Abstract
Objectives. We describe and report findings from a screening program to identify sexually transmitted infections (STIs) and HIV among female inmates in Los Angeles County Jail.
Methods. Chlamydia and gonorrhea screening was offered to entering female inmates. Women were eligible if they were (1) aged 30 years or younger, or (2) pregnant or possibly pregnant, or (3) booked on prostitution or sex-related charges. Voluntary syphilis and HIV testing was offered to all women between 2006 and 2009. This analysis reports on data collected from 2002 through 2012.
Results. A total of 76 207 women participated in the program. Chlamydia prevalence was 11.4% and gonorrhea was 3.1%. Early syphilis was identified in 1.4% (141 of 9733) and the overall prevalence of HIV was 1.1% (83 of 7448). Treatment levels for early syphilis and HIV were high (99% and 100%, respectively), but only 56% of chlamydia and 58% of gonorrhea cases were treated.
Conclusions. Screening incarcerated women in Los Angeles County revealed a high prevalence of STIs and HIV. These inmates represent a unique opportunity for the identification of STIs and HIV, although strategies to improve chlamydia and gonorrhea treatment rates are needed.
The ability of correctional facilities to provide access to medically underserved and otherwise marginalized populations makes them an ideal location for health screening and prevention measures, representing an important public health opportunity.1–3 Populations passing through correctional facilities represent a group that is at increased risk for sexually transmitted infections (STIs), including HIV, as the prevalence of risk factors such as substance use, transactional sex, previous history of an STI, and inconsistent condom use with multiple partners is high.3–6 Furthermore, in some instances correctional facilities have noted higher prevalence of STIs and HIV than other institutions (e.g., sexual health clinics) serving high-risk clients. Studies of STI prevalence conducted in jails have revealed relatively high prevalence of chlamydia among inmates ranging from 7% to 22%, with gonorrhea prevalence ranging from less than 1% to 9%.7–10 Likewise, the prevalence of HIV among jail inmates is relatively high with an estimated 1.2% to 1.8% infected, compared with 0.3% in the US general population.11,12 In fact, modeling data suggests that approximately 14% of persons living with HIV pass through a correctional facility in their lifetime, with the proportion being as high as 20% among African Americans and Hispanics.13
Beyond reducing the disease burden in correctional facilities, the potential community-level benefits from programs aimed at STI and HIV prevention, screening, and treatment are substantial.8,11,12,14–16 An examination of community-level chlamydia prevalence following the establishment of a jail screening program in San Francisco, California, revealed a significant decline in chlamydia positivity among young women testing at community clinics serving a population with high incarceration rates.8 Specifically, the authors noted that chlamydia positivity among female attendees at a clinic located in a neighborhood in which the prevalence of jail testing was high declined from 16% in 1997 to 8% in 2004, while no changes occurred in a clinic located in a neighborhood with low jail testing (5% in 1997 and 5% in 2004).8 The potential community-level impact of STI screening services has been noted in other jail settings.14,15 In New York City, implementation of universal screening for men aged 35 years and younger entering jail resulted in a 59% increase in citywide reported male chlamydia case rate and the adult jails identified and reported 40% more cases than all 10 New York City public STI clinics.15 The population-level impact of jail screening is also supported by modeling data, which suggest that the community prevalence of chlamydia can be reduced by up to 54% by using jail-based chlamydia screen-and-treat programs.16
Despite the fact that correctional facilities serve populations that are at increased risk for STIs, screening services in jails are limited.17,18 Potential reasons for this are manifold, and include the competing agendas of security and control versus health and welfare, as well as other logistical concerns including staffing, space, and rapid turnover of inmates in jail settings.1,17 However, jail-based STI and HIV interventions could potentially have a significant public health impact. Jails, which are most often run by sheriff departments or local governments, are designed to hold individuals awaiting trial or serving short sentences. As such, a much larger number of people cycle through jails than through prisons with more than 12 million admissions in the United States in 2012 compared with nearly 700 000 for prisons.19,20 Recognizing an important public health opportunity, the Los Angeles County Sheriff’s Department (LASD) in California developed a partnership with the Los Angeles County Department of Public Health (DPH) to offer STI screening for female inmates in the Los Angeles County Jail—the largest jail system in the United States.21 The objective of this report is to describe our experience and report findings from this screening program among women incarcerated in the Los Angeles County Jail from 2002 to 2012.
METHODS
The Los Angeles County Jail has an annual intake of approximately 180 000 inmates and an average daily census of nearly 20 000.21 Women, who are housed in a separate facility from men, comprise a minority of the inmate population, with roughly 27 000 bookings per year,22 and an average daily census of 2000 inmates. Each week, approximately 500 women are processed through the women’s inmate reception center where they undergo booking procedures including medical screening (oral communication, M. Malek, LASD, June 2013).
