Abstract
[15] HIV Risk Behaviors in Drug Court
A small percentage of participants in a large metropolitan felony Drug Court engaged in high-risk injection drug use, but a large percentage engaged in high-risk sexual behaviors.
[16] HIV Risk Factors in Drug Court
HIV risk behaviors were associated with being male, African–American, and younger.
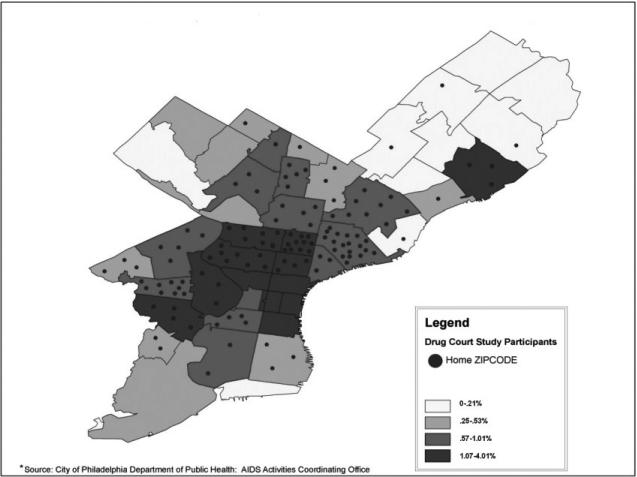
[17] Geographic Risk for HIV
A large proportion of Drug Court participants resided in areas of the city with a high prevalence of persons living with HIV/AIDS, thus heightening the probability of exposure to the virus.
ACCORDING TO RECENT ESTIMATES from the Centers for Disease Control and Prevention (CDC; Hall et al., 2008), approximately 1.2 million adults and adolescents in the United States are HIV positive, representing approximately 0.4% of the total population. An estimated 56,300 adolescents and adults were newly infected with the HIV virus in 2006. Seventy-three percent of these new infections occurred among males, 45% among African–Americans, and 17% among Hispanics. Over half of the new infections occurred among males who have sex with males (MSM).
The relationship between drug use and HIV risk is well documented. According to CDC estimates, injection drug use (22%) was the third most common high-risk behavior among individuals living with HIV [after male-to-male sexual contact (45%) and high-risk heterosexual contact (27%)]. In addition to risks of direct and indirect transmission associated with injection drug use, noninjection substance users are also disproportionately at risk for contracting HIV through sexual transmission. Substance use has been frequently linked to sexual risk behaviors and viral transmission among both heterosexuals and MSM. Clearly, drug and alcohol use can affect economic status, social network membership, and decision making with respect to partner selection and condom use. These factors often lead to unsafe sexual practices (e.g., Brewer et al., 2007; Celentano, Latimore, & Mehta, 2008; Cheng et al., 2010; Kwiatkowski & Booth, 2000; Molitor, Bautista, & Choi; Royce et al., 1997). Finally, research has demonstrated that the biological effects of drug abuse can affect a person's susceptibility to HIV infection and the progression of AIDS (e.g., Bagby et al., 2006; Samet et al., 2003, 2004).
The high rates of drug use put substance-abusing offenders at a high risk for contracting HIV infection and for transmitting the virus to others. It is estimated that approximately 80% of prison and jail inmates were under the influence of drugs or alcohol at the time of their arrest (Belenko & Peugh, 2005; James, 1988; Teplin, 1994). Of those in jail who are HIV positive, intravenous drug use is among the most predominant methods of transmission (Dean, Lansky, & Fleming, 2002; Hammett et al., 1994, as cited in Swartz, Lurigio, & Weiner, 2004). In fact, early estimates (Vlahov et al., 1989) indicated that 85% of these infections were linked to intravenous drug use. More recent estimates identify this rate to be closer to one-half (Dean et al., 2002). In addition, other factors are likely to contribute to the elevated HIV risk in incarcerated individuals including poverty, unemployment, lack of health care access (Hammet, Harmon, & Maruschak, 1999), and social networks that include high-risk associates (Friedman et al., 1999).
