Abstract
Background
HIV transmission risk among non-injection drug users is high due to the co-occurrence of drug use and sexual risk behaviors. The purpose of the current study was to identify patterns of drug use among polysubstance users within a high HIV prevalence population.
Methods
The study sample included 409 substance users from the Pretoria region of South Africa. Substances used by 20% or more the sample included: cigarettes, alcohol, marijuana and heroin in combination, marijuana and cigarettes in combination, and crack cocaine. Latent class analysis was used to identify patterns of polysubstance use based on types of drugs used. Multivariate logistic regression analyses compared classes on demographics, sexual risk behavior, and disease status.
Results
Four classes of substance use were found: MJ+Cig (40.8%), MJ+Her (30.8%), Crack (24.7%), and Low Use (3.7%). The MJ+Cig class was 6.7 times more likely to use alcohol and 3 times more likely to use drugs before/during sex with steady partners than the Crack class. The MJ+Cig class was16 times more likely to use alcohol before/during sex with steady partners than the MJ+Her class. The Crack class was 6.1 times more likely to engage in transactional sex and less likely to use drugs before/during steady sex than the MJ+Her class.
Conclusions
Findings illustrate patterns of drug use among a polysubstance using population that differ in sexual risk behavior. Intervention strategies should address substance use, particularly smoking as a route of administration (ROA), and sexual risk behaviors that best fit this high-risk population.
Keywords: polysubstance use, sexual risk behavior, infectious disease, steady sex partners, route of administration, ROA, HIV population, South Africa
1. INTRODUCTION
Substance use is prevalent among individuals in South Africa where it is estimated that 20% of women and 63% of men suffer from substance use disorders (World Health Organization, 2010). In addition, drug-related activity in South Africa has been associated with poverty, reduced productivity, unemployment, familial dysfunction, political instability, drug-related violence, gang activity, escalating rates of blood-borne illnesses such as acquired immunodeficiency syndrome (AIDS) and tuberculosis (TB), injury, and premature death (Peltzer et al., 2010; Van Wyk, 2011). Furthermore, research has indicated high rates of recent cannabis (85.7%), opiate (56.3%), and cocaine (35.6%) use among substance users in South Africa (Hedden et al., 2009). In addition, studies in sub-Saharan Africa have documented strong links between substance use and sexual risk behavior such as having multiple sex partners, having unprotected sex, and engaging in sex for money and/or gifts (Fisher et al., 2007; Kalichman et al., 2007, 2008; Morojele et al. 2005, 2006; Parry et al., 2009; Roerecke et al., 2008). This is of considerable concern given that South Africa has the world’s largest population of individuals living with HIV (Joint United Nations Programme on HIV/AIDS and World Health Organization, 2009).
Those who currently use illegal drugs rarely limit their use to one substance (Griffin et al., 2009; Kedia et al., 2007) and the increasing prevalence of polysubstance use in South Africa contributes to the already devastating HIV epidemic (Floyd et al., 2010; Kalichman et al., 2006; Wechsberg et al., 2008). In fact, polysubstance use is related to increased diagnosis of sexually transmitted HIV (Mimiaga et al., 2008) and other sexually transmitted infections (STIs; Mayer et al. 2012). In addition to risk for HIV, polysubstance has also been associated with detrimental neuropsychological effects (Verdejo-García et al., 2004, 2010), including impulsivity (Verdejo-García et al., 2010) and deficits in executive functioning (Colzato et al., 2009; Hammers and Suhr, 2010). Polysubstance use is unique in that users may report a primary drug of choice that may differ from the substance causing the most negative outcomes (Griffin et al., 2009). Understanding patterns of drug use is key to developing and implementing appropriate interventions that will maximize recovery and decrease risk among vulnerable populations.
Polysubstance use in South Africa has been cited to be common (Parry et al., 2008a; Floyd et al., 2010) and there is a strong link between substance use, sex trade, and HIV transmission in this region (Parry et al, 2008b; Hedden et al., 2009). Research suggests that the increase in the use of “sugars” in South Africa, low quality heroin and cocaine mixed with marijuana, (Pluddemann et al., 2008), use of cocaine prior to sex work (Hedden et al., 2011) for coping or increased energy (Needle et al., 2008), and heroin and marijuana after sex work for relaxation (Needle et al., 2008; Floyd et al., 2010) contributes to unsafe sex and HIV in South Africa. As the risk of contracting infectious disease may increase with the use of substances (Friedman et al., 2009; Neblet et al. 2011; Pilowsky et al., 2007; Somlai et al., 2000), it is imperative to elucidate patterns of drug use and their associated risk behaviors among this population.
Individuals who use substances are likely to engage in sexual risk behaviors while under the influence of drugs and/or alcohol (Abdala et al., 2010; Sander et al., 2010). One explanation for HIV transmission among non-injection drug users is that intoxication through the use of various substances may lead to a lack of attention to engaging in the practice of safe sex or a propensity toward engaging in high-risk sex (Castor et al., 2010; Strathdee and Sherman, 2003). For example, in a study of mostly African Americans in a high HIV-risk community, drug users were more likely than non-drug users to have multiple sex partners, exchange sex for money or drugs, have a sexual relationship with someone they knew had other sex partners, and use drugs or alcohol at their last sexual experience compared to non-drug users (Kuo et al., 2011), thus increasing the risk of exposure to blood-borne illnesses such as HIV and subsequent transmission of those illnesses. Further, among African American non-injection drug users, having personal networks with a high degree of substance use activities was associated with high-risk sexual behaviors including having multiple partners and having sex without a condom (Miller and Neaigus, 2002). The potential risk of HIV infection among these populations is also compounded by the overlap among network members (Crawford and Vlahov, 2010) and the potential for partnerships to bridge the gap between high risk and low risk members (Neaigus et al., 2001; Volz et al., 2010). These studies show that substance use in general increases the likelihood of sexual risk behaviors, thereby allowing for the possibility of HIV and other STI transmission through unprotected sex.
Although several noteworthy studies have focused on substance use, risk behavior, and HIV infection in South Africa (Floyd et al., 2010; Hedden et al., 2009, 2011; Kalichman et al., 2006; Peltzer et al., 2009; Weschberg et al., 2006), research has yet to examine patterns of substance use and risk among drug users in this population. Despite the high prevalence of substance use and high potential for exposure to, and transmission of, blood-borne illnesses, to our knowledge, no studies have explored patterns of polysubstance use, sexual risk behavior, and infectious disease in this region. The purpose of the current study is to explore patterns of drug use among a primarily polysubstance using population in South Africa. This study addresses a gap in the literature by using Latent Class Analysis (LCA) to identify patterns of polysubstance use and associations between these classes and sexual risk behaviors.
