Abstract
Private wells in the United States are unregulated for drinking water standards and are the homeowner’s responsibility to test and treat. Testing for water quality parameters such as arsenic (As) is a crucial first step for homeowners to take protective actions.
This study seeks to identify key behavioral factors influencing homeowners’ decisions to take action after receiving well As test results. A January 2013 survey of central Maine households (n=386, 73% response) who were notified 3–7 years earlier that their well water contained As above 10 μg/L found that 43% of households report installing As treatment systems. Another 30% report taking other mitigation actions such as drinking bottled water because of the As, but the remaining 27% of households did not act. Well water As level appears to be a motivation for mitigation: 31% of households with well water level between 10 and 50 μg/L did not act, compared to 13% of households with well water > 50 μg/L. Belief that the untreated water is not safe to drink (risk) and that reducing drinking water As would increase home value (instrumental attitude) were identified as significant predictors of mitigating As. Mitigating As exposure is associated with less worry about the As level (affective attitude), possibly because those acting to reduce exposure feel less worried about As. Use of a treatment system specifically was significantly predicted by confidence that one can maintain a treatment system, even if there are additional costs (self-efficacy).
An assessment of As treatment systems used by 68 of these households with well water As >10 μg/L followed up with in August-November 2013 found that 15% of treatment units failed to produce water below As 10 μg/L, suggesting there are continued risks for exposure even after the decision is made to treat.
Keywords: water treatment, arsenic, health behavior, drinking water, private well, Maine
1. Introduction
Arsenic (As) is known for its human toxicity and occurs naturally in the earth’s crust, ranking as the 19th most abundant trace element (Rudnick and Gao, 2003). In 2001 the U.S. Environmental Protection Agency (USEPA) adopted a new standard for maximum level of contaminant (MCL) for As in drinking water of 10 micrograms per liter (μg/L), replacing the old MCL of 50 μg/L in the Safe Drinking Water Act of 1974. The change was meant to address the long-term, chronic effects of exposure to low concentrations of As, which has been linked to a number of health effects including cancers of the skin, bladder, lung, and kidney, as well as cardiovascular, pulmonary, and neurological effects (USEPA, 2001). The rule went into effect in February 2002 and public water systems were given until January 2006 to comply (USEPA, 2001). As of 2011, a decade after adoption of the new standard, the USEPA estimates that nearly 800 water systems serving 1.8 million people were still not in compliance (USEPA, 2013), most of which are small rural systems serving less than 3,300 people that cannot find the funds to meet the As standard while keeping water affordable.
The failure of these small public systems to achieve compliance with the As rule is concerning; equally troubling is that private water supply from domestic wells falls out of the purview of these regulations. The Safe Drinking Water Act does not regulate private wells serving fewer than 25 individuals. It is therefore the responsibility of homeowners to have the water from their private domestic wells tested and treated if necessary. About 15 percent of the U.S. population, over 43 million people, relies on private wells for their drinking water (Huston et al., 2004), and ensuring the safety of the water from these wells is primarily the responsibility of the well owner. In New England especially, high concentrations of groundwater As has led to often unsafe levels in private bedrock wells (Ayotte et al., 2003). Roughly half of the population of Maine obtains their drinking water from a private source, of which more than 75% are drilled bedrock wells (U.S. Census, 1990). Analysis of lab test results of 11,111 private wells has identified several areas in Maine with high As occurrence (Nielsen et al., 2010). Blood As has been detected in 99% of samples from children aged 1–6 tested by the Maine State laboratory, with significantly higher blood As levels in regions with a higher known prevalence of private wells with As >5 μg/L (Rice et al, 2010). In a recent Columbia University Superfund Research Program (SRP) study on schoolchildren in 3 districts around Augusta, Maine, children consuming water >5 μg/L As showed significant reductions in full scale IQ and Index scores (Working Memory, Perceptual Reasoning, and Verbal Comprehension) compared to those with well water As levels < 5 μg/L, even after adjusting for the home environment, number of children in the home, and maternal intelligence (Wasserman et al., in revision). Cohort studies have found associations between chronic As exposure in utero and in early childhood and significantly higher risks of impaired lung function, renal cancer and death from lung cancer, lung disease and acute myocardial infarction later in life (Dauphiné et al., 2011; Yuan et al., 2010; Yuan et al., 2007; Smith et al., 2006).
Testing for water quality parameters such as As is a crucial first step for homeowners to take protective actions. Without a well test and information on exposure risk, it is unlikely that homeowners will know enough to take protective actions, whether they are risk averse or not. Studies on people’s perceptions of nitrate health risks before and after a well testing program have demonstrated that individuals do use water test results and associated information to systematically update their exposure and health risk perceptions (Poe et al., 1998). But do these updated perceptions translate into taking the protective actions necessary to reduce risk? Studies on safe water consumption and other health behaviors have shown that risk perception is often a weak predictor of health behavior change (Huber et al., 2012; Tobias and Berg, 2011; Radtke et al., 2011). When faced with uncertainty over choices, additional information should improve decision making; yet providing risk information alone (e.g. providing well test results) does not always guarantee health behavior change (e.g. As mitigation). A review of six international studies (four on As contamination) in which populations received test results that their water supply posed a known health risk concluded that despite some encouraging well switching results, the evidence for providing drinking water contamination data to consumers to improve water management behavior is still inconclusive (Lucas et al., 2011).
This reluctance to act on test results has been observed in other regions of the US. About half of surveyed private well users in Wisconsin with As levels exceeding the MCL were not taking any action to reduce As exposure (Severtson et al., 2006). Severtson et al. applied a health behavior theory on psychological processing to understand how people responded to information about As-contaminated well water and found that concrete well testing information may be incongruent with optimistic beliefs about drinking water quality which can have more psychological influence on the protective behavior. In another As hotspot in Churchill County, Nevada, survey results revealed significant proportions of households (53.3%) with private wells are consuming drinking water with As levels dangerous to health (mean 63.5 μg/L) despite high awareness of As risks in the area (Shaw et al., 2005). This study found that levels of concern were insignificant to the decision to treat water but that treatment cost significantly and negatively influenced the decision. Unexpectedly so did higher education which was found to be associated with lower perceptions of risk. Many households in this study (20.2%) also reported using a treatment method that is not effective at lowering As levels, demonstrating that self-reported treatment behavior may not be accurate. During an As information campaign in Araihazar, Bangladesh (mean As level 108 μg/L), 60% of households who learned that the well they used was unsafe (As >50 μg/L) changed to using a different well within a year (Madajewicz et al., 2007). Those with only primary education and those in the lowest quartile of asset ownership seemed to be more disadvantaged in terms of access to safe water and so rates of well switching were much lower. These studies all show that information can motivate protective behavior among a proportion of households, but households react differently to risk information for various reasons and there are still barriers to eliminating exposure for the entire at risk population. However, even with testing information, the barriers for homeowners acting on it to reduce health risks are not well understood.
