Abstract
Objective To evaluate and quantify the evidence for health promotion interventions in children and adolescents. Method 96 independent samples of smoking, physical activity, and diet studies were included. Outcomes included both objective and self-reports of health behavior, as well as proxy measures such as fitness. Results The aggregated effect was significant (g = .20, 95% confidence interval [CI] = 0.08–0.32, n = 96). A significant effect of intervention was observed at approximately 1-year follow-up (g = .07, 95% CI = 0.02–0.14, n = 20). The greatest risk of bias was failure to blind outcome assessment, which occurred in 21% of studies. Most studies lacked sufficient detail to determine the quality of their randomization sequence (58%). Additional concerns about risk of bias for individual studies were minimal. Overall, the quality of this finding was moderate using the Grading of Recommendations Assessment, Development, and Evaluation criteria. Conclusion Health promotion interventions are effective for modifying health behavior; however, effect sizes are small.
Keywords: health behavior, health promotion and prevention, meta-analysis, public health
Individual health behavior is the largest single contributor to the development of preventable chronic illnesses such as obesity, cardiovascular disease, stroke, diabetes, and cancer (Ford, Li, Zhao, & Tsai, 2011; Mokdad, Marks, Stroup, & Gerberding, 2004). In 2008, obesity costs were estimated at approximately 147 billion dollars in the United States. Moreover, costs are expected to rise exponentially, resulting in 22 billion in additional spending each year through 2020; increasing to 66 billion additional dollars per year through 2030 (Finkelstein, Trogdon, Cohen, & Dietz, 2009; Wang, McPherson, Marsh, Gortmaker, & Brown, 2011). Beyond its financial impact, obesity is expected to cost between 26 and 55 million quality-adjusted life years by 2030; meaning that not only will costs increase, but individuals with obesity will experience earlier mortality and reduced quality of life (Wang et al., 2011). Similarly, other health behaviors such as tobacco use account for at least 18.1% of all deaths in the United States and amount to nearly 200 billion dollars in direct and indirect costs annually (Adhikari, Kahende, Malarcher, Pechacek, & Tong, 2009). In light of these statistics, increasing knowledge about what types of health promotion interventions are most effective for improving health behaviors in children and adolescents is critical for policy makers and interventionists working to improve health outcomes (Fisher et al., 2011).
Childhood and adolescence represent important developmental periods where lifelong habits can be established to promote healthy lifestyles and reduce the risk of chronic disease in early adulthood. It is critical to target health behaviors as a method of primary prevention early in the developmental course because children and adolescents who do not participate in adequate physical activity, have a poor diet, and begin smoking are at increased risk for continuing these patterns and risk for the development of poor health as adults (Centers for Disease Control and Prevention, 2012; Dietz, 1998). Despite the potential of early prevention efforts, children and adolescents present a unique challenge for health promotion programs because their behavior is influenced by multiple ecological systems and individual factors including their developmental age, family system, culture, communities, school systems, and policies that govern these systems (Wilson & Lawman, 2009).
While the existing literature lacks an ecological systems approach, previous systematic reviews have addressed health promotion and prevention in children and adolescents. In a comprehensive review of obesity prevention programs Stice, Shaw, and Marti (2006) discovered that interventions were effective at reducing the potential for elevated body mass index (BMI) scores, with 21% of studies demonstrating positive findings. However, Stice et al. (2006) used a disease-centric approach and targeted only trials that examined BMI as a dependent variable. The decision to use a disease-centric approach rather than examining weight-related health behaviors was based on the evidence that trials can produce changes in diet and physical activity without changing BMI (Baranowski et al., 2003; Luepker et al., 1996).
Similarly, a more restrictive meta-analysis with an obesity intervention/prevention orientation reviewed physical activity interventions evaluated using accelerometers (Metcalf, Henley, & Wilkin, 2012). The review noted that intervention programs, on average, have relatively small effects. However, the current study expands on past research by explaining variability in effect sizes using study-level variables to explore the relative impact of intervening at various ecological systems (e.g., family, school, community, media, or with the individual).
Behavior change is not only important in the context of obesity prevention and associated behaviors; significant attention has also been paid to preventing the smoking of combustible tobacco. Reviews of tobacco prevention programs have been mixed in terms of the conclusions regarding effectiveness. However, the balance of the evidence suggests that programs can be effective at preventing the smoking of combustible tobacco in nonsmokers (Dobbins, Decorby, Manske, & Goldblatt, 2008), but that the effects may not last over time. In one example, Wiehe, Garrison, Christakis, Ebel, and Rivara (2005) found that school-based prevention interventions demonstrated no effect in long-term prevention of smoking. The decline in effectiveness appears to be due to the lack of sustained intervention through adolescence (Dobbins et al., 2008). Similarly, reviews of specific programs such as the Life Skills Training program are available (Botvin & Griffin, 2004). While most school-based studies do tend to show an effect, it appears that the effects are typically small. For this reason, it is important to determine what other systems may be amenable to intervention (e.g., family, community).
Programs designed to promote health in children and adolescents commonly target one or more systems that influence health behavior (Kazak et al., 2010; Wilson & Lawman, 2009; Wilson, 2009). While many individual programs demonstrate effectiveness, there remains a dearth of literature specifically examining what level of intervention (e.g., family, school, community, and media) is ideal for promoting change in a child’s behavior, and whether certain systems are more important for a particular behavior. In fact, no systematic review of the literature is available to guide policy makers regarding the highest value ecological system for deploying health promotion interventions. Such knowledge is critical to guiding resource allocation when policy makers set goals of changing one or more pediatric health behaviors. Evidence-informed estimates may serve to reduce the economic burden of poor health behaviors of individuals over the life span.