2. METHODS
2.1. Study Site
The current study was part of the international NEURO-HIV Epidemiologic Study that has sites in the United States, South Africa, and Russia. The NEURO-HIV Epidemiologic Study was designed to examine neuropsychological and social-behavioral risk factors of HIV, hepatitis A, hepatitis B, and hepatitis C among both injection and non-injection drug users. The present study is based on baseline data collected in the Pretoria region of South Africa between 2002 and 2006. Pretoria is considered a government center of South Africa and it is part of the Gauteng province with a population of over 8.5 million people. Although Gauteng is considered to be the fastest growing province in the region and contributes to over one-third of the country’s gross national product, the unemployment rate is high (over 25%) with a median annual income of working adults that is just under $3,500 (Joint United Nations Programme on HIV/AIDS and World Health Organization, 2008).
2.2. Participant Demographics
To be eligible for the study, participants had to be between the ages of 18 to 40 years, report using non-injection and/or injection drugs in the past 6 months, and live in or around Pretoria. The age restriction was based on the knowledge that the average life expectancy in South Africa is 54, compared to an average life expectancy in the United States of 78 (World Health Organization, 2012). As such, we chose not to include participants that would be considered relatively elderly, similar to the NEURO study in USA where the maximum age allowed was 50. The present study consisted of 409 drug users comprised of 209 women (50.4%) and 200 men (49.6%). Ninety-four percent of study participants identified as Black (n = 385). The average age of participants was 26.66 years (SD = 4.98). The majority of participants had less than a high school education (78.9%), over one-half of participants had ever been in jail (52.8%), and over one-third were legally employed (36.9%). The complete list of participant demographics can be found in Table 1.
Table 1.
Characteristics of past 6-month substance use among 409 South African drug users
| n | % | |
|---|---|---|
| Latent Class Indicators | ||
| Cigarettes | 389 | 95.1 |
| Marijuana+Cigarette – smoking | 222 | 54.3 |
| Marijuana+Heroin – smoking | 214 | 52.3 |
| Alcohol | 184 | 45.0 |
| Crack Cocaine – smoking | 101 | 24.7 |
| Heroin – smoking, nasal, injection | 23 | 5.6 |
| Marijuana | 17 | 4.2 |
| Heroin+Cigarette – smoking | 3 | 0.7 |
| Demographics | ||
| 24 Years & Older [M = 26.66, SD = 4.98] | 210 | 51.3 |
| Female Sex | 209 | 50.4 |
| Black Race | 385 | 94.1 |
| Less than high school graduate | 323 | 78.9 |
| Legal employment | 151 | 36.9 |
| Ever been in jail | 216 | 52.8 |
| Transactional Sex | 131 | 32.0 |
| Drug Use and Infectious Disease | ||
| Positive for Cannabinoids | 345 | 84.4 |
| Positive for Opioids | 227 | 55.5 |
| Positive for Cocaine | 149 | 36.4 |
| Any 6 STI | 23 | 5.6 |
| Hepatitis C | 17 | 4.2 |
| HIV | 148 | 36.2 |
2.3 Procedures and Instruments
This study was approved by the Institutional Review Board at the Johns Hopkins Bloomberg School of Public Health and in South Africa by the South African Medical Research Ethics Committee. Key investigative study staff completed the Johns Hopkins University training module for conducting research with human subjects. All study staff completed extensive training on conducting the HIV Risk-Behavior Interview and the neuropsychological assessment battery. Study staff also completed a pre- and post-test HIV counseling course. Study staff conducted assessments and counseling session. The project coordinator held regular team meetings and provided additional training and continuous support for assessment clinicians.
Participants were recruited by trained project staff using community-based word of mouth and street outreach in informal settlements, treatment programs, bars, local emergency rooms, and health clinics. The majority of participants ultimately came from street outreach and a minority came from treatment programs and health clinics. Informed consent was obtained at the initial visit prior to the baseline assessment. All assessments in were conducted face-to-face in private rooms at the research clinic site at Louis Pasteur Hospital in Pretoria. Participants were remunerated 150 ZAR (approximately $19) for the baseline assessment and an additional 50 ZAR (approximately $6) for transportation costs.
Participants enrolled in the study completed the HIV-Risk Behavior Interview, a detailed behavioral assessment of drug use and sexual practices. This version was adapted from landmark studies of HIV-risk behavior (Vlahov et al., 1991) and was pilot-tested at the South African site prior to use in the present study. The HIV-Risk Behavior Interview includes measures of drug-related HIV risk behaviors such as drug use cessation and relapse, risky injection practices, and drug use in high-risk contexts. This measure also includes detailed self-report of drug use including: type, route of administration (ROA), frequency, and quantity of drug use. A range of drugs used is included in the study battery such as alcohol, tobacco, cannabis, cocaine, heroin, and methaqualone; however, open-ended questions allow for self-report descriptions of “other” drug use not indicated in the assessment. Measures of sexual behavior include the number of sex partners, types of sex partners, type of sexual acts, condom use behavior, sex trade practices, and sexually transmitted infections. Drug use and sexual risk behaviors were assessed at five different time periods: last 24 hours, last week, last month, last six months, and lifetime. The six-month time frame was utilized in the analyses for the current study.
Blood and urine samples were collected at the baseline assessment to test for the presence of drugs. HIV testing was performed by a national pathology service. HIV testing included the standard enzyme-linked immunosorbent assay (ELISA) screening and confirmatory Western Blots. Urinalysis tested for the presence of psychoactive substances, including: cannabinoids, cocaine, opiates, and methalqualone to verify participant self-report of drug use. Detailed measures of drug use have been described elsewhere (Hedden et al., 2008).
2.4. Measures
2.4.1. Substance use
Participant substance use was assessed using items addressing past 6-month substance use in the HIV-Risk Behavior Interview. Participants responded yes or no to using cigarettes, alcohol, smoking crack cocaine, smoking, injecting or nasal use of heroin, and marijuana use in the past 6 months. Participants were also asked, “Have you smoked any other drug combo in the past 6 months?” Participants responded yes or no and then were asked to specify the drug combination used. The drug combinations that participants listed for this item included: smoking marijuana and cigarettes in combination, smoking marijuana and heroin in combination, and smoking heroin and cigarettes in combination. Injection drug use in the sample was low, with only 4 participants (1.0%) indicating that they had ever injected any drug. Past 6-month drug use is a common duration of time used in substance use research and is often defined as “recent” (e.g., Hedden et al., 2009; Walley et al., 2008). Substances used in the past 6 months are noted in Table 1.