Starting in 1999, a partnership between the DPH and LASD was established to maximize the opportunity afforded by detention of high-risk and otherwise hard-to-reach young women. The 2 agencies worked closely to establish standards for chlamydia and gonorrhea testing in the jails. Eligibility criteria for screening were informed by Centers for Disease Control and Prevention screening guidelines in place at the time23 as well as findings from a prevalence evaluation conducted in 1999 among 1000 entering female inmates. In this formative phase of the project, specimens were collected for chlamydia testing and those found to be positive for chlamydia were then screened for gonorrhea. Based on the findings from this work, all entering female inmates (“new bookings”) were determined to be eligible for chlamydia and gonorrhea screening if they met 1 of the following criteria: (1) aged 30 years or younger, or (2) pregnant or possibly pregnant (based on self-report), or (3) booked on charges related to prostitution or sex-related charges (based on self-report). Starting in 2006 screening efforts were expanded to include syphilis and HIV testing, which was offered to all entering female detainees regardless of age, pregnancy status, or sex-related charges. Syphilis and HIV screening was discontinued in 2009 because of resource and staffing issues.
Women were brought in groups from courts and police precincts throughout Los Angeles County to the jail for booking. Transport to the jail typically did not occur until later in the day with women arriving as early as 6 pm and frequently inmates continued to arrive as late as 10:30 pm, with intake and classification of inmates occurring throughout the night. All testing was conducted between the hours of 9 pm and 5 am to coincide with jail intake times. Screening for STIs and HIV was only offered to entering female inmates upon completion of jail intake procedures.
Screenings took place in the women’s inmate reception center—an oblong hall (35 × 15 yards), lined with holding cells with 1 to 20 women per cell. Sheriff deputies assisted with directing women to the testing station, which consisted of a mobile cart, table, and 2 chairs in the middle of the inmate reception center, and was staffed by health department personnel. The staff would speak individually to each inmate to obtain verbal consent, with written consent obtained only for those requesting HIV testing. Specifically, the staff would explain
that the DPH is offering free STI testing,
the importance of screening given the asymptomatic nature of most STIs,
the availability of treatment for those found positive,
the need for follow-up if those found positive are released before results are available, and
the voluntary nature of the screening program and emphasis on the fact that participation was not mandatory.
After consent procedures, women were directed to the holding cell toilet, which was located in a semiprivate space (i.e., short side-walls with no doors), to collect a urine specimen for chlamydia and gonorrhea nucleic acid amplification testing with the Aptima Combo 2 test (GenProbe, San Diego, CA). Blood samples were collected for syphilis and HIV screening via standard procedures in place at the Los Angeles County Public Health Laboratory. Specifically, syphilis testing was conducted with the rapid plasma regain test, with confirmatory testing done with the Treponema pallidum particle agglutination test, and HIV testing was based on standard antibody testing with Western blot confirmation. Specimens were picked up from the jail between 8 and 11 am on the days following screening (Tuesday–Saturday) and all specimens were processed by the public health laboratory within 96 hours of collection.
All positive test results were routed to jail medical services and those individuals still in custody were treated by LASD medical services. Test results were also released to DPH staff, who verified treatment of positive cases. In the event that an individual with a positive test result was released untreated, a health department community worker would follow up and provide field-delivered therapy, partner elicitation and notification, and counseling and health education services, as appropriate. To assist with postrelease follow-up, additional locating information was collected from women at the time of specimen collection. Other sources of locating information included LASD and Probation Department data and Department of Motor Vehicles records. In addition, all women received a “Sheriff’s department approved” palm card with health department contact information in case they chose to follow-up with the health department staff.
Demographic information including date of birth and race/ethnicity as well as laboratory testing information including the type of test taken (chlamydia, gonorrhea, syphilis, HIV) and the date of specimen collection were recorded for each inmate who participated in the screening program. Among inmates who tested positive, we obtained treatment status, date of treatment, and syphilis disposition from the health department disease registry database. We conducted descriptive statistics including means and frequency distributions for the total sample as well as by STI and HIV status. We evaluated differences between groups by using χ2 methods and we calculated associations between STIs and HIV and other factors with logistic regression analysis. We assessed trends in disease prevalence over time by using Cochran–Armitage test for trends. Data elements relevant to this analysis were available starting in 2002 and we included information collected through 2012. We conducted all analyses with SAS version 9.2 (SAS Institute, Cary, NC).
