Abstract
This study seeks to inform clinical application of cell-free fetal DNA (cffDNA) screening as a novel method for prenatal trisomy detection by investigating public attitudes towards this technology and demographic and experiential characteristics related to these attitudes. Two versions of a 25-item survey assessing interest in cffDNA and existing first-trimester combined screening for either trisomy 13 and 18 or trisomy 21 were distributed among 3,164 members of the United States public. Logistic regression was performed to determine variables predictive of interest in screening options. Approximately 47% of respondents expressed an interest in cffDNA screening for trisomy 13, 18, and 21, with a majority interested in cffDNA screening as a stand-alone technique. A significantly greater percent would consider termination of pregnancy following a diagnosis of trisomy 13 or 18 (52%) over one of trisomy 21 (44%). Willingness to consider abortion of an affected pregnancy was the strongest correlate to interest in both cffDNA and first-trimester combined screening, although markedly more respondents expressed an interest in some form of screening (69% and 71%, respectively) than would consider termination. Greater educational attainment, higher income, and insurance coverage predicted interest in cffDNA screening; stronger religious identification also corresponded to decreased interest. Prior experience with disability and genetic testing was associated with increased interest in cffDNA screening. Several of these factors, in addition to advanced age and Asian race, were, in turn, predictive of respondents’ increased willingness to consider post-diagnosis termination of pregnancy. In conclusion, divergent attitudes towards cffDNA screening - and prenatal options more generally – appear correlated with individual socioeconomic and religious backgrounds and experiences with disability and genetic testing. Clinical implementation and counseling for novel prenatal technologies should take these diverse stakeholder values into consideration.
Keywords: Cell-free fetal DNA, non-invasive prenatal screening, non-invasive prenatal testing, public attitudes, prenatal genetic counseling
Introduction
Non-invasive screening using cell-free fetal DNA (cffDNA) is poised to transform the practice of prenatal genetic diagnosis and has received significant media and academic attention (Greely, 2011). The benefits of cffDNA screening, which entails the analysis of admixed maternal and fetal DNA circulating in the blood of pregnant women, may include a lack of procedure-related miscarriage risk, early timing of use, and improved sensitivity and specificity over existing screening methods (P. A. Benn & Chapman, 2009; Lo & Chiu, 2012). CffDNA screening for trisomy 21 was introduced commercially in the United States in late 2011 by Sequenom, Inc., and the company expanded screening to include trisomy 13 and 18 detection in early 2012. At least three additional firms located in the United States have introduced similar screening over the past 2 years, covering an increasing number of detectable chromosomal anomalies (Heger, 2012). Ongoing research promises eventual application of cffDNA technology to the detection of single-gene traits and copy number variation across the whole fetal genome (Bianchi, Sehnert, & Rava, 2012; Kitzman et al., 2012; Peters et al., 2011).
Clinical uptake of Sequenom’s trisomy test has exceeded the company’s initial sales predictions, reaching a projected 120,000 orders in the first year (Heger, 2013). However, uptake to date represents a fraction of the 2,500,000 women who undergo prenatal screening and 200,000 women who receive diagnostic testing in the United States each year (Olney et al., 1995; Palomaki, Knight, McCarthy, Haddow, & donhowe, 1997). It is difficult to predict how changing test indications, performance, cost, and access, the level of familiarity among providers and patients, and the issuance of guidelines by professional organizations, such as recommendations announced by the National Society of Genetic Counselors and the American Congress of Obstetricians and Gynecologists, will affect adoption rates for this technology (P. Benn et al., 2011; “Committee opinion number 545: Noninvasive prenatal testing for fetal aneuploidy,” 2012; Devers et al., 2012). Moreover, a growing body of literature demonstrates that the attitudes of pregnant women towards prenatal screening and diagnosis are influenced by a variety of factors, including ethnic and racial identity, age, socioeconomic status, experience with disability, and cultural and religious beliefs, such as those regarding the nature of the condition being tested and the acceptability of termination of pregnancy (Case, Ramadhani, Canfield, & Wicklund, 2007; Kuppermann, Gates, & Washington, 1996; Kuppermann et al., 2011; Rapp, 1998).
Preliminary evidence suggests that uptake of cffDNA screening may stratify along demographic lines; in two previous studies, women who were older, more educated, or of white or Asian race reported greater interest in receiving non-invasive prenatal screening (Tischler, Hudgins, Blumenfeld, Greely, & Ormond, 2011; Zamerowski, Lumley, Arreola, Dukes, & Sullivan, 2001). To date, however, no comprehensive study has been conducted to determine how these factors are associated with emerging public attitudes towards this technology, particularly in comparison with extant prenatal screening and diagnostic practices. Additionally, while other studies have been limited to women of reproductive age, we survey a sample of individuals representing broad demographic characteristics of the United States general public. Prior research demonstrates that the outlook of the general public towards prenatal technology has multifaceted interplay with the sociocultural and regulatory context in which pregnant women make reproductive decisions (Garcia, Timmermans, & van Leeuwen, 2008b; Kelly & Farrimond, 2012). We provide documentation of public attitudes that may exert influence on pregnant women and their families, healthcare practitioners, technology developers, insurance providers, and policymakers.
The purpose of this study is to assess expected interest in cffDNA screening for trisomy 13, 18, and 21 among the general public of the United States in order to understand how the technology may be received by diverse stakeholders. We utilize demographic data and information regarding personal experience with parenthood, disability, and genetic testing to predict who expresses interest in undergoing cffDNA screening. We additionally query interest in existing prenatal screening methods and attitudes towards the consideration of termination following detection of trisomy in order to place cffDNA screening into the existing, complex framework of prenatal diagnosis and care.
Methods
Instrumentation
A 25-question web-based survey was designed to address attitudes towards cffDNA screening in relation to existing first-trimester combined screening and diagnostic technologies. The survey was grounded in concepts and questions posed in the literature and through previous empirical research conducted by our team (Sayres, Allyse, Norton, & Cho, 2011). A broader team of bioethics scholars reviewed this survey for readability and content.
