Abstract
In this article, we examined the concentration of Medicare expenditures among the aged for 1969, 1975, and 1982 to determine if expenditures have become more concentrated among a few heavy users of service over time. Despite an increase in reimbursements for the aged from $6.0 billion in 1969 to $41.8 billion in 1982, the distribution of those expenses remained remarkably stable, with a slight lessening in the concentration of reimbursements in 1982. Patterns were similar for both Part A (hospital insurance) and Part B (supplementary medical insurance) services. The concentration of expenditures was much greater among survivors than among people who died in both 1975 and 1982, with little change in the distribution of expenditures within either group.
Introduction
Data from the Medicare program have long shown that expenditures, and particularly hospital expenses, tend to be heavily concentrated among a small number of people who are heavy users of services. The question often arises as to whether Medicare expenditures for the aged have become more concentrated among a few heavy users of services over time. Shifts in the concentration of Medicare expenditures over time are of interest for several reasons. A trend toward a greater concentration of expenditures would reveal that the highest cost individuals are an important source of increased program expenses. This would suggest that cost-containment efforts should focus on the care given to these individuals. Trends in the distribution of expenditures among enrollees may also provide insights into the impact of new, high-cost technologies such as coronary artery bypass surgery, computerized axial tomography (CAT) scans, maintenance dialysis for end-stage renal disease, and hip replacement. The use of more sophisticated techniques for prolonging the lives of extremely ill patients (often referred to as “heroic” measures) would likely produce more high-cost individuals and could affect the distribution of expenditures. The increase in Medicare's End-Stage Renal Disease (ESRD) population has produced some new high-cost enrollees, although the number of aged ESRD enrollees is still not great.1 Cost sharing also becomes a crucial issue for high-cost individuals through deductible and coinsurance obligations. It may be desirable to restructure Medicare cost-sharing requirements to lessen the burden for certain kinds of high-cost individuals. For example, Gornick, Beebe, and Prihoda (1983) estimated that a $161 surcharge per enrollee in 1984 would have permitted a cap of $400 on beneficiary liability for deductible and coinsurance expenses.
Studies of the aged population have illustrated the concentration of expenditures among a small percent of users. Gornick, Beebe, and Prihoda (1983) determined that, in 1980, 14.1 percent of aged Medicare enrollees incurred $2,000 or more in reimbursed expenses, and they accounted for 83.7 percent of total expenditures. A large portion of Medicare expenditures are attributable to patients who are terminally ill. Lubitz and Prihoda (1984) investigated Medicare expenses incurred in the last 12 months of life for beneficiaries who died in 1978. They found that decedents comprised 5.9 percent of the Medicare aged population, but accounted for 27.9 percent of expenditures. They also found that the ratio of per capita reimbursements of decedents to survivors increased only slightly from 1967 to 1979 (4.9 percent to 5.1 percent). Birnbaum (1978) determined that, in 1974, 2.9 percent of the aged noninstitutionalized population (including those not entitled to Medicare) incurred 34 percent of total health care expenses for the noninstitutionalized aged.
Other studies not limited to the aged population also showed a concentration of expenses among a small percent of users. The Congressional Budget Office (1982) studied the health care expenses of families enrolled in the Federal Employees' Health Benefit Plan (FEHBP) through Blue Cross and Blue Shield, and found that in 1978 the costliest 5 percent of families accounted for 49 percent of medical expenses. Schroeder, Showstack, and Roberts (1979) studied 17 acute care hospitals in the San Francisco Bay area and found that the percent of patients whose yearly hospital charges exceeded $4,000 in 1976 ranged from 4 percent to 24 percent, and that these patients accounted for 20 percent to 68 percent of total yearly charges for these hospitals. Zook and Moore (1980) studied patients in six hospitals in 1976 and found that, on average, 13 percent of patients accounted for one-half of inpatient charges. Based on these data, they estimated that as few as 1.3 percent of the general population consumes more than one-half of the hospital resources used in any given year. Zook and Moore (1980) also found that persons 65 years of age or over were disproportionately represented among high-cost users.
Some studies not limited to the Medicare population have shown increases in the concentration of health expenditures over time. Andersen, Lion, and Anderson (1976), using data from interviews taken from probability samples of the noninstitutionalized population of the United States, found that, in 1963, the top 1 percent of users (in terms of expenditures) accounted for 17 percent of the total amount spent for nonfree health services. By 1970, they accounted for 23 percent of expenditures for nonfree care, excluding Medicare (24 percent including Medicare). The proportion of total expenditures accounted for by the top 5 and 10 percent of users also increased, but less dramatically. The Congressional Budget Office Report (1982) noted that the percent of expenses accounted for by the top 1 percent of families enrolled in Blue Cross and Blue Shield's FEHBP program increased from 20 percent to 22 percent between 1974 and 1978.
This article examines trends in the distribution of Medicare expenditures by comparing the concentration of expenditures among aged Medicare enrollees in 1969, 1975, and 1982. Trends are examined separately for Part A (hospital insurance), and Part B (supplementary medical insurance) of Medicare. Trends are also examined separately for decedents and survivors. The distribution of health care charges for aged persons in 1980 is also compared with that of persons under age 65, as reported by the National Medical Care Utilization and Expenditure Survey.
In analyzing the distribution of expenditures, some of the studies cited previously have been based on the entire population at risk, and others have based the analysis on the population of users of services. In studying trends in the concentration of expenditures, the results can differ depending on which population is studied. All our analyses are based on the entire population at risk rather than only the population of users.