For the motivated homeowners who have taken protective action to treat their well water for As, very concerning is the possibility that the treatment systems may be failing at their purpose and still leaving household members exposed to As. These households have had to face an array of treatment options offered by various local private companies in an unregulated market. The responsibility for maintenance and monitoring the effectiveness of treatment system again falls on the homeowner. Only a limited number of studies have evaluated the performance of these systems under real world conditions. Analysis of tap water samples in Churchill County, Nevada found that half of the 116 households that said they consume and treat their water still had tap water As concentrations above 12 μg/L (Shaw et al., 2005). Concentrations of As in treated water exceeded 10 μg/L in 18 of 59 households of Lahontan Valley, Nevada with reverse-osmosis (RO) systems installed to remove As (Walker et al., 2008). The main factors leading to As in treated water above MCL included some well As concentrations high enough that final As levels exceeded the MCL even though RO treatment removed more than 95% of the As, and trivalent As (III) as the dominant As species in 15% of the wells which significantly reduced treatment efficiency. Although the As levels have been lowered, the large number of systems still not in compliance with the MCL of As suggests that the As hazards may persist after the installation of a commercial treatment system.
In this study, we seek to identify key behavioral factors influencing homeowners’ decision to take protective action (treat their water for As or drink bottled water) after well water As testing results are made available to them. A RANAS (Risk, Attitude, Norm, Ability, Self-regulation) model (Mosler, 2012) of integrated health and social psychology theories is utilized. The RANAS model is appropriate because it goes beyond risk information as a motivator for health behavior change and outlines the blocks of psychological factors that must be favorable for a behavior, such as water treatment, to take root. Further, it has been applied to understand preferences for and uptake of various As mitigation water options in rural Bangladesh (Inauen, Tobias, and Mosler, 2013). There, a structured household questionnaire was used to understand the influential RANAS factors behind mitigation behavior, finding that the strongest predictors of the use of neighboring As-safe tube wells were high commitment, stronger descriptive norms (perceptions of normal behavior), and higher self-efficacies. A cluster-randomized controlled trial demonstrated that interventions developed to target these identified factors could motivate as many as 48% more people to switch to As-safe wells compared to an intervention based on risk information alone (Inauen and Mosler, 2013). A survey was conducted between January and February 2013 to rural households in central Maine who had been notified that their well water contained As above the MCL of 10 μg/L in 2006, 2007, or 2010. By studying homeowners who are provided directly with water quality results, remaining barriers to As mitigation can be better identified. The beliefs and actions of homeowners taken in response to the water quality test results are reported first, followed by analysis of the behavioral factors which influence the mitigation of drinking water As among Maine homeowners, utilizing the RANAS model. Finally, concentrations of As in raw and treated domestic well water samples from 68 of these households using a variety of treatment systems to treat for As are reported, obtained using test kits during household visits conducted August to November of 2013 to investigate As-removal efficiencies in real world situations. This permits an assessment of exposure risks remaining after treatment is installed.
2. Methods
2.1. Household Survey
2.1.1. Household Sample
Between 2006 and 2011 the Columbia University Superfund Research Program (SRP) and the Maine Geological Survey (MGS) tested 1,428 domestic well water samples in 17 towns encompassing over 1500 km2 (Yang et al., 2009; Yang, 2010). Over 95% of these samples were collected from drilled wells, which are at higher risk for As (Ayotte et al., 2003). All participating households received a letter informing testing results of 40 water quality parameters including As that also contained an educational brochure (“Is Your Well Water Safe to Drink?” http://www.epa.gov/region1/eco/drinkwater/pdfs/ME-Private-Well-Testing-Brochure.pdf) provided by Maine CDC and other contact information for appropriate action. Only households with well water exceeding the MCL, (As >10 μg/L), were selected for this study (n=466). Of those, 237 were notified of their As testing results in 2006, 138 in 2007 and 91 in 2010. The selected households had all previously volunteered for the well testing program held in the 17 towns, and therefore are a convenience sample not meant to be necessarily representative of the area. At the time of the survey 80 of the mailing addresses were no longer valid and those surveys were undeliverable, resulting in a survey sample of 386 households.
2.1.2. Survey Instrument
Households were mailed an 8-page questionnaire (see Appendix) on their water treatment practices, preferences, and opinions, as well as basic demographic information, similar to the instrument utilized by our recent well testing survey (see this issue). In addition to focusing more on treatment actions taken in response to As specifically, this survey also included a section with questions designed to measure the same RANAS (Risk, Attitude, Norms, Ability, Self-regulation) factors that may influence behaviors, and in this case in regards to treatment behavior. The RANAS portion of the survey included a series of statements with which respondents indicated their agreement on a scale of 1 to 6 from strongly disagree to strongly agree. The survey instrument was pre-tested on 20 well owners in Maine prior to implementation.
2.1.3. Survey Implementation
Surveys were mailed in January 2013 to the selected 466 households from Augusta (n=31), Belgrade (n=31), Chelsea (n=15), China (n=17), Farmingdale (n=4), Hallowell (n=9), Litchfield (n=49), Manchester (n=98), Monmouth (n=17), Mount Vernon (n=12), Readfield (n=34), Sidney (n=46), Vassalboro (n=15), Waterville (n=3), West Gardiner (n=35), Windsor (n=8), and Winthrop (n=39); although 80 of the surveys were undeliverable by USPS. Households were mailed a survey with a cover letter and $2 cash incentive for participation in early Jan 2013, a thank you post card 2 weeks later and a follow-up reminder with a replacement survey in early Feb 2013. Surveys were mailed from and returned to the Maine Geological Survey. The study protocol and survey instruments were approved by the Institutional Review Board of Columbia University.
2.1.4. Data Analysis
The data analysis employed SPSS 21.0 statistical software. Spearman correlations were calculated between demographic and behavior variables and mitigation actions. Binary logistic regression analysis was employed to identify the most significant behavioral predictors.