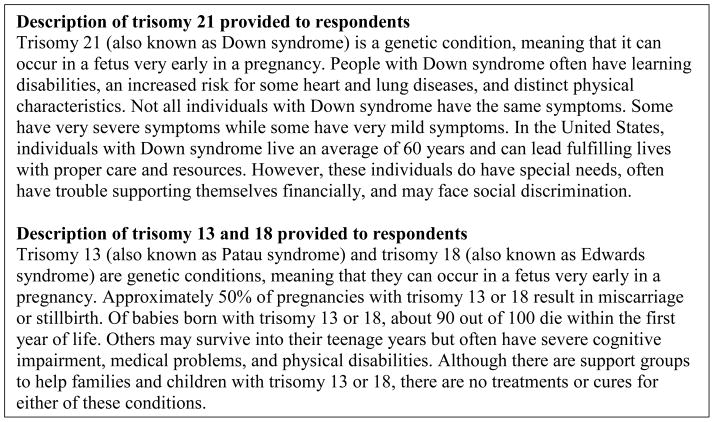
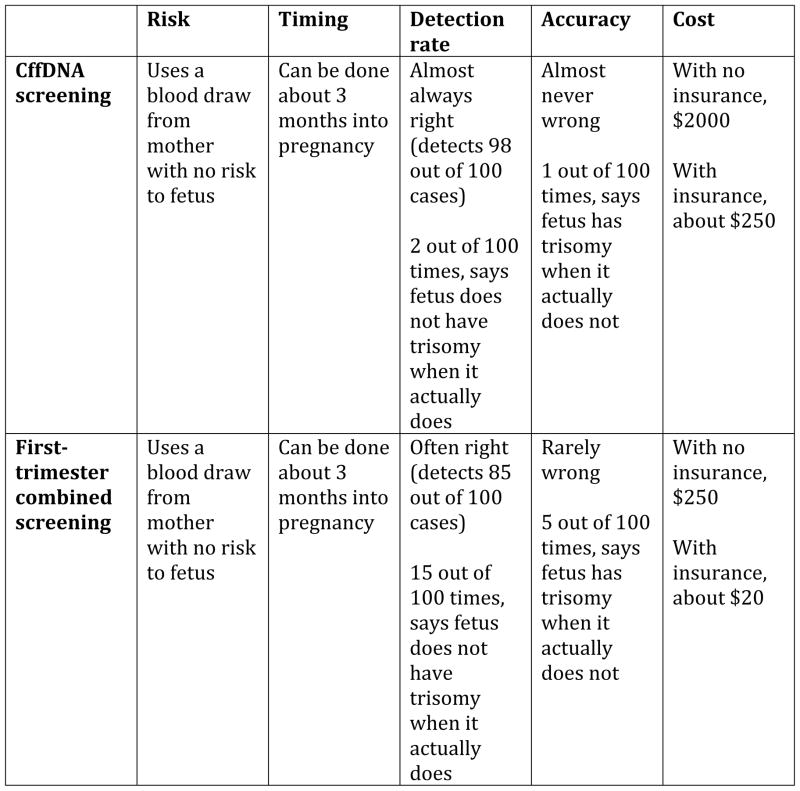
Two versions of the survey were developed - one addressing screening for trisomy 13 and 18 and the other addressing screening for trisomy 21 – and approximately half of respondents were randomly assigned to receive each version. This dichotomy of trisomy 13 and 18 and trisomy 21 as test conditions was used to establish whether the difference in morbidity and mortality associated with these conditions influenced respondents’ attitudes toward prenatal screening. We chose to use two versions to maintain a short expected length of completion (fewer than ten minutes); our sample size for each version was calculated to allow us sufficient power to perform the statistical analyses presented herein. Aside from the short descriptions of either trisomy 13 and 18 or trisomy 21 provided (see Figure 1), each version included identical sets of questions. The survey provided information about the features and costs of each screening method, including cffDNA and existing first-trimester combined screening (see Figure 2, (Malone et al., 2005)). Respondents were asked to consider questions in the appropriate prenatal context, i.e. making decisions for either themselves or a loved one. Two questions addressed respondent interest in cffDNA screening in addition to or instead of existing screening methods and whether respondents would consider termination of pregnancy following prenatal detection of trisomy 13 or 18 and trisomy 21. The survey included fifteen questions soliciting respondents’ demographic information and personal experiences that may be relevant to their attitudes towards prenatal genetic screening, including prior experience with mental illness or physical disability and doctor-ordered or purchased genetic testing. Eight additional questions regarding other aspects of respondents’ interest in prenatal screening are considered in a separate manuscript (Allyse, Sayres, Goodspeed, & Cho, 2013).
Figure 1.
Description of trisomy 13, 18, and 21 provided to respondents
Figure 2.
Description of cffDNA and first-trimester combined screening provided to respondents
Approximately two hundred individuals (one hundred individuals for the trisomy 13 and 18 version and one hundred individuals for the trisomy 21 version) completed a pilot version of the survey to ensure readability and comprehension. Following minor revisions, final versions of the survey were distributed and completed by approximately three thousand additional respondents.
Procedures
We contracted with a web-based survey provider, Zoomerang, to send this survey to a sample of adults ages eighteen years and older on the company’s user panel, which is designed to represent the primary demographic features of the United States general public. Zoomerang contacted individuals on their panel via electronic mail with a web link to the survey and permitted responses until a specified number of complete response sets are collected. Zoomerang ensured that a random, non-overlapping sample of its panel members would be invited to complete each of the two versions of the survey. To ensure the validity of responses, Zoomerang reviewed the quality of prospective panelists in advance and de-duplicated responses using digital fingerprinting. Respondents were compensated for their time and effort through the web-based survey provider; our research team did not directly communicate with the respondents or provide compensation. The Stanford University Institutional Review Board approved the exempt status of this study and waived informed consent procedures.
Data analysis
We downloaded individual responses, identified by a unique code assigned by the survey provider, through a secure website. Responses were numerically coded and statistical analysis was performed using version 20.0 of the SPSS Standard Statistics package.
Logistic regression analyses were performed to determine whether demographic and experiential indicators correlated to interest in prenatal screening and consideration of pregnancy termination following trisomy detection, adjusting for whether respondents were asked about trisomy 13 and 18 or trisomy 21. To determine whether the demographic and experiential predictors were robust, we conducted multivariate regression analyses combining all significant predictive variables. For all statistical analyses, α is set to 0.05; p-values greater than 0.05 are reported as “not significant”. Responses to trisomy 13 and 18 and trisomy 21 versions of the survey were compared using chi-square and Mann-Whitney tests for categorical and ordinal data respectively; these findings are reported in a separate manuscript (Allyse et al., 2013).
Results
Demographic and experiential characteristics
We received 3,164 responses to our survey: 1,657 for trisomy 13 and 18 and 1,507 for trisomy 21. Because the survey provider rendered the web link to the survey inactive after a predetermined number of responses, we cannot know how many individuals received the survey but chose not to complete it or did not complete it before the web link closed. Some respondents did not answer all demographic and experiential questions, and thus sample size varies slightly by question (see Tables I and II). All 3,164 respondents provided answers to all questions regarding interest in various forms of prenatal screening.
Table I.
