Significance
Thought depends on the brain, and cognitive neuroscience has shown that different sets of brain regions (systems) support different cognitive abilities. We hypothesized that complex cognition might be especially supported by hub brain locations that participate in many such systems. We studied neurological patients with focal brain lesions, and found that damage to hub locations produced much greater cognitive impairment than damage to other locations. This work may improve the understanding of outcomes of brain injuries (from, e.g., stroke, resection, or trauma) and help inform prognosis and rehabilitation efforts.
Keywords: functional connectivity, neuropsychology, fMRI, brain hubs
Abstract
Hubs are network components that hold positions of high importance for network function. Previous research has identified hubs in human brain networks derived from neuroimaging data; however, there is little consensus on the localization of such hubs. Moreover, direct evidence regarding the role of various proposed hubs in network function (e.g., cognition) is scarce. Regions of the default mode network (DMN) have been frequently identified as “cortical hubs” of brain networks. On theoretical grounds, we have argued against some of the methods used to identify these hubs and have advocated alternative approaches that identify different regions of cortex as hubs. Our framework predicts that our proposed hub locations may play influential roles in multiple aspects of cognition, and, in contrast, that hubs identified via other methods (including salient regions in the DMN) might not exert such broad influence. Here we used a neuropsychological approach to directly test these predictions by studying long-term cognitive and behavioral outcomes in 30 patients, 19 with focal lesions to six “target” hubs identified by our approaches (high system density and participation coefficient) and 11 with focal lesions to two “control” hubs (high degree centrality). In support of our predictions, we found that damage to target locations produced severe and widespread cognitive deficits, whereas damage to control locations produced more circumscribed deficits. These findings support our interpretation of how neuroimaging-derived network measures relate to cognition and augment classic neuroanatomically based predictions about cognitive and behavioral outcomes after focal brain injury.
The careful description of circumscribed cognitive and behavioral deficits following localized brain damage has provided much of our knowledge of the functional geography of the brain. In some cases, however, relatively small, circumscribed lesions seem to have broader effects than would be predicted from their size and location. Historically, these effects sometimes have been attributed to diaschisis (i.e., effects at a distance) owing to connections between affected and unaffected brain regions. The potential importance of interactivity among brain regions is supported by recent research (1–3); for example, He et al. (4) found that visuospatial inattention after right inferior parietal lesions was best explained by the effects of those lesions on more superior parietal activity.
In the broadest sense, interactive explanations of brain function can be thought of as reflecting the organization of the brain as a large-scale network. The advent of large-scale network descriptions of brain structure and function extends the possibility of richer and broader explanations of unusually severe cognitive and behavioral consequences that sometimes follow circumscribed lesions.
Some large-scale network studies have focused on “hubs,” a term from network science that indicates potential points of importance for network traffic. Two contrasting views of hubs have arisen. One view focuses on the number of connections between sets of regions, with those regions showing the most connections (i.e., highest degree) considered candidate hubs. For example, Hagmann et al. (5) reported that the posterior midline is the “core” of structural brain networks, and Buckner et al. (6) reported that “cortical hubs” are found in the precuneus/posterior cingulate (pCC) and elsewhere in the default mode network (DMN). Several other studies have found that regions of the DMN, especially the pCC, have high ratings on related measures of network importance (7–9) (Fig. S1).
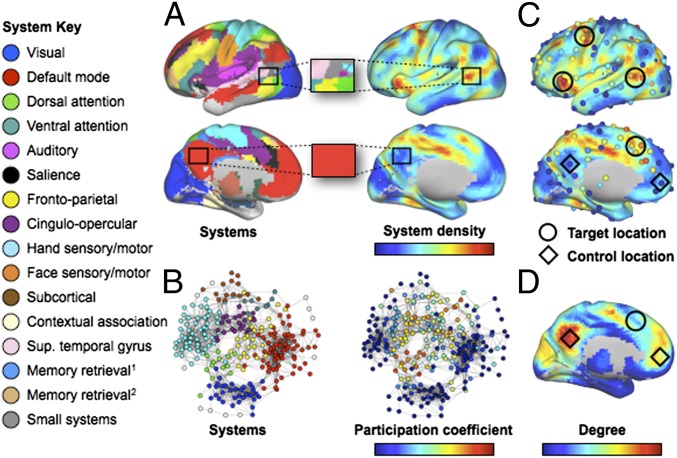
In contradistinction, we have argued that in correlation networks, such as those studied using resting state fMRI, degree may not reflect the importance of a node to network function because it can be strongly modulated by network size (10). Degree measures the number of connections that a given region makes, but not the number of unique systems connected to that region. We have predicted that lesions of brain regions exhibiting correlated activity with multiple brain systems will produce widespread effects on brain function (Fig. 1) (10). This prediction builds on investigations that partitioned the cortex into multiple functionally distinct systems based on correlated activity in spontaneous functional MRI (fMRI) signal (11–13). Analysis at the level of these systems permits new measures for brain regions (Fig. 1): system density is a measure of the physical proximity of multiple brain systems (Fig. 1A), and participation coefficient is a measure of the number of different systems with which a node has strong signal correlations (Fig. 1B).