2.4.2. Latent class indicators
Substances used at a 20% prevalence rate or greater were included in the latent class analysis. This method of using a 20% prevalence rate has been utilized in previous studies (Monga et al., 2007; Harrell et al., 2012). Using this criteria five substance use indicators were included in the analysis: cigarettes (95.1%), smoking marijuana and heroin in combination (52.3%), smoking marijuana and cigarettes in combination (54.3%), using alcohol (45.0%), and smoking crack cocaine (24.7%). As can be seen in Table 1, after smoking crack cocaine, the next most prevalent substance was heroin, but this was used by less than 6% of the sample.
2.4.3. Demographics, sexual risk behaviors, and disease status
Demographic variables were used to examine the characteristics of individuals within classes. Dichotomous variables were used for race (1 = Black), sex (1 = female), education (1 = high school diploma/GED or greater), employment (1 = income from legal employment), and jail (1 = ever been incarcerated). Previous research has indicated these factors are associated with substance use and infectious disease among this population. General sexual risk behaviors included condom use at last sex and transactional sex. Transactional sex is defined as ever having traded sex for money or drugs (Floyd et al., 2010; Hedden et al., 2009, 2011). Specific sexual risk behaviors were identified with steady and casual partners that included alcohol use before or during sex and drug use before or during sex. A casual sex relationship is defined as having sex with a partner one has known for less than three months and a steady sex relationship is defined as having sex with a partner one has known for greater than three months. Urinalysis results included cannabinoids, opioids, and cocaine. Disease status for HIV and hepatitis C was determined by blood sample screening. The presence of sexually transmitted infections (STIs), including: gonorrhea, syphilis, chlamydia, genital herpes, genital warts, or trichomoniasis were recorded via self-report. This variable was collapsed into one and a dichotomous variable was created for the presence of any 6 STI’s (1 = any 6 STIs).
2.5. Statistical analysis
All analyses were performed using Mplus 6.0 and SPSS 18.0. Descriptive statistics, frequencies, and percentages were used to demonstrate the characteristics of the sample. Latent class analysis (LCA) is a method of data reduction used to identify groupings of individuals that illustrate similar patterns or profiles of behavior (McCutcheon, 1987). This method of analysis is gaining popularity among substance abuse researchers (Harrell et al., 2011; Monga et al., 2007; Schwartz et al., 2010).
In the current study, LCA was used to identify patterns of drug use behaviors among recent drug users in Pretoria, South Africa. Because the number of classes was unknown, 5 drug use indicator variables were entered into the LCA model beginning with one class and adding classes incrementally to 6 classes. Each model was tested for fit using 3 separate measures. The Bayesian Information Criteria (BIC) is interpreted such that the lowest value is considered the best fit (Schwarz, 1978). The Lo-Mendell-Rubin adjusted likelihood ratio test (LMR; Lo et al., 2001) and the parametric bootstrap likelihood ratio test (BLRT; McLachlan and Peel, 2000) both provide comparisons between models, such that significant values indicate the model is an improved fit over the model with less classes. Entropy values were also used to evaluate the quality of classes indicated. Entropy values range from 0 to 1 with values closer to 1 representing better quality and separation of classes (Ramaswamy et al., 1993). Entropy is not used as a measure of fit, however lower entropy values associated with a given model may show that the model is not illustrating groups with uniquely separate characteristics. Meaningfulness of patterns of drug use was also considered in the selection of the final class structure.
As mentioned above, 5 drugs and/or combinations of drugs were used as indicator variables that met the criterion of greater than 20% prevalence. All models were estimated using maximum likelihood and a minimum of 500 random starts was used to ensure that global maxima was reached (Mplus 6.0; Muthén and Muthén, 2010). If necessary, the number of starts was increased until the log likelihood was replicated a minimum of five times. Mplus uses a full information maximum likelihood estimation and assumes data is missing at random (Hogan et al., 2004; Schafer and Graham, 2002). Covariance coverage ranged from 0.900–0.993, well over minimum thresholds for adequate coverage (Muthén and Muthén, 2010).
2.6. Class associations
Once the appropriate number of classes was determined, a series of associations were examined between class membership and demographic variables as well as the variables of interest. Classes were assigned using most likely class membership (Kuramoto et al., 2011). Multivariate logistic regression analyses were conducted using SPSS 18 (PASW, 2010) to illustrate associations between class membership and variables listed in Section 2.2.3. Associations were adjusted for age, sex, and race. Logistic regression models were also conducted using posterior possibilities in Mplus. Findings for this analysis were similar to those found using the most likely class membership approach.
3. RESULTS
3.1. Class membership
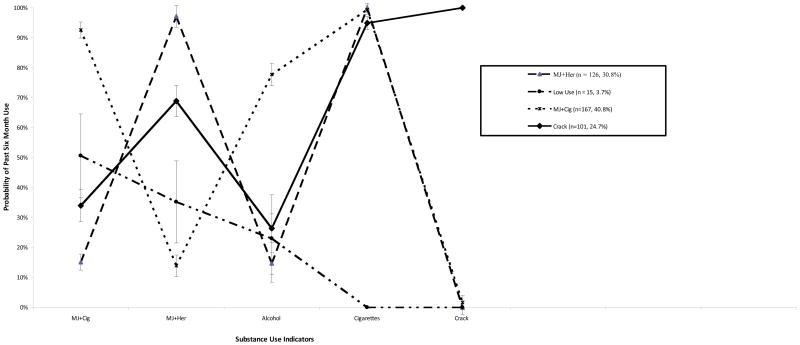
A summary of fit statistics can be found in Table 2. Fit statistics for LCA models specifying 2, 3, 4, and 5 classes were examined (Goodman, 1974). Monte Carlo simulations suggest that a BLRT fares best overall in LCA (Nylund et al., 2007). In the current analysis, the BLRT was statistically significant for classes 2, 3, and 4 (all p < 0.001). In this case, additional fit statistics were used to help identify the number of classes that represent the best fit to the data. Although the lowest BIC was associated with a 2-class model (BICs: baseline = 2340.00, two-class = 2133.49, three-class = 2144.63, four-class = 2166.65, five-class = 2197.20) the difference between BIC scores for 2, 3, and 4 classes was small. This may not be sufficient evidence for selecting a 2-class solution (Raferty, 1995; Monga et al., 2007). The 4-class solution showed improvement over the baseline solution and had a statistically significant LMR test (LL = 1014.17, p < 0.008). A higher entropy value of 0.92 for a 4-class solution compared to the 3-class solution (0.64) was also considered in the final class selection. As mentioned above, an entropy value closer to 1.0 indicates greater classification quality. Finally, the 4-class solution was chosen for meaningfulness, simplicity of interpretation, and context specific epidemiology. The resultant class names are reflective of the highest prevalence of substance use in the group besides cigarettes, due to the ubiquity of cigarette use (used by over 95% of the sample). This practice of naming classes has been utilized in other studies using LCA in substance use research (Harrell et al., 2012; Kuramoto et al., 2011). A complete list of estimated probabilities for classes can be found in Table 3. Figure 1 displays a graphical depiction of substance use by latent class.