Data and methods
The major focus of this article is on changes in the percent of reimbursements attributable to various percentiles of all aged enrollees. The data were derived from the Medicare Person Summary File, which consists of Medicare claims submitted for a 5-percent sample of the enrolled aged population. The records are organized on a person basis so that all covered services received by each sample individual are put into a single record. This analysis covers the years 1969, 1975, and 1982 so that long-term changes in expenditure patterns can be identified. For 1969, only published data were available (Office of Research and Statistics, 1975) showing numbers of persons served and total dollars associated with broad reimbursement categories (e.g., less than $50, $50-$99, etc.). The published data were used to compute a limited number of cumulative percentages of beneficiaries and reimbursement amounts. For 1975 and 1982, individual claim files were available, and consequently cumulative dollars could be calculated for a number of selected beneficiary percentile levels. The same cumulative percentages of beneficiaries derived from the 1969 data were used for 1975 and 1982 to facilitate comparisons of these years. In addition, reimbursements were computed for the top 10, 5, 1, and .1 percent of beneficiaries in 1975 and 1982. Separate computations were also prepared for survivors and decedents in 1975 and 1982.
Changes in the distribution of Part B reimbursements are influenced by the rise in the annual Part B deductible over time. The Part B deductible was $50 in 1969 and was raised to $60 in 1973, where it remained until 1982 when it rose to $75. The increase in the price of Part B services was more rapid than the increase in the Part B deductible; therefore, more people became eligible for Part B reimbursement over time because fewer units of service were required to exceed the deductible. This phenomenon can, to some extent, affect the entire distribution of Part B and, therefore, total expenditures because of an increasing number of low-service users with reimbursements barely exceeding the deductible. Part A expenses are not affected by this phenomenon because the deductible for hospital services changes annually in accordance with the average daily cost of hospital care. Thus, unlike Part B, there is no artificial shift in the concentration of Part A reimbursements caused by an increasing number of beneficiaries exceeding a constant deductible.
To control the “deductible effect,” all Part B reimbursements for 1975 and 1982 were adjusted to account for the lag in the change of the Part B deductible, after which the cumulative distributions were recomputed. Specifically, individual Part B reimbursements for 1975 and 1982 were reduced to simulate what they would have been if the Part B deductible had risen with inflation. The adjustment was made using the yearly net increase in reasonable charges for physicians' services, per enrollee, because of price changes since 1969 (Board of Trustees, Federal Supplementary Medical Insurance Trust Fund, 1983; Kunkel, 1984). Price increases for physicians' services were used because they represent the bulk of Part B services; net increases in reasonable charges were examined, rather than increases in submitted charges, because the deductible is applied to reasonable charges.
If the 1969 Part B deductible had increased at the same rate as the price of Part B services, the deductible would have risen to $65.09 in 1975. The actual deductible for that year was $60. Therefore, all individual Part B reimbursements for 1975 were reduced by $5.09 to simulate what Part B reimbursements would have been under a $65.09 deductible. The distribution of expenditures was then recomputed, using the adjusted reimbursement amounts. Similarly, it was estimated that the 1982 Part B deductible would have been $120.15 if the deductible had risen with inflation in previous years. The actual deductible for that year was $75. Therefore, all individual Part B reimbursements for 1982 were reduced by $45.15. The distribution of expenditures for 1982 was then recomputed, using the adjusted reimbursement amounts.
In this article we also compare the distribution of charges for health services received by persons 65 years of age or over with that of persons under 65 years of age using data reported by Garfinkel, Riley, and Iannacchione (1985). This comparison uses interview data obtained through the National Medical Care Utilization and Expenditure Survey. This is a survey of a national probability sample of the noninstitutionalized United States population, conducted in 1980, which recorded health care charge and utilization data. The charge data were obtained directly from respondents. If the respondent did not know the charge for a given service, a charge per service was imputed from data provided by another respondent matched on demographic characteristics. Charge data for Medicaid-eligible respondents were imputed in every case based on their reported utilization. As a result, subsequent comparisons between expenditure distributions of Medicaid and non-Medicaid eligibles reflect differences in the distribution of utilization between these groups rather than differences in the distribution of charges, per se.
Results
The degree of concentration of Medicare reimbursements among heavy users of services exhibited considerable stability over time (Table 1). The table, which does not include the adjustment for Part B expenses, indicates the percent of reimbursements attributable to a given percent of the highest cost beneficiaries, for all services and for Parts A and B services separately. (The choice of percentiles other than those ending in .5 or .0 was dictated by those calculated from the published reimbursement data available in 1969. No data tape was available for that year to enable computation of percent of reimbursement for other enrollee percentiles.) It is evident that the distributions of expenditures for 1969 and 1975 are similar, particularly for Part A and for total dollars. For example, the top 4 percent of enrollees accounted for 50.1 percent of all reimbursements in both 1969 and 1975. The top 2 percent accounted for 33.0 percent of all reimbursements in 1969 and 33.5 percent in 1975. In 1982, reimbursements exhibited a slightly smaller concentration at all levels when compared with 1969 and 1975. For example, the costliest 4 percent of enrollees in 1982 accounted for 47.9 percent of total expenses, compared to 50.1 percent in the other years. This stability is quite remarkable, given the fact that overall program expenses for the aged increased from $6.0 billion in 1969 to $12.7 billion in 1975 and to $41.8 billion in 1982.
