Abstract
Longitudinal effects of child maltreatment on cortisol regulation in infants from age 1 to 3 years were investigated in the context of a randomized preventive intervention trial. Thirteen-month-old infants from maltreating families (N = 91) and their mothers were randomly assigned to one of three intervention conditions: 1. Child-Parent Psychotherapy (CPP); 2. Psychoeducational Parenting Intervention (PPI); and 3. a control group involving standard community services (CS). A fourth group of infants from nonmaltreating families (N = 52) and their mothers comprised a nonmaltreated comparison (NC) group. The two active interventions were combined into one maltreated intervention (MI) group for statistical analyses. Saliva samples were obtained from children at 10:00 a.m. before beginning a laboratory observation session with their mothers when the children were 13 months of age (pre-intervention), 19 months (mid-intervention), 26 months (post-intervention), and 38 months (one-year post-intervention follow-up). At the initial assessment, no significant differences among groups in morning cortisol were observed. Latent growth curve analyses examined trajectories of cortisol regulation over time. Beginning at mid-intervention, divergence was found among the groups. Whereas the MI group remained indistinguishable from the NC group across time, the CS group progressively evinced lower levels of morning cortisol, statistically differing from the MI and NC groups. Results highlight the value of psychosocial interventions for early child maltreatment in normalizing biological regulatory processes.
Child maltreatment is characterized by severe dysfunction in parenting and a substantial disturbance in the parent-child relationship that may eventuate in aberrant biological and psychological development and psychopathology across the lifespan (Azar, 2002; Cicchetti & Valentino, 2006; Cyr, Euser, Bakermans-Kranenburg, & van IJzendoorn, 2010; Rogosch, Cicchetti, Shields, & Toth, 1995; Toth, Cicchetti, Macfie, Rogosch, Maughan, & van Meenen, 2000). The provision of sensitive, emotionally secure, and protective parenting is woefully lacking in the caregiving environments of maltreated infants (Cicchetti & Lynch, 1995; Cicchetti & Toth, 2005; Davies, Winter, & Cicchetti, 2006) and maltreating parents may be considered to be an aberration of the supportive, nurturant adults that are expected by infants in the evolutionary context of species-typical development (Cicchetti & Lynch, 1995; Tarullo & Gunnar, 2006). Infants and children who have been maltreated may be regarded as “caretaking casualties” (Cicchetti & Rizley, 1981; Egeland, Cicchetti, & Taraldson, 1976; Sameroff & Chandler, 1975).
In contrast to what is anticipated in response to an expectable environment, the biological, psychological, and social conditions associated with child maltreatment usher in motion a probabilistic path of epigenesis for abused and neglected children that increases the likelihood of repeated disruptions in the positive mastery of the stage-salient issues of each successive developmental period (Cicchetti & Lynch, 1993; Cicchetti & Toth, 1995). Failures in the successful resolution of these developmental tasks may create a developmental cascade of maladaptation across diverse domains of biological, socioemotional, and cognitive development and increase the probability of psychopathology as negative transactions continue to ensue between maltreated children and their environments (Masten & Cicchetti, 2010; Rogosch, Oshri, & Cicchetti, 2010).
In addition to adverse effects on socioemotional and cognitive development, infants and children who either are maltreated or who reside in maltreating environments encounter numerous stressful experiences that can exert harmful impacts upon neurobiological development and gene expression (Beach, Brody, Todorov, Gunter, & Phillibert, 2009; Cicchetti; 2002; Cicchetti & Curtis, 2005; Cicchetti & Rogosch, 2001; DeBellis, 2001, 2005; McCrory DeBrito, & Viding, 2010; Trickett, Noll, Susman, Shenk, & Putnam, 2010). In particular, maltreated infants may be particularly vulnerable to the effects of stressful experiences during periods of rapid creation or modification of neuronal connections, such as those that take place during the course of the first years of life (Black, Jones, Nelson, & Greenough, 1998; Cicchetti, 2002; Stiles, 2008; Thompson & Nelson, 2001). Extremely adverse, overwhelming, and traumatic experiences may become part of a vicious cycle, as the pathology induced in brain structure may distort the maltreated child’s experience of the world, with subsequent alternations in cognitive functioning (Cicchetti et al., 2003; Jaffee & Maikovich-Fong, 2011; Pollak, Cicchetti, Klorman, & Brumaghim, 1997; Rieder & Cicchetti, 1989; Toth, Pickreign Stronach, Rogosch, Caplan, & Cicchetti, in press) and social interactions (Rogosch, Cicchetti, & Aber, 1995; Teisl & Cicchetti, 2008) contributing to further detrimental experiences and additional brain pathology (Black et al., 1998; Cicchetti & Tucker, 1994).
During infancy and early childhood, the developing hypothalamic-pituitary-adrenal (HPA) axis is under powerful social regulation (Levine, 2005; Tarullo & Gunnar, 2006). As such, the HPA axis of maltreated youngsters is vulnerable to disturbance given the relative lack of sensitive and emotionally supportive caregiving provided. Incidents of maltreatment may engender massive acute and chronic stress in infants and children who reside in such environments. Stressful, threatening, or frightening experiences, such as those associated with child abuse and neglect, create significant challenges to adaptive development (Gunnar & Vazquez, 2006). Consequently, allostatic load processes may be unfolding very early in the development of maltreated infants and children, setting up the potential for life-long difficulties in the regulation of physiological stress systems (Juster, McEwen, & Lupien, 2009) and the emergence of concomitant neurobiological, emotional, cognitive, and physical health problems throughout the life course (Felitti, Anda, Nordenberg, Williamson, Spitz et al., 1998).
Given that maltreated children experience a magnitude of stressors that often are present during infancy, the capacity to regulate the stress hormone, cortisol (which exerts impacts on nearly all organs and tissues of the body, including the brain), is of critical importance for these youngsters. Research with rodents, non-human primates, and humans, has shown that parental caregiving mediates the regulation of the HPA axis (see, e.g., Francis, Diorio, Plotsky, & Meaney, 2002; Levine, 2005; Meaney & Szyf, 2005; Sanchez, 2006). The disruption of maternal care in rodents results in an HPA system that is not buffered against stress. Abusive or harsh treatment of monkey infants also interferes with the buffering function provided by the typical monkey mother (see, e.g., Levine, 2005; McCormack, Grand, LaPrairie, Fulks, Graff et al., 2003; Sanchez, McCormack, Grand, Fulks, Graff et al., 2010). Likewise, sensitive and emotionally secure parental caregiving also has been demonstrated to protect the HPA axis in human infants and young children, whereas the HPA axis of youngsters who do not receive responsive caregiving, such as those who are abused and neglected, is not safeguarded against stress (Brand, Brennan, Newport, Smith, Weiss, & Stowe, 2010; Bugental, Martorell, & Barraza, 2003; Hart, Gunnar, & Cicchetti, 1995; Tarullo & Gunnar, 2006).