Individuals in the criminal justice system have been found to be at a particularly high risk for HIV/AIDS infection and transmission. The relatively high prevalence rate for HIV infection has been well established in incarcerated populations. Nationwide, an estimated 22,144 HIV positive inmates were in state and federal prisons at the end of December 2008, accounting for 1.5% of the total prison population (Maruschak, 2009), almost four times higher than in the total U.S. population. Among them were 5,113 confirmed AIDS cases accounting for 0.4% of the total prison population. Furthermore, it has been estimated that 17%–25% of HIV-infected individuals pass through the prison system annually (Braithwaite & Arriola, 2003; Spalding et al., 2009).
Although the primary focus of HIV prevention efforts for the criminal justice system has been on incarcerated populations (e.g., Braithwaite & Arriola, 2003; Hammet et al., 1999), the majority of offenders are actually not incarcerated but rather are under community supervision, with over five million offenders on probation or parole (Glaze & Bonczar, 2009). Rates of drug involvement are particularly high in this population, putting them at higher risk for HIV infection. At the end of 2008, 30% of probationers had been charged with drug offenses and another 17% had been charged with driving while impaired (DWI). Approximately 37% of parolees had served a sentence for a drug offense. Belenko et al. (2004) examined the prevalence of HIV and risk behaviors in a sample of offenders who were under community supervision. They reported HIV/AIDS prevalence rates that mirrored those observed in inmates, rates of injection drug use that were slightly higher, and a high prevalence of risky sex behaviors.
Little research has focused on the rates of engagement in HIV risk behaviors in other types of community corrections settings. For instance, Drug Courts are one of the most empirically supported approaches for successfully diverting drug using offenders from incarceration to drug treatment and case management in the community (e.g., Aos et al., 2001; Latimer, Morton-Bourgon, & Chretien, 2006; Lowenkamp, Holsinger, & Latessa, 2005; Marlowe, DeMatteo, & Festinger, 2003; Marlowe, Festinger, & Lee, 2004; Wilson, Mitchell, & MacKenzie; Schaffer, 2006). Drug Courts are special criminal court dockets that provide a judicially supervised regimen of substance abuse treatment and other needed services for nonviolent, substance-abusing offenders in lieu of criminal prosecution or incarceration (Marlowe et al., 2008). The first Drug Court was established in 1989, and there are now more than 2,500 Drug Courts in the United States and its territories (National Association of Drug Court Professionals, 2011). Given the rapid expansion of Drug Courts to serve the needs of drug-involved offenders and the high prevalence of HIV risk behaviors that have been identified among other substance-abusing criminal justice populations, it is important to understand the prevalence of HIV risk behaviors among this growing population.
The purpose of this descriptive paper is to examine the prevalence of HIV drug and sex risk behaviors in a sample of participants from one felony Drug Court located in Philadelphia, Pennsylvania. Nearly two-thirds of all people living with HIV/AIDS in the city of Philadelphia are African–American, 75% are males, and almost two-thirds are under the age of 40 (Philadelphia Department of Public Health, 2009). Given these demographic disparities in HIV/AIDS rates in the city of Philadelphia, we also examined the relationship between race, gender, and age and engagement in high-risk behaviors. Findings from the study may provide an important first step in establishing the need for evidence-based HIV risk reduction interventions as a standard part of the Drug Court curriculum.
METHOD
Participants
A total of 269 participants were recruited from a felony preadjudication Drug Court located in the urban City of Philadelphia. To be eligible for the Drug Court program, participants are required to (1) be at least 18 years of age; (2) be charged with a nonviolent felony offense; (3) have no more than two prior nonviolent convictions, juvenile adjudications, or diversionary opportunities; (4) be in need of treatment for drug abuse or dependence as assessed by a clinical case manager employed by the court; and (5) be willing to participate in the Drug Court program for at least twelve months. Consecutive admissions over a 22-month period were approached at entry about their willingness to participate in the study, and the consent rate was 75% (269 of 360).
The study participants were primarily male (80%) and most self-identified as African–American (61%), Caucasian (18%), or Hispanic (24%). Their mean age was 24.31 years (SD = 7.55) and their mean educational attainment was 11.25 years (SD = 1.57). Less than one-half (44%) were regularly employed full or part time. Virtually all of the participants were unmarried (98%) and many lived in the homes of family or friends (61%) or in a controlled environment such as recovery housing (8%). They reported an average annual legal income of $7,040 (SD = $9,077) with a range of $0–$55,000. Approximately 73% reported marijuana as their primary drug of abuse, and 13% had a history of prior substance abuse treatment.