Table 2.
Fit statistics and entropy for a latent class analysis of 5 substances used in the past 6 months among 409 South African drug users
| Classes | LLa | parameters | BICb | LMRc | BLRTd | Entropy | s.c. r.f. (f)e |
|---|---|---|---|---|---|---|---|
| 1 | −1154.97 | 5 | 2340.00 | NAf | NAf | NAf | NAf |
| 2 | −1033.67 | 11 | 2133.49 | p < .001 | p < .001 | .755 | .39 (160.3) |
| 3 | −1021.20 | 17 | 2144.63 | p = .003 | p < .001 | .638 | .26 (104.9) |
| 4 | −1014.17 | 23 | 2166.65 | p = .008 | p < .001 | .921 | .03 (14.0) |
| 5 | −1011.40 | 29 | 2197.20 | p = .107 | p = 1.00 | .848 | .01 (4.9) |
Log Likelihood;
Bayesian Information Criteria;
Lo-Mendell-Rubin adjusted likelihood ratio test;
parametric Bootstrap Likelihood Ratio Test;
smallest class relative frequency (frequency);
Not Applicable
Table 3.
Estimated probabilities (with standard errors) of past 6 month drug use from the 4-class most likely class membership.
| Drug and Route of Administration | Class 1 MJ+Cigs (40.8%) n=167 | Class 2 MJ+Her (30.8%) n=126 | Class 3 Crack (24.7%), n=101 | Class 4 Low Use (3.7%) n=15 |
|---|---|---|---|---|
| Marijuana and cigarettes | 92.6 (2.7) | 15.1 (4.6) | 34.0 (5.4) | 50.6 (14.0) |
| Marijuana and heroin | 13.9 (3.6) | 97.1 (2.9) | 68.9 (5.2) | 35.2 (13.7) |
| Alcohol | 77.7 (3.7) | 23.0 (3.8) | 26.4 (4.8) | 23.0 (14.6) |
| Cigarettes alone | 99.4 (1.5) | 100.0 (0.0) | 94.9 (2.2) | 0.0 (0.0) |
| Crack | 2.4 (1.6) | 0 (0.0) | 100.0 (0.0) | 0.0 (0.0) |
Figure 1.
Four class solution of a latent class analysis of 409 polysubstance users in Pretoria, South Africa. Estimated probabilities for past six-month drug use are graphed based on latent class membership.
Class 1 consisted of 40.8% (n = 167) of the sample. The use of marijuana and cigarettes had the highest probability in this class (92.6%). Members of this class also had a 13.9% probability of smoking marijuana and heroin together, 77.7% drank alcohol, all smoked cigarettes alone, and none smoked crack. This class is labeled “MJ+Cig.”
Class 2 consisted of 30.8% (n = 126) of the sample. Besides cigarettes, the greatest substance use in this class was smoking marijuana and heroin together (97.1%). Members of this class also had a probability of 15.1% for smoking marijuana and cigarettes, 23.0% for using alcohol, 100% for smoking cigarettes alone, and no crack use. This class is labeled “MJ+Her.”
Class 3 consisted of 24.7% (n = 101) of the sample. All members of this class smoked crack (100%). Additional substance use probabilities in this group were as follows: 34.0% smoked marijuana and cigarettes, 68.9% smoked marijuana and heroin, 26.4% drank alcohol, and 94.9% smoked cigarettes. This class is labeled “Crack.”
Class 4 consisted of 3.7% (n = 15) of the sample. The highest substance use in this class was smoking marijuana and cigarettes together (50.6%), followed by marijuana and heroin (35.2%) and alcohol use (23.0%) with 0% probabilities of cigarettes or crack alone. This class is labeled “Low Use.” Due to the size of this class sample, the “Low Use” class was not included in the class associations analyses. To address concerns regarding the “Low Use” class, we re-ran the analysis including only cigarette smokers. As expected, we found that a 3-class solution provided the best fit, as determined by BIC, LMR, and BLRT. The remaining 3 classes, similar to the 4-class solution, included a class with high probability for marijuana and cigarettes usage, a class with high probability for marijuana and heroin usage, and a class with high probability for crack usage.
3.2 Characteristics of classes
Associations between latent class membership and characteristics of drug users can be found in Table 4.
Table 4.
Associations between latent class membership and characteristics of drug users in Pretoria, South Africa1
| MJ+Cig vs. Crack2 | MJ+Cig vs. MJ+Her2 | Crack vs. MJ+Her2 | |
|---|---|---|---|
| Demographics | |||
| Black race | 1.10 (0.41–3.01) | 0.74 (0.26–2.08) | 0.52 (0.16–1.67) |
| Female Sex | 0.45 (0.27–0.76)** | 0.96 (0.60–1.54) | 2.23 (1.28–3.89)** |
| 24 years and older | 0.80 (0.48–1.33) | 1.57 (0.98–2.51)† | 2.13 (1.23–3.67)** |
| Education | 0.69 (0.38–1.27) | 0.92 (0.51–1.67) | 1.40 (0.73–2.68) |
| Employment | 4.17 (0.50–34.48) | -- | -- |
| Jail | 3.09 (1.78–5.37)*** | 0.42 (0.51–1.33) | 2.58 (1.44–4.63)*** |
| Drug Use Urinalysis | |||
| Positive for cannabinoids | 0.42 (0.21–0.86) | 0.20 (0.08–0.47)*** | .44 (0.16–1.21) |
| Positive for opioids | 0.06 (0.03–0.13)*** | 0.06 (0.03–0.11)*** | .75 (0.37–1.52) |
| Positive for cocaine | 0.02 (0.01–0.04)*** | 0.22 (0.12–0.41)*** | 10.67 (5.35–21.26)*** |
| Sex Risk Behaviors3 | |||
| Consistent condom use | 0.84 (0.49–1.46) | 1.32 (0.78–2.25) | 1.55 (0.84–2.85) |
| Condom at last sex | 0.64 (0.37–1.12) | 1.16 (0.72–1.87) | 1.74 (0.97–3.15)† |
| Transactional sex | 0.17 (0.08–0.36)*** | 0.95 (0.47–1.90) | 6.12 (2.59–14.46) |
| Steady partner | |||
| Alcohol before/during sex | 6.65 (2.80–15.78)*** | 16.00 (5.43–47.18)*** | 2.69 (0.72–10.07) |
| Drug use before/during sex | 2.99 (1.44–6.22)** | 1.28 (0.63–2.59) | 0.44 (0.21–0.93)* |
| Casual partner | |||
| Alcohol before/during sex | 5.23 (0.93–29.50)† | -- | -- |
| Drug use before/during sex | -- | -- | -- |
| Disease Status | |||
| Any 6 STD | 0.69 (0.22–2.20) | 1.16 (0.42–3.20) | 1.61 (0.45–5.68) |
| Hepatitis C | 0.33 (0.07–1.46) | 0.55 (0.13–2.33) | 1.53 (0.30–7.91) |
| HIV | 0.78 (0.45–1.35) | 0.89 (0.52–1.52) | 1.14 (0.64–2.03) |
Associations are given as adjusted odds ratios with 95% confidence intervals in parentheses.