Table 1. Percent of Medicare reimbursements attributable to the highest cost groups of aged enrollees: 1969, 1975, and 1982.
| Enrollee upper percentile | 1969 | 1975 | 1982 |
|---|---|---|---|
|
| |||
| Percent of reimbursements | |||
| Total | |||
| 11.0 | 81.4 | 80.3 | 77.1 |
| 8.8 | 74.4 | 73.6 | 70.6 |
| 5.8 | 61.4 | 61.1 | 58.4 |
| 5.0 | (1) | 56.5 | 54.0 |
| 4.0 | 50.1 | 50.1 | 47.9 |
| 2.8 | 40.6 | 40.9 | 39.1 |
| 2.0 | 33.0 | 33.5 | 31.9 |
| 1.0 | (1) | 21.4 | 20.3 |
| 0.5 | (1) | 13.3 | 12.5 |
| Part A | |||
| 8.5 | 80.4 | 79.8 | 77.7 |
| 6.6 | 72.1 | 71.7 | 69.7 |
| 5.0 | (1) | 63.1 | 61.3 |
| 4.1 | 57.2 | 57.2 | 55.6 |
| 2.7 | 45.3 | 45.6 | 44.3 |
| 1.8 | 35.6 | 36.2 | 35.1 |
| 1.3 | 28.0 | 28.6 | 27.8 |
| 1.0 | (1) | 24.5 | 23.7 |
| 0.5 | (1) | 15.3 | 14.7 |
| Part B | |||
| 12.6 | 77.0 | 73.3 | 69.6 |
| 8.8 | 65.8 | 62.7 | 59.0 |
| 6.3 | 55.6 | 53.3 | 50.0 |
| 5.0 | (1) | 47.0 | 44.1 |
| 4.6 | 46.4 | 44.7 | 41.9 |
| 2.2 | 29.0 | 28.6 | 27.1 |
| 2.0 | (1) | 27.3 | 25.8 |
| 1.1 | 18.2 | 18.4 | 17.5 |
| 1.0 | (1) | 17.5 | 16.7 |
| 0.5 | (1) | 11.0 | 10.7 |
Not available for 1969.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
The decrease in concentration of expenses in 1982 was considerably less for Part A than for Part B. For example, for Part A, the top 4.1 percent of beneficiaries accounted for 55.6 percent of expenditures in 1982 compared with 57.2 percent for the other 2 years. For Part B, the top 4.6 percent of enrollees accounted for 41.9 percent of expenses in 1982, 44.7 percent in 1975, and 46.4 percent in 1969.
The stability in the concentration of Part A reimbursements from 1969 to 1982 may be an artifact of the manner in which inpatient hospital expenses were reimbursed before the implementation of prospective payment in 1983. Under cost reimbursement, hospitals normally received an interim payment for each bill based on a percent of charges or on a standard per diem amount. This interim payment was recorded in the Medicare Person Summary File, which was used for this study. For expensive hospitals stays (e.g. for a coronary artery bypass operation) an interim payment based on a per diem amount would normally underestimate the amount of hospital resources expended because the cost of additional ancillary services used would be spread across all Medicare hospital days. Because the number of hospitals receiving per diem-based interim payments increased over time (Goldstein, 1985), there may have been an increase in the extent to which the cost of expensive hospital stays was not reflected in reimbursement figures based on billing data. This in turn may have caused Part A expenditures to appear to have become less concentrated among a small percent of enrollees over time.
We examined the effect of the change in the interim payment method by computing cumulative enrollee and dollar levels for Medicare-covered Part A charges in 1975 and 1981 using the Continuous Medicare History Sample (CMHS). The CMHS is a longitudinal research file containing data on a 5-percent sample of the Medicare population. Data from 1981 were used because 1982 data are not available in the CMHS; in addition, a 1-percent subsample was used in computing the distribution of 1975 Part A charges because of data availability limitations. The similarity in the distribution of Part A charges in 1975 and 1982 confirms the stability in the concentration of Part A expenses over time (Table 2). The charge data show a slight increase in concentration over time in the 5.0 and 1.0 enrollee percentiles, in contrast to the slight lessening shown in Part A reimbursement data in Table 1. Part A reimbursements exhibited a similar, though slightly heavier concentration, than did Part A charges in 1975.
Table 2. Percent of covered Part A charges attributable to the highest cost groups of Medicare aged enrollees: 1975 and 1981.
Based on a 1-percent sample.
Based on a 5-percent sample.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
The cumulative distributions of Part B and total expenditures were also computed after applying the inflation adjustment procedure for the deductible described in the “Data and methods” section. The adjustment makes only a small difference in the concentration of total expenditures (Table 3). The 1975 and 1982 distributions of Part B and total expenditures become slightly more concentrated after the adjustment, but the same basic patterns remain. The distributions for the 3 study years remain similar, with a slightly less heavy concentration of expenditures in 1982 than in the other 2 years. For example, the costliest 4.6 percent of beneficiaries used 46.4 percent, 45.3 percent, and 44.0 percent of Part B expenditures in 1969, 1975, and 1982 respectively.
Table 3. Percent of Medicare reimbursement attributable to the highest cost groups of aged enrollees, with Part B deductible adjusted for inflation: 1969, 1975, and 1982.
