | 20.9 |
| Virginia | 673.7 | 282.3 | 148.3 | 49.5 | 17.2 | 99.3 | 23.5 | 27.4 | 26.2 |
| West Virginia | 286.3 | 124.9 | 70.4 | 16.3 | 5.7 | 41.3 | 11.3 | 6.0 | 10.5 |
| Southwest | 2,773.6 | 1,072.6 | 629.2 | 169.5 | 79.1 | 446.3 | 91.1 | 177.4 | 108.1 |
| Arizona | 307.0 | 125.4 | 78.5 | 20.9 | 8.5 | 46.3 | 6.3 | 13.0 | 7.9 |
| New Mexico | 157.7 | 69.2 | 29.9 | 10.6 | 4.2 | 25.7 | 5.5 | 5.4 | 7.1 |
| Oklahoma | 448.7 | 154.0 | 108.0 | 27.0 | 9.7 | 64.9 | 16.0 | 47.1 | 22.0 |
| Texas | 1,860.3 | 723.9 | 412.7 | 111.1 | 56.7 | 309.4 | 63.5 | 111.9 | 71.1 |
| Rocky Mountain | 920.3 | 368.3 | 202.1 | 66.6 | 25.4 | 136.4 | 41.0 | 56.7 | 33.6 |
| Colorado | 467.3 | 200.1 | 94.7 | 31.8 | 14.2 | 59.7 | 11.7 | 29.5 | 25.5 |
| Idaho | 105.3 | 34.6 | 24.5 | 8.5 | 2.7 | 20.2 | 4.7 | 8.1 | 1.9 |
| Montana | 124.0 | 47.5 | 26.3 | 7.9 | 3.2 | 20.9 | 7.5 | 8.4 | 2.4 |
| Utah | 159.0 | 58.7 | 40.4 | 14.2 | 3.6 | 26.1 | 4.4 | 8.6 | 3.1 |
| Wyoming | 64.6 | 27.3 | 16.2 | 4.1 | 1.7 | 9.5 | 2.9 | 2.1 | .8 |
| Far West | 5,915.1 | 2,136.0 | 1,473.8 | 550.5 | 186.0 | 838.8 | 182.8 | 290.2 | 210.8 |
| California | 4,560.3 | 1,658.6 | 1,148.7 | 427.1 | 150.2 | 635.3 | 175.9 | 200.7 | 163.7 |
| Nevada | 87.4 | 30.4 | 20.5 | 6.5 | 2.6 | 18.6 | 2.8 | 2.9 | 3.1 |
| Oregon | 388.0 | 130.5 | 91.4 | 37.7 | 11.4 | 57.4 | 18.8 | 33.1 | 7.7 |
| Washington | 669.8 | 219.8 | 172.1 | 62.2 | 17.7 | 102.1 | 26.0 | 48.9 | 21.1 |
| Alaska | 61.6 | 40.3 | 7.7 | 2.9 | 1.1 | 6.3 | 1.4 | .4 | 1.6 |
| Hawaii | 147.9 | 56.4 | 33.3 | 14.2 | 3.1 | 19.2 | 4.1 | 4.2 | 13.6 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Table 22. Personal health care expenditures, by type of expenditure, region, and State: Calendar year 1982.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in millions | |||||||||
| U.S. total | $282,805.1 | $133,702.8 | $61,774.6 | $19,465.4 | $7,091.9 | $21,800.6 | $5,507.8 | $26,498.4 | $6,963.6 |
| New England | 16,853.6 | 8,313.1 | 2,887.3 | 1,096.6 | 456.5 | 1,095.2 | 302.9 | 2,315.8 | 386.2 |
| Connecticut | 4,213.4 | 1,807.9 | 824.5 | 349.5 | 125.6 | 305.5 | 65.1 | 642.8 | 92.5 |
| Maine | 1,239.5 | 587.4 | 214.4 | 61.0 | 31.5 | 88.3 | 26.3 | 199.9 | 30.8 |
| Massachusetts | 8,669.9 | 4,659.4 | 1,336.5 | 500.6 | 230.2 | 497.1 | 154.1 | 1,105.7 | 186.3 |
| New Hampshire | 934.5 | 433.8 | 195.1 | 70.4 | 26.5 | 81.2 | 16.2 | 85.4 | 26.0 |
| Rhode Island | 1,287.9 | 594.2 | 241.9 | 78.6 | 28.2 | 80.1 | 26.4 | 204.4 | 34.1 |
| Vermont | 508.4 | 230.5 | 74.8 | 36.5 | 14.6 | 43.0 | 14.8 | 77.6 | 16.7 |
| Mideast | 56,026.2 | 27,821.3 | 10,755.5 | 3,645.4 | 1,909.5 | 3,680.7 | 835.5 | 5,851.2 | 1,527.1 |
| Delaware | 691.7 | 331.1 | 151.2 | 51.7 | 13.0 | 58.9 | 12.3 | 51.4 | 22.1 |
| District of Columbia | 1,776.9 | 1,264.9 | 259.9 | 45.1 | 26.4 | 74.2 | 15.1 | 34.7 | 56.5 |
| Maryland | 5,261.8 | 2,587.6 | 1,116.7 | 373.4 | 114.9 | 392.3 | 86.7 | 436.2 | 153.9 |
| New Jersey | 8,281.4 | 3,696.2 | 1,834.5 | 728.0 | 257.4 | 684.2 | 139.7 | 718.2 | 223.0 |
| New York | 24,893.3 | 11,921.6 | 4,635.4 | 1,508.0 | 1,094.2 | 1,474.6 | 316.3 | 3,233.4 | 709.9 |
| Pennsylvania | 15,121.2 | 8,019.9 | 2,757.8 | 939.1 | 403.6 | 996.5 | 265.4 | 1,377.3 | 361.7 |
| Great Lakes | 51,927.5 | 25,574.3 | 10,571.7 | 3,576.9 | 905.3 | 3,827.8 | 1,048.0 | 5,180.0 | 1,243.6 |
| Illinois | 14,998.4 | 8,027.5 | 2,805.7 | 957.1 | 304.0 | 953.9 | 323.8 | 1,251.2 | 375.1 |
| Indiana | 6,035.7 | 2,809.3 | 1,186.3 | 331.2 | 92.9 | 610.6 | 149.0 | 708.3 | 148.0 |
| Michigan | 11,678.3 | 5,724.9 | 2,420.0 | 996.4 | 177.8 | 910.7 | 182.3 | 970.0 | 296.1 |
| Ohio | 13,430.8 | 6,456.7 | 2,870.8 | 833.4 | 207.7 | 971.3 | 260.6 | 1,537.1 | 293.1 |
| Wisconsin | 5,784.3 | 2,555.8 | 1,288.9 | 458.8 | 122.8 | 381.2 | 132.2 | 713.5 | 131.2 |
| Plains | 21,531.4 | 10,259.8 | 4,154.0 | 1,340.3 | 475.0 | 1,463.0 | 492.2 | 2,981.7 | 365.3 |
| Iowa | 3,418.4 | 1,556.6 | 667.1 | 221.0 | 90.1 | 247.4 | 88.6 | 488.4 | 59.2 |
| Kansas | 3,059.7 | 1,427.5 | 646.6 | 176.6 | 62.5 | 206.5 | 99.5 | 392.4 | 48.2 |
| Minnesota | 5,078.9 | 2,233.3 | 874.9 | 395.8 | 103.5 | 321.5 | 94.6 | 971.8 | 83.5 |
| Missouri | 6,351.7 | 3,353.2 | 1,169.9 | 340.0 | 143.5 | 438.3 | 109.9 | 688.3 | 108.6 |
| Nebraska | 1,931.5 | 902.4 | 430.6 | 116.9 | 38.3 | 145.0 | 45.4 | 222.1 | 30.7 |
| North Dakota | 890.6 | 419.2 | 212.6 | 48.4 | 16.3 | 51.1 | 26.8 | 103.8 | 12.4 |
| South Dakota | 800.7 | 367.6 | 152.3 | 41.7 | 20.8 | 53.2 | 27.5 | 114.8 | 22.8 |
| Southeast | $57,366.8 | $27,430.0 | $13,405.5 | $3,383.1 | $1,085.4 | $5,353.7 | $1,044.8 | $4,343.3 | $1,321.0 |
| Alabama | 4,072.0 | 2,132.3 | 839.8 | 202.7 | 62.4 | 373.0 | 55.8 | 311.1 | 94.9 |
| Arkansas | 2,292.3 | 1,021.9 | 504.9 | 114.0 | 43.9 | 237.7 | 51.0 | 259.3 | 59.7 |
| Florida | 12,847.6 | 5,951.6 | 3,575.2 | 808.8 | 284.7 | 1,094.2 | 211.2 | 684.9 | 237.2 |
| Georgia | 5,920.3 | 2,780.6 | 1,429.9 | 360.3 | 89.3 | 562.8 | 94.4 | 443.6 | 159.5 |
| Kentucky | 3,532.7 | 1,598.9 | 757.1 | 198.5 | 87.0 | 350.3 | 77.1 | 383.5 | 80.4 |
| Louisiana | 4,847.1 | 2,408.1 | 1,096.7 | 258.9 | 97.3 | 422.9 | 77.9 | 389.4 | 95.8 |
| Mississippi | 2,303.6 | 1,106.3 | 487.3 | 102.8 | 56.4 | 223.6 | 37.7 | 230.2 | 59.3 |
| North Carolina | 5,602.0 | 2,575.1 | 1,215.5 | 367.5 | 96.5 | 647.6 | 109.3 | 452.3 | 138.1 |