2.2. Water Sample Collection and Analysis for Treatment Assessment
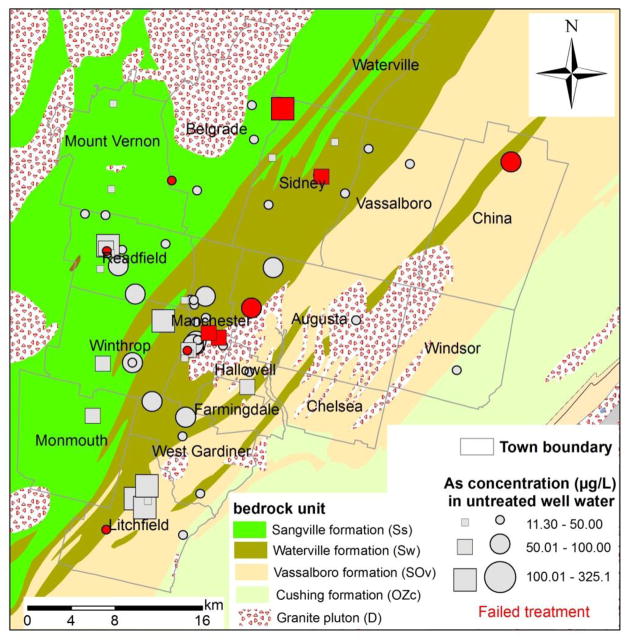
A total of 68 households with As >10 μg/L in their well water who reported in the survey that they are currently treating for As participated in a treatment system assessment conducted by the Maine Geological Survey (Figure 1). Households were identified through our mailed survey earlier that year and were selected based on their self-reported use of a treatment system for As, either at the point-of-entry (POE) or at the point-of-use (POU).
Figure 1.
68 households treating for As previously tested by ICP-MS in 2006–2010 and tested again by kit in 2013. Households tested by ICP-MS again in 2013 are marked with squares, red colored shapes (n=10) indicate treatment system installed at the household is failing to deliver drinking water <10 μg/L As.
Households were visited by staff members of MGS between August and November 2013. “Influent” well-water samples (pre-water-treatment system) were collected at the point-of-entry to the house, prior to the pressure tank and household water-treatment system(s), using the existing well-water pump. “Effluent” samples (post-water-treatment system) were collected at the kitchen faucet where POUs are located. Testing of As was performed on site in all 68 households using the Arsenic Econo-Quick test kit (Industrial Test Systems, Inc.). For quality assurance, aliquots of untreated and treated water samples were collected from 25 of the households for total (unfiltered) As. All water samples were acidified to 1% HNO3 (Optima Grade) and allowed for dissolution for a week before analysis by high resolution inductively coupled plasma-mass spectrometry (ICP-MS) following the EPA Method 200.8 by Columbia University. Repeated analyses (n=8) of the NIST standard solution 1640a with 8.075 μg/L of As and an internal artificial standard “LDEO” with 415.8 μg/L of As revealed an accuracy within 2% and a precision within 4%.
3. Results
3.1. Survey
3.1.1. Sampled and General Population Characteristics
The survey response rate among delivered surveys was 73.3%, of which 90.5% were suitable for analysis, i.e. report having a well and had a test; overall 66.3% of the 386 originally tested households with still valid mailing addresses were included in the final analysis. Of the returned surveys not included in the analysis, one household no longer had well water, 12 reported that they have never had a well As test, 12 reported they do not remember if they have, and 2 did not answer the test question. It is possible that these survey respondents were unaware that their household participated in the previous testing program or that the homeowners have changed since the previous study. Another 10 households responded to the survey but declined to participate. There were no significant differences in response rates between households by year of initial well test – 2006, 2007 or 2010. The demographic characteristics of respondents are included in Table 1. This survey sample is not randomly selected; households from the 17 project area towns had originally volunteered for Columbia University well testing and this self-selection bias is clear when comparing to the general population in this Maine area using 2010 U.S. Census data. Survey participants are slightly older, more likely to be male and homeowners, more educated, wealthier, and less likely to have children than the general population.
Table 1.
Demographic Characteristics of Well Owner Survey Respondents (n=256) and General Population in 17 towns of Kennebec County, Maine, in 2013 and 2010, respectively.
| Demographic Characteristic | Sample | Populationa |
|---|---|---|
| Median Age (years)b | 60 | 50 |
| Sex Ratio (M/F) | 55.4% / 44.6% | 48.5% / 51.5% |
| Homeownership (%Owners/%Renters) | 96.4% / 3.6%c | 83.1% / 15.9% |
| Median education | Bachelor’s degree | Associate’s degree |
| Median income | $60,000 – 79,000d | $42,108 |
| Households with children <18 Years Old | 15.6% | 30.8% |
US Census 2010, Augusta and Waterville were excluded from statistics because of high population and low domestic well water supply rates (17.6% and 2.6%, respectively)
Respondents were required to be at least 18 years old; median age reported is for population ≥18 years
Rental units are more prevalent within the bounds of public water supply systems than private well households
16% of respondents chose not to report income
3.1.2. Treatment Behaviors
Select descriptive statistics from the survey respondents are summarized in Table 2. Self-reported As level correlated with Columbia University measurements r=.664 (p<.001), with several households underestimating their results. Additionally a third of respondents did not remember their test results. About a quarter (23%) of participants reported that they consider As levels above the MCL of 10 μg/L safe. In total 42.6% of households report having installed a treatment system, either point of use (POU) or point of entry (POE), because of the As level in their well water. Another 30.5% report drinking bottled water or taking another mitigation action because of the As level, but the remaining 27% of households did not take an action to reduce their As exposure. A majority (70%) of respondents believed their well test report was “easy” or “very easy” to understand; although ease of understanding was not significantly associated with taking action in general to reduce exposure, understanding was significantly associated with installing a treatment system (rs=.187, p<.01) but negatively associated with switching to drinking bottled water (rs=−.173, p<.01).
Table 2.
Sample Descriptive Statistics for Key Variables (n=256 households with As >10 μg/L wells)
| Variables | Percentage | |
|---|---|---|
| What was the highest arsenic level measured for your well?a | <10 μg/L | 6.5% |
| 10–50 μg/L | 46.8% | |
| 51–100 μg/L | 9.7% | |
| >100 μg/L | 5.2% | |
| Don’t remember | 31.9% | |
|
| ||
| What is the highest arsenic level you consider safe? | <10 μg/L | 76.71% |
| 10–50 μg/L | 19.4% | |
| 51–100 μg/L | 3.9% | |
| >100 μg/L | 0% | |
|
| ||
| Did you take any actions because of the arsenic level in your well water? | Installed POE Treatment | 8.2% |
| Installed POU Treatment | 34.4% | |
| Switched to Bottled Water | 26.6% | |
| Other Mitigation Actionb | 3.9% | |
| No Action Taken | 27% | |
|
| ||
| If you did not take any arsenic-related action, why not?c | Treatment too Expensive | 19.9% |
| Not Concerned about As Level | 12.5% | |
| Didn’t Know What to Do | 3.5% | |
| Didn’t Know Who to Contact | 2.3% | |
| Other | 14.8% | |
Remembered As levels correlated with actual As levels measured by Columbia University r=.664, p<.001; Actual measurement distribution was 78.4% 10–50 μg/L, 15.3% 51–100 μg/L, and 6.3% >100 μg/L
e.g. carrying water from another source, mixing 50/50 bottled water, or drilled new well
This question was not answered exclusively by those who took no As action. Some respondents chose to select a reason why they took alternative action – such as switching to drinking bottled water or other, as opposed to installing a water treatment system for arsenic. For responses from only those who took no mitigation action at all, see Table 4.