Nearly all of the participants (97%) were currently charged with delivery of a controlled substance or possession with the intent to deliver a controlled substance. In addition, 28% were charged with conspiracy related to a drug offense, and small proportions were charged with forgery (1%), felony retail theft (1%), or prostitution (1%) (participants could have multiple charges). They had an average history of 1.15 (SD = 0.71) criminal arrests prior to their current charge. Most participants were represented by a public defender (84%).
To monitor potential selection bias, demographic data and criminal records were obtained for individuals who did not participate in the study. These data were received in aggregate batches from the Drug Court and were de-identified. Individuals who did not participate in the study were more likely to be male (91% vs. 80%), X2(1) = 7.76, p < .005, African–American (75% vs. 61%), X2(1) = 6.78, p < .01, and represented by private defense counsel (22% vs. 16%), X2(1) = 3.57, p = .06.
Procedures
Study procedures were approved by the Institutional Review Boards of the Treatment Research Institute and the City of Philadelphia. After participants provided informed consent to participate in the study, a research assistant administered a battery of instruments to the participants in a private room. The battery included a health behavior survey that contained six items designed to evaluate the extent to which participants engaged in drug use and sexual behaviors in the past six months that increased their risk for HIV infection. Three items were related to intravenous drug use (i.e., number of times injected drugs, number of people shared needles with, frequency of needle cleaning rated on a five-point Likert-type scale), and three items were related to high-risk sexual behavior (i.e., number of sexual partners, number of same-gender partners, frequency of condom use rated on a five-point Likert-type scale). Importantly, these items were adapted from the well-validated Risk Assessment Battery (RAB) (Metzger, Navaline, & Woody, 2001) and were selected to measure rates of engagement in HIV risk behaviors that are directly responsible for viral transmission. The 6-month time frame was selected to capture a representative sample of recent risk behavior and is standard for the RAB.
Data Analyses
Response frequencies were calculated for each item, and the results of these descriptive analyses are presented in the section that follows. In addition, chi-square analyses were used to examine differences in the rates of engagement in high-risk behaviors as a function of race (African–American vs. other) and gender. Correlation analyses were performed to examine the relationship between engagement in these behaviors and age among sexually active study participants. Finally, we used participant zip codes to map our study sample to the population-adjusted geographic concentration of HIV/AIDS in Philadelphia in order to identify their risk of coming into contact with the virus.
RESULTS
Drug-Use Risk Behaviors
Only two people in the sample (0.7%) reported injection drug use in the past six months. Both of these individuals indicated sharing needles with one person in the past six months and that they had cleaned their needles prior to use.
Sexual Risk Behaviors
Approximately 54% of participants reported having sex with multiple partners in the past six months, while 41% reported having only one partner and 6% reported not being sexually active during this time period. The average number of partners for those reporting multiple partners was 6.12 (SD = 11.20). Three percent of participants reported having sexual relations with same-gender partners.
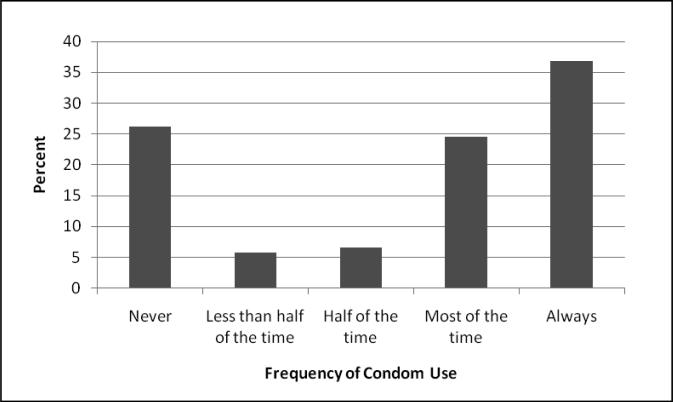
Frequency of condom use among those who were sexually active (N = 244) is presented in Figure 1 following. Almost two-thirds (62%) reported engaging in unprotected sex at least once in the past six months, and 26% reported never using a condom during sexual activity. Among those who had multiple partners (N = 139), 52% reported engaging in unprotected sex at least once in the past six months. Within the small sample of participants with same-gender partners (N = 9), 56% reported never using a condom and 44% reported always using a condom.
