Abstract
Objectives. We investigated relations between changes in neighborhood ethnic composition and changes in body mass index (BMI) and waist circumference among Chinese and Hispanic immigrants in the United States.
Methods. We used Multi-Ethnic Study of Atherosclerosis data over a median 9-year follow-up (2000–2002 to 2010–2012) among Chinese (n = 642) and Hispanic (n = 784) immigrants aged 45 to 84 years at baseline. We incorporated information about residential moves and used econometric fixed-effects models to control for confounding by time-invariant characteristics. We characterized neighborhood racial/ethnic composition with census tract–level percentage Asian for Chinese participants and percentage Hispanic for Hispanic participants (neighborhood coethnic concentration).
Results. In covariate-adjusted longitudinal fixed-effects models, results suggested associations between decreasing neighborhood coethnic concentration and increasing weight, although results were imprecise: within-person BMI increases associated with an interquartile range decrease in coethnic concentration were 0.15 kilograms per meters squared (95% confidence interval [CI] = 0.00, 0.30) among Chinese and 0.17 kilograms per meters squared (95% CI = –0.17, 0.51) among Hispanic participants. Results did not differ between those who did and did not move during follow-up.
Conclusions. Residential neighborhoods may help shape chronic disease risk among immigrants.
More than 40 million immigrants reside in the United States, 81% of whom emigrated from Latin America or Asia.1 Not only is the US foreign-born population increasing, but also is the proportion of immigrants who have resided in the United States for a long period of time. An estimated 39% of immigrants had resided in the United States for 20 years or more as of 2010, and this proportion is projected to surpass 50% by 2030.2 This demographic shift has important ramifications for population health and the health service burden because, among immigrants, both cardiovascular disease (CVD) risk and weight, a key CVD risk factor, tend to increase with longer length of stay in the United States, above and beyond the influence of age.3–7
Although explanations for immigrant health patterns often focus on how individual-level health behaviors change across time to align with those of the receiving US culture,5 broader factors may also be important. For example, the neighborhoods in which immigrants reside may contribute to weight changes associated with tenure in the United States. Recent immigrants tend to initially settle in immigrant enclaves, neighborhoods with large numbers of other immigrants of the same country of origin or ethnicity (high coethnic concentration). However, over time, many immigrants move out of immigrant enclaves to neighborhoods with lower proportions of other coethnics or immigrants.8 Classical sociological spatial assimilation theory posits that this process of residential spatial assimilation serves as one important dimension of assimilation into the dominant US culture.8–10 Although the theory does not explicitly state how health would be affected, it implies changes in exposures to neighborhood-level social and physical characteristics that could influence health.
Weight-related physical and social resources in neighborhoods with large immigrant populations may differ from those with fewer immigrants.9,11–13 For example, businesses in immigrant enclaves often provide services or products specific to their ethnic market, including food stores.9,12 Empirical findings on whether the food environment in immigrant enclaves is healthier than in other neighborhoods are inconsistent. Higher neighborhood proportions of Hispanic and Asian residents have been associated with higher numbers of convenience stores and fast-food restaurants—sources of unhealthy foods—but also with higher numbers of nonchain supermarkets and grocery stores, which may contribute to a healthier and more culturally appropriate food environment.14–16 Chinese and Hispanic participants living in immigrant enclaves have reported better availability of healthy food than participants living in other neighborhoods.13 Other aspects of the built environment that are relevant to weight, such as how conducive to walking it is, may also vary by neighborhood ethnic composition.13 Aside from physical resources, the presence of other immigrants in a neighborhood may provide psychosocial benefits by buffering residents against discrimination or by providing access to larger social networks,11,17 but the empirical evidence is again inconsistent.13 These neighborhood differences may in turn affect behavioral and psychosocial determinants of weight.18–23 For example, higher immigrant and ethnic concentration has been associated with differences in diet and physical activity,13,24–27 as well as with better mental health and less perceived discrimination,17,28–35 all of which could have an impact on weight.
Few studies have examined associations between neighborhood ethnic composition and weight among immigrants.36–41 Results have varied depending on the immigrant group examined or the composition measure used (e.g., percentage foreign-born, percentage Hispanic).36–39 Moreover, the majority of previous evidence is cross-sectional and cannot investigate patterns of residential mobility, including spatial assimilation, that may affect weight over time.42 Longitudinal studies are therefore crucial for understanding how neighborhood context may affect weight over time in immigrants.3 Despite substantial theoretical and empirical sociological research dedicated to characterizing residential patterns among immigrants, there is little research in either sociology or public health that explicitly examines the implications of these patterns for health.
We used longitudinal econometric fixed-effects models to investigate whether changes in neighborhood ethnic composition were related to changes in body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) and waist circumference (WC) over a median follow-up of 9 years among a cohort of Chinese and Hispanic immigrants in the United States. Because fixed-effects models rely only on intraindividual variability, and therefore tightly control for all time-invariant individual-level characteristics, this approach can reduce the likelihood that observed results are confounded.43 We hypothesized that decreases in neighborhood coethnic concentration would be related to increases in BMI and WC in our sample. We also hypothesized that immigrants who spatially assimilated during follow-up (i.e., who moved to a neighborhood with lower coethnic concentration, as opposed to staying in the same residence with their neighborhood changing around them) would experience greater increases in BMI and WC. Our second hypothesis was driven by the idea that, consistent with classical spatial assimilation theory, spatial assimilation may denote a greater likelihood of adopting less healthy behaviors associated with the dominant US culture.