| Enrollee upper percentile | 1969 | 1975 | 1982 |
|---|---|---|---|
|
| |||
| Percent of reimbursements | |||
| Total | |||
| 11.0 | 81.4 | 80.6 | 78.1 |
| 8.8 | 74.4 | 73.9 | 71.5 |
| 5.8 | 61.4 | 61.3 | 59.3 |
| 5.0 | (1) | 56.7 | 54.8 |
| 4.0 | 50.1 | 50.3 | 48.6 |
| 2.8 | 40.6 | 41.1 | 39.7 |
| 2.0 | 33.0 | 33.6 | 32.4 |
| 1.0 | (1) | 21.5 | 20.7 |
| 0.5 | (1) | 13.3 | 12.7 |
| Part B | |||
| 12.6 | 77.0 | 74.2 | 72.5 |
| 8.8 | 65.8 | 63.5 | 61.7 |
| 6.3 | 55.6 | 54.0 | 52.4 |
| 5.0 | (1) | 47.6 | 46.2 |
| 4.6 | 46.4 | 45.3 | 44.0 |
| 2.2 | 29.0 | 29.0 | 28.5 |
| 2.0 | (1) | 27.7 | 27.2 |
| 1.1 | 18.2 | 18.6 | 18.5 |
| 1.0 | (1) | 17.7 | 17.6 |
| 0.5 | (1) | 11.2 | 11.3 |
Not available for 1969.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
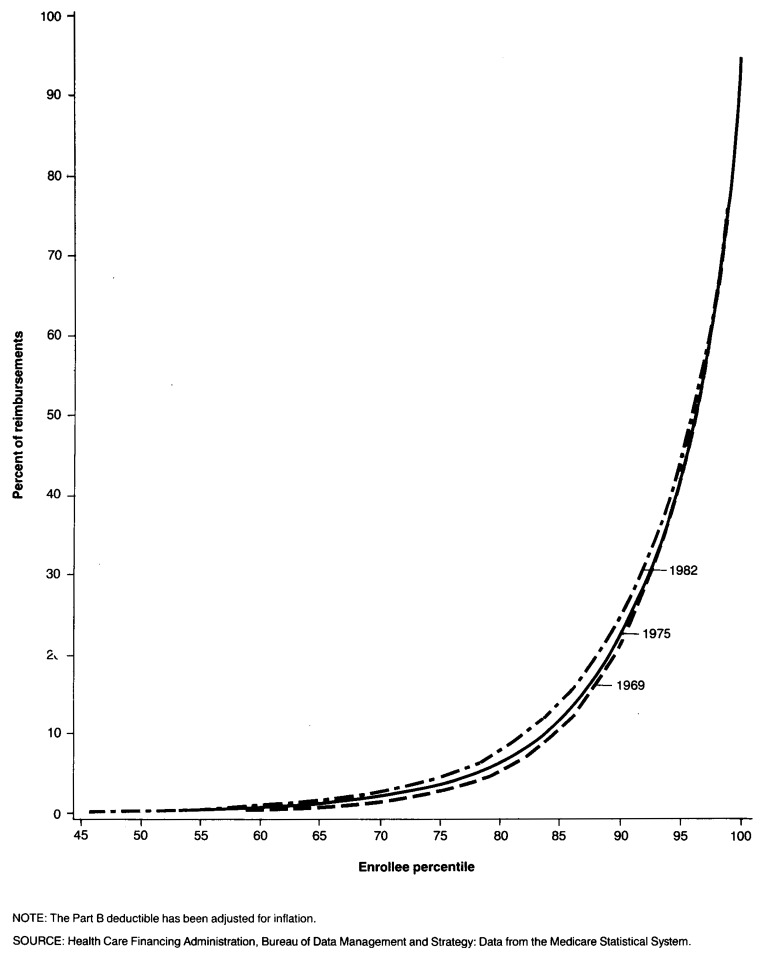
The similarity of the adjusted expenditure distributions among the 3 study years is illustrated through Lorenz curves (Figure 1) which are graphs of the cumulative percent of enrollees versus the cumulative percent of reimbursements associated with them. The further the curve deviates from a 45 degree line the more skewed is the distribution of reimbursements, and hence the more heavily concentrated are the expenditures among a relatively few beneficiaries. As seen from the figure, the distribution of adjusted total reimbursements for all 3 years are heavily skewed and are similar to each other, particularly among the upper percentiles of enrollees.
Figure 1. Cumulative percent of reimbursements attributable to various percentiles of aged Medicare enrollees: 1969, 1975, and 1982.
One aspect of the distribution of Medicare expenditures is the percent of enrollees with some Medicare reimbursements in a given year. The percent incurring reimbursements has increased substantially over time (Table 4). Only 40.3 percent of beneficiaries incurred reimbursements under Part A and/or Part B in 1969, but 61.1 percent did so in 1982. Although much of this increase is because of the slowness of the rise in the Part B deductible, relative to inflation, the adjusted figures on total reimbursements in Table 4 indicate that there would have been a substantial increase in the number of beneficiaries receiving reimbursements even without the deductible effect (from 40.3 percent in 1969 to 53.5 percent in 1982). The largest increase was in Part B services, where the adjusted percent of enrollees incurring reimbursements increased from 40.4 percent in 1969 to 54.0 percent in 1982.2 For Part A there was also a substantial increase from 19.7 percent to 23.8 percent, reflecting the increase in the number of enrollees who were hospitalized.
Table 4. Percent of Medicare aged enrollees with some reimbursement, by type of service: 1969, 1975, and 1982.
| Type of service | 1969 | 1975 | 1982 |
|---|---|---|---|
|
| |||
| Percent incurring reimbursement | |||
| Actual | |||
| Part A and/or Part B | 40.3 | 49.9 | 61.1 |
| Part A | 19.7 | 20.9 | 23.8 |
| Part B | 40.4 | 50.6 | 62.2 |
| Adjusted1 | |||
| Part A and/or Part B | 40.3 | 48.7 | 53.5 |
| Part B | 40.4 | 49.3 | 54.0 |
Part B deductible adjusted for inflation.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
A different perspective on expenditure distributions is obtained by comparing the rate of increase in reimbursements for the costliest beneficiaries to the rate of increase for the aged Medicare population in general (Table 5). As indicated in the table, the per capita reimbursements of the heavy users increased at approximately the same average annual rate as the per capita reimbursements for the entire aged population between 1969 and 1975, with a slightly greater increase in Part A expenses among the heaviest users. Between 1975 and 1982, the costliest beneficiaries exhibited similar but slightly smaller increases under both Part A and Part B relative to all beneficiaries. (Part A reimbursements for the top 1.8 percent of beneficiaries increased an average of 15.1 percent annually compared with a 15.6-percent annual average increase for all Part A enrollees; Part B reimbursement for the top 2.2 percent increased an average of 16.3 percent annually versus a 16.7-percent average annual increase for all Part B enrollees.) Consequently there is no evidence of a general shift toward a heavier concentration of expenses among a few beneficiaries. The data in Tables 1 through 5 suggest that the increase in expenses of low and moderate users of service has kept pace with those of the heaviest users.