Indicates reference class within column associations. Adjusted for age, sex, and race.
Refers to past 6 month behavior;
p < .10;
p < .05;
p < .01;
p < .001.
3.2.1. Demographics
Latent classes were compared on demographics, urinalysis, sexual risk behavior, and disease status. Significant differences were found between classes on all but three demographic characteristics: race, education, and jail. Individuals in the MJ+Cig class were less likely to be female and 3 times more likely to have been in jail than the Crack class. Individuals in the MJ+Cig class were 1.6 times more likely to be over 24 years old than individuals in the MJ+Her class. Individuals in the Crack class were 2.2 times more likely to be female, 2.1 times more likely to be older than 24, and 2.6 times more likely to have spent time in jail compared to the MJ+Her class.
3.2.2. Drug use urinalysis
Results from urinalyses were used to verify self-report of drug use and, thereby class membership. Individuals in the MJ+Cigcl ass were less likely to test positive for opioids and cocaine than the Crack class. The MJ+Cig class was less likely to test positive for cannabinoids, opioids, and cocaine than the MJ+Her group. Lastly, individuals in the Crack group were 10.7 times more likely to test positive for cocaine than the MJ+Her group.
3.2.3. Sexual risk behaviors
Compared to the Crack class, the MJ+Cig class was less likely to have engaged in transactional sex. The MJ+Cig group was 6.7 times more likely to use alcohol before or during sex with steady partners, and 3 times more likely to use drugs before or during sex with steady partners than the Crack group. The MJ+Cig group was 16 times more likely to use alcohol before or during sex with steady partners compared to the MJ+Her class.
Individuals in the Crack group were 1.7 times more likely to use a condom at last sex than the MJ+Her group and were 6.1 times more likely to engage in transactional sex. The Crack group was less likely to use drugs before or during sex with steady partners than the MJ+Her group.
The MJ+Cig class was 5.2 times more likely to use alcohol before or during casual sex than the Crack class. Regression analyses were considered for the remainder of comparisons among casual partners, however these associations could not be successfully conducted due the low response rates within these variables.
3.2.4. Disease status
The prevalence rates of HIV, hepatitis C, and any 6 STIs in the current study were 36.2% (n = 148), 4.2% (n = 17), and 5.6% (n = 23) respectively. No significant associations were found between classes and disease status in the current study population.
4. DISCUSSION
4.1. Review of major findings
As several studies have used LCA among populations of substance users in the United States (Harrell et al., 2012; Kuramoto et al., 2011; Schwartz et al. 2010), to our knowledge the current study is the first of its kind to identify patterns of polysubstance use among drug users in the Pretoria region of South Africa as well as the first study to examine risk factors associated with HIV exposure and possible transmission. Applied to the current study, the use of latent class analysis illustrates the degree and kind of substance use in this population.
With respect to sexual risk behaviors, the Crack group was more likely to engage in transactional sex than both the MJ+Cig group and MJ+Her group, yet they are also more likely to use condoms at last sex compared the MJ+Her group. This finding supports previous research that identifies successful outcomes in educational interventions that target increasing condom use among high-risk populations. Specifically, Hedden et al. (2011) found that women in South Africa who traded sex were more likely to use condoms at last sex than at their first sexual encounter. However, the MJ+Cig group was more likely to use alcohol before or during sex with casual partners than the Crack group. Research has noted the importance of considering coping strategies and psychosocial factors among South Africans related to substance use and sexual risk behavior, particularly among sex workers (Floyd et al., 2010; Needle et al., 2008).
One intriguing finding in the current study is that drug and/or alcohol use before or during sex with a steady partner may be an area of intervention that needs closer attention. Specifically, individuals in the MJ+Cig group were significantly more likely to use alcohol before or during sex with steady partners than both the Crack and MJ+Her group. In addition, individuals in the MJ+Cig and MJ+Her group were more likely to use drugs before or during sex with steady partners than the Crack group. As previous work has identified the possible success of educational interventions that target sex workers in South Africa (Hedden et al., 2011), the current study suggests that interventions be tailored to substance users who do not engage in transactional sex, but engage in high-risk behaviors with steady partners. For example, the MJ+Cig group was less likely to engage in transactional sex than the Crack group, but more likely to use alcohol and drugs before/during steady sex and more likely to use alcohol before or during casual sex than the Crack group. Likewise, the MJ+Cig group was more likely to use alcohol before/during steady sex than the MJ+Her group. Taken together, these findings indicate that interventions should target substance users who are not engaging in transactional sex.
Interestingly, because sexual risk behavior in the current study occurs with steady partners, it may indicate that individuals feel “safe” when having sex with these partners. That is, if an individual comes to the conclusion that his or her current sexual partner is “safe” he or she may be more open to engaging in high risk sexual behaviors such as unprotected sex and alcohol use before or during sex, all of which increase the likelihood of exposure to blood-borne illnesses such as HIV. This may be particularly true of individuals in steady relationships. For example, in a study of serodiscordant couples, those who reported recent substance use were over two times as likely to have had unprotected sexual episodes than couples where both partners did not report recent substance use. In addition, drug dependent partners were three and half times more likely to engage in recent unprotected sexual episodes than in couples where neither partner was drug dependent (National Institute of Mental Health Study, 2010). This behavior is troublesome given the risk of HIV transmission among substance users in a region where rates of HIV infection are high.
