Abstract
Little is known about the presence/absence and prevalence of Rickettsia spp, Bartonella spp. and Yersinia pestis in domestic and urban flea populations in tropical and subtropical African countries.
Methodology/Principal findings
Fleas collected in Benin, the United Republic of Tanzania and the Democratic Republic of the Congo were investigated for the presence and identity of Rickettsia spp., Bartonella spp. and Yersinia pestis using two qPCR systems or qPCR and standard PCR. In Xenopsylla cheopis fleas collected from Cotonou (Benin), Rickettsia typhi was detected in 1% (2/199), and an uncultured Bartonella sp. was detected in 34.7% (69/199). In the Lushoto district (United Republic of Tanzania), R. typhi DNA was detected in 10% (2/20) of Xenopsylla brasiliensis, and Rickettsia felis was detected in 65% (13/20) of Ctenocephalides felis strongylus, 71.4% (5/7) of Ctenocephalides canis and 25% (5/20) of Ctenophthalmus calceatus calceatus. In the Democratic Republic of the Congo, R. felis was detected in 56.5% (13/23) of Ct. f. felis from Kinshasa, in 26.3% (10/38) of Ct. f. felis and 9% (1/11) of Leptopsylla aethiopica aethiopica from Ituri district and in 19.2% (5/26) of Ct. f. strongylus and 4.7% (1/21) of Echidnophaga gallinacea. Bartonella sp. was also detected in 36.3% (4/11) of L. a. aethiopica. Finally, in Ituri, Y. pestis DNA was detected in 3.8% (1/26) of Ct. f. strongylus and 10% (3/30) of Pulex irritans from the villages of Wanyale and Zaa.
Conclusion
Most flea-borne infections are neglected diseases which should be monitored systematically in domestic rural and urban human populations to assess their epidemiological and clinical relevance. Finally, the presence of Y. pestis DNA in fleas captured in households was unexpected and raises a series of questions regarding the role of free fleas in the transmission of plague in rural Africa, especially in remote areas where the flea density in houses is high.
Author Summary
Fleas are associated with many bacterial diseases such as rickettsioses, bartonelloses and plague. These diseases may be severe, and little is known about their prevalence. Accordingly, we believe that our data shed light on the problem of unexplained fevers in tropical and subtropical African areas. Using molecular tools, we surveyed and studied selected flea-borne agents, namely Rickettsia spp. (R. felis and R. typhi), Bartonella spp. and Y. pestis, in fleas collected in Ituri (Linga and Rethy health zone) and Kinshasa in the Democratic Republic of the Congo, the Lushoto district in the United Republic of Tanzania and in Cotonou in Benin. We found that these bacteria are present in the studied regions. R. typhi and an unidentified Bartonella sp. were detected in fleas from Cotonou (Benin). R. felis and R. typhi were also detected in the Lushoto district (United Republic of Tanzania). Finally, we detected R. felis, Bartonella sp. and Y. pestis in the Democratic Republic of the Congo. As these emerging zoonotic diseases have a global distribution and affect public health, the implementation of vector control strategies is urgent.
Introduction
The importance of fleas in human and animal health is largely related to their ability to transmit agents of infectious diseases [1]. The transmission of these zoonotic agents to human occurs mainly through bites or inoculation of feces into pruritic bite lesions [2], [3]. Plague is the most notorious flea-borne disease known to man and is a reemerging public health issue mainly in Africa and South America [3]. The etiological agent of plague, Yersinia pestis, is a facultative gram-negative bacterium restricted nowadays to well defined endemic foci [4], [5]. In the last decade, plague reemerged in old quiescent foci of Algeria [6], the United Republic of Tanzania [7] and Libya [8] and caused remarkable bubonic and pneumonic outbreaks in known endemic foci in Madagascar [9] and in the Democratic Republic of the Congo [10]. Fleas are also associated with other bacterial diseases such as bartonelloses and rickettsioses. Rickettsia spp., the etiological agents of rickettsioses, are intracellular gram-negative bacteria that represent an emergent global threat, particularly in the tropics [11]. R. felis, an emerging pathogen, and R. typhi, the agent of murine typhus (MT), are the main rickettsial pathogens associated with fleas [1], belonging to the spotted fever group (SFG) [12] and typhus group rickettsiae, respectively [13]. Although these two flea-borne rickettsiae are distributed worldwide, R. typhi appears to be more endemic in tropical regions, coastal areas and ports, where its transmission cycles between rats (Rattus spp.) and oriental rat fleas (X. cheopis) [14]. Also, several closely related rickettsiae, referred as Rickettsia felis–like organisms (RFLO), identified in fleas and other arthropods around the world [15]. Likewise, bartonelloses are diseases caused by the fastidious, hemotropic bacteria of the genus Bartonella, especially in debilitated and immunocompromised individuals [16]. Importantly, the list of host species harboring Bartonella spp. includes a large number of mammals, mostly rodents, some of which are kept as pets [17].
An increasing number of papers have reported the occurrence of fleas and human flea-borne infections, especially in relation to wildlife and zoonotic risk. However, the identity and distribution of flea-borne agents in urban, domestic or peridomestic settings have been poorly documented in Sub-Saharan African countries such as the Democratic Republic of the Congo, the United Republic of Tanzania and Benin. Historical data about human infection with Rickettsia and Bartonella species are fragmentary, and virtually nothing is known about the current distribution of these flea-borne zoonotic agents in potential vectors and reservoir hosts in these countries.