Figure 1.
Frequency of Condom Use in Sexually Active Sample (N = 244)
Gender Differences in Sexual Risk Behaviors
Within the sexually active sample, males were significantly more likely to report having multiple sexual partners in the past six months (63% vs. 30%, X2(1) = 16.28, p < .0001). On average, men reported 4.51 (SD = 9.69) sexual partners and females reported 1.37 (SD = 0.61). There was a trend for males to be more likely to report having sex without a condom than females (74% vs. 61%, p < .10). While the overall rate was low, females were more likely than males to report having same-gender sexual partners (17% vs. 1%, p < .0001, Fisher's exact test).
Racial Differences in Sexual Risk Behaviors
Within the sexually active sample, African–Americans were significantly more likely to report having multiple sexual partners than members of other racial groups (63% vs. 47%, X2(1) = 5.92, p < .05. There were no significant differences in the reporting of sexual activity without a condom (60% vs. 67%, p = .19) or having same-gender sexual partners (4% vs. 3%, p = 1.0, Fisher's exact test).
Age Differences in Sexual Risk Behaviors
Within the sexually active sample, age was significantly related to reporting multiple sexual partners (r = –.15, p < .05). The likelihood of reporting multiple sexual partners decreased as a function of age. There was a nonsignificant trend for condom use to decrease as a function of age (r = .11, p < .10). Age was not related to having same-gender sexual partners (p = .21).
Zip Code Mapping
As displayed in Figure 2, over one-third of the Drug Court participants in this study resided in Philadelphia zip code areas with the highest prevalence (1%–4%) of the adult population currently living with AIDS. Fully 80% were from zip code areas with over 0.5% prevalence of adults living with AIDS.
Figure 2.
Prevalence of Persons Living with AIDS in Philadelphia by Participant Zip Code
DISCUSSION
The current study is among the first to provide estimates of the prevalence of HIV risk behaviors in a Drug Court population. Understanding the extent to which Drug Court participants engage in behaviors that put them at risk for contracting HIV infection is important for a number of reasons. First, research has demonstrated that individuals who are involved in the criminal justice system are at high risk of contracting HIV. In addition, criminally involved offenders who are under supervision in the community have more opportunities to engage in risky behaviors than persons in prison, which may increase their risk of contracting HIV infection. Finally, Drug Courts are becoming an increasingly popular diversion strategy for criminally involved substance abusers. The size of this population is expected to increase exponentially as more and more Drug Courts are established. Understanding the prevalence of HIV risk behaviors among Drug Court participants will help us to determine the extent of the need for HIV risk reduction interventions in Drug Court programs.
Rates of HIV drug risk behaviors were low in the current sample. The rate of injection drug use was 0.7%, only slightly higher than the rate reported for probationers and parolees (0.15%) (Belenko et al., 2004) and in the general population (0.17% in the past year) (Substance Abuse and Mental Health Services Administration, 2009). Importantly, the rate of injection drug use in the Drug Court sample is significantly lower than the rates reported among prisoners (e.g., Abiona et al., 2009; Swartz, Lurigio, & Weiner, 2004; Fox et al., 2005). Of the two people who reported any injection drug use in the past six months, both indicated that they cleaned their needles prior to use. Of course, we cannot verify the effectiveness of their cleaning methods or needle sharing behaviors. While one may have expected higher rates of IV drug use in this felony Drug Court, this rate is not surprising given the fact that almost three-fourths of the sample reported marijuana as their primary drug of abuse.