Research on the impact of early caregiving adversity in humans has revealed that the HPA axis is highly likely to exhibit evidence of dysregulation and that this dysregulation may entail both hyper- and hypo-functioning (Cicchetti & Rogosch, 2001; Cicchetti, Rogosch, Gunnar, & Toth, 2010; Gunnar & Vazquez, 2001; Heim, Newport, Mletzko, Miller, & Nemeroff, 2008). Levels of cortisol, the final hormonal product of the neuroendocrine system, that are chronically elevated during development, when neural circuits are still in the process of maturing, exert an impact on brain development by affecting neurotropic factors and regulating gene transcription, thereby influencing the manner in which neural circuits perceive and interpret environmental threat and the magnitude and duration of future stress responses (Tarullo & Gunnar, 2006). Additionally, chronically low levels of basal cortisol also can eventuate in harmful effects on the brain, as well as on physical and mental health and behavior (Juster et al., 2009; Juster, Bizik, Picard, Arsenault-Lapierre, Sindi et al., 2012; Lupien, Ouellet-Morin, Hupbach, Tu, Buss et al., 2006). Both hyper- and hypo-cortisolism can reflect allostatic load, typically defined as the result of chronic exposure to fluctuating or heightened neural or neuroendocrine responses that emerge in response to chronic environmental challenges that are perceived as especially stressful (McEwen & Stellar, 1993).
Heightened fear and activation of the HPA system as a function of early adverse care may produce an increase in allostatic load over the lifespan (Trickett et al., 2010). The HPA axis tends to down-regulate in response to prolonged hyperactivation. Consequently, chronic stressors such as child maltreatment initially evoke hyperactivity of the HPA axis, followed by later hypoactivity (Trickett et al., 2010). It is important to note that the dysregulation in HPA axis functioning commonly observed in maltreated infants and children, although often harmful in adulthood, initially may have served as an adaptive alteration (Tarullo & Gunnar, 2006). A major difficulty lies in the fact that, because the HPA stress system begins from a state of immaturity at birth and because the developing neural circuitry is influenced by early experience, the manner in which the brain will respond to stress over time may no longer be adaptive outside of the maltreating environment (Tarullo & Gunnar, 2006).
The plethora of studies documenting the neuroendocrine disturbances following child maltreatment, in concert with the likely harmful developmental sequelae of these HPA axis disturbances and the accompanying sustained allostatic load, underscore the criticality of implementing randomized control trial (RCTs) preventive interventions in order to ascertain whether they can modify and reorganize the alterations in HPA axis functioning (Cicchetti & Gunnar, 2008). In the human literature, evidence is beginning to accrue suggesting that efficacious interventions with children in foster care may modify not only maladaptive behavior, but also the neuroendocrine correlates of behavior (Dozier, Peloso, Lewis, Laurenceau, & Levine, 2008; Fisher, Gunnar, Dozier, Bruce, & Pears, 2006; Fisher, Stoolmiller, Gunnar, & Burraston, 2007). Methodologically rigorous RCTs that incorporate a multi-level measurement battery have begun to provide a unique lens through which the processes responsible for the development, maintenance, and modification of both typical and atypical functional neuroendocrine outcomes can be discerned (Gunnar, Fisher, and the Early Experience, Stress, and Prevention Network, 2006).
Investigations with rodents, non-human primates, and human children have discovered that early separations from caregivers may lead to alterations in the functioning of the HPA system (Gunnar & Quevedo, 2007; Sanchez, Ladd, & Plotsky, 2001). In an innovative illustration of the capability of psychosocial interventions to modify diurnal cortisol activity, Fisher, Stoolmiller, Gunnar and Burraston (2007) conducted a 6 – 9 month RCT of a family-based foster care therapeutic intervention for preschool children. The therapeutic intervention was compared with a regular foster care condition and a demographically comparable group of same-aged, nonmaltreated preschool children from low-socioeconomic status families. Fisher et al. (2007) collected and assayed early-morning and evening cortisol levels from the preschool children (mean age = 4.4 years) on a monthly basis from the baseline until the end of the intervention. One common disturbed cortisol pattern that emanates from disruptions in caregiving is a low early-morning cortisol that displays minimal change across the day. Fisher and colleagues (2007) found that the foster children who received the family-based therapeutic intervention exhibited cortisol activity that became comparable to the nonmaltreated comparison children over the course of the intervention. In contrast, children who received routine services in state foster care (e.g., weekly individual psychotherapy; developmental screening for delays with the subsequent provision of special education services, if needed) displayed an increasingly flattened pattern of early morning to evening cortisol activity throughout the course of the RCT. The results of this psychosocial intervention demonstrate that improvements in caregiving following the experience of early adversity have the potential to reverse or prevent disturbances in the HPA system (Fisher et al., 2007).
The study of child maltreatment as a ‘natural experiment’ provides a valuable lens into the relations between sensitive caregiving and stress regulation and reveals insights for translation of basic empirical findings into RCTs aimed are reorganizing and normalizing these relations. Moreover, the conduct of RCTs, such as that described above, yields important knowledge regarding the malleability of developmental processes. Psychosocial randomized preventive interventions with previously maltreated children placed in foster care provide important opportunities for children who have transitioned into a changed environment to manifest competent biological and behavioral functioning. For children in foster care, there may be variability with respect to the presence of continued stressful experiences. For example, the move to foster care may be traumatic for some children even if they have been placed in a better setting than their previous home or foster care experience.
In the current investigation, we report the findings of a 12-month RCT intervention with maltreated infants. One intervention, child-parent psychotherapy (CPP), is an attachment-based, non-directive approach that encourages sensitive interactions between caregivers and their children by helping parents form positive representations of themselves and the caregiver-child relationship. The second intervention, psychoeducational parenting intervention (PPI), is a didactic intervention that teaches parenting skills, relaxation techniques, and behaviors that promote social support. At post-intervention, both CPP and PPI were found to be efficacious in improving secure attachments and in decreasing disorganized attachment (Cicchetti, Rogosch, & Toth, 2006). In contrast to the maltreated children participating in the foster care interventions described above, the maltreated children in our RCT all resided in their natural homes with their biological caregiver(s). The infants in the intervention groups were compared to a group of maltreated children receiving the community standard intervention typically provided when maltreatment is identified by the local Department of Human Services. An additional nonmaltreated demographically comparable group of infants also was included. Morning cortisol was assayed at baseline, at six months mid –intervention, at post intervention, and at one year after the completion of the RCT.
Hypotheses:
Our work was guided by the following hypotheses.
Maltreated infants will display lower AM cortisol levels in comparison to those of the nonmaltreated comparisons.
The maltreated infants who received the relational or the parenting interventions will not differ from nonmaltreated comparisons in their AM cortisol levels, either at the end of the intervention or at the 1 year post-intervention follow-up assessment.
The AM cortisol levels of the maltreated children receiving the community standard will exhibit increasingly lower levels of cortisol throughout the intervention and at the post-intervention follow-up.
Method
Participants
Infants in maltreating families and their mothers were recruited for a study of the effects of child maltreatment on infant development and for an evaluation study of the efficacy of two preventive interventions designed to optimize mother-infant relationships and improve parenting. In the current report, the maltreatment sample consisted of 91 infants (43 boys, 48 girls) and their mothers. A nonmaltreated comparison group of 52 infants (28 boys, 24 girls) and their mothers also were recruited. During the initial assessment, infants were on average 13.3 months of age (SD = .80).
In order to recruit one-year-old infants in maltreating families and their mothers, a Department of Human Services (DHS) recruitment liaison was retained. As an employee of DHS, the liaison was able to access DHS Child Protective Service (CPS) and preventive service records in order to identify all infants known to have been maltreated and/or who were living in maltreating families with their biological mothers. Infants who had been placed in foster care were not targeted for inclusion because of the limited ongoing contact with their mothers. The DHS liaison contacted eligible families and explained the project to mothers. Mothers who were interested in participating signed a release form in order for their names to be given to project staff. During the initial contact by project staff, the mothers provided informed consent and permission for their infant's participation. Mothers also signed a release allowing project staff to have access to DHS records regarding the family's CPS and preventive service involvement.
