Abstract
Plasma cell leukaemia is a rare and aggressive neoplasm with survival of less than one year with conventional treatment. It can rarely present with morphology mimicking hairy cell leukaemia. We present a case of plasma cell leukaemia with hairy cell morphology for its rarity, diagnostic difficulty and aggressive course.
Introduction
Plasma cell leukaemia is a rare and aggressive plasma cell dyscrasia characterized by malignant plasma cells in the bone marrow and peripheral blood. It is classified into two clinical types. The primary type occurs in individuals without being preceded by multiple myeloma, whereas the secondary type is a rare complication of the late-stage of multiple myeloma [1, 2].
Plasma cell leukaemia may present rarely with immature form of leukemic cells causing diagnostic difficulty. Plasma cell leukaemia with hairy cell morphology is a very rare presentation. There are few case reports in literature. This case is presented because of its rarity, diagnostic difficulty and poor outcome.
Case Report
A 61 year old man was referred to our centre with complaints of generalized weakness, anorexia, abdominal distension, and decreased urine output of 10 days duration. Physical examination was suggestive of pallor, grade II dyspnoea, facial puffiness, distended abdomen with shifting dullness and pedal oedema. There was no evidence of lymphadenopathy and organomegaly Vitals and rest of the systemic examination was normal.
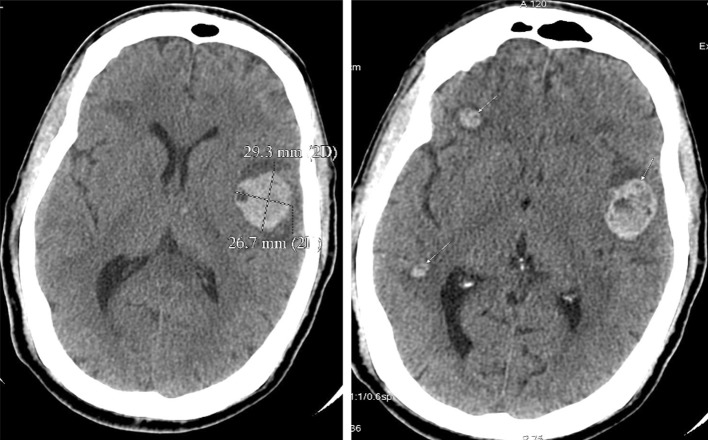
He had a haemoglobin concentration of 6.2 g/dl, white blood count of 31,900/μL, platelet count of 1,00,000/μL and a differential count of neutrophils 20 %, lymphocytes 9 % and atypical lymphoid cells 68 %. Peripheral blood smear revealed an increased number of leukocytes that consisted of a population of atypical appearing lymphoid cells. The size of the cells varied from 1.5 to 2.5 times the size of a small lymphocyte with circumferential hairy projections and round nuclei with 1–2 prominent nucleoli and deeply basophilic cytoplasm (Fig. 1).
Fig. 1.
Peripheral blood showing leukemic cells with hairy cell morphology
Red blood cells showed marked anisopoikilocytosis with microcytic hypochromic cells, macrocytes, target cells and echinocytes. Platelets: mild thrombocytopenia. Bone marrow aspiration and biopsy showed increased cellularity with prominence of atypical lymphoid cells accounting for 95 %. These cells were 1.5–2.5 times larger than small lymphocyte with large round to indented nuclei and scant cytoplasm.
Biochemical evaluation was suggestive of azotemia–blood urea: 114 mg/dl, serum creatinine: 11.8 mg/dl, serum electrolytes were normal and LDH:2203 IU/l.
Pending his flow cytometry, SPE, BJP, IF and because of diagnostic dilemma patient was supported with hemodialysis and blood products.
