Abstract
Hemophilic pseudotumor is a rare, but well-known, complication of hemophilia occurring in 1–2 % of individuals with a severe factor VIII or IX deficiency. The hemophilic pseudotumor is defined as an encapsulated hematoma that increases of volume progressively by episodes of recurrent hemorrhage; usually originate in soft tissues or in subperiosteal or intraosseous areas. Very seldom, patient with mild form of hemophilia present with intraosseous pseudotumor. This report describe an 11-year-old boy with mild factor IX deficiency (17 % of normal factor IX activity), who developed a pseudotumor of the femur.
Keywords: Hemophilia B, Intraosseous pseudotumour, Factor IX concentrates
Introduction
Pseudotumour is an uncommon but serious complication of both hemophilia A and B, which is characterized by low factor VIII and IX activity respectively. It occurs in 1–2 % of patients with severe hemophilia (factor activity: less than 1 % of normal). Hemophilic pseudotumour usually originates in soft tissues or in subperiosteal or intraosseous areas. Intraosseous pseudotumour occurs mostly in the pelvis and long bones of the lower extremities in adults with severe hemophilia, whereas hands and feet are more often affected in children [1, 2]. Its occurrence in patient with mild hemophilia (factor activity: more than 5 % of the normal) is rare. In Medline database search, it is seen that so far five such cases of intraosseous pseudotumor have been reported sporadically where all were associated with mild hemophilia A (Table 1) [3–7]. In this article, we report a rare case of a large pseudotumor of the proximal femur in an 11-year-old boy with mild form of hemophilia B. To the best of our knowledge, such a presentation was not described in the literature till now.
Table 1.
| Age (years) | Factor deficiency | Factor activity (%) | Bone involved | Year of publication | Author |
|---|---|---|---|---|---|
| 1 | VIII | 10 | Skull | 1993 | Horton et al. [3] |
| 50 | VIII | NA | Femur | 2005 | Buchowski et al. [4] |
| 21 | VIII | 19 | Cranium | 2006 | Conde et al. [5] |
| Boy | VIII | 14 | Maxilla | 2008 | Lima et al. [6] |
| NA | VIII | NA | Femur | 2004 | Li et al. [7] |
| 11 | IX | 17 | Femur | Current report | Purkait et al. |
NA not available
Case History
An 11-year-old boy with a four-month history of pain and swelling around the right hip joint and proximal thigh was referred to us for consultation. The pain was insidious in onset, dull-aching, localized to the proximal thigh, and aggravated by exertion and relieved by rest. The swelling was insidious in onset and gradually progressive. A past history of significant trauma following fall from height was present. None of the family members had coagulation disorders or similar illness in past. On examination, a large (18 × 15 cm), firm mass was found at the proximal portion of thigh over the anteromedial and anterolateral aspects (Fig. 1a). Movement of the hip joint was limited. There was no neurological deficit.
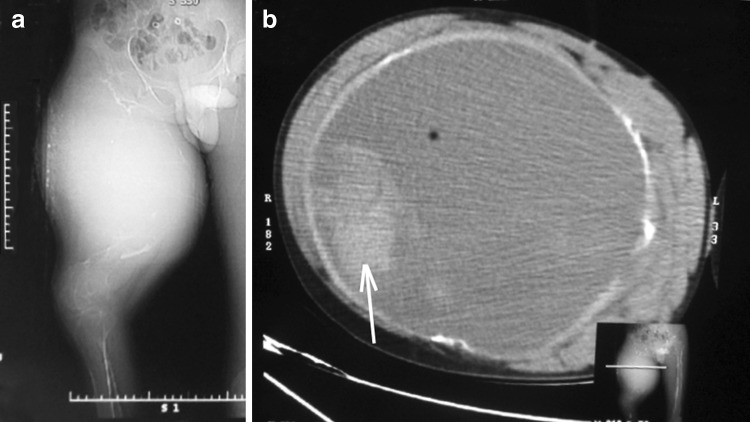
Fig. 1.
Noncontract axial CT scan showing a a large (18 × 15 cm) expansile swelling involving neck and proximal half of shaft of right femur and b heterogeneously hyperdense (blood density of varying degree) intraosseous lesion (arrow) with pressure effect, resulting cortical thinning of shaft of the femur
Complete hemogram showed hemoglobin 12.5 g/dl, MCV 85 fl, MCH 32 pg, MCHC 31 g/dl, total leucocyte count 21.5 × 103/µl with neutrophil 75 %, lymphocyte 21 %, eosinophil 2 % and monocyte 2 %; platelet count 235 × 103/µl. A noncontrast axial computed tomography (CT) scan was done, which showed heterogeneously hyperdense (blood density of varying degree) intraosseous lesion with pressure effect, resulting cortical thinning of shaft of the femur (Fig. 1b). A provisional diagnosis of intraosseous pseudotumour due to bleeding disorder was made and the child underwent further investigation regarding coagulation profile which were as follows: prothrombin time (PT): 12.3 s (control-11.8 s, INR-1.04), activated partial thromboplastin time (aPTT): 53 s (control-28.1 s). On mixing study, aPTT was corrected with normal plasma and aged serum with factor VIIIc assay: 82 % (ref. range 50–150 %) and factor IX assay: 17 % (ref. range 50–150 %). Based on the combination of history, coagulation study and characteristic imaging finding, the definite diagnosis of congenital mild hemophilia B with an intraosseous pseudotumour of the right proximal femur including hip joint was made. He was treated with plasma derived factor IX concentrate (Immunine, Baxter) with 1,200 units daily for day1 to day5 followed by 600 units daily for 6 weeks. In view of raised total leucocyte count, patient was treated with intravenous piperacilline-tazobactum three times a day for 7 days and stop after normalization of total leucocyte count. The patient’s swelling and pain started to regress by 10th day and subsided over the next 6 weeks. At 6 week, pelvis X-ray showed complete resolution of intraosseous lesion (Fig. 2). Currently child is doing well without recurrence of pseudotumour till date.