Maltreatment determinations
All DHS records pertaining to the family were accessed and independently coded by trained research staff. The Maltreatment Classification System (Barnett, Manly, & Cicchetti, 1993) was utilized to identify all forms of maltreatment that had occurred in the family and that the infant had experienced. Based on operational criteria, the MCS designates all subtypes of maltreatment (i.e., neglect, emotional maltreatment, physical abuse, sexual abuse). Coding of the DSS records was conducted by trained research staff, doctoral students, and clinical psychologists. Adequate reliability has been obtained (weighted kappas ranging from .86 to .98). Other investigators have demonstrated that the MCS is reliable and valid in classifying maltreatment (Bolger, Patterson, & Kupersmidt, 1998; Dubowitz, Pitts, Litrownik, Cox, Runyan et al., 2005; English, Upadhyaya, Litrownik, Marshall, Runyan, et al., 2005; Manly, 2005; Smith & Thornberry, 1995).
In terms of the subtypes of maltreatment, neglect involves failure to provide for the child's basic physical needs for adequate food, clothing, shelter, and medical treatment. In addition to inadequate attention to physical needs, forms of this subtype include lack of supervision, moral-legal neglect, and education neglect. Emotional maltreatment involves extreme thwarting of children's basic emotional needs for psychological safety and security, acceptance and self-esteem, and age-appropriate autonomy. Examples of emotional maltreatment of increasing severity include belittling and ridiculing the child, extreme negativity and hostility, exposure to severe marital violence, abandoning the child, and suicidal or homicidal threats. Physical abuse involves the non-accidental infliction of physical injury on the child (e.g., bruises, welts, burns, choking, broken bones). Injuries range from minor and temporary to permanently disfiguring. Finally, sexual abuse involves attempted or actual sexual contact between the child and caregiver for purposes of the caregiver's sexual satisfaction or financial benefit. Events range from exposure to pornography or adult sexual activity, to sexual touching and fondling, to forced intercourse with the child.
In the recruited sample, we considered specific subtypes of maltreatment that had been experienced by the targeted infant (individual level), as well as subtypes of maltreatment that also had occurred among all children in the family (family level), in order to characterize the broader maltreating family context. For infants in the maltreatment sample, 71.4% had directly experienced abuse and/or neglect during the first year of life. For these infants with individual level maltreatment, none had been sexually abused, whereas 10.8% had been physically abused, 83.1% had been neglected, and 69.2% had been emotionally maltreated. The majority of these infants, 55.4%, had experienced more than one subtype of maltreatment. Few cases of physical abuse were present in the subgroup of infants with individual level maltreatment because of the high likelihood of foster care placement when infants are subjected to physical abuse. The remaining subgroup of infants (28.6%) in the maltreatment sample were living in families where legally documented abuse and neglect had been experienced by siblings, i.e., at the family level only.
Despite variation in the presence of individual level abuse/neglect among the infants in the maltreatment sample, the rates of abuse and neglect occurring more broadly at the family level across siblings in these families were substantial. For the subgroup of families with infants with individual level maltreatment (71.4%) versus the subgroup of families with infants where family level maltreatment only had occurred (28.6%), the rate of family level sexual or physical abuse among children in the family was high in both groups (89.2% and 84.6%, respectively), as was the rate of family level neglect (92.3% and 88.5%, respectively). Thus, extensive child maltreatment across family members had been documented in the families comprising the maltreatment sample.
Recruitment of nonmaltreating families
Because of the predominance of poverty in the sample of maltreating families, a demographically comparable sample of mothers and infants in low-income families was recruited through the rolls of families receiving Temporary Assistance to Needy Families (TANF). The DHS liaison identified families with infants from the TANF rolls and screened these families for child maltreatment. The DHS liaison then contacted eligible families, explained the study, and for interested mothers, obtained a signed release form in order for the family's name to be given to the research staff. Subsequently, project staff obtained informed consent and signed permission for all DHS records pertaining to the family to be reviewed. DHS and preventive records were thoroughly screened to rule out the existence of documented child maltreatment in these families. Mothers also were interviewed utilizing the Maternal Maltreatment Classification Interview (Cicchetti, Toth, & Manly, 2003) regarding maltreatment and any DHS involvement to further validate nonmaltreatment status.
Sample characteristics
Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups: Child-Parent Psychotherapy (CPP), Psychoeducational Parenting Intervention (PPI), and standard services typically provided in the community, Community Standard (CS). Some mothers assigned to receive one of the theoretically-informed preventive interventions (CPP or PPI) declined to participate in treatment. Because of the noncompliance with random group assignment, these mothers (n = 46) and their infants were not included in the current report. The resulting group sizes in the current investigation were: CPP (n = 32), PPI (n = 24), and CS (n = 35). Because prior research with this sample (Cicchetti et al., 2006) demonstrated comparable post-intervention effects for the CPP and PPI groups in improving the mother-child relationship and because the two groups did not differ in cortisol levels across time, as discussed below, these two interventions were combined into one Maltreated Intervention group (MI: n = 56). The MI, CS, and NC groups were comparable on a range of demographic variables, as shown in Table 1. The groups did not differ on child gender, child minority race/ethnicity, or age at the initial assessment. Furthermore, the groups did not differ on maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. Mothers on average were 26.90 years of age (SD = 5.96), 72.5% were of minority race/ethnicity, and 30.81% of mothers were currently married or living with a partner. The average family income was $16,646.00, including welfare benefits, and 95.8% of the families were currently receiving TANF. Overall, 40.6% of the mothers had less than a high school education. However, a difference among the groups emerged, χ2 (2, N = 143) = 6.30, p = .04. The MI and the CS groups had more mothers with less than a high school education than the NC group. Finally, the groups differed on the number of children to whom the mothers had given birth, F (2,140) = 21.65, p < .001. Post hoc tests indicated that mothers in the NC group had fewer children than the mothers in the MI and CS groups. Maternal education and number of children were not significantly correlated with cortisol levels at any of the periods of assessment, and thus, these variables were not considered further. Overall, the families in the sample are characterized by poverty, relatively large family size, and single parent mothers.
Table 1.