Demographic characteristics of respondents (N=3164)*
| Gender | |
| Female | 55% (1739) |
| Male | 45% (1425) |
|
| |
| Age | |
| 18 to 24 years | 14% (451) |
| 25 to 34 years | 22% (710) |
| 35 to 44 years | 22% (700) |
| 45 to 54 years | 16% (510) |
| 55 to 64 years | 10% (330) |
| 65 years and over | 15% (463) |
|
| |
| Ethnicity | |
| Hispanic or Latino | 7% (219) |
| Not Hispanic or Latino | 93% (2743) |
|
| |
| Race† | |
| American Indian or Alaska Native | 2% (64) |
| Asian | 6% (194) |
| Black or African-American | 8% (264) |
| Native Hawaiian or Pacific Islander | 1% (21) |
| White | 84% (2642) |
|
| |
| Educational attainment | |
| Some high school | 2% (71) |
| High school diploma | 19% (596) |
| Some college | 31% (967) |
| College diploma | 34% (1072) |
| Graduate school diploma | 14% (458) |
|
| |
| Household income | |
| Under $25,000 | 20% (641) |
| $25,000 to $49,999 | 28% (887) |
| $50,000 to $74,999 | 23% (727) |
| $75,000 to $99,999 | 14% (449) |
| $100,000 and over | 15% (460) |
|
| |
| Health insurance status | |
| Insured | 86% (2692) |
| Not insured | 14% (452) |
|
| |
| Religion† | |
| Catholic | 23% (728) |
| Evangelical Protestant | 10% (303) |
| Other Protestant | 17% (538) |
| Mormon | 2% (69) |
| Jewish | 4% (127) |
| Buddhist | 1% (31) |
| Muslim | 1% (19) |
| Unaffiliated | 22% (692) |
|
| |
| Religiosity | |
| Very religious | 22% (639) |
| Somewhat religious | 41% (1226) |
| Not very religious | 21% (611) |
| Not religious | 16% (486) |
Values reported as % (#). For select questions, N<3164.
Participants may select any number of responses; thus percentages may not add to 100%.
Table II.
Experiential characteristics of respondents (N=3164)*
| Experience as a parent | |
| Yes | 59% (1877) |
| No | 41% (1287) |
|
| |
| Experience with physical disability | |
| Yes | 30% (938) |
| No | 68% (2145) |
| I don’t know | 3% (81) |
|
| |
| Experience with mental illness or disability | |
| Yes | 35% (1105) |
| No | 62% (1963) |
| I don’t know | 3% (96) |
|
| |
| Experience with doctor-ordered genetic test | |
| Yes | 9% (293) |
| No | 82% (2596) |
| I don’t know | 9% (271) |
|
| |
| Experience with purchased genetic test | |
| Yes | 6% (204) |
| No | 85% (2659) |
| I don’t know | 9% (276) |
Values reported as % (#). For select questions, N<3164.
Respondent demographic characteristics are summarized in Table I. A nearly equal proportion of females and males participated, and ages of respondents spanned cohorts from 18 to 24 years to 65 years and older. Most respondents identified as non-Hispanic and white. A majority of respondents had attended some college or had a college degree; income brackets from under $25,000 to $100,000 and higher were well-represented among respondents. Nearly all respondents carried some form of health insurance. Various denominations of Christianity, and particularly Catholicism, were the most frequently identified religious affiliations. However, one-fifth of participants did not identify with a religion, and many self-reported as “not religious” or “not very religious”.
We asked respondents about five life experiences that might affect their interest in prenatal genetic screening; our findings are summarized in Table II. Greater than one-half of respondents were parents. Many reported personal experience with disability, as either they or someone close to them had experienced physical disability or mental illness or disability. Respondents were asked whether they had experience undergoing genetic testing with several examples of said tests provided to them. Approximately one-tenth of respondents stated that they had had a doctor order a genetic test for them, and fewer noted that they had purchased a genetic test for themselves or a loved one.
Expressed interest in prenatal screening
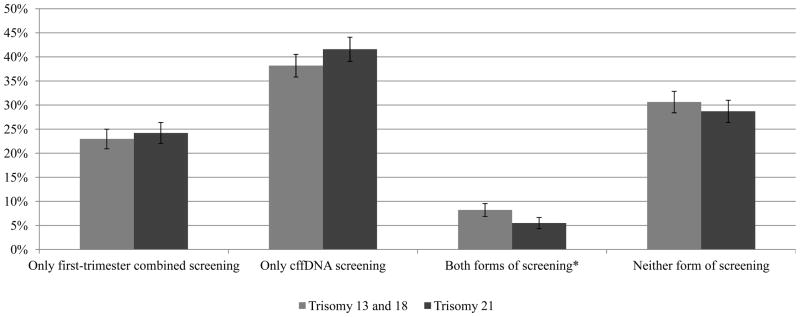
Respondents were asked to consider whether they would be interested in cffDNA or first-trimester combined screening, or both, for trisomy 13 and 18 or trisomy 21. As denoted in Figure 3, 38% of respondents to the survey on trisomy 13 and 18 expressed interest in only cffDNA screening, and 8% expressed interest in both cffDNA and first-trimester combined screening, for a sum of 46% demonstrating interest in cffDNA testing. By contrast, 42% of those responding to the trisomy 21 version preferred only cffDNA screening. and 5% showed an interest in both cffDNA and first-trimester combined screening; a total of 47% of individuals documented interest in cffDNA screening for trisomy 21. Of note, 31% and 29% respectively stated that they were not interested in any screening for trisomy 13 and 18 or trisomy 21. The only significant difference between respondents being asked about screening for trisomy 13 and 18 and trisomy 21 was the rates of individuals who noted interest in both cffDNA and combined screening, with a greater interest in both screening options when queried regarding trisomy 13 and 18 (χ2(1, N=2202)=10.601, p=0.001).
Figure 3.
Interest in first-trimester combined screening and cffDNA screening for trisomy (N=3133)
* Interest in both forms of screening varied significantly between trisomy 13 and 18 and trisomy 21 (p=0.001).
Consideration of termination of pregnancy
Respondents were asked whether they would consider termination of pregnancy following a diagnosis of fetal trisomy 13 or 18 or trisomy 21. As highlighted in Figure 4, 52% of those surveyed about trisomy 13 and 18 and 44% of those surveyed about trisomy 21 indicated that they would contemplate pregnancy termination following prenatal diagnosis. The discrepancy in rates of consideration of termination following trisomy diagnosis constitutes a statistically significant difference between responses to the trisomy 13 and 18 and trisomy 21 versions of the survey (χ2(1, N=2962)=18.775, p<0.001).
Figure 4.
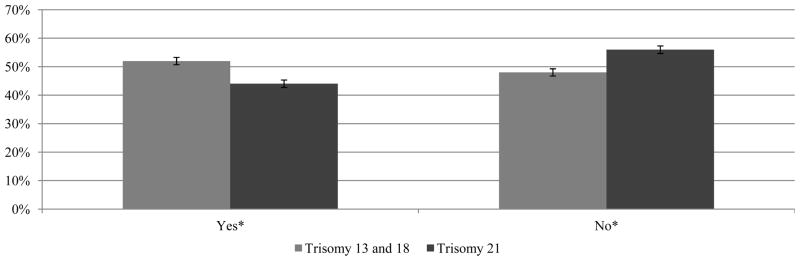
Consideration of termination of pregnancy following detection of trisomy (N=2962)
* Consideration of termination of pregnancy varied significantly between trisomy 13 and 18 and trisomy 21 (p<0.001).