Fig. 1.
Network measures. (A, Left) Consensus communities (systems) from refs. 10 and 12. (Right) Plot of the density of these systems across the cortex. The blowup boxes illustrate how certain cortical locations contain many systems (Upper: a target location) or few systems (Lower: a control location). (B, Left) Communities (systems) in a brain-wide network. (Right) Node participation coefficients, with warmer colors denoting nodes that display spontaneous BOLD activity that correlates with multiple systems. (C) Plots of system density and participation coefficients overlaid. Target locations (circles) show where lesions might produce multi-system impairment. Control locations (diamonds) are predicted not to produce widespread impairment. Only 4 of 6 target locations are shown (those in the left hemisphere). (D) Node degree, with warmer colors indicating higher degree. Note that regions with high degree (D) may have low system density and/or participation coefficient (C). Fig. S2 presents additional information about these data. The names for systems given in the left-side legend are either those commonly used (e.g., DMN) or are demonstrated functional properties of the labeled system when no consensus name exists (e.g., “Memory retrieval1” refers to data in ref. 12, and “Memory retrieval2“ refers to data in ref. 33).
Our framework makes the following predictions: first, that lesions to locations with high system density and a high participation coefficient will affect processing in multiple systems and produce impairment across several cognitive domains, and second, that lesions to locations with low scores on these measures will have more limited consequences. These predictions align with and advance an emerging perspective on the importance of connector regions in brain networks (1, 2, 14).
This investigation provides a first-order test of our hub definition by evaluating long-term cognitive and behavioral outcomes in 30 patients (Table 1 and Table S1), 19 with focal lesions to six “target” locations with high values of participation coefficient and system density as suggested by our approach, and 11 with focal lesions to two “control” locations with high degree centrality: pCC and anterior medial prefrontal cortex (amPFC). Neuropsychological data were collected and lesions were localized at >3 mo after injury. Our prediction is that damage to brain regions that are proximal to and participate with many brain systems (i.e., target locations) will produce widespread cognitive impairment. If only lesions in target locations produce this pattern, then our framework is supported, whereas if only lesions in control locations produce this pattern, then our framework is not supported. These possibilities correspond to the relative success of diversity-emphasizing versus connection-counting network measures in identifying important brain regions in fMRI correlation networks. More generally, either outcome would be a major demonstration of the utility of studying spontaneous brain activity using network analysis.
Table 1.
Demographic information for patients in the control and target groups
| Group | ROI | Case no. | Sex | Education, y | Age, y |
| Control | amPFC | 1 | F | 13 | 38 |
| amPFC | 2 | F | 13 | 55 | |
| amPFC | 3 | M | 12 | 48 | |
| amPFC | 4 | M | 14 | 26 | |
| amPFC | 5 | F | 13 | 66 | |
| amPFC | 6 | M | 18 | 56 | |
| pCC | 7 | F | 19 | 40 | |
| pCC | 8 | F | 12 | 35 | |
| pCC | 9 | F | 12 | 43 | |
| pCC | 10 | F | 16 | 34 | |
| pCC | 11 | F | 12 | 47 | |
| Mean | 14.000 | 44.364 | |||
| SD | 2.530 | 11.535 | |||
| Target | L pMFG | 12 | F | 12 | 71 |
| L pMFG | 13 | M | 12 | 35 | |
| L pMFG | 14 | F | 12 | 62 | |
| L pMFG | 15 | F | 12 | 47 | |
| L pMFG | 16 | F | 12 | 56 | |
| L pMFG | 17 | M | 12 | 68 | |
| L aIns | 18 | M | 12 | 75 | |
| L aIns | 19 | M | 12 | 29 | |
| L aIns | 20 | M | 12 | 58 | |
| L aIns | 21 | M | 11 | 57 | |
| L aIns | 22 | M | 12 | 53 | |
| L aIns | 23 | M | 16 | 49 | |
| dmPFC | 24 | F | 16 | 32 | |
| dmPFC | 25 | M | 11 | 50 | |
| R aIns | 26 | M | 16 | 64 | |
| R aIns | 27 | M | 12 | 77 | |
| R pMFG | 28 | F | 14 | 53 | |
| L pMTG | 29 | F | 12 | 67 | |
| L pMTG | 30 | F | 9 | 65 | |
| Mean | 12.474 | 56.211 | |||
| SD | 1.806 | 13.758 | |||
| Statistical difference | NS | * | * | ||
| Statistic value | Fisher | 2.224 | 2.282 | ||
| P value | 0.1 | 0.026 | 0.022 | ||
Group (bold) indicates cases in the control (upper) or target (lower) groups. Mean and SD for each variable are presented beneath each group. Between-group tests for each variable (Fisher's exact test for sex; nonparametric rank-sum test otherwise) are presented at the bottom of the table. Age refers to age of the patient at the time of research neuroimaging used for lesion tracing. Fisher refers to Fisher's exact test, which yields only a P value. dmPFC, dorsomedial prefrontal cortex; L aIns, left anterior insula; L pMFG, left posterior middle frontal gyrus; L pMTG, left posterior middle temporal gyrus; NS, not significant; R alns, right anterior insula; R pMFG, right posterior middle frontal gyrus. More information is available in Table S1.