Conversely, Drug Court participants engaged in a number of sexual behaviors that may increase their risk of contracting HIV. Over half of the sample indicated they had sex with multiple partners in the past six month, and two-thirds of the sexually active sample reported having sex without a condom at least once during the past six months. About half of participants who reported having multiple partners indicated that they had sex without a condom at least once during the past six months. These rates are slightly higher than those reported in a sample of probationers and parolees (Belenko et al., 2004). Among probationers and parolees, about half (48%) of individuals reported having vaginal sex with casual partners in the past six months. Of those with casual partners, a little more than a third (38%) reported having sex without a condom at least once in the past six months. Among the general population, estimates of the percentage of people who have had sex with multiple partners during the past year range from 9% to 13% (Holtzman, Bland, Lansky, & Mack, 2001; Leigh, Temple, & Trocki, 1993).
Consistent with the disparities in the rate of HIV transmission in the U.S. (CDC, 2008) and in line with data specific to the City of Philadelphia (Philadelphia Department of Public Health, 2009), significantly higher rates of engagement in risky behaviors were associated with being African–American and male. Results related to age were mixed. While younger people were significantly more likely to have multiple partners, there was a nonsignificant trend for them to be more likely to use condoms every time they had sex. The results related to age are consistent with those observed in other studies (e.g., Binson et al., 1993; Dolcini et al., 1993; Leigh, Temple, & Trocki, 1993; Reece et al.; Sanders et al., 2010).
Perhaps the most striking finding comes from the results of the zip code mapping analysis. Over a third of Drug Court participants resided in areas of Philadelphia with the highest density of persons living with AIDS (i.e., 1%–4%). According to the World Health Organization, an epidemic is considered generalized when greater than 1% of the population is infected. This designation not only provides a measure of prevalence but also indicates the increased potential for individuals to come in contact with the virus. In high-prevalence settings, most unprotected sex can be considered high risk. In the current sample, the great majority of participants come from high prevalence neighborhoods, and all have a history of substance use, which is associated with sexual risk and infection among heterosexuals and MSM (Metzger, Woody, & O'Brien, 2010).
This study has several limitations. First, the study relies on self-reported data that were collected during a face-to-face interview. Participants may have felt embarrassed or uncomfortable answering questions of such a personal nature and, for this reason, may have under-reported their engagement in drug and sexual risk behaviors. Second, the risk instrument had a limited number of items and was intended to be a survey rather than a risk scale. For this reason, we could not calculate composite risk scores. Future studies should evaluate HIV risk using validated risk measures that provide composite scores and that can be self-administered to help reduce self-presentation concerns (e.g., Audio Computer Assisted Self Interview RAB) (Metzger et al., 2000). Third, 25% of those approached refused to participate in the study. Because participants who refused were more likely to be male and African–American, the prevalence rates of high-risk behaviors cited in the present study may be an underestimate of rates in the Drug Court population as a whole. Finally, the study examines the prevalence of HIV risk behaviors in a single felony Drug Court in Philadelphia. Future research should be conducted in other settings in order to evaluate the generalizability of the current findings.
Despite their proven efficacy in addressing substance abuse and criminal recidivism, Drug Courts have yet to be evaluated with respect to HIV and sexually transmitted infection (STI) risk reduction. Given the prevalence of high-risk behaviors (e.g., Belenko at al., 2004) and the alarming rates of HIV infection and STIs among criminal offenders (14%–26%) (Hammet, Harmon, & Rhodes, 2002; Spaulding et al., 2009) along with the rates of high-risk behaviors found in the current study, Drug Courts may represent an important yet unexplored opportunity to deliver risk reduction interventions, HIV testing, and referral to HIV care. Research should be expanded to further document the prevalence of high-risk behaviors among Drug Court participants and to identify useful strategies for reducing risk.
Acknowledgments
This research was supported by grant #R01-DA-14566 from the National Institute on Drug Abuse (NIDA). This research has been approved by the Institutional Review Boards of the Treatment Research Institute and the City of Philadelphia. The views expressed are those of the authors and do not necessarily reflect the views of NIDA.
The authors gratefully acknowledge the continuous collaboration of the staff and clients of the Philadelphia Treatment Court as well as the Office of the District Attorney of Philadelphia, Defender Association of Philadelphia, Philadelphia Coordinating Office of Drug and Alcohol Abuse Programs, and Philadelphia Health Management Corporation. We also thank Patricia Arabia, Jason Croft, Gloria Fox, Matthew Haines, and Jason Matejkowski for their assistance with this project.