Table 5. Per capita reimbursements for highest cost Medicare aged beneficiaries: 1969, 1975, and 1982.
| Enrollee percentile | Per capita reimbursements | Average annual percent increase | |||
|---|---|---|---|---|---|
|
|
|
||||
| 1969 | 1975 | 1982 | 1969-75 | 1975-82 | |
| Total | |||||
| All aged | $280 | $524 | $1,469 | 11.0 | 15.9 |
| Top 4.0 | 3,521 | 6,602 | 17,897 | 11.0 | 15.3 |
| Top 2.0 | 4,618 | 8,802 | 23,818 | 11.3 | 15.3 |
| Part A | |||||
| All aged | 201 | 387 | 1,067 | 11.5 | 15.6 |
| Top 4.1 | 2,797 | 5,377 | 14,393 | 11.5 | 15.1 |
| Top 1.8 | 3,900 | 7,609 | 20,331 | 11.8 | 15.1 |
| Part B | |||||
| All aged | 84 | 147 | 433 | 9.8 | 16.7 |
| Top 4.6 | 856 | 1,460 | 4,167 | 9.3 | 16.2 |
| Top 2.2 | 1,134 | 1,978 | 5,702 | 9.7 | 16.3 |
NOTE: Part B deductible is adjusted for inflation.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
These findings differ somewhat from those of the Congressional Budget Office (CBO) Report, which contained data on family expenses for Federal employees covered by Blue Cross and Blue Shield in 1974 and 1978. The CBO specifically looked at expenses that exceeded certain catastrophic thresholds. The CBO report noted that expenditures for high-cost illness rose faster than expenditures for all covered services, although the difference was relatively small. CBO also found that the disproportionate growth in expenditures for high-cost illness did not contribute much to the overall increase in medical expenses. We conducted an analysis similar to that performed by CBO for Medicare reimbursements in 1969, 1975, and 1982, using several catastrophic thresholds that ranged (in 1969 dollars) from a low of $500 for Part B expenses to a high of $3,000 for total Medicare reimbursements. The threshold levels were adjusted to account for changes in Medicare reimbursement per enrollee over time. We found that for Part A reimbursements and total reimbursements, the percent of beneficiaries exceeding catastrophic thresholds, and the percent of reimbursements attributable to them, declined slightly from 1969 to 1975 and from 1975 to 1982. For Part B expenses, the percent of beneficiaries exceeding catastrophic thresholds, and the percent of reimbursements attributable to them, declined slightly from 1969 to 1975, but rose slightly from 1975 to 1982. The difference in findings may be due to the fact that our data pertain to the aged only, whereas the CBO report includes families enrolled in the FEHBP, most of whose members are under 65 years of age. Another reason may be that the CBO report looked at a different and shorter time period than we did.
It is known that a large portion of expenditures under Medicare are associated with persons who are in their last year of life (Lubitz and Prihoda, 1984). Distributions of expenditures for 1975 and 1982 were computed separately for enrollees who died in those years and for those who survived (Table 6). Unlike the Lubitz and Prihoda study, which examined expenses in the last 12 months of life, data on decedents in this present study were limited to expenses in the calendar year in which the enrollee died. We found that expenditures were much more concentrated among survivors than decedents because a relatively high proportion of decendents use a large amount of services. In 1982, the top 5 percent of survivors accounted for 56.6 percent of total reimbursements, whereas among decedents the top 5 percent accounted for only 27.3 percent of reimbursements. There was some lessening in the concentration of Part A and Part B expenditures between 1975 and 1982 for both survivors and decedents, although the reduction in concentration tended to be proportionately greater among decedents, particularly for Part B services. For example, the costliest 5 percent of survivors under Part B accounted for 48.6 percent of total expenditures in 1975 and 47.2 percent in 1982, whereas the costliest 5 percent of decedents accounted for 32.4 percent of expenditures in 1975 versus only 29.9 percent in 1982.
Table 6. Percent of Medicare reimbursements attributable to the highest cost groups of aged enrollees, by survival status: 1975 and 1982.
| Enrollee upper percentile | Survivors | Decedents | ||
|---|---|---|---|---|
|
|
|
|||
| 1975 | 1982 | 1975 | 1982 | |
|
| ||||
| Percent of reimbursements | ||||
| Total | ||||
| 10.0 | 79.5 | 76.7 | 45.8 | 42.9 |
| 5.0 | 58.8 | 56.6 | 29.4 | 27.3 |
| 2.0 | 35.3 | 34.0 | 15.7 | 14.4 |
| 1.0 | 22.8 | 21.9 | 9.5 | 8.7 |
| 0.5 | 14.2 | 13.6 | 5.6 | 5.3 |
| Part A | ||||
| 10.0 | 87.8 | 85.3 | 47.1 | 44.3 |
| 5.0 | 66.4 | 64.2 | 30.5 | 28.3 |
| 2.0 | 40.7 | 39.4 | 16.3 | 15.0 |
| 1.0 | 26.5 | 25.6 | 9.9 | 9.2 |
| 0.5 | 16.7 | 16.1 | 5.9 | 5.6 |
| Part B | ||||
| 10.0 | 68.2 | 66.6 | 49.3 | 45.5 |
| 5.0 | 48.6 | 47.2 | 32.4 | 29.9 |
| 2.0 | 28.3 | 27.9 | 17.9 | 16.6 |
| 1.0 | 18.2 | 18.1 | 11.2 | 10.5 |
| 0.5 | 11.5 | 11.7 | 7.1 | 6.5 |
NOTE: Part B deductible is adjusted for inflation.