*P < 0.05.
Results
The Iowa Neurological Patient Registry (hereinafter, “the Registry”) contains data from patients with focal, stable brain lesions who have undergone comprehensive neuropsychological testing and brain imaging in the chronic epoch (>3 mo after lesion onset). On the basis of lesion location alone (i.e., blinded to the neuropsychological data) we identified 30 patients in the Registry with a focal lesion encompassing one of the six target or two control locations. Fig. 1 and Fig. S2 present network data underlying target and control location selection, and Fig. S3 provides images of lesion locations. Lesion sizes were not significantly different between groups, and on average lesions were slightly larger in the control group than in the target group (see Methods). Selection criteria are presented in Methods.
We evaluated cognitive and behavioral data obtained from the neuropsychological profile of each patient. Neuropsychological reports and test data were reviewed by two clinical neuropsychologists (who were blinded to lesion location and not informed of the purposes of the study) to rate each patient's degree of impairment across several cognitive and behavioral domains (referred to as “cognitive domains” hereinafter) (Table S2). The cognitive domains were modeled after the domains listed in Lezak’s Neuropsychological Assessment (15), a standard clinical neuropsychology textbook. This procedure yielded a numerical score for each patient in each cognitive domain.
Impairment Ratings.
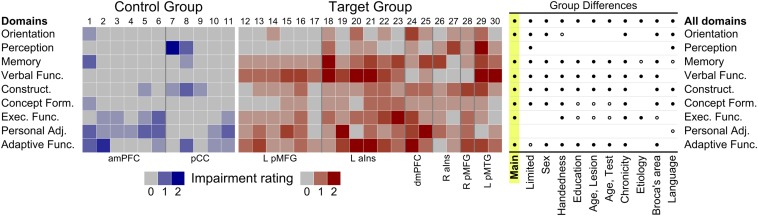
The disparity between the consequences of lesions to target versus control locations is immediately appreciable in Fig. 2 (Left). ANOVA yielded significant effects of group, cognitive domain, and interactions of group and cognitive domain; full statistical details are provided in Table S3. For the group of patients with target lesions, significant impairment (i.e., mean impairment scores > 0) was found in all nine domains. In contrast, the control group was significantly impaired in three of the nine domains (Executive Functions, Personal Adjustment/Emotional Functions, and Adaptive Functions) and marginally impaired in the Construction/Motor Performance domain. In group contrasts, patients with lesions to target locations were significantly more impaired than patients with lesions to control locations in seven of the nine domains (highlighted column of Fig. 2, Right).
Fig. 2.
Individual mean ratings for impairment and analysis summary. (Left) Neuropsychological impairment across nine cognitive and behavioral domains for the control (n = 11) and target (n = 19) groups. Control cases are at left in shades of blue, target cases are at right in shades of red. Ratings of cognitive impairment for each case by domain were as follows: 0 = no impairment (gray), 1 = moderate impairment (light), 2 = severe impairment (dark). Intermediate colors represent a score of 0.5 or 1.5 from averaging across two raters. Note the concentration of moderate and severe cognitive impairments among target cases. (Right) Summary of main analysis and follow-up analyses controlling for demographic, attribute, and lesion variables. Follow-up analyses controlling for several variables (see column labels) revealed a pattern broadly similar to the main analysis (left-most data column, highlighted) with significant impairments of the target group always evident in at least two of nine cognitive domains. Main refers to the main analysis; Limited, results for less frequently sampled target locations only; Sex, mixed-sex locations only; Handedness, fully-right handed participants only; Education, years of education, controlled by regression (R); Age, Lesion, age at injury in years, R; Age, Test, age when tested, R; Chronicity, years between injury and test, R; Etiology, etiology of stroke only; Broca's area, no damage to Broca's area; Language, no impairment in Verbal Functions. ●, target group significantly impaired relative to control group, P < 0.05; ○, marginal impairment; P < 0.10. See also Tables S3 and S4 and Fig. S4.
On average, a target lesion produced impairment in 6.89 domains (SD = 1.37), whereas a control lesion produced impairment in 2.64 domains (SD = 1.21), a statistically significant difference (Wilcox Z = 4.355, P < 0.001). This general pattern of greater impairment in the target group across many cognitive domains held regardless of whether group differences were tested using all target locations (six locations; cases 12–30), only the higher-sampled target locations (two locations; cases 12–23), or only the less-sampled target locations (four locations; cases 24–30).
Follow-Up Analyses.
We performed several follow-up analyses to evaluate the extent to which various demographic and lesion variables played a role in the cognitive and behavioral results. We found no evidence that the main finding (i.e., that the target group had greater cognitive impairment in more domains than the control group) could be thoroughly accounted for by any factor other than lesion location (Fig. 2). Although most factors had limited effects (Fig. S4 and Table S4), outcomes varied somewhat with lesion etiology (Fig. S4D). Patients with resections (n = 10; 7 control, 3 target) had group differences congruent with our predictions. Among patients with an etiology of stroke (n = 20; 4 control, 16 target), the general pattern held but the magnitude of the group difference was attenuated. This attenuation obtained because the two control cases who were most impaired (cases 1 and 8) both had an etiology of stroke, and these two cases comprised half the control sample in this stroke-only supplemental analysis.