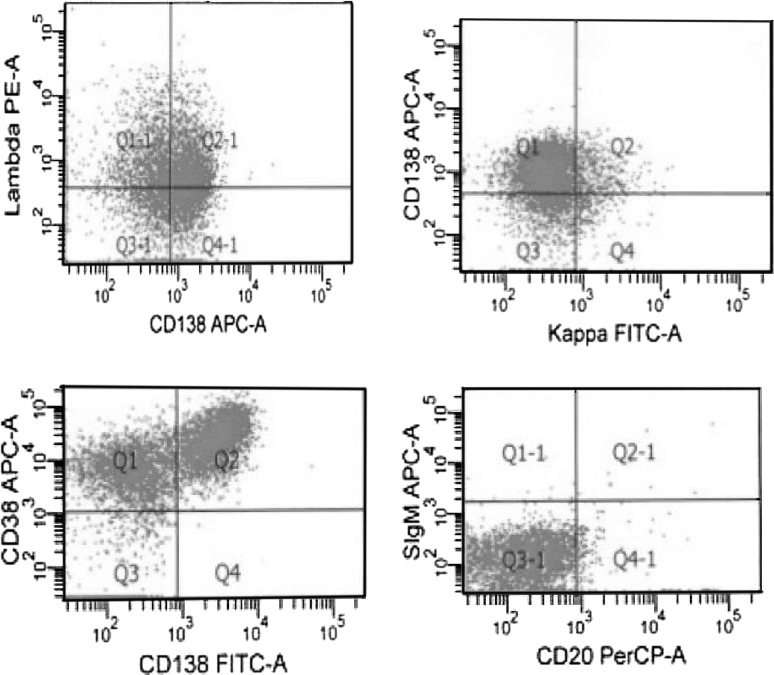
During the course of hospitalization he developed right sided hemiplegia. CT Scan of the brain showed multiple hemorrhages of varying sizes (Fig. 2).
Fig. 2.
Plain CT scan brain showing multiple haemorrhages
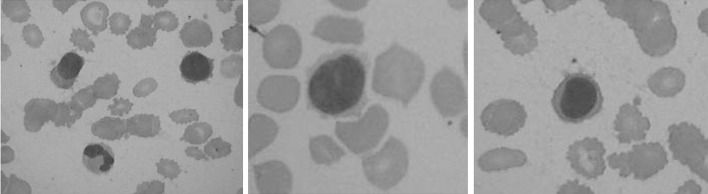
Flowcytometry showed strong positivity for CD38, CD138, Lambda and negative for CD19, CD25, CD23, CD103 (Fig. 3.)
Fig. 3.
Flowcytometry showing strong positivity for CD38, CD138
Serum protein electrophoresis, Immunofixation and urinary bence jones proteins were negative (Fig. 4). Skeletal survey was normal. He was started on bortezomib 1.3 mg/m2 on day 1, 4, 8, 11 and pulse dexamethasone 40 mg for 4 days a week. He developed right lower lobe pneumonia on day 15 with sepsis and MODS and succumbed on day 17 despite best efforts .
Fig. 4.
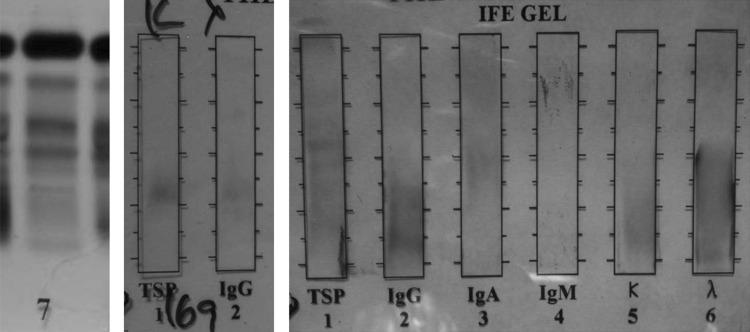
Serum electrophoresis, Immunofixation and urinary bence jones proteins negative
Discussion
Primary plasma cell leukaemia(PCL) is a rare and aggressive malignancy accounting for 0.3 % of all acute leukemias. Median survival is less than one year [3]. Plasma cell leukaemia with hairy cell morphology has been reported in some case reports earlier [4–6]. Tanioka et al. [6] published a case report of plasma cell leukaemia with hairy cell leukaemia morphology and immunohistochemical and molecular characteristics to delineate the immature stage of origin of the leukemic cells in comparison to more mature MM. Chan et al. [7] published a case report of plasma cell leukaemia with hairy cell morphology with good response to bortezomib based therapy(PAD).