Demographic and experiential predictors of interest in screening
Using logistic regression analyses adjusting for the two versions of the survey, we determined the demographic or experiential characteristics that were predictive of respondents’ expressed interest in cffDNA screening or in any prenatal screening.
Table III highlights the significant predictors of interest in cffDNA screening for trisomy. Greater educational attainment (odds ratio (OR)=1.171, p<0.001), higher household income (OR=1.271, p<0.001), and health insurance coverage (OR=1.594, p<0.001), were positively predictive of interest. Additionally, individuals who identified as Jewish were more likely to be interested cffDNA screening (OR=2.020, p=0.003), although self-reported level of religiosity corresponded negatively to a preference for screening (OR=0.886, p=0.013). Prior experience with genetic testing – either doctor-ordered (OR=1.499, p=0.010) or purchased (OR=1.591, p=0.013) – significantly predicted interest in cffDNA screening. Finally, respondents who were more likely consider termination of pregnancy following detection of fetal trisomy were more likely to note interest in cffDNA screening (OR=1.619, p<0.001).
Table III.
Predictors of interest in cffDNA screening for trisomy (N=3164)
| Demographic or experiential variable | Odds ratio | Wald χ2 statistic | p-value* |
|---|---|---|---|
| Gender | N.S. | ||
| Age | N.S. | ||
| Ethnicity | |||
| Hispanic or Latino | N.S. | ||
| Race | |||
| American Indian or Alaska Native | N.S. | ||
| Asian | N.S. | ||
| Black or African-American | N.S. | ||
| Native Hawaiian or Pacific Islander | N.S. | ||
| White | N.S. | ||
| Educational attainment | 1.171 | 20.476 | <0.001† |
| Household income | 1.271 | 46.866 | <0.001 |
| Health insurance status | 1.594 | 12.816 | <0.001† |
| Religion | |||
| Catholic | N.S. | ||
| Evangelical Protestant | N.S. | ||
| Other Protestant | N.S. | ||
| Mormon | N.S. | ||
| Jewish | 2.020 | 8.689 | 0.003† |
| Buddhist | N.S. | ||
| Muslim | N.S. | ||
| Unaffiliated | N.S. | ||
| Religiosity | 0.886 | 6.192 | 0.013† |
| Experience as a parent | N.S. | ||
| Experience with physical disability | N.S. | ||
| Experience with mental illness or disability | N.S. | ||
| Experience with doctor-ordered genetic test | 1.499 | 6.671 | 0.010† |
| Experience with purchased genetic test | 1.591 | 6.231 | 0.013† |
| Consideration of pregnancy termination | 1.619 | 24.908 | <0.001 |
N.S.=not significant. All p-values are reported using logistic regressional analysis adjusting for whether respondents were queried regarding trisomy 13 and 18 or trisomy 21.
This predictive variable does not remain significant in a multivariate logistic regression of all individually significant predictors of interest.
A multivariate logistic regression analysis containing each of these eight variables indicated adjusted significant relationships between interest in cffDNA screening and household income (OR=1.232, p<0.001) and interest in cffDNA screening and consideration of abortion (OR=1.451, p<0.001). No other variables remained predictive in this model.
Table IV displays factors that are predictive of interest in any form of trisomy screening including cffDNA screening, first-trimester combined screening, or both. Again, greater educational attainment (OR=1.137, p<0.001), higher household income (OR=1.179, p<0.001), and insurance coverage (OR=1.477, p<0.001) positively predicted interest in prenatal screening. Respondents identifying as American Indian or Alaskan Native (OR=0.470, p=0.003) or Evangelical Protestant (OR=0.480, p<0.001) expressed less interest in screening, while those who identified as Jewish (OR=3.260, p<0.001) or as unaffiliated with a religion (OR=1.263, p=0.017) were more likely to express an interest in screening. Reported level of religiosity corresponded to lower interest in prenatal screening (OR=0.793, p<0.001). Personal experience with physical disability (OR=1.274, p=0.006) and doctor-ordered (OR=1.932, p<0.001) or purchased (OR=2.031, p<0.001) genetic tests positively predicted interest in prenatal screening. Finally, respondents who would contemplate abortion following detection of fetal trisomy were significantly more likely to indicate interest in screening (OR=8.270, p<0.001).
Table IV.
Predictors for interest in any prenatal screening for trisomy (N=3164)
| Demographic or experiential variable | Odds ratio | Wald χ2 statistic | p-value* |
|---|---|---|---|
| Gender | N.S. | ||
| Age | N.S. | ||
| Ethnicity | |||
| Hispanic or Latino | N.S. | ||
| Race | |||
| American Indian or Alaska Native | 0.470 | 8.836 | 0.003 |
| Asian | N.S. | ||
| Black or African-American | N.S. | ||
| Native Hawaiian or Pacific Islander | N.S. | ||
| White | N.S. | ||
| Educational attainment | 1.137 | 17.847 | <0.001† |
| Household income | 1.179 | 29.422 | <0.001 |
| Health insurance status | 1.477 | 13.309 | <0.001† |
| Religion | |||
| Catholic | N.S. | ||
| Evangelical Protestant | 0.480 | 35.527 | <0.001 |
| Other Protestant | N.S. | ||
| Mormon | N.S. | ||
| Jewish | 3.260 | 18.090 | <0.001 |
| Buddhist | N.S. | ||
| Muslim | N.S. | ||
| Unaffiliated | 1.263 | 5.724 | 0.017 |
| Religiosity | 0.793 | 30.812 | <0.001† |
| Experience as a parent | N.S. | ||
| Experience with physical disability | 1.274 | 7.445 | 0.006† |
| Experience with mental illness or disability | N.S. | ||
| Experience with doctor-ordered genetic test | 1.932 | 17.143 | <0.001† |
| Experience with purchased genetic test | 2.031 | 13.498 | <0.001† |
| Consideration of pregnancy termination | 8.270 | 432.907 | <0.001 |
N.S.=not significant. All p-values are reported using logistic regressional analysis adjusting for whether respondents were queried regarding trisomy 13 and 18 or trisomy 21.
This predictive variable does not remain significant in a multivariate logistic regression of all individually significant predictors of interest.
Following a multivariate regression analysis of these twelve predictors, six variables remained significantly predictive: income (OR=1.091, p=0.044); self-identification as American Indian or Alaskan Native (OR=0.409, p=0.009), Evangelical Protestant (OR=0.606, p=0.001), or Jewish (OR=2.304, p=0.029); and willingness to consider termination of pregnancy (OR=8.213, p<0.001). Lack of religious affiliation remained significant but with reversed directionality: respondents who reported a lack of religious affiliation were less likely to articulate interest in prenatal screening in this model (OR=0.747, p=0.047). No other variables were predictive.
Demographic and experiential predictors of consideration of termination of pregnancy
We used similar logistic regression models, standardizing for the two versions of the survey, to determine which demographic or experiential variables were predictive of respondents’ willingness to consider termination of pregnancy following prenatal detection of trisomy 13 or 18 and trisomy 21.
