Abstract
Breast cancer is the first in the incidence of malignancies among women. The documented frequency of osseous metastasis from breast cancer is about 12.8 %. Although breast cancer cells have been documented in the bone marrow in autopsy, haematological manifestations due to metastatic disease to the marrow is rare. The prognosis of these cases is dismal and improper management worsen the condition further. IHC for ER, PR & Her 2/neu status plays a vital role in ascertaining the treatment protocol both in primary tumors as well as metastatic or recurrent tumors. Receptor conversion has been documented in metastatic and recurrent cases. We report a case of 65 year female with a history of ER, PR positive and Her 2/neu negative carcinoma breast 3½ years back, presented with anemia and low back ache diagnosed as metastatic breast carcinoma to bone marrow with receptor conversion.
Electronic supplementary material
The online version of this article (doi:10.1007/s12288-014-0394-0) contains supplementary material, which is available to authorized users.
Keywords: Metastatic breast carcinoma, Immunohistochemistry, Receptor Conversion
Introduction
With 1,000,000 new cases causing 375,000 deaths worldwide per year, breast cancer is the leading cause of female cancer death worldwide [1]. Early detection, optimal surgery and hormone receptor status based adjuvant therapy are the key strategies to improve the survival. Nevertheless, about 1/3rd of patients will develop distant metastases. And distant metastasis is the cause of death in 90 % breast cancer patients [2]. Immunohistochemical evaluation of biological markers is the mainstay of in deciding the treatment protocol e.g. chemotherapy for high Ki-67 values, endocrine therapy for ER positive and Trastuzumab therapy for Her 2/neu positive tumors have been recommended [3].
Case Report
A 65 year old female patient was admitted to MKCG Medical College & Hospital with complains of low back pain & weakness for 6 months duration. She was of average socio-economic status. Significant past history includes a left side breast carcinoma operated 3½ years back in this institute. She was diagnosed as a case of IDC–NOS her receptor status by IHC was ER & PR positive and Her 2/neu negative. Routine hematological investigations revealed moderate normocytic anemia [Hb value 7.4 gms/dL], mildly elevated ESR of 30 mm in 1st hour, total leukocyte count was within normal limits [8.44 × 109/L] and differential count showed Myeloblast [1 %], Myelocyte [4 %], Metamyelocyte [9 %], Stab [6 %], Neutrophil [62 %], Eosinophil [2 %], Basophils [0 %], Lymphocyte [15 %], Monocyte [1 %] and Nucleated RBCs 35/100 WBCs [early, intermediate and late erythroblasts seen] suggestive of a leukoerythroblastic blood picture. No tear drop cells were noted in the peripheral smear to suggest a secondary myelofibrosis.
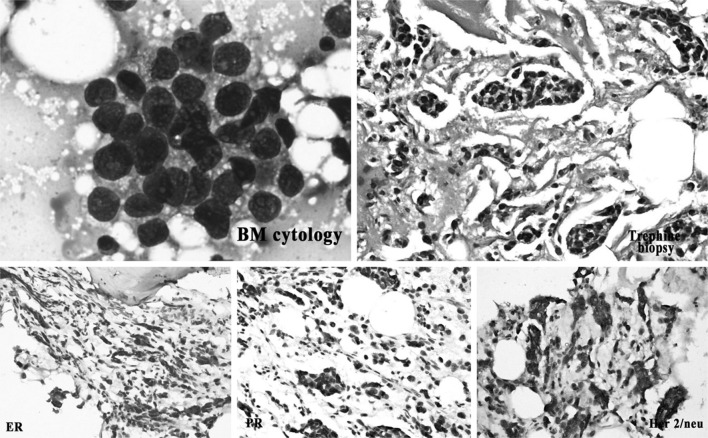
Both bone marrow aspiration cytology and trephine biopsy showed presence of pleomorphic tumor cells in acinar pattern, sheets and three dimensional clusters suggestive of adenocarcinomatous deposit with significant replacement of marrow elements. Trephine biopsy sections showed a strong desmoplastic response with increased reticulin fibres (Fig. 1).
Fig. 1.
Cytosmear show pleomorphic tumor cells forming acinar patterns, trephine biopsy section shows the tumor cells in sheets and cords in a desmoplastic stroma, IHC for ERœ, PR and Her 2/neu shows negativity for ERœ & PR and strong membrane positivity for Her 2/neu
A diligent search for primary tumor was made that included detailed clinical history, thorough clinical examination and other investigation modalities. No recurrent breast mass was found. All other investigation findings were essentially normal except (a) X-ray showed multiple osteolytic lesions in the L3, L4, L5 vertebrae and pelvic bones and (b) USG showed mild hepatomegaly with multiple hypoechoic lesions in the liver suggestive of Metastatic lesion.
Immunohistochemical staining was done on trephine biopsy tissue for breast markers which showed that the tumor cells are negative for ER & PR, Her-2/neu strong membrane positivity, p53 60 % positivity, MIB1 80 % positivity (Fig. 1).
Considering the present receptor status & bone metastasis, Trastuzumab along with Denosumab therapy was initiated. During the five months of follow up period after the initiation of therapy the quality of life of the patient has improved with significant reduction in bone pain and elevation of the Hemoglobin level to 10.2 Gms/dL from 7.4 Gms/dL at the time of diagnosis.
Discussion
The frequency of osseous metastasis from breast cancer is about 12.8 %, most commonly to vertebral body, pelvic bone & skull [4]. Aside from clinical symptoms, the diagnosis of osseous metastasis depends primarily on medical imaging. The specificity of X-ray in diagnosing osseous metastasis is 94.4 %, but the sensitivity is only 48.1 %. We cannot detect the destruction of bone by X-ray unless more than 50 % of the bone is involved. CT is more sensitive in the diagnosis of cortical bone metastasis than X-ray, but it is not sensitive in the diagnosis of bone marrow metastasis, especially when patients are elderly and suffer from osteoporosis and/or degeneration [5]. Since breast cancer frequently produces skeletal metastases, the bone marrow is an appropriate place to screen for micrometastatic cells.