Bortezomib is effective as single agent or in combination and approved for MM as first line or second line therapy in relapsed and refractory MM. Bortezomib based therapy has reversed the renal failure in MM with renal involvement [8]. There are no randomised studies till date in PCL on bortezomib based therapies, but there are several case reports showing the efficacy of Bortezomib based therapies in plasma cell leukaemia.
With this available data of bortezomib in PCL and MM with renal failure we started the patient on bortezomib and dexamethasone. On treatment the patient developed pneumonia with MODS and multiple intracranial haemorrhages and succumbed to his illness.
Misleading morphological features, absence of SPE, IF, BJP positivity and normal skeletal survey lead to the clinical dilemma and diagnostic delay. The aggressive course and lethal outcome on treatment supports the data on plasma cell leukaemia. Plasma cell leukaemia with hairy cell morphology should be considered in the differential diagnosis of hairy cell leukaemia with an aggressive course.
Contributor Information
Thota Narender Kumar, Email: narender9@gmail.com.
Kalpathi Krishnamani, Email: kkvkmani@gmail.com.
Linga Vijay Gandhi, Email: vijaygandhilinga@yahoo.com.
Gundeti Sadashivudu, Email: drssgundeti@yahoo.com.
Digumarti Raghunadharao, Email: rdigumarti@gmail.com.
References
- 1.Kosmo MA, Gale RP. Plasma cell leukemia. Semin Hematol. 1987;24:202–208. [PubMed] [Google Scholar]
- 2.Foucer K. Bone Marrow Pathology, vol 1. Chicago: ASCP Press; 1994. pp. 315–342. [Google Scholar]
- 3.Jimenez-Zepeda VH, Dominguez VJ. Plasma cell leukemia: a rare condition. Ann Hematol. 2006;85(4):263–267. doi: 10.1007/s00277-005-0054-4. [DOI] [PubMed] [Google Scholar]
- 4.Crogan TM, Spier CM. B-cell Immunoproliferative disorders, including multiple myeloma and amyloidosis. In: Knowles DM, editor. Neoplastic hematopathology. 2. Philadelphia: Lippincot Williams and Wilkins; 2001. pp. 1564–1565. [Google Scholar]
- 5.Loo SY, Bhagavan NV, Scottolini AG. Double IgA bands in serum from a patient with lymphoplasmacytoid leukemia with hairy-cell morphology. Clin Chem. 1987;33:2317–2319. [PubMed] [Google Scholar]
- 6.Tanioka F, Tamashima S, Shimizu S, Kobayashi H, Kobayashi Y, Sugimura H. A case of primary plasma cell leukemia with hairy-cell morphology and lambda-type Bence-Jones protein immunohistochemical and molecular analysis. Jpn J Clin Oncol. 2003;33:232–237. doi: 10.1093/jjco/hyg043. [DOI] [PubMed] [Google Scholar]
- 7.Chan SM, George T, Cherry AM, Medeiros BC. Complete remission of primary plasma cell leukemia with bortezomib, doxorubicin, and dexamethasone: a case report. Cases J. 2009;2(1):121. doi: 10.1186/1757-1626-2-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jagannath S, Barlogie B, Berenson JR, et al. Bortezomib in recurrent and/or refractory multiple myeloma. Initial clinical experience in patients with impaired renal function. Cancer. 2005;103(6):1195–1200. doi: 10.1002/cncr.20888. [DOI] [PubMed] [Google Scholar]