Network Properties of Lesioned Brain Regions.
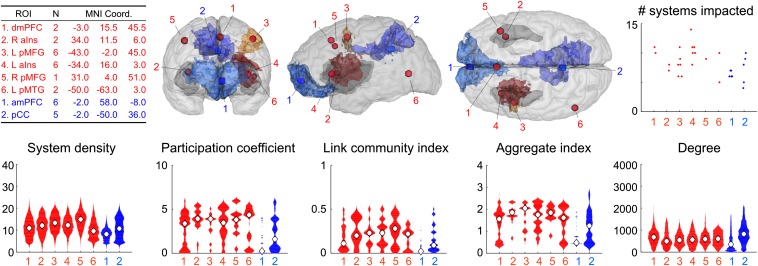
Network properties derived from functional neuroimaging data of healthy young adults were used to identify target and control locations. The actual lesions extended beyond the target and control regions of interest (ROIs) and locations, however; for example, the glass brain shown in Fig. 3 illustrates the actual regions affected at the four well-sampled lesion locations (controls, blue; targets, red). Lesion extent and overlap is illustrated for each target and control location in Fig. S3. It is important to determine whether the tissue that was actually lesioned had the network properties that we originally sought to isolate at our target and control locations.
Fig. 3.
Target and control ROIs, location, and network properties. (Upper, Left) Descriptions of each ROI, number of patients, and MNI 152 coordinates of each location. (Center) Target and control ROIs (red spheres and blue boxes, respectively) superimposed on the lesion-mapping template brain (in glass brain format) viewed from several perspectives (from left to right: frontal, left lateral, and dorsal). The cerebral cortex is shown in light gray, and the insular cortex is shown (bilaterally) in darker gray. The remaining colored portions of the figures indicate the lesion overlap of the two target and two control ROIs that were sampled most often. The illustrated degree of lesion overlap was selected on a per-group basis to best reflect the common portion of that group’s brain damage; for the four groups, the degree of lesion overlap depicted is as follows: left posterior middle frontal gyrus (L pMFG), 4 (n = 6); left anterior insula (L aIns), 5 (n = 6); amPFC, 5 (n = 6); pCC, 3 (n = 5). Lesions at each individual target and control location are shown in Fig. S3. (Right) Damage to several functional systems is evident in both groups (see also Fig. S5). (Lower) Violin plots of the network properties of the tissue sampled by the lesions, binned by lesion location. The participation coefficient is the measure that best distinguishes target and control locations.
We used the lesion masks to extract the network properties of the corresponding tissues in healthy subjects. The violin plots in Fig. 3 (Lower) show that the extended lesion territories generally had the intended network properties; for example, participation coefficients at the lesioned tissue were much higher in all target locations, and system density and link community membership were higher in most target locations. Measures of sampled degree aligned less well with expectations, but pCC lesions were associated with the highest observed degree.
Ideally, our lesion sampling would have yielded high degree for both control locations and low degree for all target locations (Fig. 1D and Fig. S2). Instead, amPFC had the lowest sampled degree, likely because the amPFC lesions often sampled inferior tissue, including the orbitofrontal cortex, where fMRI signals are susceptible to methodological artifacts that yield low degree. However, neither idealized nor observed measures of degree predicted cognitive outcomes. Instead, participation coefficient was the best predictor of the highly disparate cognitive and behavioral outcomes among patients with lesions to target or control locations.
Discussion
We found that damage to target locations (i.e., brain regions in proximity to many functional systems that show coordinated activity with surrounding systems) produced severe and widespread cognitive impairment. Other studies have considered the effects of lesions on specific brain networks (2–4, 16–18), and brain injuries affecting connector regions have been shown to alter network modularity to a greater degree than lesions of hubs (1). Here we have extended previous work (1, 10) by evaluating the neuropsychological consequences of lesions to hubs identified with specific network properties.
Practitioners of neurology and neuropsychology have long observed that despite superficially similar brain lesions, different patients often present with very different degrees of impairment and exhibit very different recovery trajectories. Extent of poststroke recovery varies with many patient-related factors (e.g., age at stroke onset, sex, handedness, socioeconomic status) and various stroke- and lesion-related factors (e.g., initial stroke severity, lesion size, stroke subtype, lesion location), but these factors have very limited predictive power for outcome (19–24). Even good predictors, including initial stroke severity and lesion volume, leave most of the variability in outcome unexplained (25–28).
Network-level considerations, especially pertaining to cross-system participation, may help explain the variability in outcomes. We speculate that focal lesions centered on highly participatory brain regions may affect communication between functional systems, thereby causing more widespread cognitive impairment than comparable damage within any single functional system. The disparate cognitive findings between patients with target lesions and those with control lesions, along with the disparate participation coefficient measures sampled by target and control lesions, support such an interpretation. By an alternative account, small amounts of damage to many systems may affect the independent functioning of each system to produce poor outcomes, perhaps via diaschisis (2). Our data provide less support for this explanation; although control lesions tended to damage fewer systems than target lesions, there was substantial overlap between the number of systems actually affected by target and control lesions (Fig. 3).