Biography
David S. Festinger, PhD, is a senior scientist and director of TRI's Section on Law and Ethics Research, as well as a faculty member in the Department of Psychiatry at the University of Pennsylvania School of Medicine. His research focuses primarily on empirically isolating the active mechanisms of Drug Courts, developing empirically based dispositional procedures for substance-abusing offenders, and bringing experimental research methods to bear on major ethical questions involving human subjects in substance abuse research.
Karen L. Dugosh, PhD, is a research scientist in TRI's Section on Law and Ethics. She has been involved in Drug Court research for almost a decade and has recently begun to examine ethical issues surrounding research participation and informed consent in vulnerable populations. Her current research focuses on the development of an assessment to measure coercive pressures to participate in research that is tailored to the doubly vulnerable population of substance-abusing offenders.
David S. Metzger, PhD, is director of the Behavioral and Social Science Core at the Center for AIDS Research, Director of the HIV Prevention Research Division in the University of Pennsylvania's Department of Psychiatry, and the scientific liaison for TRI and the University of Pennsylvania's Department of Psychiatry. Currently, his work involves testing the safety and efficacy of behavioral and biomedical prevention interventions including HIV vaccines, social network interventions, and agonist drug treatments.
Douglas B. Marlowe, JD., PhD, is chief of Science, Law and Policy at the National Association of Drug Court Professionals and senior scientist in TRI's Section on Law and Ethics. He is a lawyer and research psychologist with expertise in evaluating substance abuse interventions for criminal offenders. Dr. Marlowe has published over 150 scientific papers related to Drug Courts and other interventions for drug abusers and criminal offenders.
References
- Abiona T, Balogun J, Adefuye A, Sloan P. Pre-incarceration HIV risk behaviours of male and female inmates. International Journal of Prisoner Health. 2009;5(2):59–70. doi: 10.1080/17449200902880524. [DOI] [PubMed] [Google Scholar]
- Aos S, Phipps P, Barnoski R, Lieb R. The comparative costs and benefits of programs to reduce crime. Costs and Benefits of Preventing Crime. 2001:3–19. [Google Scholar]
- Bagby GJ, Zhang P, Purcell JE, Didier PJ, Nelson S. Chronic binge ethanol consumption accelerates progression of simian immunodeficiency virus disease. Alcoholism: Clinical and Experimental Research. 2006;30(10):1781–1790. doi: 10.1111/j.1530-0277.2006.00211.x. [DOI] [PubMed] [Google Scholar]
- Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention education among offenders under community supervision: A hidden risk group. AIDS Education and Prevention. 2004;16(4):367–385. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- Belenko S, Peugh J. Estimating drug treatment needs among state prison inmates. Drug and Alcohol Dependence. 2005;77(3):269–281. doi: 10.1016/j.drugalcdep.2004.08.023. [DOI] [PubMed] [Google Scholar]
- Binson D, Dolcini MM, Pollack LM, Catania JA. Multiple sexual partners among young adults in high-risk cities. Family Planning Perspectives. 1993;25(6):268–272. [PubMed] [Google Scholar]
- Braithwaite R, Arriola K. Braithwaite and Arriola respond. American Journal of Public Health. 2003;93(10):1617. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer TH, Zhao W, Metsch LR, Coltes A, Zenilman J. High-risk behaviors in women who use crack: Knowledge of HIV serostatus and risk behavior. Annals of Epidemiology. 2007;17(7):533–539. doi: 10.1016/j.annepidem.2007.01.029. [DOI] [PubMed] [Google Scholar]
- Celentano DD, Latimore AD, Mehta SH. Variations in sexual risks in drug users: Emerging themes in a behavioral context. Current HIV/AIDS Reports. 2008;5(4):212–218. doi: 10.1007/s11904-008-0030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention Subpopulation estimates from the HIV Incidence Surveillance System—United States, 2006. Morbidity and Mortality Weekly Report. 2008;57(36):985–989. [PubMed] [Google Scholar]