METHODS
Data came from the Multi-Ethnic Study of Atherosclerosis (MESA), a multisite cohort study of adults aged 45 to 84 years and free of clinical CVD at baseline. Study staff used population-based methods to recruit participants from 4 racial/ethnic groups: non-Hispanic White, non-Hispanic Black, Hispanic, and Chinese.44 Participants completed baseline examinations in 2000–2002, with 4 follow-up waves in 2002–2003, 2004–2005, 2006–2007, and 2010–2012. Study design details are available elsewhere.44 We drew neighborhood information from the ancillary MESA Neighborhood Study. Out of 1596 MESA participants who self-reported being foreign-born and of Chinese (n = 697) or Hispanic (n = 899) ethnicity (we excluded the few foreign-born non-Hispanic White or Black participants) and who participated in the MESA Neighborhood Study, we excluded 11 who lived outside of MESA sites with dedicated sampling of Chinese and Hispanic participants (Los Angeles, CA, and Chicago, IL, for Chinese participants; Los Angeles, Minneapolis, MN, and New York, NY, for Hispanic participants) or did not provide residential addresses that could be accurately geocoded, and an additional 151 because of missing covariate or outcome information. Because our fixed-effects approach relied on within-individual variability, we also excluded 8 participants with only a single observation. The final analysis sample included 1426 immigrants (642 Chinese and 784 Hispanic), contributing a total of 6329 observations across all waves.
Measures
Study staff measured anthropometric information at each study examination with standard procedures.44 They calculated BMI (kg/m2) with height (m) and weight (kg). For descriptive purposes, we categorized BMI as normal (< 25 kg/m2), overweight (≥ 25 and < 30 kg/m2), or obese (≥ 30 kg/m2) and WC (in cm) as normal (< 80 cm for women; < 90 cm for men), high (80–87 cm for women; 90–101 cm for men), or very high (≥ 88 cm for women; ≥ 102 cm for men).45,46
Study staff geocoded participants’ residential addresses with TeleAtlas EZ-Locate Web-based geocoding software (TeleAtlas, Lebanon, NH).3 To create the measure of neighborhood coethnic concentration, we used measures of racial/ethnic composition from 4 US Census Bureau sources, with census tracts serving as proxies for neighborhoods: the 2000 and 2010 decennial censuses and the 2005–2009 and 2007–2011 American Community Surveys (ACSs).47–50 Census tracts were the smallest administrative unit for which it was feasible to obtain estimates across our follow-up period with stable geographic boundaries.
We defined neighborhood coethnic concentration as tract percentage Asian for Chinese participants and tract percentage Hispanic for Hispanic participants. We chose these measures because they were available in Census 2010 data (which includes information on race but not nativity) and therefore provided an extra data point. With Census 2000 and ACS 2005–2009 data, the correlation between our measure and a measure based on nativity and area of origin—percentage foreign-born from China for Chinese participants and percentage foreign-born from Latin America for Hispanic participants—was 0.91.
We assigned an anchor date to each of the 4 census sources that corresponded to the midpoint of the relevant time period (July 1, 2000, for Census 2000; July 1, 2007, for ACS 2005–2009; July 1, 2009, for ACS 2007–2011; and July 1, 2010, for Census 2010) and used these data points to linearly interpolate the neighborhood coethnic concentration measure by using 4 separate tract-specific linear slopes for observations January 2000 to June 2007, July 2007 to June 2009, July 2009 to June 2010, and July 2010 to December 2012. We calculated all slopes with Census 2000 boundaries.51 To control for neighborhood socioeconomic status, we included in analyses a log-transformed measure of tract-level median household income. We interpolated values of median neighborhood income in the same manner except that, because this measure was not available from Census 2010, we estimated only 3 linear slopes for each tract corresponding to dates before July 2007, July 2007 to June 2009, and July 2009 or later.
We operationalized spatial assimilation as an interaction term between neighborhood coethnic concentration and an indicator for whether the participant moved to a different address since the previous study wave (residential mobility). This allowed the effect of change in coethnic concentration on BMI to differ for participants who experienced the change as a result of residential mobility, compared with staying in their home while the neighborhood changed around them. To create the residential mobility indicator at baseline, we used residential history information to indicate whether the participant moved during the 2 years before baseline.
Individual-level covariates measured at baseline included gender, age (mean-centered at 61 years), race/ethnicity, years lived in the United States (centered at 25), education (< high-school degree, high-school degree, some college, or ≥ bachelor’s degree), and study site. Time-varying measures were time since baseline (years), annual family income, marital status (married or cohabiting; divorced, separated, or widowed; or never married), and employment status (employed full time, employed part time, or other). We modeled annual family income, reported by participants in 13 categories from less than $5000 to $1 000 000 or more, as a continuous variable by assigning each observation the midpoint of the selected category. Because family income information was missing for 21% of observations, largely because income information was not collected in the fourth study wave, we imputed missing values with the nonmissing value closest in date.
Analysis
We conducted all analyses in SAS version 9.3 (SAS Institute, Cary, NC) and stratified by ethnicity (Chinese and Hispanic). Additional stratification by gender did not appreciably affect results, so we present results collapsed on gender. Each participant had 2 to 5 repeat observations. Because most sample census tracts contained very few participants—the median was 1—we did not account for clustering within tracts in our analyses. We used the χ2 test to test bivariate associations of covariates at baseline with baseline neighborhood coethnic concentration, baseline BMI and WC, and change in BMI and WC over follow-up.
We modeled adjusted associations of neighborhood coethnic concentration with BMI in longitudinal models by using individual-level econometric fixed-effects linear regression.43 These models are equivalent to including an indicator variable for each person. Because they tightly control by design for characteristics that are invariant within individuals over time, we excluded temporally stable variables and adjusted only for time-varying covariates (neighborhood coethnic concentration, move status, and family and neighborhood income). Because additional adjustment for time-varying measures of marital and employment status did not affect estimates for neighborhood coethnic concentration, we excluded these variables from the final models for parsimony. We also included time since baseline (and its interactions with baseline age and baseline length of US residence) to adjust for aging effects on BMI. We assessed nonlinearity in the associations between continuous variables and the outcomes by testing squared terms for these variables in adjusted models; none of the squared terms was retained in final models.