In the Democratic Republic of the Congo, recent small-scale surveys have reported serological evidence for Bartonella infection in human patients [18] and molecular data in rodents [19] and fleas [20], suggesting a global underreporting at the country scale. Rickettsioses in humans are mentioned in historical reports; however, their notification remains anecdotal, and the species identification is likely erroneous. Recently though, among febrile military patients in Kisangani, Democratic Republic of the Congo, one patient tested positive in 1999, for the R. typhi antigen using serological tools. In addition, R. felis has been found to circulate in arthropod vectors in Kinshasa [21]. As a general trend, flea-borne agents in fleas are underreported, whereas in the United Republic of Tanzania, a growing number of publications confirm their presence and wide distribution in humans [22] exposed to their bites and in infested rodents [19].
In recent years, our laboratory (Unité de Recherche sur les Maladies Infectieuses et Tropicales, the WHO Collaborative Centre for Rickettsial Diseases and Other Arthropod-Borne Bacterial Diseases in Marseille, France) initiated collaboration with correspondents and universities in the United Republic of Tanzania, the Democratic Republic of the Congo and Benin.
The present survey pursued the objectives of detecting the presence and identity of Rickettsia spp., Bartonella spp. and Y. pestis in flea specimens collected from domestic and peridomestic areas in the Democratic Republic of the Congo, the United Republic of Tanzania and Benin within the context of entomological studies.
Methods
Ethical considerations
Risk assessment was submitted to and approved by the ethical committee and decision board of each institution involved in small mammals trappings, and involved informed consent of the domestic animal owners; ethical approval are available from original publications on mammal hosts on which flea were collected [19], [23], [24]. The Ethical commitee of the University of Antwerp, Belgium and the Sokoine University of Agriculture Morogoro under the project RATZOOMAN granted by the European Commission Framework 5 Programme on International Cooperation, project contract number ICA4 CT 2002 10056, approved the experiment in the South-eastern Africa.
See here technical annex: http://projects.nri.org/ratzooman/docs/technical%20annex.pdf.
Sites of study and flea collection
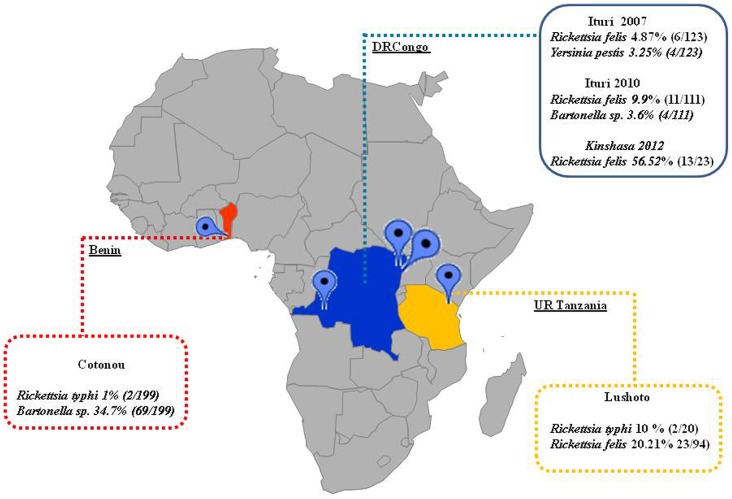
The material analyzed consisted of fleas (Siphonaptera) collected in domestic and peridomestic areas in Benin, the United Republic of Tanzania and the Democratic Republic of the Congo (Figure 1). A portion of the collected fleas was used for the present study. A convenient sample was selected according to a good representation of species, host and localities.
Figure 1. Sites of the study.
In 37 sites in the capital city of Benin, Cotonou (6°21′36″N; 2°26′24″E), rodent fleas were collected from rodents trapped monthly inside human residences and peridomestic areas between November 2009 to July 2010, as described previously [24]. In the United Republic of Tanzania, 17 sites in the Lushoto district (04°40′00″S 38°19′00″E) located in the Tanga Region were surveyed [23], [25]. Lushoto district is a mountainous area where plague was reported from the first time in 1981; this endemic plague focus has however been quiescent since 2004. Between May 2005 and November 2008, fleas were collected – as in Benin – from small mammals in domestic and peridomestic habitats during the dry and rainy seasons. Further details on the rodent measurements and flea collection have been published elsewhere [23], [25].
Finally, in March and April 2007, rodent fleas and free domestic fleas were collected from 4 villages (15 capture sites) in the Linga and Rethy health zones, Ituri district, Orientale Province, the Democratic Republic of the Congo; off-host fleas were collected in 4 villages during an investigation following a plague outbreak that occurred in the third trimester of 2006 [26]. Our investigation area was limited to Djalusene (2°12′10″5 N 30°88′02″7 E) and Kpandruma (2°05′90″1 N 30°88′70″4 E), which had confirmed plague patients, and Wanyale (2°10′11″8 N 30°80′60″5 E) and Zaa (2°14′03″2 N 30°85′65″9 E), which had several suspect cases but were considered control areas at the time of the study. We collected fleas in 40 houses (bedroom) in each village, for 3 nights in a row, using a kerosene lamp hung above a 45-cm diameter tray containing water as described in [27]. In April 2010 and July 2012, additional flea samples were collected from the Ituri district in Rethy village (1°50′N 29°30′E) and in Kinshasa (4°19′19″S 15°19′16″E) by means of light traps in human residences (bedroom) and rodent burrows, and flat tweezers on dogs.
All fleas collected in Benin, the United Republic of Tanzania and the Democratic Republic of the Congo were stored in 70% ethanol and identified morphologically using classical entomologic taxonomic keys. The samples were later processed in the WHO Collaborative Center for Rickettsial Diseases and Other Arthropod-Borne Bacterial Diseases, in Marseille, France.
DNA extraction
Fleas were rinsed twice in distilled water for 10 minutes and dried on sterile filter paper; the handling was performed in a laminar flow biosafety hood. The fleas were individually crushed in sterile Eppendorf tubes, as described [28]. A total of 50 µl of DNA was extracted from one half of each flea using the QIAamp Tissue Kit (Qiagen, Hilden, Germany) by QUIAGEN-BioRobot EZ1, according to the manufacturer's instructions. The genomic DNA was stored at −20°C under sterile conditions until used as the template in PCR assays. The remaining portion of each flea was kept at −80°C for an additional control.