Demographic characteristics.
| Group | |||
|---|---|---|---|
| Maltreated Intervention (MI) |
Community Standard (CS) |
Nonmaltreated Comparison (NC) |
|
|
N = 56 M(SD) or % |
N = 35 M(SD) or % |
N = 52 M(SD) or % |
|
| Child Gender (% female) |
51.8% | 54.3% | 46.2% |
| Child Age (mo.) | 13.36 (.87) | 13.32 (.82) | 13.32 (.71) |
| Child Minority Race/Ethnicity |
76.8% | 80.0% | 80.0% |
| Maternal Age | 27.36 (6.52) | 27.70 (5.75) | 25.81 (5.39) |
| Maternal Minority Race/Ethnicity |
69.6% | 77.1% | 73.1% |
| Maternal Education (< High School)* |
48.2% | 48.6% | 26.9% |
| Receiving TANF | 98.2% | 97.1% | 92.3% |
| Total Income ($1,000) |
15.35 (6.412) | 18.25 (8.37) | 16.96 (8.15) |
| Marital Status | |||
| Never Married | 46.4% | 37.1% | 65.4% |
| Married/Living with partner |
35.7% | 42.9% | 17.3% |
| No longer married | 17.9% | 20.0% | 17.3% |
| N of Children*** | 3.43 (1.81) | 3.60 (1.65) | 1.83 (1.04) |
p <.05;
p <.001;
Procedures
During the baseline assessment period, home- and center-based research sessions were conducted with the mothers and infants. During interviews conducted in the home by trained research assistants, mothers completed demographic interviews and a variety of self-report questionnaires. For a subsequent center-based laboratory session, mothers and infants were transported by private car to the center in the mid-morning. Given transportation time and acclimation to the center in the initial interview room, infant saliva sampling did not occur during the cortisol awakening period. During the session, mothers and infants participated in mother-child observational paradigms and other research assessments. After the mother and child had arrived for the center-based session, saliva samples were obtained from infants before beginning the laboratory assessments. For uniformity of saliva collection times, all center-based sessions were scheduled in the morning as close to 10:00 a.m., as possible (M sample time = 9:53, SD = :36) . Identical procedures for timing and sampling of saliva were followed at subsequent time periods of assessment: T2, when infants were approximately 19 months of age (mid-intervention) (M saliva sample time = 9:59, SD = :37); T3, when children were approximately 26 months of age (post-intervention) (M saliva sample time = 9:59, SD = :36); and at T4, when children were approximately 38 months of age (one year post-intervention follow-up) (M saliva sample time = 9:56, SD = :40).
Preventive Interventions
Child-Parent Psychotherapy (CPP)
This model of intervention is derived from the work of Selma Fraiberg (Fraiberg, Adelson, & Shapiro, 1975) and Alicia Lieberman (1992). A guiding assumption of CPP is that difficulties in the parent-infant relationship do not result from deficits in parenting knowledge and skill alone. Rather, the problems that maltreating mothers have in relating sensitively and responsively to their infants stem from insecure internal representational models that evolved in response to the mother's own experiences in childhood. In CPP, the patient is not the mother or the infant, but rather it is the relationship between the mother and her baby. Masters level therapists met weekly with mothers and their infants during sessions conducted in the home over the course of approximately one year (M weeks = 46.42, SD = 7.36). The approach is supportive, nondirective, and non-didactic, and includes developmental guidance based on the mother's concerns. During the sessions, the therapist and the mother engage in joint observation of the infant. Through respect, empathic concern, and unfailing positive regard, the therapeutic relationship provides the mother with a corrective emotional experience, through which the mother is able to differentiate current from past relationships, form positive internal representations of herself and of herself in relationship to others, particularly her infant. As a result of this process, mothers are able to expand their responsiveness, sensitivity, and attunement to the infant, fostering security in the mother-child relationship and promoting emerging autonomy in the child.
Psychoeducational Parenting Intervention (PPI)
This model of preventive intervention is derived from the preventive intervention work of David Olds and colleagues (Olds & Kitzman, 1990; Olds, Eckenrode, Henderson, Kitzman, Powers et al., 1997; Olds, Henderson, Cole, Eckenrode, Kitzman et al., 1998), in which nurses provided a home-based education program on infant physical and psychological development and parenting, encouraged mothers to seek further education and employment, and enhanced informal social support. From this home-based model, the PPI intervention was supplemented by a variety of cognitive and behavioral techniques in order to address parenting skill deficits and social-ecological factors, such as limited personal resources, poor social support, and stresses in the home, associated with maltreatment. Masters level therapists, experienced in working with multi-problem families, conducted home visits scheduled weekly over a 12-month period (M weeks = 49.36, SD = 4.81). The PPI model was psychoeducationally-based, striving to address current concerns, provide parental education and parenting skill training, reduce maternal stress, foster social support, and increase life satisfaction. The approach is didactic in nature, and involved training in parenting techniques, problem solving, and relaxation.
Both the CPP and PPI interventions were manualized, with central components and core principles of each approach specified. Therapists participated in individual and group supervision on a weekly basis, and checks on the fidelity of the intervention implementation for each approach were conducted throughout the course of intervention. Extensive outreach was typically necessary to engage mothers in the interventions. Both the CPP and PPI interventions were found to be efficacious in fostering securing attachment in toddlers in maltreating families (Cicchetti et al., 2006).
Community Standard (CS)
Mothers and infants randomized to the CS group did not receive enhanced services. Rather, families continued to receive services that were typically available to maltreating families in the community. Families may have continued to be monitored by CPS and may have participated in other preventive services programs.
Measures
Demographics Interview
This measure has been used extensively in research with high-risk, low-income populations. Information obtained includes: family composition, gender, race/ethnicity, birth dates, parent's education and occupation, income level, and receipt of public assistance.
Saliva sampling for cortisol assay
After mothers and infants acclimated to an interview room upon arrival to the center, saliva sampling procedures with the infant were begun. When saliva sampling began, infants had not had any food or drink in their mouths since the time that they had been picked up for transportation to the center (approximately 45 minutes). A research assistant wearing latex gloves dabbed a cotton roll in a container of Kool Aid crystals to get a few grains on the end of the cotton roll, in order to stimulate the child’s saliva production. Then the infant was allowed to suck on the cotton roll until it was saturated. Subsequently, the cotton roll was placed in a syringe, and the saliva was expressed into two 500 ul collection vials. The samples were immediately frozen and stored at −80° C. The same procedures were utilized at each of the subsequent longitudinal assessments.
Subsequently, the samples were shipped overnight on dry ice for next day delivery to Salimetrics Laboratories (State College, PA) for assay. Cortisol was assayed in duplicate by Salimetrics, Inc using an enzyme immunoassay (Salimetrics, State College, PA). This assay has a lower limit of sensitivity of 0.007 μg/dl (range up to 1.8 μg/dl), and average intra-and inter-assay coefficients of variation less than 5.0% and 10.0%, respectively. Units of cortisol are expressed in μg/dl (micrograms per deciliter). As cortisol values were positively skewed and leptokurtotic, logarithmic transformations (log10) of cortisol values were used for all statistical analyses.
At the baseline assessments at age 13 months, mean values for morning cortisol were .313 μg/dl (SD = .235), with a median of .235, 5th percentile of .092, and 95th percentile of .834. A recent study has provided normative data on cortisol levels in 300 infants over the first year, with multiple assessments obtained at 11:00 a.m. at age 6 weeks, 5 months, and 10-12 months (Tollenaar, Jansen, Beijers, Risken-Walraven, & de Weerth, 2010). A general decline in cortisol levels was observed across these longitudinal assessments. At age 10-12 months, the median morning cortisol was .283 μg/dl, with a 5th percentile of .127 and 95th percentile of .851. Thus, in comparison to this distribution, the morning cortisol levels at 13 months in the current study are generally consistent with normative levels of morning cortisol observed in the Tollenaar et al. study.
Results
In a preliminary examination of cortisol levels over time, we investigated whether the two active intervention groups, CPP and PPI, differed in morning cortisol levels at each of the four assessment periods. At each of these time points, the difference between the two groups was not statistically significant, with p values ranging from .30 to .94. Accordingly, based on power considerations, there was further justification for combining the two intervention groups into one maltreated intervention (MI) group for statistical purposes.