| South Carolina | 2,766.8 | 1,281.5 | 555.5 | 163.2 | 43.1 | 312.8 | 65.5 | 246.6 | 98.6 |
| Tennessee | 5,326.4 | 2,689.7 | 1,207.2 | 295.8 | 108.2 | 448.0 | 114.5 | 355.9 | 107.0 |
| Virginia | 5,783.3 | 2,777.1 | 1,306.8 | 406.6 | 83.4 | 495.9 | 107.4 | 464.4 | 141.7 |
| West Virginia | 2,072.7 | 1,106.9 | 429.9 | 104.0 | 33.1 | 185.0 | 43.0 | 122.2 | 48.7 |
| Southwest | 24,973.2 | 11,249.3 | 6,195.2 | 1,595.8 | 510.6 | 2,286.9 | 545.5 | 1,935.1 | 654.8 |
| Arizona | 3,216.8 | 1,441.4 | 879.1 | 267.1 | 69.3 | 272.0 | 41.2 | 154.2 | 92.4 |
| New Mexico | 1,235.6 | 613.2 | 257.0 | 85.3 | 30.1 | 103.2 | 33.3 | 67.2 | 46.3 |
| Oklahoma | 3,502.6 | 1,607.9 | 755.9 | 197.0 | 63.1 | 331.4 | 91.6 | 357.2 | 98.4 |
| Texas | 17,018.3 | 7,586.8 | 4,303.1 | 1,046.4 | 348.1 | 1,580.3 | 379.3 | 1,356.5 | 417.8 |
| Rocky Mountain | 7,248.5 | 3,225.9 | 1,649.6 | 612.1 | 205.1 | 578.4 | 169.6 | 600.9 | 206.9 |
| Colorado | 3,714.3 | 1,710.9 | 805.5 | 304.1 | 110.0 | 257.7 | 76.4 | 320.3 | 129.4 |
| Idaho | 848.1 | 327.4 | 208.2 | 75.9 | 26.7 | 87.9 | 24.5 | 81.9 | 15.6 |
| Montana | 834.2 | 358.1 | 197.3 | 64.5 | 22.3 | 68.5 | 27.1 | 74.2 | 22.1 |
| Utah | 1,407.4 | 627.1 | 338.2 | 133.1 | 34.5 | 123.8 | 21.7 | 99.7 | 29.2 |
| Wyoming | 444.5 | 202.4 | 100.3 | 34.4 | 11.6 | 40.5 | 19.9 | 24.7 | 10.6 |
| Far West | 46,877.8 | 19,829.1 | 12,155.9 | 4,215.1 | 1,544.6 | 3,514.8 | 1,069.2 | 3,290.4 | 1,258.6 |
| California | 35,829.0 | 15,450.2 | 9,458.4 | 3,085.2 | 1,213.8 | 2,585.5 | 796.5 | 2,255.9 | 983.6 |
| Nevada | 1,208.7 | 551.5 | 314.1 | 93.3 | 28.2 | 110.0 | 22.1 | 71.8 | 17.7 |
| Oregon | 3,107.5 | 1,249.6 | 743.6 | 289.6 | 86.5 | 286.8 | 86.6 | 300.9 | 64.0 |
| Washington | 4,981.3 | 1,855.3 | 1,144.8 | 558.7 | 181.6 | 393.5 | 132.3 | 587.7 | 127.4 |
| Alaska | 526.9 | 244.9 | 120.6 | 55.4 | 13.7 | 46.0 | 9.2 | 11.3 | 25.8 |
| Hawaii | 1,224.4 | 477.6 | 374.5 | 133.0 | 20.8 | 92.9 | 22.6 | 62.8 | 40.1 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
The sum of the State estimates sometimes differs from the NHE service totals. The difference is the amount spent on services provided in U.S. territories or possessions (as in the case of hospital expenditures and “other health services”); services rendered by U.S. taxpayers while living abroad (as in the case of physician, dental, and other professional expenditures); and services paid for with public funds and furnished to U.S. military and civilian personnel living abroad or stationed on military vessels (as in the case of “other health services”).
The State personal health care expenditures presented in this report incorporate 1966 and 1969 estimates previously published in Personal Health Care Expenditures by State (Cooper, Worthington, and Piro, 1975) and in theHealth Care Financing Review (Levit, 1982). Since the publication of the 1966 and 1969 estimates, concepts and definitions of some NHE types of service have been revised, and a few additional data sources have become available. Both of these changes have led to the introduction of different methodologies. Further changes in the earlier estimates result from the preparation of these series on a calendar year, rather than fiscal year, basis.
The methodology presented in this article explains the estimation procedure beginning with data for 1976. The methodology used to produce estimates for 1966-72 can be found in earlier publications (Levit, 1982; Cooper, Worthington, and Piro, 1975).
Hospital care
Expenditures for hospital care include spending for all services billed through hospitals: room and board, drugs and other medical durable and nondurable goods, hospital outpatient and emergency room services, services provided by hospital personnel (including salaried physicians), and hospital-based home health services. The fees of self-employed physicians treating patients in a hospital setting are usually billed through the physicians' offices and are included as part of expenditures for physicians' services.
Hospital care, as measured by the National Health Expenditure series, is based on the total net revenues of community hospitals and the expenses of all noncommunity hospitals. The revenue concept has been adopted for community hospitals because it reflects the actual income with which a hospital operates. Revenue data include income from sources such as endowment funds, government grants, and contributions but exclude the costs of such items as charity cases and bad debts. Expenses are assumed to be equivalent to revenues in noncommunity hospitals.
Survey data compiled by the American Hospital Association (American Hospital Association, 1976-83a), which include expenses for each hospital in the United States, constitute the major data source for State estimates of hospital expenditures. In order to correspond in concept to the national methodology, each community hospital's expenses were adjusted to reflect revenues by applying a statewide revenue-to-expense ratio (American Hospital Association, 1977-83b).2 To compensate for different reporting periods, revenue or expense estimates for individual hospitals were linked with estimates for adjoining years. These estimates were adjusted to a calendar year based on the proportion of the reported financial year falling within a given calendar year and then adjusted to NHE totals.