Metastasis to marrow can have variable presentations like Microangiopathic haemolytic anemia, Uni-, bi- and pancytopenia, DIC and leukoerythroblastic blood picture [6]. The present case presented with a leukoerythroblastic blood picture.
Bone marrow metastasis detection is of high importance to stage the disease, in assessing the prognosis and in making the decision about adjuvant therapy [7]. In cases the treatment decision was based on the ER & Her 2/neu status of primary tumor, disease free survival, recurrence site & the performance status [8].
Recent studies have indicated that receptor status of breast cancer metastases may differ from the primary tumor, generally denoted “receptor conversion”. The published studies suggest that, compared to the primary tumors, ER & PR are more frequently negative in distant metastases, whereas Her-2/neu is more often positive [9]. In 10.7 % of patients, conversion from ER+ or PR+ to ER−/PR− and in 3.4 % from ER-/PR- to ER+ or PR+ was found and that for Her-2/neu was 5.2 % on both ways [10]. Nevertheless, when a biopsy of a distant metastasis is available, hormone receptor & Her-2/neu status should be reassessed in these biopsies & the tests results should be critically evaluated in conjunction with ER, PR and Her-2/neu status of the primary tumor [11]. Receptor conversion changes the treatment protocol in metastatic cases [11, 12].
In the present case detection of Her 2/neu positivity with ER & PR negativity helped in determining the chemotherapeutic drug of choice. At present, administration of effective anti-cancer drugs prolongs the survival time and quality of life [5].
Electronic supplementary material
Abbreviations
- IHC
Immunohistochemistry
- IDC–NOS
Infiltrating duct carcinoma not otherwise specified
- Hb
Hemoglobin
- ESR
Erythrocyte sedimentation rate
- RBC
Red blood corpuscles
- WBC
White blood corpuscles
- ER
Estrogen receptor α
- PR
Progesterone receptor
- Her 2/neu
Human epidermal growth factor receptor
- MIB 1
Mindbomb E3 ubiquitin protein ligase 1
- H&E
Hematoxylin and Eosin stain
- CT
Computerized tomography
- DIC
Disseminated intravascular coagulation
Contributor Information
T. Santosh, Email: born_vss@yahoo.co.in
M. K. Patro, Email: manojkpatro@gmail.com
References
- 1.Bray F, McCarron P. Parkin DM (2004): the changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004;6:229–239. doi: 10.1186/bcr932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bendre M, Gaddy D, Nicholas RW, Suva LJ. Breast cancer metastasis to bone: it is not all about PTHrP. Clin Orthop Relat Res. 2003;415(Supplement):S39–S45. doi: 10.1097/01.blo.0000093844.72468.f4. [DOI] [PubMed] [Google Scholar]
- 3.Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thürlimann B, Senn HJ. Panel members (2009): thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol. 2009;20(8):1319–1329. doi: 10.1093/annonc/mdp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Tao Z, Ling Z, Hui G, Peng C, Dong W. Total vertebral body breast cancer metastases: one case report and literature review. Clin Oncol Cancer Res. 2009;6:456–458. doi: 10.1007/s11805-009-0456-5. [DOI] [Google Scholar]
- 5.Taoka T, Mayr NA, Lee HJ, et al. Factors influencing visualization of vertebral metastases on MR imaging versus bone scintigraphy. AJR. 2001;176:1525–1530. doi: 10.2214/ajr.176.6.1761525. [DOI] [PubMed] [Google Scholar]
- 6.Ozkalemkas Fahir, Ali Rıdvan, Ozkocaman Vildan, Ozcelik Tulay, Ozan Ulku, Ozturk Hulya, Kurt Ender, Evrensel Turkkan, Tunali Ahmet. Omer Yerci (2005): the bone marrow aspirate and biopsy in the diagnosis of unsuspected nonhematologic malignancy: a clinical study of 19 cases. BMC Cancer. 2005;5:144. doi: 10.1186/1471-2407-5-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaur G, Basu S, Kaur P, Sood T. Metastatic Bone Marrow Tumors: study of nine cases and review of the literature. J Blood Disord Transfus. 2011;2:110. doi: 10.4172/2155-9864.1000110. [DOI] [Google Scholar]
- 8.Hortobagyi GN. Treatment of breast cancer. N Engl J Med. 1998;1998(339):974–984. doi: 10.1056/NEJM199810013391407. [DOI] [PubMed] [Google Scholar]
- 9.Lower EE, Glass EL, Bradley DA, Blau R, Heffelfinger S. Impact of metastatic estrogen receptor and progesterone receptor status on survival. Breast Cancer Res Treat. 2005;90:65–70. doi: 10.1007/s10549-004-2756-z. [DOI] [PubMed] [Google Scholar]
- 10.Hoefnagel, et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res. 2010;12:R75. doi: 10.1186/bcr2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lower EE, Glass E, Blau R. Harman S (2009): HER-2/neu expression in primary and metastatic breast cancer. Breast Cancer Res Treat. 2009;113:301–306. doi: 10.1007/s10549-008-9931-6. [DOI] [PubMed] [Google Scholar]
- 12.Holdaway IM. Bowditch JV (1983): variation in receptor status between primary and metastatic breast cancer. Cancer. 1983;52:479–485. doi: 10.1002/1097-0142(19830801)52:3<479::AID-CNCR2820520317>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.