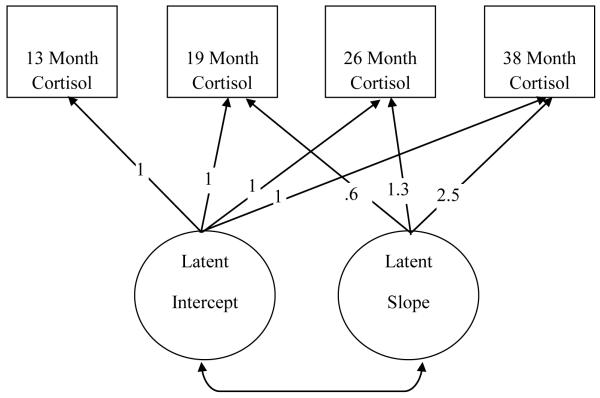
Our primary data analytic strategy utilized latent growth curves (LGC). Group differences in children’s basal cortisol levels were examined using LGC analyses which explore the existence of continuous underlying trajectories of change in longitudinal data (LGC; Meredith & Tisak, 1990). LGC analyses model both fixed-effects (group-level change) and random-effects (individual variability in change) components of the trajectory model (see Figure 1). Unconditional LGC analyses account for the non-independence of within-person observations over time through specifying separate estimates of both within-subject and between-subject variation through the following equations:
Figure 1.
Conceptual model of unconditional, linear latent growth curve model across four assessment points.
Level 1 (within individual):
where, cortit represents the value of the trajectory variable cort for the ith case at time t, αi is the random intercept for case i, βi is the random slope for case i , and λt is a constant that codes the trajectory at time i, and:
Level 2 (between individuals):
where μα and μβ are the average intercept and slope values across all cases, and ζαi and ζβi models sample variability around the average intercept and slope parameters, respectively.
Unconditional LGC models of cortisol measures across the four assessment points were specified within each group (e.g., MI, CS, NC) using AMOS 19.0 (Arbuckle, 2006). Thus, within the unconditional growth curve model, we can examine the existence and significance of the average intercept and slope within each group. Finally, in the present study, λt was coded such that the slope trajectory was indicated by the spacing interval in months across the assessments (e.g., 0,.6, 1.3, 2.5)
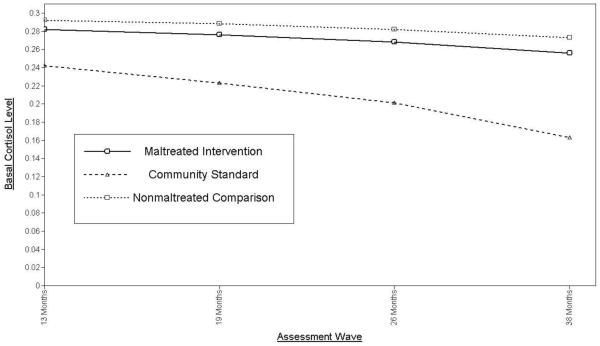
Analyses first revealed that the unconditional linear growth curve model fit the data well, χ2 (15, N = 143) = 20.80, p = .14 (CFI = .96, RMSEA = .05). Latent intercept values across the different groups were positive and significant (μαs range from .25 - .29; p < .05), suggesting that cortisol values differed from zero at baseline (see Figure 1). Importantly, pairwise parameter comparisons among the different groups revealed no significant differences in intercept values (z’s ranged from 0.13 to 1.66) suggesting that across the three conditions, children evidenced similar basal cortisol levels at baseline assessments. Thus, the effectiveness of our randomization of infants in the maltreatment sample to treatment condition was supported for initial values of cortisol, allowing us to further explore whether treatment condition is related to change in basal cortisol levels over time. Examination of the average linear slopes of cortisol assessments over time revealed interesting differences across the three groups. First, the means of the slope factors for MI group, CS group, and NC group were; μ = –0.009 (SE = .008, p = 0.31), μ = -.035 (SE = .009, p < .001), and μ = -.003 (SE = .010, p = 0.80) respectively. These findings suggested that only the CS group experienced a statistically significant linear decline in basal cortisol levels over time, while average slopes for the MI and NC groups were not significantly different from zero. In addition, pairwise parameter comparisons of the average slope values across the three groups also revealed that slopes for the MI and NC groups were significantly different from the CS group (z’s = 1.97 and 2.27, respectively), and were not statistically different from one another (z = 0.79). Model-implied trajectories of cortisol levels across the three groups are plotted in Figure 2.
Figure 2.
LGC model implied trajectories of basal cortisol values over time for the maltreated intervention, community standard, and nonmaltreated comparison groups.
In order to pinpoint the measurement interval in which the treatment effect upon basal cortisol level manifested itself, we utilized the latent growth curve model and respecified the intercept value in a series of model analyses. For example, to explore basal levels at wave 2, λt was coded such that the slope trajectory was centered (path constrained to 0) at wave 2 (e.g., -.6, 0, .7, 1.9 ). Centering was then moved to wave 3 and wave 4 in subsequent model runs. This allowed us to compare the groups across each timepoint within the same modeling framework. Analyses revealed significant differences in basal cortisol levels between the NC group and the CS group starting at wave 2 and continuing at each subsequent assessment point (z’s = 3.07, 4.50, and 4.40, respectively). Furthermore, significant differences between the MI group and the CS group on basal cortisol levels were also present at wave 2 and continued over each assessment (z’s = 2.83, 4.39 and 4.31, respectively). Finally, a non-significant difference between the MI and NC groups in basal cortisol levels was uncovered at wave 2, and continued over the remaining two assessments (z’s = 0.51, 0.92, and 1.09, respectively). These results indicated that the treatment effect on basal cortisol was evident at the first assessment post-intervention and maintained throughout the course of the study.
Discussion
Although morning cortisol levels did not differ among the MI, CS, and NC groups at baseline, infants in the maltreated group who received the community standard (CS) intervention exhibited a steady decline in basal morning cortisol levels over the course of the a two-year period of investigation. These findings may be indicative of an ongoing process of higher allostatic load in the CS group of infants and toddlers. Moreover, the differences among the MI, CS, and NC groups were apparent at the first cortisol assessment that took place at 19 months, six months following entry into the intervention. Furthermore, these relative decrements in basal cortisol in the CS group remained significantly different over time, with the gap widening sequentially. Thus, in the MI group, evidence of progressive allostatic load effects was averted. Finally, for infants in the MI group, cortisol levels were normalized (i.e., not different from the NC group) and remained so even at the one-year post-intervention follow-up period. The normalization of morning cortisol over time in the MI group bears a striking similarity to the results obtained by Fisher et al. (2007) in their RCT with maltreated preschool children in foster care. Compared to preschoolers receiving the regular foster care intervention, those randomized to a family-based therapeutic intervention displayed cortisol levels that became comparable to those exhibited by non-maltreated children. Our findings, in concert with those of Fisher and colleagues (2007), suggest that interventions designed to improve caregiving following experiences of early adversity can reverse or prevent disruptions in HPA functioning.
The ability of psychosocial interventions to reorganize the functioning of the HPA axis provides further evidence that physiological processes are not immutable (Cicchetti, 2002; Cicchetti & Gunnar, 2008). Psychosocial interventions can avert decline in normative neuroendocrine regulation, normalizing HPA functioning in high-risk infants receiving RCT preventive interventions. Thus, it is conceivable that the efficacy of any preventive intervention ultimately depends on the ability of the nervous system, either at the cellular, metabolic, or anatomical level, to be modified by experience. Such modifications are adaptive for the ongoing survival and optimal functioning of the organism (Cicchetti & Curtis, 2006; Huttenlocher, 2002; Stiles, 2008). Given the numerous negative physical and mental health sequelae associated with allostatic load, it is highly probable that the youngsters in the MI group will have a greater likelihood of improved functioning across varying domains of development.