Fig. 2.

Follow up pelvis X-ray at 6 weeks showing complete resolution of intraosseous lesion
Discussion
Hemophilia is a bleeding disorder, inherited as X-linked recessive pattern affecting exclusively the males while females are carriers. The clinical presentations in both hemophilia A and hemophilia B are almost identical. Repeated bleeding with formation of hematomas and hemarthrosis are the most frequent musculoskeletal manifestations of the disease. The severity of the disease is classified on the basis of the patient’s baseline level of factor VIII or factor IX. Severe hemophilia is characterized by having less than 1.0 U/dL of the specific clotting factor, and bleeding is often spontaneous. Patients with moderate hemophilia have 1–5 U/dL and require mild trauma to induce bleeding. Individuals with mild hemophilia have levels greater than 5 U/dL, may go many years before the condition is diagnosed, and frequently require significant trauma to cause bleeding as evident in our case [8].
Pseudotumor is a rare, but well known complication of hemophilia, occurring in 1–2 % patients with severe hemophilia. It is essentially a chronic, slowly expanding encapsulated mass containing blood at different stages of degradation resulting from chronic and recurrent bleeding. Many patients recall sustaining an injury prior to the development of pseudotumor. When left untreated, such a mass may induce compression and pressure necrosis of adjacent structures [1, 9]. The exact pathogenesis of pseudotumor of bone is not well understood. Three probable mechanisms have been suggested including extension from a hemarthrosis under pressure, bleeding into adjacent soft tissue with secondary bone invasion or subperiosteal bleeding with cyst formation [2].
Invasive techniques such as, fine needle aspiration and biopsy are strongly contraindicated to diagnose hemophilic pseudotumor due to increased risk of complications like hemorrhage, infection and fistula formation. High quality CT scan and/or magnetic resonance imaging (MRI) is an excellent tool for preoperative visualization of the extent of the lesion, its mass effect on vital surrounding structures and possible invasion of joints. CT is also best suited for detection of intralesional calcifications, internal gas bubbles due to superinfection, cortical expansion and perforation, whereas MRI is superior to CT for delineating soft tissue and intramedullary spaces [2, 9].
Although treatment of hemophilia has undergone rapid development in the past decade, but at present hemophilic pseudotumor lacks standard management guidelines. Till now, the initial treatment is conservative with clotting factor replacement to keep an activity of 100 %. For patient with inhibitors, recombinant factor VIIa or prothrombin complex concentrates can be used. In general, operative removal of the entire mass is a reliable treatment because the pseudotumor likely will reform if it is not completely removed. Non-surgical mode of treatment in form of radiotherapy alone or combined with replacement therapy has shown promising results as an alternative to a more mutilating surgery or where surgery is contraindicated, or resistant to conservative treatment [9, 10].
Acknowledgments
Competing interest
None.
References
- 1.Mittal S, Arora S, Khanna S, Maini L, Gautam VK. An unusual presentation of hemophilia B: pseudotumor of proximal tibia. Am J Orthop (Belle Mead NJ) 2011;40:E138–E140. [PubMed] [Google Scholar]
- 2.Geyskens W, Vanhoenacker FM, Van der Zijden T, Peerlinck K. MR imaging of intra-osseous hemophilic pseudotumor: case report and review of the literature. JBR-BTR. 2004;87:289–293. [PubMed] [Google Scholar]
- 3.Horton DD, Pollay M, Wilson DA, Brandon FM, Sexauer CL. Cranial hemophilic pseudotumor. Case report. J Neurosurg. 1993;79:936–938. doi: 10.3171/jns.1993.79.6.0936. [DOI] [PubMed] [Google Scholar]
- 4.Buchowski JM, Cascio BM, Streiff MB, Frassica FJ. Resection and reconstruction of a massive femoral hemophilic pseudotumor. Clin Orthop Relat Res. 2005;430:237–242. doi: 10.1097/01.blo.0000137545.37824.b0. [DOI] [PubMed] [Google Scholar]
- 5.Conde F, Lazo E, Lourido J, Domínguez J. Cranial hemophilic pseudotumor. Neurocir (Astur) 2006;17:158–161. [PubMed] [Google Scholar]
- 6.Lima GS, Robaina TF, de Queiroz Chaves Lourenço S, Dias EP. Maxillary hemophilic pseudotumor in a patient with mild hemophilia A. J Pediatr Hematol Oncol. 2008;30:605–607. doi: 10.1097/MPH.0b013e3181758926. [DOI] [PubMed] [Google Scholar]
- 7.Li DJ, Zhang DH, Zhang YZ, Liu WL. Mild type of hemophilic pseudotumor with injury of femoral nerve (one case report) Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2004;12:531–532. [PubMed] [Google Scholar]
- 8.Scott JP, Montgomery RR (2012) Hereditary clotting factor deficiencies (bleeding disorder). In: Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE (eds) Nelson textbook of pediatrics, 19th edn. Saunders, Philadelphia, p 1699–1703
- 9.Purkait R, Mukherjee A, Naskar S, Bhadra R. Nasal hemophilic pseudotumor: favorable response to radiotherapy. Indian Pediatr. 2013;50:334–335. doi: 10.1007/s13312-013-0071-7. [DOI] [PubMed] [Google Scholar]
- 10.Rijal L, Neogi DS, Ansari MT, Khan SA, Yadav CS. Hemophilic pseudotumor–is there a role of radiotherapy? Literature review and a case report. Nepal Med Coll J. 2010;12:193–197. [PubMed] [Google Scholar]