The current study not only indicates patterns of substance use among this population, but also identifies the most common ROA for illicit drugs use as smoking their substance of choice. This finding is consistent with others who have noted smoking as the most common ROA of illicit drug use in South Africa (Parry et al., 2002). More specifically, almost all participants (95.1%) in the current study reported smoking cigarettes alone. This is of notable concern given that smoking among substance abusers is associated with substantial adverse outcomes including respiratory, cardiovascular, nose-throat, and gastrointestinal complaints, as well as higher rates of mortality (Hser et al., 1994; Hurt et al., 1996; Patkar et al., 2005, 2002). Not only do these findings suggest that substance use intervention programs should target smoking cessation, but that the intervention should be targeted toward the specific substances used in combination. For example, an intervention designed to reduce smoking among MJ+Cig users may look different from a smoking reduction intervention for MJ+Her or Crack users with the latter including more emphasis on the reduction of more deleterious drug use such as heroin and crack.
Lastly, the LCA illustration in the current study can be used to inform interventions that specifically address the needs of these polysubstance users. Due to the strong link between substance use and sexually transmitted diseases, these findings have important implications for HIV primary and secondary transmission prevention interventions, especially in a part of the world that contains the greatest number of individuals living with HIV/AIDS. In South Africa the most prevalent transmission route of HIV is through heterosexual sex (Chopra et al., 2009; Heymann and Edstrom, 1991; Hunter, 1993). Given that substance use results in reductions in protective behaviors during sex, risk for transmission is elevated. Given these study findings, more work is needed to address sexual risk behaviors, specifically the use of substances before or during sex, among steady partners in this population.
4.2. Limitations and strengths
The current study is the first of its kind to identify patterns of substance use among a high-risk and often hard to reach sample. Although the current study offers valuable contributions to the literature, there are several limitations that must be noted. First, the current study is cross-sectional in nature and as such conclusions regarding causality or temporal order of variables investigated here should be reserved for longitudinal or experimental designs. Second, the current study used community-based sampling and word of mouth to recruit participants. This approach may result in non-random sampling and as a result has limited generalizability. In addition, the use of self-report for STIs other than HIV may result in an under-representation of the actual incidence of STIs in the sample. The findings discussed here may only be applicable to similar drug using populations in comparable regions of South Africa. In particular, smoking cigarettes and smoking as a ROA is ubiquitous in the current study sample and findings here have limited generalizability to samples where smoking is not the ROA.
It must also be noted that the latent class structure that is illustrated in the current study is subject to interpretation and is not absolute in nature. Alternate decision-making in inclusion variables may result in a different pattern of class structure. In addition, LCA assumes that the variables included in each class are independent of one another and, in fact, this may not be the case. For example, someone who smokes marijuana and cigarettes together may be more likely to smoke other substances together such as marijuana and heroin. However, LCA is a useful method for identifying patterns of behavior and indicate where further study is needed. Lastly, the multivariate regression analysis used here does not eliminate the possibility of intercorrelations influencing the associations between classes. It is noted that a multinomial logistic regression analysis is superior to the current design, but may be best suited to a sample with larger class sizes. Notwithstanding these study limitations, the current study has several strengths including the use of urinalyses to verify self-report of recent drug use among high-risk individuals drawn from a hard to reach population of polysubstance users in South Africa, an area of limited research knowledge.
4.3. Implications
The use of LCA in this population at high-risk for HIV helps to identify patterns of substance use in need of further targeted intervention programs. Specifically, the findings described in the current study suggest that substance use before or during sex with steady partners may be associated with reductions in protective behaviors among vulnerable populations. Future longitudinal research should address this concern to explore the possibility of causal relationships. Findings also indicate that among this population of polysubstance users, smoking is the most common route of administration and should be targeted as a means to potentially reduce the overall appeal of substance use.
Acknowledgments
Role of funding source
This research was funded by a grant awarded to William Latimer from NIDA’s Southern Africa Initiative as a supplement to the parent study conducted in the United States (R01DA014498). This research was also supported by the Drug Dependence and Epidemiology Training Grant (T32DA007292).
The authors are appreciative of their postdoctoral appointments–past and present–in the Drug Dependence and Epidemiology Training Program at the Johns Hopkins Bloomberg School of Public Health. The first author would especially like to thank Dr. William Latimer for his continued mentorship and Mercy College for their support of faculty scholarship.
Biographies
Michael Scherer, Alexandra Duncan, Paul Harrell, Department of Mental Health, Johns Hopkins University, Bloomberg School of Public Health, Department of Mental Health, 624 N. Broadway, 8th Floor, 895, Baltimore, Maryland, 21205
Anne Gloria Moleko, Department of Psychology, University of Pretoria, Private bag X20, Hatfield, Pretoria 0028
William W. Latimer, Department of Clinical and Health Psychology, College of Public Health and Health Professions, University of Florida, 101 S. Newell Drive, Room 3151, Gainesville, FL 32611
Footnotes
Contributors
Rebecca Trenz conducted the latent analysis, wrote the results section, and incorporated contributions from the authors in the first draft of the manuscript. Michael Scherer conducted the regression analysis and contributed to the introduction section. Paul Harrell conceptualized the original study design and helped structure the initial latent class analysis. Alexandra Duncan and Paul Harrell contributed to the introduction and discussion sections. William Latimer was the principal investigator of the study. All authors reviewed and assisted with revisions for the final manuscript.