Detection of Rickettsia felis
All samples were screened by quantitative real-time PCR (qPCR) targeting the biotin synthase (bioB) gene, as previously described [29]. Positive results were confirmed by another qPCR targeting a membrane phosphatase gene with primers (Rfel_phosp_MBF: 5′-GCAACCATCGGTGAAATTGA-3′ and Rfel_phosp_MBR: 5′-GCCACTGTGCTTCACAAACA-3′) and a probe (Rfel_phosp_MBP: 6FAM-CCGCTTCGTTATCCGTGGGACC-TAMRA) designed in our laboratory. The final mixture of the qPCR reaction was composed of 15 µL of mix that contained 10 µL of master mix QuantiTect Probe PCR Kit (QIAGEN, Hilden, Germany), 0.5 µL (20 pmol) of each primer, 0.5 µL (62.5 nmol) of probe, 3.5 µL of RNase DNase-free water and 5 µL of DNA extracted from fleas. qPCR was performed as follows: 15 min at 95°C, followed by 40 cycles of 1 s at 95°C, 40 s at 60°C and 40 s at 45°C, as described [29]. The negative control consisted of DNA extracted from uninfected fleas from our laboratory colony and was used for all the PCR assays in this work. The positive control was DNA extracted from a diluted strain of R. felis from our laboratory in Marseille. Positive results were recorded if the cycle threshold (Ct) value obtained was lower than 36 using the 2 PCR systems.
Detection of Rickettsia typhi
Samples were screened by qPCR targeting a fragment of the Rpr 274P gene coding for a hypothetical protein, as described previously [30]. Positive results were confirmed by qPCR targeting the glycosyltransferase gene using a previously described Rpr 331 system [31]. qPCR was conducted using the same method as described for R. felis detection. The positive control was DNA extracted from a diluted strain of R. typhi Wilmington (ATCC VR-144) cultured in our laboratory in Marseille.
Detection of Bartonella spp
DNA samples were screened by quantitative real-time PCR targeting the ITS region [32]. Positive samples with ITS primers were then confirmed by standard PCR performed with Bartonella-specific primers for the citrate synthase (gltA) gene, amplifying an approximately 334-bp fragment [33]. The positive control was B. alsatica strain IBS 382 (CIP 105477) DNA extracted from a strain and previously diluted to 10−6.
The success of PCR amplification was verified by 2% agarose gel migration. The products were purified using NucleoFast 96 PCR plates (Machery-Nagel EURL, France) as recommended by the manufacturer. The purified PCR products were sequenced with gltA primers using the BigDye version 1.1 cycle sequencing ready reaction mix (Applied Biosystems, Foster City, CA) with the ABI 31000 automated sequencer (Applied Biosystems). The sequences were assembled and analyzed with the ChromasPro program (version 1.5).
Detection of Yersinia pestis
DNA samples were screened by qPCR targeting the plasminogen activator gene (Pla) [6] using primers Yper_PLA_F (5′-ATG-GAG-CTT-ATA-CCG-GAA-AC-3′) and Yper_PLA_R (5′-GCG-ATA-CTG-GCC-TGC-AAG-3′) and probe Yper_PLA _P (6- FAM-TCC-CGA–AAG-GAG-TGC-GGG-TAA-TAGG-TAMRA). Positive results were confirmed with standard PCR targeting the glpD gene, as described [34], and then sequenced using the same method used for Bartonella spp. sequencing. The positive control was Y. pestis DNA extracted from the CSUR P 100 strain, and diluted to 10−6.
Results
Benin
In Benin, 886 fleas were collected from 199 sexually mature small mammals of four species, namely, Crocidura olivieri (17/199, 8.5%), Mastomys natalensis (36/199, 18%), Rattus norvegicus (40/199, 20.1%) and Rattus rattus (109/199, 54.7%). Three flea species were collected from rodents, with the oriental rat flea X. cheopis being the most abundant (861/886, 97.1%), followed by X. brasiliensis (24/886, 2.7%) and Ct. felis strongylus (1/886, 0.1%). In the present study, a convenient sample of 199 X. cheopis (picked off Rattus rattus) individuals – 55.78% females and 44.2% males – were selected for an initial molecular screening (the remaining fleas were preserved for subsequent studies).
All fleas tested negative for R. felis and Y. pestis. qPCR performed for the detection of R. typhi revealed 2 positive X. cheopis (2/199, 1%), with a Ct of 32.6 and 34.5, from 2 sites (Bokossi Tokpa and Dédokpo). Bartonella spp. were detected in 69/199 (34.6%) of the fleas (Ct, 31.81, +/−2.97) (24≤Ct≤35) collected from all studied sites (Table 1). DNA sequence analyses of the PCR products of the gltA gene of 8 representative samples (with high Ct values) showed 100% similarity with the Uncultured Bartonella sp. clone Pd5700t (GenBank no. FJ851115.1, 334/334 bp) detected in Praomys delectorum rodents in Mbulu district, northern Tanzania [19]. More information about the Ct value and localization of each positive flea is reported in Supplementary data S1.