SOURCE: Health Care Financing Administration, Bureau of Data Management and Strategy: Data from the Medicare Statistical System.
Because the cost of treating illness in the last year of life accounts for such a large portion of program expenditures (Lubitz and Prihoda, 1984), it is important to know whether expenses attributable to decedents are rising faster than those of survivors. Table 7 shows the ratio of per capita reimbursements for decedents to those for survivors for the years 1967, 1975, 1979, and 1982. The ratio dropped slightly (from 4.86 to 4.75) between 1967 and 1975, then rose slightly after that (5.05 in 1982). Generally, the ratio of decedent to survivor per capita reimbursements remained quite stable for Part A, Part B, and total reimbursements. Table 8 compares the average annual increase in per capita reimbursements attributable to decedents and survivors from 1967 to 1982, using two sources of published Medicare data (Helbing, 1983; Piro and Lutins, 1973). As indicated in the table, per capita reimbursements for survivors rose slightly more than those for decedents from 1967 to 1975 (12.7 versus 12.4 percent annually). From 1975 to 1979 per capita reimbursements for decedents increased at a somewhat faster rate (16.8 percent versus 14.9 percent annually), but increased at approximately the same rate from 1979 to 1982. The findings summarized in Tables 7 and 8 suggest that per capita expenses incurred by decedents and survivors have increased at similar rates, and the slightly more rapid rise in expenditures for decedents in some recent years has not had a major impact on the amount or distribution of program reimbursements. In fact, the average annual percent increases in per capita reimbursements between 1967 and 1982 for decedents and survivors were 14.5 percent and 14.3 percent, respectively. Any use of heroic measures to extend life does not appear to have resulted in extraordinary increases in the relative cost of treating dying persons as compared with persons who did not die.
Table 7. Ratio of Medicare aged per capita reimbursements, decedents to survivors: Selected years 1967-82.
| Year | Total | Part A | Part B |
|---|---|---|---|
|
| |||
| Ratio of per capita reimbursements | |||
| 1967 | 4.86 | 5.78 | 2.97 |
| 1975 | 4.75 | 5.59 | 2.69 |
| 1979 | 5.07 | 6.04 | 2.84 |
| 1982 | 5.05 | 6.03 | 2.93 |
NOTE: Data for decedents are based on the calendar year in which the enrollee died.
SOURCE: Health Care Financing Administration; (Piro and Lutins, 1973; Helbing, 1983). Data for 1975 and 1982 are from the Medicare Statistical System data for the present study.
Table 8. Average annual percent increase in per capita reimbursements for Medicare aged decedents and survivors: Selected years 1967-82.
| Year | Total | Part A | Part B | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Decedents | Survivors | Decedents | Survivors | Decedents | Survivors | |
|
| ||||||
| Average annual percent increase | ||||||
| 1967-75 | 12.4 | 12.7 | 13.0 | 13.5 | 10.6 | 12.0 |
| 1975-79 | 16.8 | 14.9 | 16.3 | 14.0 | 19.7 | 18.1 |
| 1979-82 | 17.4 | 17.6 | 17.4 | 17.4 | 17.4 | 16.2 |
NOTE: Data for decedents are based on the calendar year in which the enrollee died.
SOURCE: Health Care Financing Administration; (Piro and Lutins, 1973; Helbing, 1983). Data for 1975 and 1982 are from the Medicare Statistical System data for the present study.
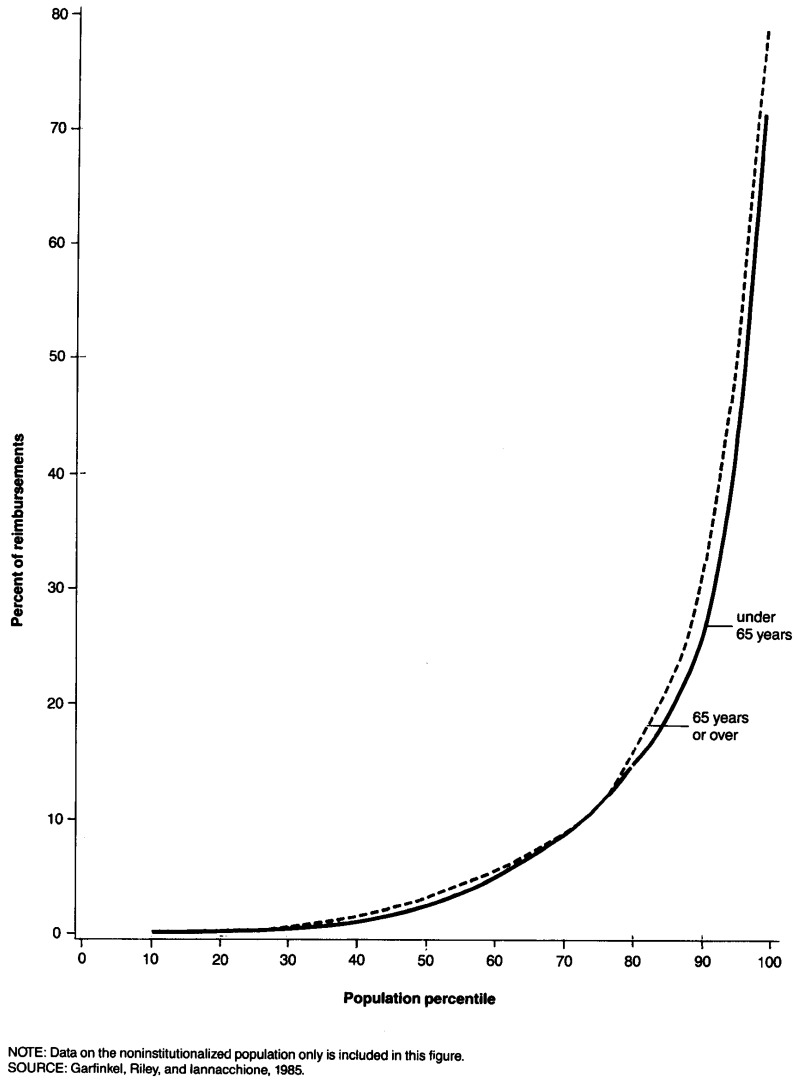
Health care expenditures of the noninstitutionalized aged population can be compared to those of other noninstitutionalized persons through the National Medical Care Utilization and Expenditure Survey (Garfinkel, Riley, and Iannacchione, 1985). The survey contains information reported by respondents on annual charges for all health care services. Table 9 contains total charges for health care services for selected percentiles of persons 65 years of age or over and persons under 65 years of age. The data suggest that the population under 65 may have a slightly heavier concentration of charges among high-cost users than the population 65 years of age or over. For example, the top 5.0 percent of the aged accounted for 50.6 percent of charges, whereas the top 5.0 percent of the population under 65 years of age accounted for 57.9 percent of charges. Similarly, 1.0 percent of the aged group accounted for 21.2 percent of total charges, whereas 1.0 percent of the population under 65 years of age accounted for 28.5 percent of charges. These differences are not statistically significant, however, and the similarity of the distributions of charges for the groups over and under 65 years of age is shown graphically in Figure 2. Although the distribution of charges is similar between the population groups, the absolute charge levels are much higher for the aged. For example, the 95th percentile of charges is $7,131 for the aged, but for the population under 65 years of age the 95th percentile of charges is only $2,126.