Table V illustrates the characteristics that were significantly predictive of consideration of termination following prenatal trisomy detection. Respondents who were older (OR=1.079, p=0.001), more educated (OR=1.136, p<0.001), or had higher household incomes (OR=1.181, p<0.001) were more likely to contemplate termination of pregnancy under these circumstances. While respondents identifying as Asian were more likely to indicate a willingness to consider abortion after prenatal detection of trisomy (OR=1.854, p<0.001), self-identification as black or African-American corresponded with a lower likelihood of considering abortion (OR=0.685, p<0.001). Respondents identifying as Evangelical Protestant (OR=0.358, p<0.001) or Mormon (OR=0.502, p=0.009) were also less likely to find pregnancy termination following trisomy detection acceptable, whereas those who identified as Jewish (OR=2.510, p<0.001) or unaffiliated with a religious tradition (OR=2.381, p<0.001) were more likely to consider this option. Higher levels of religiosity (OR=0.553, p<0.001) and parenthood (OR=0.853, p=0.035) were negatively predictive of consideration of abortion. On the other hand, experience with genetic testing – both doctor-ordered (OR=1.498, p=0.002) and purchased (OR=1.916, p<0.001) – corresponded with increased likelihood of considering termination of pregnancy.
Table V.
Predictors for consideration of termination of pregnancy following trisomy detection (N=3164)
| Demographic or experiential variable | Odds ratio | Wald χ2 statistic | p-value* |
|---|---|---|---|
| Gender | N.S. | ||
| Age | 1.079 | 10.977 | 0.001 |
| Ethnicity | |||
| Hispanic or Latino | N.S. | ||
| Race | |||
| American Indian or Alaska Native | N.S. | ||
| Asian | 1.854 | 15.486 | <0.001 |
| Black or African-American | 0.685 | 7.768 | <0.001† |
| Native Hawaiian or Pacific Islander | N.S. | ||
| White | N.S. | ||
| Educational attainment | 1.136 | 20.482 | <0.001† |
| Household income | 1.181 | 34.760 | <0.001 |
| Health insurance status | N.S. | ||
| Religion | |||
| Catholic | N.S. | ||
| Evangelical Protestant | 0.358 | 54.586 | <0.001 |
| Other Protestant | N.S. | ||
| Mormon | 0.502 | 6.897 | 0.009† |
| Jewish | 2.510 | 20.089 | <0.001 |
| Buddhist | N.S. | ||
| Muslim | N.S. | ||
| Unaffiliated | 2.381 | 87.394 | <0.001 |
| Religiosity | 0.553 | 213.935 | <0.001 |
| Experience as a parent | 0.853 | 4.450 | 0.035 |
| Experience with physical disability | N.S. | ||
| Experience with mental illness or disability | N.S. | ||
| Experience with doctor-ordered genetic test | 1.498 | 9.806 | 0.002 |
| Experience with purchased genetic test | 1.916 | 17.225 | <0.001 |
N.S.=not significant. All p-values are reported using logistic regressional analysis adjusting for whether respondents were queried regarding trisomy 13 and 18 or trisomy 21.
This predictive variable does not remain significant in a multivariate logistic regression of all individually significant predictors of consideration of termination.
Logistic regression analysis of these thirteen predictive characteristics demonstrated that older age (OR=1.222, p<0.001), higher household income (OR=1.148, p<0.001), and identification as Asian (OR=1.763, p=0.004), Evangelical Protestant (OR=0.490, p<0.001), Jewish (OR=1.673, p=0.035), or religiously unaffiliated (OR=1.297, p=0.033) remained significantly predictive. Religiosity (OR=0.554, p<0.001), parenthood (OR=0.656, p<0.001), and experience with either doctor-ordered (OR=1.628, p=0.006) or purchased (OR=1.777, p=0.005) genetic tests additionally continued to be significant in this multivariate analysis. The other adjusted variables were no longer significantly predictive.
Discussion
Expected interest in ffDNA screening and consideration of termination of pregnancy
In this study, we provide evidence of attitudes among members of society who are not necessarily women of reproductive age but still influence prenatal decision-making via complex interpersonal, social, cultural, and political relationships. Overall, our results illustrate a substantial interest in cffDNA screening for trisomy 13, 18, and 21 among the general public of the United States, consistent with the growing body of literature in this realm (Kelly & Farrimond, 2012; Kooij, Tymstra, & Berg, 2009; Sayres et al., 2011; Tischler et al., 2011; Yotsumoto et al., 2012; Zamerowski et al., 2001). While cffDNA screening for trisomy is not currently standard of care, its role in supplementing (rather than supplanting) existing prenatal screening mechanisms in high-risk populations is supported by at least four professional societies (P. Benn et al., 2011; “Committee opinion number 545: Noninvasive prenatal testing for fetal aneuploidy,” 2012; Devers et al., 2012). A majority of respondents who reported interest in some form of screening expressed a preference for cffDNA screening as a replacement for first-trimester combined screening, with a fraction of individuals indicating that they would be interested in both screening techniques. These results are consistent with a recent qualitative study of early adopters of cffDNA screening, in which women reported a belief that cffDNA screening provided a better alternative to conventional means of first- and second-trimester screening, which were deemed ‘unnecessary,’ with highly variable sensitivity and specificity rates (Yi, Hallowell, Griffiths, & Yeung Leung, 2013). In fact, one study showed that, of cffDNA screens for trisomy 21 performed in the first year following introduction, 14% were performed for women either as a primary screen or following a negative first-trimester screen. These data lend further credence to our finding that many individuals may make use of cffDNA screening in a manner at odds with current professional recommendations by foregoing recommended first-or second-trimester screens or obtaining cffDNA screening even in the event of a negative result from these conventional screening techniques (Poon et al., 2013). Thoughtful and thorough genetic counseling represents one means of ensuring that pregnant women receive prenatal screening that aligns with their values and professional practices.
Initial studies of uptake have demonstrated that, when offered as a second-tier screening test following a positive first- or second-trimester screening result, 39% of women elected to undergo cffDNA screening for trisomy 21 (Chetty, Garabedian, & Norton, 2013). While not directly comparable to our results, as we asked about cffDNA and first-trimester combined screening as separate options without a pre-determined sequence, the figure that we obtained −47% - highlights significant interest in cffDNA technology for trisomy detection. However, almost one-third of individuals were not interested in either cffDNA or first-trimester combined screening, which is consistent with previously reported levels of refusal of prenatal testing (Palomaki et al., 1997). Interest in cffDNA screening was significantly stronger for the detection of trisomy 13 and 18, most likely due to the increased severity of symptoms of these conditions over trisomy 21. Perhaps surprisingly, however, overall interest in receiving some form of screening did not vary with the targeted trisomy, suggesting that there exists a cohort among which prenatal information is not valued.