Table 1. Distribution of the positive fleas according to species and country.
| Country | Fleas species | Total | Number of fleas positive to | ||||
| R. felis | R. typhi | Bartonella sp | Yersinia pestis | ||||
| BENIN | X. cheopis | 199 | - | 2 | 69 | - | |
| UNITED REPUBLIC OF TANZANIA | Ct. f. strongylus | 20 | 13 | - | - | - | |
| Ct. canis | 7 | 5 | - | - | - | ||
| Ct. ca. calceatus | 20 | 5 | - | - | - | ||
| X. brasiliensis | 20 | - | 2 | - | - | ||
| P. irritans | 20 | - | - | - | - | ||
| N. incisus | 7 | - | - | - | - | ||
| DEMOCRATIC REPUBLIC OF THE CONGO | ITURI (2007) | Ct. f. strongylus | 26 | - | - | - | 1 |
| E. gallinacea | 21 | - | - | - | - | ||
| P. irritans | 30 | - | - | - | 3 | ||
| X. brasiliensis | 19 | - | - | - | - | ||
| L. ae. aethiopica | 1 | - | - | - | - | ||
| T. penetrans | 26 | - | - | - | - | ||
| ITURI (2010) | Ct. f. felis | 38 | 10 | - | - | - | |
| X. cheopis | 62 | - | - | - | - | ||
| L. ae. aethiopica | 11 | 1 | - | 4 | - | ||
| KINSHASA | Ct. f. felis | 23 | 13 | - | - | - | |
United Republic of Tanzania
A total of 3821 fleas (rodent fleas and free-roaming fleas present in the environment) were collected from localities of the Lushoto district (United Republic of Tanzania) and were distributed into 23 species. A total of 94 fleas belonging to six common species were screened (Supplementary data S2) (20 Ct. f. strongylus, 7 Ct. canis, 20 Ctenophthalmus calceatus calceatus, 20 X. brasiliensis, 20 Pulex irritans and 7 Nosopsyllus incisus. All tested fleas were negative for Y. pestis and Bartonella spp. DNA. However, R. typhi DNA was detected in 10% (2/20) of X. brasiliensis collected from 2 villages (Magamba and Manolo). R. felis DNA was also detected in 20.2% (23/94) of analyzed fleas, including 65% (13/20) of Ct. f. strongylus, 71.4% (5/7) of Ct. canis and 25% (5/20) of Ct. ca. calceatus.
Democratic Republic of the Congo
In 2007, in the Linga and Rethy health zones, Ituri district, 1190 fleas captured in households, belonging to 6 species (394 P. irritans, 153 Tunga penetrans, 280 Ct. f. strongylus, 89 Echidnophaga gallinacea, 88 L. a. aethiopica and 186 X. brasiliensis). A total of 123 fleas were conveniently selected for this work (Supplementary data S3). qPCR for R. typhi and Bartonella spp. was negative for all 123 fleas; however, 4.8% (6/123), namely 19.2% (5/26) of Ct. f. strongylus and 4.7% (1/21) of E. gallinacea, contained R. felis DNA (Table 1).
Y. pestis DNA was detected in 3.8% (1/26) of Ct. f. strongylus and 10% (3/30) of P. irritans from 2 villages (Wanyale and Zaa). DNA sequence analyses of the PCR products targeting the glpD gene showed 100% similarity with Yersinia pestis Angola isolated from Angola (GenBank accession no. CP000901.1, 321/333 bp).
In 2010, 111 fleas, belonging to 3 species, were collected in the same district, namely, X. cheopis (62/111, 55.8%), Ct. f. felis (38/111, 34.2%) and L. a. aethiopica (11/111, 9.9%) (Supplementary data S4). qPCR for R. typhi and Y. pestis detection was negative for all fleas (Table 1); however, 9.9% (11/111) of two flea species (Ct. f. felis and L. a. aethiopica) were positive for R. felis. A total of 10 Ct. f. felis from 38 tested (26.3%) and one of 11 L. a. aethiopica (9%) contained R. felis. Bartonella spp DNA was detected in 3.6% (4/111) of fleas, with 36.36% (4/11) from only L. a. aethiopica. Sequencing of the gltA gene fragment from these four Bartonella-positive samples showed 100% similarity with Bartonella sp. MN-ga6 (GenBank no. AJ583126.1, 320/334 bp) detected in fleas collected in South Africa.
Finally, in 2012, from the fleas collected in Kinshasa (Table 1), 56.5% (13/23) of Ct. f. felis collected from 3 dogs was positive for R. felis but negative for R. typhi, Bartonella spp. and Y. pestis by qPCR.
Discussion
We report the first direct evidence of R. typhi and Bartonella sp. in X. cheopis fleas in Benin (Cotonou). In Lushoto (United Republic of Tanzania), we detected for the first time the presence of R. typhi DNA in X. brasiliensis and R. felis DNA in Ct. f. strongylus, Ct. canis and Ct. ca. calceatus. Finally, in the Democratic Republic of the Congo, we confirmed the presence of R. felis in Ct. felis in Kinshasa and for the first time report the presence of R. felis and Bartonella DNA in L. a. aethiopica and, most importantly Y. pestis DNA in P. irritans and Ct. felis from Wanyale and Zaa villages in the Rethy health zone.
The robustness of our results and the detection of these pathogens in fleas on rodents are supported by the use of a validated method of real-time PCR and subsequent sequencing. The validity of the data that we report is based on strict laboratory procedures and controls that are commonly used in the WHO Center for Rickettsial Diseases, including rigorous positive and negative controls to validate the test. Each positive qPCR result was confirmed by another specific qPCR or confirmed with a successful DNA amplification and sequencing.
R. typhi was detected in X. cheopis collected from Rattus rattus in Bokossi Tokpa and Dédokpo sites (Cotonou, Benin) and in X. brasiliensis from the United Republic of Tanzania. X. cheopis is the primary vector of R. typhi, the etiological agent of murine typhus (MT), in most locations around the world, and X. brasiliensis appears to be an effective vector under experimental conditions [3]. MT is most often a relatively mild disease; yet R. typhi can cause acute febrile illness and death [35]. The diagnosis of MT may be missed or underreported due to its non-specific symptoms or the absence of epidemiological criteria [36], [37] because laboratory tests and validated methods of diagnosis must be performed to confirm the diagnosis [30]. Before our study, R. typhi was never detected in Benin, and it is rarely directly reported in vectors and patients in Africa, specifically in sub-Saharan Africa. R. typhi in African fleas was only detected in X. cheopis fleas collected in Algeria [38]. Additionally, R. typhi has been reported in patients using serological methods in African countries [30]. Cases have been documented in international travelers returning from Tunisia, Morocco, Ivory Coast, Central African Republic, Madagascar, Reunion and Chad [30]. In the United Republic of Tanzania, a seroprevalence study among pregnant women from the port city of Dar es Salaam found a prevalence of 28% [39] and 0.5 to 9.3% in the town of Moshi and the Mbeya region, respectively [22], [40].