Conflict of interest
The authors have no conflict of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abdala N, White E, Toussova OV, Krasnoselskikh TV, Verevochkin S, Kozlov AP, Heimer R. Comparing sexual risks and patterns of alcohol and drug use between injection drug users (IDUs) and non-IDUs who report sexual partnerships with IDUs in St. Petersburg, Russia BMC Public Health. 2010;10:676. doi: 10.1186/1471-2458-10-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castor D, Pilowsky DJ, Hadden B, Fuller C, Ompad D, de Leon CL, Neils G, Hoepner L, Andrews HF, Latkin C, Hoover DR. Sexual risk reduction among non-injection drug users: report of a randomized trial. AIDS Care. 2010;22:62–70. doi: 10.1080/09540120903012510. [DOI] [PubMed] [Google Scholar]
- Chopra M, Townsend L, Johnston L, Mathews C, Tomlinson M, O’bra H, Kendall C. Estimating HIV prevalence and risk behaviors among high-risk heterosexual men with multiple sex partners: use of respondent-driven sampling. J Acquir Immune Defic Syndr. 2009;51:72–77. doi: 10.1097/QAI.0b013e31819907de. [DOI] [PubMed] [Google Scholar]
- Colzato LS, Huizinga M, Hommel B. Recreational cocaine polydrug use impairs cognitive flexibility but not working memory. Psychopharmacol (Berl) 2009;207:225–234. doi: 10.1007/s00213-009-1650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford ND, Vlahov D. Progress in HIV reduction and prevention among injection and non-injection drug users. J Acquir Immune Defic Syndr. 2010;55:S84–S87. doi: 10.1097/QAI.0b013e3181fbca5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34:856–863. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- Floyd LJ, Hedden S, Lawson A, Salama C, Moleko AG, Latimer W. The association between poly-substance use, coping, and sex trade among black South African substance users. Subst Use Misuse. 2010;45:1971–1987. doi: 10.3109/10826081003767635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Stall R, Kidder DP, Henny KD, Courtenay-Quirk C, Aidala A, Royal S, Holtgrave DR The Project START Study Group. Associations between substance use, sexual risk taking and HIV treatment adherence among homeless people living with HIV. AIDS Care. 2009;21:692–700. doi: 10.1080/09540120802513709. [DOI] [PubMed] [Google Scholar]
- Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable model. Biometrika. 1974;61:215–231. [Google Scholar]
- Griffin ML, Kolodziej ME, Weiss RD. Measuring principal substance of abuse in comorbid patients for clinical research. Addict Behav. 2009;34:826–829. doi: 10.1016/j.addbeh.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammers DB, Suhr JA. Neuropsychological, impulsive personality, and cerebral oxygenation correlates of undergraduate polysubstance use. J Clin Exp Neuropsychol. 2010;32:599–609. doi: 10.1080/13803390903379599. [DOI] [PubMed] [Google Scholar]
- Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2011;122:220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Hulbert A, Cavanaugh CE, Parry CD, Moleko AG, Latimer WW. Alcohol, drug and sexual risk behavior correlates of recent transactional sex among female Black South African drug users. J Subst Use. 2011;16:57–67. doi: 10.3109/14659891003721141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Whitaker D, Floyd L, Latimer W. Gender differences in the prevalence and behavioral risk factors of HIV in South African drug users. AIDS Behav. 2009;13:288–296. doi: 10.1007/s10461-008-9467-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann DL, Edström K. Strategies for AIDS prevention and control in sub-Saharan Africa. AIDS. 1991;5:S197–208. [PubMed] [Google Scholar]
- Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med. 1994;23:1455–1497. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Prev Med. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- Hunter DJ. AIDS in sub-Saharan Africa: the epidemiology of heterosexual transmission and the prospects for prevention. Epidemiology. 1993;4:63–72. [PubMed] [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, Melton LJ. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA. 1996;10:1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in cape town, South Africa. Am J Drug Alcohol Abuse. 2007;3:687–698. doi: 10.1080/00952990701522716. [DOI] [PubMed] [Google Scholar]
- Kalishman SC, Simbayi L, Jooste S, Vermaak R, Cain D. Sensation seeking and alcohol use predict HIV transmission risks: prospective study of sexually transmitted infection clinic patients, Cape Town, South Africa. Addict Behav. 2008;33:1630–1633. doi: 10.1016/j.addbeh.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kagee A, Toefy Y, Jooste S, Cain D. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med. 2006;62:1641–1649. doi: 10.1016/j.socscimed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Kedia S, Sell MA, Relyea G. Mono- versus polydrug abuse patterns among publicly funded clients. Subst Abuse Treat Prev Policy. 2007;2:33. doi: 10.1186/1747-597X-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo I, Greenberg AE, Magnus M, Phillips G, Rawls A, Peterson J, Hamilton F, West-Ojo T, Hader S. High prevalence of substance use among heterosexuals living in communities with high rates of AIDS and poverty in Washington, DC. Drug Alcohol Depend. 2011;117:139–144. doi: 10.1016/j.drugalcdep.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Kuramoto SJ, Bohnert AS, Latkin CA. Understanding sub-types of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011;215:237–243. doi: 10.1016/j.drugalcdep.2011.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Mayer KH, Bush T, Henry K, Overton ET, Hammer J, Richardson J, Wood K, Conley L, Papp J, Caliendo AM, Patel P, Brooks JT, SUN Investigators. Ongoing sexually transmitted disease acquisition and risk-taking behavior among US HIV-infected patients in primary care: implications for prevention interventions. Sex Trans Dis. 2012;39:1–7. doi: 10.1097/OLQ.0b013e31823b1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCutcheon AL. Latent Class Analysis. Sage Publications; Thousand Oaks, CA: 1987. [Google Scholar]
- McLachlan GJ, Peel D. Finite Mixture Models. John Wiley and Sons; New York: 2000. [Google Scholar]
- Miller M, Neaigus A. Sex partner support, drug use and sex risk among HIV-negative noninjecting heroin users. AIDS Care. 2002;14:801–813. doi: 10.1080/0954012021000031877. [DOI] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Vanderwarker R, Gaucher MJ, O’Connor CA, Medeiros MS, Safren SA. Polysubstance use and HIV/STD risk behavior among Massachusetts men who have sex with men accessing Department of Public Health mobile van services: implications for intervention development. AIDS Patient Care STDS. 2008;22:745–51. doi: 10.1089/apc.2007.0243. [DOI] [PubMed] [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, Noel L, Tyndall M, Wild C, Leri F, Fallu JS, Bahl S. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CD, Nkowane AM, Moshia KM, Saxena S. Alcohol use and sexual risk behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med. 2006;62:217–227. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 6. Muthen and Muthen; Los Angeles, CA: 2010. [Google Scholar]
- Neaigus A, Miller M, Friedman SR, Des Jarlais DC. Sexual transmission risk among noninjecting heroin users infected with human immunodeficiency virus or hepatitis C virus. J Infect Dis. 2001;184:359–363. doi: 10.1086/322020. [DOI] [PubMed] [Google Scholar]