The current review offers a behavior-centric rather than disease-centric approach to health promotion. This approach is valuable, given that health behavior has multiple effects on biological, cognitive, and social systems that are vital to child development beyond their value for preventing disease. For example, children who engage in greater frequency and duration of physical activity demonstrate higher rates of academic and cognitive performance, higher quality of life, and increased neuroelectrical activity and blood flow in critical brain regions mediating executive functioning and achievement regardless of weight status (Davis et al., 2011; Pontifex, Saliba, Raine, Picchietti, & Hillman, 2012; Shoup, Gattshall, Dandamudi, & Estabrooks, 2008). The behavior-centric approach treats all behaviors as the same initially with the question, “can intervention programs modify health promoting behaviors?” Follow-up questions can then be addressed such as “are the findings uniform across different types of behavior?” Finally, there is also a technical benefit of the behavior-centric approach in which multiple health behaviors are aggregated. Such an aggregation allows for more pooled studies that can extend the traditional question of systematic review and meta-analysis, “do health promotion interventions change behavior” to address theoretical questions such as “what ecological systems are most important for changing behavior within a health promotion intervention?” This second question is the real innovation in the current review, and may help develop a research agenda to guide future policymaking efforts.
The current review has three primary objectives: (1) to evaluate the overall effectiveness of health promotion interventions in children and adolescents, (2) to evaluate the stability of health promotion intervention effects over the course of approximately 1 year post-intervention, and (3) to provide preliminary evidence of the ecological systems that are most impactful of study effect sizes. With regard to Aim 1, it was hypothesized that interventions would produce a significant effect on pediatric health behavior. With regard to Aim 2, it was hypothesized that health promotion interventions would have a significant lasting effect at approximately 1-year follow-up assessment. The longitudinal effect was hypothesized because behavior change programs are designed to transmit lasting individual skills even if delivered in a school, community, or via the media. Finally, with regard to Aim 3, analyses were planned to shed light on the ecological systems that are most meaningful for intervention planning both across and within the three selected health behaviors.
Methods
Literature Search
Electronic database served as the primary method of identifying eligible studies. Manual searches of relevant papers were also carried out. The current review also conducted backward reference searches of other reviews, requested information from study authors, and consulted with experts in health promotion.
Electronic Searches
Literature searches were conducted in PsychINFO, PUBMED/MEDLINE, and Educational Resources Information Center (ERIC). Primary search terms included health promotion, public health program, community-based*, public health intervention*, primary care prevention, physical activity, exercise, diet*, and tobacco prevention. The wildcard symbol (*) was used to ensure that variations of key search terms were retrieved. Each of the primary search terms was combined with secondary search terms, child* and adolescen*, for a total of 48 searches across all three databases. Search limiters were applied to exclude studies with samples of individuals who were 18 years of age or older and those written in a language other than English. Searches were conducted through April 1, 2013.
Health Promotion Definition
We use a definition of health promotion based on The Bangkok Charter for Health Promotion in a Globalized World (World Health Organization [WHO], 2006): Health promotion is the process of enabling people to increase control over their health and its determinants, and thereby improve their health.1 The current review combines this definition with a primary prevention approach to health. That is, studies included in the review are limited to those targeting children and adolescents who were not affected by a particular disease or disorder at the time of the intervention. This limitation was placed on the literature because other topical reviews in the current special issue will address secondary and tertiary prevention directly within their respective disorders (e.g., obesity and diabetes).
Inclusion/Exclusion Criteria
The current review sought to examine only randomized controlled trials (RCTs) of health promotion interventions. Studies were included in the current review if they: (1) examined a health behavior (e.g., smoking, physical activity, or diet) as a dependent variable, (2) were written in English, (3) reported on the health behavior of children and adolescents (i.e., ≤ 18 years) who were not chronically ill (e.g., obesity, cancer, asthma) during the study period, (4) were published in a peer-reviewed journal, (5) did not include a medical intervention (e.g., studies were excluded if the intervention was specific dietary modification with no behavioral component, medication, or procedures), and consistent with the recommendations of the Society of Pediatric Psychology Committee on Science and Practice (6) had at least 10 subjects in the treatment and control groups.
Data Extraction and Management
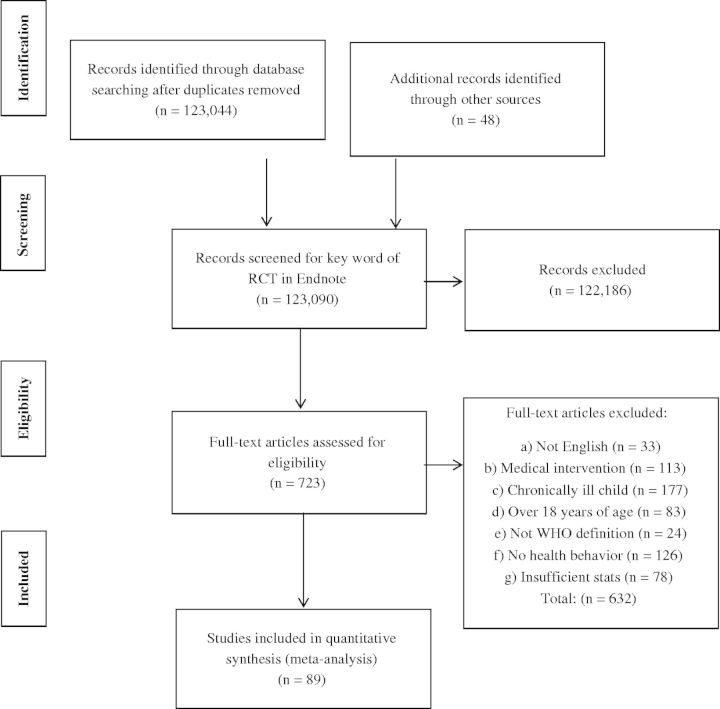
Exclusion criteria were applied in a specific order, such that while a study might be ineligible for several reasons, it would only contribute to the n-size for the first criterion met in the following list. Articles were excluded if: (a) the article was not written in English (n = 33), (b) the study reported exclusively on outcomes of a medical intervention (n = 111), (c) the study population was chronically ill (n = 177), (d) the outcome included participants who were aged 18 years or over (n = 83), (e) the study did not fit the definition of health promotion as defined by the WHO (n = 24), (f) no health behaviors that affect health promotion were targeted for intervention (n = 126), (g) the article failed to include sufficient statistical information to compute an effect size (n = 78), and (h) the study sample was already included in the current review (n = 2; see Figure 1 for a PRISMA flowchart).