R. felis is an emergent agent of infectious disease in humans, and this agent of spotted fever is known to be maintained in cat fleas (Ct. felis) [41], [42]. To date, 12 species of fleas, 8 species of ticks and 3 species of mites have been found to be infected with R. felis [42]. This Rickettsiae has also recently been detected in several mosquito species in sub-Saharan Africa [29], [43], [44]. Interestingly, the R. felis genogroup seems large with recent organisms or genotypes related as R. felis like organisms (RFLO). Our 2 qPCR were specifically designed to amplify R. felis type strain (URRWXCal2). However, the biotin synthase and membrane phosphatase gene sequences of many RFLO are not known. We however know that at least our qPCR system targeting the biotin synthase (bioB) gene do not amplify some RFLO such as Rickettsia sp. RF2125 and Rickettsia sp. SGL01. Recently, a new qPCR assay has been proposed to address this issue by providing new qPCR primers and probe to specifically amplify R. felis OmpB gene fragments [15]. The clinical features of R. felis may include fever, fatigue, headache, generalized maculopapular rash and inoculation eschar(s) [42]. R. felis seems to be a frequent agent of unknown fever in Sub-Saharan Africa [44]. We detected R. felis in 5 species of fleas (Ct. f. strongylus, Ct. canis, Ct. ca. calceatus, L. a. aethiopica and E. gallinacea); some from the United Republic of Tanzania (Lushoto district), and other from the Democratic Republic of the Congo (Ituri District). R. felis had already been detected in the Ituri district [25], but not in E. gallinacea, the fowl flea, and has been previously shown to circulate in arthropod vectors (Ctenocephalides felis) in Kinshasa, the capital city of the country [21]. E. gallinacea is usually found on poultry, and can occurs on rodents (Rattus spp.) foraging in fowl shelters around houses [45]. While chicken DNA has been found in blood meal of fleas collected on rodents in the same area [46] other Rickettsia spp. antibodies have been found in poultry in Brazil [47], whether or not R. felis and R. typhi infects poultry or if poultry can act as a source of infection to human is unknown. Furthermore, no data on the potential vertical transmission of R. felis in E. gallinacea, or on the vectorial transmission of R. felis by E. gallinacea males (females are semi-sessile) between rodents and birds, are available. The questions raised by the findings of the present study in relation to Rickettsia in fleas are of real epidemiological significance and should be further investigated.
Molecular evidence of Bartonella sp. in fleas from the Democratic Republic of the Congo is supported by a recent serological survey in human patients in the Ituri who tested seropositive for B. henselae, B. quintana or B. clarridgeiae [18]. Gundi and collaborators also found that local rodents harbor Bartonella spp. closely related to B. elizabethae or B. tribocorum which shows that a wide variety of Bartonella species is present in the country, and differ according to host [19]. Bitam and collaborators [48] report that B. elizabethae, which causes endocarditis, and B. tribocorum are usually known to be transmitted by X. cheopis fleas. However, while in our study, we detected an Uncultured Bartonella sp., clone Pd5700t (GenBank no. FJ851115.1) in X. cheopis of Benin, we also detected Bartonella sp. MN-ga6 (GenBank no. AJ583126.1) in L. a. aethiopica, from Ituri. This Bartonella sp. had been previously found in the Democratic Republic of the Congo and the United Republic of Tanzania in rodents [19].
The detection of Y. pestis DNA in fleas collected in villages and houses where no current human plague cases had been reported for the last 6 months is puzzling. About 80 species and subspecies of Siphonaptera are known to be carriers and potentially vector of Y. pestis [49], via various transmission mechanisms [50]; in particular in fleas from the genus Xenopsylla (X. cheopis), which played a major role in historical plague pandemics [9]. In the present survey, DNA of Y. pestis was detected in the human flea, P. irritans, and the cat flea Ct. felis in a well known endemic focus of the Democratic Republic of the Congo [51]. In 2006, in the Rethy and Linga health zone more than 600 human cases were reported [52], which triggered the entomological investigation reported previously [25] and the collection of fleas analyzed herein. This survey occurred 6 months after the end of the epidemics, and at the time of the flea sampling, no confirmed human plague cases were reported to the Health centre of the villages (Zaa and Wanyale) or Rethy general Hospital. Several hypotheses can be proposed to explain this finding. A first hypothesis is that infected fleas from rodents, dogs or cats could have been imported in the infested houses, did not bite people and as such no human cases occurred, at the time of collection. A second hypothesis is that infected fleas containing Y. pestis DNA remained infected and alive without biting any potential host or that no human cases were reported to the health authorities which are unlikely due to the recent outbreak and constant surveillance. Other options are that Y. pestis DNA is reminiscent in the flea but the bacterium is either dead (degraded DNA) but the targeted sequences (gene fragment and gene flanking regions are still complete) or alive but in a quiescent form or VBNC state, possibly controlled by epigenetic mechanisms causing virulence gene repression. The human flea (P. irritans) may play an important role in spreading plague via human-to-human transmission as suggested in Lushoto district [27] and could possibly harbor Y. pestis without transmission for several months. Unfortunately no fleas were cultured in the field and the viability of the strain detected cannot be proven, but this finding calls for more research at times post outbreaks in order to answer this question. Similarly, cat fleas could play such a role both in northwest Uganda [53] and in Democratic Republic of the Congo (Laudisoit and al 2014, unpublished data), where C. felis spp. is the most common flea species collected in the domestic environment above a given altitude threshold.