Willingness to consider abortion and several socioeconomic variables, including income, educational attainment, and health insurance status, robustly predicted the reported interest in prenatal screening (Dormandy, Michie, Hooper, & Marteau, 2005). These findings hold true with respect to interest in cffDNA screening specifically, which is consistent with a previous pilot study of expected uptake among pregnant women (Tischler et al., 2011). We also found that individuals identifying with certain races or religions were more or less likely to express a desire for prenatal screening; these results may be explained by the unique history and positioning of different racial or religious communities within the biomedical establishment, in addition to specific sociocultural and religious stances towards the moral status of abortion (Rapp, 1998). For example, Jewish individuals may be more likely to accept prenatal genetic testing because of their increased familiarity with preconception testing for carrier status of the gene for Tay Sachs disease (Kaback, 2000).
Interestingly, the findings that experience with genetic testing is positively associated with interest in screening and religiosity is negatively associated with interest run counter to the findings of a smaller previous study of pregnant women in which experience of genetic testing and self-reported levels of religiosity were not significant predictors of expressed interest in non-invasive prenatal screening (Tischler et al., 2011). It is, however, not surprising that individuals demonstrating prior acceptance of genetic testing - particularly when ordered by a physician - may be more comfortable receiving further genetic information in the context of pregnancy, either because they believe in the intrinsic value of information or they are more comfortable following doctor recommendations (Press & Browner, 1997). Additionally, stronger adherents to religions that forbid the termination of a pregnancy may be less likely accept information about a fetus if they feel that the knowledge is unlikely to change their prenatal decision-making and will only produce anxiety (Markens, Browner, & Press, 1999).
Along these lines, approximately half of respondents indicated a willingness to consider termination of a pregnancy following prenatal detection of trisomy 13 or 18 and trisomy 21. Of note, there is a significant increase in the percentage of respondents with an interest in any form of prenatal screening for trisomy 13 and 18 or trisomy 21 (69% and 71%, respectively) over the percentage who would consider termination (52% and 44%, respectively). This finding provides support for the presence of factors other than termination of pregnancy in motivation for receiving prenatal testing, such as reassurance or preparation for an affected child (Garcia, Timmermans, & van Leeuwen, 2008a; Parens & Asch, 2000; Suter, 2002). The rate of consideration of pregnancy termination is greater in the context of trisomy 13 and 18, which have higher levels of intrauterine lethality and infant mortality than trisomy 21 (Rasmussen, Wong, Yang, May, & Friedman, 2003). Overall, our figures are significantly lower than actual rates of termination reported in the literature, suggesting that speculation on whether termination of pregnancy would be permissible under hypothetical circumstances does not align with how prospective parents confronting such decisions actually act (Drugan et al., 1990). Moreover, our study is taken from a sample of the general public in the United States, and this population likely differs from the samples of other studies, which have mostly been limited to recently pregnant women who are receiving prenatal care. Thus, our study may better reflect the attitudes of individuals who are not able to or who would choose not to receive prenatal care.
Our findings that older maternal age, greater socioeconomic status, identification with particular races and religions, decreased strength of religious beliefs, and prior experience with genetic testing correspond to willingness to contemplate abortion following prenatal trisomy detection concord with previous research (Choi, Van Riper, & Thoyre, 2012; Kuppermann et al., 2011; Natoli, Ackerman, McDermott, & Edwards, 2012). Our data add to existing mixed evidence regarding the willingness of individuals who already have children to consider termination of pregnancy, by demonstrating that parents may be less likely to contemplate this option (Kramer et al., 1998). On one hand, individuals with existing children may not be as inclined to have more children, particularly children requiring elevated attention and resources. However, parents may also believe that love for one’s children is unconditional and recognize that all children, and not just those with trisomy, will place significant demands on their lives. Regardless, provision of unbiased informational materials and expanded access to pre- and post-natal care may allow prospective parents of all classes to make prenatal decisions that best align with their personal values.
Study limitations
To determine whether our sample was representative of the general United States public, we compared the demographic data of respondents to those available from the United States Census of 2010 and the Pew Religious Landscape Survey of 2008 using chi-square goodness-of-fit tests with α=0.05. We appear to have under-sampled males (χ2(1, N=3164)=15.590, p<0.001), individuals of Hispanic or Latino (χ2(1, N=2962)=173.432, p<0.001) and Black or African-American (χ2(1, N=3164)=74.912, p<0.001) identities, and those affiliated with Evangelical (χ2(1, N=3157)=469.142, p<0.001) or other (χ2(1, N=3157)=147.939, p<0.001) denominations of Protestantism. Additionally, distributions of age (χ2(5, N=3164)=166.340, p<0.001), household income (χ2(4, N=3164)=140.058, p<0.001), and educational attainment (χ2(4, N=3164)=469.694, p<0.001) varied significantly from findings of the Census. Additionally, a web-based survey available only in English will not be accessed by individuals who do not have access to the internet or who cannot read and write in English. Moreover, it is impossible in this format to assess whether there existed biases among responders or non-responders. However, given the significant proportion of respondents choosing to receive no prenatal screening or who are opposed to termination following a diagnosis of trisomy despite our sample’s skew towards individuals historically more likely to do so, it is possible that we have nonetheless underrepresented these values while taking account of a wide range of public attitudes.
Our findings are contingent on the descriptions of trisomy 13, 18, and 21 and the features and costs of different prenatal screening options that were provided. This fact highlights the necessity of providing potential parents with genetic counseling educational materials that address the concerns and questions surrounding screening and post-screening decision-making. It is highly likely that, over time, as the performance and cost of cffDNA screening improve, insurers will begin to cover screening for a greater number of indications, physicians will recommend screening under more circumstances, and the public will become more familiar with the availability of this technology. The realization of these prospects may lead to increased acceptance of cffDNA testing for trisomy 13, 18, and 21 beyond what is suggested in this study.
Practice implications
This is the first large study of perspectives of the United States public on cffDNA screening for trisomy 13, 18, and 21. There appears to be significant interest in this method of screening as a supplement or replacement for existing prenatal screening mechanisms, increasing the likelihood that uptake will continue to increase rapidly as the technology become more widely publicized, more widely available, less costly, and more widely covered by insurers. However, this does not negate the urgent need for healthcare providers, professional organizations, regulators, third-party payers, and other policymakers to consider the various ethical aspects of cffDNA screening, such as assurance of analytic and clinical utility, proper informed consent procedures, availability of nondirective genetic counseling, access by broad patient populations, and non-discrimination and continued support and resources for individuals living with disabilities (P. A. Benn & Chapman, 2010; Kent, 2008; Lewis, Hill, Skirton, & Chitty, 2012). Additionally, stakeholders involved in implementing cffDNA screening must be respectful of individuals who choose not to receive screening or who decide against termination of pregnancy based on diagnostic results and the social and cultural structures that may influence prenatal decisions (Lewis, Silcock, & Chitty, 2013). Test developers and providers should employ measures that encourage pregnant women and their families to make informed decisions about cffDNA screening grounded in their personal values, such as by developing and distributing unbiased educational materials and supporting access to screening by medically underserved populations. Pregnant women should be made aware of the availability and utility of diagnostic testing, including amniocentesis and chorionic villus sampling, that may be recommended in the case of a positive result of any form of prenatal screening. As our ability to non-invasively detect other chromosomal anomalies, copy number variants, and inherited or de novo polymorphisms in a fetus continues to improve, we must incorporate attitudes of the general public into the translational process early and often to ensure that this technology aligns with the priorities of its diverse stakeholders (Kitzman et al., 2012).