The American Hospital Association (AHA) data have several limitations. AHA solicits data by mail questionnaires from hospitals in the United States and U.S.-associated areas. In 1982, 90.5 percent of all AHA-registered hospitals responded.
The response rate varied by hospital size, region, and type of control. In 1982, the lowest regional response rate for registered community hospitals (83.0 percent) came from the AHA's West South Central Region (Arkansas, Louisiana, Oklahoma, and Texas). The AHA's Mountain Region (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, and Wyoming) had the highest response rate (95.6 percent). The response rate by bed size increased steadily from a low of 77.7 percent for hospitals with 6-24 beds to a high of 97.3 percent for hospitals with 400-499 beds, with the response rate declining slightly for larger hospitals. By type of control, nongovernment nonprofit hospitals were most likely to respond (95.5 percent), and nongovernment for-profit hospitals responded least (79.6 percent) (American Hospital Association, 1983b).
In cases where responses were not received, AHA estimated missing cells. Until 1978, the estimation procedure involved grouping all hospitals with similar geographic and demographic characteristics, then estimating missing data by using mean values for similar hospitals that did report. This procedure resulted in inconsistent expense data for individual hospitals; the estimated expenses were not linked to actual expenses reported in prior years. Beginning in 1978, a revised estimation procedure was used in estimating missing data cells. Whenever possible, estimated cells were linked to data for prior years.
Physician, dental, and other professional services
The major segments of spending for physician, dental, and other health professional services were estimated by using Internal Revenue Service (IRS) business tax return information.
The IRS publishes data on business receipts by business type in itsStatistics of Income (SOI) publications. SOI data are generated from stratified samples drawn from the universe of proprietorship, partnership, and corporate returns. Among the published data are tables on business receipts for the medical sector in selected States for selected types of businesses. It is this source that forms the basis for national estimates of physician, dental, and other professional health expenditures.
Over the past few years, samples extracted to produce the SOI have diminished in size, with less and less emphasis placed on stratifying the samples to yield State-reliable data. The result is an increasing proportion of suppressed information in the State tables and less reliability in the State data that are published.
In order to create the most reliable estimates possible, the Health Care Financing Administration contracted with the IRS to prepare State-by-State tabulations of tax information for the medical sector. Using the business master file (BMF) data base, total receipts for physicians, dentists, and other medical professionals were compiled by State for 1976, 1977, 1981, and 1982.
The BMF information provides a complete reliable source for estimating medical expenditures by State. It differs from the SOI sample data used to estimate the National Health Expenditures in the following ways.
First, the National Health Expenditures estimates for physicians, dentists, and other health professionals are based predominantly on IRS business receipts from the SOI sample. Total receipts from the BMF that are used to distribute spending by State include business receipts plus “investment income such as interest, rents, royalties, nonqualifying dividends, net gain from sale of noncapital assets, income from farms and other partnerships, and ‘other’ income” (Internal Revenue Service, 1979).
Second, industrial classification accounts for additional differences between business receipt data from the SOI used in the National Health Expenditures and the total receipts used to produce data on State expenditures. In the SOI, samples are drawn and industrial classification verified. As many as one-third of the sample of corporate returns are reclassified to different categories (Powell and Stubbs, unpublished). (The percentage of reclassification in the medical industry specifically and for sole proprietorships and partnerships may be considerably lower.)
The industrial classification of total receipt data, however, is not verified. For partnerships and corporations, the industry code is chosen by the filer to represent the business activity that generated the largest proportion of total receipts. For sole proprietorships, a written explanation of the business activity provided by the filer is assigned an industry code by an IRS clerk as the data are encoded for computer processing.
Spending for physician care covers all services supplied and billed through medical physicians' and osteopathic physicians' offices, including medical laboratory tests requested by the physician and direct billing by independent laboratories. Excluded is the cost of examinations performed to qualify an individual for life insurance coverage.
For 1976, 1977, 1981, and 1982, State estimates of spending for physician care relied on total receipt data tabulated by the IRS for medical and osteopathic physicians. Total receipts include all payments for services billed through physicians' offices. Estimates for 1978-80 represent a straight-line interpolation between 1977 and 1981 State estimates, subsequently adjusted to NHE totals.
Expenditures for dental care include spending for all services billed through dental offices, including services provided by dental laboratories. For 1976, 1977, 1981, and 1982, IRS tabulations of total receipts of dentists were adjusted to NHE totals. Estimates for 1978-80 were developed using a straight-line interpolation between 1977 and 1981 estimates by State. These results were adjusted to NHE totals.
“Other professional services” include the remainder of health professionals in private practice. Among these professionals are private duty nurses, chiropractors, optometrists, dieticians, podiatrists, psychologists, and physiotherapists. In addition, home health services provided through nonhospital-related agencies are included in “other professional services.” Excluded from these estimates is the portion of optometrists' receipts that accounts for the purchase of eyeglasses.
For 1976, 1977, 1981, and 1982, the distribution by State of these health professionals in private practice was based on IRS business receipt data for sole proprietorships and partnerships. The deduction of optometrist receipts for the cost of eyeglasses was allocated to States using IRS total receipts for optometrist sole proprietorships and partnerships. For 1978-80, estimates were developed using a straight-line interpolation between 1977 and 1981 estimates by State. These results were adjusted to NHE totals.
Home health expenditures by State were estimated in three parts: Medicare, Medicaid, and other. State estimates for Medicare home health were derived from interim reimbursement data recorded on home health bills for a 40-percent sample of Medicare enrollees. Data on Medicaid home health allocators came from information on Form HCFA-2082, provided by States. The remainder, less than 20 percent of home health expenditures, were based on the distribution of the population 65 years of age or over (Bureau of the Census, 1980, 1984a).
Drugs and sundries, eyeglasses and appliances
Drugs and medical sundries, eyeglasses and orthopedic appliances include expenditures for products purchased in retail stores. Specifically excluded are products furnished in hospitals, nursing homes, and the offices of medical professionals, because expenditures for these items are included in the institutions' or professionals' charges.
State distributions for drugs and medical sundries were developed from data on merchandise sales of drugs and health aids (Bureau of the Census, 1972, 1977). Data for 1972 and 1977 were extrapolated and interpolated using total resident population (Bureau of the Census, 1984b) to produce allocators for all remaining years. These allocators were adjusted to NHE totals.
The distribution of expenditures for eyeglasses and appliances is based on unpublished data from the Health Resources Administration, calculated by using unpublished IRS tabulations, on the number of optometrists by State and their average receipts. Distributions of optometrists' receipts for 1976 and 1977 were extrapolated forward to 1982 on the basis of personal income (Bureau of Economic Analysis, 1984a).
Nursing home care
Nursing home expenditures cover care rendered in skilled nursing and intermediate care facilities, including those for the mentally retarded. The costs of long-term care provided by hospitals are excluded.
The definition of “nursing home care” has been revised since the original publication of the 1966 and 1969 State series. In 1972, legislation was enacted to expand Medicaid coverage to services rendered in intermediate facilities, including facilities for the mentally retarded. At that time, the definition of nursing home care was expanded to include these services. Before that time, services rendered in intermediate care facilities were not classified as a health expenditure.
Nursing home receipts from the 1977 Census of Health Services (Bureau of the Census, 1981) form the basis of the latest State estimates. To develop estimates for 1976 and 1978-82, nursing home wages (Bureau of Economic Analysis, 1984b) were inflated to reflect revenues by applying revenue-to-wage ratios calculated by type of facility control (Bloom, 1981). The inflated wages were used to extrapolate the 1977 estimates. For 1976-82, expenditures for intermediate care facilities for the mentally retarded were estimated as an independent segment of nursing home care, using data reported by the Medicaid State agencies on Form HCFA-2082.