In conclusion, we widened knowledge of the repertoire of flea-borne bacteria present in Sub-Saharan Africa. In our study, we also illustrate the role of fleas in the entomological survey of vector -borne disease, which allow clinicians to confirm the etiological cause for some of the unknown cause of fever in African patients. Future studies on rickettsioses, bartonelloses and other vector-borne diseases should be performed to assess their epidemiological and clinical relevance in tropical and subtropical areas, to estimate the real prevalence and to allow the establishment of antivectorial control plans.
Supporting Information
Detection of flea borne diseases in Benin.
(XLS)
Detection of flea borne diseases in United Republic of Tanzania.
(XLSX)
Detection of flea borne diseases in Ituri, Democratic Republic of the Congo.
(XLSX)
Detection of flea borne diseases in Kinshasa, Democratic Republic of the Congo.
(XLSX)
Acknowledgments
The authors are grateful to all persons who helped in this study particularly those who have helped in the trapping of rodents and collection of fleas. In particular, the authors gratefully thank Mr Jean Christophe Shako for his support in the field in Ituri, and also all the owners of dogs in the Democratic Republic of the Congo. The authors thank also Renaud Piarroux, Georges Diatta, Léon Tshilolo and Diego Latasa for help in the fleas' collection in Democratic Republic of the Congo.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1. Bitam I, Dittmar K, Parola P, Whiting MF, Raoult D (2010) Fleas and flea-borne diseases. Int J Infect Dis 14: e667–e676 S1201-9712(10)00029-9 [pii]; 10.1016/j.ijid.2009.11.011 [doi] [DOI] [PubMed] [Google Scholar]
- 2. Parola P, Davoust B, Raoult D (2005) Tick- and flea-borne rickettsial emerging zoonoses. Vet Res 36: 469–492 10.1051/vetres:2005004 [doi];v4057 [pii] [DOI] [PubMed] [Google Scholar]
- 3. Eisen RJ, Gage KL (2012) Transmission of flea-borne zoonotic agents. Annu Rev Entomol 57: 61–82 10.1146/annurev-ento-120710-100717 [doi] [DOI] [PubMed] [Google Scholar]
- 4. Drancourt M (2012) Plague in the genomic area. Clin Microbiol Infect 18: 224–230 10.1111/j.1469-0691.2012.03774.x [doi] [DOI] [PubMed] [Google Scholar]
- 5. Raoult D, Mouffok N, Bitam I, Piarroux R, Drancourt M (2013) Plague: history and contemporary analysis. J Infect 66: 18–26 S0163-4453(12)00277-0 [pii]; 10.1016/j.jinf.2012.09.010 [doi] [DOI] [PubMed] [Google Scholar]
- 6. Bitam I, Ayyadurai S, Kernif T, Chetta M, Boulaghman N, Raoult D, Drancourt M (2010) New rural focus of plague, Algeria. Emerg Infect Dis 16: 1639–1640 10.3201/eid1610.091854 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Neerinckx S, Bertherat E, Leirs H (2010) Human plague occurrences in Africa: an overview from 1877 to 2008. Trans R Soc Trop Med Hyg 104: 97–103 S0035-9203(09)00264-8 [pii]; 10.1016/j.trstmh.2009.07.028 [doi] [DOI] [PubMed] [Google Scholar]
- 8. Cabanel N, Leclercq A, Chenal-Francisque V, Annajar B, Rajerison M, et al. (2013) Plague outbreak in Libya, 2009, unrelated to plague in Algeria. Emerg Infect Dis 19: 230–236 10.3201/eid1902.121031 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andrianaivoarimanana V, Kreppel K, Elissa N, Duplantier JM, Carniel E, et al. (2013) Understanding the persistence of plague foci in Madagascar. PLoS Negl Trop Dis 7: e2382 10.1371/journal.pntd.0002382 [doi];PNTD-D-12-01523 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bertherat E, Thullier P, Shako JC, England K, Kone ML, et al. (2011) Lessons learned about pneumonic plague diagnosis from two outbreaks, Democratic Republic of the Congo. Emerg Infect Dis 17: 778–784 10.3201/eid1705.100029 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parola P, Raoult D (2006) Tropical rickettsioses. Clin Dermatol 24: 191–200 S0738-081X(05)00169-0 [pii]; 10.1016/j.clindermatol.2005.11.007 [doi] [DOI] [PubMed] [Google Scholar]
- 12. Merhej V, El KK, Raoult D (2009) Whole genome-based phylogenetic analysis of Rickettsiae. Clin Microbiol Infect 15 Suppl 2: 336–337 CLM2265 [pii]; 10.1111/j.1469-0691.2008.02265.x [doi] [DOI] [PubMed] [Google Scholar]
- 13. Nogueras MM, Pons I, Ortuno A, Miret J, Pla J, et al. (2013) Molecular Detection of Rickettsia typhi in Cats and Fleas. PLoS One 8: e71386 10.1371/journal.pone.0071386 [doi];PONE-D-13-20078 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Azad AF, Radulovic S, Higgins JA, Noden BH, Troyer JM (1997) Flea-borne rickettsioses: ecologic considerations. Emerg Infect Dis 3: 319–327 10.3201/eid0303.970308 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Odhiambo AM, Maina AN, Taylor ML, Jiang J, Richards AL (2014) Development and Validation of a Quantitative Real-Time Polymerase Chain Reaction Assay Specific for the Detection of Rickettsia felis and Not Rickettsia felis-Like Organisms. Vector Borne Zoonotic Dis 14: 476–481 10.1089/vbz.2013.1518 [doi] [DOI] [PubMed] [Google Scholar]