The DPH staff specifically designated for this project included 2 full-time phlebotomy-certified community workers who conducted all the testing, 1 full-time field worker responsible for follow-up on positive cases, 1 full-time office staff person providing general support including efforts related to data collection and maintenance of records, as well as 20% time for a supervising staff person. The DPH also provided resources for all costs related to laboratory testing including the cost of the tests, any supplies needed for testing (e.g., gloves, alcohol wipes, etc.), refrigerator to store samples, and courier service to pick up samples from the jail and transport them to the public health laboratory. Resources at the jail included provision of space for testing, help from deputies in routing women to the testing station, a designated jail infection control nurse who was responsible for providing clinical services, and treatment of those found to be positive.
RESULTS
From January 2002 through December 2012, a total of 76 207 female inmates were screened for chlamydia, gonorrhea, syphilis, or HIV. By design, the majority of inmates screened were younger than 30 years (79%), with African Americans comprising the single largest racial/ethnic group (39%), followed by Hispanics (37%; Table 1).
TABLE 1—
Baseline Characteristics of Incarcerated Women Screened for Sexually Transmitted Infections and HIV in Los Angeles County Jail: Los Angeles, CA, 2002–2012
| Characteristic | No.a (%) |
| Age, y | |
| 18–19 | 8167 (10.8) |
| 20–24 | 27 504 (36.2) |
| 25–29 | 24 370 (32.1) |
| 30–39 | 9646 (12.7) |
| ≥ 40 | 6261 (8.2) |
| Race/ethnicity | |
| African American | 26 128 (38.7) |
| Hispanic | 25 904 (38.4) |
| Other | 2520 (3.7) |
| White | 12 920 (19.2) |
| Pregnant or possibly pregnant | |
| Yes | 6977 (9.6) |
| No | 65 423 (90.4) |
| Prostitution or sex-related charges | |
| Yes | 15 166 (21.0) |
| No | 57 234 (79.1) |
Note. The sample size was n = 76 207.
Sum may not equal total because of missing information—age missing n = 259 (0.3%); race/ethnicity missing n = 8735 (11%); pregnancy status missing n = 3807 (5%); prostitution or sex-related charge missing n = 3807 (5%).
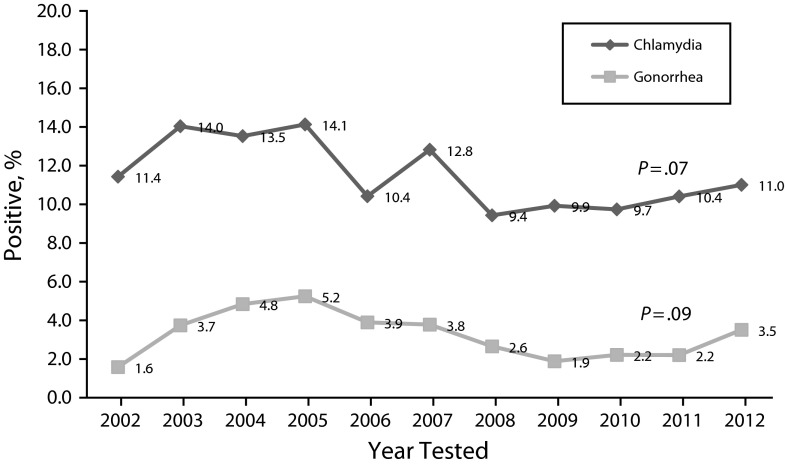
The overall prevalence of chlamydia was 11.4% and gonorrhea was 3.1% (Table 2). Although there were no statistically meaningful differences in the prevalence of these STIs over time, the highest prevalence for both chlamydia and gonorrhea was in 2005 at 14.1% and 5.2%, respectively (Figure 1). Furthermore, the prevalence of both infections was inversely related to age (Table 2), with the highest prevalence of chlamydia among those in the youngest age group (19% vs 4%; P < .01). Likewise, those in the youngest age groups had the highest prevalence of gonorrhea infection (5.3%) compared with those in the older age groups (1.7%; P < .01). Coinfections were also common, with 43% (1018 of 2355) of those testing positive for gonorrhea also testing positive for chlamydia. Although treatment information was only available for cases occurring before 2011, overall, 58% of chlamydia and 56% of gonorrhea cases were treated (4083 of 7099 and 1117 of 1999, respectively), with a median time to treatment of 8 days (interquartile range 6–12 days). The majority of the cases were treated while still in custody with 8% (n = 327) of chlamydia cases and 15% (n = 168) of gonorrhea cases receiving treatment by field staff following release from custody.