Other health services
The category “other health services” includes all personal health services that cannot be encompassed in any of the previously defined categories. Included are expenditures for such services as industrial inplant health services, medical services rendered to shipboard military personnel, school health services, spending for transportation to medical facilities by ambulance or other methods, and multifaceted health services rendered through Federal grant programs.
Allocators for industrial inplant health services are the product of the number of occupational health nurses (American Nurses' Association, 1979) and their average weekly wages (American Nurses' Association, 1978; Bureau of Labor Statistics, 1976-78). From 1978 to 1982, this distribution has remained constant.
The Department of Defense accounts for another large proportion of other health spending. The cost of health care rendered to active duty military personnel stationed in areas without access to military hospitals (shipboard medical facilities and field medical stations) and other miscellaneous care are included. The distribution by State is based on special tabulations supplied by the Department of Defense.
Federal grant programs such as Maternal and Child Health, community health centers, and community block grants and programs of the Alcohol, Drug Abuse, and Mental Health Administration fund other personal health services. Estimates of expenditures for these grant programs are distributed by State based on information on grant appropriations by State that are supplied by the funding agencies.
Data on expenditures for school health by State come from information on health services expenditures in public schools (National Center for Education Statistics, 1978, 1979, 1980, 1982). The distribution of “other health services” provided by the Veterans' Administration is estimated using data on expenditures for services in VA hospitals and nursing homes.
“Other health services” funded by Medicare include ambulance services and, starting in 1976, dialysis treatments in freestanding renal dialysis centers. This definitional change reflects legislation enacted in 1972 that extended Medicare coverage to people with kidney disease. State distributions of unpublished supplementary medical insurance (SMI) reimbursements for ambulance services were extrapolated from 1978 to 1982 using reimbursement data for physicians and other SMI suppliers. Medicare payments to freestanding dialysis centers for 1980-82 were estimated based on unpublished treatment data reported by facilities in each State. Payments were extrapolated to 1976 using the numbers of dialysis stations in freestanding facilities. The distributions for each year were adjusted to equal the NHE total.
Medicaid and other public assistance medical payments for other health services were allocated to States using State-reported spending data from Form HCFA-2082. Indian Health Service spending for other health services was distributed by State using unpublished tabulations of ambulatory and contract care appropriations.
Table 19. Personal health care expenditures, by type of expenditure, region, and State: Calendar year 1976.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in millions | |||||||||
| U.S. total | $131,517.3 | $60,152.7 | $27,556.6 | $9,444.4 | $3,193.5 | $13,022.3 | $3,412.9 | $11,318.9 | $3,416.1 |
| New England | 8,359.2 | 4,084.8 | 1,401.4 | 557.5 | 179.3 | 690.5 | 190.6 | 1,041.1 | 214.0 |
| Connecticut | 2,082.3 | 911.0 | 389.1 | 168.1 | 48.5 | 193.6 | 38.7 | 277.9 | 55.2 |
| Maine | 589.4 | 267.3 | 108.1 | 32.0 | 14.6 | 54.6 | 19.0 | 76.2 | 17.6 |
| Massachusetts | 4,365.1 | 2,299.0 | 656.3 | 270.7 | 85.6 | 319.5 | 96.1 | 540.1 | 97.9 |
| New Hampshire | 428.7 | 179.8 | 98.1 | 31.9 | 12.9 | 45.2 | 10.7 | 36.3 | 13.9 |
| Rhode Island | 636.1 | 310.4 | 115.1 | 35.7 | 11.2 | 51.9 | 17.7 | 74.0 | 20.1 |
| Vermont | 257.6 | 117.5 | 34.6 | 19.2 | 6.5 | 25.7 | 8.4 | 36.5 | 9.2 |
| Mideast | 28,439.9 | 14,181.9 | 5,156.7 | 1,878.1 | 772.2 | 2,373.8 | 566.5 | 2,670.3 | 840.4 |
| Delaware | 353.6 | 171.9 | 70.4 | 23.3 | 5.9 | 37.9 | 7.4 | 24.8 | 12.0 |
| District of Columbia | 933.4 | 625.0 | 153.1 | 25.8 | 11.0 | 58.0 | 10.2 | 15.0 | 35.4 |
| Maryland | 2,527.9 | 1,192.0 | 533.2 | 193.3 | 42.9 | 245.1 | 54.4 | 192.7 | 74.4 |
| New Jersey | 4,245.1 | 1,863.3 | 935.6 | 358.9 | 105.1 | 429.4 | 87.9 | 333.4 | 131.5 |
| New York | 13,360.1 | 6,760.2 | 2,211.0 | 844.7 | 439.5 | 969.9 | 223.1 | 1,529.5 | 382.1 |
| Pennsylvania | 7,019.8 | 3,569.5 | 1,253.3 | 432.2 | 167.6 | 633.5 | 183.7 | 574.9 | 205.1 |
| Great Lakes | 25,126.9 | 11,801.6 | 5,060.7 | 1,791.2 | 475.9 | 2,431.6 | 724.9 | 2,235.5 | 605.4 |