Figure 1.
PRISMA flowchart.
Following application of the inclusion/exclusion criteria, the search yielded 96 independent samples contributing 521 effect sizes at post-treatment. The total number of independent samples exceeds the number of papers (n = 89) because seven studies divided the sample into boys and girls. In these cases, the sample was analyzed as an independent sample effect size even though both were contained in the same written report. Of these, 20 samples provided an additional 261 effect sizes at approximately 1-year follow-up.
Type of Outcomes
Pediatric health promoting behaviors are the primary focus of this review. As has been done in previous reviews (Cushing & Steele, 2010), the current study examined multiple behavioral outcomes that are associated with health in children and adolescents. These include: (1) physical activity, (2) diet (all categories of dietary intake), and (3) tobacco use prevention. A range of strategies were observed for assessing these three independent variables. Studies were not evaluated for the quality of their dependent variable measurement; however, self-report, objective measurement, and/or a proxy measure (fitness level) were all equally weighted in the analysis. Outcomes were gathered from the first post-treatment assessment and the follow-up period closest to 1-year post-intervention.
Type of Participants
For all 89 unique papers included in the analysis, the total sample size was 131,982 children and adolescents (excluding one study that enrolled 90 households, but did not give a specific sample size; French, Gerlach, Mitchell, Hannan, & Welsh, 2011). Thirteen of the studies (14.9%) included exclusively female samples and five studies (5.7%) were completed with exclusively male samples, while the remainder of the studies (76.3%) included mixed-sex samples. The overall sample was 46.5% male (excluding three studies that did not indicate the percent of males included in their sample), with an average age of 11.9 years (excluding 20 studies that did not indicate the average age of their sample). Participant ethnicity was as follows: 23.2% White, 8.3% African American, 9.6% Hispanic, 1.4% Asian, 1.0% Mexican American, 0.4% Native American, 0.4% Native Hawaiian, 14.7% other, and 41.0% missing (see online supplementary materials for more information on study characteristics).
Data Extraction and Coding
Data Extraction Procedures
Two study authors (E.E.B. and K.I.S.) categorized all articles and extracted data from the final sample. The first author randomly assessed accuracy (10% of studies), and disagreements were resolved through discussion.
Health Promoting Behaviors
Study outcome data were abstracted for physical activity, dietary, and smoking behavior variables. Any variable used to assess any of these outcomes was coded. There are several methodological advantages to this strategy. First, it means that studies that report significant findings as “primary” with nonsignificant findings as “secondary” or “exploratory” are treated the same as those that transparently report all a priori hypotheses and outcome variables. Second, it provides an overall picture of the health promotion landscape rather than focusing narrowly on studies that use ideal assessment measures (e.g., accelerometers in physical activity interventions). This is an advantage because funded trials and studies are more likely to include ideal assessment, and may not be representative of the overall literature.
In the domain of physical activity, effect sizes were calculated for self-report, objectively assessed physical activity, and fitness tests. Dietary behavior was assessed using semi-structured food recalls, self-report diet logs, self-reported recall, and structured food recall. Smoking was assessed using self-report of smoking behavior. One of the most obvious sources of variability in the assessment strategies noted earlier is among studies using accelerometers to objectively assess physical activity compared with self-report. While self-reported physical activity is correlated with accelerometer data (Pate, Ross, Dowda, Trost, & Sirard, 2003), these correlations tend to be moderate. For that reason, objectively assessed physical activity was examined both in aggregate with self-report and separately.
Coding Ecological Variables
A coding manual with standardized definitions of study characteristics was used for coding intervention characteristics. Each study characteristic was coded categorically as present or absent. Intervention characteristics included whether the intervention acted: (1) directly on the target child, (2) on the family, (3) on the child’s school, (4) on the child’s community (e.g., providing community resources or training community members to promote health), or (5) using print or digital media. One important note with regard to school interventions is that studies were considered to be acting on the child’s school only if the program delivered a long-term change in curriculum, environment, or student activities. Delivering a small number of intervention strategies in the child’s school was considered an intervention directly on the child because the school merely serves as the setting for the program. To aid in determining what combinations of ecological interventions produce the largest effect, numeric codes were assigned to all of the combinations of the characteristics noted earlier.
Assessment of Risk of Bias in Included Studies
Studies were coded for limitations in design and implementation using the Cochrane Collaboration Risk of Bias Tool (Higgins & Green, 2011), which included risks related to: (1) random sequence generation, (2) allocation concealment, (3) blinding of outcome assessment, (4) incomplete outcome data, and (5) selective reporting. Each of these five domains was examined across all included studies to determine whether the risk of bias introduced was high, unclear, or low.
Calculation of Effect Size
All study effect sizes were expressed as Hedges’ g. To assist with data management and computation, the software program Comprehensive Meta-Analysis Version 2.2.064 was used. A wide range of study statistics were entered and used to compute effect sizes. These included, means and standard deviations (SDs), p values and sample sizes, t-statistics, F-tests, and effect sizes (Cohen’s d) reported by study authors (see Durlak, 2009, or Lipsey & Wilson, 2001, for formulas needed to calculate effect sizes).
Aggregate Effect Sizes
We included multiple health behaviors in the current review. Effect sizes were first aggregated within subgroup based on the type of health behavior or outcome assessed (i.e., diet, self-reported physical activity, objective physical activity, fitness testing, and smoking), and then an overall aggregate effect size was calculated. This allows for evaluations of multiple assessment methodologies within a given health behavior before aggregating within and across the various behaviors. For example, we were able to observe the aggregate effect size for all studies that used fitness testing, objective assessment, and self-report within physical activity interventions before aggregating these to form the final composite both within and across health behaviors. All aggregate effect sizes are reported as random-effects models to help reduce the likelihood that study-level error could inflate the estimates or bias the confidence bands (Lipsey & Wilson, 2001).