TABLE 2—
Prevalence of Chlamydia and Gonorrhea Among Incarcerated Women Testing at Los Angeles County Jail: Los Angeles, CA, 2002–2012
| Chlamydia |
Gonorrhea |
|||||
| Characteristic | No. of CT Tests | Positive CT Tests, No. (%)a | OR (95% CI) | No. of GC Tests | Positive GC Tests, No. (%)a | OR (95% CI) |
| Total | 74 567 | 8467 (11.4) | . . . | 75 303 | 2355 (3.1) | . . . |
| Age, y | ||||||
| 18–19 | 8053 | 1526 (18.9) | 5.5 (4.8, 6.3) | 8129 | 433 (5.3) | 3.3 (2.7, 4.1) |
| 20–24 | 27 152 | 3724 (13.7) | 3.7 (3.3, 4.3) | 27 399 | 931 (3.4) | 2.1 (1.7, 2.5) |
| 25–29 | 24 037 | 2317 (9.6) | 2.5 (2.2, 2.9) | 24 274 | 658 (2.7) | 1.6 (1.3, 2.0) |
| 30–39 | 9333 | 652 (7.0) | 1.8 (1.5, 2.1) | 9431 | 231 (2.4) | 1.5 (1.2, 1.9) |
| ≥ 40 | 5909 | 241 (4.1) | 1.0 (Ref) | 5982 | 100 (1.7) | 1.0 (Ref) |
| Race/ethnicity | ||||||
| African American | 25 553 | 2776 (10.9) | 1.1 (1.0, 1.2) | 25 826 | 989 (3.8) | 1.2 (1.1, 1.4) |
| Hispanic | 25 375 | 3191 (12.6) | 1.3 (1.2, 1.4) | 25 651 | 702 (2.7) | 0.9 (0.8, 1.0) |
| Other | 2453 | 287 (11.7) | 1.2 (1.0, 1.4) | 2468 | 58 (2.4) | 0.7 (0.6, 1.0) |
| White | 12 653 | 1271 (10.0) | 1.0 (Ref) | 12 802 | 399 (3.1) | 1.0 (Ref) |
| Pregnant or possibly pregnant | ||||||
| Yes | 6936 | 867 (12.5) | 1.1 (1.0, 1.2) | 6936 | 258 (3.7) | 1.2 (1.0, 1.3) |
| No | 64 720 | 7467 (11.5) | 1.0 (Ref) | 64 844 | 2070 (3.2) | 1.0 (Ref) |
| Prostitution or sex-related charges | ||||||
| Yes | 15 038 | 1562 (10.4) | 0.9 (0.8, 0.9) | 15 042 | 639 (4.2) | 1.4 (1.3, 1.6) |
| No | 56 618 | 6772 (12.0) | 1.0 (Ref) | 56 741 | 1689 (3.0) | 1.0 (Ref) |
Note. CI = confidence interval; CT = chlamydia; GC = gonorrhea; OR = odds ratio.
Sum may not equal total because of missing information—chlamydia tests: age missing n = 83 (0.1%); race/ethnicity missing n = 8533 (11%); pregnancy status missing n = 2911 (4%); prostitution or sex-related charge missing n = 2911 (4%); gonorrhea tests: age missing n = 88 (0.1%); race/ethnicity missing n = 8556 (11%); pregnancy status missing n = 3523 (n = 5%); prostitution or sex-related charge missing n = 3523 (5%).
FIGURE 1—
Prevalence of chlamydia and gonorrhea among incarcerated women in Los Angeles County Jail by year: Los Angeles, CA, 2002–2012.
Among the 9733 female inmates who were tested for syphilis, 1.4% were identified as having early syphilis defined as syphilis in the primary, secondary, or early latent stage (Table 3). Unlike chlamydia and gonorrhea, the prevalence of early syphilis was highest among those in the older age groups (4.2% among those aged 40 years or older) as well as those who identified as African American (2.3%) and White (1.8%; P < .1). A similar pattern was seen for HIV with an overall prevalence of 1.1% (83 of 7448) and higher prevalence among those in the older age groups (2.3% among those aged 40 years and older) and those who identified as White (2.3%) or African American (1.4%; P < .01). Information on sex-related charges was missing for 17% to 22% of those who tested for syphilis. Based on the data available, women booked on these charges were substantially more likely to have early syphilis (odds ratio = 6.3; 95% confidence interval = 4.0, 9.9) or HIV (odds ratio = 3.4; 95% confidence interval = 2.0, 5.8). In terms of treatment, 98.5% of early syphilis cases received treatment (n = 136), and all HIV-positive cases received treatment. Furthermore, all inmates who tested HIV-positive and were released from custody were successfully referred to a case manager to ensure linkage to health care.