We repeated analyses by using a continuous measure of WC as the outcome. Because of changes in body composition and height associated with aging, WC may be a better marker of adiposity than BMI among the elderly.52,53 In addition, there is evidence that some Asian populations, including Chinese, tend to have a higher proportion of body fat, and in particular higher central visceral adiposity—and attendant CVD risk—at a given BMI level than other populations.7,54
Sensitivity Analyses
Weight may increase most rapidly during the first 10 to 15 years of residence in the United States,6,55,56 yet more than 60% our immigrant sample had already resided in the United States for 20 years or more at baseline. If effects of neighborhood coethnic concentration or spatial assimilation on weight status diminish over time, the most important effects may have already taken place before baseline for these participants. Therefore, we conducted an additional analysis including only participants who had resided in the United States 5 years or less time at baseline.
We also repeated the analyses by using multilevel random effects linear regression with random individual-level intercepts. These models may provide more power to detect associations than fixed-effects models because they incorporate both within-person and between-person variability. However, they are subject to residual confounding by individual-level characteristics. Therefore, in addition to the covariates included in the fixed-effects models, we also adjusted the random-effects models for baseline measures of gender, years lived in the United States, education, and study site.
RESULTS
The median follow-up time was 9 years, with 95% of participants completing at least 3 study waves and 63% completing all 5. Eighty-two percent of Chinese and 90% of Hispanic participants had lived in the United States for at least 10 years at baseline; during follow-up, 48% of Chinese and 36% of Hispanic participants changed address at least once. Four percent of Chinese and 35% of Hispanic participants were obese at baseline (Table 1).
TABLE 1—
Percentage Distribution of Selected Covariates Across Tertiles of Baseline Neighborhood Coethnic Concentration Among Chinese and Hispanic Foreign-Born Participants: Multi-Ethnic Study of Atherosclerosis, United States, 2000–2002 to 2010–2012 Waves
| Chinese |
Hispanic |
|||||||||
| Variable | Total (n = 642), No. (%) | Low (0%–23%; n = 199), % | Med (23%–52%; n = 231), % | High (52%–94%; n = 212), % | Pa | Total (n = 784), No. (%) | Low (0%–40%; n = 228), % | Med (40%–72%; n = 280), % | High (72%–100%; n = 276), % | Pa |
| Baseline | ||||||||||
| Body mass index, kg/m2 | .63 | .82 | ||||||||
| < 25 (underweight or normal) | 420 (65) | 65 | 62 | 69 | 140 (18) | 19 | 17 | 18 | ||
| ≥ 25 and < 30 (overweight) | 198 (31) | 31 | 33 | 27 | 370 (47) | 47 | 49 | 45 | ||
| ≥ 30 (obese) | 24 (4) | 3 | 4 | 4 | 274 (35) | 34 | 34 | 37 | ||
| Waist circumference, cm | .69 | .15 | ||||||||
| < 80 women; < 90 men (normal) | 279 (43) | 45 | 45 | 40 | 76 (10) | 12 | 10 | 8 | ||
| 80–87 women; 90–101 men (high) | 209 (33) | 34 | 31 | 33 | 235 (30) | 24 | 33 | 32 | ||
| ≥ 88 women; ≥ 102 men (very high) | 154 (24) | 21 | 24 | 26 | 473 (60) | 64 | 57 | 61 | ||
| Age, y | < .001 | .59 | ||||||||
| 45–54 | 173 (27) | 30 | 32 | 18 | 243 (31) | 32 | 33 | 28 | ||
| 55–64 | 182 (28) | 31 | 30 | 23 | 221 (28) | 28 | 29 | 27 | ||
| 65–74 | 197 (31) | 28 | 27 | 37 | 213 (27) | 27 | 26 | 29 | ||
| 75–84 | 90 (14) | 10 | 10 | 22 | 107 (14) | 13 | 12 | 16 | ||
| Education | < .001 | < .001 | ||||||||
| < high school or GED | 151 (24) | 14 | 23 | 33 | 421 (54) | 41 | 53 | 65 | ||
| High school or GED | 107 (17) | 14 | 15 | 21 | 142 (18) | 20 | 20 | 15 | ||
| Some college, AA | 136 (21) | 21 | 23 | 19 | 148 (19) | 25 | 19 | 14 | ||
| ≥ BA | 248 (39) | 51 | 39 | 27 | 73 (9) | 15 | 9 | 6 | ||
| Annual family income, $ | < .001 | < .001 | ||||||||
| < 12 000 | 140 (22) | 20 | 18 | 28 | 191 (24) | 22 | 25 | 26 | ||
| 12 000–24 999 | 179 (28) | 21 | 30 | 33 | 248 (32) | 26 | 30 | 38 | ||
| 25 000–39 999 | 101 (16) | 13 | 18 | 17 | 187 (24) | 25 | 25 | 22 | ||
| 40 000–74 999 | 119 (19) | 19 | 23 | 13 | 121 (15) | 18 | 16 | 12 | ||
| ≥ 75 000 | 103 (16) | 27 | 12 | 9 | 37 (5) | 10 | 4 | 1 | ||
| Marital status | .02 | .12 | ||||||||
| Married or cohabiting | 523 (81) | 87 | 82 | 75 | 466 (60) | 54 | 60 | 65 | ||
| Divorced, separated, or widowed | 102 (16) | 10 | 15 | 22 | 258 (33) | 39 | 32 | 30 | ||
| Never married | 16 (3) | 3 | 3 | 2 | 53 (7) | 7 | 8 | 5 | ||