A third alternative is that perhaps target lesions, but not control lesions, degraded one common, critical system that could account for the disparity in outcomes. This possibility is reminiscent of the framework advanced by Woolgar et al. (17), in which estimated IQ loss was related to the amount of damage to a “multiple demand” system that effectively combines two systems of this study (Fig. 1: frontoparietal, yellow; cingulo-opercular, purple). However, when the systems affected by lesions in our sample were examined, only modest support was found for this explanation: frontoparietal and cingulo-opercular systems were damaged in the control lesions, and the cingulo-opercular system was completely spared by lesions at one of our target locations. Future investigations of larger numbers of target locations may help adjudicate these and other possible explanations for our findings.
Large-scale investigation of the human brain's densely networked functional systems has become possible only recently, and the promise of this approach is evident in the agreement between our predictions and our findings. Our results inform the meaning of graph-theoretic measures in the context of functional brain networks characterized with Pearson correlations; for example, with regard to our target locations, several studies have converged on fairly similar localizations of “cross-system” relationships (10, 14, 29), and it would appear that such measures identify regions that influence cognition broadly.
Meanwhile, although many previous investigations of functional neuroimaging networks have reported that the control regions that we tested have high degree, we found that degree did not identify regions of broad importance across many cognitive domains (at least insofar as the results from neuropsychological outcomes would indicate). Degree may be sufficiently influenced by system size that a given region's unique connections are not well captured or represented by the degree index. Notably, many versions of centrality that measure not only numbers of connections, but also path length information (e.g., PageRank centrality, subgraph centrality), yield patterns similar to degree centrality (Fig. S1).
Our study has some limitations. Sample sizes were relatively small, albeit comparable with those of other lesion studies with similar themes (1, 2), and highly focal lesions encompassing particular cortical locations are rare (e.g., the 30 participants reported here were drawn from a much larger pool). Because this report represents a proof-of-principle test of a novel hypothesis, we investigated only a few target and control locations, leaving others for future investigation; however, our neuropsychological predictions were supported across all locations tested and nearly all participants examined despite blinded selection based solely on neuroanatomical criteria. Lesion etiology was mixed in our patient sample, and future investigations should address any contributions of this factor by evaluating more patients with stroke. Language impairments were prevalent in the target group, but several target patients (with right-lateralized and midline lesions) had normal language but still exhibited impairment in many cognitive and behavioral domains.
In conclusion, this neuropsychological investigation provides support for our characterization of important components of brain networks. Damage to regions with high system density and high participation coefficient produced widespread cognitive deficits, whereas damage to other locations produced more circumscribed deficits, consistent with predictions derived from the framework advanced by Power et al. (10). Our findings enhance the understanding of brain organization and function in ways that may eventually translate into useful knowledge capable of informing clinical practice.
Methods
Network Measures in Resting-State MRI Data From Healthy Young Adults.
To identify locations in the brain that might serve important integrative functions, three network analyses were performed in data from 120 healthy young adults, a dataset described previously (10), along with the first two of the following three analyses. The first analysis (Fig. 1A) identified voxel-level communities in brain-wide networks, and then calculated at each voxel how many unique communities (or systems) were proximal to that voxel (system density). The second analysis (Fig. 1B) identified communities in a brain-wide network of 264 nodes, and then calculated how evenly a node’s edges were distributed among all communities using the measure of participation coefficient. Nodes with high participation coefficient display signals highly correlated to many communities and, we speculate, may facilitate communication or integration of multiple types of information (10).
A third analysis, not reported previously, was performed as well. Exactly the same matrices used in the participation coefficient analyses were used to form link matrices (30), to which the Infomap algorithm was applied (31), yielding a set of link communities. Link communities provide community assignments to edges instead of nodes. For a given analysis, for a given node, we defined link community membership as the number of link communities to which the node belongs divided by the total number of link communities present in that analysis. Thus, link community membership indexes the diversity of a node’s correlations. Echoing the methods behind the first two analyses, a summary link community index is the normalized mean value across all analyses for each node.
We have argued previously that using connection-counting measures such as degree in functional networks may not yield indices of node importance due to general properties of correlation networks (10). Instead, we have argued that the diversity of correlations exhibited by a node may reflect that node’s importance to network function. On this view, sites that score highly on the three measures described above may be especially important to brain function. To identify such locations, volumetric peaks in system density were found; then at all 264 nodes, the summary values from each of the three analyses were averaged across analyses; finally, target locations were identified where volumetric peaks were accompanied by nearby nodes with high scores across integrative measures (Fig. 1C). Brain slices showing all measures described above are presented in Fig. S2.
Identifying Target and Control Locations.