TABLE 3—
Prevalence of Early Syphilis and HIV Among Incarcerated Women Testing at Los Angeles County Jail: Los Angeles, CA, 2006–2009
| Syphilis |
HIV |
|||||
| Characteristic | No. of Syphilis Testsa | Early Syphilisb Cases, No. (%)a | OR (95% CI) | No. of HIV Testsa | Positive HIV Tests, No. (%)a | OR (95% CI) |
| Total | 9733 | 141 (1.4) | . . . | 7448 | 83 (1.1) | . . . |
| Age, y | ||||||
| 18–19 | 924 | 0 (0.0) | . . . | 792 | 0 (0.0) | . . . |
| 20–24 | 2774 | 4 (0.1) | 0.03 (0.01, 0.09) | 2332 | 14 (0.6) | 0.3 (0.1, 0.5) |
| 25–29 | 2208 | 20 (0.9) | 0.2 (0.1, 0.3) | 1762 | 18 (1.0) | 0.4 (0.2, 0.8) |
| 30–39 | 1908 | 36 (1.9) | 0.4 (0.3, 0.6) | 1258 | 21 (1.7) | 0.7 (0.4, 1.3) |
| ≥ 40 | 1914 | 81 (4.2) | 1.0 (Ref) | 1300 | 30 (2.3) | 1.0 (Ref) |
| Race/ethnicity | ||||||
| African American | 3945 | 92 (2.3) | 1.3 (0.8, 2.0) | 3034 | 43 (1.4) | 0.6 (0.4, 1.0) |
| Hispanic | 3738 | 20 (0.5) | 0.3 (0.2, 0.5) | 2952 | 14 (0.5) | 0.2 (0.1, 0.4) |
| Other | 413 | 2 (0.5) | 0.3 (0.1, 1.1) | 316 | 3 (0.9) | 0.4 (0.1, 1.4) |
| White | 1443 | 26 (1.8) | 1.0 (Ref) | 1010 | 23 (2.3) | 1.0 (Ref) |
| Pregnant or possibly pregnant | ||||||
| Yes | 815 | 7 (0.9) | 0.8 (0.3, 1.6) | 623 | 7 (1.1) | 1.2 (0.6, 2.7) |
| No | 6800 | 77 (1.1) | 1.0 (Ref) | 5536 | 51 (0.9) | 1.0 (Ref) |
| Prostitution or sex-related charges | ||||||
| Yes | 1879 | 56 (3.0) | 6.3 (4.0, 9.9) | 1484 | 30 (2.0) | 3.4 (2.0, 5.8) |
| No | 5736 | 28 (0.5) | 1.0 (Ref) | 4675 | 28 (0.6) | 1.0 (Ref) |
Note. CI = confidence interval; OR = odds ratio.
Sum may not equal total because of missing information—syphilis tests: age missing n = 5 (0.05%); race/ethnicity missing n = 194 (2%); pregnancy status missing n = 2118 (22%); prostitution or sex-related charge missing n = 2118 (22%); HIV tests: age missing n = 4 (0.05%); race/ethnicity missing n = 136 (2%); pregnancy status missing n = 1289 (17%); prostitution or sex-related charge missing n = 1289 (17%).
Early syphilis defined as primary, secondary, and early latent syphilis.
DISCUSSION
Results from this large, multiyear analysis of women in Los Angeles County Jail indicate a high positivity rate for chlamydia (11%), gonorrhea (3%), early syphilis (1.4%), and HIV (1.1%). These findings are comparable to results from other screening programs in correctional settings and in fact closely follow the prevalence noted in public STI clinics in Los Angeles County.7,24–27 Furthermore, we found that whereas treatment rates for syphilis and HIV were high, improvements in chlamydia and gonorrhea treatment rates from the current rate of 56% to 58% will help to further the overall public health impact of this program. The high treatment rates for syphilis are partly explained by the fact that Los Angeles County is a high syphilis morbidity area28 with additional resources including field staff specifically designated for prevention and control efforts targeted to syphilis. In addition, the relatively small number of inmates with syphilis and HIV makes treatment and follow-up more manageable.
By comparison, the numbers of inmates positive for chlamydia and gonorrhea were much higher, which, along with the transient nature of jail populations, creates challenges for treatment and follow-up. There is evidence to suggest that median length of stay for jail inmates can be as low as 2 days.1,22 This was also demonstrated by our data, which showed that fewer than half the women with chlamydia or gonorrhea were treated in custody with the primary reason for lack of treatment relating to release from custody before laboratory results became available (range: 3–7 days after testing). In the event that an inmate with chlamydia or gonorrhea was released untreated, a health department community worker would follow up and provide field-delivered therapy, partner elicitation and notification, and health education and counseling, as appropriate. Because of extensive efforts by field staff we were able to increase treatment rates by 8% to 15% (to the total treatment rate of 56% to 58%), but clearly other strategies are needed. One promising strategy for a high-turnover jail setting would be implementation of point-of-care tests, such as the Cepheid Xpert CT/NG (Cepheid, Sunnyvale, CA). This test has similar sensitivity and specificity as the standard laboratory nucleic acid amplification tests currently in use, is simple to use, and provides results within 90 minutes of specimen collection.29,30
Furthermore, although our finding of high chlamydia and gonorrhea positivity, especially among those in the youngest age groups, is consistent with most studies of chlamydia and gonorrhea infections,7,24,31 these findings may in fact represent an underestimate of the true extent of morbidity. Recent studies among women indicate that a nontrivial proportion of chlamydia and gonorrhea infections occur at extragenital sites.32–37 For instance, rectal and pharyngeal gonorrhea testing among women at STI clinics revealed that 20% to 40% of gonorrhea cases would be missed by urogenital testing alone.35 Although data on self-collected pharyngeal swabs for STI testing are limited, a number of studies have demonstrated the validity and acceptability of self-collected rectal swabs.38–41 The lack of private space in a jail setting may hinder collection of rectal swabs; however, the high potential for missed opportunities for the identification and treatment of bacterial STIs warrants further investigation of screening at nonurethral sites in correctional settings.