Quality of the Evidence
The quality of the evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria (Guyatt et al., 2011). For each outcome, studies included in the analysis were assessed on five categories, risk of allocation bias, indirectness, inconsistency, imprecision, and publication bias. This provided an overall rating of the quality of evidence for each outcome from high, moderate, low, or very low. Each study included in the review was an RCT, and therefore, the evidence for aggregate effect sizes begins at a high level of quality. The overall quality was then downgraded if necessary as each aforementioned domain was assessed.
Data Analysis Plan
To ensure appropriate weighting of each individual study included in the meta-analysis, studies contributing multiple outcomes were aggregated such that each one contributed a single effect size to the analysis. This approach results in more accurate standard errors and reduces bias that can result from treating nonindependent studies as independent (Gleser & Olkin, 1994). To arrive at these aggregated outcomes, each health behavior was treated as a subgroup within studies before being combined with other effect sizes. As an example, if a study used two dietary outcomes and two physical activity outcomes, two effect sizes were calculated for that study (i.e., one for diet and one for physical activity). Then, in the overall effect size aggregation, these two effects were combined with all other outcomes. All effect sizes were converted to Hedges’ g to allow comparisons across studies. Cohen (1988) provided guidelines for interpreting effect sizes; by assigning qualitative descriptors as follows: 0.20–0.49 as small, 0.50–0.79 as medium, and 0.80 and above as large.
Heterogeneity in the effect sizes was assessed using the Q-statistic. A heterogeneous Q-statistic informs the meta-analyst that there is systematic variability in the sample of study effect sizes. At the point that such heterogeneity is discovered, there are three options. First, the analyst can conclude that while the variability is not random, it cannot be explained by theoretically meaningful moderators, and end their analysis. Second, the analyst can compare meaningful groupings of studies in an attempt to explain the variability much in the same way an analysis of variance (ANOVA) would explain systematic variability using levels of an independent variable. Finally, the analyst can attempt to use meta-regression to predict the variability in effect sizes using theoretically meaningful moderators as independent variables (please see Lipsey & Wilson, 2001, for a more detailed description of these approaches). In the current study, variability in the study effect sizes was examined using the analogue to the ANOVA comparing 14 different levels of the independent variable derived from the available combinations of ecological systems interventions (i.e., individual, individual + school, individual + school + community, and so on). Comprehensive Meta-Analysis Version 2.2.064 was used to conduct the comparison of the 14 different levels of the independent variable. A mixed-effect ANOVA was conducted, and a significant between-group Q-statistic was taken to indicate significance of the comparisons (Lipsey & Wilson, 2001). However, because of the lack of statistical power to detect between-group effects at 14 levels, exploratory analyses were planned to estimate an aggregate random-effect size and compute a confidence band for each of the 14 conditions. Type of outcome assessment was examined as a moderator using a mixed-effect ANOVA in an attempt to determine whether assessing smoking, fitness, self-reported physical activity (minutes in moderate to vigorous activity, meeting recommended guidelines, active commuting to school), objective physical activity, or diet could explain variability in study effect size (calories consumed, fruit and vegetable consumption, high fat and sugar consumption, sugar-sweetened beverages).
Results
Risk of Bias
Risk of bias ratings revealed that most studies lacked sufficient detail to determine the quality of their randomization sequence, with 58% of studies receiving an unclear rating. The majority of studies (94%) demonstrated low risk of bias related to allocation concealment. The greatest risk observed in the current sample of studies was failure to blind outcome assessment, with 21% of studies demonstrating high risk in this area. Incomplete outcome data and selective reporting of outcomes were relatively infrequent (7% and 4% of studies, respectively). Please see Figure 2 for a graphical display of the risk of bias information.
Figure 2.
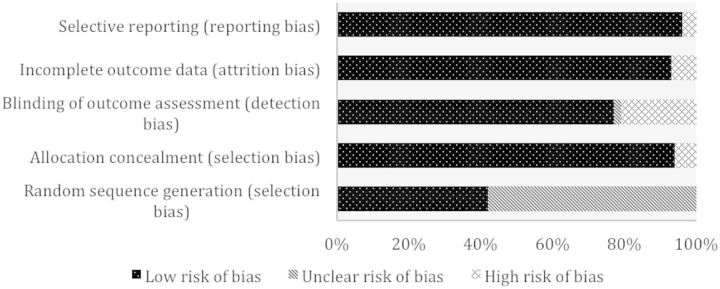
Risk of bias graph.
Adverse Events
Of the studies reviewed, only four made any mention of adverse events. Only one study (Beech et al., 2003) reported an injury to two participants that may have been due to study participation. Due to the low rate of reporting, it is impossible to determine whether health promotion interventions are likely to cause adverse events.
Aggregate Hedges’ g
The aggregate random-effects effect size was small but significant (g = .20, 95% confidence interval [CI] = 0.08–0.32, n = 96). This suggests that health promotion interventions can have a small, but significant, positive effect on pediatric health behavior. However, the Q-statistic evaluating variability in the aggregated effect sizes was significant (Q = 10060.21, p < .05, df = 95), indicating that there is significant variability among the effect sizes. This suggests that the planned follow-up moderator analysis is warranted. A classic fail-safe N calculation indicated that 30,816 null studies would be required to change the current findings from significant to nonsignificant. This yields confidence that the significant aggregated effect is unlikely to be spurious or inflated as a result of an abundance of unpublished null results.
ANOVA Examining Different Outcome Measures
The ANOVA comparing the five outcome measures (smoking, fitness, self-reported physical activity, objective physical activity, and diet) did not reveal significant between-group variability (Qb = 2.35, p < .05, df = 95). This indicates that examining the different types of outcome measures independently would not eliminate the heterogeneity in the study effect sizes. Therefore, the aforementioned results can be taken as representative of health promotion interventions generally at this stage in the literature.
Long-Term Effects of Health Promotion Interventions
To test the stability of the treatment effects observed in the aggregate analysis, studies with follow-up data were meta-analyzed. Again, while the Q-statistic was significant for this effect size (Q = 41.42, p < .05), none of the predictors for the meta-regression emerged as significant predictors, which is most likely due to low statistical power. For this reason, the random-effects aggregate effect size was examined. Health promotion interventions demonstrated a small, but significant, positive effect on pediatric health behavior at follow-up (g = .07, 95% CI = 0.02–0.14, n = 20). This suggests that health promotion interventions continue to have an effect on behavior at approximately 1-year follow-up. No moderators of effect size were examined for long-term effects due to the low statistical power to detect a difference.