Six sites were selected as target locations in our study (Figs. 1 and 3 and Fig. S2). These target location coordinates were selected before patient selection or examination of neuropsychological data. Because these analyses are proof-of-principle (i.e., testing the proposition that high degree does not reflect node importance in correlation networks, but diverse correlations may identify important nodes), we concentrated our efforts on these six target locations. Additional target locations will be the subject of future investigations. We chose two control location coordinates (Figs. 1 and 3 and Fig. S2) based on the considerations of (i) being located in association cortex (all target sites are in association cortex); (ii) low scores on the network measures used to identify target locations; (iii) being sufficiently distant from target sites to facilitate physical segregation of lesions; and (iv) previous identification as a putative brain hub. The pCC is widely viewed as a cortical hub based on degree-like measures in correlation networks (Fig. S1). Other portions of the DMN also have been identified using similar measures. Thus, we selected the pCC and amPFC as control sites, and used published coordinates (locations 3 and 6 of table 3 in ref. 6) to define our locations.
Patients with Brain Lesions.
Consent.
In compliance with the principles of the Declaration of Helsinki, all patients granted informed consent at the time of their enrollment in the Iowa Neurological Patient Registry (“the Registry”).
Selection procedure.
Participants were selected from the Registry based solely on lesion locale and extent. Selections were made by D.E.W. and J.B., who were blinded to the neuropsychological profiles of all patients during the lesion selection process. Lesion mapping (typically based on structural MRI data, but occasionally based on CT data when MRI was contraindicated) was conducted using the MAP-3 procedure (32), in which lesions are manually mapped onto a common template brain. ROIs for the eight preselected locations (i.e., six targets and two controls) were instantiated as spheres (diameter = 8 mm) at the appropriate coordinates in template space (Fig. 3), using an affine transform to warp MNI coordinates of desired target and control locations to the space of the MAP-3 template brain.
Patients were eligible for inclusion in the present study if their mapped lesion intersected with a target or control ROI. We set an inclusion criterion requiring that >50% of the ROI volume be lesioned, although this criterion was relaxed to include patients with any damage for the pCC control ROI 2, because the pCC is infrequently sampled by naturally occurring lesions. Despite this, we note that multiple studies have identified a large region of the pCC as being of high degree (Fig. S1), and that our pCC ROI is centered within this region. Therefore, even though the spherical pCC ROI is less well sampled by our lesions, the lesions encompassed much of the surrounding high-degree tissue (Fig. 3). Overall, the selection process yielded a total of 30 patients, 19 with lesions damaging a target location and 11 with lesions that damaged a control location. We emphasize that no neuropsychological data had been examined at this point in the patient selection and study enrollment process.
Demographic data.
Demographic information for the target and control groups is presented in Table 1 and Table S1. All patients suffered their brain lesion in adulthood (age ≥21 y), and all had contemporaneous structural neuroanatomical and neuropsychological studies in the chronic epoch (i.e., >3 mo after lesion onset). In accordance with their enrollment in the Registry, all patients had no history of intellectual limitation, learning disability, psychiatric disease, or dementia, and had focal, stable lesions. Raw years of education were statistically greater in the control group (Table 1); however, binned categorical education attainment (i.e., ≤12 y; 12–15 y, or ≥16 y; Table S1) did not differ significantly between the groups (P = 0.431, Fisher's exact test), and neither did professional attainment (P = 0.264, Fisher's exact test) (Table S1). The target group was statistically older than the control group, and stroke was a more frequent etiology in the target group.
To explore whether any between-group demographic or lesion differences (whether statistically significant or not, and which might work for or against our hypotheses) could account for our results, we included follow-up analyses to address these variables (Results; Fig. 2, Right; and Table S4).
Lesion volume.
We evaluated lesion volume for each group and tested for differences. Overall, the volume of lesions (in mm3) to target and control locations [T(27.131) = 0.346, P = 0.734] and (normatively predicted) gray or white matter lesion volumes [for both, T(27) <1.1, P > 0.3] did not differ between the groups. One potential exception to this pattern was that the two dmPFC target lesions were unusually large; when these were excluded, the remaining 17 target lesions were significantly smaller than the 11 control lesions [T(18.676) = 2.16, P = 0.044]. To the extent that smaller lesions might be expected to correspond to lesser cognitive impairment, this would work against our predictions.
We also considered lesion volume in the larger context of Registry patients with mapped lesions (Fig. S6, Middle). The lesion volume in the target group ranged from the 6th to the 99th percentile (mean, 49th percentile); in the control group, lesion volume ranged from the 21st to the 85th percentile (mean, 64th percentile).
Quantification of Cognitive and Behavioral Data.
Under the auspices of their enrollment in our Registry, patients underwent a comprehensive neuropsychological examination that included an interview with a board-certified clinical neuropsychologist and an extensive battery of neuropsychological tests. Standardized quantitative indices were available for all major aspects of cognition and behavior, including intellectual abilities, memory, speech and language, perception and attention, visuoconstructional ability, psychomotor and psychosensory functions, executive functions, personality and affect, and adjustment and functional status. The neuropsychological examination was completed in the chronic epoch (>3 mo after onset), contemporaneous with the structural neuroimaging studies that provided the basis for the neuroanatomical analysis (as above).