| Employment status | < .001 | .02 | ||||||||
| Employed full time | 230 (36) | 47 | 37 | 25 | 282 (36) | 42 | 37 | 30 | ||
| Employed part time | 65 (10) | 10 | 11 | 10 | 62 (8) | 10 | 7 | 7 | ||
| Otherb | 347 (54) | 44 | 52 | 66 | 440 (56) | 48 | 56 | 63 | ||
| Years lived in United States | < .001 | .01 | ||||||||
| ≤ 9 | 119 (19) | 12 | 18 | 25 | 76 (10) | 13 | 11 | 5 | ||
| 10–19 | 215 (33) | 24 | 35 | 40 | 107 (14) | 16 | 11 | 14 | ||
| 20–29 | 170 (26) | 31 | 30 | 18 | 160 (20) | 15 | 21 | 24 | ||
| ≥ 30 | 138 (22) | 32 | 17 | 17 | 441 (56) | 55 | 57 | 57 | ||
| Site | < .001 | < .001 | ||||||||
| Los Angeles, CA | 404 (63) | 27 | 80 | 78 | 282 (36) | 23 | 26 | 57 | ||
| Chicago, IL | 238 (37) | 73 | 20 | 22 | . . . | . . . | . . . | . . . | ||
| Minneapolis, MN | . . . | . . . | . . . | . . . | 138 (18) | 42 | 16 | 0 | ||
| New York, NY | . . . | . . . | . . . | . . . | 364 (46) | 35 | 59 | 43 | ||
| Neighborhood median household incomec | < .001 | < .001 | ||||||||
| Quartile 1 | 222 (35) | 18 | 28 | 57 | 270 (34) | 8 | 45 | 45 | ||
| Quartile 2 | 187 (29) | 18 | 41 | 26 | 201 (26) | 18 | 21 | 36 | ||
| Quartile 3 | 108 (17) | 16 | 22 | 11 | 193 (25) | 31 | 28 | 15 | ||
| Quartile 4 | 125 (19) | 47 | 9 | 6 | 120 (15) | 42 | 6 | 3 | ||
| Longitudinal | ||||||||||
| Moved during follow-up | .38 | .01 | ||||||||
| No | 338 (53) | 56 | 52 | 50 | 503 (64) | 56 | 66 | 69 | ||
| Yes | 304 (47) | 44 | 48 | 50 | 281 (36) | 44 | 34 | 31 | ||
| Change in body mass indexd | .94 | .63 | ||||||||
| Tertile 1 | 214 (33) | 35 | 33 | 32 | 261 (33) | 34 | 33 | 33 | ||
| Tertile 2 | 214 (33) | 34 | 34 | 33 | 262 (33) | 33 | 36 | 31 | ||
| Tertile 3 | 214 (33) | 31 | 33 | 35 | 261 (33) | 33 | 31 | 36 | ||
| Change in waist circumferencee | .32 | .84 | ||||||||
| Tertile 1 | 213 (33) | 36 | 29 | 36 | 262 (33) | 34 | 35 | 32 | ||
| Tertile 2 | 214 (33) | 35 | 33 | 33 | 261 (33) | 32 | 32 | 36 | ||
| Tertile 3 | 213 (33) | 30 | 38 | 31 | 261 (33) | 34 | 34 | 33 | ||
Note. AA = associate degree; BA = bachelor’s degree; GED = general education development credential. Percentages are column percentages. Tertile ranges appear to overlap because of rounding.
From χ2 test.
Includes homemaker, on leave, unemployed, and retired.
Neighborhood median income quartiles calculated at the census tract level. Chinese: Q1 = $11 595 to $39 686; Q2 = $39 698 to $51 386; Q3 = $51 387 to $70 419; Q4 = $70 443 to $219 580. Hispanic: Q1 = $9050 to $27 745; Q2 = $27 746 to $35 427; Q3 = $35 454 to $48 361; Q4 = $48 367 to $189 068.
Chinese: T1 = −8.799 to −0.563 kg/m2; T2 = −0.544 to 0.626 kg/m2; T3 = 0.630 to 8.490 kg/m2. Hispanic: T1 = −10.258 to −0.545 kg/m2; T2 = −0.544 to 1.074 kg/m2; T3 = 1.075 to 12.119 kg/m2.
Chinese: T1 = −31.5 to −1.1 cm; T2 = −1.0 to 3.8 cm; T3 = 3.9 to 40.2 cm. Hispanic: T1 = −25.1 to −1.4 cm; T2 = −1.3 to 4.0 cm; T3 = 4.1 to 39.7 cm.
In bivariate comparisons, most covariates were associated with neighborhood coethnic concentration (Table 1). Older age was associated with higher neighborhood coethnic concentration among Chinese but not Hispanic immigrants. Length of US residence was related to neighborhood coethnic concentration but, although the association was negative and monotonic among Chinese participants (consistent with classical spatial assimilation theory), it was nonmonotonic among Hispanic participants. Associations between baseline neighborhood coethnic concentration and baseline BMI and WC, as well as change in BMI and WC during follow-up, were minimal.
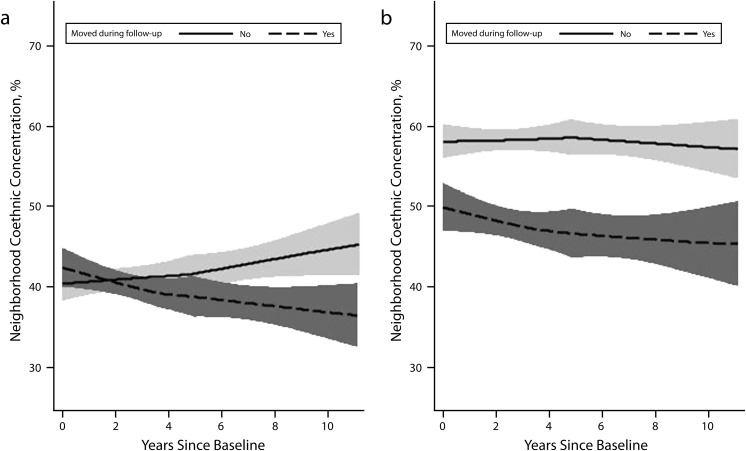
Figure 1 shows patterns of neighborhood coethnic concentration by move status. Among Chinese participants, those who moved during follow-up experienced a decline in coethnic concentration (P for time trend < .001) whereas those who did not move experienced an increase in coethnic concentration (P for trend < .001). Among Hispanic participants, those who moved during follow-up tended to live in neighborhoods with lower coethnic concentration at baseline than those who did not move (P < .001 for difference), and this difference persisted throughout follow-up. Hispanic participants who moved also experienced decreases in coethnic concentration over time (P for trend < .001) whereas nonmovers did not (P for trend = .94).
FIGURE 1—
Unadjusted locally weighted smoothed curves of neighborhood coethnic concentration over follow-up, by move status, among (a) Chinese foreign-born sample participants and (b) Hispanic foreign-born sample participants: Multi-Ethnic Study of Atherosclerosis, United States, 2000–2002 to 2010–2012 waves.