ANOVA Examining the Effect of Interventions at Differing Ecological Levels
Similar to the aforementioned heterogeneity analysis, the ANOVA examining the 14 levels of different ecological systems interventions was also not significant (Qb = 7.32, p > .05, df = 95). However, planned exploratory analyses were undertaken to determine which of the levels of the independent variable were statistically significant.
Exploratory Investigation of Combinations of Ecological Systems
To determine if there was a synergistic effect of intervening simultaneously in multiple ecological systems, random-effects models were calculated for each unique cluster of ecological systems coded in the meta-analysis. Significant random-effect sizes were observed for studies that intervened only at the individual level (g = .26, 95% CI = 0.08–0.44, n = 13), with individuals and communities (g = .35, 95% CI = 0.06–0.65, n = 4), and with individuals and families (g = .31, 95% CI = 0.10–0.52, n = 11). At the aggregate level, there is evidence that multiple strategies for structuring health promotion interventions can be effective, and investigating what combinations are most effective for a given health behavior may be of importance.
Ecological Systems in Individual Health Behaviors
In addition to the aforementioned analysis of the aggregate effect size, the unique ecological systems categories were applied to the individual health behaviors that make up the aggregate effect size models. However, there was not sufficient variability in intervention design to compare smoking interventions.
In studies targeting dietary behavior, significant random-effects models were observed for interventions targeting individuals (g = .20, 95% CI = 0.06–0.33, n = 8); schools (g = .09, 95% CI = 0.00–0.17, n = 10); individuals, families, and schools (g = .13, 95% CI = 0.05–0.21, n = 12); individuals and families (g = .19, 95% CI = 0.08–0.31, n = 10); and communities and schools (g = .71, 95% CI = 0.36–1.01, n = 2). Of particular interest to the question of ecological synergy, interventions that targeted schools and communities were significantly more effective than those that targeted schools alone. This suggests that for dietary interventions, adding a community component can significantly magnify the effect of already efficacious school interventions.
Studies targeting physical activity as a dependent variable produced significant random-effect sizes if they intervened with individuals (g = .27, 95% CI = 0.12–0.42, n = 10); individuals and families (g = .44, 95% CI = 0.23–0.66, n = 6); or individuals, schools, and with media (g = .30, 95% CI = 0.04–0.57, n = 2). The results of these studies suggest that for modifying physical activity, health promotion interventions targeting individuals and their families produce larger effect sizes.
Objectively Assessed Physical Activity
As noted earlier, there is strong reason to believe that objectively assessed physical activity would yield smaller effect sizes than other methods of assessing physical activity. Even though the ANOVA attempting to explain heterogeneity by using outcome measures as a study variable was not significant, it is possible that this could be due to a Type II error as a consequence of low sample size. For this reason, trials using accelerometers were analyzed separately. As would be expected based on previous systematic reviews (Metcalf et al., 2012), the 20 effect sizes that used objective assessment yielded small effect sizes (g = .04) and less variability (95% CI = 0.01–0.07) than the aggregate physical activity studies. However, these effect sizes are similar to the aggregate physical activity data in that they are small, but significant. Comparatively, these studies yielded a statistically significantly smaller aggregate effect size than those using self-report or fitness testing. Among studies that objectively assessed physical activity, those producing significant effect sizes intervened with families, individuals, and schools (g = .08, 95% CI = 0.03–0.15, n = 2) or with families and individuals (g = .53, 95% CI = 0.09–0.98, n = 2). Similar to findings combining a broader range of outcomes, these findings suggest that to produce a significant effect, it is necessary to intervene directly with the individual child or adolescent, and including the family amplifies intervention effectiveness.
Quality of the Evidence
The evidence for overall health promotion interventions was downgraded to moderate due to inconsistency of reported effect sizes and risk of bias (Table I). The rating of moderate means that future research is likely to have a meaningful impact on confidence in the effect size estimate and that with accumulating evidence, the conclusions may change. Few studies in the review involved blinding outcome assessment. The GRADE rating for smoking behavior was rated as moderate due to findings of imprecision and inconsistency. The effect sizes of the individual studies varied greatly, and the effect is uncertain due to the variation in CIs. Finally, the evidence for physical activity and diet was downgraded to moderate as a result of the inconsistency in reported study effects, and inconsistency in outcomes such as objective versus subjective measures of the dependent variable. There was heterogeneity in the magnitude of the effects, making the moderator analysis particularly important.
Table I.
Summary of Findings: Behavioral Therapies for Health Promotion in Children and Adolescents
| Behavioral therapies for health behavior change (diet, physical activity, sedentary behavior, smoking) in children and adolescents | ||||||
|---|---|---|---|---|---|---|
| Patient or population: Children and adolescents with no physical illness or health condition | ||||||
| Settings: Community, school, and outpatient care | ||||||
| Intervention: Health promotion interventions | ||||||
| Outcomes | Illustrative probable outcomes (95% CI) |
Relative effect (95% CI) and NNT | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Probable outcome within control | Probable outcome within intervention | |||||
| Control | Behavioral therapies | |||||
| Overall | The mean health behavior change in the intervention groups was 0.20 SDs higher (0.08 to 0.32 higher) | 127,271 (96 studies) | ⊕⊕⊕⊖ | g = .20 (.08 to .32) | ||
| Moderate | Results were statistically significant | |||||
| Physical activity | The mean physical activity in the intervention groups was 0.16 SDs higher (0.10 to 0.21 higher) | 47,634 (58 studies) | ⊕⊕⊕⊖ | g = .16 (.10 to .21) | ||
| Moderate | Results were statistically significant | |||||
| Diet | The mean diet change in the intervention groups was 0.14 SDs higher (0.10 to 0.18 higher) | 35,211 (56 studies) | ⊕⊕⊕⊖ | g = .14 (.10 to .18) | ||
| Moderate | Results were statistically significant | |||||
| Smoking | The mean smoking behavior in the intervention groups was 0.22 SDs lower (0.19 lower to 0.64 higher) | 40,982 (14 studies) | ⊕⊕⊕⊖ | g = .20 (−.18 to .59) | ||
| Moderate | Results were statistically significant | |||||
| GRADE Working Group grades of evidence: | ||||||
| High quality: Further research is very unlikely to change our confidence in the estimate of effect. | ||||||
| Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. | ||||||
| Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. | ||||||
| Very low quality: We are very uncertain about the estimate. | ||||||
Discussion
The current study is a meta-analysis of health promotion interventions targeting diet, physical activity, and smoking behaviors. In aggregate, the observed effect sizes suggest that health promotion interventions are effective for modifying children and adolescent’s health behavior. However, any change in children and adolescent’s behavior is likely to be of a small magnitude. Given that effect sizes are small, it is important to understand as much variability as possible to maximize our understanding of the factors that can produce effects at the top end of the distribution. Exploratory analyses revealed that while adding support in other ecological systems can be valuable, it is still important to focus intervention efforts on the individual child or adolescent, with two notable exceptions. That is, it appears that there may be merit in school-based interventions targeting smoking and dietary behavior. Additionally, studies intervening in both school and community systems appear to produce a medium effect size for dietary outcomes. Finally, in a small sample of studies including follow-up data (n = 20), it appears that health promotion interventions can retain their (qualitatively small) effects for up to 1 year following the completion of the intervention.