POU = Point of use; POE = Point of entry
The majority of households not taking any mitigation action are at the lower levels of exposure (10–50 μg/L) (Table 3) and their most common reason was not being concerned about the As level, though the expense of treatment was a close second (Table 4). Households not concerned about As were significantly more likely to report that they “never” used the brochure that came with the well test as a source of information on As (41% vs. 20%, p<.05). Forty percent of those not taking any action could not remember what their test results were, a higher rate of forgetfulness than among those who did take action but not significant (p>0.05). Several households also report being advised by the private sector that their low levels of As were safe enough and not worth the expense of treating. Of the 45 households with As concentrations >50 μg/L, only 7 (15.6%) did not take any action. With these few cases at the higher levels of exposure the reasons are expense, lack of motivation or misinformation. Taking action is significantly associated with actual well water As level (rs=.264, p<.001).
Table 3.
All self-reported actions taken, by Columbia-Measured As level (n=256)
| As Measured by Columbia | |||
|---|---|---|---|
| Action | 10–50 ug/L (N=201) n (%) |
51–100 ug/L (N=39) n (%) |
>100 ug/L (N=16) n (%) |
| Installed POE System | 11 (5.5%) | 7 (18%) | 3 (19%) |
| Installed POU System | 65 (32.3%) | 20 (51%) | 5 (31%) |
| Switched to Bottled | 63 (31.3%) | 7 (17.9%) | 6 (38%) |
| Other Mitigation Action | 11 (5.5%) | 3 (7,7%) | 1 (4%) |
| No Action Taken | 63 (31.3%) | 4 (10.3 %) | 2 (13%) |
Percentages add up to more than 100% because some respondents reported taking several actions, i.e. installing a system and switching to bottled water, in response to arsenic.
N, n, number of samples
Table 4.
Reasons for Lack of Action among those who did not act on As test results (n=69)
| As Measured by Columbia | |||
|---|---|---|---|
| Reason | 10–50 ug/L (n=37) | 51–100 ug/L (n=5) | >100 ug/L (n=2) |
| Not concerned about As | 26 | 1 | 0 |
| Treatment too Expensive | 20 | 2 | 0 |
| Didn’t Know What to Do | 6 | 0 | 0 |
| Didn’t Know Who to Contact | 3 | 0 | 0 |
| Other | 18 | 1a | 2b |
”Neighbors in this area have lived to an old age without any problems;”
”The danger was overstated;” “Testing stated water was ‘safe for consumption.’”
There are no significant associations between age or years in home with not taking any mitigation action (Table 5); among mitigation behaviors, use of a treatment system is associated with higher education and income whereas avoiding the well water for drinking (i.e. drinking purchased bottled water) is associated with lower education and income (Table 5).
Table 5.
Associations (rs) between demographic variables and mitigation behaviors
| Descriptive | No Action Taken | Use of Treatment System | Avoid Drinking from Well |
|---|---|---|---|
| Years in Home | .035 | −.079 | −.069 |
| Age | .055 | −.045 | −.066 |
| Education | −.008 | .157* | −.184** |
| Income | −.116 | .200** | −.165* |
Significant to the .05 level;
Significant to the .01 level
3.1.3. Behavior Influencing Factors
The mean RANAS factor response scores for the full survey sample are organized into their respective categories in Table 6. Respondents indicated their level of agreement by selecting from 1 (Strongly Disagree) to 6 (Strongly Agree), so that a mean response >3.5 suggests general agreement and <3.5 suggests general disagreement in the population. Overall there is general awareness and agreement in the risks of As-contaminated water. Respondents agree that reducing As in water is better for health (M=4.6) and home values (M=4.5) but they disagree that it is inexpensive (M=2.6) or does not require a lot of effort (M=3.4). Those not using any household treatment system believe more strongly that it costs a lot of money to treat for As than those that do. Since use of a treatment system is significantly associated with income, it makes sense that it is less relatively expensive for those with higher incomes that are treating. Norms are mixed, the surveyed households on a whole slightly agree that their neighbors are treating water (M=4.0), but disagree that their relatives are (M=2.6), although their relatives may not be living in As affected areas. When looking at only households already treating their water they are more likely to agree that both their neighbors and relatives are also treating. Injunctive norms specifically (behaviors typically approved or disapproved of by others, including recognized authorities) are low (M=2.0), and the majority of households disagree that local authorities have advised them to treat their well water (M=2.4). Half of households believe that it is difficult to compare the pros and cons of As mitigation methods.
Table 6.