Acknowledgments
All authors are supported by NIH grant P50-HG003389 (Center for Integrating Ethics and Genetic Research). Dr. Cho is additionally supported by NIH grant 1-U54-RR024374-01A1 (Stanford Center for Clinical and Translational Education and Research). We thank the Division of Biostatistics within the Stanford University School of Medicine Department of Health Research and Policy for their guidance in analyzing this data.
Footnotes
Disclosure of interest
None of the authors has a conflict of interest of a financial or other nature. Authors have full control of all primary data and agree to allow the journal to review our data upon request.
References
- Allyse M, Sayres LC, Goodspeed TA, Cho MK. Attitudes towards non-invasive prenatal testing for aneuploidy among United States adults of reproductive age. 2013. Submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benn PA, Chapman AR. Practical and ethical considerations of noninvasive prenatal diagnosis. JAMA. 2009;301(20):2154–2156. doi: 10.1001/jama.2009.707. [DOI] [PubMed] [Google Scholar]
- Benn PA, Chapman AR. Ethical challenges in providing noninvasive prenatal diagnosis. Current opinion in obstetrics & gynecology. 2010;22(2):128–134. doi: 10.1097/GCO.0b013e3283372352. [DOI] [PubMed] [Google Scholar]
- Benn P, Borrell A, Cuckle H, Dugoff L, Gross S, Johnson J, Yaron Y. Prenatal detection of Down syndrome using massively parallel sequencing (MPS): a rapid response statement from a committee on behalf of the Board of the International Society for Prenatal Diagnosis. 2011 doi: 10.1002/pd.2919. from http://www.ispdhome.org/public/news/2011/ISPD_RapidResponse_MPS_24Oct11.pdf. [DOI] [PubMed]
- Bianchi DW, Sehnert AJ, Rava RP. Genome-wide fetal aneuploidy detection by maternal plasma DNA sequencing. Obstetrics and gynecology. 2012;119(6):1270–1271. doi: 10.1097/AOG.0b013e318258c419. [DOI] [PubMed] [Google Scholar]
- Case AP, Ramadhani TA, Canfield MA, Wicklund CA. Awareness and attitudes regarding prenatal testing among Texas women of childbearing age. Journal of genetic counseling. 2007;16(5):655–661. doi: 10.1007/s10897-007-9103-6. [DOI] [PubMed] [Google Scholar]
- Chetty S, Garabedian MJ, Norton ME. Uptake of noninvasive prenatal testing (NIPT) in women following positive aneuploidy screening. Prenat Diagn. 2013;33(6):542–546. doi: 10.1002/pd.4125. [DOI] [PubMed] [Google Scholar]
- Choi H, Van Riper M, Thoyre S. Decision making following a prenatal diagnosis of Down syndrome: an integrative review. Journal of midwifery & women’s health. 2012;57(2):156–164. doi: 10.1111/j.1542-2011.2011.00109.x. [DOI] [PubMed] [Google Scholar]
- Committee opinion number 545. Noninvasive prenatal testing for fetal aneuploidy. Obstetrics and gynecology. 2012;120(6):1532–1534. doi: 10.1097/01.AOG.0000423819.85283.f4. [DOI] [PubMed] [Google Scholar]
- Devers PL, Cronister A, Ormond KE, Facio F, Brasington CK, Flodman P. Noninvasive prenatal testing/noninvasive prenatal diagnosis: the position of the National Society of Genetic Counselors. 2012 doi: 10.1007/s10897-012-9564-0. from http://www.nsgc.org/Portals/0/Advocacy/NSGC%20Noninvasive%20Prenatal%20Testing%204-17-2012.pdf. [DOI] [PubMed]
- Dormandy E, Michie S, Hooper R, Marteau TM. Low uptake of prenatal screening for Down syndrome in minority ethnic groups and socially deprived groups: a reflection of women’s attitudes or a failure to facilitate informed choices? International journal of epidemiology. 2005;34(2):346–352. doi: 10.1093/ije/dyi021. [DOI] [PubMed] [Google Scholar]
- Drugan A, Greb A, Johnson MP, Krivchenia EL, Uhlmann WR, Moghissi KS, Evans MI. Determinants of parental decisions to abort for chromosome abnormalities. Prenatal diagnosis. 1990;10(8):483–490. doi: 10.1002/pd.1970100802. [DOI] [PubMed] [Google Scholar]
- Garcia E, Timmermans DR, van Leeuwen E. The impact of ethical beliefs on decisions about prenatal screening tests: searching for justification. Soc Sci Med. 2008a;66(3):753–764. doi: 10.1016/j.socscimed.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Garcia E, Timmermans DR, van Leeuwen E. Rethinking autonomy in the context of prenatal screening decision-making. Prenat Diagn. 2008b;28(2):115–120. doi: 10.1002/pd.1920. [DOI] [PubMed] [Google Scholar]
- Greely HT. Get ready for the flood of fetal gene screening. Nature. 2011;469(7330):289–291. doi: 10.1038/469289a. [DOI] [PubMed] [Google Scholar]
- Heger M. Sequenom sees steady growth of MaterniT21 test despite competition. GenomeWeb. 2012 Retrieved from http://www.genomeweb.com/sequencing/sequenom-sees-steady-growth-maternit21-test-despite-competition.
- Heger M. Facing increased competition, Sequenom sees continued growth of MaterniT21 test in Q4 2012. GenomeWeb. 2013 Retrieved from http://www.genomeweb.com/sequencing/facing-increased-competition-sequenom-sees-continued-growth-maternit21-test-q4-2.