These findings must also be characterized in the context of the quality of the studies that provided the effect sizes. Many studies failed to report the random sequence generation and did not blind participants or staff. As noted earlier, given that the effect sizes are small, these risks are given even more weight. In all cases, the quality of the evidence had to be downgraded to moderate in the current report. This means that future research is likely to have an impact on confidence in the effect size estimate in this report and may ultimately change the estimate as more studies are added to the literature. Consequentially, it is clear that our most definitive conclusion from these findings is that we need more carefully reported health promotion studies that better utilize objective assessments whenever possible. However, the current data do provide some suggestion for ways to move forward in developing this line of evidence.
Ecological Synergy
While the current study cannot directly address the prediction that programs intervening at multiple systemic levels confer a greater impact than those that target fewer systems (Sallis, Owen, & Fisher, 2008), several findings do provide preliminary support. For example, within studies that attempted to change dietary behavior, significantly larger effect sizes were observed for those studies that intervened at the school and community level than those addressing only schools. This finding is important, as it may suggest that while school interventions can be effective for changing dietary behavior, the synergistic effect of adding community-level interventions significantly amplifies their effectiveness. Again this is of critical importance because dietary interventions when evaluated in aggregate produce qualitatively small effect sizes, while those intervening in both schools and communities produce qualitatively medium effect sizes.
Examining individual studies in the meta-analysis also provides evidence for ecological synergy. One of the most effective smoking prevention studies (Biglan, Ary, Smolkowski, Duncan, & Black, 2000) had at its foundation an intensive school-based prevention program, but also engaged community members to act as advocates in publicizing the harms of tobacco use, and developed print advertisements and cable programs. Moreover, participants were instructed by leaders in the community to develop materials specifically to engage and persuade peers. The communities were encouraged to alter the materials to fit the public mindset and to elicit participation from at-risk youth. Finally, the program was designed to encourage open communication among parents and adolescents, and increase the parental use of contingent rewards in regard to tobacco use. Taken with the results of the exploratory analysis, the fact that this individual study intervened so thoroughly at multiple ecological systems levels and produced such a large effect gives some confidence that our theoretical models suggesting synergy between intervention components have some preliminary support in health promotion.
Differential Impact on Individual Health Behaviors
Recent studies indicate that the choice of ecological system for deploying a health promotion intervention may vary depending on the type of health behavior being modified (Lawman & Wilson, 2012). In the current study, targeting individuals in campaigns designed to change dietary behavior appears to be an effective strategy; however, interventions targeting schools and communities in isolation were also effective. This suggests that while intervening with individuals may be appropriate, programs can also have an effect in the absence of a direct and tailored intervention targeting the individual. On the contrary, when it comes to physical activity, interventions that ignore a targeted individualized behavior change program for the child or adolescent are unlikely to produce an effect on physical activity, and to date, most programs produce small effects when physical activity is measured objectively.
Implications of the Current Study on Policy and Practice
As noted early in this manuscript, many of the public health problems that lead to tremendous economic costs, lost quality of life years, and the development of disease and individual suffering are attributable to poor lifestyle behaviors. From the outset, our aim has been to help evaluate the health promotion literature, with the end goal of helping interventionists and policy makers by providing an overview of the state of the science at this cross-section in time. As a framework for organizing our current findings, we find Michie, van Stralen, and West’s (2011) Behavior Change Wheel (BCW) to be a useful system for describing the ways that policy can shape behavior change and drive primary prevention. The BCW begins with the idea that an individual must have the capability, opportunity, and motivation to perform a given health behavior. In addition to other behavioral theories that similarly address these concepts, the BCW goes on to describe a wide range of combinations of interventions and policy systems that could help the individual acquire these three traits. Underscoring that the primary targets of interventions should integrate behavioral skills and create positive social environments, which will ultimately lead to sustained motivation over time.
In the context of the current paper, the most germane subset of these ideas are communication/marketing policies that educate, persuade, or model healthy behavior and service provision that educates about behavior and health, and trains in self-regulation strategies. Using the BCW, our findings and other reviews of pediatric health behavior (Cushing & Steele, 2010; Kahana, Drotar, & Frazier, 2008) suggest that health behavior can be improved by leveraging multiple ecological systems to help children and adolescents self-regulate their own behavior. A common theme is that successful intervention programs teach children to set goals, self-monitor their behavior, and seek feedback on their goal performance. Investing in formal policymaking efforts to help children learn to self-regulate their own behavior should be explored as a cost containment strategy. This falls under the capability domain of the BCW. In the domain of motivation, our results suggest that interventions delivered in cooperation with schools, communities, and the media may hold potential for modifying behavior through positive modeling, instruction, prompting practice, and prompting intention formation. Here the child needs to be supported in what behavior to perform and how to perform it while also having choice and input, before applying self-regulation strategies to ensure that the behavior is performed.