Our results also demonstrate that the prevalence of early syphilis was relatively high. The proportion of women in correctional settings with reactive nontreponemal tests for syphilis ranges from 0.3% to 23.8%24; however, few studies report on syphilis disposition and whether reactive tests indicate active infection. Findings from incarcerated women in Rhode Island revealed that 0.4% were identified as having early syphilis,42 which is substantially lower than the 1.4% noted in our analyses. In fact, the prevalence of early syphilis among women was comparable to rates found among incarcerated men who have sex with men in Los Angeles.43 These findings lend additional support to the recommendation from the Centers for Disease Control and Prevention’s Jail Sexually Transmitted Disease Prevalence Monitoring Group that screening women in jails should be an integral part of syphilis prevention activities, especially in communities with high rates of active disease.24
The findings of this project should be interpreted in light of some of the limitations. Most importantly, the data for this project were collected as part of public health surveillance. Therefore, the extent of data was limited with no behavioral or medical history, and little incarceration data available for this analysis. Missing data for some of the factors of interest (e.g., solicitation charges among those testing for syphilis and HIV) also limit our interpretation of these findings. Furthermore, not all those meeting the eligibility criteria were tested. This was attributable to a number of factors including availability of space and staff, which limited testing to certain days and times. Also, the testing data represent each encounter with the system and not an individual inmate. It is likely that over the duration of the 10-year screening period women were reincarcerated and retested as part of the program. Although the implications of this may be limited in terms of the acute STIs such as chlamydia and gonorrhea, this has particular relevance for the HIV testing data, in that multiple tests may represent multiple encounters by the same inmate and not the number of persons who test positive or negative.
Despite these limitations, the surveillance data provide a useful and unique description of STI and HIV prevalence among women incarcerated in jail and suggest that jail-based testing can successfully reach an at-risk population, particularly one that may have limited access or be underserved by the health care system. Furthermore, we were able to demonstrate that successful collaborations between local health departments and jail officials can lead to the identification and treatment of a large number of STIs and HIV among female inmates.
Acknowledgments
M. Javanbakht was supported by a grant from the National Institutes of Health, National Institutes of Allergy and Infectious Diseases (grant K01AI091861).
Human Participant Protection
This project received exemption from the institutional review board because it was deemed to be an evaluation of an existing public health program.
References
- 1.Spaulding AC, Perez SD, Seals RM et al. Diversity of release patterns for jail detainees: implications for public health interventions. Am J Public Health. 2011;101(suppl 1):S347–S352. doi: 10.2105/AJPH.2010.300004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glaser JB, Greifinger RB. Correctional health care: a public health opportunity. Ann Intern Med. 1993;118(2):139–145. doi: 10.7326/0003-4819-118-2-199301150-00010. [DOI] [PubMed] [Google Scholar]
- 3.Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000;90(12):1939–1941. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cotten-Oldenburg NU, Jordan BK, Martin SL et al. Women inmates’ risky sex and drug behaviors: are they related? Am J Drug Alcohol Abuse. 1999;25(1):129–149. doi: 10.1081/ada-100101850. [DOI] [PubMed] [Google Scholar]
- 5.Washington, DC: Bureau of Justice Statistics; 2004. Profile of jail inmates, 2002. NCJ 201932. [Google Scholar]