- 16. Chomel BB, Boulouis HJ, Breitschwerdt EB, Kasten RW, Vayssier-Taussat M, et al. (2009) Ecological fitness and strategies of adaptation of Bartonella species to their hosts and vectors. Vet Res 40: 29 10.1051/vetres/2009011 [doi];v09181 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Breitschwerdt EB, Maggi RG, Chomel BB, Lappin MR (2010) Bartonellosis: an emerging infectious disease of zoonotic importance to animals and human beings. J Vet Emerg Crit Care (San Antonio) 20: 8–30 VEC496 [pii]; 10.1111/j.1476-4431.2009.00496.x [doi] [DOI] [PubMed] [Google Scholar]
- 18. Laudisoit A, Iverson J, Neerinckx S, Shako JC, Nsabimana JM, et al. (2011) Human seroreactivity against Bartonella species in the Democratic Republic of Congo. Asian Pac J Trop Med 4: 320–322 S1995-7645(11)60094-1 [pii]; 10.1016/S1995-7645(11)60094-1 [doi] [DOI] [PubMed] [Google Scholar]
- 19. Gundi VA, Kosoy MY, Makundi RH, Laudisoit A (2012) Identification of diverse Bartonella genotypes among small mammals from Democratic Republic of Congo and Tanzania. Am J Trop Med Hyg 87: 319–326 87/2/319 [pii]; 10.4269/ajtmh.2012.11-0555 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Laudisoit A, Falay D, Amundala N, Akaibe D, de Bellocq JG, et al. (2014) High Prevalence of Rickettsia typhi and Bartonella species in Rats and Fleas, Kisangani, Democratic Republic of the Congo. Am J Trop Med Hyg ajtmh.13-0216 [pii]; 10.4269/ajtmh.13-0216 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mediannikov O, Davoust B, Socolovschi C, Tshilolo L, Raoult D, et al. (2012) Spotted fever group rickettsiae in ticks and fleas from the Democratic Republic of the Congo. Ticks Tick Borne Dis 3: 371–373 S1877-959X(12)00100-8 [pii]; 10.1016/j.ttbdis.2012.10.015 [doi] [DOI] [PubMed] [Google Scholar]
- 22. Dill T, Dobler G, Saathoff E, Clowes P, Kroidl I, et al. (2013) High seroprevalence for typhus group rickettsiae, southwestern Tanzania. Emerg Infect Dis 19: 317–320 10.3201/eid1902.120601 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Laudisoit A, Leirs H, Makundi R, Krasnov BR (2009) Seasonal and habitat dependence of fleas parasitic on small mammals in Tanzania. Integr Zool 4: 196–212 10.1111/j.1749-4877.2009.00150.x [doi] [DOI] [PubMed] [Google Scholar]
- 24. Houemenou G, Ahmed A, Libois R, Hartskeerl RA (2013) Leptospira spp. Prevalence in Small Mammal Populations in Cotonou, Benin. International Scholarly Research Notices 2013: 1–8. [Google Scholar]
- 25. Laudisoit A, Beaucournu JC (2009) [Siphonaptera from Tanzania. Description of two taxa and complementary description of Ctenophthalmus cophurus Hemingwayi Hubbard, 1963 (Siphonaptera: Ctenophthalmidae)]. Parasite 16: 275–281. [DOI] [PubMed] [Google Scholar]
- 26. Sackal C, Laudisoit A, Kosoy M, Massung R, Eremeeva ME, et al. (2008) Bartonella spp. and Rickettsia felis in fleas, Democratic Republic of Congo. Emerg Infect Dis 14: 1972–1974 10.3201/eid1412.080610 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Laudisoit A, Leirs H, Makundi RH, Van DS, Davis S, et al. (2007) Plague and the human flea, Tanzania. Emerg Infect Dis 13: 687–693 10.3201/eid1305.061084 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bitam I, Parola P, De La Cruz KD, Matsumoto K, Baziz B, et al. (2006) First molecular detection of Rickettsia felis in fleas from Algeria. Am J Trop Med Hyg 74: 532–535 74/4/532 [pii] [PubMed] [Google Scholar]
- 29. Socolovschi C, Pages F, Raoult D (2012) Rickettsia felis in Aedes albopictus mosquitoes, Libreville, Gabon. Emerg Infect Dis 18: 1687–1689 10.3201/eid1810.120178 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Walter G, Botelho-Nevers E, Socolovschi C, Raoult D, Parola P (2012) Murine typhus in returned travelers: a report of thirty-two cases. Am J Trop Med Hyg 86: 1049–1053 86/6/1049 [pii]; 10.4269/ajtmh.2012.11-0794 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Socolovschi C, Mediannikov O, Sokhna C, Tall A, Diatta G, et al. (2010) Rickettsia felis-associated uneruptive fever, Senegal. Emerg Infect Dis 16: 1140–1142 10.3201/eid1607.100070 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Varagnol M, Parola P, Jouan R, Beaucournu JC, Rolain JM, et al. (2009) First detection of Rickettsia felis and Bartonella clarridgeiae in fleas from Laos. Clin Microbiol Infect 15 Suppl 2: 334–335 CLM2272 [pii]; 10.1111/j.1469-0691.2008.02272.x [doi] [DOI] [PubMed] [Google Scholar]