Understanding these factors provides a framework for what to do when an interventionist or a policy maker begins a health promotion campaign. The remaining decisions have to do with what policy systems are at the disposal of the individual attempting to prompt behavior. According to the BCW approach, interventions can map directly on to policy implications that include developing guidelines, environmental and social planning, communication/marketing, legislation, service provision, fiscal measures, and regulation (Michie et al., 2011). There is no “gold standard” to developing policies, but rather components of the interventions and capacity will guide the appropriate linkages to relevant policy. Stakeholders will be a key element in guiding effective policy development and should be incorporated into the process at an early stage.
Limitations and Future Directions
The current study is limited to a relatively small number of health behaviors. As such, the results can only be taken to characterize smoking, physical activity, and dietary behavior interventions. Moreover, many trials intervened on more than one health behavior in a given study. It is possible that making changes to one health behavior increases the likelihood that a child or adolescent would make changes to a related behavior (e.g., changes to diet might increase the likelihood of changes to physical activity), and the current approach cannot account for this. Some studies have used Abraham and Michie’s (2008) behavior change taxonomy as moderator variables in the data analysis. As the number of studies meeting the inclusion criteria in this study increase, it may be possible to conduct an analysis that could determine precisely what behavior change strategies influence effect sizes rather than the descriptive approach adopted in this study. One of the specific limitations of the review in the area of physical activity is that recent studies indicate the adoption of adequate physical activity is associated with neighborhood built environment or other nonhuman community variables in Bronfenbrenner’s (1977) framework (Grow et al., 2008; Saelens et al., 2012). However, few examples of community rehabilitation projects exist in the psychological literature. For this reason, the current study cannot be taken as a comprehensive review of all possible interventions at any level, but this is especially true for variables such as the built environment.
The confidence in the conclusions from the current study is moderate based on the overall GRADE rating. To improve the state of the literature, it will be necessary to conduct additional RCTs, but several considerations will need to be addressed to ensure that new studies are of high quality. A high rating of quality of evidence would require studies that use objectively validated outcome measures and produce robust effect sizes utilizing large samples across the aggregated RCTs. Moreover, there will need to be a relatively large number of studies to establish homogeneity of the CIs that make up the effect sizes in the literature. Future RCTs should be mindful of delivering evidence-based interventions that target healthy children and incorporate objective and validated assessments of primary outcomes. Specifically, the field needs many more studies examining physical activity interventions that use accelerometers in healthy children. Adhering to these recommendations should serve to maximize the quality of the conclusions that can be drawn from the available literature.
Conclusion
The current study provides evidence that health promotion interventions can serve to increase the adoption of healthy behavior and decrease the adoption of unhealthy behavior in children and adolescents, and that for studies providing follow-up data, this finding is relatively stable at 1-year follow-up. However, it is clear that a great deal more work needs to be done to definitively suggest where we should invest the bulk of our health promotion dollars. Results of the current review indicate that the health behavior targeted for intervention may dictate the ecological system that is most critical for intervention. For instance, while dietary interventions can be effective without intervening directly with individuals, physical activity interventions hold little chance of producing change without addressing the individual child or adolescent in some way. While the current results can speak in a limited manner to efficacy, future efforts are needed to evaluate cost-effectiveness and cost-savings of effective interventions (Goodell, Cohen, & Neumann, 2009).
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/
Conflicts of interest: None declared.
Funding
The effort on this paper was partially supported by a grant (R01 HD072153) funded by the National Institute of Child Health and Development to Dawn K. Wilson, Ph.D.
Supplementary Material
Footnotes
1 While we acknowledge that quality of life outcomes are important in determining the effectiveness of a given health promotion intervention, this review will focus solely on health behaviors.
References
(see online supplement for papers included in the meta-analysis)
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology. 2008;27:379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- Adhikari B, Kahende J, Malarcher A, Pechacek T, Tong V. Smoking-attributable mortality, years of potential life lost, and productivity losses. Oncology Times. 2009;31:40. [Google Scholar]
- Baranowski T, Baranowski J C, Cullen K W, Thompson D I, Nicklas T, Zakeri I E, Rochon J. The Fun, Food, and Fitness Project (FFFP): The Baylor GEMS pilot study. Ethnic Disparities. 2003;13:30–39. [PubMed] [Google Scholar]
- Beech B M, Klesges R C, Kumanyika S K, Murray D M, Klesges L, McClanahan B, Slawson D, Nunnally C, Rochon J, McLain-Allen B, Pree-Cary J. Child and parent-targeted interventions: The Memphis GEMS pilot study. Ethnicity and Disease. 2003;13:S1–S40. [PubMed] [Google Scholar]
- Biglan A, Ary DV, Smolkowski K, Duncan T, Black C. A randomized controlled trial of a community intervention to prevent adolescent tobacco use. Tobacco Control. 2000;9:24–32. doi: 10.1136/tc.9.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin G J, Griffin K W. Life skills training: Empirical findings and future directions. Journal of Primary Prevention. 2004;25:211–232. doi:10.1023/B:JOPP.0000042391.58573.5b. [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513. [Google Scholar]
- Centers for Disease Control and Prevention, Office on Smoking and Health. Preventing tobacco use among youth and young adults: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services; 2012. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cushing C C, Steele R G. A meta-analytic review of eHealth interventions for pediatric health promoting and maintaining behaviors. Journal of Pediatric Psychology. 2010;35:937–949. doi: 10.1093/jpepsy/jsq023. doi:10.1093/jpepsy/jsq023. [DOI] [PubMed] [Google Scholar]