- Kaback MM. Population-based genetic screening for reproductive counseling: the Tay-Sachs disease model. European journal of pediatrics. 2000;159(Suppl 3):S192–195. doi: 10.1007/pl00014401. [DOI] [PubMed] [Google Scholar]
- Kelly SE, Farrimond HR. Non-invasive prenatal genetic testing: a study of public attitudes. Public Health Genomics. 2012;15(2):73–81. doi: 10.1159/000331254. [DOI] [PubMed] [Google Scholar]
- Kent A. Non-invasive prenatal diagnosis: public and patient perceptions. Seminars in fetal & neonatal medicine. 2008;13(2):109–112. doi: 10.1016/j.siny.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Kitzman JO, Snyder MW, Ventura M, Lewis AP, Qiu R, Simmons LE, Shendure J. Noninvasive whole-genome sequencing of a human fetus. Science translational medicine. 2012;4(137):137ra176. doi: 10.1126/scitranslmed.3004323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooij L, Tymstra T, Berg P. The attitude of women toward current and future possibilities of diagnostic testing in maternal blood using fetal DNA. Prenatal diagnosis. 2009;29(2):164–168. doi: 10.1002/pd.2205. [DOI] [PubMed] [Google Scholar]
- Kramer RL, Jarve RK, Yaron Y, Johnson MP, Lampinen J, Kasperski SB, Evans MI. Determinants of parental decisions after the prenatal diagnosis of Down syndrome. Am J Med Genet. 1998;79(3):172–174. doi: 10.1002/(sici)1096-8628(19980923)79:3<172::aid-ajmg4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Kuppermann M, Gates E, Washington AE. Racial-ethnic differences in prenatal diagnostic test use and outcomes: preferences, socioeconomics, or patient knowledge? Obstetrics and gynecology. 1996;87(5 Pt 1):675–682. doi: 10.1016/0029-7844(96)00017-8. [DOI] [PubMed] [Google Scholar]
- Kuppermann M, Nakagawa S, Cohen SR, Dominguez-Pareto I, Shaffer BL, Holloway SD. Attitudes toward prenatal testing and pregnancy termination among a diverse population of parents of children with intellectual disabilities. Prenatal diagnosis. 2011;31(13):1251–1258. doi: 10.1002/pd.2880. [DOI] [PubMed] [Google Scholar]
- Lewis C, Hill M, Skirton H, Chitty LS. Fetal sex determination using cell-free fetal DNA: service users’ experiences of and preferences for service delivery. Prenatal diagnosis. 2012:1–7. doi: 10.1002/pd.3893. [DOI] [PubMed] [Google Scholar]
- Lewis C, Silcock C, Chitty LS. Non-invasive prenatal testing for Down’s syndrome: pregnant women’s views and likely uptake. Public Health Genomics. 2013;16(5):223–232. doi: 10.1159/000353523. [DOI] [PubMed] [Google Scholar]
- Lo YM, Chiu RW. Genomic analysis of fetal nucleic acids in maternal blood. Annu Rev Genomics Hum Genet. 2012;13:285–306. doi: 10.1146/annurev-genom-090711-163806. [DOI] [PubMed] [Google Scholar]
- Malone FD, Canick JA, Ball RH, Nyberg DA, Comstock CH, Bukowski R Second-Trimester Evaluation of Risk Research Consortium. First-trimester or second-trimester screening, or both, for Down’s syndrome. N Engl J Med. 2005;353(19):2001–2011. doi: 10.1056/NEJMoa043693. [DOI] [PubMed] [Google Scholar]
- Markens S, Browner CH, Press N. ‘Because of the risks’: how US pregnant women account for refusing prenatal screening. Social science & medicine. 1999;49(3):359–369. doi: 10.1016/s0277-9536(99)00097-0. [DOI] [PubMed] [Google Scholar]
- Natoli JL, Ackerman DL, McDermott S, Edwards JG. Prenatal diagnosis of Down syndrome: a systematic review of termination rates (1995–2011) Prenatal diagnosis. 2012;32(2):142–153. doi: 10.1002/pd.2910. [DOI] [PubMed] [Google Scholar]
- Olney RS, Moore CA, Khoury MJ, Erickson JD, Edmonds LD, Botto LD, Atrash HK. Chorionic villus sampling and amniocentesis: recommendations for prenatal counseling. Morbidity and Mortality Weekly Report Recommendations and Reports. 1995;44(RR-9):1–12. [PubMed] [Google Scholar]
- Palomaki GE, Knight GJ, McCarthy JE, Haddow JE, donhowe JM. Maternal serum screening for Down syndrome in the United States: a 1995 survey. American journal of obstetrics and gynecology. 1997;176(5):1046–1051. doi: 10.1016/s0002-9378(97)70400-9. [DOI] [PubMed] [Google Scholar]
- Parens Erik, Asch Adrienne. Prenatal testing and disability rights. Washington, D.C: Georgetown University Press; 2000. [Google Scholar]
- Peters D, Chu T, Yatsenko SA, Hendrix N, Hogge WA, Surti U, Rajkovic A. Noninvasive prenatal diagnosis of a fetal microdeletion syndrome. The New England journal of medicine. 2011;365(19):1847–1848. doi: 10.1056/NEJMc1106975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon C, Ng W, Kou K, Lau B, Ma T, Leung K. Impact of introduction of non-invasive prenatal testing in private on the uptake of prenatal testing for Down syndrome in a public hospital. Ultrasound in Obstetrics & Gynecology. 2013;42(s1):130. [Google Scholar]
- Press N, Browner CH. Why women say yes to prenatal diagnosis. Social science & medicine. 1997;45(7):979–989. doi: 10.1016/s0277-9536(97)00011-7. [DOI] [PubMed] [Google Scholar]
- Rapp R. Refusing prenatal diagnosis: the meanings of bioscience in a multicultural world. Science, technology & human values. 1998;23(1):45–70. doi: 10.1177/016224399802300103. [DOI] [PubMed] [Google Scholar]
- Rasmussen SA, Wong LY, Yang Q, May KM, Friedman JM. Population-based analyses of mortality in trisomy 13 and trisomy 18. Pediatrics. 2003;111(4 Pt 1):777–784. doi: 10.1542/peds.111.4.777. [DOI] [PubMed] [Google Scholar]
- Sayres LC, Allyse M, Norton ME, Cho MK. Cell-free fetal DNA testing: a pilot study of obstetric healthcare provider attitudes toward clinical implementation. Prenatal diagnosis. 2011 doi: 10.1002/pd.2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter SM. The routinization of prenatal testing. Am J Law Med. 2002;28(2–3):233–270. [PubMed] [Google Scholar]
- Tischler R, Hudgins L, Blumenfeld YJ, Greely HT, Ormond KE. Noninvasive prenatal diagnosis: pregnant women’s interest and expected uptake. Prenatal diagnosis. 2011;31(13):1292–1299. doi: 10.1002/pd.2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi H, Hallowell N, Griffiths S, Yeung Leung T. Motivations for undertaking DNA sequencing-based non-invasive prenatal testing for fetal aneuploidy: a qualitative study with early adopter patients in Hong Kong. PLoS One. 2013;8(11):e81794. doi: 10.1371/journal.pone.0081794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yotsumoto J, Sekizawa A, Koide K, Purwosunu Y, Ichizuka K, Matsuoka R, Okai T. Attitudes toward non-invasive prenatal diagnosis among pregnant women and health professionals in Japan. Prenatal diagnosis. 2012:1–6. doi: 10.1002/pd.3886. [DOI] [PubMed] [Google Scholar]
- Zamerowski ST, Lumley MA, Arreola RA, Dukes K, Sullivan L. Favorable attitudes toward testing for chromosomal abnormalities via analysis of fetal cells in maternal blood. Genetics in medicine : official journal of the American College of Medical Genetics. 2001;3(4):301–309. doi: 10.1097/00125817-200107000-00006. [DOI] [PubMed] [Google Scholar]