| Illinois | 7,192.1 | 3,667.1 | 1,297.1 | 473.5 | 139.0 | 612.3 | 221.0 | 590.5 | 191.7 |
| Indiana | 2,918.9 | 1,265.2 | 554.5 | 174.2 | 59.0 | 376.5 | 105.7 | 309.5 | 74.4 |
| Michigan | 5,795.3 | 2,696.9 | 1,216.3 | 494.1 | 97.0 | 586.6 | 136.3 | 442.0 | 126.1 |
| Ohio | 6,418.6 | 2,940.4 | 1,389.1 | 436.7 | 125.3 | 625.2 | 182.3 | 566.1 | 153.4 |
| Wisconsin | 2,802.0 | 1,232.1 | 603.7 | 212.7 | 55.6 | 231.0 | 79.7 | 327.4 | 59.8 |
| Plains | 10,083.8 | 4,560.4 | 1,978.4 | 695.3 | 244.6 | 914.5 | 316.9 | 1,167.5 | 206.2 |
| Iowa | 1,634.3 | 689.9 | 294.6 | 117.0 | 47.7 | 156.6 | 60.8 | 235.0 | 32.8 |
| Kansas | 1,306.6 | 620.0 | 224.6 | 62.8 | 30.1 | 130.6 | 60.2 | 149.6 | 28.7 |
| Minnesota | 2,386.1 | 1,076.9 | 413.3 | 181.7 | 43.4 | 195.5 | 61.0 | 362.7 | 51.6 |
| Missouri | 3,034.2 | 1,427.8 | 675.7 | 216.0 | 78.9 | 275.5 | 72.0 | 229.1 | 59.1 |
| Nebraska | 927.6 | 402.1 | 197.0 | 63.3 | 21.3 | 91.3 | 29.8 | 105.4 | 17.4 |
| North Dakota | 437.0 | 183.0 | 116.5 | 34.1 | 11.2 | 30.8 | 15.8 | 38.7 | 6.9 |
| South Dakota | 358.0 | 160.6 | 56.8 | 20.3 | 12.0 | 34.0 | 17.4 | 47.1 | 9.7 |
| Southeast | $25,172.7 | $11,335.6 | $5,658.8 | $1,662.2 | $545.4 | $3,063.9 | $622.7 | $1,642.6 | $641.5 |
| Alabama | 1,872.9 | 890.0 | 384.0 | 111.4 | 33.2 | 222.9 | 38.5 | 149.5 | 43.3 |
| Arkansas | 1,019.3 | 428.6 | 208.7 | 54.1 | 22.3 | 138.6 | 31.2 | 107.8 | 28.0 |
| Florida | 5,401.0 | 2,318.5 | 1,459.7 | 412.6 | 154.0 | 579.0 | 100.1 | 272.7 | 104.5 |
| Georgia | 2,641.4 | 1,168.2 | 610.4 | 185.5 | 44.1 | 320.3 | 55.0 | 187.9 | 70.1 |
| Kentucky | 1,567.1 | 713.2 | 277.6 | 81.7 | 39.7 | 212.9 | 50.6 | 140.6 | 50.7 |
| Louisiana | 2,020.0 | 944.7 | 436.6 | 118.0 | 42.7 | 243.1 | 45.3 | 149.0 | 40.5 |
| Mississippi | 1,032.4 | 481.8 | 214.0 | 56.0 | 26.2 | 131.1 | 24.2 | 72.2 | 26.9 |
| North Carolina | 2,586.5 | 1,129.9 | 544.3 | 182.3 | 52.9 | 374.6 | 68.9 | 166.3 | 67.3 |
| South Carolina | 1,246.7 | 552.1 | 244.9 | 75.3 | 23.2 | 176.4 | 39.1 | 82.5 | 53.3 |
| Tennessee | 2,306.4 | 1,094.3 | 506.6 | 146.3 | 47.4 | 262.7 | 69.2 | 122.3 | 57.6 |
| Virginia | 2,524.7 | 1,118.5 | 586.9 | 192.5 | 41.6 | 290.2 | 69.4 | 154.8 | 70.8 |
| West Virginia | 954.3 | 495.7 | 185.0 | 46.3 | 18.2 | 112.2 | 31.4 | 37.1 | 28.4 |
| Southwest | 10,513.1 | 4,498.3 | 2,423.0 | 687.5 | 260.7 | 1,227.8 | 288.0 | 860.4 | 267.2 |
| Arizona | 1,365.8 | 599.9 | 363.1 | 110.7 | 32.4 | 141.4 | 22.6 | 52.0 | 43.6 |
| New Mexico | 544.8 | 263.9 | 113.0 | 37.2 | 14.3 | 58.9 | 16.3 | 19.5 | 21.8 |
| Oklahoma | 1,522.8 | 632.8 | 327.5 | 89.2 | 35.4 | 185.3 | 46.9 | 164.1 | 41.7 |
| Texas | 7,079.7 | 3,001.7 | 1,619.6 | 450.5 | 178.7 | 842.2 | 202.3 | 624.7 | 160.1 |
| Rocky Mountain | 3,132.5 | 1,320.4 | 686.2 | 269.1 | 87.0 | 323.5 | 93.2 | 261.4 | 91.8 |
| Colorado | 1,593.4 | 721.7 | 323.9 | 131.2 | 41.0 | 144.7 | 37.7 | 142.1 | 51.1 |
| Idaho | 389.7 | 139.1 | 91.9 | 33.0 | 12.2 | 50.9 | 14.5 | 39.0 | 9.0 |
| Montana | 385.9 | 145.8 | 90.2 | 33.1 | 12.8 | 42.0 | 19.1 | 32.3 | 10.6 |
| Utah | 584.4 | 239.3 | 141.1 | 57.7 | 15.1 | 64.7 | 12.8 | 38.4 | 15.3 |
| Wyoming | 179.0 | 74.5 | 39.0 | 14.1 | 5.9 | 21.1 | 9.2 | 9.5 | 5.7 |
| Far West | 20,689.3 | 8,369.6 | 5,191.4 | 1,903.5 | 628.4 | 1,996.8 | 609.7 | 1,440.1 | 549.6 |
| California | 15,943.4 | 6,547.9 | 4,117.1 | 1,400.3 | 492.8 | 1,480.4 | 456.8 | 1,027.4 | 420.7 |
| Nevada | 425.9 | 176.4 | 113.6 | 39.4 | 9.6 | 51.0 | 9.4 | 18.9 | 7.6 |
| Oregon | 1,396.4 | 519.9 | 314.4 | 142.4 | 39.4 | 161.1 | 53.8 | 136.7 | 28.8 |
| Washington | 2,158.4 | 823.1 | 450.0 | 241.3 | 72.5 | 223.7 | 70.9 | 225.3 | 51.6 |
| Alaska | 224.7 | 102.1 | 45.8 | 21.5 | 4.0 | 24.6 | 6.6 | 6.8 | 13.2 |
| Hawaii | 540.4 | 200.3 | 150.6 | 58.7 | 10.0 | 55.9 | 12.3 | 25.0 | 27.7 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Table 20. Personal health care expenditures, by type of expenditure, region, and State: Calendar year 1978.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in millions | |||||||||
| U.S. total | $165,968.5 | $75,375.0 | $35,801.0 | $11,776.6 | $4,103.5 | $15,419.8 | $4,154.8 | $15,092.6 | $4,245.1 |
| New England | 10,250.9 | 5,009.0 | 1,708.4 | 667.2 | 237.5 | 800.8 | 223.5 | 1,350.1 | 254.4 |
| Connecticut | 2,539.2 | 1,094.9 | 482.8 | 206.4 | 69.7 | 223.6 | 47.3 | 356.5 | 58.0 |
| Maine | 736.2 | 333.2 | 130.9 | 41.1 | 18.4 | 64.0 | 19.7 | 107.8 | 21.0 |
| Massachusetts | 5,331.7 | 2,839.2 | 795.9 | 311.8 | 111.6 | 366.9 | 114.0 | 670.3 | 121.9 |
| New Hampshire | 541.2 | 229.9 | 116.2 | 42.2 | 15.1 | 56.5 | 11.4 | 52.4 | 17.5 |
| Rhode Island | 790.7 | 375.4 | 138.4 | 43.7 | 13.8 | 59.2 | 20.2 | 114.7 | 25.2 |
| Vermont | 311.9 | 136.3 | 44.2 | 22.0 | 8.9 | 30.5 | 11.0 | 48.4 | 10.7 |