Means (M) and Standard Deviations (SD) of RANAS Variables (n=256), and Associations (rs) and Summary of Binary Logistic Regression Analysisa (n=155) for RANAS Variables Predicting the Behavior of Mitigating (Treating with Reverse Osmosis/Adsorbent Media Systems or rarely/never drinking well water)
| Variable (1 = Strongly Disagree; 6 = Strongly Agree) | Mb | SD | rs | OR | 95% CI of OR | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| I. Risk | ||||||
| a. Vulnerability | ||||||
| Household is at risk of drinking arsenic-contaminated water | 4.6 | 1.6 | .22** | 0.81 | 0.48 | 1.37 |
| My untreated water is not safe to drink | 4.4 | 1.7 | .59** | 3.52** | 1.99 | 6.23 |
| b. Severity | ||||||
| Arsenic-contaminated water is serious problem for household | 4.0 | 1.8 | .28** | 1.57 | 0.85 | 2.89 |
| Arsenic-related health effects from our well water likely serious | 4.1 | 1.7 | .24** | 1.23 | 0.74 | 2.07 |
| Health risks from arsenic exposure not overblown | 4.5 | 1.5 | .20** | 1.44 | 0.91 | 2.27 |
| c. Knowledge | ||||||
| Households in area often have arsenic-contaminated well water | 5.2 | 1.1 | .15* | 1.07 | 0.61 | 1.86 |
| Household members are exposed to arsenic from our untreated well water | 4.8 | 1.5 | .29** | 1.02 | 0.55 | 1.89 |
| Number of years using our untreated well water increases risks | 4.6 | 1.5 | .26** | 0.60 | 0.30 | 1.20 |
| Well arsenic level can change over time | 4.1 | 1.5 | −.08 | 0.88 | 0.60 | 1.27 |
| II. Attitude | ||||||
| a. Instrumental | ||||||
| Drinking less of untreated water is better for health | 4.6 | 1.7 | .23** | 0.92 | 0.62 | 1.37 |
| Our well arsenic level (untreated) decreases property value | 4.2 | 1.6 | .22** | 0.70 | 0.45 | 1.11 |
| Reducing drinking water arsenic would increase home value | 4.5 | 1.5 | .29** | 2.02** | 1.24 | 3.30 |
| Does not take a lot of effort to decrease arsenic exposure | 3.4 | 1.5 | −.03 | 1.14 | 0.71 | 1.83 |
| Does not cost a lot of money to decrease arsenic exposure | 2.6 | 1.6 | −.07 | 0.63 | 0.38 | 1.06 |
| b. Affective | ||||||
| Feel concerned about arsenic well level | 4.4 | 1.5 | .25** | 0.68 | 0.38 | 1.21 |
| Feel worried about arsenic well level | 3.6 | 1.8 | .15* | 0.62* | 0.40 | 0.95 |
| Concerned about water despite drinking long time with no problem | 4.5 | 1.7 | .26** | 0.78 | 0.51 | 1.18 |
| Do not like my untreated well water (e.g. taste, smell, looks) | 3.2 | 2.0 | .32** | 0.99 | 0.75 | 1.30 |
| III. Norms | ||||||
| a. Descriptive | ||||||
| Neighbors treat well water | 4.0 | 1.5 | .21** | 0.94 | 0.62 | 1.43 |
| Relatives treat well water | 2.6 | 1.7 | .08 | 1.21 | 0.85 | 1.71 |
| b. Injunctive | ||||||
| Neighbors expect me to treat well water | 2.0 | 1.4 | .22** | 1.38 | 0.88 | 2.16 |
| Local authorities advised not to drink well water untreated | 2.4 | 1.8 | .25** | 1.23 | 0.89 | 1.71 |
| IV. Ability | ||||||
| a. Action Knowledge | ||||||
| Know how to find company to install water treatment system for arsenic | 4.8 | 1.7 | .11 | 0.97 | 0.66 | 1.43 |
| b. Self-efficacy | ||||||
| Easy to compare pros and cons of arsenic control methods | 3.7 | 1.6 | .14* | 1.47 | 0.99 | 2.19 |
| Confident can maintain treatment system, even if additional costs | 4.6 | 1.6 | .14* | 0.93 | 0.59 | 1.47 |
| Something can be done about arsenic level in water | 5.1 | 1.3 | .06 | 1.01 | 0.63 | 1.61 |
| V. Self-regulation | ||||||
| a. Commitment | ||||||
| Committed to decreasing our arsenic exposure | 4.5 | 1.6 | .34** | 0.96 | 0.56 | 1.63 |
p<.05;
p<.01;
Nagelkerke R Square = .589; Overall predictive rate of 83.2%
<3.5 means disagreement on average, >3.5 means average agreement
OR = Odds Ratio, CI = Confidence Interval
In addition to describing the opinions of the participants these factors were analyzed for their influence on specific behaviors, comparing the responses of those performing or not performing the behavior. Overall 21 out of 27 factors in the questionnaire were significantly associated with the behavior of mitigating As exposure – i.e. either currently treating their water with a reverse osmosis or adsorbent media system or reporting that they rarely or never drink from their well. When these variables are all entered into binary logistic regression analysis, 3 are identified as significant predictors of the behavior. Belief that the untreated water is not safe to drink (risk) (OR = 3.52) and that reducing drinking water As would increase home value (instrumental attitude) (OR = 2.02) significantly predicted the behavior of mitigating As. Feeling worried about the As level (affective attitude) actually decreases the odds of mitigating As exposure (OR = 0.62). When looking at the behavior of using a treatment system alone, not combined with other mitigation behaviors such as drinking bottled water, confidence that one can maintain a treatment system, even if there are additional costs (self-efficacy), also becomes a significant predictor. Seventy percent of respondents who indicated their treatment systems in use were intended to remove arsenic report that they perform routine maintenance on their treatment system “as recommended.”
3.2. Treatment Assessment
Treatment failure is a risk, based on comparison of untreated and treated well water samples tested on site by ITS As test kit during the study of 68 households with self-reported POE or POU treatment systems for As in place. The overall failure rate for the 68 treatment systems was nearly 15% (Table 7). Ten systems were failing to remove As to below the MCL; breaking down the performance of treatment systems by As level there appears to be a higher risk of failure when untreated As levels are higher (>50 μg/L), although the number of households in this sample is too low to detect statistical significance. These households had taken action themselves to treat for As in response to receiving test results, and observations during household visits revealed a variety of locally available water treatment products in use, some commonly recognized as capable of removing As such as through reverse osmosis or iron oxide adsorbent media, while others who reported treating for As in fact only had a common sediment filter or water softener in place. From these brief visits it was not possible to determine the cause for each system’s failure, possible explanations could include use of inappropriate systems, homeowner maintenance behavior, or water chemistry interference with removal efficacy.
Table 7.