Note. Shaded bands represent 95% confidence intervals.
Results from fixed-effects longitudinal models for Chinese and Hispanic participants are shown in Tables 2 and 3, respectively. Supporting our first hypothesis, in models adjusted only for within-person aging effects (model 1), an interquartile range decrease in neighborhood coethnic concentration (42 and 51 percentage points among Chinese and Hispanic participants, respectively) was associated with an increase in BMI among Chinese participants (difference = 0.16 kg/m2; 95% confidence interval [CI] = 0.02, 0.31). We observed a similar pattern in Hispanic participants, but the CI was wide (difference = 0.20 kg/m2; 95% CI = –0.11, 0.52). Changes in coethnic concentration were weakly associated with increases in WC but CIs were wide for both groups (Chinese: difference = 0.17; 95% CI = –0.44, 0.79; Hispanics: difference = 0.16; 95% CI = –0.97, 1.20).
TABLE 2—
Mean Changes in Body Mass Index and Waist Circumference Associated With Within-Person Changes in Covariates From Fixed-Effects Linear Regression Models Among Chinese Participants: Multi-Ethnic Study of Atherosclerosis, United States, 2000–2002 to 2010–2012 Waves
| Body Mass Index (kg/m2) |
Waist Circumference (cm) |
|||||
| Variable | Model 1, Diff (95% CI) | Model 2, Diff (95% CI) | Model 3, Diff (95% CI) | Model 1, Diff (95% CI) | Model 2, Diff (95% CI) | Model 3, Diff (95% CI) |
| Ethnic congruence (decrease 75th to 25th percentile)a | 0.16* (0.02, 0.31) | 0.15 (0.00, 0.30) | 0.12 (–0.05, 0.29) | 0.17 (–0.44, 0.79) | 0.18 (–0.46, 0.81) | 0.02 (–0.69, 0.73) |
| Time since baseline (y)b | 0.02* (0.00, 0.03) | –0.001 (–0.02, 0.01) | –0.002 (–0.02, 0.01) | 0.24** (0.18, 0.30) | 0.19** (0.12, 0.26) | 0.19** (0.12, 0.25) |
| Time × baseline ageb | –0.01** (–0.01, 0.00) | –0.005 (–0.01, 0.00) | –0.005 (–0.01, 0.00) | –0.02* (–0.04, 0.00) | –0.02 (–0.04, 0.01) | –0.02 (–0.04, 0.01) |
| Time × baseline years in United Statesb | –0.01** (–0.02, –0.01) | –0.01** (–0.02, –0.01) | –0.04** (–0.06, –0.02) | –0.04** (–0.06, –0.02) | ||
| Annual family income (increase 25th to 75th percentile)c | 0.01 (–0.06, 0.08) | 0.01 (–0.06, 0.08) | –0.12 (–0.41, 0.17) | –0.12 (–0.42, 0.17) | ||
| Natural logarithm (neighborhood median household income)b | 0.01 (–0.18, 0.20) | 0.01 (–0.18, 0.20) | –0.28 (–1.08, 0.52) | –0.27 (–1.07, 0.53) | ||
| Moved since previous examination | –0.08 (–0.18, 0.02) | –0.12 (–0.26, 0.02) | –0.26 (–0.69, 0.18) | –0.43 (–1.00, 0.14) | ||
| Ethnic congruence × moved | 0.07 (–0.10, 0.25) | 0.34 (–0.38, 1.06) | ||||
Note. CI = confidence interval.
Interquartile range decrease = −42 percentage points.
Centered at population mean value. Baseline age and years in United States are in 5-year units.
Interquartile range increase = $31 000.
*P < .05; **P < .01.
TABLE 3—
Mean Changes in Body Mass Index and Waist Circumference Associated With Within-Person Changes in Covariates From Fixed-Effects Linear Regression Models Among Hispanic Participants: Multi-Ethnic Study of Atherosclerosis, United States, 2000–2002 to 2010–2012 Waves
| Body Mass Index (kg/m2) |
Waist Circumference (cm) |
|||||
| Variable | Model 1, Diff (95% CI) | Model 2, Diff (95% CI) | Model 3, Diff (95% CI) | Model 1, Diff (95% CI) | Model 2, Diff (95% CI) | Model 3, Diff (95% CI) |
| Ethnic congruence (decrease 75th to 25th percentile)a | 0.20 (–0.11, 0.52) | 0.17 (–0.17, 0.51) | 0.08 (–0.28, 0.43) | 0.16 (–0.97, 1.20) | –0.15 (–1.25, 0.95) | –0.36 (–1.52, 0.81) |
| Time since baseline (y)b | 0.06** (0.04, 0.08) | 0.07** (0.04, 0.09) | 0.07** (0.04, 0.09) | 0.28** (0.22, 0.35) | 0.26** (0.20, 0.33) | 0.27** (0.20, 0.34) |
| Time × baseline ageb | –0.02** (–0.03, –0.01) | –0.02** (–0.02, –0.01) | –0.02** (–0.02, –0.01) | –0.07** (–0.10, –0.05) | –0.07** (–0.09, –0.04) | –0.07** (–0.09, –0.04) |
| Time × baseline years in United Statesb | –0.01** (–0.02, 0.00) | –0.01** (–0.02, 0.00) | –0.01 (–0.03, 0.01) | –0.01 (–0.03, 0.01) | ||
| Annual family income (increase 25th to 75th percentile)c | 0.03 (–0.12, 0.17) | 0.03 (–0.11, 0.18) | 0.25 (–0.22, 0.72) | 0.26 (–0.22, 0.73) | ||
| Natural logarithm (neighborhood median household income)b | –0.04 (–0.37, 0.29) | –0.04 (–0.37, 0.29) | 0.76 (–0.32, 1.83) | 0.76 (–0.32, 1.84) | ||
| Moved since previous examination | 0.11 (–0.07, 0.28) | –0.05 (–0.31, 0.21) | 0.21 (–0.35, 0.77) | –0.14 (–1.00, 0.72) | ||
| Ethnic congruence × moved | 0.23 (–0.06, 0.53) | 0.52 (–0.44, 1.48) | ||||
Note. CI = confidence interval.