- Davis C L, Tomporowski P D, McDowell J E, Austin B P, Miller P H, Yanasak N E, Allison J D, Naglieri J A. Exercise improves executive function and achievement and alters brain activation in overweight children: A randomized, controlled trial. Health Psychology. 2011;30:91–98. doi: 10.1037/a0021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz W H. Health consequences of obesity in youth: Childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- Dobbins M, DeCorby K, Manske S, Goldblatt E. Effective practices for school-based tobacco use prevention. Preventive Medicine. 2008;46:289–297. doi: 10.1016/j.ypmed.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Durlak J A. How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology. 2009;34:917–928. doi: 10.1093/jpepsy/jsp004. doi:10.1093/jpepsy/jsp004. [DOI] [PubMed] [Google Scholar]
- Finkelstein E A, Trogdon J G, Cohen J W, Dietz W. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health Affairs. 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- Fisher E B, Fitzgibbon M L, Glasgow R E, Haire-Joshu D, Hayman L L, Kaplan R M, Nanney M S, Ockene J K. Behavior matters. American Journal of Preventive Medicine. 2011;40:e15–e30. doi: 10.1016/j.amepre.2010.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford E S, Li C, Zhao G, Tsai J. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. International Journal of Obesity. 2011;35:736–743. doi: 10.1038/ijo.2010.186. [DOI] [PubMed] [Google Scholar]
- French S A, Gerlach A F, Mitchell N R, Hannan P J, Welsh E M. Household obesity prevention: Take Action—a group-randomized trial. Obesity. 2011;19:2082–2088. doi: 10.1038/oby.2010.328. doi:10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleser L J, Olkin I. Stochastically dependent effect sizes. In: Cooper H, Hedges L V, editors. The handbook of research synthesis. New York, NY: Russell Sage Foundation; 1994. pp. 339–355. [Google Scholar]
- Goodell S, Cohen J T, Neumann P. Cost savings and cost-effectiveness of clinical preventive care. The Synthesis Project. Research Synthesis Report. 2009;18:1–4. [PubMed] [Google Scholar]
- Grow H, Saelens B, Kerr J, Durant N, Norman G, Sallis J. Where are youth active? Roles of proximity, active transport, and built environment. Medicine and Science in Sports and Exercise. 2008;40:2071–2079. doi: 10.1249/MSS.0b013e3181817baa. [DOI] [PubMed] [Google Scholar]
- Guyatt G, Oxman A D, Akl E A, Kunz R, Visit G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann H J. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- Higgins J P T, Green S, editors. Cochrane handbook for systematic reviews of interventions (Version 5.1.0) 2011. The Cochrane Collaboration. 2011. Retrieved from http://www.cochrane-handbook.org. [Google Scholar]
- Kahana S, Drotar D, Frazier T. Meta analysis of psychological interventions to promote adherence to treatment in pediatric chronic health conditions. Journal of Pediatric Psychology. 2008;33:590–611. doi: 10.1093/jpepsy/jsm128. [DOI] [PubMed] [Google Scholar]
- Kazak A E, Hoagwood K, Weisz J R, Hood K, Kratochwill T R, Vargas L A, Banez G A. A meta-systems approach to evidence-based practice for children and adolescents. American Psychologist. 2010;65:85. doi: 10.1037/a0017784. [DOI] [PubMed] [Google Scholar]
- Lawman H G, Wilson D K. A review of family and environmental correlates of health behaviors in high-risk youth. Obesity. 2012;20:1142–1157. doi: 10.1038/oby.2011.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey M W, Wilson D B. Practical meta-analysis. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Luepker R V, Perry C L, McKinlay S M, Nader P R, Parcel G S, Stone E J, Webber L S, Elder J P, Feldman H A, Johnson C C. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The child and adolescent trial for cardiovascular health. CATCH collaborative group. The Journal of the American Medical Association. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. doi:10.1001/jama.275.10.768. [DOI] [PubMed] [Google Scholar]
- Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54) BMJ British Medical Journal. 2012;345:e5888. doi: 10.1136/bmj.e5888. doi: http://dx.doi.org/10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- Michie S, van Stralen M M, West R. The behavior change wheel: A new method for characterizing and designing behavior change interventions. Implementation Science. 2011;6:1–11. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A H, Marks J S, Stroup D F, Gerberding J L. Actual causes of death in the United States, 2000. JAMA: the Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Pate R R, Ross R, Dowda M, Trost S G, Sirard J R. Validation of a 3-day physical activity recall instrument in female youth. Pediatric Exercise Science. 2003;15:257–265. [Google Scholar]
- Pontifex M B, Saliba B J, Raine L B, Picchietti D L, Hillman C H. Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. The Journal of Pediatrics. 2012;162:543–551. doi: 10.1016/j.jpeds.2012.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens B E, Sallis J F, Frank L D, Couch S C, Zhou C, Colburn T, Cain K L, Chapman J, Glanz K. Obesogenic neighborhood environments, child and parent obesity: The Neighborhood Impact on Kids study. American Journal of Preventive Medicine. 2012;42:e57–e64. doi: 10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J F, Owen N, Fisher E B. Ecological models of health behavior. Health Behavior and Health Education: Theory, Research, and Practice. 2008;4:465–486. [Google Scholar]
- Shoup J A, Gattshall M, Dandamudi P, Estabrooks P. Physical activity, quality of life, and weight status in overweight children. Quality of Life Research. 2008;17:407–412. doi: 10.1007/s11136-008-9312-y. [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti C N. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychological Bulletin. 2006; 132:667. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y C, McPherson K, Marsh T, Gortmaker S L, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378:815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- Wiehe S E, Garrison M M, Christakis D A, Ebel B E, Rivara F P. A systematic review of school-based smoking prevention trials with long-term follow-up. Journal of Adolescent Health. 2005;36:162–169. doi: 10.1016/j.jadohealth.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Wilson D W. New perspectives on health disparities and obesity interventions in youth. Journal of Pediatric Psychology. 2009;34:231–244. doi: 10.1093/jpepsy/jsn137. doi:10.1093/jpepsy/jsn137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson D, Lawman H. Handbook of Pediatric Psychology. 4th ed. New York, NY: The Guilford Press; 2009. Health promotion in children and adolescents: An integration of the biopsychosocial model and ecological approaches to behavior change. [Google Scholar]
- World Health Organization. The Bangkok charter for health promotion in a globalized world. Health Promotion International. 2006;21:10–14. doi: 10.1093/heapro/dal046. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.