2013 test kit results from 68 central Maine households (HHs) treating their well water for Arsenic
| Untreated Water As Level | # of HHs Treating | # of HHs with treated water As >10 μg/L | Failure Rate |
|---|---|---|---|
| >10–50 μg/L | 36 | 4 | 11.1% |
| >50–100 μg/L | 29 | 5 | 17.2% |
| >100 μg/L | 3 | 1 | 33.3% |
| All >10 μg/L | 68 | 10 | 14.7% |
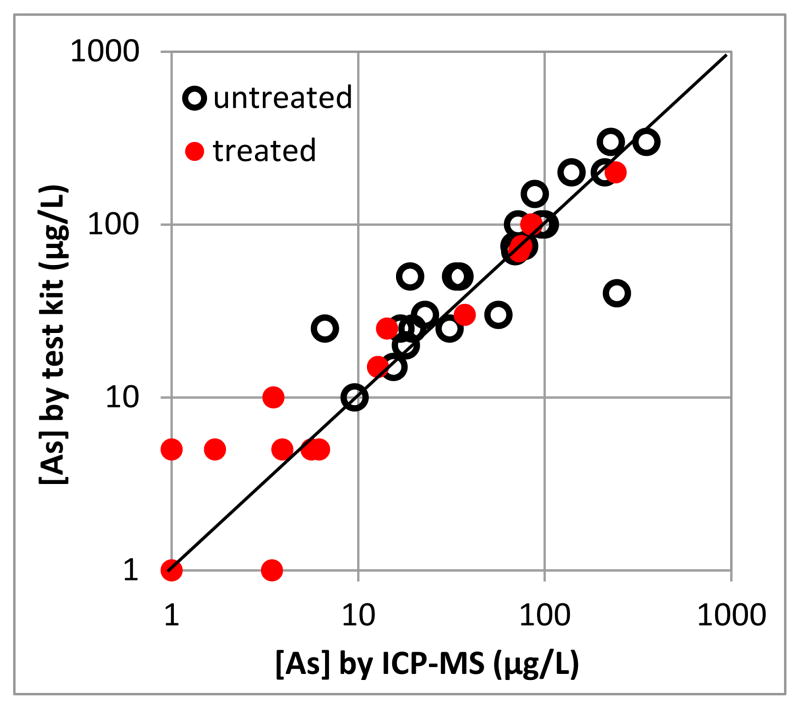
Treated and untreated water samples were collected from 25 households during the visits or As testing by ICP-MS at Columbia University. Comparing the 50 As measurements from these households obtained by kit testing to the those from ICP-MS finds that they are in agreement (Figure 2). Importantly, there is not a single false negative for <10 μg/L (n=17) by kit testing, confirming previous evaluations of performance of the same test kit (George et al., 2012; Steinmaus et al., 2006). There is only one false positive for the ≥10 μg/L (n=33) category, with a water sample of 7 μg/L As based on ICP-MS yielding 25 μg/L As by kit.
Figure 2.
Comparison of 2013 test kit and ICP-MS Arsenic measurements (n=50) for treated and untreated well water samples
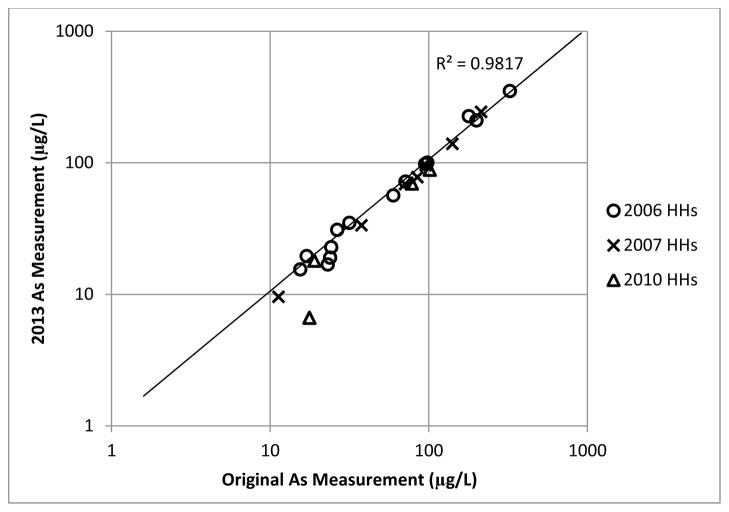
The households participating in this treatment assessment had their untreated well water first tested for As during our earlier testing program in the area during 2006–2010. Retesting these 25 household samples for As by ICP-MS in 2013 gave us the opportunity to compare domestic well As measurements over time. Figure 3 shows that there is a strong correlation (r2=0.98) between the ICP-MS measurements taken in 2006 (n=14), 2007 (n=7), and 2010 (n=4) and their repeat measurements taken in 2013, despite being drawn from bedrock wells with different geology (Figure 1).
Figure 3.
Comparison of original ICP-MS Arsenic measurements (2006–2010) to 2013 measurements for untreated well water samples of selected households (HHs) (n=25)
4. Discussion
Based on self-reporting by survey respondents, the water quality testing program and dissemination of As test results did motivate 73% of participating households to take some kind of action to reduce As exposure, a significant achievement. That taking action was associated with increasing As levels among this surveyed population is also encouraging, since there is a known dose response to the adverse health effects of chronic As exposure and those drinking higher concentrations are at higher risk.
The association of taking action to reduce As exposure with increasing As levels also confirms risk can be a motivator for protective action. And indeed the RANAS analysis identified perceived personal risk (“my untreated water is not safe”) as one of the three most significant predictors of mitigation behavior. Additionally the belief that treatment can improve home value is a significant predictor that homeowners take action and install a system for removing As. Yet the separate treatment system assessment finds that high As in water is in turn a risk for treatment failure; clearly, getting a homeowner to treat their well water will not guarantee to reduce the exposure to below the MCL despite of reduction of exposure in most cases. More needs to be understood about the treatment systems, the private market providing service to homeowners and the performance of As removal systems in real world conditions.
The mailed survey population was a convenience sample of previous well testing volunteers, which is a limitation in the generalizability of findings. But similar to other studies observing reluctance to act on test results, this survey found that nearly a third of homeowners did not take any protective action when notified that their well water contained As above recommended levels. Forty percent of these households do not remember their As test result (not significantly different from those taking action) but the majority not taking action also did have lower levels of As in their water (<50 μg/L) and their reasons for not taking action seem to be a combination of low risk perception and an unfavorable cost-benefit ratio. Yet half of the households not taking action that cited treatment as being too expensive reported annual household income of >$60,000, above the median income in the population of $42k. It is not clear whether these households went so far as to compare quotes for treatment systems and so are speaking to a known real cost, or whether it is a perceived cost of treatment that may be influenced in turn by perceived risk. More than 20% of total respondents still believe that As levels above 10 μg/L, the current MCL, and less than 50 μg/L, the MCL before 2001, are safe, and comments by survey participants indicate that this belief is being perpetuated by local private authorities like plumbers, well drillers, and treatment specialists. Although government officials were the most common first choice when survey respondents were asked who they would contact for information to help them manage the safety and quality of their well water, private company representatives were a very close second and so have influence in the community.