Interquartile range decrease = −51 percentage points.
Centered at population mean value. Baseline age and years in United States are in 5-year units.
Interquartile range increase = $31 000.
**P < .01.
After we adjusted for additional covariates (model 2), the association between an interquartile range decrease in neighborhood coethnic concentration and increased BMI was similar in magnitude between the 2 ethnic groups and retained borderline statistical significance only among Chinese participants (difference = 0.15 kg/m2; 95% CI = 0.00, 0.30; Table 2; model 2); the difference was 0.17 (95% CI = –0.17, 0.51) among Hispanics (Table 3, model 2). As in model 1, associations between changes in coethnic concentration and WC were weak in both groups.
Model 3 (Tables 2 and 3) includes the interaction term between neighborhood coethnic concentration and the residential mobility indicator. This tests our second hypothesis that spatial assimilation, which we defined as a joint effect of moving and a decrease in coethnic concentration, results in greater increases in BMI and WC. We did not find evidence that this was the case; although all the interaction coefficients were in the positive direction, consistent with our hypothesis, there was little statistical evidence of interaction (BMI: interaction P = .41 among Chinese; P = .12 among Hispanics; WC: P = .35 among Chinese; P = .29 among Hispanics).
Seventy-three Chinese participants and 38 Hispanic participants had lived in the United States 5 years or less time at baseline (Tables A and B, available as supplements to the online version of this article at http://www.ajph.org). Point estimates testing both hypotheses in this subsample analysis were larger in magnitude than in the main analysis, and estimates for neighborhood coethnic concentration achieved statistical significance among Chinese participants for both outcomes despite small sample sizes. In the fully adjusted model (model 2), an interquartile range decrease in neighborhood coethnic concentration was associated with increases in BMI of 0.40 kilograms per meter squared (95% CI = 0.05, 0.75) and in WC of 1.45 cm (95% CI = 0.00, 2.89) among Chinese participants. Among Hispanic participants, estimated differences were 0.53 kilograms per meter squared (95% CI = -0.79, 1.86) for BMI and 2.27 cm (95% CI = -1.87, 6.40) for WC.
Results from the multilevel random effects sensitivity analysis were consistent with the fixed-effects approach (data not shown).
DISCUSSION
Over a median 9 years of follow-up among a multisite sample of older Chinese and Hispanic immigrants to the United States, we observed evidence suggesting that decreases in neighborhood coethnic concentration are related to increases in BMI, particularly among Chinese immigrants. Although we observed a similar pattern in Hispanics, the association had a wide confidence interval. Contrary to our hypothesis, there was little evidence that effects of decreasing neighborhood coethnic concentration differed between residents who moved (i.e., experienced spatial assimilation) or remained in place while their neighborhoods changed around them. Neighborhood Hispanic composition has been inconsistently related to BMI among Hispanics in several cross-sectional studies.36–38,40 Neighborhood immigrant composition was not associated with weight change in a longitudinal study of adults in Los Angeles.39 Our analysis extends this previous, mostly cross-sectional, literature by incorporating information about residential moves and using a fixed-effects approach to tightly control for confounding by time-invariant individual characteristics.
In contrast to results for BMI, changes in neighborhood coethnic concentration were only weakly associated with changes in WC in the full sample. However, associations in expected directions were larger in magnitude and statistically stronger for both outcomes among the most recent Chinese and Hispanic immigrants, although still imprecise among recent Hispanic immigrants. Waist circumference may have been measured with more error than weight, diminishing the ability to detect smaller within-person changes among the full sample. Although BMI diminishes with aging, it nevertheless remains an important predictor of cardiovascular health. Furthermore, 35% of the Hispanic participants in our sample were obese (BMI ≥ 30 kg/m2) at baseline; a BMI at this level is considered a risk factor even among older populations.4,52
Classical spatial assimilation theory has been challenged of late: in 1993, Portes and Zhou proposed the concept of segmented assimilation to describe how different immigrant groups may assimilate into different segments of the American population, such that all groups do not necessarily integrate with middle-class White society over time.9,57 One possible illustration of segmented assimilation in our data is that although longer length of residence in the United States was associated monotonically with lower neighborhood coethnic concentration among Chinese immigrants at baseline, this was not the case for Hispanic immigrants (Table 1). One possibility is that Hispanics in our sample may have encountered structural barriers that affect residential opportunities, such as discriminatory housing practices or hostile receptions from host communities, which may not have affected Chinese participants in the same way.42,58,59 This heterogeneity has implications for how immigrants assimilate into US culture, including their residential spatial assimilation out of ethnically concentrated neighborhoods. Residential and assimilation processes also vary within ethnic groups according to factors such as age, age of immigration, country of origin, individual socioeconomic status, race, or region of residence.10,56,60,61 These differences may have ramifications for how neighborhood context relates to BMI and overall CVD risk.
Our analysis results among the most recent immigrants suggest that the long tenure of the majority of our participants in the United States before baseline hampered our ability to detect associations between neighborhood coethnic concentration and changes in BMI or WC in the full sample. The bulk of the spatial assimilation experienced by many participants may also have taken place before baseline; indeed, in our sample, residential mobility during follow-up was markedly higher among participants who had resided in the United States for less time at baseline.
Census tract boundaries—or any administrative boundaries— are unlikely to coincide perfectly with boundaries that would best describe differences in neighborhood environments.62,63 In fact, the most relevant geographic areas likely differ in scale and boundary location for different causal mechanisms related to neighborhood coethnic concentration. For example, access to healthy foods may depend on the locations of major thoroughfares in a several-mile area, whereas psychosocial pathways may operate primarily between neighbors living in adjacent homes. These discrepancies between true and proxy neighborhood boundaries likely contributed to measurement error in our neighborhood variables.