- 6.Beltrami JF, Cohen DA, Hamrick JT et al. Rapid screening and treatment for sexually transmitted diseases in arrestees: a feasible control measure. Am J Public Health. 1997;87(9):1423–1426. doi: 10.2105/ajph.87.9.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mertz KJ, Schwebke JR, Gaydos CA et al. Screening women in jails for chlamydial and gonococcal infection using urine tests: feasibility, acceptability, prevalence, and treatment rates. Sex Transm Dis. 2002;29(5):271–276. doi: 10.1097/00007435-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Barry PM, Kent CK, Scott KC et al. Is jail screening associated with a decrease in chlamydia positivity among females seeking health services at community clinics?—San Francisco, 1997–2004. Sex Transm Dis. 2009;36(2 suppl):S22–S28. doi: 10.1097/OLQ.0b013e31815ed7c8. [DOI] [PubMed] [Google Scholar]
- 9.Joesoef MR, Weinstock HS, Kent CK et al. Sex and age correlates of chlamydia prevalence in adolescents and adults entering correctional facilities, 2005: implications for screening policy. Sex Transm Dis. 2009;36(2 suppl):S67–S71. doi: 10.1097/OLQ.0b013e31815d6de8. [DOI] [PubMed] [Google Scholar]
- 10.Arriola KR, Braithwaite RL, Kennedy S et al. A collaborative effort to enhance HIV/STI screening in five county jails. Public Health Rep. 2001;116(6):520–529. doi: 10.1016/S0033-3549(04)50084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The health status of soon-to-be released inmates. Chicago, IL: National Commission on Correctional Health Care; 2002. a report to congress. Vol 1. [Google Scholar]
- 12.The health status of soon-to-be released inmates. Chicago, IL: National Commission on Correctional Health Care; 2002. a report to congress. Vol 2; pp. 1–239. [Google Scholar]
- 13.Spaulding AC, Seals RM, Page MJ et al. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4:e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broad J, Cox T, Rodriguez S et al. The impact of discontinuation of male STD screening services at a large urban county jail: Chicago, 2002–2004. Sex Transm Dis. 2009;36(2 suppl):S49–S52. doi: 10.1097/OLQ.0b013e318156159a. [DOI] [PubMed] [Google Scholar]
- 15.Pathela P, Hennessy RR, Blank S et al. The contribution of a urine-based jail screening program to citywide male chlamydia and gonorrhea case rates in New York City. Sex Transm Dis. 2009;36(2 suppl):S58–S61. doi: 10.1097/OLQ.0b013e31815615bb. [DOI] [PubMed] [Google Scholar]
- 16.Owusu-Edusei K, Jr, Gift TL, Chesson HW et al. Investigating the potential public health benefit of jail-based screening and treatment programs for chlamydia. Am J Epidemiol. 2013;177(5):463–473. doi: 10.1093/aje/kws240. [DOI] [PubMed] [Google Scholar]
- 17.Parece MS, Herrera GA, Voigt RF et al. STD testing policies and practices in U.S. city and county jails. Sex Transm Dis. 1999;26(8):431–437. doi: 10.1097/00007435-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Chicago, IL: National Commission on Correctional Health Care; 2008. Standards for health services in jails. [Google Scholar]
- 19.Minton T. Washington, DC: Bureau of Justice Statistics; 2013. Jail inmates at midyear 2012—statistical tables. NCJ Publication No. 241264. [Google Scholar]
- 20.Carson EA, Mulako-Wangota J. Bureau of Justice Statistics. Count of total admissions, generated using the Corrections Statistical Analysis Tool (CSAT) – prisoners. Available at: http://www.bjs.gov. Accessed August 2, 2013.
- 21.Minton T. Washington, DC: Bureau of Justice Statistics; 2011. Jail inmates at midyear 2010—statistical tables. NCJ Publication No. 233431. [Google Scholar]
- 22.Malek M, Bazazi AR, Cox G et al. Implementing opt-out programs at Los Angeles county jail: a gateway to novel research and interventions. J Correct Health Care. 2011;17(1):69–76. doi: 10.1177/1078345810385916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep. 2002;51(RR-6):1–78. [PubMed] [Google Scholar]
- 24.Mertz KJ, Voigt RA, Hutchins K et al. Findings from STD screening of adolescents and adults entering corrections facilities: implications for STD control strategies. Sex Transm Dis. 2002;29(12):834–839. doi: 10.1097/00007435-200212000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Los Angeles, CA: Los Angeles County Department of Public Health, Sexually Transmitted Disease Program; 2010. STD clinic morbidity report, Los Angeles County; pp. I-1–XIV-8. [Google Scholar]
- 26.Los Angeles, CA: Los Angeles County Department of Public Health, Sexually Transmitted Disease Program; 2007. STD clinic morbidity report, Los Angeles County; pp. I-1–XVII-2. [Google Scholar]
- 27.Willers DM, Peipert JF, Allsworth JE et al. Prevalence and predictors of sexually transmitted infection among newly incarcerated females. Sex Transm Dis. 2008;35(1):68–72. doi: 10.1097/OLQ.0b013e318154bdb2. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2012. Atlanta, GA: US Department of Health and Human Services; 2013. [Google Scholar]