| Mideast | 33,960.9 | 16,673.2 | 6,434.3 | 2,260.8 | 996.7 | 2,722.6 | 645.2 | 3,279.1 | 949.1 |
| Delaware | 434.0 | 205.8 | 87.9 | 30.2 | 7.5 | 43.2 | 9.5 | 35.8 | 14.1 |
| District of Columbia | 1,102.3 | 740.7 | 187.2 | 29.2 | 15.4 | 58.3 | 12.2 | 18.8 | 40.5 |
| Maryland | 3,126.0 | 1,503.9 | 656.4 | 228.5 | 57.0 | 284.4 | 65.8 | 235.2 | 94.7 |
| New Jersey | 5,104.7 | 2,178.0 | 1,178.3 | 445.5 | 147.6 | 501.1 | 104.9 | 391.3 | 158.0 |
| New York | 15,210.4 | 7,429.7 | 2,720.5 | 981.8 | 556.8 | 1,098.2 | 243.6 | 1,784.5 | 395.3 |
| Pennsylvania | 8,983.5 | 4,615.1 | 1,604.0 | 545.6 | 212.4 | 737.3 | 209.2 | 813.4 | 246.4 |
| Great Lakes | 31,551.6 | 14,758.1 | 6,521.4 | 2,218.4 | 607.6 | 2,831.3 | 872.1 | 3,012.7 | 730.1 |
| Illinois | 9,101.2 | 4,644.2 | 1,652.3 | 588.4 | 192.2 | 702.6 | 265.5 | 838.6 | 217.4 |
| Indiana | 3,679.5 | 1,589.1 | 719.0 | 211.5 | 72.3 | 450.8 | 125.6 | 415.7 | 95.5 |
| Michigan | 7,345.3 | 3,417.6 | 1,595.9 | 621.0 | 125.4 | 681.4 | 162.1 | 586.7 | 155.1 |
| Ohio | 7,962.3 | 3,638.0 | 1,782.8 | 522.3 | 140.7 | 720.3 | 215.1 | 751.3 | 191.8 |
| Wisconsin | 3,463.3 | 1,469.2 | 771.5 | 275.1 | 76.9 | 276.1 | 103.7 | 420.5 | 70.4 |
| Plains | 12,793.5 | 5,830.7 | 2,502.4 | 857.0 | 286.6 | 1,065.3 | 381.6 | 1,619.7 | 250.3 |
| Iowa | 2,125.3 | 906.4 | 387.1 | 142.7 | 60.9 | 183.9 | 74.3 | 330.2 | 40.0 |
| Kansas | 1,716.0 | 801.6 | 317.7 | 89.4 | 36.2 | 148.3 | 73.1 | 215.7 | 34.1 |
| Minnesota | 2,961.4 | 1,309.0 | 505.4 | 230.6 | 53.9 | 231.1 | 72.4 | 499.7 | 59.3 |
| Missouri | 3,838.7 | 1,874.7 | 821.0 | 253.7 | 90.9 | 320.8 | 85.5 | 319.7 | 72.4 |
| Nebraska | 1,155.3 | 509.9 | 250.3 | 77.4 | 21.9 | 105.6 | 34.8 | 133.3 | 22.2 |
| North Dakota | 537.2 | 230.7 | 138.3 | 38.5 | 11.4 | 36.6 | 19.8 | 53.4 | 8.4 |
| South Dakota | 459.7 | 198.5 | 82.7 | 24.7 | 11.5 | 39.1 | 21.8 | 67.6 | 13.9 |
| Southeast | $32,635.8 | $14,659.3 | $7,550.1 | $2,075.2 | $693.4 | $3,721.1 | $765.5 | $2,320.8 | $850.6 |
| Alabama | 2,417.7 | 1,180.2 | 489.5 | 144.3 | 42.3 | 268.4 | 43.8 | 193.0 | 56.2 |
| Arkansas | 1,307.9 | 542.9 | 276.4 | 68.6 | 25.6 | 171.0 | 39.7 | 148.0 | 35.7 |
| Florida | 7,004.6 | 2,997.5 | 1,962.2 | 501.1 | 198.4 | 704.1 | 139.9 | 356.2 | 145.2 |
| Georgia | 3,434.2 | 1,507.9 | 804.7 | 233.2 | 60.4 | 390.5 | 68.7 | 270.7 | 98.1 |
| Kentucky | 2,002.1 | 881.9 | 402.9 | 108.2 | 45.9 | 253.4 | 59.2 | 191.7 | 58.9 |
| Louisiana | 2,647.9 | 1,228.5 | 598.5 | 151.7 | 61.9 | 290.5 | 53.6 | 207.7 | 55.5 |
| Mississippi | 1,377.5 | 633.9 | 284.1 | 71.8 | 35.1 | 160.2 | 29.1 | 124.3 | 39.0 |
| North Carolina | 3,322.2 | 1,443.8 | 709.1 | 225.4 | 60.4 | 458.5 | 82.8 | 249.1 | 93.0 |
| South Carolina | 1,603.6 | 693.4 | 324.8 | 98.6 | 29.7 | 218.3 | 48.8 | 127.0 | 62.9 |
| Tennessee | 3,015.6 | 1,439.8 | 677.5 | 181.2 | 59.7 | 319.4 | 88.1 | 178.7 | 71.3 |
| Virginia | 3,313.6 | 1,495.4 | 777.0 | 234.0 | 50.5 | 352.6 | 78.1 | 226.7 | 99.4 |
| West Virginia | 1,189.0 | 614.0 | 243.2 | 57.2 | 23.6 | 134.2 | 33.6 | 47.6 | 35.5 |
| Southwest | 13,697.2 | 5,912.5 | 3,211.8 | 886.7 | 327.7 | 1,495.7 | 357.6 | 1,137.1 | 368.0 |
| Arizona | 1,767.1 | 792.9 | 467.3 | 139.0 | 36.7 | 175.0 | 28.4 | 70.3 | 57.5 |
| New Mexico | 709.9 | 343.6 | 146.2 | 49.2 | 18.1 | 69.1 | 23.8 | 29.5 | 30.4 |
| Oklahoma | 1,941.7 | 827.1 | 411.1 | 112.6 | 42.1 | 221.7 | 58.5 | 214.2 | 54.4 |
| Texas | 9,278.4 | 3,949.0 | 2,187.2 | 586.0 | 230.8 | 1,029.8 | 246.9 | 823.0 | 225.7 |
| Rocky Mountain | 4,020.0 | 1,655.9 | 904.5 | 346.6 | 110.2 | 387.0 | 120.9 | 369.3 | 125.5 |
| Colorado | 2,004.8 | 865.9 | 427.6 | 166.8 | 55.8 | 171.8 | 50.8 | 194.3 | 71.8 |
| Idaho | 508.1 | 180.9 | 123.9 | 44.3 | 16.8 | 60.6 | 19.4 | 51.5 | 10.6 |
| Montana | 499.1 | 200.0 | 112.1 | 42.0 | 14.6 | 49.3 | 21.6 | 44.6 | 14.8 |
| Utah | 770.2 | 311.1 | 186.5 | 73.8 | 16.5 | 79.7 | 15.7 | 66.2 | 20.7 |
| Wyoming | 237.7 | 98.0 | 54.3 | 19.6 | 6.6 | 25.5 | 13.4 | 12.8 | 7.6 |
| Far West | 27,058.6 | 10,876.4 | 6,968.1 | 2,464.8 | 843.8 | 2,396.2 | 788.5 | 2,003.7 | 717.1 |
| California | 20,815.7 | 8,528.2 | 5,494.6 | 1,808.3 | 661.4 | 1,769.0 | 581.1 | 1,432.1 | 540.9 |
| Nevada | 611.2 | 250.1 | 167.0 | 52.9 | 15.2 | 66.8 | 15.4 | 32.1 | 11.8 |
| Oregon | 1,837.3 | 679.6 | 422.8 | 182.6 | 51.3 | 200.3 | 70.8 | 193.0 | 37.0 |
| Washington | 2,799.3 | 1,018.9 | 614.2 | 314.2 | 97.8 | 264.8 | 97.9 | 313.5 | 78.1 |
| Alaska | 297.2 | 139.3 | 62.4 | 31.7 | 5.1 | 31.0 | 6.2 | 4.5 | 17.0 |
| Hawaii | 697.8 | 260.3 | 207.1 | 75.2 | 12.9 | 64.3 | 17.1 | 28.5 | 32.4 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Table 21. Personal health care expenditures, by type of expenditure, region, and State: Calendar year 1980.