Among those taking action to reduce As exposure, use of a treatment system was associated with higher income and higher education whereas drinking bottled water was associated with lower income and lower education. Similarly the recent Columbia SRP study on schoolchildren in central Maine which interviewed mothers during home visits found that those who had not completed college were significantly more likely to report that the family relied on bottled water as an alternative source of drinking water. Also mothers with a college degree or higher were significantly more likely to report that their home included either a water filtration or treatment system (Wasserman et al., in revision). So there seems to be a connection between education/income and method of As mitigation. Among our respondents income was significantly and negatively associated with belief that “it costs a lot of money to reduce As exposure.” Although our study found a negative association between income and reliance on purchased bottled water, meaning that those with lower income are more likely to drink bottled water when mitigating than a install treatment system, treatment is more cost-effective for As reduction than purchased water for households greater than one person (Sargent-Michaud et al., 2006). Households with lower income that rely on bottled water are actually spending more money annually than those installing treatment systems when looked at over the lifespan of the system. But installation of an As treatment system requires a large capital investment at the front-end (up to several thousands of dollars) that may be prohibitive for lower-income families. On the other hand, use of bottled water for drinking does relieve the pressures and additional costs of vigilant monitoring and maintenance of water quality produced by treatment systems and so may be a decision not based entirely on costs. The survey found that use of a treatment system, as opposed to drinking bottled water, is predicted by confidence that one can maintain that system, so the need for maintenance may be another prohibitive factor in favor of purchasing water.
In our experience working with this community, the concept of treating water is not entirely alien to Maine well owners; our community survey in early 2013 found the majority (57%) does in fact treat their water in some way prior to drinking, the most common methods being sediment filters (25%), pitcher or refrigerator filters (20%), and water softeners (15%). Our observations in follow-up visits to households with As >10 μg/L that did not install As-specific treatment systems revealed that many still had these other types of water treatment in place. Although treatment of well water is common, treating for an invisible and tasteless contaminant like As, however, may be facing additional barriers to adoption related to the risk perceptions of owners and their perceived value of the costs involved. Although it may cost more in the long-run, the households not treating for As but choosing to purchase bottled water for drinking instead are still taking action to reduce their As exposure, which can be considered an arsenic mitigation success.
Also worth noting is that the survey found those who feel more worried about their As well level are less likely to be mitigating their As exposure. This is possibly because those that are already treating their drinking water to reduce As exposure therefore feel less worried about the As in their well. But considering the real risk of household treatment system failure observed, there is a danger that the reassurance home owners feel by the act of installing a treatment system may lead to poor maintenance and monitoring behaviors that could contribute to failure and persistent exposure. Careful messaging is needed to empower homeowners to take action and reduce their As exposure through treatment, without promoting overconfidence in guaranteed success. Observation during our home visits revealed that several households who believed they were treating for As actually were using systems that may not even be capable of removing As, whether these systems were installed by homeowner error or under advice from local treatment companies is unknown. Even when treatment systems use recognized As-removal technologies there is still a lack of understanding about how household As removal systems work under real conditions. Treatment systems developed and evaluated in lab settings perform as expected only if they are installed and maintained correctly and if there is no interference from the other chemical constituents in water. These systems are likely to perform differently when groundwater chemistry and homeowner behavior are involved, as demonstrated by the high failure rate in our treatment assessment. For public health officials to provide well owners with the best advice for reducing As exposure from well water, it is necessary to evaluate further the performance of these As treatment systems in the real world.
5. Conclusion
Public water systems in the U.S. are held to the standards of the Safe Drinking Water Act, but for the 15% of Americans served by private wells, their drinking water is unregulated. The well owner must take responsibility to ensure the safety of the water first by regularly testing for a variety of chemical substrates and biological agents and second by treating the water as appropriate, bearing the full costs along the way. Considering the risk of treatment failure, there must necessarily be a third step of regularly monitoring any treatment systems in use. But even in areas of frequent As occurrence, regular testing behaviors, especially for As, are inadequate (see Flanagan et al., this issue). This study found that even if the initial barriers of testing are removed and homeowners are directly provided with water quality results, a portion of households, nearly one third in this rural central Maine group, still do not take action to reduce their As exposures. Among households that have taken action by installing a treatment system, there is still a risk they will unknowingly remain exposed unless they vigilantly monitor the quality of the water produced.
This all demonstrates the need for a stage-wise approach to As mitigation. We have identified the necessary steps toward exposure mitigation – test, treat (or avoid), and regularly monitor treatment; motivating home owners through these steps will require different interventions and approaches at each step because there are different barriers and behavioral factors involved. Well owners clearly need more support and guidance to navigate this path if As exposure is to be reduced significantly at the population level.
Supplementary Material
Highlights.
Wells serving <25 people are not regulated by the US Safe Drinking Water Act
30% of well owners in the Central Maine study did not act on arsenic test results
Perceived risk is the strongest predictor of protective behavior
Belief that reducing arsenic would increase home value also predicted mitigation
Lack of concern about arsenic and costs are barriers for protective behavior
Acknowledgments
This research is funded by the U.S. National Institute of Environmental Health Sciences Superfund Research Program 3 P42 ES10349 to Y. Zheng. We thank A. Smith and colleagues of Maine Center for Disease Control and Prevention and J. Inauen of University of Zurich for helpful discussions. Thanks also to the staff of Maine Geological Survey for assistance in survey implementation. This is LDEO contribution #####.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ayotte JD, Montgomery DL, Flanagan SM, Robinson KW. Arsenic in groundwater in eastern New England: Occurrence, controls, and human health implications. Environ Sci Technol. 2003;37:2075–2083. doi: 10.1021/es026211g. [DOI] [PubMed] [Google Scholar]