As with any observational study, our results may have been affected by unmeasured confounding. However, the fixed-effects longitudinal analytic approach substantially strengthened our causal inference by controlling for all temporally stable confounders, even if unmeasured.43 Our results may also have been affected by attrition if loss to follow-up was related to tendencies for BMI change that were not captured in our analysis. Although the MESA sample was not designed to be representative of the US population, comparisons of the MESA Hispanic and Chinese sample to US demographics suggest that our results may be generalizable.13 However, our results may not be representative of younger immigrants, of those from other countries, or of those more recently arrived to the United States. Future research should also explore ethnic composition measures that are more specific to a given ethnic group or area of origin.
Few previous studies have examined longitudinal neighborhood patterns for health,64 much less among immigrants. Our analysis points to the need for longitudinal data with adequate samples of immigrant populations, particularly recent immigrants, to elucidate health processes in these increasing populations. Our results also demonstrate the need for further research into the mechanisms behind increases in CVD risk among immigrant populations over time. One contribution of our study is to distinguish conceptually between 2 different paths to experience neighborhood change—through residential mobility versus through aging in place while the neighborhood itself changes—which may influence health through different mechanisms. A better understanding of these mechanisms may help in the development of interventions to reduce cardiovascular risk not only among immigrants but also among the population as a whole.
Acknowledgments
This research was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-RR-024156 and UL1-RR-025005 from the National Center for Research Resources and R01 HL071759 from National Heart, Lung, and Blood Institute at the National Institutes of Health. S. S. Albrecht received support from the Population Research Training grant (T32 HD007168) and the Population Research Infrastructure Program (R24 HD050924) awarded to the Carolina Population Center at The University of North Carolina at Chapel Hill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
The Multi-Ethnic Study of Atherosclerosis was approved by the institutional review boards at each study site and all participants gave written informed consent.
References
- 1.Wasem RE. US Immigration Policy: Chart Book of Key Trends. Washington, DC: Congressional Research Service; 2013. [Google Scholar]
- 2.Pitkin J, Myers D. Los Angeles, CA: University of Southern California School of Policy, Planning, and Development; 2011. Projections of the US population, 2010–2040, by immigrant generation and foreign-born duration in the US. [Google Scholar]
- 3.Albrecht SS, Diez Roux AV, Aiello AE, Schulz AJ, Abraido-Lanza AF. Secular trends in the association between nativity/length of US residence with body mass index and waist circumference among Mexican-Americans, 1988–2008. Int J Public Health. 2013;58(4):573–581. doi: 10.1007/s00038-012-0414-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Argeseanu Cunningham S, Ruben JD, Narayan KM. Health of foreign-born people in the United States: a review. Health Place. 2008;14(4):623–635. doi: 10.1016/j.healthplace.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oza-Frank R, Cunningham SA. The weight of US residence among immigrants: a systematic review. Obes Rev. 2010;11(4):271–280. doi: 10.1111/j.1467-789X.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- 7.Palaniappan LP, Araneta MR, Assimes TL et al. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation. 2010;122(12):1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iceland J, Scopilliti M. Immigrant residential segregation in US metropolitan areas, 1990–2000. Demography. 2008;45(1):79–94. doi: 10.1353/dem.2008.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Portes A, Rumbaut RG. Immigrant America: A Portrait. 3rd ed. Berkeley, CA: University of California; 2006. [Google Scholar]
- 10.South SJ, Crowder K, Chavez E. Migration and spatial assimilation among U.S. Latinos: classical versus segmented trajectories. Demography. 2005;42(3):497–521. doi: 10.1353/dem.2005.0025. [DOI] [PubMed] [Google Scholar]
- 11.Almeida J, Kawachi I, Molnar BE, Subramanian SV. A multilevel analysis of social ties and social cohesion among Latinos and their neighborhoods: results from Chicago. J Urban Health. 2009;86(5):745–759. doi: 10.1007/s11524-009-9375-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie Y, Gough M. Ethnic enclaves and the earnings of immigrants. Demography. 2011;48(4):1293–1315. doi: 10.1007/s13524-011-0058-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osypuk TL, Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The Multi-Ethnic Study of Atherosclerosis. Soc Sci Med. 2009;69(1):110–120. doi: 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102(9):1644–1654. doi: 10.2105/AJPH.2012.300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96(2):325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health. 2008;13(4):321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- 18.Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev. 2008;66(1):2–20. doi: 10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- 19.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80(4):569–589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC, Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the Multi-Ethnic Study of Atherosclerosis) Obesity (Silver Spring) 2013;21(3):621–628. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(5, suppl 1):S110–S117. doi: 10.1016/j.jada.2005.02.045. [DOI] [PubMed] [Google Scholar]
- 22.Gibson DM. The neighborhood food environment and adult weight status: estimates from longitudinal data. Am J Public Health. 2011;101(1):71–78. doi: 10.2105/AJPH.2009.187567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zick CD, Hanson H, Fan JX et al. Re-visiting the relationship between neighbourhood environment and BMI: an instrumental variables approach to correcting for residential selection bias. Int J Behav Nutr Phys Act. 2013;10:27. doi: 10.1186/1479-5868-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubowitz T, Subramanian SV, Acevedo-Garcia D, Osypuk TL, Peterson KE. Individual and neighborhood differences in diet among low-income foreign and US-born women. Womens Health Issues. 2008;18(3):181–190. doi: 10.1016/j.whi.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee RE, Cubbin C. Neighborhood context and youth cardiovascular health behaviors. Am J Public Health. 2002;92(3):428–436. doi: 10.2105/ajph.92.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park Y, Neckerman K, Quinn J, Weiss C, Jacobson J, Rundle A. Neighbourhood immigrant acculturation and diet among Hispanic female residents of New York City. Public Health Nutr. 2011;14(9):1593–1600. doi: 10.1017/S136898001100019X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Afable-Munsuz A, Ponce NA, Rodriguez M, Perez-Stable EJ. Immigrant generation and physical activity among Mexican, Chinese & Filipino adults in the US. Soc Sci Med. 2010;70(12):1997–2005. doi: 10.1016/j.socscimed.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15(3):670–678. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Gee GC, Ro A, Shariff-Marco S, Chae D. Racial discrimination and health among Asian Americans: evidence, assessment, and directions for future research. Epidemiol Rev. 2009;31:130–151. doi: 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwag KH, Jang Y, Chiriboga DA. Acculturation and depressive symptoms in Hispanic older adults: does perceived ethnic density moderate their relationship? J Immigr Minor Health. 2012;14(6):1107–1111. doi: 10.1007/s10903-011-9569-z. [DOI] [PubMed] [Google Scholar]