Within the intervention group, there are a number of possible mechanisms that may have produced changes in the ability of the brain to process information it confronts during stressful situations. The interventions likely reduced the stress experienced in the child rearing environment. In addition, mothers in the intervention may have become better able to cope with the demands of rearing infants and toddlers. As a consequence, these mothers could have become more able to pay greater attention and become more responsive to infant/toddler needs. Likewise, changes in parenting or mother-child relational processes may have promoted positive self-representations in the caregiver as well as positive representations of her infant/toddler, resulting in improved functioning of the child’s HPA axis through the concomitant reduction in relational stress.
The achievement of normalized HPA functioning and the prevention of an extended process of allostatic load in the MI group also is likely to exert a positive influence on other aspects of stress neurobiology and related biological systems such as immune, metabolic, and cardiovascular functioning (Herman & Cullinan, 1997; Juster et al., 2009; Shonkoff, Boyce, & McEwen, 2009). Furthermore, the intervention received by the MI group served not only a protective function by preventing prolonged allostatic load, but also may have helped to avoid the longer-term physical and mental health problems typically accompanying hypocortisolism (Cicchetti & Rogosch, 2001; Gunnar & Vazquez, 2001). In contrast, the infants in the community standard intervention group, who exhibited a steady decrease in morning cortisol levels over a two-year period, are at high-risk for developing future mental and physical health problems (Danese, Caspi, Williams, Ambler, Sugden et al., 2011; Danese, Moffitt, Pariante, Ambler, Poulton, & Caspi, 2008; Danese, Pariante, Caspi, Taylor, & Poulton, 2007; Miller, Chen, Fok, Walker, Lim et al., 2009).
Infants in the MI group very likely develop enhanced self-righting capacities that may promote the development of resilient functioning (Cicchetti, 2010; Cicchetti & Rogosch, 1997). The normalization of the HPA axis in these youngsters may aid in their ability to perceive threat accurately and to regulate their stress systems so as not to be overly sensitive to adverse experience (Cicchetti & Rogosch, 2007). In contrast, infants in the CS group are highly likely not to manifest improvement in their self-righting abilities, succumbing to allostatic load processes and exhibiting a sequential worsening of morning cortisol regulation over time (Cicchetti & Rogosch, 2001). Moreover, the infants in the CS group are likely to have fewer self-righting capabilities and this bodes poorly for their ability to function in a resilient fashion (Cicchetti, 2010). The several year process of increasing HPA dysregulation is not likely to be the result of an acute reaction. Rather, this HPA dysregulation may eventuate in life-long neurobiological problems in the absence of having a more developmentally appropriate and intensive intervention, such as that received by infants in the MI group, provided.
Despite its strengths, our RCT does possess several limitations. Only one cortisol sample was collected and assayed at each time period assessed. Nonetheless, the consistency in the time of collection across the four assessment waves is remarkable. In addition, we did not include other biomarkers of allostatic load assessed throughout the duration of the RCT. Moreover, we were not able to delineate definitive mechanisms of change contributing to our differential patterns of cortisol regulation over time. Finally, because maltreated infants in foster care were excluded, and because these infants are likely to have experienced more severe early maltreatment, our findings may not be generalizable to maltreated infants residing in foster care. Importantly, however, the results of our RCT with home reared maltreated infants are markedly similar to the results obtained by Fisher and colleagues (2007) with early morning cortisol in their RCT with maltreated preschoolers in foster care.
In future research, it will be critical to assess other aspects of HPA axis functioning, such as diurnal variation and reactivity and recovery from stressors. Moreover, other biomarkers of allostatic load should also be assessed (see Juster et al., 2009; Juster et al., 2012). A multilevel perspective, consisting of assessments of other psychological and biological systems in conjunction with HPA axis functioning, would provide vital information on cross-system relationships and shed light on the next wave of transdisciplinary multiple-levels-of-analysis research on the effects of psychosocial interventions.
Finally, it will be important for researchers to investigate the longer-term effects of intervention on promoting psychological and physical health. In this regard, the positive effects obtained in our RCT may be epigenetic in nature and illustrative of the processes by which a markedly altered environment (i.e., achieved through intervention) can influence methylation and modify gene expression (Meaney, 2010). Consequently, as part of future long-term follow-ups of RCTs, DNA and RNA should be collected and assayed during each assessment point of the longitudinal investigation (e.g., baseline, post-intervention, one-year follow-up). Examining the nature of genetic and epigenetic effects, in conjunction with other psychological and biological domains, has the potential to advance the field with respect to understanding the multiple systems that are influenced by psychosocial interventions. Such work is currently being conducted in our laboratory.
The identification of stress-sensitive neural processes may provide a firm empirical basis for the development of interventions to prevent and to ameliorate the deleterious effects of early maltreatment experiences. Moreover, the inclusion of neurobiological assessments in evaluations of preventive interventions designed to normalize the developmental trajectories of children experiencing maltreatment will enable researchers to discover whether the various components of multi-faceted interventions each exert a differential impact on separate brain systems. As it is increasingly demonstrated that the nervous system can be modified by experience, then successful preventive interventions could be conceptualized as examples of experience-dependent neural plasticity (Cicchetti & Curtis, 2006).
The growing body of research demonstrating that behavioral interventions may positively alter not only psychological processes, but also neurobiological functioning, possesses important implications for the social policy arena. Because resources may be more readily expended for the prevention of negative physical rather than mental health consequences, findings such as those reported herein may ultimately increase the availability of resources that can be directed toward the prevention of child abuse and neglect and toward the extensive treatment needs of these vulnerable children.
Acknowledgements
This research was supported by grants from the National Institute of Mental Health (MH54643), and the Spunk Fund, Inc.