To quantify the cognitive and behavioral data, neuropsychological reports and test data were reviewed to rate each patient's degree of impairment across classic cognitive and behavioral domains (15). Each patient’s status was rated in nine domains: Orientation/Attention, Perception, Memory, Verbal Functions/Language Skills, Construction/Motor Skills, Concept Formation/Reasoning, Executive Functions, Personal Adjustment/Emotional Functions, and Adaptive Functions (i.e., outcome) (Table S2). For each domain, the following rating scale was used: 0 = no impairment, meaning no significant impairment; 1 = moderate impairment, neuropsychological performance 1.5–2 SD below normative expectations and some effect on activities of daily living; 2 = severe impairment, neuropsychological performance at least 2 SD and typically ≥3 SD below normative expectations that substantially affect activities of daily living.
Each patient was rated independently by two experienced clinical neuropsychologists (N.L.D. and E.J.W.). The raters evaluated each patient’s history, clinical notes, and neuropsychological dataset, and rendered ratings for each of the nine domains. Both raters were blinded to the specific lesion details of all participating patients in this rating phase, and both were deliberately blinded to the purpose, hypotheses, and motivating theoretical perspective of the study until after the rating phase. After the independent ratings were completed, an average of the two raters' scores was taken for each patient for each domain. Disparities were minor, and the overall interrater reliability from the independent ratings was acceptable (Fleiss–Cohen weighted κ = 0.502).
Analysis.
Impairment rating data were used to evaluate group-level differences. Per-domain and overall impairment ratings were analyzed by testing for a main effect of group membership using parametric repeated-measures ANOVA, followed by planned tests of between-group differences per domain using nonparametric Wilcox tests (chosen to minimize the possibility of type I errors because of small sample sizes). Within-group impairments versus an expectation of no impairment (i.e., impairment score of 0) were tested using one-sample Wilcox tests. Overall cognitive impairment was evaluated by taking the mean rating of impairment across all domains for each patient and testing these per-patient aggregate ratings of impairment between groups. The significance of all statistical tests was determined using α = 0.05.
Follow-up analyses intended to control for influence of demographic variables, including education, age, and chronicity, were conducted by first regressing impairment scores on the demographic variables and then analyzing the residual values. For the remaining follow-up analyses, smaller samples of patients were used to limit the effects of the variable of concern (e.g., sex, handedness, damage to Broca's area, language deficits). That these variables did not cause control vs. target dissociations can be immediately appreciated in Fig. S4, which represents Fig. 2 with various cases (columns) eliminated based on exclusion criteria. The degree of damage to putative functional systems (see Fig. 1) for the target and control groups is summarized in Fig. S5. In addition, the relationship between lesion volume and neuropsychological profile in each group was evaluated using correlation measures (Fig. S6, Bottom).
Supplementary Material
Acknowledgments
This work was supported by National Institutes of Health (NIH) Grant P01 NS19632 (to D.T.), NIH Grant R21NS061144 (to S.E.P.), the McDonnell Foundation Collaborative Action Awards (to S.E.P. and D.T.), Simons Foundation Award 95177 (to S.E.P.), National Institutes of Mental Health Grant R01 MH062500 (to D.E.W.), and NIH Grant F30 MH940322 (to J.D.P.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1322173111/-/DCSupplemental.
References
- 1.Gratton C, Nomura EM, Pérez F, D’Esposito M. Focal brain lesions to critical locations cause widespread disruption of the modular organization of the brain. J Cogn Neurosci. 2012;24(6):1275–1285. doi: 10.1162/jocn_a_00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nomura EM, et al. Double dissociation of two cognitive control networks in patients with focal brain lesions. Proc Natl Acad Sci USA. 2010;107(26):12017–12022. doi: 10.1073/pnas.1002431107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carter AR, et al. Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Ann Neurol. 2010;67(3):365–375. doi: 10.1002/ana.21905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He BJ, et al. Breakdown of functional connectivity in frontoparietal networks underlies behavioral deficits in spatial neglect. Neuron. 2007;53(6):905–918. doi: 10.1016/j.neuron.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Hagmann P, et al. Mapping the structural core of human cerebral cortex. PLoS Biol. 2008;6(7):e159. doi: 10.1371/journal.pbio.0060159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckner RL, et al. Cortical hubs revealed by intrinsic functional connectivity: Mapping, assessment of stability, and relation to Alzheimer’s disease. J Neurosci. 2009;29(6):1860–1873. doi: 10.1523/JNEUROSCI.5062-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cole MW, Pathak S, Schneider W. Identifying the brain’s most globally connected regions. Neuroimage. 2010;49(4):3132–3148. doi: 10.1016/j.neuroimage.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Tomasi D, Volkow ND. Functional connectivity hubs in the human brain. Neuroimage. 2011;57(3):908–917. doi: 10.1016/j.neuroimage.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zuo XN, et al. Network centrality in the human functional connectome. Cereb Cortex. 2012;22(8):1862–1875. doi: 10.1093/cercor/bhr269. [DOI] [PubMed] [Google Scholar]