- 31.Mair C, Diez Roux AV, Osypuk TL, Rapp SR, Seeman T, Watson KE. Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Soc Sci Med. 2010;71(3):541–550. doi: 10.1016/j.socscimed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ornelas IJ, Perreira KM. The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Soc Sci Med. 2011;73(8):1169–1177. doi: 10.1016/j.socscimed.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. J Epidemiol Community Health. 2003;57(12):987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Syed M, Juan MJD. Discrimination and psychological distress: examining the moderating role of social context in a nationally representative study of Asian American adults. Asian Am J Psychol. 2012;3(2):104–120. [Google Scholar]
- 35.Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A. Stress and adiposity: a meta-analysis of longitudinal studies. Obesity (Silver Spring) 2011;19(4):771–778. doi: 10.1038/oby.2010.241. [DOI] [PubMed] [Google Scholar]
- 36.Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988–1994) Econ Hum Biol. 2007;5(2):179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grafova IB, Freedman VA, Kumar R, Rogowski J. Neighborhoods and obesity in later life. Am J Public Health. 2008;98(11):2065–2071. doi: 10.2105/AJPH.2007.127712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kirby JB, Liang L, Chen HJ, Wang Y. Race, place, and obesity: the complex relationships among community racial/ethnic composition, individual race/ethnicity, and obesity in the United States. Am J Public Health. 2012;102(8):1572–1578. doi: 10.2105/AJPH.2011.300452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ullmann SH, Goldman N, Pebley AR. Contextual factors and weight change over time: a comparison between U.S. Hispanics and other population sub-groups. Soc Sci Med. 2013;90:40–48. doi: 10.1016/j.socscimed.2013.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wen M, Maloney TN. Latino residential isolation and the risk of obesity in Utah: the role of neighborhood socioeconomic, built-environmental, and subcultural context. J Immigr Minor Health. 2011;13(6):1134–1141. doi: 10.1007/s10903-011-9439-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bertoni AG, Whitt-Glover MC, Chung H et al. The association between physical activity and subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2009;169(4):444–454. doi: 10.1093/aje/kwn350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Osypuk TL. Invited commentary: integrating a life-course perspective and social theory to advance research on residential segregation and health. Am J Epidemiol. 2013;177(4):310–315. doi: 10.1093/aje/kws371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allison P Fixed effects regression methods in SAS. Proceedings of the Thirty-first Annual SAS Users Group International Conference. Cary, NC: SAS Institute Inc; 2006. [Google Scholar]
- 44.Bild DE, Bluemke DA, Burke GL et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156(9):871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 46.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Washington, DC: US Census Bureau; 2001. Census 2000 summary file 1 and summary file 3—United States. [Google Scholar]
- 48.Washington, DC: US Census Bureau; 2012. Census 2010 summary file 1—United States. [Google Scholar]
- 49.Washington, DC: US Census Bureau; 2010. American Community Survey 5-year small area estimates 2005–2009. [Google Scholar]
- 50.Washington, DC: US Census Bureau; 2013. American Community Survey 5-year small area estimates 2007–2011. [Google Scholar]
- 51.Logan JR, Xu Z, Stults B. Interpolating US Decennial census tract data from as early as 1970 to 2010: a longitudinal tract database. Prof Geogr. 2014;66(3):2014. doi: 10.1080/00330124.2014.905156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moran A, Diez Roux AV, Jackson SA et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20(4):354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 53.Hu F. Obesity Epidemiology. New York, NY: Oxford University Press; 2008. [Google Scholar]
- 54.World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 55.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 56.Albrecht SS, Roux AV, Kandula NR, Osypuk TL, Ni H, Shrager S. Immigrant assimilation and BMI and waist size: a longitudinal examination among Hispanic and Chinese participants in the Multi-Ethnic Study of Atherosclerosis. Obesity (Silver Spring) 2013;21(8):1695–1703. doi: 10.1002/oby.20104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Portes A, Zhou M. The new second generation: segmented assimilation and its variants. Ann Am Acad Pol Soc Sci. 1993;530:74–96. [Google Scholar]
- 58.Osypuk TL, Bates LM, Acevedo-Garcia D. Another Mexican birthweight paradox? The role of residential enclaves and neighborhood poverty in the birthweight of Mexican-origin infants. Soc Sci Med. 2010;70(4):550–560. doi: 10.1016/j.socscimed.2009.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Portes A, Rumbaut RG. Not Everyone Is Chosen: Segmented Assimilation and Its Determinants. Legacies: The Story of the Immigrant Second Generation. Berkeley, CA: University of California Press; 2001. pp. 44–69. [Google Scholar]
- 60.Logan JR, Stults B. Separate and Unequal: The Neighborhood Gap for Blacks, Hispanics and Asians in Metropolitan America. Providence, RI: Brown University; 2011. [Google Scholar]
- 61.Kershaw KN, Albrecht SS. Metropolitan-level ethnic residential segregation, racial identity, and body mass index among US Hispanic adults: a multilevel cross-sectional study. BMC Public Health. 2014;14:283. doi: 10.1186/1471-2458-14-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Osypuk TL, Galea S. What level macro? Choosing appropriate levels to assess how place influences population health. In: Galea S, editor. Macrosocial Determinants of Population Health. New York, NY: Springer; 2005. pp. 399–435. [Google Scholar]
- 64.Lemelin ET, Diez Roux AV, Franklin TG et al. Life-course socioeconomic positions and subclinical atherosclerosis in the Multi-Ethnic Study of Atherosclerosis. Soc Sci Med. 2009;68(3):444–451. doi: 10.1016/j.socscimed.2008.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]