Table 9. Percent of medical care charges attributable to the heaviest users of services in the United States, by age: 1980.
| Enrollee percentile | Average per capita charge | Percent of charges | Standard error of percent of charges |
|---|---|---|---|
| 65 years or over | |||
| 10.0 | $4,001 | 68.4 | 2.50 |
| 5.0 | 7,131 | 50.6 | 3.47 |
| 1.0 | 16,701 | 21.2 | 4.07 |
| Under 65 years | |||
| 10.0 | 1,012 | 73.3 | 0.95 |
| 5.0 | 2,126 | 57.9 | 1.48 |
| 1.0 | 6,833 | 28.5 | 2.24 |
NOTE: Data on the noninstitutionalized population only is included in this table.
SOURCE: (Garfinkel, Riley, and Iannacchione, 1985).
Figure 2. Cumulative percent of charges attributable to various percentiles of United States residents, by age: 1980.
Discussion
The extent to which Medicare expenditures are concentrated among a relatively few costly enrollees has remained quite stable over time for both Part A and Part B services. Reimbursements under both Parts A and B exhibited a slight lessening in concentration between 1975 and 1982. The costliest 2.7 percent of Part A enrollees accounted for 45.3 percent of Part A reimbursements in 1969, 45.6 percent in 1975, and 44.3 percent in 1982; for Part B the top 2.2 percent of beneficiaries accounted for 29.0 percent of reimbursements in 1969, 29.0 percent of inflation-adjusted reimbursements in 1975, and 28.5 percent of inflation-adjusted reimbursements in 1982. Although these differences are rather slight, it is important to remember that a slight shift in the distribution of Medicare expenditures can represent a large amount in dollars. We also found that the percent of enrollees receiving reimbursement for Medicare services in a year has increased. Thus, more enrollees are receiving program benefits than in the past.
Our findings suggest that the large and consistent increases in Medicare program expenses that have occurred during the last several years have not been driven only by the increasing costs of the heaviest users, but appear to represent increases in service use across the entire spectrum of enrollees. There is some indication that expenses attributable to decedents are increasing at approximately the same rate as those attributable to survivors, and any differences do not appear to have had a major effect on the distribution or level of program expenditures. This suggests that expensive methods of prolonging the lives of terminally ill patients are not the culprit behind increasing Medicare program costs. This finding supports the conclusions drawn by Scitovsky (1984), who reviewed existing research on the costs of care rendered to terminally ill patients. Drawing largely from studies of the Medicare population, she concluded that, “The high cost of medical care at the end of life is not a recent development … ”, and that the data do not support the contention that, “… high medical expenses at the end of life are due largely to aggressive, intensive treatment of patients who are moribund.”
There has been considerable speculation that sophisticated and expensive new technologies, such as CAT scans and total hip replacement, may have had a strong impact on the increase in Medicare expenditures and their distribution among aged enrollees. This speculation centers on the creation of a new class of high-cost enrollees. Although issues surrounding expensive technologies cannot be addressed directly with our data, this article provides indirect evidence that visible, expensive technologies have not profoundly changed the distribution of Medicare program expenditures among the aged. This finding is in line with the results of other research that indicates that high-cost patients are often not users of advanced technology. For example, Zook and Moore (1981) found that relatively few high-cost patients in their sample hospitals used high technology services. Schroeder, Showstack, and Roberts (1979) determined that it was the amount, more than the kinds, of services that distinguished high-cost patients from others. It is likely that many new medical technologies are of relatively low cost, and that low, moderate, and high-cost users have all benefited. New medical technologies, as measured by increases in intensity of services, have clearly produced a general upward shift in costs (Ruther, 1983; Office of Technology Assessment, 1984; Congressional Budget Office, 1979), but they have not altered the overall relative distribution of health care costs of the Medicare aged.
Evans (1983 a and b) has commented on the nature and inevitability of allocating limited health care resources. He has noted that research has indicated that much of the increase in health care costs attributable to the proliferation of health care technologies is not due to new, big, expensive procedures, but to the proliferation of new procedures that are not expensive individually. This article suggests that these new procedures are probably not concentrated among a small number of users, but rather are distributed among low-, moderate-, and high-cost users. This suggests that if attempts are made to ration new technologies, they will be difficult to implement in many instances because so many providers and patients would be affected.