- 10.Power JD, Schlaggar BL, Lessov-Schlaggar CN, Petersen SE. Evidence for hubs in human functional brain networks. Neuron. 2013;79(4):798–813. doi: 10.1016/j.neuron.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith SM, et al. Network modelling methods for FMRI. Neuroimage. 2011;54(2):875–891. doi: 10.1016/j.neuroimage.2010.08.063. [DOI] [PubMed] [Google Scholar]
- 12.Power JD, et al. Functional network organization of the human brain. Neuron. 2011;72(4):665–678. doi: 10.1016/j.neuron.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeo BT, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106(3):1125–1165. doi: 10.1152/jn.00338.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braga RM, Sharp DJ, Leeson C, Wise RJ, Leech R. Echoes of the brain within default mode, association, and heteromodal cortices. J Neurosci. 2013;33(35):14031–14039. doi: 10.1523/JNEUROSCI.0570-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological Assessment. New York: Oxford Univ Press; 2012. [Google Scholar]
- 16.Carter AR, Shulman GL, Corbetta M. Why use a connectivity-based approach to study stroke and recovery of function? Neuroimage. 2012;62(4):2271–2280. doi: 10.1016/j.neuroimage.2012.02.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolgar A, et al. Fluid intelligence loss linked to restricted regions of damage within frontal and parietal cortex. Proc Natl Acad Sci USA. 2010;107(33):14899–14902. doi: 10.1073/pnas.1007928107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James GA, et al. Changes in resting state effective connectivity in the motor network following rehabilitation of upper extremity poststroke paresis. Top Stroke Rehabil. 2009;16(4):270–281. doi: 10.1310/tsr1604-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glymour MM, et al. Lesion characteristics, NIH stroke scale, and functional recovery after stroke. Am J Phys Med Rehabil. 2007;86(9):725–733. doi: 10.1097/PHM.0b013e31813e0a32. [DOI] [PubMed] [Google Scholar]
- 20.Jaillard A, Grand S, Le Bas JF, Hommel M. Predicting cognitive dysfunctioning in nondemented patients early after stroke. Cerebrovasc Dis. 2010;29(5):415–423. doi: 10.1159/000289344. [DOI] [PubMed] [Google Scholar]
- 21.Patel MD, McKevitt C, Lawrence E, Rudd AG, Wolfe CD. Clinical determinants of long-term quality of life after stroke. Age Ageing. 2007;36(3):316–322. doi: 10.1093/ageing/afm014. [DOI] [PubMed] [Google Scholar]
- 22.Plowman E, Hentz B, Ellis C., Jr Post-stroke aphasia prognosis: A review of patient-related and stroke-related factors. J Eval Clin Pract. 2012;18(3):689–694. doi: 10.1111/j.1365-2753.2011.01650.x. [DOI] [PubMed] [Google Scholar]
- 23.Pohjasvaara TI, et al. White matter lesions are related to impaired instrumental activities of daily living poststroke. J Stroke Cerebrovasc Dis. 2007;16(6):251–258. doi: 10.1016/j.jstrokecerebrovasdis.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Ween JE, Alexander MP, D’Esposito M, Roberts M. Factors predictive of stroke outcome in a rehabilitation setting. Neurology. 1996;47(2):388–392. doi: 10.1212/wnl.47.2.388. [DOI] [PubMed] [Google Scholar]
- 25.Bagher-Ebadian H, et al. Predicting final extent of ischemic infarction using artificial neural network analysis of multi-parametric MRI in patients with stroke. PLoS ONE. 2011;6(8):e22626. doi: 10.1371/journal.pone.0022626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beaulieu C, et al. Longitudinal magnetic resonance imaging study of perfusion and diffusion in stroke: Evolution of lesion volume and correlation with clinical outcome. Ann Neurol. 1999;46(4):568–578. doi: 10.1002/1531-8249(199910)46:4<568::aid-ana4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 27.Jokinen H, et al. White matter hyperintensities as a predictor of neuropsychological deficits post-stroke. J Neurol Neurosurg Psychiatry. 2005;76(9):1229–1233. doi: 10.1136/jnnp.2004.055657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lövblad KO, et al. Ischemic lesion volumes in acute stroke by diffusion-weighted magnetic resonance imaging correlate with clinical outcome. Ann Neurol. 1997;42(2):164–170. doi: 10.1002/ana.410420206. [DOI] [PubMed] [Google Scholar]
- 29.Yeo BT, Krienen FM, Chee MW, Buckner RL. Estimates of segregation and overlap of functional connectivity networks in the human cerebral cortex. Neuroimage. 2013;88C:212–227. doi: 10.1016/j.neuroimage.2013.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahn YY, Bagrow JP, Lehmann S. Link communities reveal multiscale complexity in networks. Nature. 2010;466(7307):761–764. doi: 10.1038/nature09182. [DOI] [PubMed] [Google Scholar]
- 31.Rosvall M, Bergstrom CT. Maps of random walks on complex networks reveal community structure. Proc Natl Acad Sci USA. 2008;105(4):1118–1123. doi: 10.1073/pnas.0706851105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Damasio H, Frank R. Three-dimensional in vivo mapping of brain lesions in humans. Arch Neurol. 1992;49(2):137–143. doi: 10.1001/archneur.1992.00530260037016. [DOI] [PubMed] [Google Scholar]
- 33.Nelson SM, et al. A parcellation scheme for human left lateral parietal cortex. Neuron. 2010;67(1):156–170. doi: 10.1016/j.neuron.2010.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.