References
- Arbuckle JL. Amos (Version 7.0) [Computer Program] SPSS; Chicago: 2006. [Google Scholar]
- Azar ST. Parenting and child maltreatment. In: Bornstein MH, editor. Handbook of parenting: Social conditions and applied parenting. 2nd Vol. 4. Lawrence Erlbaum Associates; Mahwah, NJ: 2002. pp. 361–388. [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Child abuse, child development, and social policy. Ablex; Norwood, NJ: 1993. pp. 7–74. [Google Scholar]
- Beach SRH, Brody GH, Todorov A, Gunter T, Philibert RA. Methylation at SLC6A4 is linked to family history of child abuse: An examination of the Iowa Adoptee Sample. American Journal of Medical Genetics: Part B Neuropsychiatric Genetics. 2009;153:710–713. doi: 10.1002/ajmg.b.31028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black J, Jones TA, Nelson CA, Greenough WT. Neuronal plasticity and the developing brain. In: Alessi NE, Coyle JT, Harrison SI, Eth S, editors. Handbook of child and adolescent psychiatry. Wiley; New York: 1998. pp. 31–53. [Google Scholar]
- Bolger KE, Patterson CJ, Kupersmidt JB. Peer relationships and self-esteem among children who have been maltreated. Child Development. 1998;69:1171–1197. [PubMed] [Google Scholar]
- Brand SR, Brennan PA, Newport DJ, Smith AK, Weiss T, Stowe ZN. The impact of maternal childhood abuse on maternal and infant HPA axis function in the postpartum period. Psychoneuroendocrinology. 2010;35:686–693. doi: 10.1016/j.psyneuen.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugental DB, Martorell GA, Barraza V. The hormonal costs of subtle forms of infant maltreatment. Hormones and Behavior. 2003;43:237–244. doi: 10.1016/s0018-506x(02)00008-9. [DOI] [PubMed] [Google Scholar]
- Cicchetti D. How a child builds a brain: Insights from normality and psychopathology. In: Hartup W, Weinberg R, editors. Minnesota symposia on child psychology: Child psychology in retrospect and prospect. Vol. 32. Lawrence Erlbaum Associates; Mahwah, NJ: 2002. pp. 23–71. [Google Scholar]
- Cicchetti D. Resilience under conditions of extreme stress: A multilevel perspective [Special Article] World Psychiatry. 2010;9:1–10. doi: 10.1002/j.2051-5545.2010.tb00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Curtis WJ. An event-related potential (ERP) study of processing of affective facial expressions in young children who have experienced maltreatment during the first year of life. Development and Psychopathology. 2005;17:641–677. doi: 10.1017/S0954579405050315. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Curtis WJ. The developing brain and neural plasticity: Implications for normality, psychopathology, and resilience. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Developmental neuroscience. 2nd Vol. 2. Wiley; New York: 2006. pp. 1–64. [Google Scholar]
- Cicchetti D, Gunnar MR. Integrating biological processes into the design and evaluation of preventive interventions. Development and Psychopathology. 2008;20:737–743. doi: 10.1017/S0954579408000357. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children's development. Psychiatry. 1993;56:96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Failures in the expectable environment and their impact on individual development: The case of child maltreatment. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. Vol. 2. Wiley; New York: 1995. pp. 32–71. [Google Scholar]
- Cicchetti D, Rizley R. Developmental perspectives on the etiology, intergenerational transmission and sequelae of child maltreatment. New Directions for Child Development. 1981;11:31–55. [Google Scholar]
- Cicchetti D, Rogosch FA. The role of self-organization in the promotion of resilience in maltreated children. Development and Psychopathology. 1997;9:799–817. doi: 10.1017/s0954579497001442. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Diverse patterns of neuroendocrine activity in maltreated children. Development and Psychopathology. 2001;13:677–694. doi: 10.1017/s0954579401003145. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Personality, adrenal steroid hormones, and resilience in maltreated children: A multi-level perspective. Development and Psychopathology. 2007;19(3):787–809. doi: 10.1017/S0954579407000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, Toth SL. The differential impacts of early abuse on internalizing problems and diurnal cortisol activity in school-aged children. Child Development. 2010;25:252–269. doi: 10.1111/j.1467-8624.2009.01393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Maughan A, Toth SL, Bruce J. False belief understanding in maltreated children. Development and Psychopathology. 2003;15:1067–1091. doi: 10.1017/s0954579403000440. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Fostering secure attachment in infants in maltreating families through preventive interventions. Development and Psychopathology. 2006;18(3):623–650. doi: 10.1017/s0954579406060329. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. A developmental psychopathology perspective on child abuse and neglect. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:541–565. doi: 10.1097/00004583-199505000-00008. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, Manly JT. Maternal Maltreatment Interview. Rochester, NY: 2003. Unpublished manuscript. [Google Scholar]
- Cicchetti D, Tucker D. Development and self-regulatory structures of the mind. Development and Psychopathology. 1994;6:533–549. [Google Scholar]
- Cicchetti D, Valentino K. An ecological transactional perspective on child maltreatment: Failure of the average expectable environment and its influence upon child development. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology. 2nd Vol. 3. Wiley; New York: 2006. pp. 129–201. [Google Scholar]
- Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van IJzendoorn MH. Attachment and security and disorganization in maltreating and high-risk families: A series of meta-analyses. Development and Psychopathology. 2010;22:87–108. doi: 10.1017/S0954579409990289. [DOI] [PubMed] [Google Scholar]
- Danese A, Caspi A, Williams B, Ambler A, Sugden K, Mika J, et al. Biological embedding of stress through inflammation processes in childhood. Molecular Psychiatry. 2011;16:244–246. doi: 10.1038/mp.2010.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Pariante CM, Ambler A, Poulton R, Caspi A. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Archives of General Psychiatry. 2008;65:409–415. doi: 10.1001/archpsyc.65.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:1319–1324. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Winter MA, Cicchetti D. The implications of emotional security theory for understanding and treating childhood psychopathology. Development and Psychopathology. 2006;18:707–736. doi: 10.1017/s0954579406060354. [DOI] [PubMed] [Google Scholar]
- DeBellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- DeBellis MD. The psychobiology of neglect. Child Maltreatment. 2005;10:150–172. doi: 10.1177/1077559505275116. [DOI] [PubMed] [Google Scholar]
- Dozier M, Peloso E, Lewis E, Laurenceau JP, Levine S. Effects of an attachment-based intervention on the cortisol production of infants and toddlers in foster care. Development and Psychopathology. 2008;20:845–859. doi: 10.1017/S0954579408000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz H, Pitts SC, Litrownik AJ, Cox CE, Runyan D, Black MM. Defining child neglect based on child protective services data. Child Abuse & Neglect. 2005;29:493–511. doi: 10.1016/j.chiabu.2003.09.024. [DOI] [PubMed] [Google Scholar]
- Egeland B, Cicchetti D, Taraldson B. Child abuse: A family affair. In Seminaire de recherche Nathalie Masse: Les enfants victimes de mauvais traitments. 1976:28–52. [Google Scholar]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, et al. Maltreatment's wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect. 2005;29:597–619. doi: 10.1016/j.chiabu.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leding causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Gunnar MR, Dozier M, Bruce J, Pears KC. Effects of therapeutic interventions for foster children on behavioral problems, caregiver attachment, and stress regulatory neural systems. Annals of the New York Academy of Sciences. 2006;1094:215–225. doi: 10.1196/annals.1376.023. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on daytime cortisol activity. Psychoneuroendocrinology. 2007;32:892–905. doi: 10.1016/j.psyneuen.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraiberg S, Adelson E, Shapiro V. Ghosts in the nursery: A psychoanalytic approach to impaired infant-mother relationships. Journal of the American Academy of Child Psychiatry. 1975;14:387–421. doi: 10.1016/s0002-7138(09)61442-4. [DOI] [PubMed] [Google Scholar]