Acknowledgments
The authors wish to express their appreciation to Marian Gornick and Allen Dobson of the Health Care Financing Administration for their helpful comments on earlier drafts of this article.
Footnotes
In 1976 and 1982, ESRD patients comprised .015 percent and .036 percent of the aged population, respectively. Yet these small numbers of beneficiaries accounted for .52 percent and .68 percent of all Medicare expenditures on the aged in 1976 and 1982, respectively.
Reprint requests: Gerald Riley, Health Care Financing Administration, 2-C-15 Oak Meadows Building, 6325 Security Boulevard, Baltimore, Maryland 21207.
The Part B deductible carryover provision helped beneficiaries meet the Part B deductible before it was eliminated in 1980.
References
- Andersen R, Lion J, Anderson O. Two Decades of Health Services: Social Survey Trends in Use and Expenditure. Cambridge, Mass.: Ballinger Publishing Co.; 1976. [Google Scholar]
- Birnbaum H. The Cost of Catastrophic Illness. Lexington, Mass.: Lexington Books; 1978. [Google Scholar]
- Board of Trustees. 1983 Annual Report of the Board of Trustees of the Federal Supplementary Medical Insurance Trust Fund. Washington, D.C.: Jun 24, 1983. Federal Supplementary Medical Insurance Trust Fund. [Google Scholar]
- Congressional Budget Office. Controlling Rising Hospital Costs. Washington, D.C.: Congress of the United States; Sept. 1979. [Google Scholar]
- Congressional Budget Office. Catastrophic Medical Expenses: Patterns in the Non-Elderly, Non-Poor Population. Washington, D.C.: Congress of the United States; Dec. 1982. [Google Scholar]
- Evans R. Health care technology and the inevitability of resource allocation and rationing decisions: I. Journal of the American Medical Association. 1983a Apr.249(15):2047–2053. [PubMed] [Google Scholar]
- Evans R. Health care technology and the inevitability of resource allocation and rationing decisions: II. Journal of the American Medical Association. 1983b Apr.249(16):2208–2219. [PubMed] [Google Scholar]
- Garfinkel S, Riley G, Iannacchione V. High cost users of services. Draft report based on data from National Medical Care Utilization and Expenditure Survey. 1985 [Google Scholar]
- Goldstein I. Jul 22, 1985. Personal communication. [Google Scholar]
- Gornick M, Beebe J, Prihoda R. Health Care Financing Review. No. 1. Vol. 5. Washington: U.S. Government Printing Office; Fall. 1983. Options for change under Medicare: Impact of a cap on catastrophic illness expense. HCFA Pub. No. 03154. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- Helbing C. Health Care Financing Notes. No. 1. Office of Research and Demonstrations, Health Care Financing Administration; Nov. 1983. Medicare: Use and reimbursement for aged persons by survival status, 1979. HCFA Pub. No. 03166. [Google Scholar]
- Kunkel S. Mar 5, 1984. Personal communication. [Google Scholar]
- Lubitz J, Prihoda R. Health Care Financing Review. No. 3. Vol. 5. Washington: U.S. Government Printing Office; Spring. 1984. The use and costs of Medicare services in the last 2 years of life. HCFA Pub. No. 03169. Office of Research and Demonstrations, Health Care Financing Administration. [PMC free article] [PubMed] [Google Scholar]
- McMillan A, Pine P, Newton M. Health Care Financing Program Statistics. Washington: U.S. Government Printing Office; Mar. 1983. Medicare: Use of physicians' services under the supplementary medical insurance program, 1975-1978. HCFA Pub. No. 03151. Office of Research and Demonstrations, Health Care Financing Administration. [Google Scholar]
- Office of Research and Statistics, Social Security Administration. Medicare: Health Insurance for the Aged, 1969, Section 1: Summary. Washington, D.C.: 1975. [Google Scholar]
- Office of Technology Assessment. Medical Technology and Costs of the Medicare Program. Washington: U.S. Government Printing Office; Jul, 1984. OTA-H-227. U.S. Congress. [Google Scholar]
- Piro P, Lutins T. Health Insurance Statistics, HI 51. Washington: U.S. Government Printing Office; Oct. 1973. Utilization and reimbursements under Medicare for persons who died in 1967 and 1968. DHEW Pub. No.(SSA)74-11702. Office of Research and Statistics, Social Security Administration. [Google Scholar]
- Ruther M. Health Care Financing Program Statistics. Washington: U.S. Government Printing Office; Jun, 1983. Medicare: Use of short-stay hospitals by aged and disabled inpatients, 1978. HCFA Pub. No. 03147. Office of Research and Demonstrations. Health Care Financing Administration. [Google Scholar]
- Schroeder S, Showstack J, Roberts H. Frequency and clinical description of high-cost patients in 17 acute-care hospitals. N Engl J Med. 1979 Jun 7;300(23):1306–1309. doi: 10.1056/NEJM197906073002304. [DOI] [PubMed] [Google Scholar]
- Scitovsky A. The high cost of dying: What do the data show? Milbank Memorial Fund Quarterly/Health and Society. 1984;62(4):591–608. [PubMed] [Google Scholar]
- Zook C, Moore F. High-cost users of medical care. N Engl J Med. 1980 May 1;302(18):996–1002. doi: 10.1056/NEJM198005013021804. [DOI] [PubMed] [Google Scholar]
- Zook C, Moore F, Zeckhauser R. Catastrophic health insurance: A misguided prescription? The Public Interest. 1981 Winter;(62):66–81. [PubMed] [Google Scholar]