| Region and State | Total | Hospital care | Physicians' services | Dentists' services | Other professional services | Drugs and medical sundries | Eyeglasses and appliances | Nursing home care | Other health services |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount in millions | |||||||||
| U.S. total | $217,587.4 | $100,242.1 | $46,838.4 | $15,408.8 | $5,603.3 | $18,538.7 | $5,128.2 | $20,375.5 | $5,452.5 |
| New England | 13,077.6 | 6,368.9 | 2,160.1 | 856.3 | 350.6 | 946.4 | 276.9 | 1,795.7 | 322.8 |
| Connecticut | 3,251.5 | 1,380.6 | 611.5 | 268.5 | 106.9 | 264.3 | 59.6 | 486.1 | 74.0 |
| Maine | 979.3 | 462.2 | 164.4 | 50.2 | 24.7 | 76.0 | 24.2 | 150.3 | 27.4 |
| Massachusetts | 6,739.8 | 3,577.9 | 1,003.3 | 395.5 | 163.3 | 431.3 | 140.5 | 872.3 | 155.8 |
| New Hampshire | 701.7 | 308.5 | 146.0 | 55.8 | 21.6 | 68.7 | 14.4 | 65.2 | 21.6 |
| Rhode Island | 1,007.0 | 466.8 | 178.3 | 58.4 | 21.0 | 69.3 | 24.7 | 159.9 | 28.7 |
| Vermont | 398.2 | 172.9 | 56.7 | 27.9 | 13.1 | 36.8 | 13.5 | 62.0 | 15.3 |
| Mideast | 43,386.9 | 21,387.4 | 8,173.1 | 2,846.9 | 1,411.4 | 3,191.1 | 779.8 | 4,362.9 | 1,234.3 |
| Delaware | 542.7 | 259.8 | 114.5 | 37.8 | 9.6 | 50.8 | 11.5 | 39.7 | 19.0 |
| District of Columbia | 1,395.5 | 962.7 | 218.1 | 35.4 | 22.1 | 65.6 | 14.2 | 27.1 | 50.4 |
| Maryland | 4,040.7 | 1,961.9 | 845.4 | 290.8 | 81.7 | 337.2 | 80.6 | 317.3 | 125.9 |
| New Jersey | 6,461.9 | 2,734.5 | 1,475.1 | 568.4 | 204.3 | 590.4 | 128.3 | 569.9 | 191.1 |
| New York | 19,420.7 | 9,479.1 | 3,445.5 | 1,218.2 | 794.3 | 1,281.5 | 293.0 | 2,360.0 | 549.1 |
| Pennsylvania | 11,525.5 | 5,989.5 | 2,074.5 | 696.4 | 299.5 | 865.6 | 252.1 | 1,048.9 | 299.0 |
| Great Lakes | 40,703.2 | 19,358.5 | 8,356.5 | 2,918.7 | 766.9 | 3,336.3 | 1,029.1 | 4,019.8 | 917.5 |
| Illinois | 11,801.8 | 6,156.7 | 2,172.3 | 778.4 | 253.6 | 826.3 | 311.5 | 1,031.7 | 271.4 |
| Indiana | 4,720.0 | 2,101.5 | 901.8 | 271.4 | 90.9 | 531.1 | 147.4 | 558.7 | 117.2 |
| Michigan | 9,358.5 | 4,403.1 | 2,004.4 | 823.0 | 147.0 | 803.1 | 187.3 | 796.1 | 194.5 |
| Ohio | 10,326.7 | 4,805.4 | 2,262.9 | 667.1 | 177.4 | 845.9 | 255.8 | 1,065.1 | 247.1 |
| Wisconsin | 4,496.2 | 1,891.7 | 1,015.1 | 378.8 | 98.0 | 329.9 | 127.1 | 568.2 | 87.4 |
| Plains | 16,719.8 | 7,747.5 | 3,219.6 | 1,101.5 | 382.9 | 1,260.7 | 457.0 | 2,245.5 | 305.1 |
| Iowa | 2,718.7 | 1,174.5 | 521.8 | 183.9 | 75.4 | 215.5 | 85.5 | 415.0 | 47.3 |
| Kansas | 2,339.1 | 1,067.7 | 470.7 | 135.1 | 54.9 | 176.4 | 90.5 | 306.7 | 37.1 |
| Minnesota | 3,982.3 | 1,735.6 | 691.1 | 320.9 | 78.4 | 275.9 | 88.9 | 715.0 | 76.6 |
| Missouri | 4,903.1 | 2,507.8 | 945.5 | 291.8 | 117.7 | 379.4 | 102.9 | 469.1 | 88.9 |
| Nebraska | 1,489.3 | 674.2 | 321.3 | 96.4 | 28.7 | 124.6 | 40.8 | 175.6 | 27.7 |
| North Dakota | 676.4 | 313.3 | 159.9 | 41.5 | 12.8 | 43.2 | 23.0 | 73.1 | 9.7 |
| South Dakota | 610.9 | 274.4 | 109.4 | 31.9 | 15.0 | 45.9 | 25.3 | 91.0 | 17.9 |
| Southeast | $43,814.2 | $20,206.9 | $10,101.3 | $2,747.7 | $936.4 | $4,522.1 | $954.3 | $3,275.7 | $1,070.0 |
| Alabama | 3,151.2 | 1,587.4 | 640.5 | 181.2 | 53.3 | 320.2 | 52.6 | 243.2 | 72.7 |
| Arkansas | 1,757.4 | 744.5 | 365.5 | 90.0 | 38.1 | 205.7 | 47.5 | 217.6 | 48.6 |
| Florida | 9,670.8 | 4,302.1 | 2,673.3 | 668.6 | 268.2 | 896.7 | 187.1 | 476.2 | 198.5 |
| Georgia | 4,627.1 | 2,118.0 | 1,073.4 | 304.2 | 80.9 | 474.5 | 84.6 | 365.8 | 125.7 |
| Kentucky | 2,703.6 | 1,192.5 | 560.8 | 152.5 | 60.3 | 301.8 | 71.4 | 295.8 | 68.5 |
| Louisiana | 3,625.4 | 1,744.8 | 808.8 | 203.6 | 87.8 | 353.9 | 69.6 | 286.0 | 70.9 |
| Mississippi | 1,842.9 | 864.8 | 385.8 | 95.7 | 44.8 | 190.7 | 35.0 | 178.9 | 47.2 |
| North Carolina | 4,341.2 | 1,906.6 | 952.1 | 298.7 | 81.9 | 550.3 | 101.0 | 341.2 | 109.3 |
| South Carolina | 2,150.5 | 949.1 | 434.5 | 133.1 | 37.4 | 263.3 | 60.5 | 194.9 | 77.7 |
| Tennessee | 4,015.1 | 1,974.3 | 888.9 | 231.9 | 83.1 | 384.1 | 107.1 | 258.1 | 87.6 |
| Virginia | 4,355.0 | 1,995.9 | 1,000.1 | 313.1 | 66.5 | 421.1 | 96.6 | 337.8 | 123.9 |
| West Virginia | 1,574.1 | 826.8 | 317.7 | 75.1 | 33.9 | 159.8 | 41.1 | 80.4 | 39.4 |
| Southwest | 18,555.6 | 8,146.4 | 4,371.5 | 1,203.5 | 445.6 | 1,862.3 | 472.5 | 1,550.0 | 503.8 |
| Arizona | 2,417.1 | 1,086.6 | 640.2 | 191.3 | 48.9 | 223.1 | 38.1 | 112.4 | 76.5 |
| New Mexico | 943.9 | 455.7 | 192.2 | 68.6 | 26.4 | 85.5 | 30.2 | 44.9 | 40.4 |
| Oklahoma | 2,594.6 | 1,149.7 | 531.3 | 152.2 | 57.8 | 271.1 | 78.0 | 276.8 | 77.7 |
| Texas | 12,600.0 | 5,454.4 | 3,007.9 | 791.4 | 312.4 | 1,282.5 | 326.3 | 1,115.9 | 309.2 |
| Rocky Mountain | 5,430.6 | 2,340.2 | 1,206.2 | 465.7 | 155.7 | 477.5 | 154.2 | 467.8 | 163.2 |
| Colorado | 2,743.6 | 1,231.1 | 579.5 | 224.6 | 80.4 | 211.6 | 66.5 | 250.6 | 99.4 |
| Idaho | 659.9 | 240.7 | 158.7 | 59.7 | 24.0 | 74.0 | 23.7 | 65.9 | 13.3 |
| Montana | 630.9 | 265.0 | 139.7 | 53.5 | 19.5 | 58.3 | 25.6 | 51.7 | 17.5 |
| Utah | 1,056.8 | 454.1 | 252.8 | 100.1 | 23.3 | 100.7 | 19.9 | 81.7 | 24.2 |
| Wyoming | 339.3 | 149.4 | 75.5 | 27.7 | 8.5 | 32.8 | 18.6 | 17.9 | 8.9 |
| Far West | 35,899.6 | 14,686.3 | 9,250.1 | 3,268.6 | 1,154.0 | 2,942.4 | 1,004.4 | 2,658.0 | 935.8 |
| California | 27,450.6 | 11,407.2 | 7,265.2 | 2,379.3 | 916.4 | 2,161.7 | 743.3 | 1,868.3 | 709.2 |
| Nevada | 945.1 | 438.7 | 234.1 | 76.1 | 23.9 | 88.0 | 20.6 | 49.0 | 14.7 |
| Oregon | 2,407.3 | 915.5 | 557.4 | 240.0 | 67.7 | 246.4 | 87.1 | 248.2 | 45.1 |
| Washington | 3,803.5 | 1,402.8 | 829.3 | 430.6 | 120.7 | 331.6 | 124.9 | 451.4 | 112.2 |
| Alaska | 389.1 | 180.8 | 88.3 | 41.1 | 8.5 | 36.2 | 7.1 | 5.8 | 21.2 |
| Hawaii | 903.8 | 341.3 | 275.9 | 101.4 | 16.8 | 78.5 | 21.3 | 35.2 | 33.5 |
SOURCE: Health Care Financing Administration: Data from the Office of the Actuary.