- Neblett RC, Davey-Rothwell M, Chandler G, Latkin CA. Social network characteristics and HIV sexual risk behavior among urban African American women. J Urban Health. 2011;88:54–65. doi: 10.1007/s11524-010-9513-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needle R, Kroeger K, Belani H, Achrekar A, Parry CD, Dewing S. Sex, drugs, and HIV: rapid assessment of HIV risk behaviors among street-based drug using sex workers in Durban, South Africa. Soc Sci Med. 2008;67:1447–1455. doi: 10.1016/j.socscimed.2008.06.031. [DOI] [PubMed] [Google Scholar]
- Nyland KL, Asparoutiov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Eq Model. 2007;14:535–569. [Google Scholar]
- Parry CD, Bhana A, Pluddemann A, Myers B, Siegfried N, Morojele NK, Flisher AJ, Kozel NJ. The South African community epidemiology network on drug use (SACENDU): description, findings (1997–1999) and policy implications. Addiction. 2002;97:969–976. doi: 10.1046/j.1360-0443.2002.00145.x. [DOI] [PubMed] [Google Scholar]
- Parry CD, Carney T, Peterson P, Dewing S, Needle R. HIV-risk behavior among injecting or non-injecting drug users in Cape Town, Durban, and Pretoria, South Africa. SAHARA J. 2009;5:113–119. [Google Scholar]
- Parry CD, Dewing S, Petersen P, Carney T, Needle R, Kroeger K. Rapid assessment of HIV risk behavior in drug using sex workers in three cities in South Africa. AIDS Behav. 2008a;13:849–859. doi: 10.1007/s10461-008-9367-3. [DOI] [PubMed] [Google Scholar]
- Parry C, Petersen P, Carney T, Dewing S, Needle R. Rapid assessment of drug use and sexual HIV risk patterns among vulnerable drug-using populations in Cape Town, Durban, and Pretoria, South Africa. SAHARA J. 2008b;5:113–119. doi: 10.1080/17290376.2008.9724909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patkar AA, Batra V, Mannelli P, Evers-Casey S, Vergare MJ, Leone FT. Medical symptoms associated with tobacco smoking with and without marijuana abuse among crack cocaine-dependent patients. Am J Addict. 2005;14:43–53. doi: 10.1080/10550490590899844. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Sterling RC, Leone FT, Lundy A, Weinstein SP. Relationship between tobacco smoking and medical symptoms among cocaine-, alcohol-, and opiate-dependent patients. Am J Addict. 2002;11:209–218. doi: 10.1080/10550490290087974. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Ramlagan S, Johnson BD, Phaswana-Mafuya N. Illicit drug use and treatment in South Africa: a review. Subst Use Misuse. 2010;45:2221–2243. doi: 10.3109/10826084.2010.481594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Simbayi L, Kalichman S, Jooste S, Cloete A, Mbelle N. Drug use and HIV risk behavior in three urban South African communities. J Soc Sci. 2009;18:143–149. [Google Scholar]
- Pilowsky DJ, Hoover D, Hadden B, Fuller C, Ompad D, Andrews HF, De Leon CL, Hoepner L, Xia Q, Latkin C. Impact of social network characteristics on high-risk sexual behaviors among non-injection drug users. Subst Use Misuse. 2007;42:1629–1649. doi: 10.1080/10826080701205372. [DOI] [PubMed] [Google Scholar]
- Pluddemann A, Parry C, Bhana A. Alcohol and Drug Abuse Trends: July–December 2007 (phase 23) South African Community Epidemiology Network on Drug Use and Alcohol Drug Abuse Research Unit, Medical Research Council; Cape Town: 2008. pp. 1–2. (SACENDU) Update. [Google Scholar]
- Raferty AE. Bayesian model selection in social research (with discussion by Andrew Gelman, Donald B. Rubin and Robert M. Hauser) In: Marsden PV, editor. Social Methodology. Blackwells; Oxford: 1995. pp. 111–196. [Google Scholar]
- Ramaswamy V, Desarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS Data. Market Sci. 1993;12:103–124. [Google Scholar]
- Roerecke M, Obot I, Patra J, Rehm J. Volume of alcohol consumption, patterns of drinking, and burden of disease in sub-Saharan Africa. Afr J Drug Alcohol Stud. 2008;7:1–16. [Google Scholar]
- Sander PM, Colea SR, Ostrowb DG, Mehtac SH, Kirkc GD. Determinants of alcohol consumption in HIV-uninfected injection drug users. Drug Alcohol Depend. 2010;111:173–176. doi: 10.1016/j.drugalcdep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Somlai AM, Kelly JA, Heckman TG, Hackl K, Runge L, Wright C. Life optimism, substance use, and AIDS-specific attitudes associated with HIV risk behavior among disadvantaged innercity women. J Womens Health Gend Based Med. 2000;9:1101–1111. doi: 10.1089/152460900446018. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80:iii7–iii14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- Schwartz B, Wetzler S, Swanson A, Sung SC. Subtyping of substance use disorders in a high-risk welfare-to-work sample: a latent class analysis. J Subst Abuse Treat. 2010;38:366–374. doi: 10.1016/j.jsat.2010.03.001. [DOI] [PubMed] [Google Scholar]
- The NIMH Multisite HIV/STD Prevention Trial for African American Couples Group. The contribution of male and female partners’ substance use to sexual risks and STDs among African American serodiscordant couples. AIDS Behav. 2010;14:1045–1054. doi: 10.1007/s10461-010-9695-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS and WHO. Report on the Global AIDS Epidemic. Joint United Nations Programme on HIV/AIDS and World Health Organization; Geneva: 2010. [Google Scholar]
- Van Wyk C. The burden of disease: substance abuse in South Africa. Afr J Psychiatry. 2011;14:80. [Google Scholar]
- Verdejo-García A, Del Mar Sánchez-Fernández M, Alonso-Maroto LM, Fernández-Calderón F, Perales JC, Lozano O, Pérez-García M. Impulsivity and executive functions in polysubstance-using rave attenders. Psychopharmacology. 2010;210:377–92. doi: 10.1007/s00213-010-1833-8. [DOI] [PubMed] [Google Scholar]
- Verdejo-García A, López-Torrecillas F, Giménez CO, Pérez-García M. Clinical implications and methodological challenges in the study of the neuropsychological correlates of cannabis, stimulant, and opioid abuse. Neuropsychol Rev. 2004;14:1–41. doi: 10.1023/b:nerv.0000026647.71528.83. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Anthony JC, Celentano D, Solomon L, Chowdhury N. Trends of HIV-1 risk reduction among initiates into intravenous drug use 1982–1987. Am J Drug Alcohol Abuse. 1991;17:39–48. doi: 10.3109/00952999108992808. [DOI] [PubMed] [Google Scholar]
- Volz E, Frost SDW, Rothenberg R, Meyers LA. Epidemiological bridging by injection drug use drives an early HIV epidemic. Epidemics. 2010;2:155–164. doi: 10.1016/j.epidem.2010.06.003. [DOI] [PubMed] [Google Scholar]
- Walley AY, Cheng DM, Libman H, Nunes D, Horsburgh CR, Saitz R, Samet JH. Recent drug use, homelessness and increased short-term mortality in HIV-infected persons with alcohol problems. AIDS. 2008;22:415–420. doi: 10.1097/QAD.0b013e3282f423f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Karg RS, Young S, Rodman N, Myers B, Parry C. Alcohol, cannabis, and methamphetamine use and other risk behaviors among black and coloured South African women: a small randomized trial in the Western Cape. Int J Drug Policy. 2008;19:130–139. doi: 10.1016/j.drugpo.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Lam WKK, Parry CDH, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS Behav. 2006;10:131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- WHO. [Accessed October 20, 2012];Global health observatory data repository: life expectancy tables. 2012 www.who.int/countries/en/
- World Health Report. ATLAS 2010: Global Report on Substance Use. World Health Organization; Geneva: 2010. [Google Scholar]