- 33. Norman AF, Regnery R, Jameson P, Greene C, Krause DC (1995) Differentiation of Bartonella-like isolates at the species level by PCR-restriction fragment length polymorphism in the citrate synthase gene. J Clin Microbiol 33: 1797–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Drancourt M, Signoli M, Dang LV, Bizot B, Roux V, et al. (2007) Yersinia pestis Orientalis in remains of ancient plague patients. Emerg Infect Dis 13: 332–333 10.3201/eid1302.060197 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Adjemian J, Parks S, McElroy K, Campbell J, Eremeeva ME, et al. (2010) Murine typhus in Austin, Texas, USA, 2008. Emerg Infect Dis 16: 412–417 10.3201/eid1603.091028 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nogueras MM, Cardenosa N, Sanfeliu I, Munoz T, Font B, et al. (2006) Evidence of infection in humans with Rickettsia typhi and Rickettsia felis in Catalonia in the Northeast of Spain. Ann N Y Acad Sci 1078: 159–161 1078/1/159 [pii]; 10.1196/annals.1374.028 [doi] [DOI] [PubMed] [Google Scholar]
- 37. Civen R, Ngo V (2008) Murine typhus: an unrecognized suburban vectorborne disease. Clin Infect Dis 46: 913–918 10.1086/527443 [doi] [DOI] [PubMed] [Google Scholar]
- 38. Bitam I, Baziz B, Kernif T, Harrat Z, Parola P, et al. (2009) Molecular detection of Rickettsia typhi and Rickettsia felis in fleas from Algeria. Clin Microbiol Infect 15 Suppl 2: 255–256 CLM2275 [pii]; 10.1111/j.1469-0691.2008.02275.x [doi] [DOI] [PubMed] [Google Scholar]
- 39. Anstey NM, Tissot DH, Hahn CG, Mwaikambo ED, McDonald MI, et al. (1997) Seroepidemiology of Rickettsia typhi, spotted fever group rickettsiae, and Coxiella burnetti infection in pregnant women from urban Tanzania. Am J Trop Med Hyg 57: 187–189. [DOI] [PubMed] [Google Scholar]
- 40. Prabhu M, Nicholson WL, Roche AJ, Kersh GJ, Fitzpatrick KA, et al. (2011) Q fever, spotted fever group, and typhus group rickettsioses among hospitalized febrile patients in northern Tanzania. Clin Infect Dis 53: e8–15 cir411 [pii]; 10.1093/cid/cir411 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. La SB, Meconi S, Fenollar F, Rolain JM, Roux V, et al. (2002) Emended description of Rickettsia felis (Bouyer et al. 2001), a temperature-dependent cultured bacterium. Int J Syst Evol Microbiol 52: 2035–2041. [DOI] [PubMed] [Google Scholar]
- 42. Parola P (2011) Rickettsia felis: from a rare disease in the USA to a common cause of fever in sub-Saharan Africa. Clin Microbiol Infect 17: 996–1000 10.1111/j.1469-0691.2011.03516.x [doi] [DOI] [PubMed] [Google Scholar]
- 43. Keita AK, Socolovschi C, Ahuka-Mundeke S, Ratmanov P, Butel C, et al. (2013) Molecular evidence for the presence of Rickettsia felis in the feces of wild-living African apes. PLoS One 8: e54679 10.1371/journal.pone.0054679 [doi];PONE-D-12-33654 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 44. Mediannikov O, Socolovschi C, Edouard S, Fenollar F, Mouffok N, et al. (2013) Common epidemiology of Rickettsia felis infection and malaria, Africa. Emerg Infect Dis 19: 1775–1783 10.3201/eid1911.130361 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kapoor R, Elston DM (2012) What's eating you? The sticktight flea (Echidnophaga gallinacea). Cutis 89: 157–158. [PubMed] [Google Scholar]
- 46. Woods ME, Montenieri JA, Eisen RJ, Zeidner NS, Borchert JN, et al. (2009) Identification of flea blood meals using multiplexed real-time polymerase chain reaction targeting mitochondrial gene fragments. Am J Trop Med Hyg 80: 998–1003 80/6/998 [pii] [PubMed] [Google Scholar]
- 47. Maciel JF, Krawczak FdS, Oliveira CSd, Moraes-Filho J, Labruna MB, et al. (2013) Detection of anti: Rickettsia spp. antibodies in domestic chickens of extensive breeding in an endemic area for spotted fever in the state of Rio Grande do Sul, Brazil. Ci_Òncia Rural 43: 2037–2041. [Google Scholar]
- 48. Bitam I, Dittmar K, Parola P, Whiting MF, Raoult D (2010) Fleas and flea-borne diseases. Int J Infect Dis 14: e667–e676 S1201-9712(10)00029-9 [pii]; 10.1016/j.ijid.2009.11.011 [doi] [DOI] [PubMed] [Google Scholar]
- 49. Hinnebusch BJ (2005) The evolution of flea-borne transmission in Yersinia pestis . Curr Issues Mol Biol 7: 197–212. [PubMed] [Google Scholar]
- 50. Eisen RJ, Bearden SW, Wilder AP, Montenieri JA, Antolin MF, et al. (2006) Early-phase transmission of Yersinia pestis by unblocked fleas as a mechanism explaining rapidly spreading plague epizootics. Proc Natl Acad Sci U S A 103: 15380–15385 0606831103 [pii]; 10.1073/pnas.0606831103 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Janssens PG, Pattyn SR (1994) [Plague in Zaire]. Verh K Acad Geneeskd Belg 56: 281–360. [PubMed] [Google Scholar]
- 52. WORLD HEALTH ORGANIZATION Geneva (2006) Plague, Democratic Republic of the Congo. Weekly epidemiological record 25: 241–248. [Google Scholar]
- 53. Stenseth NC, Atshabar BB, Begon M, Belmain SR, Bertherat E, et al. (2008) Plague: past, present, and future. PLoS Med 5: e3 06-PLME-ND-0545 [pii]; 10.1371/journal.pmed.0050003 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detection of flea borne diseases in Benin.
(XLS)
Detection of flea borne diseases in United Republic of Tanzania.
(XLSX)
Detection of flea borne diseases in Ituri, Democratic Republic of the Congo.
(XLSX)
Detection of flea borne diseases in Kinshasa, Democratic Republic of the Congo.
(XLSX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.