- 29.Gaydos CA, Van Der Pol B, Jett-Goheen M et al. Performance of the Cepheid CT/NG Xpert Rapid PCR Test for detection of Chlamydia trachomatis and Neisseria gonorrhoeae. J Clin Microbiol. 2013;51(6):1666–1672. doi: 10.1128/JCM.03461-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldenberg SD, Finn J, Sedudzi E et al. Performance of the GeneXpert CT/NG assay compared to that of the Aptima AC2 assay for detection of rectal Chlamydia trachomatis and Neisseria gonorrhoeae by use of residual Aptima samples. J Clin Microbiol. 2012;50(12):3867–3869. doi: 10.1128/JCM.01930-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bernstein KT, Stephens SC, Barry PM et al. Chlamydia trachomatis and Neisseria gonorrhoeae transmission from the oropharynx to the urethra among men who have sex with men. Clin Infect Dis. 2009;49(12):1793–1797. doi: 10.1086/648427. [DOI] [PubMed] [Google Scholar]
- 32.Barry PM, Kent CK, Philip SS et al. Results of a program to test women for rectal chlamydia and gonorrhea. Obstet Gynecol. 2010;115(4):753–759. doi: 10.1097/AOG.0b013e3181d444f6. [DOI] [PubMed] [Google Scholar]
- 33.Javanbakht M, Gorbach P, Stirland A et al. Prevalence and correlates of rectal chlamydia and gonorrhea among female clients at sexually transmitted disease clinics. Sex Transm Dis. 2012;39(12):917–922. doi: 10.1097/OLQ.0b013e31826ae9a2. [DOI] [PubMed] [Google Scholar]
- 34.Hunte T, Alcaide M, Castro J. Rectal infections with chlamydia and gonorrhoea in women attending a multiethnic sexually transmitted diseases urban clinic. Int J STD AIDS. 2010;21(12):819–822. doi: 10.1258/ijsa.2010.009279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giannini CM, Kim HK, Mortensen J et al. Culture of non-genital sites increases the detection of gonorrhea in women. J Pediatr Adolesc Gynecol. 2010;23(4):246–252. doi: 10.1016/j.jpag.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Peters RP, Nijsten N, Mutsaers J et al. Screening of oropharynx and anorectum increases prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae infection in female STD clinic visitors. Sex Transm Dis. 2011;38(9):783–787. doi: 10.1097/OLQ.0b013e31821890e9. [DOI] [PubMed] [Google Scholar]
- 37.Shaw SG, Hassan-Ibrahim M, Soni S. Are we missing pharyngeal and rectal infections in women by not testing those who report oral and anal sex? Sex Transm Infect. 2013;89(5):397. doi: 10.1136/sextrans-2013-051159. [DOI] [PubMed] [Google Scholar]
- 38.Freeman AH, Bernstein KT, Kohn RP et al. Evaluation of self-collected versus clinician-collected swabs for the detection of Chlamydia trachomatis and Neisseria gonorrhoeae pharyngeal infection among men who have sex with men. Sex Transm Dis. 2011;38(11):1036–1039. doi: 10.1097/OLQ.0b013e318227713e. [DOI] [PubMed] [Google Scholar]
- 39.Alexander S, Ison C, Parry J et al. Self-taken pharyngeal and rectal swabs are appropriate for the detection of Chlamydia trachomatis and Neisseria gonorrhoeae in asymptomatic men who have sex with men. Sex Transm Infect. 2008;84(6):488–492. doi: 10.1136/sti.2008.031443. [DOI] [PubMed] [Google Scholar]
- 40.Moncada J, Schachter J, Liska S et al. Evaluation of self-collected glans and rectal swabs from men who have sex with men for detection of Chlamydia trachomatis and Neisseria gonorrhoeae by use of nucleic acid amplification tests. J Clin Microbiol. 2009;47(6):1657–1662. doi: 10.1128/JCM.02269-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van der Helm JJ, Hoebe CJ, van Rooijen MS et al. High performance and acceptability of self-collected rectal swabs for diagnosis of Chlamydia trachomatis and Neisseria gonorrhoeae in men who have sex with men and women. Sex Transm Dis. 2009;36(8):493–497. doi: 10.1097/OLQ.0b013e3181a44b8c. [DOI] [PubMed] [Google Scholar]
- 42.Rich JD, Hou JC, Charuvastra A et al. Risk factors for syphilis among incarcerated women in Rhode Island. AIDS Patient Care STDS. 2001;15(11):581–585. doi: 10.1089/108729101753287676. [DOI] [PubMed] [Google Scholar]
- 43.Javanbakht M, Murphy R, Harawa N et al. Sexually transmitted infections and HIV prevalence among incarcerated men who have sex with men, 2000–2005. Sex Transm Dis. 2009;36(2 suppl):S17–S21. doi: 10.1097/OLQ.0b013e31815e4152. [DOI] [PubMed] [Google Scholar]