- Francis D, Diorio J, Plotsky PM, Meaney MJ. Environmental enrichment reverses the effects of maternal separation on stress reactivity. Journal of Neuroscience. 2002;22:7840–7843. doi: 10.1523/JNEUROSCI.22-18-07840.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar MR, Fisher PA, The Early Experience, Stress, and Prevention Network Bringing basic research on early experience and stress neurobiology to bear on preventive interventions for neglected and maltreated children. Development and Psychopathology. 2006;18:651–678. [PubMed] [Google Scholar]
- Gunnar MR, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Vazquez D. Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology. 2001;13:515–538. doi: 10.1017/s0954579401003066. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Vazquez D. Stress neurobiology and developmental psychopathology. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2nd. Vol. 2. Wiley; New York: 2006. pp. 533–577. Developmental Neuroscience. [Google Scholar]
- Hart J, Gunnar M, Cicchetti D. Salivary cortisol in maltreated children: Evidence of relations between neuroendocrine activity and social competence. Development and Psychopathology. 1995;7:11–26. [Google Scholar]
- Heim C, Newport JD, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Herman JP, Cullinan WE. Neurocircuitry of stress: Central control of the hypothalamo-pituitary-adrenocortical axis. Trends in Neurosciences. 1997;20:78–84. doi: 10.1016/s0166-2236(96)10069-2. [DOI] [PubMed] [Google Scholar]
- Huttenlocher P. Neural plasticity: The effects of environment on the development of the cerebral cortex. Harvard University Press; Cambridge, MA: 2002. [Google Scholar]
- Jaffee SR, Maikovich-Fong AK. Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. Journal of Child Psychology and Psychiatry. 2011;52:184–194. doi: 10.1111/j.1469-7610.2010.02304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster RP, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, et al. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout lifespan development. Development and Psychopathology. 2012;23(3) doi: 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews. 2009;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Levine S. Developmental determinants of sensitivity and resistance to stress. Psychoneuroendocrinology. 2005;30:939–946. doi: 10.1016/j.psyneuen.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Lieberman AF. Infant-parent psychotherapy with toddlers. Development and Psychopathology. 1992;4:559–574. [Google Scholar]
- Lupien SJ, Ouellet-Morin I, Hupbach A, Tu MT, Buss C, Walker D, et al. Beyond the stress concept: Allostatic load – a developmental biological and cognitive perspective. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2nd. Vol. 2. Wiley; New York: 2006. pp. 578–628. Developmental Neuroscience. [Google Scholar]
- Manly JT. Advances in research definitions of child maltreatment. Child Abuse & Neglect. 2005;29:425–439. doi: 10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Masten AS, Cicchetti D. Editorial: Developmental cascades. Developmental Cascades [Special Issue, Part 1], Development and Psychopathology. 2010;22:491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- McCormack KM, Grand A, LaPrairie J, Fulks R, Graff A, Maestripieri D, et al. Behavioral and neuroendocrine outcomes of infant maltreatment in rhesus monkeys: The first four months. Society for Neuroscience Abstracts. 2003;641:14. [Google Scholar]
- McCrory E, DeBrito SA, Viding E. Research review: The neurobiology and genetics of maltreatment and adversity. Journal of Child Psychology and Psychiatry. 2010;51:1079–1095. doi: 10.1111/j.1469-7610.2010.02271.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–2101. [PubMed] [Google Scholar]
- Meaney MJ. Epigenetics and parental effects. Child Development. 2010;32:818–827. doi: 10.1002/bies.201000015. [DOI] [PubMed] [Google Scholar]
- Meaney MJ, Szyf M. Environmental programming of stress responses through DNA methylation: Life at the interface between a dynamic environment and a fixed genome. Dialogues in Clinical Neuroscience. 2005;7:103–123. doi: 10.31887/DCNS.2005.7.2/mmeaney. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith W, Tisak J. Latent curve analysis. Psychometrika. 1990;55:107–122. [Google Scholar]
- Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:14716–14721. doi: 10.1073/pnas.0902971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Kitzman H. Can home visitation improve the health of women and children at environmental risk? Pediatrics. 1990;86:108–116. [PubMed] [Google Scholar]
- Olds DL, Eckenrode J, Henderson CR, Jr., Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: 15-year follow-up of a randomized trial. Journal of the American Medical Association. 1997;278:637–643. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr., Cole R, Eckenrode J, Kitzman H, Luckey D, et al. Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized trial. Journal of the American Medical Association. 1998;280:1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Klorman R, Brumaghim J. Cognitive brain event-related potentials and emotion processing in maltreated children. Child Development. 1997;68:773–787. doi: 10.1111/j.1467-8624.1997.tb01961.x. [DOI] [PubMed] [Google Scholar]
- Rieder C, Cicchetti D. Organizational perspective on cognitive control functioning and cognitive-affective balance in maltreated children. Developmental Psychology. 1989;25:382–393. [Google Scholar]
- Rogosch FA, Cicchetti D, Aber JL. The role of child maltreatment in early deviations in cognitive and affective processing abilities and later peer relationship problems. Development and Psychopathology. 1995;7:591–609. [Google Scholar]
- Rogosch FA, Cicchetti D, Shields A, Toth SL. Parenting dysfunction in child maltreatment. In: Bornstein MH, editor. Handbook of parenting. Vol. 4. Lawrence Erlbaum Associates; Hillsdale, NJ: 1995. pp. 127–159. [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology. 2010;22:883–897. doi: 10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff AJ, Chandler MJ. Reproductive risk and the continuum of caretaking casualty. In: Horowitz FD, editor. Review of child development research. Vol. 4. University of Chicago Press; Chicago: 1975. pp. 187–244. [Google Scholar]
- Sanchez MM. The impact of early adverse care on HPA axis development: Nonhuman primate models. Hormones and Behavior. 2006;50:623–631. doi: 10.1016/j.yhbeh.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Sanchez MM, Ladd CO, Plotsky PM. Early adverse experience as a developmental risk factor for later psychopathology: Evidence from rodent and primate models. Development and Psychopathology. 2001;13:419–450. doi: 10.1017/s0954579401003029. [DOI] [PubMed] [Google Scholar]
- Sanchez MM, McCormack K, Grand AP, Fulks R, Graff A, Maestripieri D. Effects of sex and early maternal abuse on adrenocorticotropin hormone and cortisol responses to the corticotrophin-releasing hormone challenge during the first 3 years of life in group-living rhesus monkeys. Development and Psychopathology. 2010;22:45–53. doi: 10.1017/S0954579409990253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. Journal of the American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Smith CA, Thornberry T. The relationship between child maltreatment and adolescent involvement in delinquency. Criminology. 1995;33:451–481. [Google Scholar]
- Stiles J. The fundamentals of brain development: Integrating nature and nurture. Harvard University Press; Cambridge, MA: 2008. [Google Scholar]
- Tarullo AR, Gunnar MR. Child maltreatment and the developing HPA axis. Hormones and Behavior. 2006;50:632–639. doi: 10.1016/j.yhbeh.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Teisl M, Cicchetti D. Physical abuse, cognitive and emotional processes, and aggressive/disruptive behavior problems. Social Development. 2008;16:1–23. [Google Scholar]
- Thompson RA, Nelson CA. Developmental science and the media: Early brain development. American Psychologist. 2001;56:5–15. doi: 10.1037/0003-066x.56.1.5. [DOI] [PubMed] [Google Scholar]
- Tollenaar MS, Jansen J, Beijers R, Riksen-Walraven JM, de Weerth C. Cortisol in the first year of life: Normative values and intra-individual variability. Early Human Development. 2010;86:13–16. doi: 10.1016/j.earlhumdev.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Toth SL, Cicchetti D, Macfie J, Maughan A, VanMeenan K. Narrative representations of caregivers and self in maltreated preschoolers. Attachment and Human Development. 2000;2:271–305. doi: 10.1080/14616730010000849. [DOI] [PubMed] [Google Scholar]
- Toth SL, Pickreign Stronach E, Rogosch FA, Caplan R, Cicchetti D. Thought disorder in maltreated children. Journal of the American Academy of Child and Adolescent Psychiatry. doi: 10.1016/j.jaac.2011.03.002. in press. [DOI] [PubMed] [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, Putnam FW. Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology. 2010;22:165–175. doi: 10.1017/S0954579409990332. [DOI] [PMC free article] [PubMed] [Google Scholar]