- Cheng WS, Garfein RS, Semple SJ, Strathdee SA, Zians JK, Patterson TL. Binge use and sex and drug use behaviors among HIV(-), heterosexual methamphetamine users in San Diego. Substance Use & Misuse. 2010;45(1–2):116–133. doi: 10.3109/10826080902869620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean HD, Lansky A, Fleming PL. HIV surveillance methods for the incarcerated population. AIDS Education and Prevention. 2002;14(5 Supplement):65–74. doi: 10.1521/aeap.14.7.65.23859. [DOI] [PubMed] [Google Scholar]
- Dolcini MM, Catania JA, Coates TJ, Stall R, Hudes ES, Gagnon JH, Pollack LM. Demographic characteristics of heterosexuals with multiple partners: The National AIDS Behavioral Surveys. Family Planning Perspectives. 1993;25(5):208–214. [PubMed] [Google Scholar]
- Fox RK, Currie SL, Evans J, Wright TL, Tobler L, Phelps B, Page-Shafer KA. Hepatitis C virus infection among prisoners in the California state correctional system. Clinical Infectious Diseases. 2005;41(2):177–186. doi: 10.1086/430913. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Curtis R, Neaigus A, Jose B, Des Jarlais DC. Social networks, drug injectors’ lives, and HIV/AIDS. Kluwer Academic; New York: 1999. [Google Scholar]
- Glaze LE, Bonczar TP. Probation and parole in the United States. 20092008 website: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1764.(NCJ 228230). Retrieved from U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics
- Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA: Journal of the American Medical Association. 2008;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett T, Harmon P, Maruschak L. Issues and practices in criminal justice. National Institute of Justice, U.S. Department of Justice; Washington, DC: 1999. 1997 update: HIV/AIDS, STDs, and TB in correctional facilities. [Google Scholar]
- Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from U.S. correctional facilities, 1997. American Journal of Public Health. 2002;92(11):1789–1794. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett TM, Harold L, Gross M, Epstein J. HIV AIDS in correctional facilities: Issues and options. National Institute of Justice; Washington, DC: 1994. [Google Scholar]
- Holtzman D, Bland SD, Lansky A, Mack KA. HIV-related behaviors and perceptions among adults in 25 states: 1997 Behavioral Risk Factor Surveillance System. American Journal of Public Health. 2001;91(11):1882–1888. doi: 10.2105/ajph.91.11.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James D. Prison, mental illness, and identity. Lancet. 1988;2(8624):1371. doi: 10.1016/s0140-6736(88)90912-9. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski CF, Booth RE. Differences in HIV risk behaviors among women who exchange sex for drugs, money, or both drugs and money. AIDS and Behavior. 2000;4(3):233–240. [Google Scholar]
- Latimer J, Morton-Bourgon K, Chretien J. A meta-analytic examination of drug treatment courts: Do they reduce recidivism? 2006 website: http://www.justice.gc.ca/eng/pi/rs/reprap/2006/rr06_7/rr06_7.pdf.Retrieved from Department of Justice Canada, Research and Statistics Division
- Leigh BC, Temple MT, Trocki KF. The sexual behavior of U.S. adults: Results from a national survey. American Journal of Public Health. 1993;83(10):1400–1408. doi: 10.2105/ajph.83.10.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenkamp CT, Holsinger AM, Latessa EJ. Are drug courts ef fective: A meta-analytic review. Journal of Community Corrections. 2005:5–28. Fall. [Google Scholar]
- Marlowe DB, DeMatteo DS, Festinger DS. A sober assessment of drug courts. Federal Sentencing Reporter. 2003;16:153–157. [Google Scholar]
- Marlowe DB, Festinger DS, Dugosh KL, Arabia PL, Kirby KC. An effectiveness trial of contingency management in a felony preadjudication drug court. Journal of Applied Behavior Analysis. 2008;41(4):565–577. doi: 10.1901/jaba.2008.41-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA. The judge is a key component of drug court. Drug Court Review. 2004;4(2):1–34. [Google Scholar]