Acknowledgments
This article was prepared in the Division of National Cost Estimates—George Kowalczyk, Director—under the general supervision of Daniel Waldo, Chief, Health Expenditures Branch. Helen Lazenby, Sue Donham, Frank Eppig, and Deborah Miller made important contributions to this article. The author is grateful to Mae Robinson and Charles Helbing for computer and program data assistance and to Carol Pearson for secretarial assistance.
Estimates published in Personal Health Care Expenditures by State, Volume II, by Barbara S. Cooper, Nancy L. Worthington, and Paula A. Piro form the basis for the 1966 and 1969 estimates presented in this report.
Footnotes
Reprint requests: Katharine R. Levit, Division of National Cost Estimates, Room L-l, EQ05, 6325 Security Boulevard, Baltimore, MD 21207.
Community hospitals, mainly acute care facilities, are all non-Federal, short-stay general and other hospitals. Excluded from this category are hospital units in institutions, Federal hospitals, psychiatric hospitals, and other long-term care hospitals. There were 5,801 community hospitals in operation in the United States in 1982 (American Hospital Association, 1983b).
Ratios were calculated from revenues and expenses for (1) nongovernment nonprofit hospitals and (2) for-profit and State and local government hospitals.
References
- American Hospital Association. Guide to the Health Care Field. 1976-83. Chicago: 1976-83a. [Google Scholar]
- American Hospital Association. Hospital Statistics. 1977-83. Chicago: 1977-83b. [Google Scholar]
- American Medical Association. Distribution of Physicians Hospitals and Hospital Beds in the US. 1969. Chicago: 1969. [Google Scholar]
- American Medical Association. Physician Characteristics and Distribution in the US. 1982. Chicago: 1982. [Google Scholar]
- American Nurses' Association. Facts About Nursing for 1976-77. Kansas City: 1978. [Google Scholar]
- American Nurses' Association. Inventory of Registered Nurses for 1977-78. Kansas City: 1979. [Google Scholar]
- Bloom B. Vital and Health Statistics. No. 53. Washington: U.S. Government Printing Office; Aug. 1981. Utilization patterns and financial characteristics of nursing homes in the United States 1977 National Nursing Home Survey. (13). DHHS Pub. No. (PHS) 81-1714. National Center for Health Statistics Public Health Service. [PubMed] [Google Scholar]
- Bureau of the Census Merchandise sales lines. Census of Retail Trade. U.S. Department of Commerce. Microfiche; 1972 and 1977. [Google Scholar]
- Bureau of the Census. Current Population Reports. No. 875. Washington: U.S. Government Printing Office; 1980. Estimates of the population of States by age. (P-25). U.S. Department of Commerce. [Google Scholar]
- Bureau of the Census. Health Services Subject Series. Washington: U.S. Government Printing Office; 1981. 1977 Census of Service Industries. U.S. Department of Commerce. [Google Scholar]
- Bureau of the Census. Current Population Reports. No. 951. Washington: U.S. Government Printing Office; 1984a. Estimates of the population of States by age. (P-25). U.S. Department of Commerce. [PubMed] [Google Scholar]
- Bureau of the Census. Current Population Reports. No. 957. Washington: U.S. Government Printing Office; 1984b. Estimates of the population of States: 1970 to 1983. (P-25). U.S. Department of Commerce. [Google Scholar]
- Bureau of Economic Analysis, U.S. Department of Commerce. State personal income 1929-1983. Data from the Regional Economic Information System. 1984a [Google Scholar]
- Bureau of Economic Analysis, U.S. Department of Commerce. Nursing home wages. 1984b. Unpublished data. [Google Scholar]
- Bureau of Labor Statistics. Area Wage Surveys Selected Metropolitan Areas. 1976. Bulletin 1900-81. 1977. Bulletin 1950-76. 1978. U.S. Department of Labor; Washington: 1976-78. [Google Scholar]
- Cooper BS, Worthington NL, Piro PA. Personal Health Care Expenditures by State Vol II Public and Private Funds 1966 and 1969. Washington: U.S. Government Printing Office; 1975. DHEW Pub. No. (SSA) 75-11906. Social Security Administration. [Google Scholar]
- Fisher C. Health Care Financing Review. No. 4. Vol. 1. Washington: U.S. Government Printing Office; Spring. 1980. Differences by age groups in health care spending. HCFA Pub. No. 03045. Office of Research Demonstrations and Statistics Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Garnick D. US Department of Commerce News. Bureau of Economic Analysis; Washington: Oct. 1982. Narrowing of regional differences in per capita personal income 1929-81. BEA Pub. No. 82-56. [Google Scholar]
- Gibson R, Levit K, Lazenby H, Waldo D. Health Care Financing Review. No. 2. Vol. 6. Washington: U.S. Government Printing Office; Winter. 1984. National health expenditures 1983. HCFA Pub. No. 03195. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Internal Revenue Service. 1976 Statistics of Income Business Income Tax Returns Sole Proprietorships Partnerships. Washington: U.S. Government Printing Office; 1979. U.S. Department of the Treasury. [Google Scholar]
- Lave J, Dobson H, Walton C. Health Care Financing Review. No. 1. Vol. 5. Washington: U.S. Government Printing Office; Fall. 1983. The potential use of Health Care Financing Administration data sets for health care services research. HCFA Pub. No. 03154. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Levit K. Health Care Financing Review. No. 2. Vol. 4. Washington: U.S. Government Printing Office; Dec. 1982. Personal health care expenditures by State selected years 1966-78. HCFA Pub. No. 03149. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- National Center for Education Statistics. Revenues and Expenditures for Public Elementary and Secondary Education. 1975-76. 1976-77. 1977-78. 1978-79. Washington: U.S. Government Printing Office; 1978, 1979, 1980, and 1982. NCES Pub. No. 78-102. NCES Pub. No. 79-108. NCES Pub. No. 80-100. NCES Pub. No. 82-100. U.S. Department of Education. [Google Scholar]
- Office of Technology Assessment. Variations in Hospital Length of Stay Their Relationship to Health Outcomes. Washington: U.S. Government Printing Office; Aug. 1983. Health Technology Case Study 24. U.S. Congress. [Google Scholar]
- Powell W, Stubbs J. Using Business Master File Data for Statistics of Income Purposes. Internal Revenue Service, U.S. Department of the Treasury; Unpublished paper. [Google Scholar]
- Sirrocco A. Vital and Health Statistics. No. 29. Washington: U.S. Government Printing Office; Dec. 1983. Nursing and related care homes. (14). DHHS Pub. No. (PHS) 84-1824. National Center for Health Statistics, Public Health Service. [PubMed] [Google Scholar]
- Waldo D, Lazenby H. Health Care Financing Review. No. 1. Vol. 6. Washington: U.S. Government Printing Office; Fall. 1984. Demographic characteristics and health care use and expenditures by the aged in the United States 1977-1984. HCFA Pub. No. 03176. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Wennberg J. Health Affairs. Millwood, Va.: Project HOPE; Summer. 1984. Dealing with medical practice variations a proposal for action. [DOI] [PubMed] [Google Scholar]