- Dauphiné DC, Ferreccio C, Guntur S, Yuan Y, Hammond S, Balmes J, et al. Lung function in adults following in utero and childhood exposure to arsenic in drinking water: preliminary findings. Int Arch Occup Environ Health. 2011;84:591–600. doi: 10.1007/s00420-010-0591-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CM, Zheng Y, Graziano JH, Rasul SB, Hossain Z, Mey JL, van Geen A. Evaluation of an Arsenic Test Kit for Rapid Well Screening in Bangladesh. Environmental Science & Technology. 2012;46:11213–11219. doi: 10.1021/es300253p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber AC, Bhend S, Mosler HJ. Determinants of exclusive consumption of fluoride-free water: A cross-sectional household study in rural Ethiopia. Journal of Public Health. 2012;20:269–278. [Google Scholar]
- Huston SS, Barber NL, Kenney JF, Linsey KS, Lumia DS, Maupin MA. Circular. Vol. 1268. United States Geological Survey; 2004. Estimated use of water in the United States in 2000. [Google Scholar]
- Inauen J, Mosler H-J. Developing and testing theory-based and evidence-based interventions to promote switching to arsenic-safe wells in Bangladesh. Journal of Health Psychology. 2013 doi: 10.1177/1359105313493811. Advance Online Publication. [DOI] [PubMed] [Google Scholar]
- Inauen J, Tobias R, Mosler HJ. Predicting water consumption habits for seven arsenic-safe water options in Bangladesh. BMC Public Health. 2013;13(1):417. doi: 10.1186/1471-2458-13-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas PJ, Cabral C, Colford JM., Jr Dissemination of drinking water contamination data to consumers: A systematic review of impact on consumer behaviors. PLoS ONE. 2011;6(6):e21098. doi: 10.1371/journal.pone.0021098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madajewicz M, Pfaff A, van Geen A, Graziano J, Hussein I, Momotaj H, Sylvi R, Ahsan H. Can information alone change behavior? Response to arsenic contamination of groundwater in Bangladesh. Journal of Development Economics. 2007;84:731–754. [Google Scholar]
- Mosler HJ. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. International Journal of Environmental Health Research. 2012;22(5):431–449. doi: 10.1080/09603123.2011.650156. [DOI] [PubMed] [Google Scholar]
- Nielsen MG, Lombard PJ, Schalk LF. US Geological Survey Scientific Investigations Report 2010–5199. 2010. Assessment of arsenic concentrations in domestic wells by town in Maine 2005–2009. [Google Scholar]
- Poe GL, van Es HM, VandenBerg TP, Bishop RC. Do participants in well testing programs update their exposure and health risk perceptions? Journal of Soil and Water Conservation. 1998;53(4):320–325. [Google Scholar]
- Radtke T, Scholz U, Keller R, Hornung R. Smoking is ok as long as I eat healthily: Compensatory health beliefs and their role for intentions and smoking within the health action process approach. Psychology & Health. 2012;27(sup2):91–107. doi: 10.1080/08870446.2011.603422. [DOI] [PubMed] [Google Scholar]
- Rudnick RL, Gao S. Composition of the Continental Crust. In: Holland Heinrich D, Turekian Karl K, Rudnick RL., editors. The Crust, in Treatise On Geochemistry. Vol. 3. Oxford; 2003. [Google Scholar]
- Sargent-Michaud J, Boyle KJ, Smith AE. Cost effective arsenic reductions in private well water in Maine. Journal of the American Water Resources Association. 2006;42(5):1237–1245. [Google Scholar]
- Severtson DJ, Baumann LC, Brown RL. Applying a health behavior theory to explore the influence of information and experience on arsenic risk representations, policy beliefs, and protective behavior. Risk Analysis. 2006;26(2):353–368. doi: 10.1111/j.1539-6924.2006.00737.x. [DOI] [PubMed] [Google Scholar]
- Shaw WD, Walker M, Benson M. Treating and drinking well water in the presence of health risks from arsenic contamination: Results from a U.S. hot spot. Risk Analysis. 2005;25(6):1531–1543. doi: 10.1111/j.1539-6924.2005.00698.x. [DOI] [PubMed] [Google Scholar]
- Smith AH, Marshall G, Yuan Y, Fereccio C, Liaw J, von Ehrenstein O, et al. Increased mortality from lung cancer and bronchiectasis in young adults after exposure to arsenic in utero and in early childhood. Environ Health Perspect. 2006;114:1293–6. doi: 10.1289/ehp.8832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmaus CM, George CM, Kalman DA, Smith AH. Evaluation of two new arsenic field test kits capable of detecting arsenic water concentrations close to 10 ug/L. Environmenal Science and Technology. 2006;40:3362–3366. doi: 10.1021/es060015i. [DOI] [PubMed] [Google Scholar]
- Tobias R, Berg M. Sustainable use of arsenic-removing sand filters in Vietnam: Psychological and social factors. Environmental Science & Technology. 2011;45(8):3260–3267. doi: 10.1021/es102076x. [DOI] [PubMed] [Google Scholar]
- United States Bureau of the Census. Census of Housing, Detailed Housing Characteristics, Maine, CH-2-21. U.S. Department of Commerce; Washington, DC: 1990. [Google Scholar]
- United States Environmental Protection Agency (USEPA) Fiscal Year 2011: Drinking Water and Ground Water Statistics, Office of Water (4606M) EPA 816-R-13-003. 2013 Retrieved June 2013 from < http://water.epa.gov/scitech/datait/databases/drink/sdwisfed/upload/epa816r13003.pdf>.
- United States Environmental Protection Agency (USEPA) National Primary Drinking Water Regulations; Arsenic and Clarifications to Compliance and New source Contaminants Monitoring. 2001 Retrieved June 2013 from < http://www.epa.gov/fedrgstr/EPA-WATER/2001/January/Day-22/w1668.htm>.
- United States Environmental Protection Agency (USEPA) Arsenic in Drinking Water Rule: Economic Analysis, EPA document 815-R-00-026. Washington, DC: 2000. [Google Scholar]
- Walker M, Seiler RL, Meinert M. Effectiveness of household reverse-osmosis systems in a Western U.S. region with high arsenic in groundwater. Science of the Total Environment. 2008;389:245–252. doi: 10.1016/j.scitotenv.2007.08.061. [DOI] [PubMed] [Google Scholar]
- Wasserman GA, Liu X, LoIacono N, Kline J, Factor-Litvak P, van Geen A, Mey JL, Levy D, Abramson R, Schwartz A, Graziano JH. Exposure to arsenic from household wells and intelligence, in Maine schoolchildren. Environmental Health. doi: 10.1186/1476-069X-13-23. in review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q, Jung HB, Culbertson CW, Marvinney RG, Loiselle MC, Locke DB, Cheek H, Thibodeau H, Zheng Y. Spatial Pattern of Groundwater Arsenic Occurrence and Association with Bedrock Geology in Greater Augusta. Maine: Environmental Science & Technology. 2009;43(8):2714–2719. doi: 10.1021/es803141m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q. Arsenic in fractured bedrock aquifers in Greater Augusta, Maine, USA, Earth and Environmental Sciences. City University of New York; New York: 2010. [Google Scholar]
- Yuan Y, Marshall G, Ferreccio C, Steinmaus C, Liaw J, Bates M, et al. Kidney cancer mortality: fifty-year latency patterns related to arsenic exposure. Epidemiology. 2010;21:103–8. doi: 10.1097/EDE.0b013e3181c21e46. [DOI] [PubMed] [Google Scholar]
- Yuan Y, Marshall G, Ferreccio C, Steinmaus C, Selvin S. Acute myocardial infarction mortality in comparison with lung and bladder cancer mortality in arsenic-exposed region II of Chile from 1950 to 2000. Am J Epidemiol. 2007;166:1381–91. doi: 10.1093/aje/kwm238. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.