- Maruschak LM, Beavers R. HIV in prisons, 2007–08 (NCJ 228307). 2009 website: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1747.Retrieved from U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics
- Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, et al. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. American Journal of Epidemiology. 2000;152(2):99–106. doi: 10.1093/aje/152.2.99. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Navaline HA, Woody GE. Assessment of substance abuse: HIV risk assessment battery (RAB). In: Carson-DeWitt R, editor. Encyclopedia of drugs, alcohol, and addictive behavior. 2nd Ed. Macmillan-Thompson/Gale; 2001. [Google Scholar]
- Metzger DS, Woody GE, O'Brien CP. Drug treatment as HIV prevention: A research update. Journal of Acquired Immune Deficiency Syndromes. 2010;55(Suppl. 1):S32–S36. doi: 10.1097/QAI.0b013e3181f9c10b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molitor TW, Bautista EM, Choi CS. Immunity to PRRSV: double-edged sword. Veterinary Microbiology. 1997;55:265–276. doi: 10.1016/S0378-1135(96)01327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of Drug Court Professionals . The facts on drugs and crime in America. Office of Justice Programs, U.S. Department of Justice; Washington, DC: 2011. [Google Scholar]
- Philadelphia Department of Public Health Philadelphia AIDS demographics, 2002–2008. 2009 Web site: http://www.phila.gov/health/AACO/AACODataResearch.html.Retrieved from Philadelphia Department of Public Health
- Reece M, Herbenick D, Schick V, Sanders SA, Dodge B, Fortenberry JD. Condom use rates in a national probability sample of males and females ages 14 to 94 in the United States. Journal of Sexual Medicine. 2010;7(Suppl. 5):266–276. doi: 10.1111/j.1743-6109.2010.02017.x. [DOI] [PubMed] [Google Scholar]
- Royce RA, Sena A, Cates W, Jr., Cohen MS. Sexual transmission of HIV. New England Journal of Medicine. 1997;336(15):1072–1078. doi: 10.1056/NEJM199704103361507. [DOI] [PubMed] [Google Scholar]
- Samet JH, Horton NJ, Meli S, Freedberg KA, Palepu A. Alcohol consumption and antiretroviral adherence among HIV-infected persons with alcohol problems. Alcoholism: Clinical and Experimental Research. 2004;28(4):572–577. doi: 10.1097/01.alc.0000122103.74491.78. [DOI] [PubMed] [Google Scholar]
- Samet JH, Horton NJ, Traphagen ET, Lyon SM, Freedberg KA. Alcohol consumption and HIV disease progression: Are they related? Alcoholism: Clinical and Experimental Research. 2003;27(5):862–867. doi: 10.1097/01.ALC.0000065438.80967.56. [DOI] [PubMed] [Google Scholar]
- Sanders SA, Reece M, Herbenick D, Schick V, Dodge B, Fortenberry JD. Condom use during most recent vaginal intercourse event among a probability sample of adults in the United States. Journal of Sexual Medicine. 2010;7(Suppl. 5):362–373. doi: 10.1111/j.1743-6109.2010.02011.x. [DOI] [PubMed] [Google Scholar]
- Shaffer DK. Reconsidering drug court effectiveness: A meta-analytic review. Dept. of Criminal Justice, University of Nevada; Las Vegas, NV: 2006. [Google Scholar]
- Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammet TM. HIV/AIDS among inmates of and releasees from U.S. correctional facilities, 2006: Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11) doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies . The NSDUH Report: Injection drug use and related risk behaviors. Rockville, MD: Oct 29, 2009. [Google Scholar]
- Swartz JA, Lurigio AJ, Weiner DA. Correlates of HIV-risk behaviors among prison inmates: Implica tions for tailored AIDS prevention programming. The Prison Journal. 2004;84(4):486. [Google Scholar]
- Teplin LA. Psychiatric and substance abuse disorders among male urban jail detainees. American Journal of Public Health. 1994;84(2):290–293. doi: 10.2105/ajph.84.2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Brewer TF, Munoz A, Taylor E, Hall D, Polk BF. Temporal trends of (HIV-1) infection among inmates entering a statewide prison system, 1985–1987. Journal of Acquired Immune Deficiency Syndrome. 1989;1:283–290. [PubMed] [Google Scholar]
- Wilson DB, Mitchell O, MacKenzie DL. A systematic review of drug court effects on recidivism. Journal of Experimental Criminology. 2006;2(4):459–487. [Google Scholar]